Spinal Cord Injuries Dr Mohamed abdul jalil altamimi
Spinal Cord Injuries Dr Mohamed abdul jalil altamimi Consultant neurosurgeon Department of surgery 2016 -2017
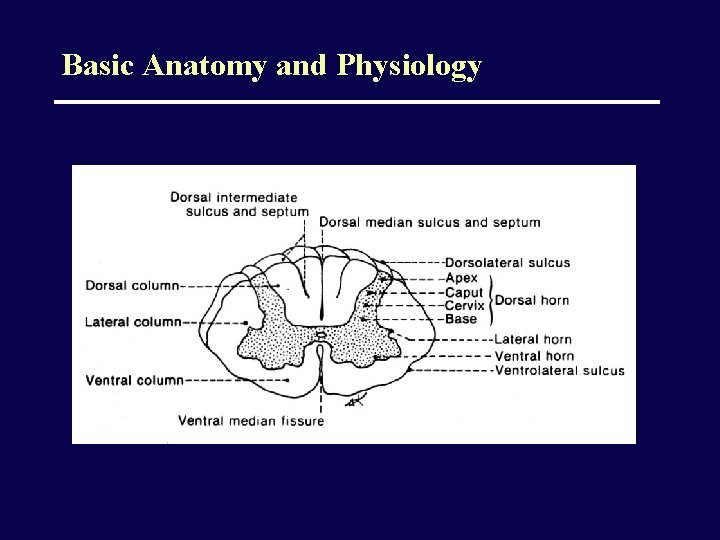
Basic Anatomy and Physiology
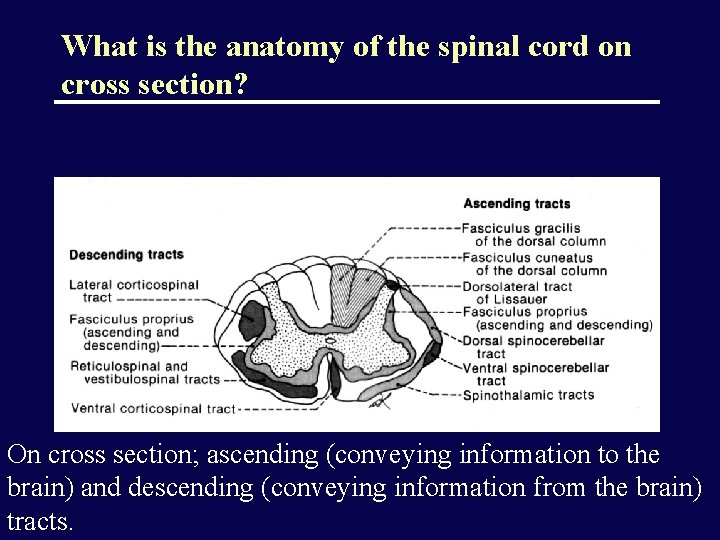
What is the anatomy of the spinal cord on cross section? On cross section; ascending (conveying information to the brain) and descending (conveying information from the brain) tracts.
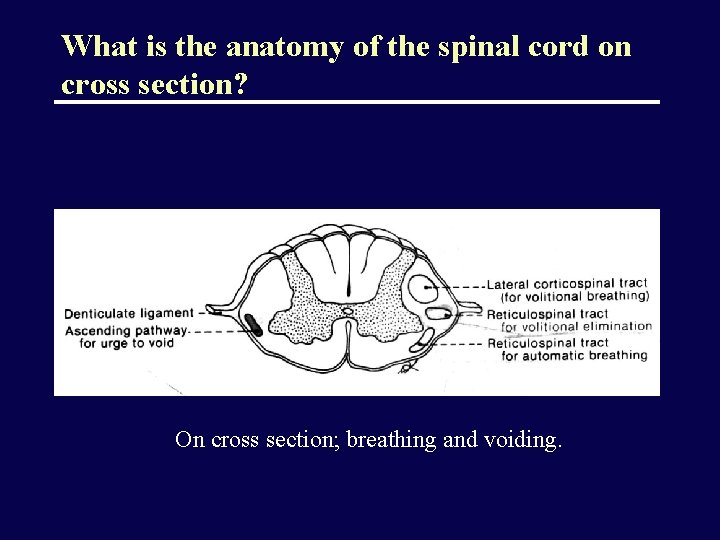
What is the anatomy of the spinal cord on cross section? On cross section; breathing and voiding.
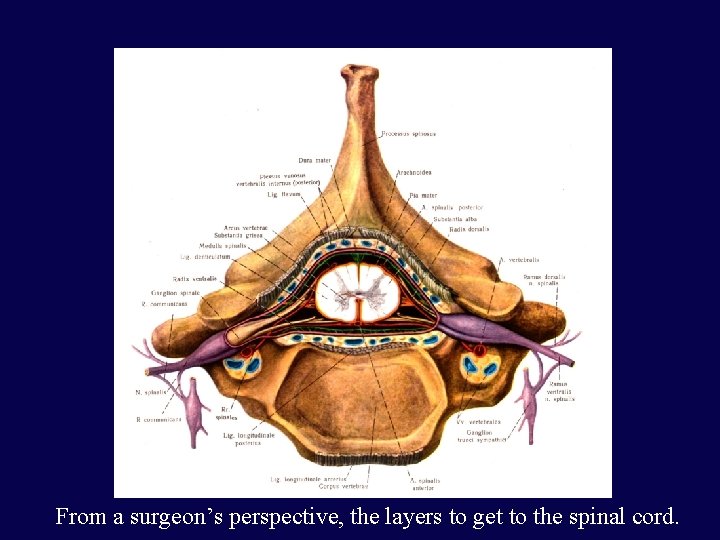
From a surgeon’s perspective, the layers to get to the spinal cord.
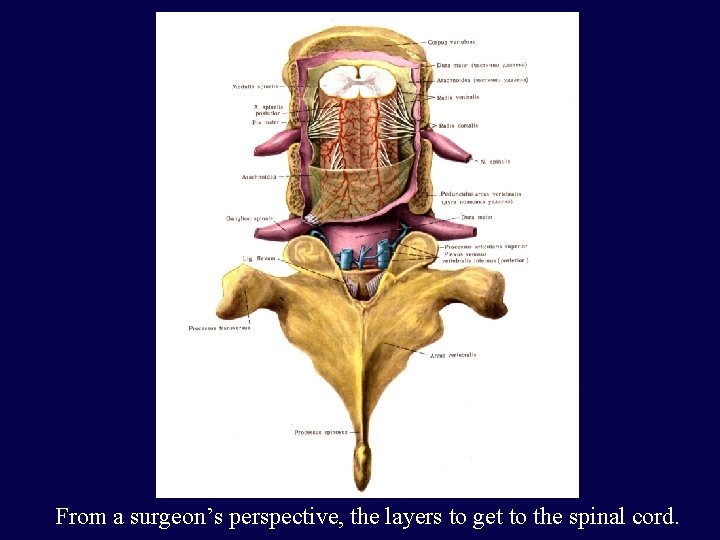
From a surgeon’s perspective, the layers to get to the spinal cord.
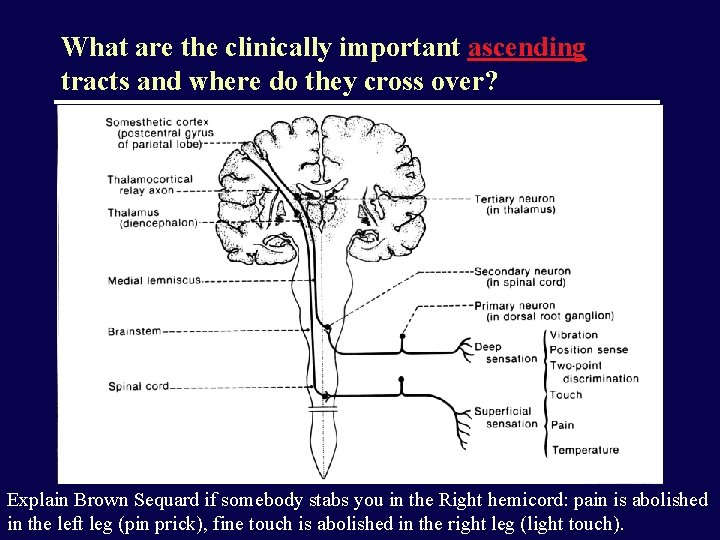
What are the clinically important ascending tracts and where do they cross over? Explain Brown Sequard if somebody stabs you in the Right hemicord: pain is abolished in the left leg (pin prick), fine touch is abolished in the right leg (light touch).
