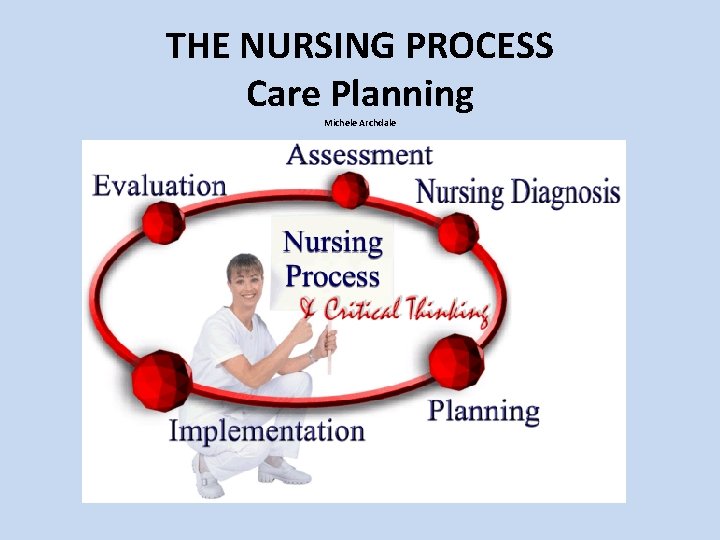
THE NURSING PROCESS Care Planning Michele Archdale Care

- Slides: 76
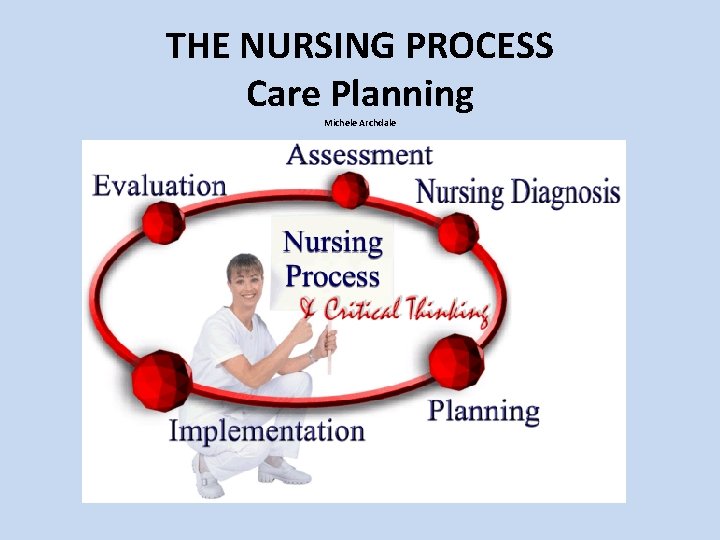
THE NURSING PROCESS Care Planning Michele Archdale
Care Planning The Who, What, Why, and How of Care Plans for Nurses July 2010 © Ausmed. Online PPPRES 30 v 1. 0 2
What is a Care Plan? A care plan is a document that outlines the nursing care that is planned for a patient. Care plans evolved as a way for nurses to monitor nursing care and to communicate between incoming and outgoing shifts (Arets and Morle, 1995). Care plans ensure that nursing care is planned, measured, documented, and evidence-based, and that outcomes are examined regularly (Greenwood, 1996). © Ausmed. Online PPPRES 30 v 1. 0 3 July 2010
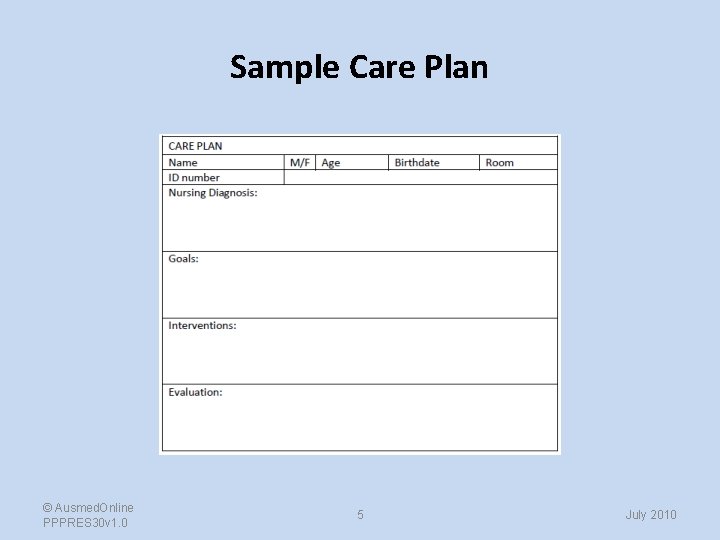
What Does a Care Plan Look Like? • Care plan formats vary from facility to facility. • Generally, a care plan has sections that correspond to each step of the nursing process (ADPIE). You will document your observations and choices in the spaces. • Usually, there is a care plan for each nursing diagnosis. © Ausmed. Online PPPRES 30 v 1. 0 4 July 2010
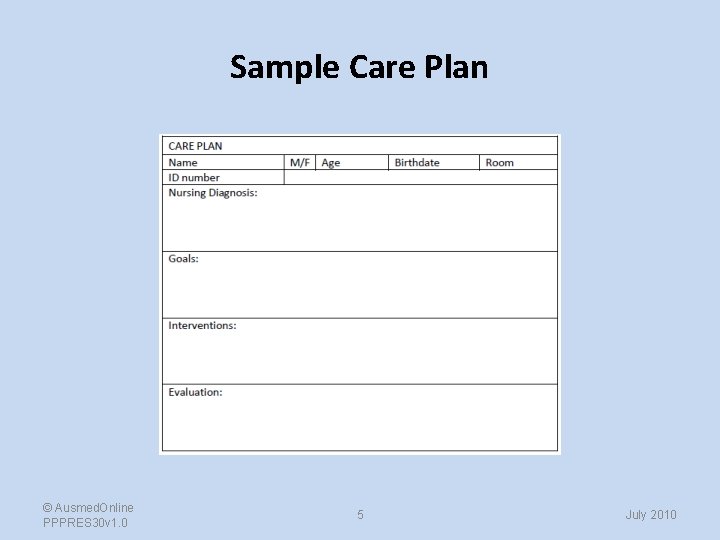
Sample Care Plan © Ausmed. Online PPPRES 30 v 1. 0 5 July 2010
Care Planning is Ongoing ‣ Care planning is an ongoing, dynamic process. It makes no sense to make a care plan, and then leave it to collect dust. As the patient’s situation changes, so should the care plan. ‣ Care plans are not static. They are modified, updated, corrected and extended according to the patient’s changing needs. © Ausmed. Online PPPRES 30 v 1. 0 6 July 2010
Example Your patient is 5 days post-op for total knee replacement. Her care plan, written 1 day post-op, states that she requires a one -person assist to ambulate. However, she has progressed to ambulating independently with a walker. Does it make any sense for the care plan to indicate that she requires a one-person assist? Of course not. This is why we reassess and update the care plan on a regular basis. © Ausmed. Online PPPRES 30 v 1. 0 7 July 2010
Where Do Care Plans Come From? • Nurses develop individualized care plans for each patient with a series of defined steps called the nursing process. • Therefore, to develop care plans, you have to know what the nursing process is. © Ausmed. Online PPPRES 30 v 1. 0 8 July 2010
The Nursing Process: Purpose “The purpose of the nursing process is to provide a systematic approach for processing patient care information for handling actual or potential patient care problems. ” (Huckabay, 2009) © Ausmed. Online PPPRES 30 v 1. 0 9 July 2010
The Nursing Process: Background The nursing process addresses the need for nursing care to be: § § © Ausmed. Online PPPRES 30 v 1. 0 Holistic Individualized Evidence-based Documented 10 July 2010
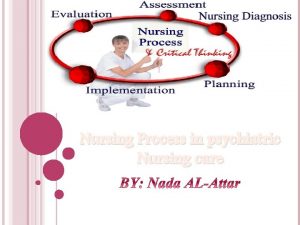
The Nursing Process: ADPIE • Historically, the nursing process had several formats. The gold standard is ADPIE (Assessment, Diagnosis, Planning, Implementation, Evaluation) (Pesut & Herman, 1999). © Ausmed. Online PPPRES 30 v 1. 0 11 July 2010
The Gold Standard Remember the 5 steps of the nursing process with this acronym: ADPIE © Ausmed. Online PPPRES 30 v 1. 0 12 July 2010
What Does ADPIE Stand For? • Assessment • Diagnosis • Planning • Implementation • Evaluation © Ausmed. Online PPPRES 30 v 1. 0 13 July 2010
