DIFFERENTIAL DIAGNOSIS OF SOLITARY NODULE THYROID DENIS MATHEWS






















- Slides: 96
DIFFERENTIAL DIAGNOSIS OF SOLITARY NODULE THYROID DENIS MATHEWS 2002 BATCH ROLL: 24
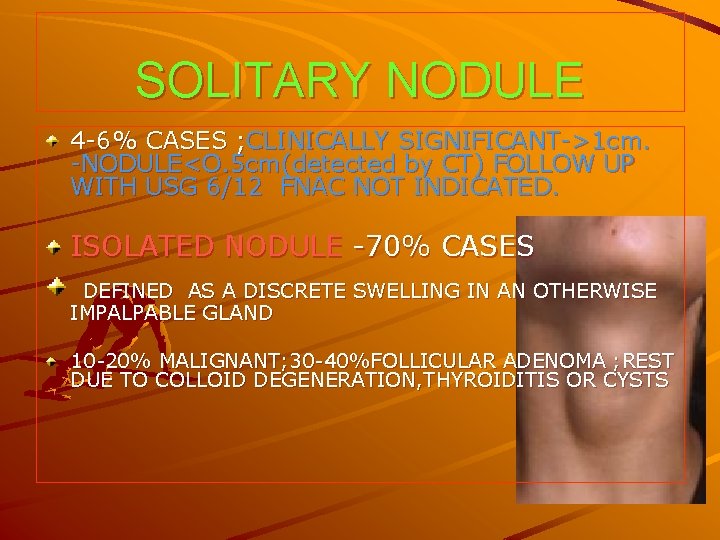
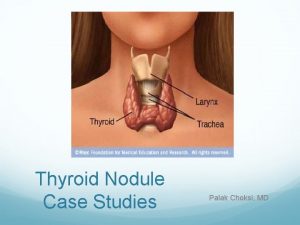
SOLITARY NODULE 4 -6% CASES ; CLINICALLY SIGNIFICANT->1 cm. -NODULE<O. 5 cm(detected by CT) FOLLOW UP WITH USG 6/12 FNAC NOT INDICATED. ISOLATED NODULE -70% CASES DEFINED AS A DISCRETE SWELLING IN AN OTHERWISE IMPALPABLE GLAND 10 -20% MALIGNANT; 30 -40%FOLLICULAR ADENOMA ; REST DUE TO COLLOID DEGENERATION, THYROIDITIS OR CYSTS
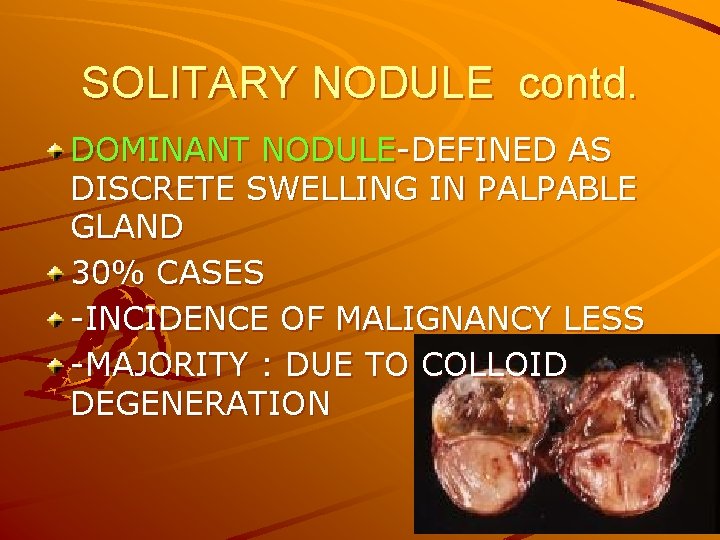
SOLITARY NODULE contd. DOMINANT NODULE-DEFINED AS DISCRETE SWELLING IN PALPABLE GLAND 30% CASES -INCIDENCE OF MALIGNANCY LESS -MAJORITY : DUE TO COLLOID DEGENERATION

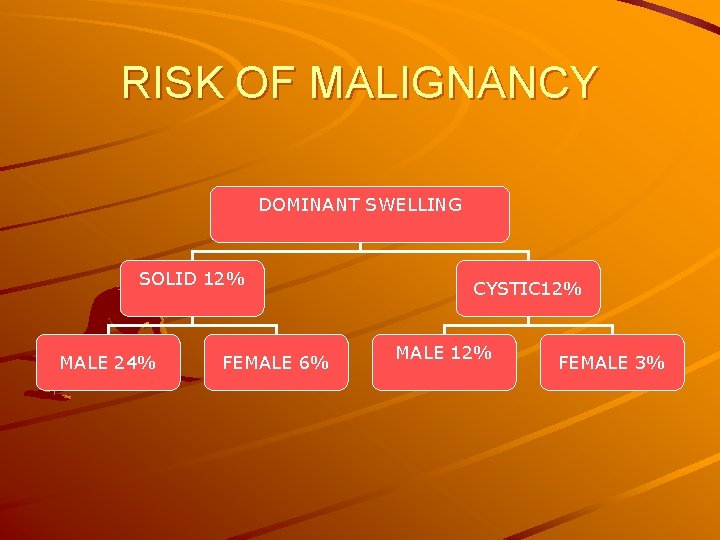
RISK OF MALIGNANCY IN SNT RULE OF 12 –CANCER IN SNT EXPRESSED AS FACTOR OF 12. RISK GREATOR IN ISOLATED , SOLID NODULE ; MORE IN MEN ISOLATED THYROID SWELLING SOLID 24% MALE 48% FEMALE 12% CYSTIC 12% MALE 24% FEMALE 6%
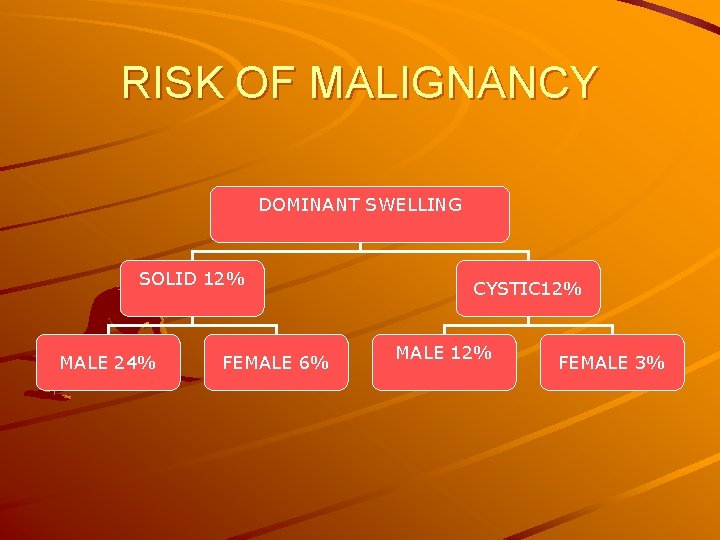
RISK OF MALIGNANCY DOMINANT SWELLING SOLID 12% MALE 24% FEMALE 6% CYSTIC 12% MALE 12% FEMALE 3%
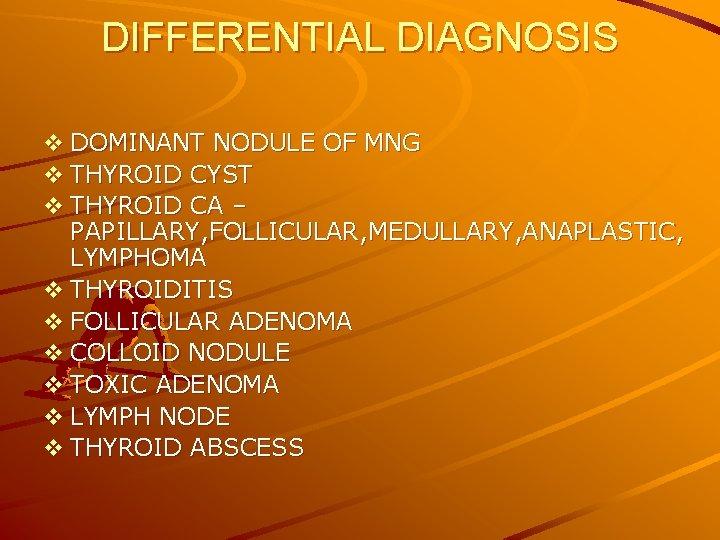
DIFFERENTIAL DIAGNOSIS v DOMINANT NODULE OF MNG v THYROID CYST v THYROID CA – PAPILLARY, FOLLICULAR, MEDULLARY, ANAPLASTIC, LYMPHOMA v THYROIDITIS v FOLLICULAR ADENOMA v COLLOID NODULE v TOXIC ADENOMA v LYMPH NODE v THYROID ABSCESS
CLINICAL EVALUATION DETAILED HISTORY: SNT COMMON IN FEMALES NODULE IN CHILD, ADULT MALE OVER 40 yrs, FEMALE OVER 50 yrs LIKELY TO BE MALIGNANT RAPIDLY INCREASING-MALIGNANT D/DHGE INTO NODULE H/O IRRADIATION TO HEAD&NECK, FAMILY HISTORY 15% SNT -MALIGNANT
PHYSICAL EXAMINATION DETERMINE WHETHER ISOLATED OR DOMINANT FEATURES OF MALIGNANCY: @HARD NODULE @IRREGULAR SURFACE @ FIXITY TO SURROUNDING STRUCTURES @PALPABLE CERVICAL NODULE @REC. LARYNGEAL N PALSY @SYMPTOMS: DYSNOEA, DYSPHAGIA, HOARS ENESS, HORNERS SYND

