Neonatal Jaundice Clinical Guideline Education Presentation V 2
- Slides: 32
Neonatal Jaundice Clinical Guideline Education Presentation V 2. 0 30 minutes Towards your CPD Hours
References: The Queensland Maternity and Neonatal Clinical Guidelines Program clinical guideline Neonatal jaundice is the primary reference for this package. Recommended citation: Queensland Maternity and Neonatal Clinical Guidelines Program. Neonatal jaundice. Clinical Guideline Education Presentation V 2. 0. Queensland Health. 2013. Disclaimer: This presentation is an implementation tool and should be used in conjunction with the published guideline. This information does not supersede or replace the guideline. Consult the guideline for further information and references. Feedback and contact details: M: GPO Box 48 Brisbane QLD 4001 | E: MN-Guidelines@health. qld. gov. au | URL: www. health. qld. gov. au/qcg Funding: The Queensland Maternity and Neonatal Clinical Guidelines Program is supported by the Clinical Access and Redesign Unit, Queensland Health. Copyright: © State of Queensland (Queensland Health) 2013 This work is licensed under a Creative Commons Attribution Non-Commercial No Derivatives 3. 0 Australia licence. In essence, you are free to copy and communicate the work in its current form for non-commercial purposes, as long as you attribute the Queensland Maternity and Neonatal Clinical Guidelines Program, Queensland Health and abide by the licence terms. You may not alter or adapt the work in any way. To view a copy of this licence, visit http: //creativecommons. org/licenses/by-nc-nd/3. 0/au/deed. en For further information contact Queensland Maternity and Neonatal Clinical Guidelines Program, RBWH Post Office, Herston Qld 4029, email MN-guidelines@health. qld. gov. au, phone (+61) 07 3131 6777. For permissions beyond the scope of this licence contact: Intellectual Property Officer, Queensland Health, GPO Box 48, Brisbane Qld 4001, email ip_officer@health. qld. gov. au, phone (07) 3234 1479. Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 2
