The Great Pretender Rona Marie Leonor M D































- Slides: 100
The Great Pretender Rona Marie Leonor, M. D. November 12, 2009 9/F Ledesma Hall
OBJECTIVES � To present a case of a patient with persistent fever. � To discuss the approach and management in patient with persistence of fever.

GENERAL DATA � R. B, 58 -year-old male, � married, Filipino � Farmer 5, 2009 from Tuguegarao, admitted on July

CHIEF COMPLAINT
HISTORY OF PRESENT ILLNESS � 3 WEEKS PTA › fever, undocumented › right upper quadrant pain › No change in bowel movement

HISTORY OF PRESENT ILLNESS › local Institution in Tuguegarao. › A> enteric fever › Cotrimoxazole and Metronidazole. › A> Malaria › Chloroquine started as an empiric treatment. › opted to go home , and was lost to follow up

HISTORY OF PRESENT ILLNESS � 2 WEEKS PTA › Fever and Right upper quadrant pain › Dyspnea › No cough, chest pain
HISTORY OF PRESENT ILLNESS � local institution Tuguegarao. � Abdominal Ultrasound: Cholesterolosis � Chest xray and Chest Ultrasound : pleural effusion on the right. � Thoracentesis 1 liter

HISTORY OF PRESENT ILLNESS � Empirically treated with Ceftriaxone, Ciprofloxacin and eventually Anti koch’s medication � Opted to go home � Pleural fluid Culture and histopath results unknown to patient � consult in MMC for further management
REVIEW OF SYSTEMS � generalized weakness � weight loss � Loss of appetite � no headache � no palpitations � No signs of bleeding � no dysuria/ frequency/ hematuria � no joint stiffness/ weakness
PAST MEDICAL HISTORY � No Diabetes Mellitus � No hypertension � No Asthma � No Pulmonary Tuberculosis � No history of accidents or injuries � No history of blood transfusion � No history of hepatitis � No previous surgeries

PERSONAL & SOCIAL HISTORY � Non smoker � Non alcoholic beverage drinker � No illicit drug use � Denies exposure to a PTB patient
FAMILY HISTORY � No Hypertension � No Cancer � No Diabetes Mellitus � No asthma � No PTB
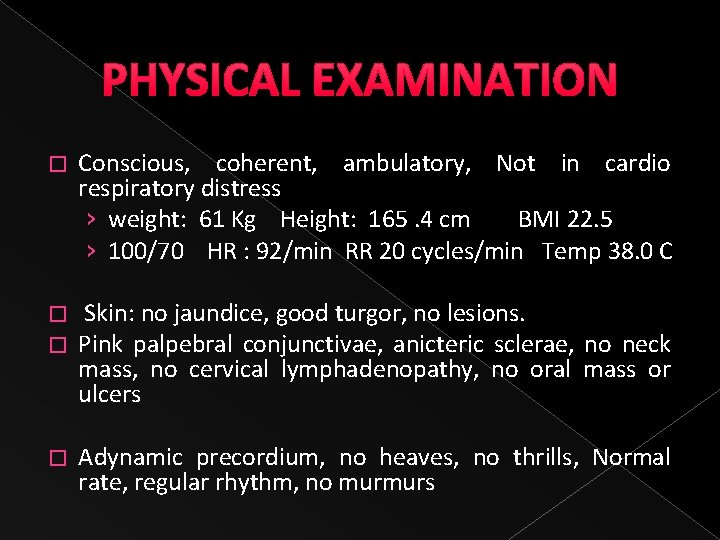
PHYSICAL EXAMINATION � Conscious, coherent, ambulatory, Not in cardio respiratory distress › weight: 61 Kg Height: 165. 4 cm BMI 22. 5 › 100/70 HR : 92/min RR 20 cycles/min Temp 38. 0 C � � Skin: no jaundice, good turgor, no lesions. Pink palpebral conjunctivae, anicteric sclerae, no neck mass, no cervical lymphadenopathy, no oral mass or ulcers � Adynamic precordium, no heaves, no thrills, Normal rate, regular rhythm, no murmurs
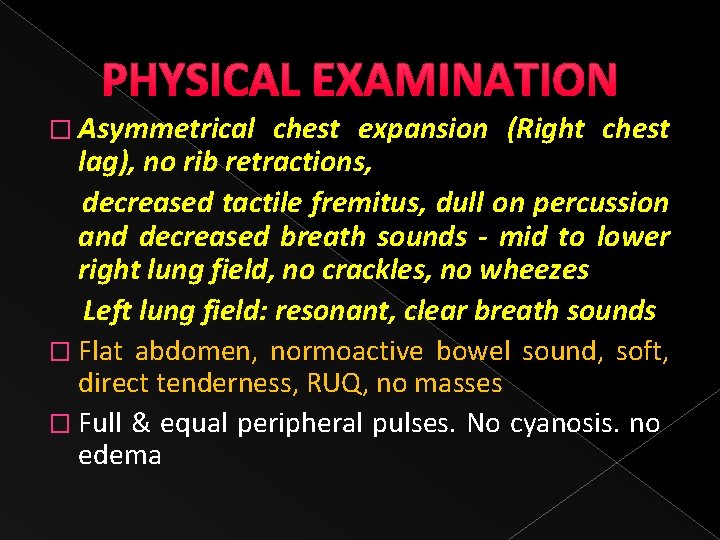
PHYSICAL EXAMINATION � Asymmetrical chest expansion (Right chest lag), no rib retractions, decreased tactile fremitus, dull on percussion and decreased breath sounds - mid to lower right lung field, no crackles, no wheezes Left lung field: resonant, clear breath sounds � Flat abdomen, normoactive bowel sound, soft, direct tenderness, RUQ, no masses � Full & equal peripheral pulses. No cyanosis. no edema
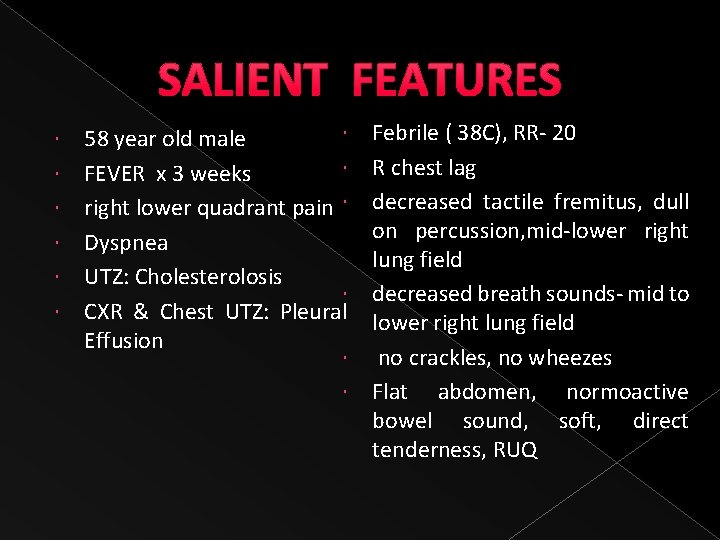
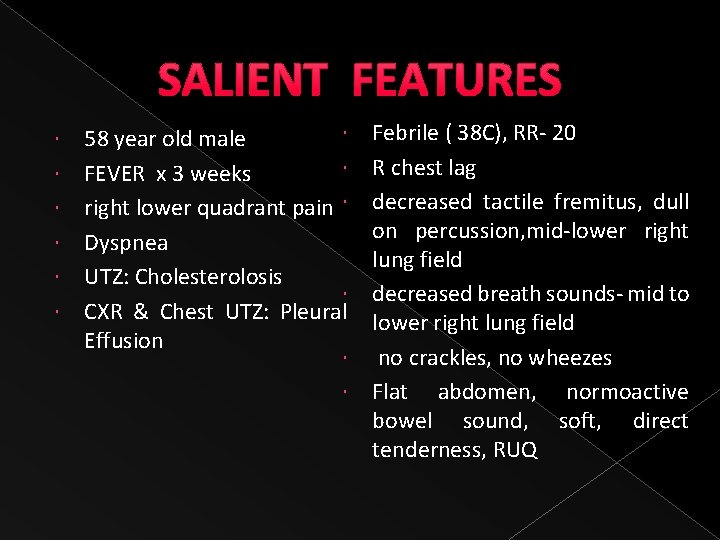
SALIENT FEATURES Febrile ( 38 C), RR- 20 R chest lag decreased tactile fremitus, dull on percussion, mid-lower right lung field decreased breath sounds- mid to lower right lung field no crackles, no wheezes Flat abdomen, normoactive bowel sound, soft, direct tenderness, RUQ 58 year old male FEVER x 3 weeks right lower quadrant pain Dyspnea UTZ: Cholesterolosis CXR & Chest UTZ: Pleural Effusion

