Infective Endocarditis and Valvular Disease Geoff Lampard PGY1


- Slides: 39
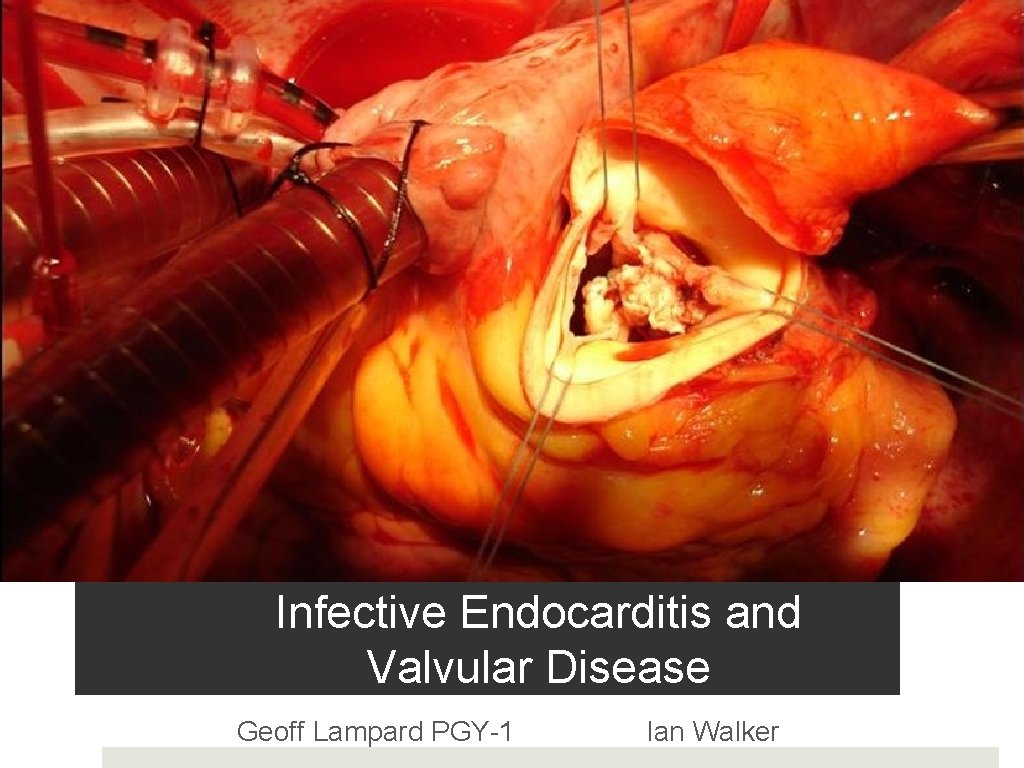
Infective Endocarditis and Valvular Disease Geoff Lampard PGY-1 Ian Walker
Outline What will be covered � Infective Endocarditis � Aortic Stenosis � What murmurs need workup? What will not be covered � The rest……
Doctor! I gotta fever! � 55 yo male � Fever of 24 hours � No focal symptoms � Past history includes mechanical aortic valve for symptomatic AS � Faint I/VI SEM but "that's not new"

the making of the beast a 4 step process � 1. Endocardial injury � 2. Sterile thrombus formation � 3. Transient bacteremia and seeding � 4. Maturation
epidemiology • Epidemiology has changed dramatically over the past 50 years • 2 -10 episodes/100, 000 patient years in general population • 1 -3/1000 in IVDU • M>F • Mean age ≈ 60 • Mortality is steadily increasing
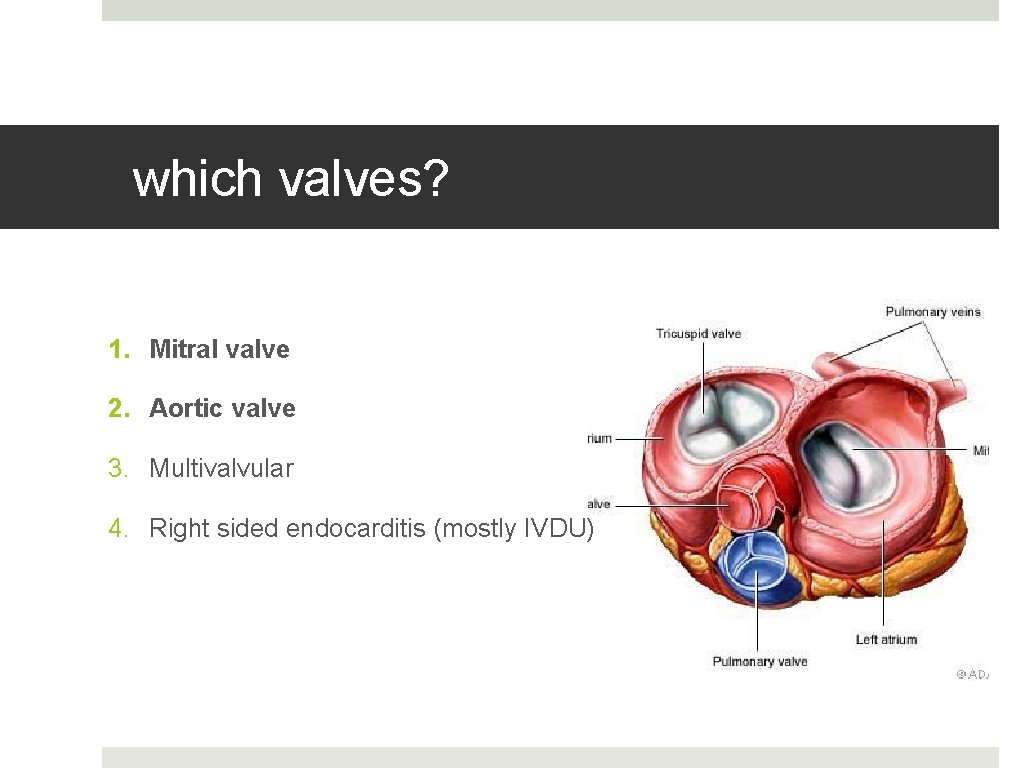
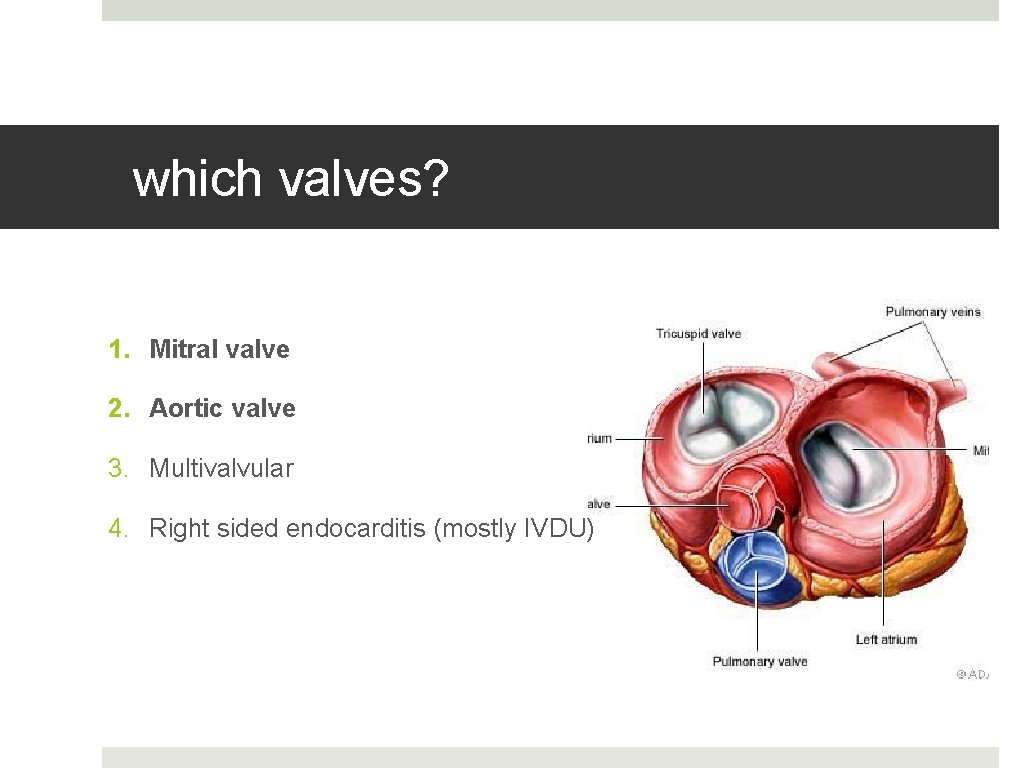
which valves? 1. Mitral valve 2. Aortic valve 3. Multivalvular 4. Right sided endocarditis (mostly IVDU)
IE risk factors 1. Structural valvular lesion or prosthetic valve (75%) Also: • Prior IE • Invasive Procedure/Line • IVDU • Age
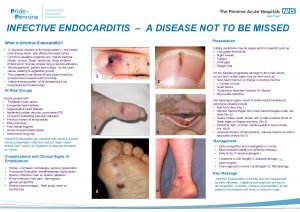
2 very different presentations 1. Acute IE � acute fever � CHF +/- hemodynamic instability � peripheral signs of embolism 2. Subacute Bacterial Endocarditis (SBE) � Fever (85%), malaise (80%) � Murmur is unpredictable � Others: weakness, myalgias, back pain, dyspnea, chest pain, cough, headaches. � Commonly misdiagnosed as viral illness � Check their hands and eyes!
