PEPTIC ULCER DISEASE GASTRIC ULCER AETIOLOGY Atrophic gastritis

- Slides: 32
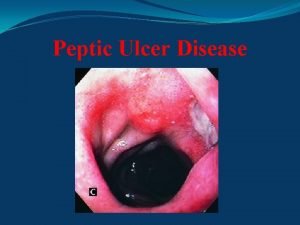
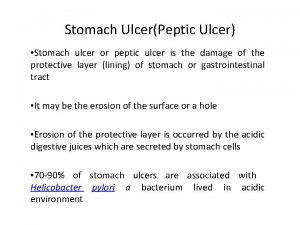
PEPTIC ULCER DISEASE
GASTRIC ULCER
AETIOLOGY • Atrophic gastritis, gastric stasis, abnormalities in acid and pepsin secretion. • Duodenal bile reflux - bile salts and lysolecithin break the mucosal barrier making it more vulnerable for injury, action of drugs and pepsin injury • Smoking, alcohol, NSAIDs, steroids. • Helicobacter pylori infection (70%). • Altered mucosal barrier mechanism. • Mucosal ischaemia
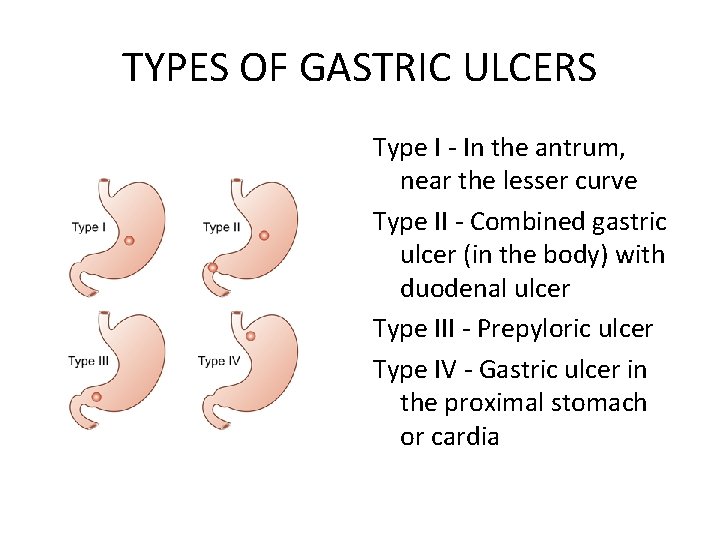
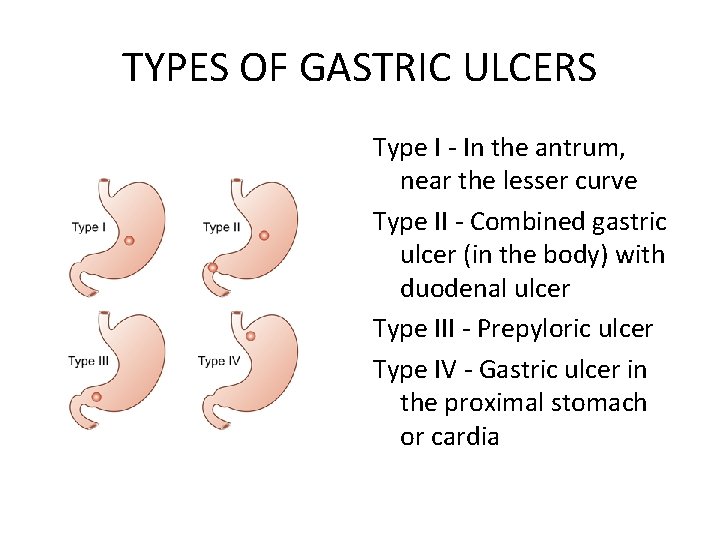
TYPES OF GASTRIC ULCERS Type I - In the antrum, near the lesser curve Type II - Combined gastric ulcer (in the body) with duodenal ulcer Type III - Prepyloric ulcer Type IV - Gastric ulcer in the proximal stomach or cardia
CLINICAL FEATURES • M = F, >40 yrs • Pain in epigastric region after taking food, lasting up to two hours. Pain is uncommon during night. It is relieved by vomiting or by inducing vomiting. • Periodicity: Symptom free interval may be 2 -6 months. Often with seasonal variation. • Haematemesis and melaena • Hesitant to eat, because eating induces pain and that results in loss of weight.
