INFECTIVE ENDOCARDITIS Gao Xiuren Definition Infective endocarditis IE


- Slides: 38
INFECTIVE ENDOCARDITIS Gao Xiuren
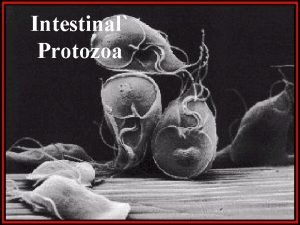
Definition Ø Infective endocarditis (IE) is a microbial infection of the endothelial surface of the heart. Ø The characteristic lesion, the vegetation, is a variably sized amorphous mass of platelets and fibrin in which abundant microorganisms and scant inflammatory cells are enmeshed.
Clinical classification Ø Native valve endocarditis Ø Prosthetic valve endocarditis Ø Introvenous drug abuser endocarditis
According to the course of disease it can be divided into acute IE and subacute IE
Acute IE presents with marked toxicity, progresses over days to several weeks to valvular destruction and metastatic infection. In contrast; sub-acute IE envolve over weeks to months with only modest toxicity and rarely causes metastatic infection, the infection of staphylococcus stand for about 25% in native valve IE and streptococcus stand for nearly 65% in native valve IE.
The acute IE mainly causes by staphylococcus aureu infection. Nevertheless; the sub-acute IE more likely causes by streptococcus, enterococcus or gram-negative coccobacilli.
Pathogenosis v. Basically heart disease (predisposing condition) For example: rheumatic heart disease, congenital heart disease, mitral valve prolapse, degenerative heart disease, intravenouse drug abuse mitral valve regurgitatiom aortic valve regurgitation fistula It seldom occurs in valve stenosis
v Development of nonbacterial thrombolic Endocarditis(NBET) Endothelial damage Three hemodynamic circustances may injure the endothelium initiating NBTE: a) high-velocity jet impacting endothelium b) flow from a high-to a low-pressure chamber c) flow across a narrow orifice at high velocity
v. White thrombosis The deposition of platelet-fibrin to shape the white thrombosis. The white thrombosis is more receptive to colonization by bacterial than intact endothelium
v Red thrombosis The adherence of microorganism to NBTE is a pivotal early event in the development of IE. Certain bacterial are advantage in there ability to colonize and infect NBTE. The red blood cells, white blood cells; platelet; and fibrin deposition to form the red thrombosis(vegetation).
The red thrombosis is easier to rupture and involve peripheral manifestation and result in hemotogenous seeding of remote sites. Antibody response to the infection organism with subsequent tissue injury, due to antibody and antigens complexes reaction.
Clinical feature Ø Incubation The incubation of infection in NVE is short (2 weeks) in contrast the incubation of infection in PVE is relatively longer, sometimes may reach to 2~5 months.
ØFever Nearly all patients have fever. In generally, the sub-acute IE has lower temperature (<39ºC) compare with the acute IE.

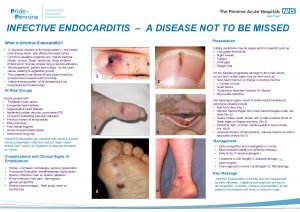
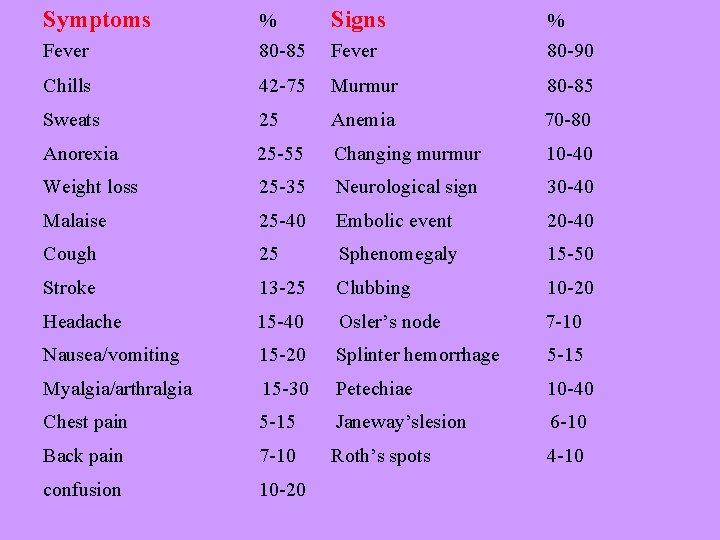
Ø Symptoms and signs: The symptoms come from toxicity and periphearal organs infarction. The signs include changing/new heart murmur and peripheral manifestation.