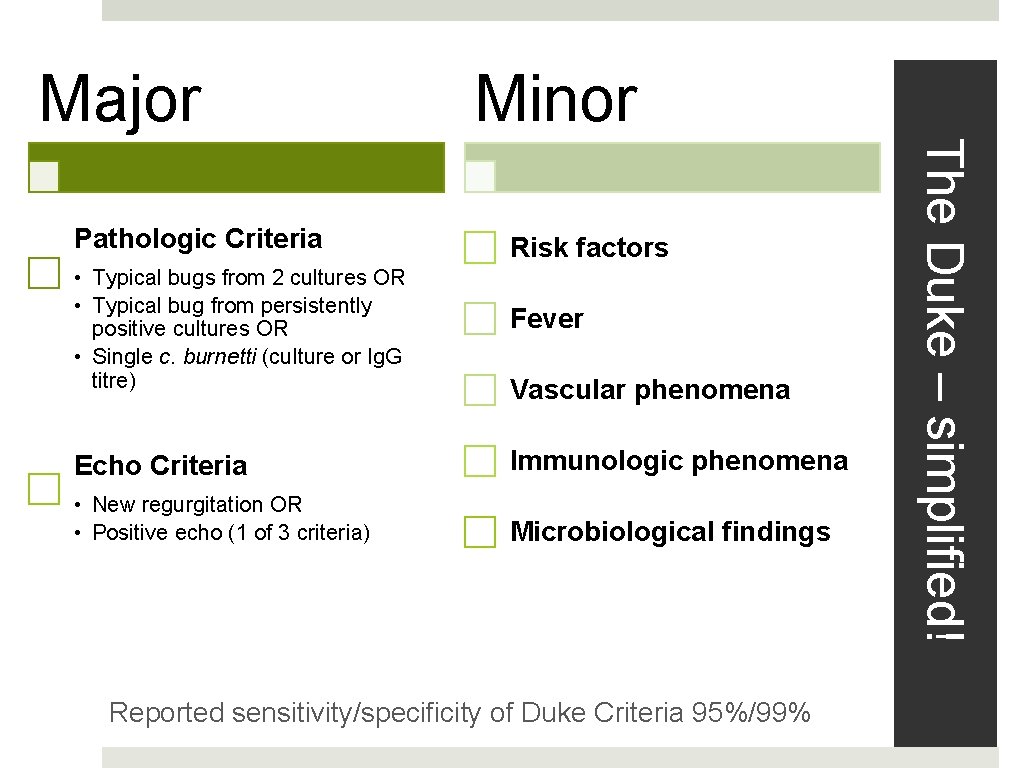
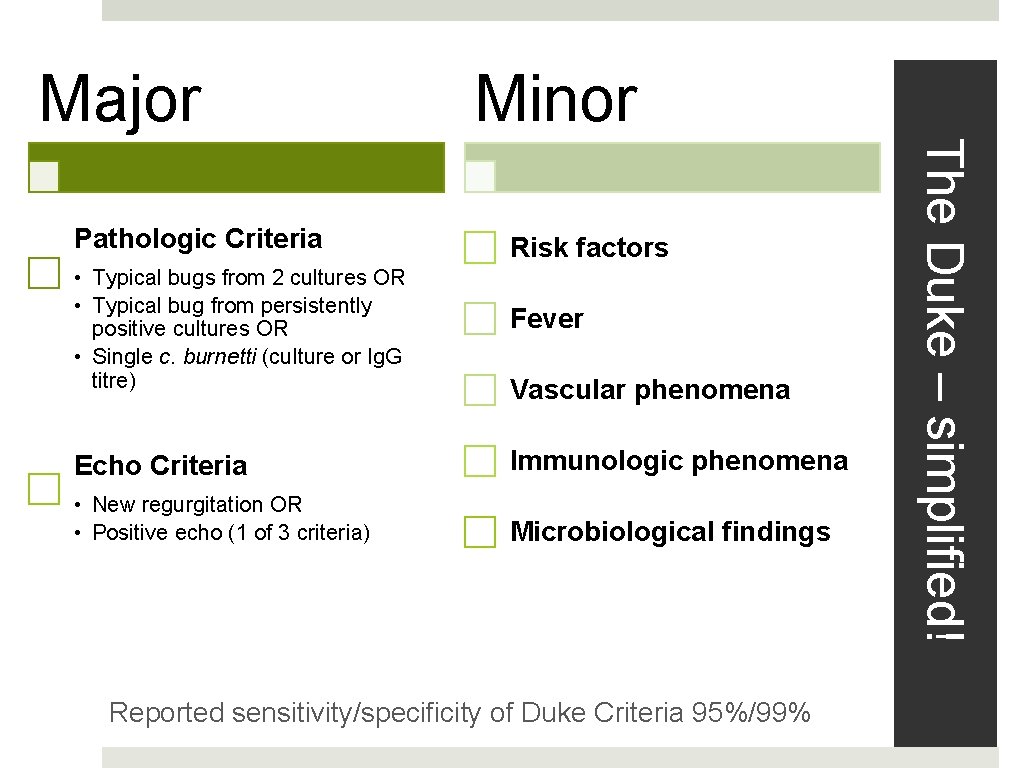
Major Minor Risk factors • Typical bugs from 2 cultures OR • Typical bug from persistently positive cultures OR • Single c. burnetti (culture or Ig. G titre) Fever Echo Criteria Immunologic phenomena • New regurgitation OR • Positive echo (1 of 3 criteria) Microbiological findings Vascular phenomena Reported sensitivity/specificity of Duke Criteria 95%/99% The Duke – simplified! Pathologic Criteria
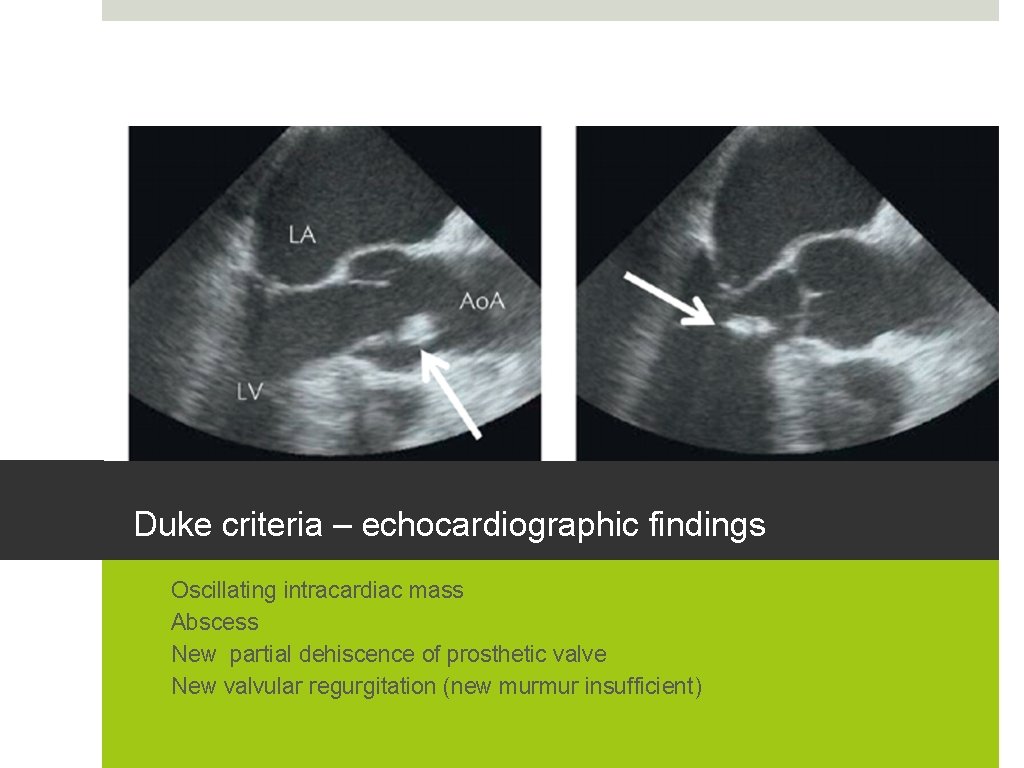
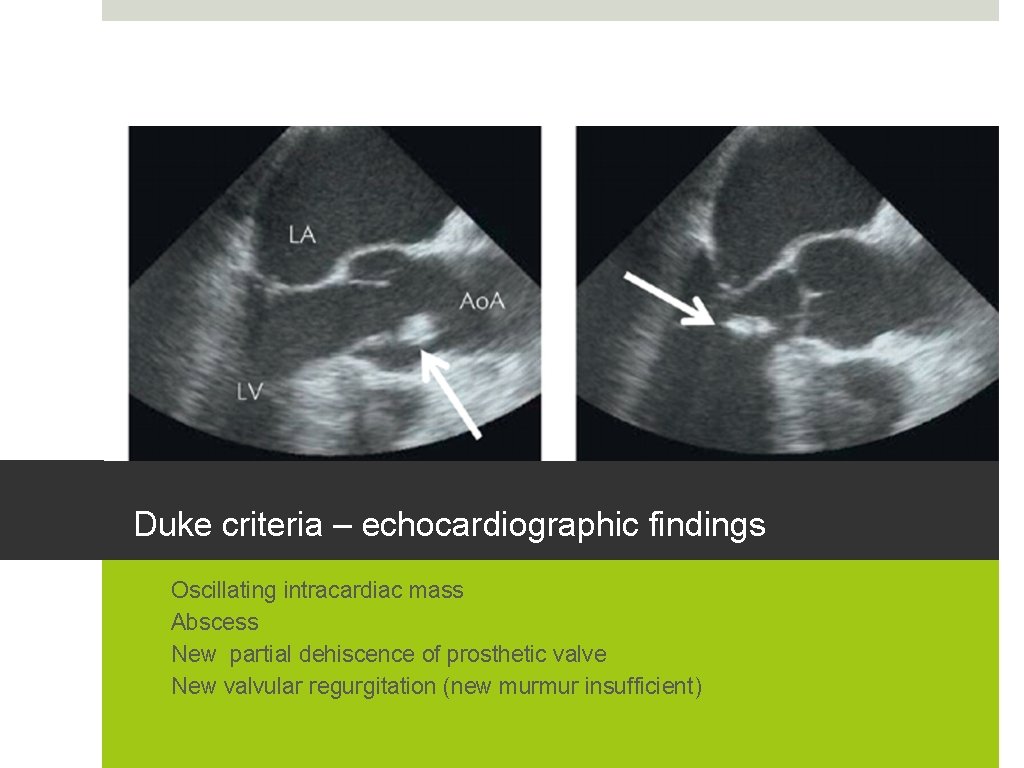
Duke criteria – echocardiographic findings 1. 2. 3. 4. Oscillating intracardiac mass Abscess New partial dehiscence of prosthetic valve New valvular regurgitation (new murmur insufficient)
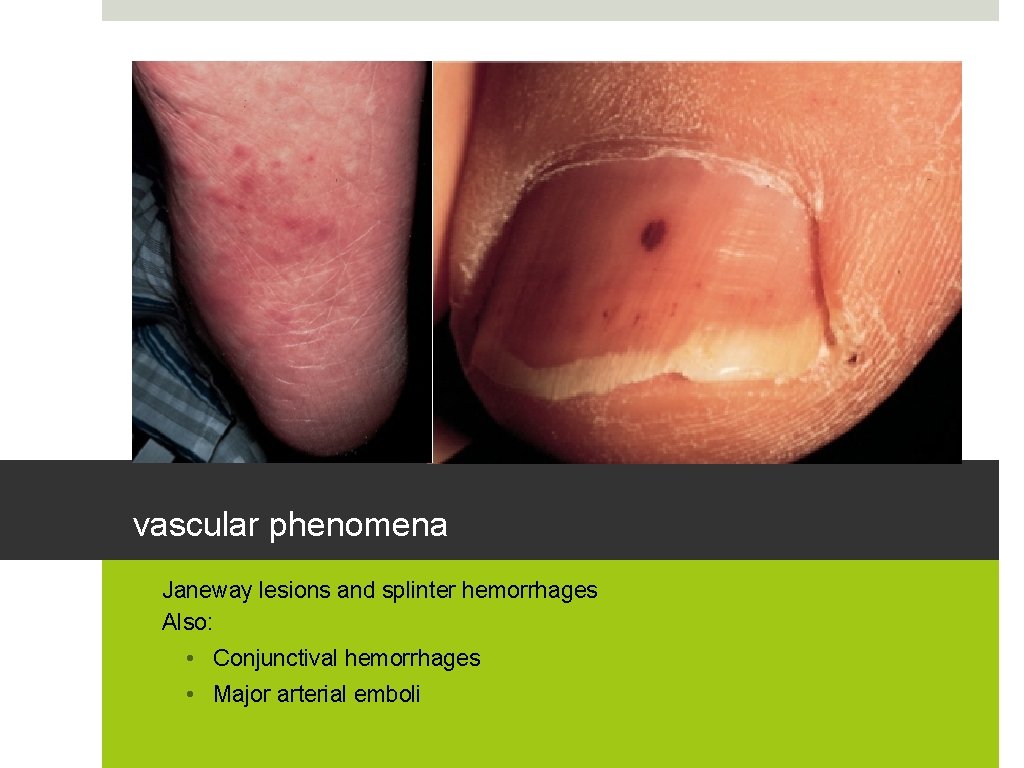
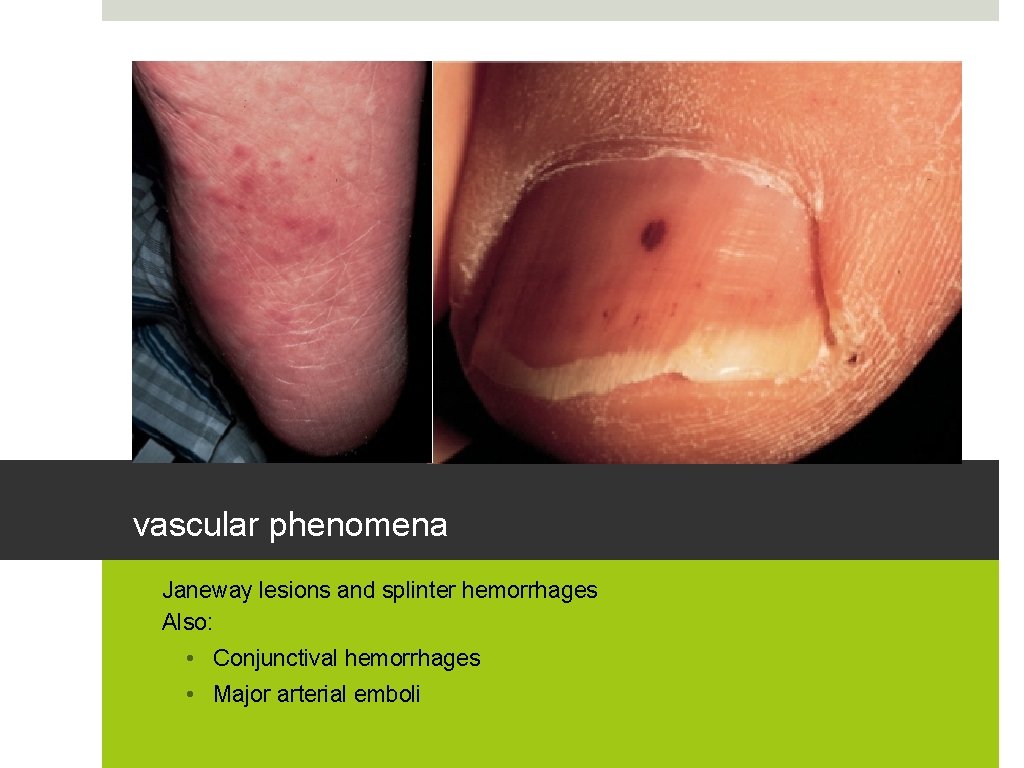
vascular phenomena • Janeway lesions and splinter hemorrhages • Also: • Conjunctival hemorrhages • Major arterial emboli
