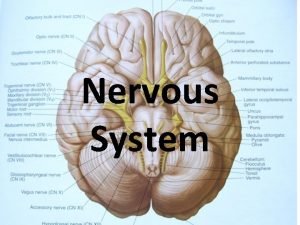
Nervous System MR OGUNDELE Nervous system The nervous




















- Slides: 110

Nervous System MR OGUNDELE

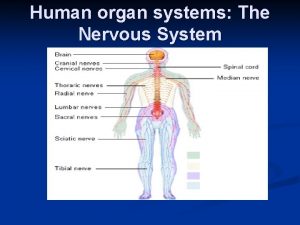
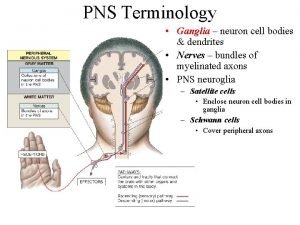
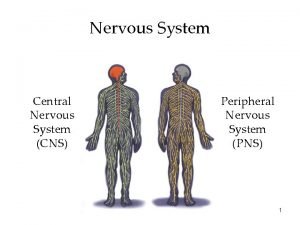
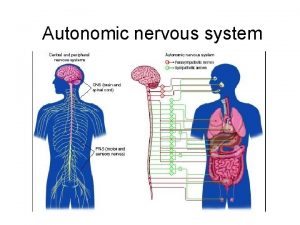
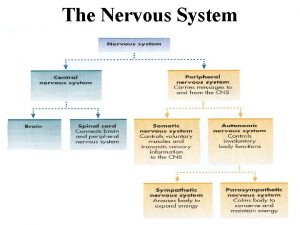
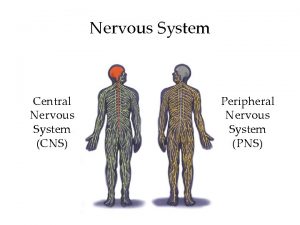
Nervous system • The nervous system has two divisions. The central nervous system (CNS) consists of the brain and spinal cord. The peripheral nervous system (PNS) consists of cranial nerves and spinal nerves. • The peripheral nervous system relays information to and from the central nervous system, and the brain is the center of activity that integrates this information, initiates responses.
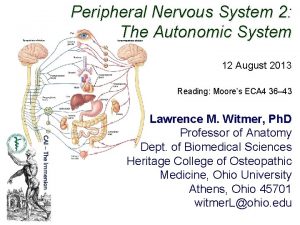
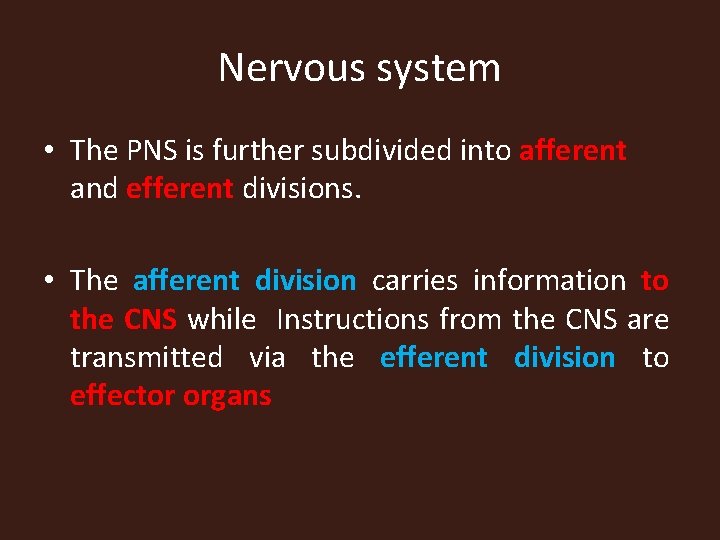
Nervous system • The PNS is further subdivided into afferent and efferent divisions. • The afferent division carries information to the CNS while Instructions from the CNS are transmitted via the efferent division to effector organs

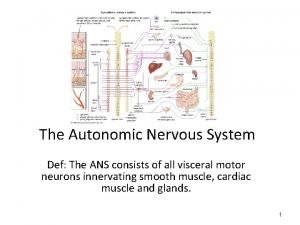
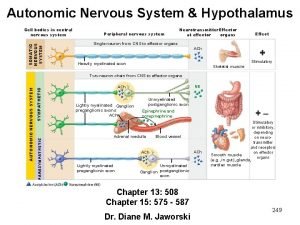
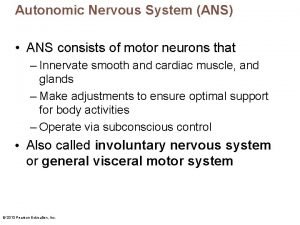
Nervous system • The efferent nervous system is divided into: • The somatic nervous system, which consists of the fibers of the motor neurons that supply the skeletal muscles; and • The autonomic nervous system, which consists of fibers that innervate smooth muscle, cardiac muscle, and glands. ANS is further subdivided into the sympathetic nervous system and the parasympathetic nervous system.
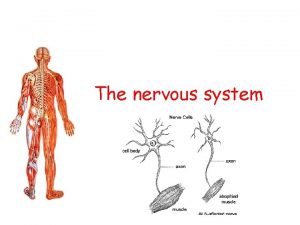
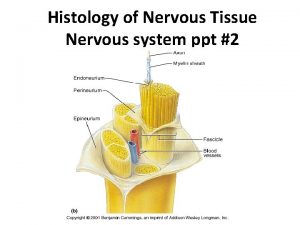
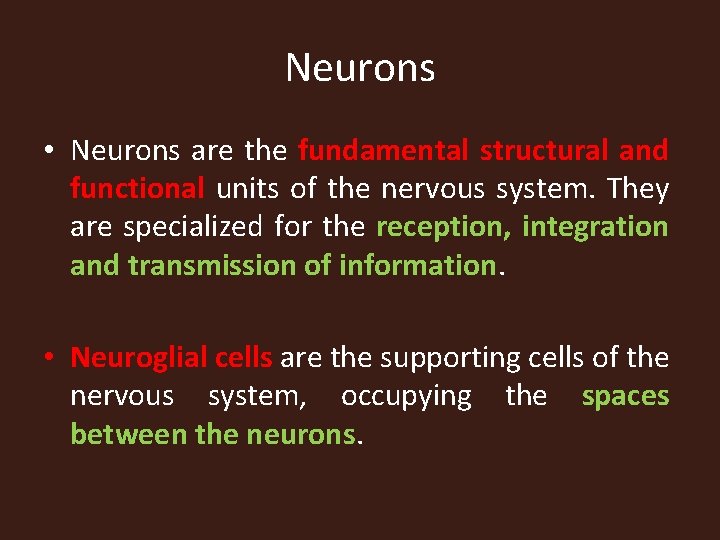
Neurons • Neurons are the fundamental structural and functional units of the nervous system. They are specialized for the reception, integration and transmission of information. • Neuroglial cells are the supporting cells of the nervous system, occupying the spaces between the neurons.
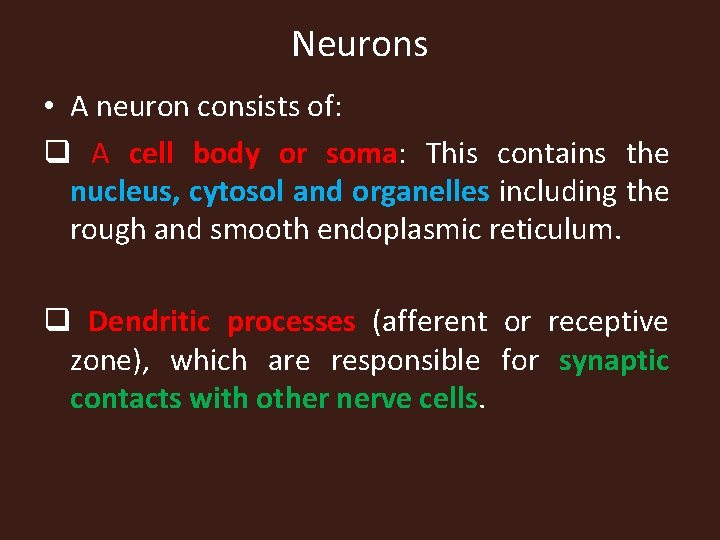
Neurons • A neuron consists of: q A cell body or soma: This contains the nucleus, cytosol and organelles including the rough and smooth endoplasmic reticulum. q Dendritic processes (afferent or receptive zone), which are responsible for synaptic contacts with other nerve cells.
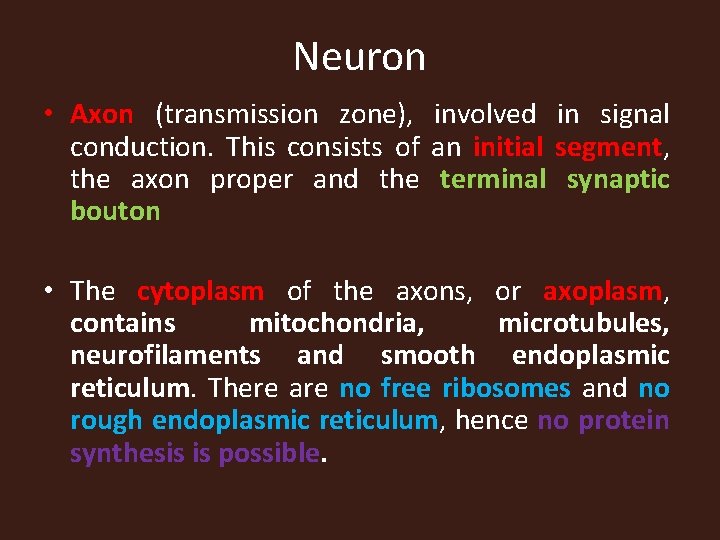
Neuron • Axon (transmission zone), involved in signal conduction. This consists of an initial segment, the axon proper and the terminal synaptic bouton • The cytoplasm of the axons, or axoplasm, contains mitochondria, microtubules, neurofilaments and smooth endoplasmic reticulum. There are no free ribosomes and no rough endoplasmic reticulum, hence no protein synthesis is possible.
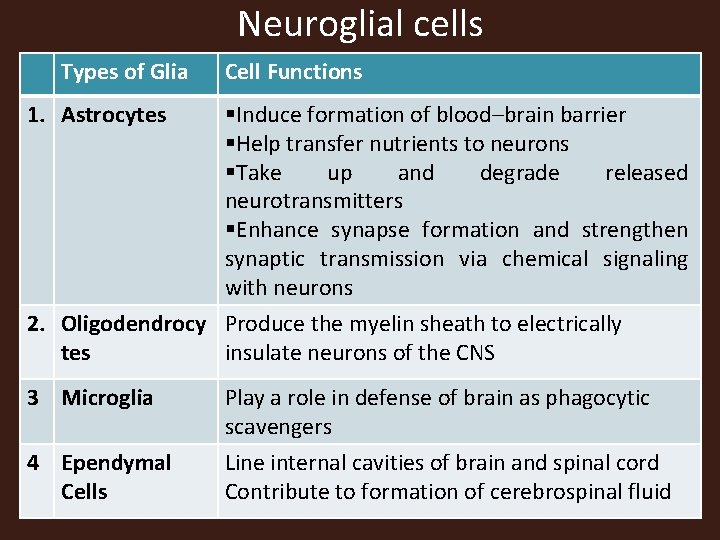
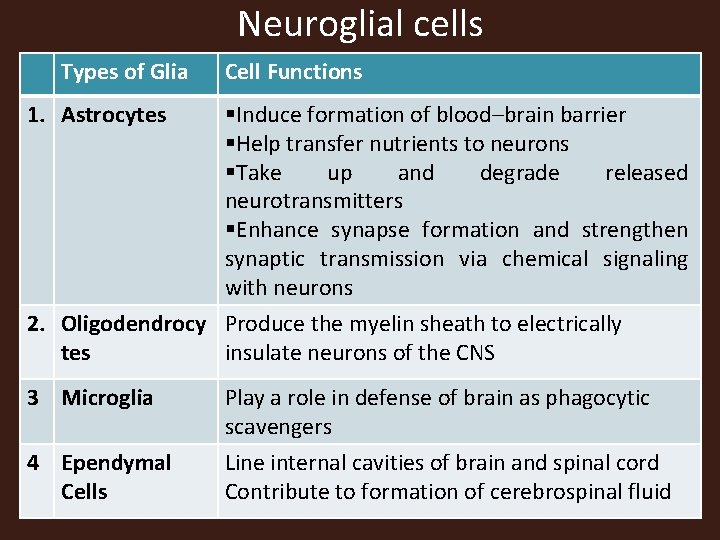
Neuroglial cells Types of Glia Cell Functions 1. Astrocytes §Induce formation of blood–brain barrier §Help transfer nutrients to neurons §Take up and degrade released neurotransmitters §Enhance synapse formation and strengthen synaptic transmission via chemical signaling with neurons 2. Oligodendrocy Produce the myelin sheath to electrically tes insulate neurons of the CNS 3 Microglia 4 Ependymal Cells Play a role in defense of brain as phagocytic scavengers Line internal cavities of brain and spinal cord Contribute to formation of cerebrospinal fluid
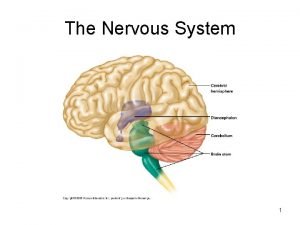
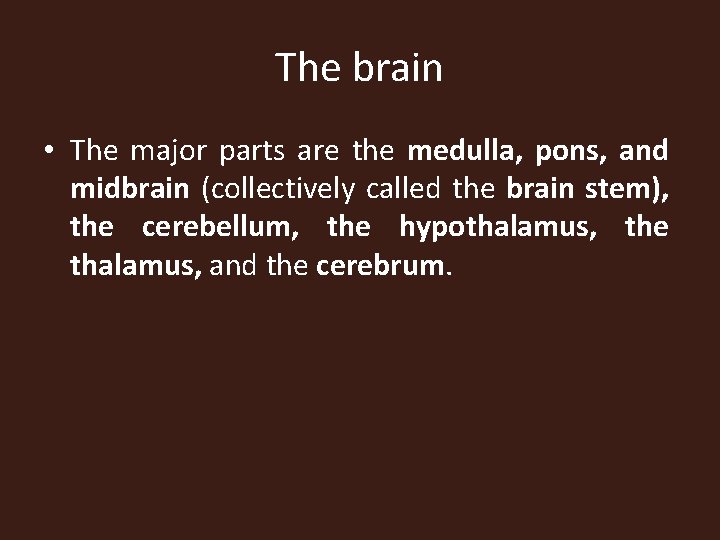
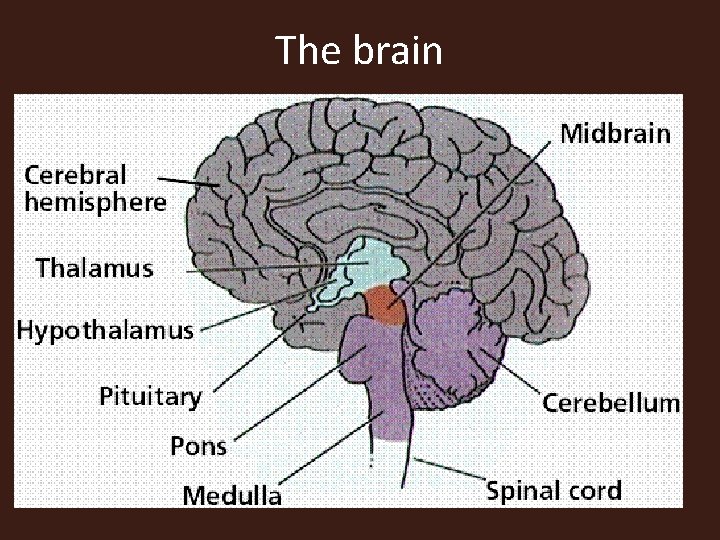
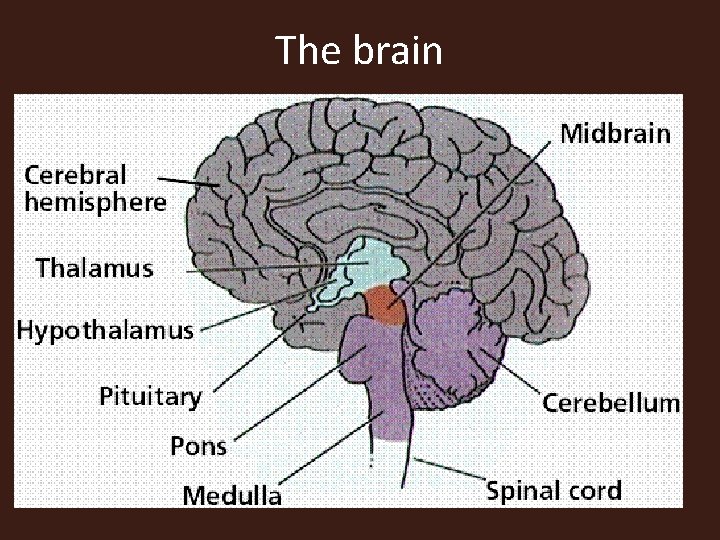
The brain • The major parts are the medulla, pons, and midbrain (collectively called the brain stem), the cerebellum, the hypothalamus, the thalamus, and the cerebrum.
The brain

