Disease of Spine and Spinal Cord THE SPINAL







- Slides: 76
Disease of Spine and Spinal Cord
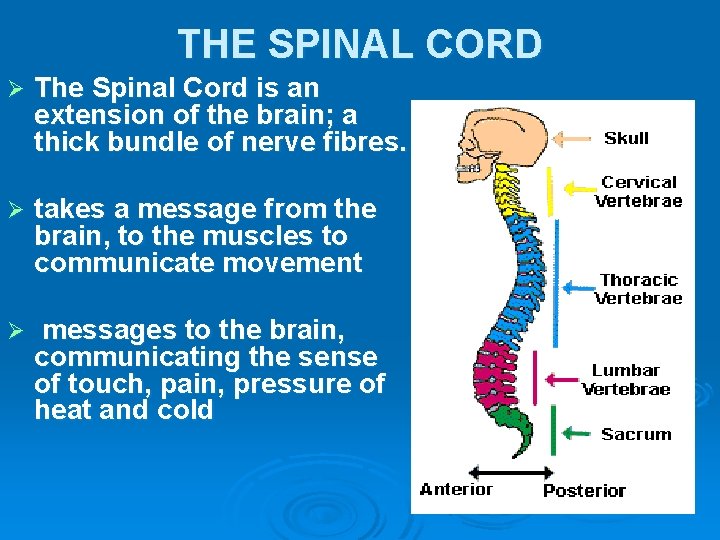
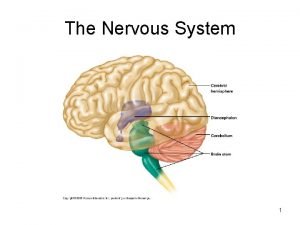
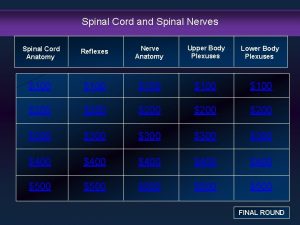
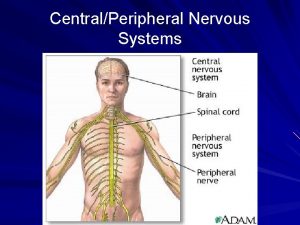
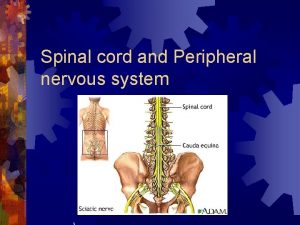
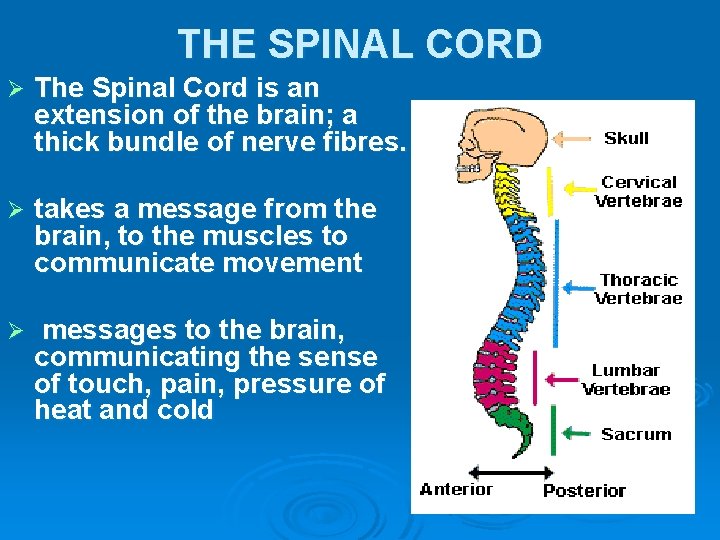
THE SPINAL CORD Ø The Spinal Cord is an extension of the brain; a thick bundle of nerve fibres. Ø takes a message from the brain, to the muscles to communicate movement Ø messages to the brain, communicating the sense of touch, pain, pressure of heat and cold
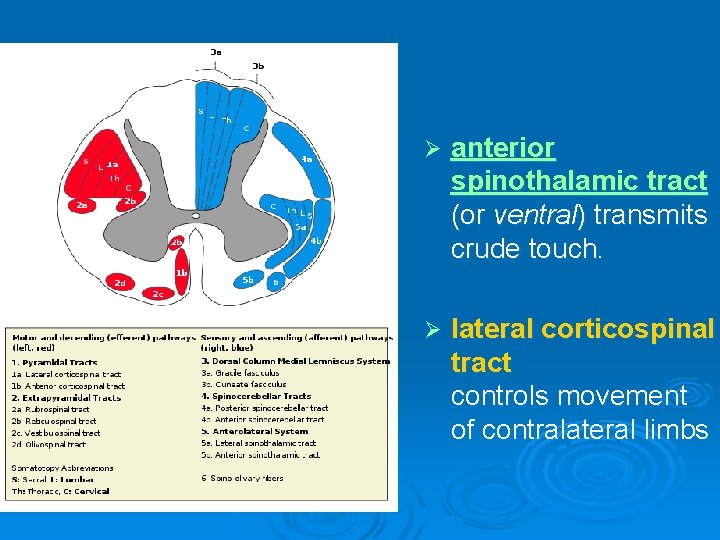
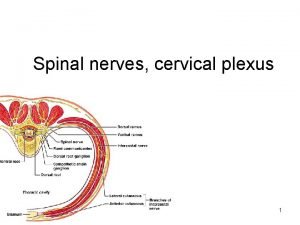
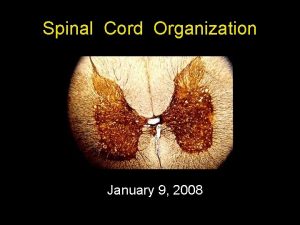
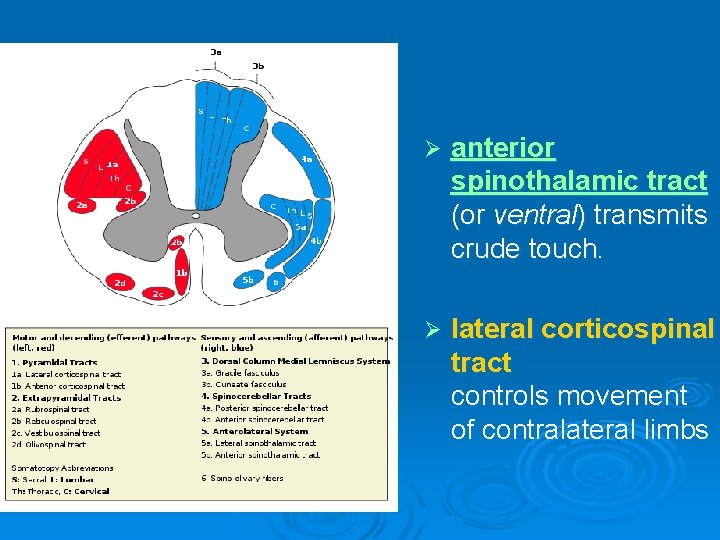
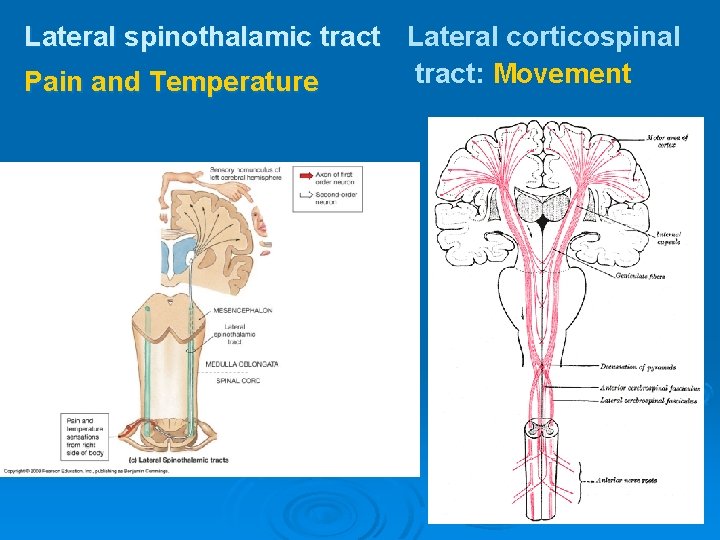
Ø anterior spinothalamic tract (or ventral) transmits crude touch. Ø lateral corticospinal tract controls movement of contralateral limbs
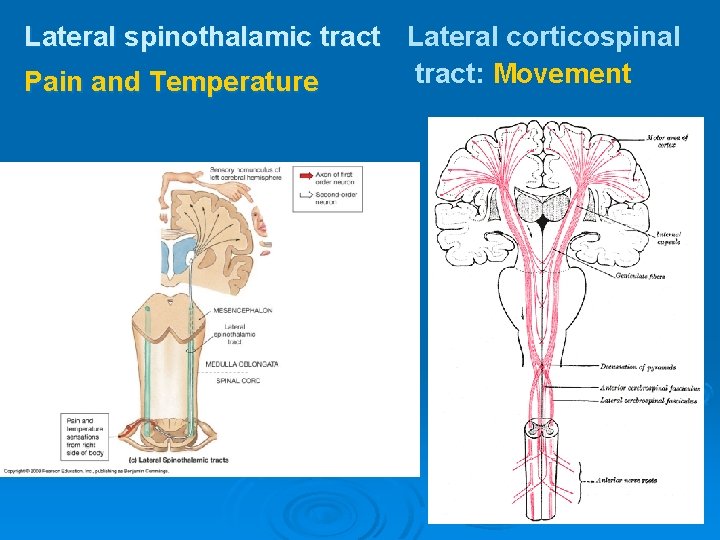
Lateral spinothalamic tract Lateral corticospinal tract: Movement Pain and Temperature
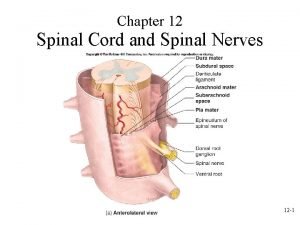
General view Spinal Cord Injury is damage to the spinal cord that results in a loss of function such as mobility or feeling. Frequent causes of damage are trauma and disease. Ø Spinal Cord is the major bundle of nerves that carry impulses to/from the brain to the rest of the body. Ø Spinal Cord is surrounded by rings of bonevertebra. They function to protect the spinal cord. Ø
Prognosis Ø Ø Ø Patients with a complete cord injury have a less than 5% chance of recovery. If complete paralysis persists at 72 hours after injury, recovery is essentially zero. The prognosis is much better for the incomplete cord syndromes. If some sensory function is preserved, the chance that the patient will eventually be able walk is greater than 50%. Ultimately, 90% of patients with SCI return to their homes and regain independence. In the early 1900 s, the mortality rate 1 year after injury in patients with complete lesions approached 100%. Much of the improvement since then can be attributed to the introduction of antibiotics to treat pneumonia and urinary tract infection. Currently, the 5 -year survival rate for patients with a traumatic quadriplegia exceeds 90%. The hospital mortality rate for isolated acute SCI is low.