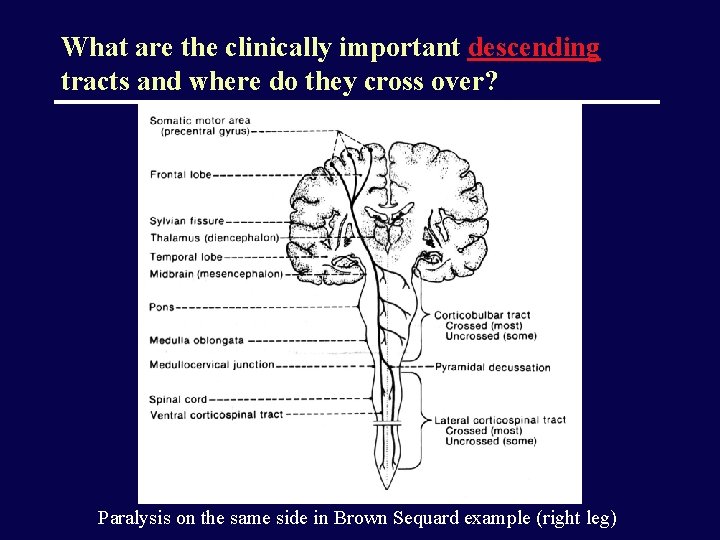
What are the clinically important descending tracts and where do they cross over? Paralysis on the same side in Brown Sequard example (right leg)
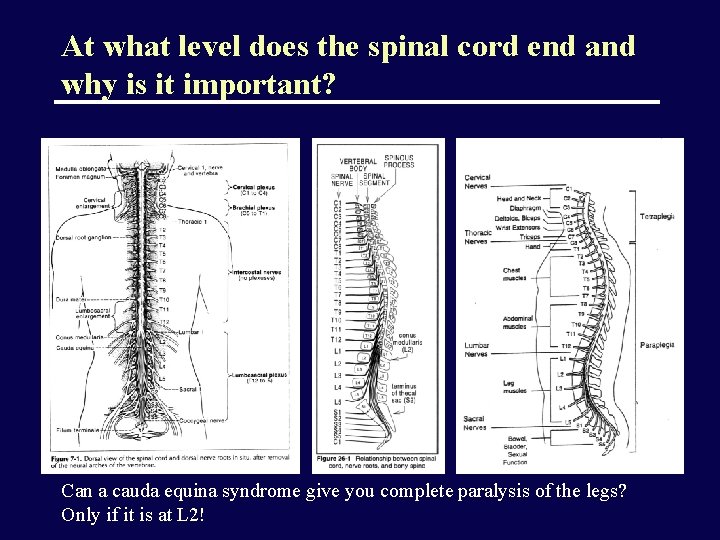
At what level does the spinal cord end and why is it important? Can a cauda equina syndrome give you complete paralysis of the legs? Only if it is at L 2!
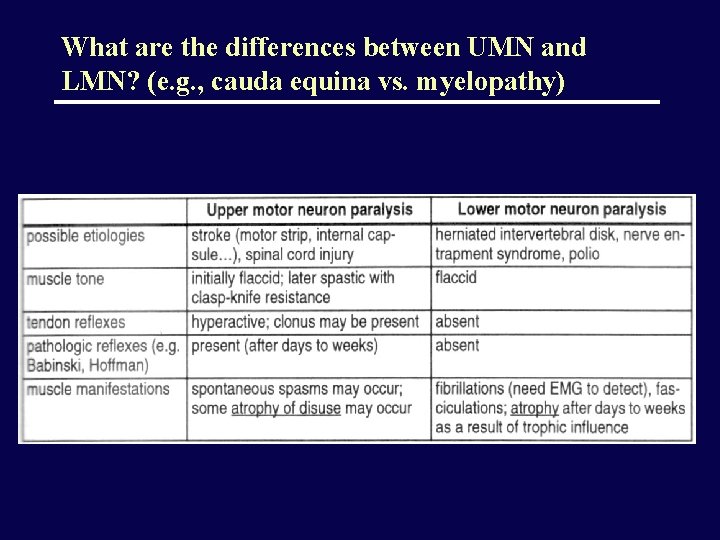
What are the differences between UMN and LMN? (e. g. , cauda equina vs. myelopathy)
SPINAL TRAUMA
Acute vs. chronic injuries; complete vs. incomplete injuries • “Acute”=sudden onset of symptoms • “Complete” ?
What is a complete spinal cord injury? • “Complete” = absence of sensory and motor function in the perianal area (S 4 -S 5)
Terminology • Plegia = complete lesion • Paresis = some muscle strength is preserved • Tetraplegia (or quadriplegia) • Injury of the cervical spinal cord • Patient can usually still move his arms using the segments above the injury (e. g. , in a C 7 injury, the patient can still flex his forearms, using the C 5 segment) • Paraplegia • Injury of the thoracic or lumbo-sacral cord, or cauda equina • Hemiplegia • Paralysis of one half of the body • Usually in brain injuries (e. g. , stroke)
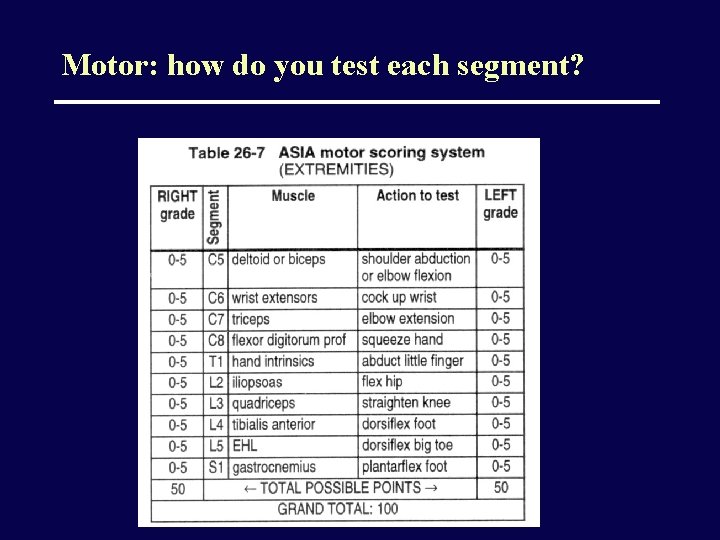
Motor: how do you test each segment?
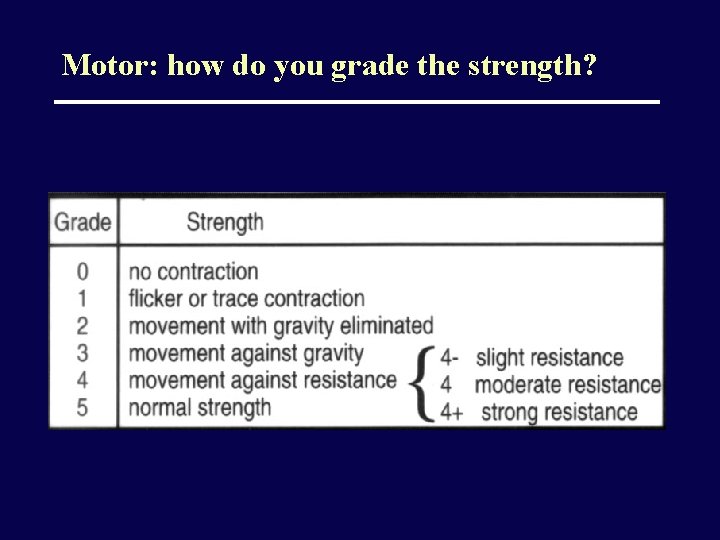
Motor: how do you grade the strength?
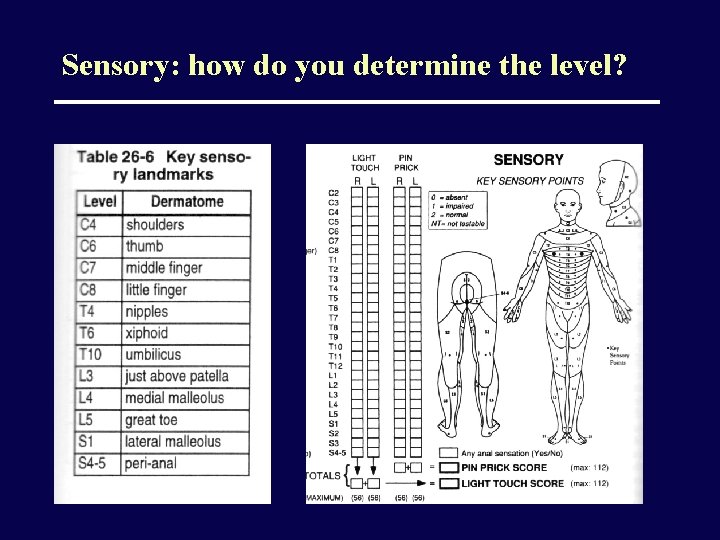
Sensory: how do you determine the level?
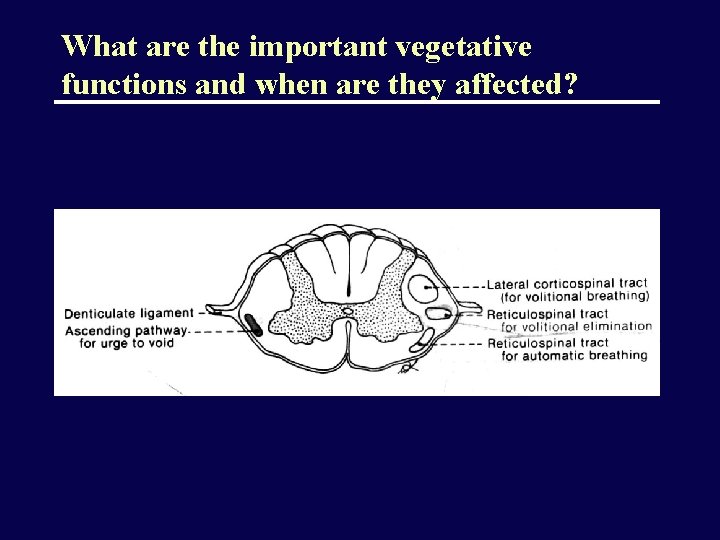
What are the important vegetative functions and when are they affected?