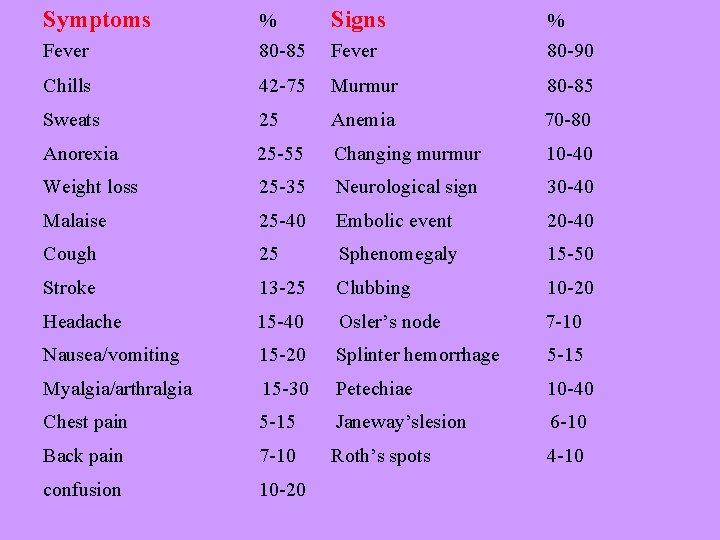
Symptoms Signs Fever % 80 -85 Fever % 80 -90 Chills 42 -75 Murmur 80 -85 Sweats 25 Anemia 70 -80 Anorexia 25 -55 Changing murmur 10 -40 Weight loss 25 -35 Neurological sign 30 -40 Malaise 25 -40 Embolic event 20 -40 Cough 25 Sphenomegaly 15 -50 Stroke 13 -25 Clubbing 10 -20 Headache 15 -40 Osler’s node 7 -10 Nausea/vomiting 15 -20 Splinter hemorrhage 5 -15 Myalgia/arthralgia 15 -30 Petechiae 10 -40 Chest pain 5 -15 Janeway’slesion 6 -10 Back pain 7 -10 Roth’s spots 4 -10 confusion 10 -20
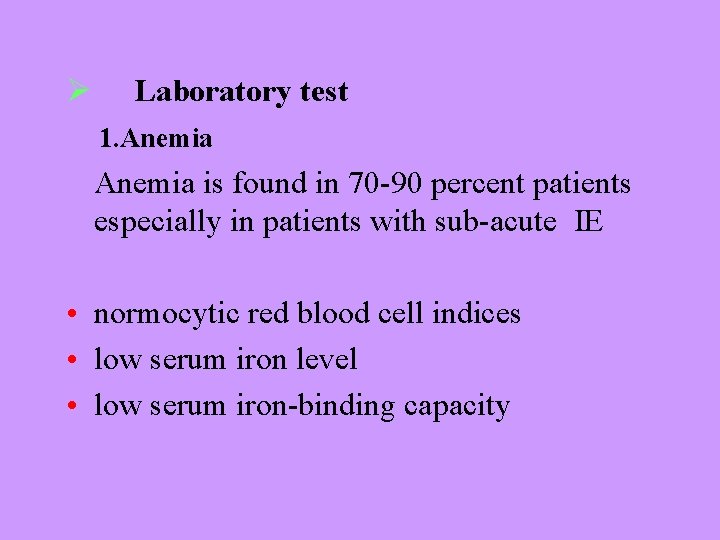
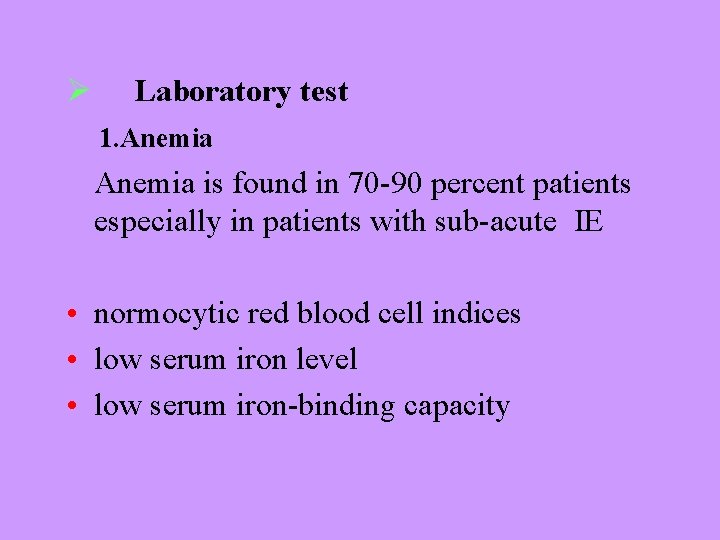
Ø Laboratory test 1. Anemia is found in 70 -90 percent patients especially in patients with sub-acute IE • normocytic red blood cell indices • low serum iron level • low serum iron-binding capacity
2. Echocardiography through thorax echocardiogram(TTE) the sensitive about 80~90% through esophagus echocardiogram(TEE) the sensitive is about 95%. It can find less than 2 -3 mm 2 vegetation
3. Blood culture Three separate sets of blood cultures, obtained over first 24 hours are recommended. a) at least 10 ml~20 ml blood should placed b) fist day 3 sets, second day 1 -2 sets c) every hour interval
The cultures should include staphylococci, steptococci, mycobateria, rickettsiae, chlamydozoan, mycoplosmal, coccobacilli, fungi, and other special organisms. Sensitive to the antibiotic drug should be done. minimal inhibitory concentration MIC minimal bactericidal concentration MBC
