IN THE NAME OF GOD Orofacial Pain Dr





- Slides: 65
IN THE NAME OF GOD
Orofacial Pain Dr. HR. Saeidi Associate Prof of Neurosurgery KUMS
Pain unpleasant sensory & emotional experience associated with actual & potential tissue damage.
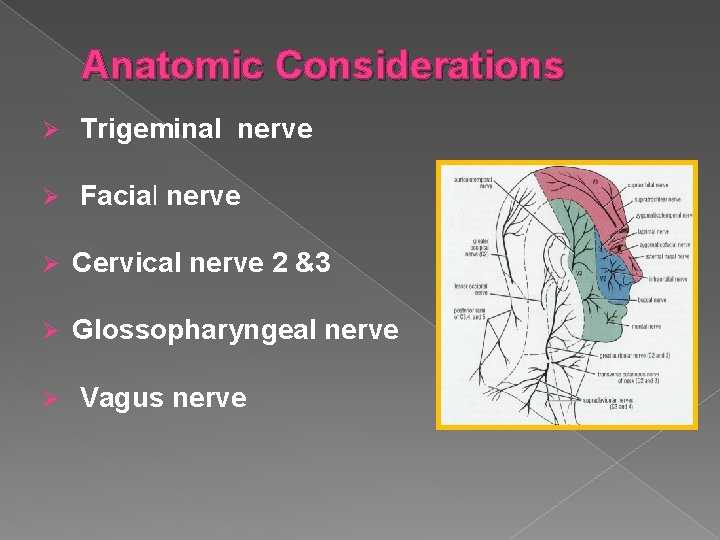
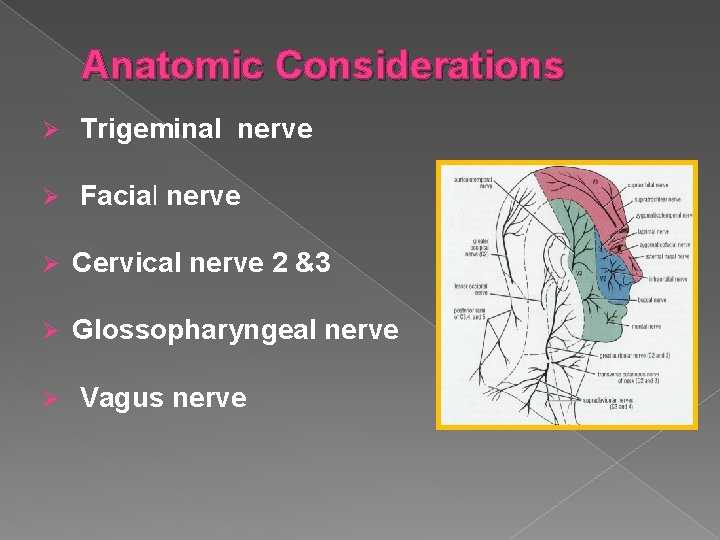
Anatomic Considerations Ø Trigeminal nerve Ø Facial nerve Ø Cervical nerve 2 &3 Ø Glossopharyngeal nerve Ø Vagus nerve
v. Categories 1 - Local pain: Ø Ø Ø Dental Gingival Mucosal Salivary gland Temporomandibular joint Maxillary sinus
v. Categories of orofacial pain 2 - Neurological pain: TN Ø Glossopharyngeal neu Ø Ramsy hunt synd Ø Postherpetic neu Ø 3 - Vascular : Giant cell arteritis Ø Migraine Ø Cluster headache Ø
v. Categories of orofacial pain 4 - Psychogenic pain: Atypical facial pain Ø Atypical odontalgia Ø 5 - Referred pain: Ø Cardiac pain
Evaluation and assessment history: 1 -Chief complaint. 2 - Pain Characteristics � Onset & Intensity � Quality& location � Duration & timing of pain � Course of symptoms since onset � Activities that ↑ or ↓ pain � Associated symptoms � Previous treatments
Past medical history -Connective tissue dis. -Demyelination dis -Metastatic dis. -IHD Social history: - traumatic event prior to onset of pain. -Change in work, or problem marital state.