ADMITTING IMPRESSION � Fever secondary to Pulmonary Tuberculosis vs. Pneumonia r/o malignancy � Pleural effusion, right � Cholesterolosis
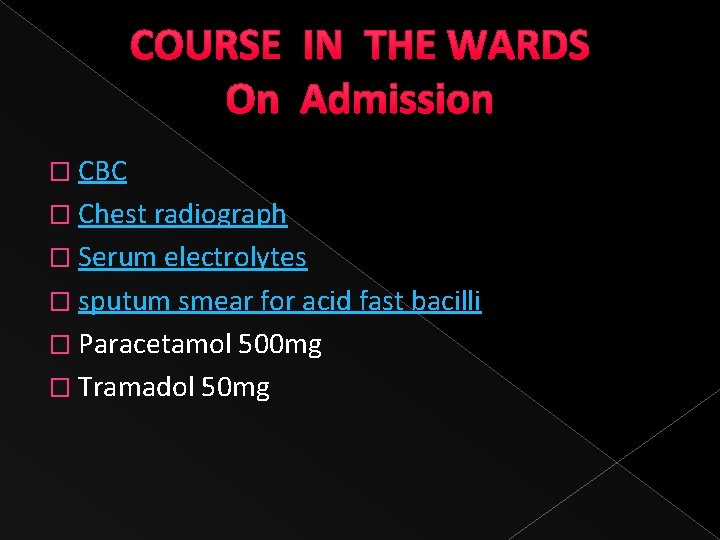
COURSE IN THE WARDS On Admission � CBC � Chest radiograph � Serum electrolytes � sputum smear for acid fast bacilli � Paracetamol 500 mg � Tramadol 50 mg
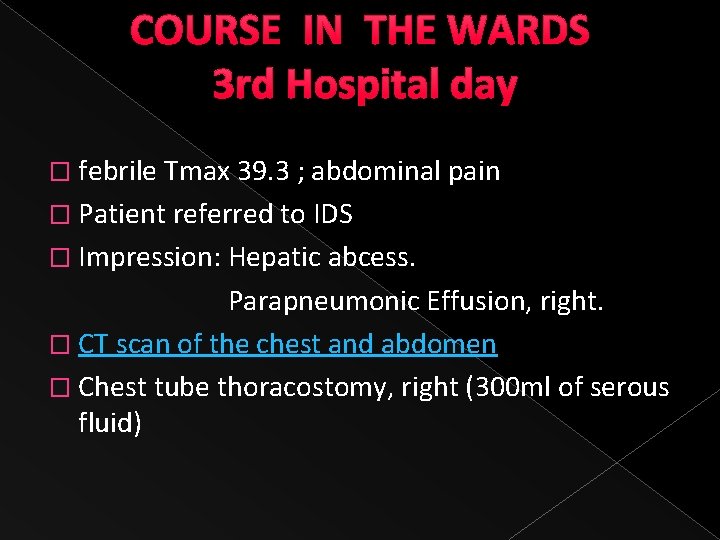
COURSE IN THE WARDS 3 rd Hospital day � febrile Tmax 39. 3 ; abdominal pain � Patient referred to IDS � Impression: Hepatic abcess. Parapneumonic Effusion, right. � CT scan of the chest and abdomen � Chest tube thoracostomy, right (300 ml of serous fluid)
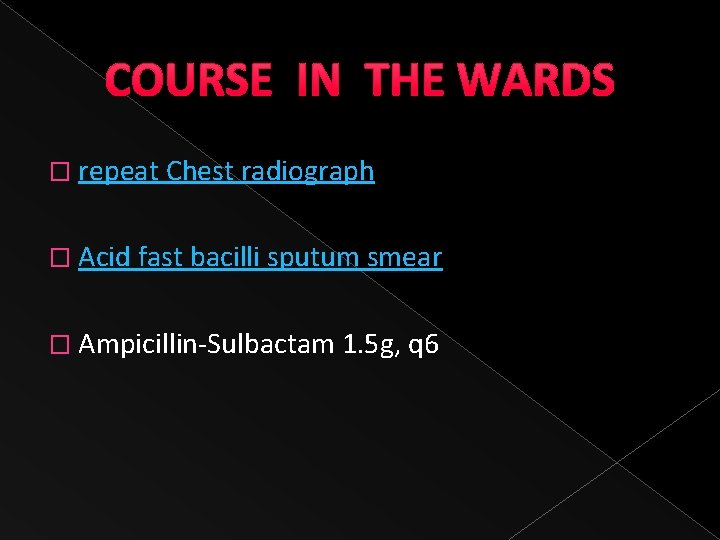
COURSE IN THE WARDS � repeat Chest radiograph � Acid fast bacilli sputum smear � Ampicillin-Sulbactam 1. 5 g, q 6
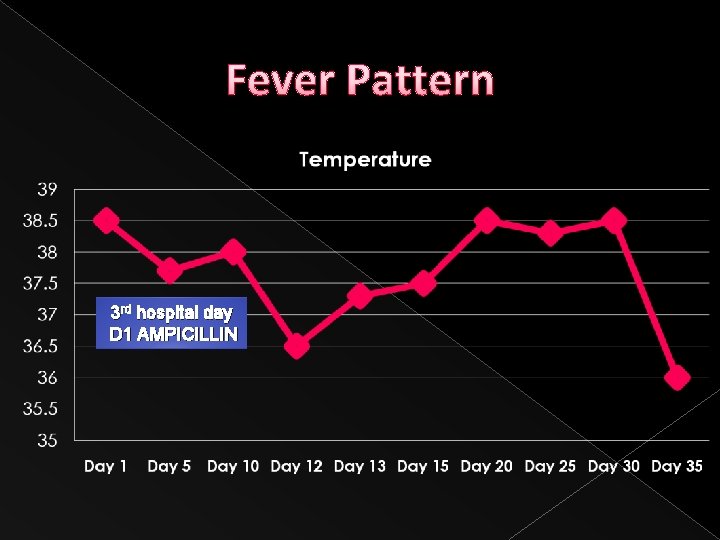
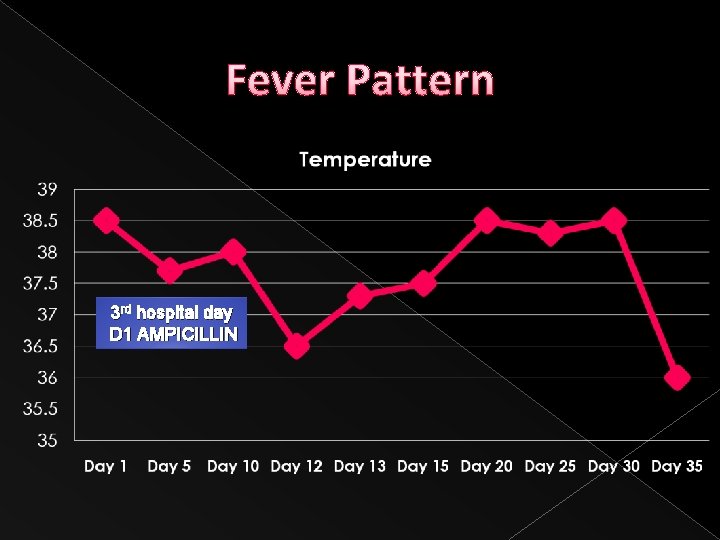
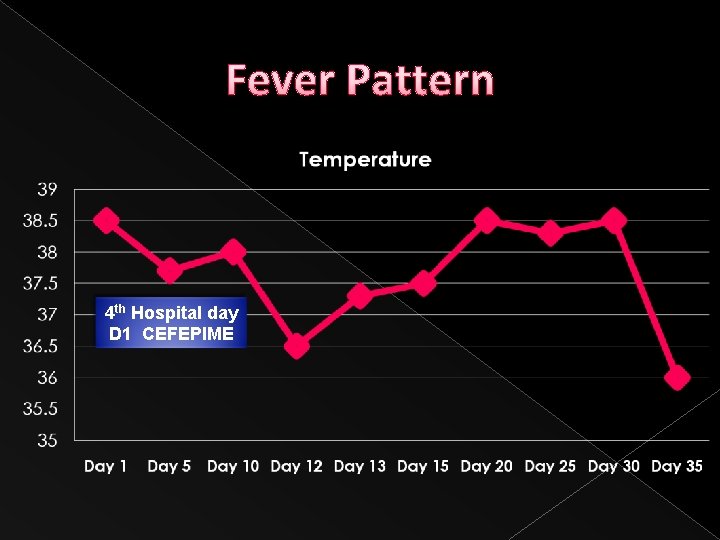
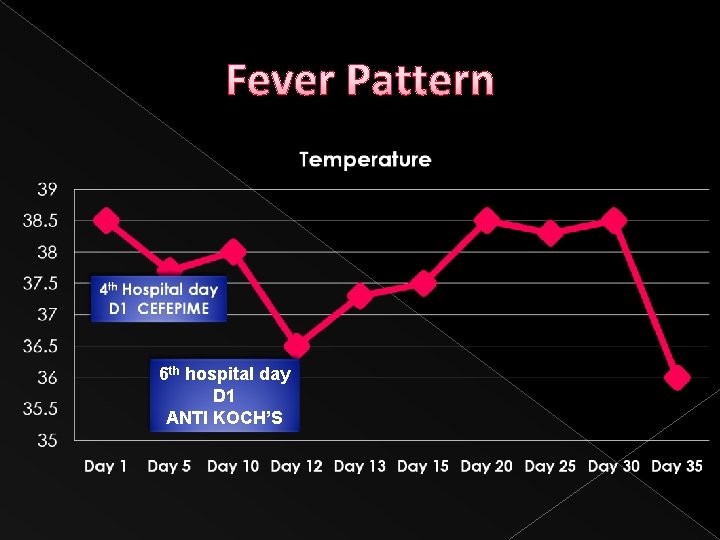
Fever Pattern 3 rd hospital day D 1 AMPICILLIN
COURSE IN THE WARDS Pleural fluid gram staining • Ampicillin-Sulbactam was shifted to Cefepime 1 g, every 12 hrs. •
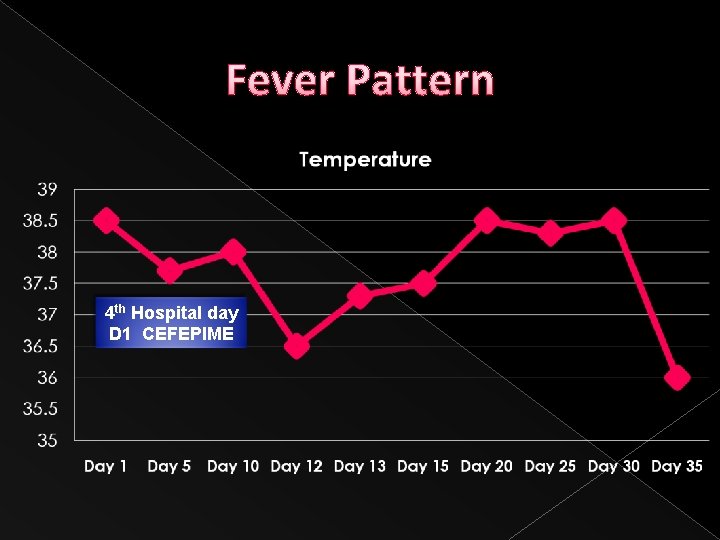
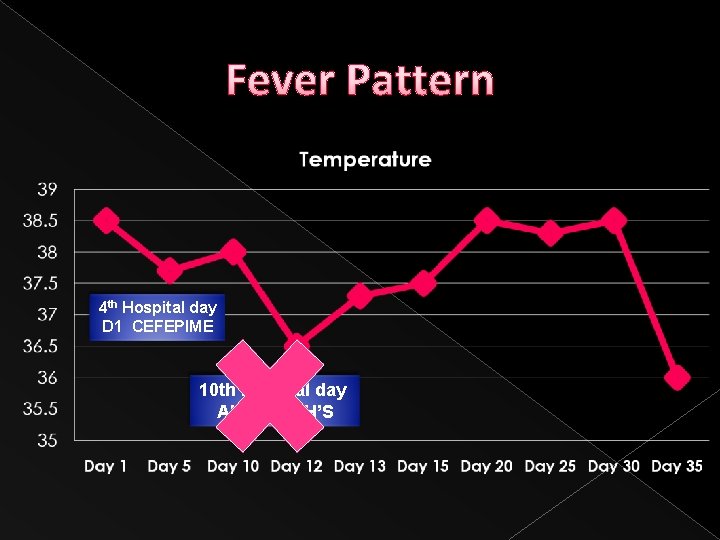
Fever Pattern 4 th Hospital day D 1 CEFEPIME
COURSE IN THE WARDS 6 th Hospital day � Febrile Tmax 39. 1 � CBC � Blood culture � Acid fast bacilli smear of pleural fluid � Acid fast bacilli culture � HRZE (Myrin P forte) 4 tablets, once a day.
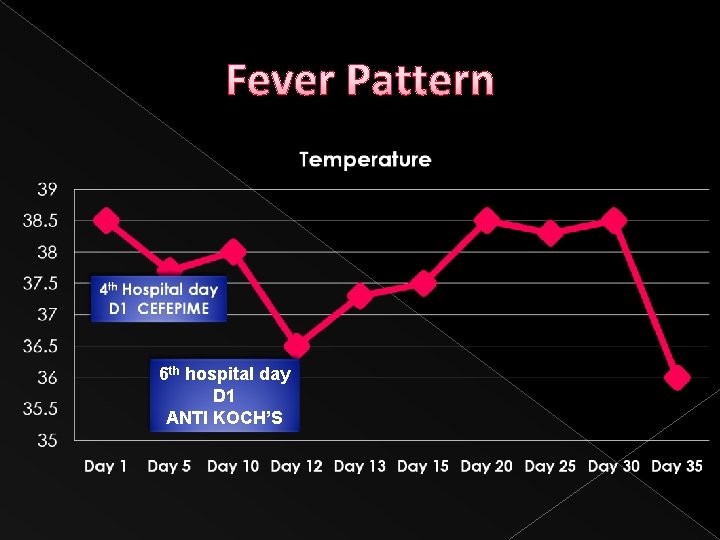
Fever Pattern 6 th hospital day D 1 ANTI KOCH’S
COURSE IN THE WARDS 8 th hospital day › › › febrile Tmax 39 C loss of appetite Dizziness loose bowel movement Pleural fluid cytology Myrin P Forte discontinued
COURSE IN THE WARDS � INH 300 mg, 1 tab, before breakfast � Rifampicin 600 mg, 1 tab, before breakfast; � Ethambutol 400 mg, 3 tabs, after breakfast � PZA 500 mg, 4 tablets, after lunch
COURSE IN THE WARDS 10 th hospital day � Febrile Tmax 38. 9 � Headache, vomiting, dizziness and tinnitus � Impresssion: Drug induced vs central cause R/O Connective tissue disease