INVESTIGATION IN SNT TFT –TSH , T 3, T 4 ASSESSED IF TSH normal: DO FNAC IF TSH LOW&T 3, T 4 HIGH –TOXIC ADENOMA TOXICITY&NODULARITY-THYROIDSCAN THROID SCAN-3 findings hot nodule-takes more isotope than surrounding 5% (4%MALIGNANT) warm nodule-takes isotope similar to surrounding-10 -15%(9%MALIGNANT) cold nodule-does not take isotope -85%-(10 -15% MALIGNANT) AUTO ANTIBODY TITRE-C/C LYMPHOCYTIC THYROIDITIS ; ABSENT IN GRANULOMATOUS THYROIDITIS SERUM CALCIUM&PHOSPHOROUS-PARATYHROID FN
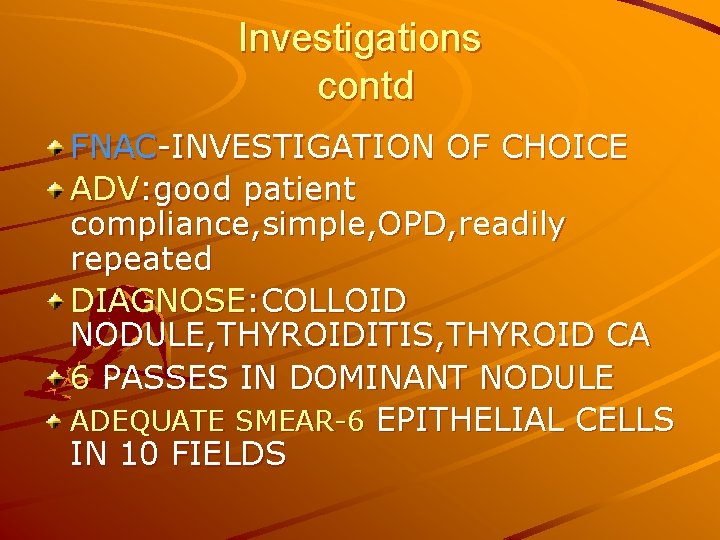
Investigations contd FNAC-INVESTIGATION OF CHOICE ADV: good patient compliance, simple, OPD, readily repeated DIAGNOSE: COLLOID NODULE, THYROIDITIS, THYROID CA 6 PASSES IN DOMINANT NODULE ADEQUATE SMEAR-6 EPITHELIAL CELLS IN 10 FIELDS
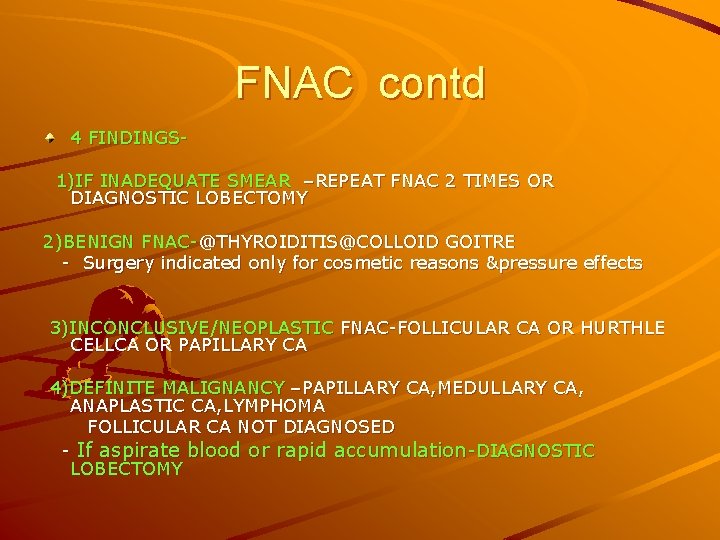
FNAC contd 4 FINDINGS 1)IF INADEQUATE SMEAR –REPEAT FNAC 2 TIMES OR DIAGNOSTIC LOBECTOMY 2)BENIGN FNAC-@THYROIDITIS@COLLOID GOITRE - Surgery indicated only for cosmetic reasons &pressure effects 3)INCONCLUSIVE/NEOPLASTIC FNAC-FOLLICULAR CA OR HURTHLE CELLCA OR PAPILLARY CA 4)DEFINITE MALIGNANCY –PAPILLARY CA, MEDULLARY CA, ANAPLASTIC CA, LYMPHOMA FOLLICULAR CA NOT DIAGNOSED - If aspirate blood or rapid accumulation-DIAGNOSTIC LOBECTOMY
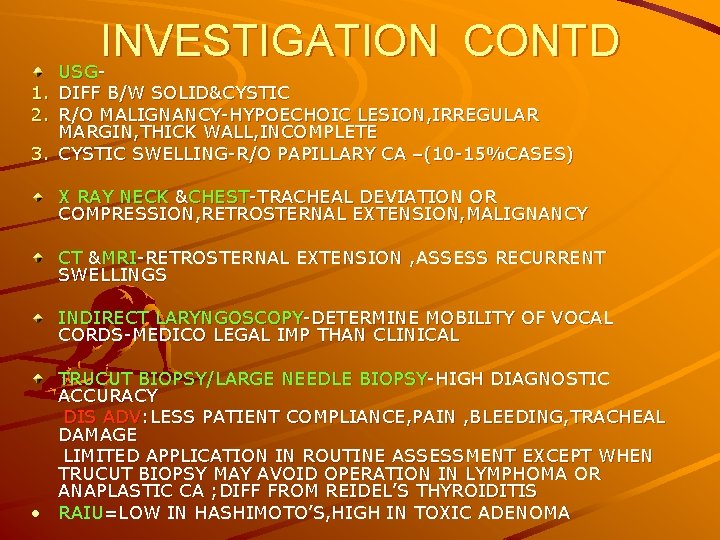
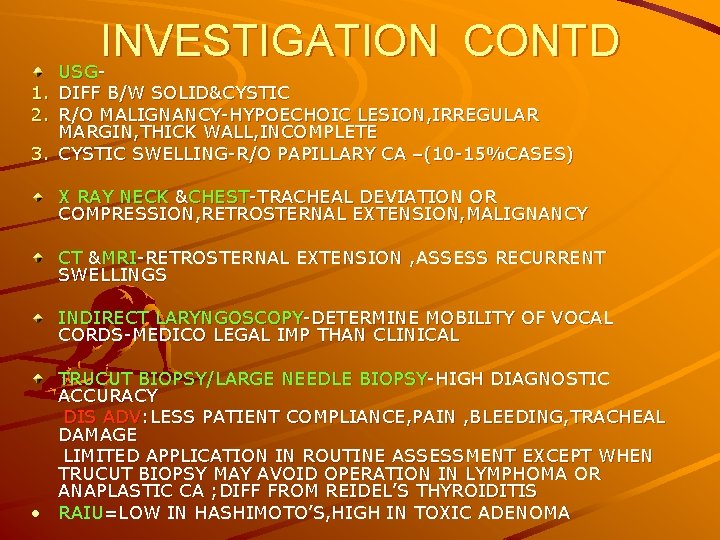
INVESTIGATION CONTD USG- 1. DIFF B/W SOLID&CYSTIC 2. R/O MALIGNANCY-HYPOECHOIC LESION, IRREGULAR MARGIN, THICK WALL, INCOMPLETE 3. CYSTIC SWELLING-R/O PAPILLARY CA –(10 -15%CASES) X RAY NECK &CHEST-TRACHEAL DEVIATION OR COMPRESSION, RETROSTERNAL EXTENSION, MALIGNANCY CT &MRI-RETROSTERNAL EXTENSION , ASSESS RECURRENT SWELLINGS INDIRECT LARYNGOSCOPY-DETERMINE MOBILITY OF VOCAL CORDS-MEDICO LEGAL IMP THAN CLINICAL TRUCUT BIOPSY/LARGE NEEDLE BIOPSY-HIGH DIAGNOSTIC ACCURACY DIS ADV: LESS PATIENT COMPLIANCE, PAIN , BLEEDING, TRACHEAL DAMAGE LIMITED APPLICATION IN ROUTINE ASSESSMENT EXCEPT WHEN TRUCUT BIOPSY MAY AVOID OPERATION IN LYMPHOMA OR ANAPLASTIC CA ; DIFF FROM REIDEL’S THYROIDITIS • RAIU=LOW IN HASHIMOTO’S, HIGH IN TOXIC ADENOMA
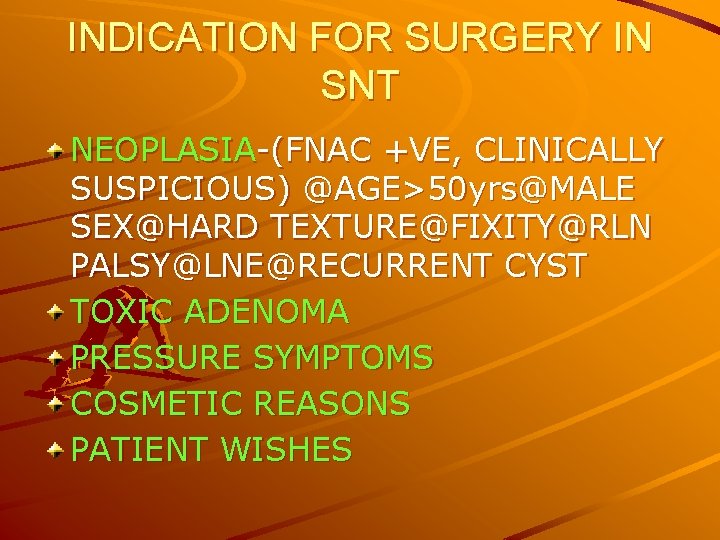
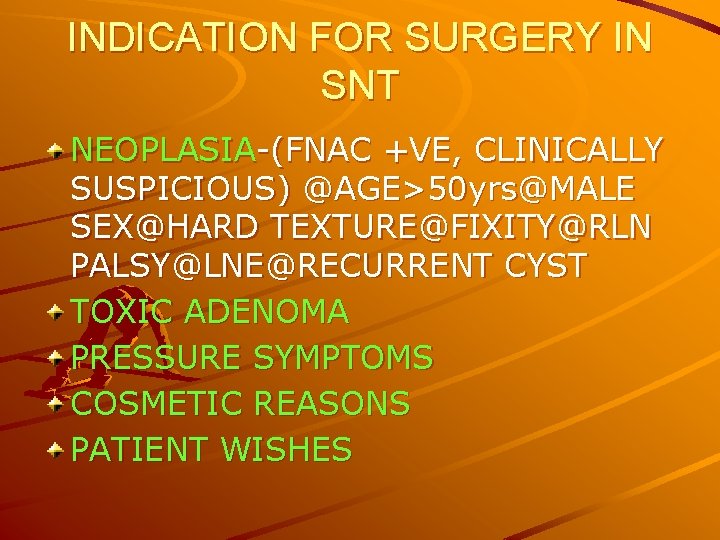
INDICATION FOR SURGERY IN SNT NEOPLASIA-(FNAC +VE, CLINICALLY SUSPICIOUS) @AGE>50 yrs@MALE SEX@HARD TEXTURE@FIXITY@RLN PALSY@LNE@RECURRENT CYST TOXIC ADENOMA PRESSURE SYMPTOMS COSMETIC REASONS PATIENT WISHES
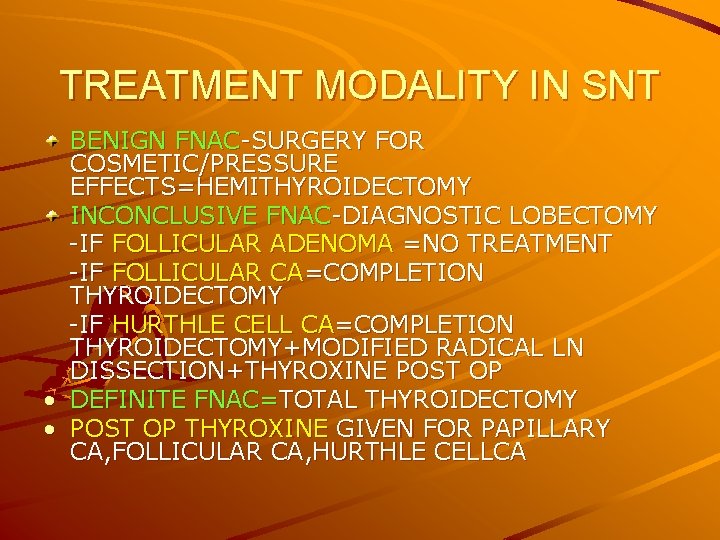
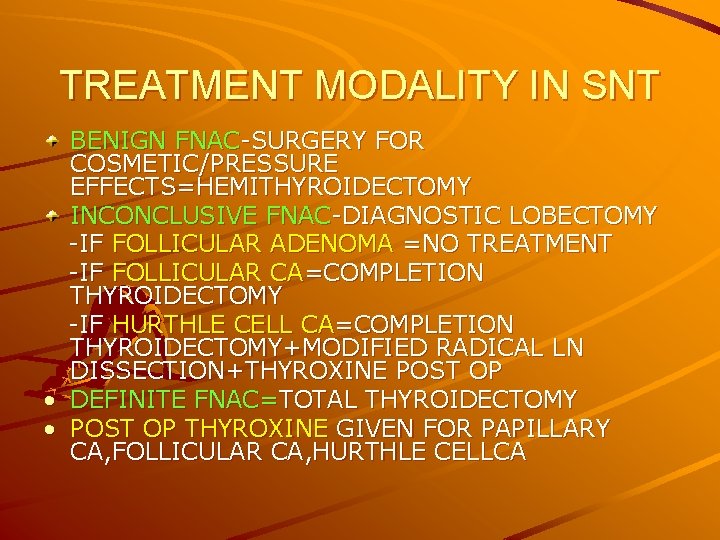
TREATMENT MODALITY IN SNT BENIGN FNAC-SURGERY FOR COSMETIC/PRESSURE EFFECTS=HEMITHYROIDECTOMY INCONCLUSIVE FNAC-DIAGNOSTIC LOBECTOMY -IF FOLLICULAR ADENOMA =NO TREATMENT -IF FOLLICULAR CA=COMPLETION THYROIDECTOMY -IF HURTHLE CELL CA=COMPLETION THYROIDECTOMY+MODIFIED RADICAL LN DISSECTION+THYROXINE POST OP • DEFINITE FNAC=TOTAL THYROIDECTOMY • POST OP THYROXINE GIVEN FOR PAPILLARY CA, FOLLICULAR CA, HURTHLE CELLCA