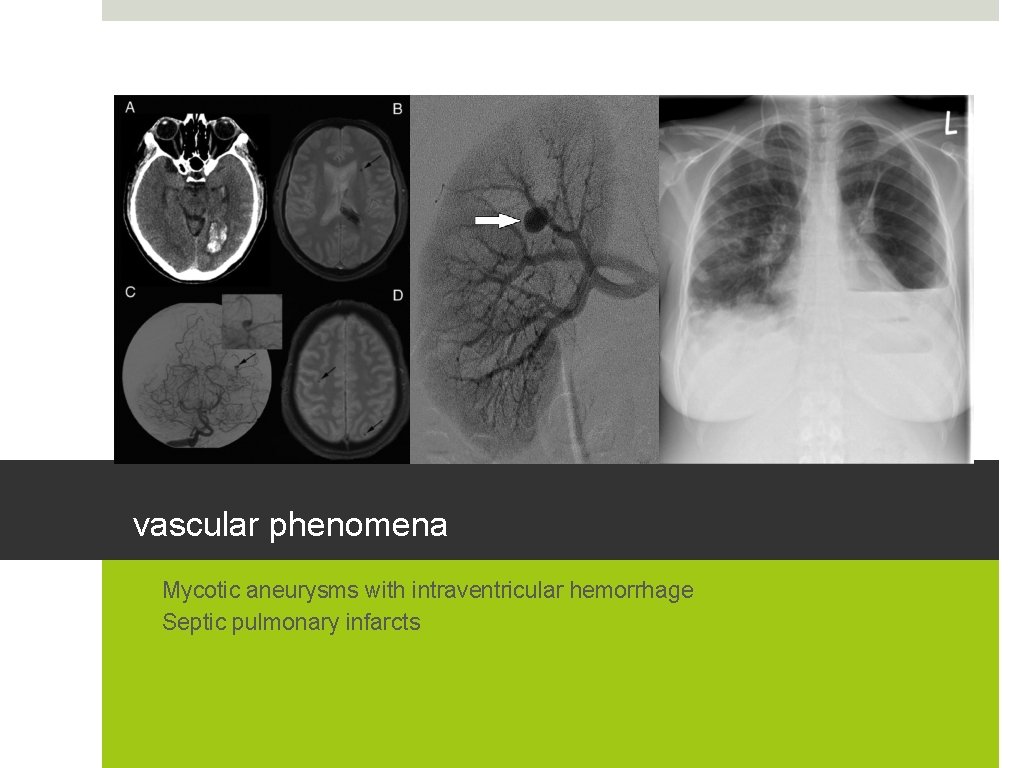
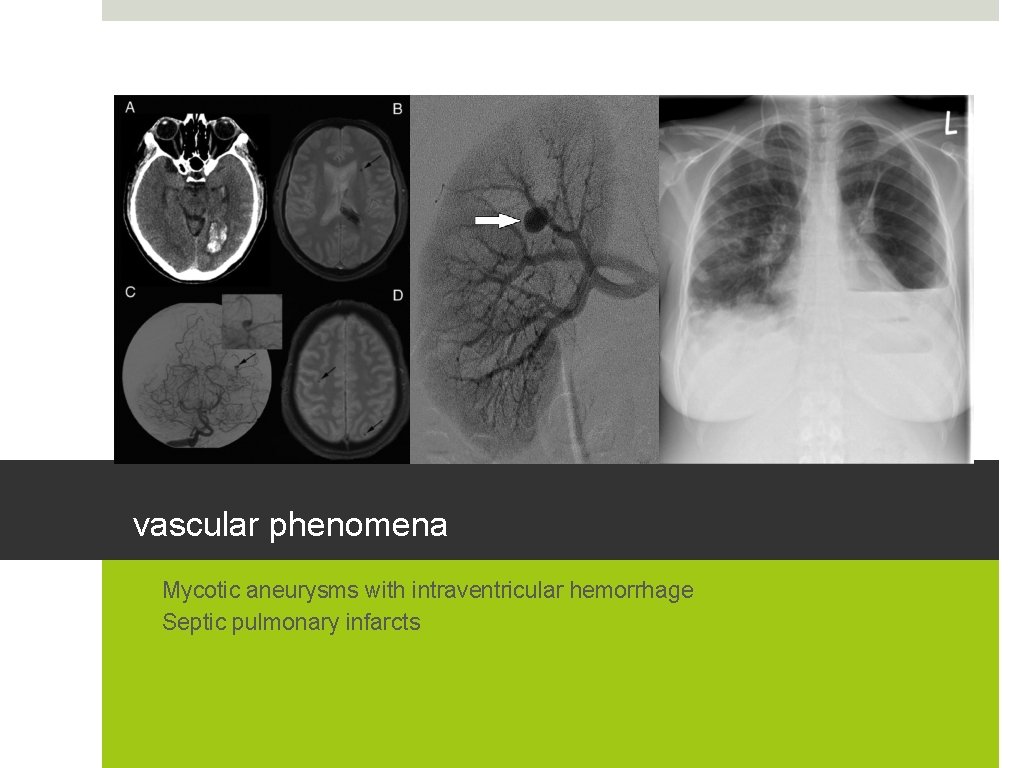
vascular phenomena • Mycotic aneurysms with intraventricular hemorrhage • Septic pulmonary infarcts

immunologic phenomena – eponymous potpourri! • Osler nodes and Roth spots • Glomerulonephritis and elevated rheumatoid factor • Much more likely to occur in SBE
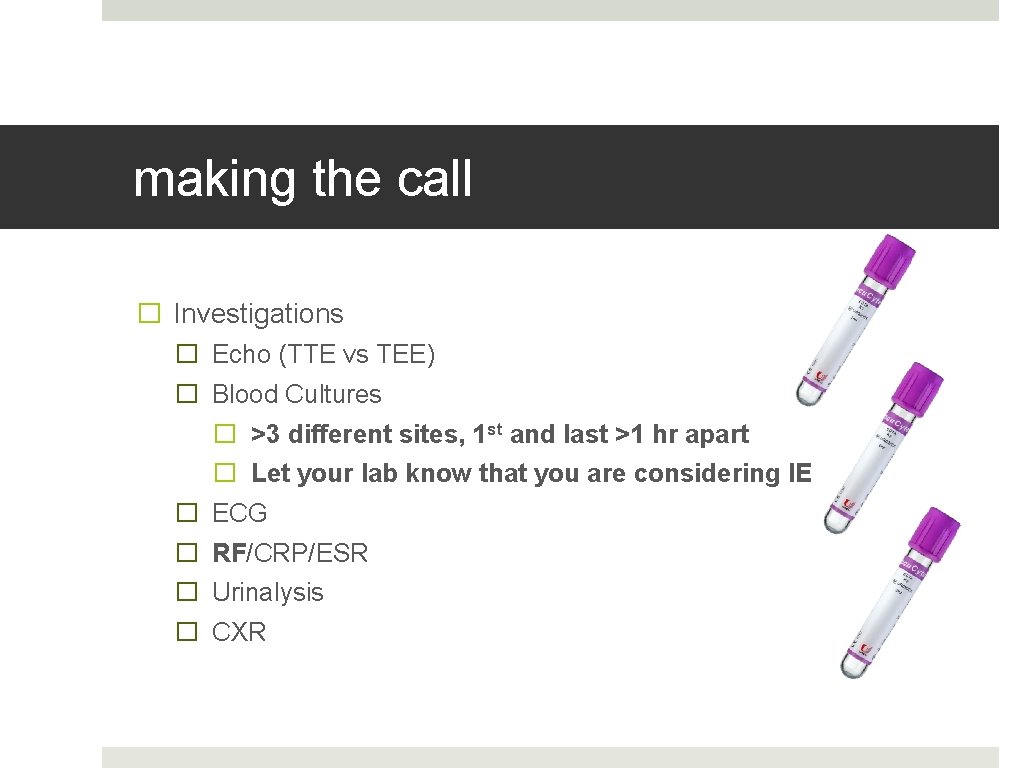
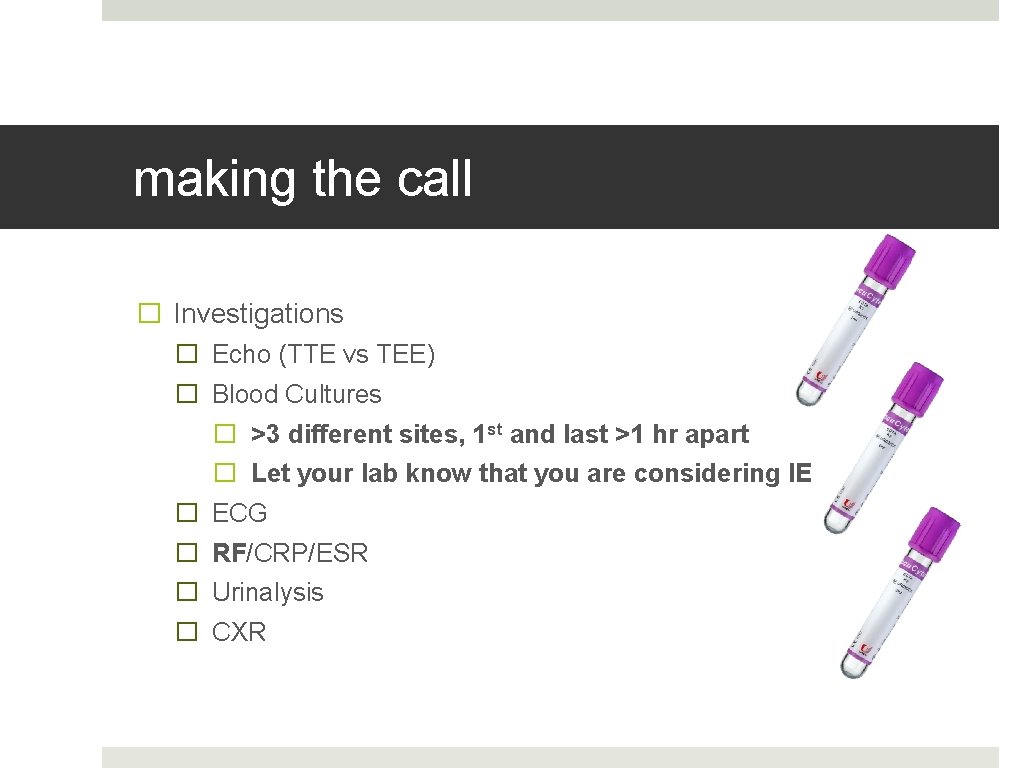
making the call � Investigations � Echo (TTE vs TEE) � Blood Cultures � >3 different sites, 1 st and last >1 hr apart � Let your lab know that you are considering IE � ECG � RF/CRP/ESR � Urinalysis � CXR
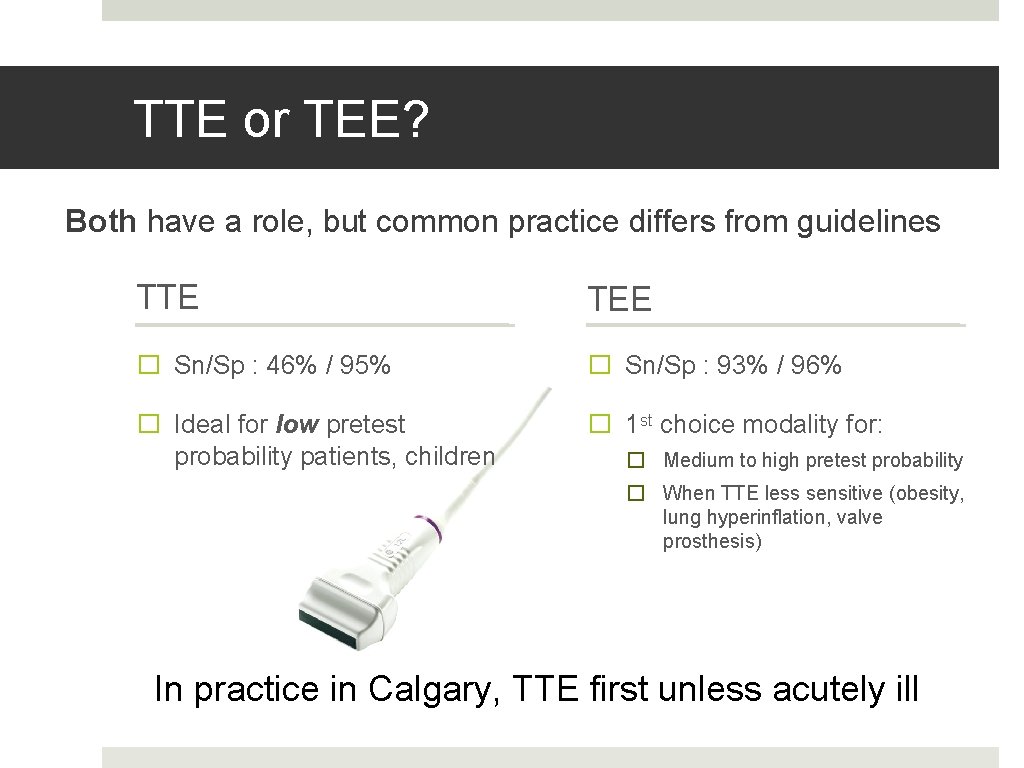
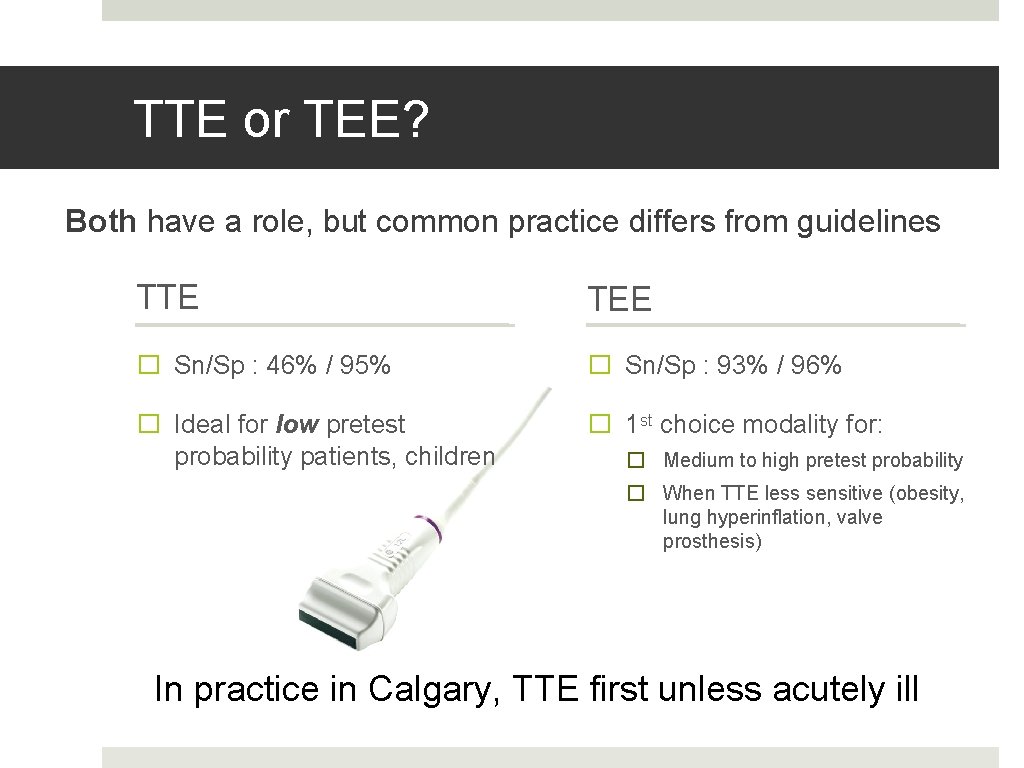
TTE or TEE? Both have a role, but common practice differs from guidelines TTE TEE � Sn/Sp : 46% / 95% � Sn/Sp : 93% / 96% � Ideal for low pretest probability patients, children � 1 st choice modality