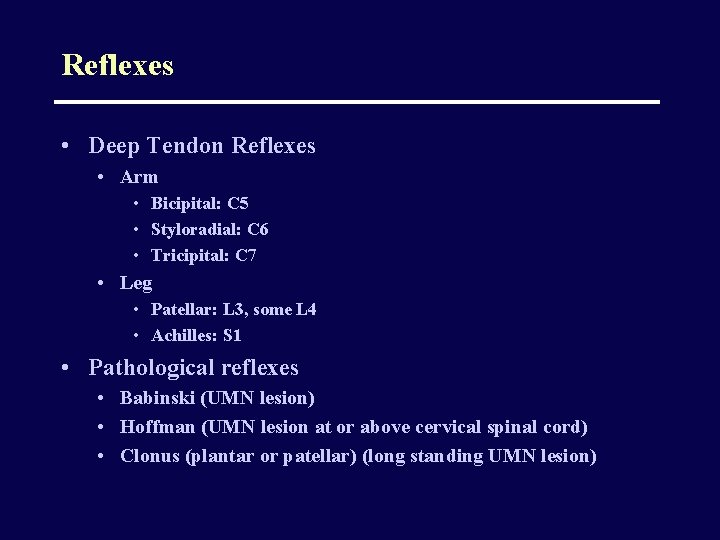
Reflexes • Deep Tendon Reflexes • Arm • Bicipital: C 5 • Styloradial: C 6 • Tricipital: C 7 • Leg • Patellar: L 3, some L 4 • Achilles: S 1 • Pathological reflexes • Babinski (UMN lesion) • Hoffman (UMN lesion at or above cervical spinal cord) • Clonus (plantar or patellar) (long standing UMN lesion)
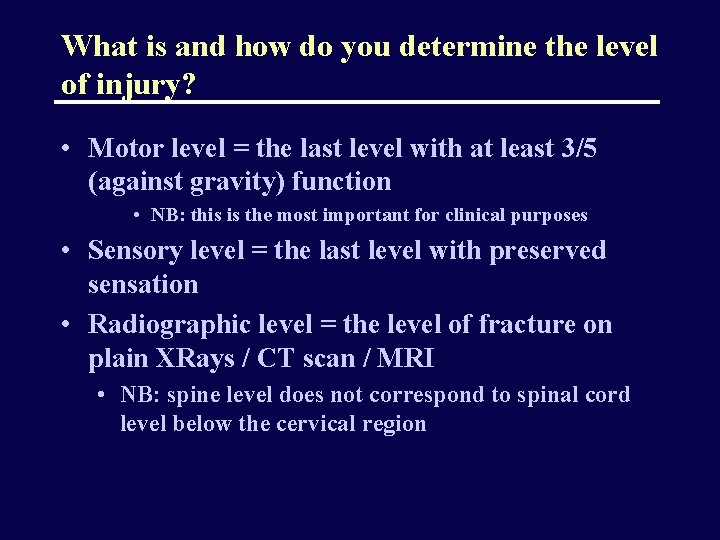
What is and how do you determine the level of injury? • Motor level = the last level with at least 3/5 (against gravity) function • NB: this is the most important for clinical purposes • Sensory level = the last level with preserved sensation • Radiographic level = the level of fracture on plain XRays / CT scan / MRI • NB: spine level does not correspond to spinal cord level below the cervical region
Case scenario • • 25 y/o white male Fell off the roof (20 feet) Had to be intubated at the scene by EMS Consciousness regained shortly thereafter Could not move arms or legs Could close and open eyes to command Not able to breathe by himself–totally dependent on mechanical ventilation
High cervical injuries (C 3 and above) • Motor and sensory deficits involve the entire arms and legs • Dependent on mechanical ventilation for breathing (diaphragm is innervated by C 3 -C 5 levels)
Case scenario • • 19 y/o white male Diving accident (shallow water) No loss of consciousness Could not understand why he could not move his legs, forearms and hands (he could shrug shoulders and elevate arms) • BP 75/40, HR 54/’ • Had difficulties breathing and required intubation a few hours after the accident
Midcervical injuries (C 3 -C 5) • Varying degrees of diaphragm dysfunction • Usually need ventilatory assistance in the acute phase • Shock
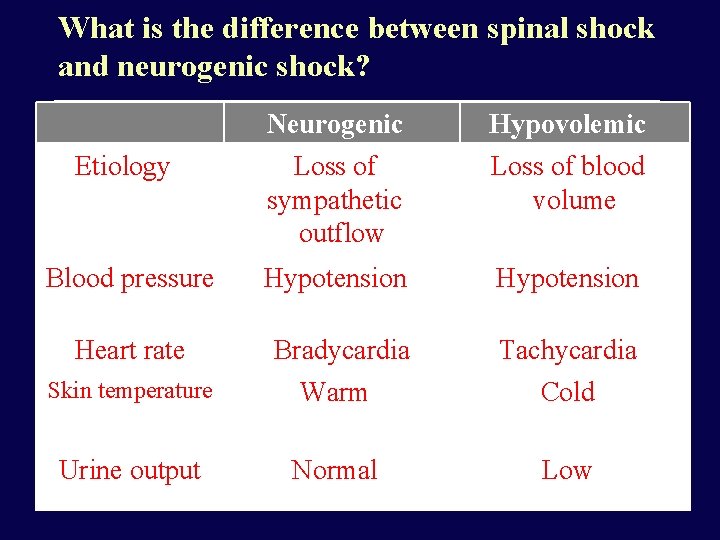
What is the difference between spinal shock and neurogenic shock? Neurogenic Hypovolemic Etiology Loss of sympathetic outflow Loss of blood volume Blood pressure Hypotension Heart rate Bradycardia Tachycardia Skin temperature Warm Cold Urine output Normal Low
Neurogenic shock • Seen in cervical injuries • Due to interruption of the sympathetic input from hypothalamus to the cardiovascular centers • Hallmark: hypotension (due to vasodilation, due to loss of sympathetic tonic input) is associated with bradycardia (not tachycardia, the usual response), due to inability to convey the information to the vasomotor centers in the spinal cord
Low cervical injuries (C 6 -T 1) • Usually able to breathe, although occasionally cord swelling can lead to temporary C 3 -C 5 involvement (need mechanical ventilation) • The level can be determined by physical exam
So what do you expect with a cervical lesion? • • Quadriplegia or quadriparesis Bowel/bladder retention (spastic) Various degrees of breathing difficulties Neurogenic and/or spinal shock
Case scenario • • • 22 y/o female Motor vehicle accident (hit a pole at 60 mph) Short term loss of consciousness (10’) Not able to move or feel her legs No bladder / bowel control or sensation Sensory level at the umbilicus
Thoracic injuries (T 2 -L 1) • Paraparesis or paraplegia • UMN (upper motor neuron) signs
Case scenario • • • 22 y/o female Motor vehicle accident Not able to move or feel her legs below the knee Could flex thighs against gravity No bladder / bowel control or sensation Sensory level above the knee on L, below the knee on R
Cauda equina injuries (L 2 or below) • Paraparesis or paraplegia • LMN (lower motor neuron) signs • Thigh flexion is almost always preserved to some degree
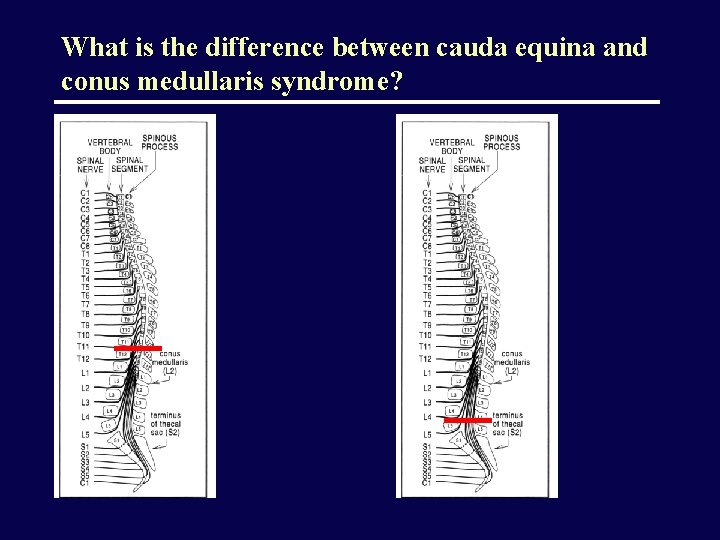
What is the difference between cauda equina and conus medullaris syndrome?
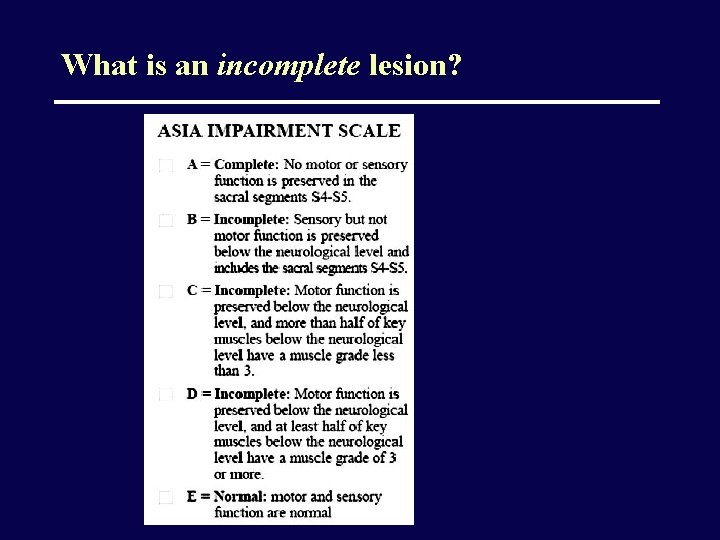
What is an incomplete lesion?
