Sepsis Severe Sepsis Septic Shock Meral SNMEZOLU Prof

- Slides: 86
Sepsis, Severe Sepsis & Septic Shock Meral SÖNMEZOĞLU, Prof Yeditepe University Hospital Infectious Diseases Department 1
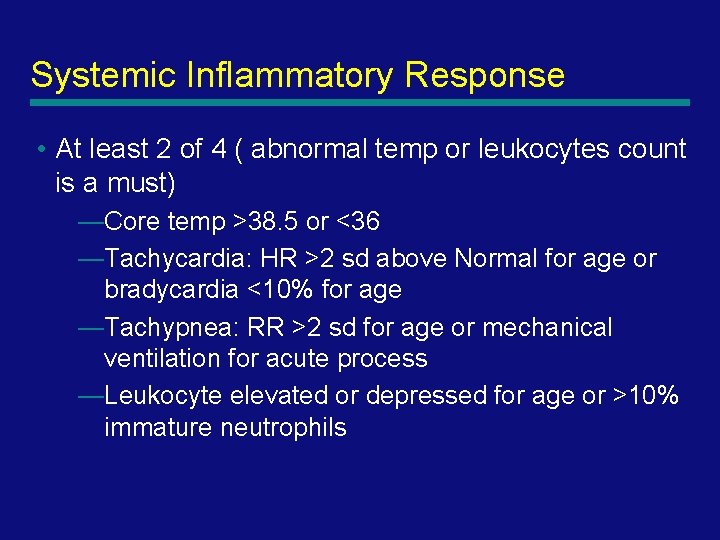
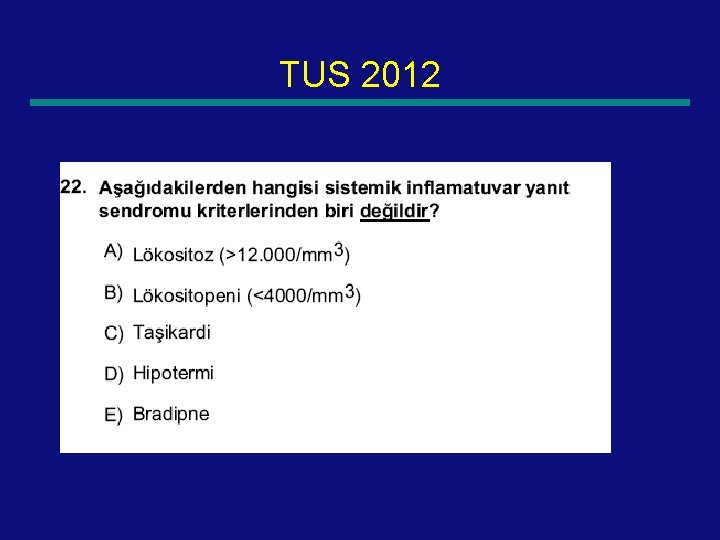
Systemic Inflammatory Response • At least 2 of 4 ( abnormal temp or leukocytes count is a must) —Core temp >38. 5 or <36 —Tachycardia: HR >2 sd above Normal for age or bradycardia <10% for age —Tachypnea: RR >2 sd for age or mechanical ventilation for acute process —Leukocyte elevated or depressed for age or >10% immature neutrophils 2
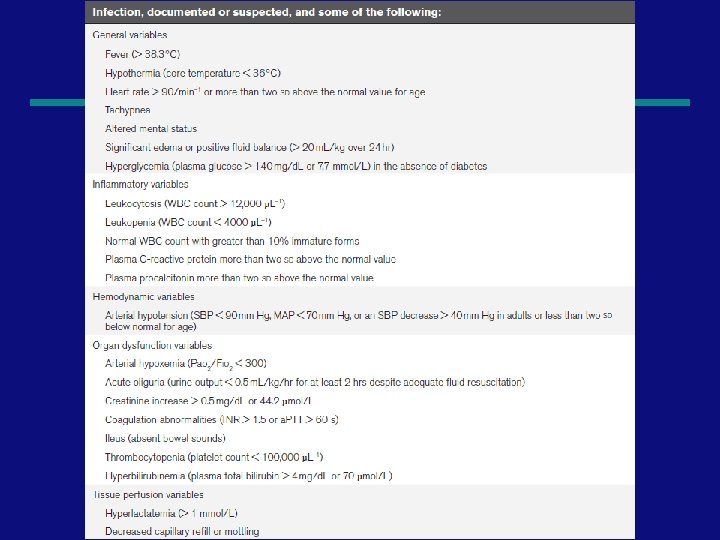
Definitions • Infection: Suspected or proven caused by any pathogen Or clinical syndrome associated with high probability of infection • Sepsis: SIRS in the presence of or as a result of suspected of proven infection 3
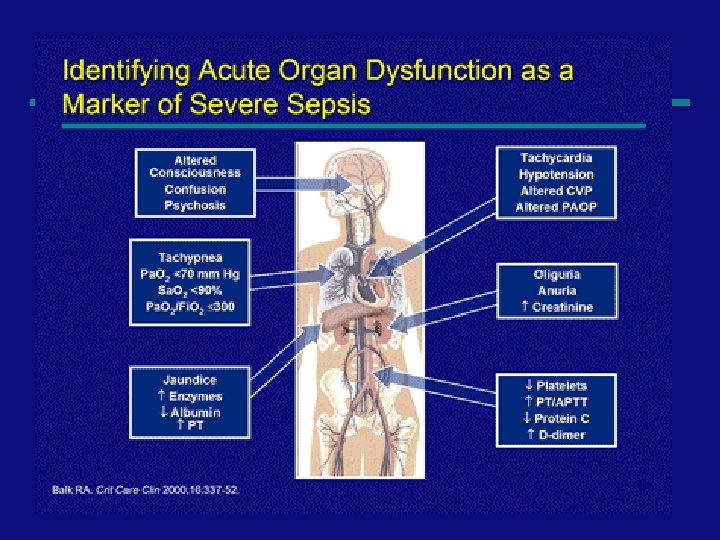
Definitions • Severe Sepsis: sepsis + one —Cardiovascular dysfunction —ARDS —OR 2 or more other organ dysfunctions • Septic shock —Sepsis and cardiovascular organ dysfunction 4
5
The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) Mervyn Singer, MD, FRCP 1; Clifford S. Deutschman, MD, MS 2; Christopher Warren Seymour, MD, MSc 3 JAMA. 2016; 315(8): 801 -810 6
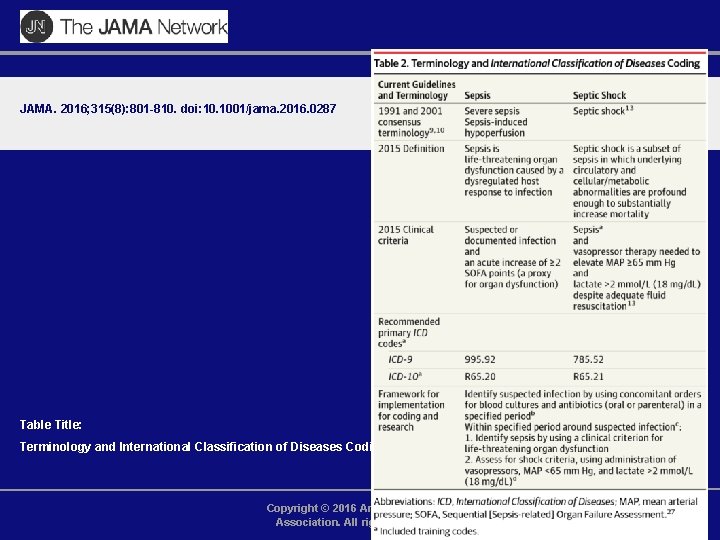
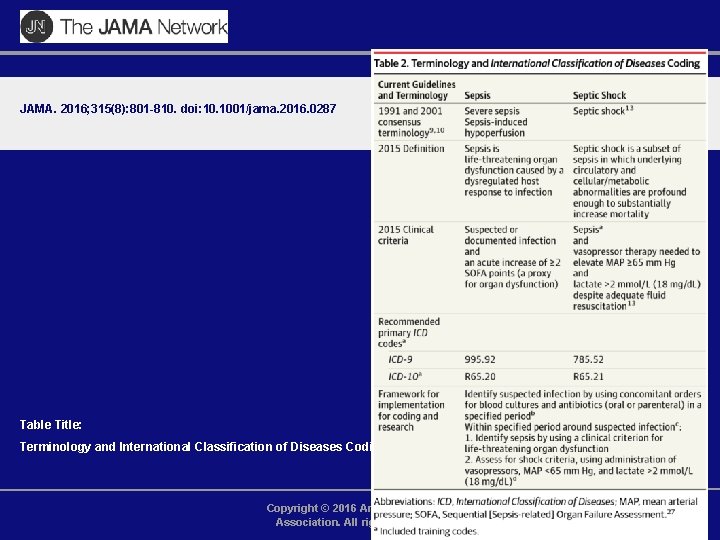
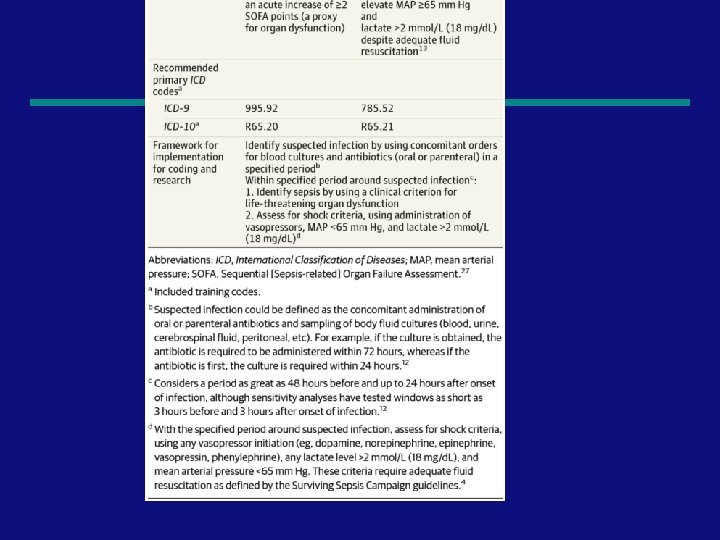
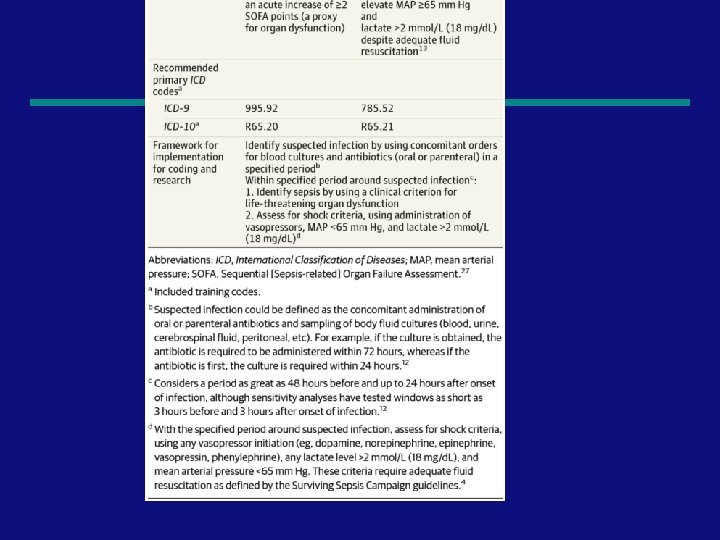
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Table Title: Terminology and International Classification of Diseases Coding Copyright © 2016 American Medical Association. All rights reserved.
8
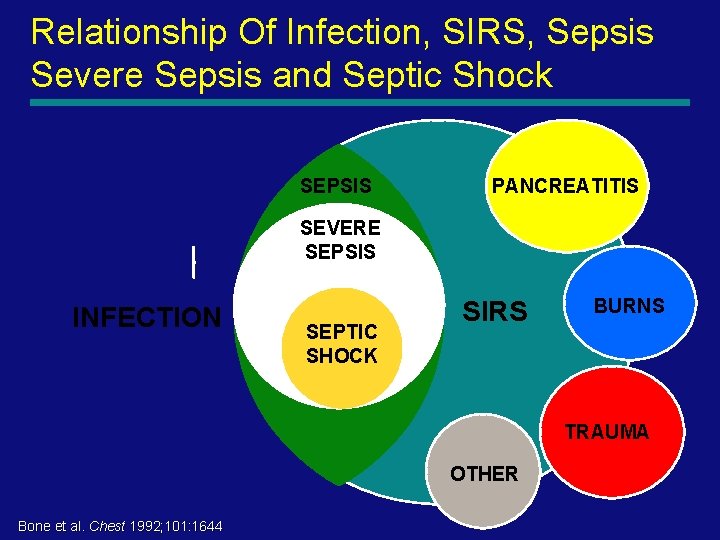
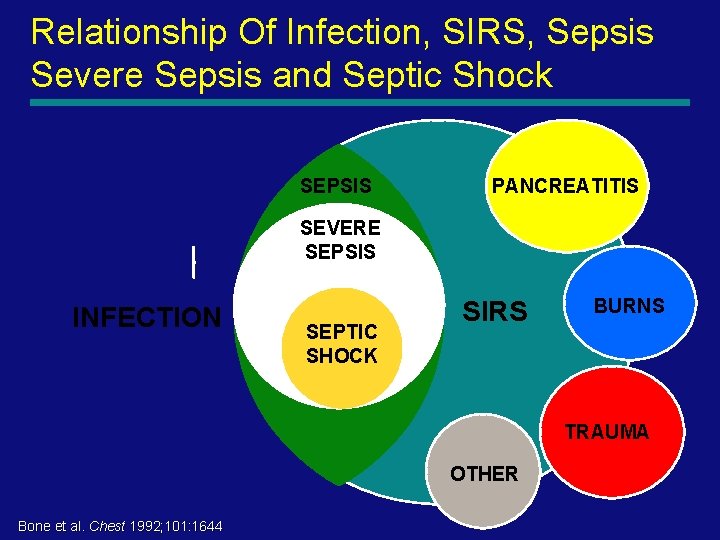
Relationship Of Infection, SIRS, Sepsis Severe Sepsis and Septic Shock SEPSIS PANCREATITIS SEVERE SEPSIS INFECTION SEPTIC SHOCK SIRS BURNS TRAUMA OTHER 9 Bone et al. Chest 1992; 101: 1644
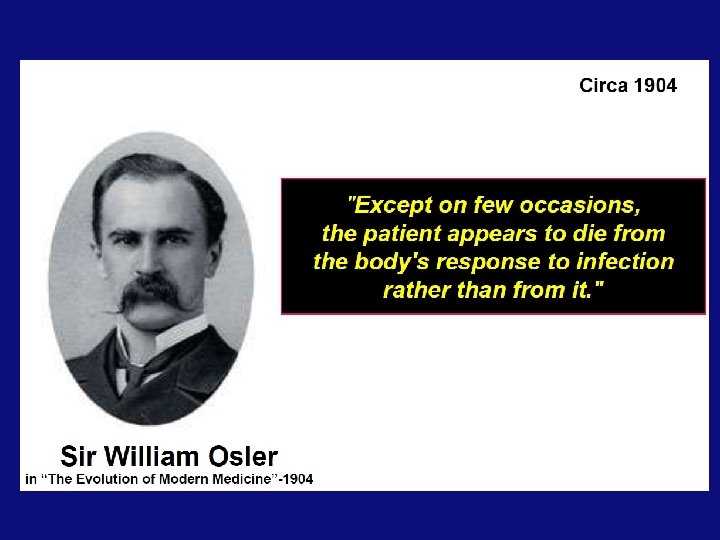
Sepsis • Sepsis is one of the oldest and most elusive syndromes in medicine. • Hippocrates, Semmelweis, Pasteur, and others, claimed that sepsis was recast as a systemic infection, often described as “blood poisoning, ” and assumed to be the result of the host's invasion by pathogenic organisms that then spread in the bloodstream. 10
Sepsis • However, with the advent of modern antibiotics, germ theory did not fully explain the pathogenesis of sepsis: many patients with sepsis died despite successful eradication of the inciting pathogen. • Thus, researchers suggested that it was the host, not the germ, that drove the pathogenesis of sepsis. 11
Incidence and causes • Estimated up to 19 million cases worldwide per year. • The true incidence is presumably far higher • Severe sepsis occurs as a result of both community-acquired and health care–associated infections. • Pneumonia is the most common cause, accounting for about half of all cases, followed by intraabdominal and urinary tract infections 12
Pathogens • Blood cultures are typically positive in only 1/3 of cases, • 1/3 cases, cultures from all sites are negative. • Staphylococcus aureus and Streptococcus pneumoniae are the most common gram-positive isolates, • Escherichia coli, Klebsiella species, and Pseudomonas aeruginosa predominate among gram-negative isolates • 14, 000 ICU patients in 75 countries, gram-negative 13 bacteria were isolated in 62%
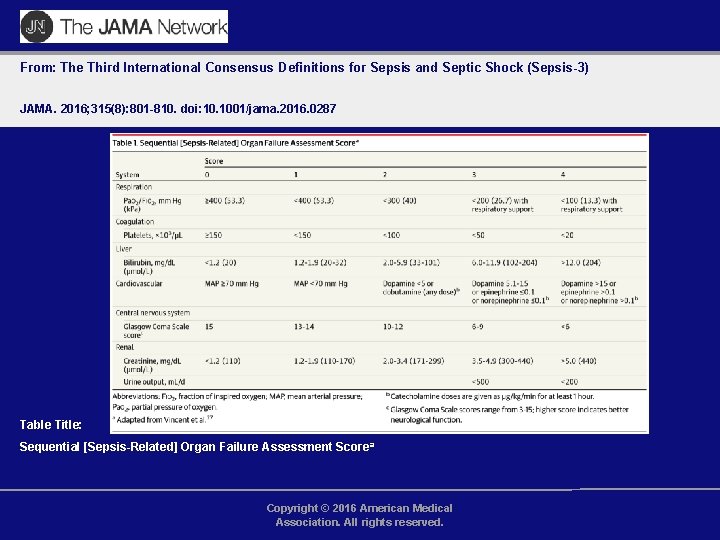
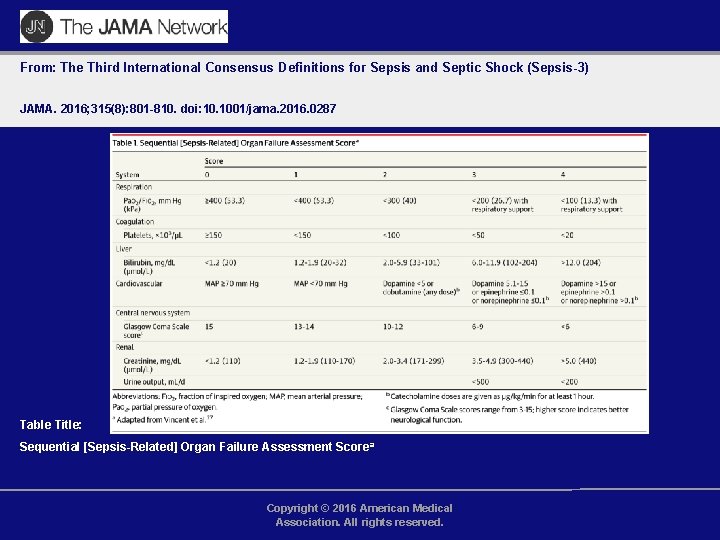
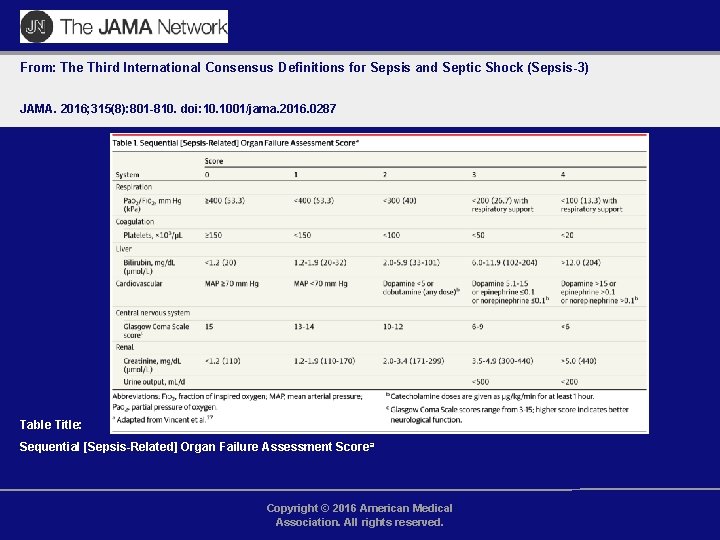
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Table Title: Sequential [Sepsis-Related] Organ Failure Assessment Scorea Copyright © 2016 American Medical Association. All rights reserved.