4. Urine tests hematuria proteinuria tubular proteinuria
5. ECG 6. X-ray It can find metastatic abscesses in lungs or enlargement of heart
Diagnosis Criteria • Major criteria • Minor criteria
v Major criteria 1. Positive blood culture • Typical microorganism for infective endocarditis from two separate blood cultures • persistently positive blood culture, • blood cultures draw more than 12 hrs apart, All of three or a majority of four or more separate blood culture, with first and last drawn at least 1 hour apart
2. Evidence of endo-cardium involvement Positive echocardiogram • Oscillating mass (vegetation) • Abscess • New/changing murmur (valvular regurgitation)
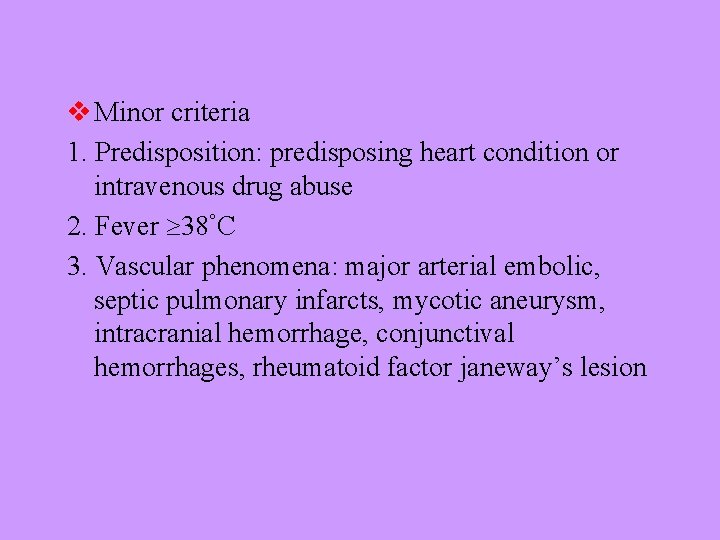
v Minor criteria 1. Predisposition: predisposing heart condition or intravenous drug abuse 2. Fever 38°C 3. Vascular phenomena: major arterial embolic, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, rheumatoid factor janeway’s lesion
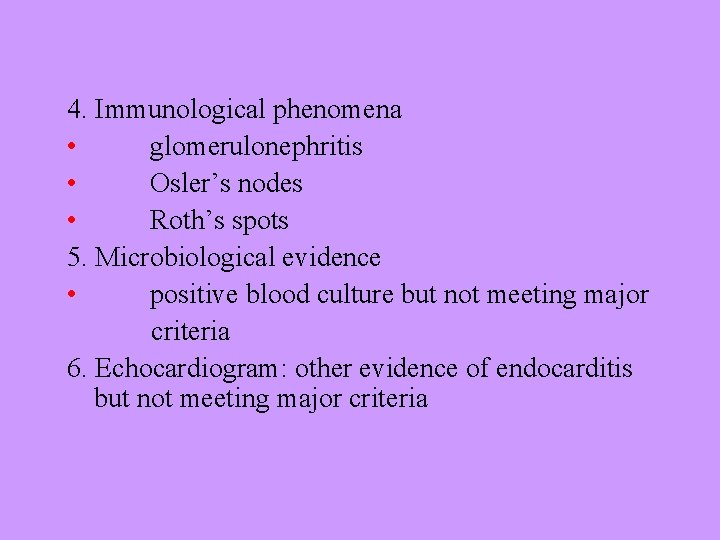
4. Immunological phenomena • glomerulonephritis • Osler’s nodes • Roth’s spots 5. Microbiological evidence • positive blood culture but not meeting major criteria 6. Echocardiogram: other evidence of endocarditis but not meeting major criteria
Diagnosis of infective endocarditis v Clinical criteria: fever, chill, sweat, weight lose anemia, murmur, Osler’node, Janeway’s lesion, Roth’s spots and so on.