Physical examination: 1. head & neck skin, 2. Palpation of masticatory muscles, 3. range of mandibular movement. 4. Palpation of soft tissue. 5. Palpation of the TM joint 6. Palpation of cervical muscles 7. Cranial nerve 8. ears, nose, teeth, oropharyngeal
Diagnostic Imaging Ø - confirm diagnosis R/O serious dis Ø -Extent of an identified dis Ø -Most OFP not produce abnormality
v. TMJ DISORDERS 1 -Myofascial pain. 2 -Traumatic injuries. 3 -Arthritis &Arthrosis: infective , systemic, degenerative. 4 -Internal derangement.
v Myofascial Ø Ø Ø pain diffuse poorly localized periauricular pain may be severe in morning ↑ pain in tension & anxiety ↓ range of mandibular movemen Ø "trigger points Ø
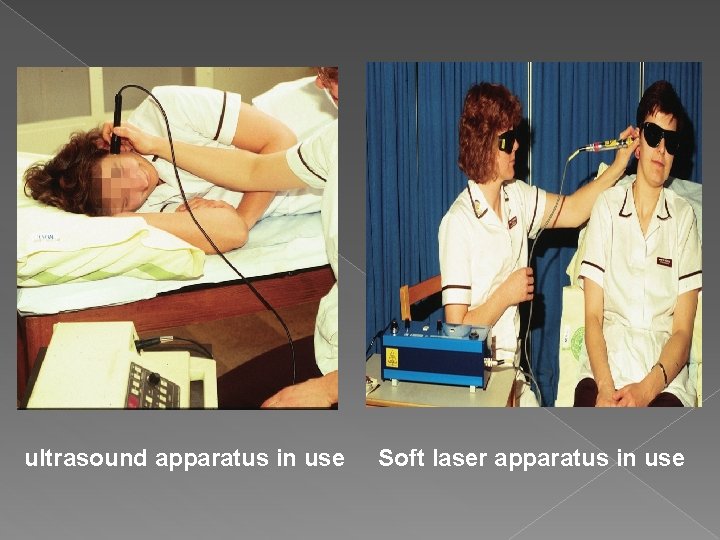
Manage of myofascial pain -Education of patient & self care of teeth. � -thermal therapy(U/S, laser ). � � ü ü -Pharmacotherapy: -NSAID, muscle relaxant -Antianexiety&TCA Botox injection. Trigger point block therapies
INTERNAL DERANGMENT OF TMJ � Pain on palpation over TMJ. � ↓ joint range of motion. � Deviation on opening. � Joint noises with pain. � Joint crepitus