Brain stem • The brain stem controls many of the lifesustaining processes, such as respiration, circulation, and digestion that are common to all vertebrates. These processes are often referred to as vegetative functions, meaning functions performed unconsciously or involuntarily.


MEDULLA The medulla extends from the spinal cord to the pons and is anterior to the cerebellum. The medulla contains cardiac centers that regulate heart rate, vasomotor centers that regulate the diameter of blood vessels, and respiratory centers that regulate breathing. Medulla has reflex centers for coughing, sneezing, swallowing, and vomiting.

PONS • The pons bulges anteriorly from the upper part of the medulla. Within the pons are two respiratory centers that work with those in the medulla to produce a normal breathing rhythm. The many other neurons in the pons connect the medulla with other parts of the brain.
MIDBRAIN • The midbrain extends from the pons to the hypothalamus and encloses the cerebral aqueduct, a tunnel that connects the third and fourth ventricles. Several different kinds of reflexes are integrated in the midbrain, including visual and auditory reflexes.
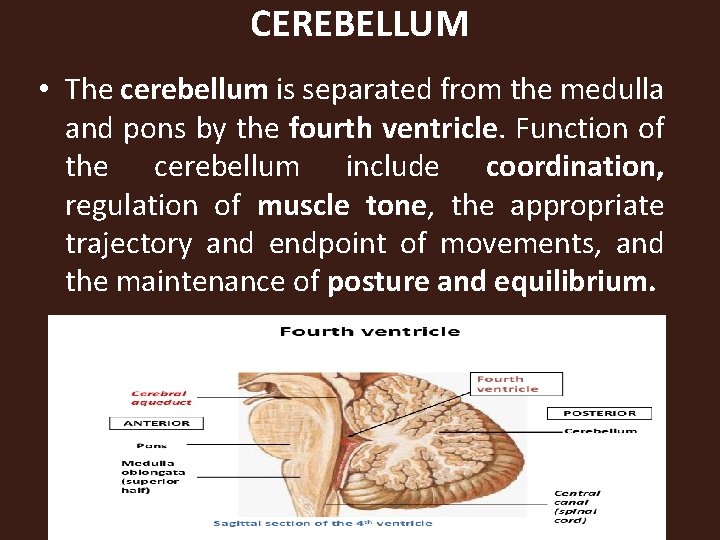
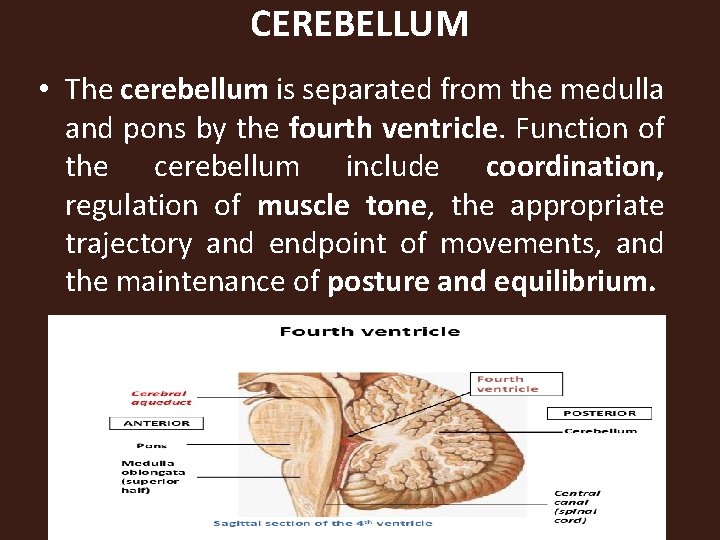
CEREBELLUM • The cerebellum is separated from the medulla and pons by the fourth ventricle. Function of the cerebellum include coordination, regulation of muscle tone, the appropriate trajectory and endpoint of movements, and the maintenance of posture and equilibrium.

HYPOTHALAMUS Located superior to the pituitary gland inferior to the thalamus, the hypothalamus is a small area of the brain with many diverse functions: 1. Production of antidiuretic hormone (ADH) and oxytocin; these hormones are then stored in the posterior pituitary gland
Functions of hypothalamus 2. Regulation of body temperature by promoting responses such as sweating in a warm environment or shivering in a cold environment. secretion of hormones, sleep cycles, changes in mood, or mental Alertness
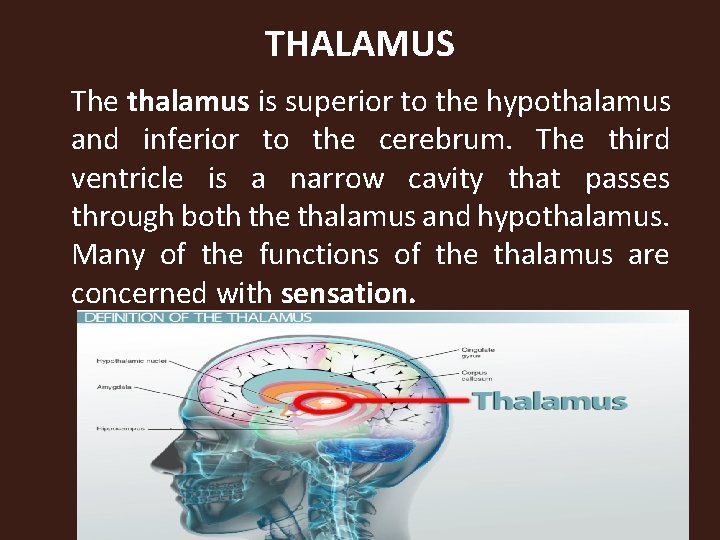
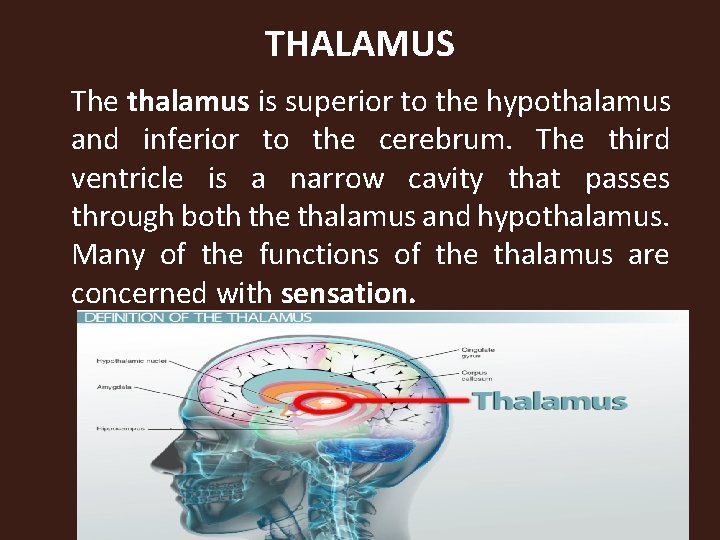
THALAMUS The thalamus is superior to the hypothalamus and inferior to the cerebrum. The third ventricle is a narrow cavity that passes through both the thalamus and hypothalamus. Many of the functions of the thalamus are concerned with sensation.
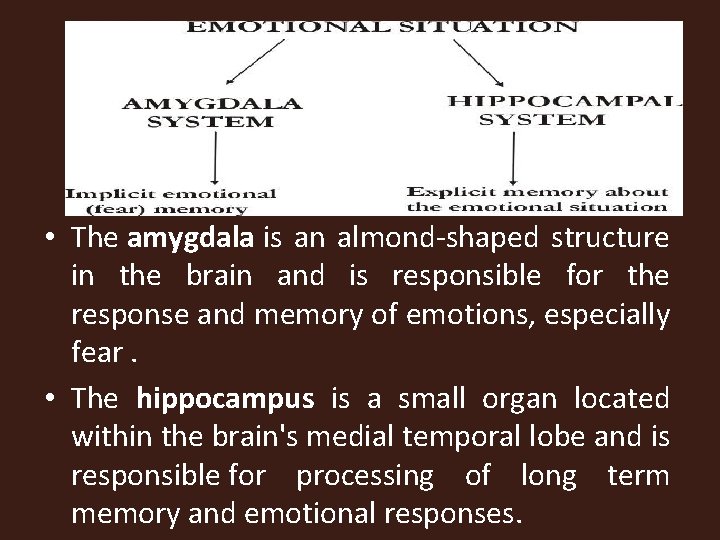
• The amygdala is an almond-shaped structure in the brain and is responsible for the response and memory of emotions, especially fear. • The hippocampus is a small organ located within the brain's medial temporal lobe and is responsible for processing of long term memory and emotional responses.
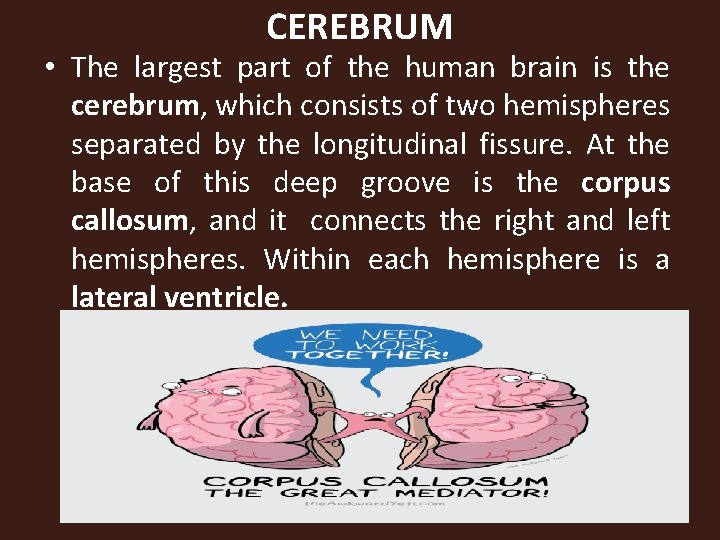
CEREBRUM • The largest part of the human brain is the cerebrum, which consists of two hemispheres separated by the longitudinal fissure. At the base of this deep groove is the corpus callosum, and it connects the right and left hemispheres. Within each hemisphere is a lateral ventricle.
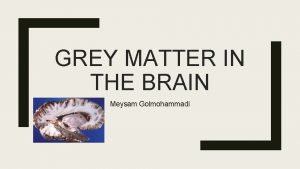
Cerebrum • The surface of the cerebrum is gray matter called the cerebral cortex. Gray matter consists of cell bodies of neurons. Internal to the gray matter is white matter, made of myelinated axons and dendrites that connect the lobes of the cerebrum to one another and to all other parts of the brain.