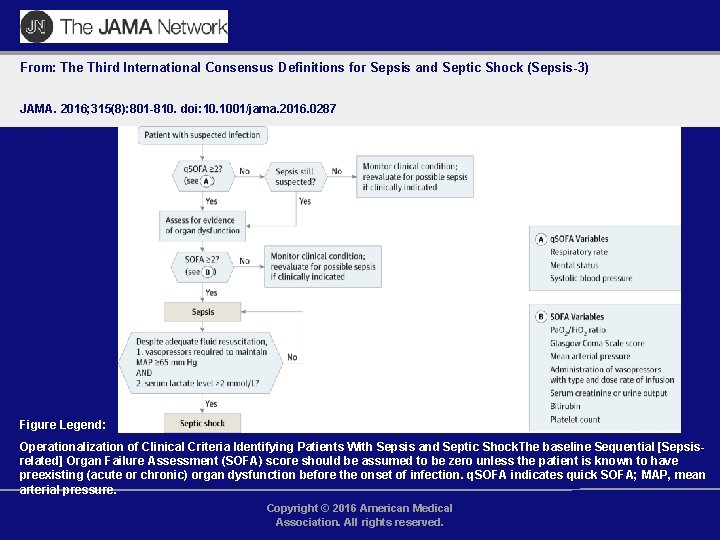
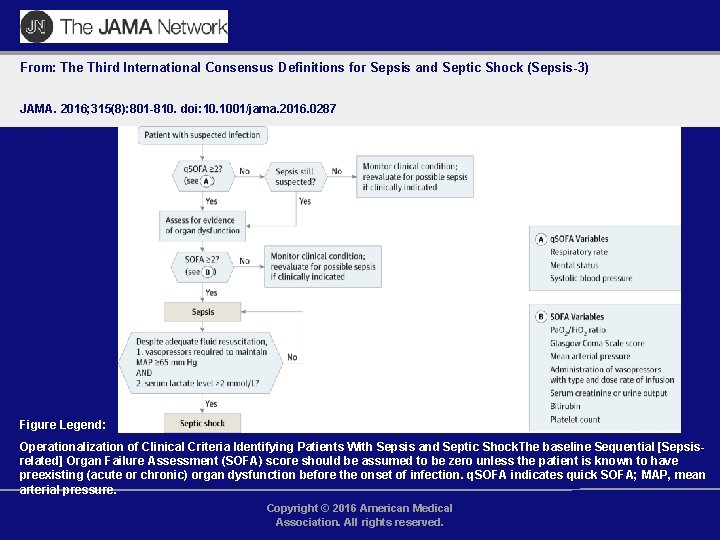
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Figure Legend: Operationalization of Clinical Criteria Identifying Patients With Sepsis and Septic Shock. The baseline Sequential [Sepsisrelated] Organ Failure Assessment (SOFA) score should be assumed to be zero unless the patient is known to have preexisting (acute or chronic) organ dysfunction before the onset of infection. q. SOFA indicates quick SOFA; MAP, mean arterial pressure. Copyright © 2016 American Medical Association. All rights reserved.
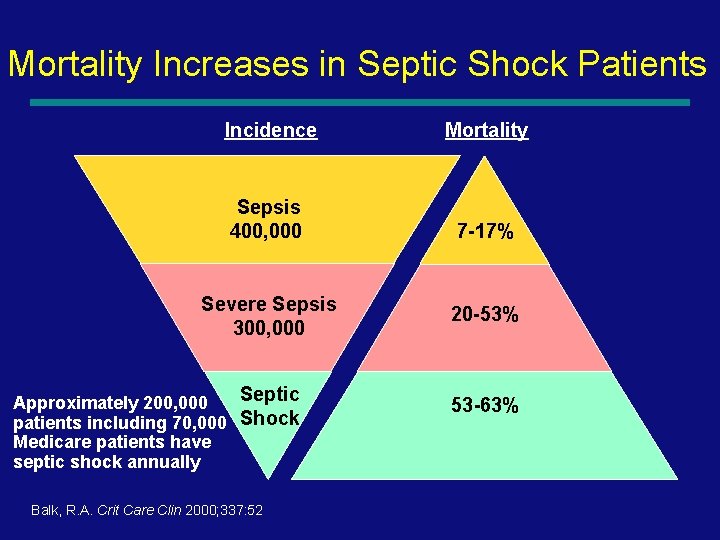
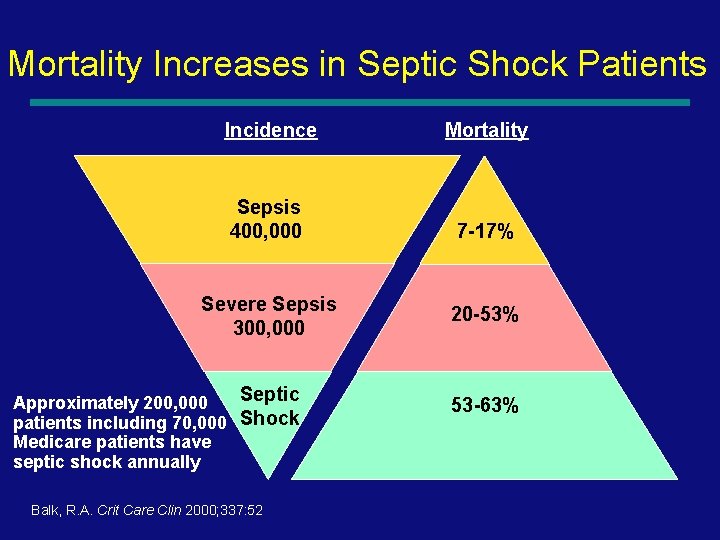
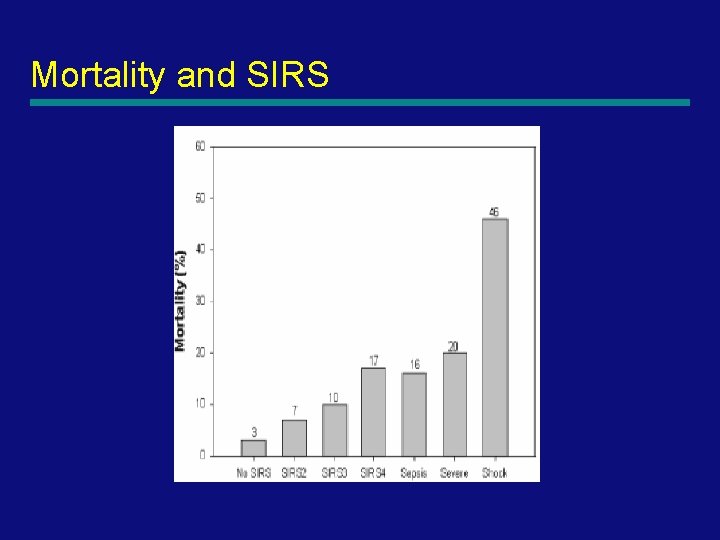
Mortality Increases in Septic Shock Patients Incidence Mortality Sepsis 400, 000 7 -17% Severe Sepsis 300, 000 Septic Approximately 200, 000 patients including 70, 000 Shock Medicare patients have septic shock annually Balk, R. A. Crit Care Clin 2000; 337: 52 20 -53% 53 -63% 16
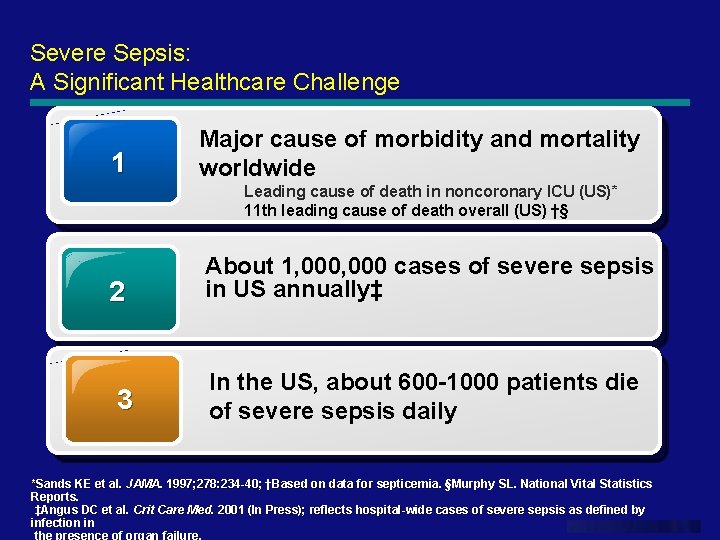
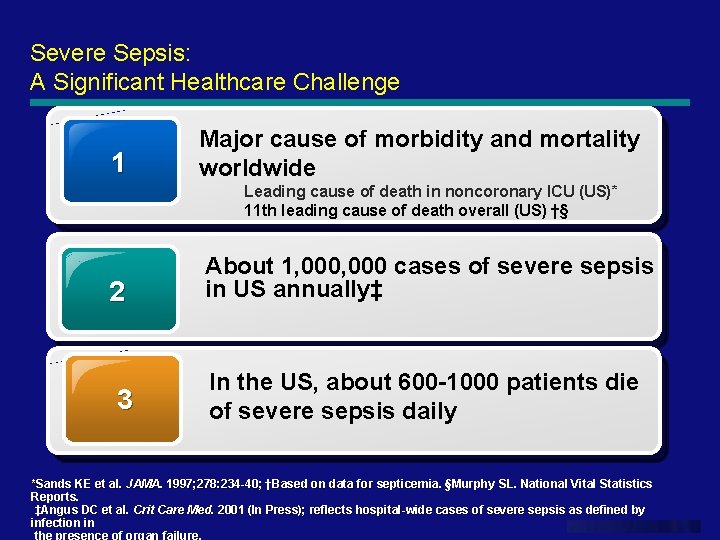
Severe Sepsis: A Significant Healthcare Challenge 1 Major cause of morbidity and mortality worldwide Leading cause of death in noncoronary ICU (US)* 11 th leading cause of death overall (US) †§ 2 3 About 1, 000 cases of severe sepsis in US annually‡ In the US, about 600 -1000 patients die of severe sepsis daily *Sands KE et al. JAMA. Based on data for septicemia. §Murphy SL. National Vital Statistics JAMA. 1997; 278: 234 -40; †Based Reports. ‡Angus DC et al. Crit Care Med. 2001 (In Press); reflects hospital-wide cases of severe sepsis as defined by infection in www. themegallery. com the presence of organ failure.
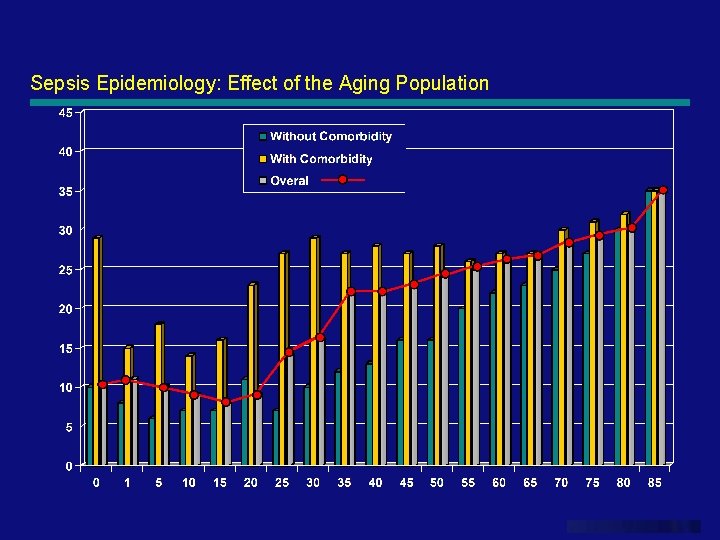
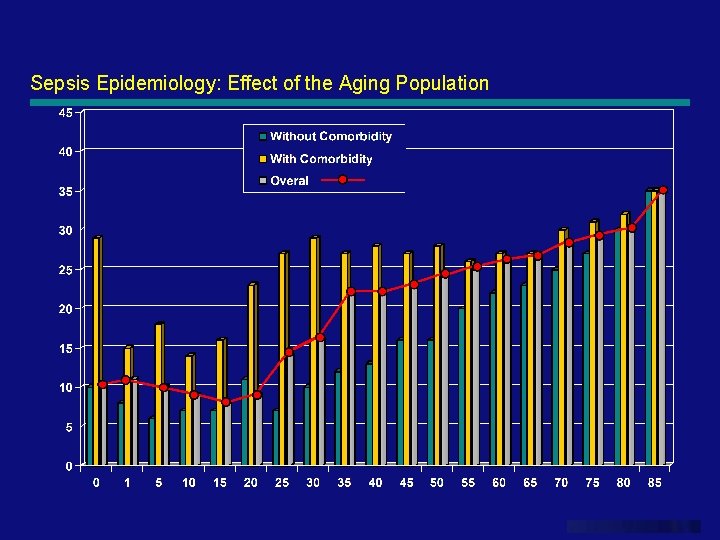
Sepsis Epidemiology: Effect of the Aging Population www. themegallery. com
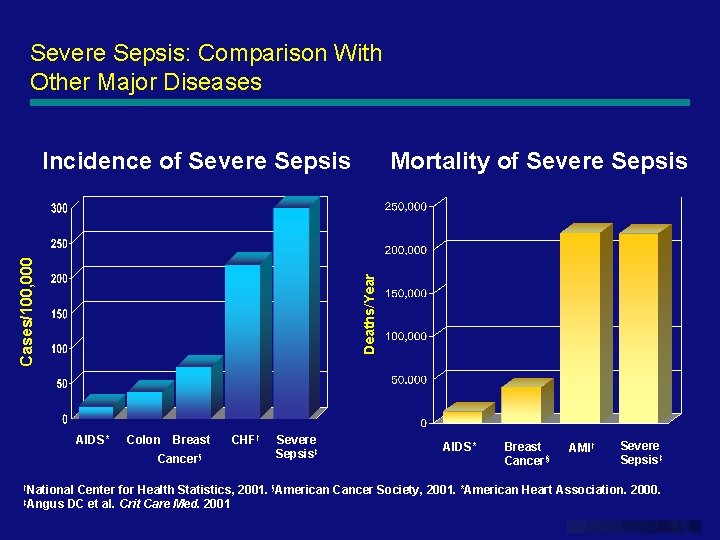
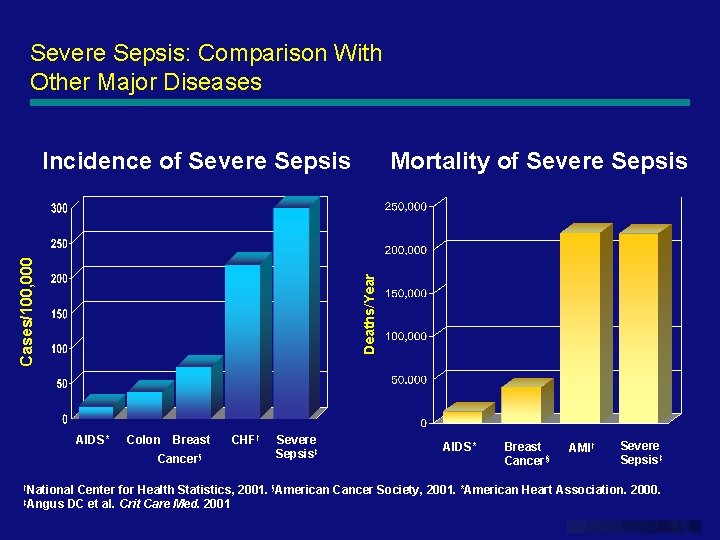
Severe Sepsis: Comparison With Other Major Diseases Mortality of Severe Sepsis Deaths/Year Cases/100, 000 Incidence of Severe Sepsis AIDS* Colon Breast Cancer§ CHF† Severe Sepsis‡ AIDS* Breast Cancer§ AMI† Severe Sepsis‡ †National Center for Health Statistics, 2001. §American Cancer Society, 2001. *American Heart Association. 2000. ‡Angus DC et al. Crit Care Med. 2001 www. themegallery. com
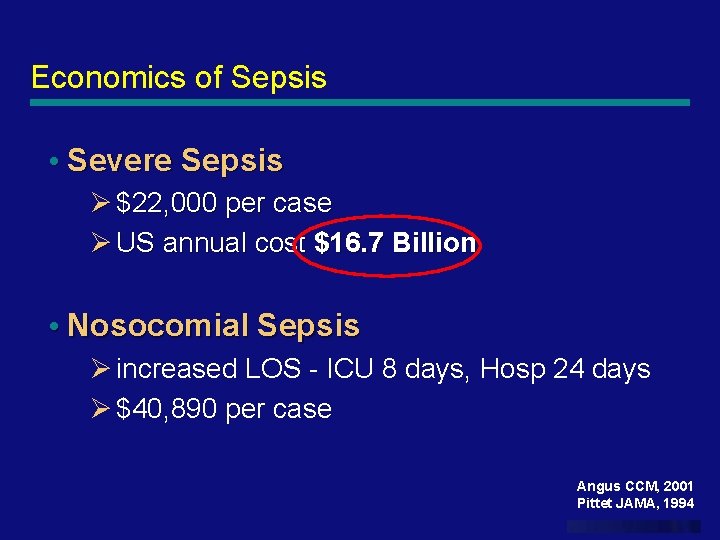
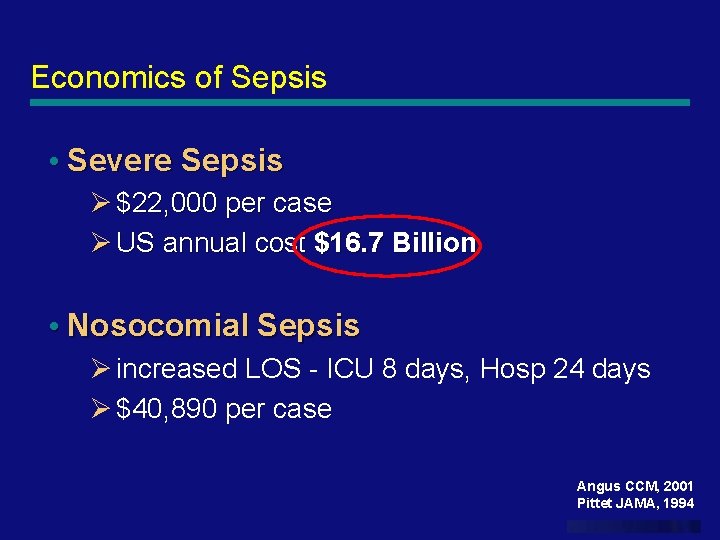
Economics of Sepsis • Severe Sepsis Ø $22, 000 per case Ø US annual cost $16. 7 Billion • Nosocomial Sepsis Ø increased LOS - ICU 8 days, Hosp 24 days Ø $40, 890 per case Angus CCM, 2001 Pittet JAMA, 1994 www. themegallery. com
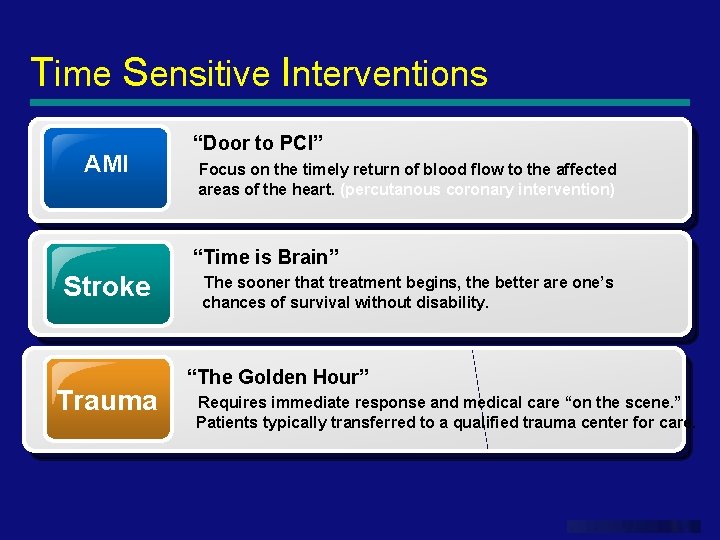
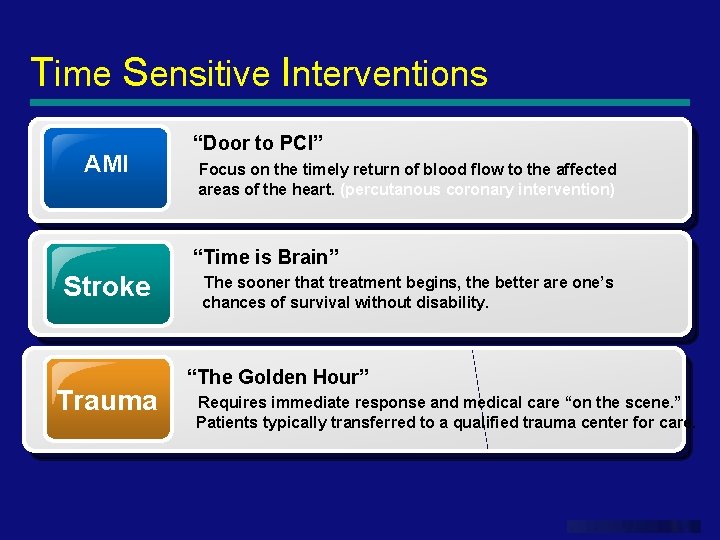
Time Sensitive Interventions AMI “Door to PCI” Focus on the timely return of blood flow to the affected areas of the heart. (percutanous coronary intervention) “Time is Brain” Stroke Trauma The sooner that treatment begins, the better are one’s chances of survival without disability. “The Golden Hour” Requires immediate response and medical care “on the scene. ” Patients typically transferred to a qualified trauma center for care. www. themegallery. com
Trauma vs. Sepsis Patient Care Where we spend our efforts www. themegallery. com
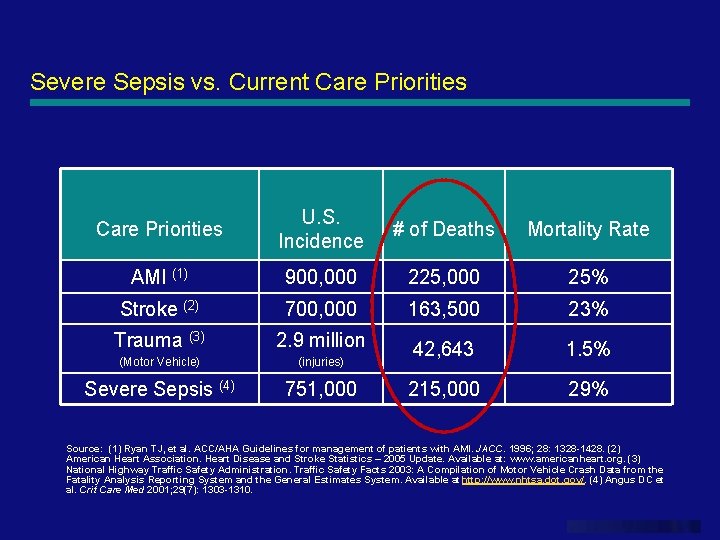
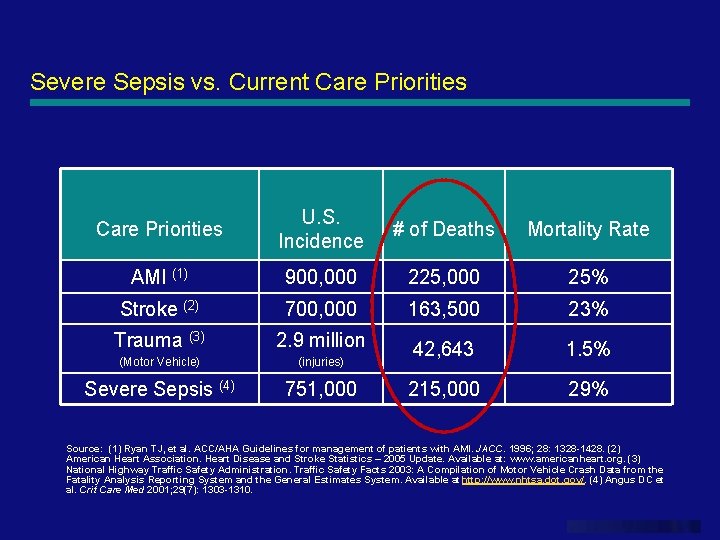