DOMINANT NODULE OF MNG v FEMALE: MALE=8: 1 v CLINICALLY PRESENT AS NECK MASS; MOVES UP ON DEGLUTTION; DOES NOT MOVE ON PROTRUSION OF TONGUE; SUDDEN PAIN IN NECK WITH INCREASE IN SIZE OF THYROID DUE TO H’GE v <5%CHANCE OF MALIGNANCY EXCEPT-FAMILY HISTORY, H/O IRRADIATION v ENDEMIC VARIETY COMMON v Grossly; Assymetric &EXTREMELY ENLARGED v CUT SECTION; @NODULARITY&POOR ENCAPSULATION @FIBROUS SCARRING @HAEMORRAGES @FOCAL CALCIFICATION @CYSTIC DEGENERATION

DOMINANT NODULE OF MNG MICROSCOPY; @PARTIAL OR INCOMPLETE ENCAPSULATION @FOLLICLES CONTAIN COLLOID &LINED BY FLAT EPITHELIUM @AREAS OF H”GE @FIBROUS SCARRING &FOCI OF CALCIFICATION
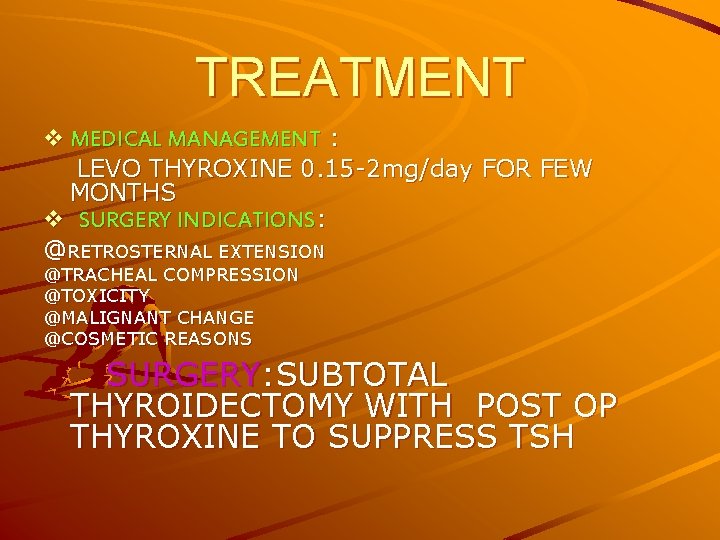
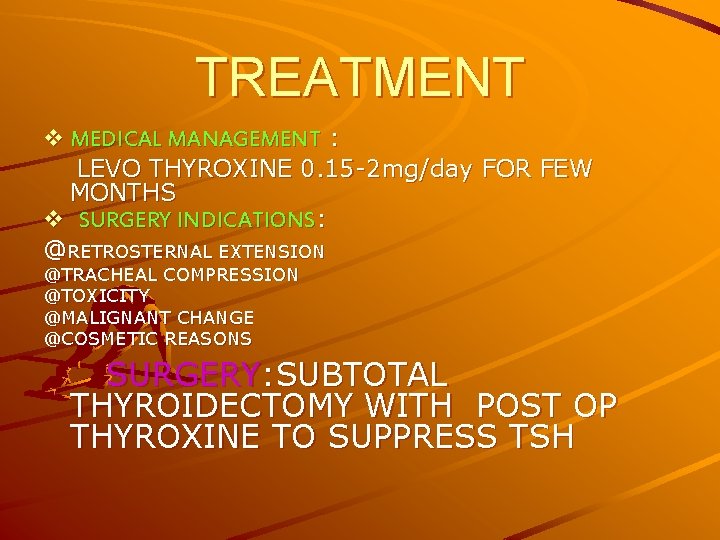
TREATMENT v MEDICAL MANAGEMENT : LEVO THYROXINE 0. 15 -2 mg/day FOR FEW MONTHS v SURGERY INDICATIONS: @RETROSTERNAL EXTENSION @TRACHEAL COMPRESSION @TOXICITY @MALIGNANT CHANGE @COSMETIC REASONS SURGERY: SUBTOTAL THYROIDECTOMY WITH POST OP THYROXINE TO SUPPRESS TSH
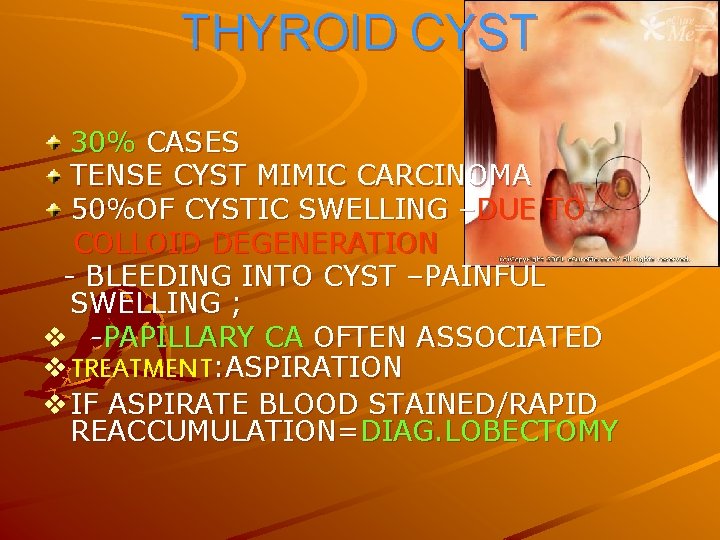
THYROID CYST 30% CASES TENSE CYST MIMIC CARCINOMA 50%OF CYSTIC SWELLING –DUE TO COLLOID DEGENERATION - BLEEDING INTO CYST –PAINFUL SWELLING ; v -PAPILLARY CA OFTEN ASSOCIATED v TREATMENT: ASPIRATION v IF ASPIRATE BLOOD STAINED/RAPID REACCUMULATION=DIAG. LOBECTOMY
THYROID CARCINOMA PAPILLARY CA FOLLICULAR CA MEDULLARY CA ANAPLASTIC CA THYROID LYMPHOMA
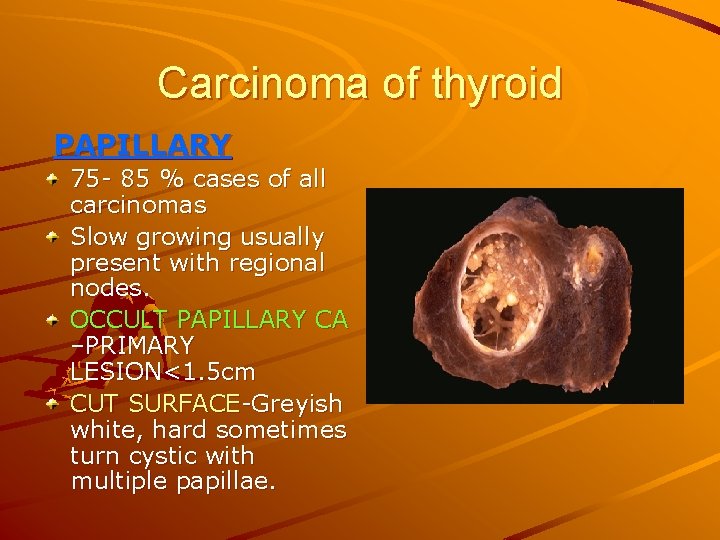
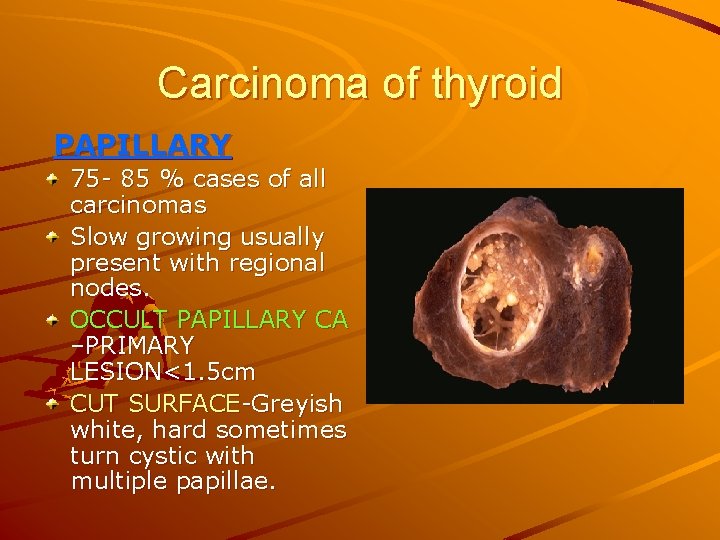
Carcinoma of thyroid PAPILLARY 75 - 85 % cases of all carcinomas Slow growing usually present with regional nodes. OCCULT PAPILLARY CA –PRIMARY LESION<1. 5 cm CUT SURFACE-Greyish white, hard sometimes turn cystic with multiple papillae.