DIFFERENTIAL DIAGNOSIS • • • Hiatus hernia Cholecystitis Chronic pancreatitis Chronic gastritis Dyspepsia Carcinoma stomach
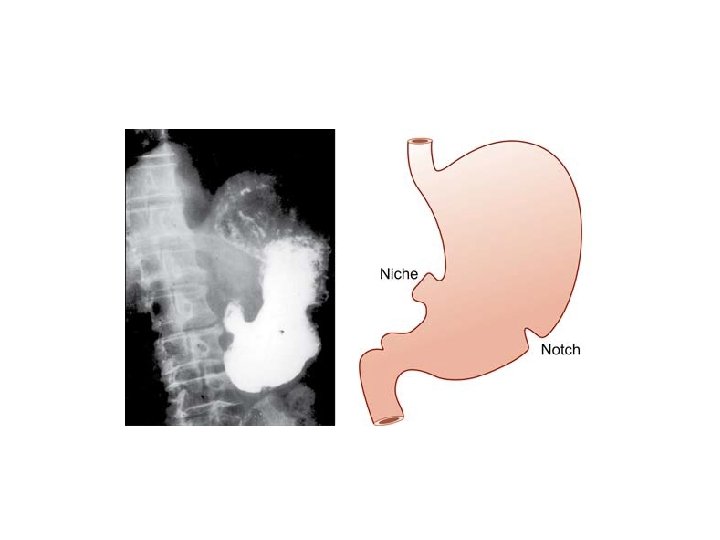
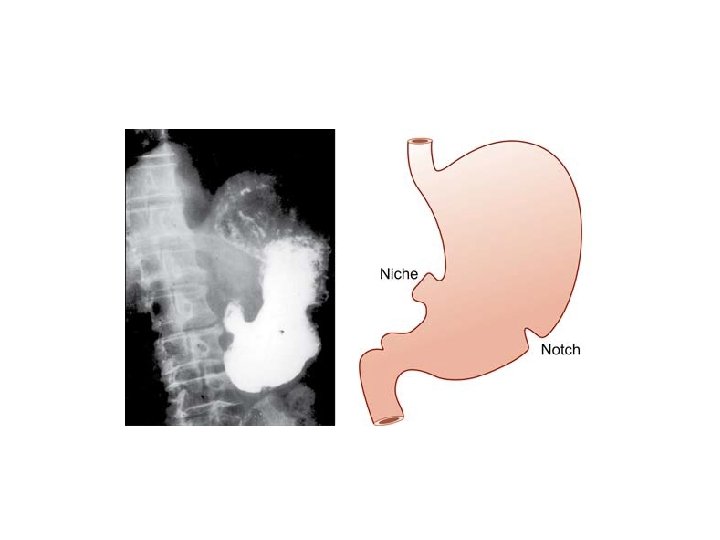
INVESTIGATIONS • BARIUM MEAL – Niche on the lesser curve with notch on the greater curvature – Ulcer crater projects beyond the lumen of the ulcer – Regular/round margin of the ulcer crater— spoke wheel pattern – Overhanging mucosa at the margins of