v. Pathological criteria • Microorganism: demonstrated by culture or histology in a vegetation, or in a vegetation that has embolized, or intracardiac abscess, • Pathological lesions: vegetation or intracardiac abscess present comfirmed by histology showing active endocarditis
Clinical diagnosis criteria § Two major criteria § One major and three minor criteria § Five minor criteria
v Rejected • Not meeting pathological and clinical diagnosis criteria, predisposing other disease • no pathological evidence at surgery or autopsy, after antibiotic therapy for 4 days or less
antibiotic therapy v. The regular antibiotic therapy include flow 1. Early use as soon as clinical diagnosis has been set up 2. High serum concentration 3. Treatment is continued for prolonged period at least 4~6 weeks 4. Bactericidal antibiotics should be chosen 5. Monitoring serum bactericidal titer 6. Combination bactericidal and bacteriostatic
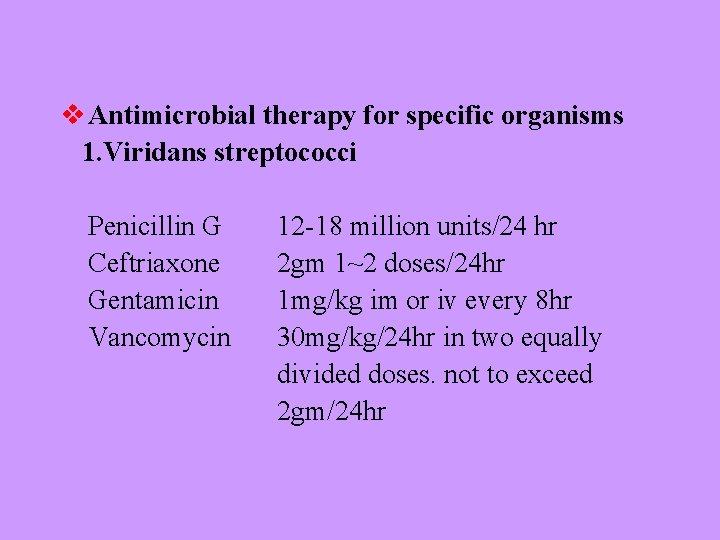
v Antimicrobial therapy for specific organisms 1. Viridans streptococci Penicillin G Ceftriaxone Gentamicin Vancomycin 12 -18 million units/24 hr 2 gm 1~2 doses/24 hr 1 mg/kg im or iv every 8 hr 30 mg/kg/24 hr in two equally divided doses. not to exceed 2 gm/24 hr
