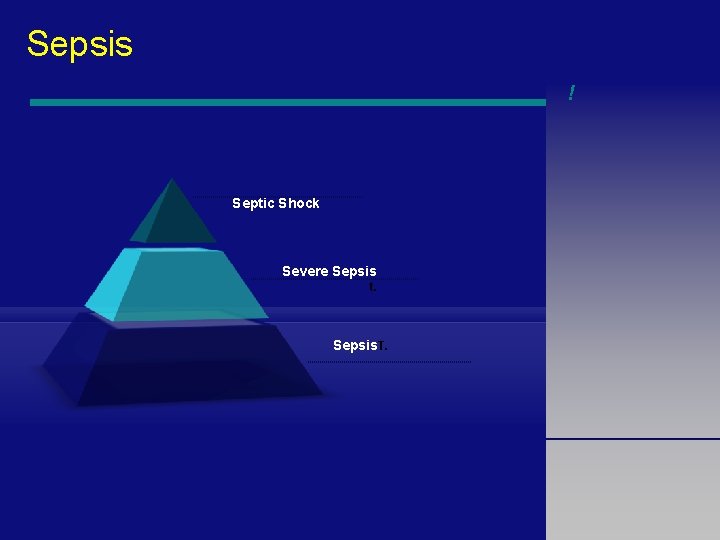
Sepsis Severe Sepsis Septic Shock Meral SNMEZOLU Prof


![Epidemiology Incidence of Sepsis [1993 -2001]. . . a 75% increase in. . . Epidemiology Incidence of Sepsis [1993 -2001]. . . a 75% increase in. . .](https://slidetodoc.com/presentation_image_h/d2c6812addc4372c8f0e71f70ee1b18f/image-32.jpg)















- Slides: 113
Sepsis, Severe Sepsis & Septic Shock Meral SÖNMEZOĞLU, Prof Yeditepe University Hospital Infectious Diseases Department 1
Overview • Differentiation between Septic Shock in relation to other conditions in current code, Sepsis, and Severe Sepsis • Disease Epidemiology, Incidence and Mortality • Inadequacy of Current Diagnostic Codes • Proposed Modifications and Clarification • Discussion 2
KEY POINTS • Severe sepsis and septic shock have high prevalence and mortality. • Treatment is time-sensitive and depends on early identification and risk-stratification. • Treatment must include antibiotics and targeted therapies designed to optimize oxygen delivery. • Adherence to a treatment algorithm decreases mortality 3
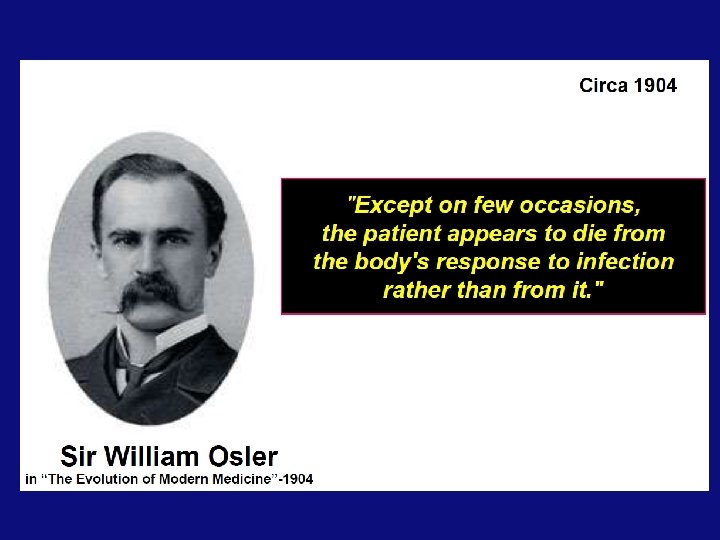
4
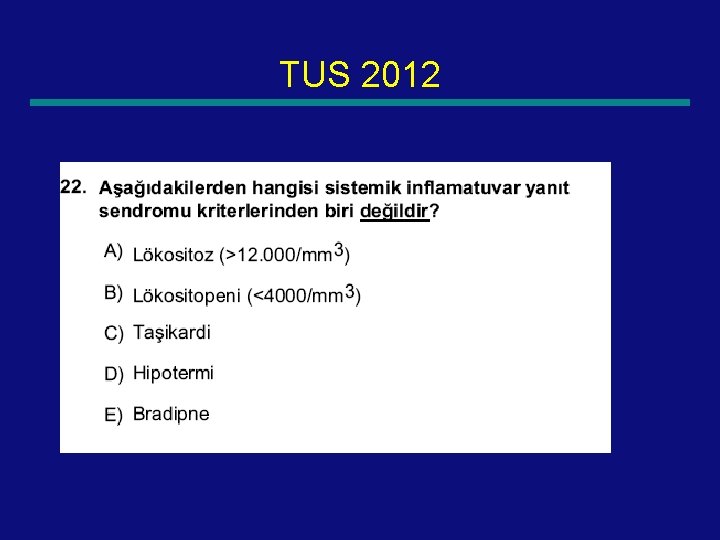
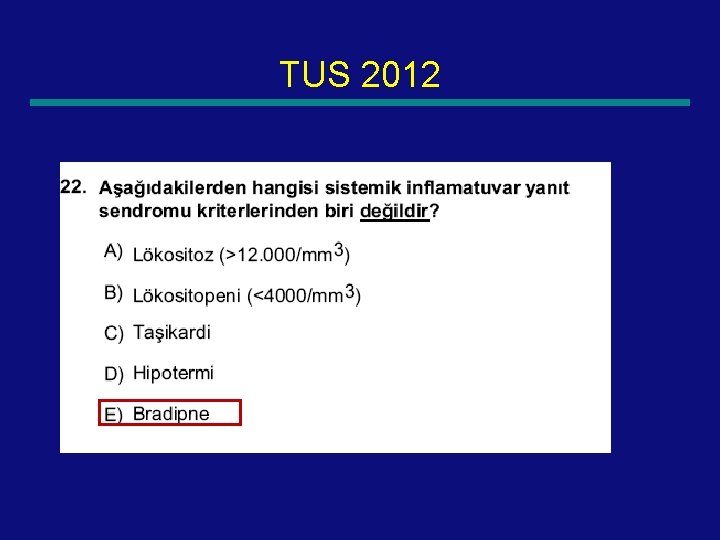
Systemic Inflammatory Response • At least 2 of 4 ( abnormal temp or leukocytes count is a must) —Core temp >38. 5 or <36 —Tachycardia: HR >2 sd above Normal for age or bradycardia <10% for age —Tachypnea: RR >2 sd for age or mechanical ventilation for acute process —Leukocyte elevated or depressed for age or >10% immature neutrophils 5
Definitions • Infection: Suspected or proven caused by any pathogen Or clinical syndrome associated with high probability of infection • Sepsis: SIRS in the presence of or as a result of suspected of proven infection 6
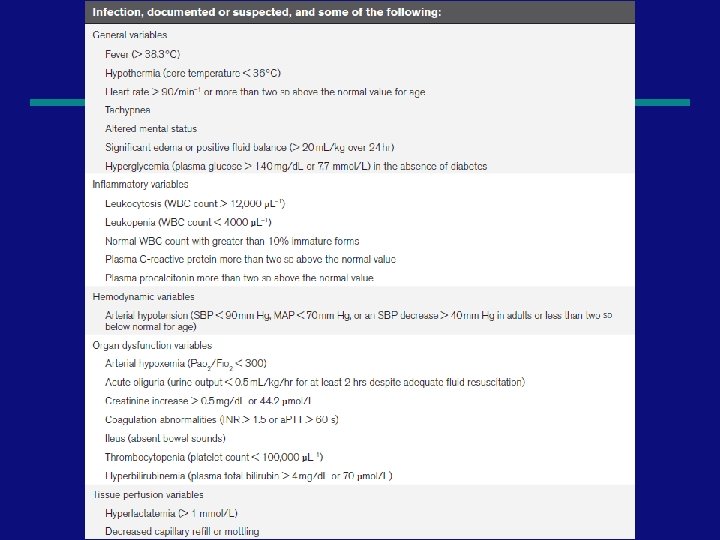
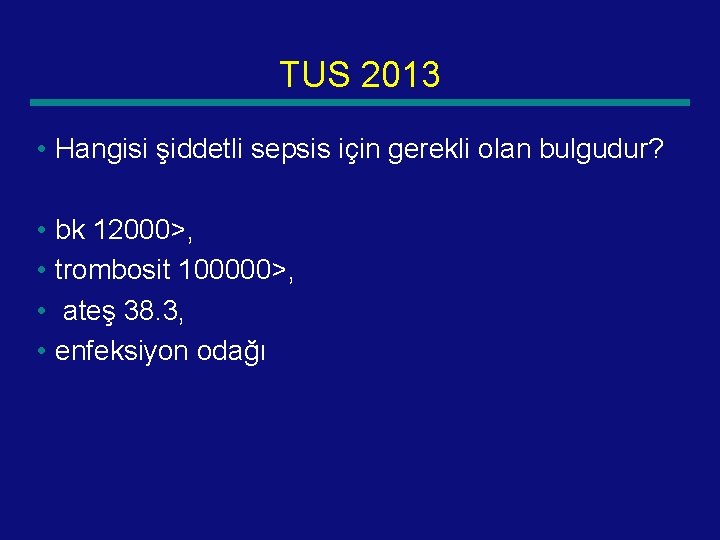
Definitions • Sepsis is defined as the presence (probable or documented) of infection together with systemic manifestations of infection. • Severe sepsis is defined as sepsis plus sepsisinduced organ dysfunction or tissue hypoperfusion 7
Definitions • Severe Sepsis: sepsis + one —Cardiovascular dysfunction —ARDS —OR 2 or more other organ dysfunctions • Septic shock —Sepsis and cardiovascular organ dysfunction 8
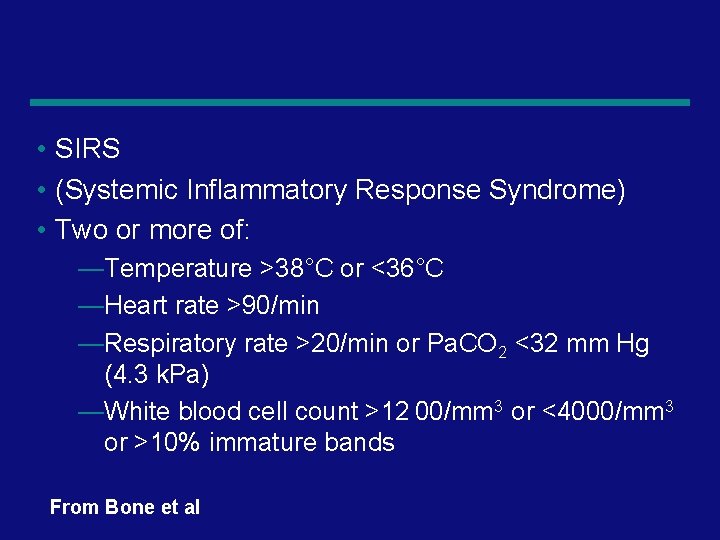
Definitions • Septic shock —Sepsis and cardiovascular organ dysfunction • Septic shock is defined as sepsis-induced hypotension persisting despite adequate fluid • resuscitation. • Sepsis-induced tissue hypoperfusion is defined • as infection-induced hypotension, elevated lactate, or oliguria 9
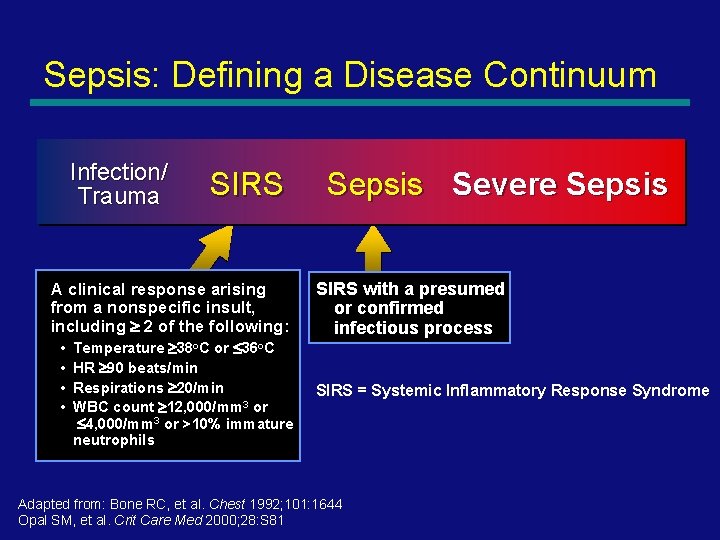
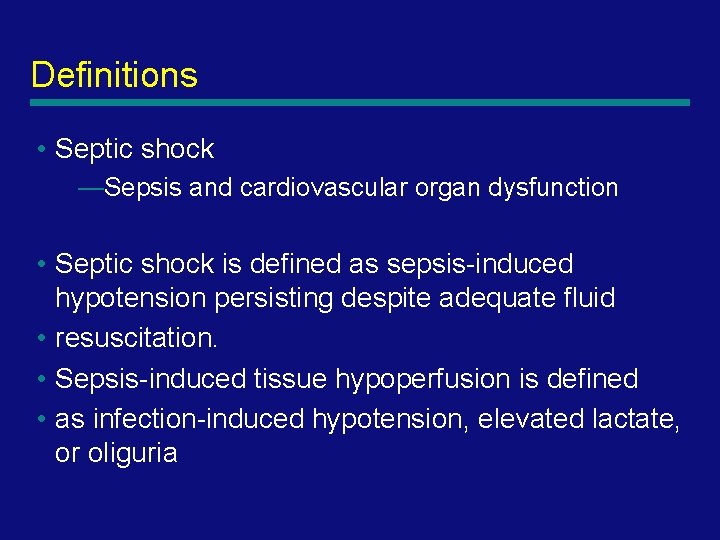
Sepsis: Defining a Disease Continuum Infection/ Trauma SIRS A clinical response arising from a nonspecific insult, including 2 of the following: • • Temperature 38 o. C or 36 o. C HR 90 beats/min Respirations 20/min WBC count 12, 000/mm 3 or 4, 000/mm 3 or >10% immature neutrophils Sepsis Severe Sepsis SIRS with a presumed or confirmed infectious process SIRS = Systemic Inflammatory Response Syndrome Adapted from: Bone RC, et al. Chest 1992; 101: 1644 Opal SM, et al. Crit Care Med 2000; 28: S 81 10
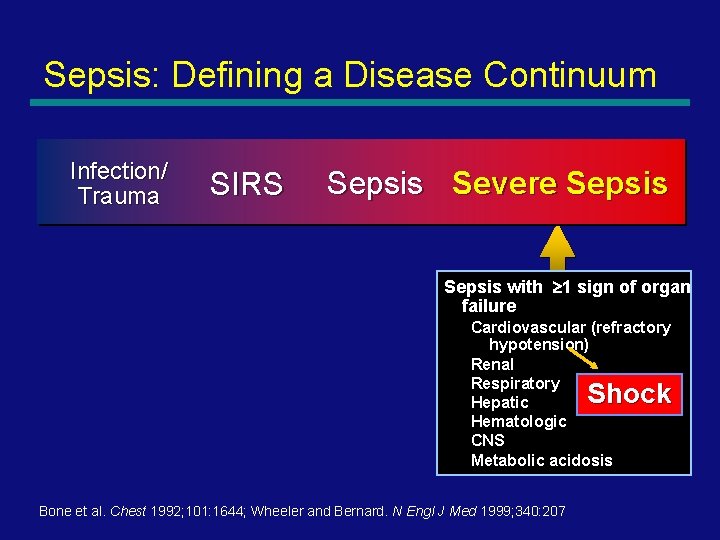
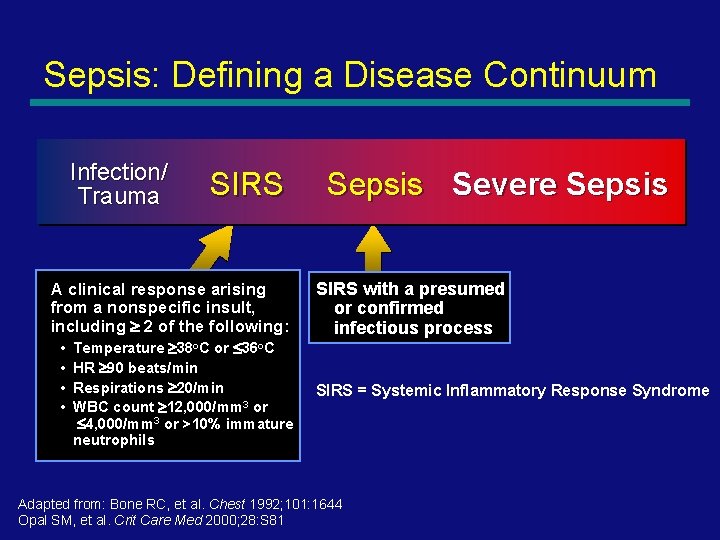
Sepsis: Defining a Disease Continuum Infection/ Trauma SIRS Sepsis Severe Sepsis with 1 sign of organ failure Cardiovascular (refractory hypotension) Renal Respiratory Hepatic Hematologic CNS Metabolic acidosis Shock Bone et al. Chest 1992; 101: 1644; Wheeler and Bernard. N Engl J Med 1999; 340: 207 11
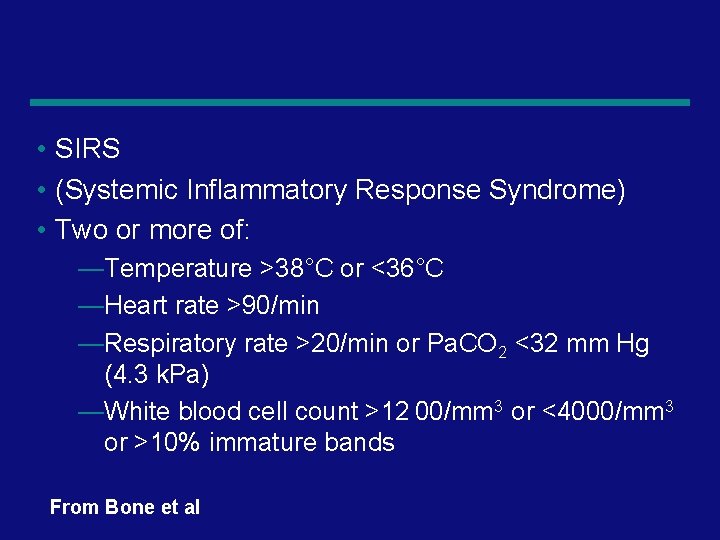
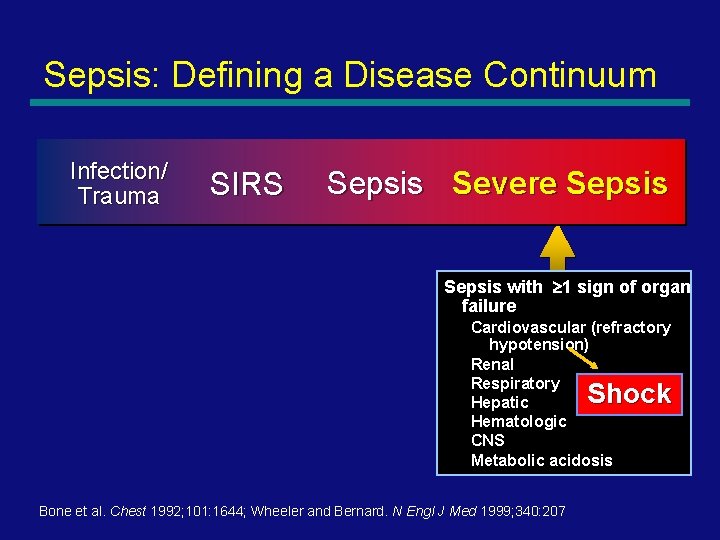
• SIRS • (Systemic Inflammatory Response Syndrome) • Two or more of: —Temperature >38°C or <36°C —Heart rate >90/min —Respiratory rate >20/min or Pa. CO 2 <32 mm Hg (4. 3 k. Pa) —White blood cell count >12 00/mm 3 or <4000/mm 3 or >10% immature bands From Bone et al 12
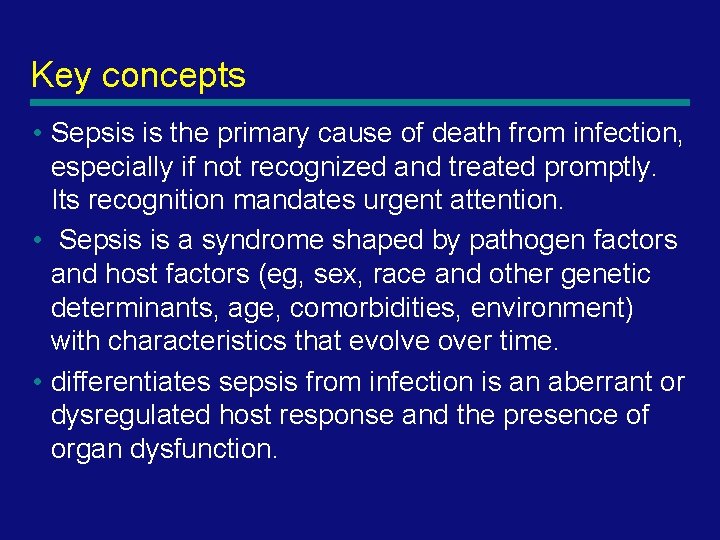
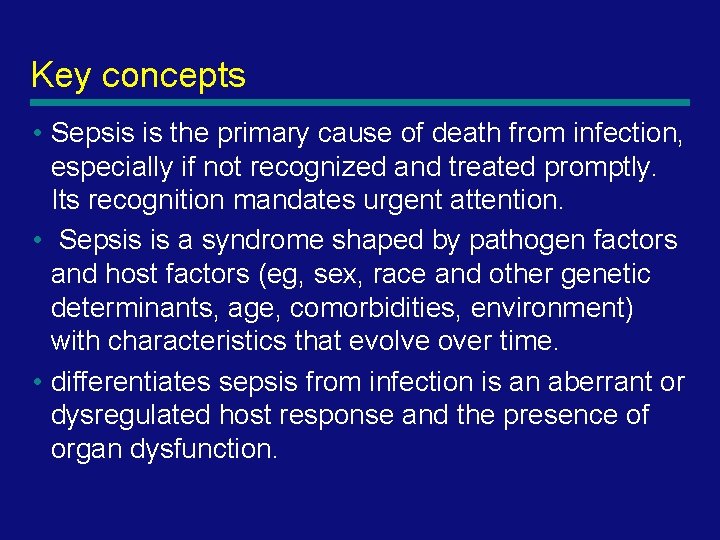
Key concepts • Sepsis is the primary cause of death from infection, especially if not recognized and treated promptly. Its recognition mandates urgent attention. • Sepsis is a syndrome shaped by pathogen factors and host factors (eg, sex, race and other genetic determinants, age, comorbidities, environment) with characteristics that evolve over time. • differentiates sepsis from infection is an aberrant or dysregulated host response and the presence of organ dysfunction. 13
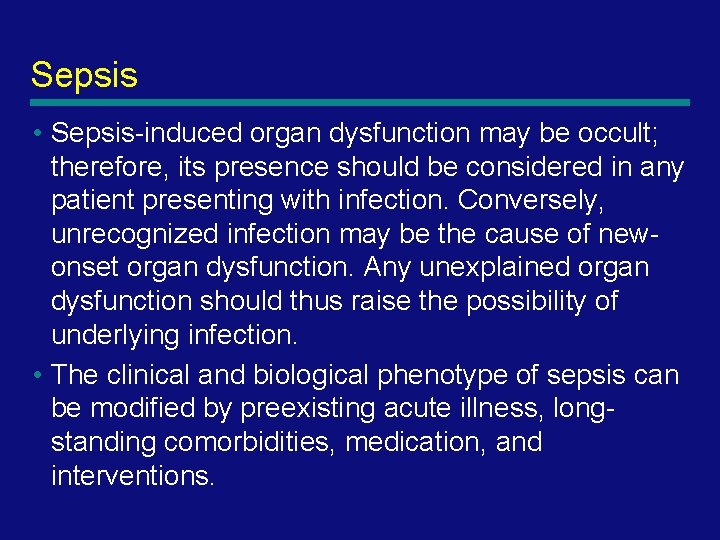
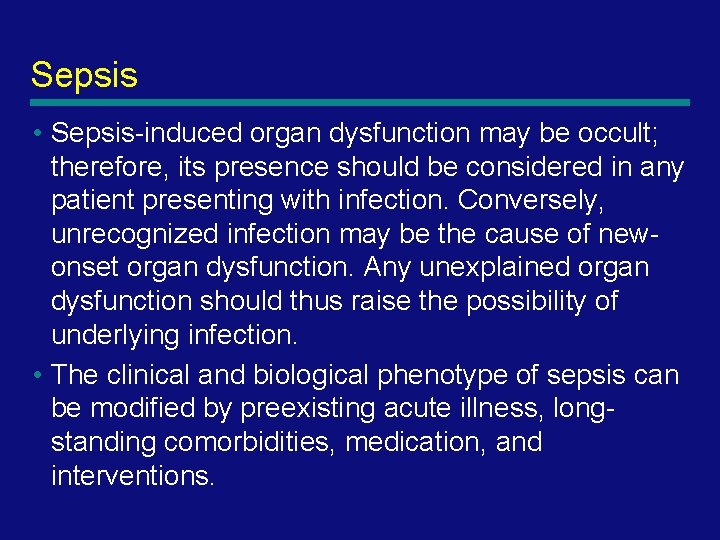
Sepsis • Sepsis-induced organ dysfunction may be occult; therefore, its presence should be considered in any patient presenting with infection. Conversely, unrecognized infection may be the cause of newonset organ dysfunction. Any unexplained organ dysfunction should thus raise the possibility of underlying infection. • The clinical and biological phenotype of sepsis can be modified by preexisting acute illness, longstanding comorbidities, medication, and interventions. 14
Sepsis • Specific infections may result in local organ dysfunction without generating a dysregulated systemic host response. • Severity of organ dysfunction has been assessed with various scoring systems that quantify abnormalities according to clinical findings, laboratory data, or therapeutic interventions 15