Assessment • • History taking Collecting data Examination and observation Validating data Organizing data Identifying patterns/testing first impressions Reporting and recording data 14
• Subjective data – stated • Objective data – observed 15
Resources • • • Client Other individuals Previous records Consultations Diagnostics studies Relevant literature 16
The Nursing Process (ADPIE): Assessment • Assessment This is what you find when you examine and talk to the patient. It is an ongoing process. (Wright, 2005). For example: “The patient has dry, cracked lips, dry mucous membranes and low urine output. The patient’s skin turgor is slow to return and the patient states that he is thirsty. ” © Ausmed. Online PPPRES 30 v 1. 0 17 July 2010
The Nursing Process (ADPIE): Diagnosis • Diagnosis (defining problem) This is a description of what the nursing problem is. The language may be your own, or chosen from a list of over 200 standardized nursing diagnoses from the North American Nursing Diagnosis Association (NANDA) (Palese, et al. , 2009). © Ausmed. Online PPPRES 30 v 1. 0 18 July 2010
Nursing Diagnosis – Analysing and interpreting information obtained to identify actual or potential problems of the client the nurse can help to resolve or prevent through nursing intervention. – made after a client's information has been obtained and compared with normal functioning for that client. – The nurse makes assessments or inferences about the significance of the information and identifies the client's problems. • • (Funnell, Rita. Tabbner's Nursing Care, 5 th Edition. Elsevier Australia, 12/1/2008. p. 230). <vbk: 978 -0 -7295 -3857 -2#outline(19. 5. 2)> 19
The Nursing Process (ADPIE): Diagnosis • Your assessment findings are often included in the nursing diagnosis, using the phrase “as evidenced by”. • The nursing diagnosis is what you determine to be an actual or potential reaction to the patient’s state of being. The diagnosis also helps guide you towards appropriate interventions. © Ausmed. Online PPPRES 30 v 1. 0 20 July 2010
The Nursing Process (ADPIE): Diagnosis • The nursing diagnosis is not a medical diagnosis, such as diagnosis of a disease or health condition. Rather, it is a description of the patient’s response to their current situation. • That is, “multiple sclerosis” is a medical diagnosis, not a nursing diagnosis. “At risk for powerlessness due to disease process” is a nursing diagnosis (NANDA, 2010). © Ausmed. Online PPPRES 30 v 1. 0 21 July 2010
The Nursing Process (ADPIE): Diagnosis For the patient we assessed earlier, the NANDA nursing diagnosis would be: Deficient fluid volume You would individualize by adding “as evidenced by dry mucous membranes, low urine output, slow-to-return skin turgor and expressed feelings of thirst”. This is our nursing diagnosis! (Gulanick et al. , 2006) © Ausmed. Online PPPRES 30 v 1. 0 22 July 2010
Planning • Setting priorities • Establishing clear goals and outcomes for the patient to achieve. – Choosing nursing interventions to meet those outcomes. • • Determining interventions Care planning Time and resource management Documentation. 23
Priorities • Enables the nurse and patient to make the best use of time, energy, and health care dollars. • Designs the plan with the patient and significant others not for them. 24