Objectives • To gain an understanding of neonatal jaundice: ◦ ◦ Definition Primary prevention strategies Assessment and investigations Treatment options § Phototherapy § Exchange transfusion § Pharmacological therapy ◦ Discharge planning Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 3
Definition • Neonatal jaundice ◦ Refers to the yellow discolouration in the skin and mucous membranes ◦ Associated with hyperbilirubinaemia § Raised levels of bilirubin in the blood • Significant hyperbilirubinaemia ◦ Serum bilirubin elevated to a level that requires treatment Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 4
Incidence • Term babies: 50 -60% • Preterm babies: 80% • Physiological ◦ Most common • Pathological ◦ Significant because the cause requires investigation ◦ Aim to prevent bilirubin encephalopathy Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 5
Physiological jaundice • Occurs in newborns due to a: ◦ Higher concentration of red blood cells ◦ Shorter life span of newborn red blood cells ◦ Slower metabolism, circulation and excretion of bilirubin • • Frequently exacerbated by inadequate milk intake Not associated with underlying disease Usually benign Breast milk jaundice is benign Source: Mamatoto midwves [accessed 2013 March 18; http: //mamatotomidwives. com. au/ ] Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 6
Pathological jaundice • Investigate: ◦ Jaundice occurring within 24 hours of age ◦ Increase of bilirubin > 8. 5 micromol/L/hour ◦ Jaundice persisting after 2 weeks in term or 3 weeks in preterm babies ◦ Clay or white coloured stools ◦ Conjugated bilirubin > 25 micromol/L • Seek paediatrician / neonatology advice Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 7