a benign gastric ulcer—projects inwards towards the ulcer— Hamptom’s line – Converging mucosal folds towards the base of the ulcer – Symmetrical normal gastric mucosal folds
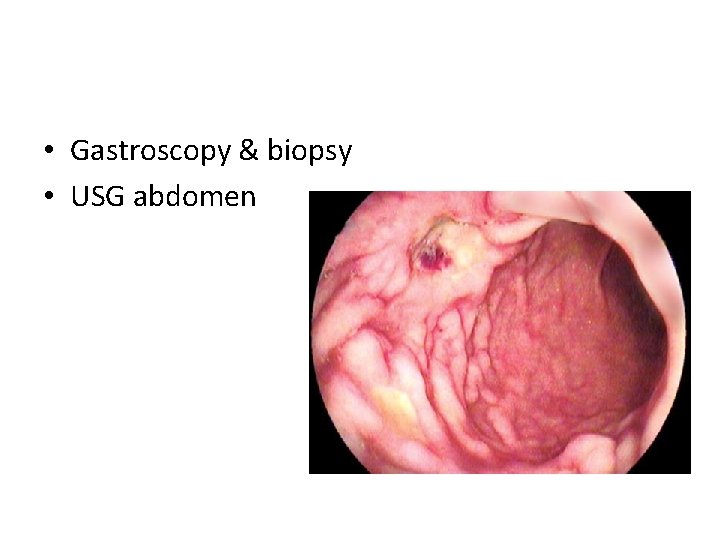
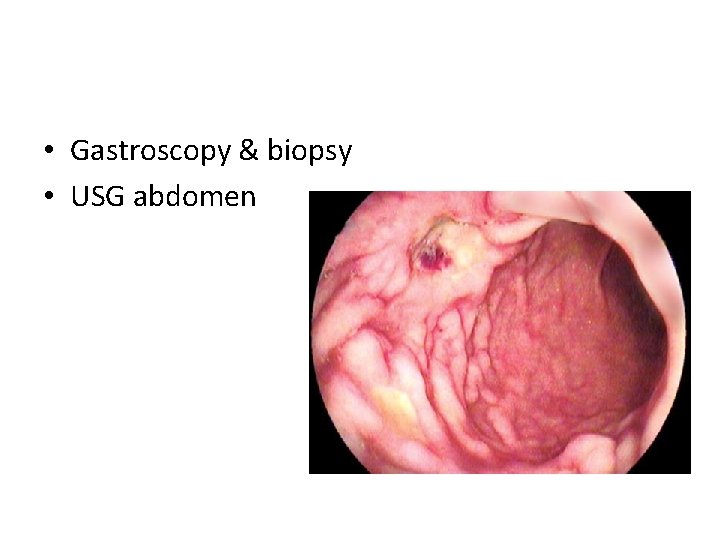
• Gastroscopy & biopsy • USG abdomen
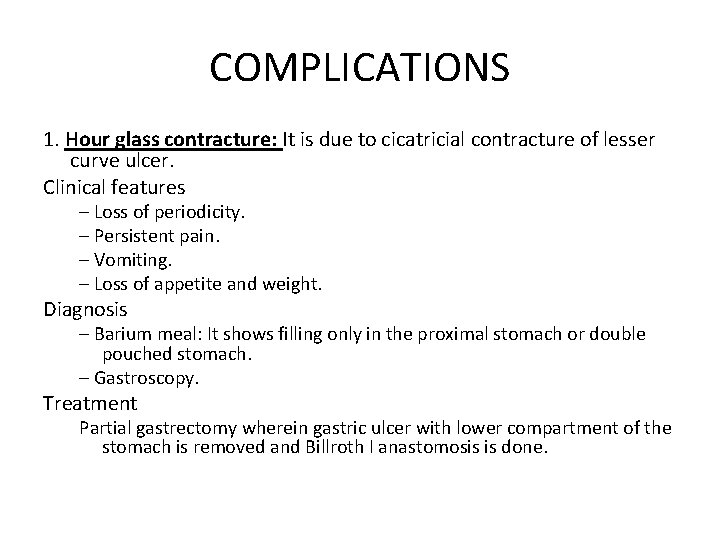
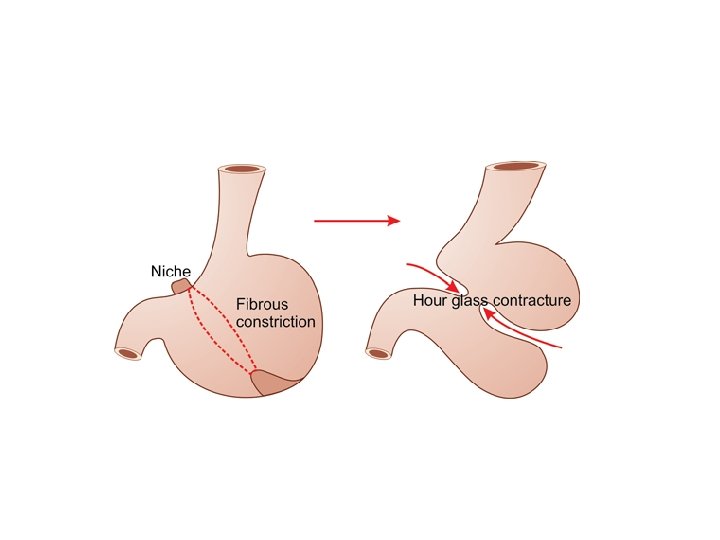
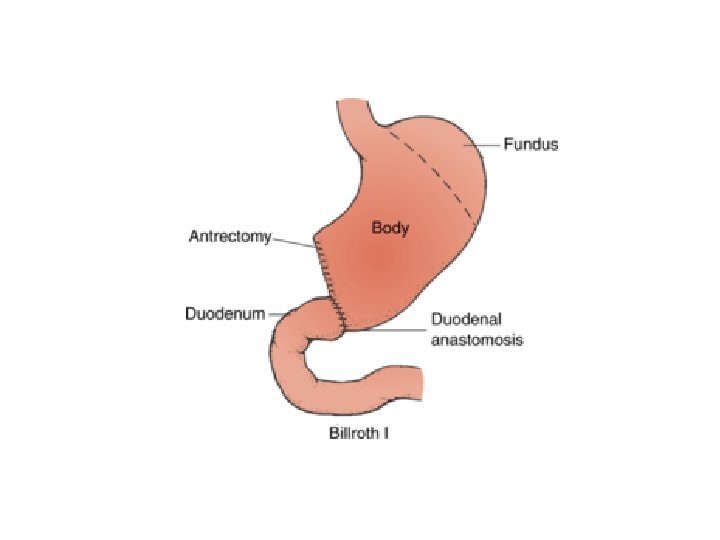
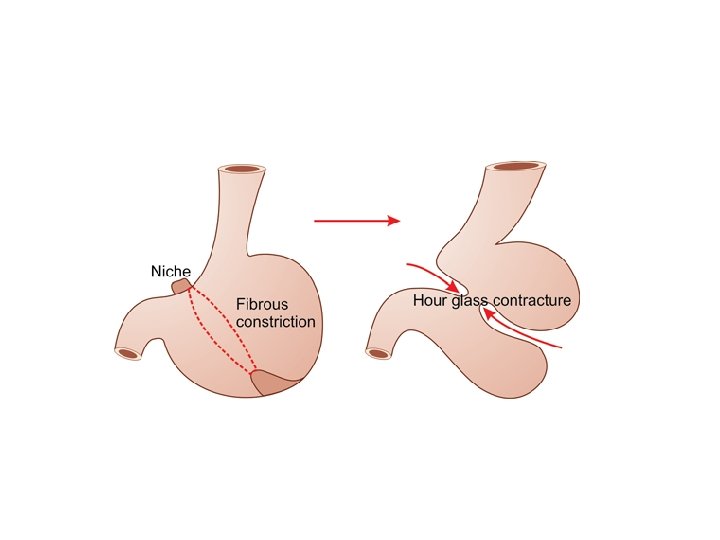
COMPLICATIONS 1. Hour glass contracture: It is due to cicatricial contracture of lesser curve ulcer. Clinical features – Loss of periodicity. – Persistent pain. – Vomiting. – Loss of appetite and weight. Diagnosis – Barium meal: It shows filling only in the proximal stomach or double pouched stomach. – Gastroscopy. Treatment Partial gastrectomy wherein gastric ulcer with lower compartment of the stomach is removed and Billroth I anastomosis is done.