The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) Mervyn Singer, MD, FRCP 1; Clifford S. Deutschman, MD, MS 2; Christopher Warren Seymour, MD, MSc 3 JAMA. 2016; 315(8): 801 -810 16
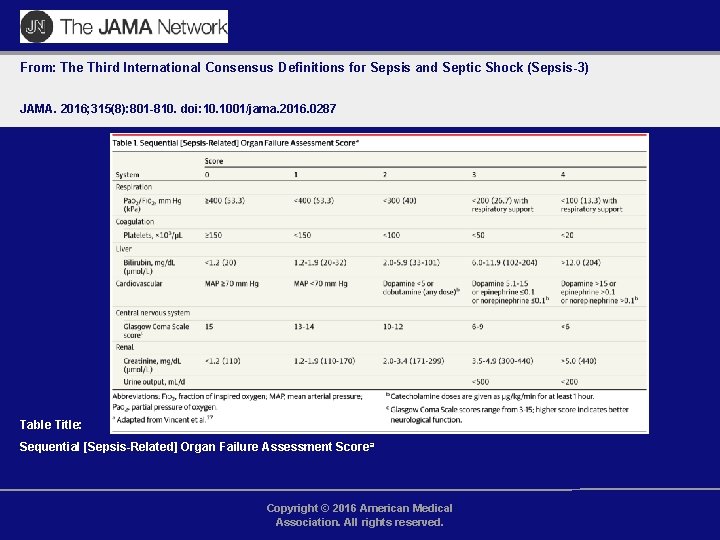
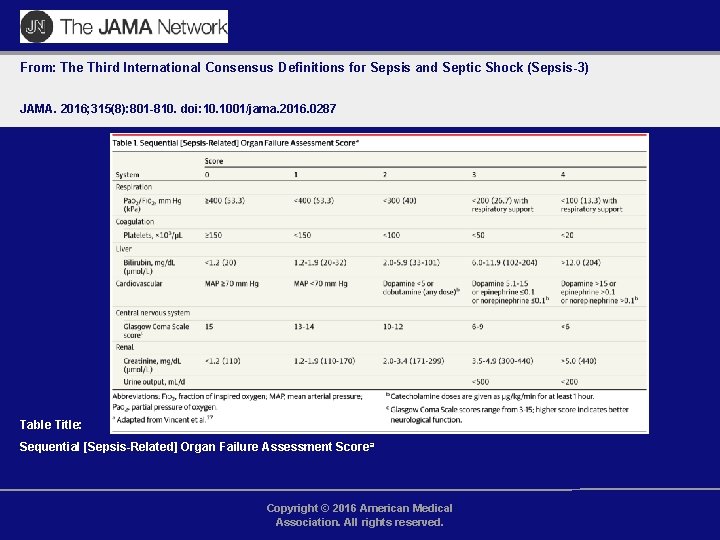
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Table Title: Sequential [Sepsis-Related] Organ Failure Assessment Scorea Copyright © 2016 American Medical Association. All rights reserved.
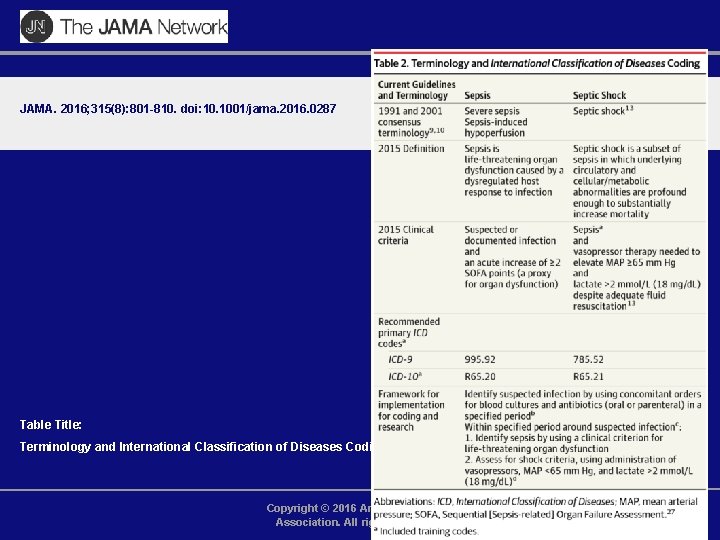
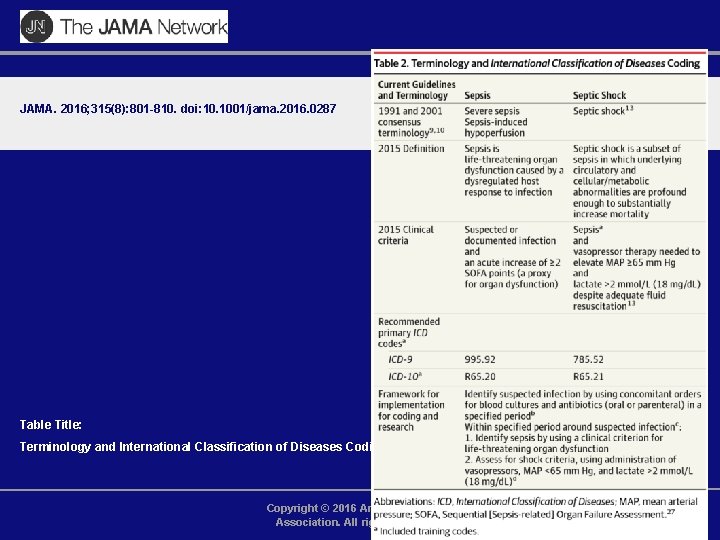
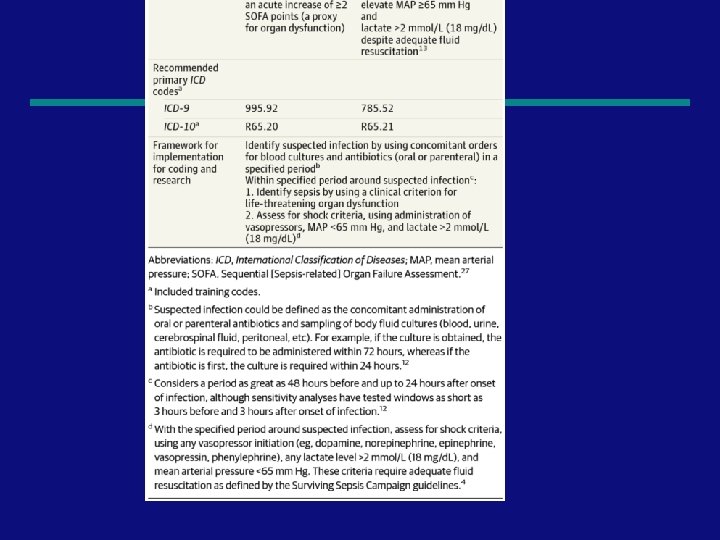
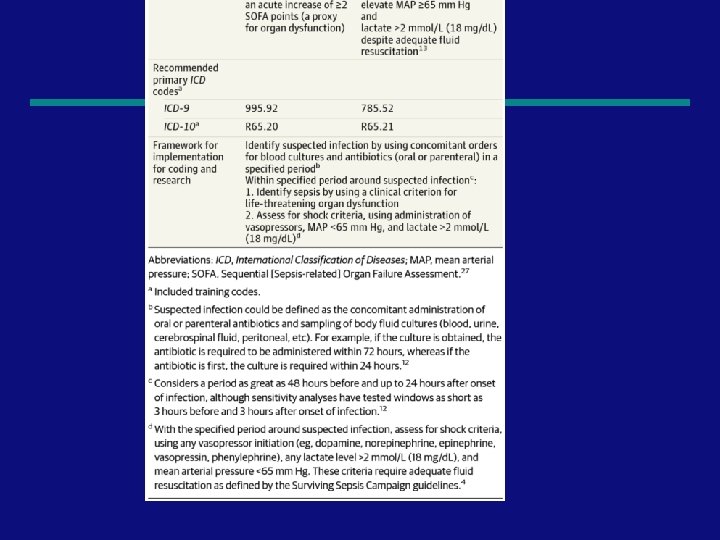
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Table Title: Terminology and International Classification of Diseases Coding Copyright © 2016 American Medical Association. All rights reserved.
19
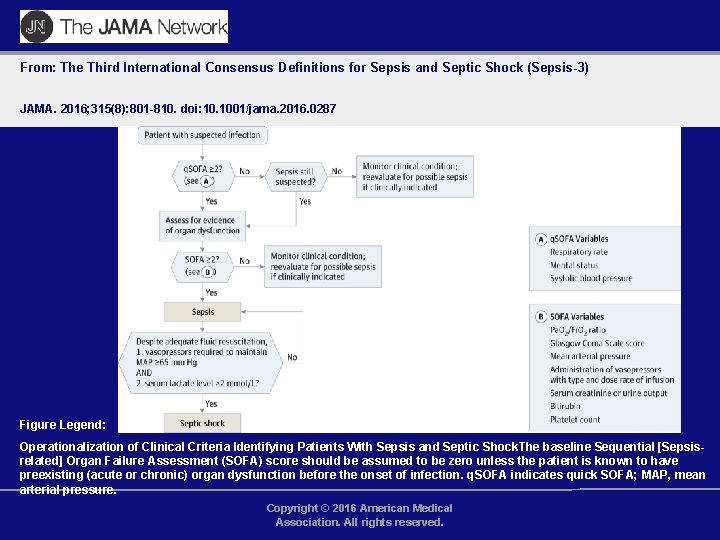
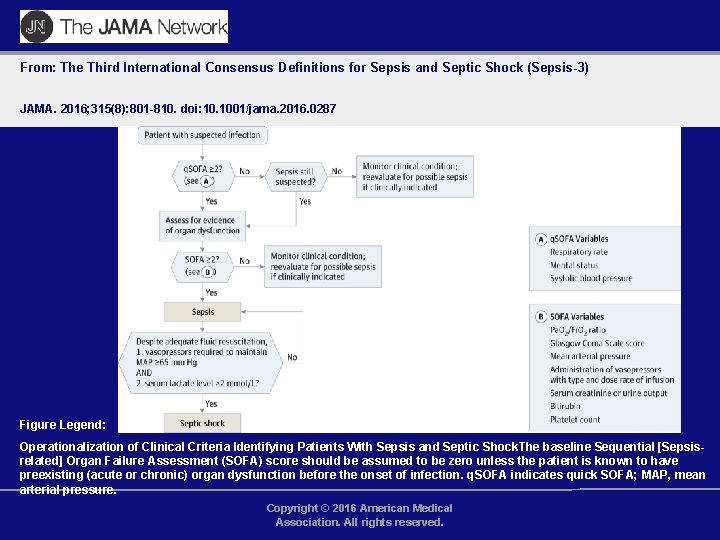
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Figure Legend: Operationalization of Clinical Criteria Identifying Patients With Sepsis and Septic Shock. The baseline Sequential [Sepsisrelated] Organ Failure Assessment (SOFA) score should be assumed to be zero unless the patient is known to have preexisting (acute or chronic) organ dysfunction before the onset of infection. q. SOFA indicates quick SOFA; MAP, mean arterial pressure. Copyright © 2016 American Medical Association. All rights reserved.
21