Cerebrum • In the human brain the cerebral cortex is folded extensively. The folds are called convolutions or gyri and the grooves between them are fissures or sulci • The cerebral cortex is divided into lobes that have the same names as the cranial bones
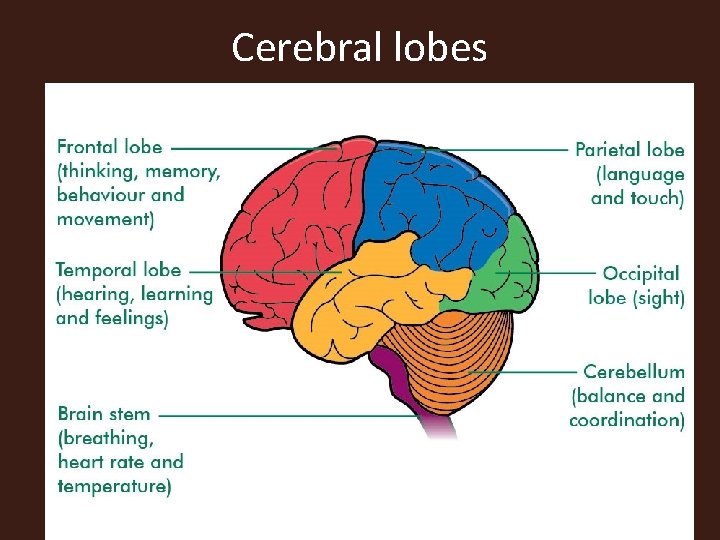
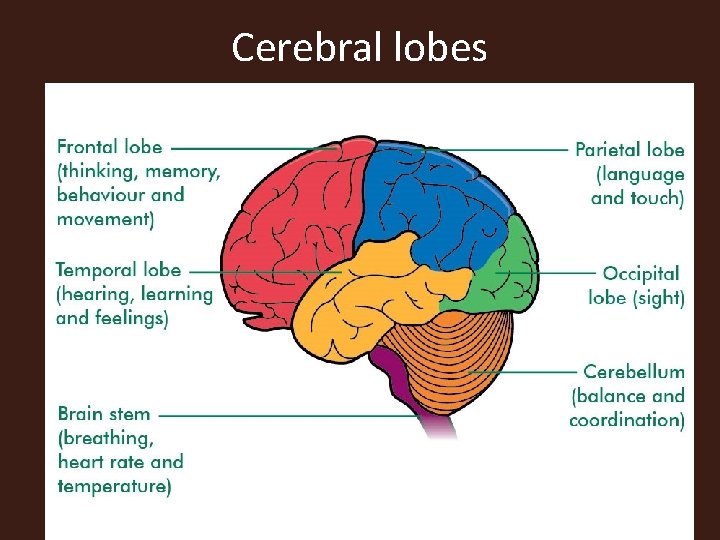
Cerebral lobes
Frontal Lobes • Within the frontal lobes are the motor areas that generate the impulses for voluntary movement Anterior to the motor areas are the premotor areas, which are concerned with learned motor skills that require a sequence of movements • Also in the frontal lobe, usually only the left lobe for most right-handed people, is Broca’s motor speech area, which controls the movements of the mouth involved in speaking.
Parietal Lobes • The general sensory areas in the parietal lobes receive impulses from receptors in the skin and feel and interpret the cutaneous sensations. • The taste areas, which overlap the parietal and temporal lobes, receive impulses from taste buds on the tongue and elsewhere in the oral cavity.
Temporal Lobes • The olfactory areas in the temporal lobes receive impulses from receptors in the nasal cavities for the sense of smell. • The auditory areas, as their name suggests, receive impulses from receptors in the inner ear for hearing.
Occipital Lobes • Impulses from the retinas of the eyes travel along the optic nerves to the visual areas in the occipital lobes
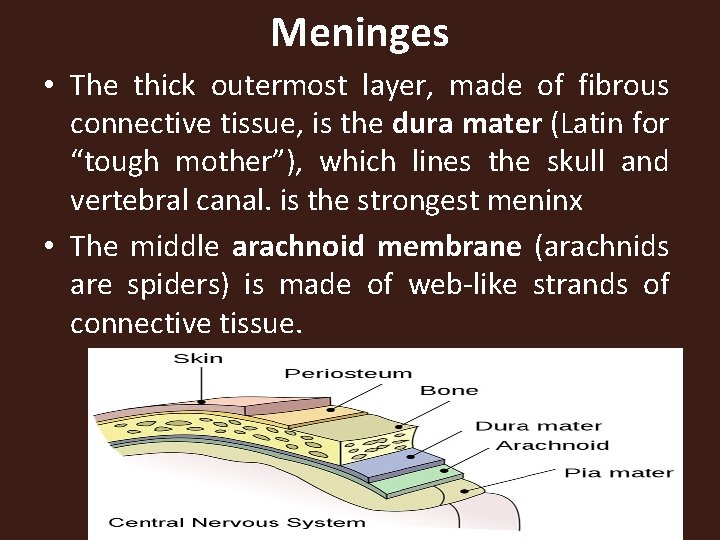
MENINGES AND CEREBROSPINAL FLUID • The connective tissue membranes that cover the brain and spinal cord are called meninges; The three layers are : Dura layer Arachnoid layer Pia Layer
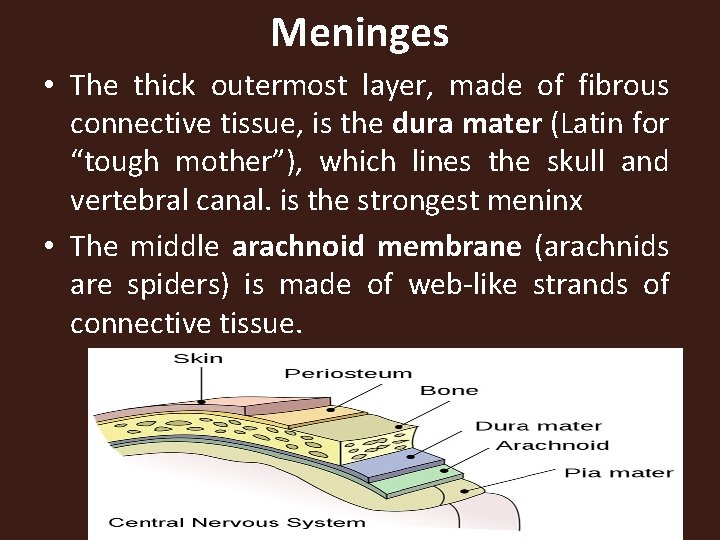
Meninges • The thick outermost layer, made of fibrous connective tissue, is the dura mater (Latin for “tough mother”), which lines the skull and vertebral canal. is the strongest meninx • The middle arachnoid membrane (arachnids are spiders) is made of web-like strands of connective tissue.
Meninges • The innermost pia mater (Latin for “gentle mother”) is a very thin membrane on the surface of the spinal cord and brain. Between the arachnoid and the pia mater is the subarachnoid space, which contains cerebrospinal fluid (CSF), the tissue fluid of the central nervous system.

CEREBROSPINAL FLUID • The ventricles (cavities) of the brain: two lateral ventricles, the third ventricle, and the fourth ventricle. Each contains a choroid plexus, a capillary network that forms cerebrospinal fluid from blood plasma.
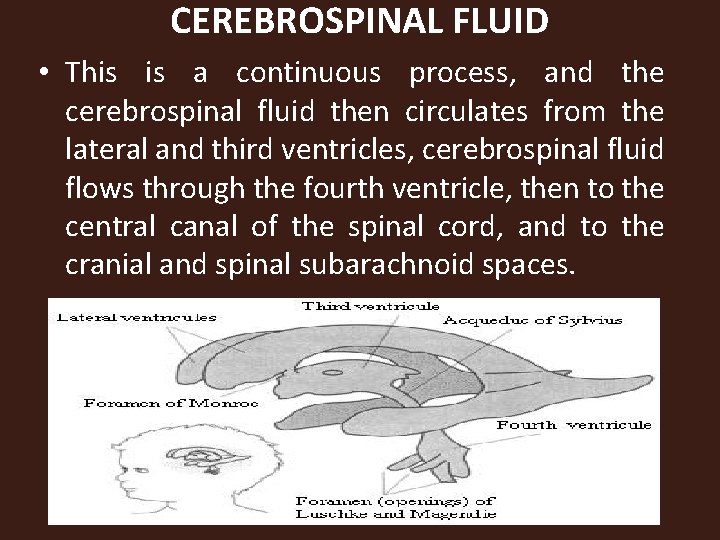
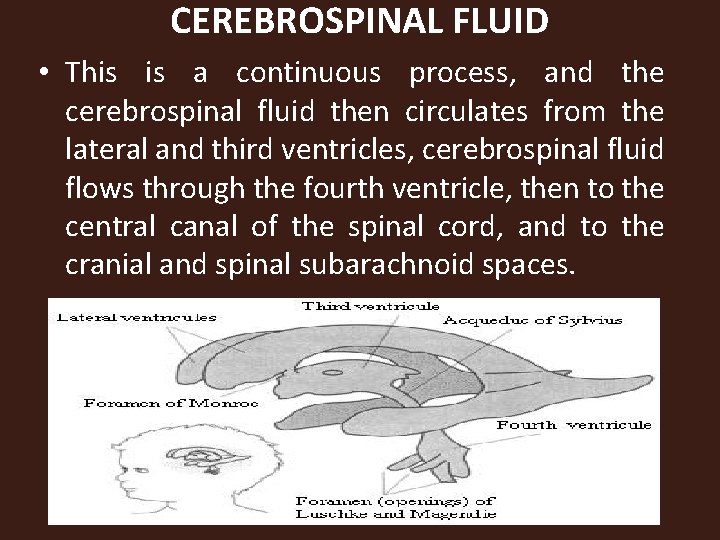
CEREBROSPINAL FLUID • This is a continuous process, and the cerebrospinal fluid then circulates from the lateral and third ventricles, cerebrospinal fluid flows through the fourth ventricle, then to the central canal of the spinal cord, and to the cranial and spinal subarachnoid spaces.
CSF • The total volume of cerebrospinal fluid is approximately 150 ml and it is produced at a rate of 450 ml per day (thus replacing itself three times a day). • 50% to 70% of the CSF is secreted by cells of the choroid plexus and ependyma cells in the ventricle while the rest is secreted by ultrafiltration of blood plasma through choroid capillaries.
CSF • CSF circulates from lateral ventricles through foramina of monro into the third ventricle and flows from the third ventricle to the fourth through aqueduct of Sylvius and flows into subarachnoid space by means of three foramina: A single medial aperture (foramen of Magendie) and a pair of lateral aperture (foramen of Luschka) • .