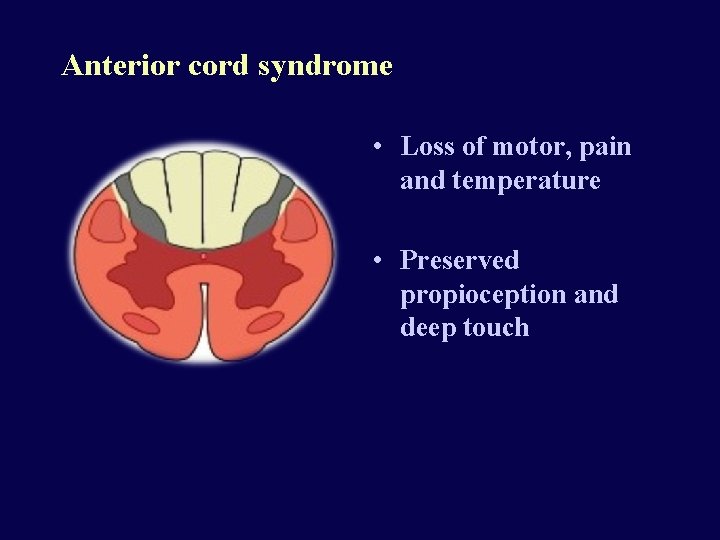
Anterior cord syndrome • Loss of motor, pain and temperature • Preserved propioception and deep touch
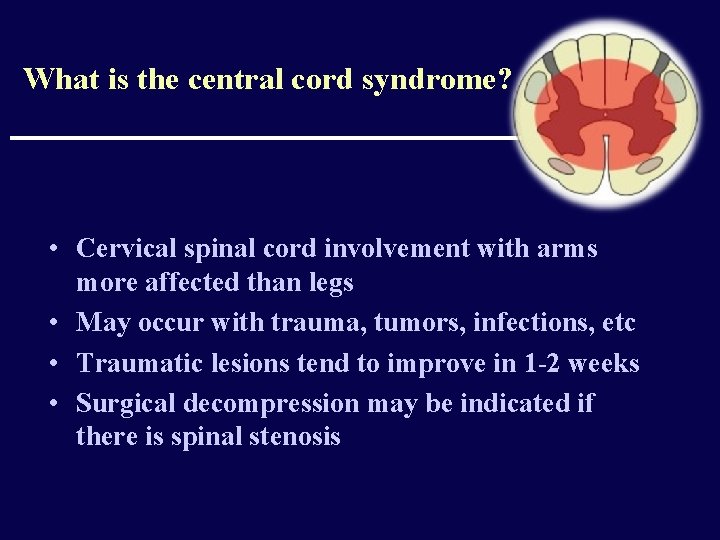
What is the central cord syndrome? • Cervical spinal cord involvement with arms more affected than legs • May occur with trauma, tumors, infections, etc • Traumatic lesions tend to improve in 1 -2 weeks • Surgical decompression may be indicated if there is spinal stenosis
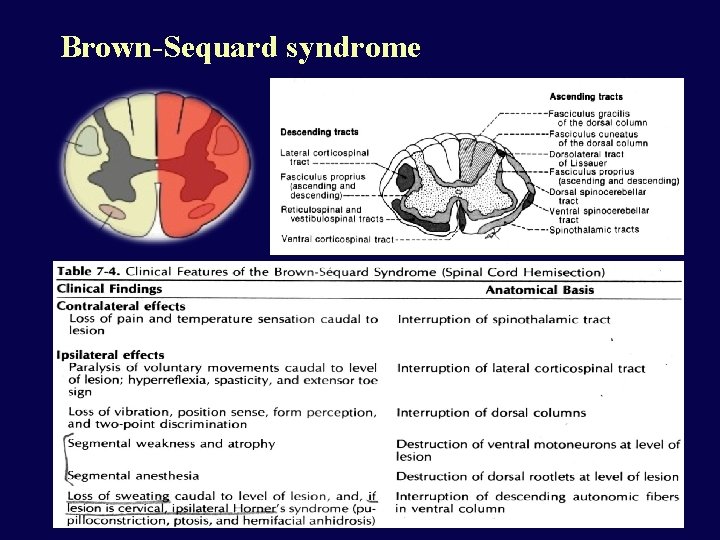
Brown-Sequard syndrome
Goal of spine trauma care • Protect further injury during evaluation and management • Identify spine injury or document absence of spine injury • Optimize conditions for maximal neurologic recovery
Suspected Spinal Injury • • • High speed crash Unconscious Multiple injuries Neurological deficit Spinal pain/tenderness Up to 15% of spinal injuries have a second (possibly non adjacent) fracture elsewhere in the spine
Initial Management • Immobilization • • Rigid collar Sandbags and straps Spine board Log-roll to turn • Prevent hypotension • Pressors: Dopamine, not Neosynephrine • Fluids to replace losses; do not overhydrate • Maintain oxygenation • O 2 per nasal canula • If intubation is needed, do NOT move the neck. Advance Trauma Life Support (ATLS) guidelines
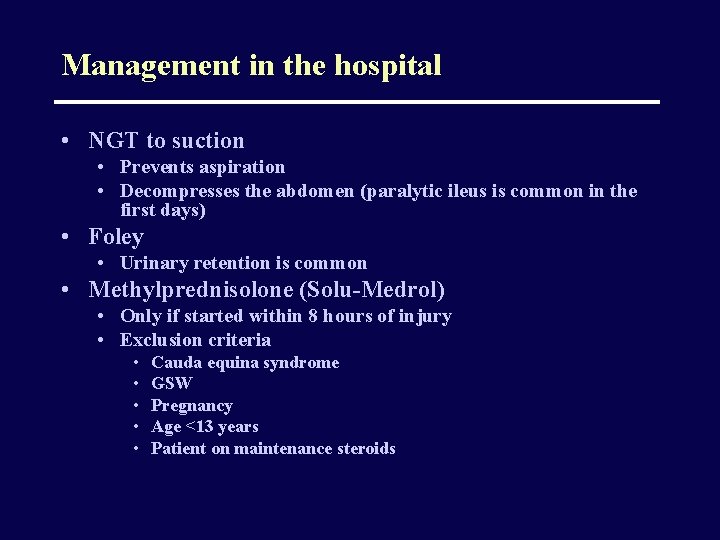
Management in the hospital • NGT to suction • Prevents aspiration • Decompresses the abdomen (paralytic ileus is common in the first days) • Foley • Urinary retention is common • Methylprednisolone (Solu-Medrol) • Only if started within 8 hours of injury • Exclusion criteria • • • Cauda equina syndrome GSW Pregnancy Age <13 years Patient on maintenance steroids
Radiolographic evaluation X-ray Guidelines (cervical) AABBCDS • • • Adequacy, Alignment Bone abnormality, Base of skull Cartilage Disc space Soft tissue
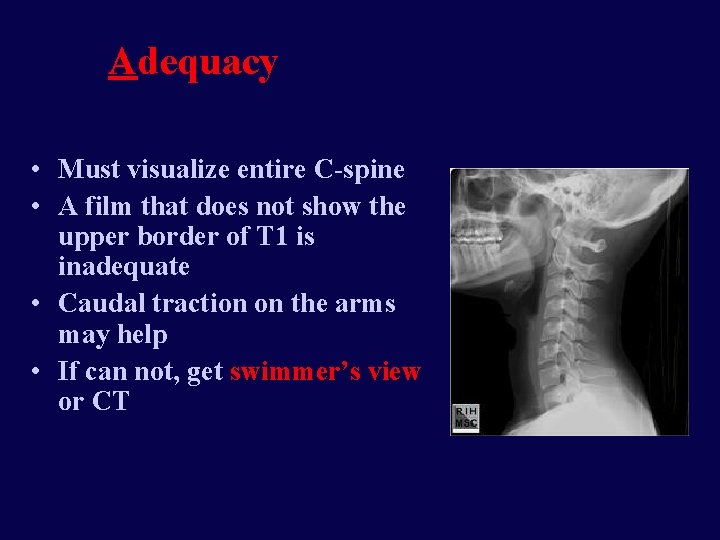