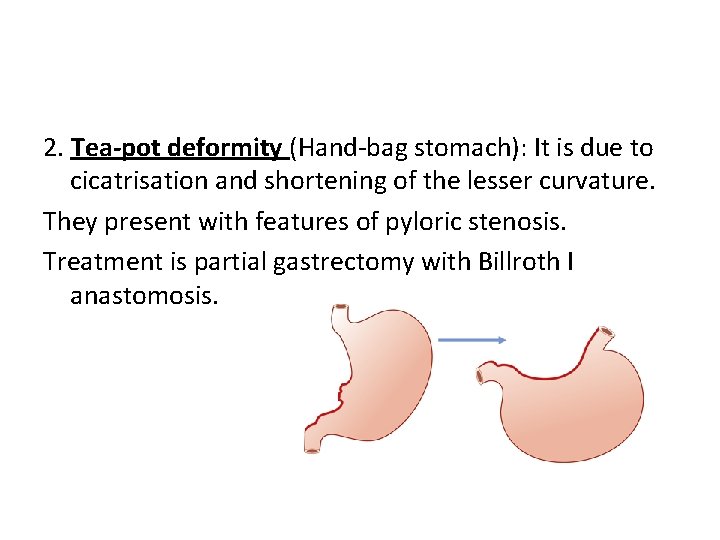
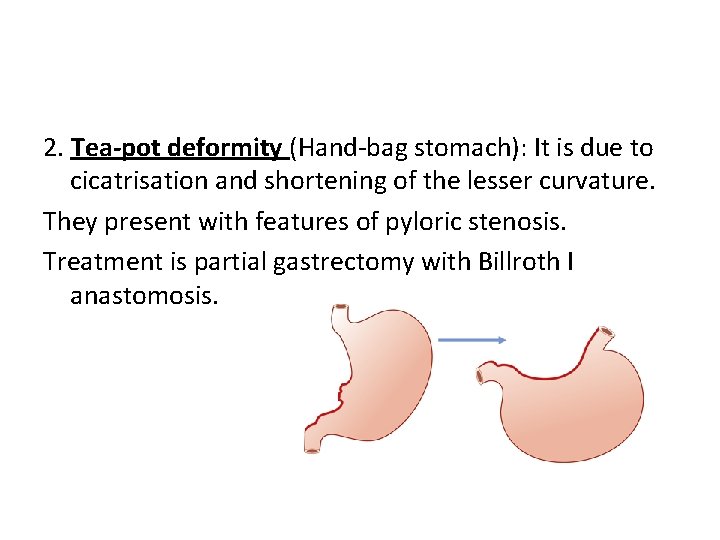
2. Tea-pot deformity (Hand-bag stomach): It is due to cicatrisation and shortening of the lesser curvature. They present with features of pyloric stenosis. Treatment is partial gastrectomy with Billroth I anastomosis.
3. Perforation - most frequent. 4. Bleeding by erosion into the left gastric and rarely splenic vessels or to vessels in the wall of ulcer— 35%. 5. Malignant transformation – adenocarcinoma stomach
TREATMENT MEDICAL THERAPY • H 2 antagoists and proton-pump inhibitors • Eradication therapy A diagnosis of Zollinger–Ellison syndrome should be suspected in H. pylori negative, non. NSAID-related peptic ulceration and serum gastrin levels should be measured.
SURGICAL TREATMENT In addition to reducing exposure to acid secretion, in gastric ulceration the diseased tissue is usually removed as well. This has the advantage that malignancy can then be confidently excluded.
