Neonatal Jaundice Physical Exam General appearance Jaundiced infant




- Slides: 24
Neonatal Jaundice 新生兒黃疸


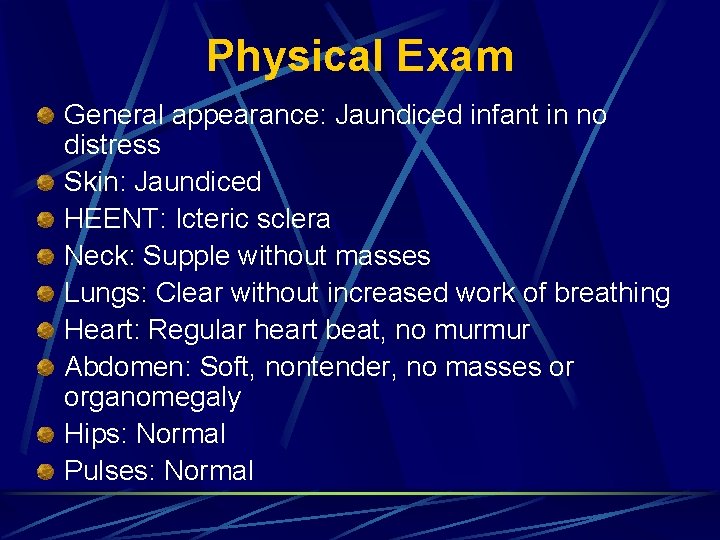
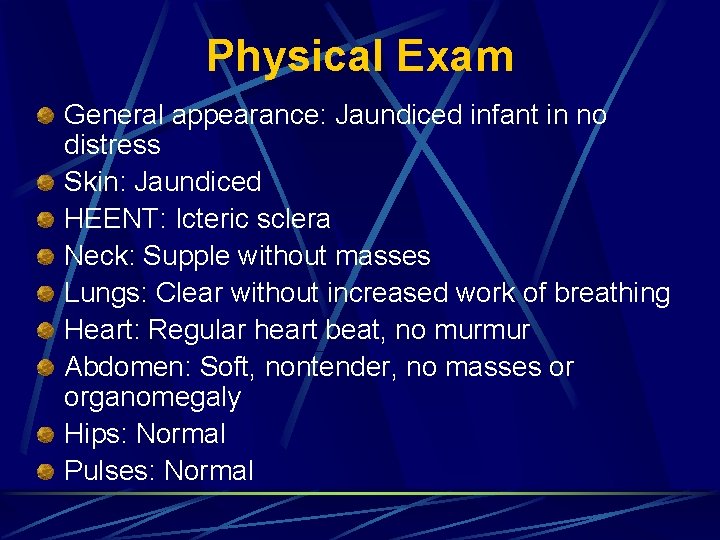
Physical Exam General appearance: Jaundiced infant in no distress Skin: Jaundiced HEENT: Icteric sclera Neck: Supple without masses Lungs: Clear without increased work of breathing Heart: Regular heart beat, no murmur Abdomen: Soft, nontender, no masses or organomegaly Hips: Normal Pulses: Normal
What is your differential diagnosis? Physiologic jaundice Breast milk jaundice Hemolytic disease of the newborn Congenital viral infection Breastfeeding jaundice Glucose-6 -phosphate dehydrogenase (G 6 PD) deficiency
Re-Evaluation of Differential Diagnosis Physiologic jaundice Explanation: l Jaundice that appears at birth or within the first 24 hours of life is always pathologic. Physiologic jaundice can be diagnosed by ruling out disorders by history, clinical findings, or laboratory results. Because this infants bilirubin was elevated prior to 24 hours of life, it is not physiologic.
Re-Evaluation of Differential Diagnosis Breast milk jaundice Explanation: l Breast milk jaundice develops in breastfed infants at approximately the first week of life. It gradually decreases over 3 -10 weeks. It is an indirect hyperbilirubinemia. Jaundice developed too early in this newborn.
Re-Evaluation of Differential Diagnosis Hemolytic disease of the newborn Explanation: l Whenever the indirect bilirubin increases quickly, especially in the first 24 hours of life, hemolytic disease of the newborn must be considered. The mothers blood type is O positive, which would put the infant at risk with a blood type of A or B.
Re-Evaluation of Differential Diagnosis Congenital viral infection Explanation: l Congenital viral infections usually are associated with an increase in direct or conjugated bilirubin. These infections may be associated with growth restriction, hepatosplenomegaly, microcephaly, and rashes
Re-Evaluation of Differential Diagnosis Breastfeeding jaundice Explanation: l Breastfeeding jaundice occurs in the first days of life. It is associated with decreased milk intake and possibly dehydration. This infants history reveals good intake with minimal weight loss.
Re-Evaluation of Differential Diagnosis Glucose-6 -phosphate dehydrogenase (G 6 PD) deficiency Explanation: l G 6 PD deficiency must be considered in a newborn with an indirect bilirubin approaching exchange levels or a level that is not responding to phototherapy.
What laboratory or x-ray studies would you order? Total bilirubin Direct or conjugated bilirubin Liver function tests Coombs test Complete blood count Liver ultrasound Reticulocyte count G 6 PD level
Laboratory and Radiologic Studies Total bilirubin Explanation: l A newborn who appears jaundiced requires a total bilirubin level be drawn. Estimation of the total bilirubin cannot be made by observation.
Laboratory and Radiologic Studies Direct or conjugated bilirubin Explanation: l Conjugated bilirubin needs to be checked with the first laboratory draw in a jaundiced newborn. A direct bilirubin 2 mg/d. L or 20 of the total bilirubin is always pathologic and requires a more extensive workup for liver disease and metabolic abnormalities.
