UNIT IV JAUNDICE JAUNDICE Jaundice or icterus refers



- Slides: 22
UNIT IV JAUNDICE
JAUNDICE • Jaundice or icterus refers to the yellow pigmentation of the skin or sclerae by bilirubin. • Bilirubin pigment has high affinity for elastic tissue - noticeable in tissues rich in elastin content. • High bilirubin in blood- hyper-bilirubin-aemia • Normal serum bilirubin - 0. 3 -1. 3 mg/dl, about 80% of which is unconjugated • Jaundice -clinically evident - total serum bilirubin exceeds 2 mg/dl NORMAL BILIRUBIN METABOLISM • Describe by: Source, transport, hepatic phase, intestinal phase 1. SOURCE OF BILIRUBIN • About 80 -85% derived -catabolism of haemoglobin • destruction of erythrocytes -bone marrow, spleen and liver.
• 15 -20% of the bilirubin - non-haemoglobin haemcontaining pigments such as myoglobin, catalase and cytochromes. • haem -converted to biliverdin by microsomal haem oxygenase • Bilirubin from- biliverdin by biliverdin reductase 2. TRANSPORT OF BILIRUBIN • Bilirubin release from macrophages- circulates as unconjugated bilirubin in plasma bound to albumin. • sulfonamides and salicylates compete for albumin binding and displace bilirubin from albumin, • facilitating bilirubin to enter into brain in neonates and increase risk of kernicterus. • Bilirubin found in body fluids- proportion to their albumin content - CSF, joint effusions, cysts
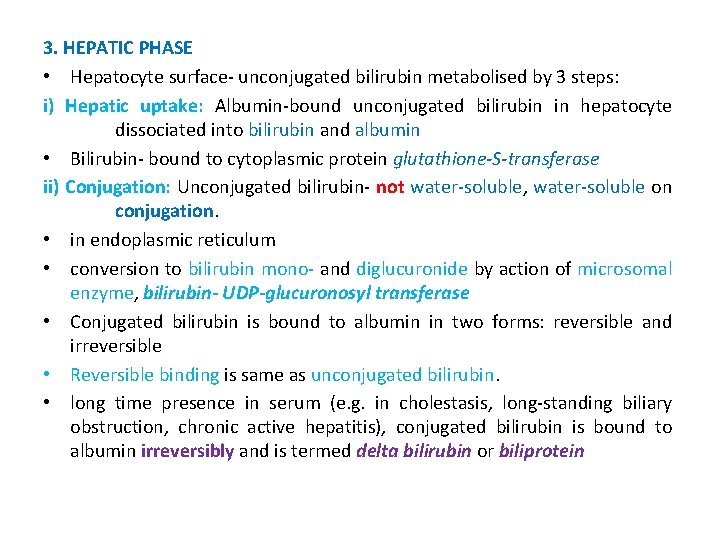
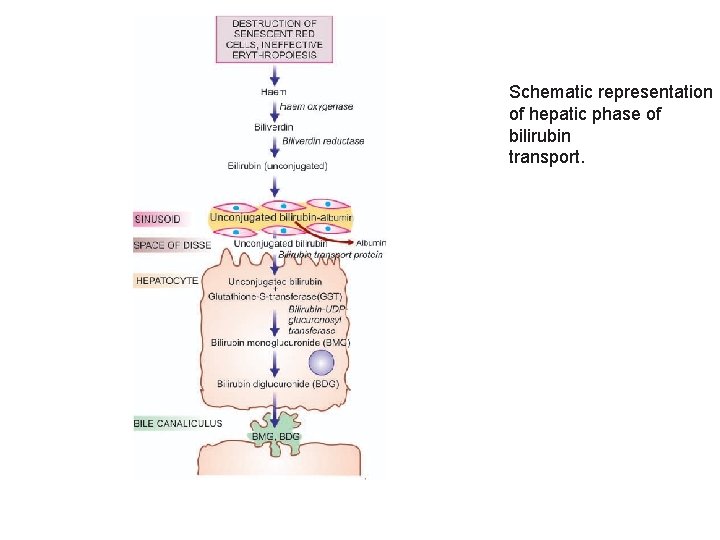
3. HEPATIC PHASE • Hepatocyte surface- unconjugated bilirubin metabolised by 3 steps: i) Hepatic uptake: Albumin-bound unconjugated bilirubin in hepatocyte dissociated into bilirubin and albumin • Bilirubin- bound to cytoplasmic protein glutathione-S-transferase ii) Conjugation: Unconjugated bilirubin- not water-soluble, water-soluble on conjugation. • in endoplasmic reticulum • conversion to bilirubin mono- and diglucuronide by action of microsomal enzyme, bilirubin- UDP-glucuronosyl