General Guidelines for Setting Priorities • • Take care of immediate lifethreatening issues. Safety issues. Patient-identified issues. Nurse-identified priorities based on the overall picture, the patient as a whole person, and availability of time and resources. 25
Implementation • Putting the nursing plan into action (nursing interventions) • the actual performance of the activities that have been selected to help the client achieve the set goals. • The client's needs are reassessed continuously during the implementation stage • Any new needs can be identified and the nursing care plan can be modified or adapted. 26
The Nursing Process (ADPIE): Planning and Implementation Planning Describes what you expect will occur for the patient. It can be helpful to think of this step as Goals or Outcomes. Implementation Describes what you plan to do to meet the patient’s needs, guided in part by your NANDA diagnosis (Hughes, et al. , 2008). Sometimes termed Interventions. © Ausmed. Online PPPRES 30 v 1. 0 27 July 2010
The Nursing Process (ADPIE): Planning and Implementation • Use the acronym SMART to guide your Planning and Implementation: §Specific §Measureable §Achievable §Realistic §Time-specific (Wright, 2005) © Ausmed. Online PPPRES 30 v 1. 0 28 July 2010
The Nursing Process (ADPIE): Planning Nursing Outcome Classifications (NOC) is standardized language available to describe Planning, similar to NANDA for Diagnosis. For our patient example, appropriate NOC terminology for Planning (desired outcome) is: Fluid balance (Kautz et al. , 2006) © Ausmed. Online PPPRES 30 v 1. 0 29 July 2010
The Nursing Process (ADPIE): Implementation Nursing Interventions Classification (NIC) is standardized language available to describe Implementation, again similar to NANDA for diagnosis. For our patient example, appropriate NIC terminology for Implementation is: Measure intake and output (Kautz et al. , 2006) © Ausmed. Online PPPRES 30 v 1. 0 30 July 2010
The Nursing Process (ADPIE): Implementation Practice • For our patient with a nursing diagnosis of deficient fluid volume, our plan is to achieve fluid balance, and so far, our implementation is to measure input and output. • What other interventions might be appropriate? © Ausmed. Online PPPRES 30 v 1. 0 31 July 2010
The Nursing Process (ADPIE): Implementation Practice • Additional interventions: § § Daily weights Vital signs Encourage oral fluid intake Administer IV fluids as ordered © Ausmed. Online PPPRES 30 v 1. 0 32 July 2010
The Nursing Process (ADPIE): Planning and Implementation • Planning and Implementation must be evidencebased. • You communicate the evidence base for your choices by giving a rationale. In nursing school, you need to provide the rationale and references to show your instructors that you are utilizing the nursing process. Most workplaces do not require a stated rationale or references on care plans. © Ausmed. Online PPPRES 30 v 1. 0 33 July 2010
The Nursing Process (ADPIE): Planning and Implementation A rationale for measuring urinary output for the patient in our example is: Reduced urinary output can indicate dehydration. Normal urinary output is considered to be >30 m. L per hour for an adult (Berman, et al. , 2008). © Ausmed. Online PPPRES 30 v 1. 0 34 July 2010
