Sensory Disorders Fall 2009 Sensory Disorders Topics Sensory
- Slides: 131
Sensory Disorders Fall 2009
Sensory Disorders: Topics • • • Sensory and The Effects of Aging Eyes and Vision Ears and Hearing Sensory (other) We will primarily discuss vision and hearing. The other senses, taste, smell and touch will be discussed briefly, in much less detail 3/6/2021 2
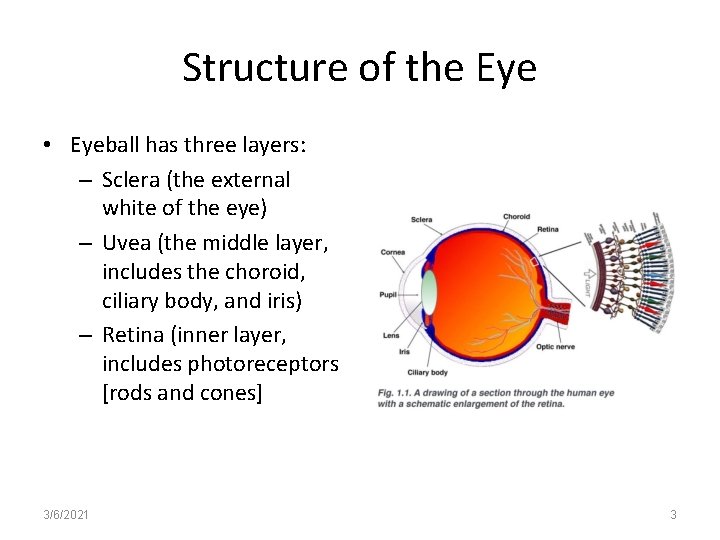
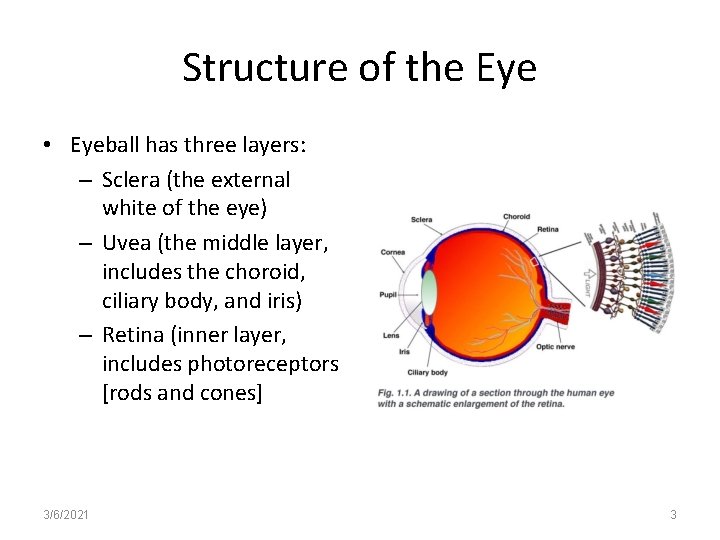
Structure of the Eye • Eyeball has three layers: – Sclera (the external white of the eye) – Uvea (the middle layer, includes the choroid, ciliary body, and iris) – Retina (inner layer, includes photoreceptors [rods and cones] 3/6/2021 3
Anatomy of the globe (eyeball) • The eyeball has several coverings: 1. Conjunctiva thin, single cell transparent layer that covers the eyeball and is continuous with the eyelids 2. Cornea is the outermost fibrous layer, covers the iris, transparent and avascular. Helps to focus light as it is curved. Most frequently transplanted tissue. The avascularity prevents circulating antibodies from attacking the transplant. Has pain fibers – response tears. 3/6/2021 4
Anatomy con’t 3. Sclera “hard” is the white part of the eye. Firm covering that maintains the shape of the globe; provides some protection to inner structures 4. Uvea is the middle, vascular layer – Iris the color portion of the uvea; contains circular (parasympathetic) muscles to constrict the pupil and radial (sympathetic) muscles to open the pupil. Legal & illegal drugs mimic the parasympathetic system • Iris acts like the shutter of a camera • Parasympathomimetics – Narcotics, adrenalize, pilocarpine – used in gluacoma to constrict the pupil. 3/6/2021 5
Anatomy con’t Ciliary body (2 nd most vascular)consists of ciliary muscles to change the shape of the lens and ciliary processes to secrete fluid that fills the eye. 5. Choroid provides vascular supply to retina 6. Retina inner (nervous) layer at back of eye; beginning of perception of light. Optic disc contains the blind spot, a single artery & single vein and is the egress for this retinal artery, vein, and Optic Nerve (CN II) 3/6/2021 6
Anatomy con’t • Retina con’t; – Contains 120 million rods, for photoreception; can see shades of gray, black & white, perceive movement and shapes; increase in number as one moves eye peripherally. Therefore, best vision in darkness is peripheral vision; a survival advantage against predators 3/6/2021 7
Anatomy con’t • Retina con’t – Retina also has 6 million cone-shaped photoreceptors; the color receptors; allow for color vision in bright light conditions; no colors are seen in dim light (night vision) because the cones do not function in dark conditions • 7. Maculae lutea (yellow spot) the direct center of the retina. Provides the clearest vision 3/6/2021 8
Anatomy con’t • Eyeball has 3 chambers – Anterior – between cornea and iris. Aqueous humor nourishes the lens. Canal of Schlemn regulates inraocular pressure. Glaucoma results when pressure builds up in the eyball either from overproduction of aqueous humor or failure of the canal of Schlemn. – Posterior between the iris and the lens – Vitreous between the lens and retina – filled with vitreous, a jelly-like substance 3/6/2021 9
Anatomy con’t • The eye is a hollow organ. For the eye to function properly, the gel in the posterior segment (vitreous humor) and the fluid in the anterior segment (aqueous humor) must be present in set amounts that apply pressure inside the eye to keep it ballshaped. • Once eye growth is complete, the gel (vitreous) does not change in volume, however the aqueous humor is continuously made from blood plamsa. 3/6/2021 10
Anatomy con’t • The eye has the following accessories: – Palpebrae (pal-pee-bry) are the eyelids which spread tears and protect eye from trauma – Eyelashes filter dust and debris and signal their approach – Lacrimal glands and lacrimal ducts. The glands produce 1 ml of fluid/day, which drains into nose (why your nose runs when you cry) 3/6/2021 11
Anatomy con’t • Six extrinsic eye muscles – Lateral and medial rectus muscles control lateral (outside) and medial (toward midline) movements. – Inferior and superior obliques control rotational, upward and downward movement. Eyes rotate slightly to keep perception on the horizon relatively flat – Superior and inferior rectus for upward and dwonward movement – Controlled by CN III, IV, VI; provide finest motor control in body • To supress blurring, the brain directs the eyes to pick a fixed point in a moving landscape, follow it until it disappears, then pick another point. (like watching a speeding train go by). This is called nystagmus (quick-skip-quick-skip). • Abnormal nystagmus can indicate brain damage. 3/6/2021 12
Structure of the Eye • Cornea - the clear, dome-shaped tissue covering the front of the eye. • Iris - the colored part of the eye - it controls the amount of light that enters the eye by changing the size of the pupil • Lens - a crystalline structure located just behind the iris - it focuses light onto the retina • Optic nerve - the nerve that transmits electrical impulses from the retina to the brain 3/6/2021 13
Structure of the Eye • Pupil - the opening in the center of the iris- it changes size as the amount of light changes (the more light, the smaller the hole) • Vitreous - a thick, transparent liquid that fills the center of the eye - it is mostly water and gives the eye its form and shape (also called the vitreous humor or aqueous humor) 3/6/2021 14