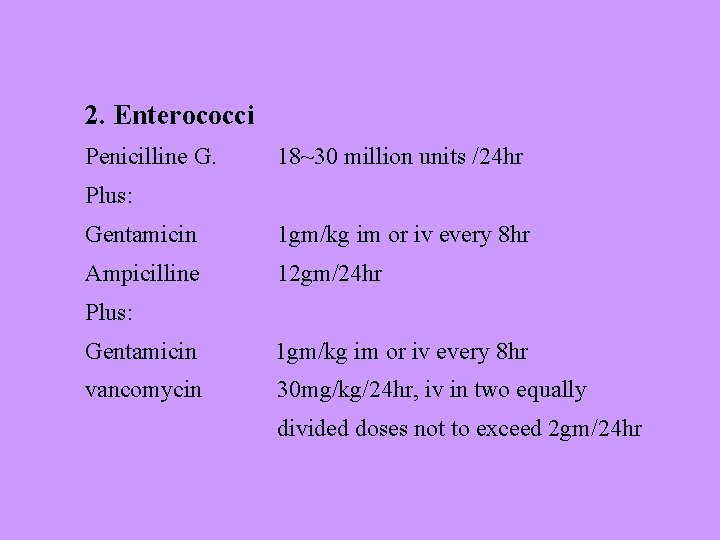
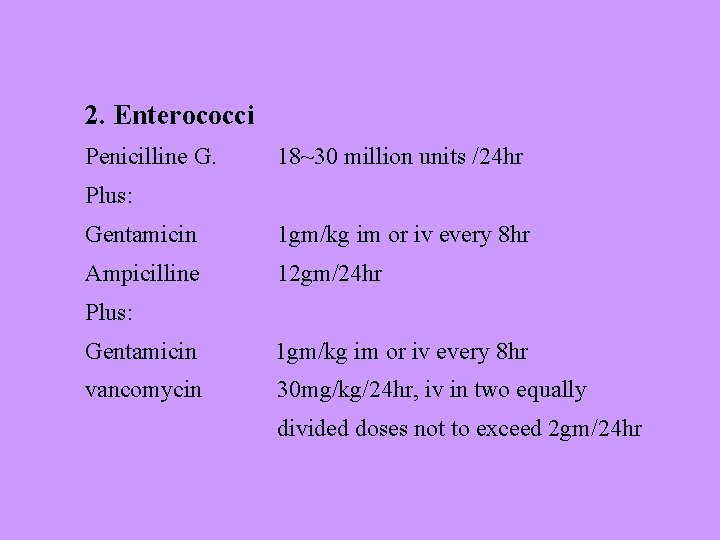
2. Enterococci Penicilline G. 18~30 million units /24 hr Plus: Gentamicin 1 gm/kg im or iv every 8 hr Ampicilline 12 gm/24 hr Plus: Gentamicin 1 gm/kg im or iv every 8 hr vancomycin 30 mg/kg/24 hr, iv in two equally divided doses not to exceed 2 gm/24 hr
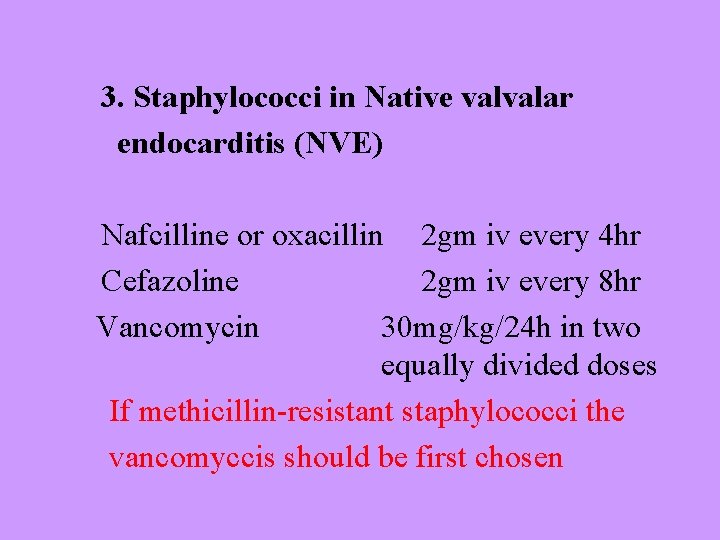
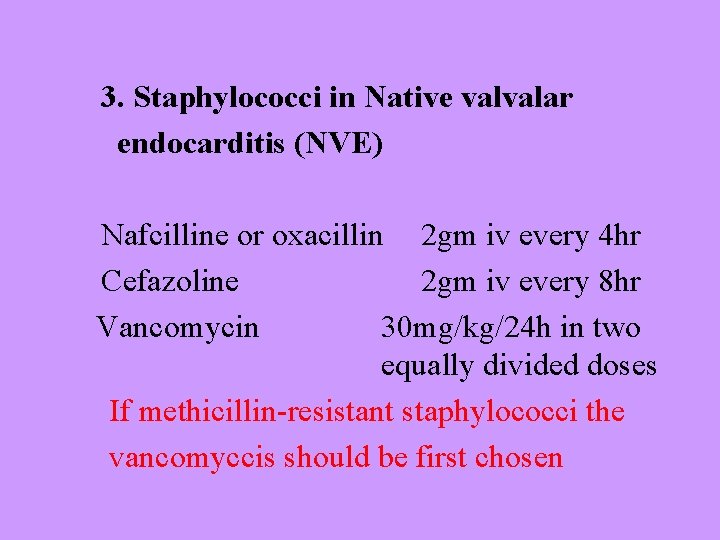
3. Staphylococci in Native valvalar endocarditis (NVE) Nafcilline or oxacillin 2 gm iv every 4 hr Cefazoline 2 gm iv every 8 hr Vancomycin 30 mg/kg/24 h in two equally divided doses If methicillin-resistant staphylococci the vancomyccis should be first chosen
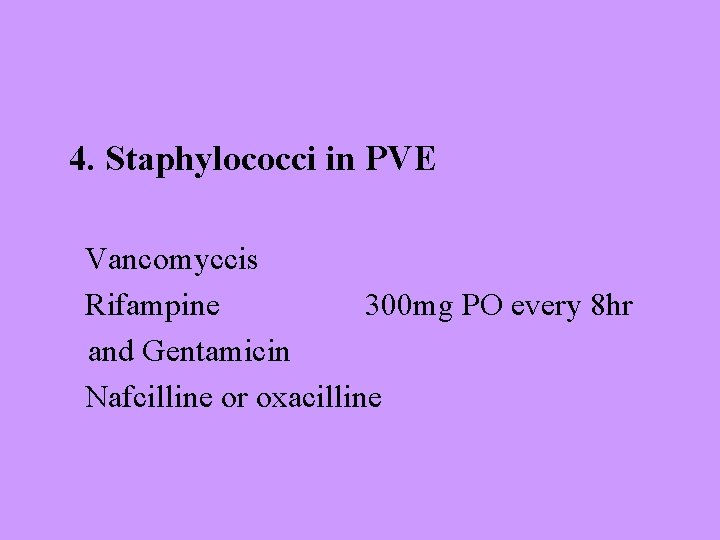
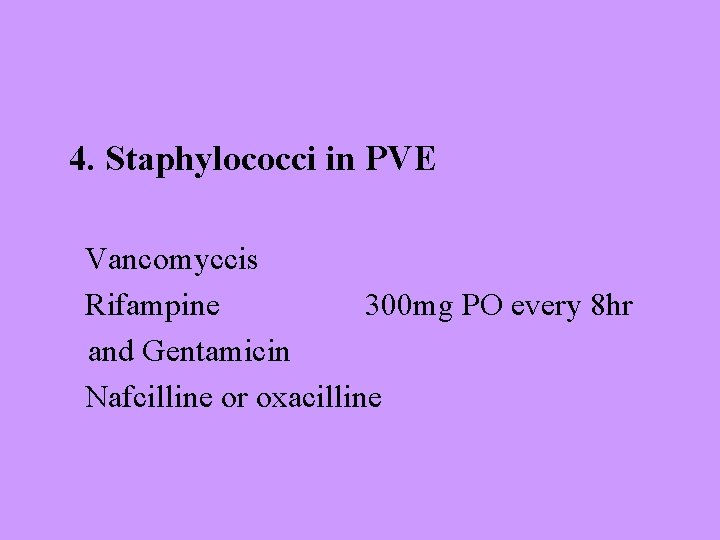
4. Staphylococci in PVE Vancomyccis Rifampine 300 mg PO every 8 hr and Gentamicin Nafcilline or oxacilline
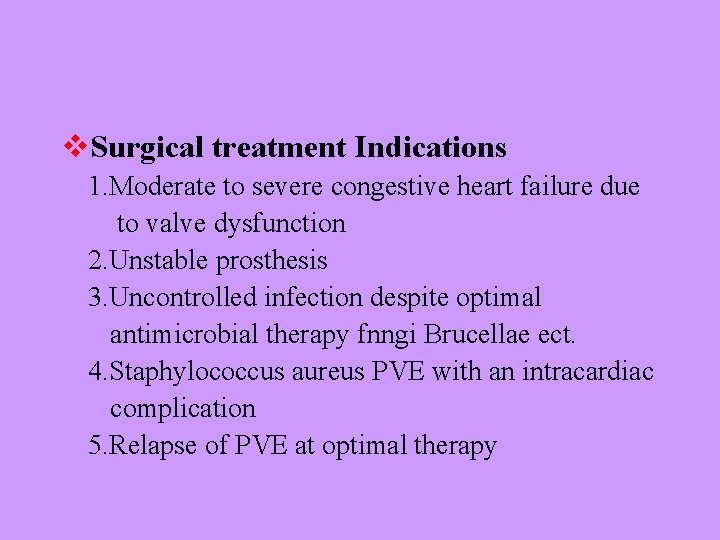
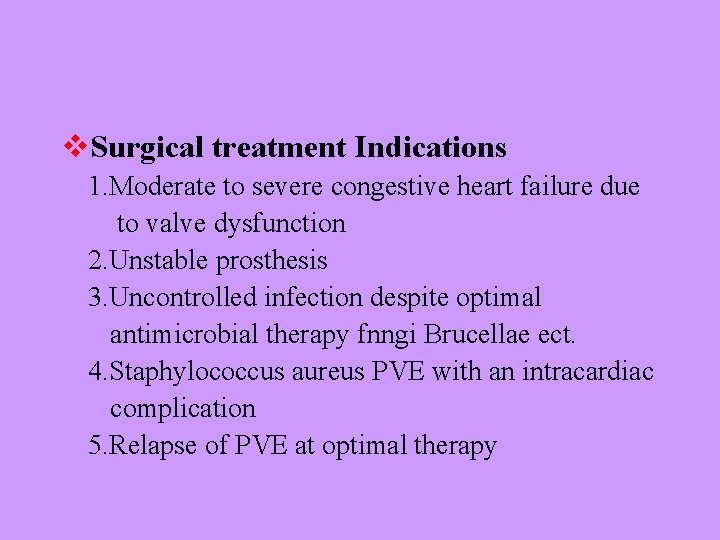