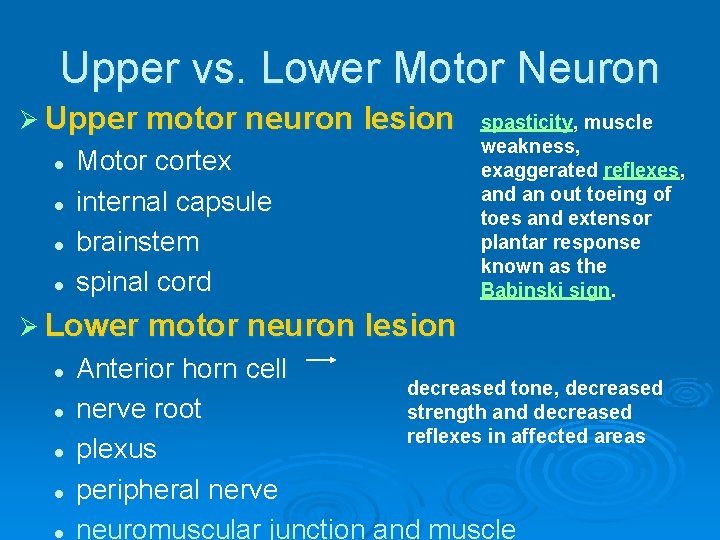
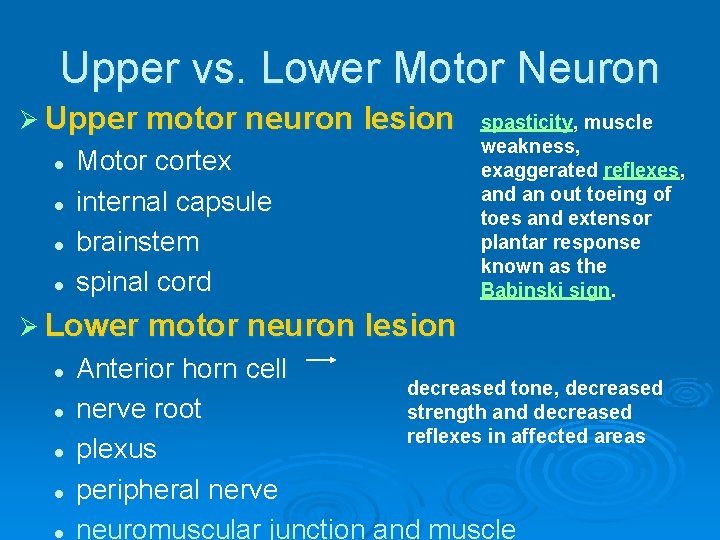
Upper vs. Lower Motor Neuron Ø Upper motor neuron lesion l l Motor cortex internal capsule brainstem spinal cord spasticity, muscle weakness, exaggerated reflexes, and an out toeing of toes and extensor plantar response known as the Babinski sign. Ø Lower motor neuron lesion l l l Anterior horn cell decreased tone, decreased nerve root strength and decreased reflexes in affected areas plexus peripheral nerve neuromuscular junction and muscle
Basic Features of Spinal Cord Disease Ø UMN findings below the lesion l Hyperreflexia and Babinski’s Ø Sensory and motor involvement that localizes to a spinal cord level Ø Bowel and Bladder dysfunction common
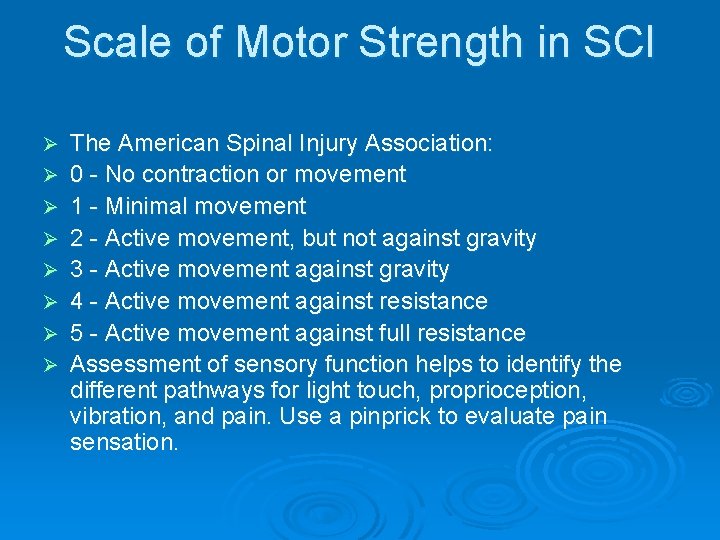
Scale of Motor Strength in SCI Ø The American Spinal Injury Association: l l l Ø 0 - No contraction or movement 1 - Minimal movement 2 - Active movement, but not against gravity 3 - Active movement against gravity 4 - Active movement against resistance 5 - Active movement against full resistance Assessment of sensory function helps to identify the different pathways for light touch, proprioception, vibration, and pain. Use a pinprick to evaluate pain sensation
Types of Spinal Cord Paralysis Ø Ø Ø Depending on the location and the extent of the injury different forms of paralysis can occur. Monoplegia- paralysis of one limb Diplegia- paralysis of both upper or lower limbs Paraplegia- paralysis of both lower limbs, Injury in the thoracic, lumbar, or sacral segments, including the cauda equina and conus medullaris Hemiplegia- paralysis of upper limb, torso and lower leg on one side of the body Tetraplegia (Quadraplegia)- paralysis of all four limbs
History Ø Ø Onset l Acute, subacute, chronic Symptoms l Pain l Weakness l Sensory l Autonomic Past history Family history
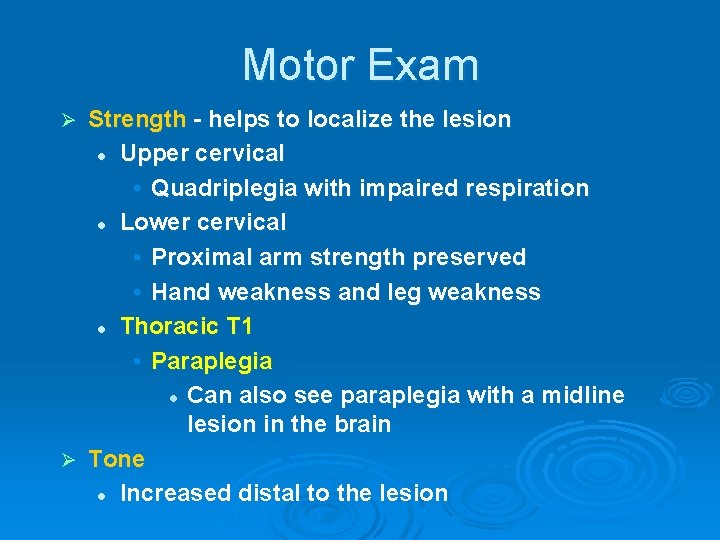
Motor Exam Strength - helps to localize the lesion l Upper cervical • Quadriplegia with impaired respiration l Lower cervical • Proximal arm strength preserved • Hand weakness and leg weakness l Thoracic T 1 • Paraplegia l Can also see paraplegia with a midline lesion in the brain Ø Tone l Increased distal to the lesion Ø
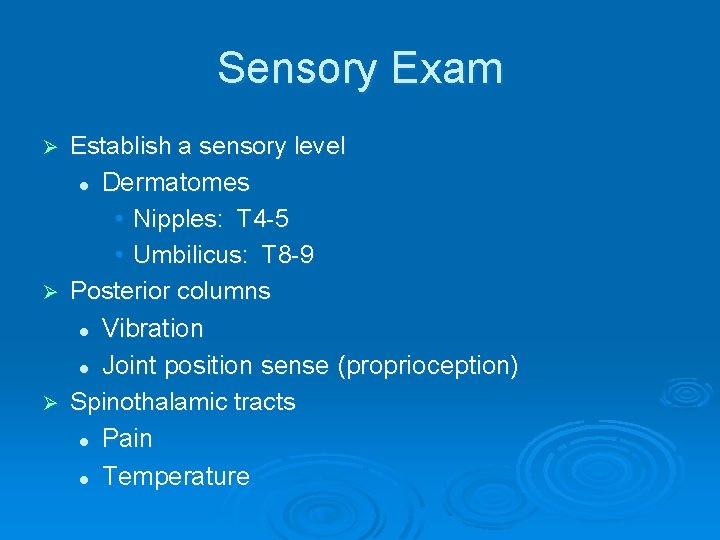
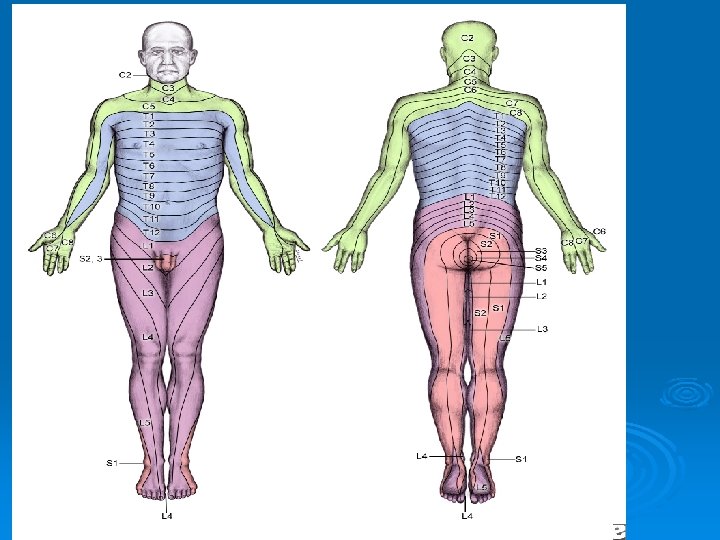
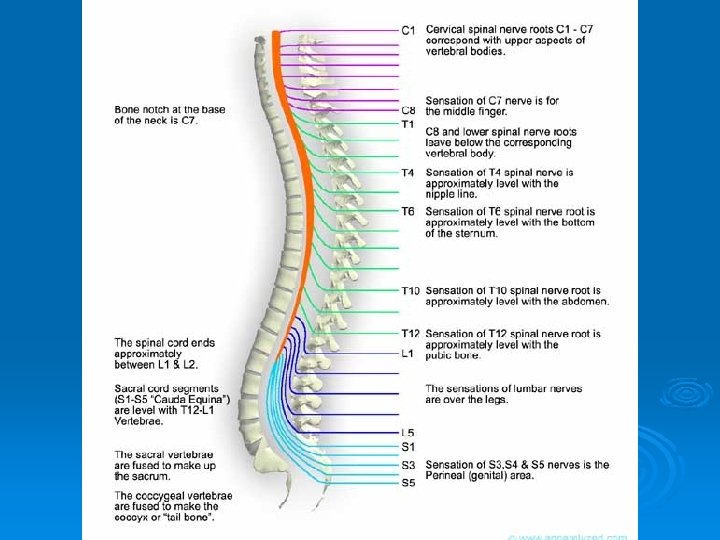
Sensory Exam Establish a sensory level l Dermatomes • Nipples: T 4 -5 • Umbilicus: T 8 -9 Ø Posterior columns l Vibration l Joint position sense (proprioception) Ø Spinothalamic tracts l Pain l Temperature Ø
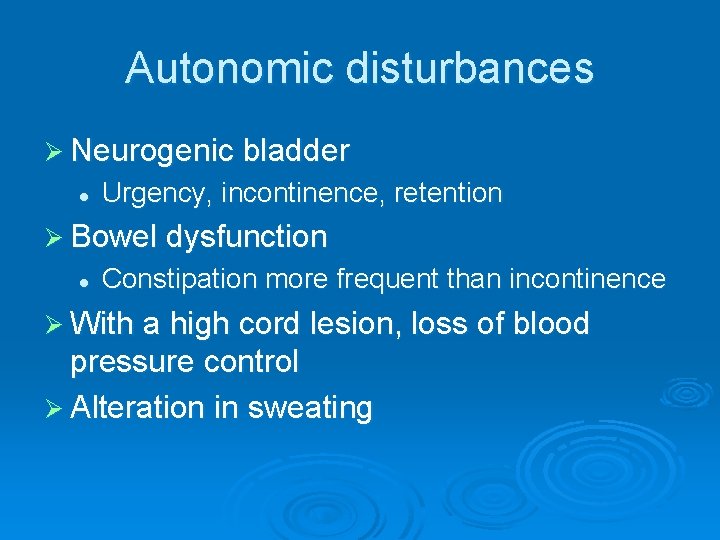
Autonomic disturbances Ø Neurogenic bladder l Urgency, incontinence, retention Ø Bowel dysfunction l Constipation more frequent than incontinence Ø With a high cord lesion, loss of blood pressure control Ø Alteration in sweating
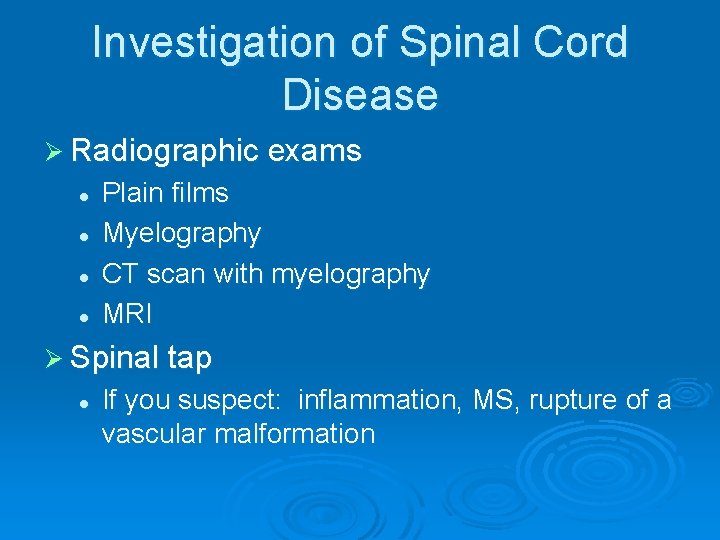
Investigation of Spinal Cord Disease Ø Radiographic exams l l Plain films Myelography CT scan with myelography MRI Ø Spinal tap l If you suspect: inflammation, MS, rupture of a vascular malformation
Etiology of Spinal Cord Disease
Traumatic Spinal Cord Disease Ø 10, 000 new spinal cord injuries per year Ø MVA, sports injuries the most common Ø Victims under 30 yrs old, male>>females Ø Fx/dislocation of vertabrae most likely to occur at: l l l C 5, 6 T 12, L 1 C 1, 2
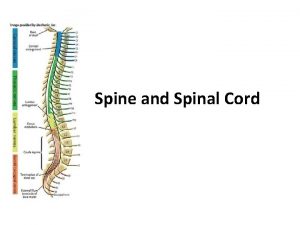
Vertebral column injury, with or without neurological deficits, must always be sought and excluded in a patient with �� Multiple trauma. �� Any injury above the clavicle �� Spine injury �� Cervical spine 55% �� Thoracic spine 15% �� Thoracolumbar junction 15% �� Lumboscaral spine 15%
Ø Spinal cord injury (SCI) is an insult to the spinal cord resulting in a change, either temporary or permanent, in its normal motor, sensory, or autonomic function.