CSF • This then drains into the subarachnoid space which surrounds the entire brain and spinal cord. The resorption of CSF takes place in the arachnoid granulation (arachnoid villi: these are protrusion of the arachnoid through the dura mater projecting into the intracranial venous sinus) and is emptied into the several venous sinuses of the cerebrum. It is then returned into the venous circulation.
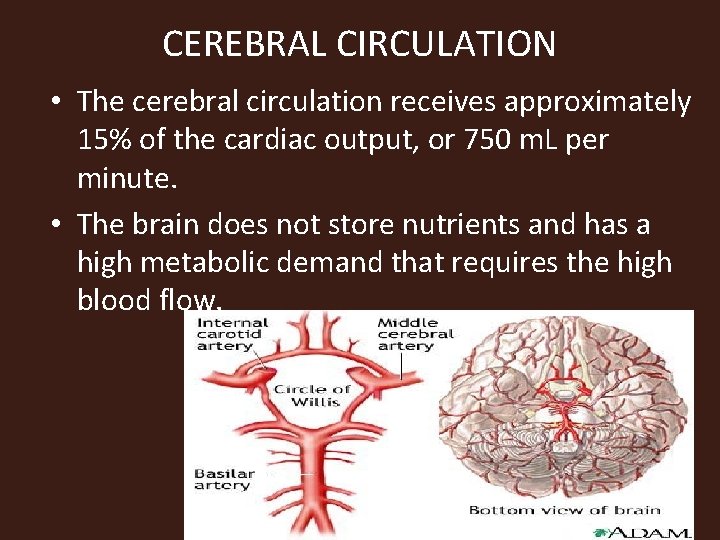
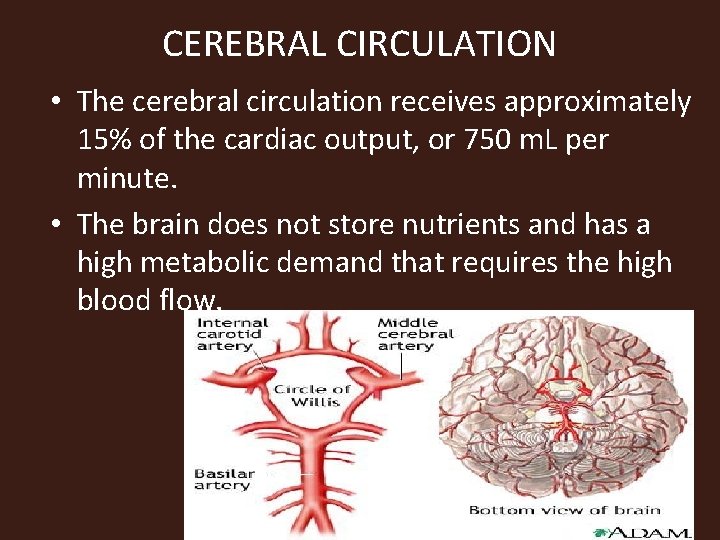
CEREBRAL CIRCULATION • The cerebral circulation receives approximately 15% of the cardiac output, or 750 m. L per minute. • The brain does not store nutrients and has a high metabolic demand that requires the high blood flow.
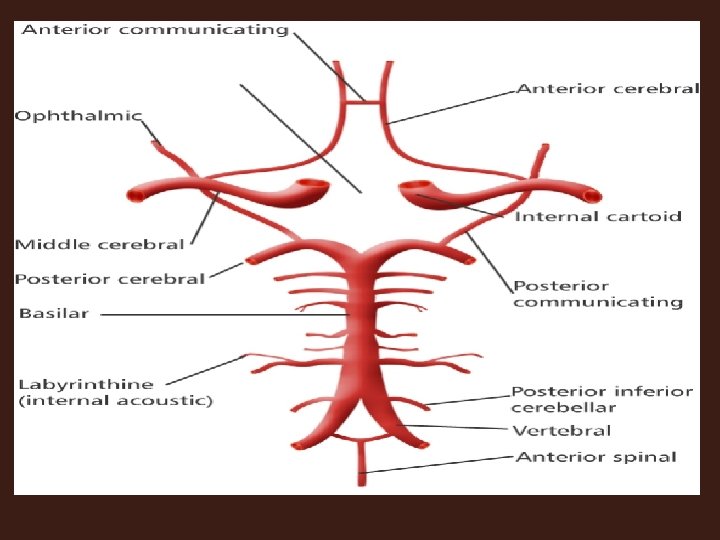
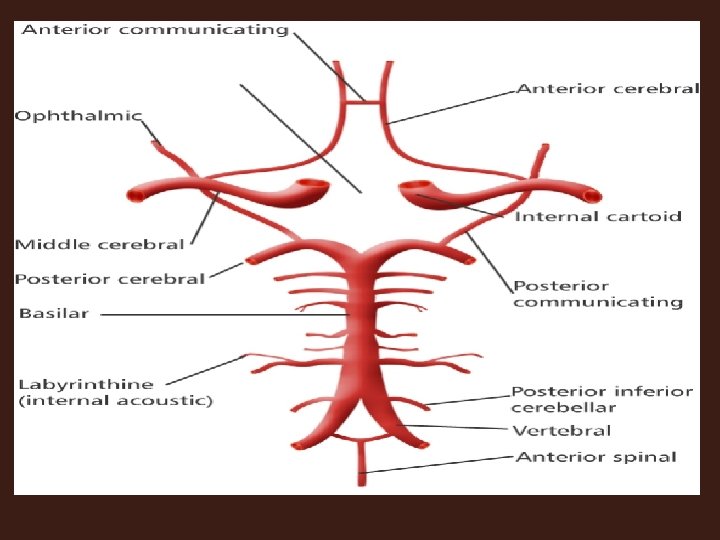
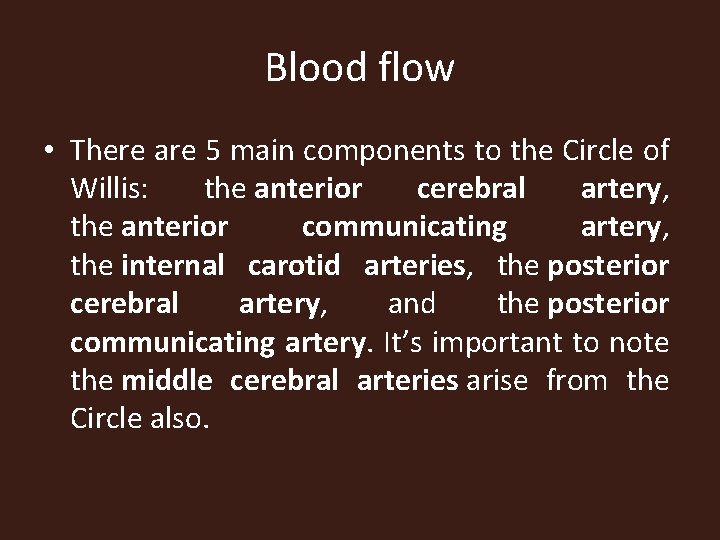
Blood flow • There are 5 main components to the Circle of Willis: the anterior cerebral artery, the anterior communicating artery, the internal carotid arteries, the posterior cerebral artery, and the posterior communicating artery. It’s important to note the middle cerebral arteries arise from the Circle also.
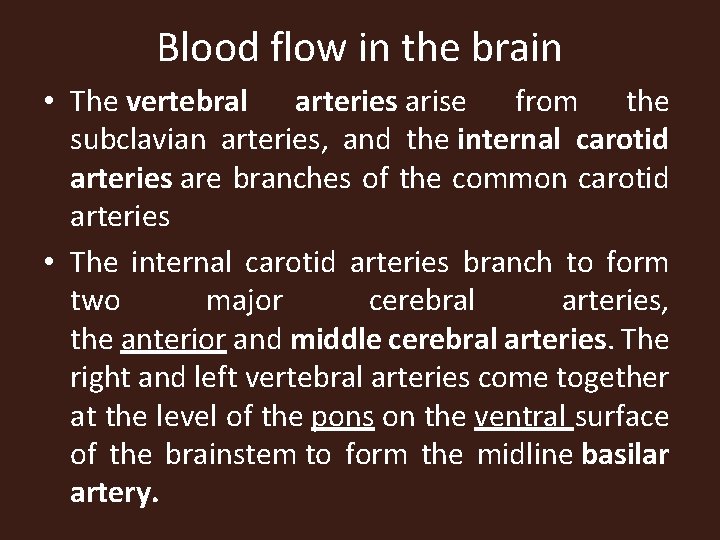
Blood flow in the brain • The vertebral arteries arise from the subclavian arteries, and the internal carotid arteries are branches of the common carotid arteries • The internal carotid arteries branch to form two major cerebral arteries, the anterior and middle cerebral arteries. The right and left vertebral arteries come together at the level of the pons on the ventral surface of the brainstem to form the midline basilar artery.
Blood flow in the brain • The basilar artery joins the blood supply from the internal carotids in an arterial ring at the base of the brain called the circle of Willis • The posterior cerebral arteries arise at this confluence, and supplies blood to the occipital lobe and part of the temporal lobe. The posterior communicating arteries provides communication between the carotid and vertebral arteries
Blood flow in the brain • The anterior and posterior communicating arteries conjoined the two major sources of cerebral vascular supply and improves the chances of any region of the brain to receive blood if one of the major arteries becomes occluded
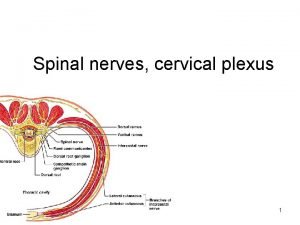
Spinal Cord • The spinal cord transmits impulses to and from the brain and is the integrating center for the spinal cord reflexes. • It extends from the foramen magnum of the occipital bone to the intervertebral disk between the first and • second lumbar vertebrae. The spinal nerves emerge from the intervertebral foramina.
spinal nerves • There are 31 pairs of spinal nerves, named according to their respective vertebrae: • 8 cervical pairs, • 12 thoracic pairs, • 5 lumbar pairs, • 5 sacral pairs, • 1 very small coccygeal pair
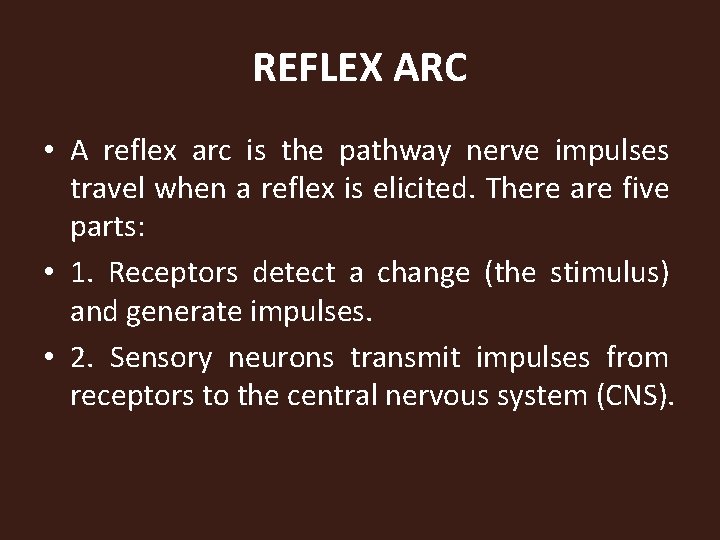
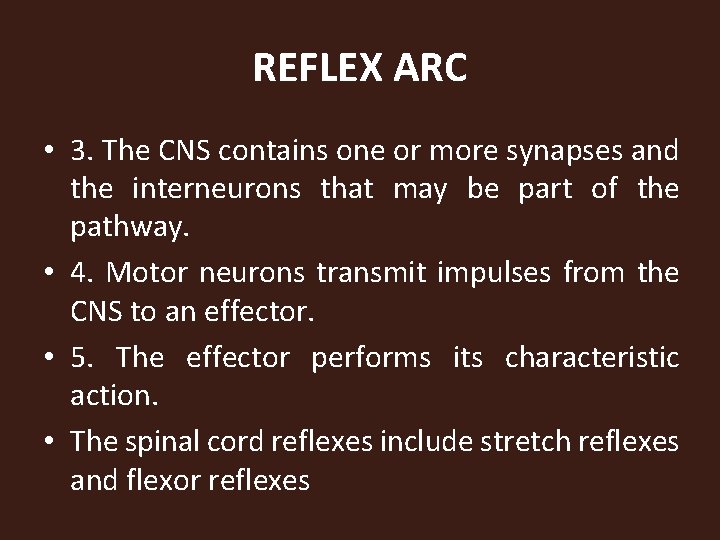
REFLEX ARC • A reflex arc is the pathway nerve impulses travel when a reflex is elicited. There are five parts: • 1. Receptors detect a change (the stimulus) and generate impulses. • 2. Sensory neurons transmit impulses from receptors to the central nervous system (CNS).
REFLEX ARC • 3. The CNS contains one or more synapses and the interneurons that may be part of the pathway. • 4. Motor neurons transmit impulses from the CNS to an effector. • 5. The effector performs its characteristic action. • The spinal cord reflexes include stretch reflexes and flexor reflexes
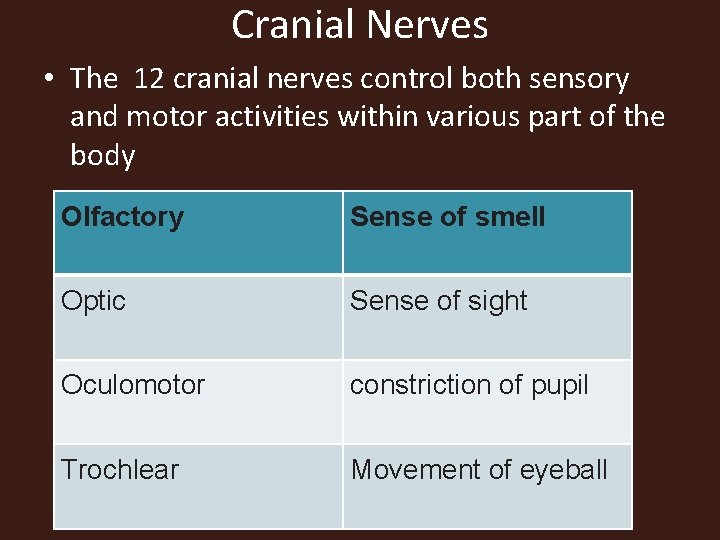
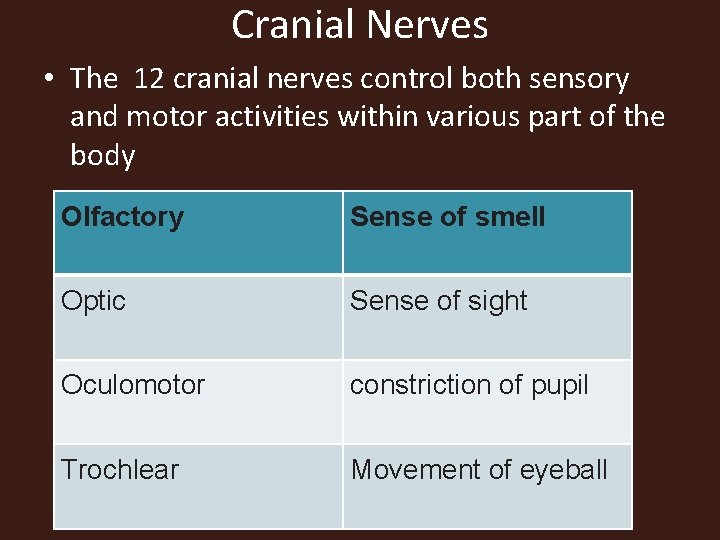
Cranial Nerves • The 12 cranial nerves control both sensory and motor activities within various part of the body Olfactory Sense of smell Optic Sense of sight Oculomotor constriction of pupil Trochlear Movement of eyeball
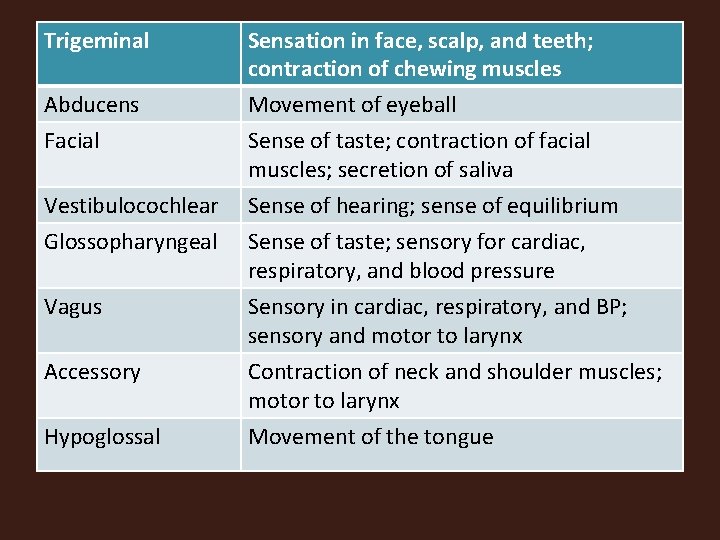
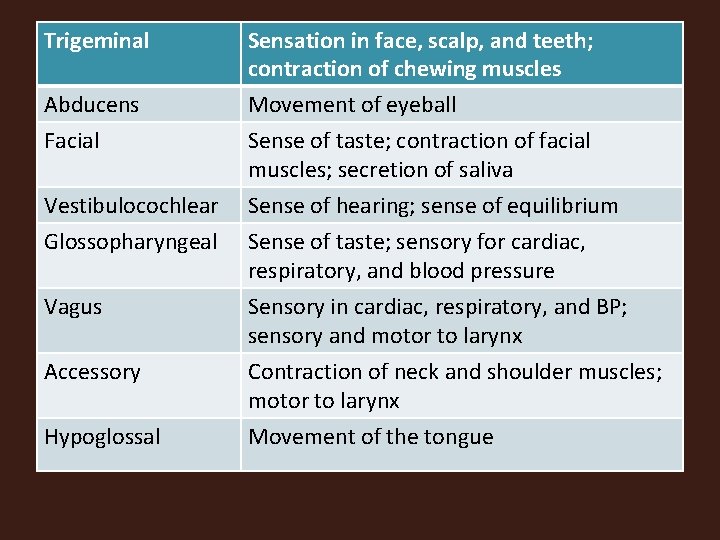
Trigeminal Abducens Facial Vestibulocochlear Glossopharyngeal Vagus Accessory Hypoglossal Sensation in face, scalp, and teeth; contraction of chewing muscles Movement of eyeball Sense of taste; contraction of facial muscles; secretion of saliva Sense of hearing; sense of equilibrium Sense of taste; sensory for cardiac, respiratory, and blood pressure Sensory in cardiac, respiratory, and BP; sensory and motor to larynx Contraction of neck and shoulder muscles; motor to larynx Movement of the tongue
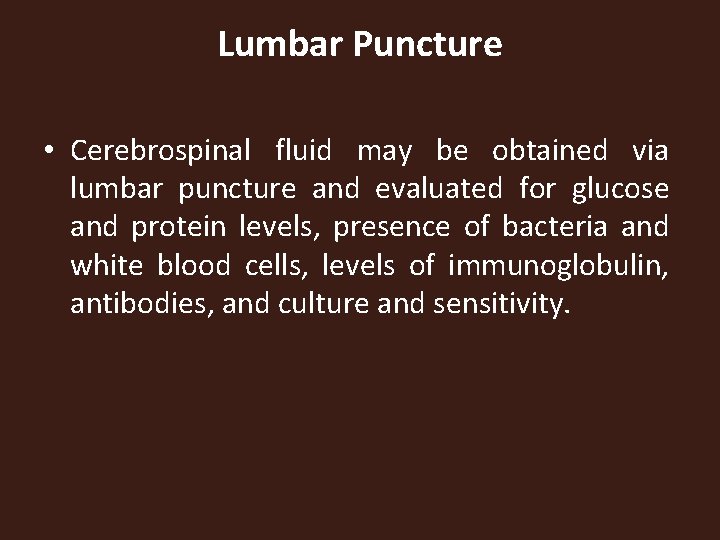
Lumbar Puncture • Cerebrospinal fluid may be obtained via lumbar puncture and evaluated for glucose and protein levels, presence of bacteria and white blood cells, levels of immunoglobulin, antibodies, and culture and sensitivity.
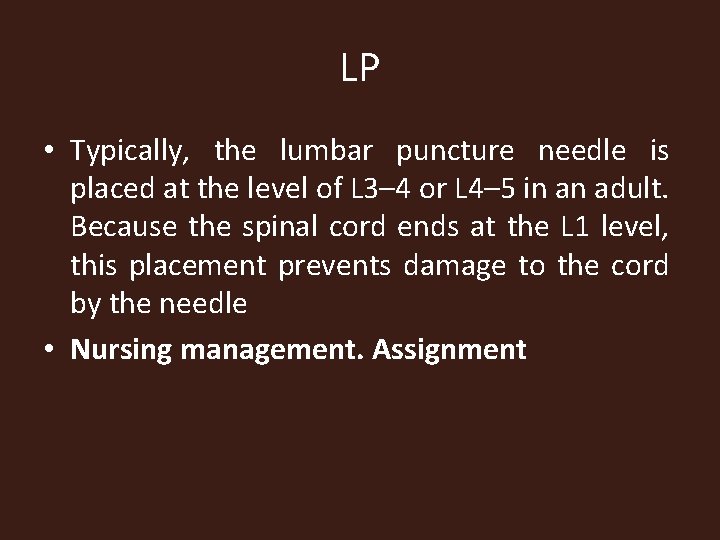
LP • Typically, the lumbar puncture needle is placed at the level of L 3– 4 or L 4– 5 in an adult. Because the spinal cord ends at the L 1 level, this placement prevents damage to the cord by the needle • Nursing management. Assignment
X-Ray Examination • Spinal x-ray examinations are done to determine the status of individual vertebrae and their relationship to one another. If the patient experiences pain with certain movements, he or she may be asked to flex and extend the area of the spine being examined while the radiographs are taken. Skull radiographs may be taken to detect skull fractures or foreign •
Computed Tomography • A computed tomographic (CT) scan is used for diagnosing neurological disorders of the brain or the spine. bodies. CT is used when MRI is contraindicated because of metal aneurysm clips or other metal implants. • Nursing management.
Magnetic Resonance Imaging • Magnetic resonance imaging (MRI) gives a more detailed picture of soft tissue than a CT scan. . MRI is used for diagnosis of degenerative diseases such as multiple sclerosis, arteriovenous malformations, small tumors, hemorrhages, and cerebral and spinal cord edema.
Angiogram • An angiogram is an x-ray study of blood vessels that is used when an abnormality of cerebral or spinal blood vessels is suspected or to obtain information about blood supply to a tumor. • Myelogram • A myelogram is an x-ray examination of the spinal canal and its contents.
Electroencephalogram • Evaluation of the electrical activity of the brain is obtained by use of an electroencephalogram (EEG). Electrodes are attached to the scalp with an adhesive. Electrical activity is transmitted through the electrodes to a tracing. Analysis of the tracing can identify areas of abnormality, such as a seizure focus or areas of slowed activity.