Relationship Of Infection, SIRS, Sepsis Severe Sepsis and Septic Shock SEPSIS PANCREATITIS SEVERE SEPSIS INFECTION SEPTIC SHOCK SIRS BURNS TRAUMA OTHER 22 Bone et al. Chest 1992; 101: 1644
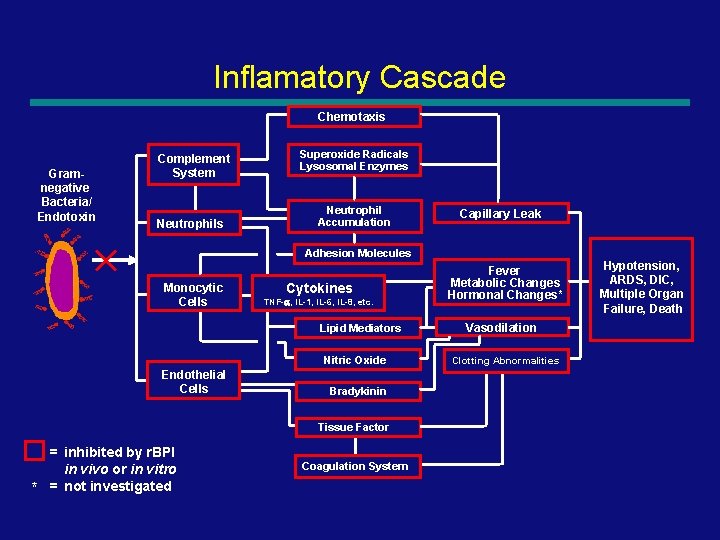
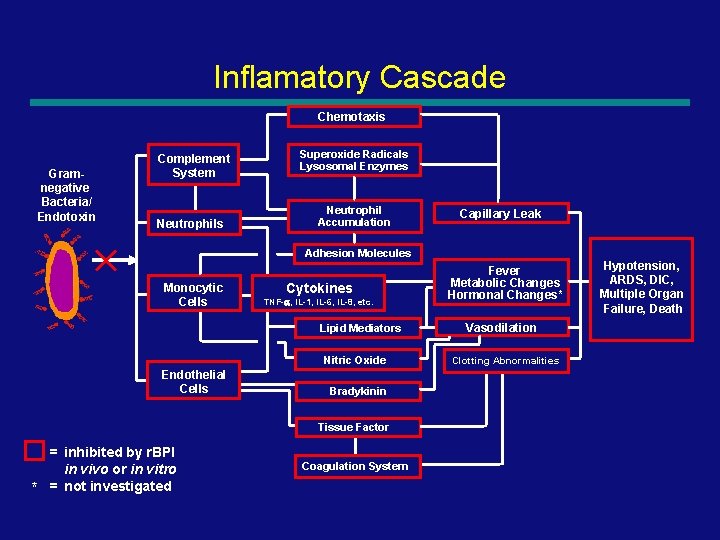
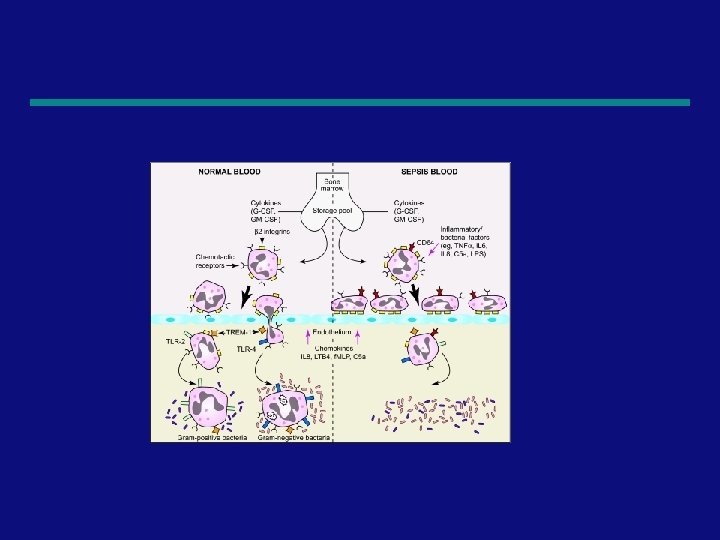
Inflamatory Cascade Chemotaxis Gramnegative Bacteria/ Endotoxin Complement System Neutrophils Superoxide Radicals Lysosomal Enzymes Neutrophil Accumulation Capillary Leak Adhesion Molecules Monocytic Cells Cytokines TNF-a, IL-1, IL-6, IL-8, etc. Lipid Mediators Nitric Oxide Endothelial Cells Fever Metabolic Changes Hormonal Changes* Hypotension, ARDS, DIC, Multiple Organ Failure, Death Vasodilation Clotting Abnormalities Bradykinin Tissue Factor * = inhibited by r. BPI in vivo or in vitro = not investigated Coagulation System 23
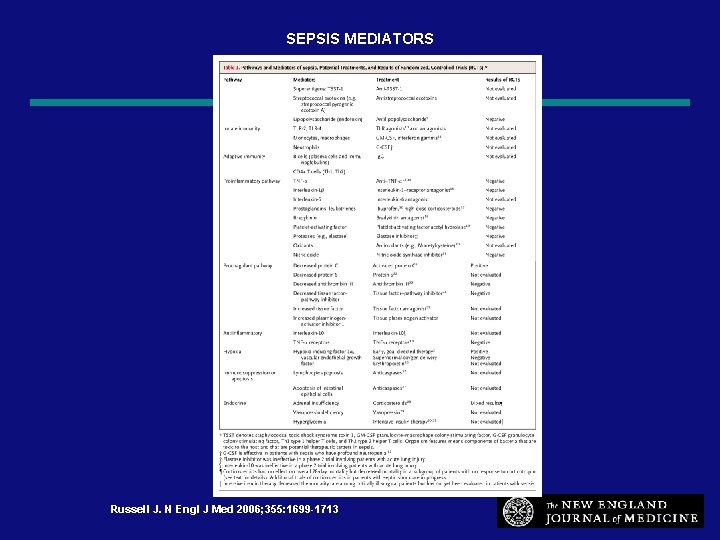
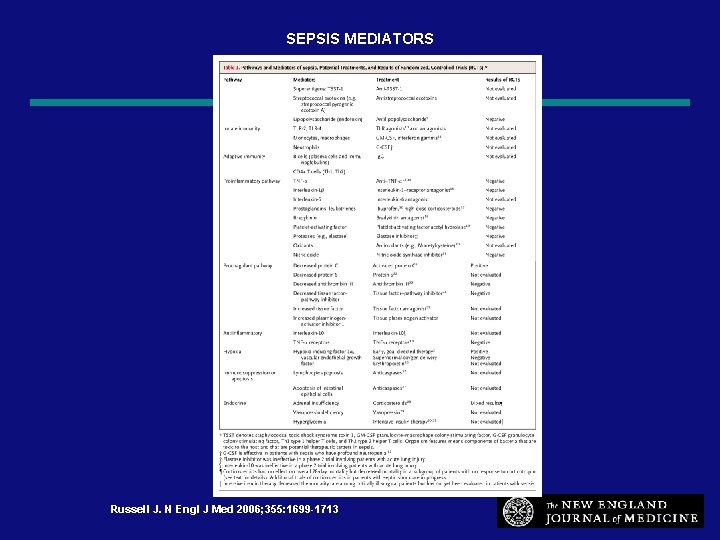
SEPSIS MEDIATORS Russell J. N Engl J Med 2006; 355: 1699 -1713 24
Sepsis ! Septic Shock Severe Sepsis t. Sepsis. T.
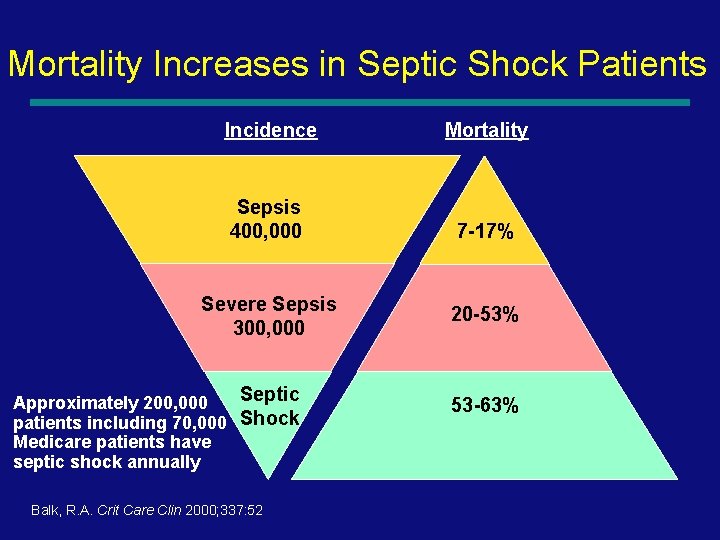
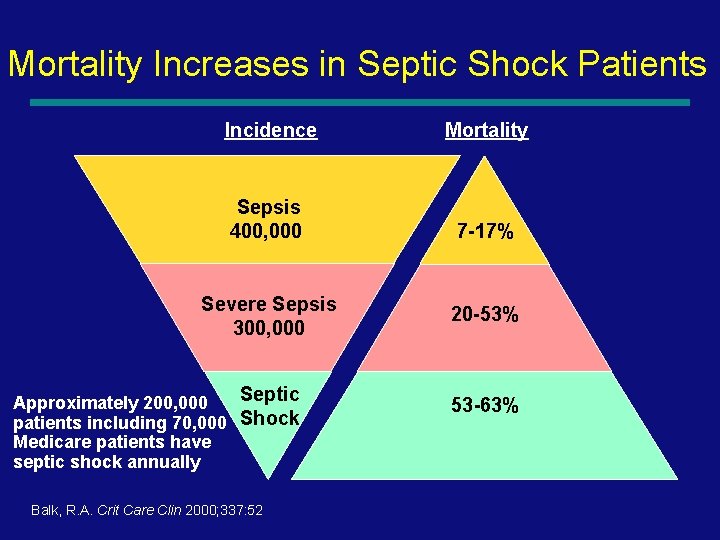
Mortality Increases in Septic Shock Patients Incidence Mortality Sepsis 400, 000 7 -17% Severe Sepsis 300, 000 Approximately 200, 000 Septic patients including 70, 000 Shock Medicare patients have septic shock annually Balk, R. A. Crit Care Clin 2000; 337: 52 20 -53% 53 -63% 26
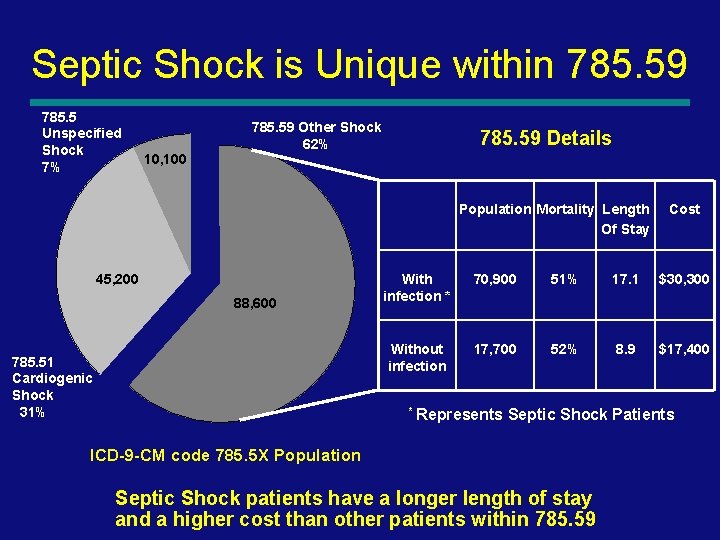
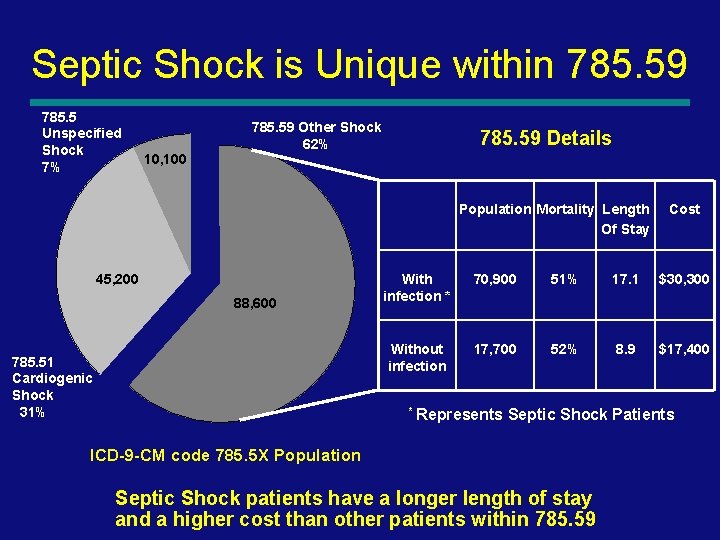
Septic Shock is Unique within 785. 59 785. 5 Unspecified Shock 7% 10, 100 785. 59 Other Shock 62% 785. 59 Details Population Mortality Length Of Stay 45, 200 88, 600 785. 51 Cardiogenic Shock 31% Cost With infection * 70, 900 51% 17. 1 $30, 300 Without infection 17, 700 52% 8. 9 $17, 400 * Represents Septic Shock Patients ICD-9 -CM code 785. 5 X Population Septic Shock patients have a longer length of stay and a higher cost than other patients within 785. 59 27
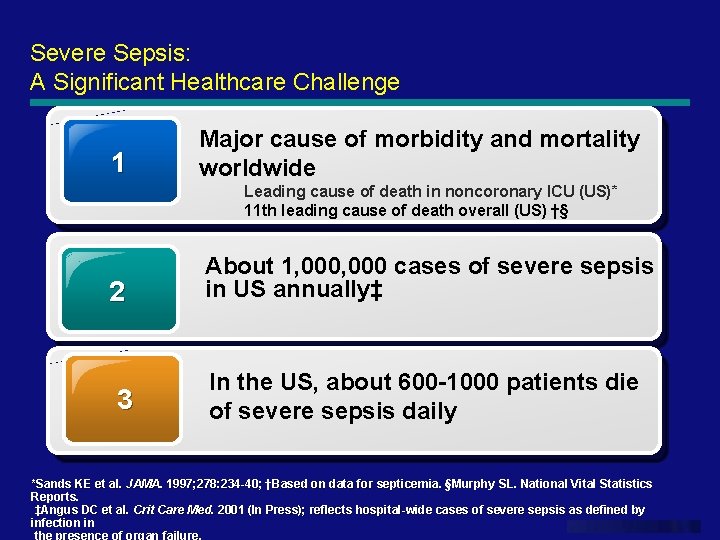
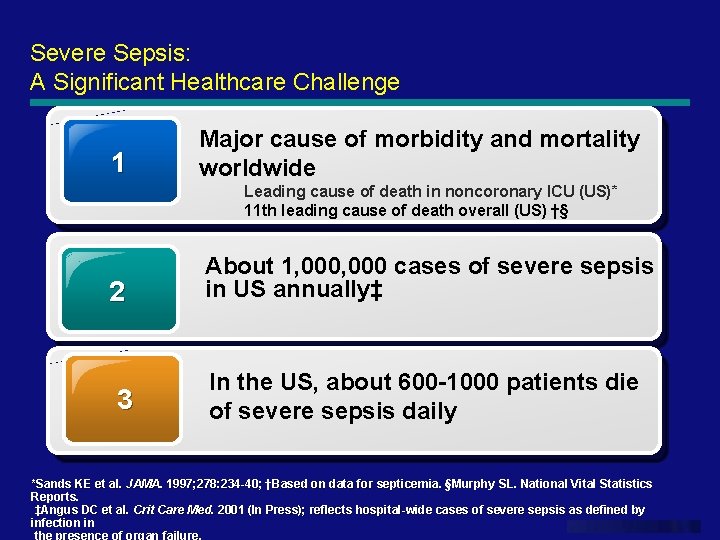
Severe Sepsis: A Significant Healthcare Challenge 1 Major cause of morbidity and mortality worldwide Leading cause of death in noncoronary ICU (US)* 11 th leading cause of death overall (US) †§ 2 3 About 1, 000 cases of severe sepsis in US annually‡ In the US, about 600 -1000 patients die of severe sepsis daily *Sands KE et al. JAMA. 1997; 278: 234 -40; †Based on data for septicemia. §Murphy SL. National Vital Statistics *Sands KE et al. JAMA. 1997; 278: 234 -40; Reports. ‡Angus DC et al. Crit Care Med. 2001 (In Press); reflects hospital-wide cases of severe sepsis as defined by infection in www. themegallery. com the presence of organ failure.
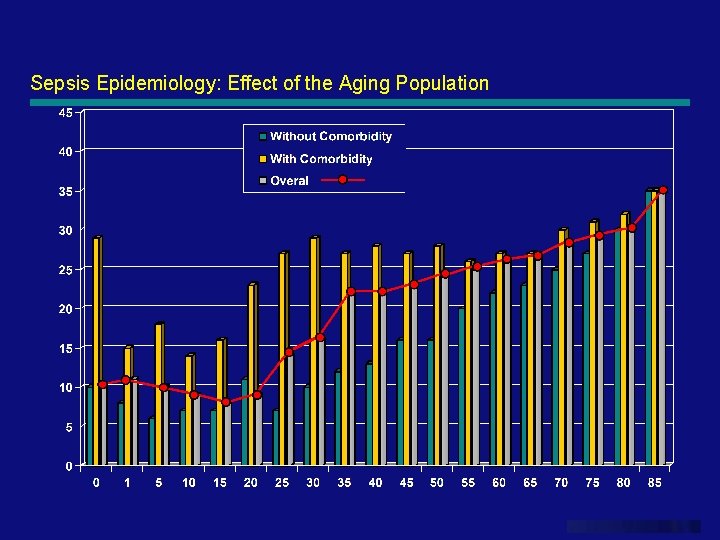
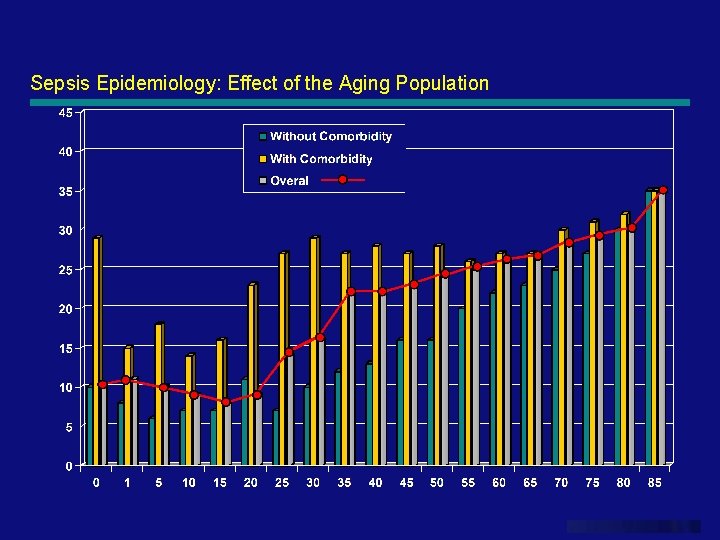
Sepsis Epidemiology: Effect of the Aging Population www. themegallery. com
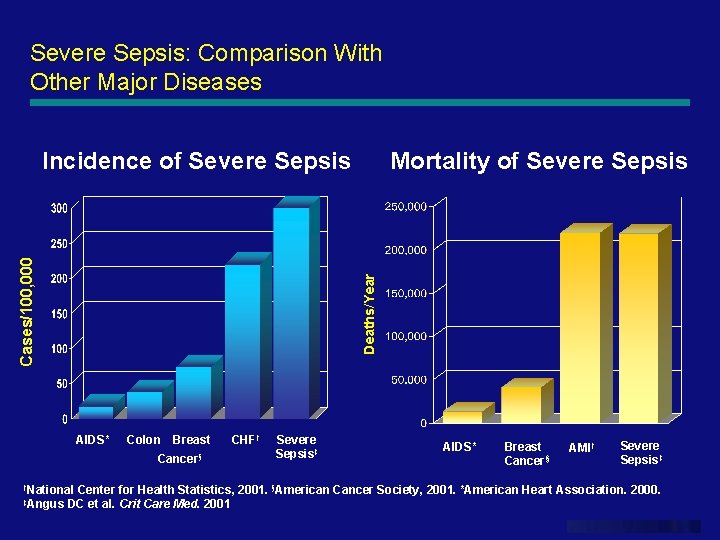
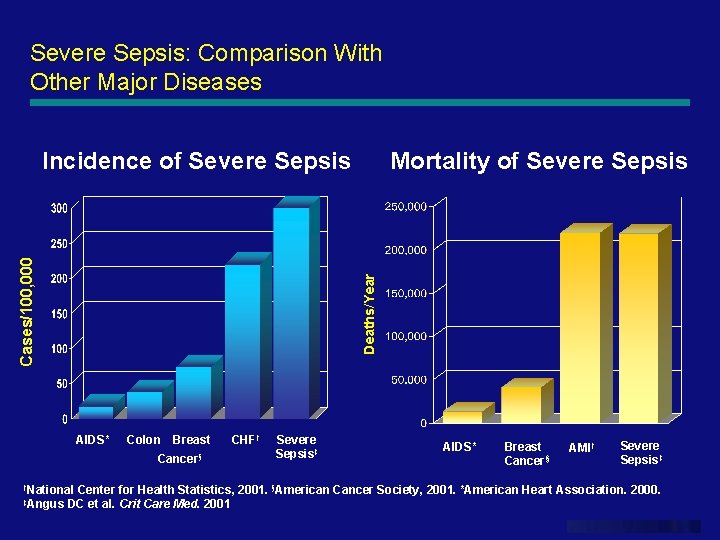
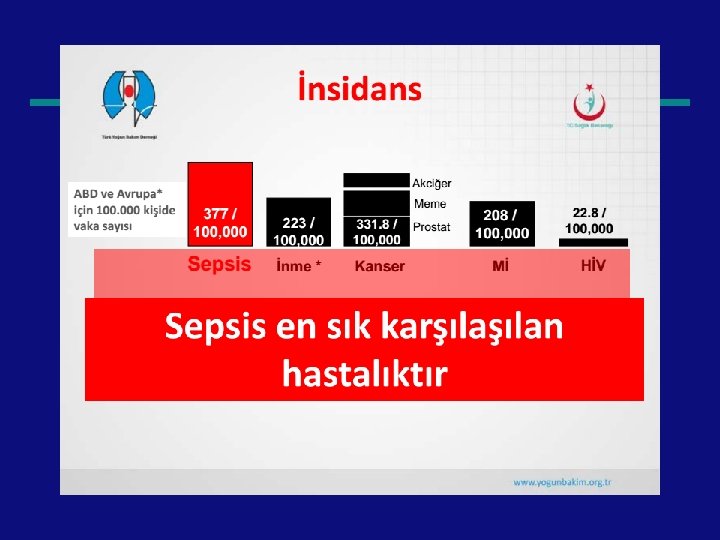
Severe Sepsis: Comparison With Other Major Diseases Mortality of Severe Sepsis Deaths/Year Cases/100, 000 Incidence of Severe Sepsis AIDS* Colon Breast Cancer§ CHF† Severe Sepsis‡ AIDS* Breast Cancer§ AMI† Severe Sepsis‡ †National Center for Health Statistics, 2001. §American Cancer Society, 2001. *American Heart Association. 2000. ‡Angus DC et al. Crit Care Med. 2001 www. themegallery. com
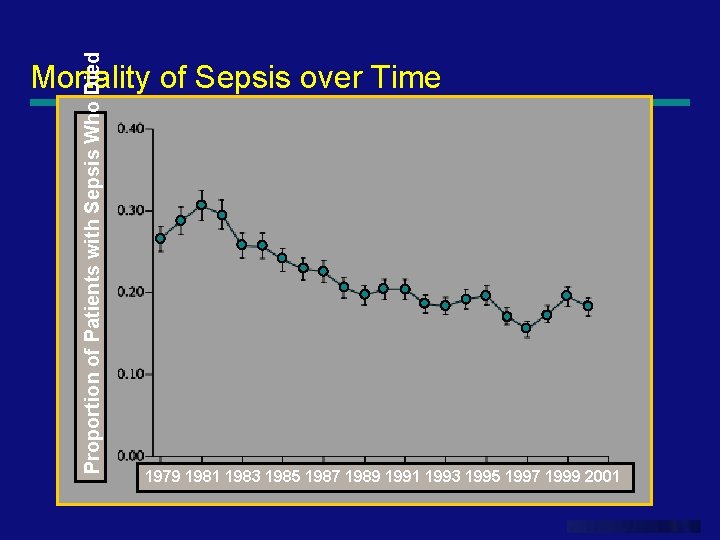
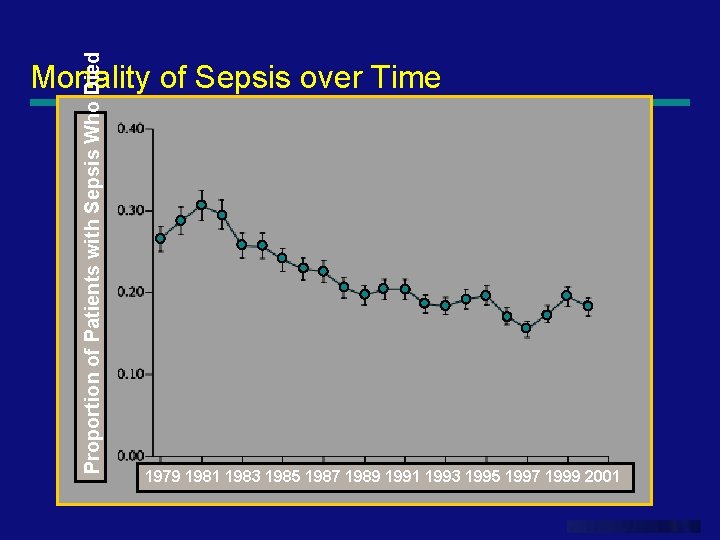
Proportion of Patients with Sepsis Who Died Mortality of Sepsis over Time 1979 1981 1983 1985 1987 1989 1991 1993 1995 1997 1999 2001 www. themegallery. com
![Epidemiology Incidence of Sepsis 1993 2001 a 75 increase in Epidemiology Incidence of Sepsis [1993 -2001]. . . a 75% increase in. . .](https://slidetodoc.com/presentation_image_h/d2c6812addc4372c8f0e71f70ee1b18f/image-32.jpg)
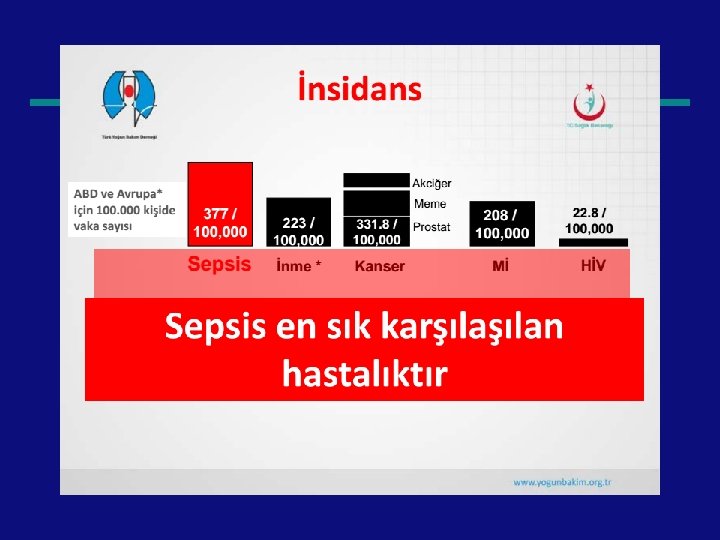
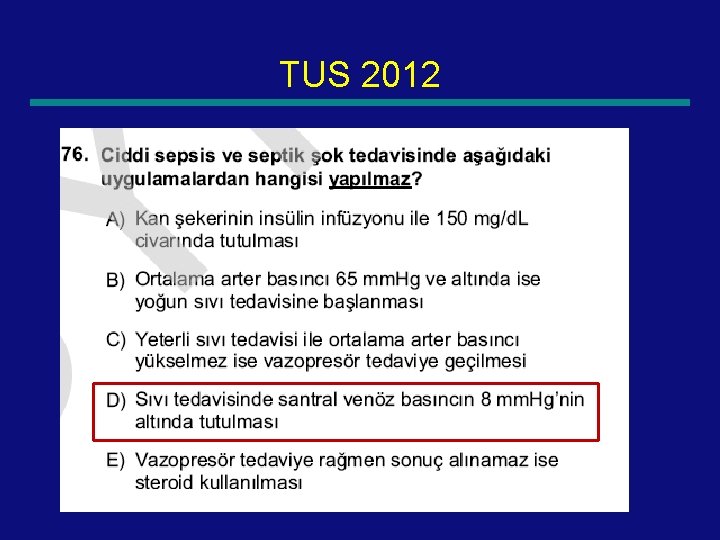
Epidemiology Incidence of Sepsis [1993 -2001]. . . a 75% increase in. . . severe sepsis. . . Mortality of Sepsis [1993 - 2001]. . . a 17% reduction in mortality. Martin, G. S. , Mannino, D. M. , Eaton, S. , & Moss, M. (2003). The epidemiology of sepsis in the United States from 1979 through 2000. New England Journal of Medicine, 348(16), 1546– 1554. Brun-Buisson, C. , Meshaka, P. , Pinton, P. , Vallet, B. , EPISEPSIS Study Group. (2004). EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Medicine, 30(4), 580– 588. Harrison, D. A. , Welch, C. A. , & Eddleston, J. M. (2006). The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996 to 2004: secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Critical Care, 10(2), R 42.
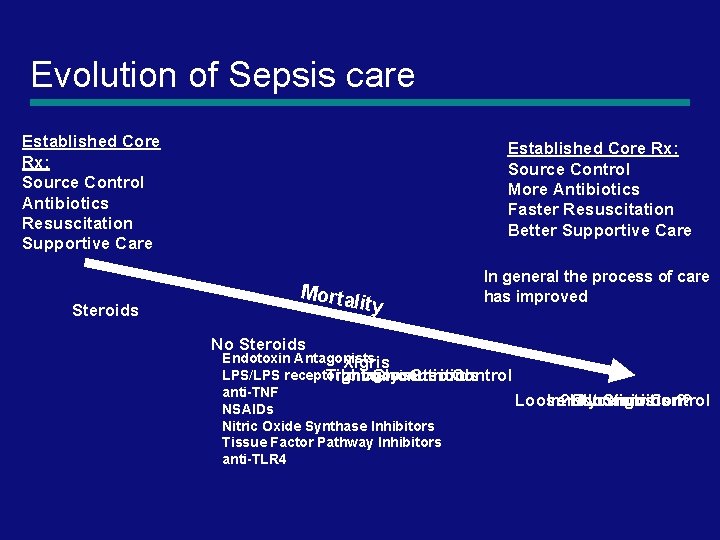
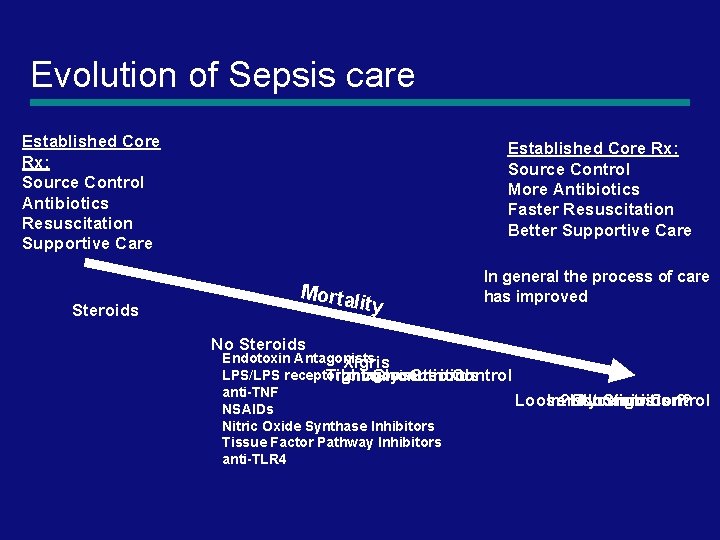
Evolution of Sepsis care Established Core Rx: Source Control Antibiotics Resuscitation Supportive Care Steroids Established Core Rx: Source Control More Antibiotics Faster Resuscitation Better Supportive Care Morta lity No Steroids In general the process of care has improved Endotoxin Antagonists Xigris LPS/LPS receptor antagonist Tight Glycemic Control Immunonutrition Steroids anti-TNF Loose Glycemic Control Immunonutrition? ? Not Steroids ? No Xigris NSAIDs Nitric Oxide Synthase Inhibitors Tissue Factor Pathway Inhibitors anti-TLR 4
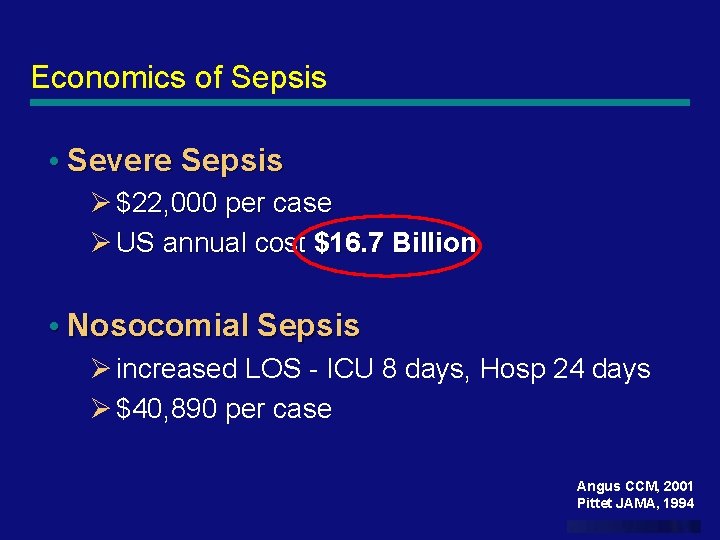
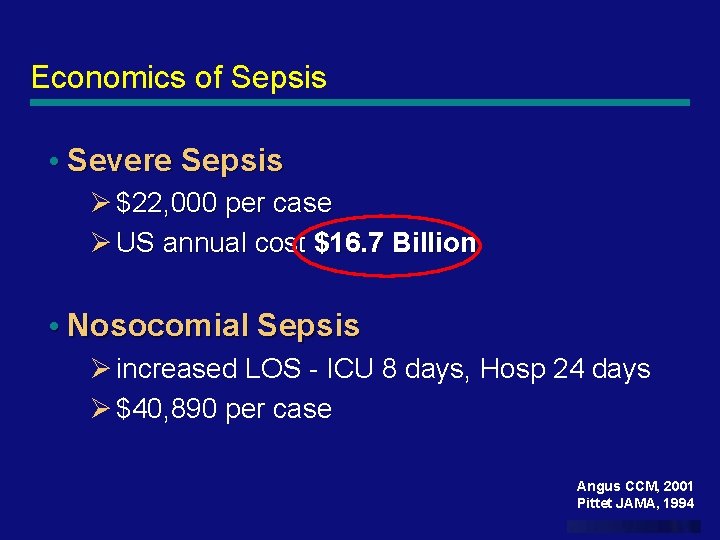
Economics of Sepsis • Severe Sepsis Ø $22, 000 per case Ø US annual cost $16. 7 Billion • Nosocomial Sepsis Ø increased LOS - ICU 8 days, Hosp 24 days Ø $40, 890 per case Angus CCM, 2001 Pittet JAMA, 1994 www. themegallery. com
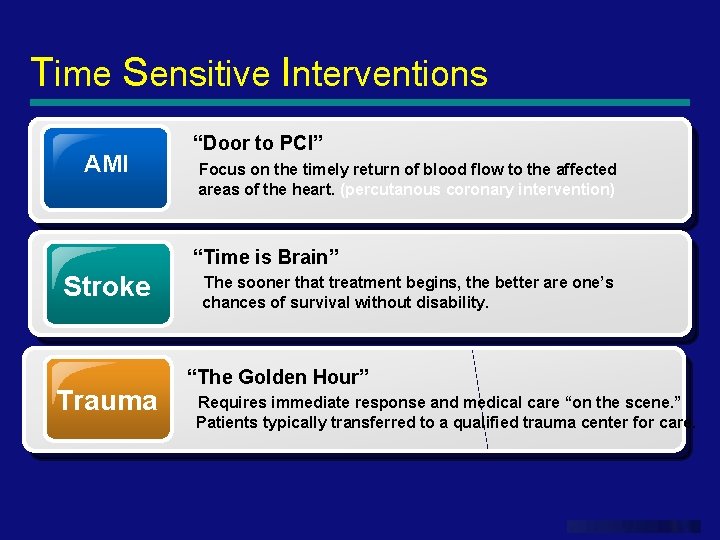
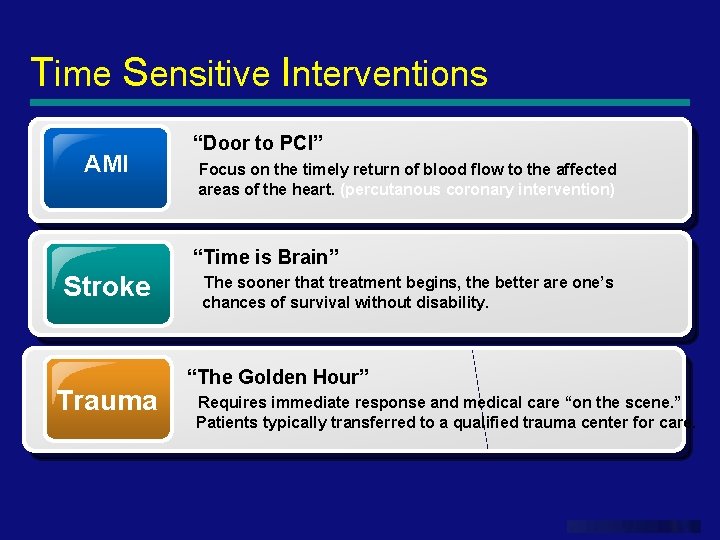
Time Sensitive Interventions AMI “Door to PCI” Focus on the timely return of blood flow to the affected areas of the heart. (percutanous coronary intervention) Stroke Trauma “Time is Brain” The sooner that treatment begins, the better are one’s chances of survival without disability. “The Golden Hour” Requires immediate response and medical care “on the scene. ” Patients typically transferred to a qualified trauma center for care. www. themegallery. com
Trauma vs. Sepsis Patient Care Where we spend our efforts www. themegallery. com
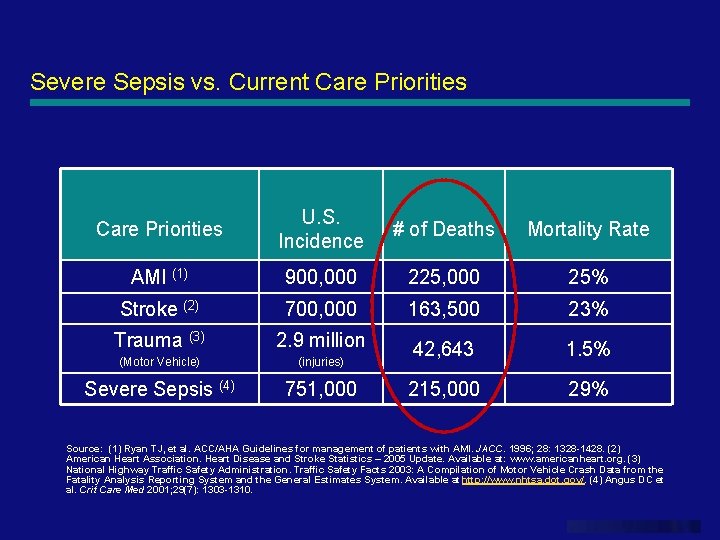
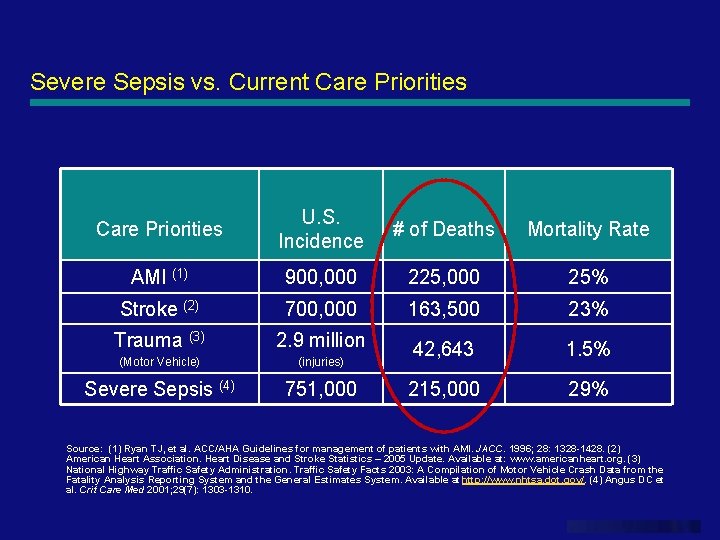
Severe Sepsis vs. Current Care Priorities U. S. Incidence # of Deaths Mortality Rate AMI (1) 900, 000 225, 000 25% Stroke (2) 700, 000 163, 500 23% Trauma (3) 2. 9 million (Motor Vehicle) (injuries) 42, 643 1. 5% Severe Sepsis (4) 751, 000 215, 000 29% Source: (1) Ryan TJ, et al. ACC/AHA Guidelines for management of patients with AMI. JACC. 1996; 28: 1328 -1428. (2) American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. Available at: www. americanheart. org. (3) National Highway Traffic Safety Administration. Traffic Safety Facts 2003: A Compilation of Motor Vehicle Crash Data from the Fatality Analysis Reporting System and the General Estimates System. Available at http: //www. nhtsa. dot. gov/. (4) Angus DC et al. Crit Care Med 2001; 29(7): 1303 -1310. www. themegallery. com
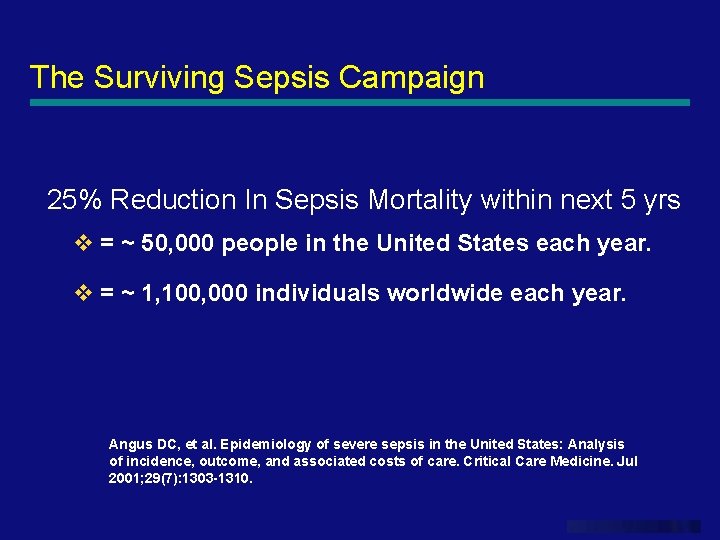
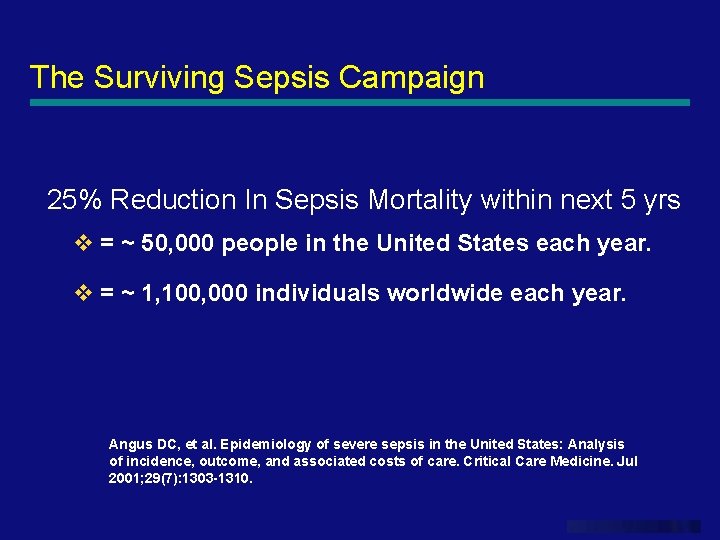
The Surviving Sepsis Campaign 25% Reduction In Sepsis Mortality within next 5 yrs v = ~ 50, 000 people in the United States each year. v = ~ 1, 100, 000 individuals worldwide each year. Angus DC, et al. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Critical Care Medicine. Jul 2001; 29(7): 1303 -1310. www. themegallery. com