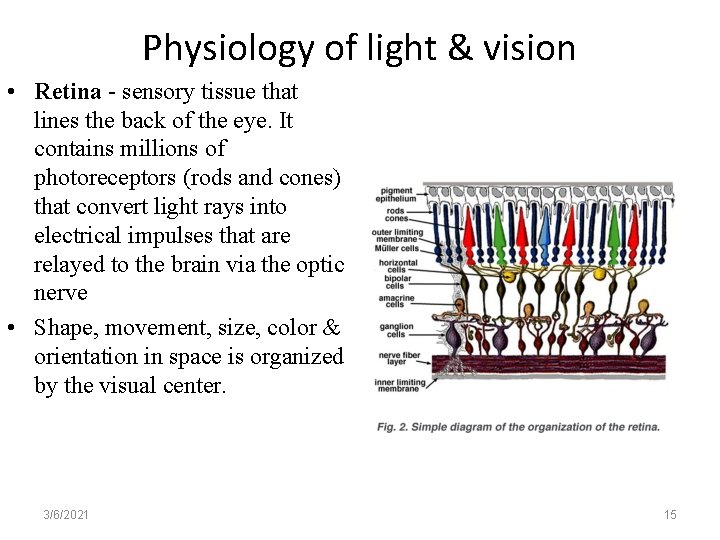
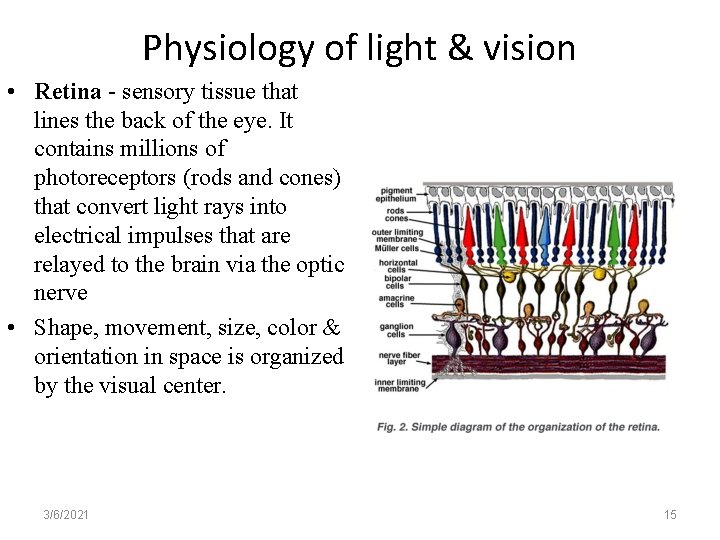
Physiology of light & vision • Retina - sensory tissue that lines the back of the eye. It contains millions of photoreceptors (rods and cones) that convert light rays into electrical impulses that are relayed to the brain via the optic nerve • Shape, movement, size, color & orientation in space is organized by the visual center. 3/6/2021 15
Cont from prior page • Light strikes the retina, stimulating the rods and cones • Photoreceptors convert light energy into chemical energy (photons) • Chemical energy is converted into nerve conduction • Chemical action is Vitamin A dependent for renewal • The signal finally reaches the neurons in the optic nerve (CN II) to the brain • The rods tend to converge into one nerve cell and thus offer better vision in dim light (movement) at the cost of blurring shapes • The cones tend to have one nerve each and therefore, give sharper images (resolution) in color while sacrificing sensitivity. 3/6/2021 16
Eye Function • Eye function consists of – Refraction – Pupil constriction – Accommodation – Convergence • Portion of the trigeminal nerve (CN V) stimulates blinking when the cornea is touched • CN VII (facial nerve) innervates tear glands and the muscles associated with closing the eyelid 3/6/2021 17
Refraction • Refraction (the bending of light to focus images on the retina) • Hyperopia (farsightedness) – Inability of the eye to adequately refract (break-up) light – Eyeball may be too short or the cornea have too little curvature – Objects at a distance are seen clearly; close objects are blurred • Myopia (nearsightedness) • Astigmatism 3/6/2021 18
Refraction • Myopia (nearsightedness) – Objects at a distance are blurred; close objects are seen clearly – Eyeball may be too long or the cornea have too much curvature – Light coming into the eye does not focus correctly creating a blurred image of distant objects • Astigmatism – Uneven surface on, or in the eye (esp the cornea) which distorts vision 3/6/2021 19
Pupil Constriction • Constriction and dilation control the amount of light that enters the eye. • If the level of light to one or both eyes is increased, both pupils constrict. • The amount of constriction depends on how much light is available and how well the retina can adapt to light changes • Constriction (miosis); dilation (mydriasis) 3/6/2021 20
Accommodation • Allows the healthy eye to focus images sharply on the retina whether the image is close or far away • The process of maintaining a clear visual image when gaze is shifted from distant to near object is known as accommodation. • The eye can adjust its focus by changing the shape of the lens 3/6/2021 21
Convergence • Ability to turn both eyes inward toward the nose to ensure only a single image of close objects is seen. 3/6/2021 22
Treatment of Common Refractory Errors • Corrective glasses • Contact lenses • Refractory surgery - Photorefractive keratectomy (PRK) - Laser-in-situ keratomileusis (LASIK) 3/6/2021 23
Structural Changes of the Eye Related to Aging • Appearance of the eye – Arcus senilis (a product of hyperlipidemia; bluish white ring around the cornea); does not affect vision – Sclera takes on a yellowish (r/t fat deposits) or bluish hue (do not confuse w/jaundice in elderly – look for other S&S of jaundice such as skin, liver enzymes) • Cornea – With aging, flattens. Result is blurred and distorted vision 3/6/2021 24
Structural Changes of the Eye Related to Aging • Ocular muscles – Strength decreases – pt must refocus to maintain a single image • Lens – Hardens and becomes compact (Cataracts) – wear corrective lenses • Iris – Decreased ability to dilate – need better lighting – Smaller pupil – Poor adaptation to darkness 3/6/2021 25
Structural Changes of the Eye Related to Aging • Pupil – Size is smaller; Reduced ability to see in dim light • Color Vision – Ability to differentiate between colors of short wavelength (green, blue, violet) decreases • Tears – Diminished tearing – Dry eyes – Risk for infection – Discomfort 3/6/2021 26
Structural Changes of the Eye Related to Aging • Presbyopia • Lens yellows with age, aging lens hardens, shrinks and loses elasticity. Loss of elasticity results in loss of accommodation-must hold objects away to focus; narrow field of vision – Reading glasses! 3/6/2021 27
Assessment of the Eyes: Overview • History – Obtain subjective data • Demographic data – Age is a biggie! – Why? • Family history and genetic risk – Sometimes relevant • Personal history – Any systemic problems that can be r/t eye/vision problem? – Taking decongestants and antihistamines? (May dry eyes and increase IOP) 3/6/2021 28
Considerations for the Elderly • Health history – Chronic conditions may have an adverse effect on vision – Examples: diabetes; cataracts; others? • Medications – Antihistamines and decongestants (dry eyes) – Blurred or double vision (diplopia) 3/6/2021 29
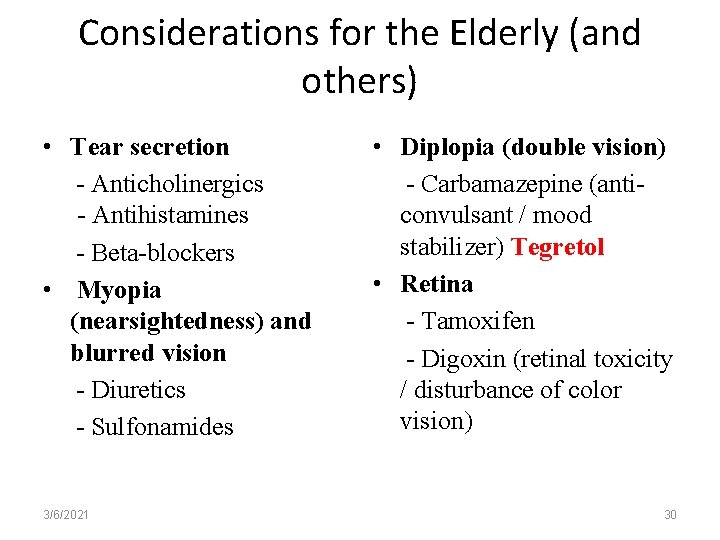
Considerations for the Elderly (and others) • Tear secretion - Anticholinergics - Antihistamines - Beta-blockers • Myopia (nearsightedness) and blurred vision - Diuretics - Sulfonamides 3/6/2021 • Diplopia (double vision) - Carbamazepine (anticonvulsant / mood stabilizer) Tegretol • Retina - Tamoxifen - Digoxin (retinal toxicity / disturbance of color vision) 30