Bilirubin encephalopathy • Risk factors: ◦ Preterm birth ◦ Rapid rate of rise of serum bilirubin ◦ Hypoalbuminaemia ◦ Other co-morbidities, e. g. § Sepsis § Asphyxia § Acidosis Source: Stanford School of Medicine [accessed 2013 March 5 http: //newborns. stanford. edu/Photo. Gallery/] Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 8
Acute bilirubin encephalopathy • Clinical manifestations of bilirubin toxicity seen in the first few weeks after birth • Initial signs: ◦ ◦ Lethargy Irritability Apnoea Hypotonia and poor suck Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 9
Chronic bilirubin encephalopathy • Persistent brain dysfunction ◦ ◦ ◦ Athetoid cerebral palsy Hearing deficit Oculomotor disturbances Dental dysplasia Intellectual impairment • Kernicterus ◦ Pathological term ◦ Clinically used to refer to the syndrome and sequelae of bilirubin encephalopathy Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 10
Prevention • Test all pregnant women: ◦ ABO and Rh (D) blood types ◦ Red cell antibodies: § If present → test cord blood: – – Blood group including the Rh type Direct antiglobulin test (DAT/Coombs test) Full blood count for haemoglobin and haematocrit Discuss with neonatologist • Ensure adequate support for all breastfeeding women ◦ Refer to Guideline: Breastfeeding initiation Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 11
Care for all babies • Assess risk factors for significant hyperbilirubinaemia: ◦ Gestational age < 38 weeks ◦ Sibling with neonatal jaundice who required phototherapy ◦ Mother's intention to breastfeed exclusively ◦ Visible jaundice in the first 24 hours following birth • Early visual inspection for jaundice • Educate and encourage parents to observe for signs of adequate hydration, feeding and jaundice Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 12