COURSE IN THE WARDS • Lupus Panel • Plan: Cranial CT scan & Lumbar Tap • Anti Koch’s, Tramadol were discontinued • Betahistine was started
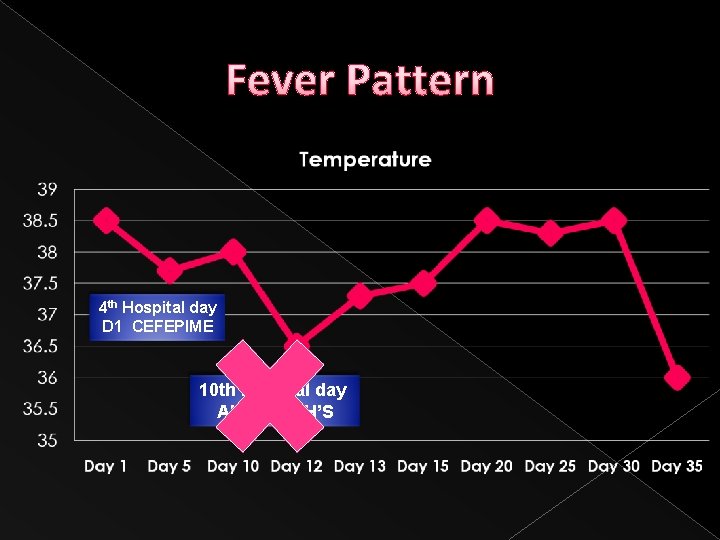
Fever Pattern 4 th Hospital day D 1 CEFEPIME 10 th hospital day ANTI KOCH’S
COURSE IN THE WARDS 12 th hospital day � Fever secondary to Infection vs. Malignancy � Naproxen 375 mg, BID and later decreased to 275 mg, BID � Cefepime discontinued
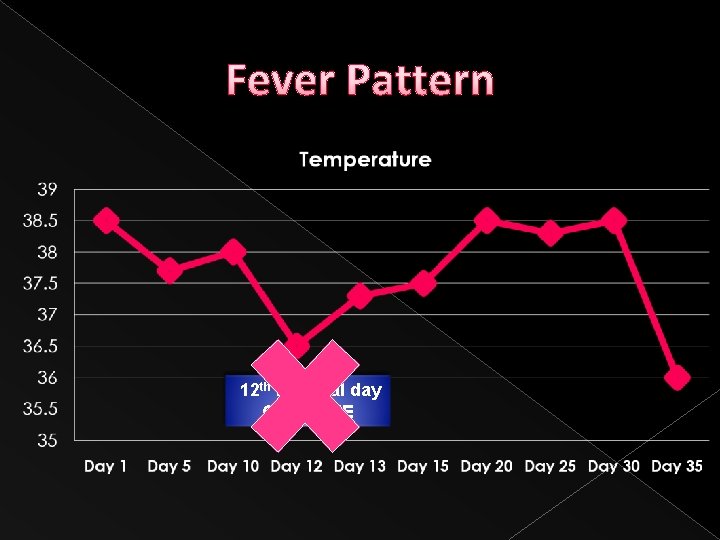
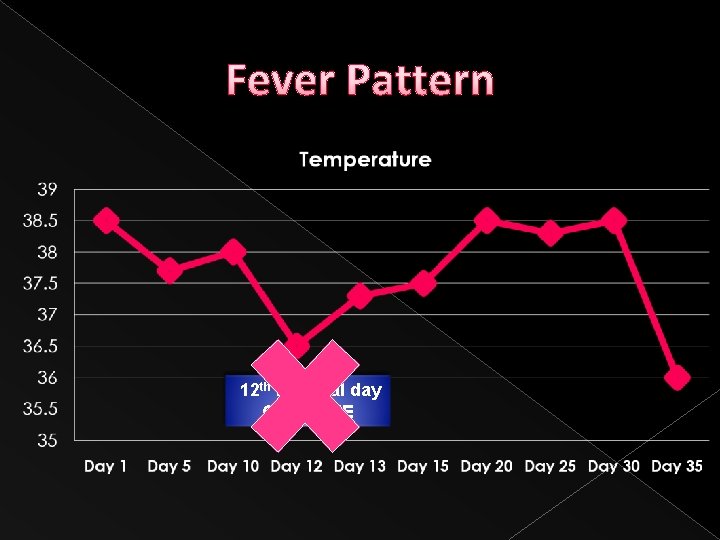
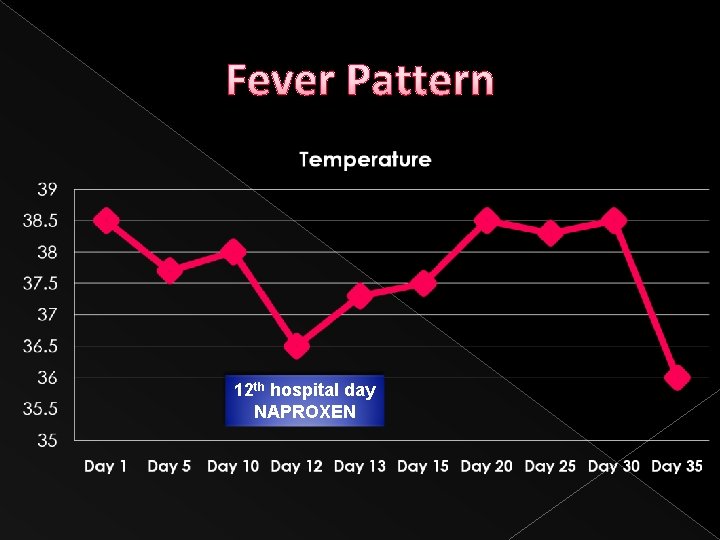
Fever Pattern 12 th hospital day CEFEPIME
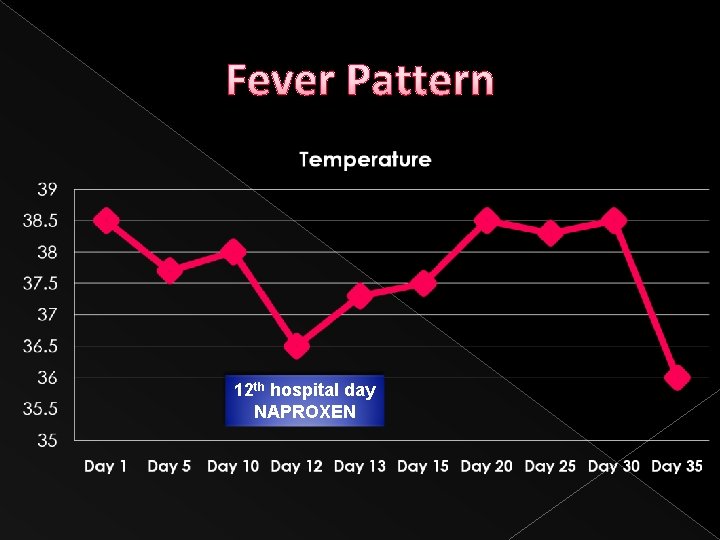
Fever Pattern 12 th hospital day NAPROXEN
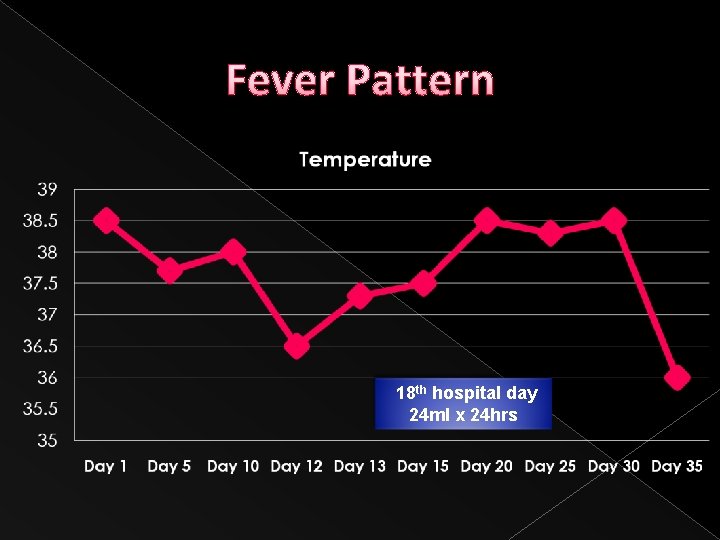
COURSE IN THE WARDS 18 th Hospital day � Fever � Pleural fluid cytology CYTOSPIN � Chest tube thoracostomy drainage (24 ml for 24 hrs) � Contrast chest CT scan done. � Chest tube removed. � Video- assisted Thoracoscopic surgery.
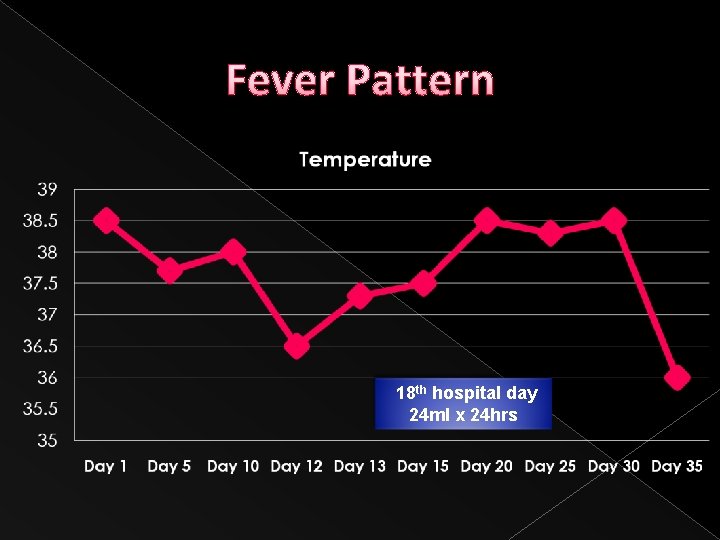
Fever Pattern 18 th hospital day 24 ml x 24 hrs

COURSE IN THE WARDS 25 th Hospital day � Post MINI thoracostomy, Decortication with pleural and lung biopsy � Isoniazid 300 mg, 1 tab, after dinner (Aug 1) � Rifampicin 600 mg, 1 tab, before dinner (Aug 2) � Ethambutol, 400 mg, 3 tabs, after dinner (Aug 4