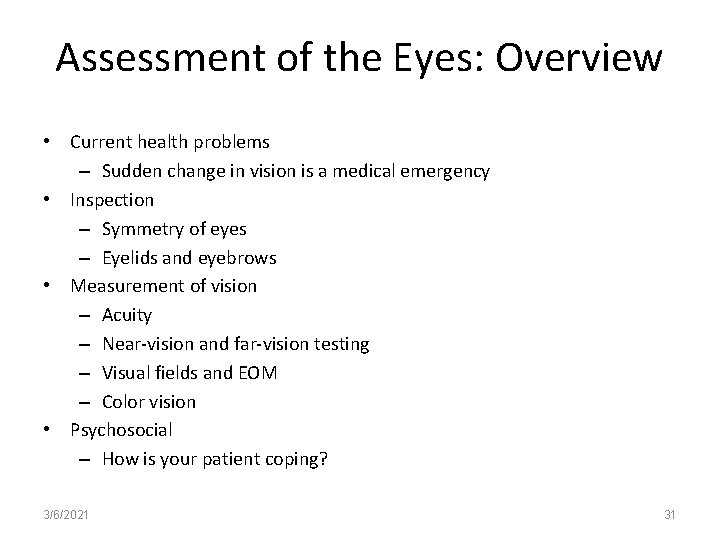
Assessment of the Eyes: Overview • Current health problems – Sudden change in vision is a medical emergency • Inspection – Symmetry of eyes – Eyelids and eyebrows • Measurement of vision – Acuity – Near-vision and far-vision testing – Visual fields and EOM – Color vision • Psychosocial – How is your patient coping? 3/6/2021 31
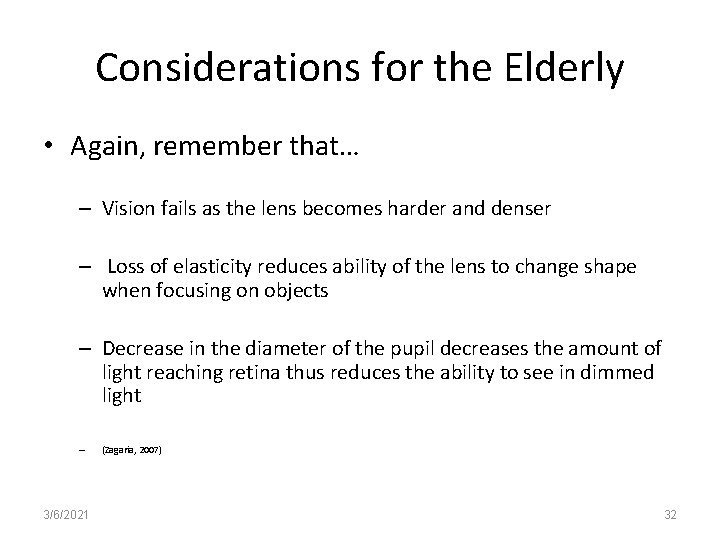
Considerations for the Elderly • Again, remember that… – Vision fails as the lens becomes harder and denser – Loss of elasticity reduces ability of the lens to change shape when focusing on objects – Decrease in the diameter of the pupil decreases the amount of light reaching retina thus reduces the ability to see in dimmed light – 3/6/2021 (Zagaria, 2007) 32
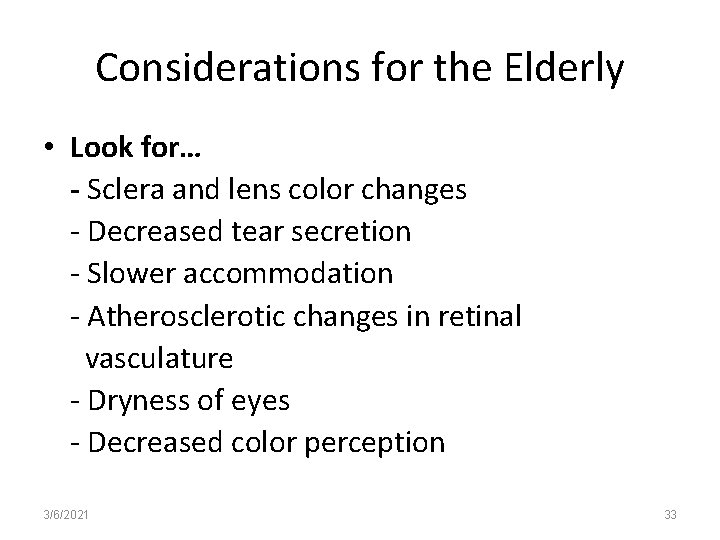
Considerations for the Elderly • Look for… - Sclera and lens color changes - Decreased tear secretion - Slower accommodation - Atherosclerotic changes in retinal vasculature - Dryness of eyes - Decreased color perception 3/6/2021 33
Nursing Considerations • Safe and effective care environment • Health promotion and maintenance • Psychosocial Integrity – Partial or complete vision loss – Use of support groups and local resources – Diagnostic procedures and follow up care • Physiologic Integrity 3/6/2021 34
Assessment of the Eye • Assess if patient has problems with eyes/vision • Acuity – Measures distance and near vision – Snellen chart used to measure distance (20 feet from chart) – Rosenbaum pocket vision tests near vision (use in patients over 40 years of age-hold card @14 ft) – Why? • Confrontational Test – Tests peripheral vision 3/6/2021 35
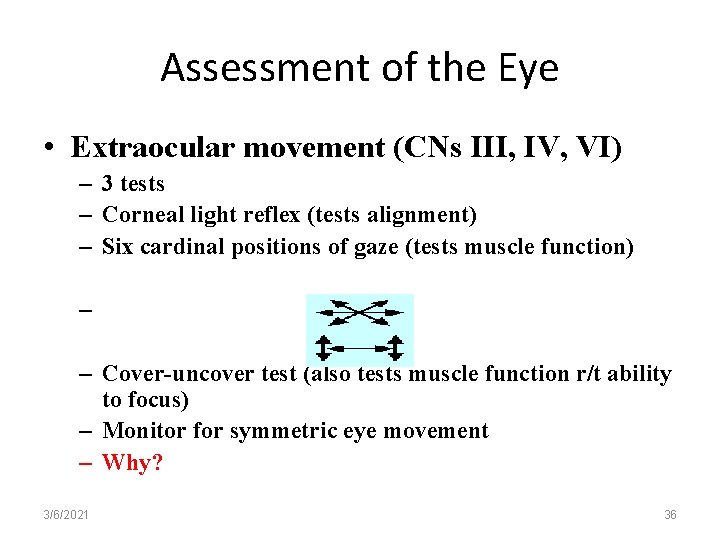
Assessment of the Eye • Extraocular movement (CNs III, IV, VI) – 3 tests – Corneal light reflex (tests alignment) – Six cardinal positions of gaze (tests muscle function) – – Cover-uncover test (also tests muscle function r/t ability to focus) – Monitor for symmetric eye movement – Why? 3/6/2021 36
Assessment of the Eye • • Culture and smear of corneal or conjunctival swaps to Dx infection Ophthalmoscopy (Permits viewing of external and internal eye structures Slit lamp microscopy (Uses microscopic technology to examine anterior ocular structures) Tonometry (Tool used to measure IOP. Normal IOP: 10 to 21 mm Hg) – When might IOP be higher during the day? Corneal staining (Used as evaluation tool in cases of trauma; foreign bodies; ulcers; abrasions) CT scan (useful in examining the EOMs; bony structures and eye itself, can detect tumor) MRI (replaced CT for examining optic nerve and orbit) 3/6/2021 37
Assessment of the Eye – Common Abnormalities • Hordeolum – “stye” – Inflammation of gland – Caused by bacterial infection (staph and strep) – Tx w/ warm compresses and antibacterial ointment • Chalazion – Swollen sebaceous gland of eyelid r/t block in gland’s duct – Tx w/ warm compress, antibacterial ointment, surgery • Blepharitis – Inflammation of the eyelids – Can be associated with having dandruff of the scalp – Tx w/ anti-tear shampoo, warm compress 3/6/2021 38
Assessment of the Eye – Common Abnormalities • Ptosis – Drooping of the upper eyelid – Can be r/t disorder of oculomotor nerve (CN III) • Hemorrhage – traumatized blood vessel, usually well defined bright red area in conjunctiva. Resolves on own • Conjunctivitis – (pink eye) – – – 3/6/2021 Inflammation of conjunctiva – edema, burning, itching, tears Viral or bacterial – easily transmitted from person to person Staph, H. Influenza, Pseudomonas Tx with topical antibiotics, handwashing Caused by allergy (pollen; animal dander; dust) 39
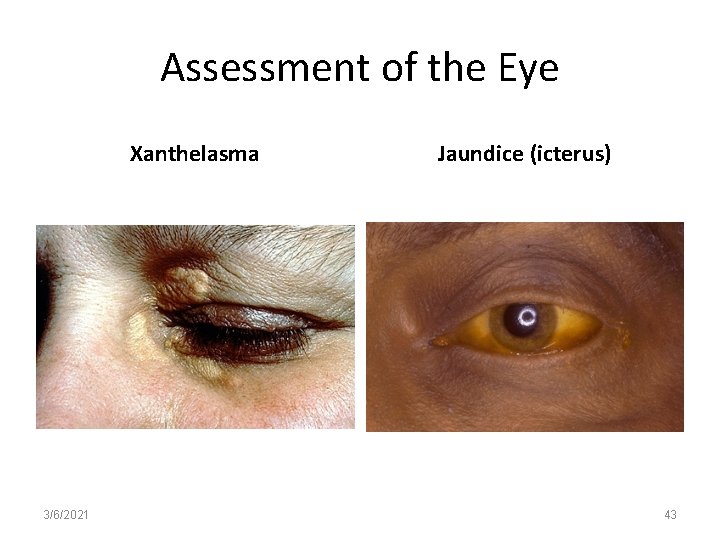
Assessment of the Eye – Common Abnormalities • Jaundice – Hepatitis – Yellowish color is a normal variant in elderly • Arcus senilus – Grayish line (ring-like) in the periphery of cornea – Common in elderly (fatty deposits) – Abnormal finding in younger individuals (hyperlipidemia) • Exophthalmos – Protrusion of eyeballs – Associated with hyperthyroidism 3/6/2021 40
Assessment of the Eye – Common Abnormalities • Heterochromia – Different eye color – Congenital or r/t inflammation; tumor of iris • Strabismus – Abnormal alignment of the eyes What else to know… Legal blindness is defined as a visual acuity of 20/200 or less in the better eye with the best correction possible 3/6/2021 41
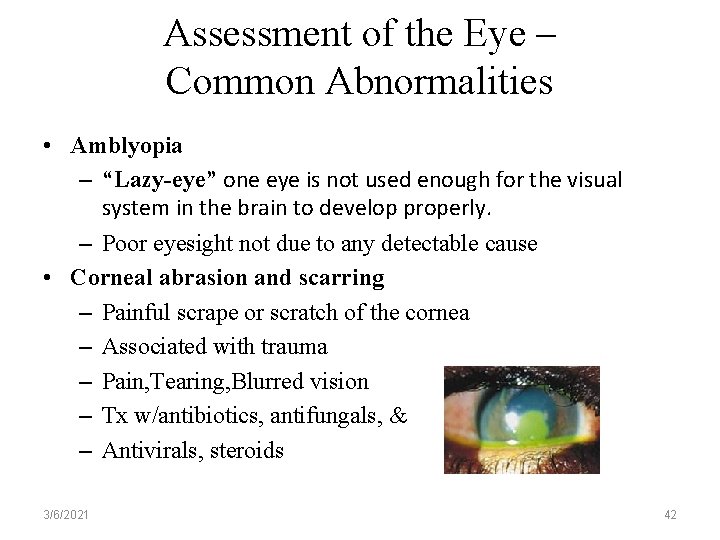
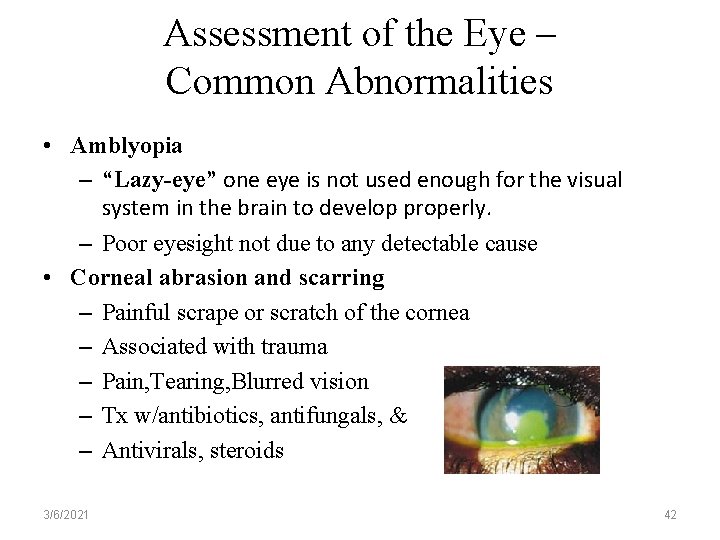
Assessment of the Eye – Common Abnormalities • Amblyopia – “Lazy-eye” one eye is not used enough for the visual system in the brain to develop properly. – Poor eyesight not due to any detectable cause • Corneal abrasion and scarring – Painful scrape or scratch of the cornea – Associated with trauma – Pain, Tearing, Blurred vision – Tx w/antibiotics, antifungals, & – Antivirals, steroids 3/6/2021 42
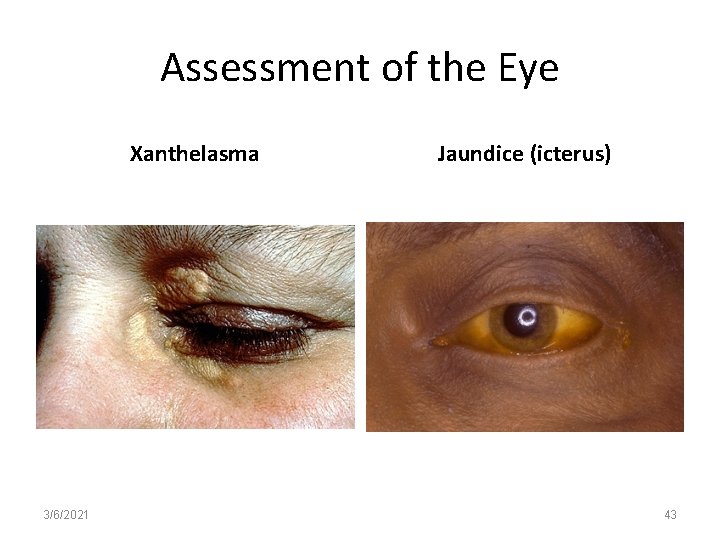
Assessment of the Eye Xanthelasma 3/6/2021 Jaundice (icterus) 43
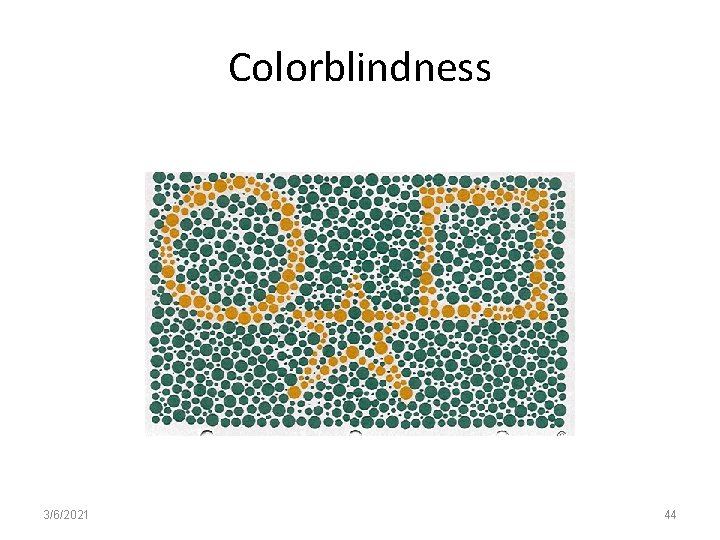
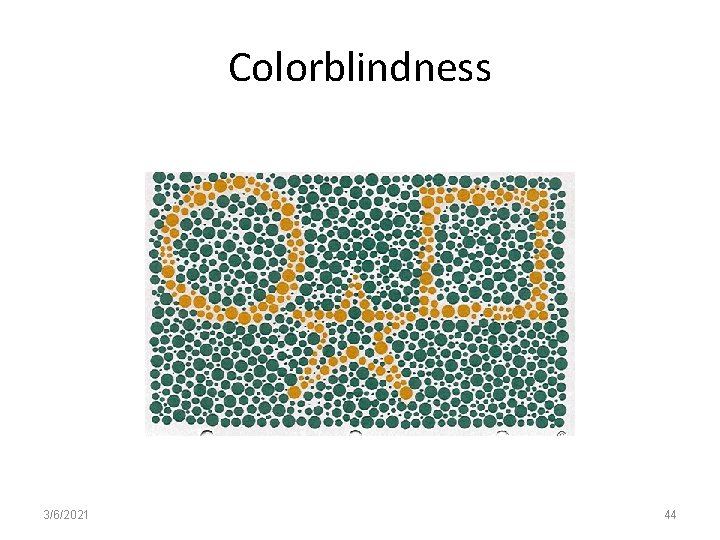
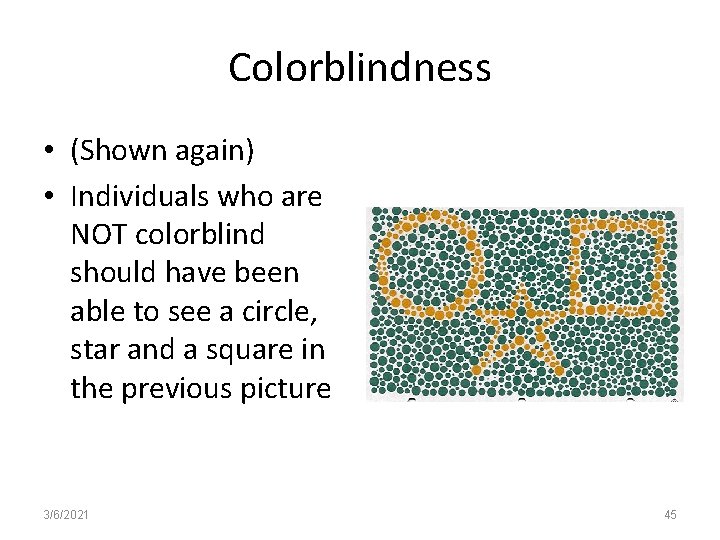
Colorblindness 3/6/2021 44
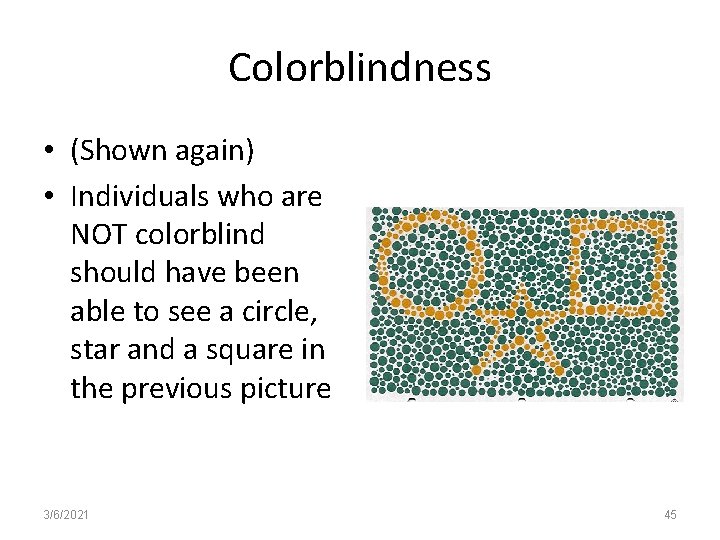
Colorblindness • (Shown again) • Individuals who are NOT colorblind should have been able to see a circle, star and a square in the previous picture 3/6/2021 45
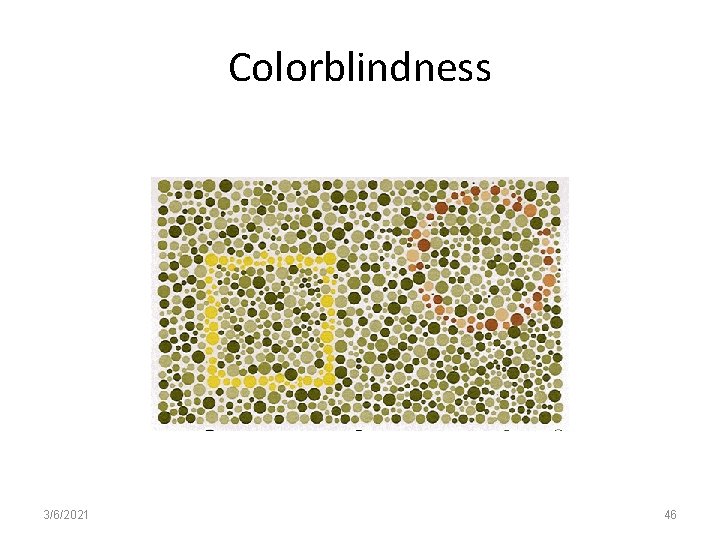