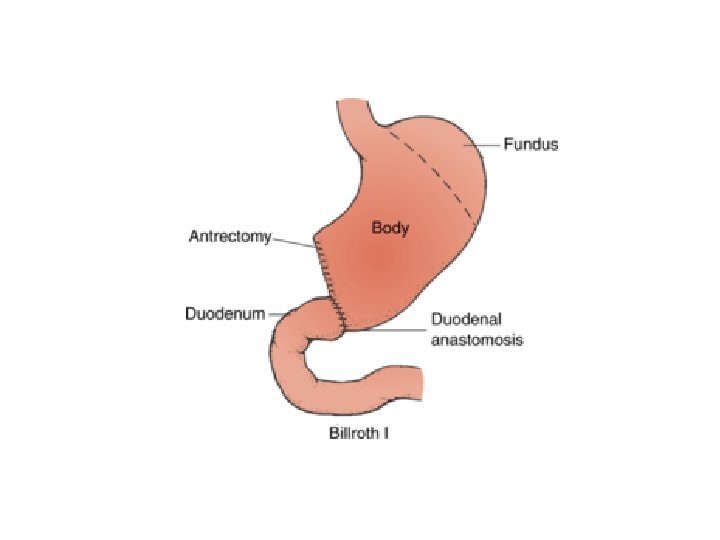
BILLROTH I GASRECTOMY • The distal stomach is mobilised and resected should include the ulcer that is usually situated on the lesser curve. • The cut edge of the remnant is then partially closed from the lesser curve aspect, leaving a stoma at the greater curve aspect, which should be similar in size to the duodenum. • Reconstruction may be facilitated by mobilising the duodenum using Kocher’s manoeuvre.
Other surgical procedures • • • Pauchet’s procedure. De Miguel’s antrectomy Mak’s pylorus preserving gastrectomy Kelling Madlener procedure Csendes procedure
DUODENAL ULCERS
AETIOLOGY • Blood group O +ve. • Stress, anxiety—‘hurry, worry, curry’. • Helicobacter pylori infection is an important aetiology for duodenal ulcer (90%). • NSAIDs, steroids • Endocrine causes: Zollinger-Ellison syndrome, MEN syndrome, hyperparathyroidism. • Other causes: Alcohol, smoking, vitamin deficiency
PATHOLOGY • Ulcer occurs in the first part of duodenum, usually with in the first inch, involving the muscular layer. • Eventually it shows cicatrisation causing pyloric stenosis. SITES: a. In the bulb (bulbar)— 95%. b. Post-bulbar (5%).
• Sometimes two opposing ulcers, i. e. over anterior and posterior surfaces of duodenum are present and are called ‘kissing ulcers’. • An anterior ulcer perforates, posterior ulcer bleeds or penetrates.