Severe Sepsis vs. Current Care Priorities U. S. Incidence # of Deaths Mortality Rate AMI (1) 900, 000 225, 000 25% Stroke (2) 700, 000 163, 500 23% Trauma (3) 2. 9 million (Motor Vehicle) (injuries) 42, 643 1. 5% Severe Sepsis (4) 751, 000 215, 000 29% Source: (1) Ryan TJ, et al. ACC/AHA Guidelines for management of patients with AMI. JACC. 1996; 28: 1328 -1428. (2) American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. Available at: www. americanheart. org. (3) National Highway Traffic Safety Administration. Traffic Safety Facts 2003: A Compilation of Motor Vehicle Crash Data from the Fatality Analysis Reporting System and the General Estimates System. Available at http: //www. nhtsa. dot. gov/. (4) Angus DC et al. Crit Care Med 2001; 29(7): 1303 -1310. www. themegallery. com
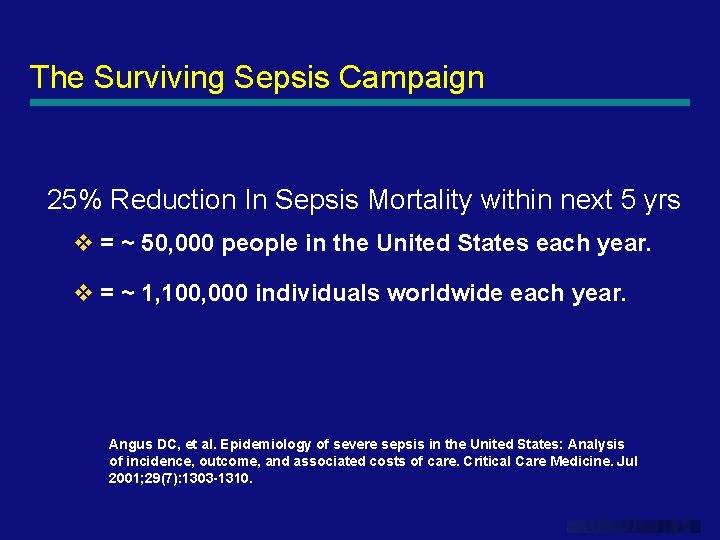
The Surviving Sepsis Campaign 25% Reduction In Sepsis Mortality within next 5 yrs v = ~ 50, 000 people in the United States each year. v = ~ 1, 100, 000 individuals worldwide each year. Angus DC, et al. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Critical Care Medicine. Jul 2001; 29(7): 1303 -1310. www. themegallery. com
PATHOGENESIS 25
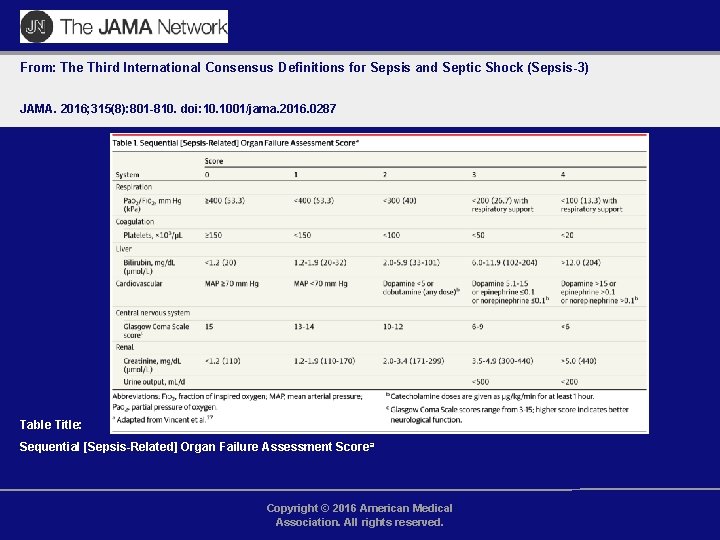
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Table Title: Sequential [Sepsis-Related] Organ Failure Assessment Scorea Copyright © 2016 American Medical Association. All rights reserved.
27
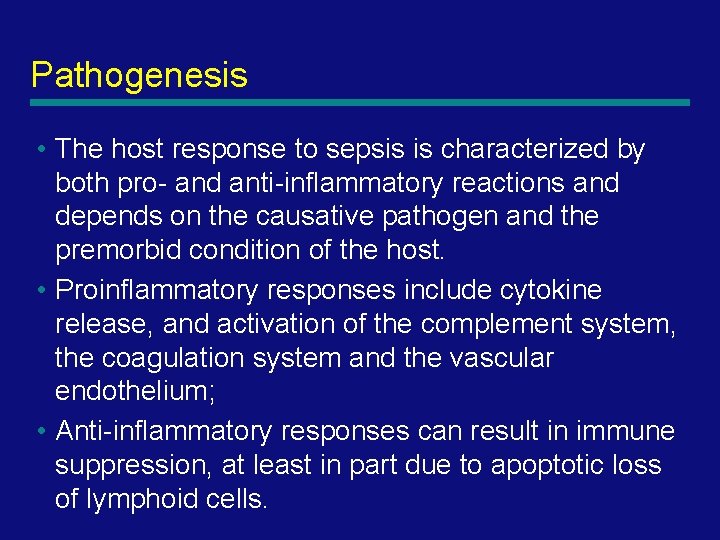
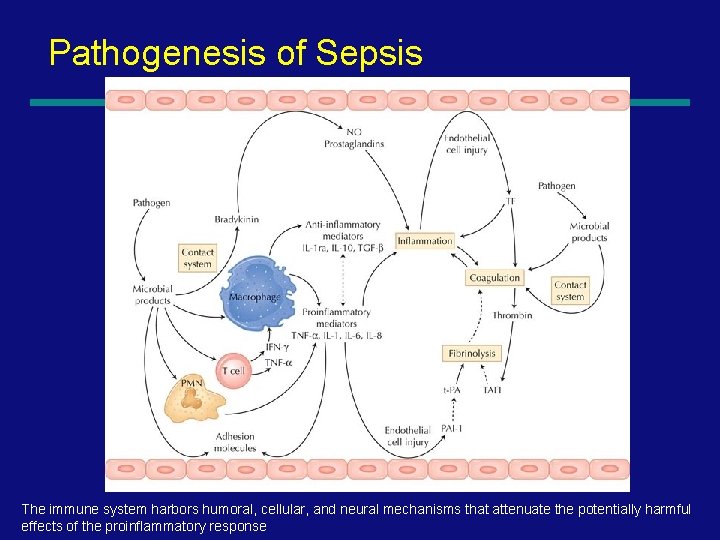
Pathogenesis • The host response to sepsis is characterized by both pro- and anti-inflammatory reactions and depends on the causative pathogen and the premorbid condition of the host. • Proinflammatory responses include cytokine release, and activation of the complement system, the coagulation system and the vascular endothelium; • Anti-inflammatory responses can result in immune suppression, at least in part due to apoptotic loss of lymphoid cells. 28
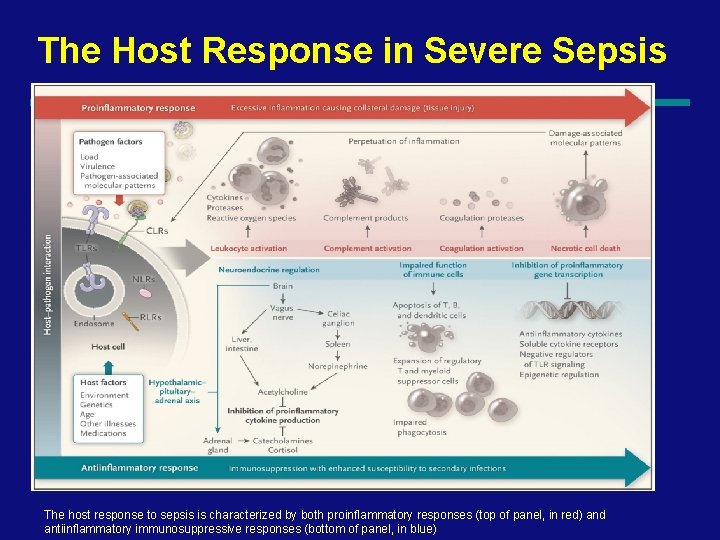
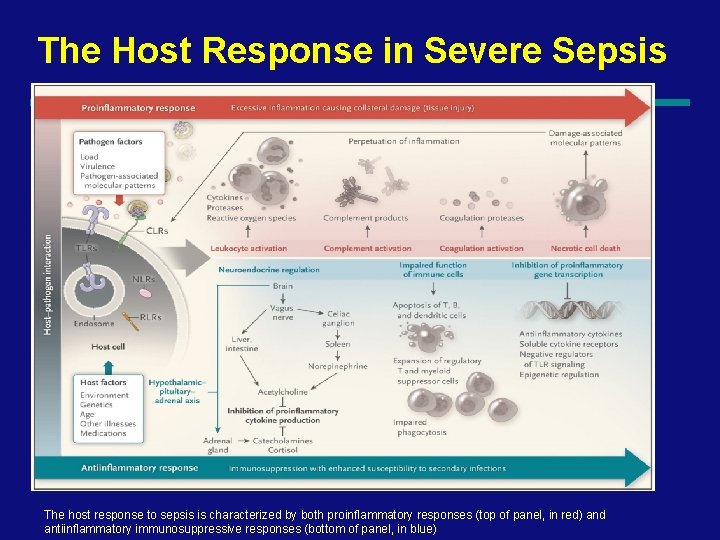
The Host Response in Severe Sepsis The host response to sepsis is characterized by both proinflammatory responses (top of panel, in red) and antiinflammatory immunosuppressive responses (bottom of panel, in blue) 29
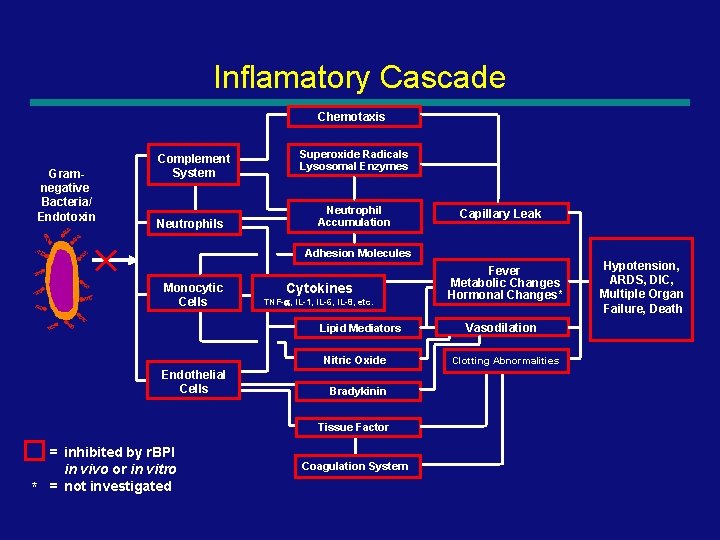
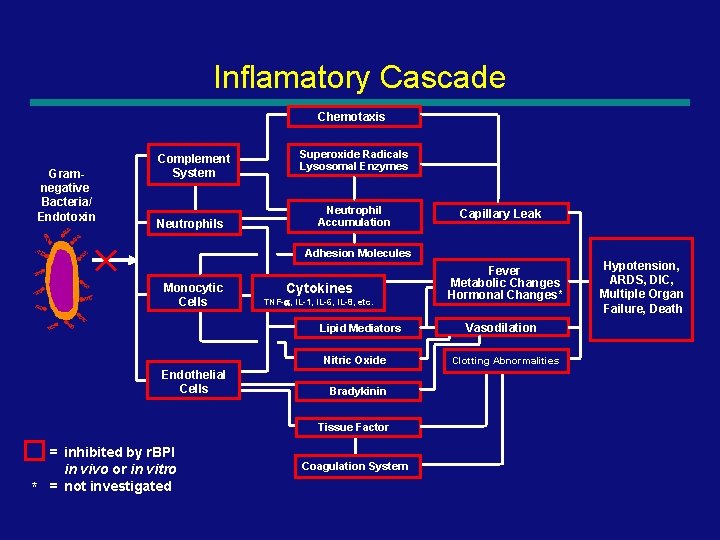
Inflamatory Cascade Chemotaxis Gramnegative Bacteria/ Endotoxin Complement System Neutrophils Superoxide Radicals Lysosomal Enzymes Neutrophil Accumulation Capillary Leak Adhesion Molecules Monocytic Cells Cytokines TNF-a, IL-1, IL-6, IL-8, etc. Lipid Mediators Nitric Oxide Endothelial Cells Fever Metabolic Changes Hormonal Changes* Hypotension, ARDS, DIC, Multiple Organ Failure, Death Vasodilation Clotting Abnormalities Bradykinin Tissue Factor * = inhibited by r. BPI in vivo or in vitro = not investigated Coagulation System 30
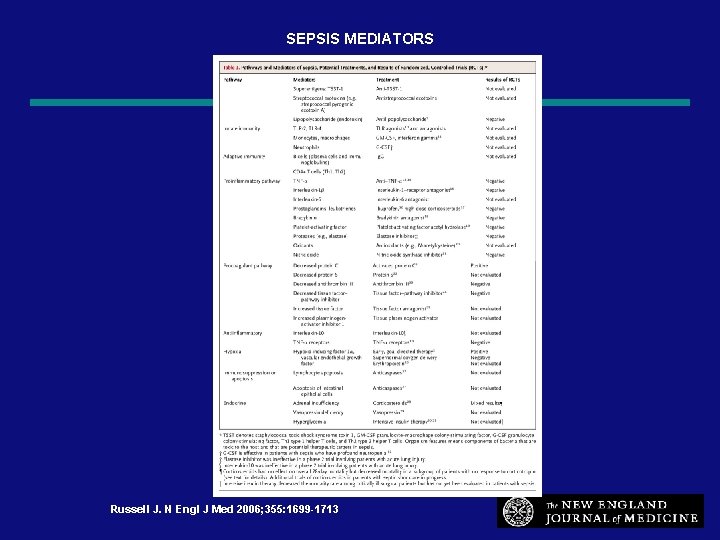
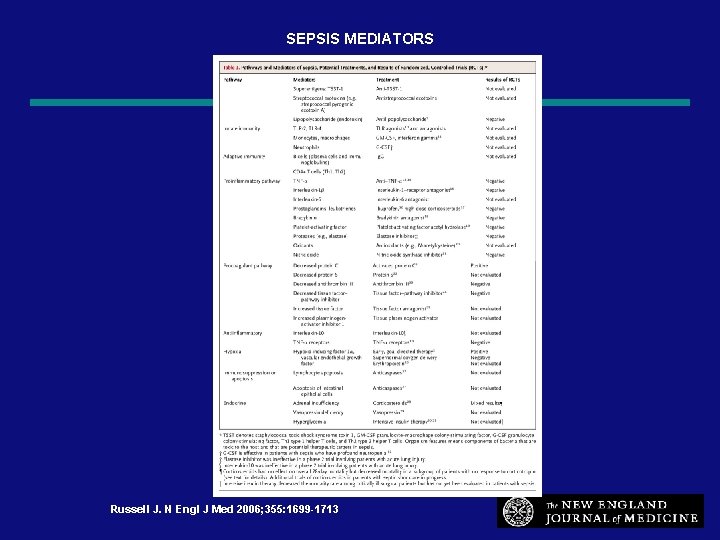
SEPSIS MEDIATORS Russell J. N Engl J Med 2006; 355: 1699 -1713 31
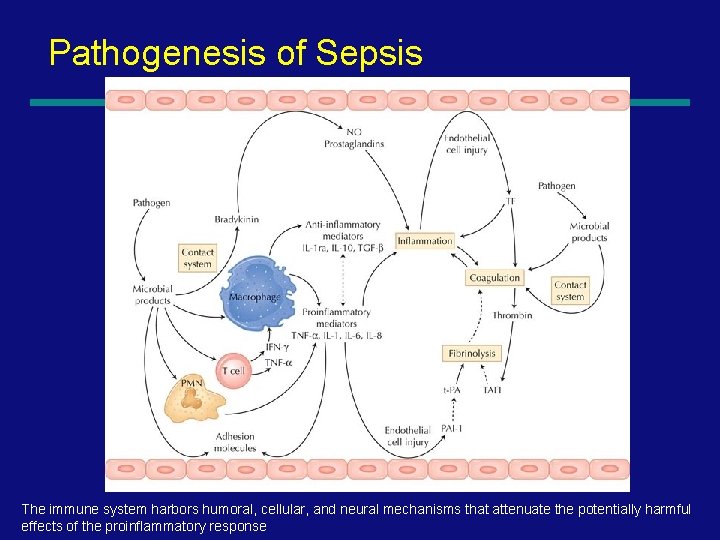
Pathogenesis of Sepsis The immune system harbors humoral, cellular, and neural mechanisms that attenuate the potentially harmful effects of the proinflammatory response
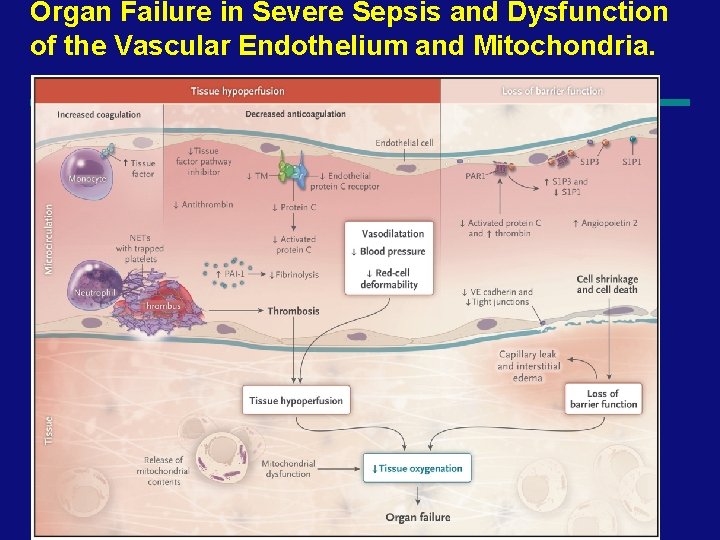
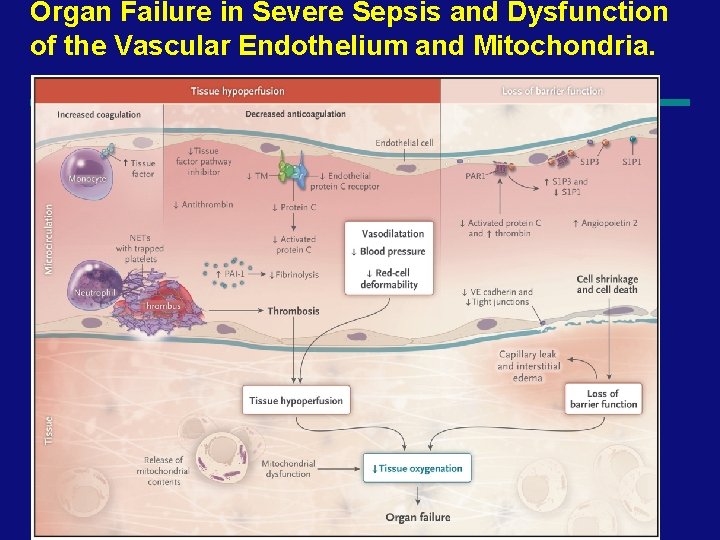
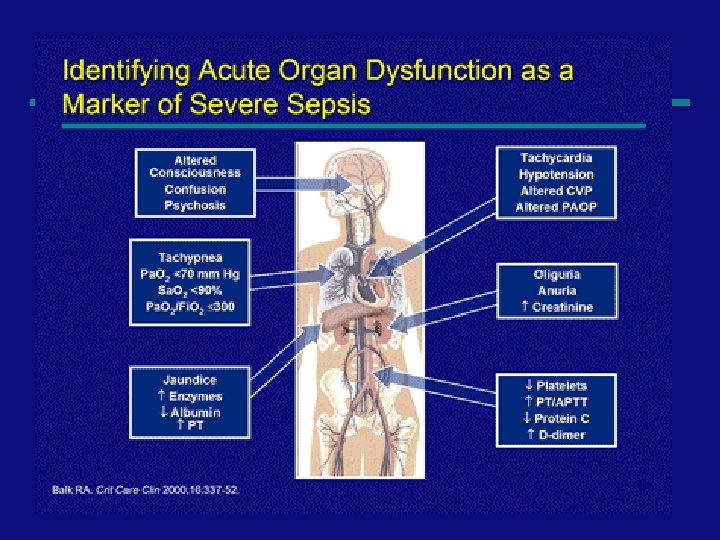
Organ Failure in Severe Sepsis and Dysfunction of the Vascular Endothelium and Mitochondria. 33
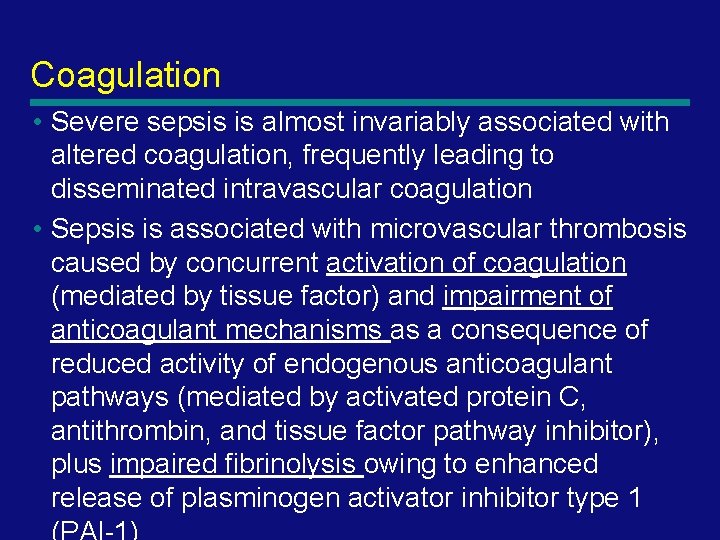
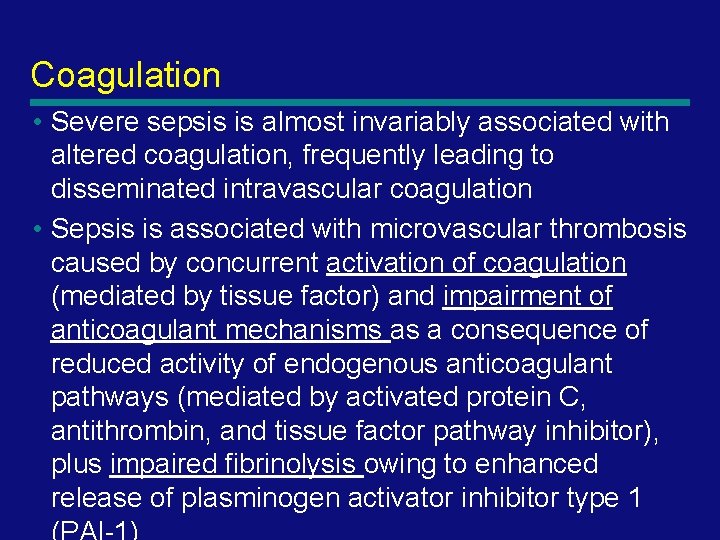