Fever Pattern 25 th hospital day S/P VATS

COURSE IN THE WARDS 32 nd hospital Day � Afebrile Chest x-ray no recurrence of fever noted
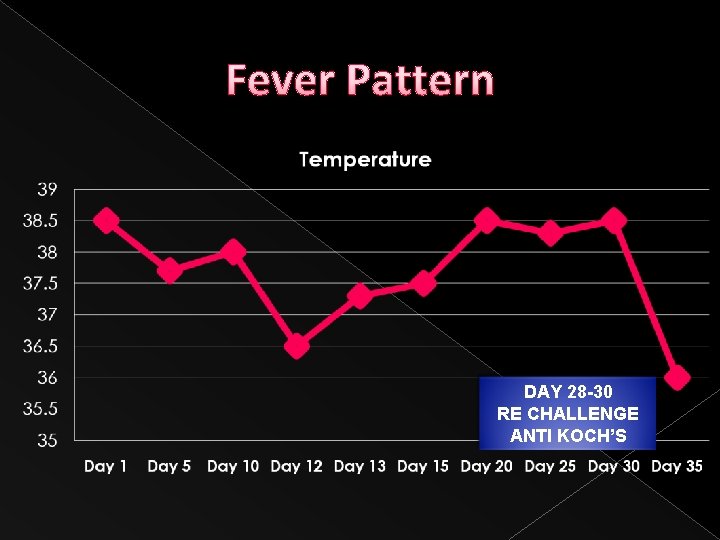
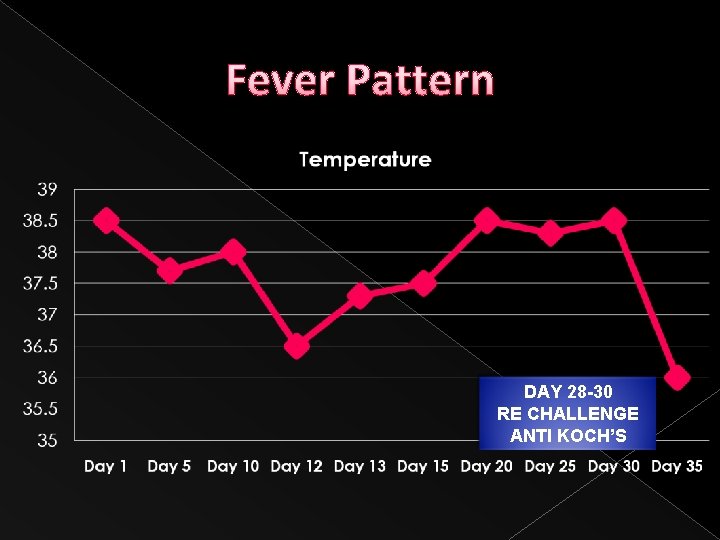
Fever Pattern DAY 28 -30 RE CHALLENGE ANTI KOCH’S
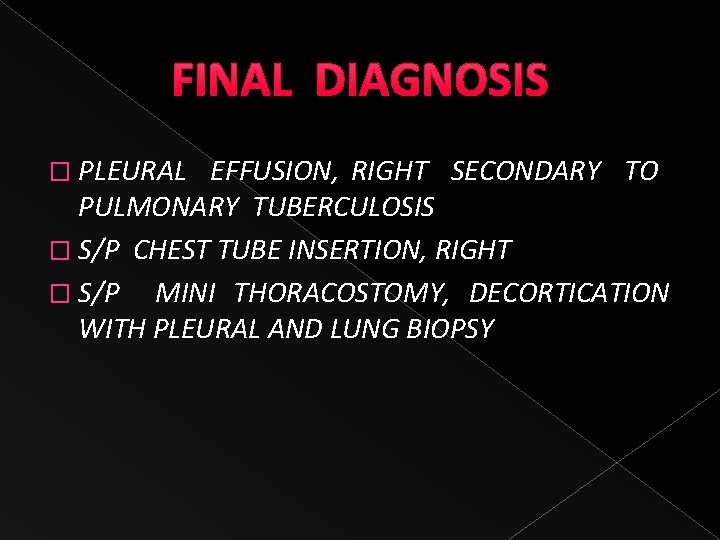
FINAL DIAGNOSIS � PLEURAL EFFUSION, RIGHT SECONDARY TO PULMONARY TUBERCULOSIS � S/P CHEST TUBE INSERTION, RIGHT � S/P MINI THORACOSTOMY, DECORTICATION WITH PLEURAL AND LUNG BIOPSY
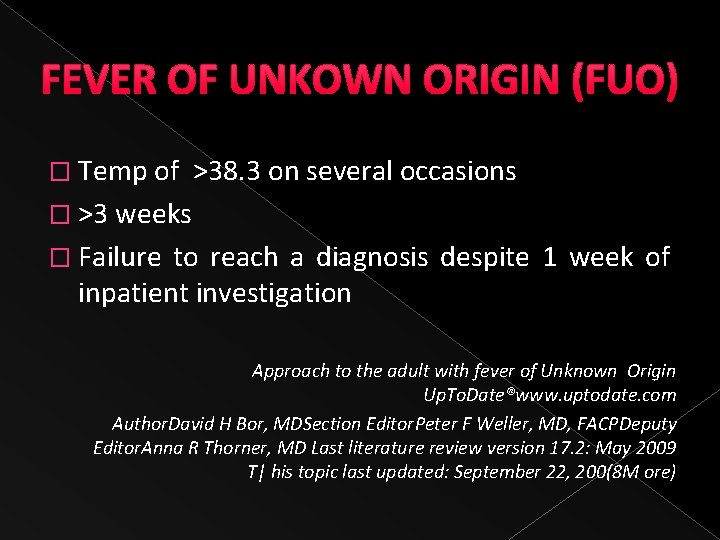
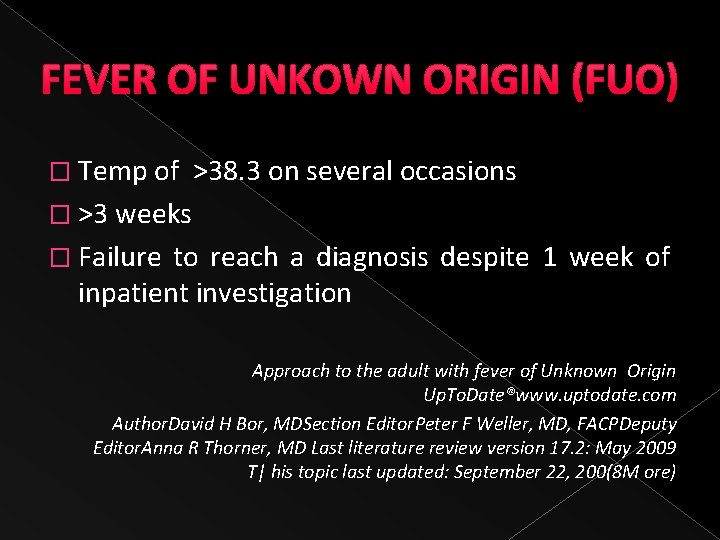
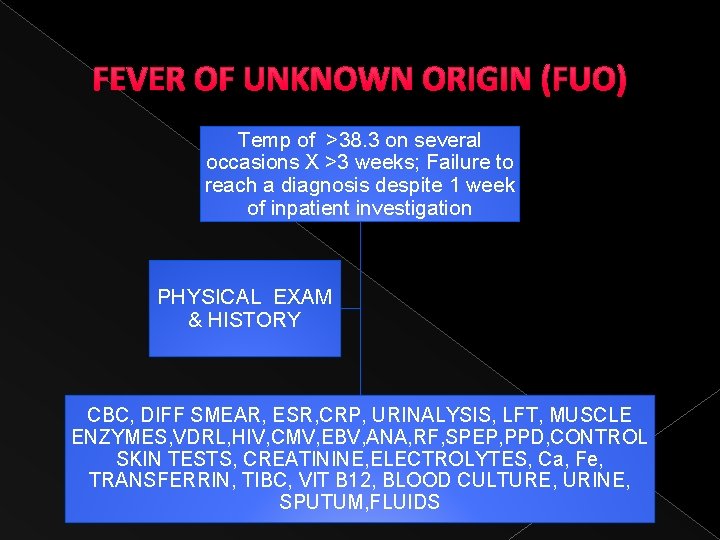
FEVER OF UNKOWN ORIGIN (FUO) � Temp of >38. 3 on several occasions � >3 weeks � Failure to reach a diagnosis despite 1 week of inpatient investigation Approach to the adult with fever of Unknown Origin Up. To. Date®www. uptodate. com Author. David H Bor, MDSection Editor. Peter F Weller, MD, FACPDeputy Editor. Anna R Thorner, MD Last literature review version 17. 2: May 2009 T| his topic last updated: September 22, 200(8 M ore)
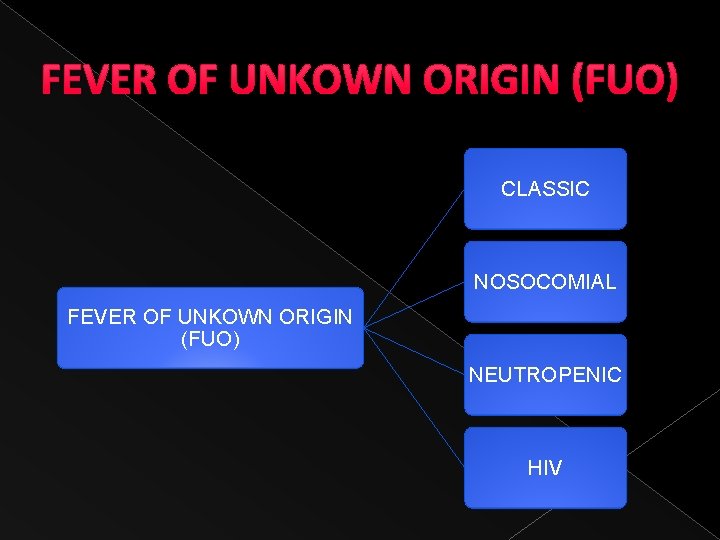
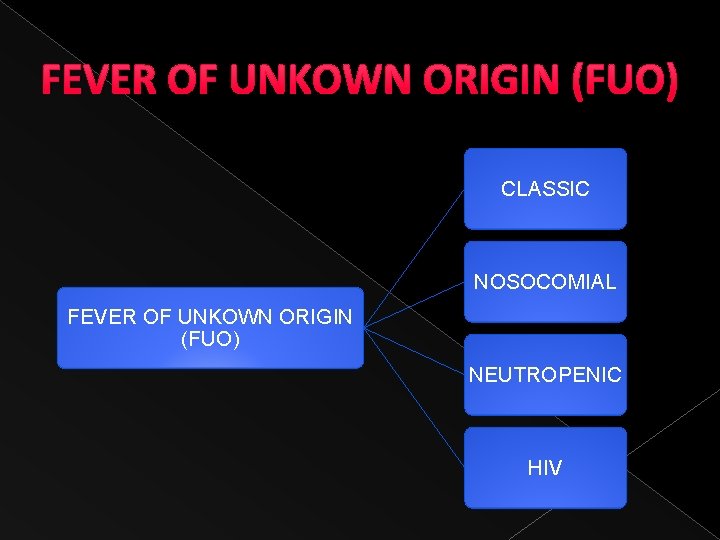
FEVER OF UNKOWN ORIGIN (FUO) CLASSIC NOSOCOMIAL FEVER OF UNKOWN ORIGIN (FUO) NEUTROPENIC HIV

DIFFERENTIAL DIAGNOSIS 58 year old male FEVER x 3 wks RUQ pain Dyspnea Decreased tactile fremitus dull on percussion decreased breath soundsmid to lower right lung field no crackles no wheezes INFECTIONS NEOPLASMS COLLAGEN VASCULAR DISEASES MISCELLANEOUS CONDITION
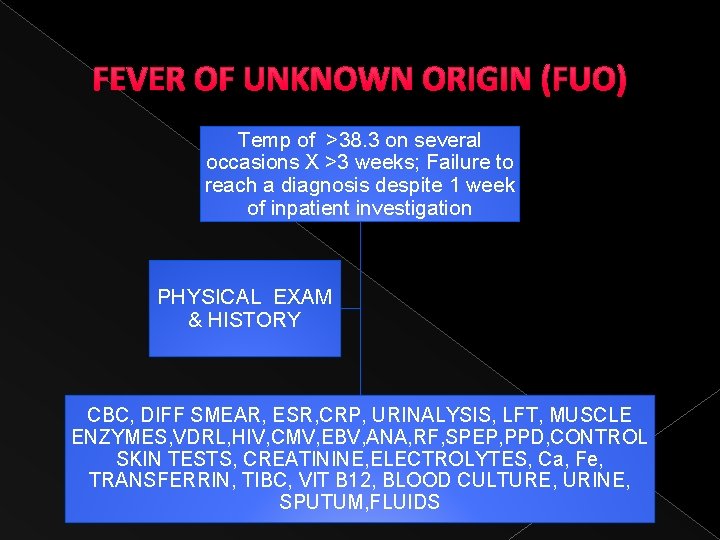
FEVER OF UNKNOWN ORIGIN (FUO) Temp of >38. 3 on several occasions X >3 weeks; Failure to reach a diagnosis despite 1 week of inpatient investigation PHYSICAL EXAM & HISTORY CBC, DIFF SMEAR, ESR, CRP, URINALYSIS, LFT, MUSCLE ENZYMES, VDRL, HIV, CMV, EBV, ANA, RF, SPEP, PPD, CONTROL SKIN TESTS, CREATININE, ELECTROLYTES, Ca, Fe, TRANSFERRIN, TIBC, VIT B 12, BLOOD CULTURE, URINE, SPUTUM, FLUIDS
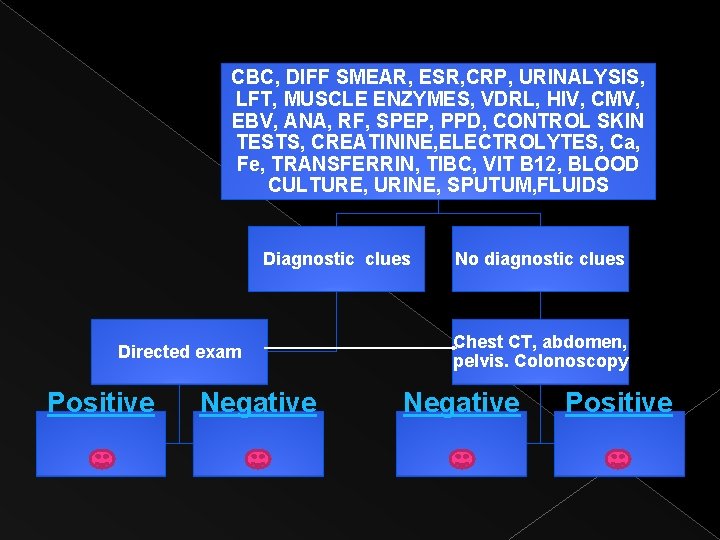
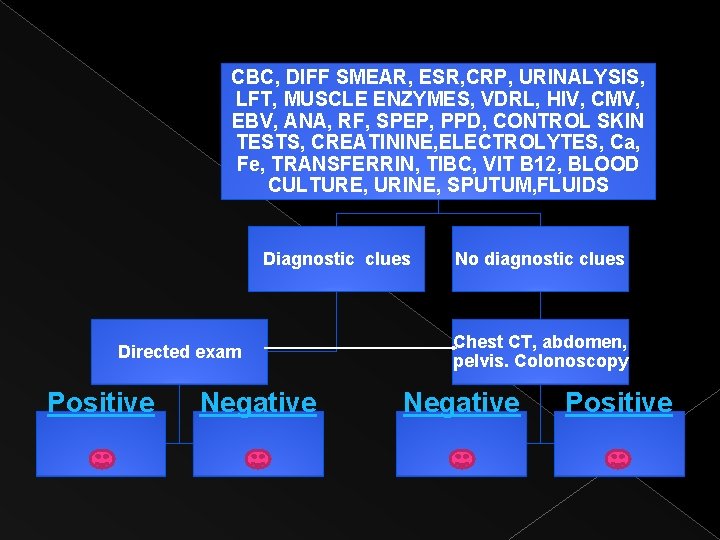
CBC, DIFF SMEAR, ESR, CRP, URINALYSIS, LFT, MUSCLE ENZYMES, VDRL, HIV, CMV, EBV, ANA, RF, SPEP, PPD, CONTROL SKIN TESTS, CREATININE, ELECTROLYTES, Ca, Fe, TRANSFERRIN, TIBC, VIT B 12, BLOOD CULTURE, URINE, SPUTUM, FLUIDS Diagnostic clues Directed exam Positive Negative No diagnostic clues Chest CT, abdomen, pelvis. Colonoscopy Negative Positive
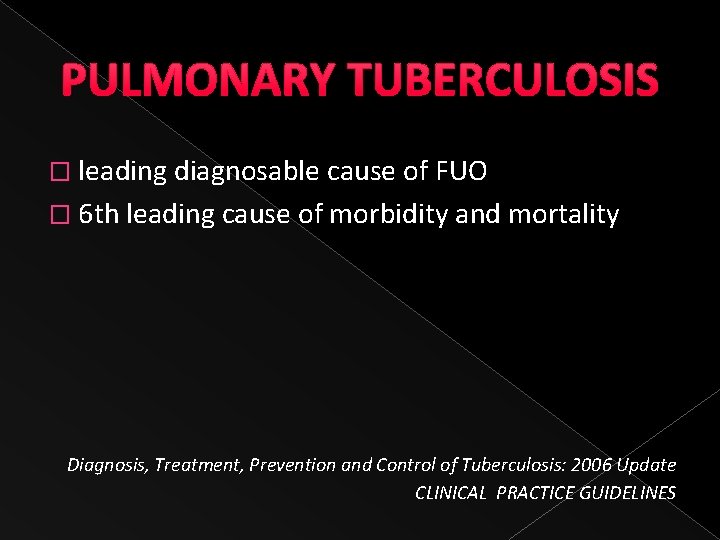
PULMONARY TUBERCULOSIS � leading diagnosable cause of FUO � 6 th leading cause of morbidity and mortality Diagnosis, Treatment, Prevention and Control of Tuberculosis: 2006 Update CLINICAL PRACTICE GUIDELINES
PULMONARY TUBERCULOSIS � When should one suspect that patient may have PTB? › Cough of two weeks or more › Cough with or without the ff: night sweats, weight loss, anorexia, unexplained fever and chills, chest pain, fatigue and body malaise › Cough x 2 weeks or more with or without accompanying symptoms TB SYMPTOMATIC