Ø Excessive manipulation and inadequate immobilization of a patient with a spinal cord injury can cause additional neurological damage and worsen the patient’s outcome.
SPINAL CORD INJURIES Caused by sudden trauma
Incidence: Ø Ø Ø Ø Race Whites at 66. 4%, African Americans at 21. 1%, Hispanics at 8. 8%, Asians at 1. 6%, Native Americans at 1. 1%, and others at 1%. Sex The male-to-female ratio of individuals with SCI is 4: 1 Age 50% , aged 16 -30 years. Traumatic SCI < 40 years, Nontraumatic SCI > 40 years.
Associated injuries Ø Bone fractures (29. 3%), Ø Loss of consciousness (17. 8%), Ø Traumatic brain injury affecting emotional/cognitive functioning (11. 5%).
Mechanism: Destruction from direct trauma Ø Compression by bone fragments, hematoma, or disk material Ø Ischemia from damage or impingement on the spinal arteries Ø Edema could ensue subsequent to any of these types of damage. The different clinical presentations of the above causes of tissue damage are explained further below. Ø
Spinal Shock An immediate loss of reflex function, called areflexia, below the level of injury Ø Signs: Ø l l l Ø Slow heart rate Low blood pressure Flaccid paralysis of skeletal muscles Loss of somatic sensations Urinary bladder dysfunction Spinal shock may begin within an hour after injury and last from several minutes to several months, after which reflex activity gradually returns
Neurogenic shock Ø Neurogenic shock is manifested by the triad of hypotension, bradycardia, and hypothermia. Ø Shock tends to occur more commonly in injuries above T 6, secondary to the disruption of the sympathetic outflow from T 1 -L 2 and to unopposed vagal tone, leading to decrease in vascular resistance with associated vascular dilatation. Ø Neurogenic shock needs to be differentiated from spinal and hypovolemic shock. Hypovolemic shock tends to be associated with tachycardia
Spinal Shock An immediate loss of reflex function, called areflexia, below the level of injury Ø Signs: Ø l l l Ø Slow heart rate Low blood pressure Flaccid paralysis of skeletal muscles Loss of somatic sensations Urinary bladder dysfunction Spinal shock may begin within an hour after injury and last from several minutes to several months, after which reflex activity gradually returns
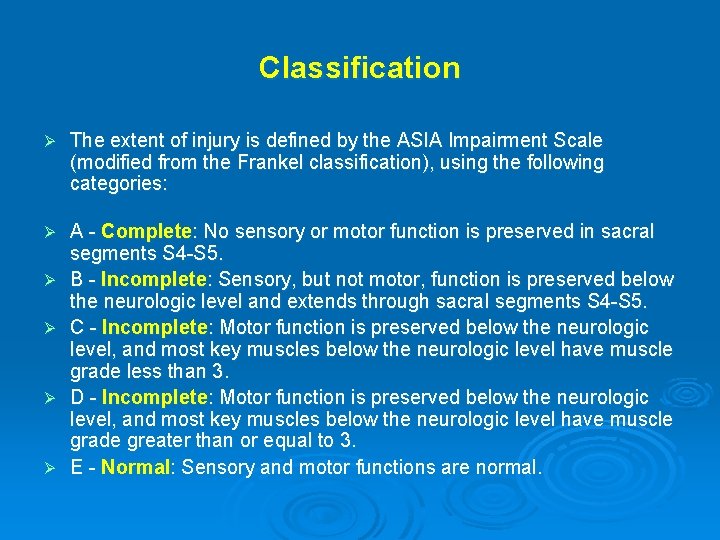
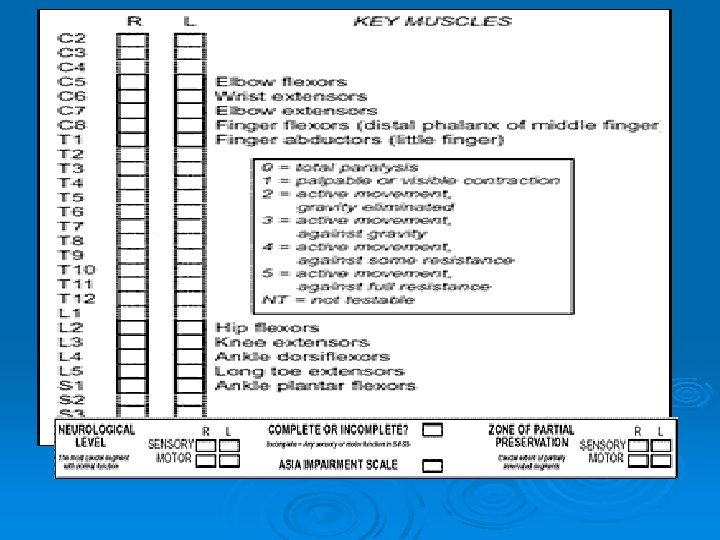
Classification Ø The extent of injury is defined by the ASIA Impairment Scale (modified from the Frankel classification), using the following categories: Ø A - Complete: No sensory or motor function is preserved in sacral segments S 4 -S 5. B - Incomplete: Sensory, but not motor, function is preserved below the neurologic level and extends through sacral segments S 4 -S 5. C - Incomplete: Motor function is preserved below the neurologic level, and most key muscles below the neurologic level have muscle grade less than 3. D - Incomplete: Motor function is preserved below the neurologic level, and most key muscles below the neurologic level have muscle grade greater than or equal to 3. E - Normal: Sensory and motor functions are normal. Ø Ø
Spinal Cord Syndromes can be classified into either complete or incomplete categories Ø Complete – characterized as complete loss of motor and sensory function below the level of the traumatic lesion Ø Incomplete – characterized by variable neurological findings with partial loss of sensory and/or motor function below the lesion
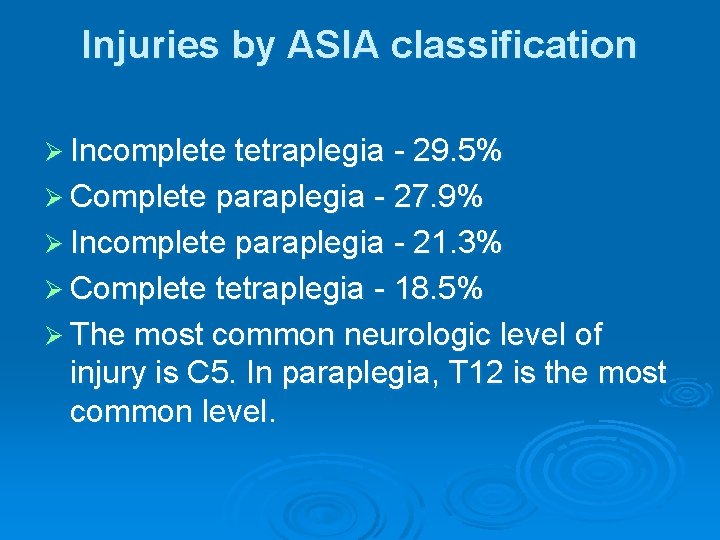
Injuries by ASIA classification Ø Incomplete tetraplegia - 29. 5% Ø Complete paraplegia - 27. 9% Ø Incomplete paraplegia - 21. 3% Ø Complete tetraplegia - 18. 5% Ø The most common neurologic level of injury is C 5. In paraplegia, T 12 is the most common level.
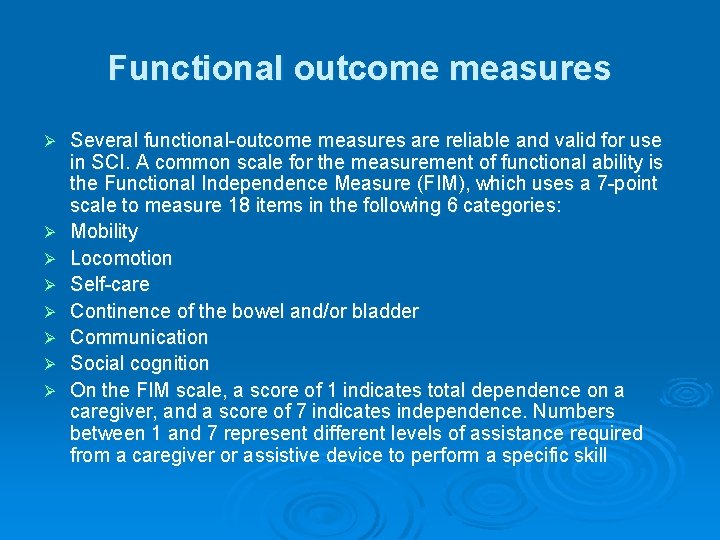
Functional outcome measures Ø Ø Ø Ø Several functional-outcome measures are reliable and valid for use in SCI. A common scale for the measurement of functional ability is the Functional Independence Measure (FIM), which uses a 7 -point scale to measure 18 items in the following 6 categories: Mobility Locomotion Self-care Continence of the bowel and/or bladder Communication Social cognition On the FIM scale, a score of 1 indicates total dependence on a caregiver, and a score of 7 indicates independence. Numbers between 1 and 7 represent different levels of assistance required from a caregiver or assistive device to perform a specific skill
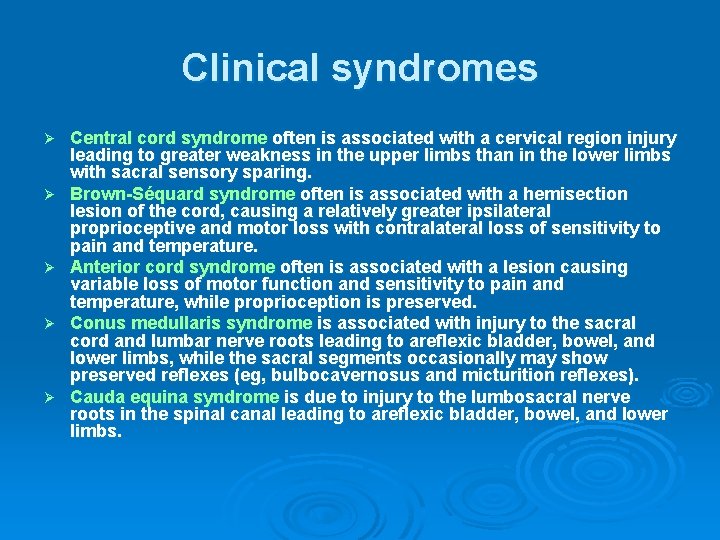
Clinical syndromes Ø Ø Ø Central cord syndrome often is associated with a cervical region injury leading to greater weakness in the upper limbs than in the lower limbs with sacral sensory sparing. Brown-Séquard syndrome often is associated with a hemisection lesion of the cord, causing a relatively greater ipsilateral proprioceptive and motor loss with contralateral loss of sensitivity to pain and temperature. Anterior cord syndrome often is associated with a lesion causing variable loss of motor function and sensitivity to pain and temperature, while proprioception is preserved. Conus medullaris syndrome is associated with injury to the sacral cord and lumbar nerve roots leading to areflexic bladder, bowel, and lower limbs, while the sacral segments occasionally may show preserved reflexes (eg, bulbocavernosus and micturition reflexes). Cauda equina syndrome is due to injury to the lumbosacral nerve roots in the spinal canal leading to areflexic bladder, bowel, and lower limbs.