Implementation - Setting Priorities 1. 2. 3. 4. 5. Make initial rounds. Verify critical information Identify urgent problems List problems Determine interventions that would best address the problems 6. What can the patient do themselves? 7. Worksheet 35
Evaluation • • • Determining outcome achievement Identifying the variables affecting outcome achievement Deciding whether to continue, modify, or terminate the plan 36
• Thinking and collecting information about the patient’s responses after some nursing care is provided. • Working with the patient to determine whether the patient’s outcomes have been met and how well they have been met. 37
The Nursing Process (ADPIE): Evaluation • Evaluation This is when you review your patient’s progress to see if your interventions were effective. • Your evaluation may indicate you need to change your approach to achieve your planned goals (outcomes). (Wright, 2005) © Ausmed. Online PPPRES 30 v 1. 0 38 July 2010
The Nursing Process (ADPIE): Evaluation • Perform evaluations as often as necessary to keep track of your patient’s progress and changing needs. Usually, this translates to once a shift (or more often) in an acute, in-patient setting, and monthly or quarterly in a nursing home. © Ausmed. Online PPPRES 30 v 1. 0 39 July 2010
Documentation • You use the nursing process to generate care plans. Care plans must be documented. • Care plans are legal documents and should be treated accordingly. • When you make additions or changes to a care plan, initial all entries to ensure you are recognized for your contribution, and you leave a record of your actions. © Ausmed. Online PPPRES 30 v 1. 0 40 July 2010
Documentation Do’s • DO: Sign (or initial) and date all changes or entries to the care plan so that it is clear who made the revisions or changes. • DO: Review your care plan on a regular basis. The frequency of your review really depends on the setting, the situation and your employer’s policies. © Ausmed. Online PPPRES 30 v 1. 0 41 July 2010
Documentation Don’t’s • DON’T use white out on a paper care plan. Cross out an error with one line (so your error remains legible), write the word ‘error’ and add your initials. For electronic records, follow your facility’s policy. • DON’T attempt to delete or remove unsuccessful interventions from a care plan. You will adapt your care according to your evaluations, and this should be reflected in your documentation. © Ausmed. Online PPPRES 30 v 1. 0 42 July 2010
Documentation ‣ You may want to document all of your findings, normal or otherwise, regardless of the facility’s policy. Your employer’s policy is important, but no one should fault you for doing more than the minimum requirement. ‣ Ensure that you cover yourself legally with your documentation. Ask yourself if you could accurately describe a situation years later in court, based only on your charted notes. © Ausmed. Online PPPRES 30 v 1. 0 43 July 2010
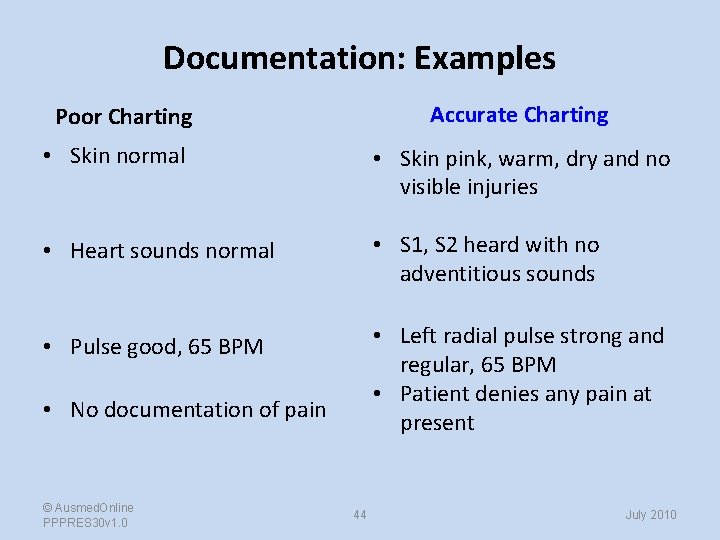
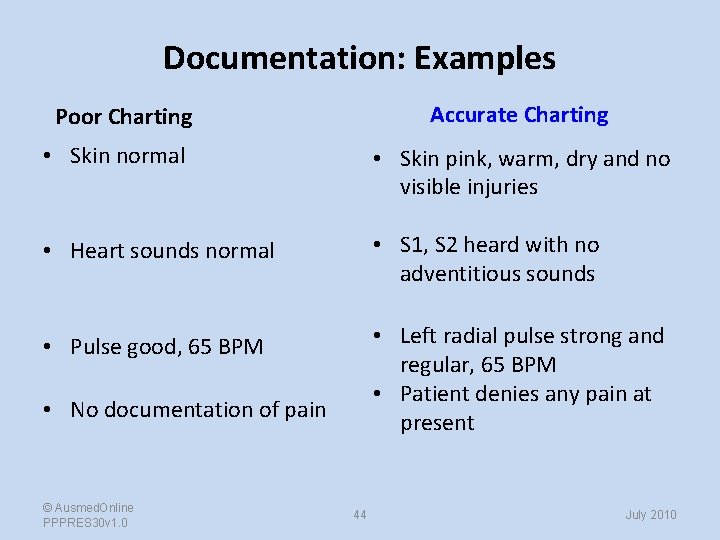
Documentation: Examples Accurate Charting Poor Charting • Skin normal • Skin pink, warm, dry and no visible injuries • Heart sounds normal • S 1, S 2 heard with no adventitious sounds • Pulse good, 65 BPM • Left radial pulse strong and regular, 65 BPM • Patient denies any pain at present • No documentation of pain © Ausmed. Online PPPRES 30 v 1. 0 44 July 2010