Care for all babies Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 13
Parent education • Educate and encourage parents to observe for signs of adequate hydration, feeding and jaundice • Seek advice if concerned Source: Stanford School of Medicine [accessed 2013 March 5 http: //newborns. stanford. edu/Photo. Gallery/] Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 14
Visual examination • Check the naked baby in bright and preferably natural light • Examination of the sclerae, gums and blanched skin is useful across all skin tones • Cephalo-caudal progression of jaundice • Can lead to errors, particularly in babies: ◦ ◦ With darker skin tones Who are preterm Under 36 hours of age Receiving phototherapy Source: Mamatoto midwves [accessed 2013 March 18; http: //mamatotomidwives. com. au/ ] Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 15
Transcutaneous bilirubin • For babies ◦ Gestational age of 35 weeks or more ◦ More than 24 hours of age • May decrease the number of heel pricks and/or invasive blood tests • If not available → measure serum bilirubin • If Tc. B level greater than 250 micromol/litre → measure serum bilirubin Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 16
Total serum bilirubin • If Tc. B not available or indicated • For babies ◦ Gestational age < 35 weeks ◦ < 24 hours of age • If bilirubin level > 250 micromol/L • Preferred once baby is at the relevant treatment threshold and for subsequent measurements Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 17
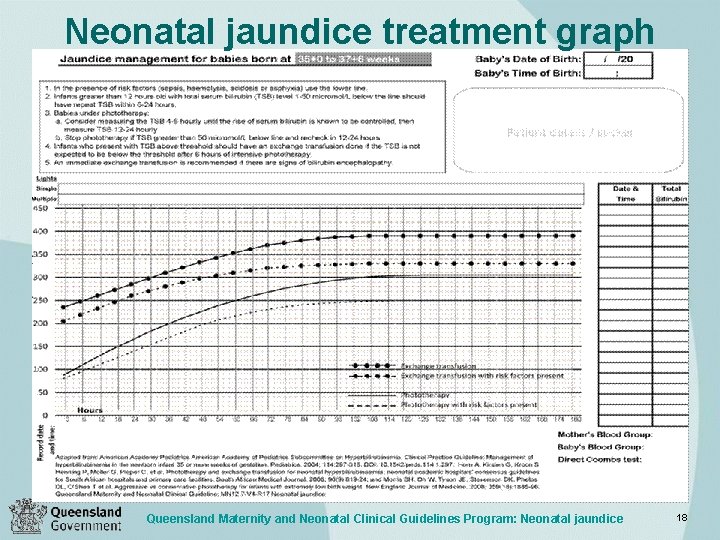
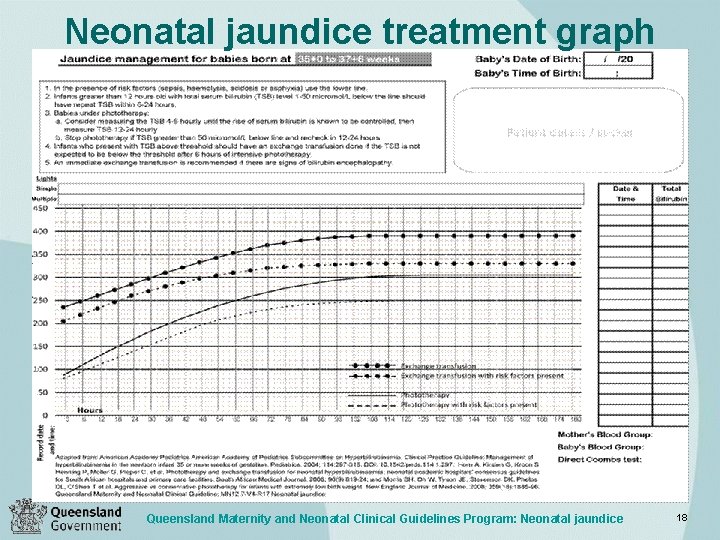
Neonatal jaundice treatment graph Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 18