for: � Medium to high pretest probability � When TTE less sensitive (obesity, lung hyperinflation, valve prosthesis) In practice in Calgary, TTE first unless acutely ill
some antibiotic principles � Long durations required � Parenteral preferred � Stable SBE: forgo antibiotics until cultures return � Acute IE: obtain cultures first, then treat � Think of 3 treatment groups: � NVE � IVDU � PVE
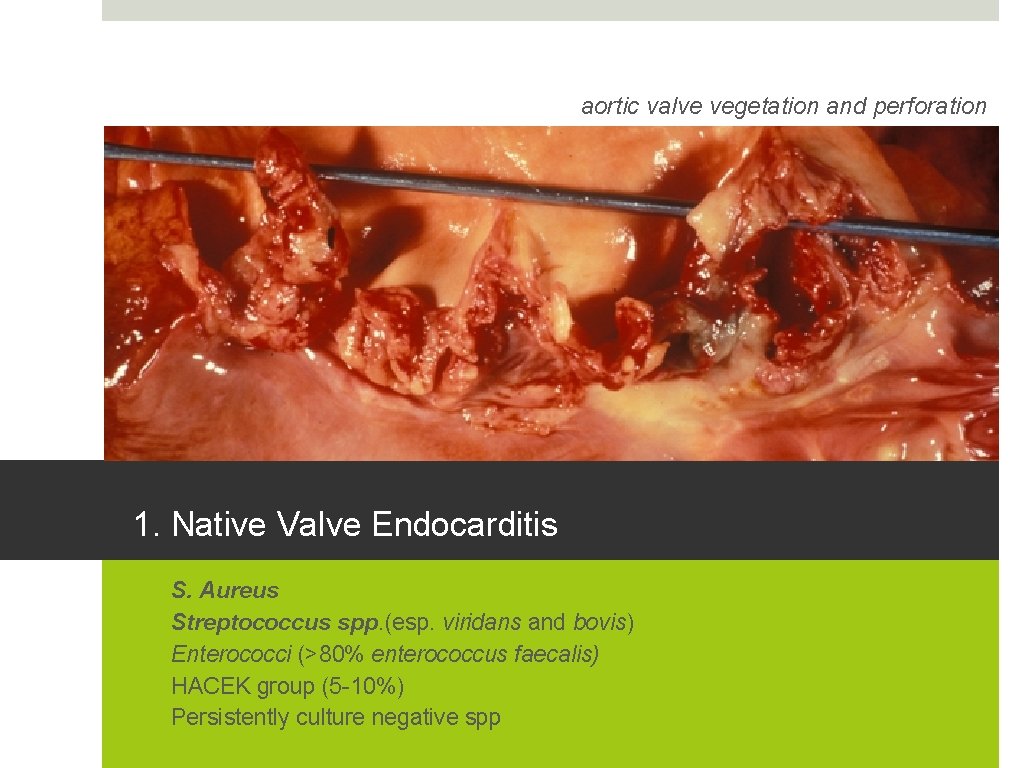
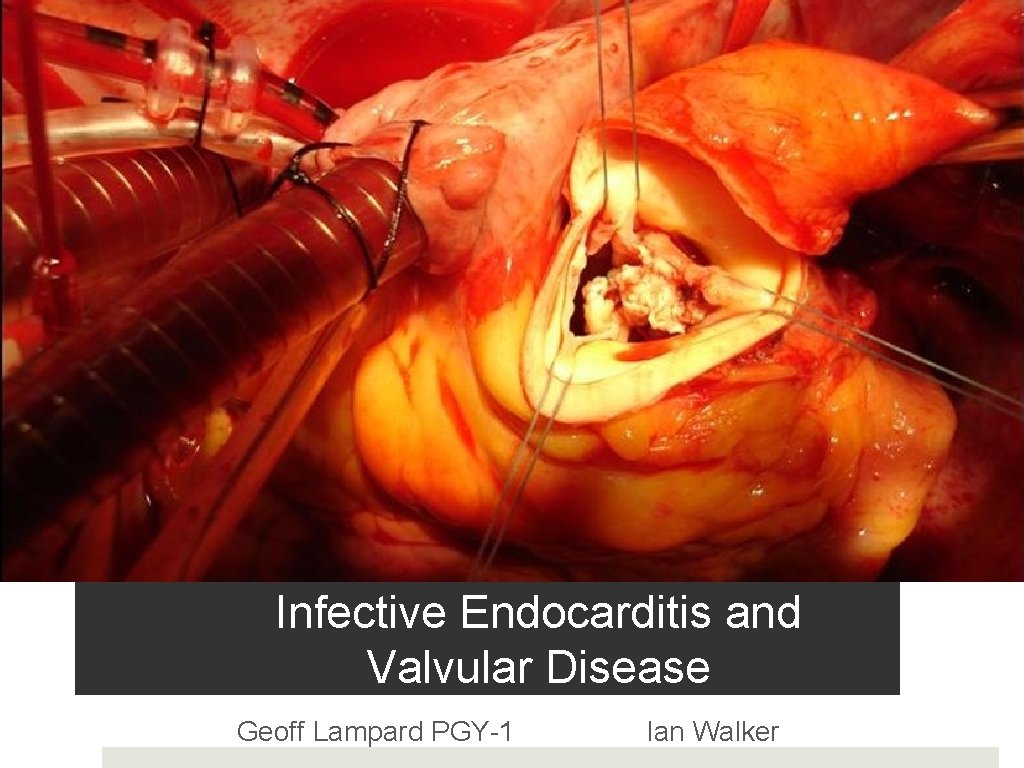
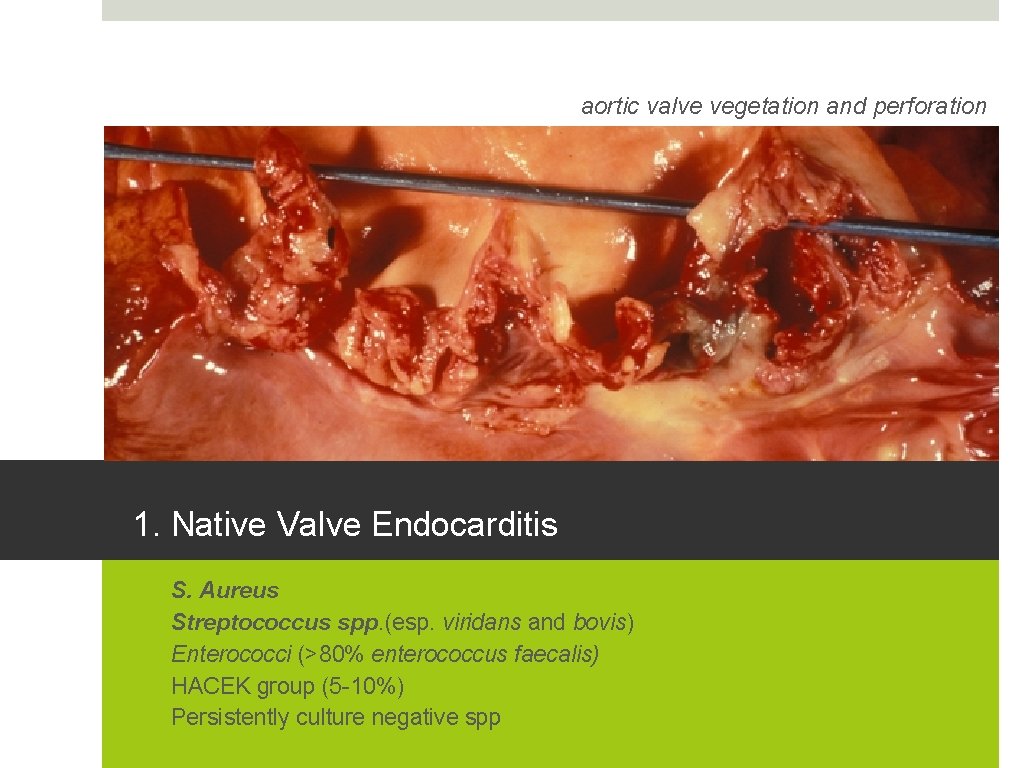
aortic valve vegetation and perforation 1. Native Valve Endocarditis 1. 2. 3. 4. 5. S. Aureus Streptococcus spp. (esp. viridans and bovis) Enterococci (>80% enterococcus faecalis) HACEK group (5 -10%) Persistently culture negative spp
HACEK group – can you name them? • Haemophilus species • Actinobacillus actinomycetemcomitans • Cardiobacterium hominis • Eikenella corrodens • Kingella Kingae colony of actinobacillus actinomycetemcomitans