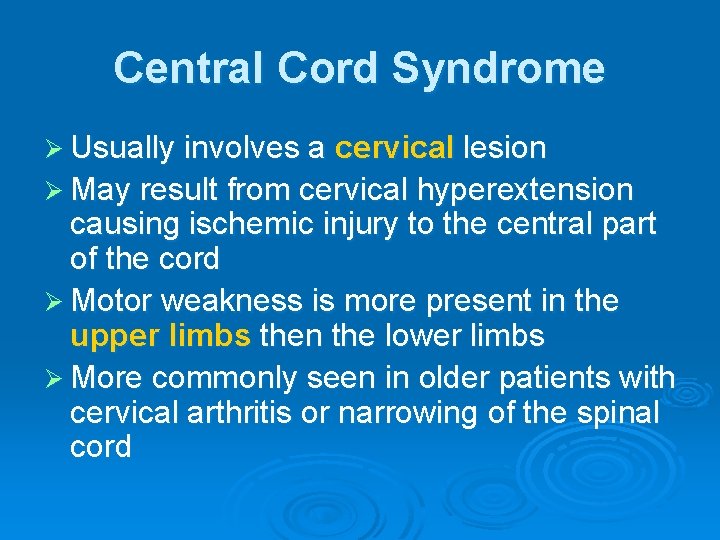
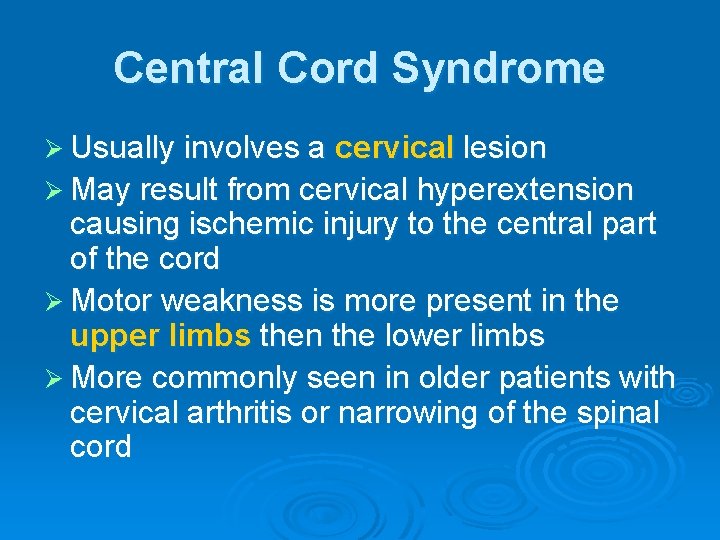
Central Cord Syndrome Ø Usually involves a cervical lesion Ø May result from cervical hyperextension causing ischemic injury to the central part of the cord Ø Motor weakness is more present in the upper limbs then the lower limbs Ø More commonly seen in older patients with cervical arthritis or narrowing of the spinal cord
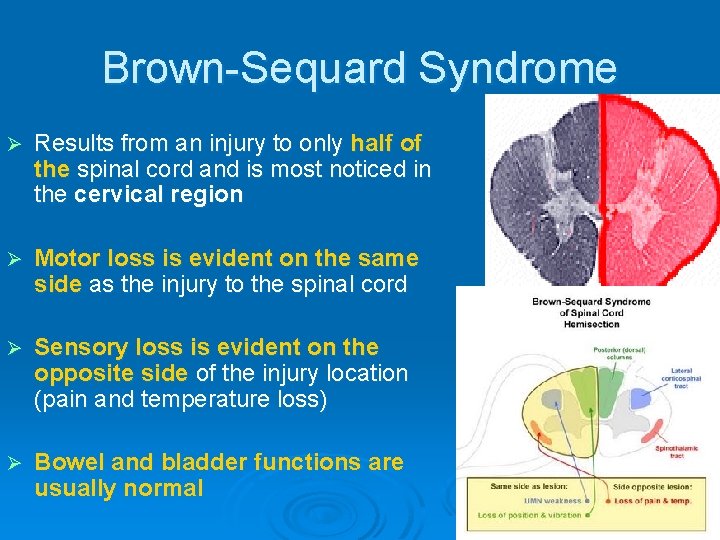
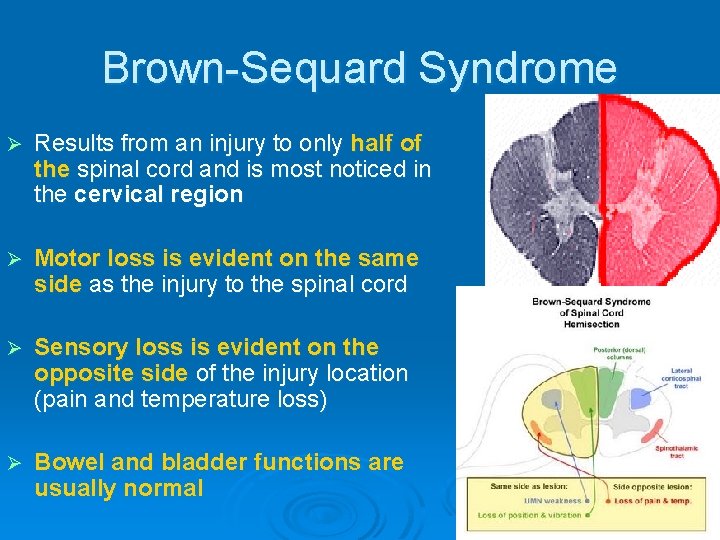
Brown-Sequard Syndrome Ø Results from an injury to only half of the spinal cord and is most noticed in the cervical region Ø Motor loss is evident on the same side as the injury to the spinal cord Ø Sensory loss is evident on the opposite side of the injury location (pain and temperature loss) Ø Bowel and bladder functions are usually normal
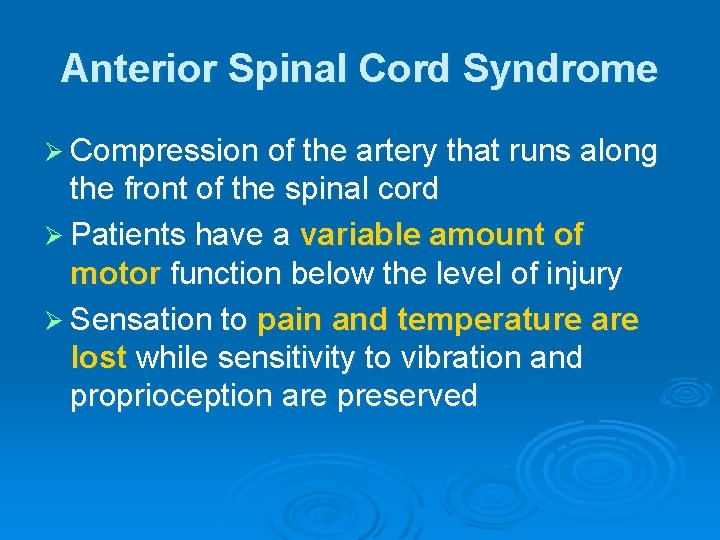
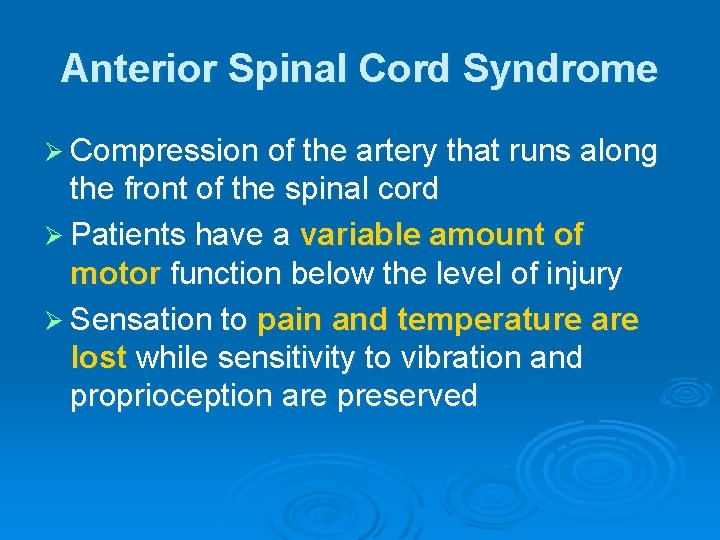
Anterior Spinal Cord Syndrome Ø Compression of the artery that runs along the front of the spinal cord Ø Patients have a variable amount of motor function below the level of injury Ø Sensation to pain and temperature are lost while sensitivity to vibration and proprioception are preserved
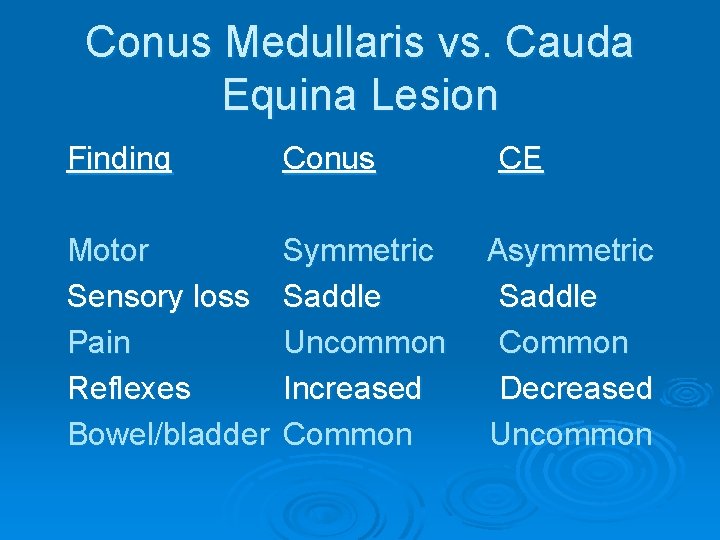
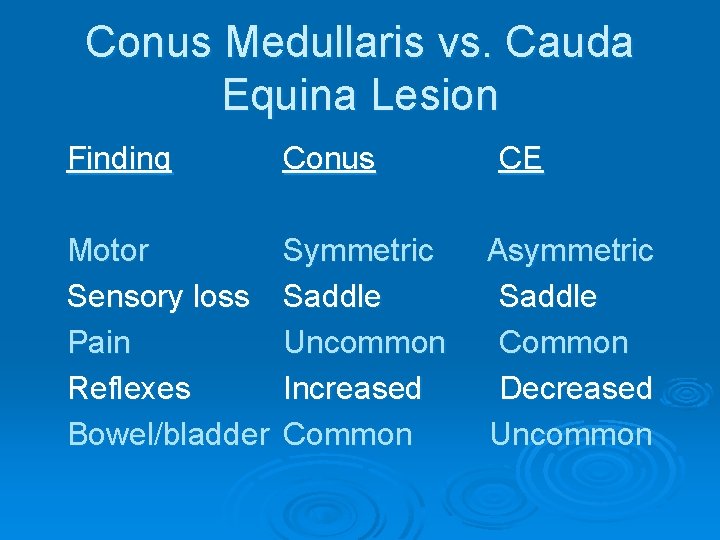
Conus Medullaris vs. Cauda Equina Lesion Finding Conus Motor Sensory loss Pain Reflexes Bowel/bladder Symmetric Saddle Uncommon Increased Common CE Asymmetric Saddle Common Decreased Uncommon
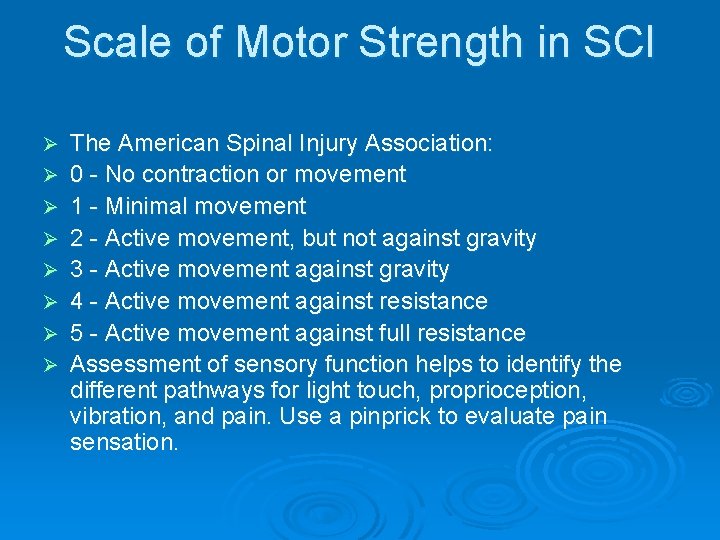
Scale of Motor Strength in SCI Ø Ø Ø Ø The American Spinal Injury Association: 0 - No contraction or movement 1 - Minimal movement 2 - Active movement, but not against gravity 3 - Active movement against gravity 4 - Active movement against resistance 5 - Active movement against full resistance Assessment of sensory function helps to identify the different pathways for light touch, proprioception, vibration, and pain. Use a pinprick to evaluate pain sensation.