Papillary carcinoma MICROSCOPY-Papillae has fibrovascular core and covered by tumor cells Tumour cells – clear or oxyphilic cytoplasm & overlapping pale nuclei. (ground glass appearance) “Orphan Annie nuclei” – Uniformly light blue staining round cells with a dense nucleus and clear cytoplasm INVADES thyroid capsule and intra thyroid lymphatics Typical feature –Psammoma bodies – Small concentric calcified spherules
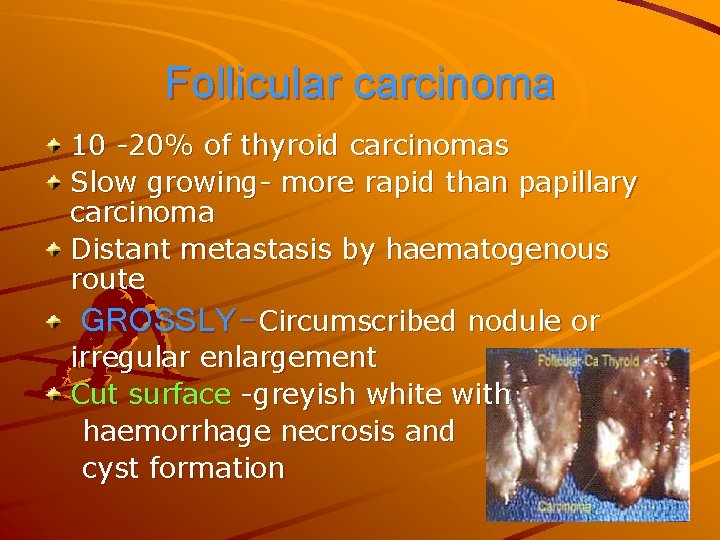
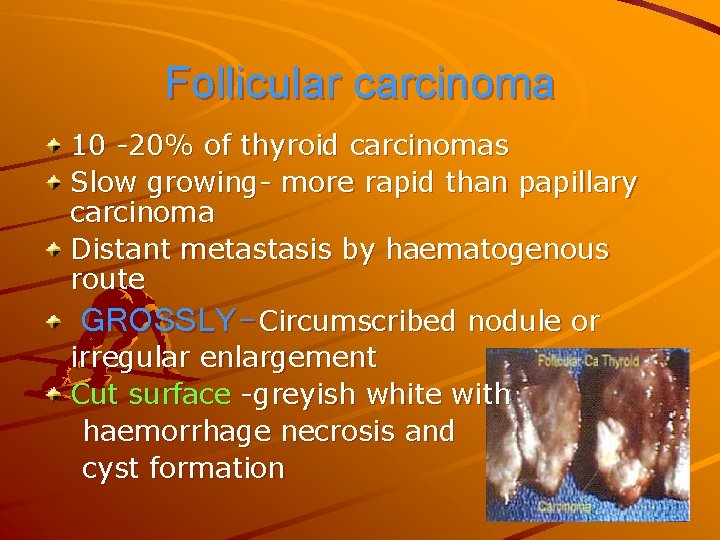
Follicular carcinoma 10 -20% of thyroid carcinomas Slow growing- more rapid than papillary carcinoma Distant metastasis by haematogenous route GROSSLY-Circumscribed nodule or irregular enlargement Cut surface -greyish white with haemorrhage necrosis and cyst formation
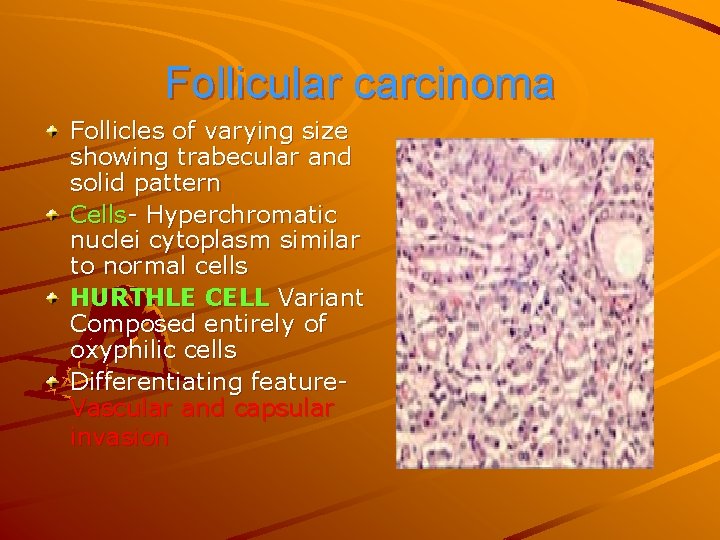
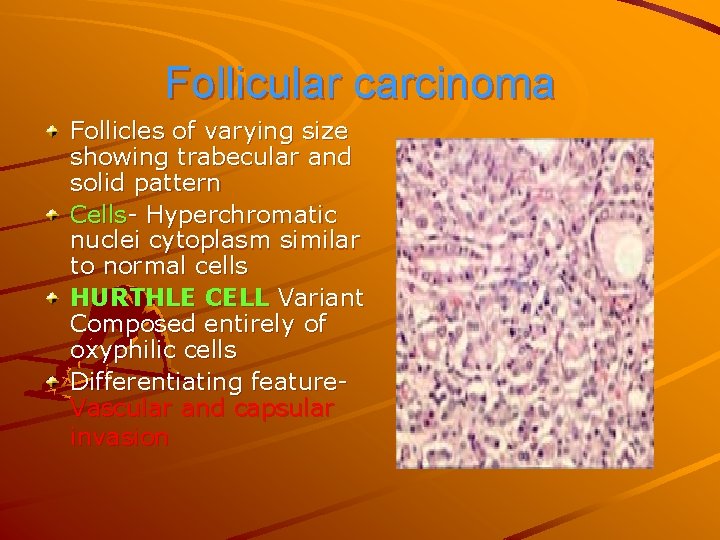
Follicular carcinoma Follicles of varying size showing trabecular and solid pattern Cells- Hyperchromatic nuclei cytoplasm similar to normal cells HURTHLE CELL Variant Composed entirely of oxyphilic cells Differentiating feature. Vascular and capsular invasion
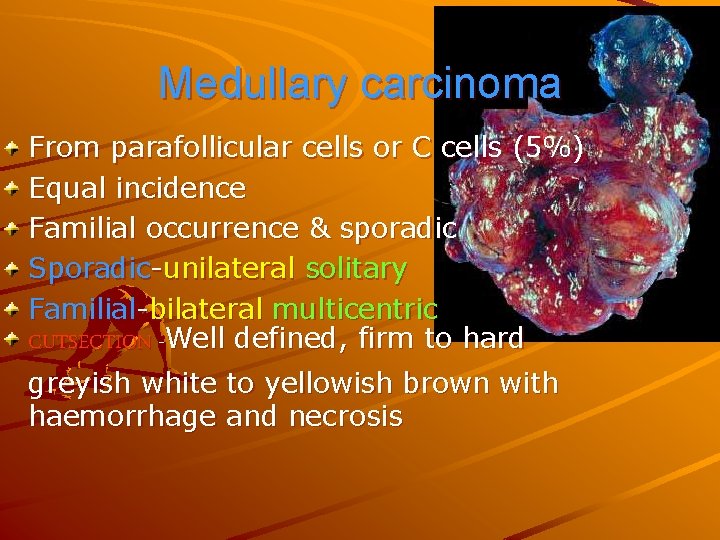
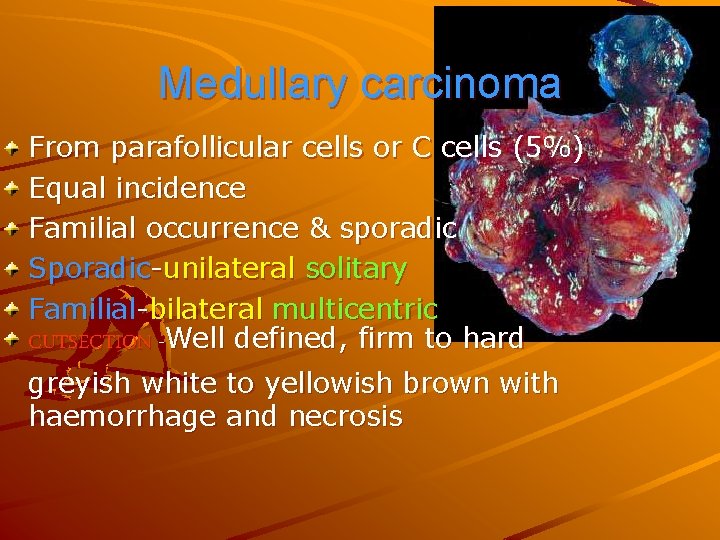
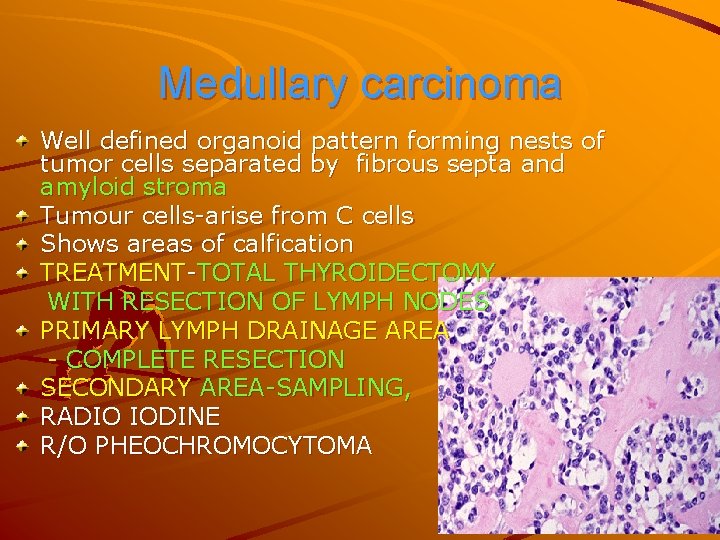
Medullary carcinoma From parafollicular cells or C cells (5%) Equal incidence Familial occurrence & sporadic Sporadic-unilateral solitary Familial-bilateral multicentric CUTSECTION -Well defined, firm to hard greyish white to yellowish brown with haemorrhage and necrosis
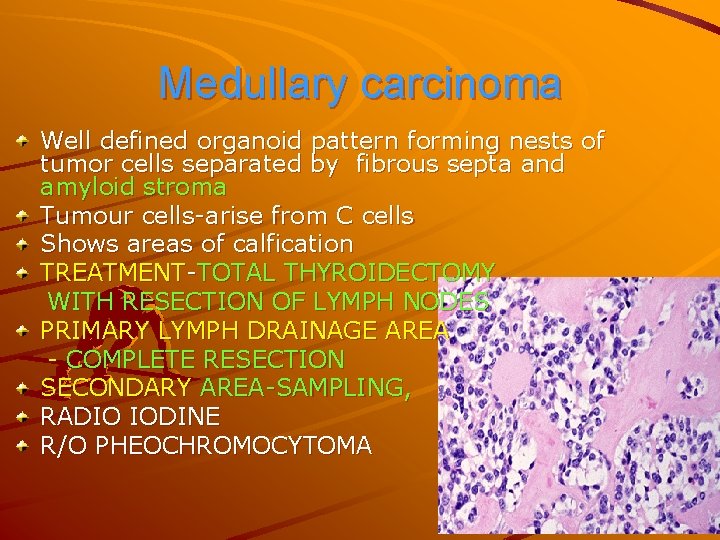
Medullary carcinoma Well defined organoid pattern forming nests of tumor cells separated by fibrous septa and amyloid stroma Tumour cells-arise from C cells Shows areas of calfication TREATMENT-TOTAL THYROIDECTOMY WITH RESECTION OF LYMPH NODES PRIMARY LYMPH DRAINAGE AREA - COMPLETE RESECTION SECONDARY AREA-SAMPLING, RADIO IODINE R/O PHEOCHROMOCYTOMA