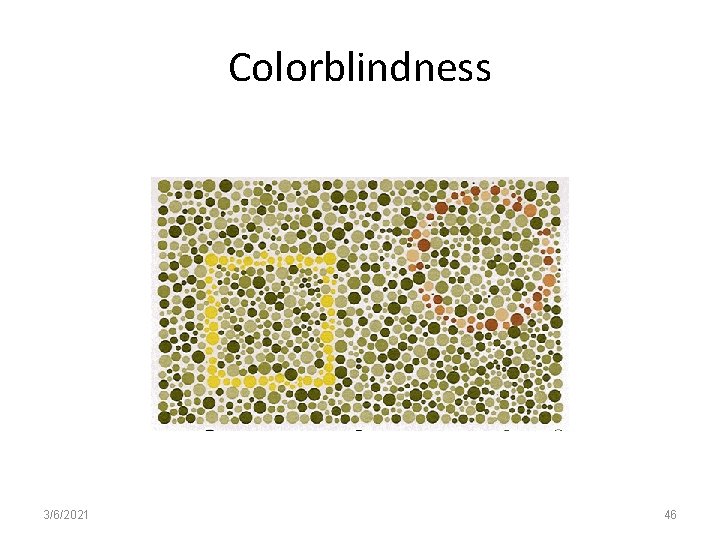
Colorblindness 3/6/2021 46
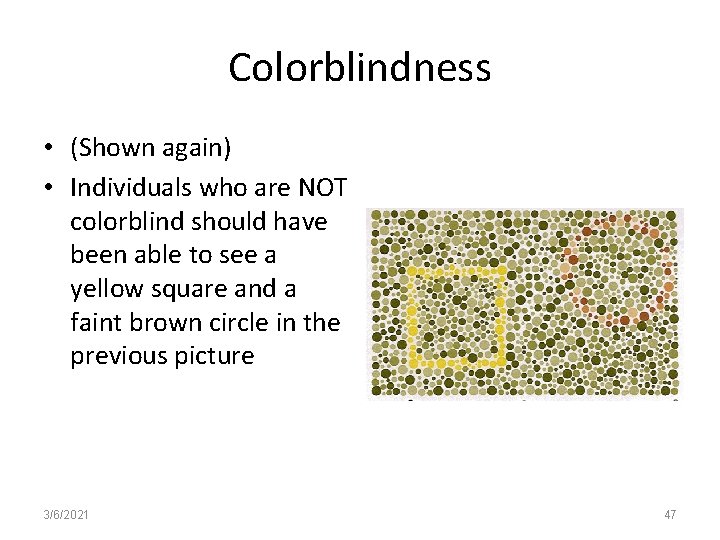
Colorblindness • (Shown again) • Individuals who are NOT colorblind should have been able to see a yellow square and a faint brown circle in the previous picture 3/6/2021 47
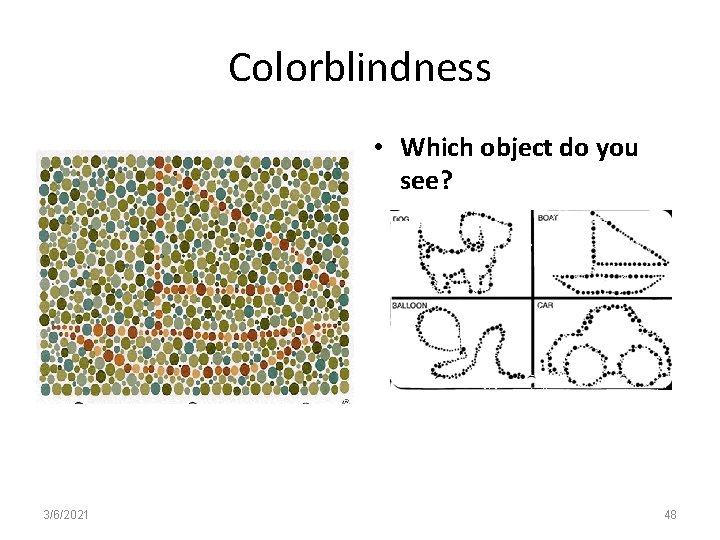
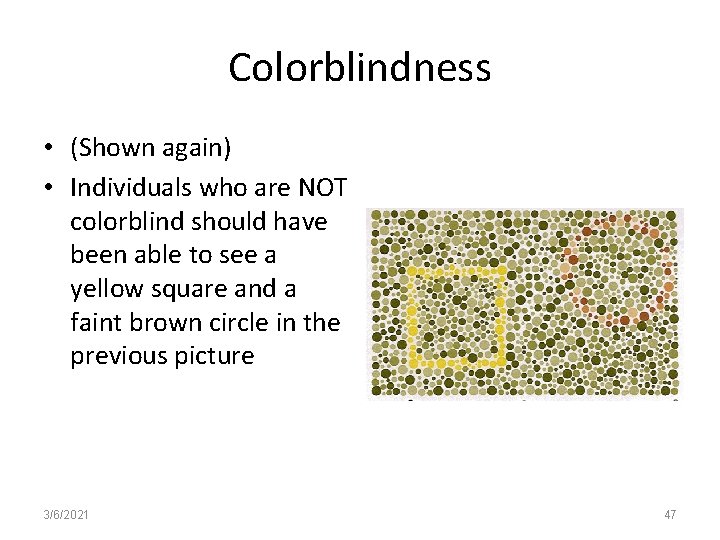
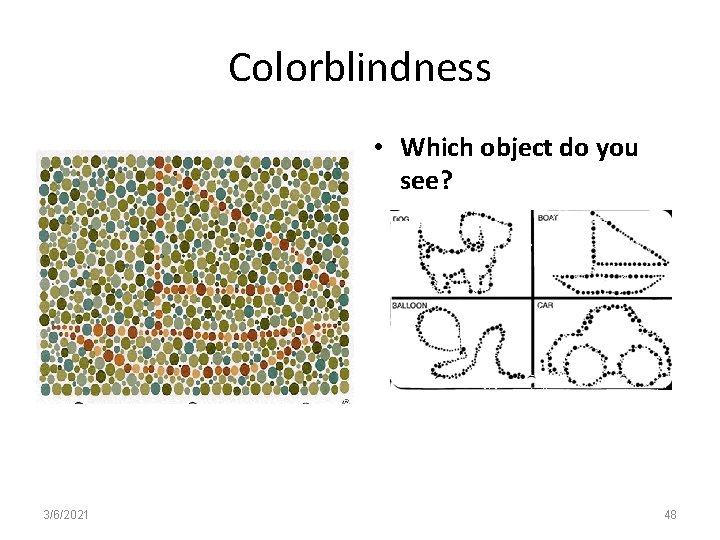
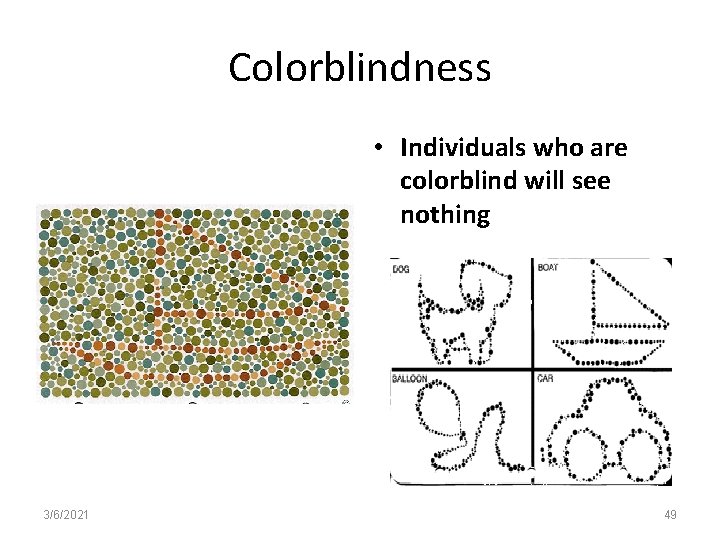
Colorblindness • Which object do you see? 3/6/2021 48
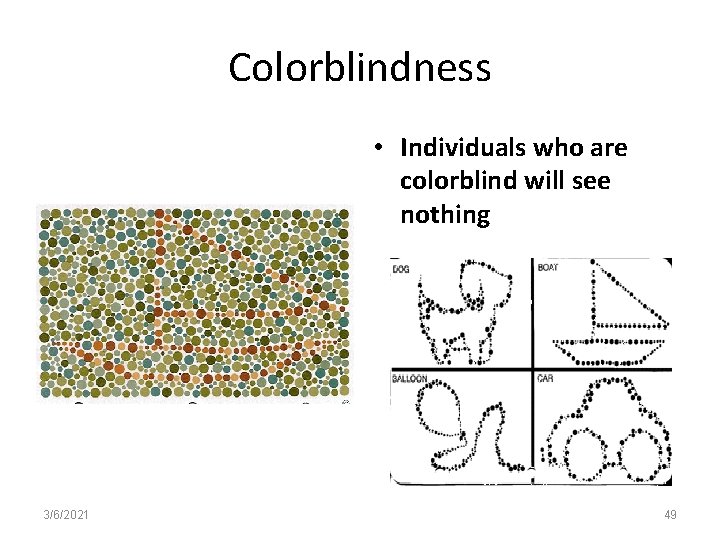
Colorblindness • Individuals who are colorblind will see nothing 3/6/2021 49
Eye Trauma • Etiology Traumatic hyphema (bleeding in the eye) - Penetrating injury Chemical (acidic p. H< 4; alkaline p. H > 10) exploded car batteries - Thermal (destroys rods and cones) - Enucleation • Treatment - Corneal transplant (for clouding; scarring) 3/6/2021 50
Cataracts • An opacity or clouding of the crystalline lens that blocks the passage of light needed for vision, distorts image projected onto retina • Is the 3 rd leading cause of blindness in the US • Etiology • - Aging • - Congenital • - Traumatic • - Secondary to UV exposure, steroids, DM • The lens will enlarge causing increased IOP resulting in Glaucoma 3/6/2021 51
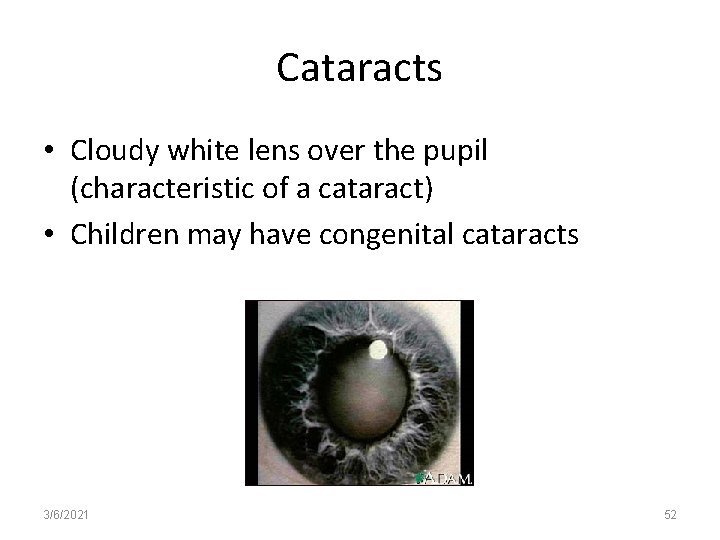
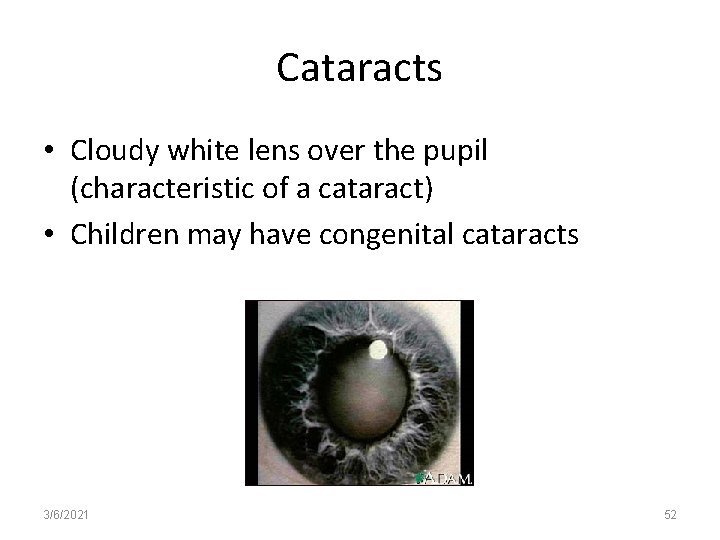
Cataracts • Cloudy white lens over the pupil (characteristic of a cataract) • Children may have congenital cataracts 3/6/2021 52
Cataracts - Assessment • • Opacity or cloudy white pupil Decreased vision Glare Obliteration of parts of images Decreased perception of color Distorted images Photophobia (sensitivity to light) 3/6/2021 53
Cataracts - Treatment • Non-surgical – Reading glasses – Increased lighting • Surgical - outpatient – Removal of cataract (extracapsular extraction) with implantation of intraocular lens (IOL) 3/6/2021 54
Cataracts – Post-op Patient Education • Elevate HOB 30 -45 degrees immediately post-op; Eye drops (antibiotics, steroids, analgesic) several times/day for 2 -4 weeks • ADLs are resumed as the patient feels able • Instruct on methods to prevent increased IOP – – – 3/6/2021 Do not sleep on operated side for 3 -4 weeks Avoid rubbing; protect the eyes with patch/sunglasses Do not bend over below waistline Avoid heavy physical activity x 6 weeks Avoid sneezing, coughing, straining, vomiting Assess appearance of eye 55
Cataracts – Post-op Patient Education • Notify if… – Redness of the eye increases or eye pain is severe – If discharge from eye increases or changes color (to greenish) – Vision decreases – Alert patient that vision may not be “normal” immediately after surgery 3/6/2021 56
Glaucoma • Second leading cause of blindness • May damage the eye without the person being aware of it • Characterized by increased IOP (NL 10 -21 mm Hg) associated with progressive loss of peripheral vision • Cupping of the optic disc and optic nerve destruction • Progressively destroys the optic nerve 3/6/2021 57
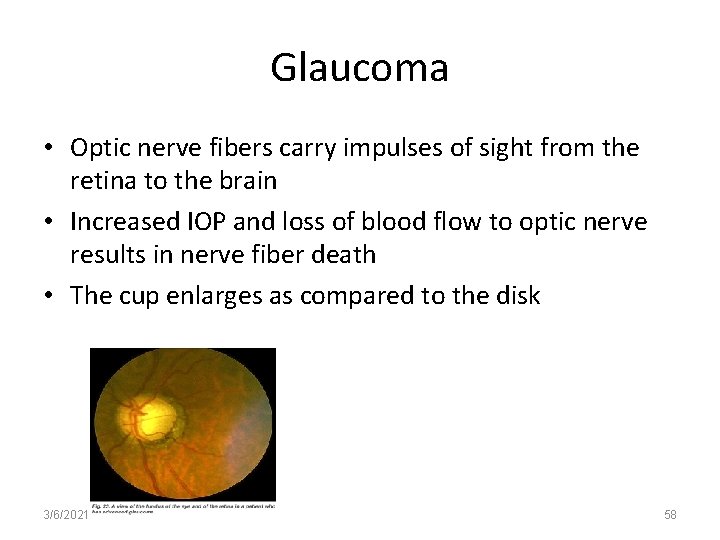
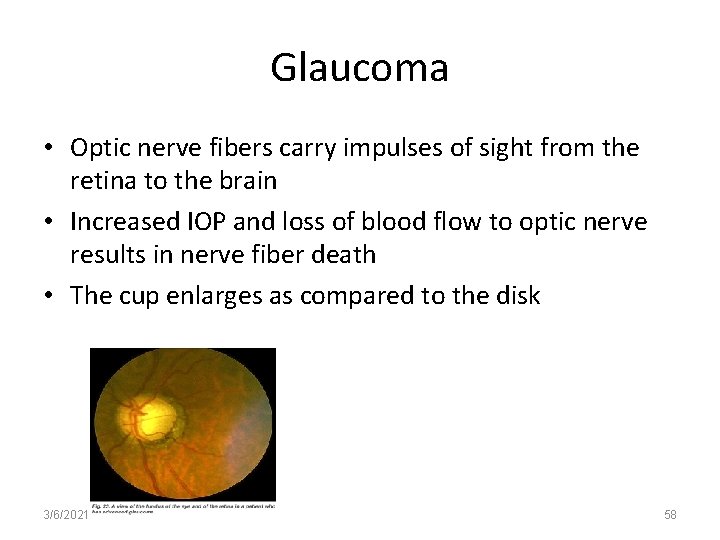
Glaucoma • Optic nerve fibers carry impulses of sight from the retina to the brain • Increased IOP and loss of blood flow to optic nerve results in nerve fiber death • The cup enlarges as compared to the disk 3/6/2021 58
Types of Glaucoma • Primary/Chronic Open Angle (90%) – Caused by a reduction in the outflow of aqueous humor due to obstruction in trabecular meshwork – Develops slowly; no symptoms • Primary/Chronic Closed Angle – Outflow of aqueous humor is impaired due to narrowing of the angle between the iris and cornea • Acute Closed Angle – Sudden onset, severe eye pain; nausea and vomiting; colored halos; blurred vision; ocular redness. MEDICAL EMERGENCY 3/6/2021 59
Primary/Chronic Open-Angle Glaucoma • Symptoms – Frequent change in eye glasses without any improvement in vision – Inability of eyes to adjust to darkened rooms – Loss of peripheral vision – Rainbow colored rings around lights – Persistent dull eye pain – Headaches 3/6/2021 60
Primary/Chronic Open-Angle Glaucoma • Diagnosis – Tonometry • Normal pressure 10 -21 mm. Hg • For glaucoma 22 -32 mm. Hg – Exam with Ophthalmoscope • Evaluation of color and configuration of optic disk – Perimetry-measurement of the central field of vision – Cupping of the optic disk is the most reliable sign in chronic simple glaucoma 3/6/2021 61
Treatment for Primary/Chronic Open-Angle Glaucoma • Medical (Important) – Beta-adrenergic blockers (Timoptic) decreases aqueous humor production (used in the treatment of glaucoma) – Carbonic anhydrase inhibitors (Diamox) Decreases aqeous humor production. Watch for signs of potassium depletion (used in the treatment of glaucoma; epileptic seizures) – Miotic eye drops (pilocarpine) constrict pupils and contract the ciliary muscle, increasing the outflow of aqueous humor. Decreases visual acuity, particularly when poorly illuminated 3/6/2021 62
Primary/Chronic Open-Angle Glaucoma Surgical Treatment • Indicated when conservative treatment measures fail – Trabeculoplasty – applications of laser beam on trabecular meshwork; changes the configuration and leads to increased outflow of aqueous humor – Trabeculectomy – an opening is made under a partial thickness scleral flap allowing aqueous humor to flow 3/6/2021 63