PULMONARY TUBERCULOSIS CATEGORIES NEW RELAPSE RETURN TO TREATMENT AFTER DEFAULT DEFINITION A patient who has never had treatment for TB or, if with previous anti TB medications, taken for less than 4 weeks. Declared cured of any form of TB in the past by a physician after one full course of anti TB medications, & now has become sputum smear (+) Stops medications for 2 months or more and comes back to the clinic smear (+)

PULMONARY TUBERCULOSIS CATEGORIES FAILURE TRANSFER –IN CHRONIC CASE DEFINITION While on treatment, remained or become smear (+) again at the fifth month of anti TB treatment or later; or a patient who was smear (-) at the start of treatment and becomes smear (+) at the 2 nd month Management was started from another area and now transferred to a new clinic Became or remained smear (+) after completing fully a supervised retreatment regimen
PULMONARY TUBERCULOSIS � What is the initial work up for a TB symptomatic? › Sputum microscopy (preferably 3 should be sent) › Collected first thing in the morning for 3 consecutive days
PULMONARY TUBERCULOSIS � INTERPRETATION OF RESULTS: › SMEAR POSITIVE: If at least two sputum specimens are AFB (+) › SMEAR NEGATIVE: If none of the specimens are AFB (+)
PULMONARY TUBERCULOSIS � DOUBTFUL: When only one of the 3 sputum specimens is (+) › When results are doubtful, a second set of the three must be collected › One of the second three is (+): SMEAR POSITIVE › All of the second three are (-): SMEAR NEGATIVE

PULMONARY TUBERCULOSIS � What additional tests should be done after a TB symptomatic has been found to be SMEAR POSITIVE? › No further tests are required

PULMONARY TUBERCULOSIS � Chest radiographs are not routinely necessary in the management of a TB symptomatic patient who is smear positive � PPD (Purified Protein derivative) testing will not additional information
PULMONARY TUBERCULOSIS � Blood/serum tests maybe taken when specific risks for possible adverse events during treatment are present
PULMONARY TUBERCULOSIS � All adults suspected to have PTB should have TB culture � Drug susceptibility testing is recommended: › Retreatment › Treatment failure › Smear positive patients suspected to have one or multi-drug resistant TB (MDR-TB)

PULMONARY TUBERCULOSIS � What tests are recommended for TB symtomatics who are smear negative? › TB culture with Drug susceptibilty › Chest Radiograph

PULMONARY TUBERCULOSIS � RECOMMENDED TREATMENT FOR NEWLY DIAGNOSED SMEAR POSITIVE › Short course chemotherapy (SCC) regimen � 2 months isonoazid, rifampicin, pyrazinamide and ethambutol
PULMONARY TUBERCULOSIS � 4 moths isoniazid and rifampicin �Given daily as initial phase followed by daily or thrice weekly administration of isoniazid and rifampicin during the continuation phase
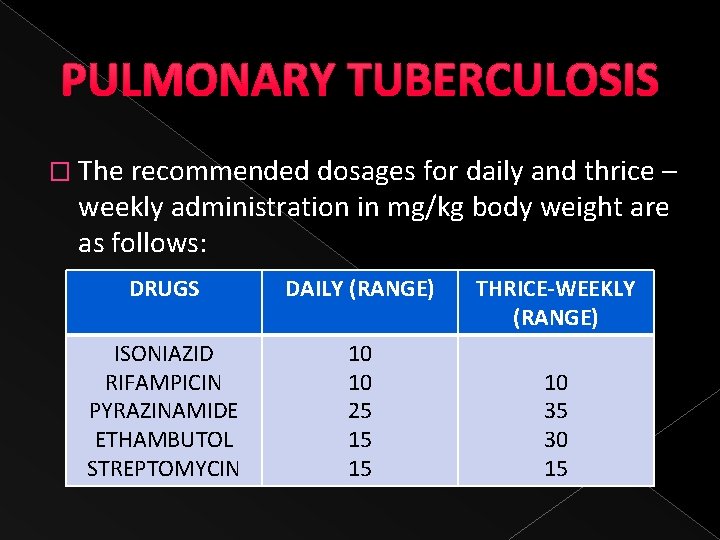
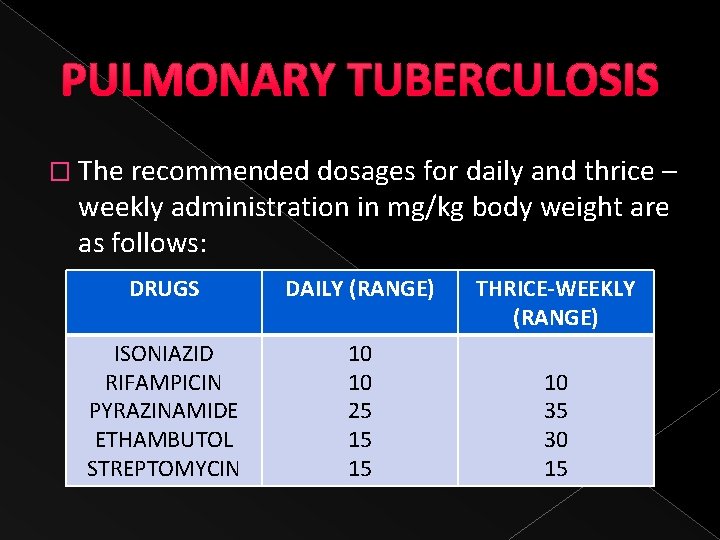
PULMONARY TUBERCULOSIS � The recommended dosages for daily and thrice – weekly administration in mg/kg body weight are as follows: DRUGS DAILY (RANGE) ISONIAZID RIFAMPICIN PYRAZINAMIDE ETHAMBUTOL STREPTOMYCIN 10 10 25 15 15 THRICE-WEEKLY (RANGE) 10 35 30 15

PULMONARY TUBERCULOSIS � RECOMMENDED TREATMENT FOR NEWLY DIAGNOSED SMEAR NEGATIVE � 2 HRZE/4 HR (WITHOUT HIV OR WITH AN UNKNOWN HIV)
PULMONARY TUBERCULOSIS � How can one reliably diagnose extrapulmonary tuberculosis (EPTB)? › High degree of suspicion in a patient at risk › Appropriate specimen should be processed for microbiologic, both microscopy, culture and histopathologic examinations

PULMONARY TUBERCULOSIS � What is the effective treatment regimen for EXTRAPULMONARY TUBERCULOSIS? › 6 -9 month regimen consisting of 2 months Isoniazid, Rifampicin, Pyrazinamide and Ethambutol (Initial Phase) › 4 -7 months Isoniazid and Rifampicin (Continuation Phase)
PULMONARY TUBERCULOSIS � TUBERCULOUS PLEURAL EFFUSION �Microscopic examination detecs acid fast bacilli in about 5 -10% of cases
PULMONARY TUBERCULOSIS � TREATMENT ADMINISTRATION › FIXED DOSE COMBINATION �Recommended for newly diagnosed TB patients: �Minimize the risk of monotherapy �Minimize drug resistance �Improve adherence with lesser number of pills to swallow �Reduce prescription errors
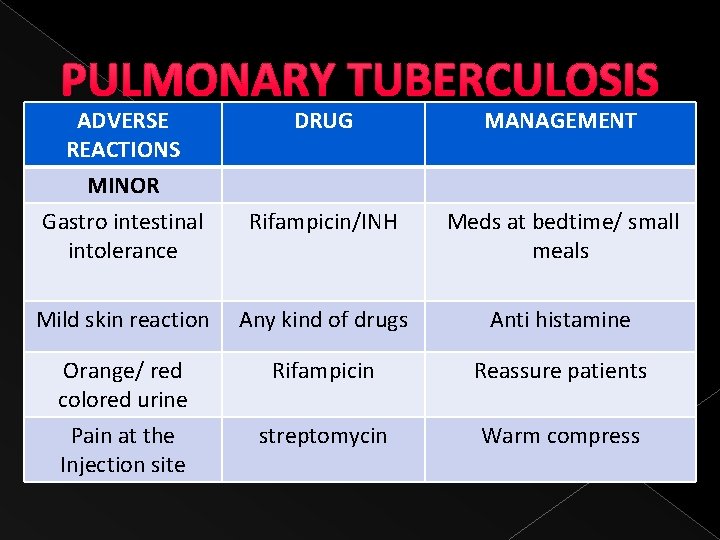
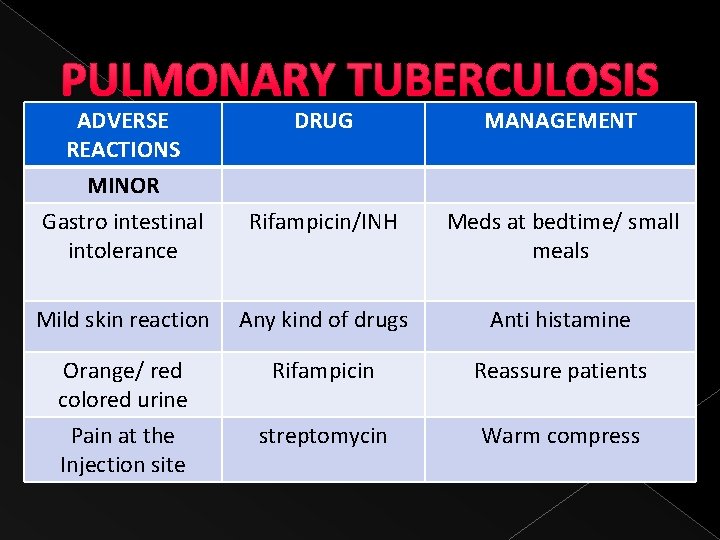
PULMONARY TUBERCULOSIS ADVERSE REACTIONS MINOR Gastro intestinal intolerance DRUG MANAGEMENT Rifampicin/INH Meds at bedtime/ small meals Mild skin reaction Any kind of drugs Anti histamine Orange/ red colored urine Pain at the Injection site Rifampicin Reassure patients streptomycin Warm compress
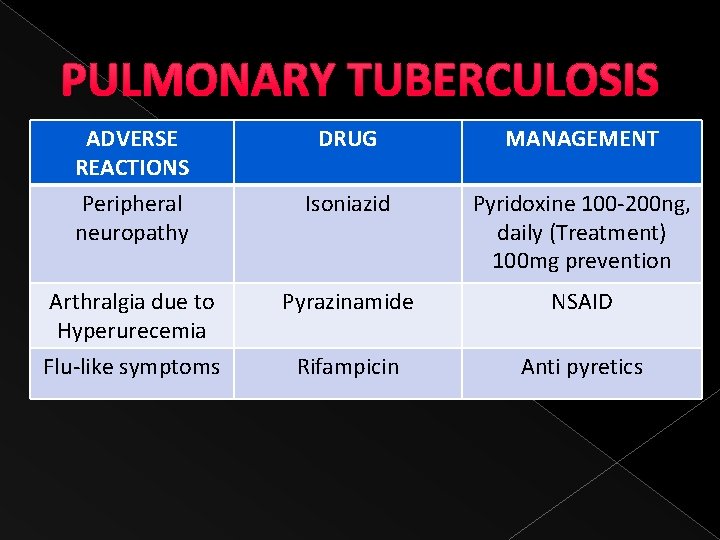
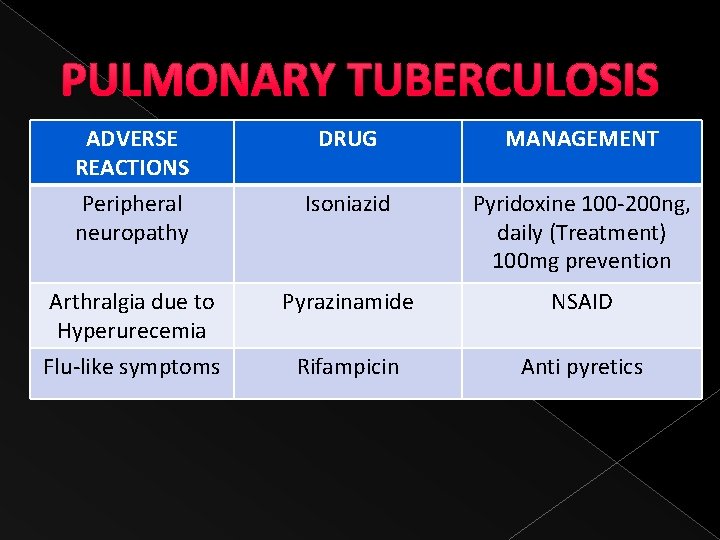
PULMONARY TUBERCULOSIS ADVERSE REACTIONS Peripheral neuropathy Arthralgia due to Hyperurecemia Flu-like symptoms DRUG MANAGEMENT Isoniazid Pyridoxine 100 -200 ng, daily (Treatment) 100 mg prevention Pyrazinamide NSAID Rifampicin Anti pyretics
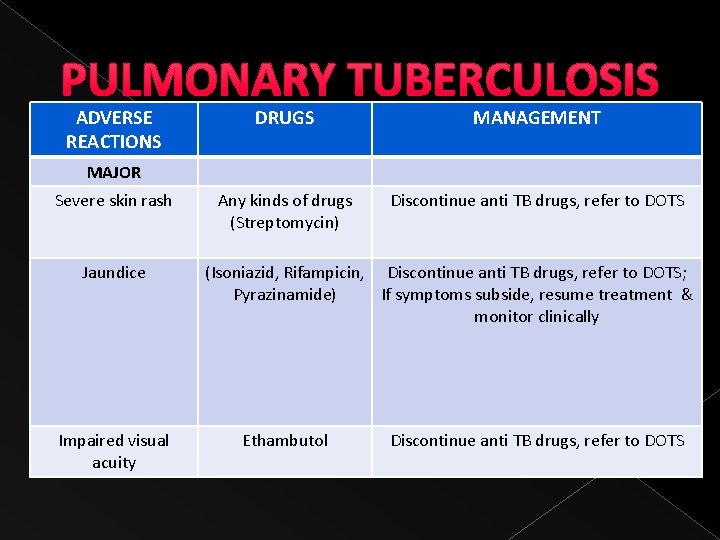
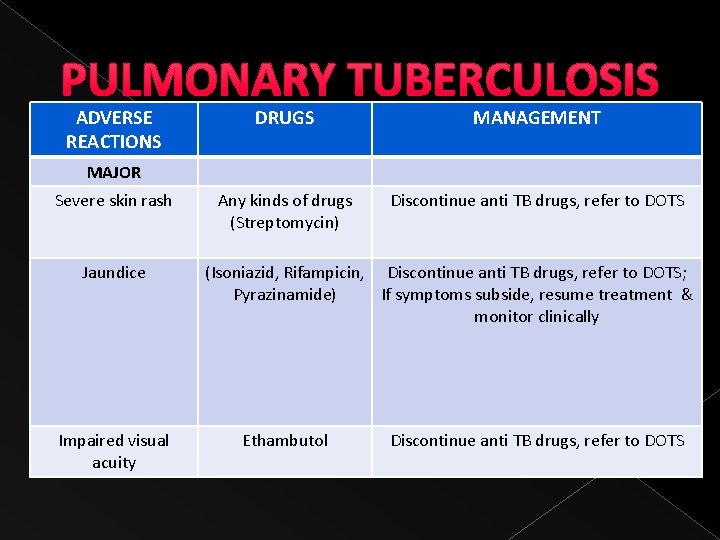
PULMONARY TUBERCULOSIS ADVERSE REACTIONS DRUGS MANAGEMENT Any kinds of drugs (Streptomycin) Discontinue anti TB drugs, refer to DOTS MAJOR Severe skin rash Jaundice Impaired visual acuity (Isoniazid, Rifampicin, Discontinue anti TB drugs, refer to DOTS; Pyrazinamide) If symptoms subside, resume treatment & monitor clinically Ethambutol Discontinue anti TB drugs, refer to DOTS
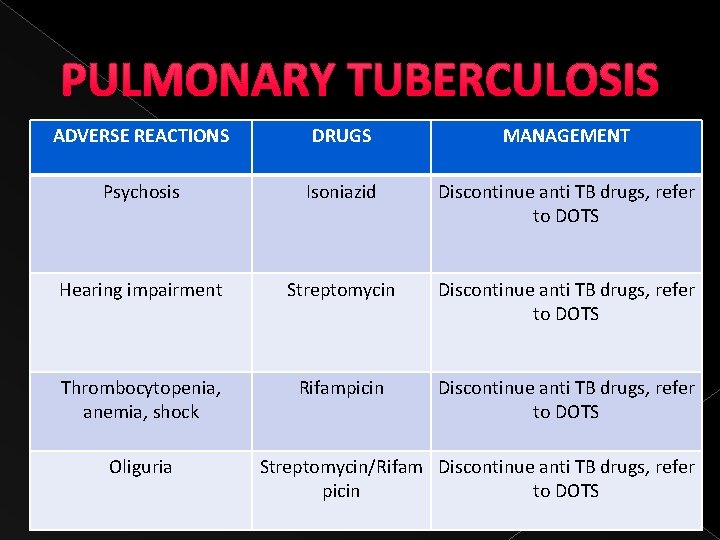
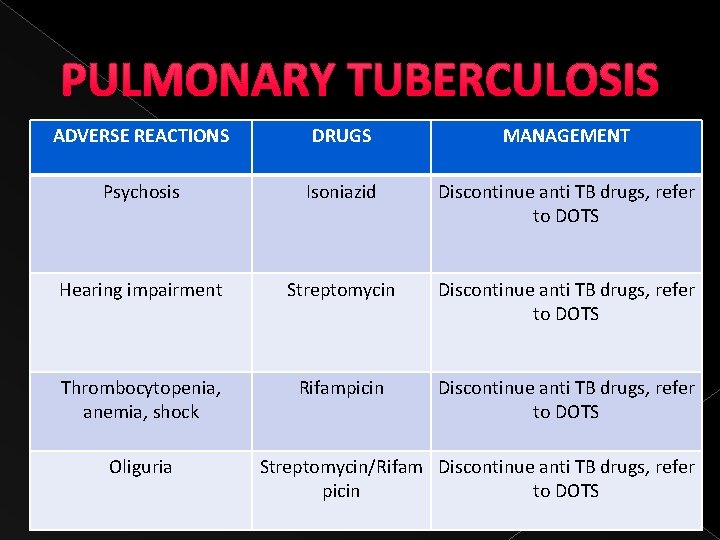
PULMONARY TUBERCULOSIS ADVERSE REACTIONS DRUGS MANAGEMENT Psychosis Isoniazid Discontinue anti TB drugs, refer to DOTS Hearing impairment Streptomycin Discontinue anti TB drugs, refer to DOTS Thrombocytopenia, anemia, shock Rifampicin Discontinue anti TB drugs, refer to DOTS Oliguria Streptomycin/Rifam Discontinue anti TB drugs, refer picin to DOTS