Anaplastic carcinoma Most malignant tumour Aggressive and rapidly growing with extensive invasion GROSSLY-White and firm invading adjacent structures of neck CUT SECTION-Areas of necrosis and hemorrhage Poorly differentiated Contains three cell types
Anaplastic carcinoma VARIANTS Small cell carcinoma - Closely packed small cells with hyperchromatic nuclei and numerous mitoses Spindle cell carcinoma - Resembling sarcoma Giant cell carcinoma - Highly anaplastic giant cells showing numerous atypical mitoses & lobed nuclei with some spindle cells.
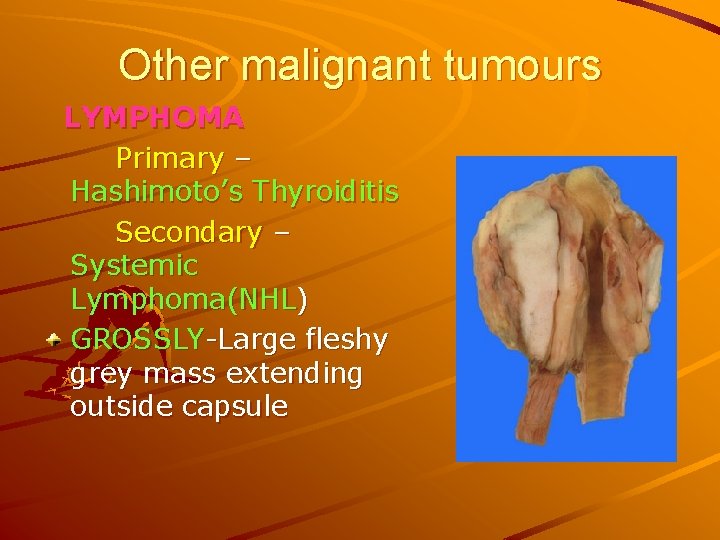
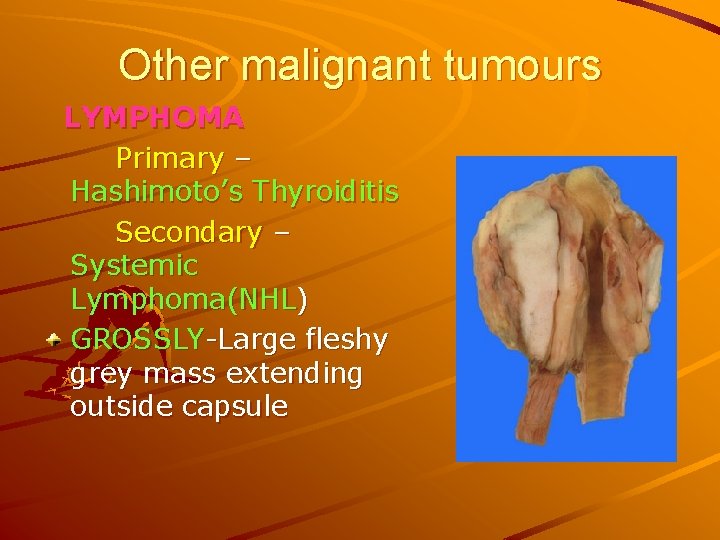
Other malignant tumours LYMPHOMA Primary – Hashimoto’s Thyroiditis Secondary – Systemic Lymphoma(NHL) GROSSLY-Large fleshy grey mass extending outside capsule
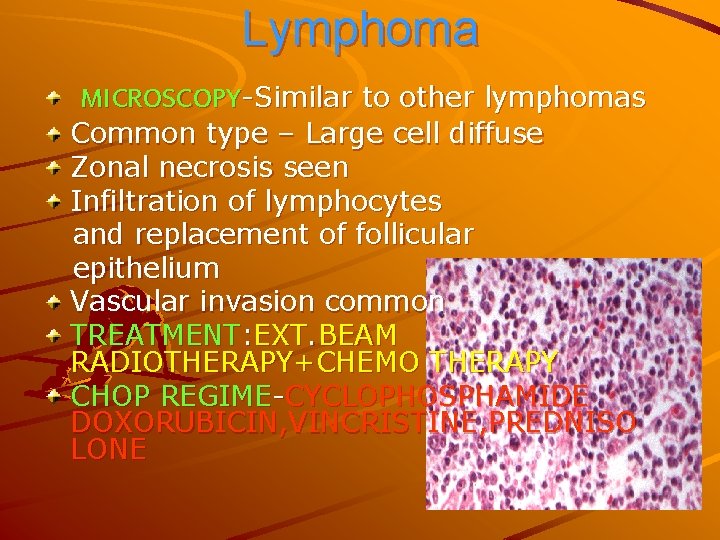
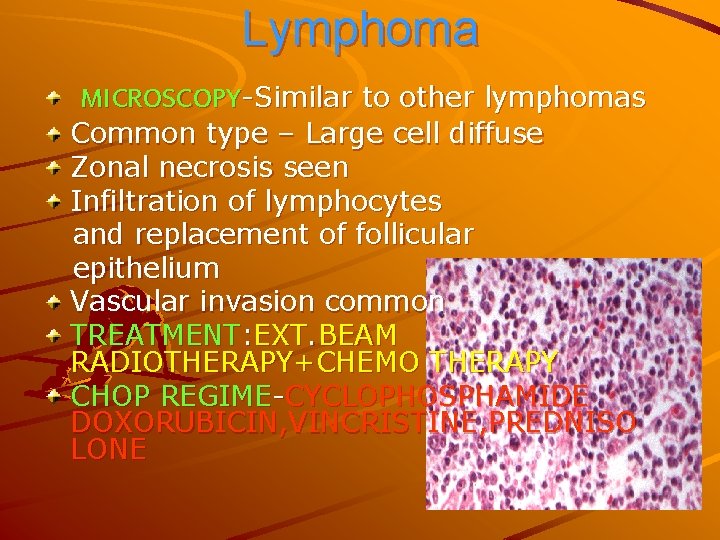
Lymphoma MICROSCOPY-Similar to other lymphomas Common type – Large cell diffuse Zonal necrosis seen Infiltration of lymphocytes and replacement of follicular epithelium Vascular invasion common TREATMENT: EXT. BEAM RADIOTHERAPY+CHEMO THERAPY CHOP REGIME-CYCLOPHOSPHAMIDE DOXORUBICIN, VINCRISTINE, PREDNISO LONE
Metastatic tumours of thyroid Direct spread – Larynx, Pharynx, Trachea, Oesophagus Haematogenous spread –from bronchogenic ca, malignant melanoma, renal cell ca Most common metastatic tumourhypernephroma Retrograde lymphatic flow from cervical nodes Solitary circumscribed mass Histology resembles to primary tumour
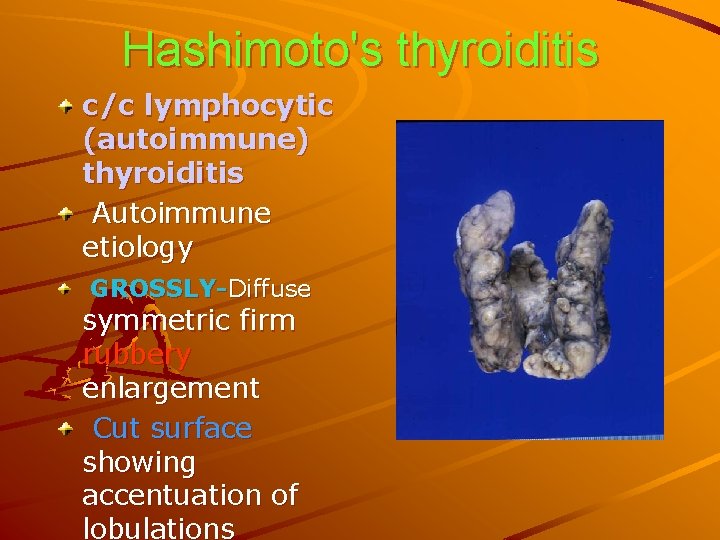
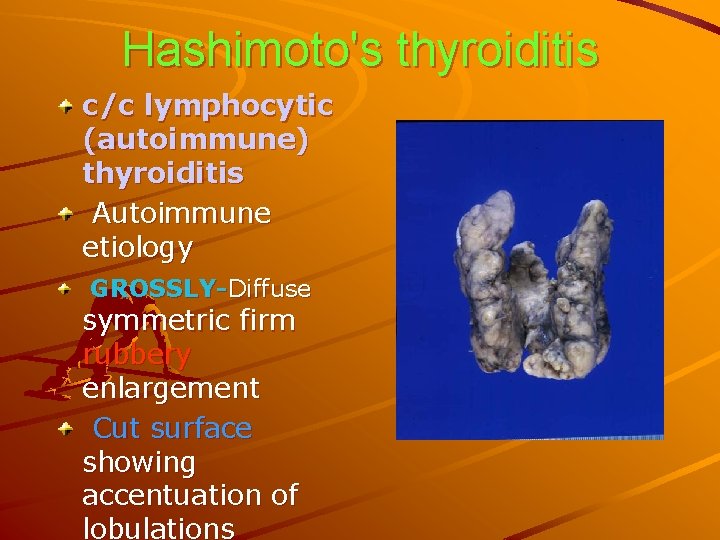
Hashimoto's thyroiditis c/c lymphocytic (autoimmune) thyroiditis Autoimmune etiology GROSSLY-Diffuse symmetric firm rubbery enlargement Cut surface showing accentuation of lobulations