transferase • Conjugated bilirubin is bound to albumin in two forms: reversible and irreversible • Reversible binding is same as unconjugated bilirubin. • long time presence in serum (e. g. in cholestasis, long-standing biliary obstruction, chronic active hepatitis), conjugated bilirubin is bound to albumin irreversibly and is termed delta bilirubin or biliprotein
• conjugated bilirubin is not excreted by kidney, and remains detectable in serum for sufficient time after recovery from diseases listed above iii) Secretion into bile: Conjugated (water-soluble) bilirubin is rapidly transported directly into bile canaliculi by energydependent process and then excreted into the bile
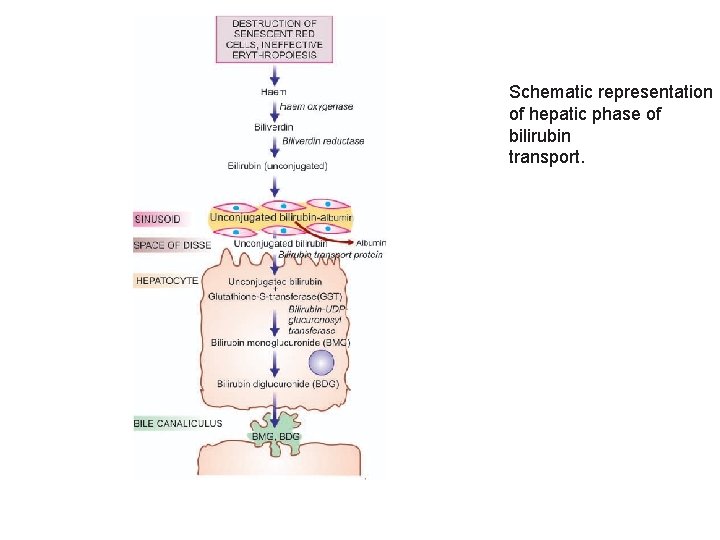
Schematic representation of hepatic phase of bilirubin transport.
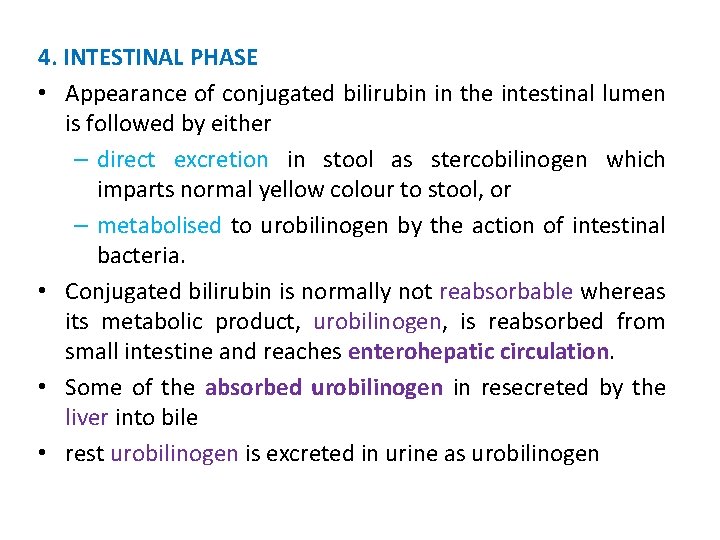
4. INTESTINAL PHASE • Appearance of conjugated bilirubin in the intestinal lumen is followed by either – direct excretion in stool as stercobilinogen which imparts normal yellow colour to stool, or – metabolised to urobilinogen by the action of intestinal bacteria. • Conjugated bilirubin is normally not reabsorbable whereas its metabolic product, urobilinogen, is reabsorbed from small intestine and reaches enterohepatic circulation. • Some of the absorbed urobilinogen in resecreted by the liver into bile • rest urobilinogen is excreted in urine as urobilinogen

CLASSIFICATION AND FEATURES OF JAUNDICE • Based on pathophysiology, jaundice may result from one or more of following mechanisms: 1. Increased bilirubin production 2. Decreased hepatic uptake 3. Decreased hepatic conjugation 4. Decreased excretion of bilirubin into bile • old classification 3 predominant types: – pre-hepatic (haemolytic) – hepatic – post-hepatic cholestatic • hyperbilirubinaemia due to first three mechanisms is mainly unconjugated • last variety yields mainly conjugated hyperbilirubinaemia.