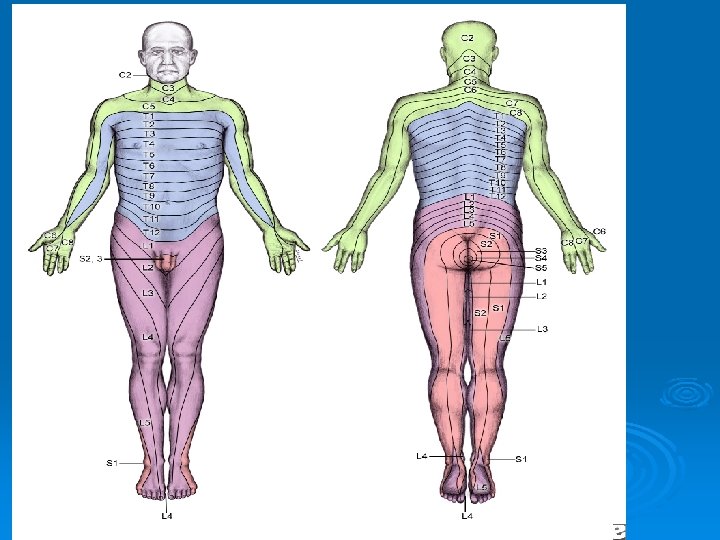
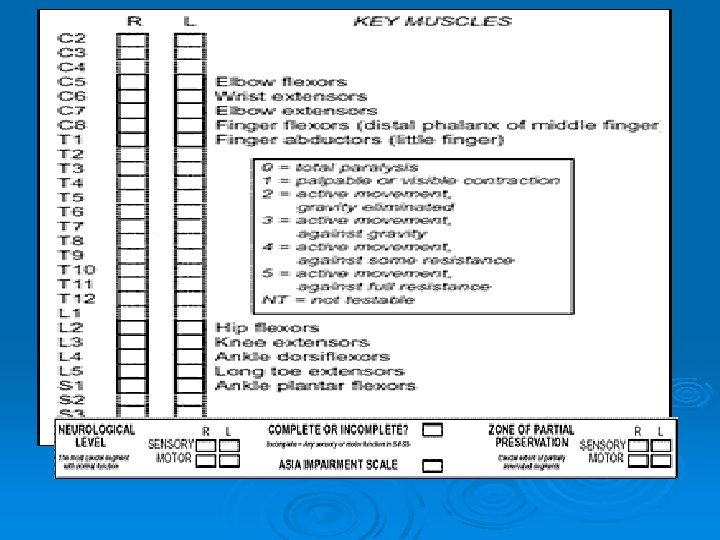
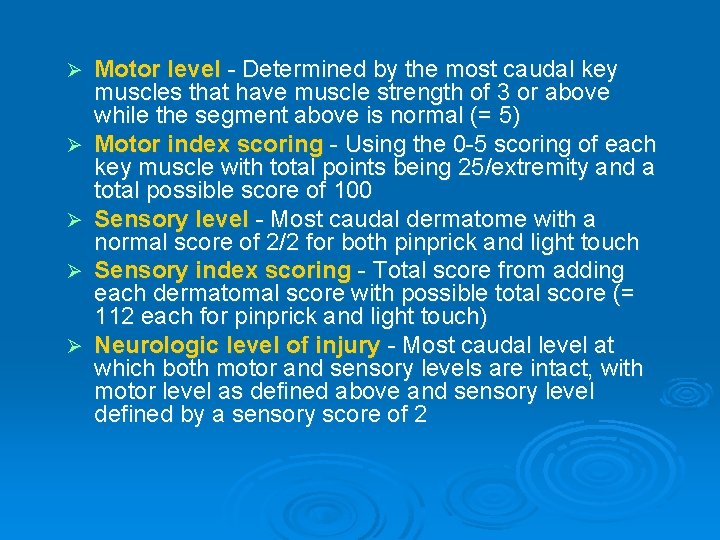
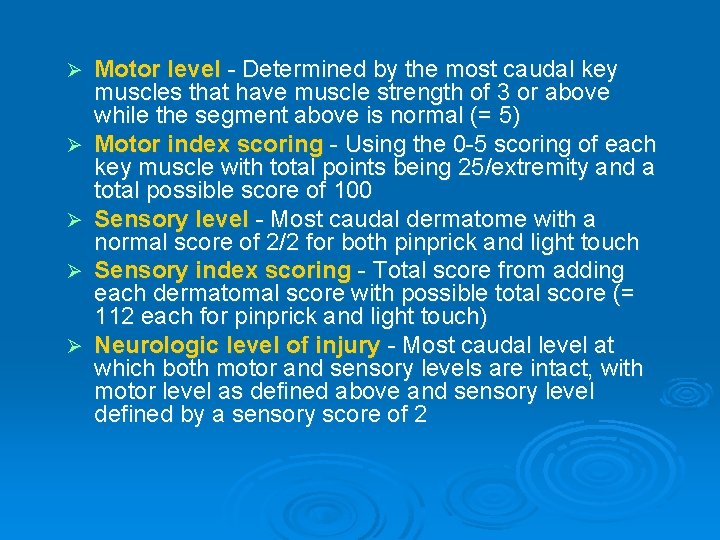
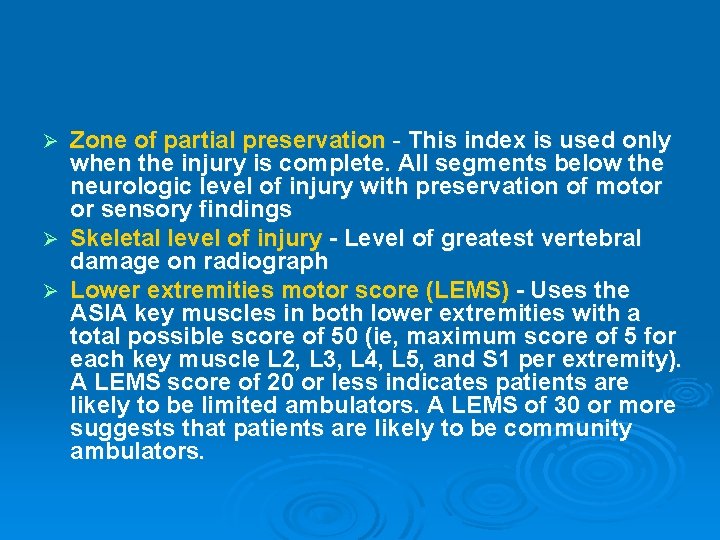
Ø Ø Ø Motor level - Determined by the most caudal key muscles that have muscle strength of 3 or above while the segment above is normal (= 5) Motor index scoring - Using the 0 -5 scoring of each key muscle with total points being 25/extremity and a total possible score of 100 Sensory level - Most caudal dermatome with a normal score of 2/2 for both pinprick and light touch Sensory index scoring - Total score from adding each dermatomal score with possible total score (= 112 each for pinprick and light touch) Neurologic level of injury - Most caudal level at which both motor and sensory levels are intact, with motor level as defined above and sensory level defined by a sensory score of 2
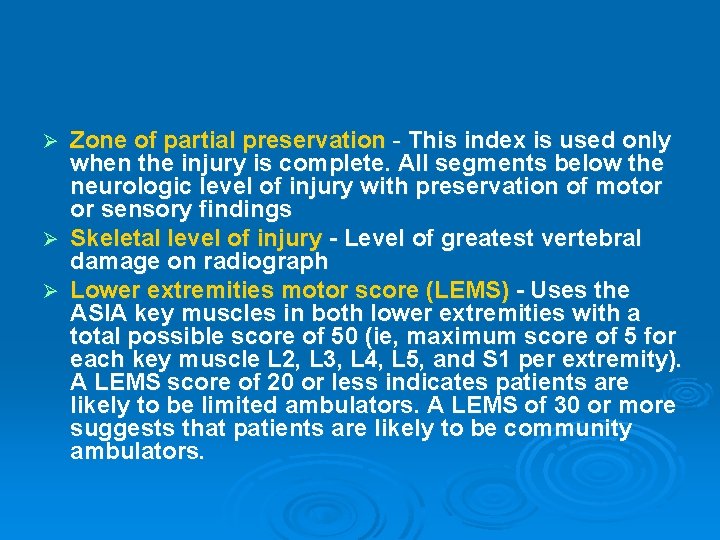
Zone of partial preservation - This index is used only when the injury is complete. All segments below the neurologic level of injury with preservation of motor or sensory findings Ø Skeletal level of injury - Level of greatest vertebral damage on radiograph Ø Lower extremities motor score (LEMS) - Uses the ASIA key muscles in both lower extremities with a total possible score of 50 (ie, maximum score of 5 for each key muscle L 2, L 3, L 4, L 5, and S 1 per extremity). A LEMS score of 20 or less indicates patients are likely to be limited ambulators. A LEMS of 30 or more suggests that patients are likely to be community ambulators. Ø
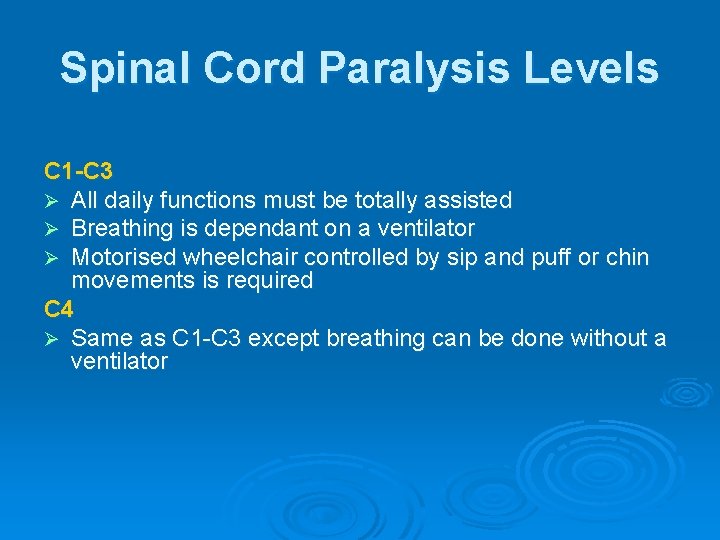