Meningitis • Meningitis means inflammation of the membrane covering the brain and spinal cord, and can be caused by various infectious agents, including viruses, fungi, and protozoans, but bacteria produce the most life-threatening forms. • Meningeal infections generally originate in one of two ways: through the bloodstream or direct invasion for example traumatic injury to the head or post surgical procedure. It can also spread from spinal cord and sinuses to the brain
Causes • Different strain of bacteria can cause meningitis but the most common bacteria causing meningitis include Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b • Several virus can cause meningitis and the most common ones are enteroviruses, arboviruses, HIV and hepex simplex virus
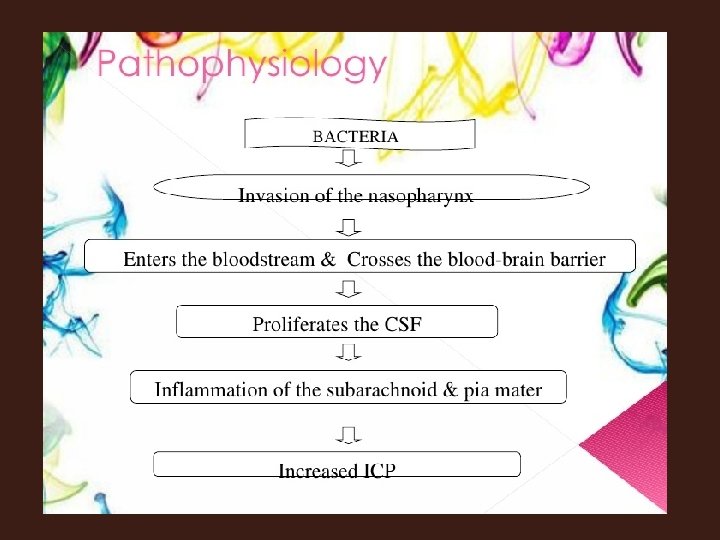
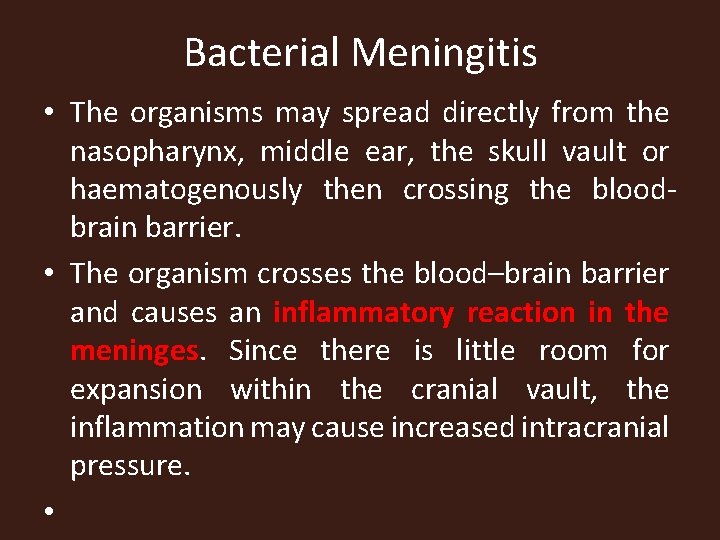
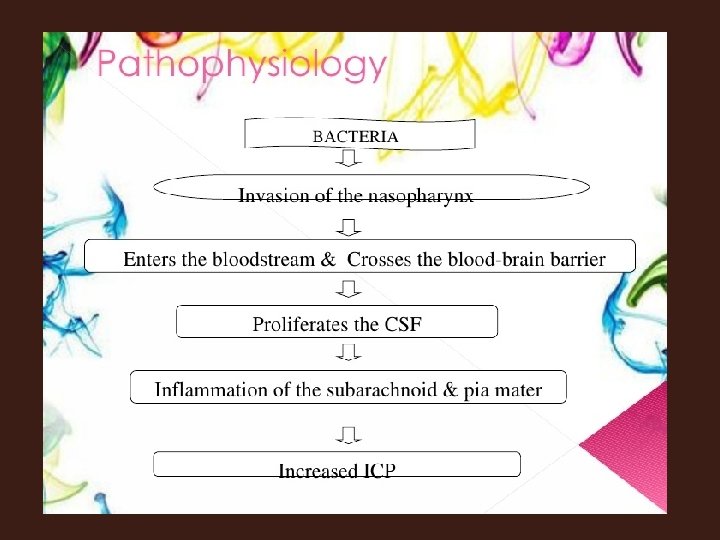
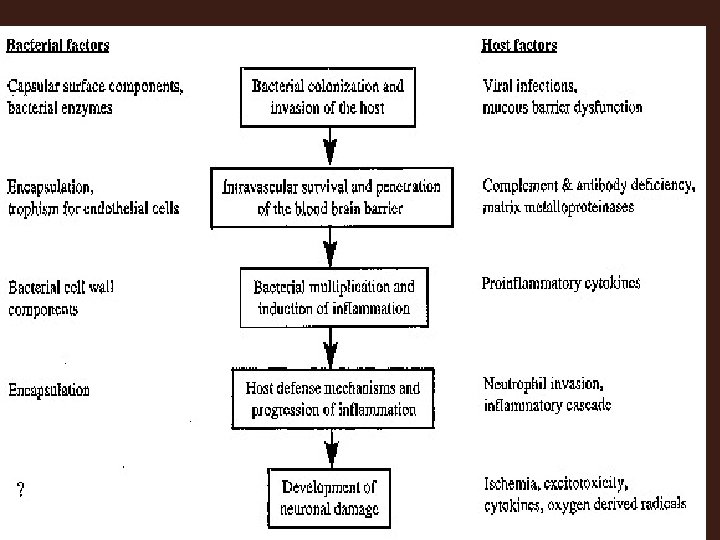
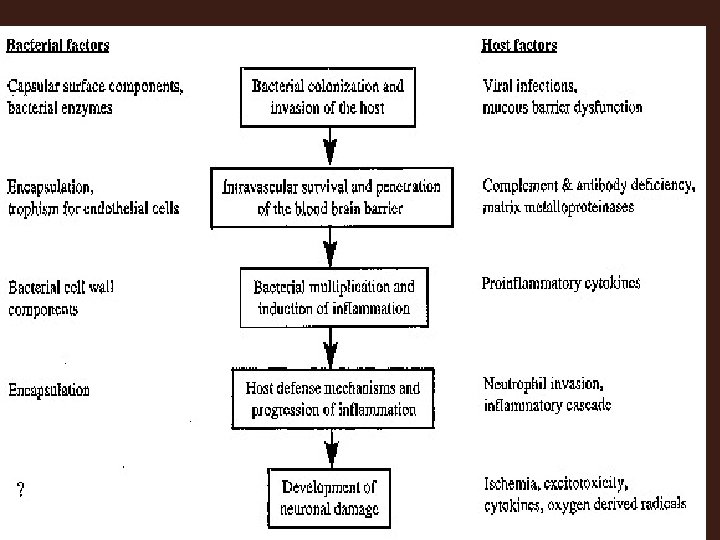
Bacterial Meningitis • The organisms may spread directly from the nasopharynx, middle ear, the skull vault or haematogenously then crossing the bloodbrain barrier. • The organism crosses the blood–brain barrier and causes an inflammatory reaction in the meninges. Since there is little room for expansion within the cranial vault, the inflammation may cause increased intracranial pressure. •
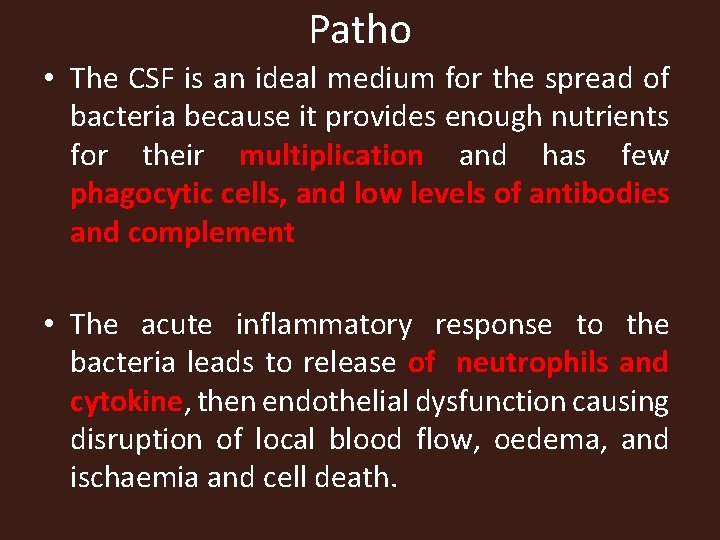
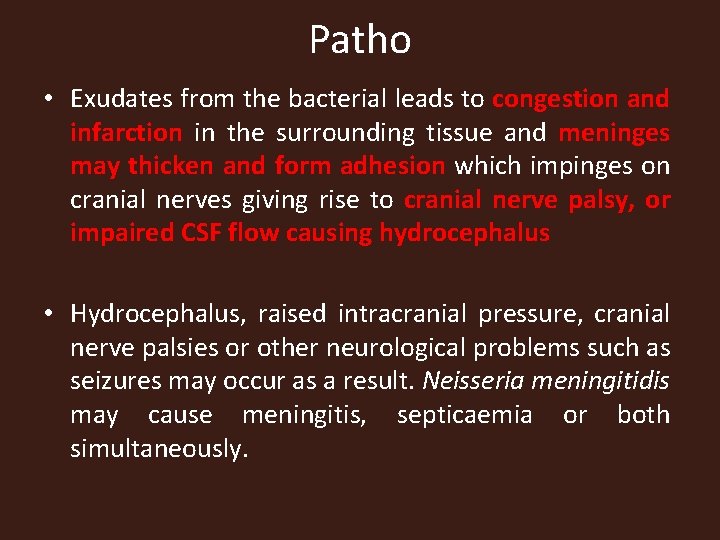
Patho • The CSF is an ideal medium for the spread of bacteria because it provides enough nutrients for their multiplication and has few phagocytic cells, and low levels of antibodies and complement • The acute inflammatory response to the bacteria leads to release of neutrophils and cytokine, then endothelial dysfunction causing disruption of local blood flow, oedema, and ischaemia and cell death.
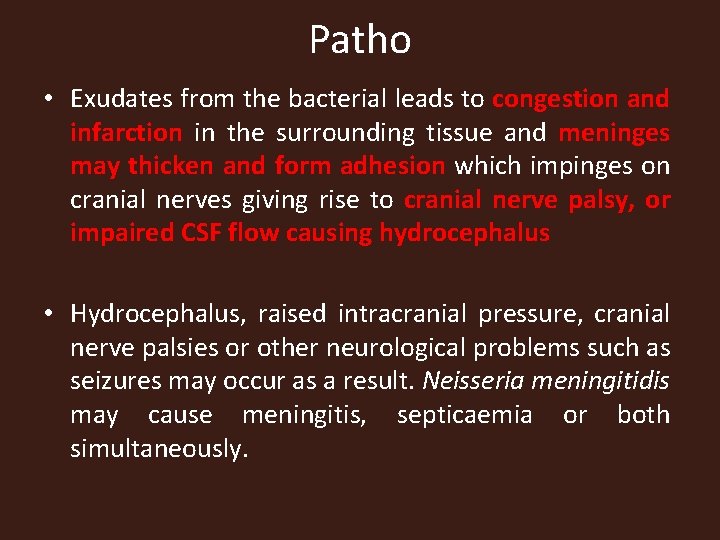
Patho • Exudates from the bacterial leads to congestion and infarction in the surrounding tissue and meninges may thicken and form adhesion which impinges on cranial nerves giving rise to cranial nerve palsy, or impaired CSF flow causing hydrocephalus • Hydrocephalus, raised intracranial pressure, cranial nerve palsies or other neurological problems such as seizures may occur as a result. Neisseria meningitidis may cause meningitis, septicaemia or both simultaneously.