Coagulation • Severe sepsis is almost invariably associated with altered coagulation, frequently leading to disseminated intravascular coagulation • Sepsis is associated with microvascular thrombosis caused by concurrent activation of coagulation (mediated by tissue factor) and impairment of anticoagulant mechanisms as a consequence of reduced activity of endogenous anticoagulant pathways (mediated by activated protein C, antithrombin, and tissue factor pathway inhibitor), plus impaired fibrinolysis owing to enhanced release of plasminogen activator inhibitor type 1 34
Coagulation • Thrombus formation results in • -tissue hypoperfusion, • -which is aggravated by vasodilatation, • -hypotension, • -and reduced red-cell deformability. 35
Organ Disfunction • Impaired tissue oxygenation plays a key role • Several factors — including hypotension, reduced red-cell deformability, and microvascular thrombosis — contribute to diminished oxygen delivery in septic shock. • Inflammation cause dysfunction of the vascular endothelium, accompanied by cell death and loss of barrier integrity, giving rise to subcutaneous and body-cavity edema • Mitochondrial damage caused by oxidative stress and other mechanisms impairs cellular oxygen use 36
37
Cardiovascular Dysfunction • Despite administration of isotonic intravenous fluid • bolus ≥ 40 m. L/kg in 1 hr — Hypotension: BP <5 th % or <2 sd OR — Need for vasoactive drug to maintain BP (dopamine >5 mcg/kg/min or dob, epi, or norepi at any dose) OR — Two of the following § § § Unexplained metabolic acidosis: Base deficit >5. 0 m. Eq/L Arterial lactate: >2 times upper limit of normal Oliguria: Urine output <0. 5 m. L/kg/hr Capillary refill: >5 secs Core to peripheral temperature gap >3°C 38
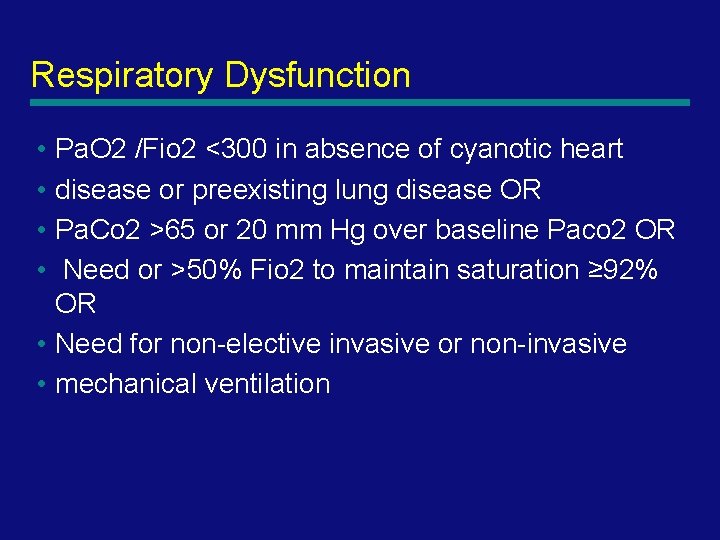
Respiratory Dysfunction • Pa. O 2 /Fio 2 <300 in absence of cyanotic heart • disease or preexisting lung disease OR • Pa. Co 2 >65 or 20 mm Hg over baseline Paco 2 OR • Need or >50% Fio 2 to maintain saturation ≥ 92% OR • Need for non-elective invasive or non-invasive • mechanical ventilation 39
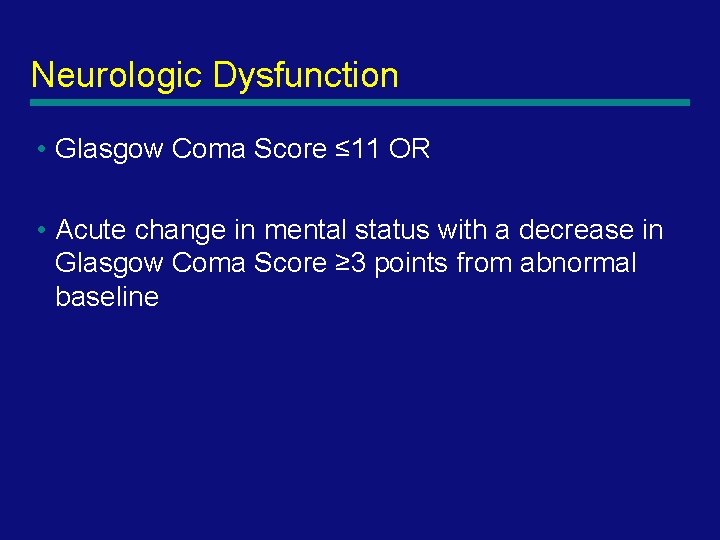
Neurologic Dysfunction • Glasgow Coma Score ≤ 11 OR • Acute change in mental status with a decrease in Glasgow Coma Score ≥ 3 points from abnormal baseline 40
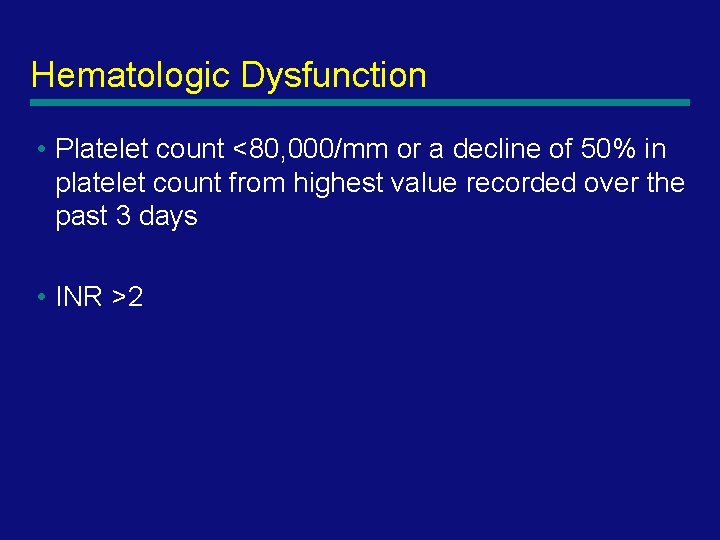
Hematologic Dysfunction • Platelet count <80, 000/mm or a decline of 50% in platelet count from highest value recorded over the past 3 days • INR >2 41
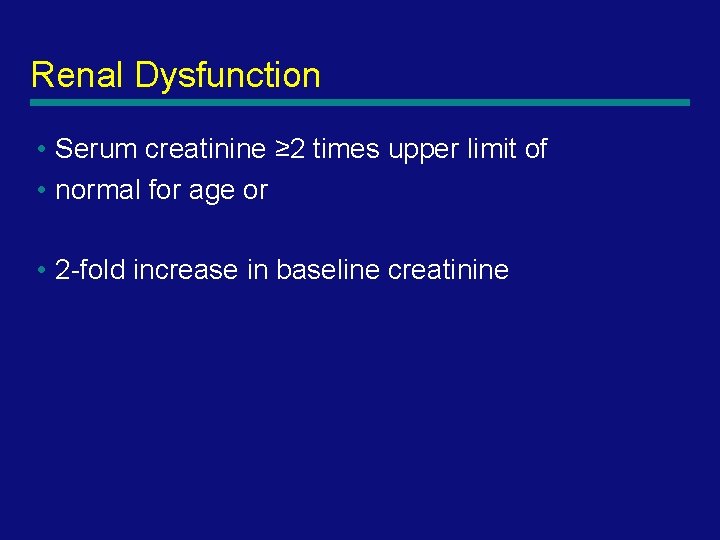
Renal Dysfunction • Serum creatinine ≥ 2 times upper limit of • normal for age or • 2 -fold increase in baseline creatinine 42
Hepatic Dysfunction • Total bilirubin ≥ 4 mg/d. L (not applicable for • newborn) OR • ALT 2 times upper limit of normal for age 43
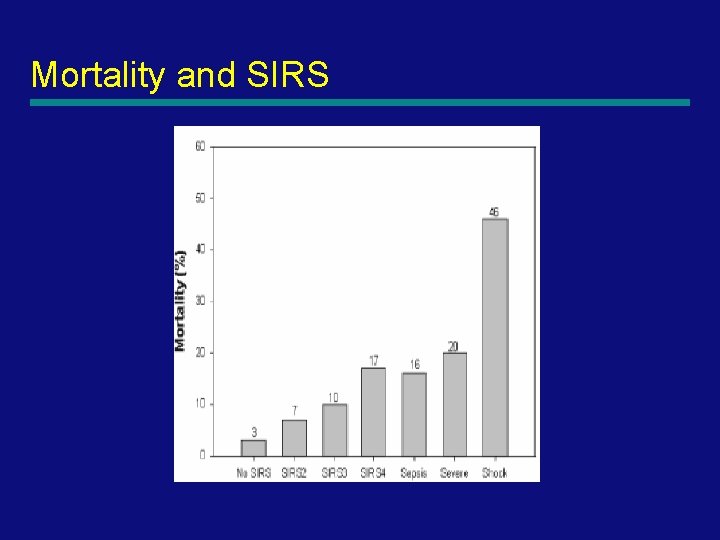
Mortality and SIRS 44
Treatment
Sepsis Resuscitation Emergency Department and Intensive Care Unit

47
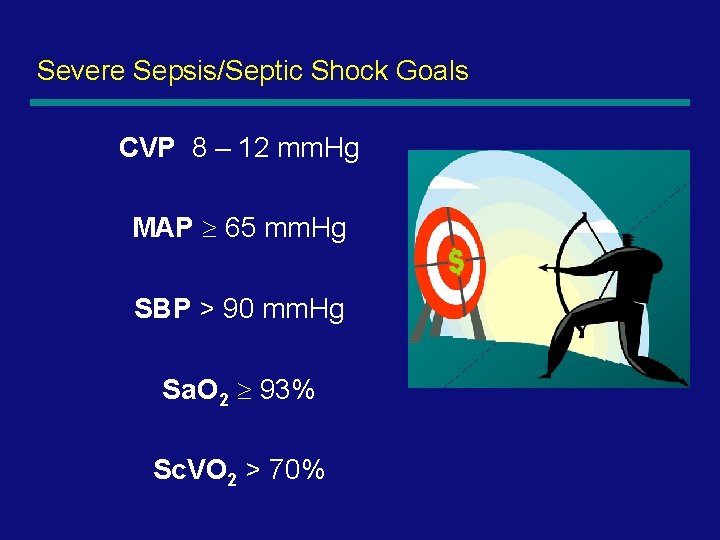
Severe Sepsis/Septic Shock Goals CVP 8 – 12 mm. Hg MAP 65 mm. Hg SBP > 90 mm. Hg Sa. O 2 93% Sc. VO 2 > 70%
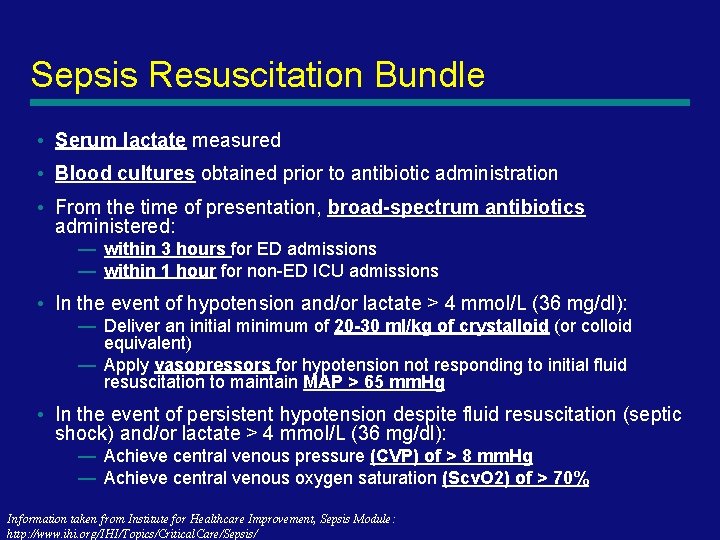
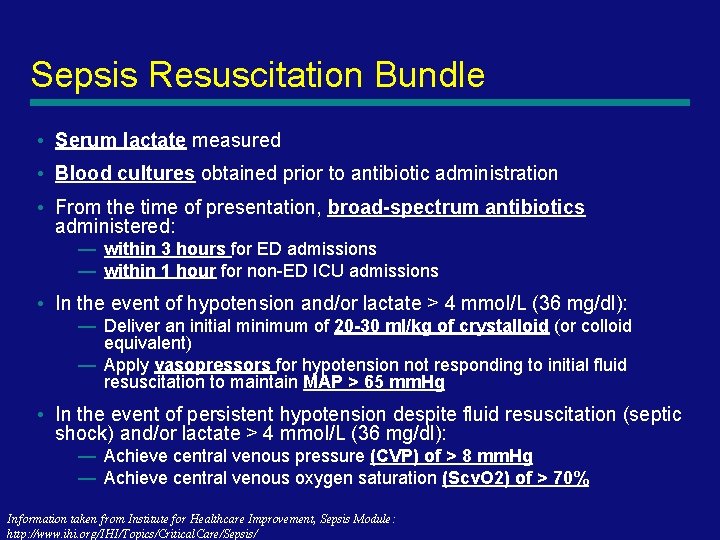
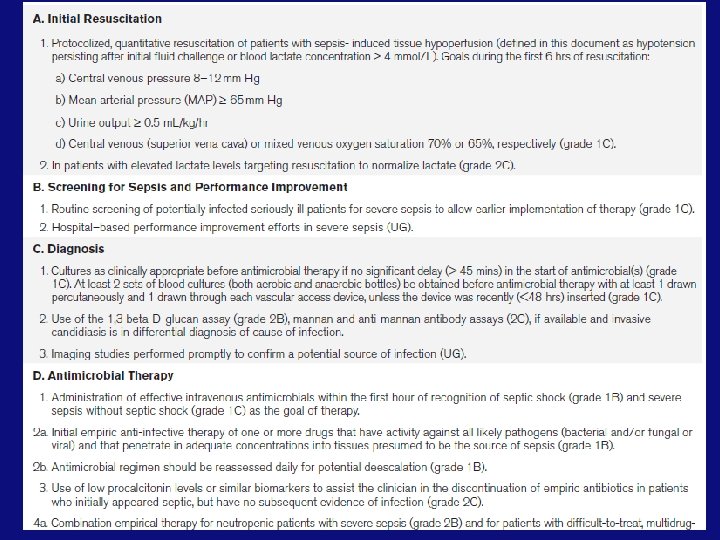