Adequacy • Must visualize entire C-spine • A film that does not show the upper border of T 1 is inadequate • Caudal traction on the arms may help • If can not, get swimmer’s view or CT
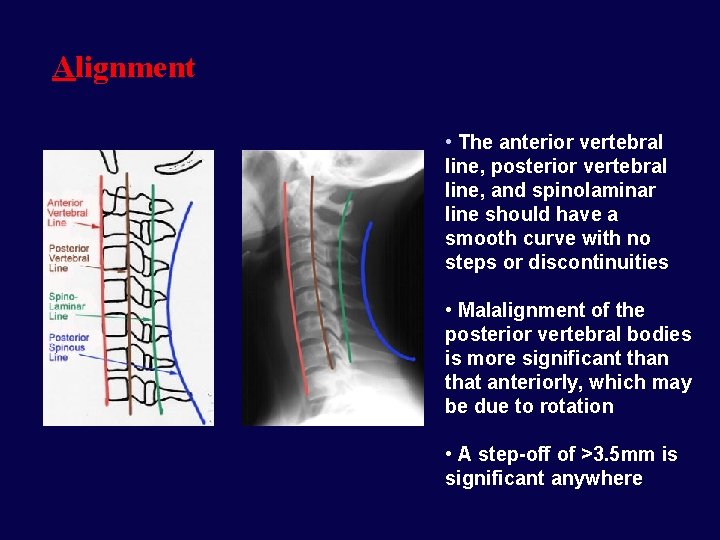
Alignment • The anterior vertebral line, posterior vertebral line, and spinolaminar line should have a smooth curve with no steps or discontinuities • Malalignment of the posterior vertebral bodies is more significant than that anteriorly, which may be due to rotation • A step-off of >3. 5 mm is significant anywhere
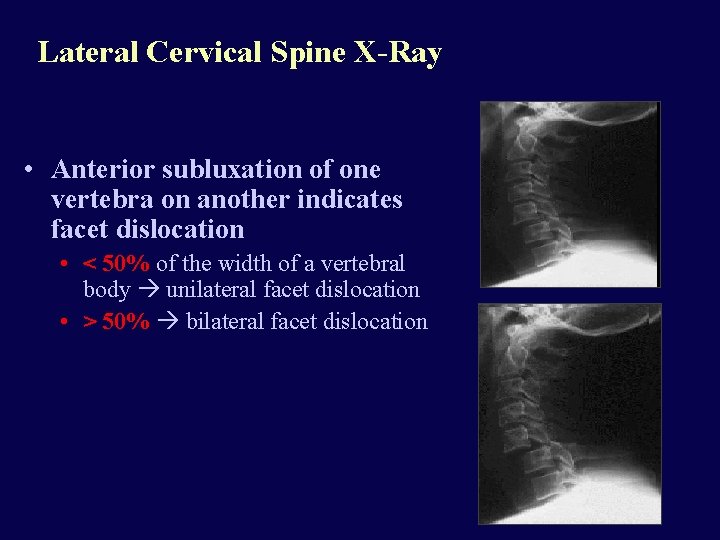
Lateral Cervical Spine X-Ray • Anterior subluxation of one vertebra on another indicates facet dislocation • < 50% of the width of a vertebral body unilateral facet dislocation • > 50% bilateral facet dislocation
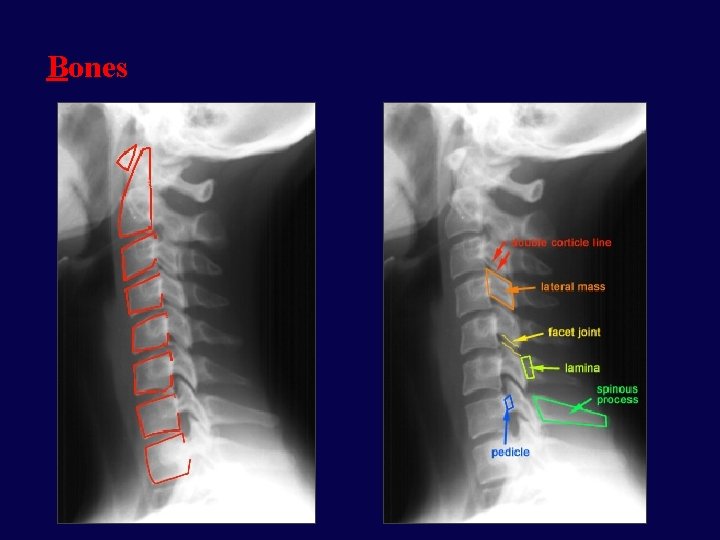
Bones
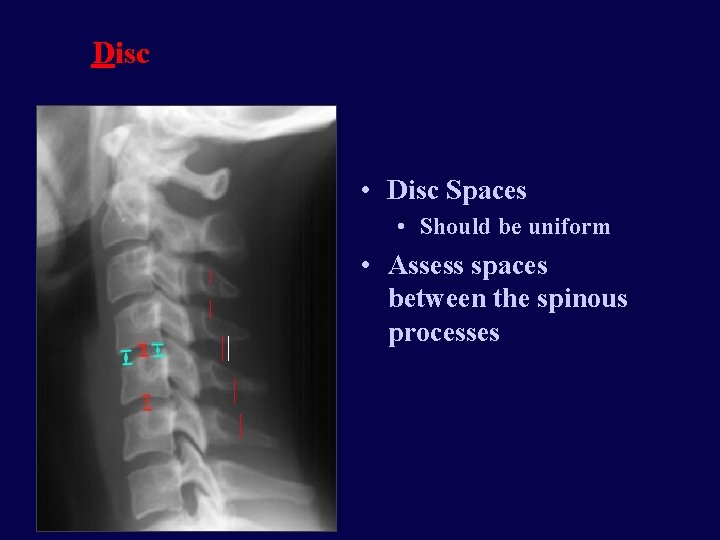
Disc • Disc Spaces • Should be uniform • Assess spaces between the spinous processes
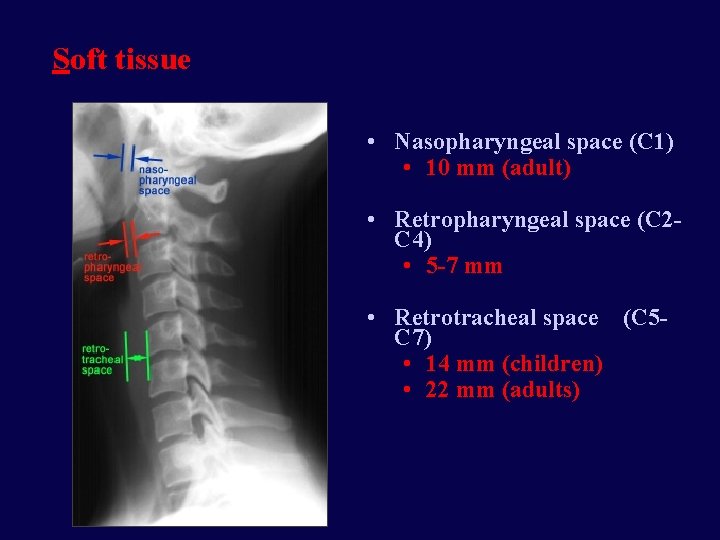
Soft tissue • Nasopharyngeal space (C 1) • 10 mm (adult) • Retropharyngeal space (C 2 C 4) • 5 -7 mm • Retrotracheal space (C 5 C 7) • 14 mm (children) • 22 mm (adults)
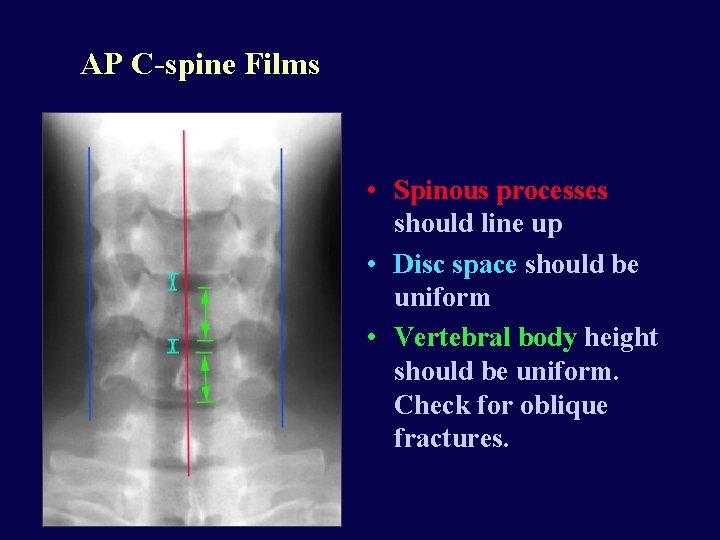
AP C-spine Films • Spinous processes should line up • Disc space should be uniform • Vertebral body height should be uniform. Check for oblique fractures.
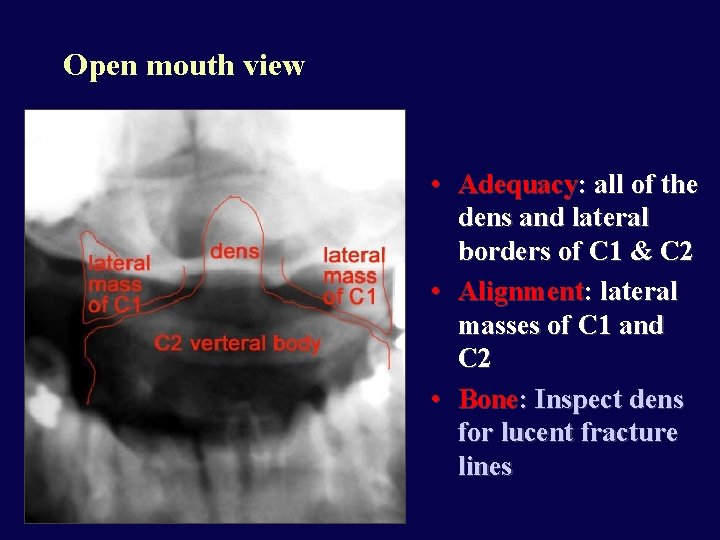
Open mouth view • Adequacy: all of the dens and lateral borders of C 1 & C 2 • Alignment: lateral masses of C 1 and C 2 • Bone: Inspect dens for lucent fracture lines
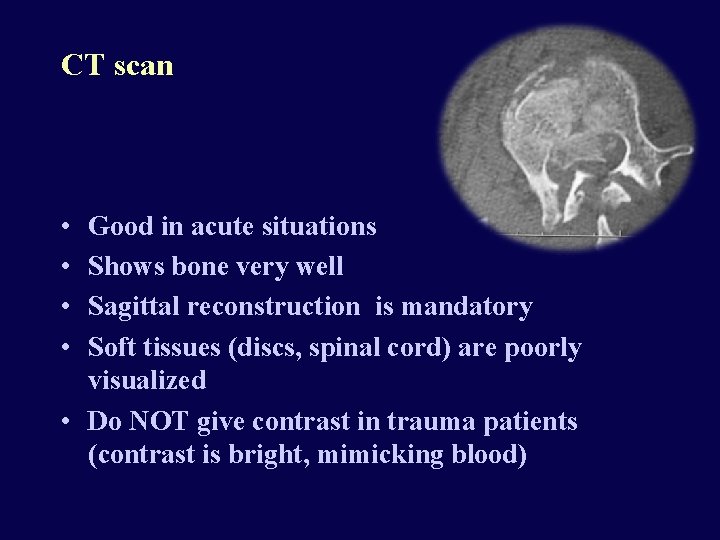
CT scan • • Good in acute situations Shows bone very well Sagittal reconstruction is mandatory Soft tissues (discs, spinal cord) are poorly visualized • Do NOT give contrast in trauma patients (contrast is bright, mimicking blood)
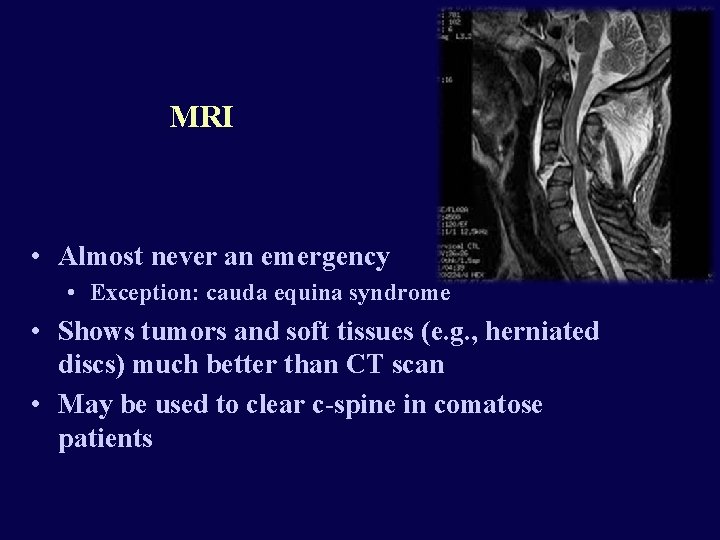