Acute Closed-Angle Glaucoma • A medical emergency! • Symptoms – Severe pain – Decreased vision – Pupil enlarged and fixed – Colored rings (halos) around lights – Eye is red – Steamy cornea – IOP 50 mm. Hg or higher • What happens – A blockage of the trabecular meshwork at the point of fluid outflow. IOP increases and may cause damage to the optic nerve. (Optic nerve transmits images from the eye to the brain) 3/6/2021 64
Treatment for Acute Closed-Angle Glaucoma • Medical – Osmotic diuretics (Mannitol) potent diuretic; rapidly reduces the production of aqueous humor in the eye; decreases IOP – Primarily used to treat acute attacks or in preparation for surgery. Not for chronic use – Carbonic anhydrase inhibitors (Diamox) Decreases aqeous humor production. Watch for signs of potassium depletion (used in the treatment of glaucoma; epileptic seizures) – Miotic eye drops (pilocarpine) constrict pupils and contract the ciliary muscle, increasing the outflow of aqueous humor. Decreases visual acuity, particularly in poor illumination 3/6/2021 65
Surgical Treatment for Acute Closed. Angle Glaucoma • Laser iridotomy – Attempts to lower IOP by directly damaging the ciliary bodies (permanently) – Procedure frequently needs to be repeated – Patients are at risk for severe inflammation; retinal detachment and hemorrhaging • Peripheral iridectomy – Performed to form a permanent connection between the anterior and posterior chambers – Prevents the iris from occluding the anterior chamber – Performed when laser treatment is unsuccessful 3/6/2021 66
Preventative Measures for Individuals with Glaucoma Keep a reserve bottle of eye drops Carry eye drops when away from home Carry ID for glaucoma and eye drops Be aware of the location of the closest 24 -hour drug store • Medications are required for a lifetime • Know the name, dosage, frequency, and side effects of medications • • 3/6/2021 67
Preventative Measures for Individuals with Glaucoma • Know the signs/symptoms that should be reported immediately – Acute eye pain deep in the eye – Sudden change in vision – Halos around lights – Vital sign changes 3/6/2021 68
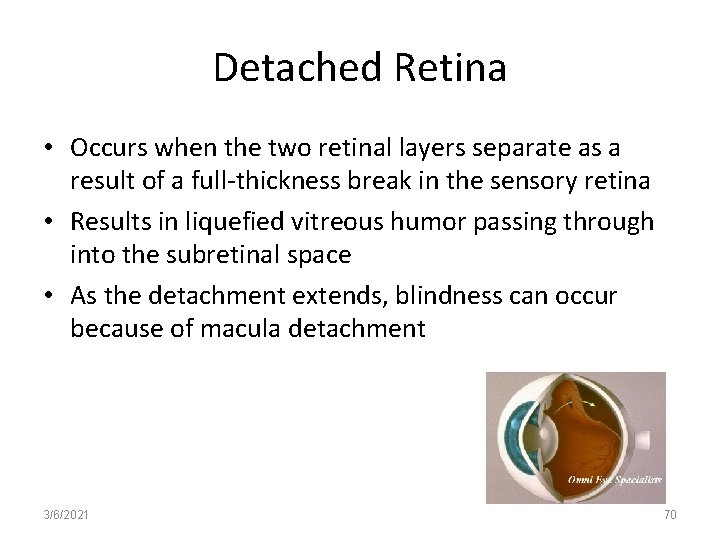
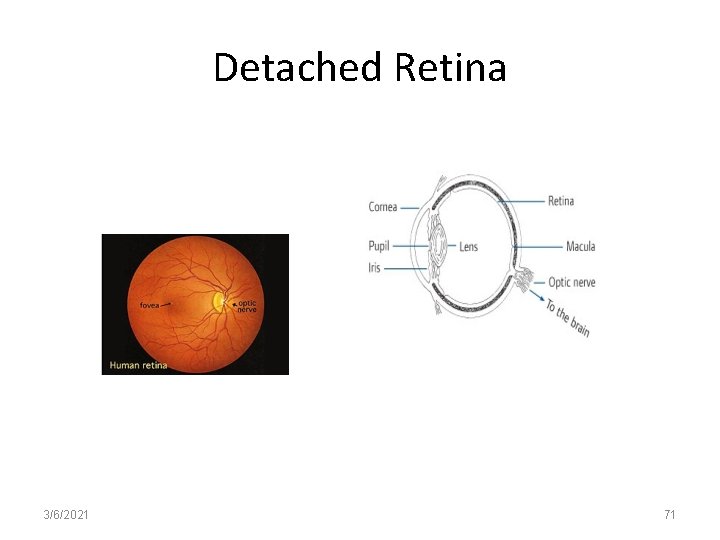
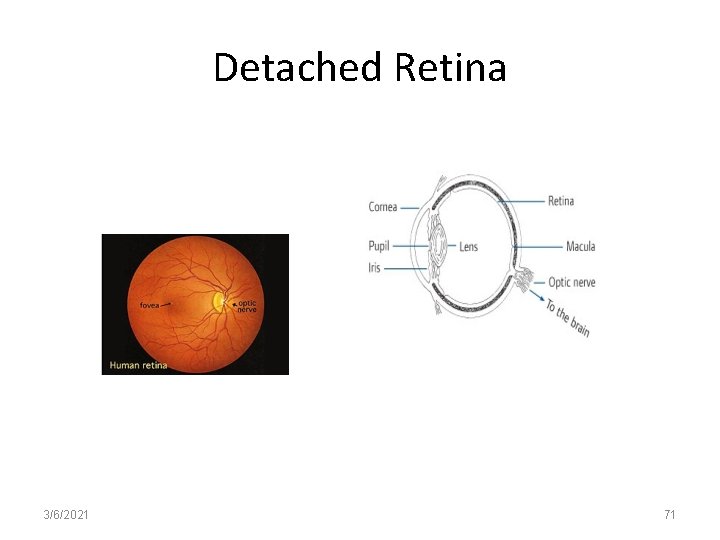
Detached Retina • What is retinal detachment? – Retinal detachments often develop in eyes with retinas weakened by a hole or tear – Fluid seeps underneath weakening the attachment – Retina detaches – (Like wallpaper peeling off a wall) – When detached, the retina cannot compose a clear image from incoming light and vision is blurred and dim 3/6/2021 69
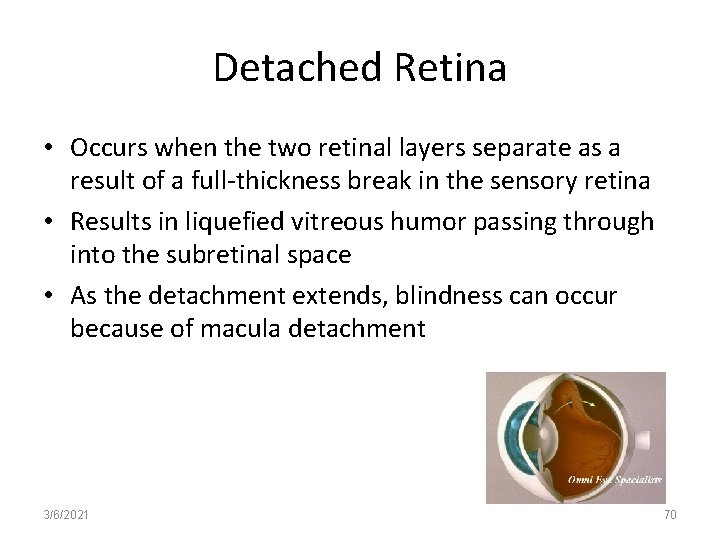
Detached Retina • Occurs when the two retinal layers separate as a result of a full-thickness break in the sensory retina • Results in liquefied vitreous humor passing through into the subretinal space • As the detachment extends, blindness can occur because of macula detachment 3/6/2021 70
Detached Retina 3/6/2021 71
Detached Retina (Causes) Trauma Myopic degeneration Tumors Hemorrhage May follow sudden severe physical exertion in a debilitated individual • May occur suddenly or develop over time • • • 3/6/2021 72
Detached Retina – Symptoms • Usually sudden and painless (no pain fibers) • Floaters and flashers (photopsia) • Floating spots or opacities before the eyes (blood and cells freed at time of tear) • Flashes of light (vitreous traction on the retina) • Progressive loss of vision in one area (curtain-drawn before eyes) 3/6/2021 73
Detached Retina – Diagnosing Based on ophthalmoscopic exam of retina Prevention is based upon early detection High risk individuals Diabetic retinopathy (damage to blood vessels of the retina) • High degree of myopia (distant objects are blurred) • • 3/6/2021 74
Surgical Treatment of Detached Retina • Goal is to seal off areas of tears • Scleral Buckling – Sclera and choroid are indented toward area of break • Photocoagulation – Produces inflammatory reaction at the site of the tear that causes chorioretinal adhesions • Cryopexy – Subfreezing temperatures used to produce inflammatory reaction • Pneumatic retinopexy – Intraocular injection of air or gas to tamponade the tear 3/6/2021 75
Diabetic Retinopathy Pathophysiology • A disorder of the blood vessels of the retina which usually appears about 10 years after the onset of DM • Can be detected in 65% of individuals with Type I diabetes for 15 years and in 60% of individuals with Type II diabetes • Responsible for 10% of newly reported cases of blindness each year 3/6/2021 76
Diabetic Retinopathy Pathophysiology • Retinal blood flow is poor; hypoxia develops; retinal cells secrete a “growth factor” – stimulates new vessel formation. Vessels are fragile, thin, week and bleed • Lead to hemorrhage and vision loss • Tiny microaneurysms develop in the retinal capillary walls • Retinal veins widen and become tortuous; small hemorrhages develop leaving small scars in those areas • Protein leaks causing retinal edema, especially in the area of the macula • Linked to fasting BG levels >129 mg/dl. HTN icreases rate of development too – Glycemic control is imperative to keep at near normal BG levels 3/6/2021 77
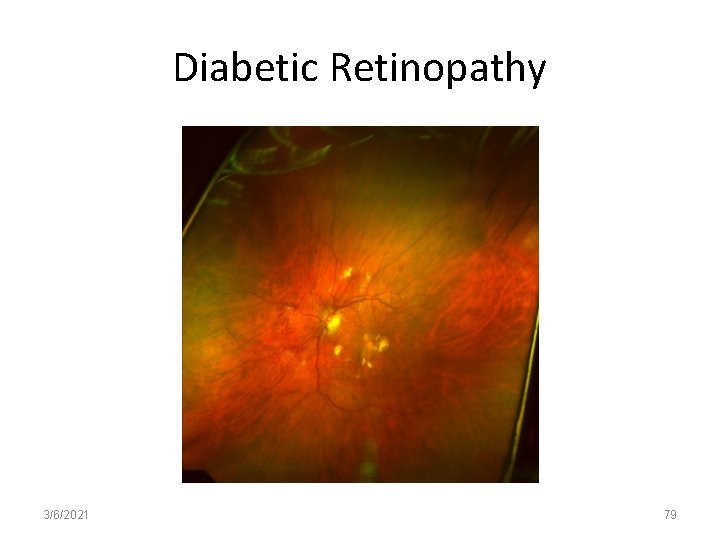
Diabetic Retinopathy Tortuous vessels Micro-aneurysms “Fluffy wool” exudates on the retina New vessel formation As the disease progresses, multiple spots or “floaters” • Increasing loss of vision • • • 3/6/2021 78
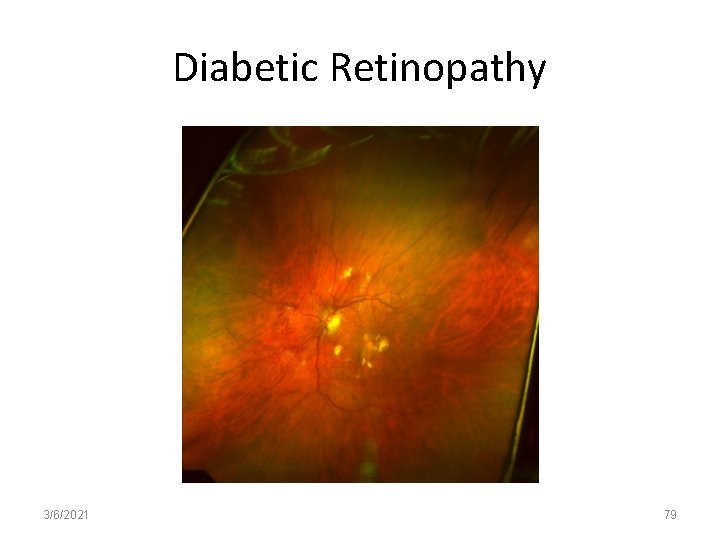
Diabetic Retinopathy 3/6/2021 79