PULMONARY TUBERCULOSIS � SINGLE DOSE PREPARATION › Adverse reactions › Co morbid conditions requiring dose adjustments › Disease conditions where treatment is expected to have significant drug interactions with Anti TB drugs › At risk for adverse reactions
PULMONARY TUBERCULOSIS
PULMONARY TUBERCULOSIS � MONITORING OF OUTCOMES AND RESPONSE DURING TREATMENT › Defervesence occurred within 2 weeks in 78% of patients with drug susceptible organisms while only 9% of patients with multi drug resistance became afebrile › Teo SK. Four month chemotherapy in the treatment of smear negative PTB: results at 30 -60 months. Ann Acad Med Singapore 2002; 31: 175 -81
“Possible causes of persistent fever in pulmonary tuberculosis (once non-compliance and supraadded infections have been excluded) include cytokine release, drug induced fever, drug resistance, and drug malabsorption. ” BMJ 1996; 313: 1543 -1545 (14 December) Education and debate Grand Rounds--Hammersmith Hospital: Persistent fever in pulmonary tuberculosis Hammersmith Hospital, London W 12 0 HS Case presented by: Maha T Barakat, senior house officer in respiratory medicine Chairman: J Scott, director of medicine.
“Naproxen test” as a clinical tool in the differential diagnosis of fever of undetermined origin (FUO) � � � Patients with cancer in a study conducted at the Oncology Unit of the Good Samaritan Hospital in Dayton, Ohio. Patients with FUO and suspected or diagnosed malignancy Naproxen 250 mg twice a day orally at 12 -hourly intervals for at least 3 days Validity was not established because of the lack of an independent, blind comparison with a reference standard Correlation of the final diagnoses of FUO in all patients with their response to antibiotics and naproxen
Recommendation: More appropriate reference standard would be the absence of infection after extensive and thorough laboratory work-up coupled with the absence of any clinical deterioration without administration of any antibiotics on continued follow-up for at least a period of 2 weeks. Utility of Naproxen in the Differential Diagnosis of Fever of Undetermined Origin in Patients with Cancer: A Commentary Marissa M. Alejandria, M. D. * (*Infectious Disease Fellow, UP-PGH, Taft Avenue, Manila) (Phil J Microbiol Infect Dis 1999; 28(2): 73 -74)
RECHALLENGE � Restart each anti koch’s one by one. � To determine which the drug that the patient had allergic reaction

CBC JULY 5 JULY 10 JULY 27 HEMOGLOBIN 11. 6 12. 0 12 HEMATOCRIT 33 34. 4 36 WBC 3. 94 6. 79 11. 7 SEGMENTER 69 66 76 LYMPHOCYTE 18 17 13 MONOCYTE 9 11 9 PLATELETS 493, 00 401, 000 349, 000

Sodium Potassium Creatinine BUN Glucose Calcium albumin Alkaline phosphatase AST ALT 7/5 139 3. 8 0. 90 7/6 137 4. 3 1. 0 75. 9 137 8. 3 2. 7 152 28 42 7/15 7/23 7/30 0. 9 21 34 1. 0 8/4
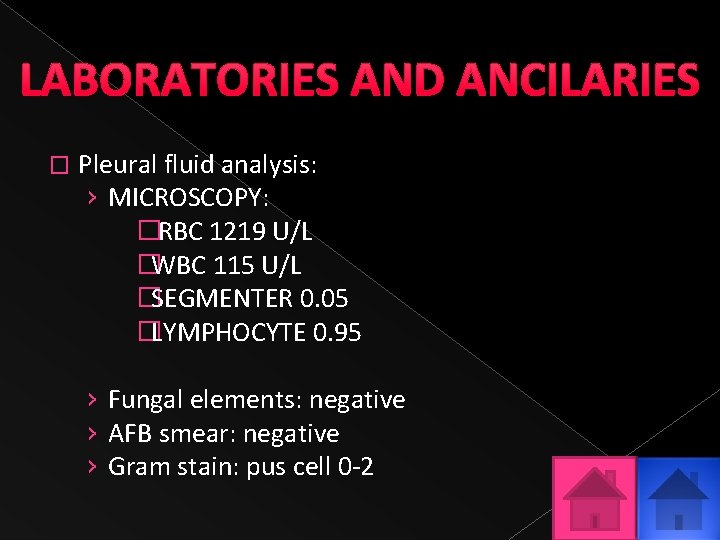
LABORATORIES AND ANCILARIES � Pleural fluid analysis: › MICROSCOPY: � RBC 1219 U/L �WBC 115 U/L �SEGMENTER 0. 05 �LYMPHOCYTE 0. 95 › Fungal elements: negative › AFB smear: negative › Gram stain: pus cell 0 -2
� Pleural Fluid culture (July 8): no growth � Pleural cells Fluid Cytology: negative for malignant � Cytospin: Chronic Inflammatory process
LABORATORIES AND ANCILARIES � Pleural Tissue and Lung Biopsy › CHRONIC GRANULOMATOUS INFLAMMATION, CONSISTENT WITH TUBERCULOSIS, RIGHT PLEURAL BIOPSY › Congestion and atelectasis, adjacent lung tissue
LABORATORIES AND ANCILARIES � Lupus panel : negative
LABORATORIES AND ANCILARIES � AFB Sputum x 3 days (July 5 -7, 2009): Negative � AFB sputum culture July 8, 2009: no growth � Blood Culture July 6, 09: No growth after 5 days

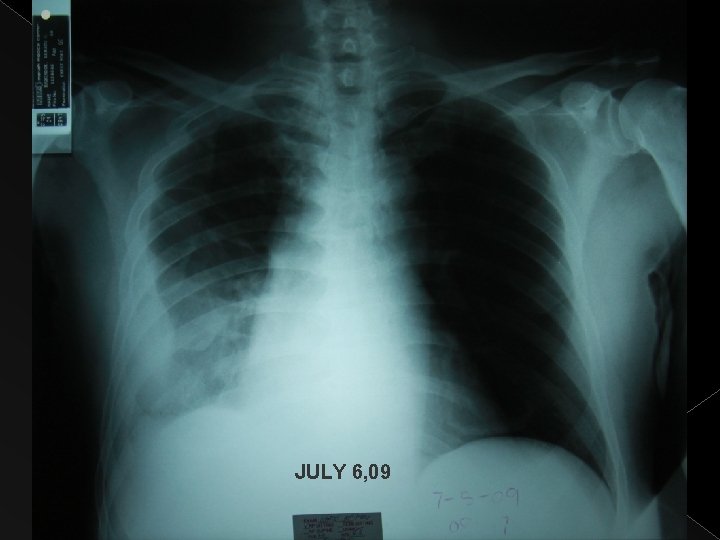
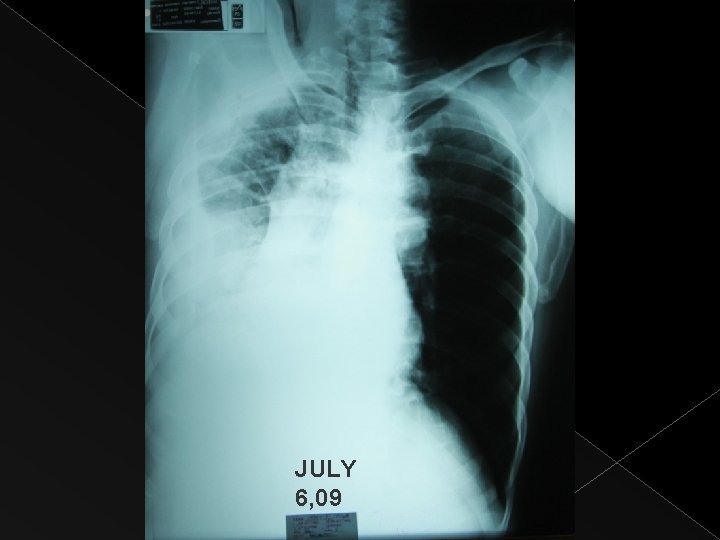
LABORATORIES AND ANCILARIES Chest x-ray July 6, 2009 Decreased in the pleural density at the right mid-lower outer lung with blunting of the costophrenic sulcus. No layering seen in the right lateral decubitus view. Loculated pleural effusion and /or thickening considered. Underlying parenchymal pathology not ruled out. The heart is not enlarged.