MRI • Almost never an emergency • Exception: cauda equina syndrome • Shows tumors and soft tissues (e. g. , herniated discs) much better than CT scan • May be used to clear c-spine in comatose patients
Lumbar Puncture • Sedate the patient and make your life easier • Measure opening pressure with legs straight • Always get head CT prior to LP to r/o increased ICP or brain tumor
Cervical Spine Clearance • Occiput to T 1 need to be cleared • ER, Neurosurgery or Orthopedics physician • If the patient • Is awake and oriented • Has no distracting injuries • Has no drugs on board • Has no neck pain • Is neurologically intact then the c-spine can be cleared clinically, without any need for XRays • CT and/or MRI is necessary if the patient is comatose or has neck pain • Subluxation >3. 5 mm is usually unstable
Cervical Traction • Gardner-Wells tongs • Provides temporary stability of the cervical spine • Contraindicated in unstable hyperextension injuries • Weight depends on the level (usually 5 lb/level, start with 3 lb/level, do not exceed 10 lb/level) • Cervical collar can be removed while patient is in traction • Pin care: clean q shift with appropriate solution, then apply povidone-iodine ointment • Take XRays at regular intervals and after every move from bed
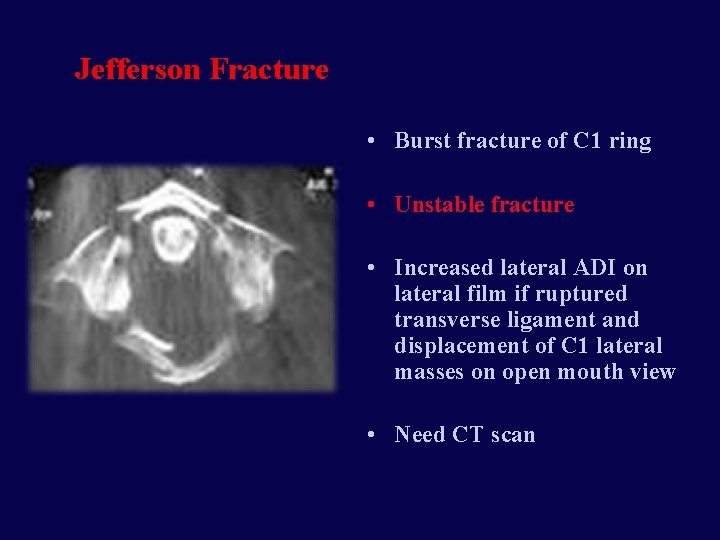
Jefferson Fracture • Burst fracture of C 1 ring • Unstable fracture • Increased lateral ADI on lateral film if ruptured transverse ligament and displacement of C 1 lateral masses on open mouth view • Need CT scan
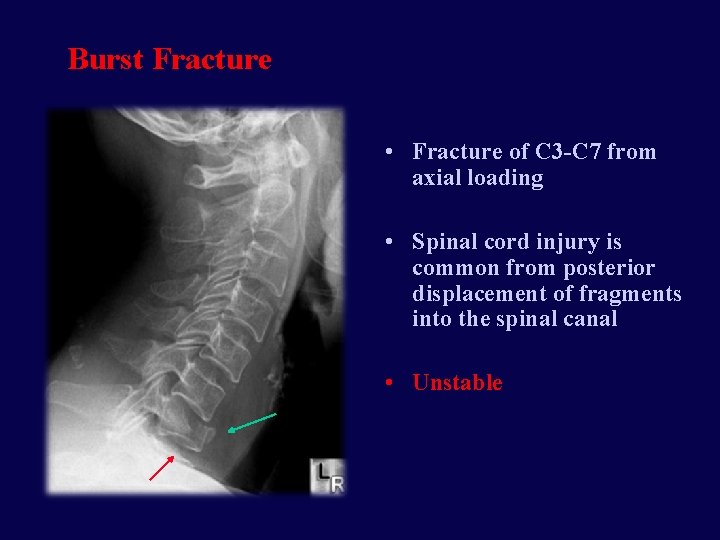
Burst Fracture • Fracture of C 3 -C 7 from axial loading • Spinal cord injury is common from posterior displacement of fragments into the spinal canal • Unstable
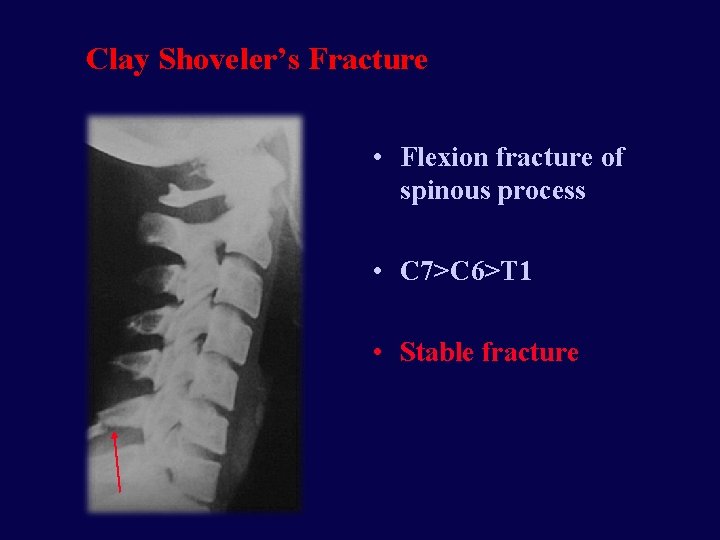
Clay Shoveler’s Fracture • Flexion fracture of spinous process • C 7>C 6>T 1 • Stable fracture
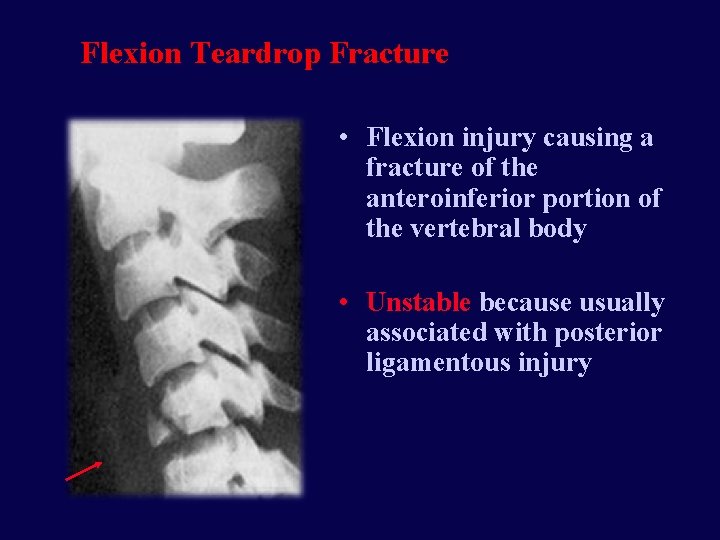