Hashimoto's thyroiditis MICRO-extensive mononuclear inflammatory infiltrate well developed germinal centre atrophic thyroid follicles Hurthle cells or Askanzy or oxyphil Increased interstitial fibrous tissue TREATMRNT: throxine for hypothyroidism SURGERY FOR PRESSURE SYMPTOMS: SUB TOTAL THYROIDECTOMY IF CA SUSPECTED-INITIAL LOBECTOMY. IF CA CONFIRMED-NEAR TOTAL THYROIDECTOMY
Infectious thyroiditis Seen in malnourished, debiliated & immunocompromised individuals Bacterial, fungal (candida, aspergillus, cryptococcus), mycobacteria, spirochaetes, parasites etc. Direct extension from head & neck or haematogenous or lymphatic CUT SECTION-Diffuse or focally softened areas with microabscesses & necrosed areas containing microorganism FNAC : REVEALS PUS TREATMENT: DRAINAGE OF PUS&ANTIBIOTICS
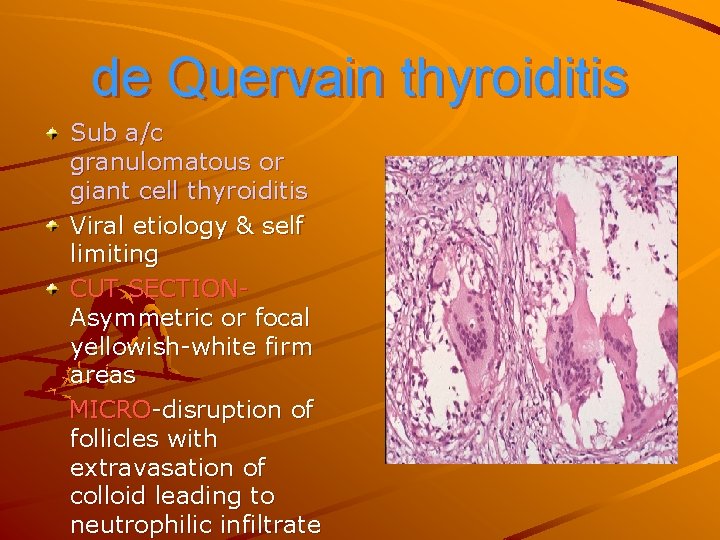
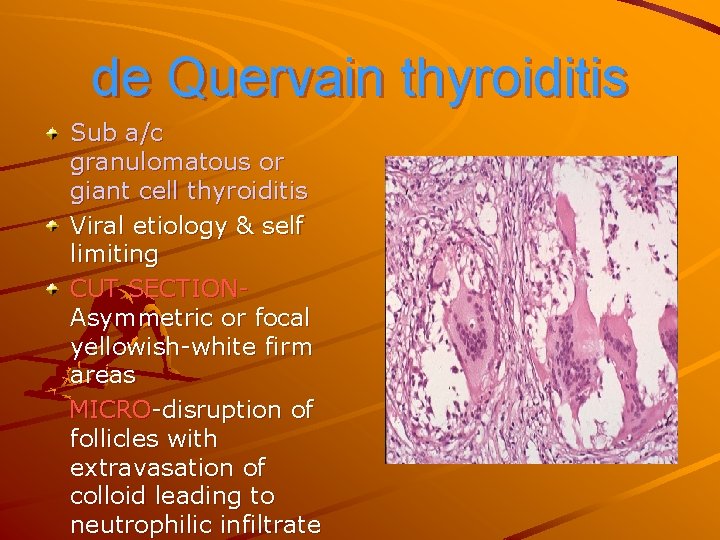
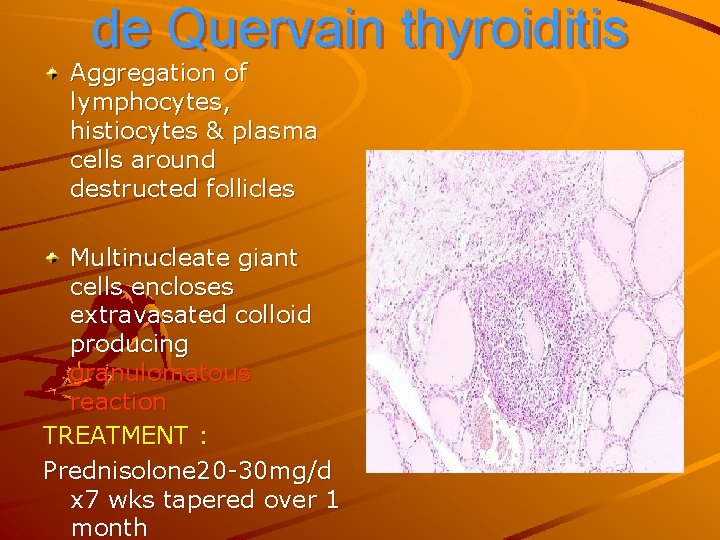
de Quervain thyroiditis Sub a/c granulomatous or giant cell thyroiditis Viral etiology & self limiting CUT SECTIONAsymmetric or focal yellowish-white firm areas MICRO-disruption of follicles with extravasation of colloid leading to neutrophilic infiltrate
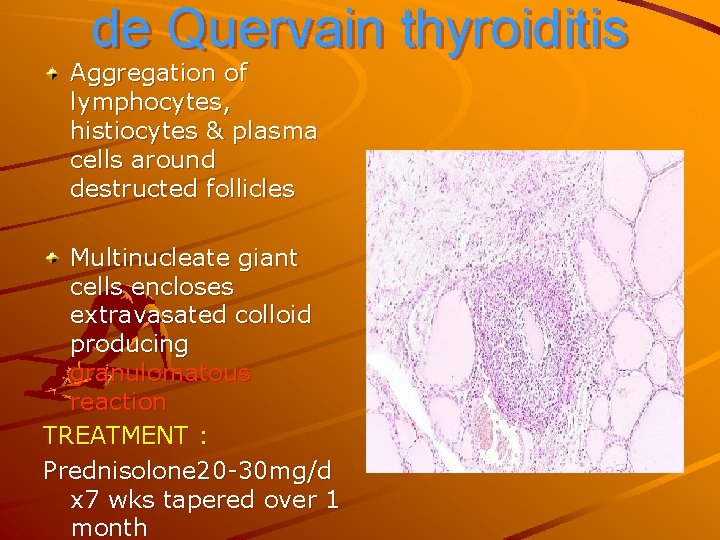
de Quervain thyroiditis Aggregation of lymphocytes, histiocytes & plasma cells around destructed follicles Multinucleate giant cells encloses extravasated colloid producing granulomatous reaction TREATMENT : Prednisolone 20 -30 mg/d x 7 wks tapered over 1 month
Riedel’s thyroiditis Invasive fibrous thyroiditis or Riedel`s struma Resembles thyroid cancer Stony hard thyroid mass adherent to surrounding neck structures Extensive fibrocollagenous replacement with atrophy of parenchyma Focally shattered lymphocytic infiltration TREATMENT: THYROXINE REPLACEMENT HIGH DOSE STEROIDS
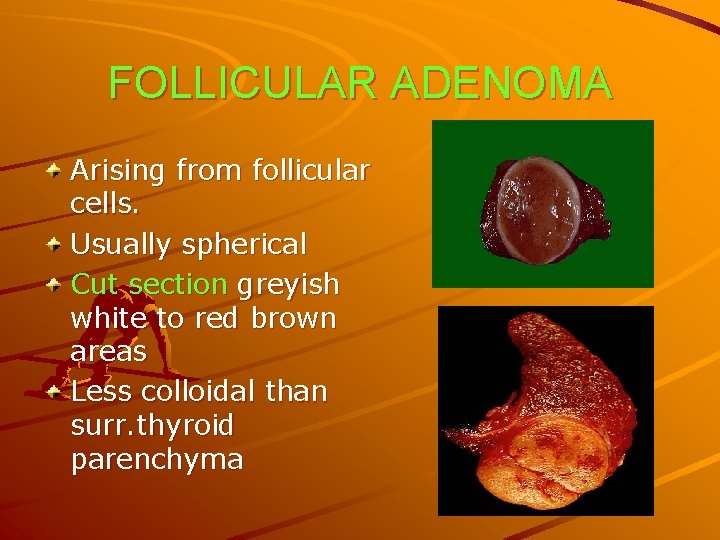
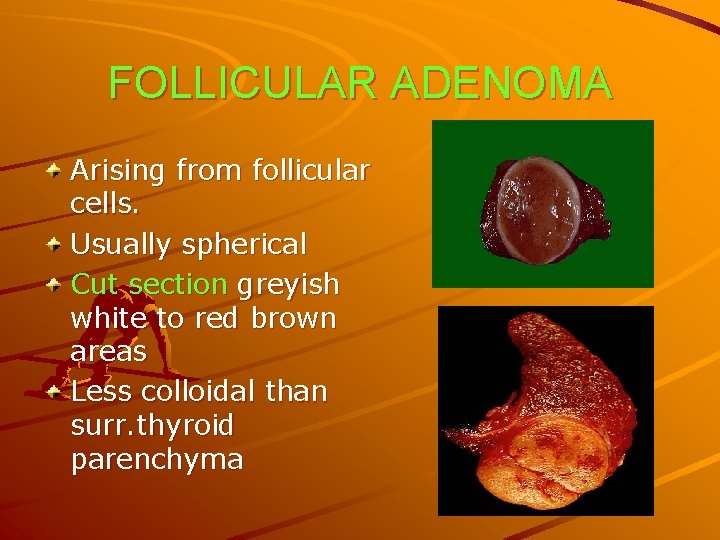
FOLLICULAR ADENOMA Arising from follicular cells. Usually spherical Cut section greyish white to red brown areas Less colloidal than surr. thyroid parenchyma
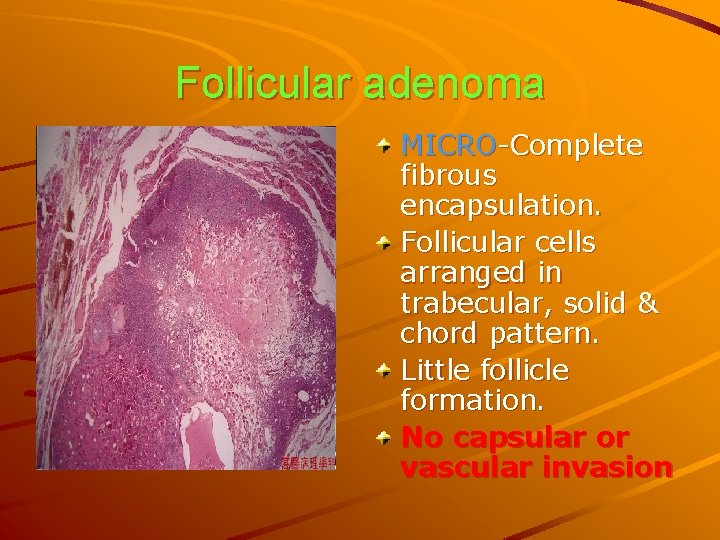
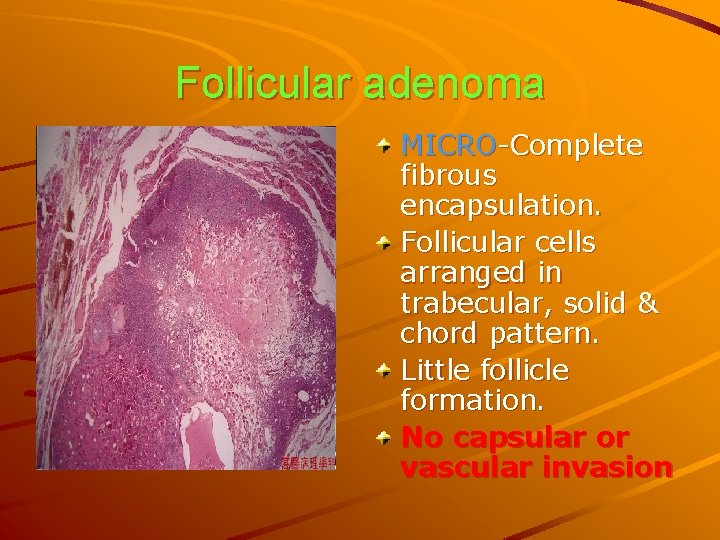
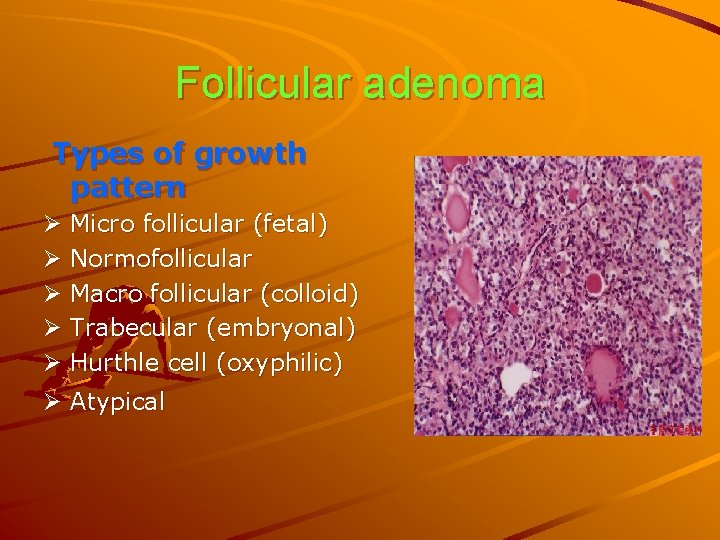
Follicular adenoma MICRO-Complete fibrous encapsulation. Follicular cells arranged in trabecular, solid & chord pattern. Little follicle formation. No capsular or vascular invasion
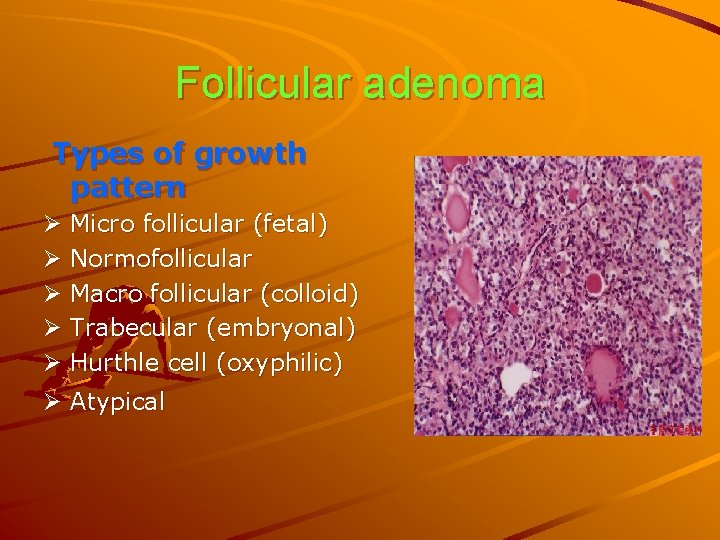
Follicular adenoma Types of growth pattern Ø Micro follicular (fetal) Ø Normofollicular Ø Macro follicular (colloid) Ø Trabecular (embryonal) Ø Hurthle cell (oxyphilic) Ø Atypical