Sepsis Resuscitation Bundle • Serum lactate measured • Blood cultures obtained prior to antibiotic administration • From the time of presentation, broad-spectrum antibiotics administered: — within 3 hours for ED admissions — within 1 hour for non-ED ICU admissions • In the event of hypotension and/or lactate > 4 mmol/L (36 mg/dl): — Deliver an initial minimum of 20 -30 ml/kg of crystalloid (or colloid equivalent) — Apply vasopressors for hypotension not responding to initial fluid resuscitation to maintain MAP > 65 mm. Hg • In the event of persistent hypotension despite fluid resuscitation (septic shock) and/or lactate > 4 mmol/L (36 mg/dl): — Achieve central venous pressure (CVP) of > 8 mm. Hg — Achieve central venous oxygen saturation (Scv. O 2) of > 70% Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
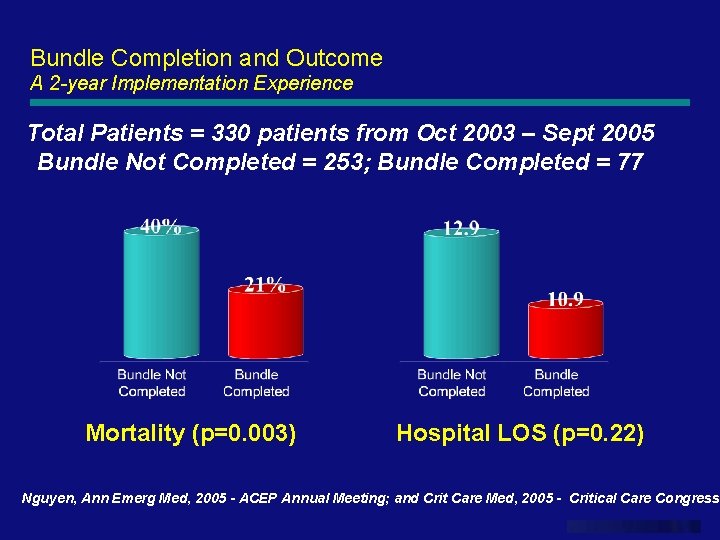
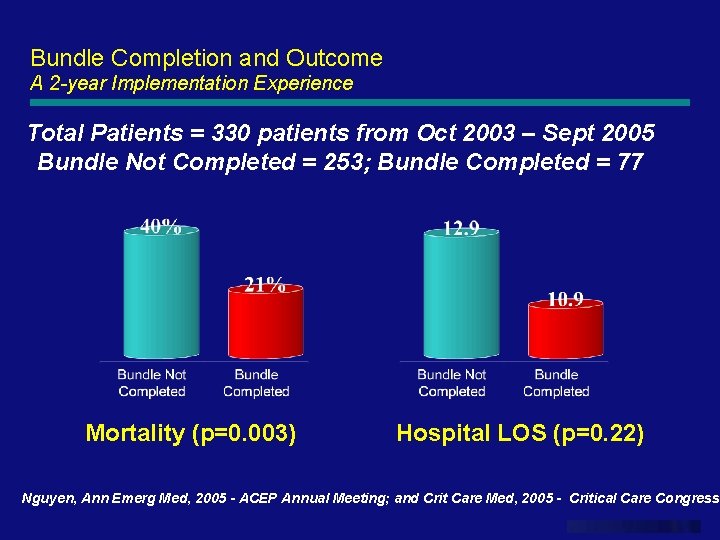
Bundle Completion and Outcome A 2 -year Implementation Experience Total Patients = 330 patients from Oct 2003 – Sept 2005 Bundle Not Completed = 253; Bundle Completed = 77 Mortality (p=0. 003) Hospital LOS (p=0. 22) Nguyen, Ann Emerg Med, 2005 - ACEP Annual Meeting; and Crit Care Med, 2005 - Critical Care Congress www. themegallery. com
51
52
53
Hemodynamic support and adjunctive therapy 54
Initial Resussitation • Begin as soon as the sepsis syndrome is recognized 55
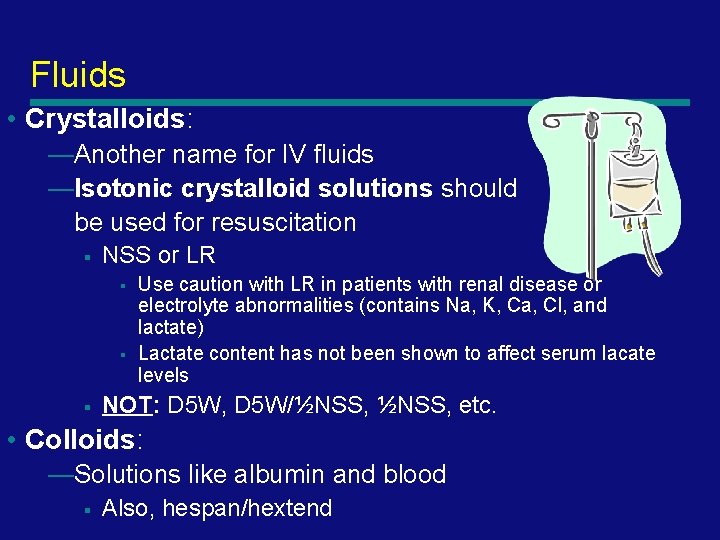
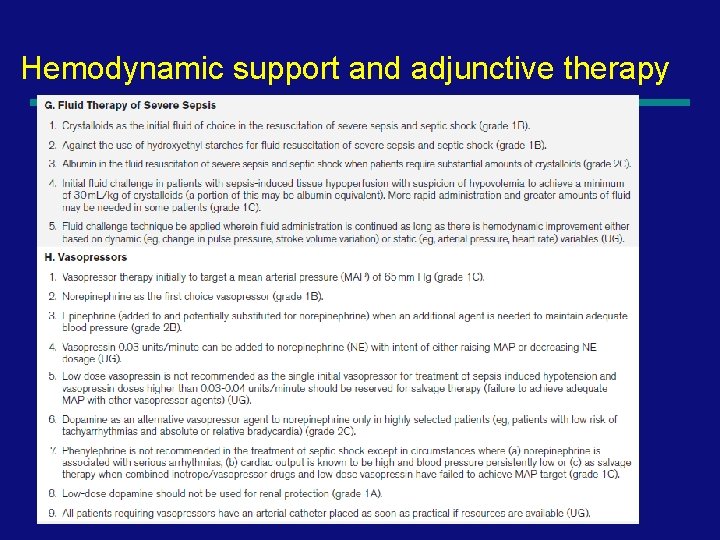
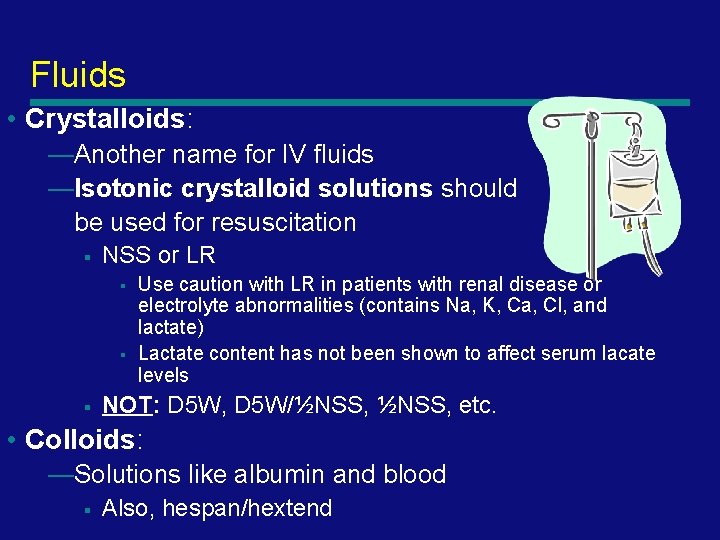
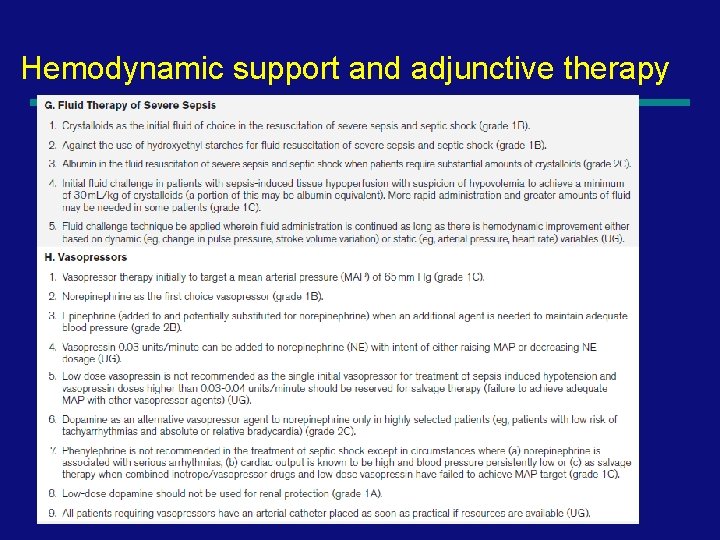
Fluids • Crystalloids: —Another name for IV fluids —Isotonic crystalloid solutions should be used for resuscitation § NSS or LR § § § Use caution with LR in patients with renal disease or electrolyte abnormalities (contains Na, K, Ca, Cl, and lactate) Lactate content has not been shown to affect serum lacate levels NOT: D 5 W, D 5 W/½NSS, etc. • Colloids: —Solutions like albumin and blood § Also, hespan/hextend
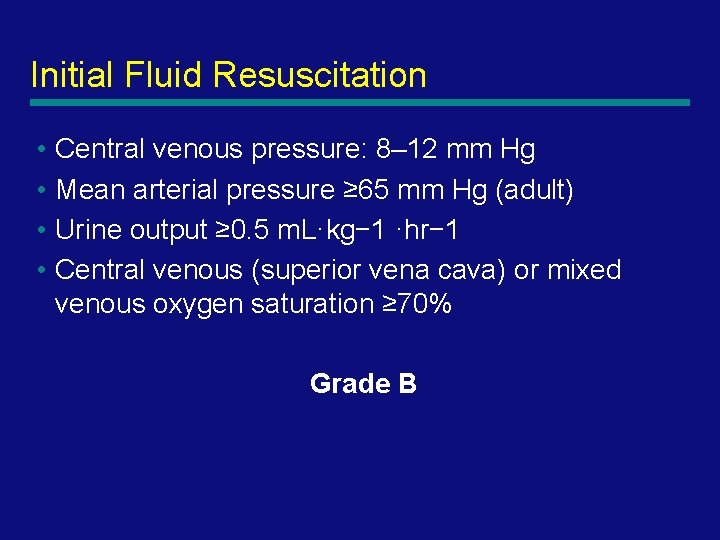
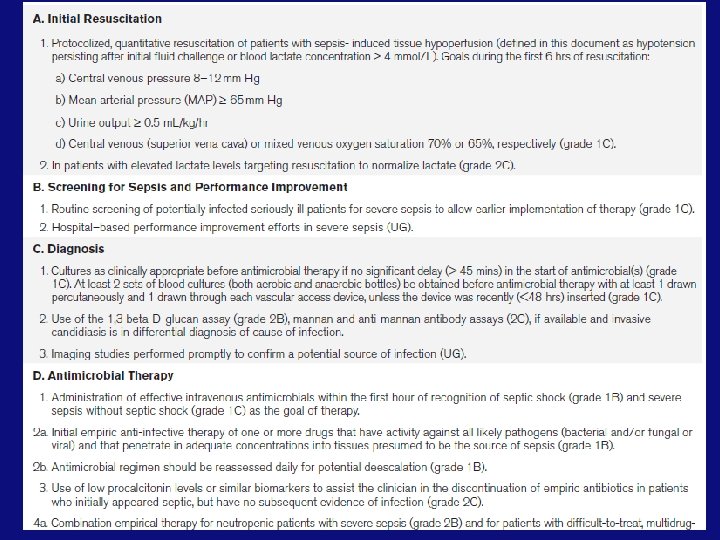
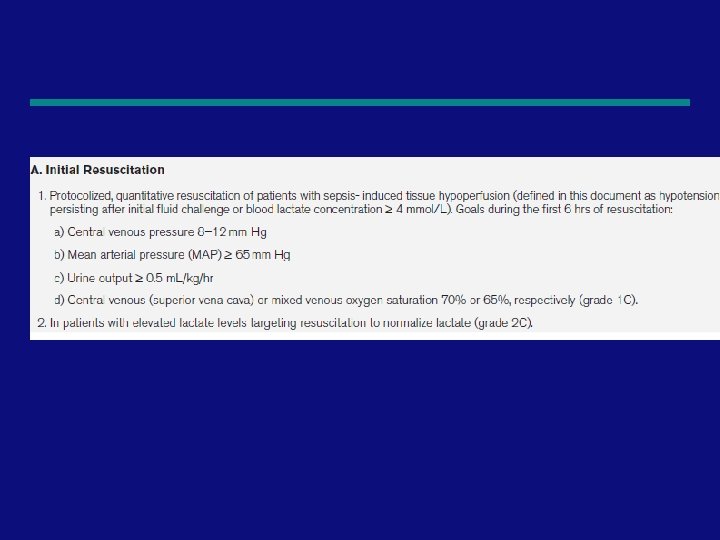
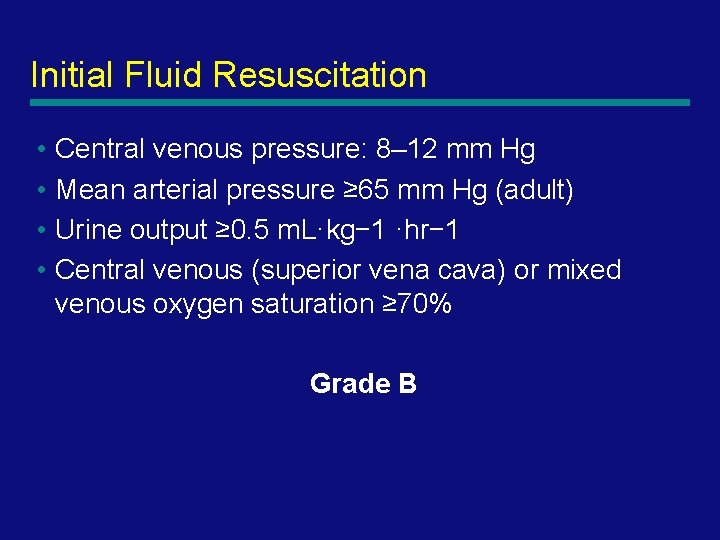
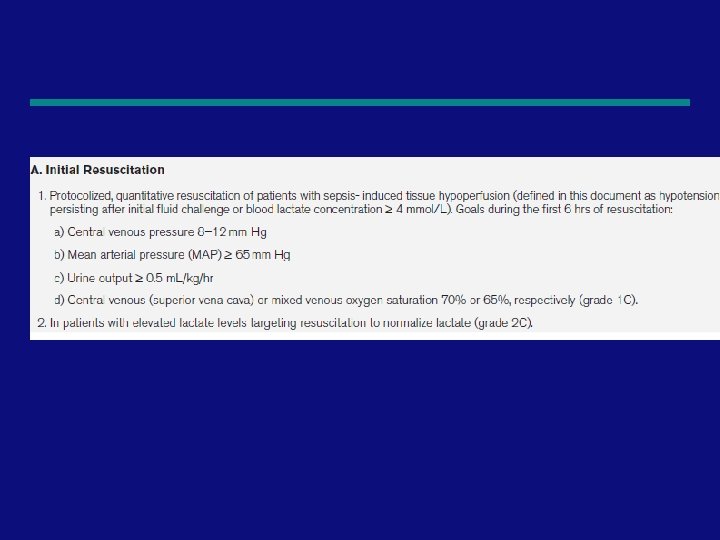
Initial Fluid Resuscitation • Central venous pressure: 8– 12 mm Hg • Mean arterial pressure ≥ 65 mm Hg (adult) • Urine output ≥ 0. 5 m. L·kg− 1 ·hr− 1 • Central venous (superior vena cava) or mixed venous oxygen saturation ≥ 70% Grade B 57
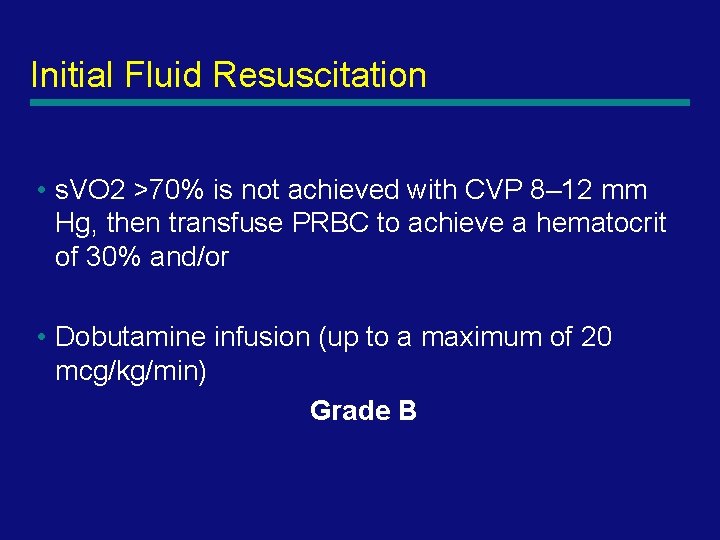
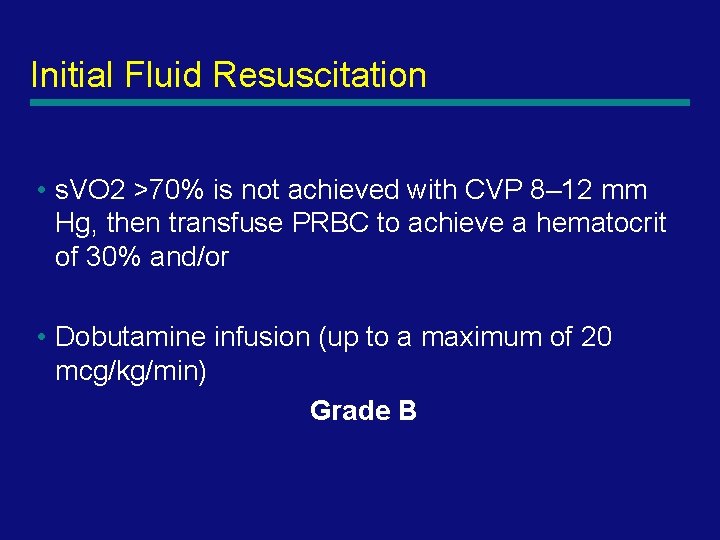
Initial Fluid Resuscitation • s. VO 2 >70% is not achieved with CVP 8– 12 mm Hg, then transfuse PRBC to achieve a hematocrit of 30% and/or • Dobutamine infusion (up to a maximum of 20 mcg/kg/min) Grade B 58
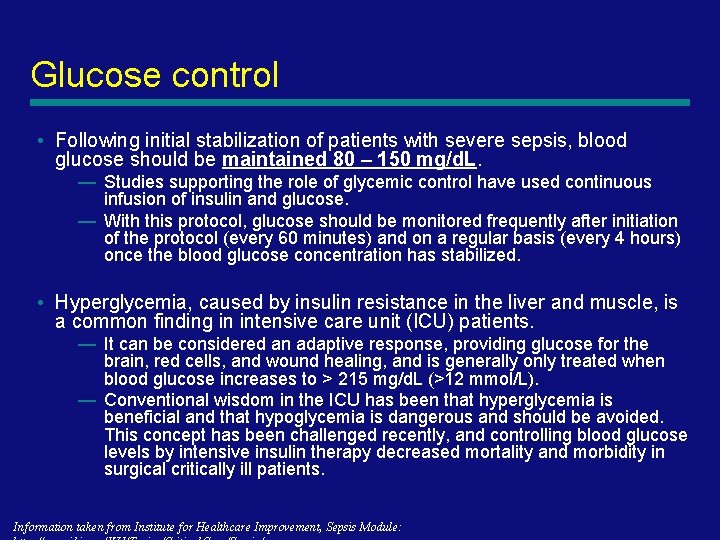
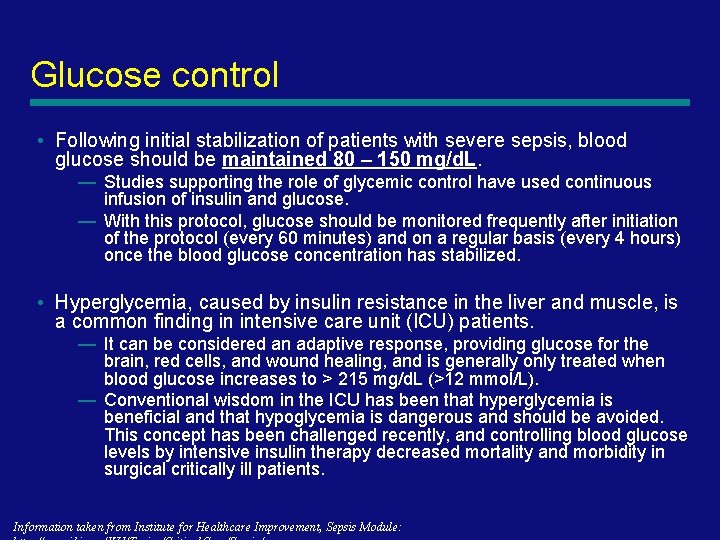
Glucose control • Following initial stabilization of patients with severe sepsis, blood glucose should be maintained 80 – 150 mg/d. L. — Studies supporting the role of glycemic control have used continuous infusion of insulin and glucose. — With this protocol, glucose should be monitored frequently after initiation of the protocol (every 60 minutes) and on a regular basis (every 4 hours) once the blood glucose concentration has stabilized. • Hyperglycemia, caused by insulin resistance in the liver and muscle, is a common finding in intensive care unit (ICU) patients. — It can be considered an adaptive response, providing glucose for the brain, red cells, and wound healing, and is generally only treated when blood glucose increases to > 215 mg/d. L (>12 mmol/L). — Conventional wisdom in the ICU has been that hyperglycemia is beneficial and that hypoglycemia is dangerous and should be avoided. This concept has been challenged recently, and controlling blood glucose levels by intensive insulin therapy decreased mortality and morbidity in surgical critically ill patients. Information taken from Institute for Healthcare Improvement, Sepsis Module:
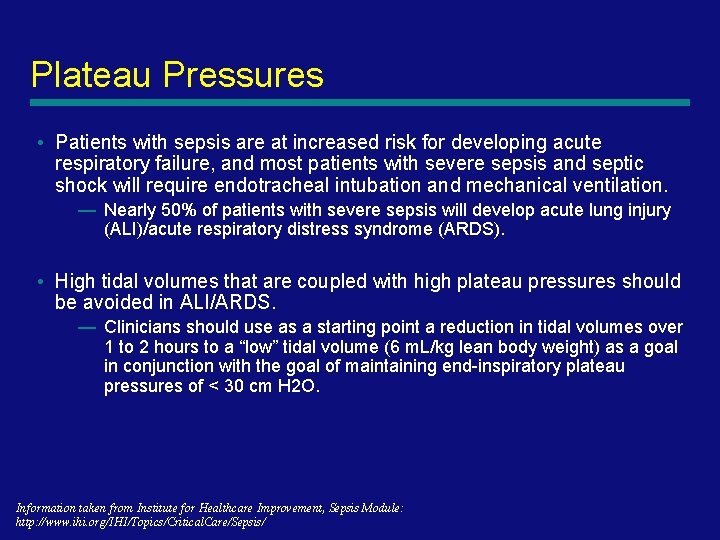
Plateau Pressures • Patients with sepsis are at increased risk for developing acute respiratory failure, and most patients with severe sepsis and septic shock will require endotracheal intubation and mechanical ventilation. — Nearly 50% of patients with severe sepsis will develop acute lung injury (ALI)/acute respiratory distress syndrome (ARDS). • High tidal volumes that are coupled with high plateau pressures should be avoided in ALI/ARDS. — Clinicians should use as a starting point a reduction in tidal volumes over 1 to 2 hours to a “low” tidal volume (6 m. L/kg lean body weight) as a goal in conjunction with the goal of maintaining end-inspiratory plateau pressures of < 30 cm H 2 O. Information taken from Institute for Healthcare Improvement, Sepsis Module: http: //www. ihi. org/IHI/Topics/Critical. Care/Sepsis/
Vasopressors • Norepinephrine and Dopamine —First line therapy —Central line preferred • Vasopressin —Give at doses of 0. 04 units/minute in addition to norepinephrine or dopamine —Not titrated • Phenylephrine/Epinephrine —Not used as first line due to risk of ischemia —In septic patients, it is added in shock refractory to norepinephrine or dopamine
Dobutamine • When it’s used: after fluid resuscitation, it is considered (in conjunction with hematocrit evaluation) to increase Sc. VO 2 > 70%. • How it works: Dobutamine directly stimulates ß 1 receptors of the heart to increase myocardial contractility and stroke volume, resulting in increased cardiac output. • Dosing: — Increase by 2 mcg/kg/minute with each Sc. VO 2 reading that is < 70% • Monitoring: — Monitor for hypotension, arrhythmia
Blood products • When it’s used: if the Sc. VO 2 remains < 70% despite adequate fluid resuscitation, consider transfusion to a hematocrit of 30%. • How it works: Increases blood carrying capacity to the tissues. • Dosing: — Patient specific (however, 1 unit of PRBCs should increase the hematocrit by ~3%) • Monitoring: — Per routine
Antibiotic Therapy • Started within the first hour of recognition of severe sepsis after cultures (Grade E) • One or more drugs with activity against the likely pathogens • Penetrate into the presumed source of sepsis • Guided by the susceptibility patterns of mo. s in the community and in the hospital (Grade D) • Reassess after 48– 72 hrs, aim for narrow spectrum antibiotic • Duration 7– 10 days and guided by clinical response. (Grade E) 64
Summary • • • Sepsis may be obvious or subtle early There is a high mortality and morbidity Have a high index of suspicion Know local organisms / susceptibilities Take appropriate cultures Treat early and aggressively Investigate early and aggressively Refer early and aggressively Be aware of new developments 65
66
67
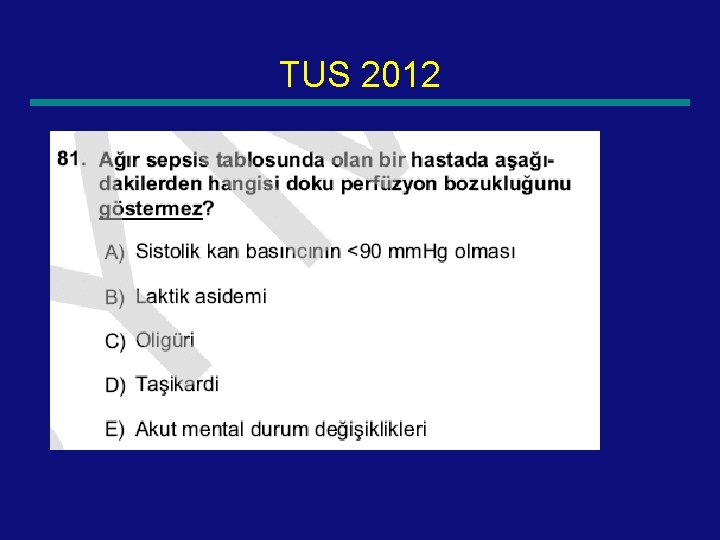
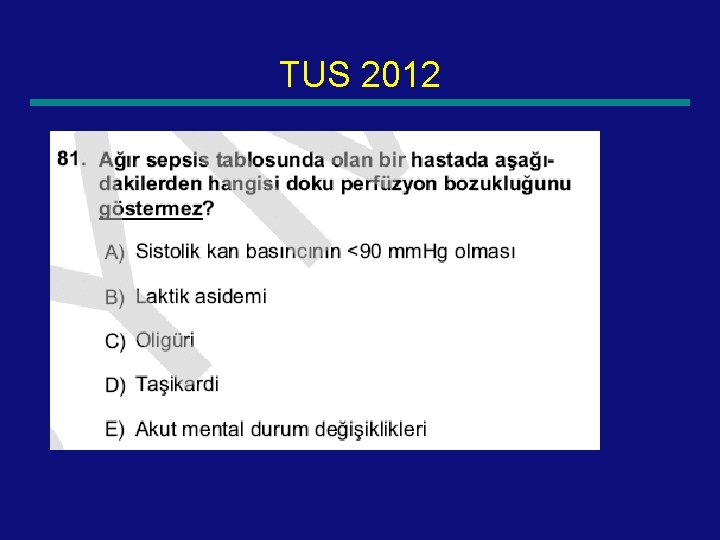
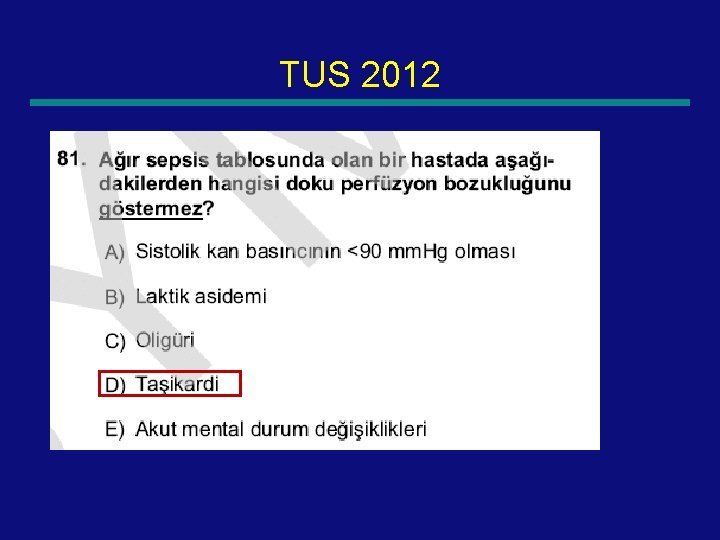
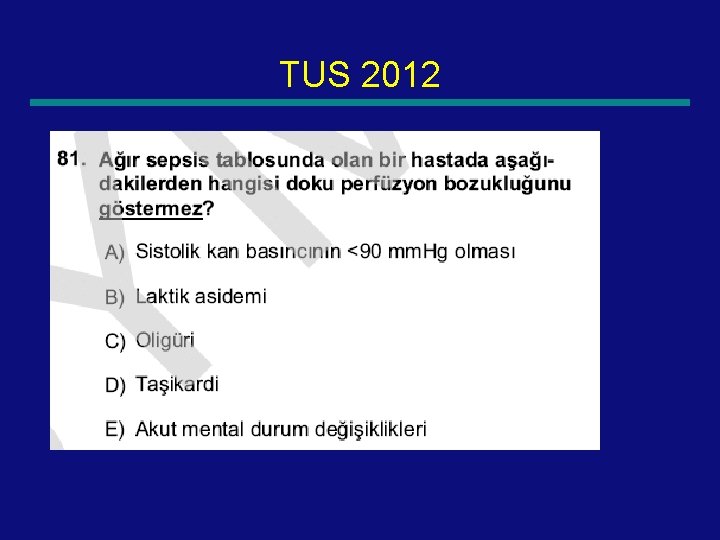
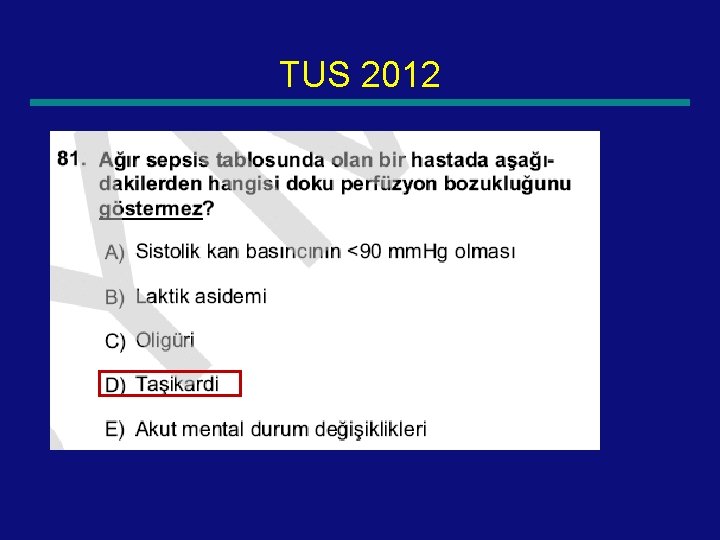
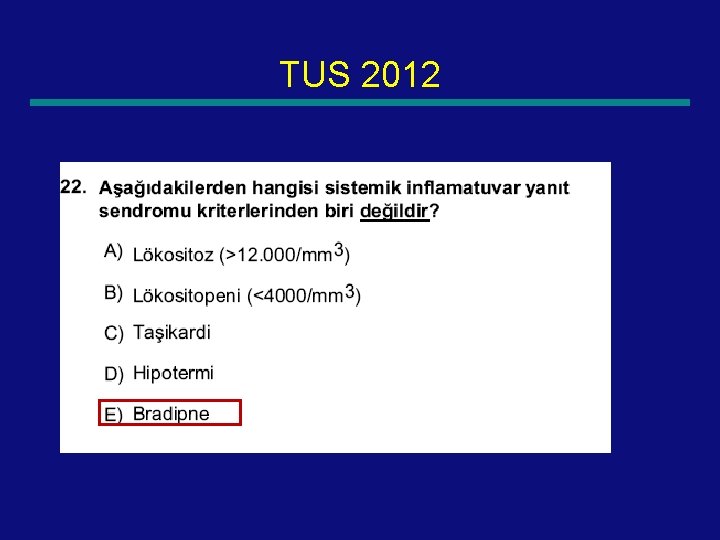
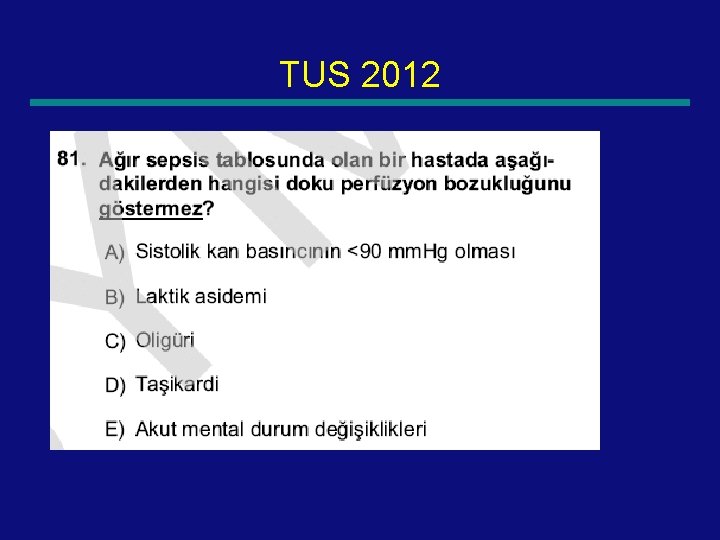
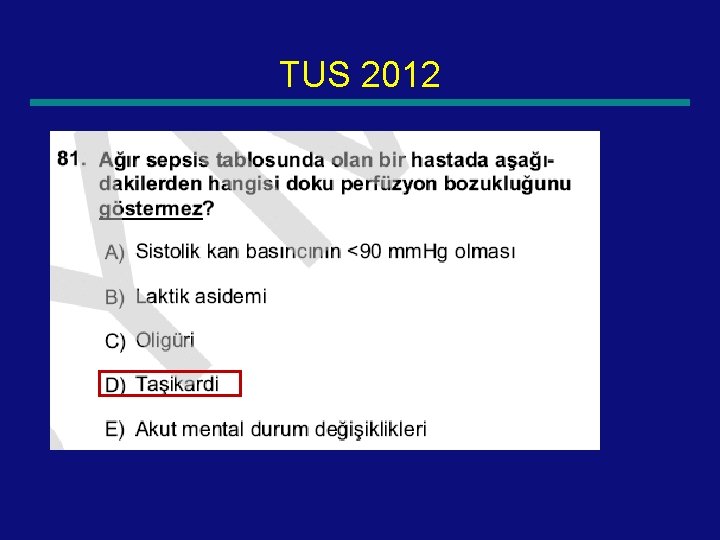
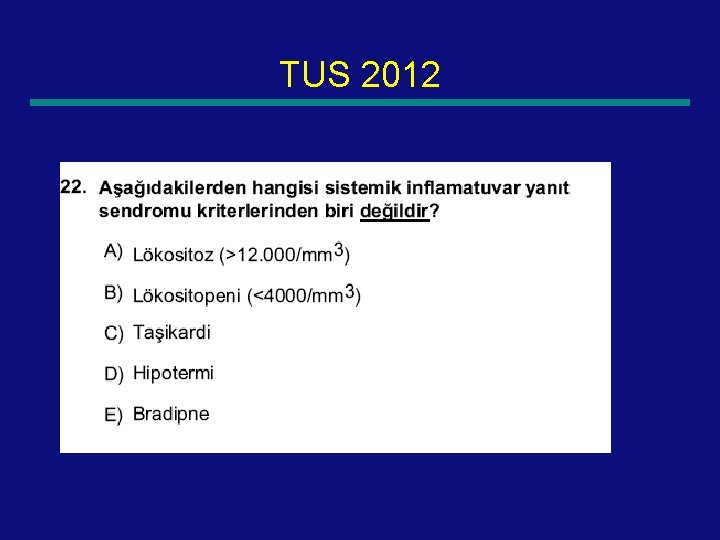
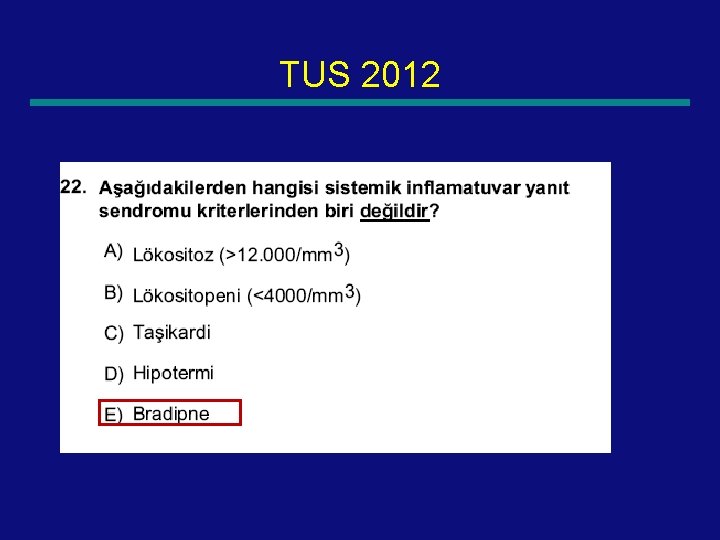
TUS 2012 68
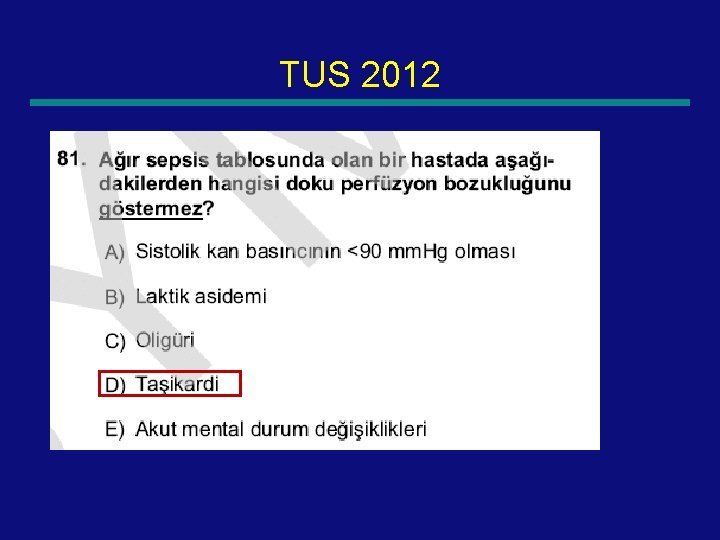
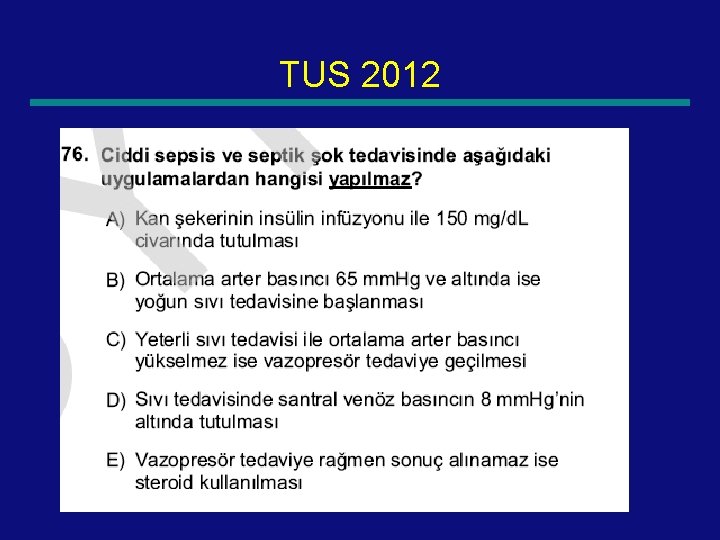
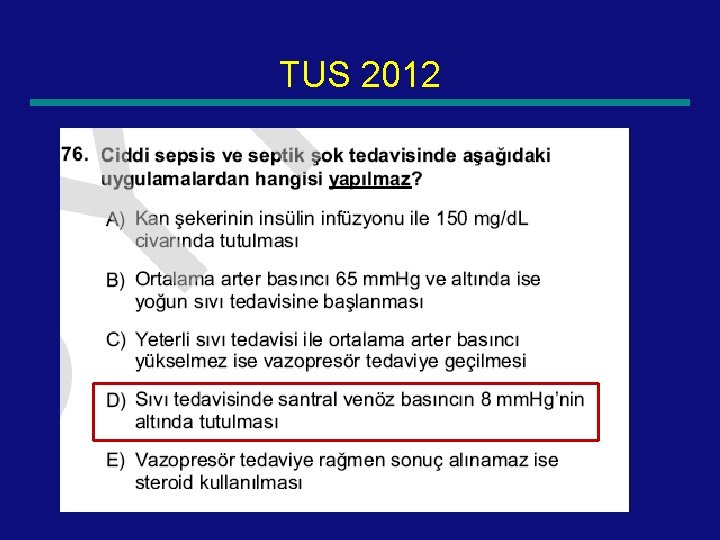
TUS 2012 69
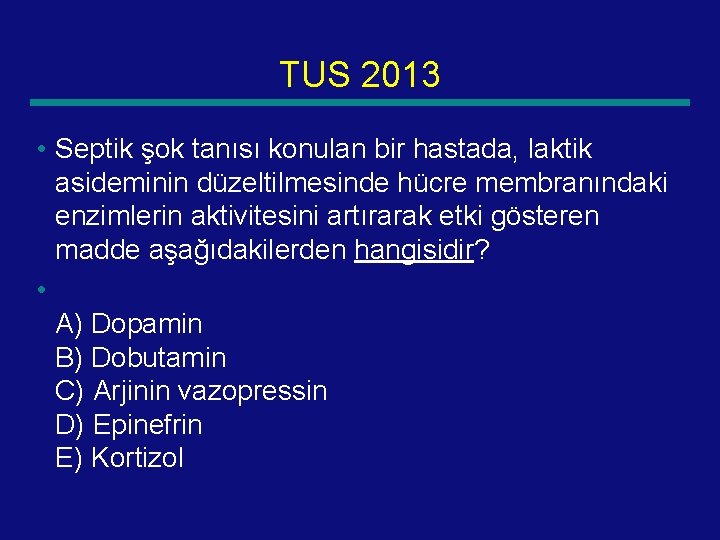
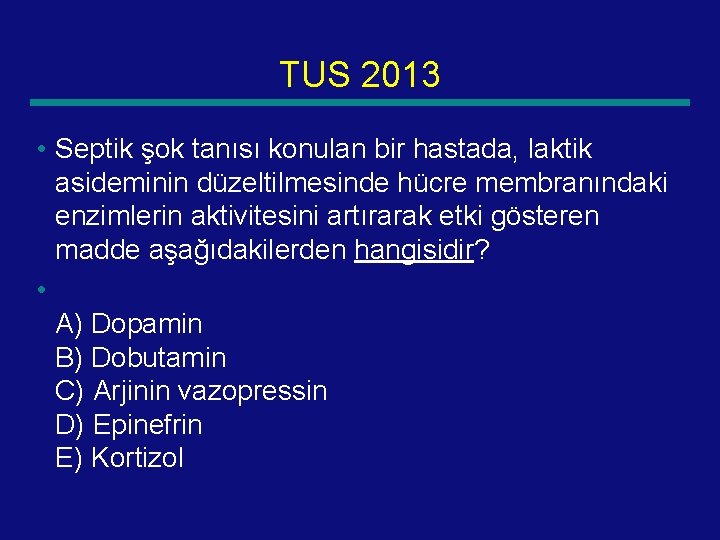
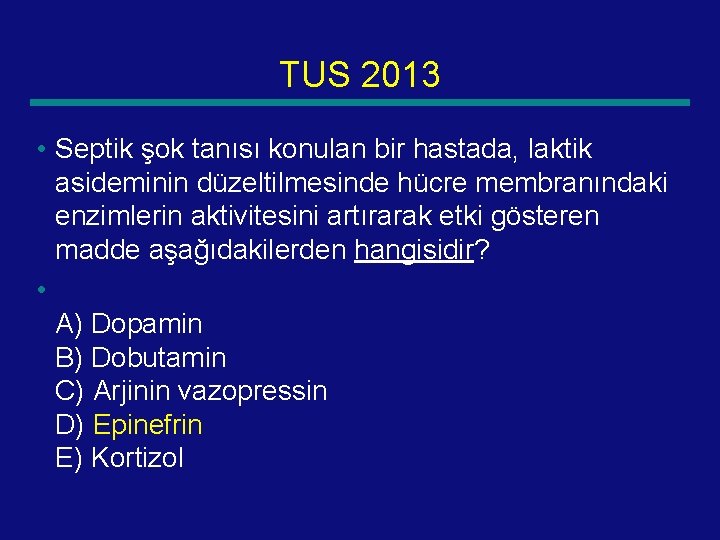