What Are Care Plans REALLY For? Care plans: ‣ Define how we look at patients and approach their care. ‣ Force us to really think about what we are doing with patients, and why we are doing it. ‣ Provide a structure for constant reassessment of the plan for patient care (Wright, 2005). ‣ Are a valuable communication tool among nurses and other health professionals (Greenwood, 1996). ‣ Help maintain consistency of care. © Ausmed. Online PPPRES 30 v 1. 0 45 July 2010
Modern Care Planning ‣ Some facilities have electronic care planning resources. ‣ Some believe that the electronic care plan will revolutionize care planning, and enhance the care planning process. ‣ Some feel that nursing care plans are unnecessary. (Greenwood, 1996; Kennedy, et al. , 2009; Lieber, 2010) © Ausmed. Online PPPRES 30 v 1. 0 46 July 2010
Modern Care Planning ‣ Most experts, including nursing licensing bodies and regulators, believe that care plans are essential (Greenwood, 1996). ‣ Imagine working in an unfamiliar area, or starting an orientation period on a new floor. An existing care plan allows you to plan your care. It also helps other, experienced nurses know how to help you. © Ausmed. Online PPPRES 30 v 1. 0 47 July 2010
Remember to be SMART Remember, your Planning and Implementation should be: §Specific §Measureable §Achievable §Realistic §Time-specific © Ausmed. Online PPPRES 30 v 1. 0 (Wright, 2005) 48 July 2010
Day-to-Day Use of Care Plans ‣ Not every workplace enforces the use of care plans. You can still use them, regardless of policy. ‣ Care plans will improve the quality of your patient care, even if you have to manually add brief care plans to your progress notes. © Ausmed. Online PPPRES 30 v 1. 0 49 July 2010
Day-to-Day Use of Care Plans ‣ NANDA, NOC and NIC provide a universal language for care plans, which improves consistency and understanding among caregivers. ‣ You may find the same interventions are recommended in different care plans for the same patient. Try to not repeat yourself when preparing care plans. (Adams-Wending, et al. , 2008) © Ausmed. Online PPPRES 30 v 1. 0 50 July 2010
Care Plan Resources ü Books: Crofton, Christine, & Witney, Gaye, ‘Nursing Documentation in Aged Care’, Ausmed Publications, 2004. ü Richmond, Jennifer, . ‘Nursing Documentation – writing what we do’, Ausmed Publications 1997. ü Free access to information about NOC and NIC: http: //www. nursing. uiowa. edu/excellence/nursing_knowledge/clinical_effectiveness/noc. htm ü NANDA web site: http: //www. nanda. org/ ü Contains the NANDA diagnoses and classifications for 2009 -2011: http: //www. amazon. ca/gp/product/1405187182/ref=pd_lpo_k 2_dp_sr_3? pf_rd_p=485327511&pf_rd_s=l po-topstripe&pf_rd_t=201&pf_rd_i=0323039545&pf_rd_m=A 3 DWYIK 6 Y 9 EEQB&pf_rd_r=1 H 2 K 1 EM 4 DGHSEYBFC 6 DE © Ausmed. Online PPPRES 30 v 1. 0 51 July 2010
Care Plan Resources ü Free download of a searchable NANDA diagnosis program for PDAs: http: //www. pdacortex. com/Nursing_Diagnosis_Download. htm ü Care planning reference book: http: //www. amazon. com/exec/obidos/ASIN/0323016278/medismartcom ü Free online care plan generator – uses NANDA, NOC, and NIC: http: //www 1. us. elsevierhealth. com/MERLIN/Gulanick/Constructor/ ü Free online care plan generator – uses NANDA, NOC, and NIC: http: //www 1. us. elsevierhealth. com/Evolve/Ackley/NDH 6 e/Constructor/H-O. html © Ausmed. Online PPPRES 30 v 1. 0 52 July 2010