All jaundiced babies • Do not use sunlight as treatment for hyperbilirubinaemia • Discuss with and provide parent and carer information • Encourage mother to breastfeed every 3 hours and wake baby if necessary • Do not subtract conjugated bilirubin from total serum bilirubin when making decisions about the management of hyperbilirubinaemia Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 19
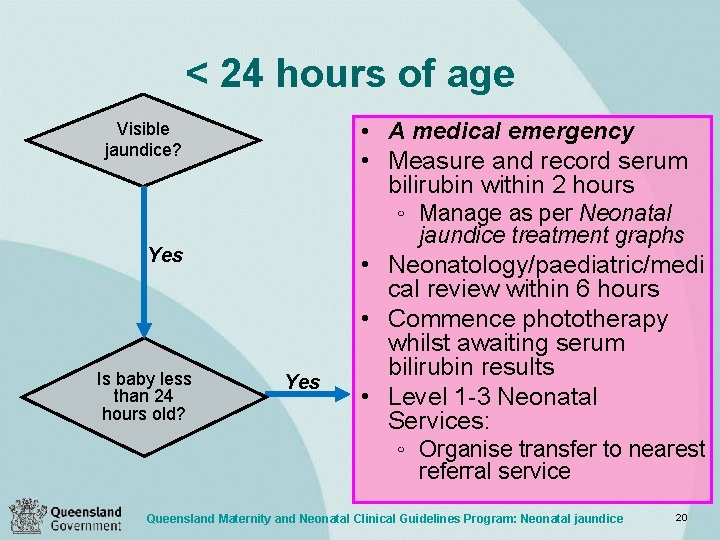
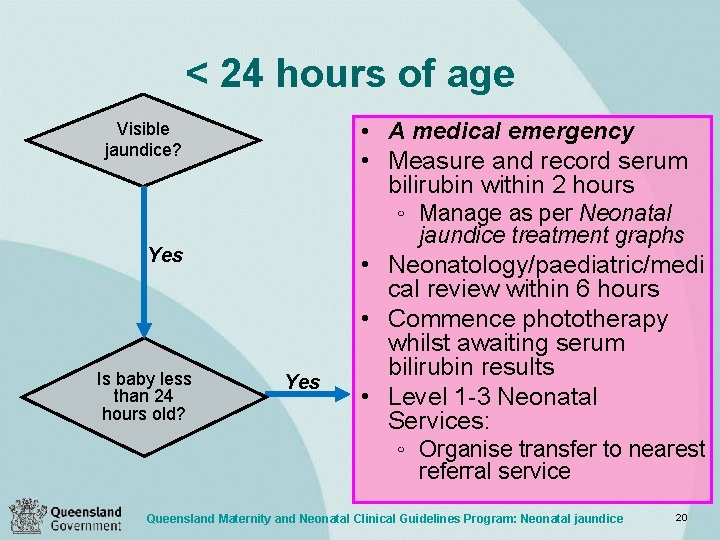
< 24 hours of age • A medical emergency • Measure and record serum bilirubin within 2 hours ◦ Manage as per Neonatal Visible jaundice? jaundice treatment graphs Yes Is baby less than 24 hours old? Yes • Neonatology/paediatric/medi cal review within 6 hours • Commence phototherapy whilst awaiting serum bilirubin results • Level 1 -3 Neonatal Services: ◦ Organise transfer to nearest referral service Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 20
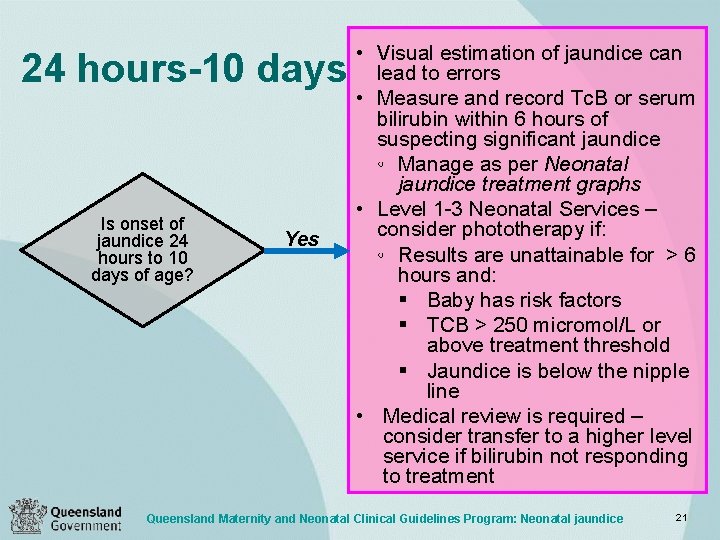
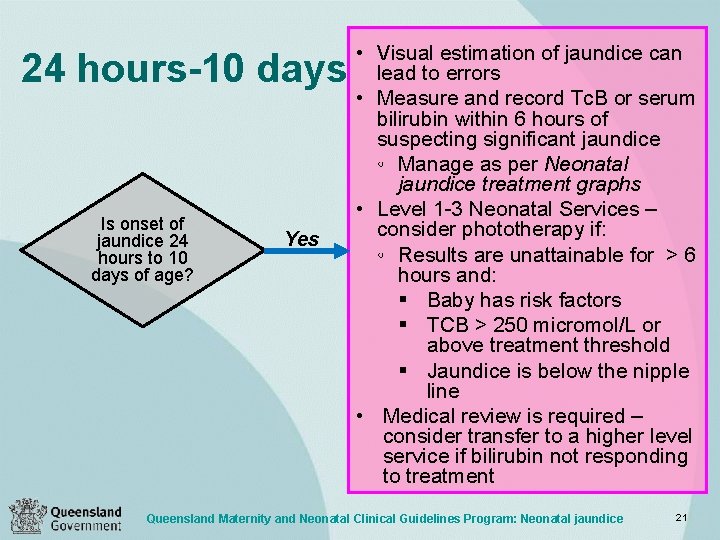
24 hours-10 days Is onset of jaundice 24 hours to 10 days of age? Yes • Visual estimation of jaundice can lead to errors • Measure and record Tc. B or serum bilirubin within 6 hours of suspecting significant jaundice ◦ Manage as per Neonatal jaundice treatment graphs • Level 1 -3 Neonatal Services – consider phototherapy if: ◦ Results are unattainable for > 6 hours and: § Baby has risk factors § TCB > 250 micromol/L or above treatment threshold § Jaundice is below the nipple line • Medical review is required – consider transfer to a higher level service if bilirubin not responding to treatment Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 21
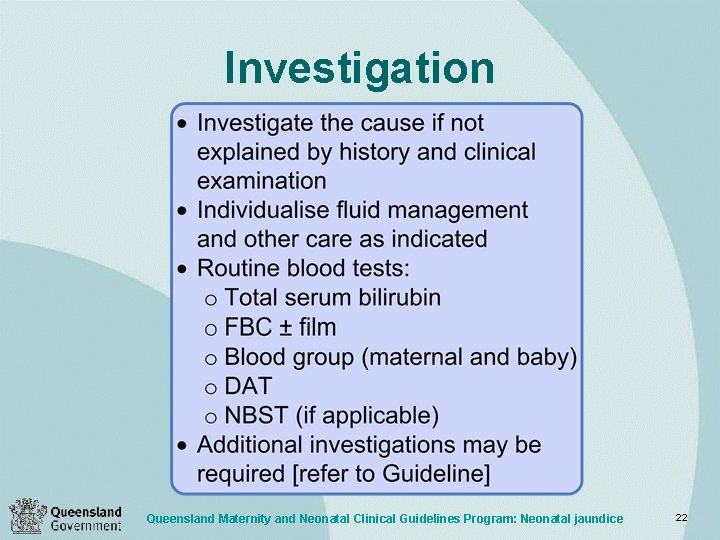
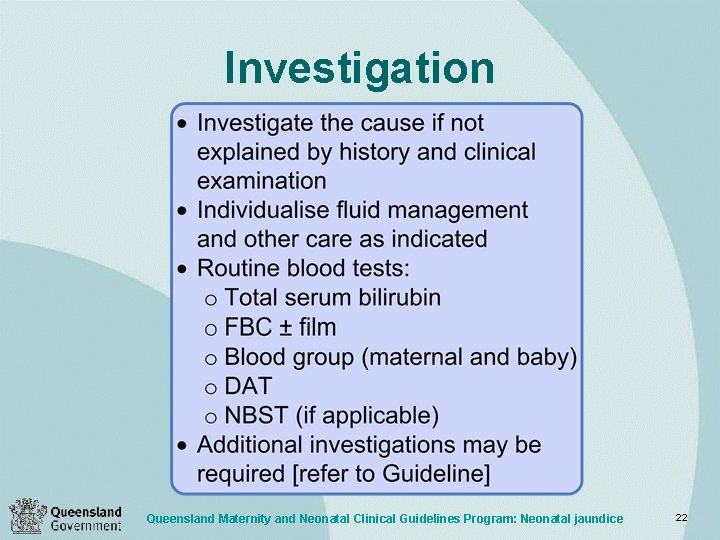
Investigation Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 22
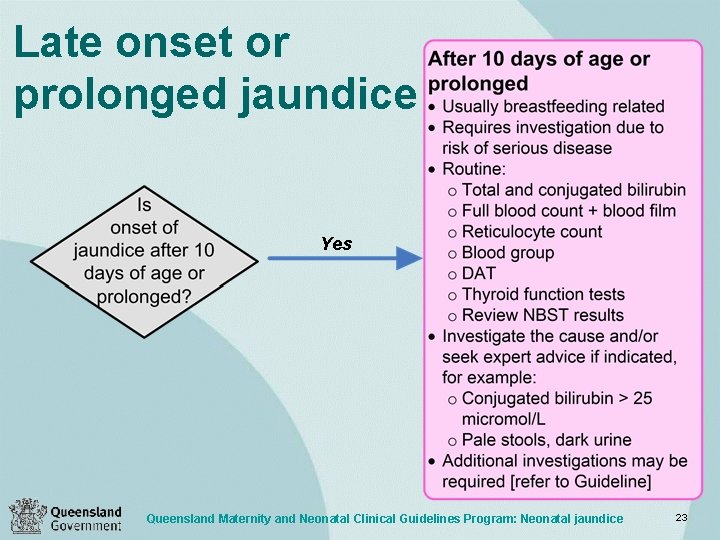
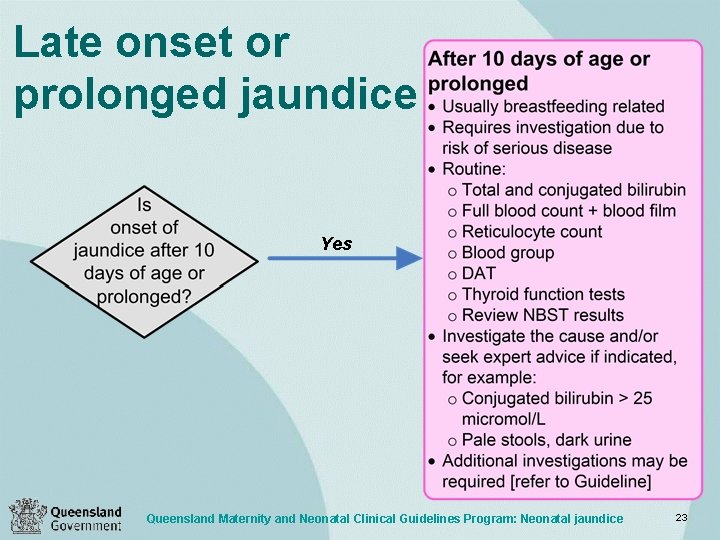