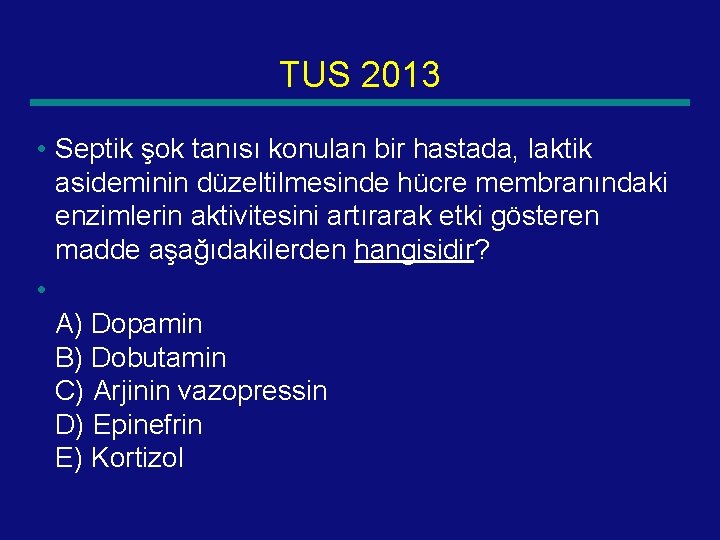
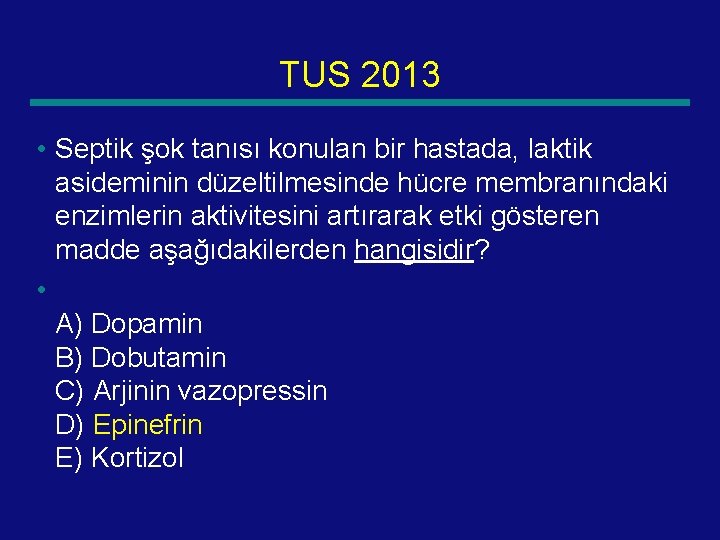
TUS 2013 • Septik şok tanısı konulan bir hastada, laktik asideminin düzeltilmesinde hücre membranındaki enzimlerin aktivitesini artırarak etki gösteren madde aşağıdakilerden hangisidir? • A) Dopamin B) Dobutamin C) Arjinin vazopressin D) Epinefrin E) Kortizol 70
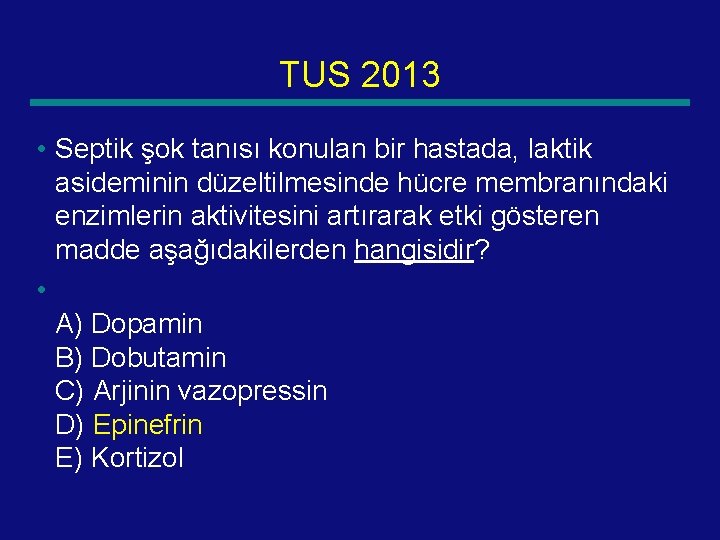
TUS 2013 • Septik şok tanısı konulan bir hastada, laktik asideminin düzeltilmesinde hücre membranındaki enzimlerin aktivitesini artırarak etki gösteren madde aşağıdakilerden hangisidir? • A) Dopamin B) Dobutamin C) Arjinin vazopressin D) Epinefrin E) Kortizol 71
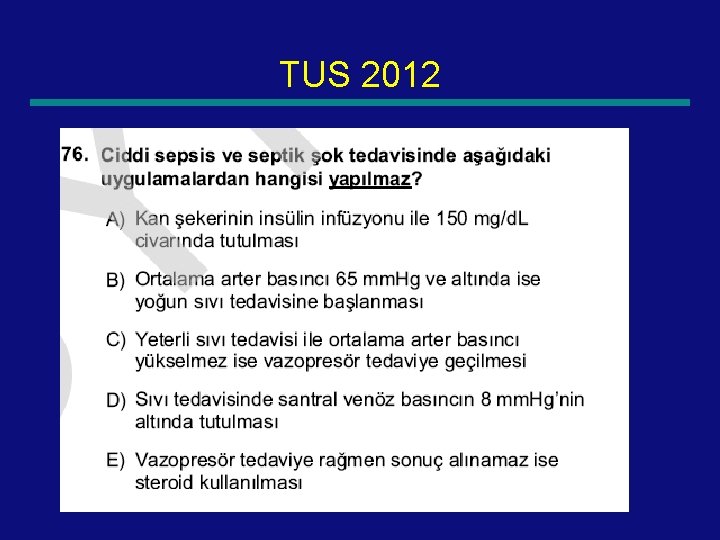
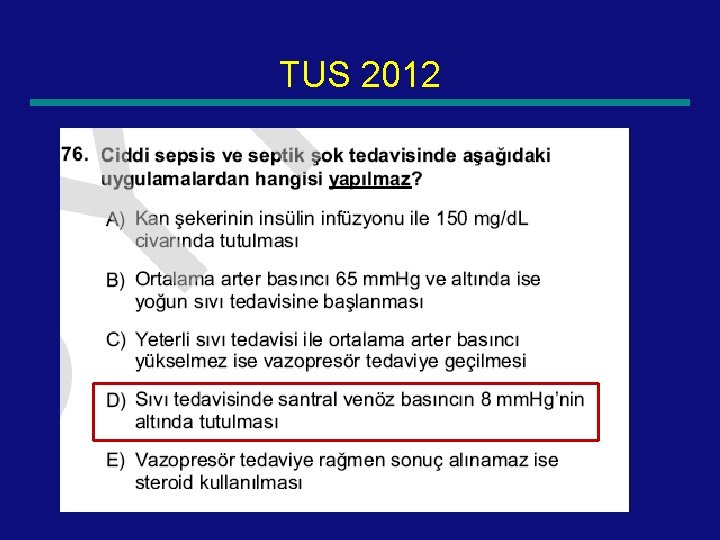
TUS 2012 72
TUS 2012 73
TUS 2012 74
TUS 2012 75
TUS 2012 76
TUS 2012 77
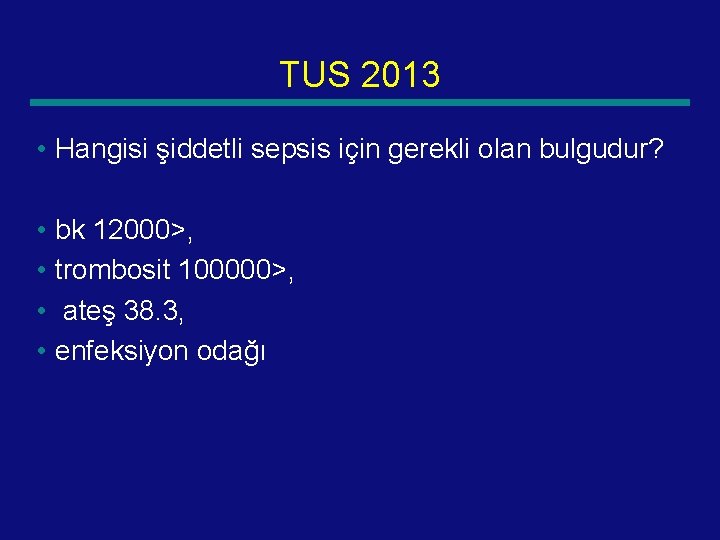
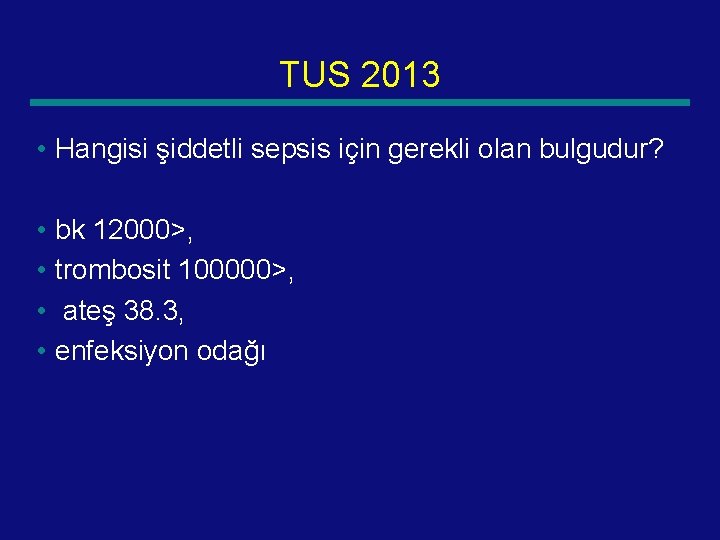
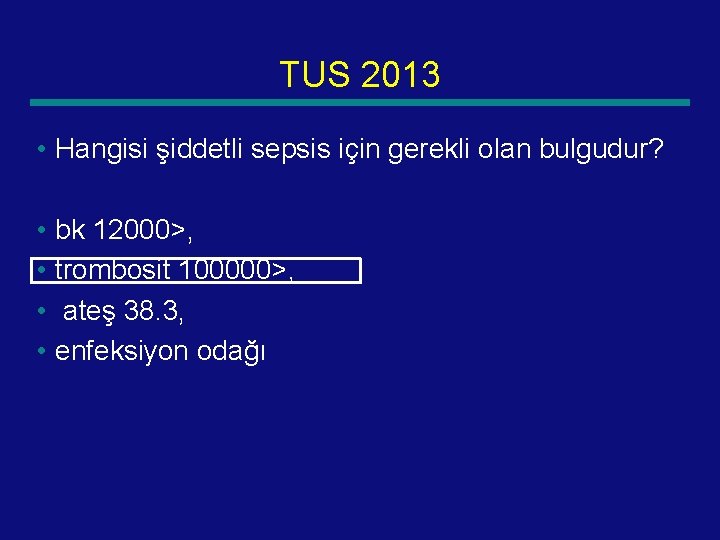
TUS 2013 • Hangisi şiddetli sepsis için gerekli olan bulgudur? • bk 12000>, • trombosit 100000>, • ateş 38. 3, • enfeksiyon odağı 78
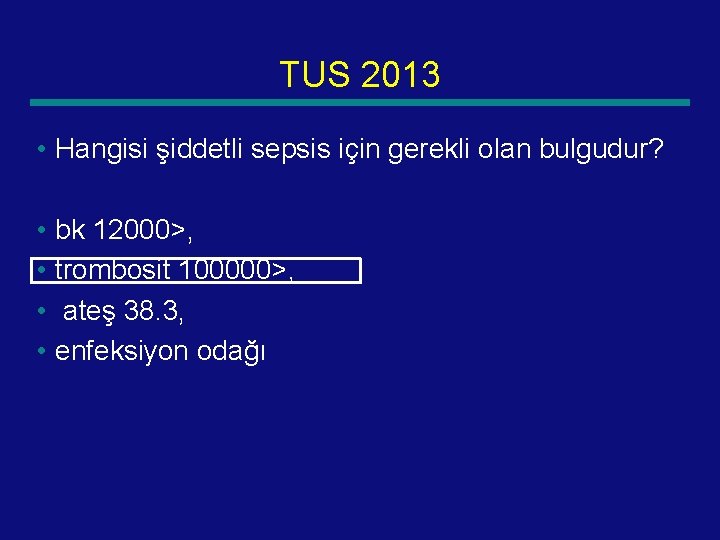
TUS 2013 • Hangisi şiddetli sepsis için gerekli olan bulgudur? • bk 12000>, • trombosit 100000>, • ateş 38. 3, • enfeksiyon odağı 79
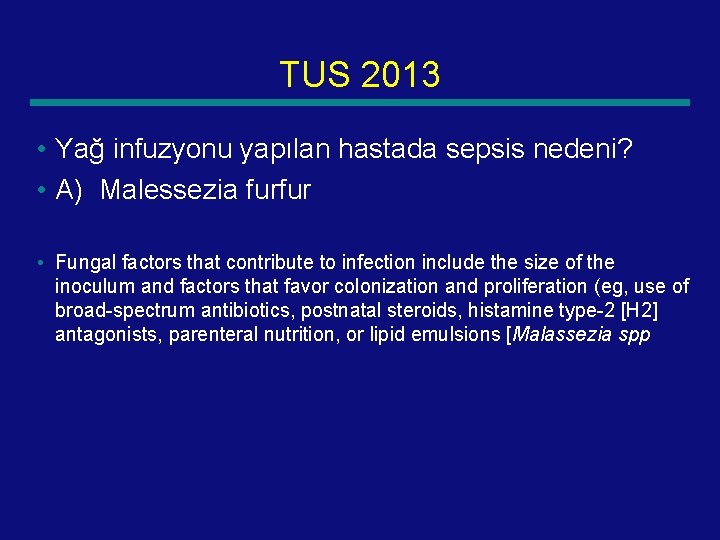
TUS 2013 • Yağ infuzyonu yapılan hastada sepsis nedeni? • A) Malessezia furfur • Fungal factors that contribute to infection include the size of the inoculum and factors that favor colonization and proliferation (eg, use of broad-spectrum antibiotics, postnatal steroids, histamine type-2 [H 2] antagonists, parenteral nutrition, or lipid emulsions [Malassezia spp 80
TUS 2013 • Septik şok tanısı konulan bir hastada, laktik asideminin düzeltilmesinde hücre membranındaki enzimlerin aktivitesini artırarak etki gösteren madde aşağıdakilerden hangisidir? • A) Dopamin B) Dobutamin C) Arjinin vazopressin D) Epinefrin E) Kortizol 81
TUS 2013 • Septik şok tanısı konulan bir hastada, laktik asideminin düzeltilmesinde hücre membranındaki enzimlerin aktivitesini artırarak etki gösteren madde aşağıdakilerden hangisidir? • A) Dopamin B) Dobutamin C) Arjinin vazopressin D) Epinefrin E) Kortizol 82
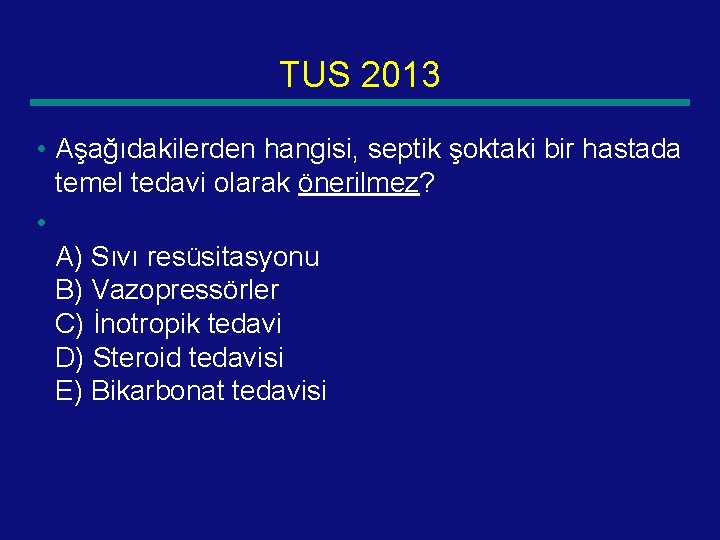
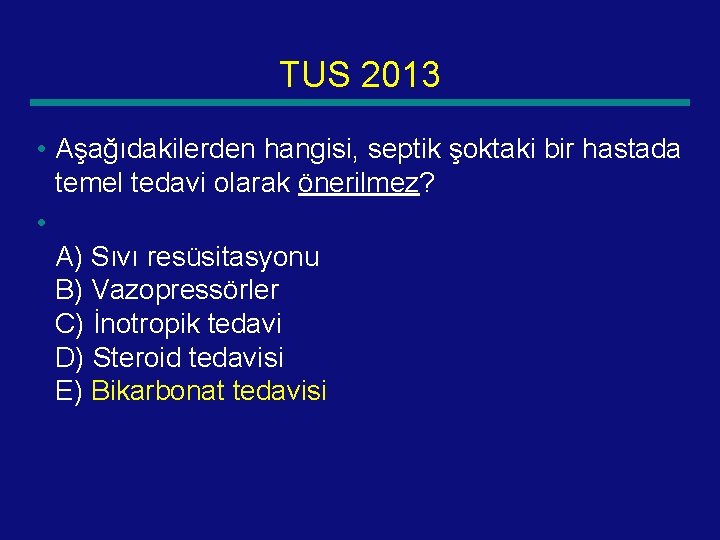
TUS 2013 • Aşağıdakilerden hangisi, septik şoktaki bir hastada temel tedavi olarak önerilmez? • A) Sıvı resüsitasyonu B) Vazopressörler C) İnotropik tedavi D) Steroid tedavisi E) Bikarbonat tedavisi 83
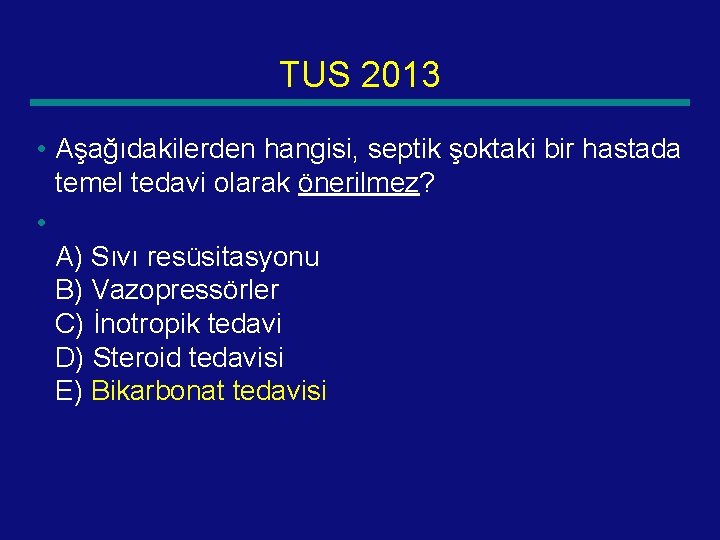
TUS 2013 • Aşağıdakilerden hangisi, septik şoktaki bir hastada temel tedavi olarak önerilmez? • A) Sıvı resüsitasyonu B) Vazopressörler C) İnotropik tedavi D) Steroid tedavisi E) Bikarbonat tedavisi 84
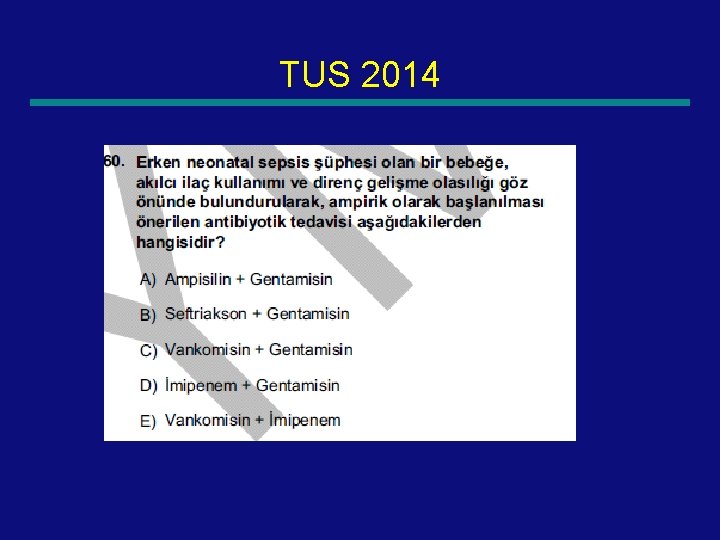
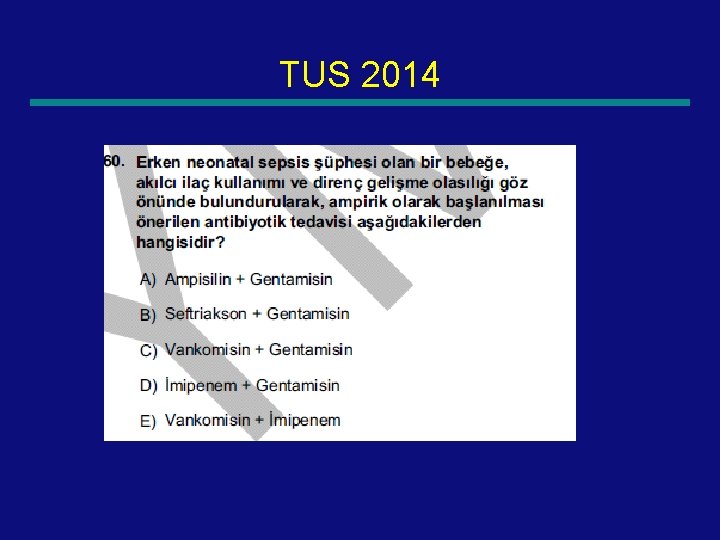
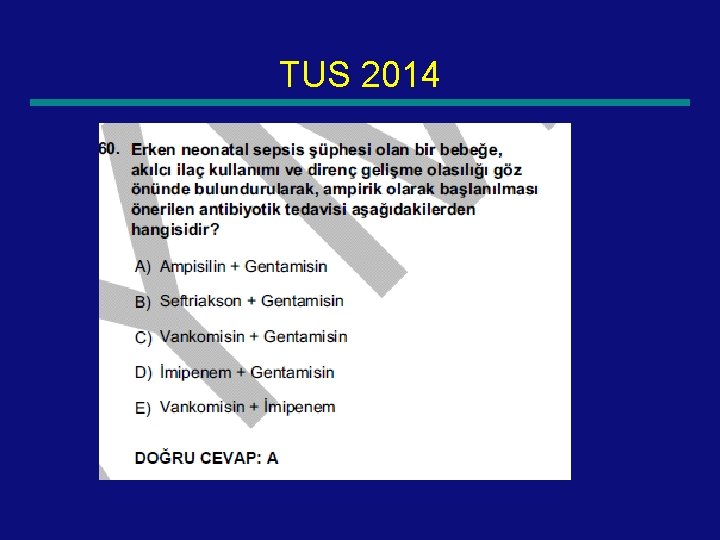
TUS 2014 85
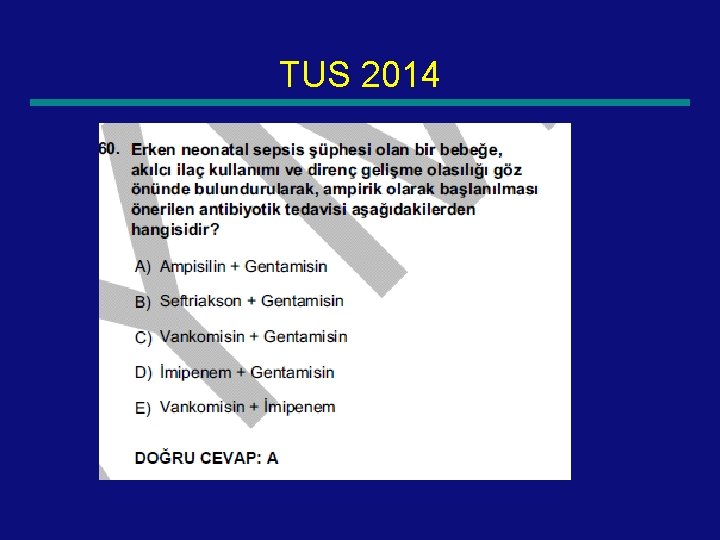
TUS 2014 86
 Sepsis 2 vs sepsis 3
Sepsis 2 vs sepsis 3 T10 spinal cord
T10 spinal cord Site:slidetodoc.com
Site:slidetodoc.com Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Shock normovolemico
Shock normovolemico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Pınar seden meral
Pınar seden meral Meral aban
Meral aban Meral nur ergin
Meral nur ergin Meral dogan
Meral dogan Meral yılmaz öğretmen
Meral yılmaz öğretmen Protokol sıralaması
Protokol sıralaması Hypovolumic
Hypovolumic Anaphylactic shock hemodynamics
Anaphylactic shock hemodynamics Shock prof
Shock prof Jea septic tank phase out