Care Plan Resources ü Care planning reference book: http: //www. amazon. ca/Nursing-Care-Plans. Diagnosis-Intervention/dp/0323039545 ü An interactive CD-ROM from Mosby to assist you in producing over 90 different care plans: http: //www. amazon. com/exec/obidos/ASIN/0323024025/medismartcom ü A paid membership site: http: //www. careplans. com/ © Ausmed. Online PPPRES 30 v 1. 0 53 July 2010
Care Plan Resources ü Free sample care plans: http: //www. medi-smart. com/carepl 10. htm ü Subscription site for nursing home [residential] care planning: http: //www. cncplan. com/ ü Care planning specifically for MS patients: http: //www. cnsonline. org/www/archive/ms/ms-07. html ü Free tips and comments on nursing care plans: http: //www. virtualnurse. com/blog/category/nursing-care-plans/ © Ausmed. Online PPPRES 30 v 1. 0 54 July 2010
Care Plan Resources ü Application for i. Pod Touch or i. Phone to help formulate care plans: http: //itunes. apple. com/ca/app/handbook-nursing-diagnosis/id 311016899? mt=8 ü Nursing diagnosis handbook: http: //www. amazon. ca/gp/product/0323048269/ref=pd_lpo_k 2_dp_sr_1? pf_rd_ p=485327511&pf_rd_s=lpo-topstripe&pf_rd_t=201&pf_rd_i=0323039545&pf_rd_m=A 3 DWYIK 6 Y 9 EEQB&pf_rd_r= 1 H 2 K 1 EM 4 DGHSEYBFC 6 DE © Ausmed. Online PPPRES 30 v 1. 0 55 July 2010
References • Adams-Wendling, L. , Paimjariyakul, U. , Bott, M. , & Taunton, R. L. (2008). Strategies for translating the resident care plan into daily practice. Journal of Gerontological Nursing, 34 (8), 50 -56. • Arets, J. & Morle, K. (1995). The nursing process: an introduction. In: Basford, L. , Slevin, O. , Arets, J. , et al. eds. Theory and Practice of Nursing. Edinburgh, Scotland: Campion Press. pp. 304 -317. • Berman, A. , Kozier, B. , Erb, G. , & Snyder, S. J. (2008). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice (8 th ed. ). Upper Saddle River, New Jersey, U. S. A. : Pearson Education, Inc. Accessed at www. statref. com on 17 June 2010. • Castledine, G. (2010). Critical thinking is crucial. British Journal of Nursing, 19 (4), 271. • Doenges, M. E. , Moorhouse, M. F. , & Geissler-Murr, A. C. (2004). Nurse’s pocket guide: Diagnoses, interventions and rationales (9 th ed. ). Philadelphia, Pennsylvania, U. S. A. : F. A. Davis Company. © Ausmed. Online PPPRES 30 v 1. 0 56 July 2010
References • Greenwood, D. (1997). Nursing care plans: Issues and solutions. Nursing Management, 27 (3), 33 -40. • Gulanick, M. , Myers, J. L. , & Galanes, S. (2006). Nursing care plans: Nursing diagnosis and interventions, 6 th ed. Toronto, Ontario, Canada: Mosby. • Henderson, V. (1982). The nursing process: is the title right? Journal of Advanced Nursing, 7 (2), 103 -109. • Huckabay, L. M. (2009). Clinical reasoned judgment and the nursing process. Nursing Forum, 44 (2), 72 -78. • Hughes, R. , Lloyd, D. , & Clark, J. (2008). A conceptual model for nursing information. International Journal of Nursing Terminologies and Classifications, 19 (2), 48 -56. • Kautz, D. D. , Kuiper, R. , Pesut, D. J. , & Williams, R. L. (2006). Using NANDA, NIC, and NOC (NNN) language for clinical reasoning with the outcome-present state-test (OPT) model. International Journal of Nursing Terminologies and Classifications, 17 (30), 129 -138. © Ausmed. Online PPPRES 30 v 1. 0 57 July 2010