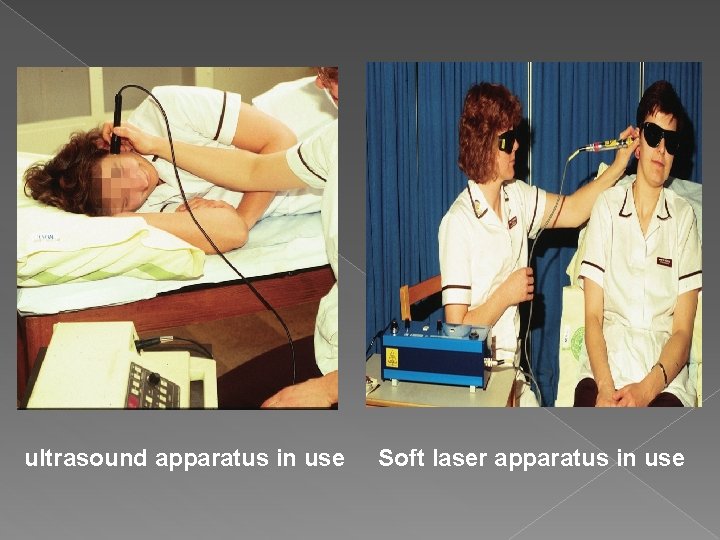
ultrasound apparatus in use Soft laser apparatus in use
v. NEURALGIA: CAVITATIONAL OSTEONECROSIS Ø Ø Ø Rare continuous lancinating in site of previous tooth extraction. Usually in lower 3 rd molar region Pain not interfere with sleep RG: mooth eaten in site of extraction Treated by resection of bone with pain
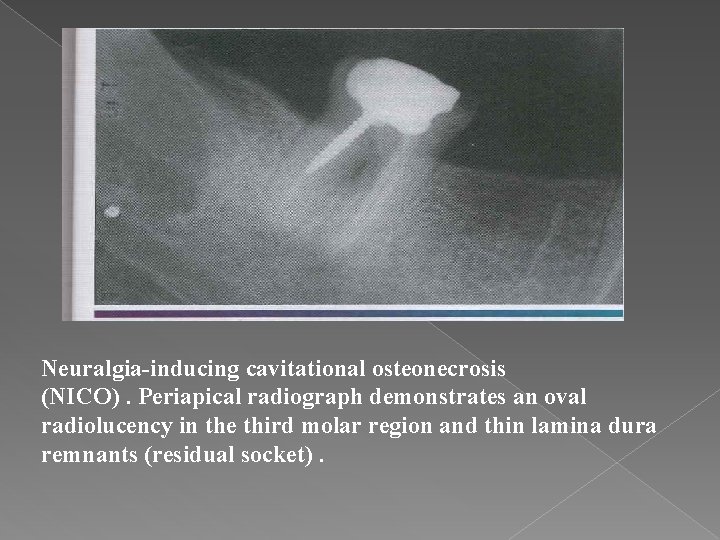
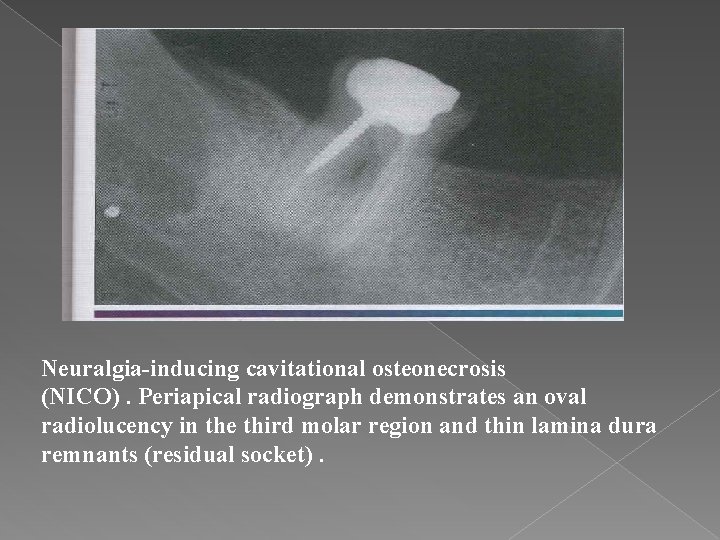
Neuralgia-inducing cavitational osteonecrosis (NICO). Periapical radiograph demonstrates an oval radiolucency in the third molar region and thin lamina dura remnants (residual socket).
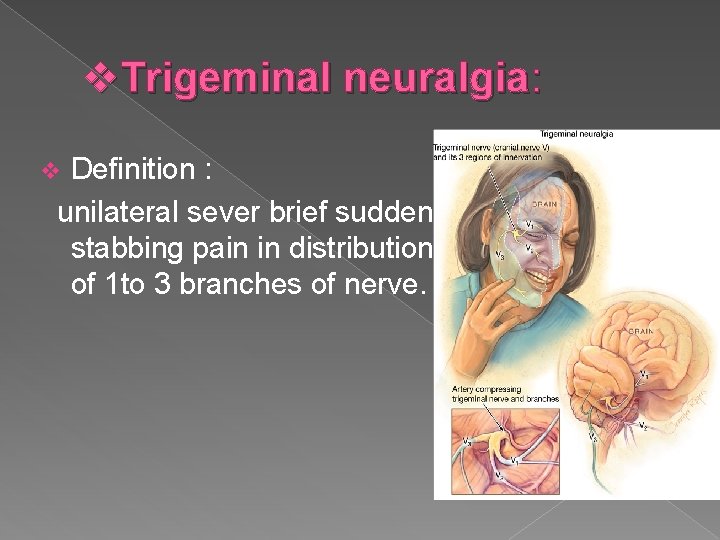
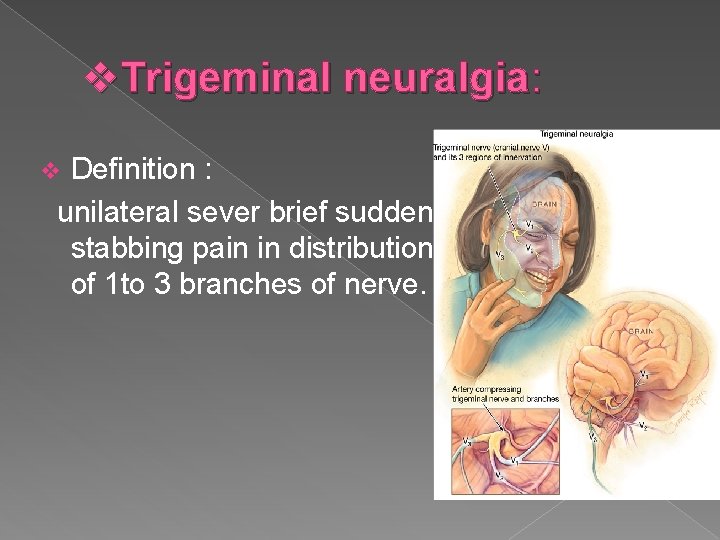
v. Trigeminal neuralgia: Definition : unilateral sever brief sudden stabbing pain in distribution of 1 to 3 branches of nerve. v
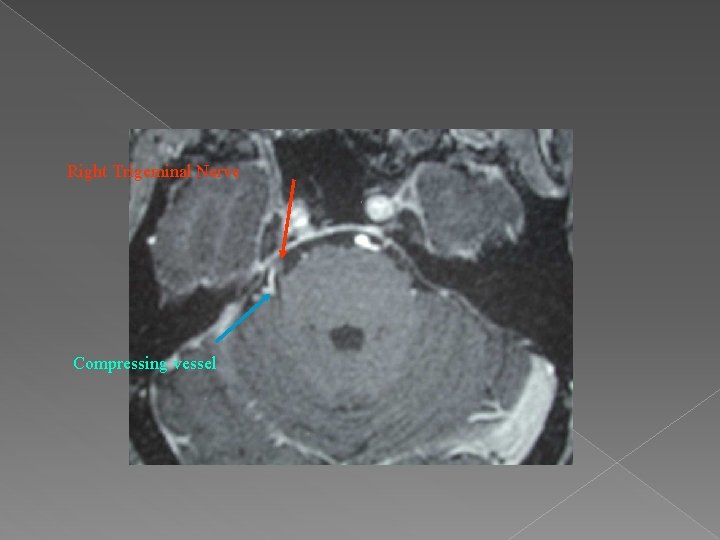
v. Etiology and pathophysiology Ø primary : vascular compression of nerve near its entry into the pons (superior cerebellar artery). Ø Secondary : MS, tumors , basilar artery eneurysim.