Jea septic tank phase out Nongonococcal septic arthritis
Nongonococcal septic arthritis Oxygen sag curve
Oxygen sag curve Septic arthritis antibiotics
Septic arthritis antibiotics Septic squeeze test tonsillitis
Septic squeeze test tonsillitis Summit county septic permit
Summit county septic permit Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Septic arthritis complications
Septic arthritis complications Septic tank contamination groundwater
Septic tank contamination groundwater Thymoma location
Thymoma location Septic arthritis complications
Septic arthritis complications Bat septic
Bat septic Advantex ax20
Advantex ax20 Admixtures
Admixtures Satellitism in haemophilus influenzae
Satellitism in haemophilus influenzae Panhandle health septic
Panhandle health septic Gonorrhea symptoms
Gonorrhea symptoms Septic workup
Septic workup Doc's septic tank cleaning
Doc's septic tank cleaning Multiflow septic system
Multiflow septic system Barnstable county septic loan
Barnstable county septic loan Carmody septic
Carmody septic Example of gram negative cocci
Example of gram negative cocci Septic arthritis antibiotics
Septic arthritis antibiotics Indianapolis septic tank elimination program
Indianapolis septic tank elimination program Septic
Septic Enthesitis
Enthesitis Puraflo peat septic system
Puraflo peat septic system Pickwickian syndrome in dogs
Pickwickian syndrome in dogs The severe style is characterized by
The severe style is characterized by Dehydration types
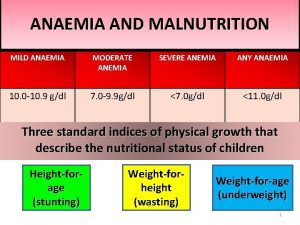
Dehydration types Severe preeclampsia criteria
Severe preeclampsia criteria International severe asthma registry
International severe asthma registry Domina petric
Domina petric Wmo severe weather
Wmo severe weather Severe weather data inventory
Severe weather data inventory What is life
What is life Types of bronchial asthma
Types of bronchial asthma Severe obesity
Severe obesity Combined immunodeficiency
Combined immunodeficiency Hypocalcemia range
Hypocalcemia range Cumulus mature dissipating
Cumulus mature dissipating Severe pong game cards
Severe pong game cards Iron studies interpretation
Iron studies interpretation Nabozenstvo na severe afriky
Nabozenstvo na severe afriky Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation Match the description with the example whmis
Match the description with the example whmis Severe weather safety precautions worksheet
Severe weather safety precautions worksheet Potassium dose calculation
Potassium dose calculation Edrolo
Edrolo Severe weather graphic organizer
Severe weather graphic organizer Define mitral stenosis
Define mitral stenosis Asthma index
Asthma index Severe hypocalcemia
Severe hypocalcemia Siadh euvolemic hyponatremia
Siadh euvolemic hyponatremia Singulutus
Singulutus Switching antidepressants chart
Switching antidepressants chart Unmet needs in severe asthma
Unmet needs in severe asthma Severe npdr definition
Severe npdr definition Dka criteria
Dka criteria Malnutrition case study
Malnutrition case study None mild moderate severe
None mild moderate severe Cholera
Cholera Outsiders chapter 7 vocabulary
Outsiders chapter 7 vocabulary Emt chapter 24 trauma overview
Emt chapter 24 trauma overview Severe anemia
Severe anemia Fluid of choice in severe dehydration
Fluid of choice in severe dehydration Types of dehydration
Types of dehydration Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Red bouncing ball game
Red bouncing ball game Domina severe
Domina severe