Late onset or prolonged jaundice Yes Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 23
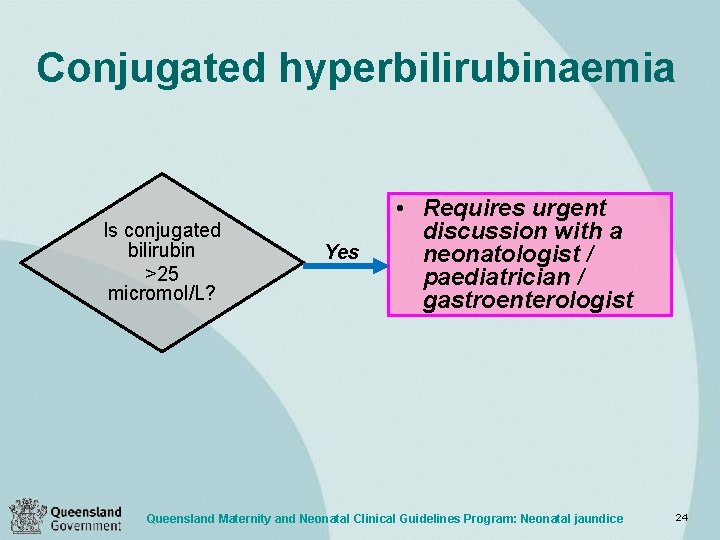
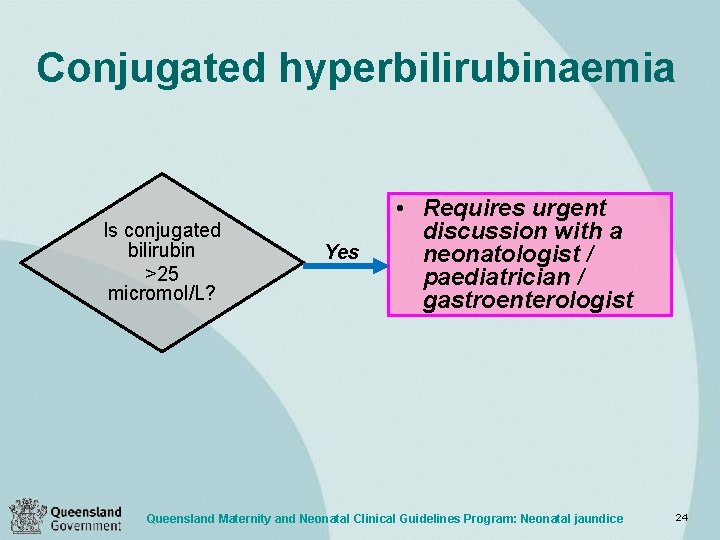
Conjugated hyperbilirubinaemia Is conjugated bilirubin >25 micromol/L? Yes • Requires urgent discussion with a neonatologist / paediatrician / gastroenterologist Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 24
Treatment http: //www. draeger. com. au/media/10/01/34/10013438 /jaundice_booklet_for_parents_9050615_en. pdf • Phototherapy • Exchange transfusion • Pharmacological agents • Adequate hydration is important Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 25
• Fibreoptic phototherapy is not recommended for babies > 37 weeks • Use fibreoptic, LED or conventional lights in babies < 37 weeks • Initiate continuous multiple lights if SBR: ◦ Is rising rapidly (>8. 5 mmol/L per hour) ◦ Is < 50 micromol/L below the exchange transfusion threshold ◦ Fails to respond to single bank of lights within 6 hours of starting Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice Source: http: //upload. wikimedia. org /wikipedia/commons/d/d 9/Jaundice_p hototherapy. jpg Accessed: 19/11/12 Phototherapy 26
Phototherapy parent information • • Why treatment is necessary Maximum area of skin exposed Need for eye protection and eye care Temperature monitored (thermoneutral environment) • Potential impact on breastfeeding – reassure cuddle time allowed • Need for additional fluids – not routine Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 27
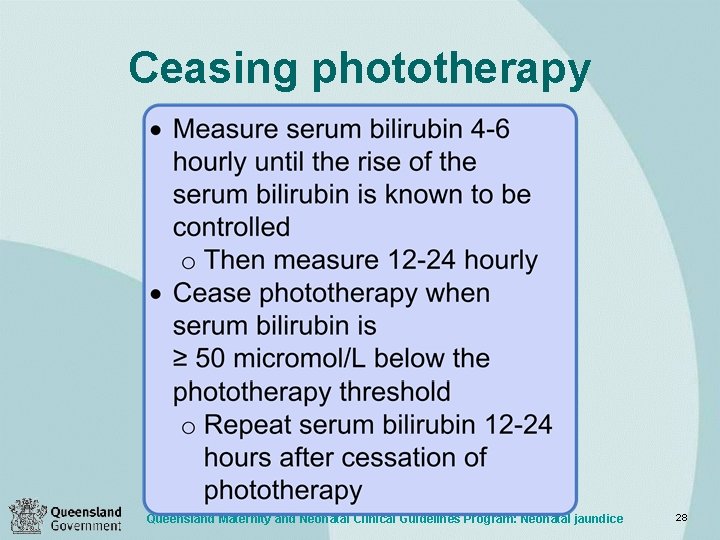
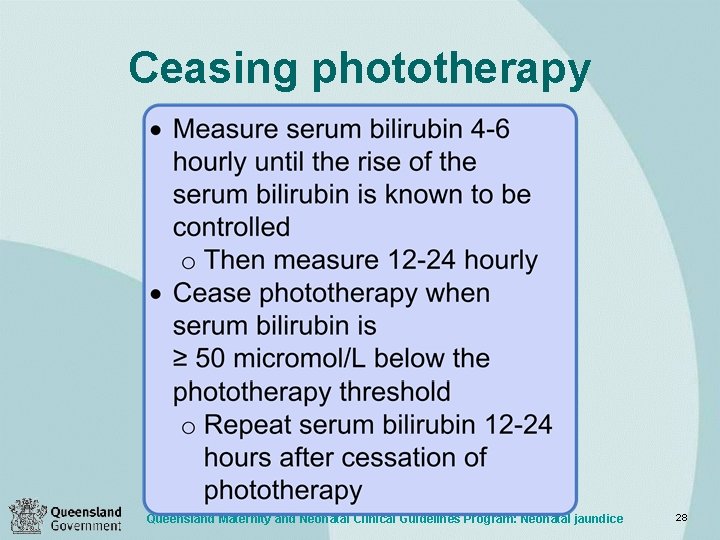
Ceasing phototherapy Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 28
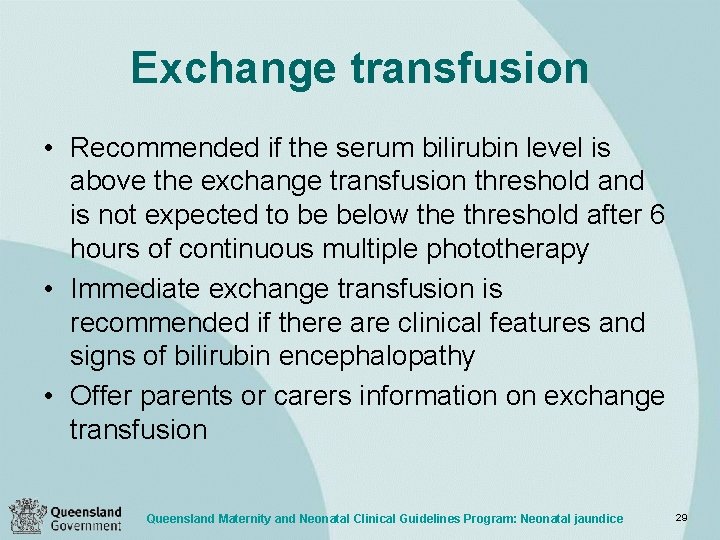
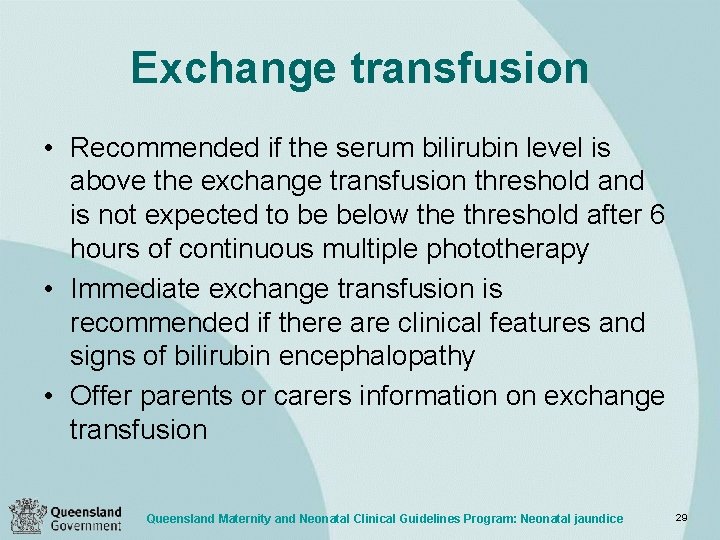