v Clinical features Ø Ø Ø episodic , recurrent unilateral facial, sudden high intensity stabbing or electric shock pain few seconds to minutes triggered by stimulation: touching of face, washing , shaving , chewing and talking.
v. TN Clinical features It occurs mostly after 5 th decade. Ø PE of face is nearly always normal. Ø If sensory loss is present a mass lesion is more likely Ø In young pts MS should be considered. Ø
v. TN Diagnosis: history, PE. Ø A careful search for ipsilateral dental pathology Ø MRI & MRA if there is suspicion of underlying pathology. Ø
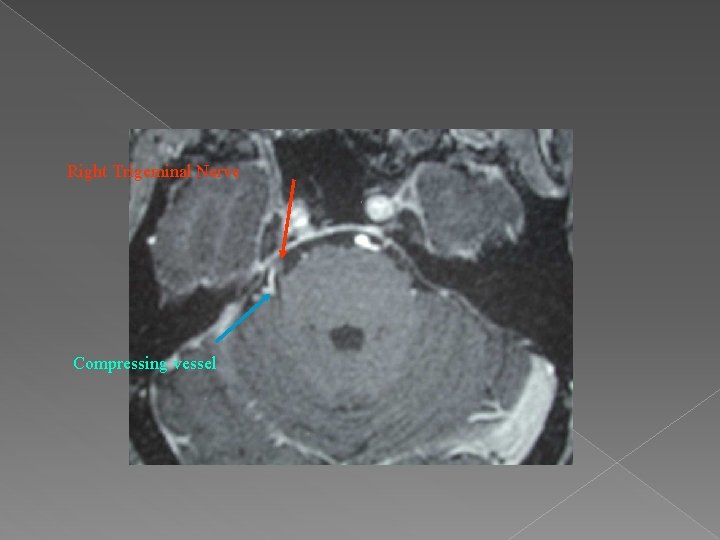
Right Trigeminal Nerve Compressing vessel
v. Medical Treatment of TN ü ü ü ü Carbamazepine(effective in 75% as first line) Oxcarbazepine in pts sensitive to Carbamazepine. Baclofen Gabapentine Lamotrigine Clonazepam Phenytoin Valproate
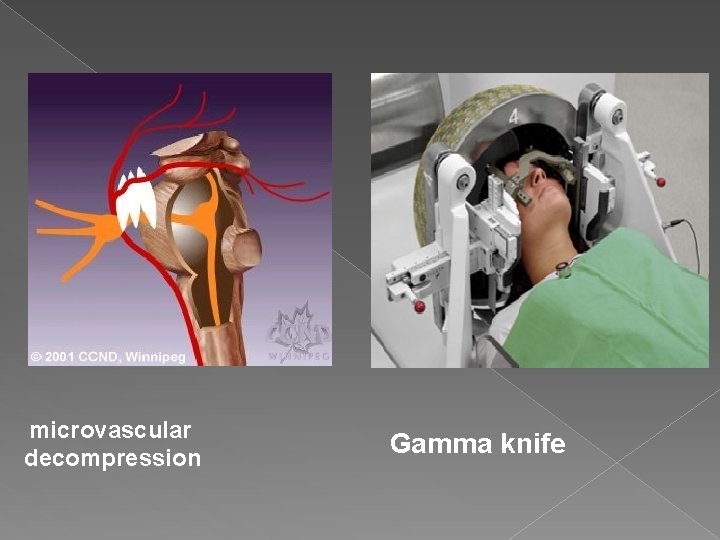
v. Surgical treatment of TN If medical treatment (carb) has been ineffective after 4 weeks at maximum tolerated dose. a) peripheral procedures : alcohol injection, cryosurgery , nerve avulsion a) Percutaneous ganglion procedure: RF thermocoaglation , glycerol injection , balloon compression, Gamma knife. Open operations : MVD , trigeminal root section, b)