s. aureus 2. IVDU associated endocarditis 1. S. Aureus (70%) 2. Polymicrobial 3. Streptococcus spp. 4. Pseudomonus aeruginosa Must also consider fungal species (candida, aspergillus)
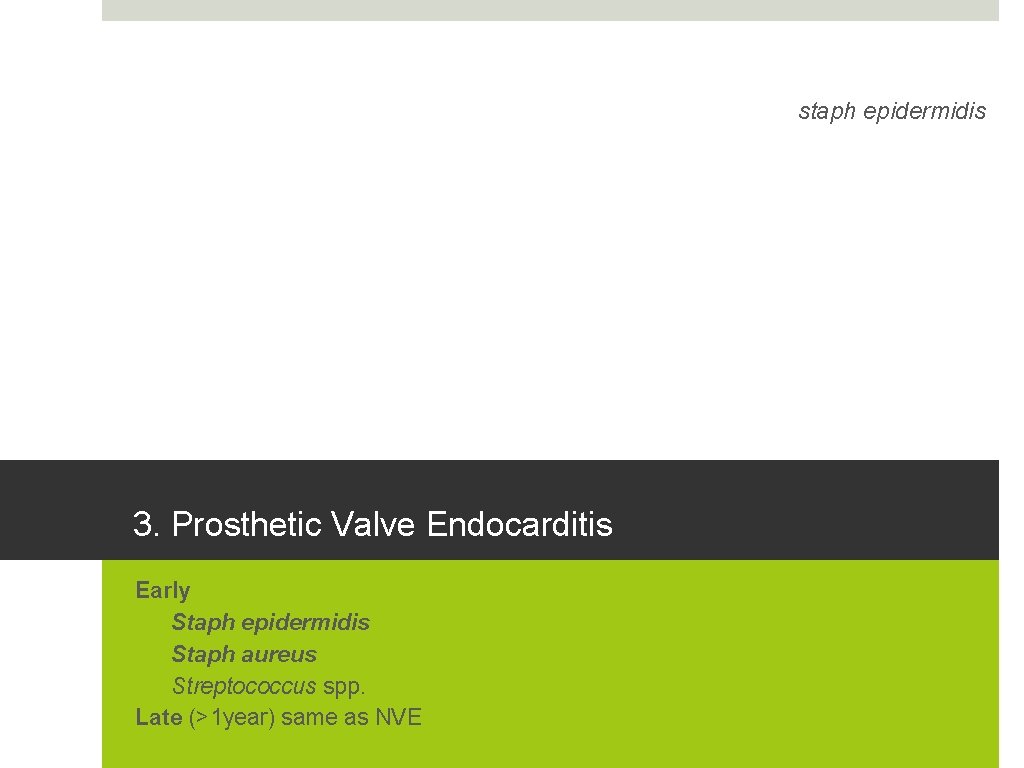
staph epidermidis 3. Prosthetic Valve Endocarditis Early 1. Staph epidermidis 2. Staph aureus 3. Streptococcus spp. Late (>1 year) same as NVE
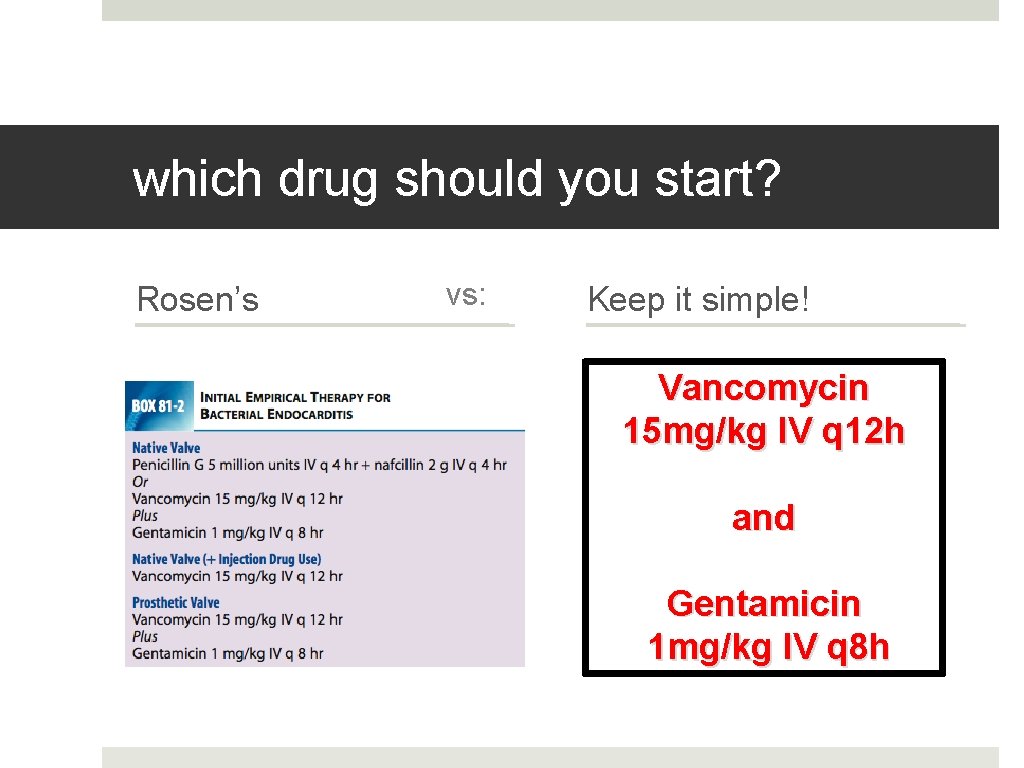
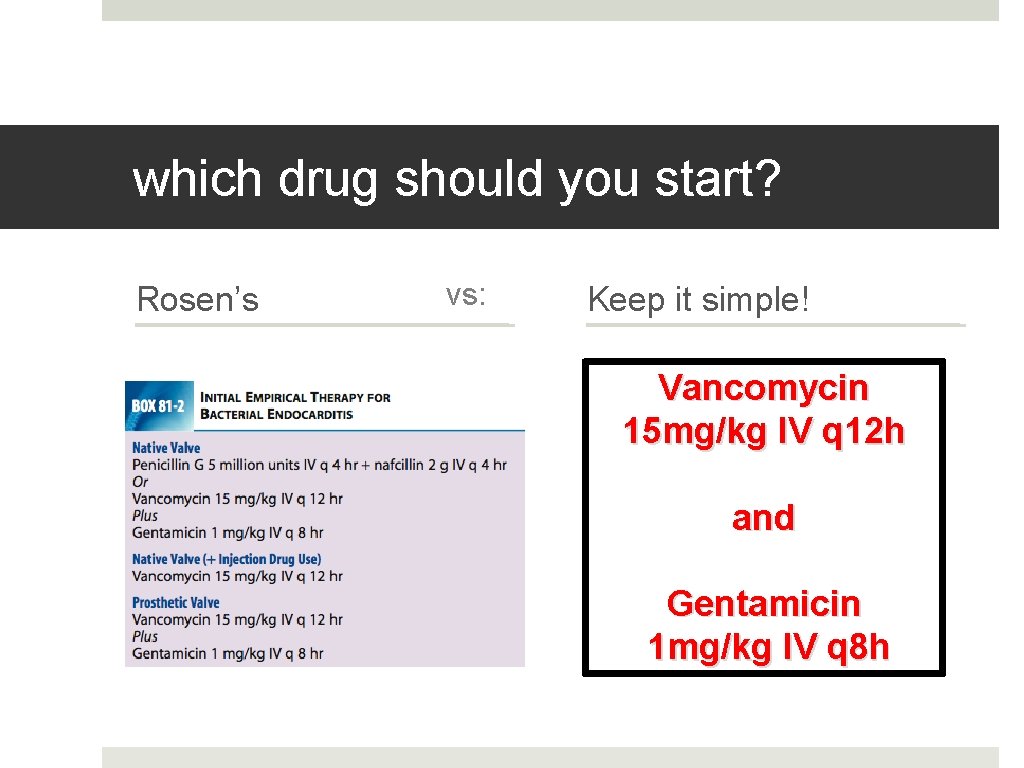
which drug should you start? Rosen’s vs: Keep it simple! Vancomycin 15 mg/kg IV q 12 h and Gentamicin 1 mg/kg IV q 8 h
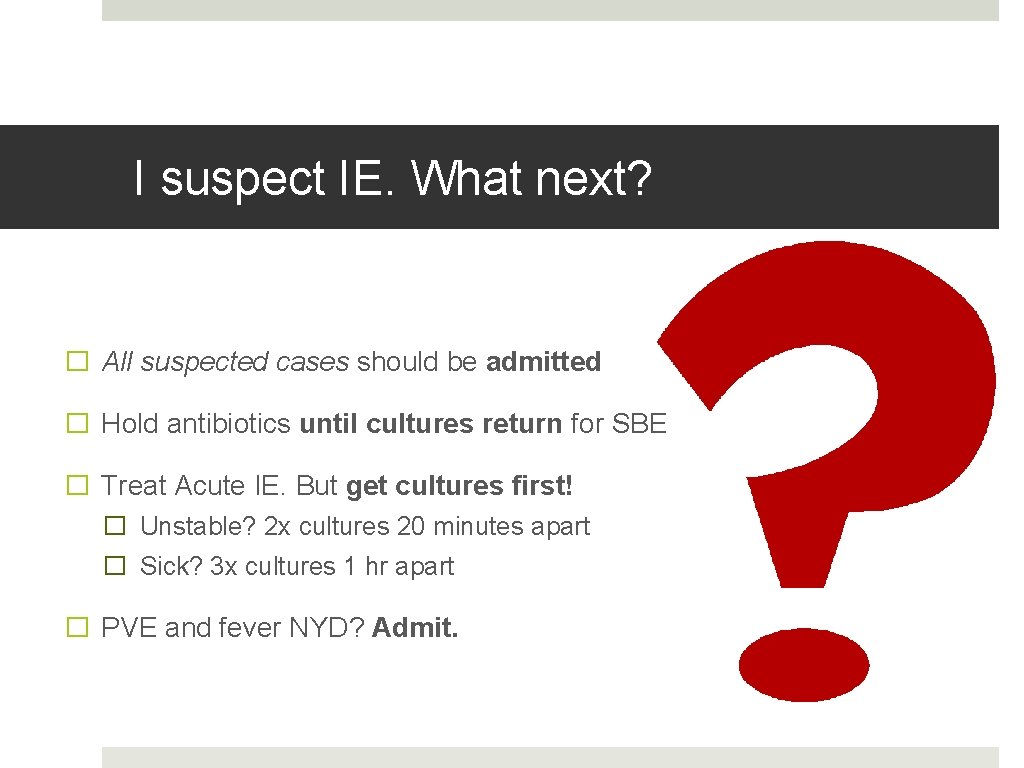
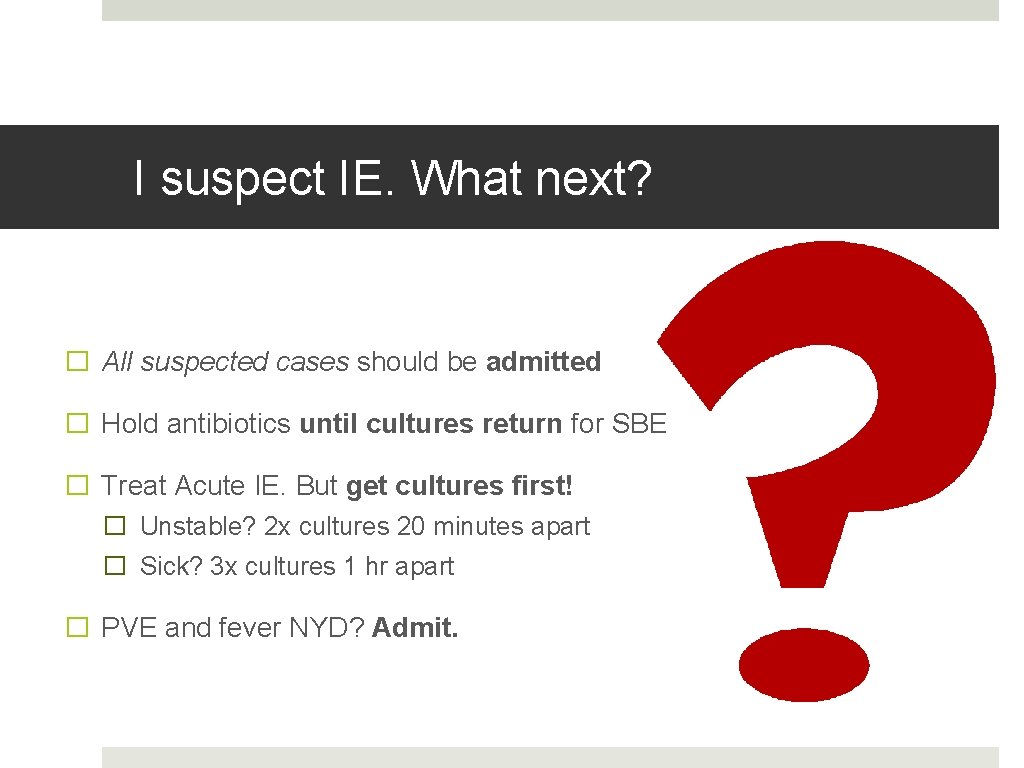
I suspect IE. What next? � All suspected cases should be admitted � Hold antibiotics until cultures return for SBE � Treat Acute IE. But get cultures first! � Unstable? 2 x cultures 20 minutes apart � Sick? 3 x cultures 1 hr apart � PVE and fever NYD? Admit.