References • Kennedy, D. , Pallikkathayil, L. , & Warren, J. J. (2009). Using a modified electronic health record to develop nursing process skills. Journal of Nursing Education, 48 (20), 96 -100. • Lieber, H. S. (2010). Balancing act: Technology must be part of an overall patient-care plan. Modern Healthcare, 40 (9), 18. • North American Nursing Diagnosis Association (2010). Nursing diagnosis frequently-asked questions. Retrieved from http: //www. nanda. org/Nursing. Diagnosis. FAQ. aspx. • Palese, A. , De Silvestre, D. , Valoppi, G. , & Tomietto, M. (2009). A 10 -year retrospective study of teaching nursing diagnosis to baccalaureate students in Italy. International Journal of Nursing Terminologies and Classifications, 20 (2), 64 -75. • Pesut, D. J. , & Herman, J. (1999). Clinical reasoning: The art and science of critical and creative thinking. New York, U. S. A. : Delmar Cengage Learning. • Wright, K. (2005). Care planning: An easy guide for nurses. Nursing and residential care, 7 (2), 71 -73. © Ausmed. Online PPPRES 30 v 1. 0 58 July 2010
PRINCIPLES OF DOCUMENTATION

Professional Documentation • “All forms of documentation by a nurse recorded in a professional capacity in relation to the provision of care. • • • Written Electronic Health Records Audio Video Emails Faxes Photographic images Observation Charts Check lists Communication books Incident Reports Clinical nursing notes
Nursing Records or Reports • • • Patient assessment tools and charts Diagnosis – past and present Nursing notes Test results Written instructions Drug orders Client referrals Clinical pathways – health risk factors Care plans – patient’s progress Computerised reporting
Documentation promotes Compliance with ANMC competency standards High standard of care Evidence of nursing care Continuity of care Improved communication and delivery of information Accurate account of assessment, care planning, treatment and care evaluation • Ability to look back and assess achievements / goals • Early detection of variances • • •
WHY DOCUMENT? • As a tool – evidence based practice • Communication method – reliable & permanent • Demonstrates responsibility & accountability – evidence of care received • Legal requirement – Legislation • Quality improvement tool • Health research • Track resources, efficiencies in management
Principles for Documentation should be a record of first hand • • • Knowledge Observation Actions Decisions Outcomes
Who should document? • • • Registered Nurses (RN) Enrolled Nurses (EN) Clients Health Professionals Other care providers
What to document? • All aspects of nursing care • Collaboration and interventions from other health professional / care providers • Subjective and Objective information • Observation, assessment, actions, outcomes • Variances in outcome or usual protocol • Rationale for decisions and actions • Critical incidents that involve the client
When to document? As a time line recording actions and events In a timely manner The action or event Nursing or allied health professional interventions • Variances to expected outcomes • Emergency situations • Retrospectively as a late entry • •
How do you document? • • • Comprehensive & flexible In a concise manner, accurate and true Clearly and legible – Can anyone read your writing? Permanent– Never in pencil always in pen. At certain times colours are required as per hospital policy. Identifiable – sign and write your name Current – date and time Confidentiality and Privacy issues Evidence based – not speculation Avoid abbreviations Understand use appropriate terminology