COLLOID NODULE FEMALES COMMON ENDEMIC VARIETY COMMON Grossly; MODERATELY ENLARGED NODULE Cutsection; GELATINOUS&TRANSLUCENT Microscopy; LARGE FOLLICLE DISTENDED BY COLLOID&LINED BY FLATTENED EPITHELIUM RX-SURGERY ONLY FOR COSMETIC/PRESSURE EFFECTS

TOXIC ADENOMA COLLOID NODULE WITH HYPERPLASIA PRESENT AS SOLITARY NODULE >3 cm&FEATURES OF THYROTOXICOSIS MICROSCOPY; HYPERPLASIA OF ACINI LINED BY COLUMNAR EPITHELIUM SOME EMPTY &SOME CONTAIN VACUOLATED COLLOID WITH CHARACTERISTIC SCALLOPED PATTERN ADJACENT TO THYROCYTES
TOXIC ADENOMA TREATMENT: SURGERY OR RADIO IODINE {>45 yrs} SURGERY; SUBTOTAL THYROIDECTOMY
MANAGEMENT OF THYROID CARCINOMA • PAPILLARY CA • FOLLICULAR CA • ANAPLASTIC CA

INVESTIGATIONS
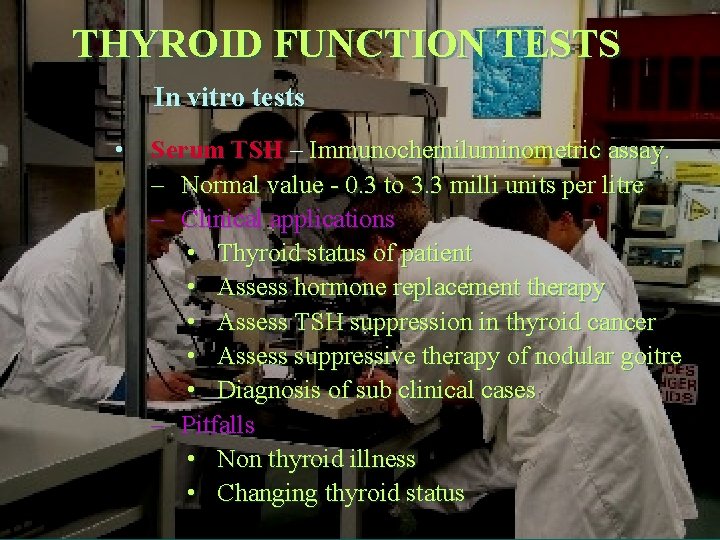
THYROID FUNCTION TESTS In vitro tests • Serum TSH – Immunochemiluminometric assay. – Normal value - 0. 3 to 3. 3 milli units per litre – Clinical applications • Thyroid status of patient • Assess hormone replacement therapy • Assess TSH suppression in thyroid cancer • Assess suppressive therapy of nodular goitre • Diagnosis of sub clinical cases – Pitfalls • Non thyroid illness • Changing thyroid status
THYROID FUNCTION TESTS • Serum total thyroxine (TT 4) – Measured by radioimmunoassay – normal value – 5 to 12 mcg per dl – Factors altering Total T 4 levels • Change in concentration of thyroid binding globulin • In familial disalbuminemic hyperthyroxinemia • Endogenous antibodies to T 4 • Non thyroid illness • Free T 4 – Gold standard of thyroid metabolic status – Normal value – 10 to 30 nmol per litre – Commercially measured by immunoassay
THYROID FUNCTION TESTS TT 4 • Free T 4 index • Serum total T 3 Thyroid uptake TT 4* T 3 uptake – Measured by radioimmunoassay – normal value – 75 to 175 ng per d. L – Assess severity of hyperthyroidism – Confirm suspected thyrotoxicosis – Evaluate autonomous thyroid functioning – T 3 toxicosis • Serum free T 3 – Measured by radioimmunoassay – normal value – 3. 5 to 7. 5 micro mol per litre – Free T 3 index calculated similarly
SEROLOGICAL TESTS • Thyroid antibodies – Estimated by sensitive immunoassay – Antimicrosomal (thyroid peroxidase) – Antithyroglobulin – Seen in autoimmune thyroid diseases – More than 25 units per ml significant – Usually AMA used – Positive AMA titre- possibility of hypothyroidism – Prognostic value when conjugated with serum TSH • Thyroid stimulating antibodies – Diagnosis of non evident graves disease – Hyperthyroidism in pregnancy – Predict neonatal hypothyroidism or thyrotoxicosis

SEROLOGICAL TESTS • Serum thyroglobulin – Measured by radioimmunoassay – Normal value – 1 to 20 mcg per dl – Tumour marker of well differentiated follicular and papillary carcinomas – Rising levels shows recurrence or persistence of tumour • Serum calcitonin – Tumour marker of medullary carcinoma – Also to screen the family members for familial disorders