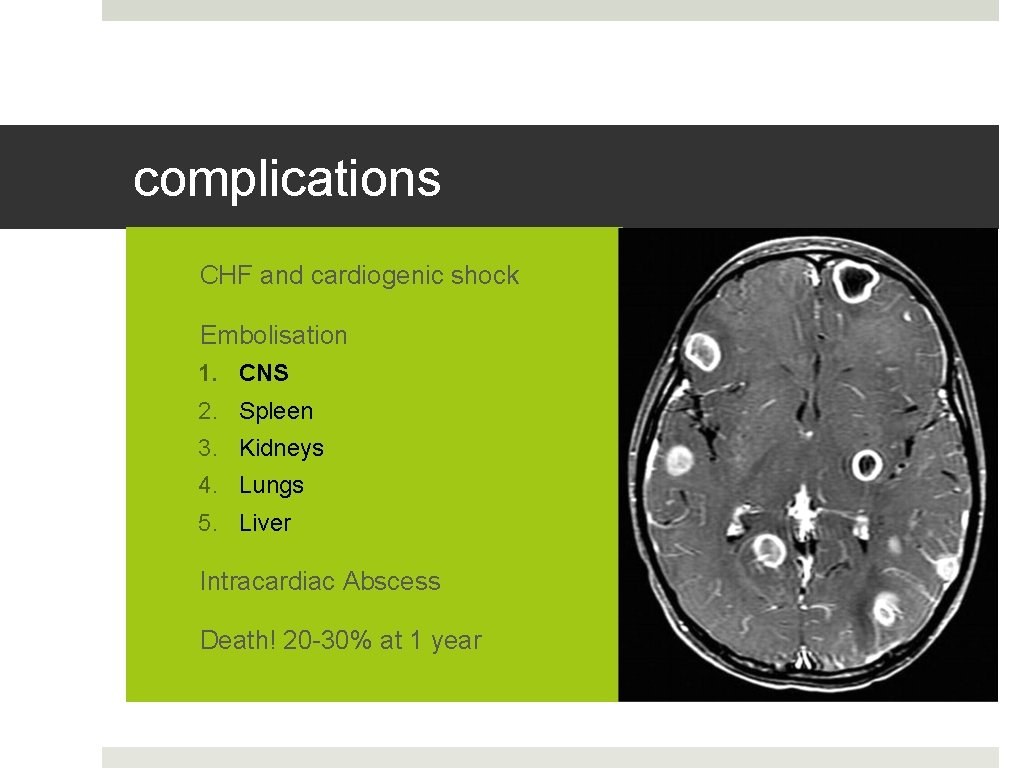
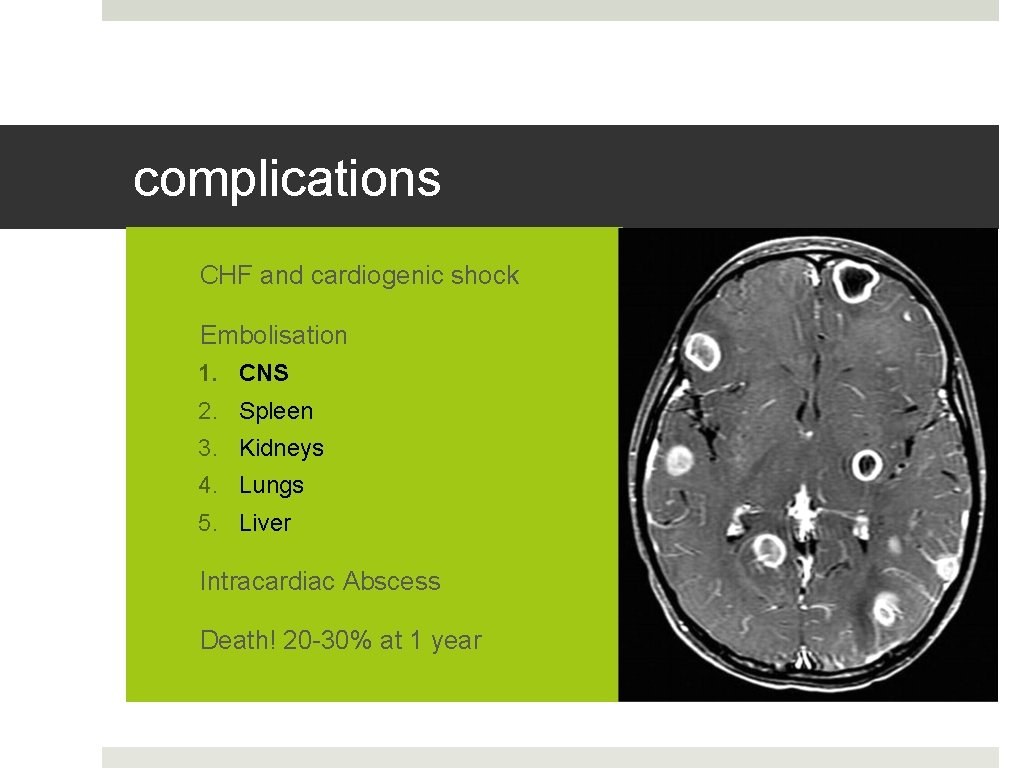
complications 1. CHF and cardiogenic shock 2. Embolisation 1. CNS 2. Spleen 3. Kidneys 4. Lungs 5. Liver 3. Intracardiac Abscess 4. Death! 20 -30% at 1 year
the IV drug user � 79% of IVDU IE is right sided � 70% s. aureus � Only 35% will have a murmur on admission � Septic pulmonary emboli: hallmark of disease � 80% of tricuspid valve IE will have CXR findings on presentation
what about prostheses? � Risk is highest in the 1 st year � Low threshold for admission of Fever NYD + admission � Aggressive organisms � High risk of dehiscence � TTE very low sensitivity � Pacemakers can get infected too!
who needs emergent surgery? � Practically speaking, CHF + cardiogenic shock is only true indication for emergent surgery. � Consult cardiac surgeon early for: � CHF or severe valvular dysfunction likely to precipitate CHF � Invasive valvular complications on echo � Pseudomonas, fungi, or MDR organisms � High risk of embolism � PVE
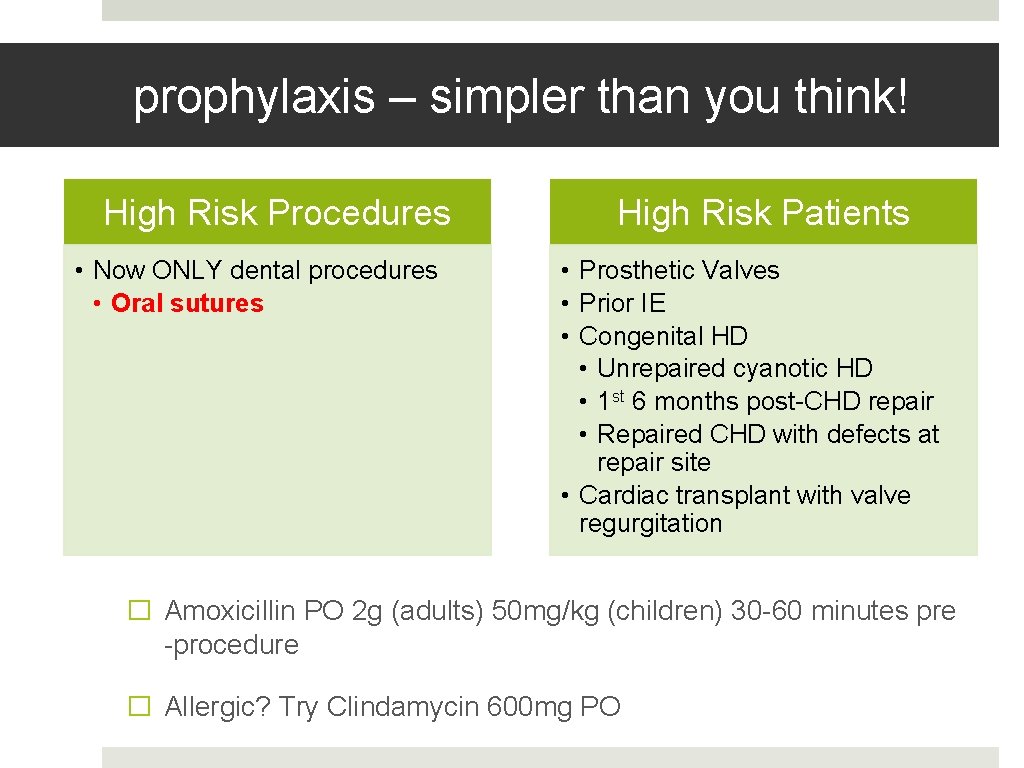
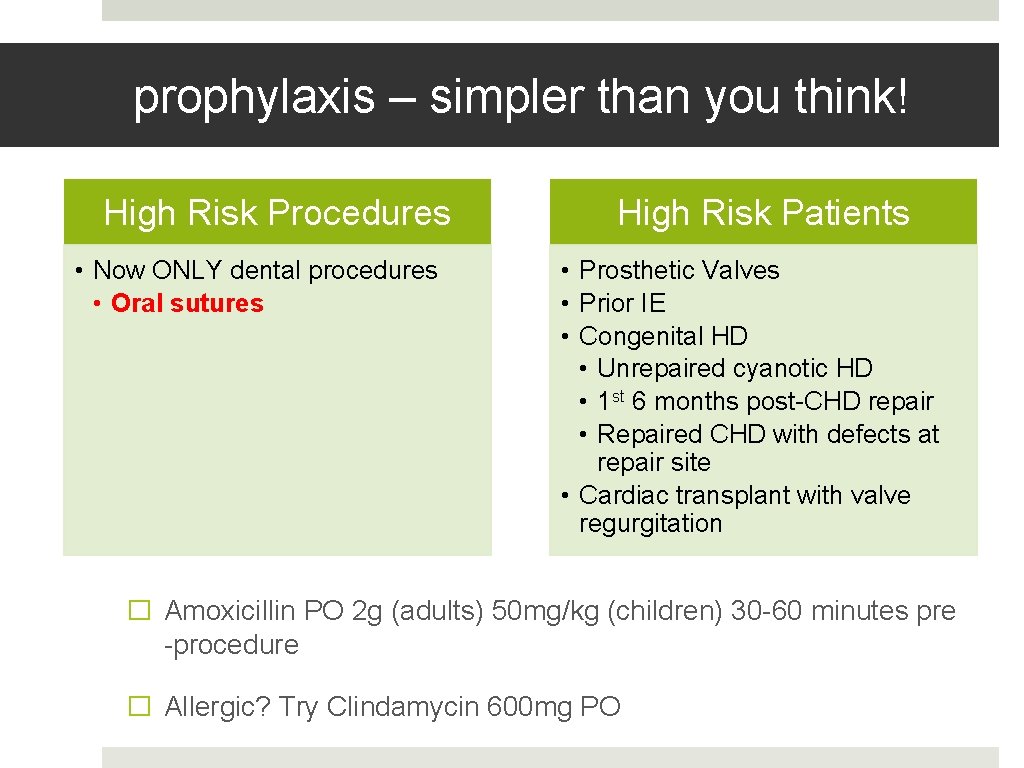
prophylaxis – simpler than you think! High Risk Procedures • Now ONLY dental procedures • Oral sutures High Risk Patients • Prosthetic Valves • Prior IE • Congenital HD • Unrepaired cyanotic HD • 1 st 6 months post-CHD repair • Repaired CHD with defects at repair site • Cardiac transplant with valve regurgitation � Amoxicillin PO 2 g (adults) 50 mg/kg (children) 30 -60 minutes pre -procedure � Allergic? Try Clindamycin 600 mg PO
aortic stenosis A few handy principles
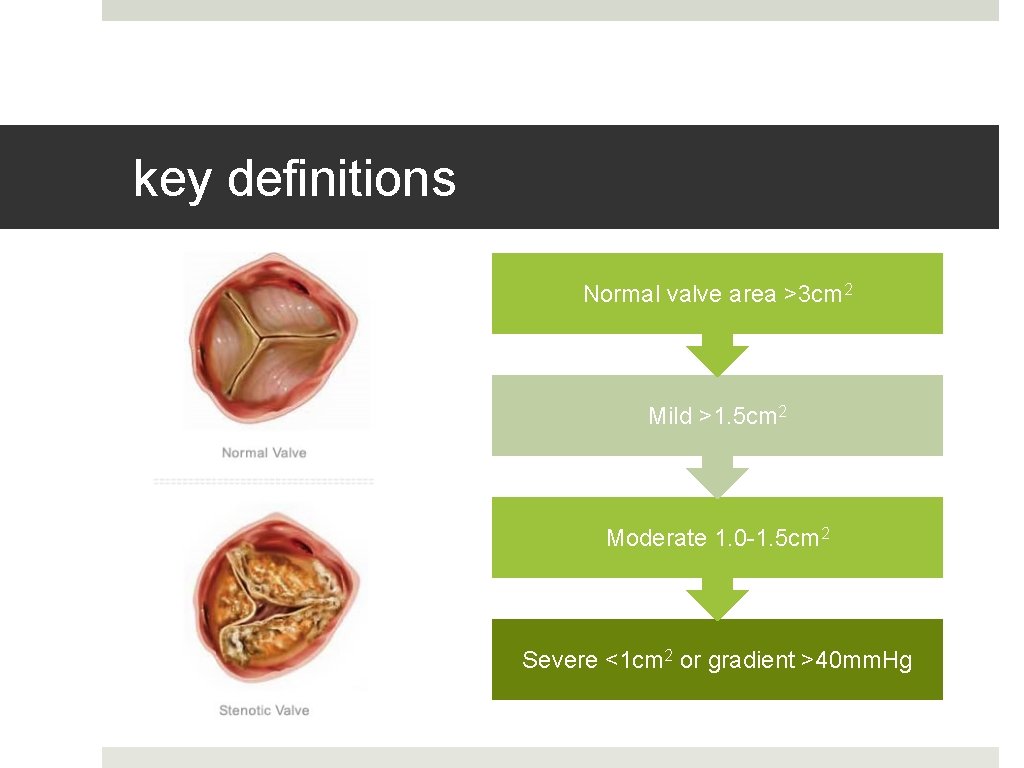
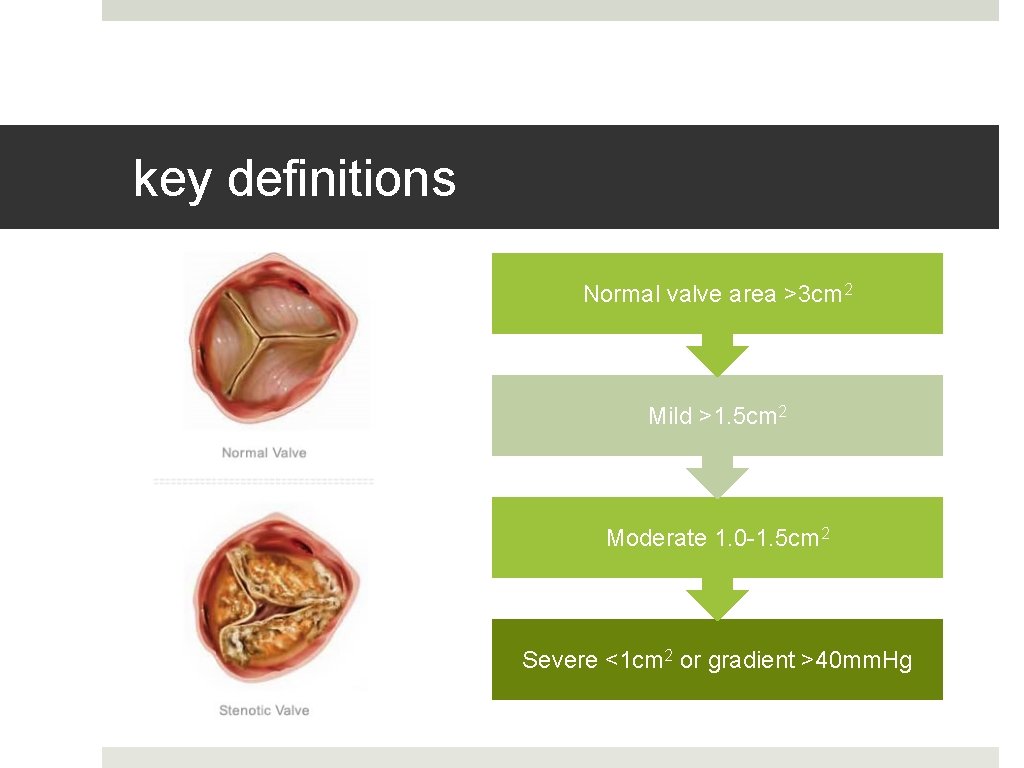
key definitions Normal valve area >3 cm 2 Mild >1. 5 cm 2 Moderate 1. 0 -1. 5 cm 2 Severe <1 cm 2 or gradient >40 mm. Hg
who gets it? By far 3 most common causes: • Calcific degeneration • Bicuspid aortic valve • Rheumatic disease
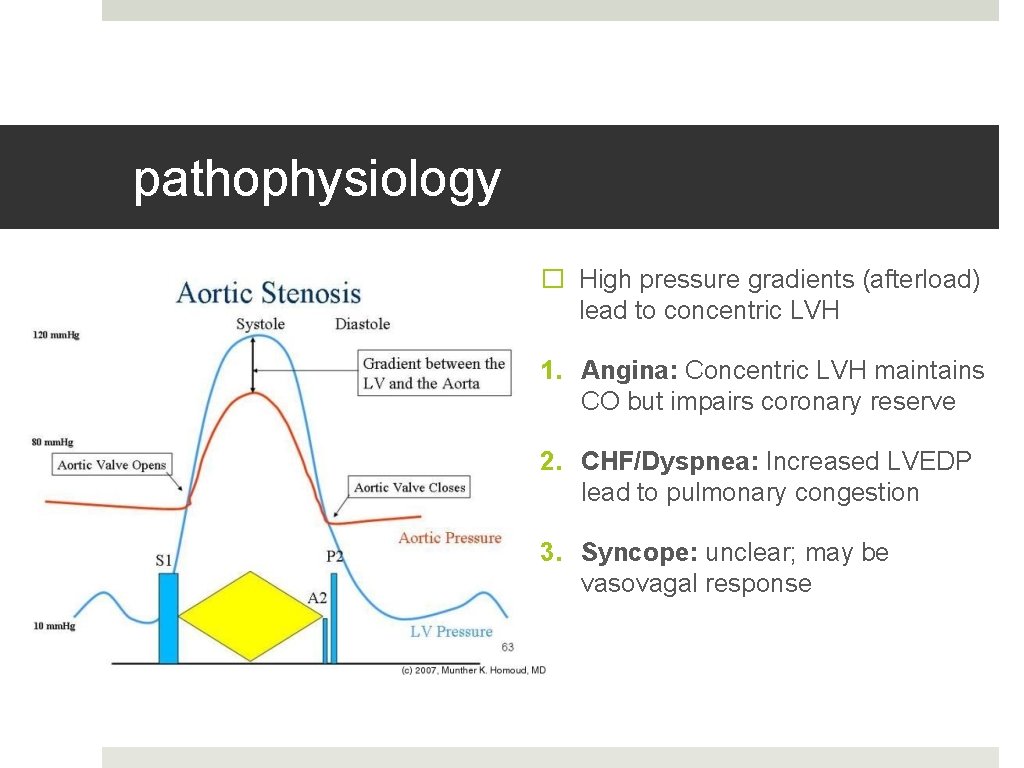
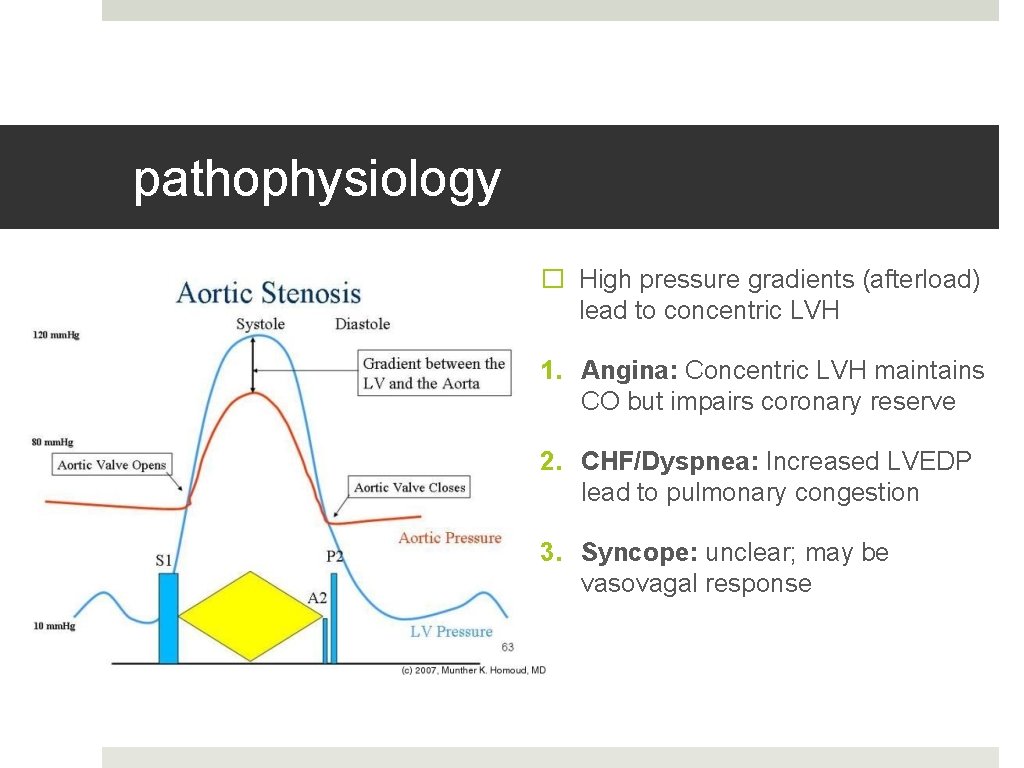