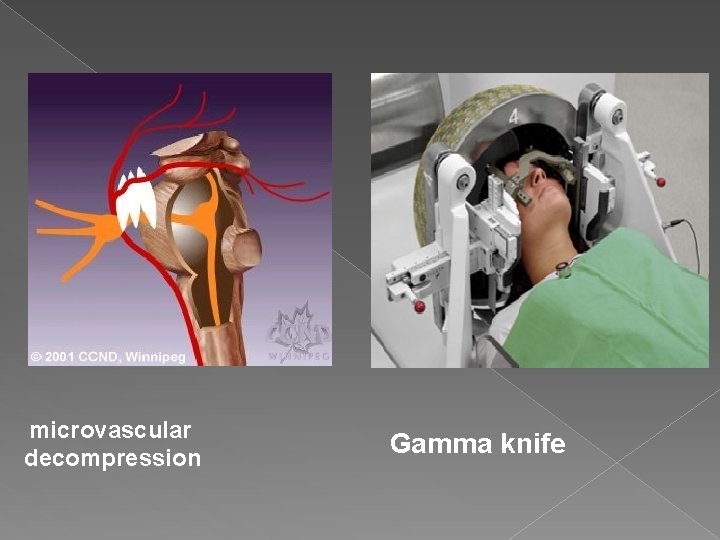
microvascular decompression Gamma knife
v. Post-herpetic neuralgia -Pain : aching, burning, shock like. � -Potential sequela of infection with herpes zoster. � � Pain persist longer than one month after healing vesicle classified as PHN.
Management: � -Antiviral and corticosteroids after presentation of rash reduce PHN � -Anticonvulsant drugs � -Local anesthesia injected to painful site.
v. Glossopharangeal neuralgia Clinical features : Ø Ø Ø Pain similar to TN. Affect tonsil , tongue base, ear, intra articular area. Patient often point just to behind mandible angle. Triggered by yawing and swallowing. may be associated with a vasovagal reflex, The application of a topical anesthetic to the pharyngeal mucosa eliminates nerve pain.
v. Glossopharangeal neuralgia Etiology: Causes : are intra or extracranial tumors & vascular abnormalities that compress CN IX. Management: -Anti convulsion : carbamazepine. Ø -NVD Ø -Percutaneous R. F at jugular foramen. Ø Ø -Intra or extra cranial neuroectomy.