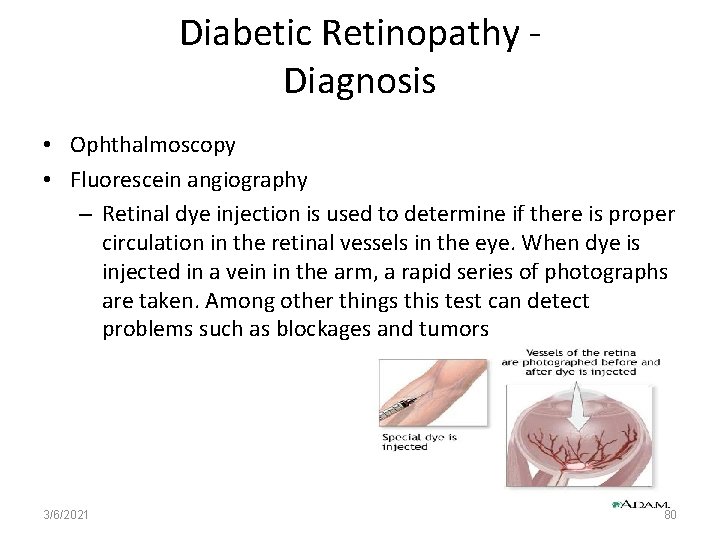
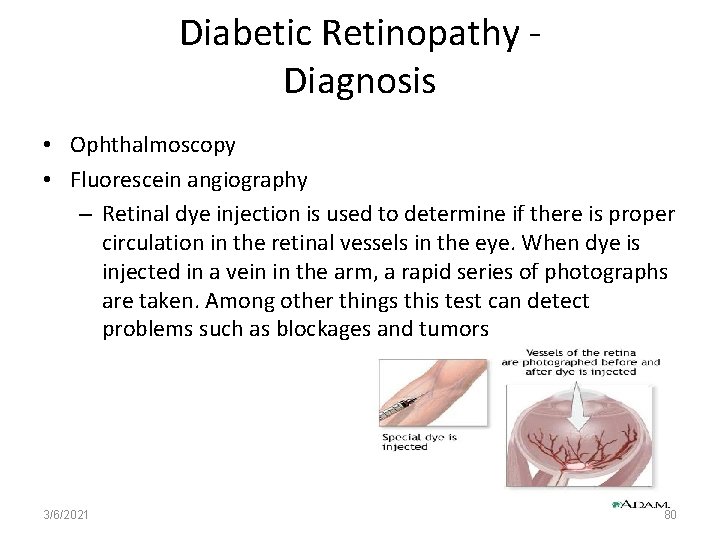
Diabetic Retinopathy Diagnosis • Ophthalmoscopy • Fluorescein angiography – Retinal dye injection is used to determine if there is proper circulation in the retinal vessels in the eye. When dye is injected in a vein in the arm, a rapid series of photographs are taken. Among other things this test can detect problems such as blockages and tumors 3/6/2021 80
Diabetic Retinopathy - Prevention • Type I DM – See ophthalmologist within three years of diagnosis; then yearly • Type II DM – At diagnosis and yearly – Women who are pregnant should be examined each trimester • Complications – May lead to massive retinal hemorrhage and retinal detachment 3/6/2021 81
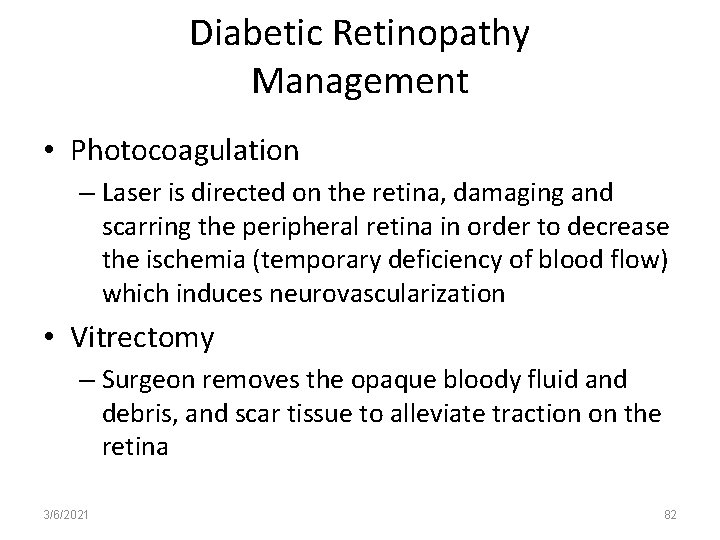
Diabetic Retinopathy Management • Photocoagulation – Laser is directed on the retina, damaging and scarring the peripheral retina in order to decrease the ischemia (temporary deficiency of blood flow) which induces neurovascularization • Vitrectomy – Surgeon removes the opaque bloody fluid and debris, and scar tissue to alleviate traction on the retina 3/6/2021 82
Diabetic Retinopathy – Nursing Considerations • Patient teaching regarding: – DM – Tight glycemic control – Importance of regular eye exams • Assess ability to administer insulin if vision is impaired 3/6/2021 83
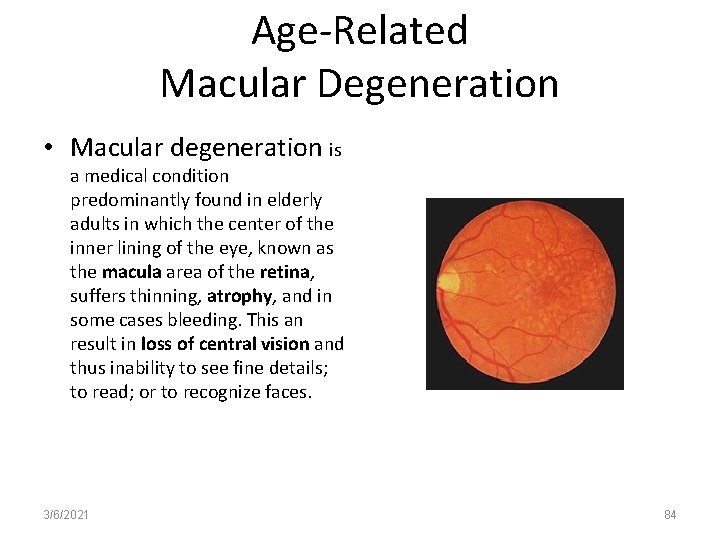
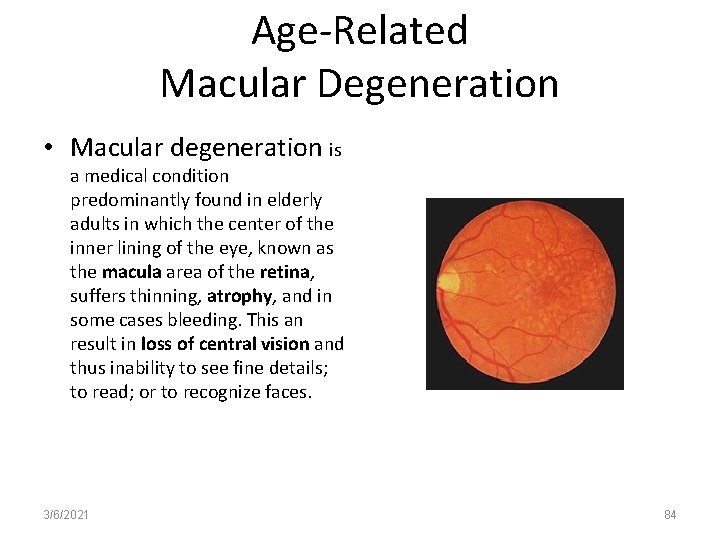
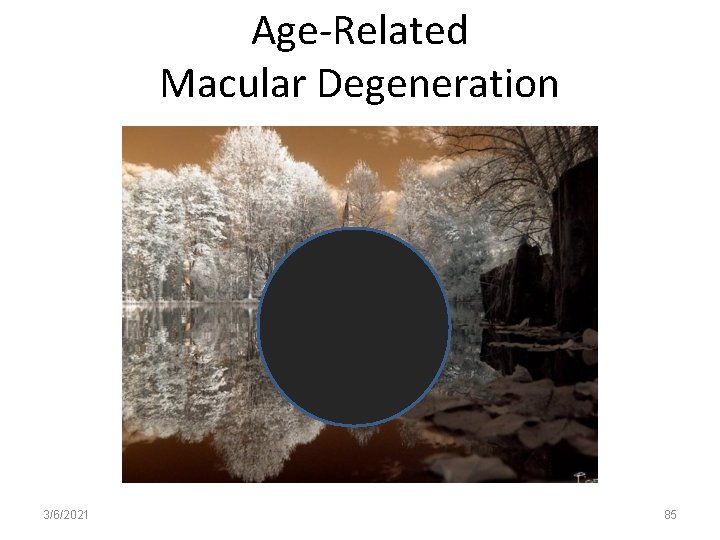
Age-Related Macular Degeneration • Macular degeneration is a medical condition predominantly found in elderly adults in which the center of the inner lining of the eye, known as the macula area of the retina, suffers thinning, atrophy, and in some cases bleeding. This an result in loss of central vision and thus inability to see fine details; to read; or to recognize faces. 3/6/2021 84
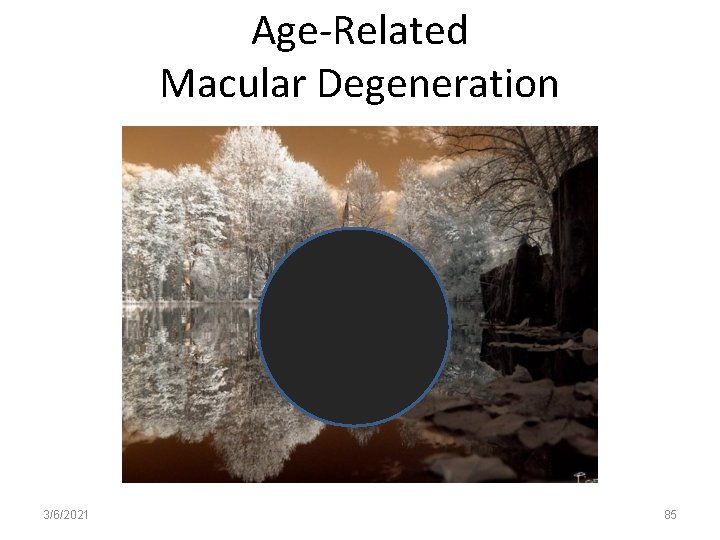
Age-Related Macular Degeneration 3/6/2021 85
Age-Related Macular Degeneration • A disease of the aging retina; cause is unknown • Cigarette smokers are at a significantly higher risk • Results from degenerative changes to the choriocapillaries or the retinal pigment epithelium 3/6/2021 86
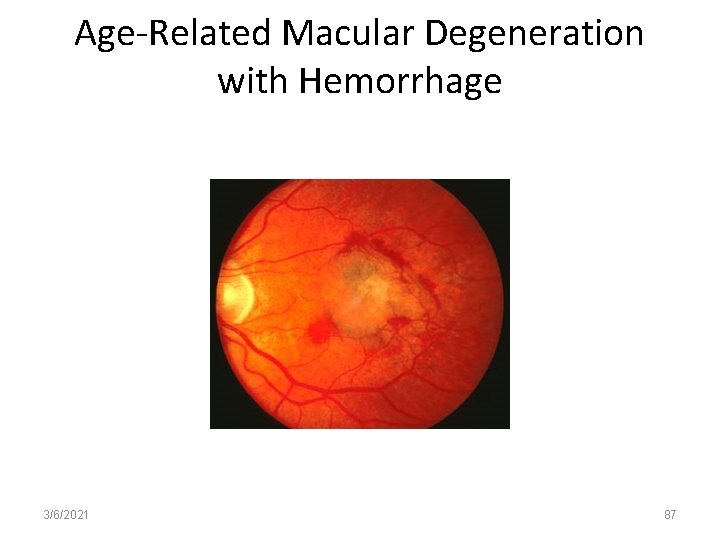
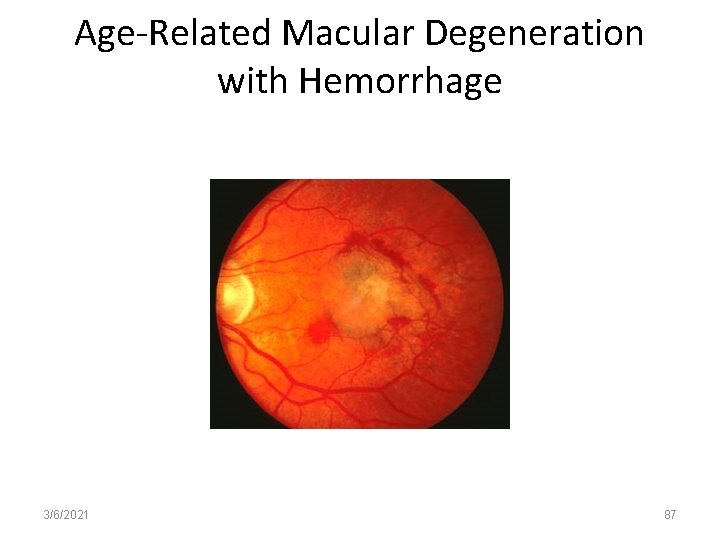
Age-Related Macular Degeneration with Hemorrhage 3/6/2021 87
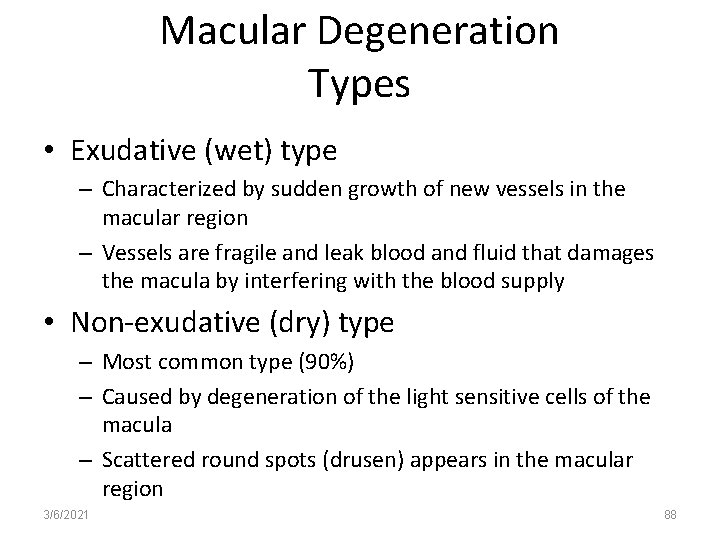
Macular Degeneration Types • Exudative (wet) type – Characterized by sudden growth of new vessels in the macular region – Vessels are fragile and leak blood and fluid that damages the macula by interfering with the blood supply • Non-exudative (dry) type – Most common type (90%) – Caused by degeneration of the light sensitive cells of the macula – Scattered round spots (drusen) appears in the macular region 3/6/2021 88
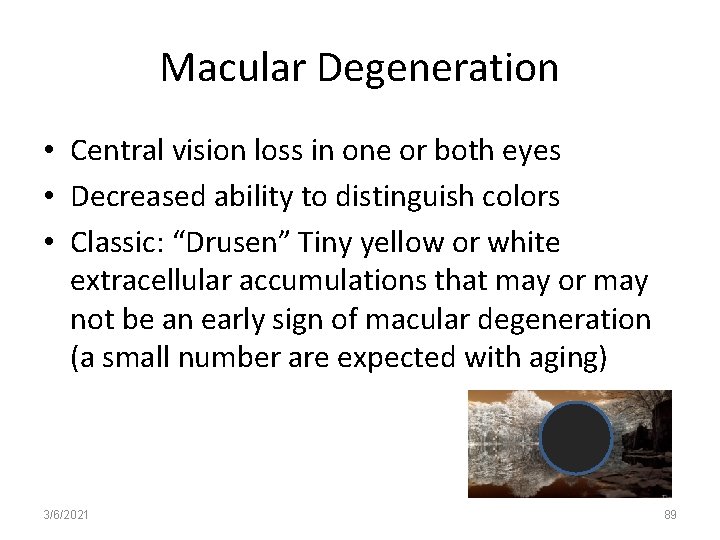
Macular Degeneration • Central vision loss in one or both eyes • Decreased ability to distinguish colors • Classic: “Drusen” Tiny yellow or white extracellular accumulations that may or may not be an early sign of macular degeneration (a small number are expected with aging) 3/6/2021 89
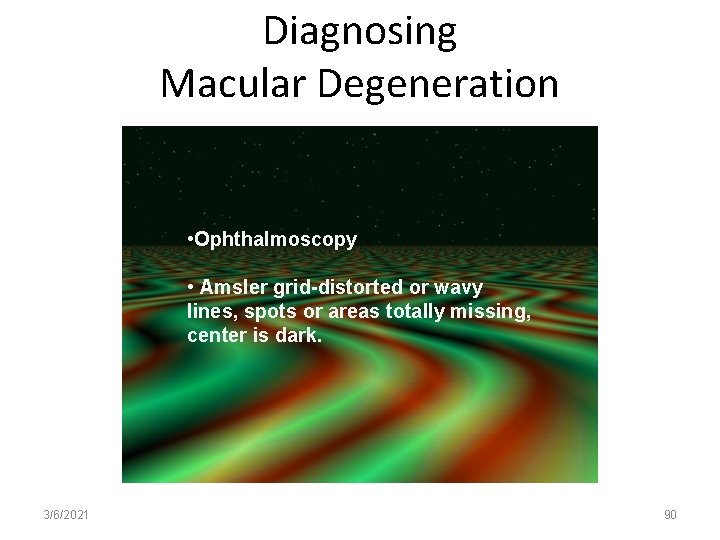
Diagnosing Macular Degeneration • Ophthalmoscopy • Amsler grid-distorted or wavy lines, spots or areas totally missing, center is dark. 3/6/2021 90
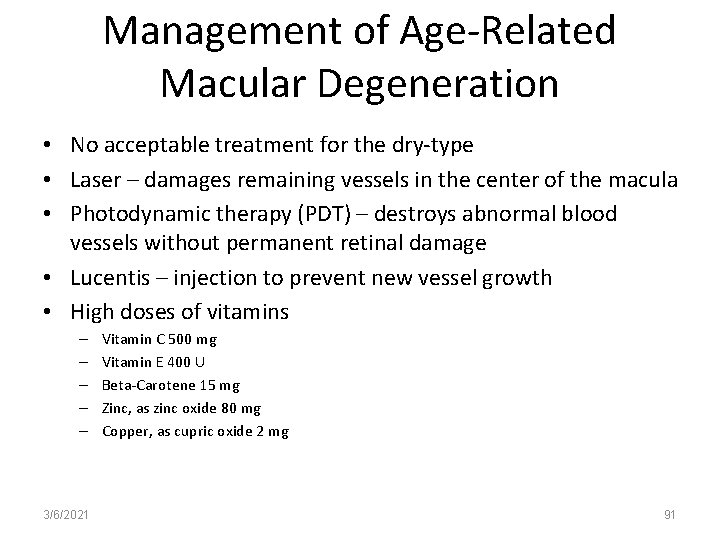
Management of Age-Related Macular Degeneration • No acceptable treatment for the dry-type • Laser – damages remaining vessels in the center of the macula • Photodynamic therapy (PDT) – destroys abnormal blood vessels without permanent retinal damage • Lucentis – injection to prevent new vessel growth • High doses of vitamins – – – 3/6/2021 Vitamin C 500 mg Vitamin E 400 U Beta-Carotene 15 mg Zinc, as zinc oxide 80 mg Copper, as cupric oxide 2 mg 91
Retinitis Pigmentosa • Group of inherited disorders that slowly leads to degeneration of part of the retina, primarily photoreceptors, that over time leads to blindness • First loss is night vision; then peripheral vision, resulting in tunnel vision; then color vision; then blindness • Hereditary; can begin in childhood • No cure – high dose vitamin-A may slow progression. Research on retinal microchip implantation and stem cell therapy 3/6/2021 92
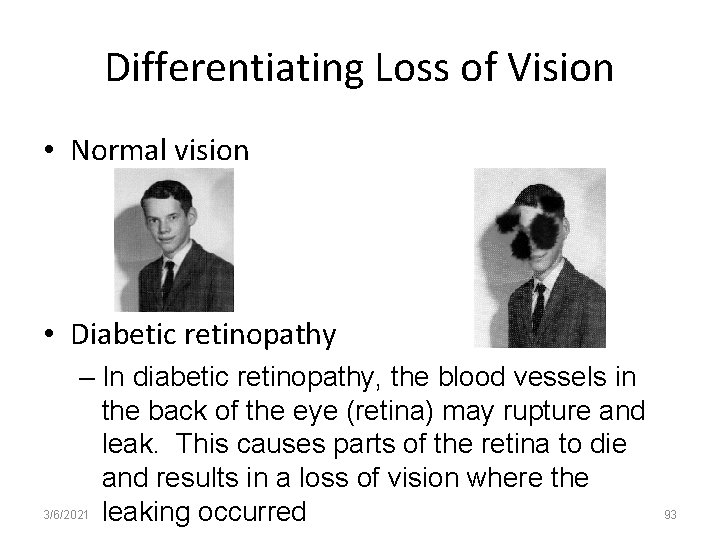
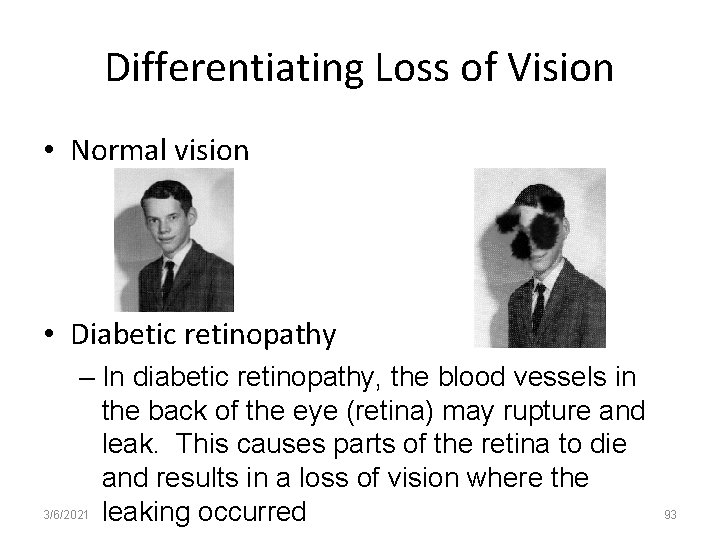
Differentiating Loss of Vision • Normal vision • Diabetic retinopathy – In diabetic retinopathy, the blood vessels in the back of the eye (retina) may rupture and leak. This causes parts of the retina to die and results in a loss of vision where the 3/6/2021 leaking occurred 93
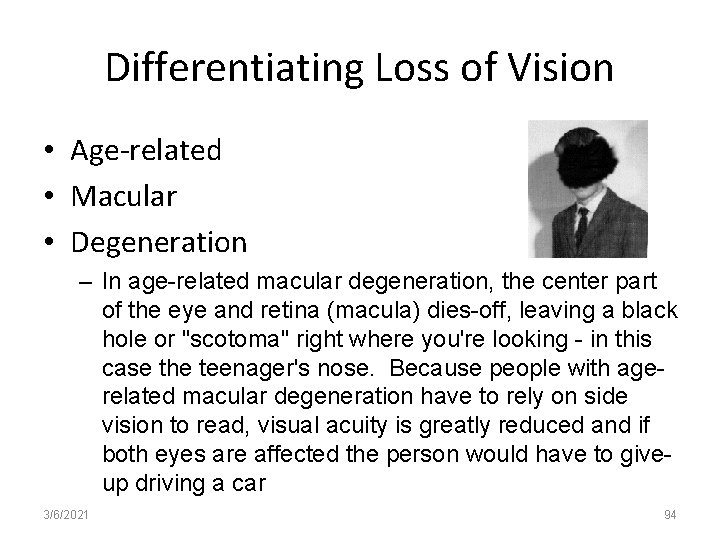
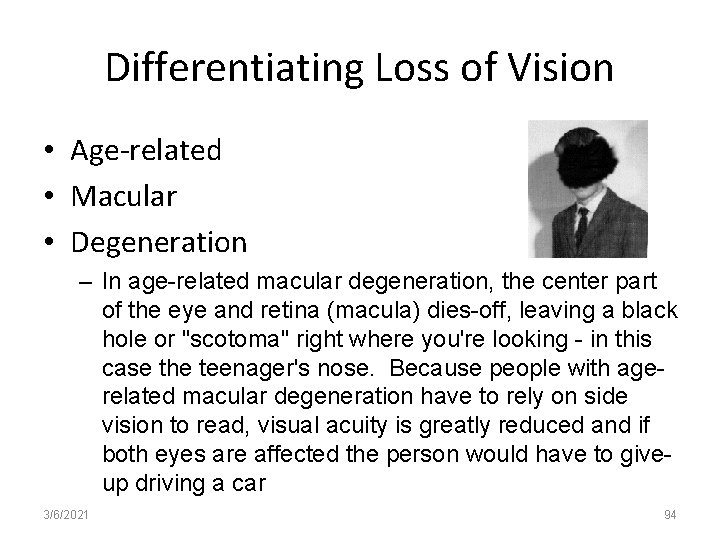
Differentiating Loss of Vision • Age-related • Macular • Degeneration – In age-related macular degeneration, the center part of the eye and retina (macula) dies-off, leaving a black hole or "scotoma" right where you're looking - in this case the teenager's nose. Because people with agerelated macular degeneration have to rely on side vision to read, visual acuity is greatly reduced and if both eyes are affected the person would have to giveup driving a car 3/6/2021 94
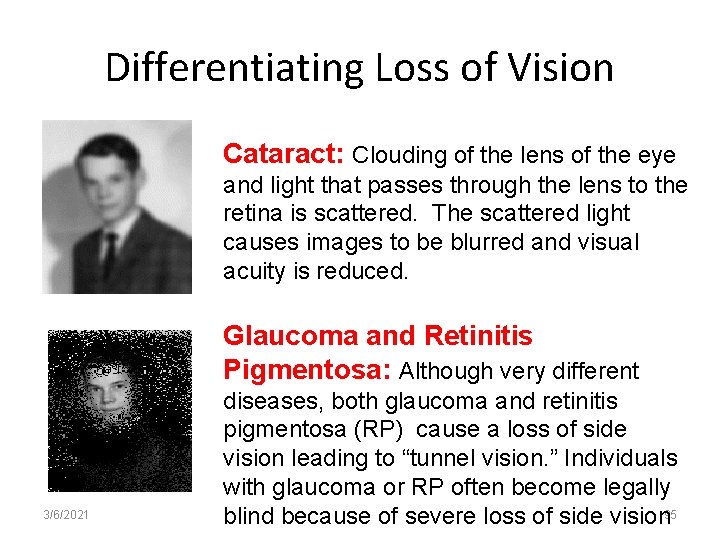
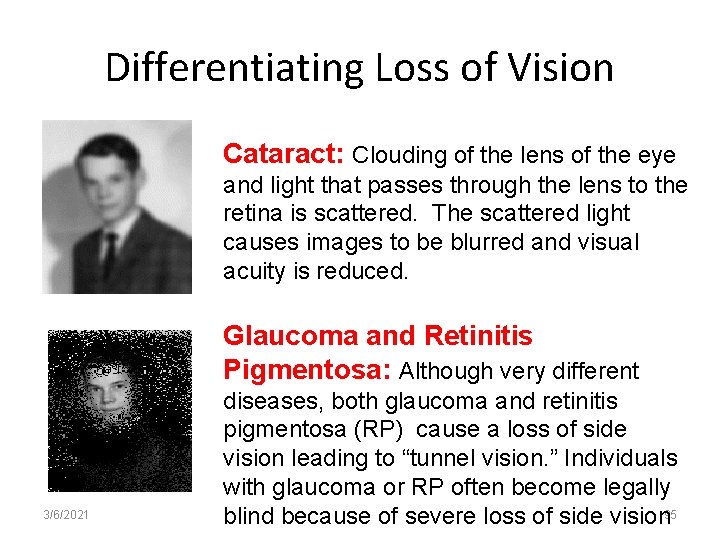