• simple test: differentiate hyperbilirubinaemia is of unconjugated or conjugated variety – Its presence in urine or not; – its absence in urine suggests unconjugated hyperbilirubinaemia since unconjugated bilirubin is not filtered by the glomerulus • Based on these mechanisms, the pathogenesis and main features of the two predominant forms of hyperbilirubinaemia are discussed below I. Predominantly Unconjugated Hyperbilirubinaemia This form of jaundice can result from the following three sets of conditions: 1. Increased Bilirubin Production (Haemolytic, Acholuric Or Prehepatic Jaundice). • results from excessive red cell destruction as occurs in intra and extravascular haemolysis or due to ineffective erythropoiesis.

• increased release of haemoglobin from excessive breakdown of red cells -overproduction of bilirubin. • Hyperbilirubinaemia- capacity of the liver to conjugate large amount of bilirubin is exceeded. • premature infants: liver is deficient in enzyme necessary for conjugation while the rate of red cell destruction is high. • Since there is predominantly unconjugated hyperbilirubinaemia in such cases, – danger of permanent brain damage in these infants from kernicterus – when serum level of unconjugated bilirubin exceeds 20 mg/dl. • Laboratory data in haemolytic jaundice, – reveal normal serum levels of transaminases, alkaline phosphatase and proteins. – Bile pigment being unconjugated type is absent from urine • there is dark brown colour of stools and urine due to excessive faecal excretion of bile pigment and increased urinary excretion of urobilinogen
2. DECREASED HEPATIC UPTAKE • dissociation of the pigment from albumin and its binding to cytoplasmic protein, GST or ligandin, may be deranged in certain conditions e. g. due to drugs, prolonged starvation and sepsis. 3. DECREASED BILIRUBIN CONJUGATION • deranged hepatic conjugation due to defect or deficiency of enzyme, glucuronosyl transferase • occur in certain inherited disorders of the enzyme (e. g. Gilbert’s syndrome and Crigler-Najjar syndrome), or • acquired defects in its activity (e. g. due to drugs, hepatitis, cirrhosis). • physiologic neonatal jaundice is also partly due to relative deficiency of UDP-glucuronosyl transferase in neonatal liver and is partly due to increased rate of red cell destruction in neonates.
II. Predominantly Conjugated Hyperbilirubinaemia (Cholestasis) • failure of normal amounts of bile to reach the duodenum • Morphologically, cholestasis means accumulation of bile in liver cells and biliary passages • defect in excretion may be within biliary canaliculi of hepatocyte and in microscopic bile ducts (intrahepatic cholestasis or medical jaundice), or • there may be mechanical obstruction to extrahepatic biliary excretory apparatus (extrahepatic cholestasis or obstructive jaundice). • extrahepatic cholestasis or obstructive jaundice is often treatable with surgery, • intrahepatic cholestasis or medical jaundice cannot be benefitted by surgery but worsen • Prolonged cholestasis of either of the two types may progress to biliary cirrhosis
1. INTRAHEPATIC CHOLESTASIS • Intrahepatic cholestasis is due to impaired hepatic excretion of bile and may occur from hereditary or acquired disorders. i) Hereditary disorders • producing intrahepatic obstruction to biliary excretion are characterised by ‘pure cholestasis’ e. g. in Dubin-Johnson syndrome, Rotor syndrome, fibrocystic disease of pancreas and cholestatic jaundice of pregnancy. ii) Acquired disorders • intrahepatic excretory defect of bilirubin are largely due to hepatocellular diseases and hence are termed ‘hepatocellular cholestasis’ e. g. in viral hepatitis, alcoholic hepatitis, and druginduced cholestasis such as from administration of chlorpromazine and oral contraceptives.