CLINICAL FEATURES • Type A personality • Pain is more before food, in early morning and decreases after taking food. It is classically called as hunger pain. Night pains are common. • Common in males. • Periodicity is more common than in chronic gastric ulcer with seasonal variation. • Water-brash, heart burn, vomiting may be present. • Melaena is more common, haematemesis also can occur. • Appetite is good and there is gain in weight
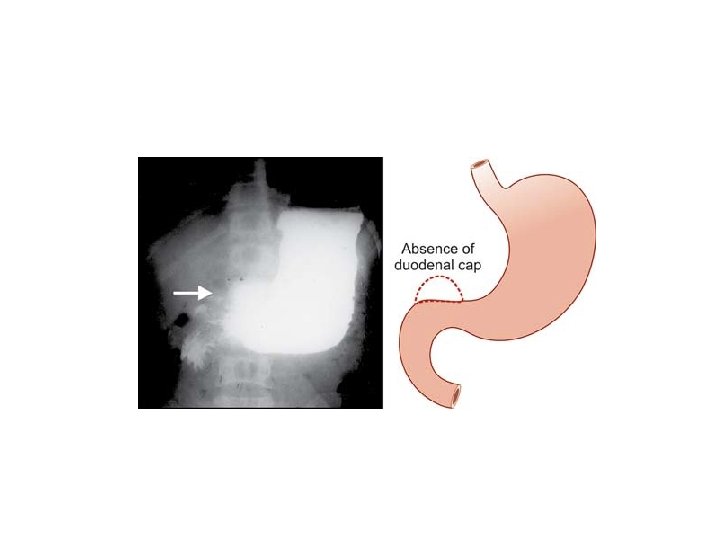
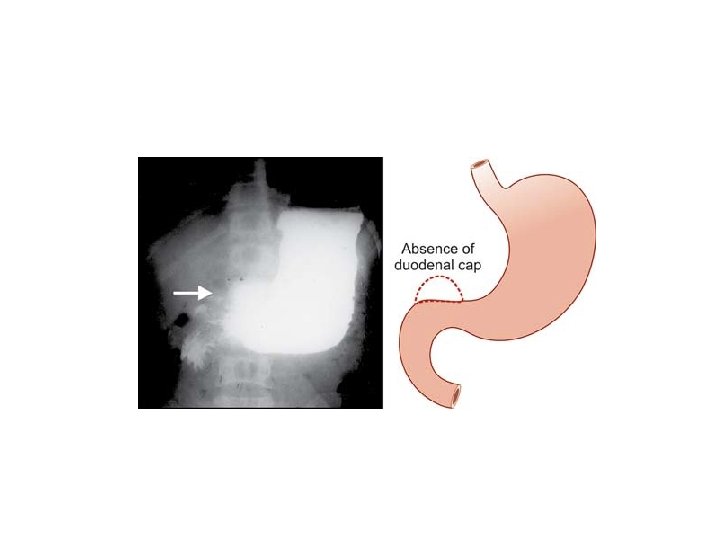
INVESTIGATIONS • Barium meal X-ray – – Deformed or absence of duodenal cap (because of spasm). – Appearance of ‘trifoliate’ duodenum is due to secondary duodenal diverticula which occurs as a result of scarring of ulcer. • Gastroscopy & biopsy • Estimation of serum gastrin level, serum calcium level.
DIFFERENTIAL DIAGNOSIS • Carcinoma stomach (pylorus) • Dyspepsia due to other causes – Hiatus hernia – Oesophagitis – Cholecystitis – Chronic pancreatitis

COMPLICATIONS • Pyloric stenosis: Due to scarring and cicatrisation of first part of the duodenum. • Bleeding (10%) • Perforation (5%) - Anterior ulcers perforate. • Residual abscess • Penetration to pancreas
TREATMENT MEDICAL THERAPY • H 2 antagoists and proton-pump inhibitors • Eradication therapy
SURGICAL TREATMENT Procedures devised for the treatment of duodenal ulcers have the common aim of excluding the damaging effects of acid from the duodenum. This has been achieved by diversion of the acid away from the duodenum, reducing the secretory potential of the stomach, or both.