Exchange transfusion • Recommended if the serum bilirubin level is above the exchange transfusion threshold and is not expected to be below the threshold after 6 hours of continuous multiple phototherapy • Immediate exchange transfusion is recommended if there are clinical features and signs of bilirubin encephalopathy • Offer parents or carers information on exchange transfusion Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 29
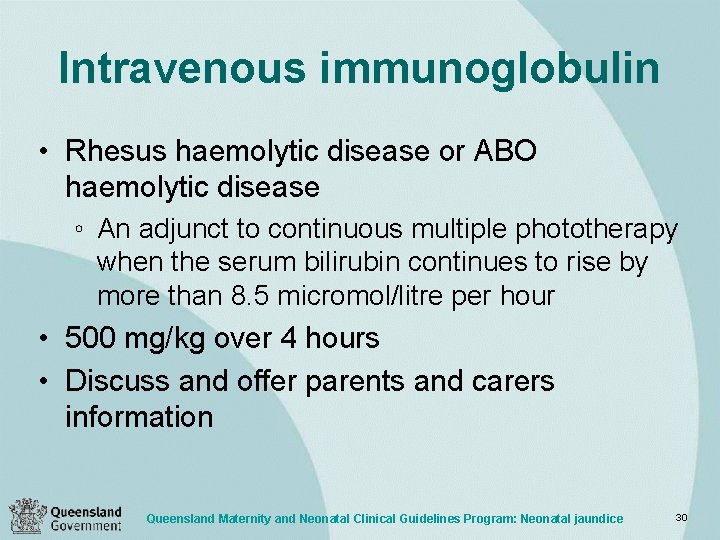
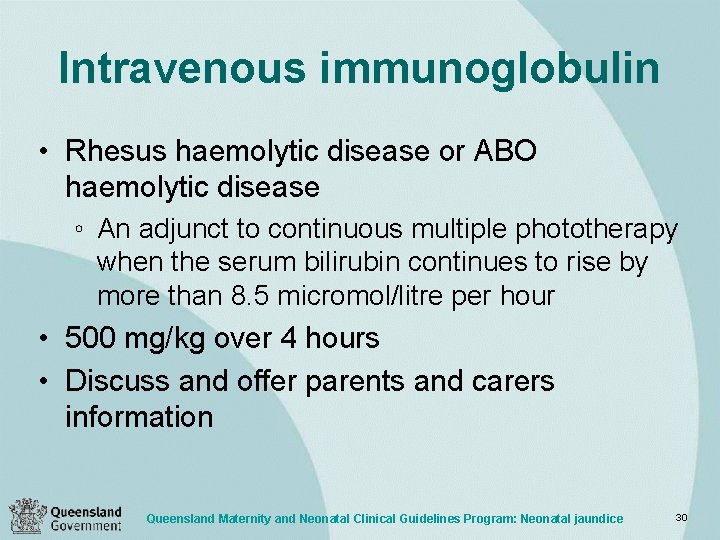
Intravenous immunoglobulin • Rhesus haemolytic disease or ABO haemolytic disease ◦ An adjunct to continuous multiple phototherapy when the serum bilirubin continues to rise by more than 8. 5 micromol/litre per hour • 500 mg/kg over 4 hours • Discuss and offer parents and carers information Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 30
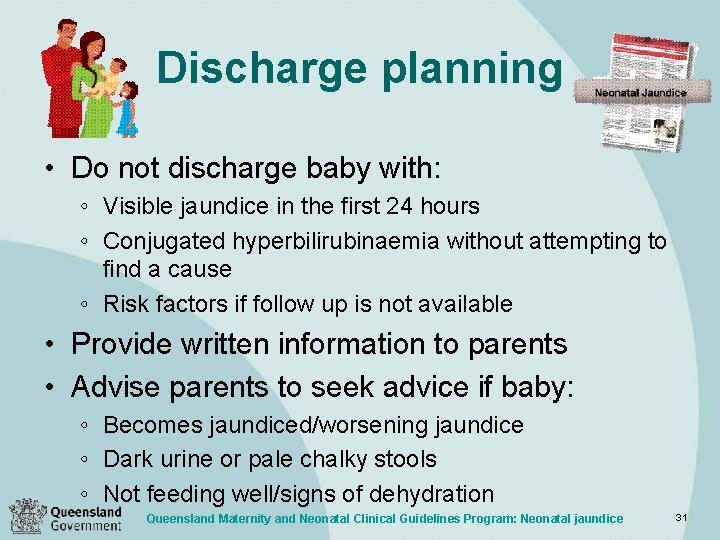
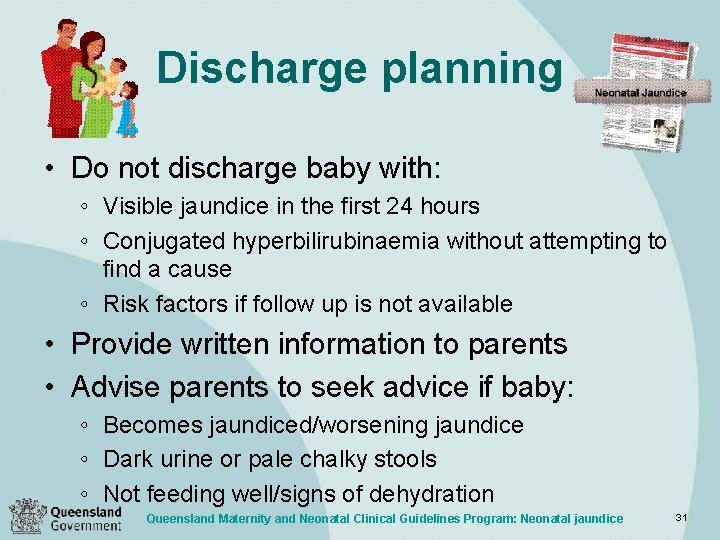
Discharge planning • Do not discharge baby with: ◦ Visible jaundice in the first 24 hours ◦ Conjugated hyperbilirubinaemia without attempting to find a cause ◦ Risk factors if follow up is not available • Provide written information to parents • Advise parents to seek advice if baby: ◦ Becomes jaundiced/worsening jaundice ◦ Dark urine or pale chalky stools ◦ Not feeding well/signs of dehydration Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 31
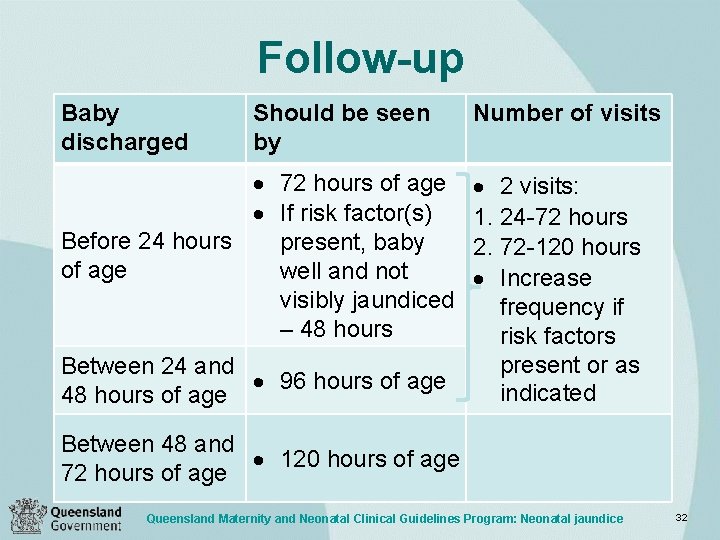
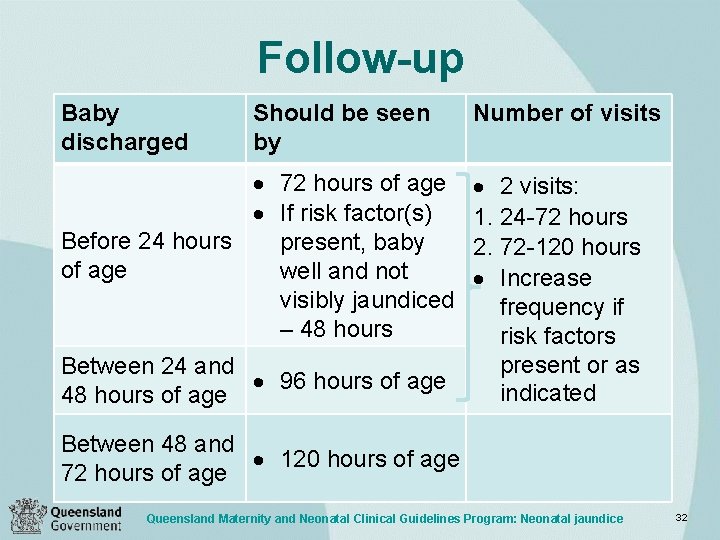
Follow-up Baby discharged Should be seen by 72 hours of age If risk factor(s) Before 24 hours present, baby of age well and not visibly jaundiced – 48 hours Between 24 and 96 hours of age 48 hours of age Number of visits 2 visits: 1. 24 -72 hours 2. 72 -120 hours Increase frequency if risk factors present or as indicated Between 48 and 120 hours of age 72 hours of age Queensland Maternity and Neonatal Clinical Guidelines Program: Neonatal jaundice 32
 Parts of phototherapy machine