pathophysiology � High pressure gradients (afterload) lead to concentric LVH 1. Angina: Concentric LVH maintains CO but impairs coronary reserve 2. CHF/Dyspnea: Increased LVEDP lead to pulmonary congestion 3. Syncope: unclear; may be vasovagal response
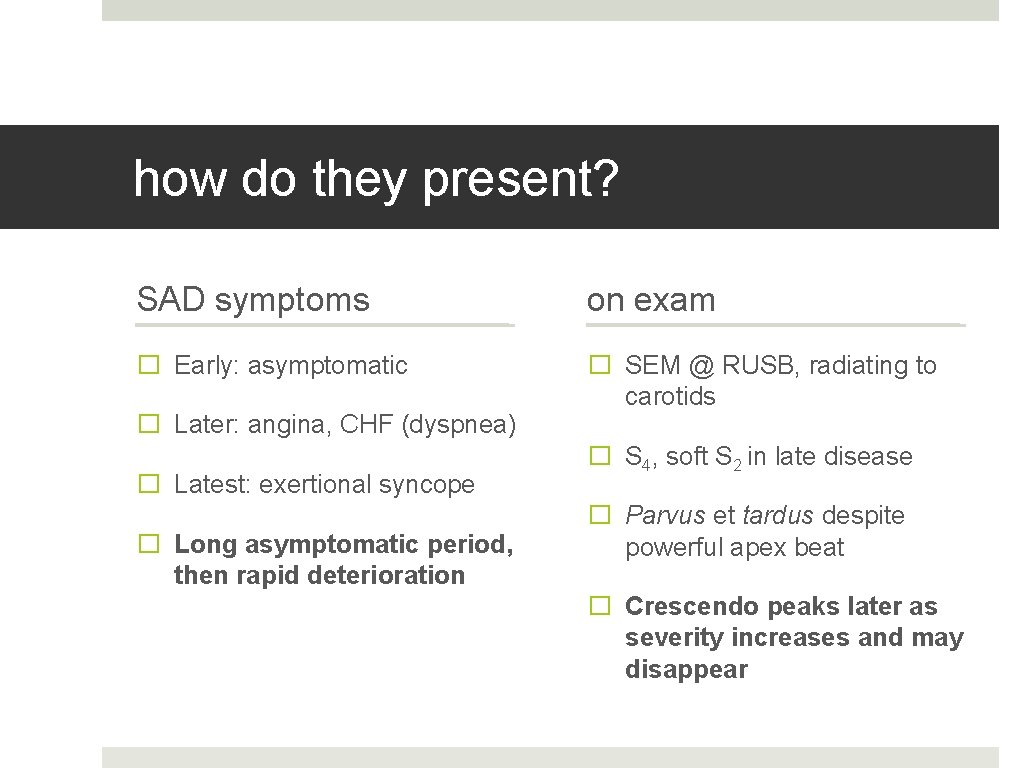
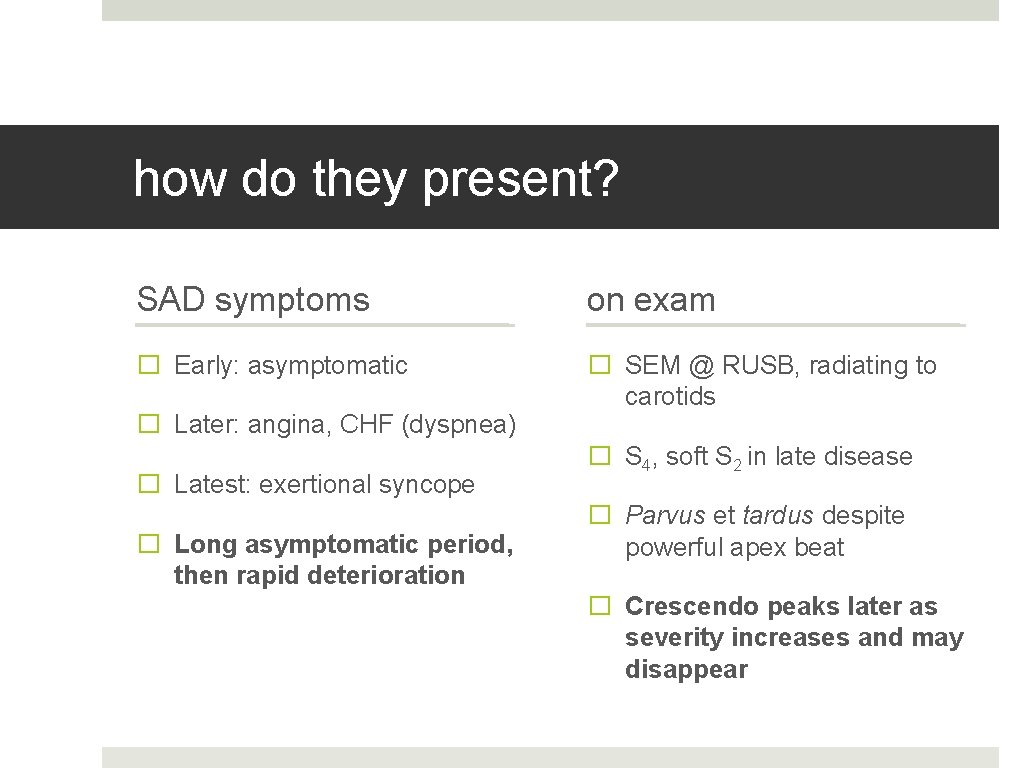
how do they present? SAD symptoms on exam � Early: asymptomatic � SEM @ RUSB, radiating to carotids � Later: angina, CHF (dyspnea) � Latest: exertional syncope � Long asymptomatic period, then rapid deterioration � S 4, soft S 2 in late disease � Parvus et tardus despite powerful apex beat � Crescendo peaks later as severity increases and may disappear
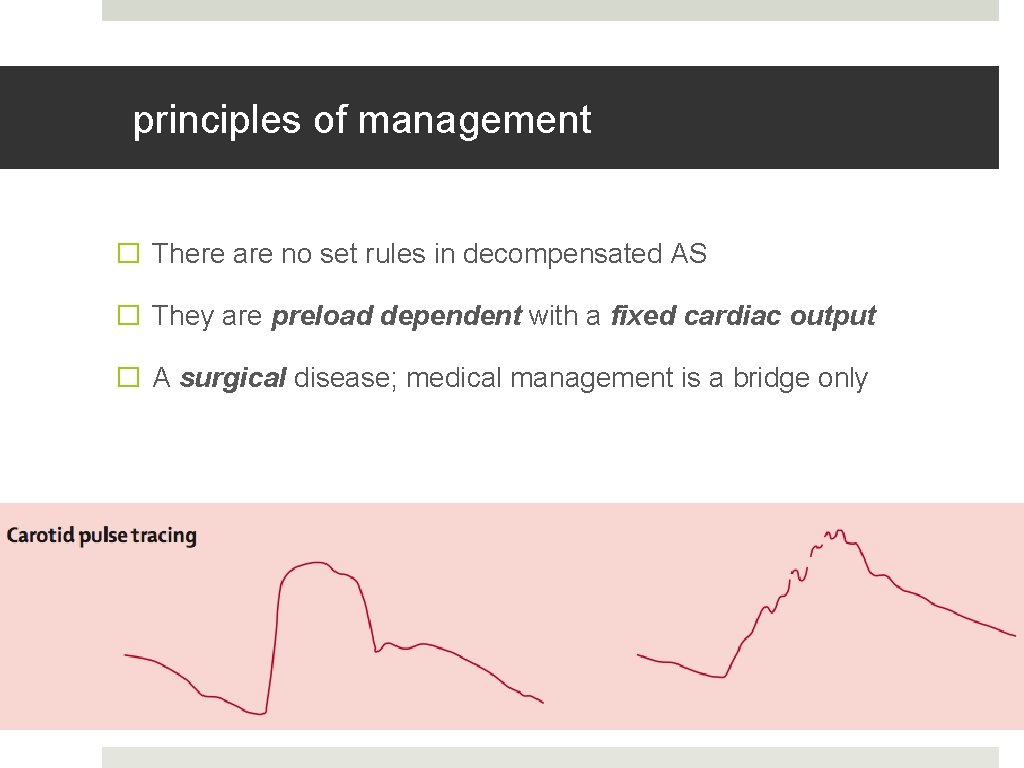
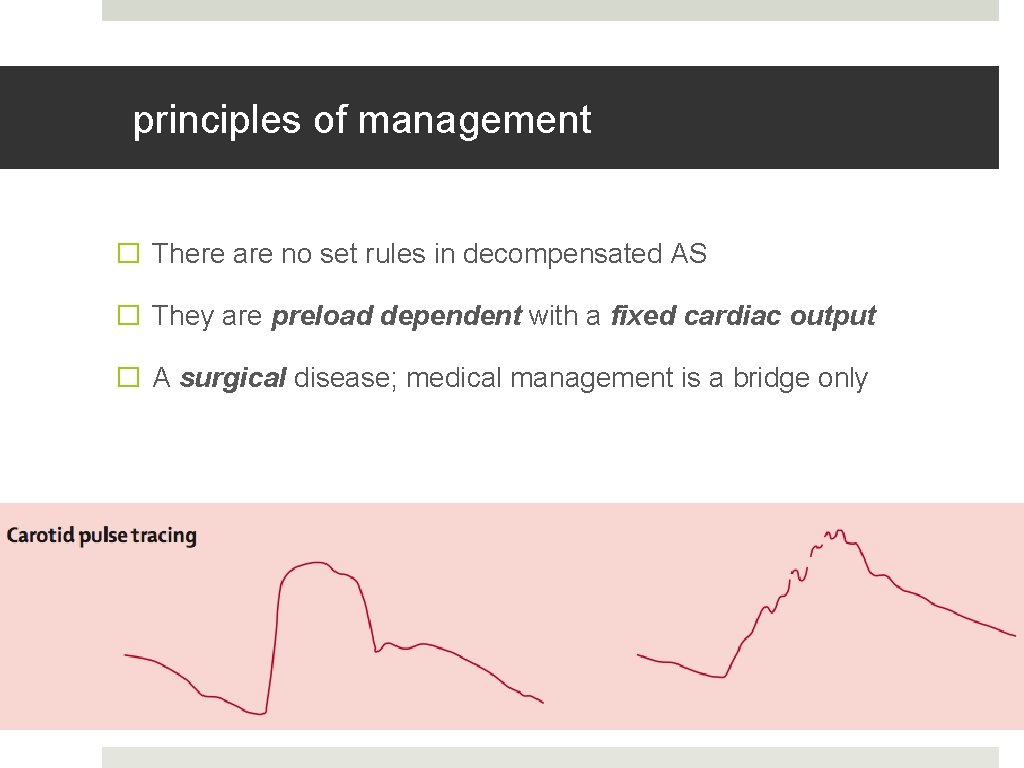
principles of management � There are no set rules in decompensated AS � They are preload dependent with a fixed cardiac output � A surgical disease; medical management is a bridge only
and the CHF patient with AS? � Vasodilation has a narrow therapeutic range � Bi. PAP, nitrates, and diuretics should be used cautiously � Use something titratable! � Evidence exists for Na-nitroprusside in ICU setting � Inotropic support for cardiogenic shock � Call CCU! They need definitive treatment.
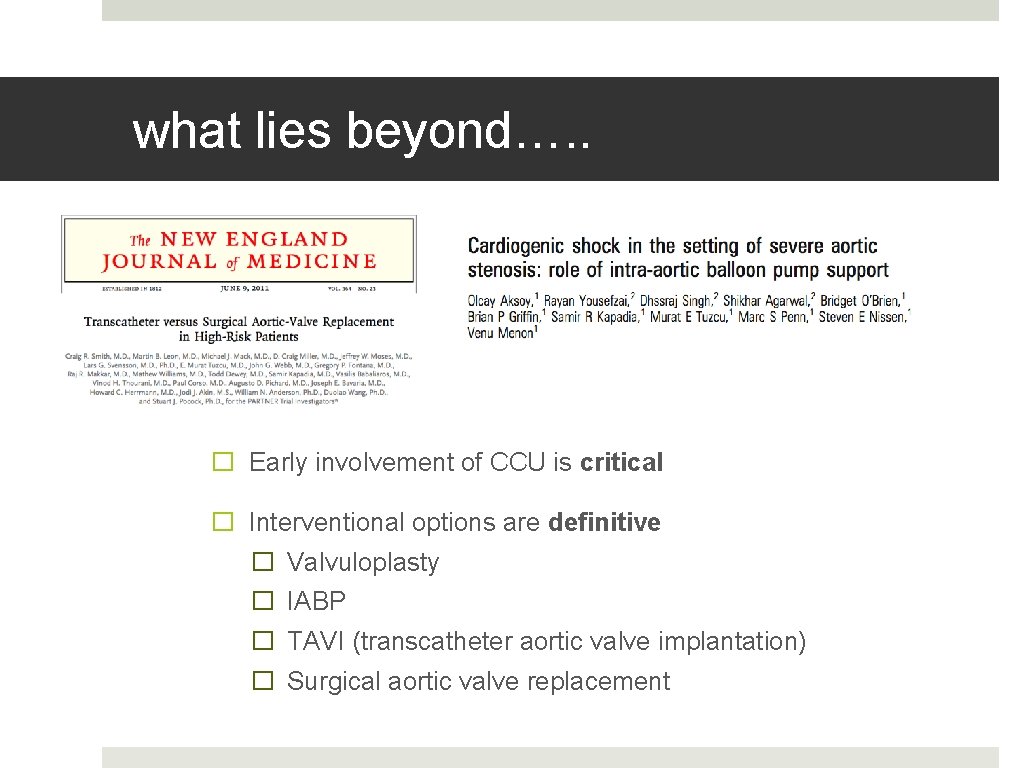
what lies beyond…. . � Early involvement of CCU is critical � Interventional options are definitive � Valvuloplasty � IABP � TAVI (transcatheter aortic valve implantation) � Surgical aortic valve replacement
which murmurs need workup? � Incidental murmurs are common in the ED � AHA 2006 Guidelines: � Diastolic � Continuous � Holosystolic � Late systolic � Ejection clicks � Radiation to neck or back
if you remember nothing else � Suspect IE in patients with fever/malaise and structural valvular disease � Examine hands, feet, and eyes! � 3 blood cultures, 3 different sites, at least 1 hr apart � Admit all suspected IE. If acute, obtain fast cultures and treat empirically (Vanco + Gent). � If SBE and stable, delay ABx until cultures return � Amoxil 2 g prophylaxis for oral procedures