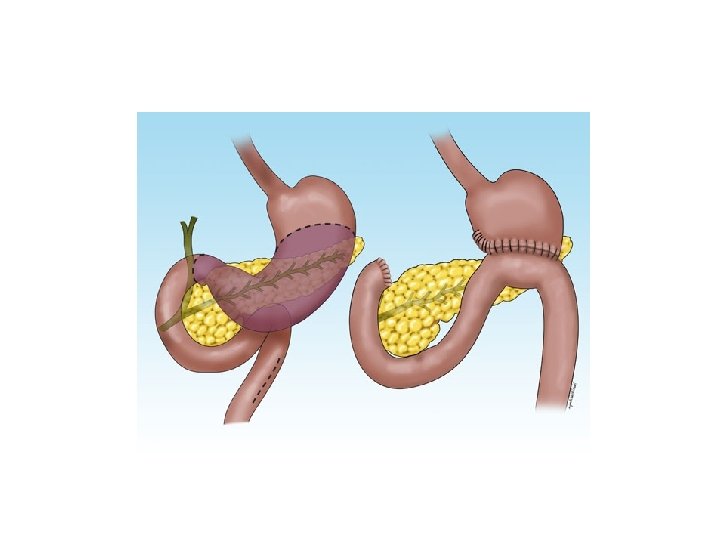
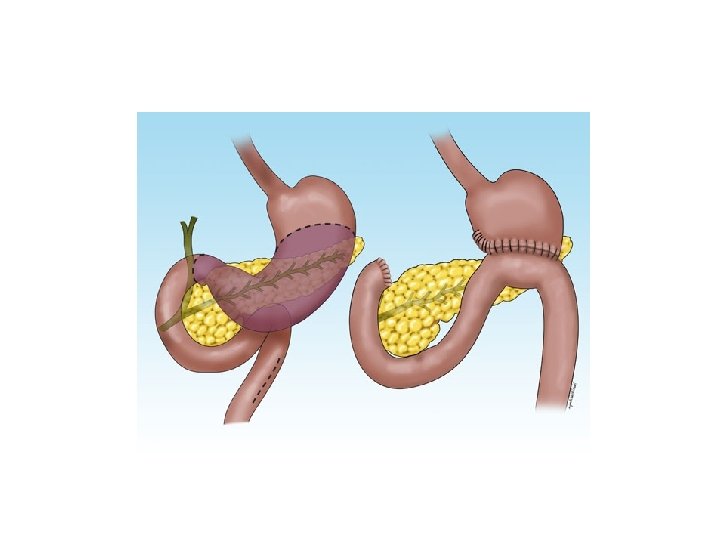
BILLROTH II GASTRECTOMY • Antrum and disal part of the body of stomach is mobilised by opening the greater and lesser omentum and dividing the gastroepiploic arteries, right gastric artery and the left gastric artery arcade at the limit of the resection. • The duodenum is closed off. • Following resection, the distal end of the stomach is narrowed by the closure of the lesser curve aspect of the remnant. • The greater curve aspect is then anastomosed, usually in a retrocolic fashion, to the jejunum.
• Trunkal / highly selective vagotomy
 Gastric ulcer
Gastric ulcer Peptic ulcer disease
Peptic ulcer disease Objectives of peptic ulcer
Objectives of peptic ulcer Salisylates
Salisylates Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Arsas symptoms
Arsas symptoms Patient counselling for peptic ulcer disease
Patient counselling for peptic ulcer disease Stomach ulcer diet menu
Stomach ulcer diet menu Modified johnson classification for gastric ulcer
Modified johnson classification for gastric ulcer Peptic ulcer diseas
Peptic ulcer diseas Gastric ulcer
Gastric ulcer Stages of peptic ulcer perforation
Stages of peptic ulcer perforation Johnson classification ulcer
Johnson classification ulcer Proton pump inhibitor
Proton pump inhibitor Stomach ulcer definition
Stomach ulcer definition Acholorhydria
Acholorhydria Goose neck deformity
Goose neck deformity Tea pot deformity of stomach
Tea pot deformity of stomach Classification of ulcer
Classification of ulcer Haemtemesis
Haemtemesis Clasificarea johnson ulcerelor
Clasificarea johnson ulcerelor Atrophic rhinitis
Atrophic rhinitis Primary atrophic rhinitis
Primary atrophic rhinitis Nasordin drop
Nasordin drop Gmail
Gmail Atrophic rhinitis
Atrophic rhinitis Primary atrophic rhinitis
Primary atrophic rhinitis Kavram çeşitleri
Kavram çeşitleri Atrophic vaginitis
Atrophic vaginitis Atrophic rhinitis
Atrophic rhinitis Atrophic rhinitis
Atrophic rhinitis Primary atrophic rhinitis
Primary atrophic rhinitis Typhoid ulcer and tuberculous ulcer
Typhoid ulcer and tuberculous ulcer