Cardiovascular Dysfunction • Despite administration of isotonic intravenous fluid • bolus ≥ 40 m. L/kg in 1 hr — Hypotension: BP <5 th % or <2 sd OR — Need for vasoactive drug to maintain BP (dopamine >5 mcg/kg/min or dob, epi, or norepi at any dose) OR — Two of the following § § § Unexplained metabolic acidosis: Base deficit >5. 0 m. Eq/L Arterial lactate: >2 times upper limit of normal Oliguria: Urine output <0. 5 m. L/kg/hr Capillary refill: >5 secs Core to peripheral temperature gap >3°C 39
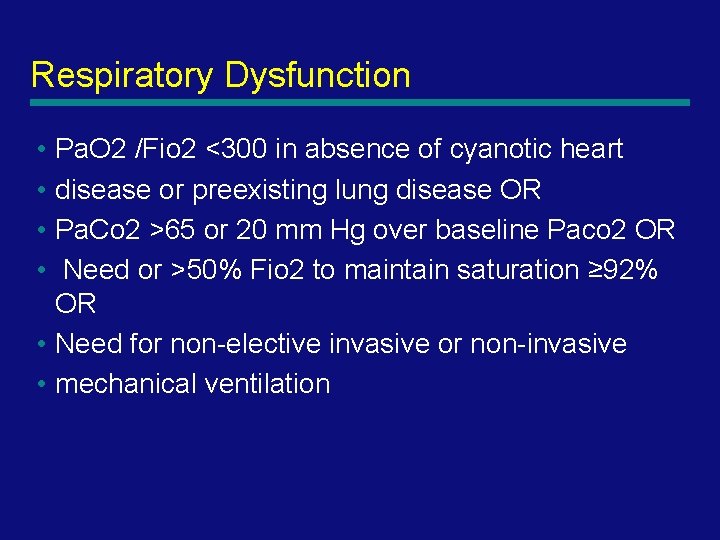
Respiratory Dysfunction • Pa. O 2 /Fio 2 <300 in absence of cyanotic heart • disease or preexisting lung disease OR • Pa. Co 2 >65 or 20 mm Hg over baseline Paco 2 OR • Need or >50% Fio 2 to maintain saturation ≥ 92% OR • Need for non-elective invasive or non-invasive • mechanical ventilation 40
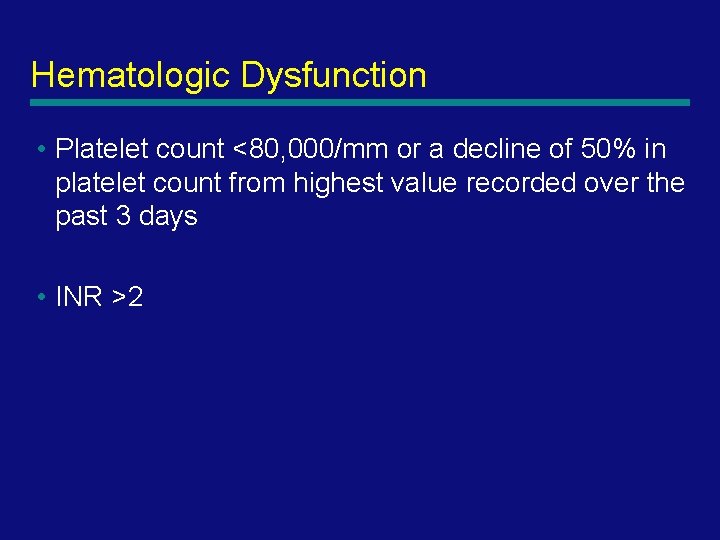
Neurologic Dysfunction • Glasgow Coma Score ≤ 11 OR • Acute change in mental status with a decrease in Glasgow Coma Score ≥ 3 points from abnormal baseline 41
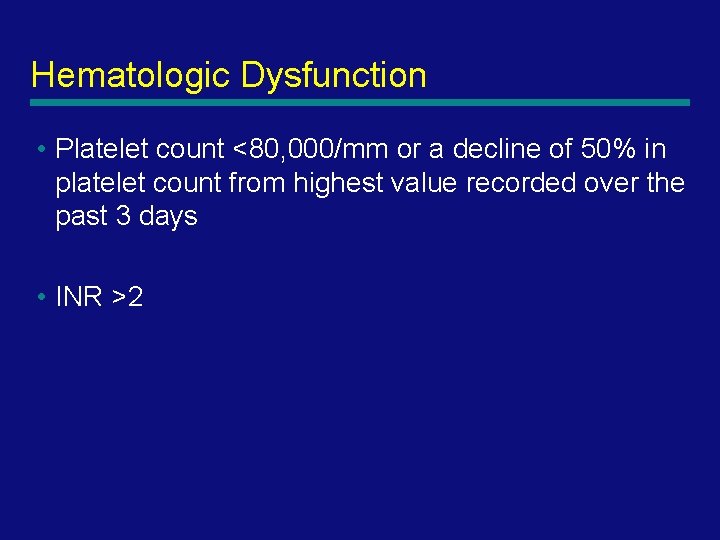
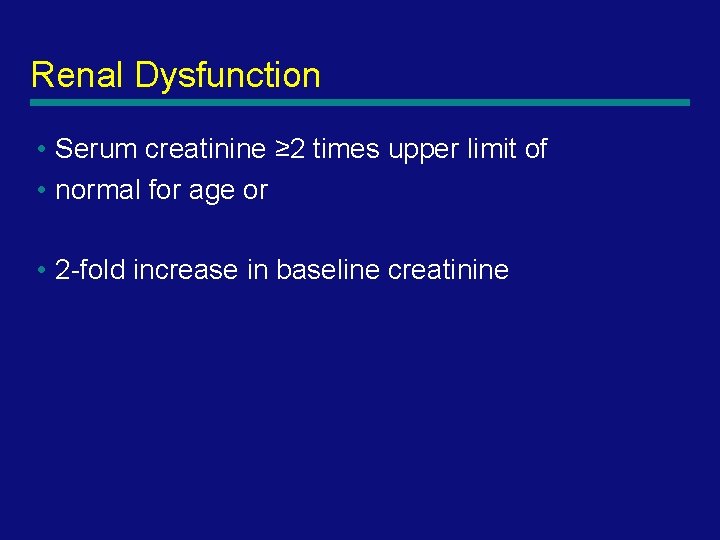
Hematologic Dysfunction • Platelet count <80, 000/mm or a decline of 50% in platelet count from highest value recorded over the past 3 days • INR >2 42
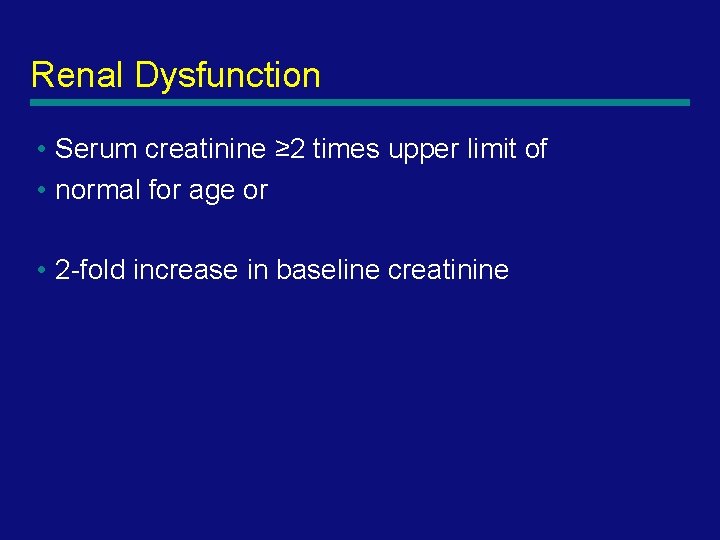
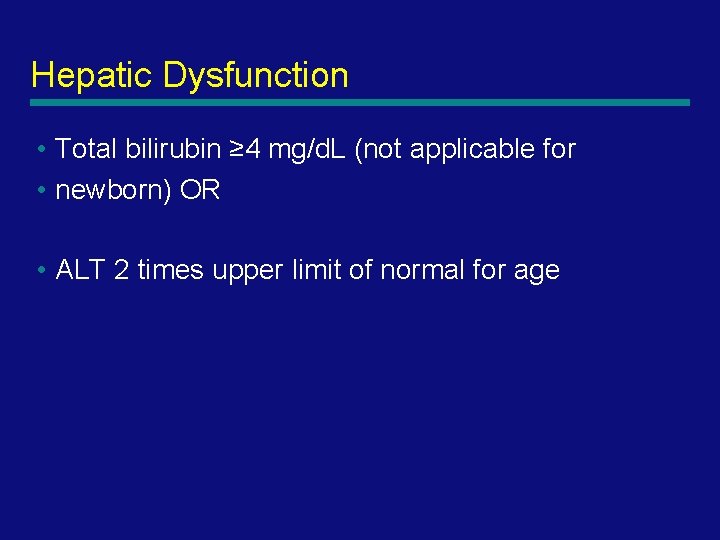
Renal Dysfunction • Serum creatinine ≥ 2 times upper limit of • normal for age or • 2 -fold increase in baseline creatinine 43
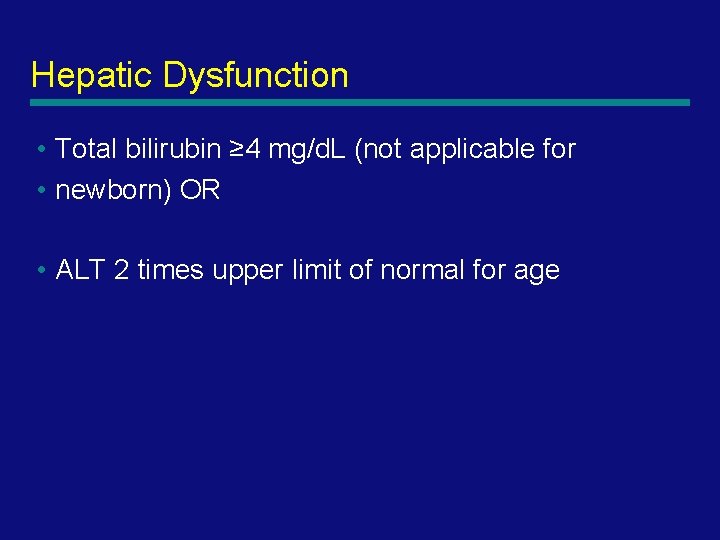
Hepatic Dysfunction • Total bilirubin ≥ 4 mg/d. L (not applicable for • newborn) OR • ALT 2 times upper limit of normal for age 44
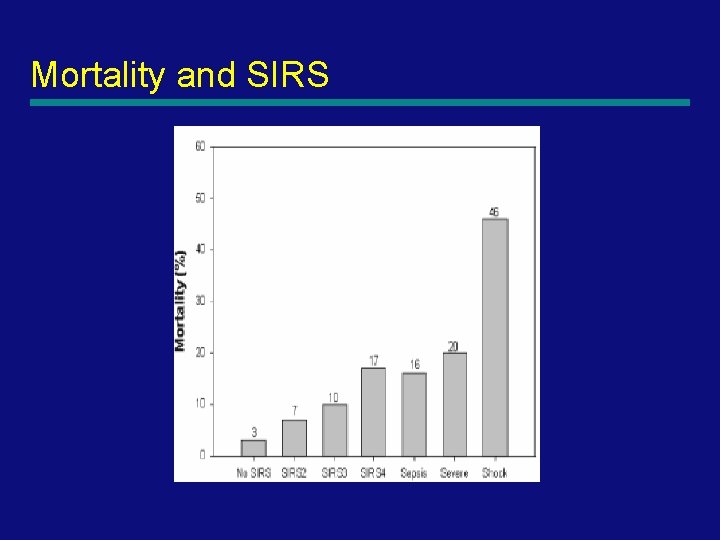
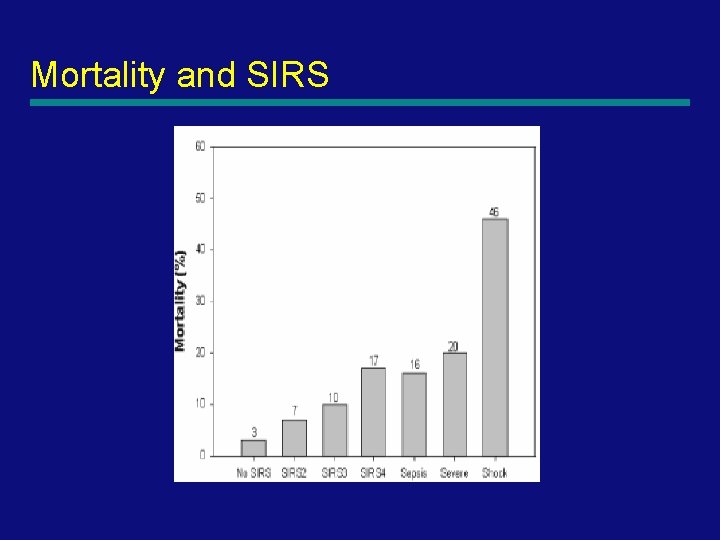
Mortality and SIRS 45
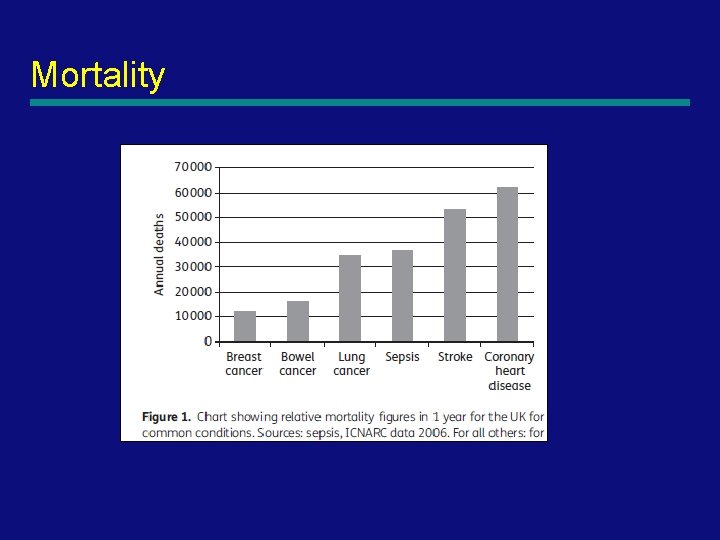
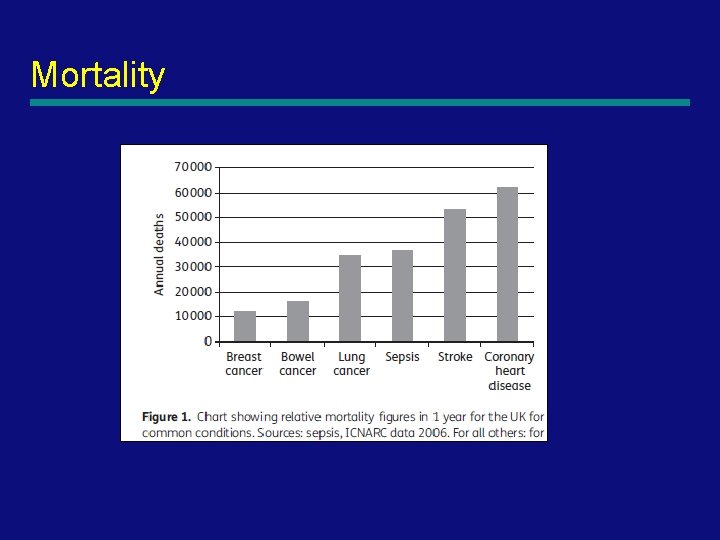
Mortality
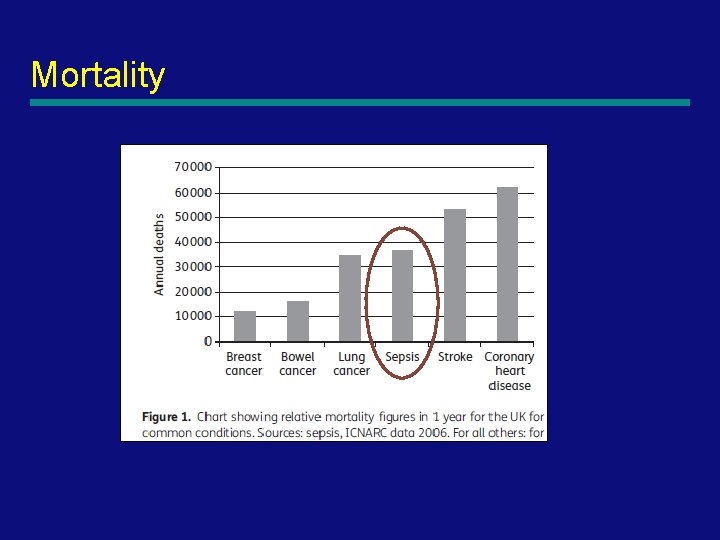
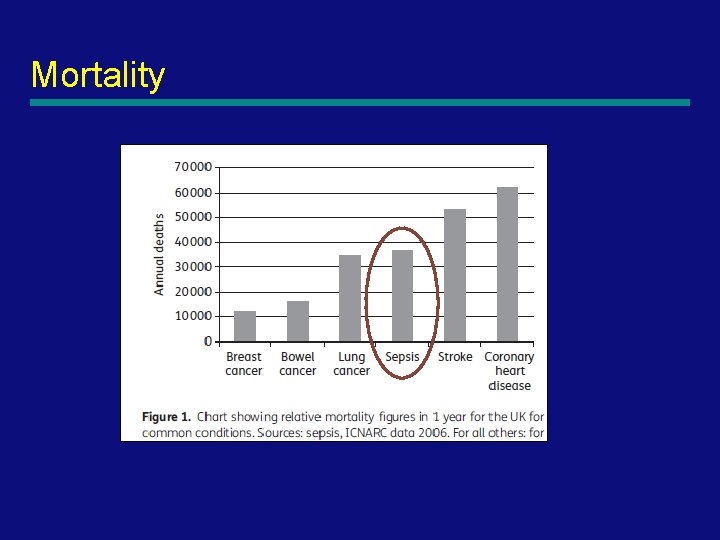
Mortality
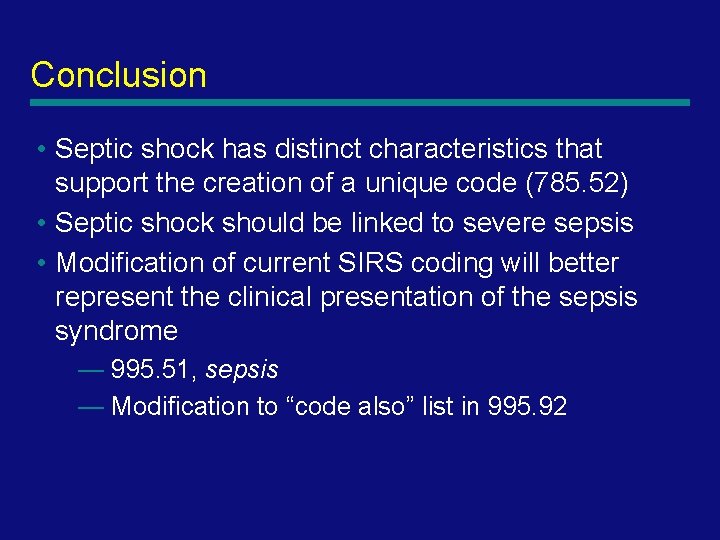
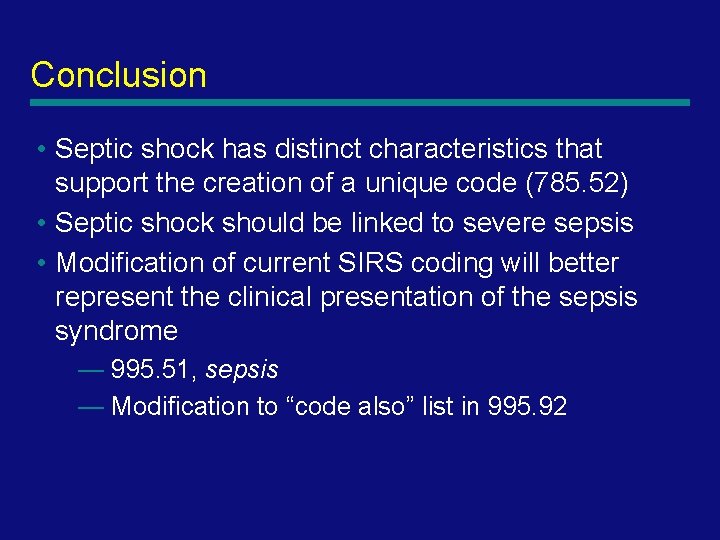
Conclusion • Septic shock has distinct characteristics that support the creation of a unique code (785. 52) • Septic shock should be linked to severe sepsis • Modification of current SIRS coding will better represent the clinical presentation of the sepsis syndrome — 995. 51, sepsis — Modification to “code also” list in 995. 92 48
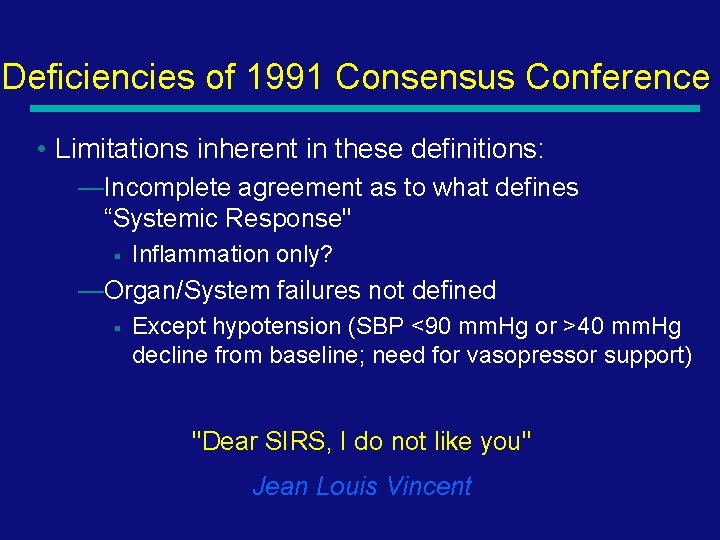
Deficiencies of 1991 Consensus Conference • Limitations inherent in these definitions: —Incomplete agreement as to what defines “Systemic Response" § Inflammation only? —Organ/System failures not defined § Except hypotension (SBP <90 mm. Hg or >40 mm. Hg decline from baseline; need for vasopressor support) "Dear SIRS, I do not like you" Jean Louis Vincent
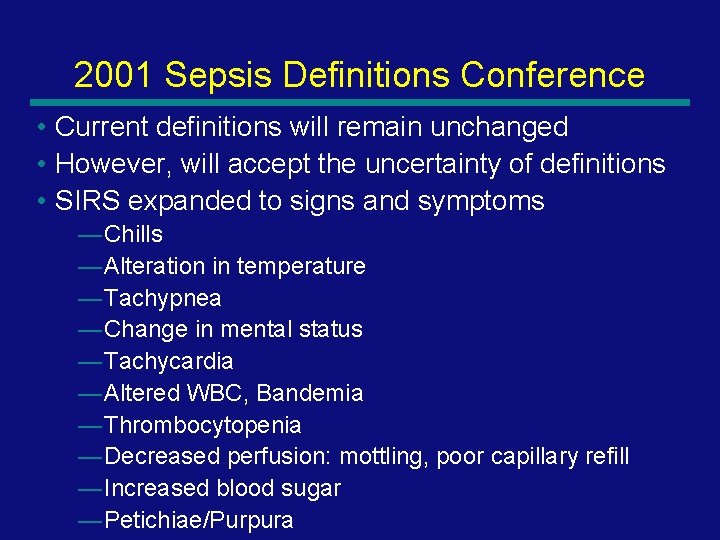
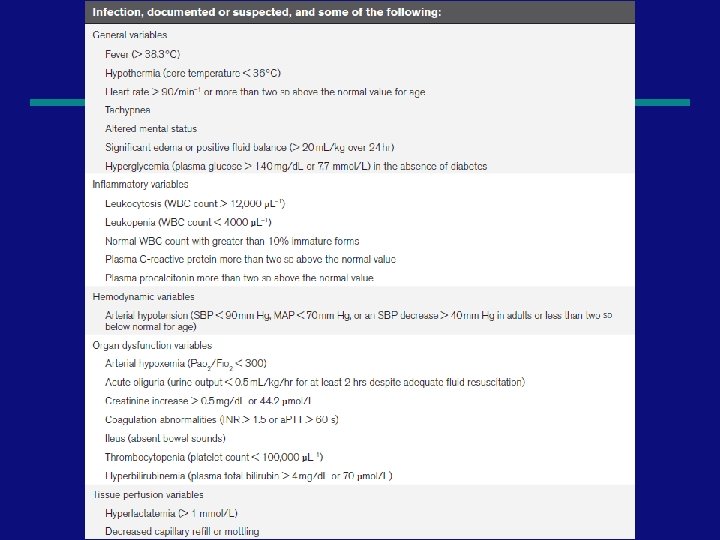
2001 Sepsis Definitions Conference • Current definitions will remain unchanged • However, will accept the uncertainty of definitions • SIRS expanded to signs and symptoms — Chills — Alteration in temperature — Tachypnea — Change in mental status — Tachycardia — Altered WBC, Bandemia — Thrombocytopenia — Decreased perfusion: mottling, poor capillary refill — Increased blood sugar — Petichiae/Purpura 50
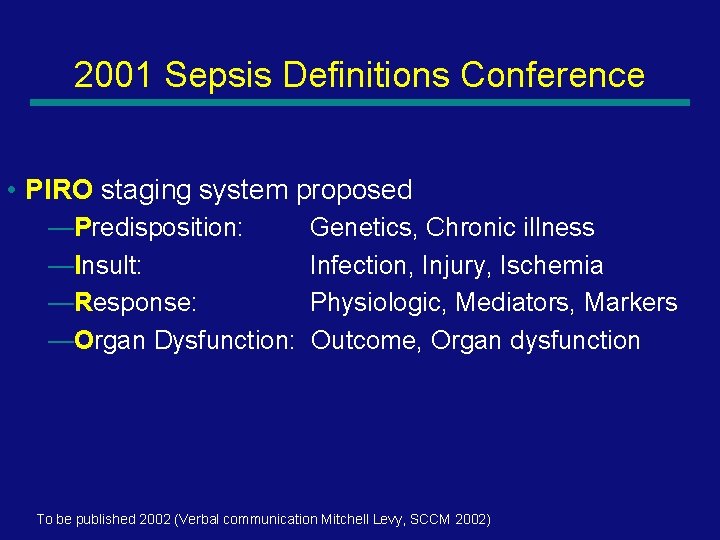
2001 Sepsis Definitions Conference • PIRO staging system proposed —Predisposition: Genetics, Chronic illness —Insult: Infection, Injury, Ischemia —Response: Physiologic, Mediators, Markers —Organ Dysfunction: Outcome, Organ dysfunction To be published 2002 (Verbal communication Mitchell Levy, SCCM 2002) 51
52
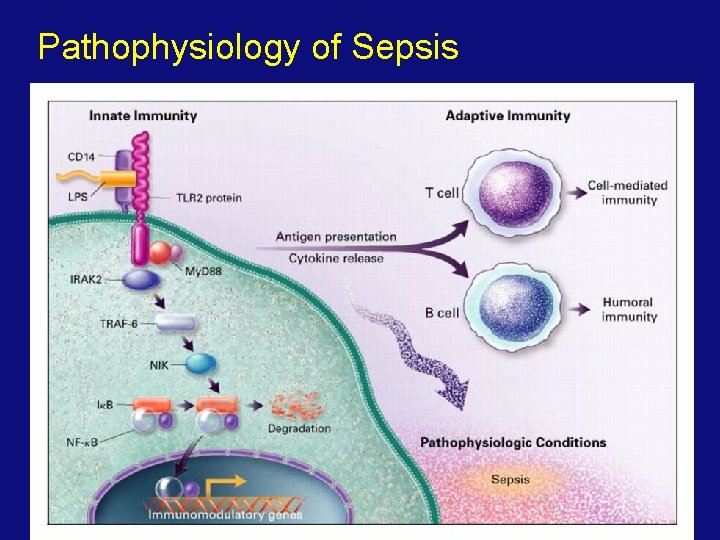
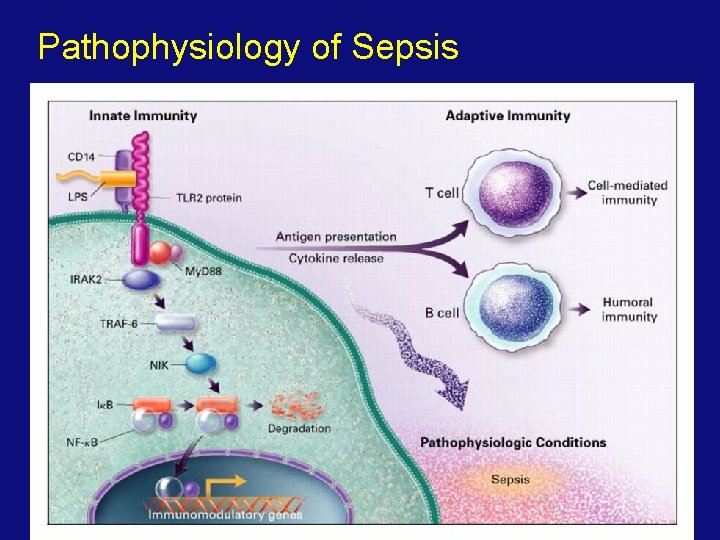
Pathophysiology of Sepsis
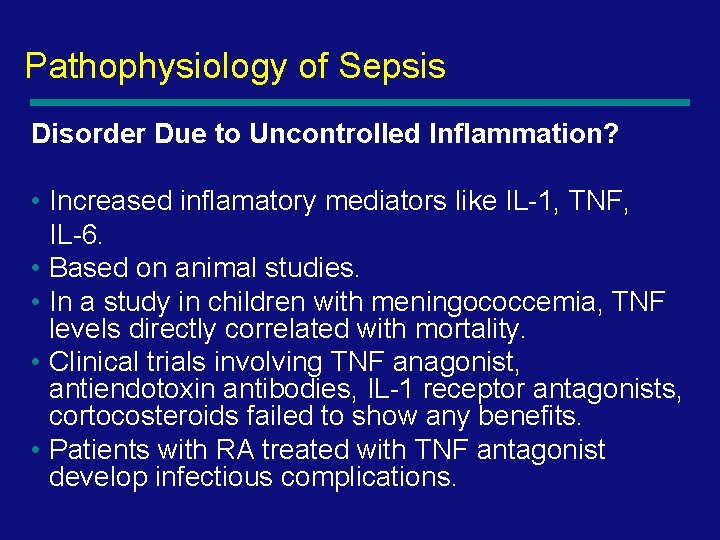
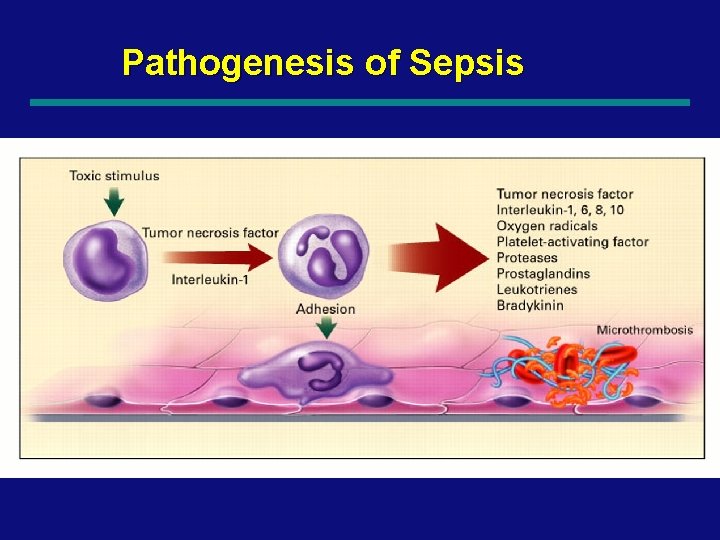
Pathophysiology of Sepsis Disorder Due to Uncontrolled Inflammation? • Increased inflamatory mediators like IL-1, TNF, IL-6. • Based on animal studies. • In a study in children with meningococcemia, TNF levels directly correlated with mortality. • Clinical trials involving TNF anagonist, antiendotoxin antibodies, IL-1 receptor antagonists, cortocosteroids failed to show any benefits. • Patients with RA treated with TNF antagonist develop infectious complications.