Effective communication • Health care workers may only be present for short periods of time – continuity issues • A multidisciplinary team, that may never actually meet • Health care records must act as a communication tool
DOCUMENTATION MUST!! • • Be accurate Current Relevant Factual Organised Concise Complete
Consequences of Poor Documentation • • • Fragmented care Repetition of care Delayed interventions Omitted interventions Delayed recovery
Legal responsibilities • Every activity of the nurse in the performance of her nursing services is subject of potential analysis by the law. • The laws are made to protect the health and welfare of the public. • Ignorance of the law is no excuse. When a law exists and the nurse violates it, the nurse is subject to criminal charges. • Always document appropriately – If it’s not written down it did not happen! - you could need to refer to your notes at any time in the future when you can not recall what happened.
Preparing for Report • Show up on the unit in time to prepare for report / handover. • Review charts briefly before report. • Be ready to listen. • Use worksheet to organize reported data. 74
Getting Report / handover • • Worksheet 1. Organizes data 2. Cues to information 3. Worksheet for the day Do not become totally dependent on worksheets 75
Giving Report • • • Use your worksheet Give basic info first Be specific Evidence based statements only Be descriptive Stress the abnormal 76
 Nursing care plan for obsessive compulsive disorder
Nursing care plan for obsessive compulsive disorder Cataracts nursing interventions
Cataracts nursing interventions 3 part nursing diagnosis examples
3 part nursing diagnosis examples Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Planning phase in nursing process
Planning phase in nursing process Nursing process steps
Nursing process steps Levels of care primary secondary tertiary
Levels of care primary secondary tertiary Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Thang điểm glasgow
Thang điểm glasgow Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng từ đua
Môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Số nguyên tố là
Số nguyên tố là Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Michele weiss
Michele weiss Michele amorena
Michele amorena Saldatura
Saldatura Michele vas
Michele vas Michele cirelli
Michele cirelli Michele doro
Michele doro Michele banko
Michele banko Michèle torr pas bien dans sa vie
Michèle torr pas bien dans sa vie Michele della ventura
Michele della ventura Scarponi michele
Scarponi michele Michele curioni
Michele curioni Michele battisti
Michele battisti Fisiopatologia respiratoria brescia
Fisiopatologia respiratoria brescia Cpucs
Cpucs Michele de pasquale
Michele de pasquale Michele kahane
Michele kahane Michele gubian
Michele gubian Michele jacobsen
Michele jacobsen Michele chaban
Michele chaban Michele hugin
Michele hugin Michele pestalozzi
Michele pestalozzi Michele innocenti
Michele innocenti Michele marie montgomery
Michele marie montgomery Kelly roper simile poem
Kelly roper simile poem Michele rubinelli monaco
Michele rubinelli monaco Isabella savella
Isabella savella Michele vitacca model
Michele vitacca model Cornell dining nutrition
Cornell dining nutrition