Laboratory and Radiologic Studies Liver function tests Explanation: l Liver function tests do not need to be checked, unless there is evidence of liver disease on examination or an increase in conjugated bilirubin (infection, hemorrhage, hemolysis, galactosemia, hypothyroidism).
Laboratory and Radiologic Studies Coombs test Explanation: l Hemolysis is a common cause of indirect hyperbilirubinemia in the first 24 hours. A common cause is ABO incompatibility. Coombs test is usually positive. Rh incompatibility is not in the differential diagnosis of this patient because the mother is Rh positive.
Laboratory and Radiologic Studies Complete blood count Explanation: l Because hemolysis is a common cause of indirect hyperbilirubinemia, the complete blood count is needed to check for anemia, and the smear is needed to look for signs of hemolysis or other causes of anemia.
Laboratory and Radiologic Studies Liver ultrasound Explanation: l There is no evidence of liver disease from examination or from an increase in direct bilirubin. At this point, there is no reason to perform an ultrasound scan of the liver.
Laboratory and Radiologic Studies Reticulocyte count Explanation: l The reticulocyte count may help determine if hemolysis is present. ~~ ↑ when hemolysis/hemorrhage ≥ 3 days
Laboratory and Radiologic Studies G 6 PD level Explanation: l If the workup for hemolytic disease of the newborn is negative, other causes of a rapid increase in indirect bilirubin must be sought.
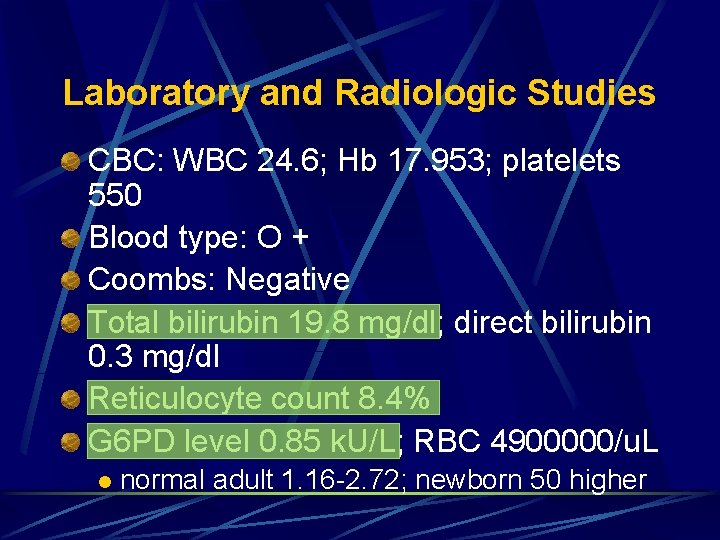
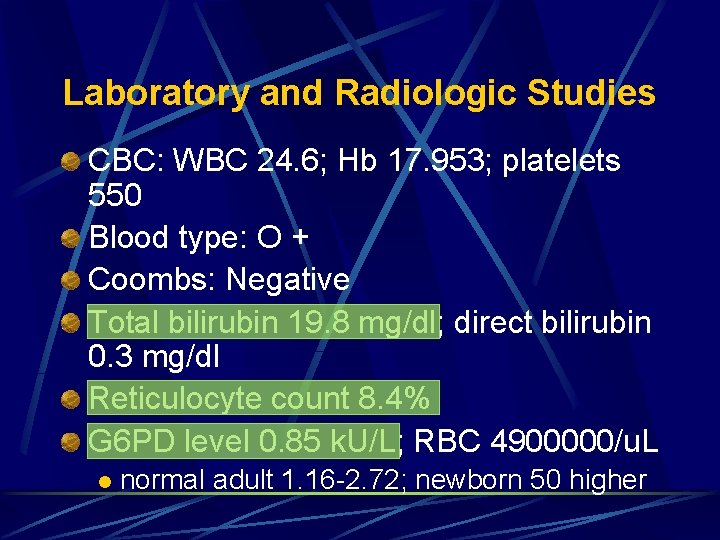
Laboratory and Radiologic Studies CBC: WBC 24. 6; Hb 17. 953; platelets 550 Blood type: O + Coombs: Negative Total bilirubin 19. 8 mg/dl; direct bilirubin 0. 3 mg/dl Reticulocyte count 8. 4% G 6 PD level 0. 85 k. U/L; RBC 4900000/u. L l normal adult 1. 16 -2. 72; newborn 50 higher
Final Diagnosis G 6 PD deficiency


 Neonatal jaundice physical examination
Neonatal jaundice physical examination A person screaming
A person screaming Verbal pain assessment
Verbal pain assessment Phototherapy function
Phototherapy function Jaundice chart
Jaundice chart Nursing diagnosis for neonatal jaundice
Nursing diagnosis for neonatal jaundice Hepatomogaly
Hepatomogaly Biliary atresia
Biliary atresia Obstructive jaundice differential diagnosis
Obstructive jaundice differential diagnosis General appearence
General appearence General physical exam
General physical exam General physical examination
General physical examination General appearance ill looking
General appearance ill looking General appearance description
General appearance description Describe george wilson. how does he react to tom's arrival?
Describe george wilson. how does he react to tom's arrival? Speeds
Speeds The best laid plans of mice and men poem
The best laid plans of mice and men poem Two-bit physical description
Two-bit physical description Leopard cycle
Leopard cycle Examples of co dominance
Examples of co dominance Mrs foul
Mrs foul I am not contraction
I am not contraction Aice general paper discursive essay
Aice general paper discursive essay Hand approach general paper
Hand approach general paper Yorkshire neonatal network
Yorkshire neonatal network