v. Occipital Neuralgia paroxysmal stabbing pain in greater or lesser occipital nerves area. Ø may be caused by trauma, Ø Palpation below the superior nuchal line may reveal a tender spot. Ø Treatment has included occipital nerve block, neurolysis, C 2 dorsal root gangionectomy , Ø
v. Post -Traumatic Neuropathic Pain Its caused by 5 th nerve injuries from facial trauma or surgical procedures, such as the removal of impacted third molars, the placement of dental implant Ø Clinical Manifestations: The pain may be persistent or occur only in response to a stimulus, such as a light touch. Ø Patients may experience anesthesia , paresthesia, allodynia , or hyperalgesia.
v. Post -Traumatic Neuropathic Pain Treatment: Ø Ø Ø may be surgical , nonsurgical, or both, Systemic corticosteroids a when administered within the first week after a nerve injury. TCAs Anticonvulsant drugs, Gabapentin. Topical capsaicin.
v. Complex Regional Pain Syndrome( CRPs) chronic pain conditions that develop as a result of injury. Ø patients suffer from allodynia, hyperalgesia, and spontaneous pain that extends beyond the affected nerve dermatome. Ø it accompanied by motor and sweat abnormalities, atrophic changes in muscles and skin, edema, Ø
v. Complex Regional Pain Syndrome Types of CRPs : 1 - CRPS I was previously termed reflex sympathetic dystrophy (RSD), 2 - CRPS II was previously termed causalgia. Etiology and Pathogenesis: Ø believed to result from changes after trauma that couples sensory nerve fibers with sympathetic fibers.

Complex Regional Pain Syn treatment physical therapy. Ø block of regional sympathetic ganglia or regional intravenous blockades with guanethidine , reserpine, or phenoxybenzamine, Ø Bisphonates such as alendronate or pamidronate. Ø
v. Nervous Intermedius (Geniculate) Neuralgia Paroxysmal pain of facial nerve, may result of herpes zoster of geniculate ganglion. -Clinical features: Ø -Pain at the ear, anterior tongue, soft palate. Ø -Not intense like T. N. Ø - Ramsay-hunt syndrome may develop(Facial paralysis , vesicle , tinnitus & vertigo) v
Management: � -High dose of steroid for 2 -3 weeks. � -Acyclovir significantly ↓ duration. � -Anti convulsion , Carbamezipine. � -Surgery: section of nerve intermedius.

v. Bell's palsy Ø about 50% of pts , pain occur in the ear but sometimes spreading down the jaw, either precedes or develops at the same time as the palsy. Ø Treatment: prednisolone , acyclovir.
v. Atypical facial pain Ø Constant dull aching pain , deep , diffuse variable intensity in absence of identifiable organic disease. Its more common in female. Ø Most patient middle age and elderly. Ø
v. Atypical facial pain Clinical features: Ø Ø Ø Ø Often difficult for pts to describe symptoms. described as deep , constant ache or burning. Doesn't awake patient. NO anatomical pattern and may be bilateral. Affect maxilla more than mandible. Often initiated or ↑ by dental treatment. PE entirely normal. Often have other complaints such as IBS , dry mouth and chronic pain syndrome.
v. Atypical facial pain treatment Often rewarded with limited response. Ø TAD have some effect in some pts. Ø 30% of pt. S respond to Gabapentine Ø Cognitive behavior therapy Ø
v. Atypical odontalgia (phantom) Most frequently in women in 4 TH, 5 TH of life, Ø Constant dull, aching pain without an apparent cause that can be detected by examination , Ø After dental extraction or endodontic treatment , Ø Period of pain free after 2 th dental management. Ø
-Management: patient reassurance , consultation to other specialty Ø -T. C. A. like amitriptyline , nortriptyline at low dose. 10 -25 mg at night Ø -Anti convulsant drugs. Ø
Burning mouth syndrome Burning sensation of oral mucosa , usually tongue, in absence of any identifiable clinical abnormality or cause. Epidemiology: 5 per 100, 000 , higher in middle age and elderly, affect female more than male. Causes: unknown but hormonal factors , anxiety , and stress have been implicated.
Clinical features: Complain of dry mouth with altered or bad taste. � Burning sensation affecting tongue , anterior palate and less common lips. � May be aggravated by certain foods. � Usually bilateral. � Doesn't awake patient. But may present at awaking � Examination entirely normal. �
v. Burning mouth syndrome Investigation: FBS , haematinics , swab for Candida. Treatment: Ø Ø Ø Reassurance. Avoidance of stimulating factors. Some patients may respond to TCA, SSRIs topical clonazepam, sucking and spitting 2 -month course alfa-lipoic acid. Cognitive behavior therapy.