Flexion Teardrop Fracture • Flexion injury causing a fracture of the anteroinferior portion of the vertebral body • Unstable because usually associated with posterior ligamentous injury
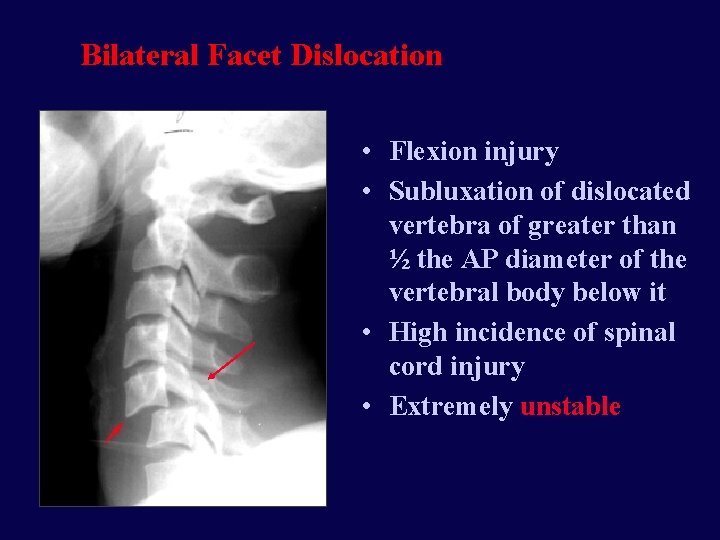
Bilateral Facet Dislocation • Flexion injury • Subluxation of dislocated vertebra of greater than ½ the AP diameter of the vertebral body below it • High incidence of spinal cord injury • Extremely unstable
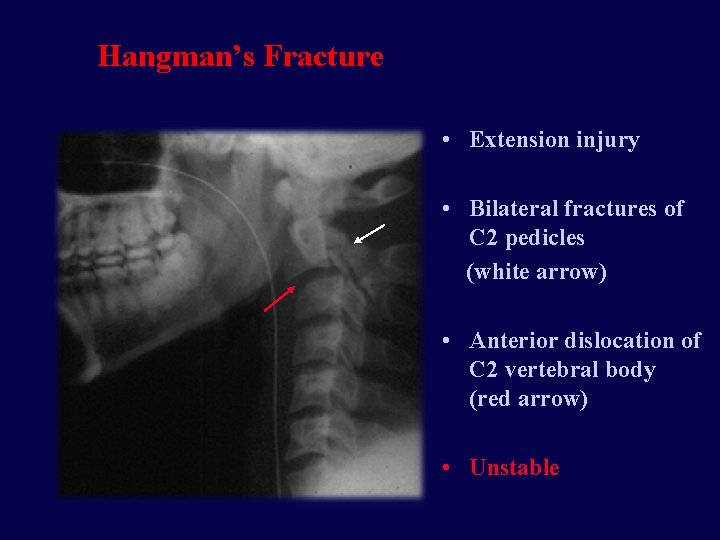
Hangman’s Fracture • Extension injury • Bilateral fractures of C 2 pedicles (white arrow) • Anterior dislocation of C 2 vertebral body (red arrow) • Unstable
Odontoid Fractures • Complex mechanism of injury • Generally unstable • Type 1 fracture through the tip • Rare • Type 2 fracture through the base • Most common • Type 3 fracture through the base and body of axis • Best prognosis
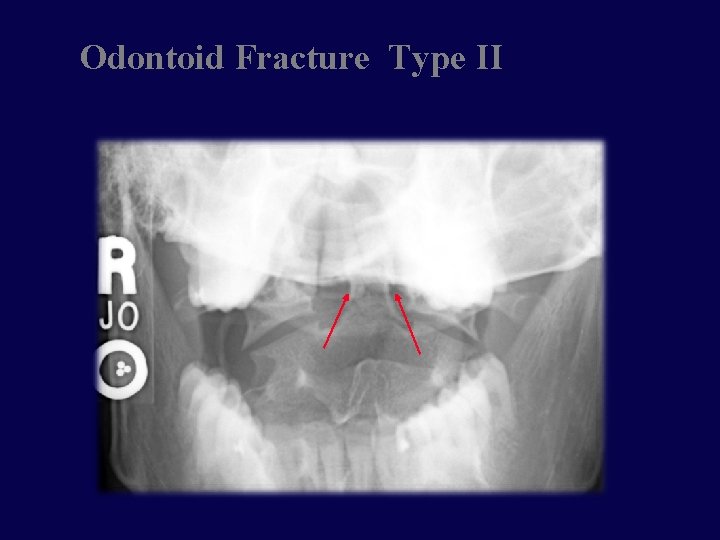
Odontoid Fracture Type II
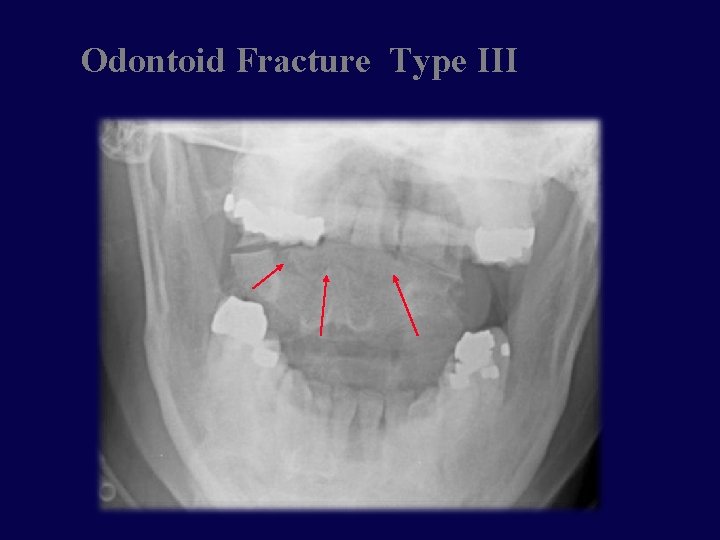
Odontoid Fracture Type III
Gardner-Wells tongs
Surgical Decompression and/or Fusion • Indications • Decompression of the neural elements (spinal cord/nerves) • Stabilization of the bony elements (spine) • Timing • Emergent • Incomplete lesions with progressive neurologic deficit • Elective • Complete lesions (3 -7 days post injury) • Central cord syndrome (2 -3 weeks post injury)
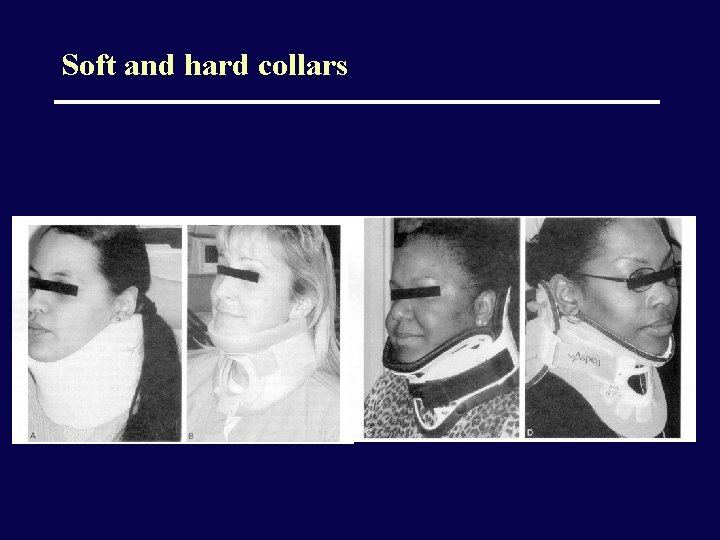
Soft and hard collars
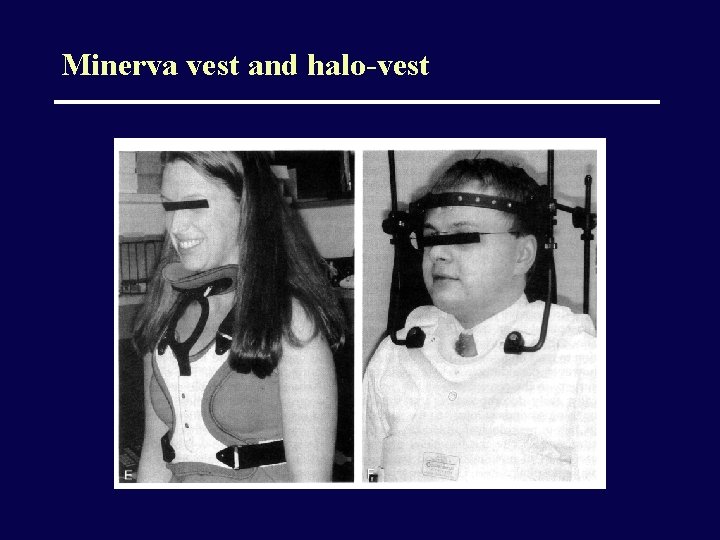
Minerva vest and halo-vest
Thoraco lumbar spine major fractures
Flexion • Wedge compression fractures: stable and unstable • Chance fractures • Dislocations and fracture-dislocations
Compression Fractures • Stable: Isolated to body, less than 50% loss of height, 1 or 2 levels only • Unstable: Posterior arch involved, or more than 50% loss of height, or more than 2 levels • Look for loss of height, loss of straight or anterior concave surface of body • Mechanism: FLEXION. Very common • Neurologic injury: Uncommon