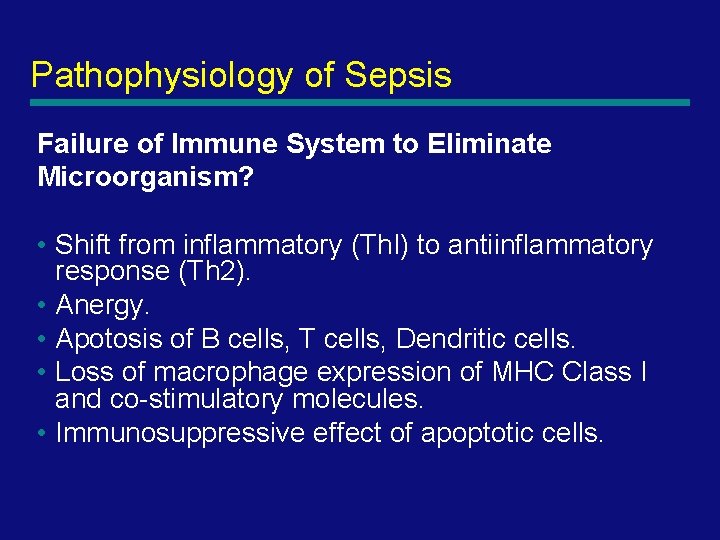
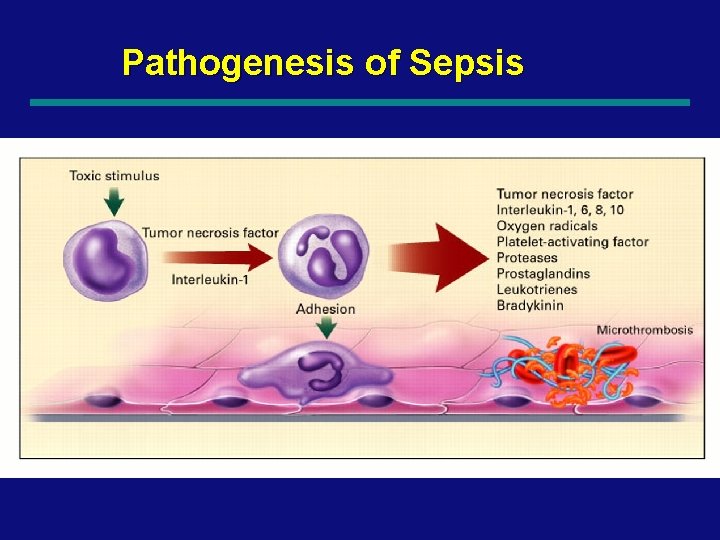
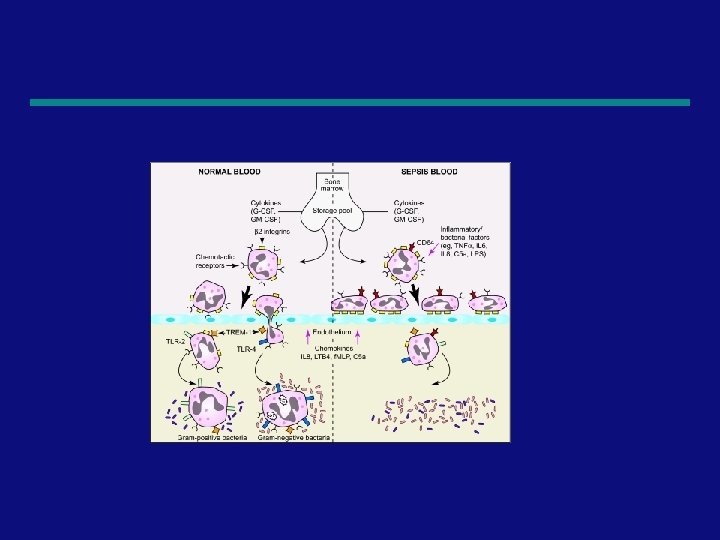
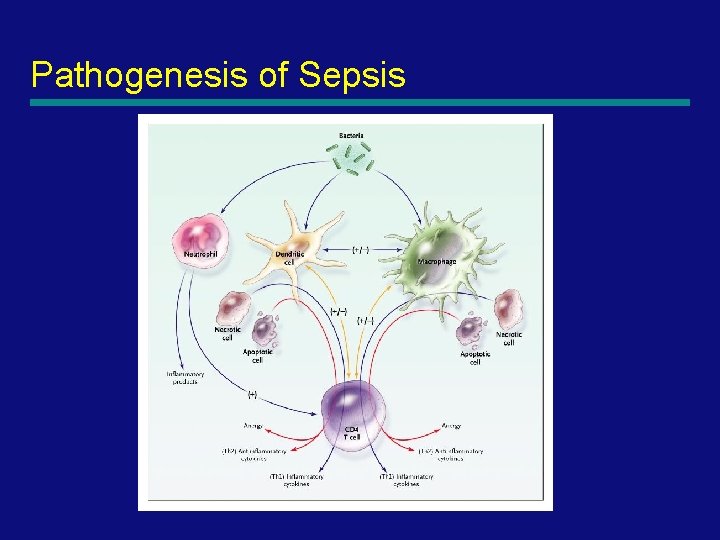
Pathogenesis of Sepsis
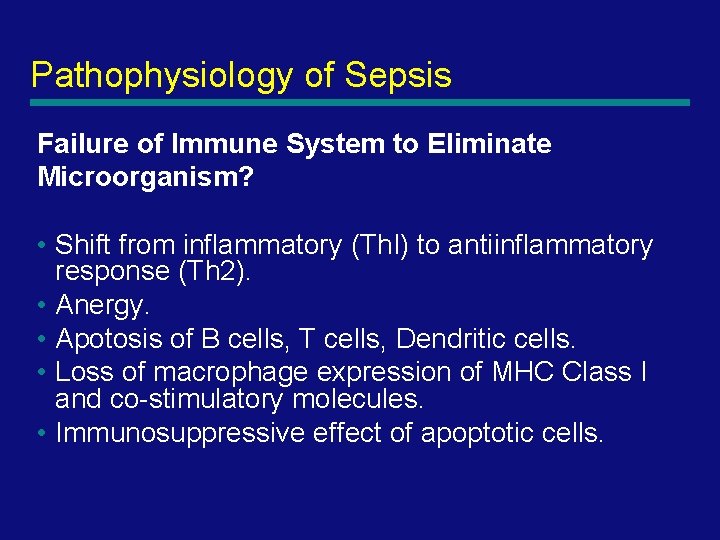
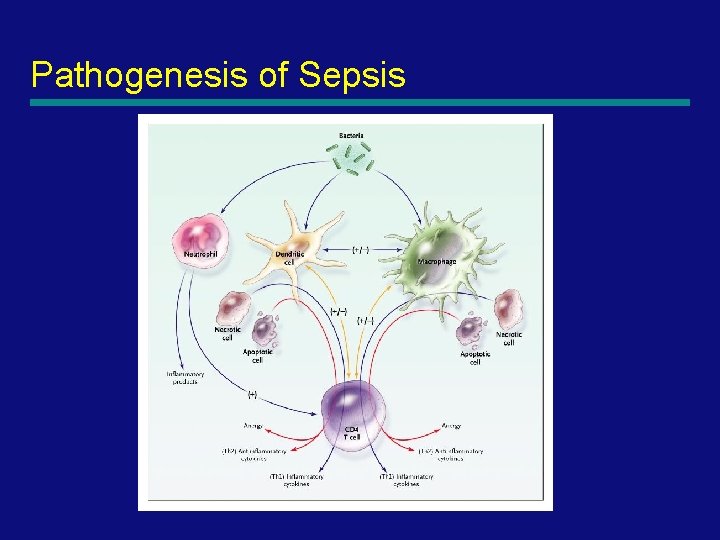
Pathophysiology of Sepsis Failure of Immune System to Eliminate Microorganism? • Shift from inflammatory (Th. I) to antiinflammatory response (Th 2). • Anergy. • Apotosis of B cells, T cells, Dendritic cells. • Loss of macrophage expression of MHC Class I and co-stimulatory molecules. • Immunosuppressive effect of apoptotic cells.
Pathogenesis of Sepsis
Pathogenesis of Sepsis
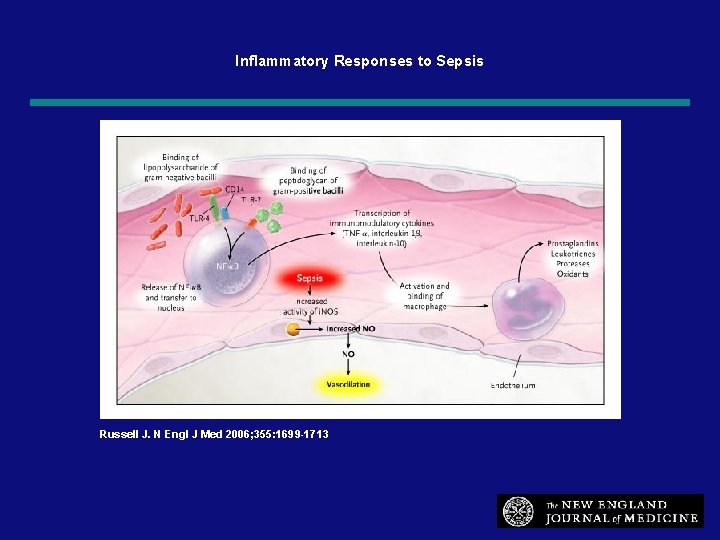
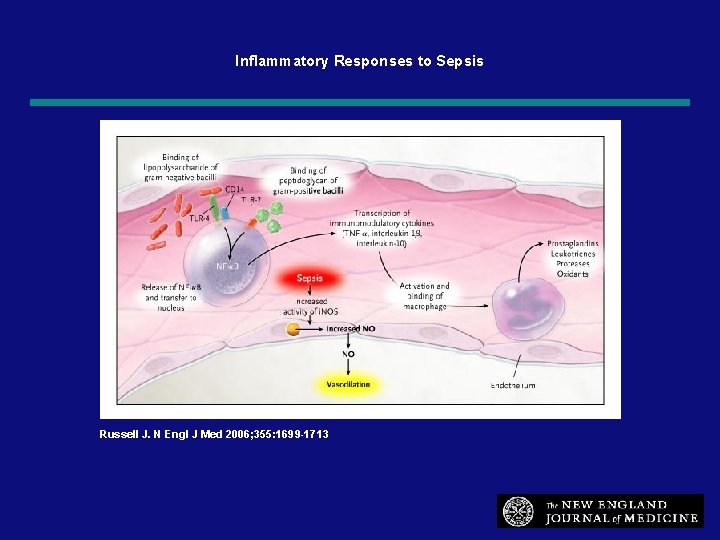
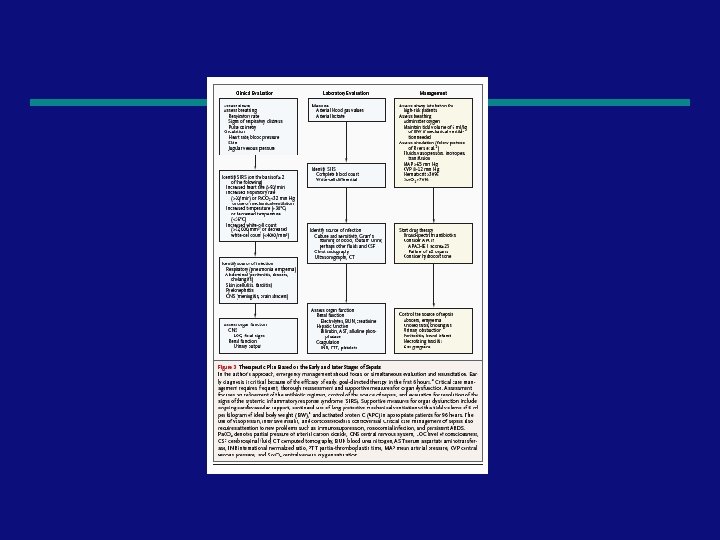
Inflammatory Responses to Sepsis Russell J. N Engl J Med 2006; 355: 1699 -1713 59
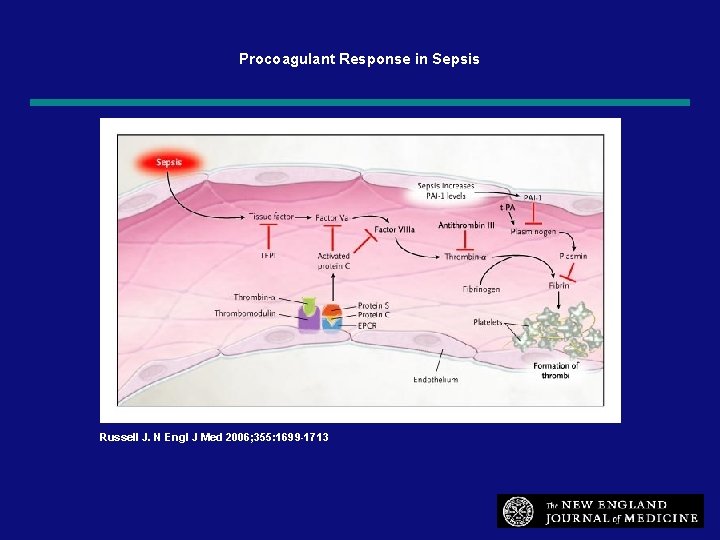
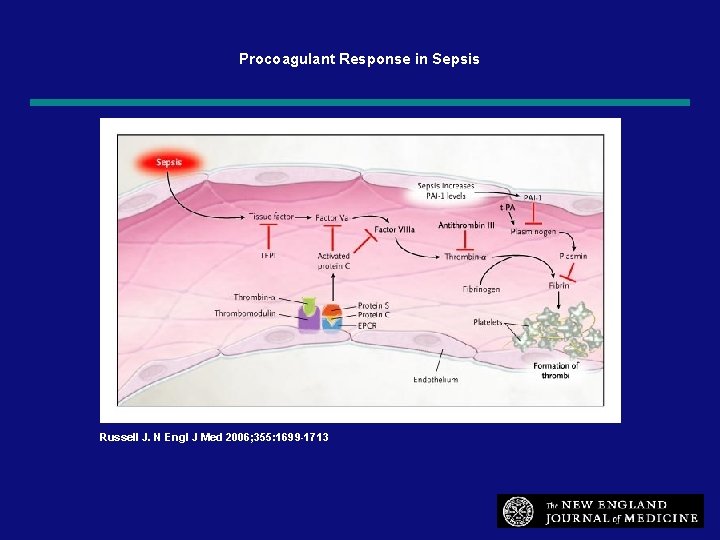
Procoagulant Response in Sepsis Russell J. N Engl J Med 2006; 355: 1699 -1713 60