JUNE 27, 09
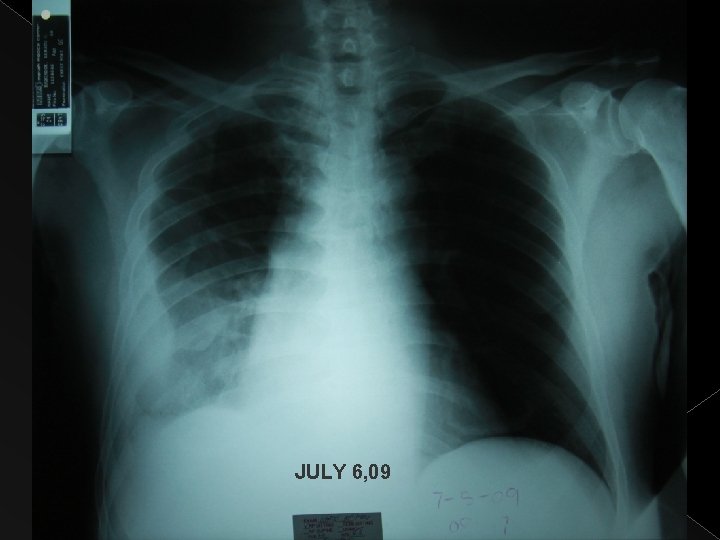
JULY 6, 09
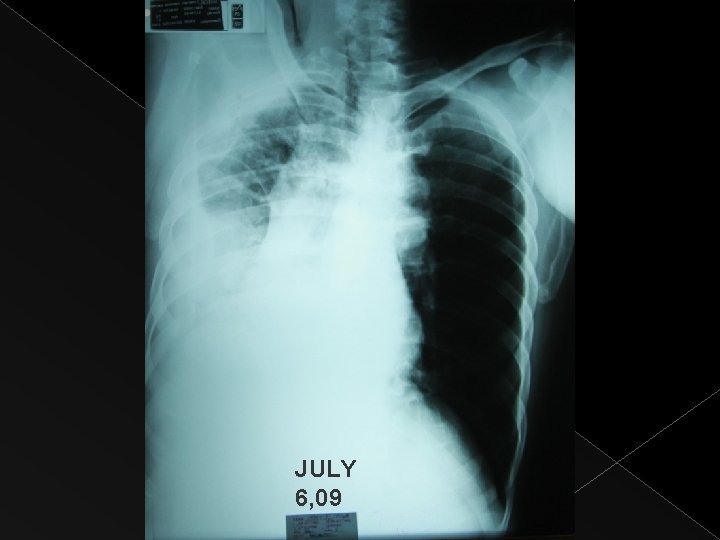
JULY 6, 09

JULY 6, 09
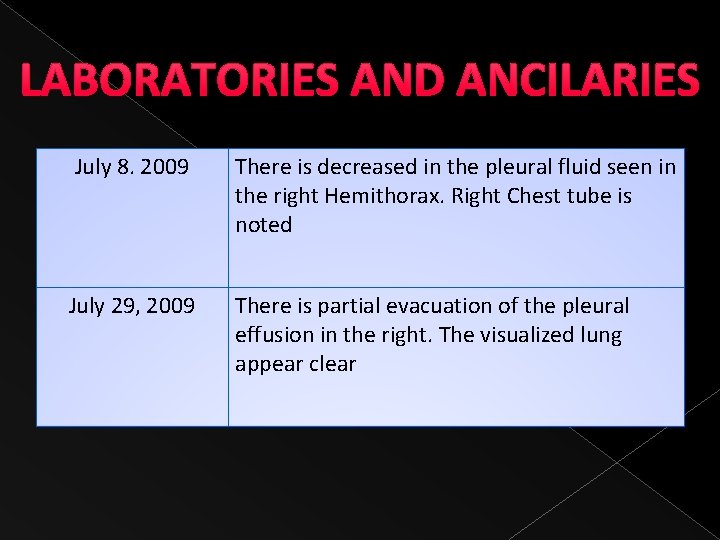
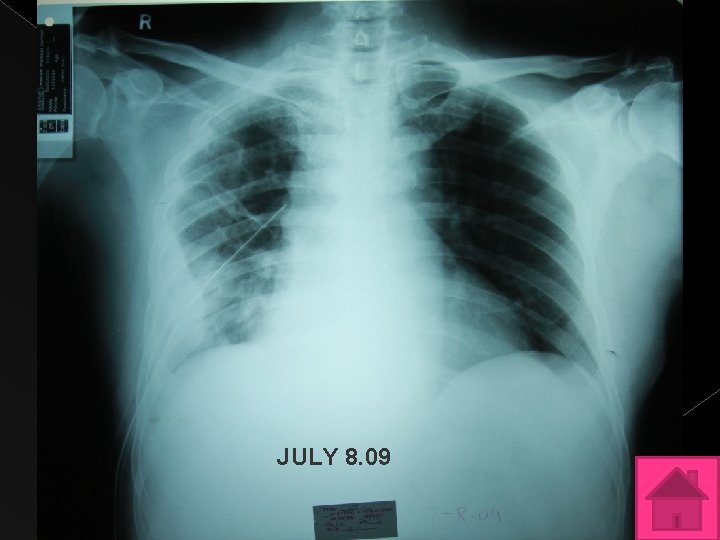
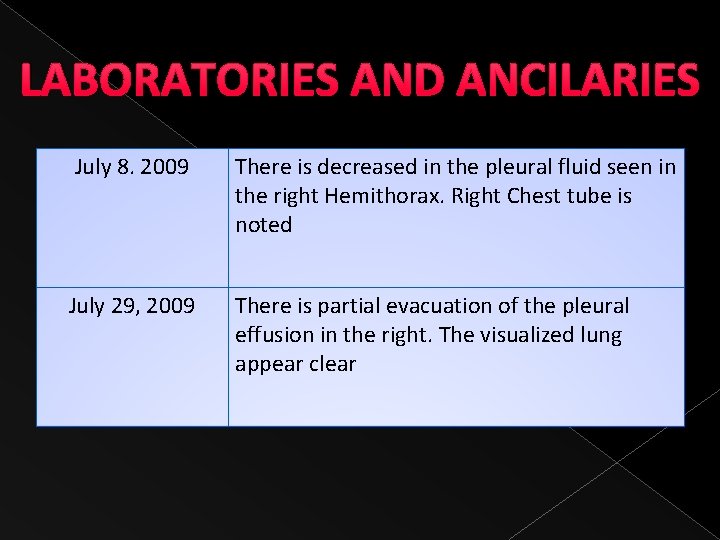
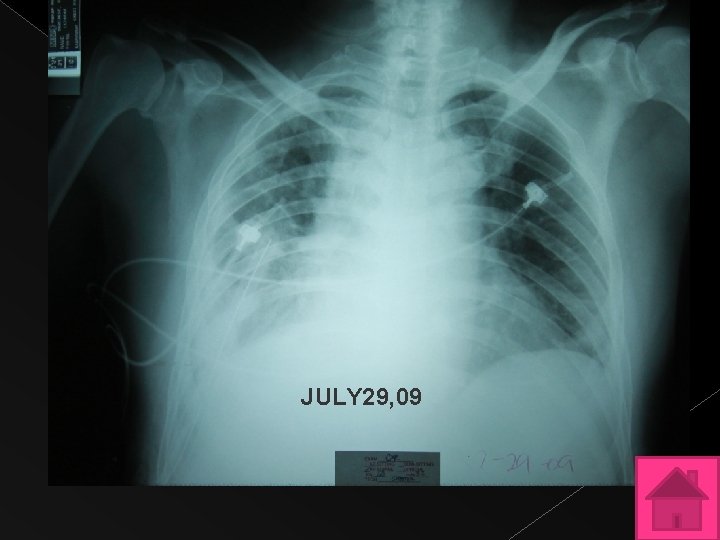
LABORATORIES AND ANCILARIES July 8. 2009 There is decreased in the pleural fluid seen in the right Hemithorax. Right Chest tube is noted July 29, 2009 There is partial evacuation of the pleural effusion in the right. The visualized lung appear clear
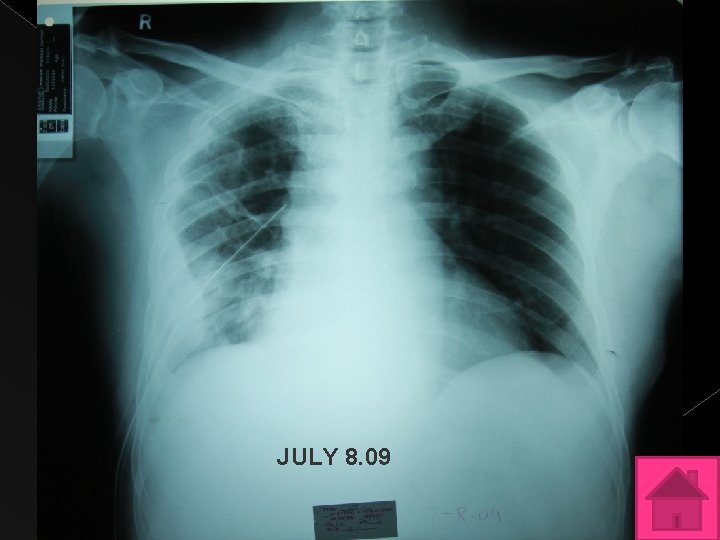
JULY 8. 09
LABORATORIES AND ANCILARIES July 8. 2009 There is decreased in the pleural fluid seen in the right Hemithorax. Right Chest tube is noted July 29, 2009 There is partial evacuation of the pleural effusion in the right. The visualized lung appear clear
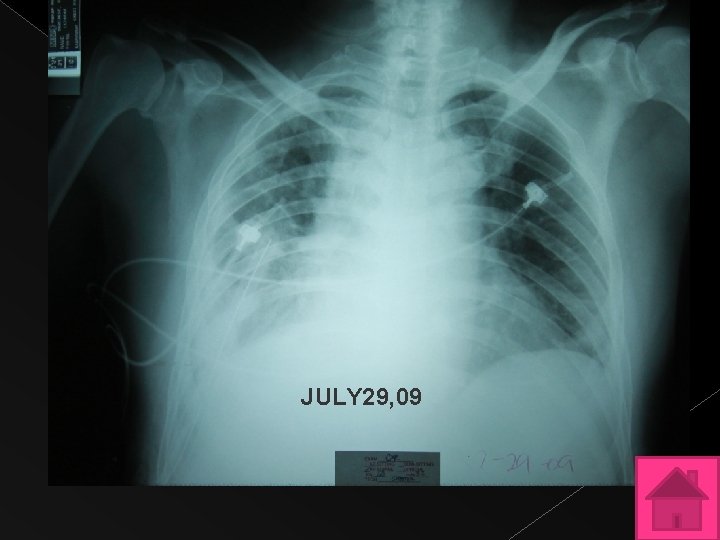
JULY 29, 09

LABORATORIES AND ANCILARIES � CT SCAN OF THE CHEST July 7, 2009: › Consider Pneumonia vs PTB, right upper lobe. › Moderate pleural effusion, right › passive atelectasis of the posterior basal segment of the right lower lobe prominent paratracheal lymph nodes, not enlarged by CT criteria › Subcentimeter cyst, right kidney, Bosniak I Category › Normal contrast enhanced CT scan of the rest of the abdominal organs