Differentiating Loss of Vision Cataract: Clouding of the lens of the eye and light that passes through the lens to the retina is scattered. The scattered light causes images to be blurred and visual acuity is reduced. Glaucoma and Retinitis Pigmentosa: Although very different 3/6/2021 diseases, both glaucoma and retinitis pigmentosa (RP) cause a loss of side vision leading to “tunnel vision. ” Individuals with glaucoma or RP often become legally blind because of severe loss of side vision 95
Cyotomegalvirus (CMV) Retinitis • Member of the herpes group of viruses • Direct viral invasion of retinal cells • CMV infection is present in many individuals and problematic when disease is evident • Most common site for CMV is in the individual with HIV 3/6/2021 96
Symptoms of Cytomegalvirus (CMV) Retinitis • • Blurred vision Decreased vision Floaters May lead to blindness (causes chorioretinitis, an exudative inflammatory process that involves retinal vessels) 3/6/2021 97
Diagnosis of Cytomegalvirus (CMV) Retinitis • Patient history • Immunocompromised patient • Fundoscopic exam (one or many small white lesions, or “cotton wool spots” along vessels can be associated) 3/6/2021 98
Management of Cytomegalvirus (CMV) Retinitis • Gancyclovir (IV or PO) – Anemia – Phlebitis • Foscarnet (IV) – Renal failure – Anemia • Gancyclovir implants or intra-orbitally 3/6/2021 99
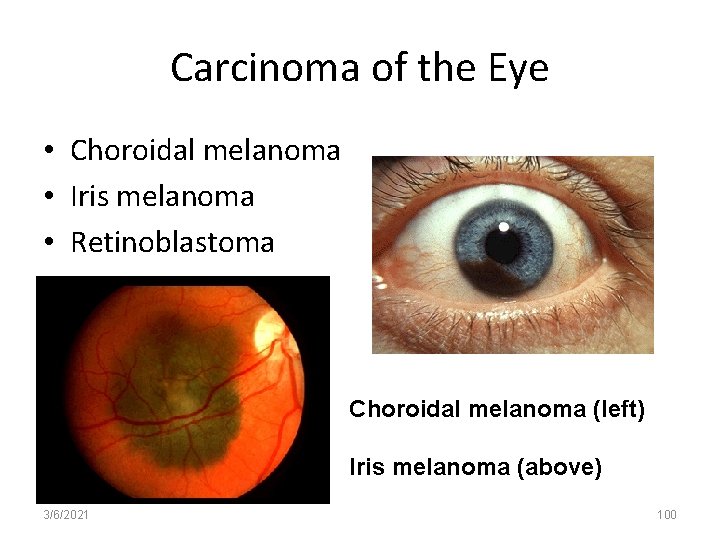
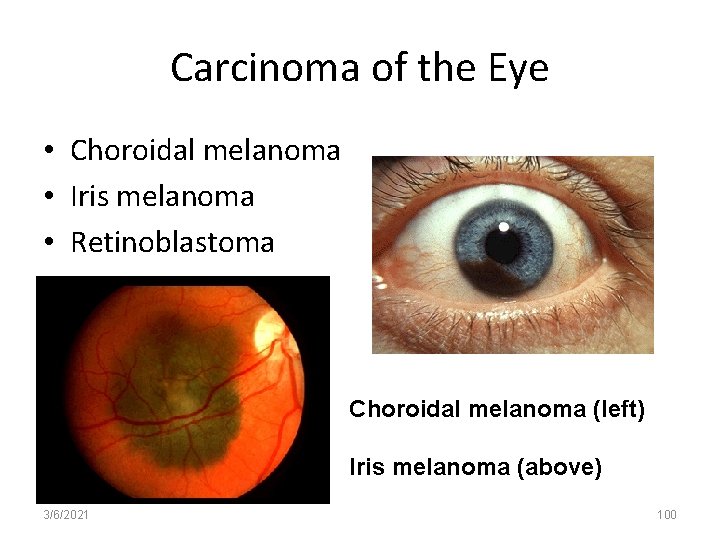
Carcinoma of the Eye • Choroidal melanoma • Iris melanoma • Retinoblastoma Choroidal melanoma (left) Iris melanoma (above) 3/6/2021 100
Common Nursing Diagnoses for Eye Problems Disturbed sensory perception r/t visual deficit Risk for injury r/t visual impairment Self-care deficit r/t visual impairment Anticipatory grieving r/t loss of functional vision loss Acute pain r/t pathophysiologic process and/or surgical correction • Noncompliance r/t inconvenience of lifelong meds • • • 3/6/2021 101
Question • Which of the following would be a sign of a post-operative cataract complication? – Change in color vision – Sudden loss of vision – Hallucinations; headache; changes in color vision; flashes of light – Flashes of light; floaters; increased tearing 3/6/2021 102
Question • Which of the following would be a sign of a postoperative cataract complication? • Answer: Flashes of light; floaters; increased tearing 3/6/2021 103
Question • A 37 -year-old Type I diabetic is admitted with a hyperglycemic episode. The patient describes frequent episodes of blurred vision. An examination of the eye fundus by opthalmoscopy reveals – – 3/6/2021 Narrowing of retinal arteries and hemianopsis Scattered round white spots in the macular region Tortuous vessels, fluffy wool exudates, new vessel growth Cupping of the optic disc 104
Question • A 37 -year-old Type I diabetic is admitted with a hyperglycemic episode. The patient describes frequent episodes of blurred vision. An examination of the eye fundus by opthalmoscopy reveals • Answer: Tortuous vessels, fluffy wool exudates, new vessel growth 3/6/2021 105
Which Med for Which Condition? • Midriatic (pupil dilates, example is Atropine) • Miotic (constricts pupil and contracts the ciliary muscle allowing for enhanced circulation of aqueous humor) • Osmotic (draws fluid into intravascular space to lower IOP) • Anti-inflammatory 3/6/2021 • Acute closed-angle glaucoma • Chronic closed-angle glaucoma • Corneal abrasion • Conjunctivitis • Ophthalmoscopy 106
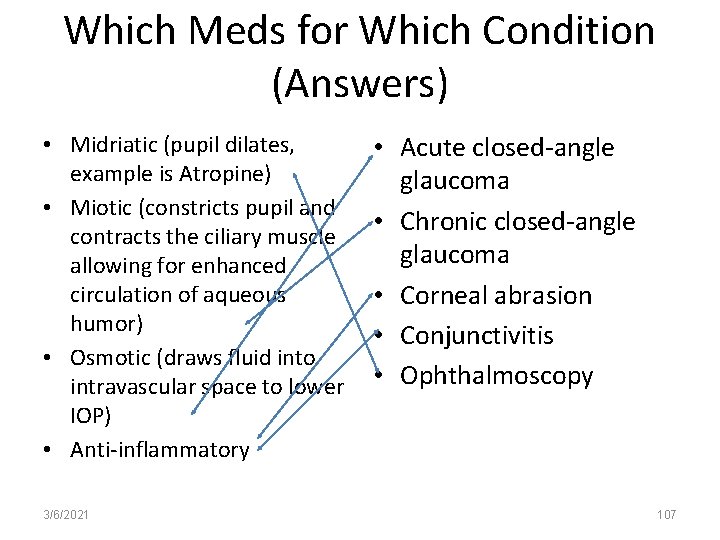
Which Meds for Which Condition (Answers) • Midriatic (pupil dilates, example is Atropine) • Miotic (constricts pupil and contracts the ciliary muscle allowing for enhanced circulation of aqueous humor) • Osmotic (draws fluid into intravascular space to lower IOP) • Anti-inflammatory 3/6/2021 • Acute closed-angle glaucoma • Chronic closed-angle glaucoma • Corneal abrasion • Conjunctivitis • Ophthalmoscopy 107
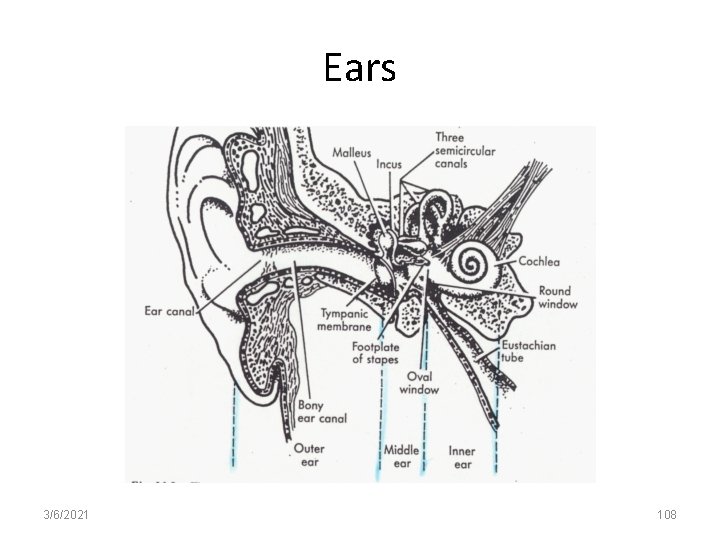
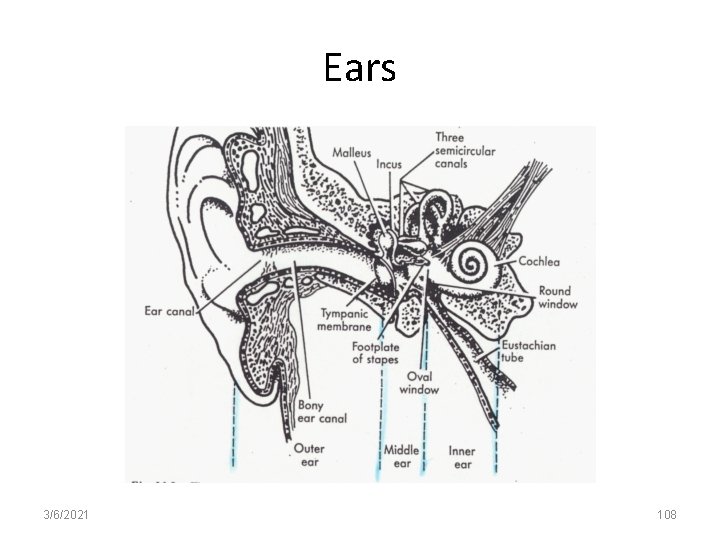
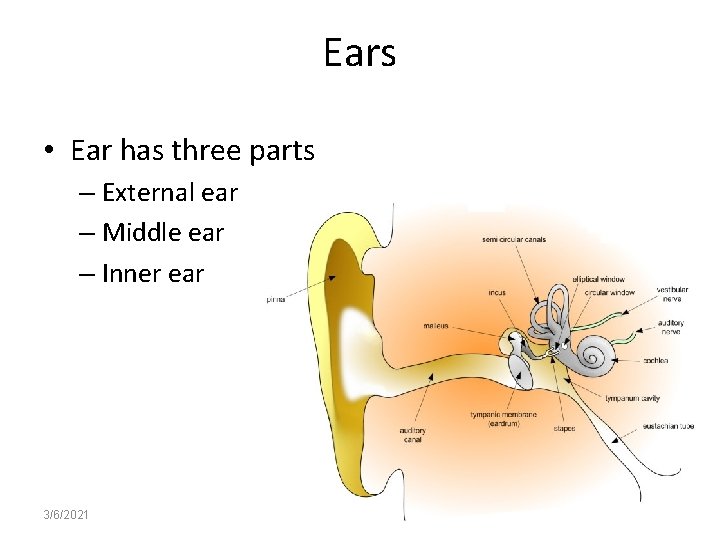
Ears 3/6/2021 108
Ears • Ear has three parts – External ear – Middle ear – Inner ear 3/6/2021 109
Ears and Hearing: Assessment • Obtain a thorough history • Demographics – Gender (some hearing disorders more common men than in women and vice versa) – Age (elderly) • Family history and Genetic risk – 70% of people with Down syndrome develop hearing loss in adulthood • 3/6/2021 110
Ears and Hearing: Assessment • Personal history – Ask about past and present problems with pain, vertigo tinnitus, loss of hearing, difficulty understanding people who are talking • Socioeconomic status – Availability of healthcare • Current health problems – Dizziness or vertigo • Physical assessment 3/6/2021 111
Assessment of the Ear • Otoscopic examination • Auditory assessment – Air versus bone conduction sound – Transmission – Conductive, sensorineural or mixed • Vestibular assessment 3/6/2021 112
Diagnostic Testing and the Ear • CT • Audiometry – Pure tone (tests hearing threshold levels) – Speech • Electronystagmography – Artificial stimulation of the vestibular apparatus – Involves induced nystagmus (rapid involuntary movement of the eye) – Can suggest etiology of vertigo – Purpose is in determining if there is something wrong with the vestibular portion of the inner ear. – If dizziness is not caused by the inner ear, it might be caused by disorders of the brain, or by medical disorders (low blood pressure) 3/6/2021 113