Viral meningitis • Acute viral infection of the meninges is the most common cause of meningitis • It often occurs as combined meningoencephalitis • In viral meningitis there is a predominantly lymphoid immune reaction without the formation of pus or adhesions, there is no cerebral oedema unless encephalitis occurs.
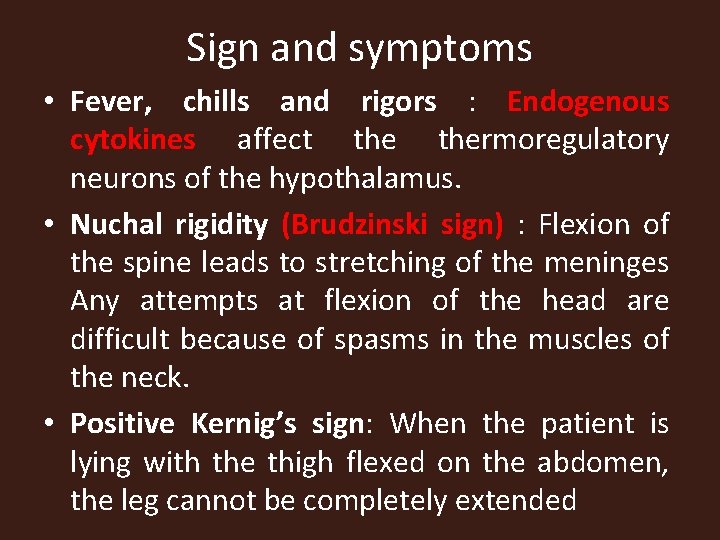
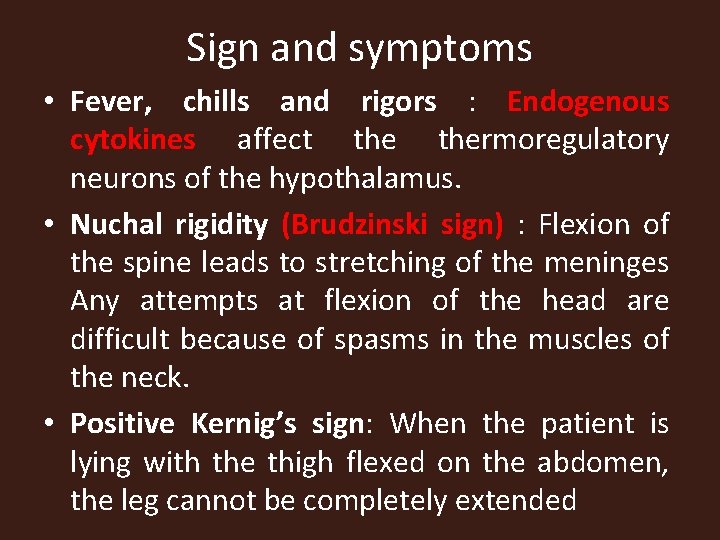
Sign and symptoms • Fever, chills and rigors : Endogenous cytokines affect thermoregulatory neurons of the hypothalamus. • Nuchal rigidity (Brudzinski sign) : Flexion of the spine leads to stretching of the meninges Any attempts at flexion of the head are difficult because of spasms in the muscles of the neck. • Positive Kernig’s sign: When the patient is lying with the thigh flexed on the abdomen, the leg cannot be completely extended
Kernig’s sign