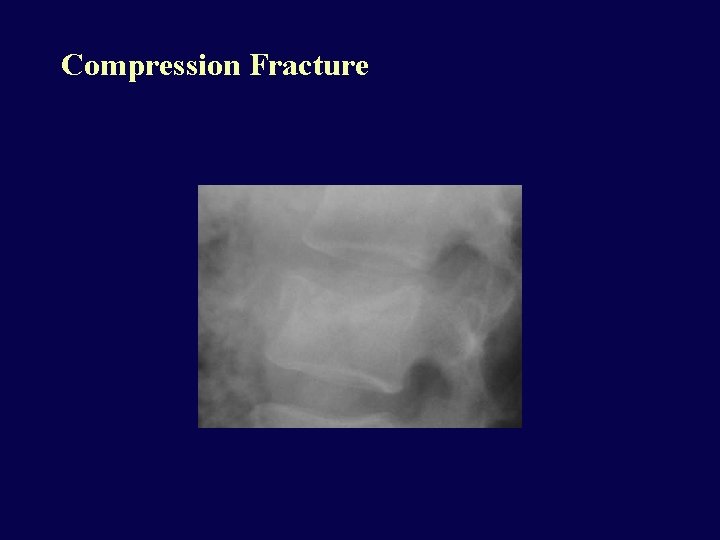
Compression Fracture
Chance Fracture • Compression fracture of body and transverse posterior arch fracture • Most common at T 10 -L 2 • Unstable • Neurologic injury in 15%, abdominal injury in 50% (tear of mesentery, bowel injury): always CT spine AND abdomen • Mechanism: FLEXION over a lap seat belt
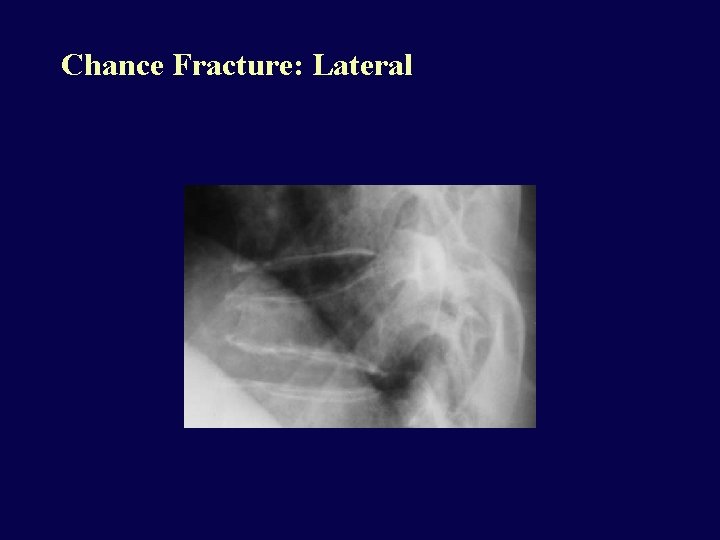
Chance Fracture: Lateral
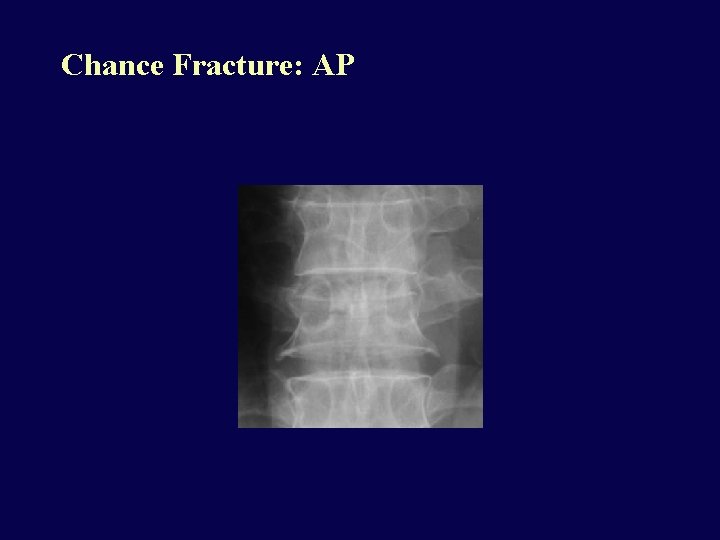
Chance Fracture: AP
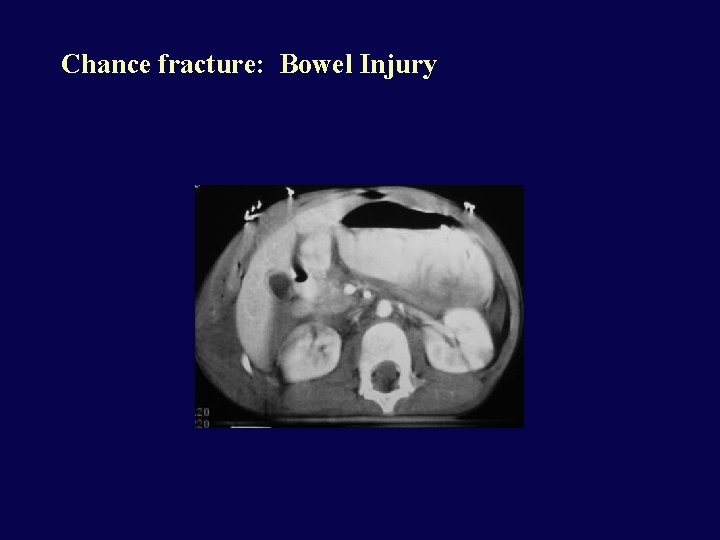
Chance fracture: Bowel Injury
Fracture-dislocation • • Marked flexion force Frequently at T 10 -L 2 Very unstable Severe cord/cauda equina injury is common
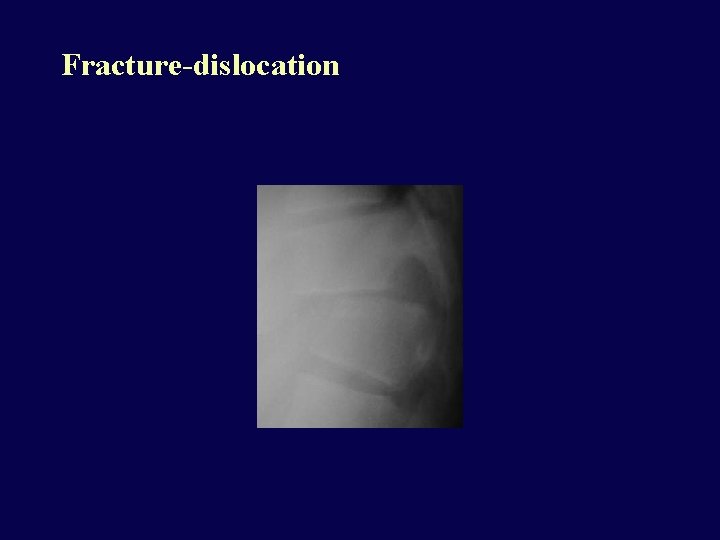
Fracture-dislocation
Burst Fracture • Compression fracture of body with superior and inferior end plate fractures, posterior arch fracture with laterally displaced pedicles • Very unstable • Over 2/3 have cord injury from retropulsed fragments. • Axial load/flexion combined mechanism
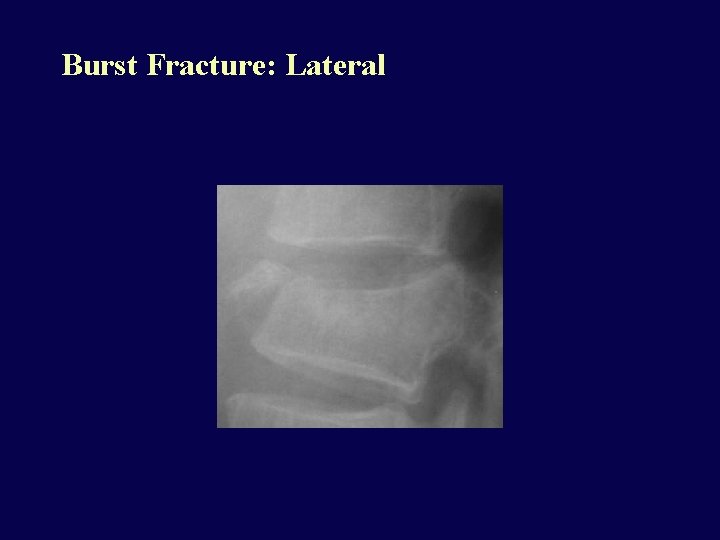
Burst Fracture: Lateral
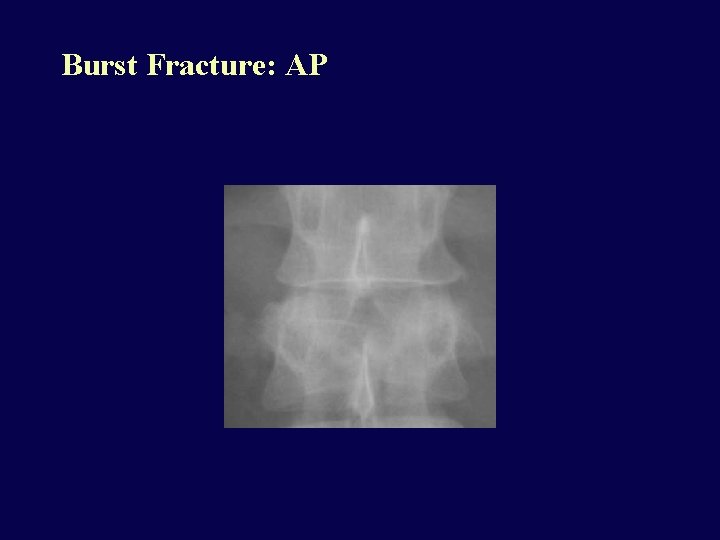
Burst Fracture: AP
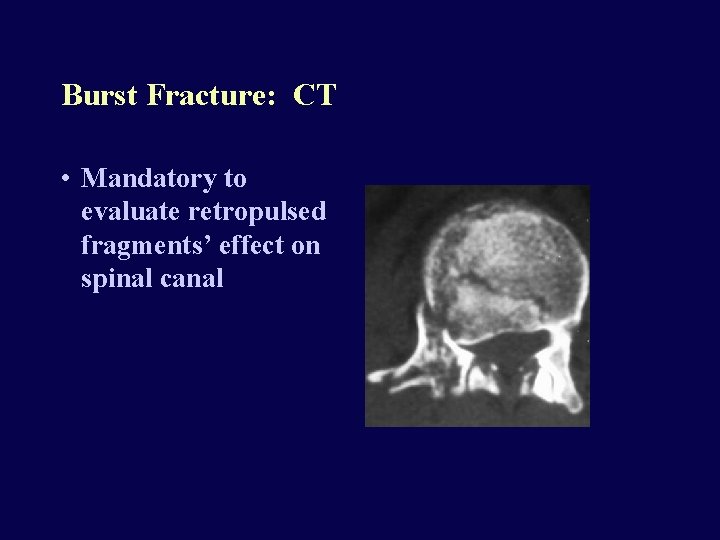
Burst Fracture: CT • Mandatory to evaluate retropulsed fragments’ effect on spinal canal
Shear Injuries • Marked shearing force causing severe fractures and dislocations, very unstable, severe cord injury.
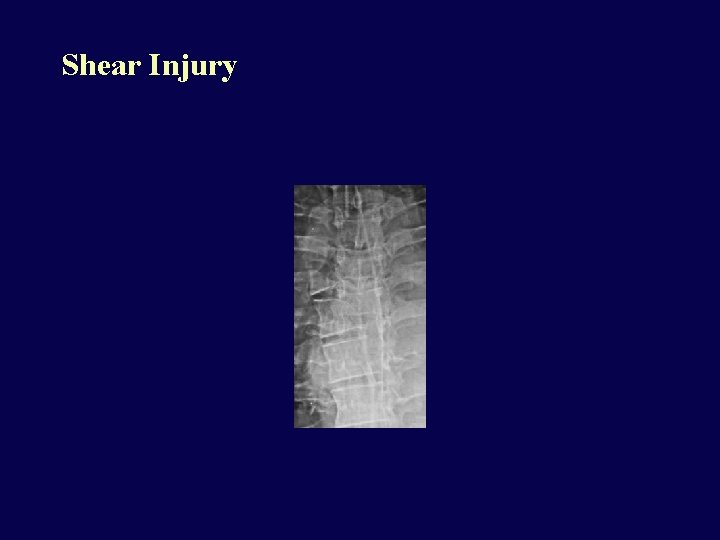
Shear Injury
Extension Injuries • Predisposing conditions: Degenerative spondylosis, DISH, seronegative spondyloarthropathies (e. g. ankylosing spondylitis). These are conditions that reduce spine elasticity. • Often unstable • Central or complete cord syndromes common, even with relatively minor trauma.
Extension Injury: DISH
Long term care • Rehab for maximizing motor function • Bladder/bowel training • Psychological and social support
- Slides: 87