… and for aortic stenosis � AS is a surgical disease � They are preload dependent with a fixed cardiac output � Medical management may hinder more than help � Get CCU involved quickly for decompensating patients
 Signs of infective endocarditis
Signs of infective endocarditis Infective endocarditis
Infective endocarditis Infective endocarditis
Infective endocarditis Heart pathology
Heart pathology Dukes criteria
Dukes criteria Janway lesion
Janway lesion Glumerolo
Glumerolo Infective endocarditis
Infective endocarditis Mitral regurgitation symptoms
Mitral regurgitation symptoms Site:slidetodoc.com
Site:slidetodoc.com Upper lobe vein diversion
Upper lobe vein diversion Dopamine uses
Dopamine uses Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Right sided heart failure
Right sided heart failure Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Causes of valvular heart disease
Causes of valvular heart disease Site:slidetodoc.com
Site:slidetodoc.com Fanta competitors
Fanta competitors Traslape valvular
Traslape valvular Carbomazine
Carbomazine Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Trichomonas vaginalis infective stage
Trichomonas vaginalis infective stage Infective stage
Infective stage Infective stage
Infective stage Ascaris lumbricoides infective stage
Ascaris lumbricoides infective stage Communicable disease and non communicable disease
Communicable disease and non communicable disease Libman sacks endocarditis echo
Libman sacks endocarditis echo Endocarditis
Endocarditis Criterios duke
Criterios duke Hacek endocarditis
Hacek endocarditis Sle libman sacks endocarditis
Sle libman sacks endocarditis Non bacterial thrombotic endocarditis
Non bacterial thrombotic endocarditis Criterios duke endocarditis infecciosa
Criterios duke endocarditis infecciosa Geoff grenier
Geoff grenier Icedip model of creative thinking
Icedip model of creative thinking Geoff hulten
Geoff hulten Geoff hollington
Geoff hollington Geoff squire
Geoff squire Geoff savage
Geoff savage Geoff wilson lexington ky
Geoff wilson lexington ky