v. Surgical treatment Indications 1. Moderate to severe congestive heart failure due to valve dysfunction 2. Unstable prosthesis 3. Uncontrolled infection despite optimal antimicrobial therapy fnngi Brucellae ect. 4. Staphylococcus aureus PVE with an intracardiac complication 5. Relapse of PVE at optimal therapy
v Relative surgical Indications 1. Perivalvular extension of infection, intracardiac fistula 2. Pooly responsive staphylococcus aureus NVE 3. Culture-negative NVE or PVE with persistent fever 4. Large hypermobile vegetation 5. Endocarditis due to highly antibiotic-resistant enterococci

Thank you!
 Signs of infective endocarditis
Signs of infective endocarditis Infective endocarditis
Infective endocarditis Infective endocarditis
Infective endocarditis Cardiac vegetation definition
Cardiac vegetation definition Duke criteria
Duke criteria Duke criteria
Duke criteria Duke criteria mnemonic
Duke criteria mnemonic Infective endocarditis
Infective endocarditis H nana egg
H nana egg Xuiren
Xuiren Filariasis treatment
Filariasis treatment Periodontal management of medically compromised patients
Periodontal management of medically compromised patients Enterotest giardia
Enterotest giardia Infective stage
Infective stage Entamoeba histolytica infective stage
Entamoeba histolytica infective stage Entrobiasis
Entrobiasis Libman sacks endocarditis echo
Libman sacks endocarditis echo Endocarditis
Endocarditis Criterios duke
Criterios duke Tsia
Tsia Sle libman sacks endocarditis
Sle libman sacks endocarditis Non bacterial thrombotic endocarditis
Non bacterial thrombotic endocarditis Criterios duke endocarditis
Criterios duke endocarditis Cây gạo ngoài bến sông
Cây gạo ngoài bến sông Xifeng gao
Xifeng gao Umass ustore
Umass ustore Ground rules earthwork estimating software
Ground rules earthwork estimating software Pgexxx
Pgexxx Fam checklist
Fam checklist Har gow siu mai
Har gow siu mai Hongyu gao
Hongyu gao Gao schedule assessment guide
Gao schedule assessment guide Dr xiao ke gao
Dr xiao ke gao Einstein rosen bridge equation
Einstein rosen bridge equation Gao images
Gao images Ben chester cheong
Ben chester cheong Xiaoming gao
Xiaoming gao Jacky gao
Jacky gao Hạt gạo làng ta
Hạt gạo làng ta