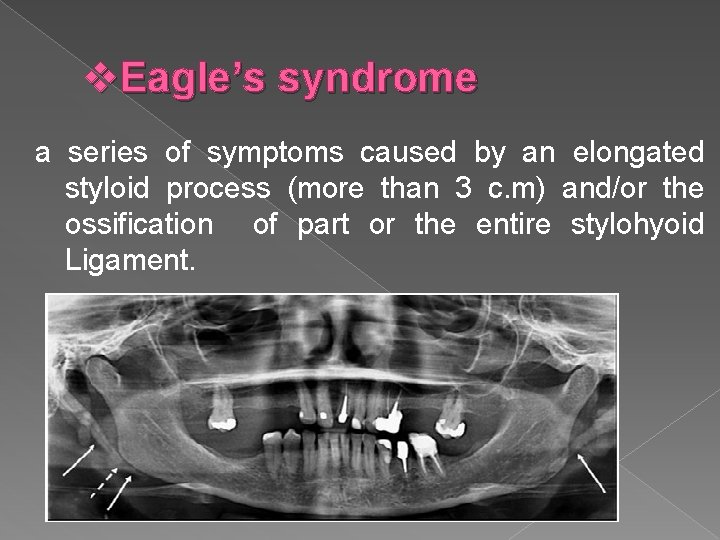
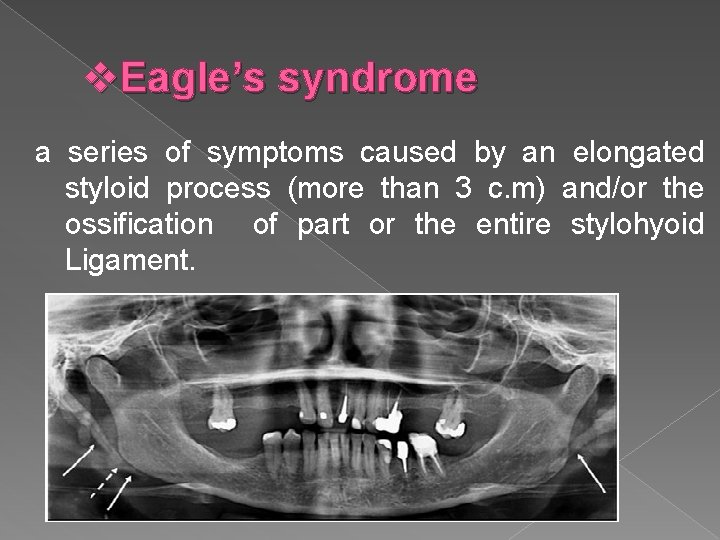
v. Eagle’s syndrome a series of symptoms caused by an elongated styloid process (more than 3 c. m) and/or the ossification of part or the entire stylohyoid Ligament.
v. Types of Eagles syndrome: 1 -Classic : the symptoms are persistent pharyngeal pain ↑ by swallowing & radiate to the ear , with sensation of foreign body within pharynx pain arise following tonsillectomy due to scar tissue around the tip of the styloid process.
2 - stylo-carotid artery syndrome(vascular): Attributed to impingement of the carotid artery by the styloid process This can cause a compression when turning the head resulting in a transient ischemic accident or stroke. 3 -Traumatic Eagle syndrome: in which symptoms develop after fracture of a mineralized stylohyoid ligament.

v. Diagnosis: (1)clinical manifestations, (2) digital palpation of the process in the tonsillar fossa, (3) radiological findings. (4) lidocaine infiltration test. v Treatment: Medical: NSAID & injecting steroids& anesthetics into the lesser cornu of the hyoid or tonsillar fossa Surgical: intra oral or extra oral styloidectomy
Migraine Before puberty , female > male. Ø Aura before headache in 40%. Ø may triggered by foods : nuts, chocolate, red wine , stress, sleep deprivation, hunger. Ø
Clinical manifestation: A-classic migraine (start with aura for 20 -30 min ) � Flashing lights Scotoma Sensitivity to light Sensory and motor deficit Aura followed by severe unilateral throbbing pain. � Headaches may last for hours or up to 2 or 3 days. � � B-common migraine (not preceded by aura) Severe unilateral throbbing pain � Sensitivity to light and noise � Nausea and vomiting �
C-facial migraine(carotidynia): � � � 30 -50 years of age. Pain last for minutes to hours and recurs several times per week. Throbbing pain of neck and jaw. Patients often seek dental consultation, Tenderness of carotid artery D-Basilar migraine : The symptoms are primarily neurologic and include aphasia, temporary blindness, vertigo, confusion, and ataxia. � may be accompanied by an occipital headache. �
Migraine treatment Avoid trigger factors v Acute attack: analgesics, Sumatriptan , ergotamin. v v Prophylaxis : pizotifen , propranolol , ca channel blockers. TCAs
Cluster headache Clinical Manifestations: � � � 80%of pts with CH are men. The attacks are sudden, unilateral, stabbing , causing pts to pace, cry out, or even strike objects. Some exhibit violent behavior in attacks. pain as a hot metal rod in or around the eye. attack lasts from 15 min to 2 hrs & recurs several times daily. A majority of episodes at night, awaking the pts.