Brudzinski sign
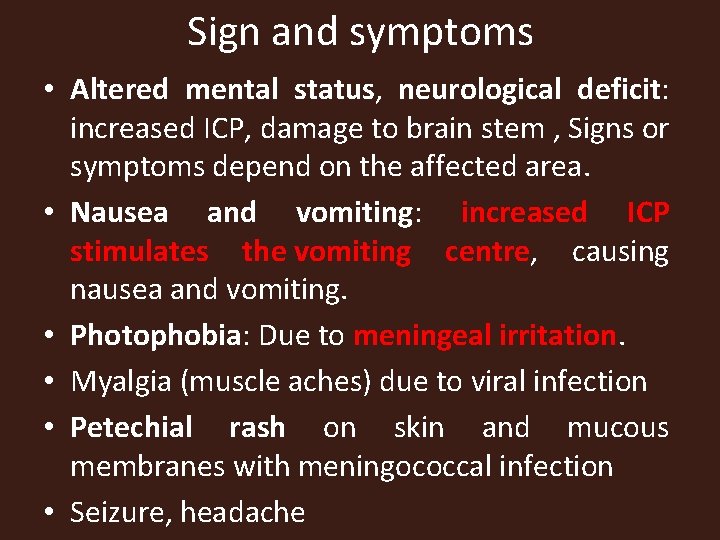
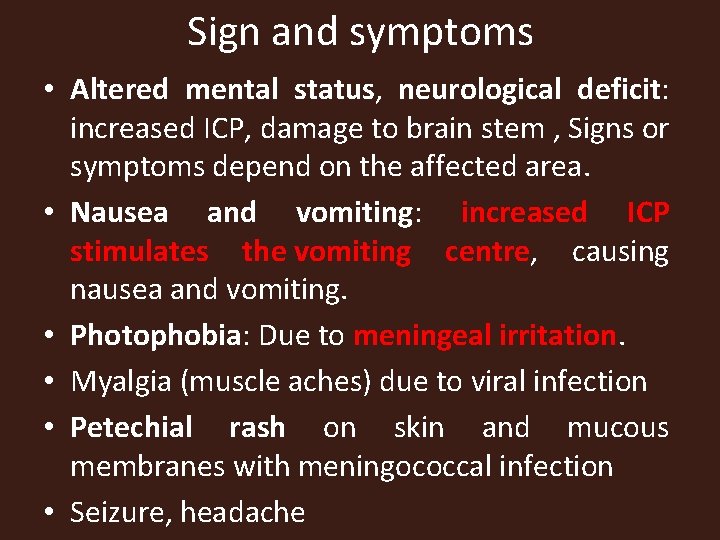
Sign and symptoms • Altered mental status, neurological deficit: increased ICP, damage to brain stem , Signs or symptoms depend on the affected area. • Nausea and vomiting: increased ICP stimulates the vomiting centre, causing nausea and vomiting. • Photophobia: Due to meningeal irritation. • Myalgia (muscle aches) due to viral infection • Petechial rash on skin and mucous membranes with meningococcal infection • Seizure, headache

Diagnosis • Lumbar puncture: • Polymerase chain reaction (PCR) test of cerebrospinal fluid to test for organism • Complete blood count • Culture and sensitivity • CT scan
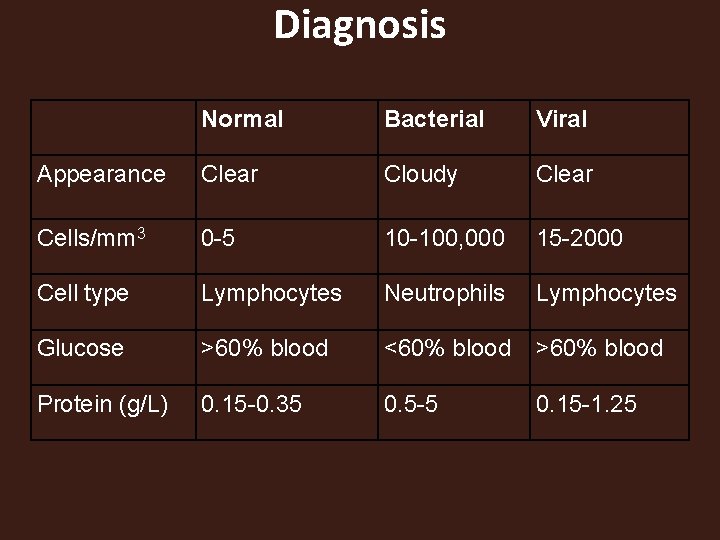
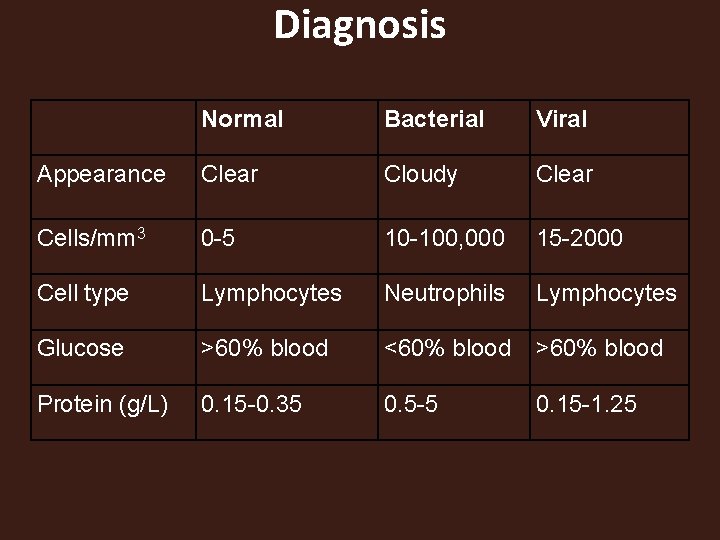
Diagnosis Normal Bacterial Viral Appearance Clear Cloudy Clear Cells/mm 3 0 -5 10 -100, 000 15 -2000 Cell type Lymphocytes Neutrophils Lymphocytes Glucose >60% blood <60% blood >60% blood Protein (g/L) 0. 15 -0. 35 0. 5 -5 0. 15 -1. 25
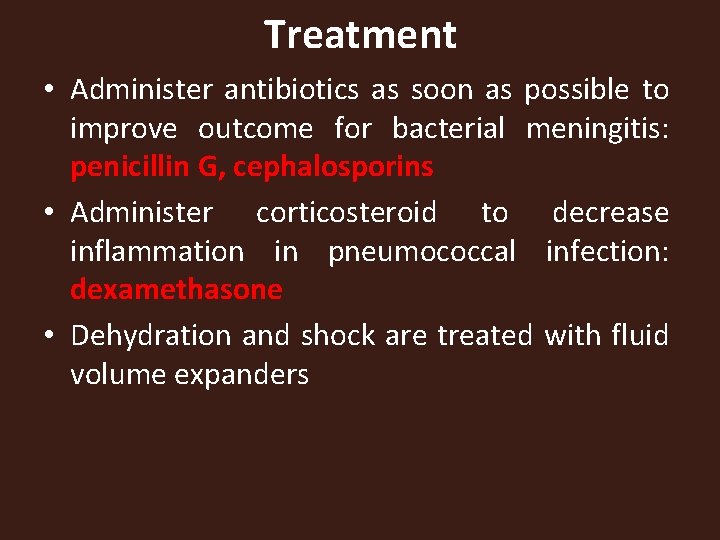
Treatment • Administer antibiotics as soon as possible to improve outcome for bacterial meningitis: penicillin G, cephalosporins • Administer corticosteroid to decrease inflammation in pneumococcal infection: dexamethasone • Dehydration and shock are treated with fluid volume expanders
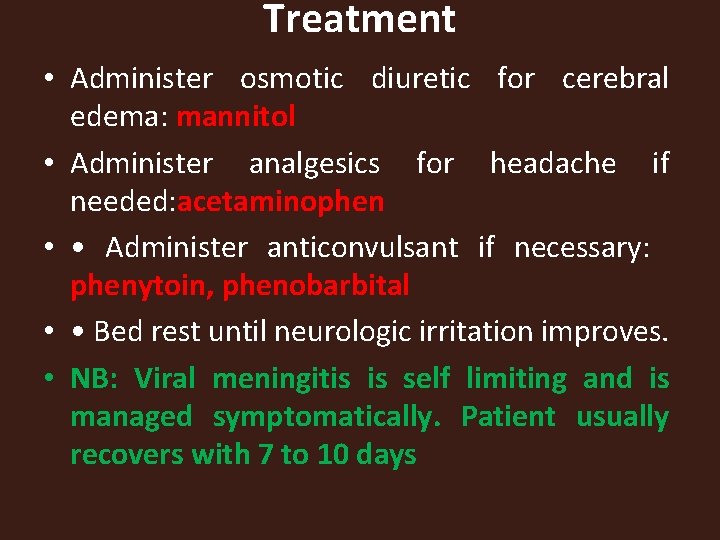
Treatment • Administer osmotic diuretic for cerebral edema: mannitol • Administer analgesics for headache if needed: acetaminophen • • Administer anticonvulsant if necessary: phenytoin, phenobarbital • • Bed rest until neurologic irritation improves. • NB: Viral meningitis is self limiting and is managed symptomatically. Patient usually recovers with 7 to 10 days
Nursing care • Neurologic status and vital signs are continually assessed. Pulse oximetry and arterial blood gas values are used to quickly. Identify the need for respiratory support as the increasing. • Rapid intravenous (IV) fluid replacement may be prescribed. • Keep room darkened due to photophobia. • Monitoring body weight, serum electrolytes, and urine volume

Nursing care • Protecting the patient from injury secondary to seizure activity or altered level of consciousness • Preventing complications associated with immobility, such as pressure ulcers and pneumonia • Instituting droplet precautions until 24 hours after the initiation of antibiotic therapy (oral and nasal discharge is considered infectious)
Encephalitis • Inflammation of the brain parenchyma caused by viruses Causes • This is an uncommon disease, but the most common cause in herpes simplex virus (HSV). • Other viruses causing encephalopathy include echovirus, varicella zoster, cytomegalovirus, Epstein–Barr virus). • Tick and mosquito are the vector that transmit the disease

Encephalitis • Encephalitis may occur as a complication of viral disease such as chicken pox, measles , mumps • Post viral encephalitis is an immune mediated disorder and follows the end of viral infection by 2 to 12 days. • Once the virus crosses the blood brain barrier and enters the neural cells •

Encephalitis • It leads to disruption of normal neural function, hemorrhage and an inflammatory response occurs • Neurological impairment is caused by direct infection of the neural cell • Inflammation affects the meninges and parenchyma causing oedema and hence raised intracranial pressure, diffuse and focal neurological dysfunction. • Severity can be mild or fatal and can lead to coma and death.
S/S • • • It may be sudden or insidious Behavior and personality change Stiff neck Photophobia Lethargy : Seizure and Confusion Encephalitis is different from meningitis because there is altered mental status, motor or sensory deficit and speech or movement disorder