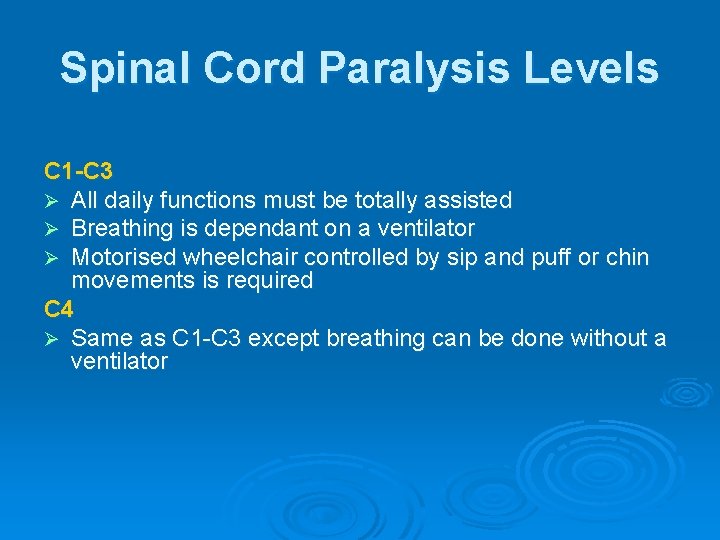
Spinal Cord Paralysis Levels C 1 -C 3 Ø All daily functions must be totally assisted Ø Breathing is dependant on a ventilator Ø Motorised wheelchair controlled by sip and puff or chin movements is required C 4 Ø Same as C 1 -C 3 except breathing can be done without a ventilator
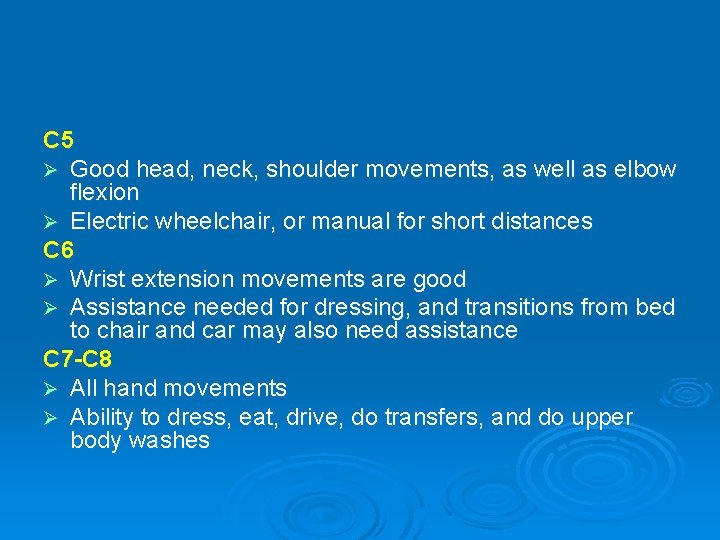
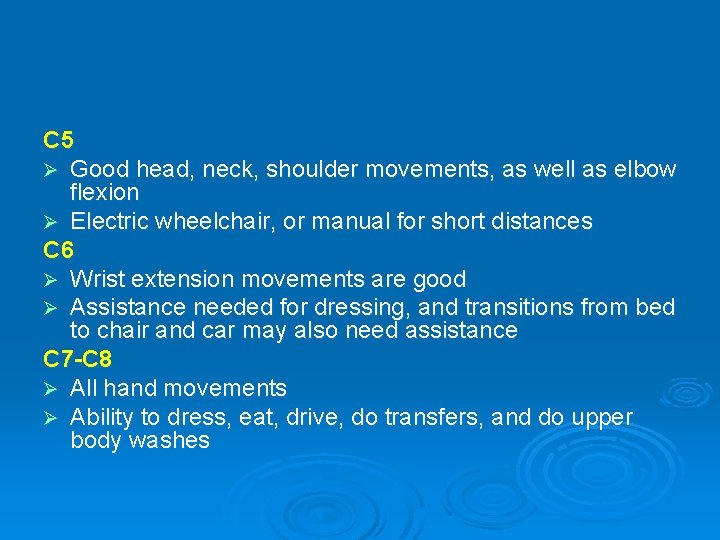
C 5 Ø Good head, neck, shoulder movements, as well as elbow flexion Ø Electric wheelchair, or manual for short distances C 6 Ø Wrist extension movements are good Ø Assistance needed for dressing, and transitions from bed to chair and car may also need assistance C 7 -C 8 Ø All hand movements Ø Ability to dress, eat, drive, do transfers, and do upper body washes

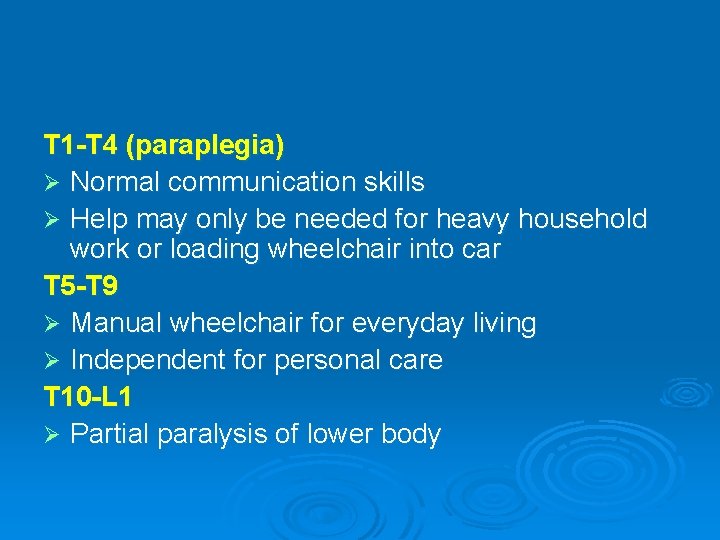
T 1 -T 4 (paraplegia) Ø Normal communication skills Ø Help may only be needed for heavy household work or loading wheelchair into car T 5 -T 9 Ø Manual wheelchair for everyday living Ø Independent for personal care T 10 -L 1 Ø Partial paralysis of lower body
L 2 -S 5 Ø Some knee, hip and foot movements with possible slow difficult walking with assistance or aids Ø Only heavy home maintenance and hard cleaning will need assistance
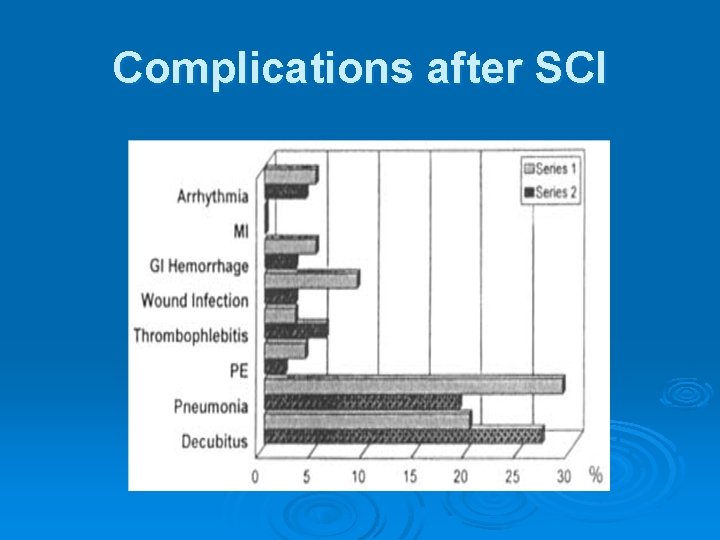
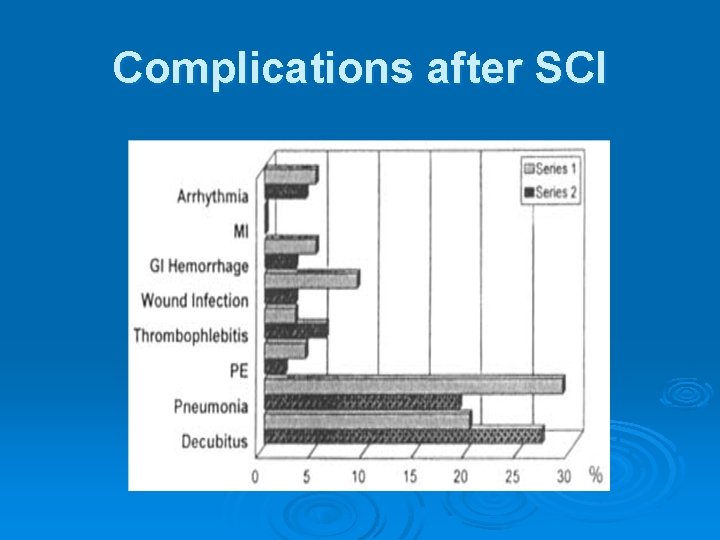
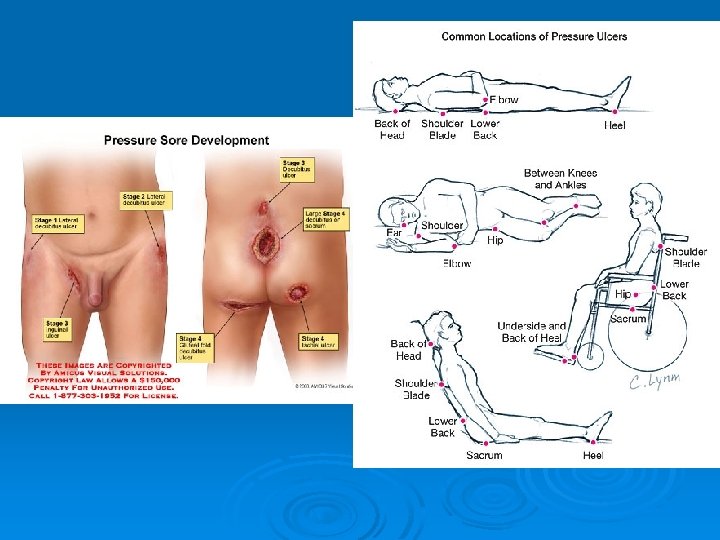
Complications after SCI

DVT
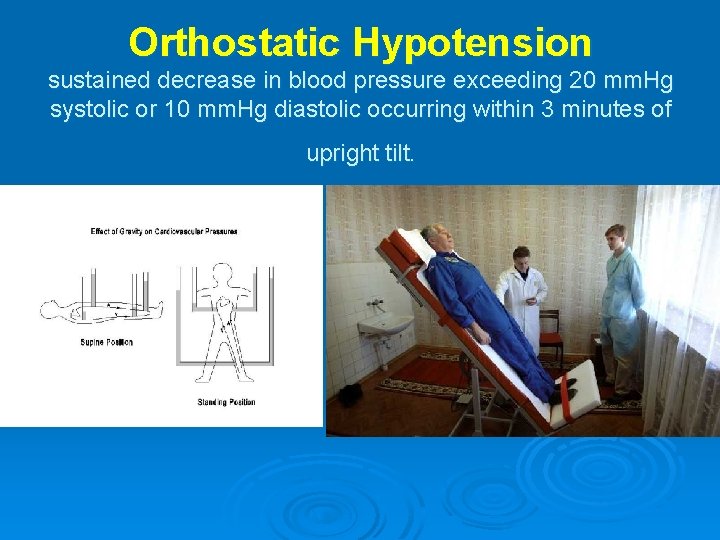
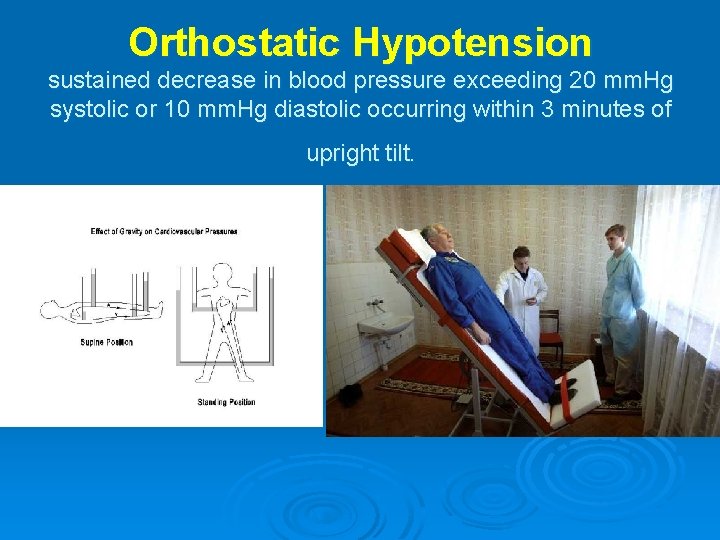
Orthostatic Hypotension sustained decrease in blood pressure exceeding 20 mm. Hg systolic or 10 mm. Hg diastolic occurring within 3 minutes of upright tilt.