Cluster headache Clinical Manifestations: pain with nasal congestion, tearing, Sweating of the face, ptosis, ↑ salivation, edema of the eyelid. � pain in posterior maxilla that mimic dental pain. � Trigger by alcohol. �
CH treatment Ø An acute attack: 100% oxygen (its effectiveness is diagnostic), Injection of sumatriptan or sublingual or inhaled ergotamine Ø Prophylaxis : lithium, ergotamine, prednisone, and calcium channel blockers.
Chronic Paroxysmal Hemicrania Ø A form of CH that occurs predominantly in women between 30 - 40 years. Ø The episodes of pain tend be shorter, but attacks of 5 to 20 min, can occur up to 30 times daily. Ø It responds dramatically to indomethacin , which stops the attacks within 1 to 2 days.
v. Temporal Arteritis -Its inflammation(vasculitis) of cranial arteries due to to giant cell arteritis Clinical features: Ø most frequently affects adults > 50 years. Dull aching or throbbing temporal pain with generalized symptoms : fever, malaise, ↓ appetite. Ø Jaw claudication during mastication. Ø
v. Temporal Arteritis Diagnosis: Ø elevated ESR 50 -100. Ø elevated CRP. Ø Biopsy. -Treatment: Ø high dose of steroid(prednisolone) Ø the steroid is tapered once the signs of the disease are controlled. Ø Patients are maintained on systemic steroids for 1 to 2 years after symptoms resolve.

Thanks for Your Attention

 Pain x mad
Pain x mad How to know if your period is coming or your pregnant
How to know if your period is coming or your pregnant Period vs pregnancy symptoms
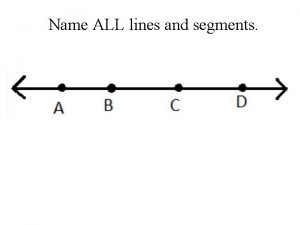
Period vs pregnancy symptoms Draw three noncollinear points j k and l
Draw three noncollinear points j k and l God understands our pain
God understands our pain Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worms-breton
Tư thế worms-breton Chúa sống lại
Chúa sống lại Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Các số nguyên tố là gì
Các số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Our god is an awesome god vine
Our god is an awesome god vine Our god is an awesome god he reigns
Our god is an awesome god he reigns God is an awesome god and greatly to be praised
God is an awesome god and greatly to be praised God is good god is great speed
God is good god is great speed O god you are my god earnestly i seek you
O god you are my god earnestly i seek you God-given virtues that direct us to our loving, triune god.
God-given virtues that direct us to our loving, triune god. Justice new testament
Justice new testament My god's bigger than your god
My god's bigger than your god Using god's name in vain meaning
Using god's name in vain meaning God's covenant
God's covenant Oh lord my lord how excellent is thy name
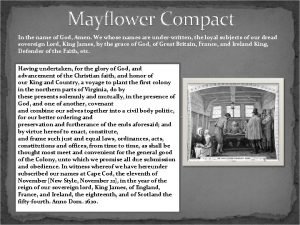
Oh lord my lord how excellent is thy name In the name of god amen mayflower compact
In the name of god amen mayflower compact In the name of god, most gracious, most merciful prayer
In the name of god, most gracious, most merciful prayer 馮定華
馮定華 Hermes roman name
Hermes roman name In the name of god the beneficent the merciful
In the name of god the beneficent the merciful In the name of god the beneficent the merciful
In the name of god the beneficent the merciful The most gracious
The most gracious God of secrets name
God of secrets name