The features of intrahepatic cholestasis include: • predominant conjugated hyper-bilirubinaemia due to regurgitation of conjugated bilirubin into blood, • bilirubinuria, elevated levels of serum bile acids and consequent pruritus, • elevated serum alkaline phosphatase • hyperlipidaemia • hypo-prothrombinaemia. • ‘Pure cholestasis’ can be distinguished from ‘hepatocellular cholestasis’ by elevated serum levels of transaminases in latter due to liver cell injury

• Liver biopsy in cases with intrahepatic cholestasis reveals milder degree of cholestasis than the extrahepatic disorders • biliary canaliculi of the hepatocytes are dilated and contain characteristic elongated green-brown bile plugs (Figure). • The cytoplasm of the affected hepatocytes shows feathery degeneration. • Canalicular bile stasis eventually causes proliferation of intralobular ductules followed by periportal fibrosis and produces a picture resembling biliary cirrhosis 2. EXTRAHEPATIC CHOLESTASIS • Extrahepatic cholestasis results from mechanical obstruction to large bile ducts outside the liver or within the porta hepatis • common causes: gallstones, inflammatory strictures, carcinoma head of pancreas, tumours of bile duct, sclerosing cholangitis and congenital atresia of extrahepatic ducts • obstruction may be complete and sudden with eventual progressive obstructive jaundice, or • obstruction may be partial and incomplete resulting in intermittent jaundice.
• features of extrahepatic cholestasis (obstructive jaundice), like in intrahepatic cholestasis, are: • predominant conjugated hyperbilirubinaemia, • bilirubinuria, • elevated serum bile acids causing intense pruritus, • high serum alkaline phosphatase and • hyperlipidaemia
• In obstructive jaundice, there is – malabsorption of fat-soluble vitamins (A, D, E and K) and – Steatorrhoea (high fats in stool) resulting in vitamin K deficiency. • In such cases: – Prolonged prothrombin time: shows improvement following parenteral administration of vitamin K, whereas – hypoprothrombinaemia due to hepatocellular disease shows no improvement in prothrombin time with vitamin K administration • Stools of such patients are clay-coloured due to absence of bilirubin metabolite, stercobilin, in faeces and disappearance of urobilinogen from urine • patients may have fever due to high incidence of bacterial infections
• Liver biopsy in cases with extrahepatic cholestasis shows more marked changes of cholestasis • Since obstruction is in extrahepatic bile ducts, there is progressive retrograde extension of bile stasis into intrahepatic duct system • This results in dilatation of bile ducts and rupture of canaliculi with extravasation of bile producing bile lakes. • Since bile is toxic, regions of bile lakes are surrounded by focal necrosis of hepatocytes • Stasis of bile predisposes to ascending bacterial infections with accumulation of polymorphs around the dilated ducts • Eventually, there is proliferation of bile ducts and appearance may mimic biliary cirrhosis
• Reference: Textbook of Pathology, by Harsh Mohan (Author), JAYPEE Publication
 Pre-hepatic jaundice
Pre-hepatic jaundice Jaundice levels
Jaundice levels Pathologic jaundice
Pathologic jaundice Grading of jaundice in neonates
Grading of jaundice in neonates Conjugated hyperbilirubinemia
Conjugated hyperbilirubinemia Jaundice
Jaundice Cern icterus
Cern icterus Icterus neonati
Icterus neonati Rotor syndrome
Rotor syndrome Icterus neonati
Icterus neonati Icterus neonati
Icterus neonati Pseudocysta jelentése
Pseudocysta jelentése Post hepatic jaundice
Post hepatic jaundice Dr bino
Dr bino Unit 10, unit 10 review tests, unit 10 general test
Unit 10, unit 10 review tests, unit 10 general test Post hepatic jaundice
Post hepatic jaundice Phototherapy machine parts
Phototherapy machine parts Palmar erythema causes
Palmar erythema causes Digestion
Digestion Benjamin classification obstructive jaundice
Benjamin classification obstructive jaundice Jaundice differential diagnosis
Jaundice differential diagnosis Pathologic jaundice
Pathologic jaundice Management of neonatal jaundice pdf
Management of neonatal jaundice pdf