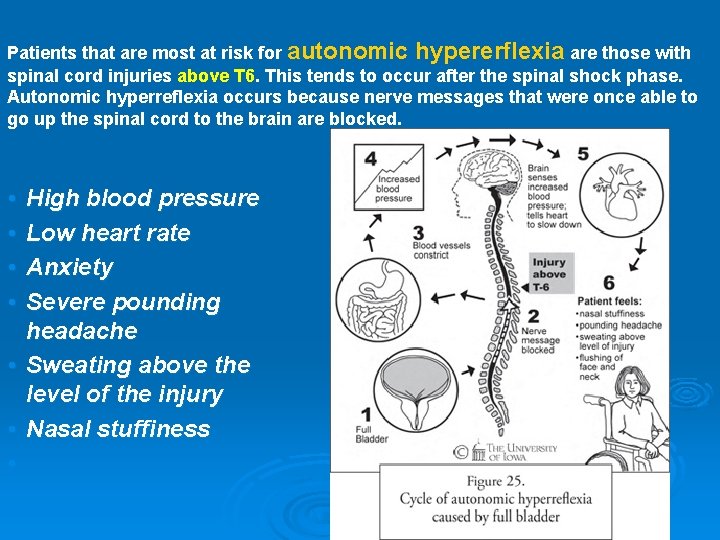
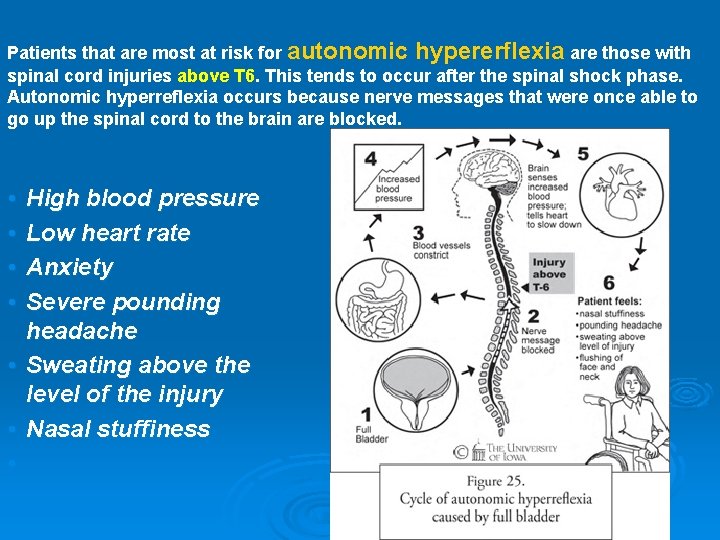
Patients that are most at risk for autonomic hypererflexia are those with spinal cord injuries above T 6. This tends to occur after the spinal shock phase. Autonomic hyperreflexia occurs because nerve messages that were once able to go up the spinal cord to the brain are blocked. • • High blood pressure Low heart rate Anxiety Severe pounding headache • Sweating above the level of the injury • Nasal stuffiness •
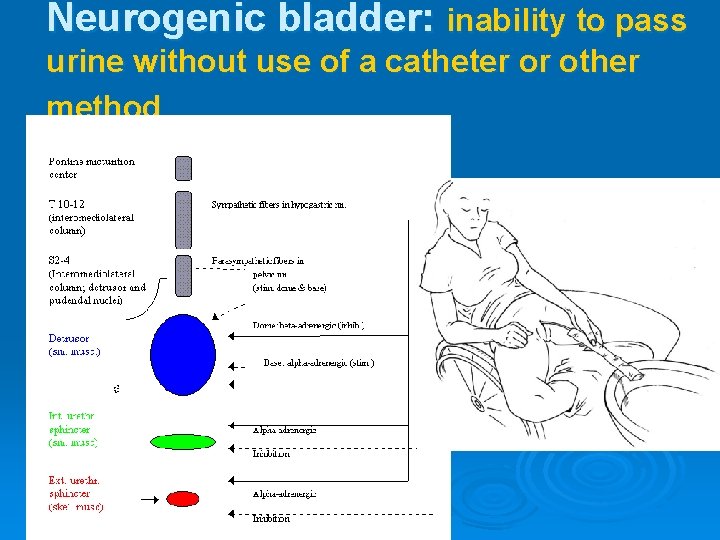
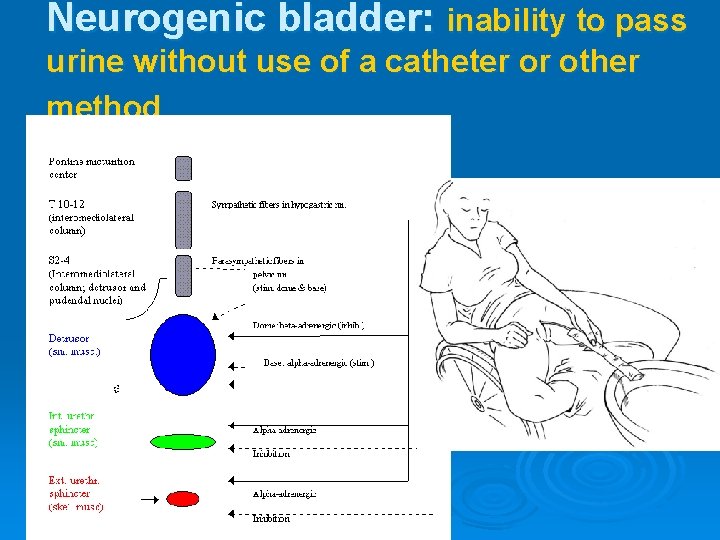
Neurogenic bladder: inability to pass urine without use of a catheter or other method
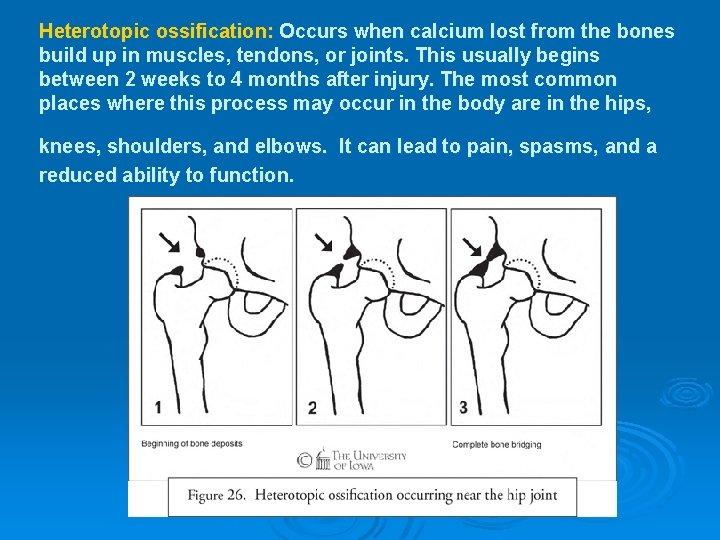
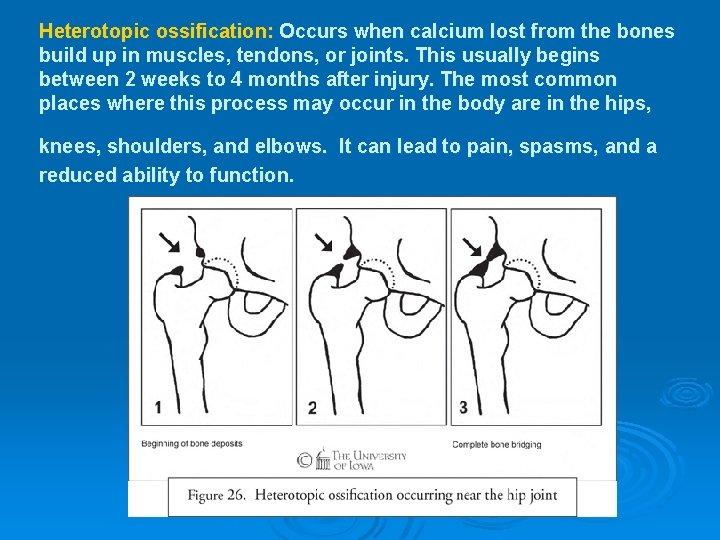
Heterotopic ossification: Occurs when calcium lost from the bones build up in muscles, tendons, or joints. This usually begins between 2 weeks to 4 months after injury. The most common places where this process may occur in the body are in the hips, knees, shoulders, and elbows. It can lead to pain, spasms, and a reduced ability to function.



Treatment Ø Ø Ø Fifty years ago, a spinal cord injury was usually fatal. At that time, most injuries were severe, complete injuries and little treatment was available. Today, there's still no way to reverse damage to the spinal cord. But modern injuries are usually less severe, partial spinal cord injuries. And advances in recent years have improved the recovery of people with a spinal cord injury and significantly reduced the amount of time survivors must spend in the hospital. Researchers are working on new treatments, including innovative treatments, prostheses and medications that may promote nerve cell regeneration or improve the function of the nerves that remain after a spinal cord injury. In the meantime, spinal cord injury treatment focuses on preventing further injury and enabling people with a spinal cord injury to return to an active and productive life within the limits of their disability. This requires urgent emergency attention and ongoing care.
Emergency actions Ø Urgent medical attention is critical to minimizing the long-term effects of any head or neck trauma. So treatment for a spinal cord injury often begins at the scene of the accident. Ø Attend to three immediate concerns: l l l Maintaining the ability to breathe Keeping the patient from going into shock Immobilizing the neck to prevent further spinal cord damage
Three procedures are crucial in treating spinal cord injuries: Ø Treatment with the steroid medication methylprednisolone to reduce swelling. Used within 8 hours after an injury, this medication may help prevent nerve damage. Ø Ø Relief of pressure on the spine using surgery or traction (a mechanical system of weights). Ø Treatment to stabilize the spine using screws, metal plates, and other devices. This is often done during an operation. Sometimes, traction may be used instead.