62
63

64
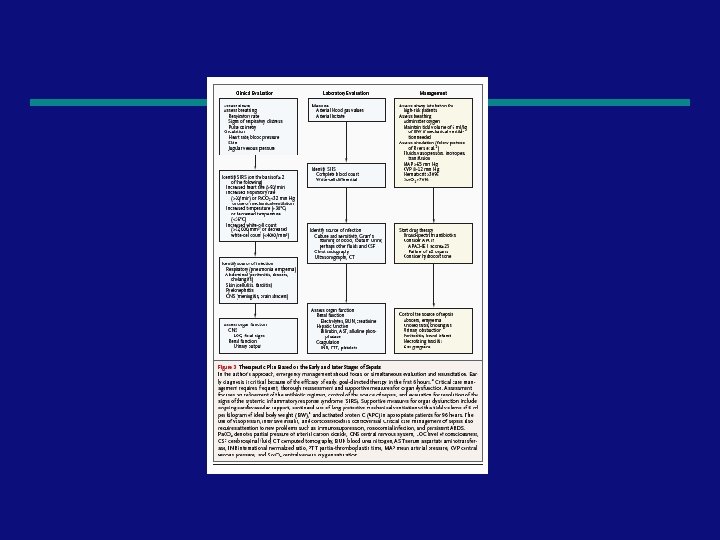
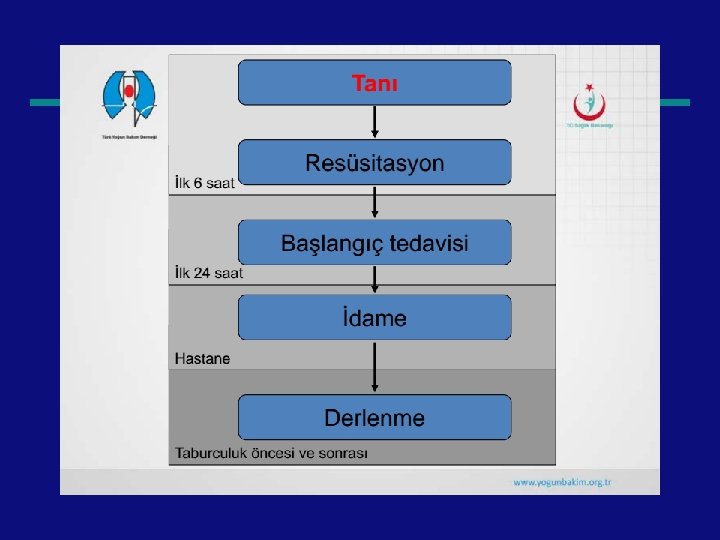
Treatment
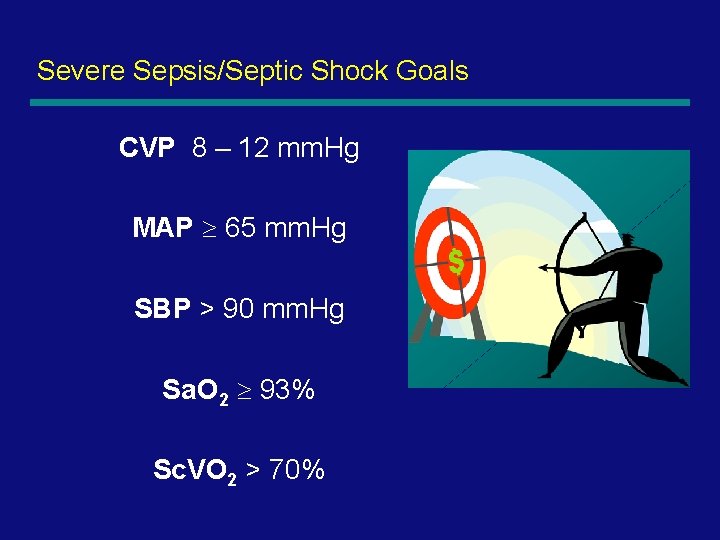
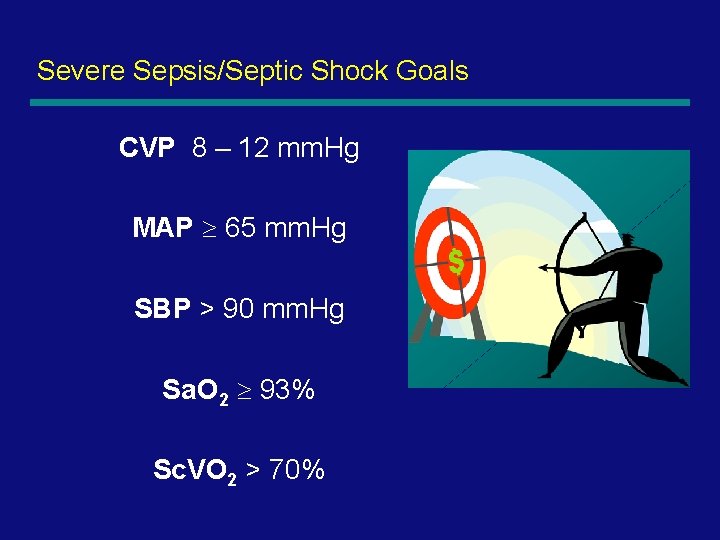
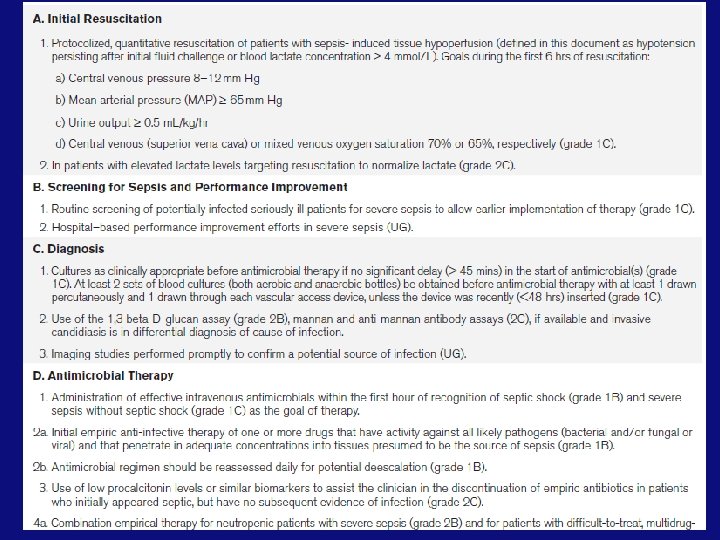
Severe Sepsis/Septic Shock Goals CVP 8 – 12 mm. Hg MAP 65 mm. Hg SBP > 90 mm. Hg Sa. O 2 93% Sc. VO 2 > 70%

Sepsis Resuscitation Emergency Department and Intensive Care Unit
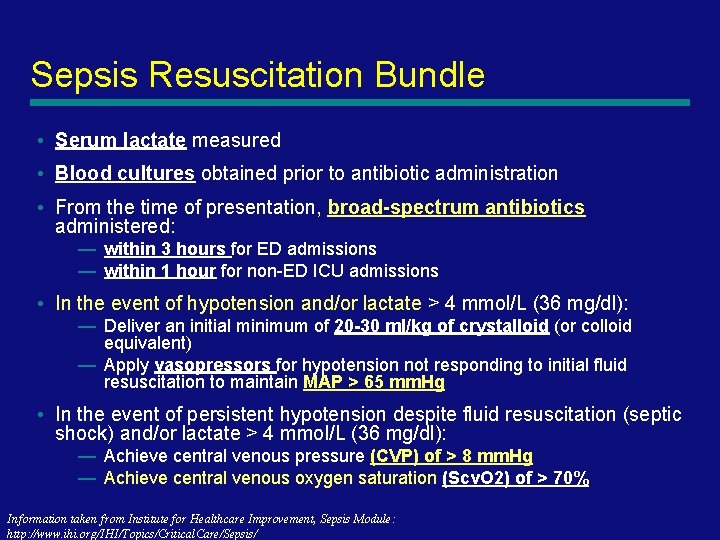
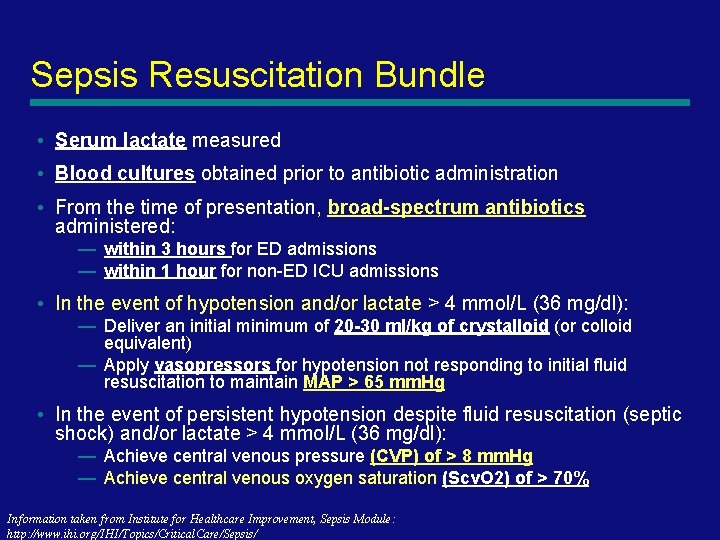
Sepsis Resuscitation Bundle • Serum lactate measured • Blood cultures obtained prior to antibiotic administration • From the time of presentation, broad-spectrum antibiotics administered: — within 3 hours for ED admissions — within 1 hour for non-ED ICU admissions • In the event of hypotension and/or lactate > 4 mmol/L (36 mg/dl): — Deliver an initial minimum of 20 -30 ml/kg of crystalloid (or colloid equivalent) — Apply vasopressors for hypotension not responding to initial fluid resuscitation to maintain MAP > 65 mm. Hg • In the event of persistent hypotension despite fluid resuscitation (septic shock) and/or lactate > 4 mmol/L (36 mg/dl): — Achieve central venous pressure (CVP) of > 8 mm. Hg — Achieve central venous oxygen saturation (Scv. O 2) of > 70% Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
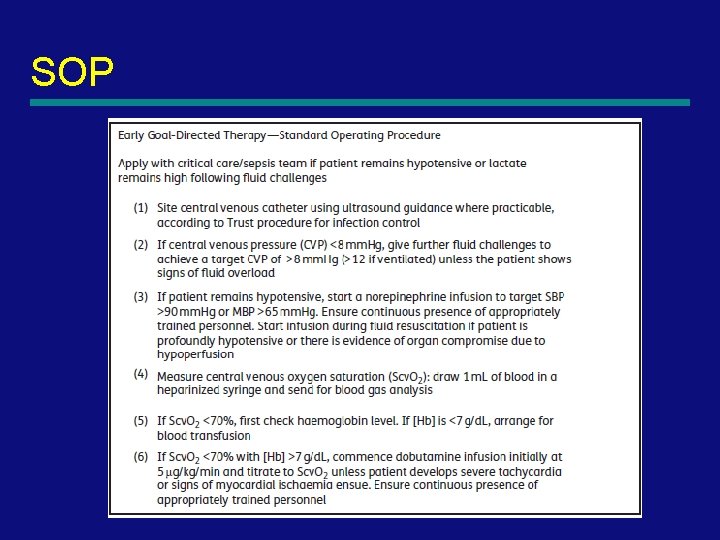
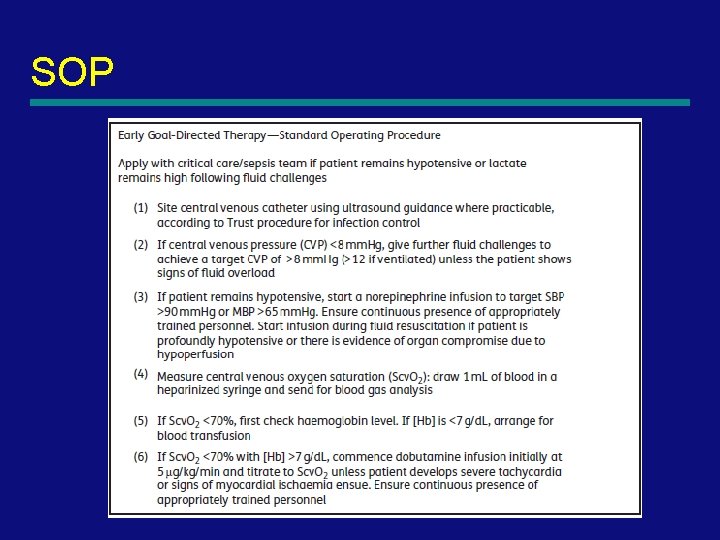
SOP