Classification of Hearing Loss • • • Conductive hearing loss – i. e. , problem conducting sound waves – Obstruction – Otosclerosis (overgrowth of bone in the inner ear) Sensorineural hearing loss – Root cause sometimes found in CN VIII, (Vestibulocochlear nerve) – Resulting from exposure to loud noises – Diabetes – Damage to inner ear – Meniere’s Disease Mixed hearing loss – Combination of conductive hearing loss and sensorineural hearing loss 3/6/2021 114
The Outer Ear • Infections – External otitis • PAIN • Itching or ear canal • Inflammation • Cerumen • Foreign body • Problems of Tympanic membrane – Chronic otitis media (middle ear infection) is a common cause of hearing loss; trauma 3/6/2021 115
Some Acute Perforations Will Heal Spontaneously • Myringoplasty – Performed if the perforation if only the membrane with no other accompanying damage • Tympanoplasty – Performed if the middle ear is involved • Post-op – Do not blow nose; sneeze or cough with mouth open – Avoid physical activity for one week – Keep ear dry for six weeks – Do not shampoo hair for one week – Avoid airplane travel for one week 3/6/2021 116
Middle Ear • Infections – Otitis media • Throbbing pain, drainage, fever, bulging tympanic membrane with possible perforation • Otosclerosis – Hardening of the ear (stapes); normal canal and ear drum; progressive conductive hearing loss • Trauma – To the tympanic membrane from a blast or blunt injury – Can cause a fracture or dislocation of the ossicle – Facial nerve is also vulnerable • Eustachian tube disorders – Most common blockage due to enlarged adenoid tissue 3/6/2021 117
Inner Ear • Infections – Labyrinthitis; can be viral or bacterial • Tumors – Acoustic neuroma of CN VIII; most common benign tumor • Balance Disorders – Meniere’s disease, a triad of symptoms – vertigo, dizziness, tinnitus, and hearing loss. Affects CN VIII – Tinnitus • Ringing noise – Vertigo • When eyes are open, world seems to be spinning 3/6/2021 118
Meniere’s Disease • Assessment – History of falls – Disability in relation to ADLs – Fears – Hearing acuity fluctuations – Sense of fullness of the hear – Autonomic response: Pallor; sweating; N/V – Progressive, permanent hearing loss 3/6/2021 119
Meniere’s Disease: Diagnosis • Audiometric testing – Tests amount of hearing loss • MRI – Used to identify presence of tumors or masses 3/6/2021 120
Meniere’s Disease Treatment • Bed rest during attack • Avoid sudden movement • Medications – Dimenhydrinate (Dramamine) – Cyclizine hydrochloride (Marezine) – Meclizine (Bonine; Antivert; sedatives and hypnotics) 3/6/2021 121
Nursing Diagnosis Risk for injury falls Fear: Uncertainty of attacks Anxiety: Vertigo as threat to self-concept Fluid volume deficit: Nausea and vomiting Knowledge deficit r/t lack of exposure to information • To move slowly; not turn head quickly • • • 3/6/2021 122
Noise Induced Hearing Loss • Major portion of hearing impairment among individuals 35 – 65 years of age • Can be traumatic – Sudden loud noise; i. e. , blast) • Over time from repeated injury from noise • Major causes – Individual noise – Firearms (second) – Loss of higher frequencies 3/6/2021 123
Presbycusis • • Hearing loss related to aging More common after age 50 Hearing loss of higher frequencies Accompanied by tinnitis 3/6/2021 124
Hearing Aids • All hearing aids consist of – – Microphone Amplifier Battery Receiver • In the ear for hearing loss of 25 – 65 d. B; worn in ear concha (pinna) • In the canal for hearing loss of 25 – 50 d. B; worn in ear canal • Postauricular – for hearing loss of 25 -80 d. B; worn behind ear 3/6/2021 125
Care of Hearing Aids • Turn off when not using • Open battery compartment at night to avoid draining the battery • Keep extra batteries available at all times • Wash earmold frequently with mild soap and water with the use of pipe cleaner to cleanse the cannula • Do not wear if ear infection 3/6/2021 126
Sense of Taste • Taste (gustation) serves as a protector from rotten or putrid food and provides delightful sensations of creamy , chocolate, crunchy chips, chew taffy and fruitful pies • Taste sensors ara most efficient at room temp and respond only to substances in solution • Taste buds are locate in four areas of the tongue that sense sweet, salt, bitter & sour. • Tongue also aids in swallowing and speech 3/6/2021 127
Taste con’t • Motor movement controlled by CN XII; temp and position controlled by CN V and IX • Sensation is altered secondary to neuro disorders & trauma. Evaluate for possible causes including diet, medication, smoking, caffeine and olfactory disturbances • Works closely with CN 1 to identify tastes 3/6/2021 128
Sense of Smell • Sense of smell (olfaction) serves as guardian from danger. Warns of impending danger from gas leaks, smoke, fires, rancid meat/fish, sour dairy products • Disorders often undetected • Emotional changes assoc with loss of smell • New research may offer clues to alterations in diet habits, wt loss or gain, anorexia, malnourishment, even ADL such as bathing and brushing teeth. 3/6/2021 129
Sense of Touch • Sense of touch (tactile) includes sensations pertaining to the skin • Tactile receptors located thru-out skin • Cutaneous sensations of touch, pressure, vibration, cold, heat and pain • Pts unable to sense temp variations need interventions regarding heat and cold therapies, bath water, cooking and exposure • Immobility, skin integrity big issues for nurses 3/6/2021 130
The End! Sensory