Parts of phototherapy machine Neonatal jaundice curve
Neonatal jaundice curve Jaundice level
Jaundice level Neonatal jaundice
Neonatal jaundice Intrahepatic jaundice
Intrahepatic jaundice Neonatal jaundice physical examination
Neonatal jaundice physical examination Obstructive jaundice lab diagnosis
Obstructive jaundice lab diagnosis Guideline clinical nutrition in patients with stroke
Guideline clinical nutrition in patients with stroke Aki kdigo 2012
Aki kdigo 2012 Dr friedman cushing's
Dr friedman cushing's Jaundice case presentation
Jaundice case presentation Clinical presentation of hodgkin's lymphoma
Clinical presentation of hodgkin's lymphoma Pulmonary embolism shock
Pulmonary embolism shock Cll clinical presentation
Cll clinical presentation Botulims
Botulims Waikato stormwater management guideline
Waikato stormwater management guideline Interview guideline template
Interview guideline template Anemia in pregnancy guideline
Anemia in pregnancy guideline Autoanamnesa
Autoanamnesa National guideline for patient safety incident
National guideline for patient safety incident Msqh guideline
Msqh guideline Guideline anamnesa
Guideline anamnesa East guideline
East guideline En feeding guide
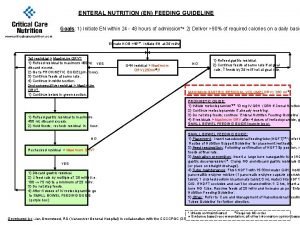
En feeding guide Effilating
Effilating What is a guideline for hoisting a hoseline?
What is a guideline for hoisting a hoseline? 8 points of turnbull
8 points of turnbull 5 guideline for cumbersome calculations
5 guideline for cumbersome calculations Multiplication rule for 4
Multiplication rule for 4 Who guideline on country pharmaceutical pricing policies
Who guideline on country pharmaceutical pricing policies Outside counsel guidelines
Outside counsel guidelines Canadian chiropractic guideline initiative
Canadian chiropractic guideline initiative Acg chronic pancreatitis
Acg chronic pancreatitis