Diagnosis • LP : CSF analysis • MRI • EEG
Management • In all cases except herpes simplex encephalitis there is no effective treatment apart from supportive management. • Treatment is usually symptomatic • Seizures are treated with anticonvulsants. • Supportive measure to maintain cardiac and respiratory function • Herpes Simplex type 1 Encephalitis is treated with Acyclovir
Mgt • Administer corticosteroid to decrease inflammation: dexamethasone • Administer antipyretics to reduce fever: acetaminophen • Administer anticonvulsants to decrease chance of seizure activity: phenytoin, phenobarbital • Administer diuretics to decrease cerebral edema, if indicated:
Nursing Care Monitor respiratory status for compromise. • Monitor neurologic function for change. Range of motion exercises—active or passive. Turn and position patient. Monitor neurologic status for changes— typically use Glasgow Coma Scale • Provide a quiet environment to decrease unnecessary stimulation. • • Monitor fluid input and output. • • •
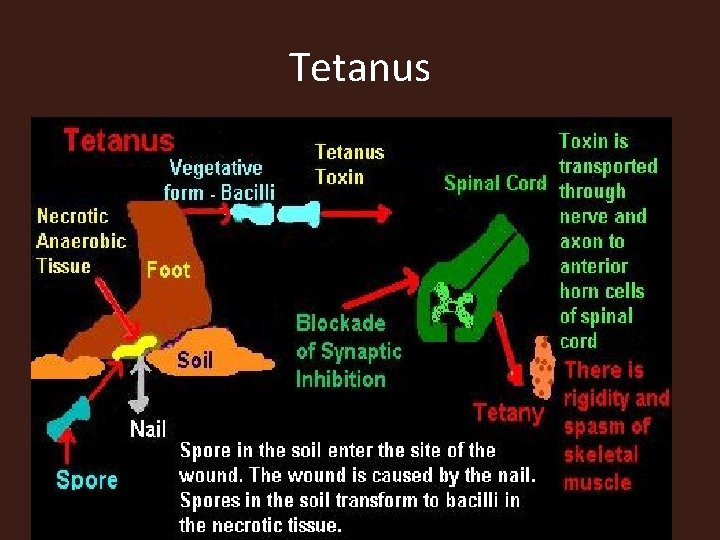
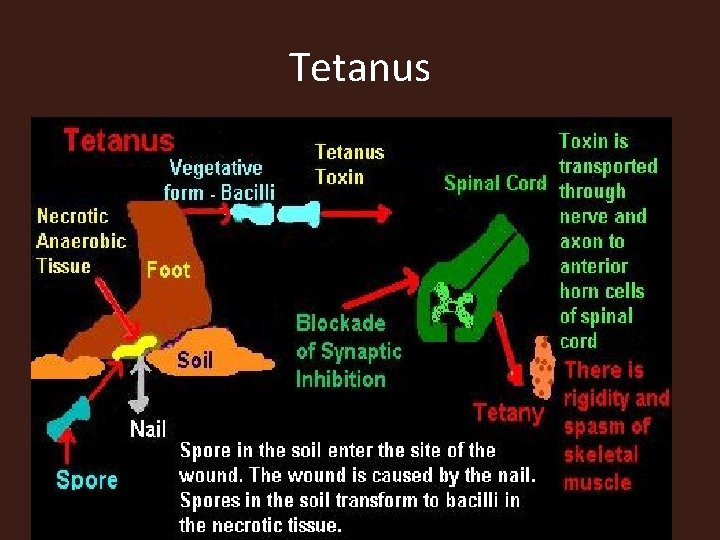
Tetanus • Tetanus is a toxin mediated condition causing muscle spasms following a wound infection. Aetiology It is caused by an exotoxin, tetanospasmin, produced by Clostridium tetani (the causative organism), an anaerobic spore forming bacillus, originates from the faeces of domestic animals.
Pathophysiology • The bacteria enter the body at the site of a wound and proliferates in ischaemic or necrotic tissue, usually in a poorly tended wound. They replicate and produce a neurotoxin, tetanospasmin • This toxin travels along the sheaths of peripheral nerves to the CNS and acts by blocking the release of inhibitory mediators in the spinal motor synapses. • It inhibits the release of acetylcholine from nerve endings in muscle, but more importantly it interferes with synaptic reflexes in the spinal cord, causing spasms and autonomic dysfunction.
Tetanus
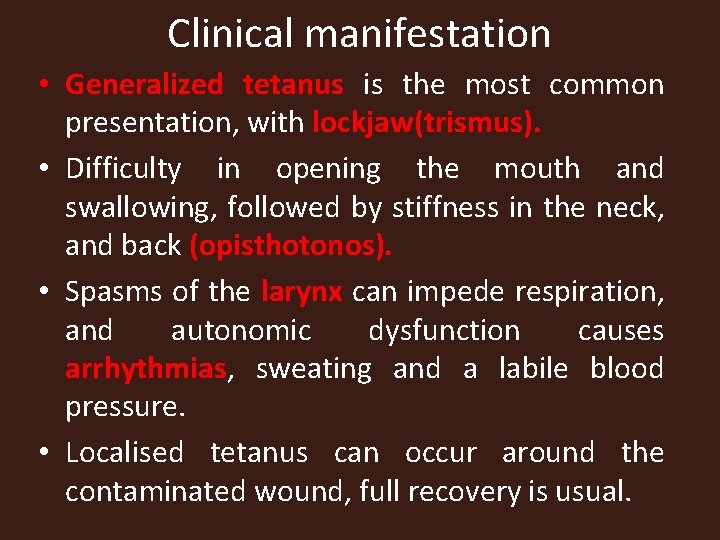
Clinical manifestation • Generalized tetanus is the most common presentation, with lockjaw(trismus). • Difficulty in opening the mouth and swallowing, followed by stiffness in the neck, and back (opisthotonos). • Spasms of the larynx can impede respiration, and autonomic dysfunction causes arrhythmias, sweating and a labile blood pressure. • Localised tetanus can occur around the contaminated wound, full recovery is usual.
Management • Following contaminated injury, toxin production is prevented by local debridement of wounds and treatment with metronidazole 500 mg intravenously 6 -hourly. • Human tetanus immune globulin (passive immunisation) in high titre is given to neutralize free toxin. • A booster dose with tetanus toxoid (which is an inactivated toxin which induces active immunisation), should additionally be given. • Antibiotics may also be indicated. • Nutrition is maintained enterally or parenterally
MGT • Active tetanus: Patients should be nursed in a quiet, dark area to reduce spasms. • Intravenous penicillin and high doses of human tetanus immune globulin should be given i. m. (some around the wound). However, the immunoglobulin can only neutralize circulating toxin.
MGT • Large doses of diazepam may be needed to reduce spasms and cardiovascular instability is controlled with β blockers. • Tracheostomy and ventilatory support may be necessary for severe laryngeal spasm.
ASSIGNMENT • Nursing management
CVA • Cerebrovascular accident is the infarction (death) of brain tissue caused by the disruption of blood flow to the brain.
Pathophysiology • Cerebral function is dependent on oxygen and glucose delivery to neurons of the brain. • The brain has no capability to store oxygen or glucose and when blood supply is compromised or absent, the oxygen and glucose needed to meet the brain’s metabolic needs are not available and the brain dies.
CVA • CVA results from an interruption of blood flow to a specific area of the brain (cerebral ischemia) • Ischemia of cell directly cause cellular necrosis (death) and infarct Ischemia can be caused by Ø Cerebral thrombosis Ø Embolus pressure on blood vessel Ø Intercerebral haemorrhage
CVA • There are two general classifications of CVAs: ischemic and hemorrhagic. • Ischemic CVAs develop from a prolonged blockage in arterial blood flow to a part of the brain. • Hemorrhagic CVAs occur as a result of bleeding into the brain.
Ischemic Stroke • The arterial blockage causing an ischemic stroke may occur as a result of a thrombus (a blood clot in the cerebral artery) or an embolus (a blood clot that has traveled to the brain from elsewhere in the body). • The carotid arteries supply a major portion of the blood that goes to the brain If plaque forms in these arteries as a result of atherosclerosis, the person is at risk of stroke as blood supply to the brain is diminished or stopped.
Hemorrhagic stroke • A hemorrhagic stroke occurs when a blood vessel in the brain is broken, leading to ischemia (reduced flow) and hypoxia downstream. Causes of hemorrhagic stroke include hypertension, a burst aneurysm, or an arteriovenous malformation (abnormal connection). Hemorrhage in the brain significantly increases ICP, worsening the resulting brain injury.

Signs and symptoms • The particular vessel or vessels involved determine the area of the brain affected and therefore the symptoms that result. Neurological effect of stroke can range from mild motor disturbance to profound coma. • There may be weakness (hemiparesis), inability to speak or understand (aphasia), difficulty with vision, loss of balance , decrease level of consciousness, confusion and incontinence may occur.
Signs and symptoms • Motor function deficit affects mobility, respiratory function, swallowing, and speech, gag reflex self care abilities. • Paralysis, weakness, or numbness can present. • The onset will be sudden and generally involves one side of the body, the side of the body opposite to the damaged area.
Signs and symptoms • Language disorder involves expression and comprehension of both written and spoken words. • Aphasia or dysphasia may be present. Aphasia refers to the absence of language; dysphasia refers to difficulty with speech and is not as severe as aphasia. • The patient may experience trouble selecting correct words, use incomprehensible or nonsense speech, have trouble understanding others’ speech, and have trouble writing or reading.
Signs and symptoms • Memory and judgment may be affected by stroke. • Bladder and bowel incontinence usually temporary after stroke. Emotional changes, personality changes might be present • Visual field disturbances are also a common symptom of a stroke. The visual loss is painless and may involve loss of all or part of the vision in one eye.
Diagnosis • • • Physical and neurological examination CT scan Cerebral angiogram MRI Carotid Doppler testing can determine if stenosis of the carotid arteries exists
Management Initial emergency care • ABCs (airway, breathing, and circulation) should be monitored. • Oxygen should be administered to maintain oxygen saturation greater than 90%. • Vital signs and heart rhythm should be monitored.
Management • Once the specific cause has been determined, systemic tissue plasminogen activator (t-PA) is used to dissolve clot and emboli in non hemorrhagic stroke. • Cerebral hemorrhage is a major complication of thrombolytic Therapy therefore Intracerebral hemorrhage must be ruled out before t-PA therapy
Management • Antihypertensive drugs are ordered as appropriate e. g nifedipine. The patient may receive an antiseizure medication as a prophylactic
Surgical intervention • About one third of all stroke can be traced to obstruction of the arteries that supply the brain. • This arteries are generally accessible to surgeon and it can be opened and the plaque removed. The mechanical embolus removal in cerebral ischemia can be used up to 8 hours after the onset of stroke.
Complication • Seizure: seizure are common complication of a stroke because neural pathway are interuppted when blood flow is blocked or there is irritation of cerebral cortex from an intercranial bleed. • Hydrocephalus: if blood leaks into ventricle system, it interferes with the resorption of CSF, causing hydrocephalus.
NSG MANAGEMENT • Monitor vital signs for changes. • Assess neurological status for signs of deterioration—perform neurological • Checks at least every 4 hours—typically use Glasgow Coma Scale • Monitor for signs of increased intracranial pressure—diminished level of consciousness, headaches, restlessness, confusion, nausea and vomiting, speech changes, or seizures. • •
NSG MANAGEMENT • Develop a means of communication with the patient—aphasia may compromise use of call bell system or intercom. • Provide psychological support • Encourage and educate patient on rehabilitation • Involve family in the care
Nursing diagnosis • Self care deficit related to neurological impairment. . • Impaired physical mobility to weakness, paralysis. . . . • Ineffective breathing pattern related to neurological disruption of respiration • Disturbed sensory perception related to decreased level of consciousness • Risk of injury related to decreased level of consciousness
 Neural circuits the organization of neuronal pools
Neural circuits the organization of neuronal pools Sensory input and motor output
Sensory input and motor output What are neuron processes
What are neuron processes Nervous system and digestive system
Nervous system and digestive system Endocrine system vs nervous system
Endocrine system vs nervous system Mechanism of action of hormones
Mechanism of action of hormones Adh function
Adh function Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worm breton là gì
Tư thế worm breton là gì Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V. c c
V. c c Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tia chieu sa te
Tia chieu sa te Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể So nguyen to
So nguyen to Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
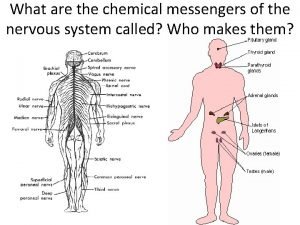
Thế nào là mạng điện lắp đặt kiểu nổi Chemical messengers of the nervous system
Chemical messengers of the nervous system Platyhelminthes asexual reproduction
Platyhelminthes asexual reproduction The nervous system is made up of
The nervous system is made up of Neuron anatomy
Neuron anatomy Nervous system learning objectives
Nervous system learning objectives Componentes componentes
Componentes componentes Stimulus in nervous system
Stimulus in nervous system Spinal cord structure
Spinal cord structure Autonomic nervous system visceral
Autonomic nervous system visceral Alpha 1 receptors
Alpha 1 receptors Spinal nerves
Spinal nerves Sns somatic nervous system
Sns somatic nervous system The nervous system brain scienstructable
The nervous system brain scienstructable Skeletal muscle autonomic nervous system
Skeletal muscle autonomic nervous system Roundworms nervous system
Roundworms nervous system Phylum arthropoda characteristics
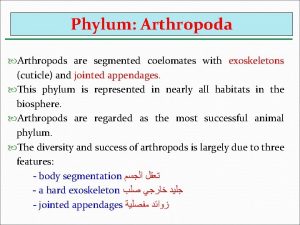
Phylum arthropoda characteristics Nervous system of arthropods
Nervous system of arthropods Are arthropods coelomates
Are arthropods coelomates Division of central nervous system
Division of central nervous system Parasympathatic nervous system
Parasympathatic nervous system Nervous system in coelenterata
Nervous system in coelenterata Autonomic nervous system consists of
Autonomic nervous system consists of Module 10 the nervous and endocrine systems
Module 10 the nervous and endocrine systems Section 35-1 human body systems answer key
Section 35-1 human body systems answer key Somatic and autonomic nervous system
Somatic and autonomic nervous system Human nervous system ppt
Human nervous system ppt Basic unit of nervous system
Basic unit of nervous system Blood clot feedback loop
Blood clot feedback loop Histology of cns ppt
Histology of cns ppt What is white matter made of
What is white matter made of Comparison of endocrine and nervous system
Comparison of endocrine and nervous system 8 divisions of the nervous system
8 divisions of the nervous system How to take care of your nervous system
How to take care of your nervous system Nervous system effector cells
Nervous system effector cells Chapter 15 nervous system diseases and disorders
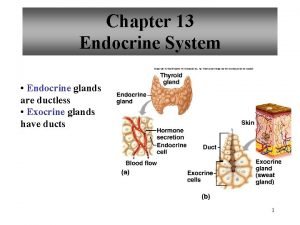
Chapter 15 nervous system diseases and disorders Are endocrine glands ductless
Are endocrine glands ductless Beta-blockers for overactive sympathetic nervous system
Beta-blockers for overactive sympathetic nervous system Somatic motor function
Somatic motor function Spinal cord dorsal and ventral roots
Spinal cord dorsal and ventral roots Excretory system of silkworm
Excretory system of silkworm 35-3 divisions of the nervous system
35-3 divisions of the nervous system Building block of the nervous system
Building block of the nervous system Structure of nervous system graphic organizer
Structure of nervous system graphic organizer Medunerve
Medunerve Planaria nervous system
Planaria nervous system Ctenophora vs cnidaria
Ctenophora vs cnidaria Referred pain
Referred pain Sympathetic and parasympathetic nervous system difference
Sympathetic and parasympathetic nervous system difference Nervous
Nervous Divisions of the nervous system
Divisions of the nervous system Limb apraxia
Limb apraxia Nervous tissue
Nervous tissue Disorders of the nervous system
Disorders of the nervous system Osteochthyes
Osteochthyes How the nervous system works
How the nervous system works Nervous system of computer
Nervous system of computer Enteric plexus
Enteric plexus Pak pandani
Pak pandani Chapter 8 the nervous system
Chapter 8 the nervous system Nervous system
Nervous system Section 35-3 divisions of the nervous system
Section 35-3 divisions of the nervous system Autonomic nervous system
Autonomic nervous system