Ongoing care Ø Medications: Ø To control pain and muscle spasticity, İmprove bladder control, bowel control and sexual functioning. Ø Short-term medications from time to time, such as antibiotics for urinary tract infections. Ø
SCI Rehabilitation: Physiotherapy for patients with spinal cord injuries can include; Ø exercises and stretches Ø joint care Ø pain control Ø breathing exercises and chest clearance techniques Ø anticipating and minimising secondary complications Ø

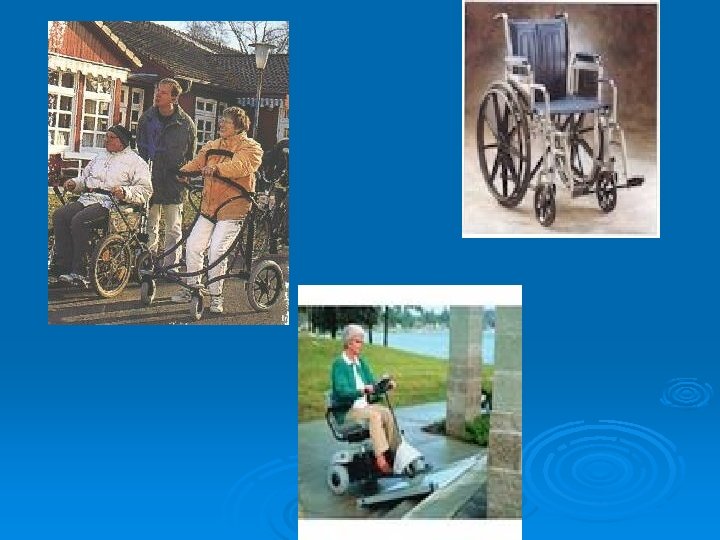
Rehabilitation provision of equipment, orthoses, and wheelchairs Ø advice on handling techniques Ø teaching how to use specialised exercise equipment Ø teach transfers (getting in and out of a wheelchair, bed, car, shower/bath and onto and off a toilet). Ø teaching wheelchair skills Ø hydrotherapy treatment Ø referral to appropriate health professionals Ø
The effects of physiotherapy can be: Ø increased quality of life Ø increased independence Ø increased muscle strength Ø increased energy levels Ø reduced pain and muscle spasms Ø reduced stiffness Ø reduced risk of chest infections
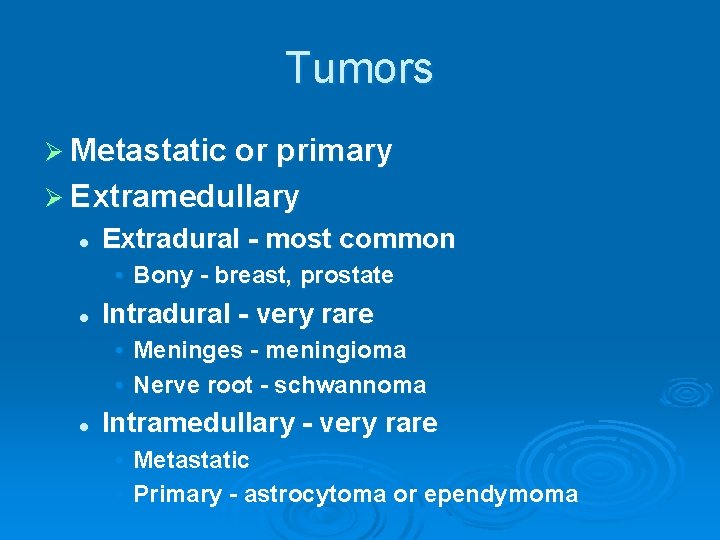
Tumors Ø Metastatic or primary Ø Extramedullary l Extradural - most common • Bony - breast, prostate l Intradural - very rare • Meninges - meningioma • Nerve root - schwannoma l Intramedullary - very rare • Metastatic • Primary - astrocytoma or ependymoma
Transverse myelitis Ø Inflammation of the spinal cord l l l Post-infectious Post-vaccinial Multiple sclerosis Ø Pain at level of lesion may preceed onset of weakness/sensory change / b&b disturbance
B 12 Deficiency Ø Subacute combined degeneration of the cord Ø B 12 deficiency l l malabsorption of B 12 secondary to pernicious anemia or surgery insufficient dietary intake - vegan Ø Posterior columns and CST involvement with a superimposed peripheral neuropathy
Infections Involving the Spinal Cord Ø Polio l only the anterior horn cells are infected Ø Tabes dorsalis l l l dorsal root ganglia and dorsal columns are involved tertiary syphillis sensory ataxia, “lightening pains” Ø HIV myelopathy l mimics B 12 deficiency Ø HTLV-1 myelopathy - tropical spastic
Multiple Sclerosis Ø Demyelination is the underlying pathology Ø Cord disease can be presenting feature of MS or occur at any time during the course of the disease Ø Lesion can be at any level of the cord l l Patchy Transverse Ø Devic’s syndrome or myelitis optica l Transverse myelitis with optic neuritis
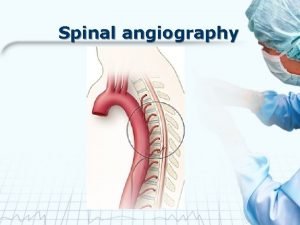
Vascular Diseases of the Spinal Cord Ø Infarcts Ø Anterior spinal artery infarct
Vascular Diseases of the Spinal Cord Arteriovenous malformation (AVM) and venous angiomas l Both occur in primarily the thoracic cord l May present either acutely, subacutely or chronically (act as a compressive lesion) l Can cause recurrent symptoms l If they bleed • Associated with pain and bloody CSF l Notoriously difficult to diagnose Ø Hematoma - trauma, occasionally tumor Ø
Other Disease of the Spinal Cord Ø Ø Hereditary spastic paraparesis l Usually autosomal dominant Infectious process of the vertabrae l TB, bacterial Herniated disc with cord compression l Most herniated discs are lateral and only compress a nerve root Degenerative disease of the vertabrae l Cervical spondylosis with a myelopathy l Spinal stenosis
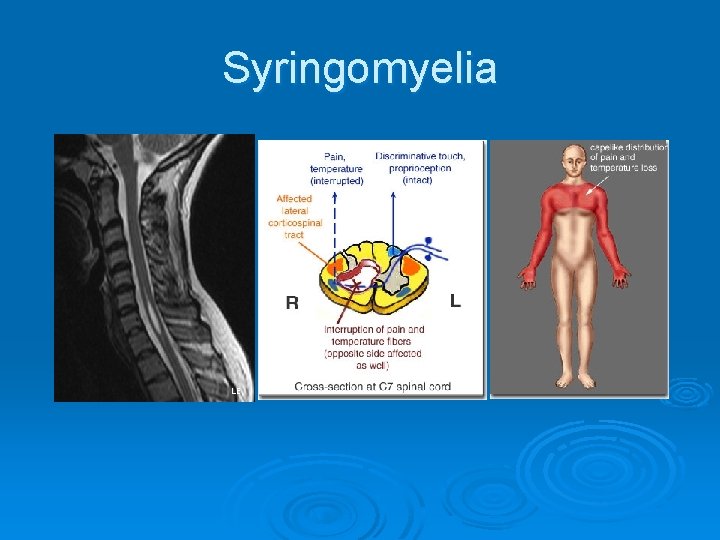
Syringomyelia Ø Ø Fluid filled cavitation in the center of the cord Cervical cord most common site l Loss of pain and temperature related to the crossing fibers occurs early • cape like sensory loss l Weakness of muscles in arms with atrophy and hyporeflexia (AHC) l Later - CST involvement with brisk reflexes in the legs, spasticity, and weakness May occur as a late sequelae to trauma Can see in association with Arnold Chiari malformation
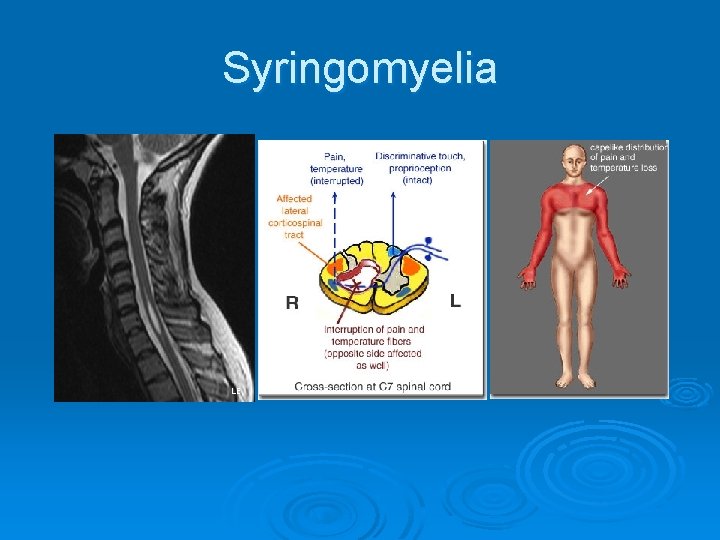
Syringomyelia

 Our old trusty truck cranial nerves
Our old trusty truck cranial nerves Spine meninges
Spine meninges Lateral pectoral nerve
Lateral pectoral nerve Spinal cord layers
Spinal cord layers Dermatome map
Dermatome map Spinal cord and brain
Spinal cord and brain Brain and spinal cord nervous system
Brain and spinal cord nervous system Somi brace
Somi brace Autonomic
Autonomic Spinal cord denticulate ligament
Spinal cord denticulate ligament Spinal cord structures
Spinal cord structures Causes of spinal cord compression
Causes of spinal cord compression Spinal cord tumors
Spinal cord tumors Pons function
Pons function Posterior median furrow
Posterior median furrow Spinal cord extends from
Spinal cord extends from Christopher reeve spinal cord injury level
Christopher reeve spinal cord injury level Dorsal nerve cord vs notochord
Dorsal nerve cord vs notochord What covers spinal cord
What covers spinal cord Slidetodoc
Slidetodoc Spinal cord organization
Spinal cord organization Plexus brachialis
Plexus brachialis Osd sindrom
Osd sindrom What is the spinal cord made of
What is the spinal cord made of Spinal angiogram anatomy
Spinal angiogram anatomy Spinal cord
Spinal cord Spinal cord
Spinal cord Stretch reflex
Stretch reflex Functions of spinal cord ppt
Functions of spinal cord ppt Eat well live well with spinal cord injury
Eat well live well with spinal cord injury The spinebreal code
The spinebreal code Pain pathway spinal cord
Pain pathway spinal cord Low back rom
Low back rom Spinal cord cross section
Spinal cord cross section Posterior spinal cord
Posterior spinal cord Spinal cord injury protocol
Spinal cord injury protocol Spinal cord structure
Spinal cord structure Spinal cord injury shoulder exercises
Spinal cord injury shoulder exercises Tendon histology
Tendon histology Articularis cubiti
Articularis cubiti Spinal cord
Spinal cord Phylum of frog
Phylum of frog Pyramidal tract
Pyramidal tract Spinal cord
Spinal cord Spinal cord nerve anatomy
Spinal cord nerve anatomy Spinal cord anterior
Spinal cord anterior Functional unit of nervous system
Functional unit of nervous system Spinal cord
Spinal cord Spinomedullary junction
Spinomedullary junction Gray commissure
Gray commissure Site of somatic motor neuron cell bodies
Site of somatic motor neuron cell bodies Objectives of nervous system
Objectives of nervous system Nerve regions of the body
Nerve regions of the body Boston scientific spinal cord stimulator
Boston scientific spinal cord stimulator Lumbar enlargement
Lumbar enlargement Spinal cord injury rehabilitation st. louis
Spinal cord injury rehabilitation st. louis Spinal cord
Spinal cord Mcb 160
Mcb 160 Spinal cord
Spinal cord Spinal cord muscles
Spinal cord muscles Spinal cord venous drainage
Spinal cord venous drainage Spinal shock symptoms
Spinal shock symptoms Spinal cord development
Spinal cord development Spinal cord vibration
Spinal cord vibration Spinal cord compression nice
Spinal cord compression nice Spinal cord parts
Spinal cord parts Spinal cord spasticity
Spinal cord spasticity Nerves branching beyond the spinal cord into the body
Nerves branching beyond the spinal cord into the body Communicable disease and non communicable disease
Communicable disease and non communicable disease Chapter 28 head and spine injuries
Chapter 28 head and spine injuries Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Thoracic facet joint pain referral patterns
Thoracic facet joint pain referral patterns Harborside spine and sports
Harborside spine and sports Back pain kings park
Back pain kings park Sentinel injuries in infants are
Sentinel injuries in infants are Sway back posture
Sway back posture Dorsolumbar spine
Dorsolumbar spine