70

Bundle Completion and Outcome A 2 -year Implementation Experience Total Patients = 330 patients from Oct 2003 – Sept 2005 Bundle Not Completed = 253; Bundle Completed = 77 Mortality (p=0. 003) Hospital LOS (p=0. 22) Nguyen, Ann Emerg Med, 2005 - ACEP Annual Meeting; and Crit Care Med, 2005 - Critical Care Congress www. themegallery. com
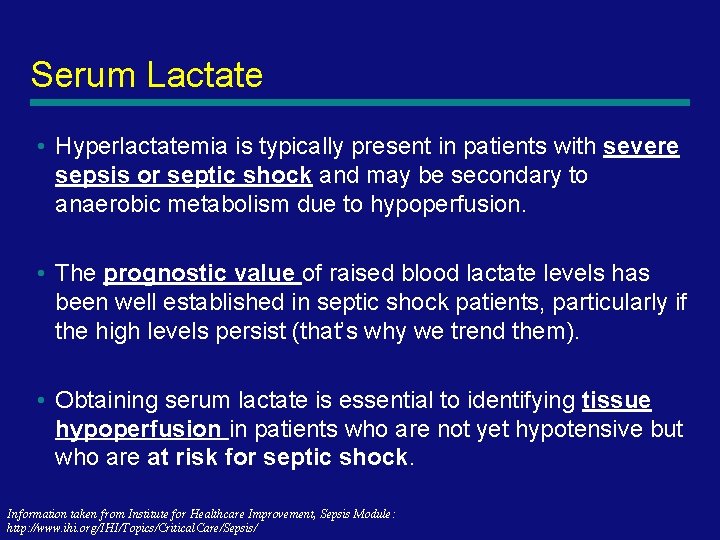
Serum Lactate • Hyperlactatemia is typically present in patients with severe sepsis or septic shock and may be secondary to anaerobic metabolism due to hypoperfusion. • The prognostic value of raised blood lactate levels has been well established in septic shock patients, particularly if the high levels persist (that’s why we trend them). • Obtaining serum lactate is essential to identifying tissue hypoperfusion in patients who are not yet hypotensive but who are at risk for septic shock. Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
Blood cultures • The incidence of sepsis and bacteremia in critically ill patients has been increasing in the past two decades. — 30 - 50% of patients presenting with a clinical syndrome of severe sepsis or shock have positive blood cultures. — Therefore, blood should be obtained for culture in any critically ill septic patient. • Collecting blood cultures prior to antibiotic administration offers the best hope of identifying the organism that caused severe sepsis in an individual patient. — Failure to check blood cultures prior to antibiotic infusion will perhaps affect the growth of any blood borne bacteria and prevent a culture from becoming positive later. Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
Broad Spectrum Antibiotics • The balance of evidence unwaveringly suggests that early administration of appropriate antibiotics reduces mortality in patients with Gram-positive and Gram-negative bacteremias. — Some of the evidence supporting early administration is based upon the assumption that patients who fail to receive appropriate antibiotics essentially represent a set of patients for whom delay has occurred in antibiotic delivery. — Several studies have confirmed the mortality benefit associated with appropriate antimicrobials in patients with severe infections due to Gramnegative and Gram-positive bacteria. — All patients should receive a full loading dose of each antimicrobial. § However, patients with sepsis or septic shock often have abnormal renal or hepatic function and may have abnormal volumes of distribution due to aggressive fluid resuscitation. The ICU pharmacist should be consulted to ensure that serum concentrations are attained that maximize efficacy and minimize toxicity Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
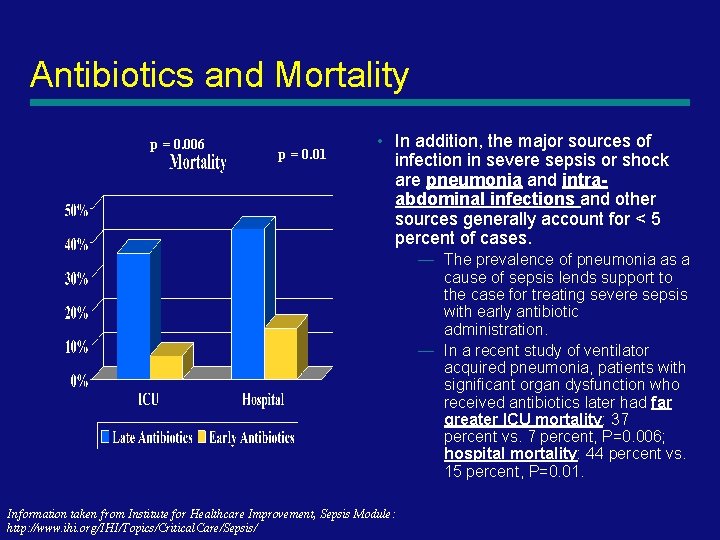
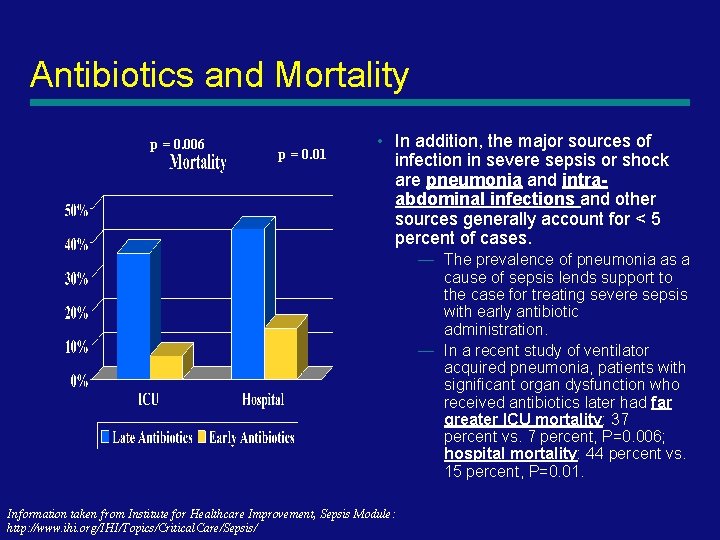
Antibiotics and Mortality p = 0. 006 p = 0. 01 • In addition, the major sources of infection in severe sepsis or shock are pneumonia and intraabdominal infections and other sources generally account for < 5 percent of cases. — The prevalence of pneumonia as a cause of sepsis lends support to the case for treating severe sepsis with early antibiotic administration. — In a recent study of ventilator acquired pneumonia, patients with significant organ dysfunction who received antibiotics later had far greater ICU mortality: 37 percent vs. 7 percent, P=0. 006; hospital mortality: 44 percent vs. 15 percent, P=0. 01. Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
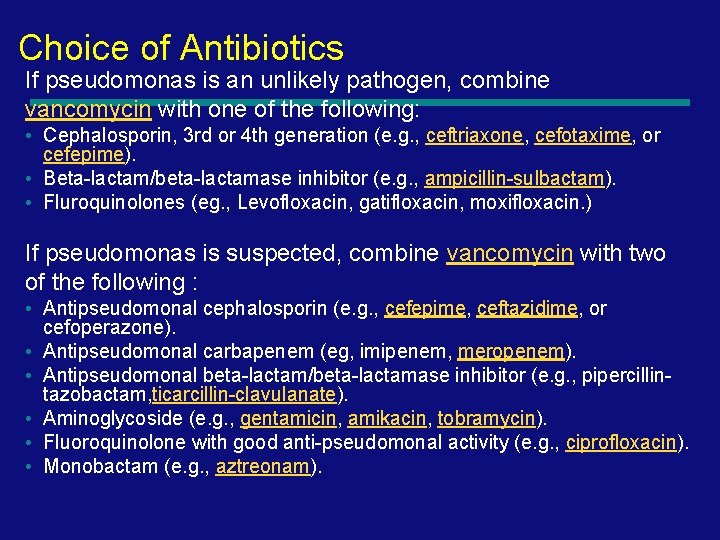
Choice of Antibiotics If pseudomonas is an unlikely pathogen, combine vancomycin with one of the following: • Cephalosporin, 3 rd or 4 th generation (e. g. , ceftriaxone, cefotaxime, or cefepime). • Beta-lactam/beta-lactamase inhibitor (e. g. , ampicillin-sulbactam). • Fluroquinolones (eg. , Levofloxacin, gatifloxacin, moxifloxacin. ) If pseudomonas is suspected, combine vancomycin with two of the following : • Antipseudomonal cephalosporin (e. g. , cefepime, ceftazidime, or cefoperazone). • Antipseudomonal carbapenem (eg, imipenem, meropenem). • Antipseudomonal beta-lactam/beta-lactamase inhibitor (e. g. , pipercillintazobactam, ticarcillin-clavulanate). • Aminoglycoside (e. g. , gentamicin, amikacin, tobramycin). • Fluoroquinolone with good anti-pseudomonal activity (e. g. , ciprofloxacin). • Monobactam (e. g. , aztreonam).
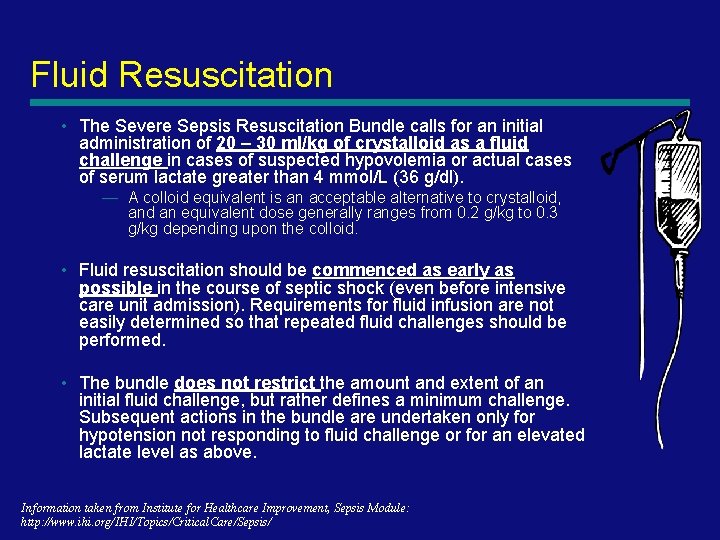
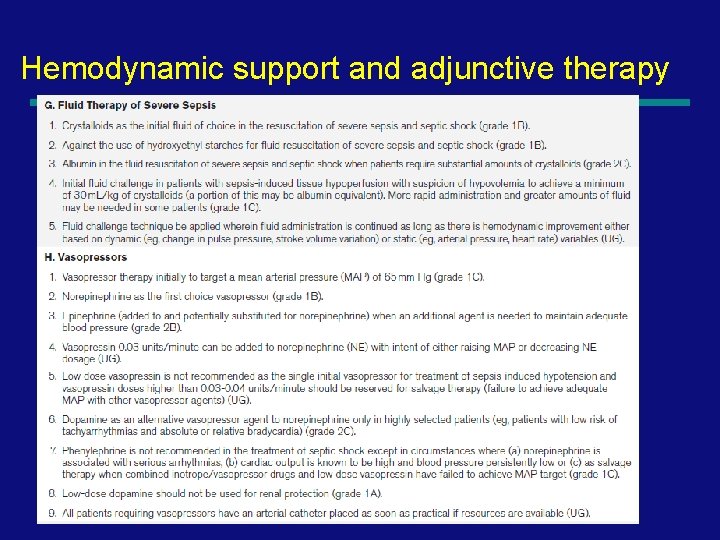
Fluid Resuscitation • The Severe Sepsis Resuscitation Bundle calls for an initial administration of 20 – 30 ml/kg of crystalloid as a fluid challenge in cases of suspected hypovolemia or actual cases of serum lactate greater than 4 mmol/L (36 g/dl). — A colloid equivalent is an acceptable alternative to crystalloid, and an equivalent dose generally ranges from 0. 2 g/kg to 0. 3 g/kg depending upon the colloid. • Fluid resuscitation should be commenced as early as possible in the course of septic shock (even before intensive care unit admission). Requirements for fluid infusion are not easily determined so that repeated fluid challenges should be performed. • The bundle does not restrict the amount and extent of an initial fluid challenge, but rather defines a minimum challenge. Subsequent actions in the bundle are undertaken only for hypotension not responding to fluid challenge or for an elevated lactate level as above. Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
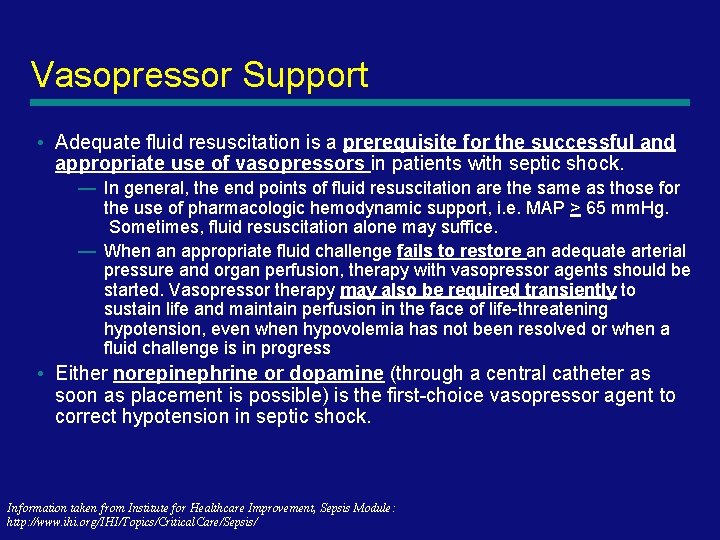
Vasopressor Support • Adequate fluid resuscitation is a prerequisite for the successful and appropriate use of vasopressors in patients with septic shock. — In general, the end points of fluid resuscitation are the same as those for the use of pharmacologic hemodynamic support, i. e. MAP > 65 mm. Hg. Sometimes, fluid resuscitation alone may suffice. — When an appropriate fluid challenge fails to restore an adequate arterial pressure and organ perfusion, therapy with vasopressor agents should be started. Vasopressor therapy may also be required transiently to sustain life and maintain perfusion in the face of life-threatening hypotension, even when hypovolemia has not been resolved or when a fluid challenge is in progress • Either norepinephrine or dopamine (through a central catheter as soon as placement is possible) is the first-choice vasopressor agent to correct hypotension in septic shock. Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
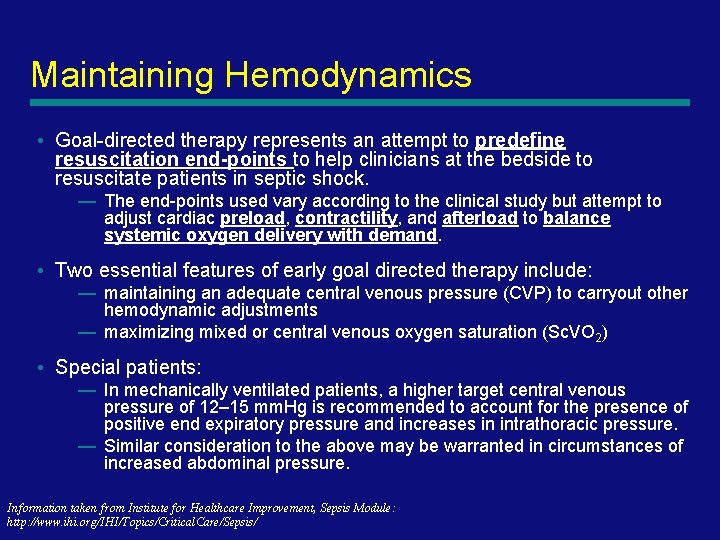
Maintaining Hemodynamics • Goal-directed therapy represents an attempt to predefine resuscitation end-points to help clinicians at the bedside to resuscitate patients in septic shock. — The end-points used vary according to the clinical study but attempt to adjust cardiac preload, contractility, and afterload to balance systemic oxygen delivery with demand. • Two essential features of early goal directed therapy include: — maintaining an adequate central venous pressure (CVP) to carryout other hemodynamic adjustments — maximizing mixed or central venous oxygen saturation (Sc. VO 2) • Special patients: — In mechanically ventilated patients, a higher target central venous pressure of 12– 15 mm. Hg is recommended to account for the presence of positive end expiratory pressure and increases in intrathoracic pressure. — Similar consideration to the above may be warranted in circumstances of increased abdominal pressure. Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
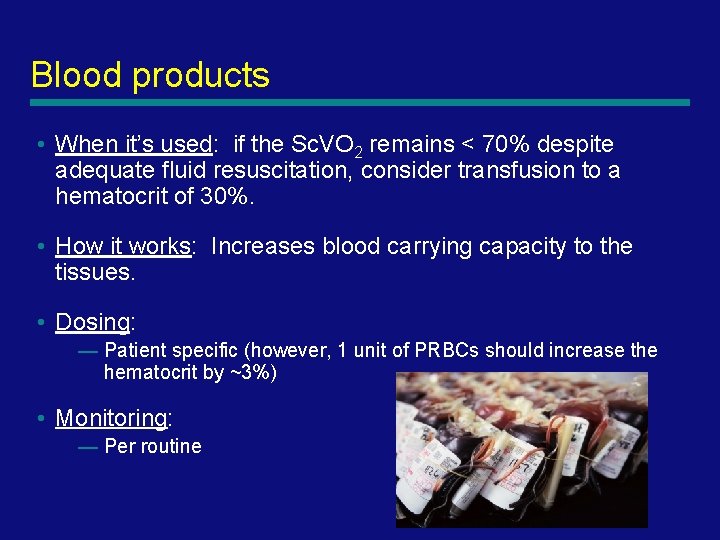
Blood products • When it’s used: if the Sc. VO 2 remains < 70% despite adequate fluid resuscitation, consider transfusion to a hematocrit of 30%. • How it works: Increases blood carrying capacity to the tissues. • Dosing: — Patient specific (however, 1 unit of PRBCs should increase the hematocrit by ~3%) • Monitoring: — Per routine

Sepsis Management Intensive Care Unit

Early Goal-directed therapy in the treatment of severe sepsis and septic shock Rivers et al; NEJM 2001; 345: 1368
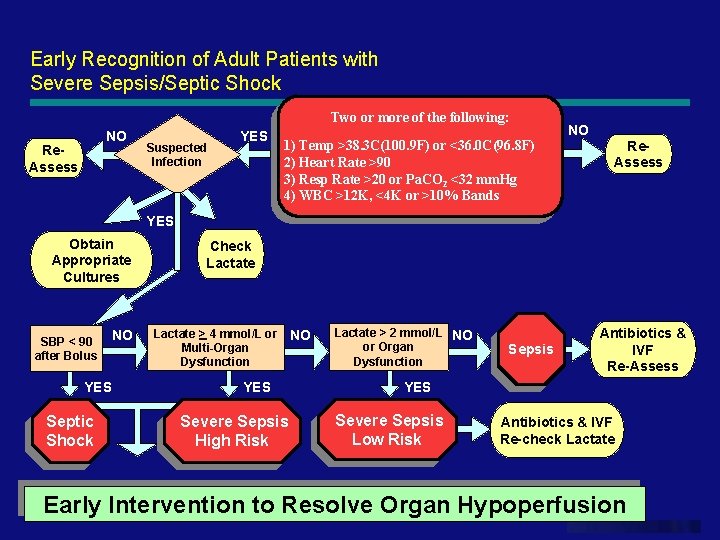
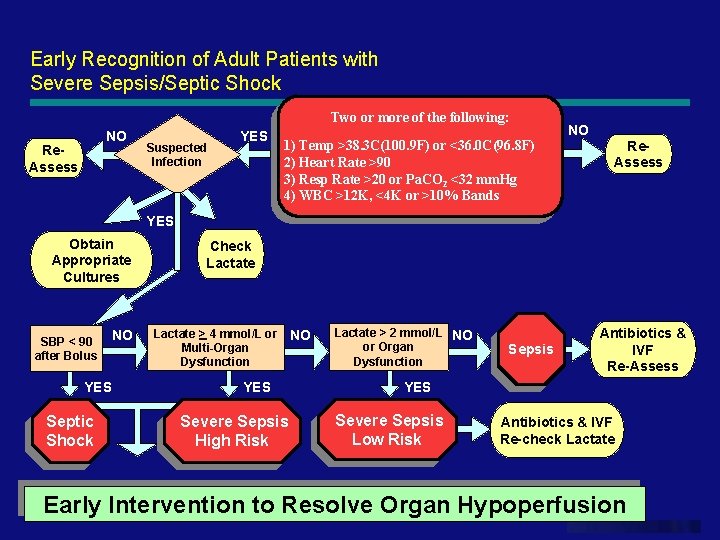
Early Recognition of Adult Patients with Severe Sepsis/Septic Shock Two or more of the following: NO Re. Assess Suspected Infection YES 1) Temp >38. 3 C(100. 9 F) or <36. 0 C(96. 8 F) 2) Heart Rate >90 3) Resp Rate >20 or Pa. CO 2 <32 mm. Hg 4) WBC >12 K, <4 K or >10% Bands NO Re. Assess YES Obtain Appropriate Cultures SBP < 90 after Bolus NO YES Septic Shock Check Lactate > 4 mmol/L or NO Multi-Organ Dysfunction YES Severe Sepsis High Risk Lactate > 2 mmol/L NO or Organ Dysfunction Sepsis Antibiotics & IVF Re-Assess YES Severe Sepsis Low Risk Antibiotics & IVF Re-check Lactate Early Intervention to Resolve Organ Hypoperfusion www. themegallery. com
84
85

86
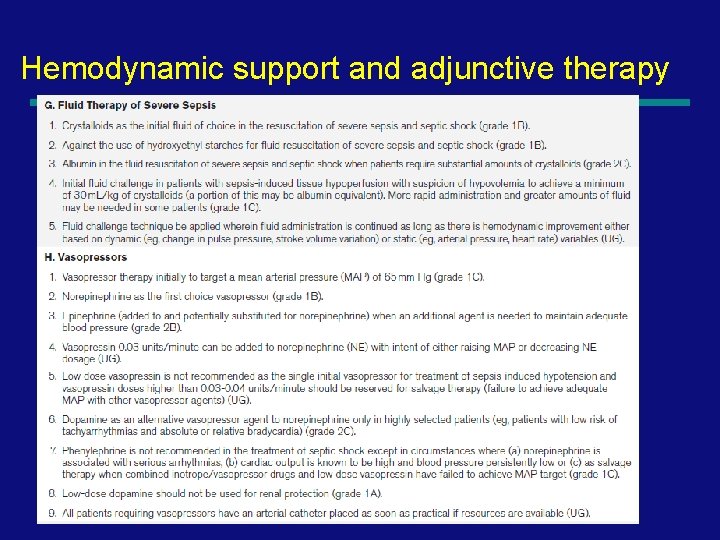
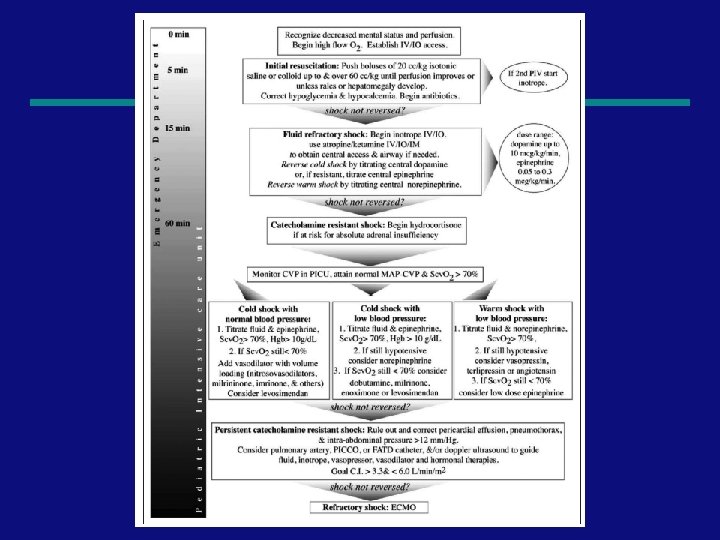
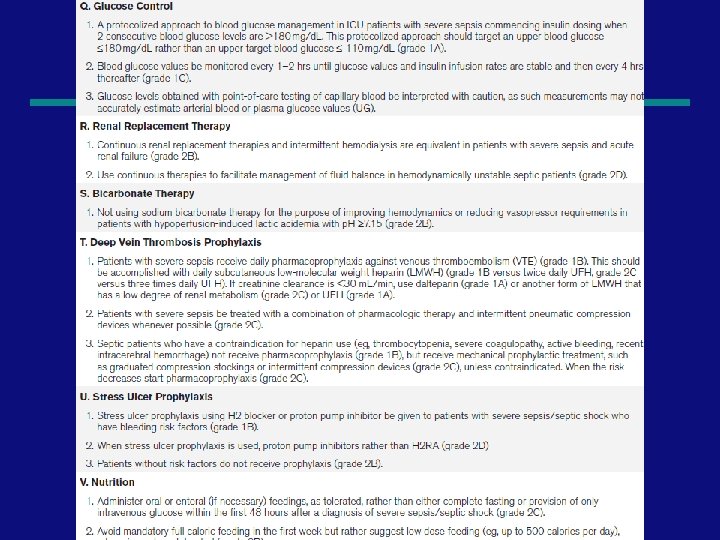
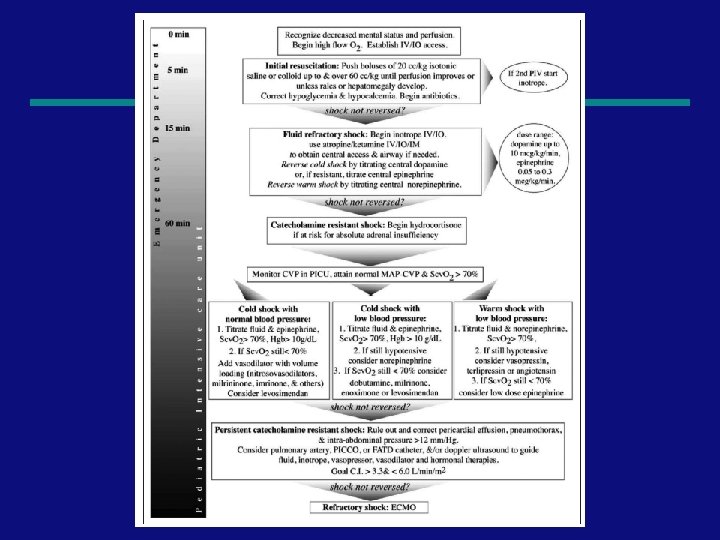
Hemodynamic support and adjunctive therapy 87
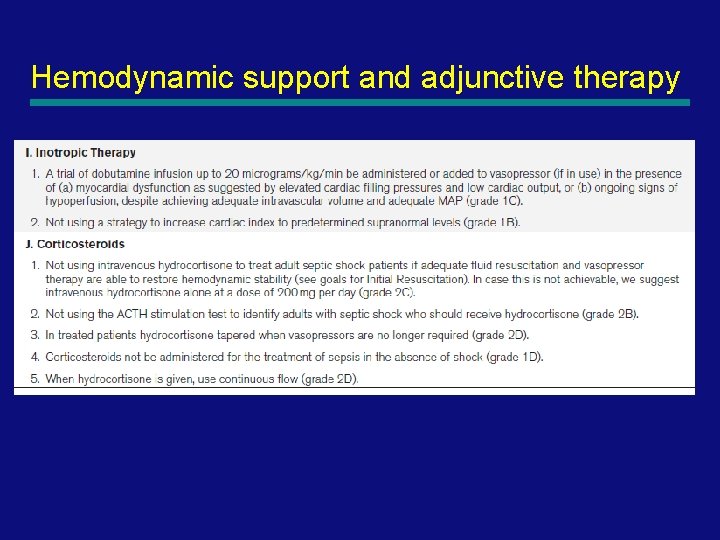
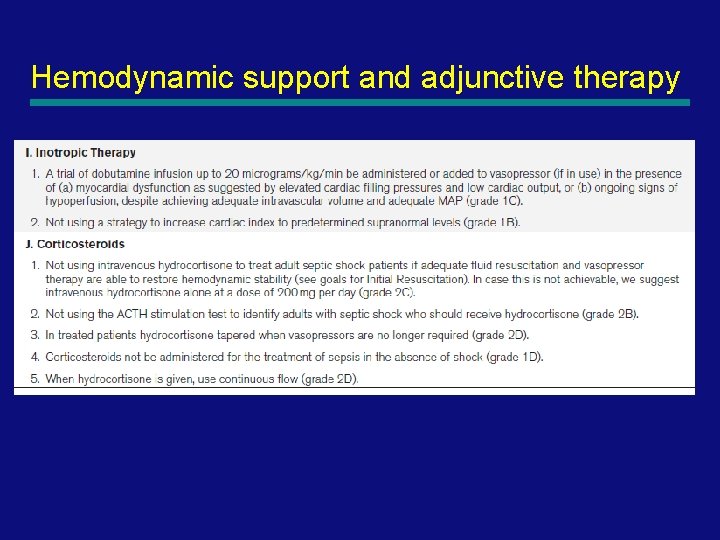
Hemodynamic support and adjunctive therapy 88
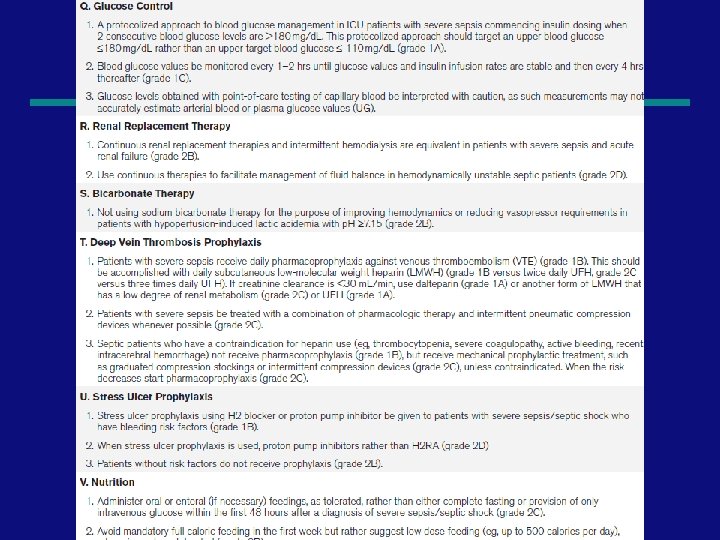
89
90
Summary • • • Sepsis may be obvious or subtle early There is a high mortality and morbidity Have a high index of suspicion Know local organisms / susceptibilities Take appropriate cultures Treat early and aggressively Investigate early and aggressively Refer early and aggressively Be aware of new developments 91
92