LABORATORIES AND ANCILARIES � CT SCAN OF THE CHEST July 23, 2009: › Interval placement of the right thoracostomy tube with residual pleural effusion › Possibilty of loculation is entertained › No interval change in the right pulmonary infiltrates since the previous examination › Present note of focal atelectasis in the right lower lobe seen › Prominent pretracheal and precarinal lymph node, relatively unchanged.
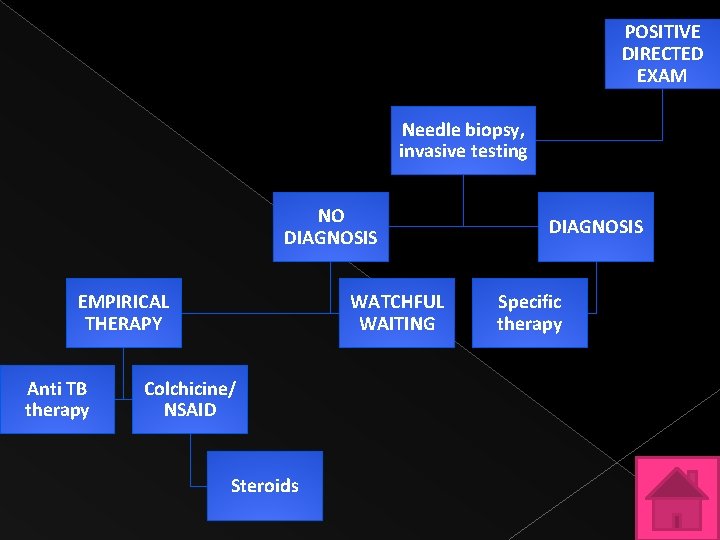
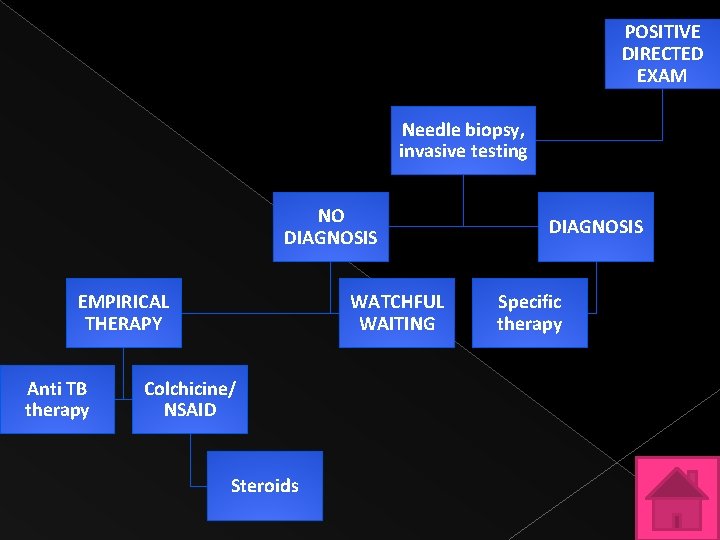
POSITIVE DIRECTED EXAM Needle biopsy, invasive testing NO DIAGNOSIS EMPIRICAL THERAPY Anti TB therapy WATCHFUL WAITING Colchicine/ NSAID Steroids DIAGNOSIS Specific therapy
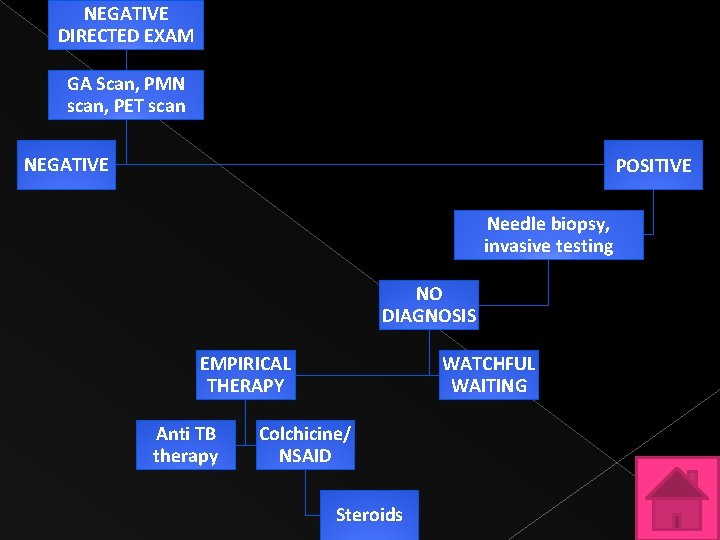
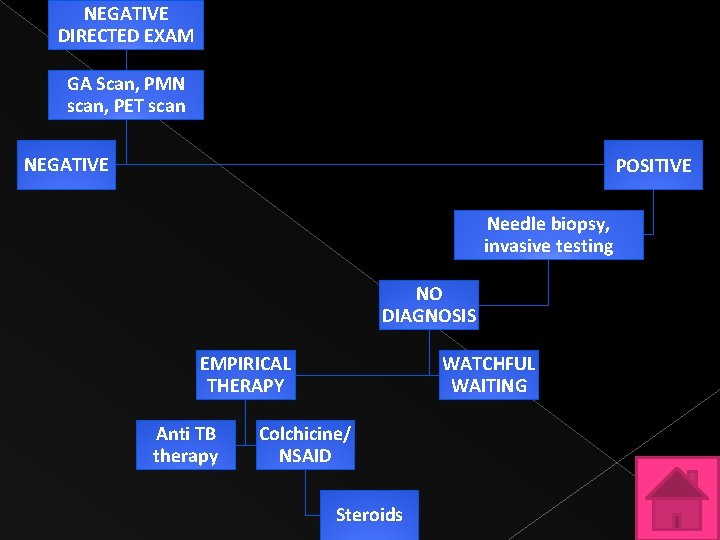
NEGATIVE DIRECTED EXAM GA Scan, PMN scan, PET scan NEGATIVE POSITIVE Needle biopsy, invasive testing NO DIAGNOSIS EMPIRICAL THERAPY Anti TB therapy WATCHFUL WAITING Colchicine/ NSAID Steroids

NEGATIVE CT chest, abdomen, pelvis and colonoscopy GA Scan, PMN scan, PET scan POSITIVE NEGATIVE Needle biopsy, invasive testing No diagnosis Empirical therapy Anti TB therapy Watchful waiting Colchicine/ NSAID Steroids
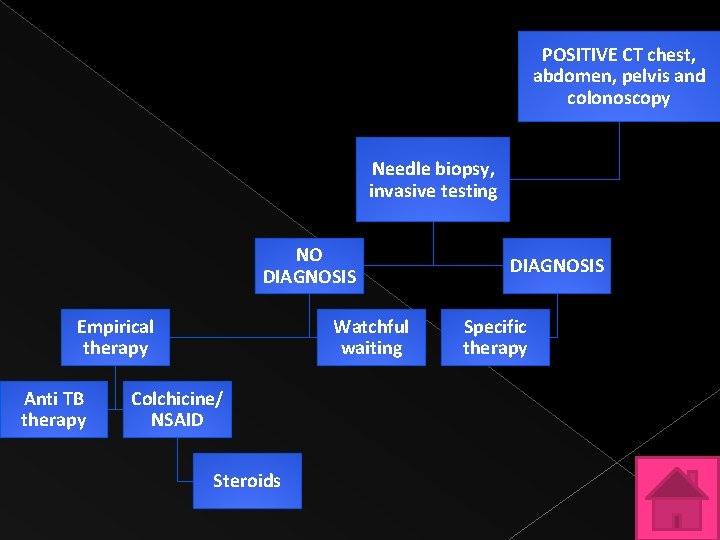
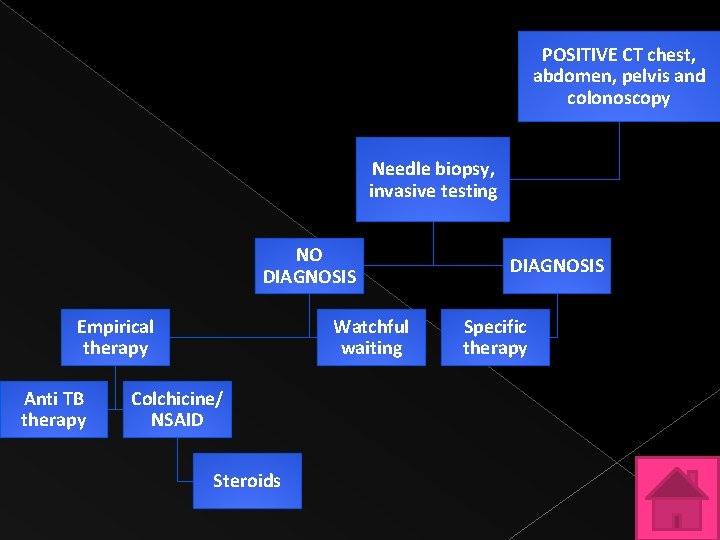
POSITIVE CT chest, abdomen, pelvis and colonoscopy Needle biopsy, invasive testing NO DIAGNOSIS Empirical therapy Anti TB therapy Watchful waiting Colchicine/ NSAID Steroids DIAGNOSIS Specific therapy

SUMMARY � PTB leading diagnosable cause of FUO Defervesence occurred within 2 weeks in 78% of patients with drug susceptible organisms while only 9% of patients with multi drug resistance became afebrile Validty is not established in Naproxen test � Should be treated accordingly

Thank you!!!
 Great pretender marie
Great pretender marie Spirochetales
Spirochetales Great pretender protein
Great pretender protein Curva de ballesta
Curva de ballesta Map rizal's second sojourn
Map rizal's second sojourn Aborted duel with antonio luna
Aborted duel with antonio luna Why rizal called champion of filipino youth
Why rizal called champion of filipino youth Desiliencia
Desiliencia Rainha d. leonor
Rainha d. leonor Rona cooper
Rona cooper Rona patey
Rona patey Mga karapatan ng bata sa wastong nutrisyon
Mga karapatan ng bata sa wastong nutrisyon Foto rona
Foto rona Roña
Roña Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết Bảng số nguyên tố
Bảng số nguyên tố Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Chụp tư thế worms-breton
Chụp tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Cái miệng nó xinh thế
Cái miệng nó xinh thế Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Tư thế ngồi viết
Tư thế ngồi viết Thứ tự các dấu thăng giáng ở hóa biểu
Thứ tự các dấu thăng giáng ở hóa biểu Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Thể thơ truyền thống
Thể thơ truyền thống Hát lên người ơi
Hát lên người ơi Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Cong thức tính động năng
Cong thức tính động năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Môn thể thao bắt đầu bằng từ đua
Môn thể thao bắt đầu bằng từ đua Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ điện thế nghỉ
điện thế nghỉ Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Gấu đi như thế nào
Gấu đi như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Tia chieu sa te
Tia chieu sa te A great deal vs a great many
A great deal vs a great many Great faces great places
Great faces great places Did alexander the great deserve to be called great
Did alexander the great deserve to be called great With great power comes great responsibility
With great power comes great responsibility Responsible leadership
Responsible leadership Frederick the great enlightened despot
Frederick the great enlightened despot Does alexander deserve to be called the great
Does alexander deserve to be called the great Do hammerhead sharks attack people
Do hammerhead sharks attack people With great expectations comes great responsibility
With great expectations comes great responsibility No shadow of turning
No shadow of turning Turning great strategy into great performance
Turning great strategy into great performance Types of anticoagulants
Types of anticoagulants Marie toullec théry co intervention
Marie toullec théry co intervention Ene parv
Ene parv Marie curie pharmacy
Marie curie pharmacy Jeanne marie kegelin
Jeanne marie kegelin Marie vavasseur
Marie vavasseur Antoine marie joseph artaud
Antoine marie joseph artaud Alex brizendine
Alex brizendine Bréviligne
Bréviligne Dawn marie's dream
Dawn marie's dream Maison natale de ronsard
Maison natale de ronsard Doena marie
Doena marie Ts ivana marie
Ts ivana marie Plan de sauvegarde des biens culturels
Plan de sauvegarde des biens culturels Marie wall almquist
Marie wall almquist Marie curiová pierre curie
Marie curiová pierre curie Il faut chanter pour toutes les mamans du monde
Il faut chanter pour toutes les mamans du monde Marie curie facts
Marie curie facts Elementos de marie curie
Elementos de marie curie Atelier lucie marie
Atelier lucie marie Isabella maria swan
Isabella maria swan Tina marie farmer
Tina marie farmer Land art richard long
Land art richard long Zierikzeese marie
Zierikzeese marie Marie
Marie Marie huckins
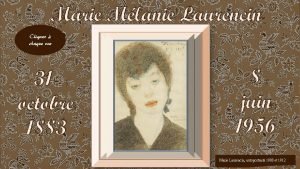
Marie huckins La princesse de cleves marie laurencin
La princesse de cleves marie laurencin El aprendizaje segun bandura
El aprendizaje segun bandura Jean marie clausse
Jean marie clausse Polybase limitations
Polybase limitations Marie-geneviève navarre
Marie-geneviève navarre Jean marie klinkenberg
Jean marie klinkenberg Dr marie stewart
Dr marie stewart Julia marie schlatter
Julia marie schlatter