93

94
95

96
97
98
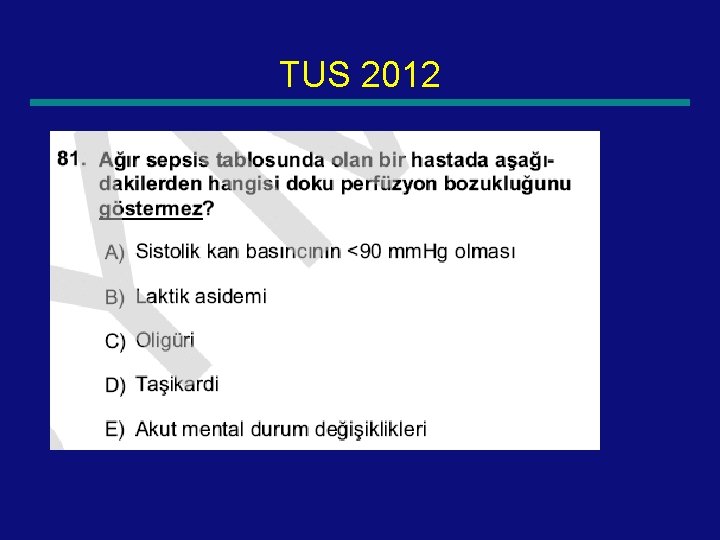
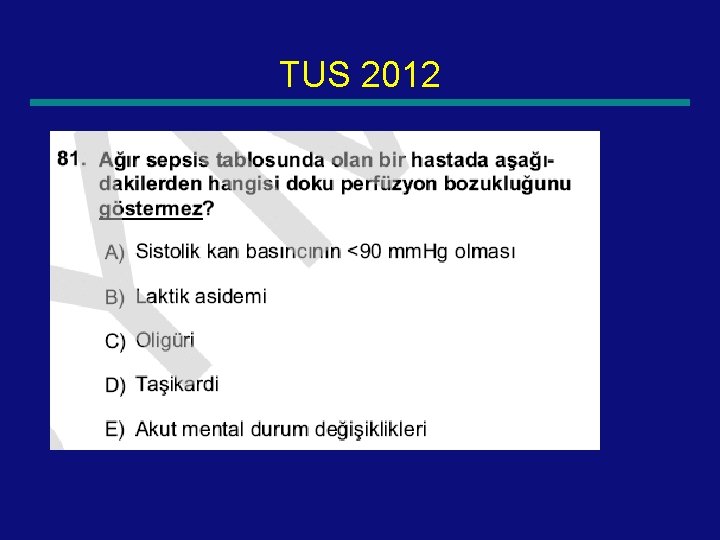
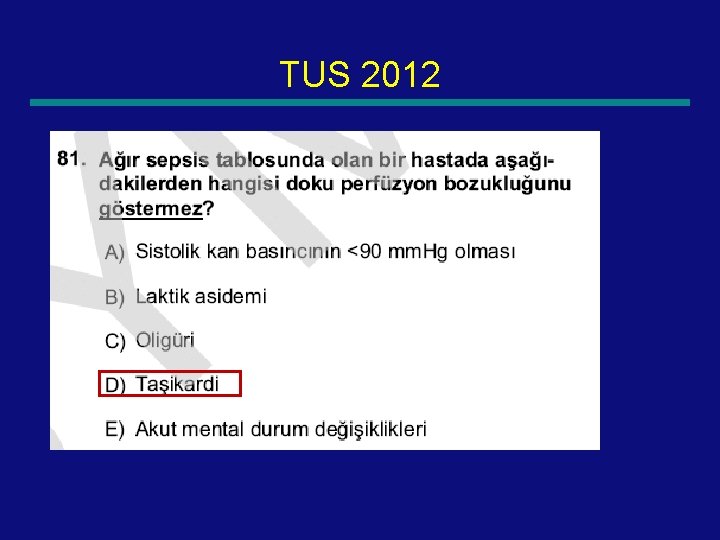
TUS 2012 99
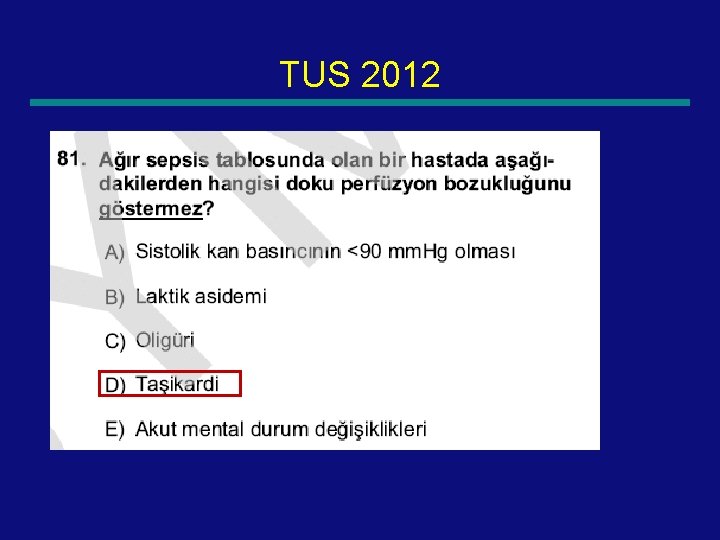
TUS 2012 100
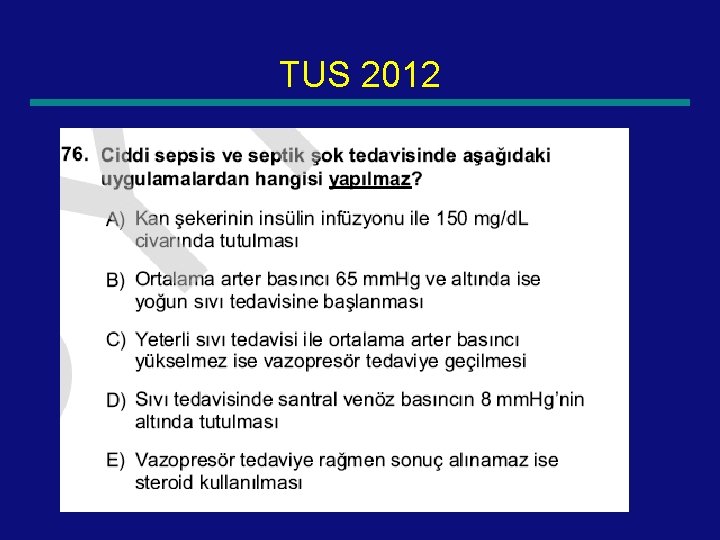
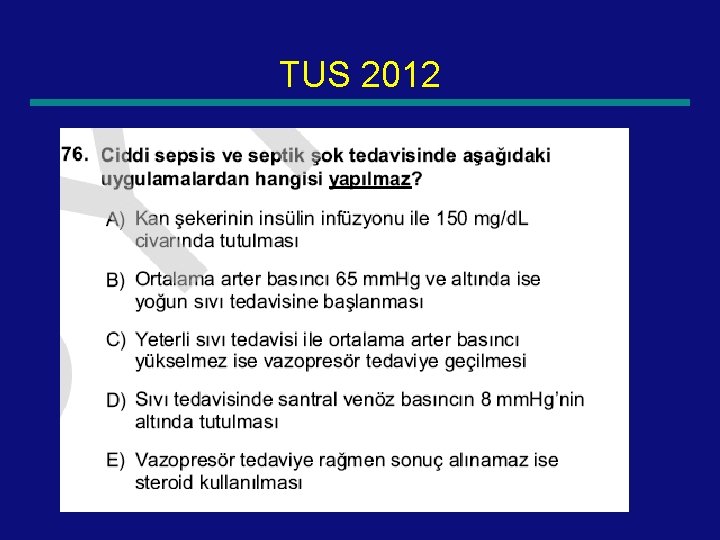
TUS 2012 101
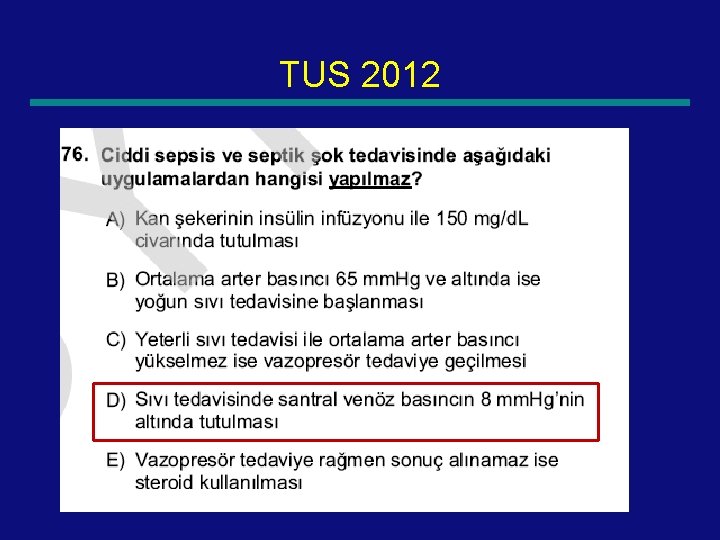
TUS 2012 102
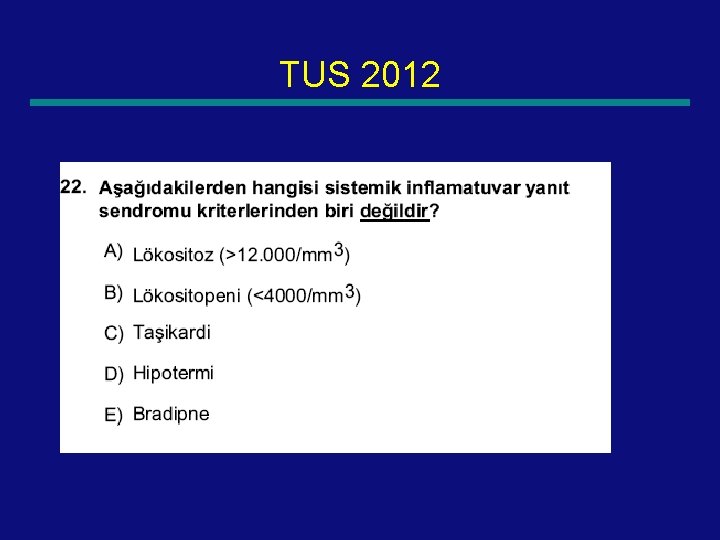
TUS 2012 103
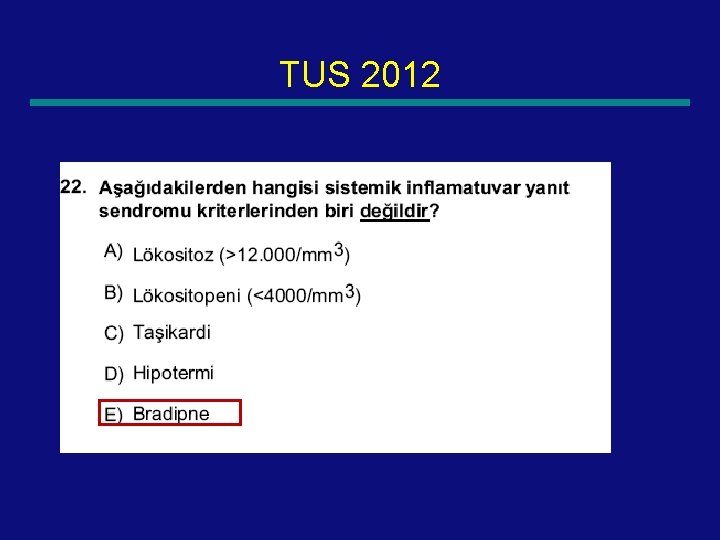
TUS 2012 104
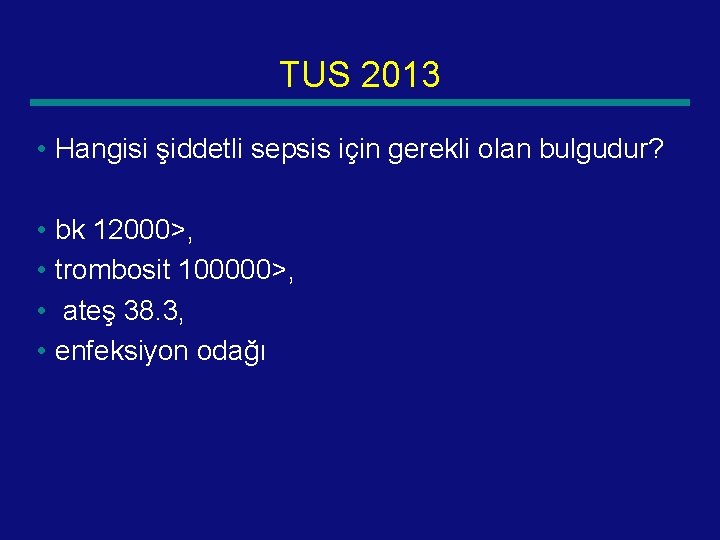
TUS 2013 • Hangisi şiddetli sepsis için gerekli olan bulgudur? • bk 12000>, • trombosit 100000>, • ateş 38. 3, • enfeksiyon odağı 105
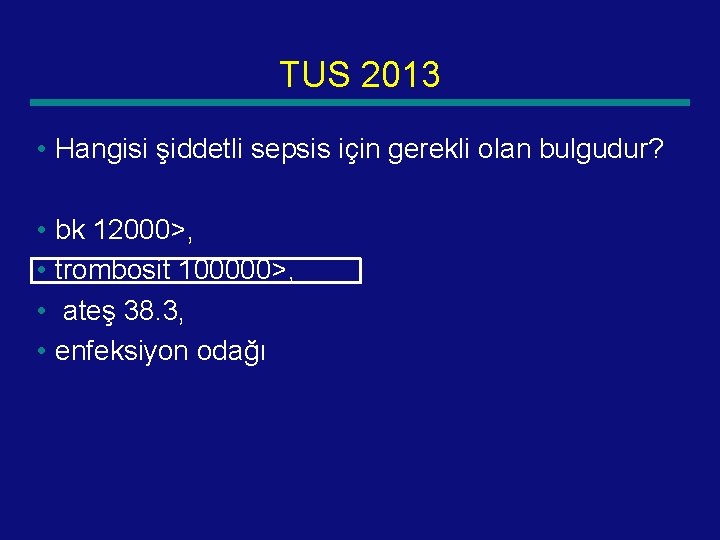
TUS 2013 • Hangisi şiddetli sepsis için gerekli olan bulgudur? • bk 12000>, • trombosit 100000>, • ateş 38. 3, • enfeksiyon odağı 106
TUS 2013 • Yağ infuzyonu yapılan hastada sepsis nedeni? • A) Malessezia furfur • Fungal factors that contribute to infection include the size of the inoculum and factors that favor colonization and proliferation (eg, use of broad-spectrum antibiotics, postnatal steroids, histamine type-2 [H 2] antagonists, parenteral nutrition, or lipid emulsions [Malassezia spp 107
TUS 2013 • Septik şok tanısı konulan bir hastada, laktik asideminin düzeltilmesinde hücre membranındaki enzimlerin aktivitesini artırarak etki gösteren madde aşağıdakilerden hangisidir? • A) Dopamin B) Dobutamin C) Arjinin vazopressin D) Epinefrin E) Kortizol 108
TUS 2013 • Septik şok tanısı konulan bir hastada, laktik asideminin düzeltilmesinde hücre membranındaki enzimlerin aktivitesini artırarak etki gösteren madde aşağıdakilerden hangisidir? • A) Dopamin B) Dobutamin C) Arjinin vazopressin D) Epinefrin E) Kortizol 109
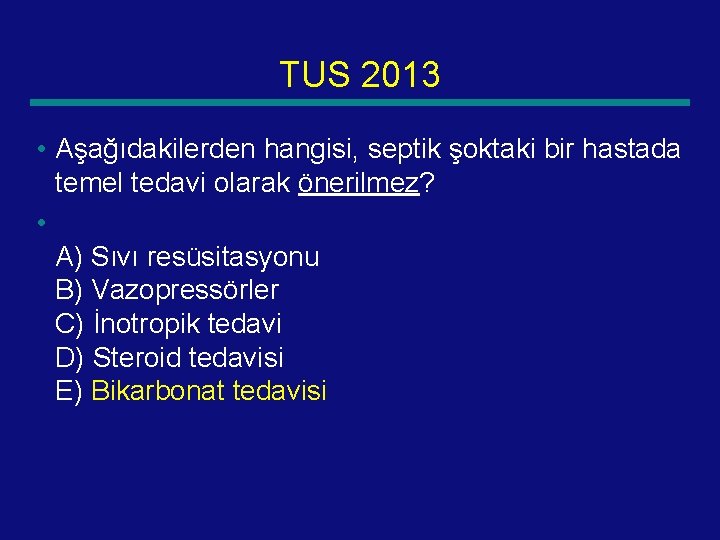
TUS 2013 • Aşağıdakilerden hangisi, septik şoktaki bir hastada temel tedavi olarak önerilmez? • A) Sıvı resüsitasyonu B) Vazopressörler C) İnotropik tedavi D) Steroid tedavisi E) Bikarbonat tedavisi 110
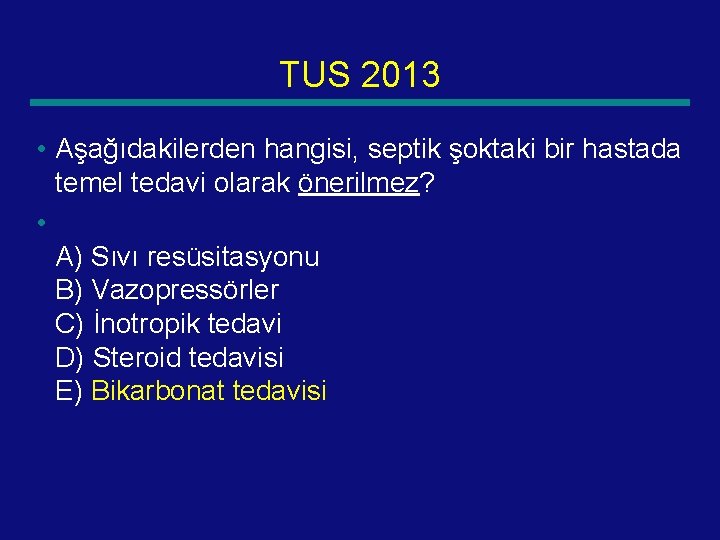
TUS 2013 • Aşağıdakilerden hangisi, septik şoktaki bir hastada temel tedavi olarak önerilmez? • A) Sıvı resüsitasyonu B) Vazopressörler C) İnotropik tedavi D) Steroid tedavisi E) Bikarbonat tedavisi 111
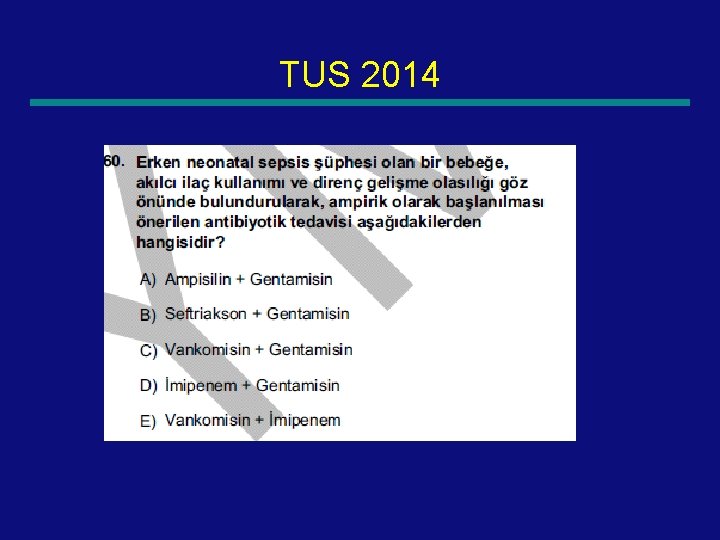
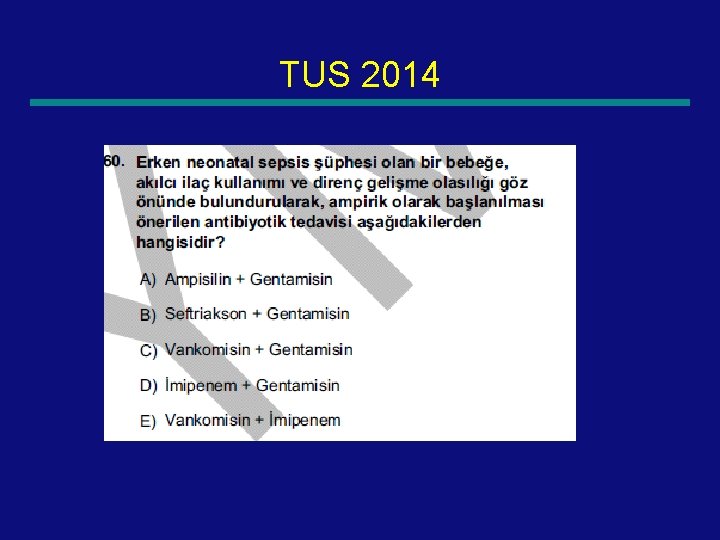
TUS 2014 112

TUS 2014 113
 Q sofa
Q sofa T10 spinal cord
T10 spinal cord Site:slidetodoc.com
Site:slidetodoc.com Subacute combined degeneration
Subacute combined degeneration Diferencia entre shock medular y shock neurogenico
Diferencia entre shock medular y shock neurogenico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Endocervix
Endocervix Meral güneş ergin
Meral güneş ergin Meral dogan
Meral dogan Meral yılmaz öğretmen
Meral yılmaz öğretmen Büyükelçilik protokol sıra düzeni
Büyükelçilik protokol sıra düzeni Pınar seden meral
Pınar seden meral Shock prof
Shock prof Shock prof
Shock prof Hypovolumic
Hypovolumic Ervin moore sign
Ervin moore sign Summit county septic permit
Summit county septic permit Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Septic arthritis complications
Septic arthritis complications Septic tank contamination groundwater
Septic tank contamination groundwater Haemotopoisis
Haemotopoisis Qqq10
Qqq10 Septic arthritis complications
Septic arthritis complications Advantex ax20 price
Advantex ax20 price Rock solid septic
Rock solid septic Satellitism in haemophilus influenzae
Satellitism in haemophilus influenzae Panhandle health septic
Panhandle health septic Hypoandrogenism
Hypoandrogenism Septic arthritis workup
Septic arthritis workup Multi flo aerator replacement
Multi flo aerator replacement Doc's septic tank cleaning
Doc's septic tank cleaning Barnstable county septic loan
Barnstable county septic loan Carmody septic
Carmody septic Streptococcus gram negative
Streptococcus gram negative Septic arthritis antibiotics
Septic arthritis antibiotics Septic systems indianapolis
Septic systems indianapolis Septic
Septic Puraflo peat
Puraflo peat Septic arthritis
Septic arthritis Septic implantation syndrome
Septic implantation syndrome Jea septic tank phase out
Jea septic tank phase out Gonococcal vs nongonococcal arthritis
Gonococcal vs nongonococcal arthritis Chemical oxygen demand
Chemical oxygen demand Septic arthritis antibiotics
Septic arthritis antibiotics Etiology of bronchial asthma
Etiology of bronchial asthma What is life
What is life Combined immunodeficiency
Combined immunodeficiency Hypocalcemia causes
Hypocalcemia causes Severe obesity
Severe obesity Bill nye thunderstorms
Bill nye thunderstorms Pong game cards
Pong game cards What is severe iron deficiency
What is severe iron deficiency Najredšie osídlené oblasti afriky
Najredšie osídlené oblasti afriky Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation Severe weather safety precautions worksheet
Severe weather safety precautions worksheet Potassium dose calculation
Potassium dose calculation Pictograms can be easily identified because
Pictograms can be easily identified because Severe anxiety
Severe anxiety Severe weather graphic organizer
Severe weather graphic organizer Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation S2 os gap
S2 os gap What is bowl in medical term
What is bowl in medical term Trousseau sign
Trousseau sign Euvolemic hyponatremia
Euvolemic hyponatremia Switching antidepressants chart
Switching antidepressants chart Causes of cotton wool spots
Causes of cotton wool spots Unmet needs in severe asthma
Unmet needs in severe asthma Potassium replacement
Potassium replacement Malnutrition case study example
Malnutrition case study example Katrine zhiroff
Katrine zhiroff Diarrhea plan a
Diarrhea plan a The outsiders chapter 7 vocabulary
The outsiders chapter 7 vocabulary Chapter 24 trauma overview
Chapter 24 trauma overview Natremia
Natremia Severe anemia
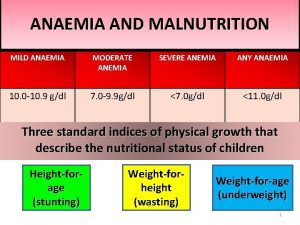
Severe anemia Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Mild moderate severe dehydration
Mild moderate severe dehydration Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Pong game scratch
Pong game scratch Wmo severe weather
Wmo severe weather Domina severe
Domina severe Fluid of choice in severe dehydration
Fluid of choice in severe dehydration Chapter 16 understanding weather answer key
Chapter 16 understanding weather answer key Dr sofi
Dr sofi Severe dehydration
Severe dehydration Laxative effect
Laxative effect Severe dehydration
Severe dehydration Severe angle blocking
Severe angle blocking Causes of metabolic acidosis
Causes of metabolic acidosis The severe style is characterized by
The severe style is characterized by Types of dehydration
Types of dehydration International severe asthma registry
International severe asthma registry Severe preeclampsia criteria
Severe preeclampsia criteria Swfdp
Swfdp Rexocef 100
Rexocef 100 Severe weather data inventory
Severe weather data inventory Riesgo de sepsis nanda
Riesgo de sepsis nanda Peicarditis
Peicarditis How do you get sepsis
How do you get sepsis Sepsis
Sepsis Dr ali hieatt
Dr ali hieatt Sepsis 6 bundle
Sepsis 6 bundle La hora dorada medicina
La hora dorada medicina Sepsis triangle
Sepsis triangle Surviving sepsis definition
Surviving sepsis definition Sepsis bundle
Sepsis bundle Storch infection
Storch infection Bjarni geir viðarsson
Bjarni geir viðarsson Stages of sepsis
Stages of sepsis Cuarro
Cuarro Neonatal sepsis symptoms
Neonatal sepsis symptoms Gdp sepsis decision support tool
Gdp sepsis decision support tool Sepsis care near palo alto
Sepsis care near palo alto Sepsis pp respiratorio
Sepsis pp respiratorio