THYROID FUNCTION TESTS In vivo tests • Radioiodine uptake test – Administering an isotope and measuring the percentage of isotope trapped by the gland. Radiopharmaceuticals for thyroid • Iodine 131 – – – Physical half life – 8 days. Biological half life – more than Iodine 123. High energy radiation. Used in uptake studies – 5 to 10 micro Ci. Also used in imaging – 50 to 100 micro Ci.
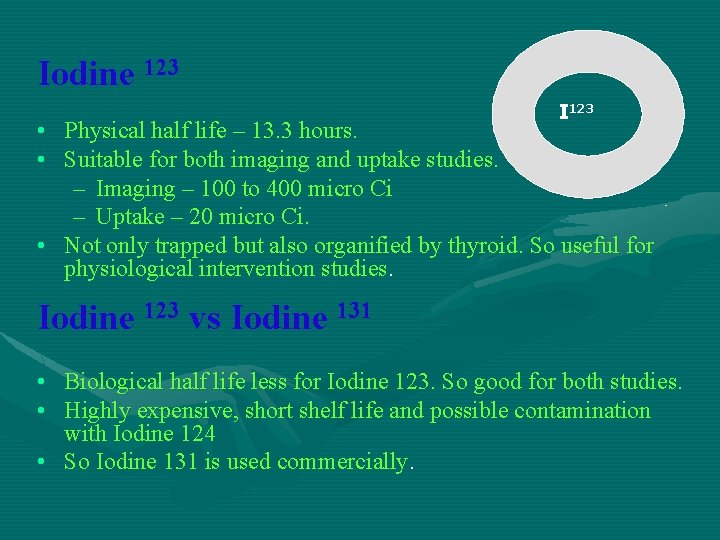
Iodine 123 I 123 • Physical half life – 13. 3 hours. • Suitable for both imaging and uptake studies. – Imaging – 100 to 400 micro Ci – Uptake – 20 micro Ci. • Not only trapped but also organified by thyroid. So useful for physiological intervention studies. Iodine 123 vs Iodine 131 • Biological half life less for Iodine 123. So good for both studies. • Highly expensive, short shelf life and possible contamination with Iodine 124 • So Iodine 131 is used commercially.
• Can assess the perfusion and nodules in the gland also anatomy of glands especially in patients with low iodine uptake. Thallium 201 • • • Used as Thallous chloride for imaging. Incorporated into gland by perfusion. Used for imaging of – Hypofunctioning gland – Patients with high Iodine pool – Extra thyroidal metastasis of thyroid carcinoma.
with neck phantom • Imaging – Rectilinear scaner – Scintillation camera Uptake interpretation • Low uptake – Primary and secondary hyperthyroidism – Large Iodide pool – Patients with exogenous thyroid administration • Elevated uptake – Graves disease, Iodine deficiency goitre and toxic nodular goitre – Occasionally in Hashimoto’s disease
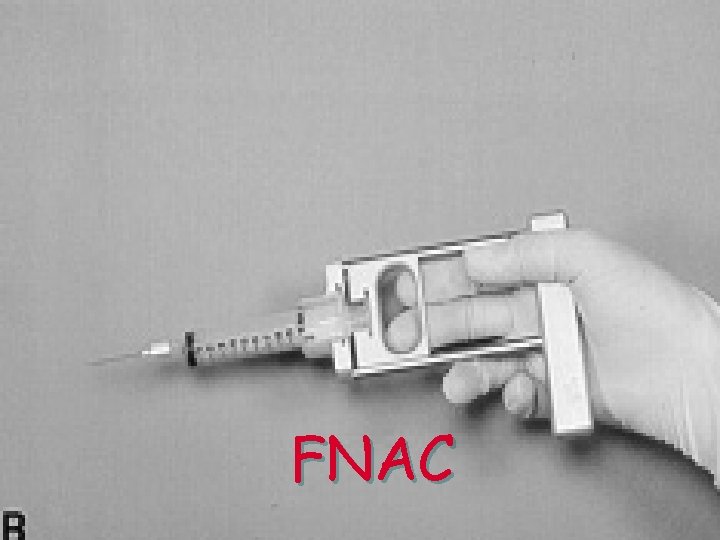
FNAC
• Accurate diagnostic test • First step of evaluation for nodular lesions
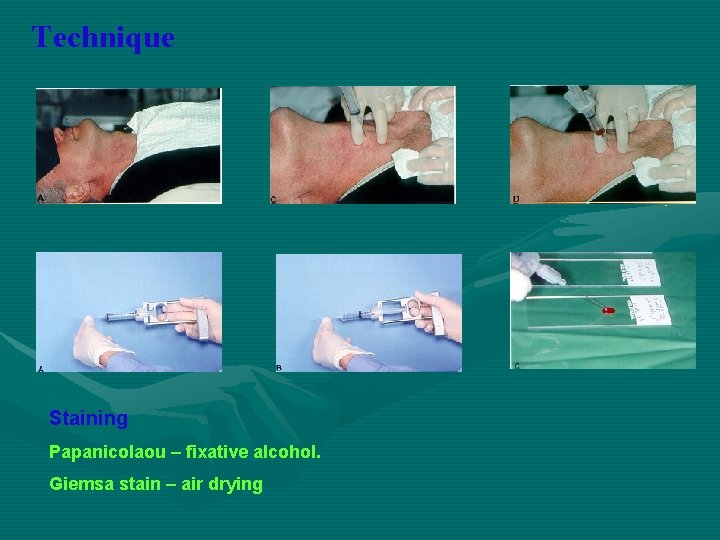
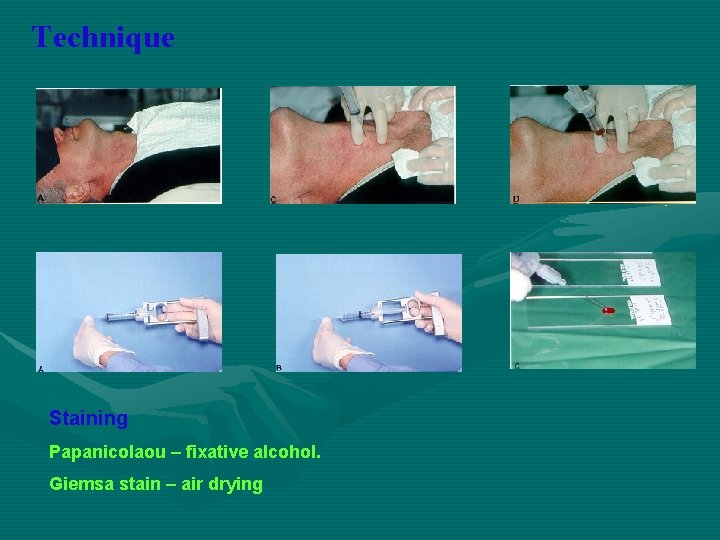
Technique Staining Papanicolaou – fixative alcohol. Giemsa stain – air drying
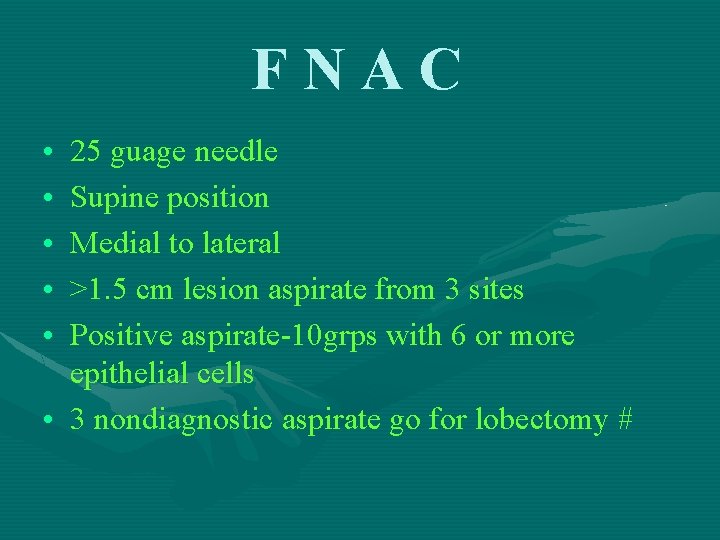
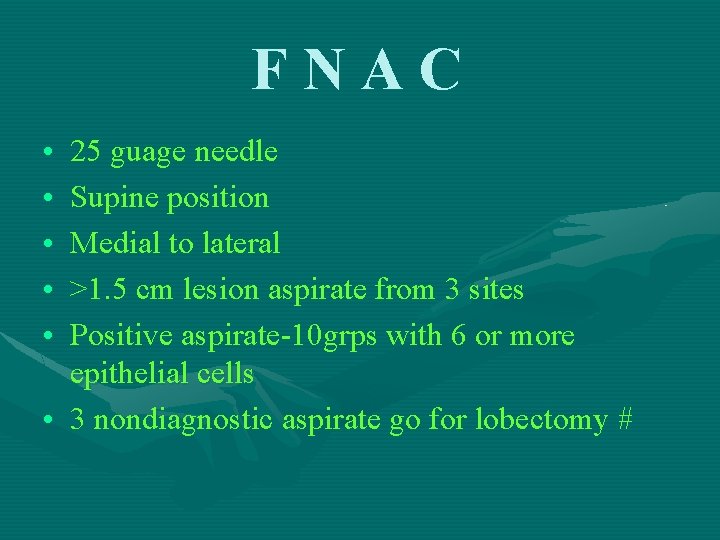
FNAC • • • 25 guage needle Supine position Medial to lateral >1. 5 cm lesion aspirate from 3 sites Positive aspirate-10 grps with 6 or more epithelial cells • 3 nondiagnostic aspirate go for lobectomy #

Complications • Puncture site pain and skin discolouration • Post aspiration haemorrhage to cyst FNNA biopsy • No syringe used • Minimize trauma to gland reduce blood contamination

Grading • • 0 – no aspirate 1 – inadequate aspiration 2 – no cells 3 – benign 4 – atypia 5 – suspicious malignancy 6 – malignancy • False negative – missed malignancy – 5%. – Commonly lymphoma as Hashimoto’s – In too small and too large nodules • False positive – Commonly Hashimoto’s as lymphoma – Follicular and Hurthle cell adenoma as carcinoma
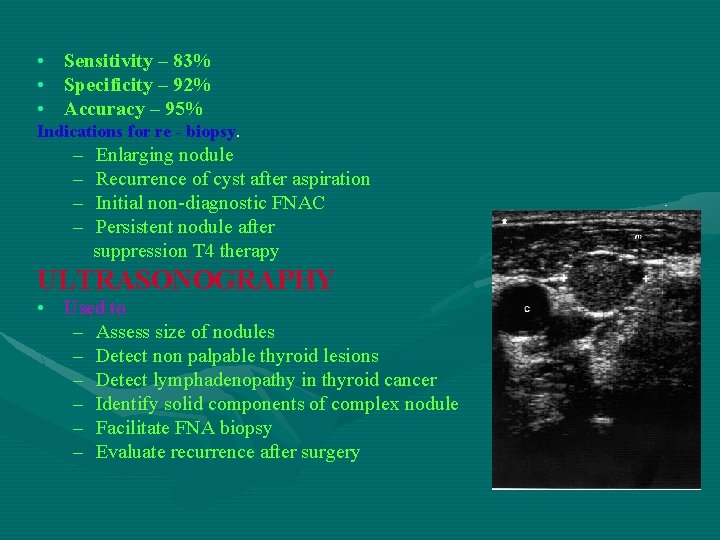
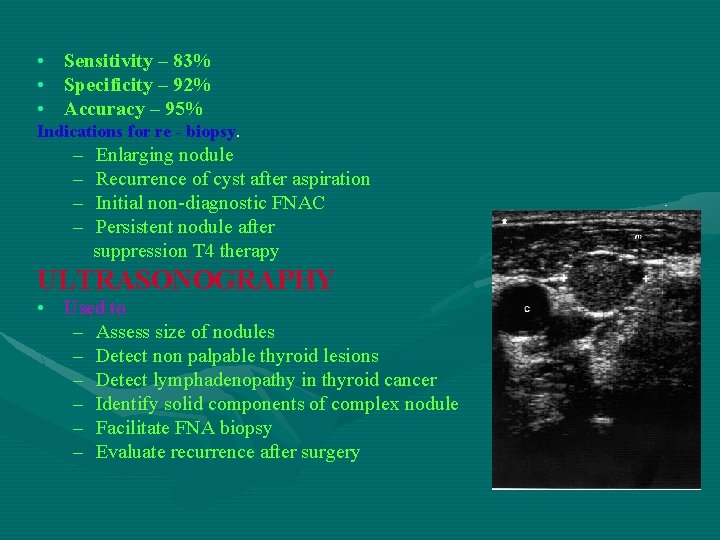
• Sensitivity – 83% • Specificity – 92% • Accuracy – 95% Indications for re - biopsy. – – Enlarging nodule Recurrence of cyst after aspiration Initial non-diagnostic FNAC Persistent nodule after suppression T 4 therapy ULTRASONOGRAPHY • Used to – Assess size of nodules – Detect non palpable thyroid lesions – Detect lymphadenopathy in thyroid cancer – Identify solid components of complex nodule – Facilitate FNA biopsy – Evaluate recurrence after surgery
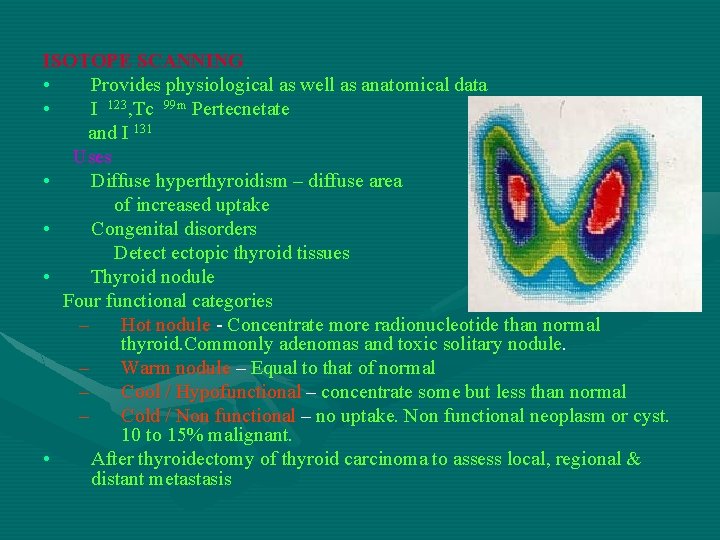
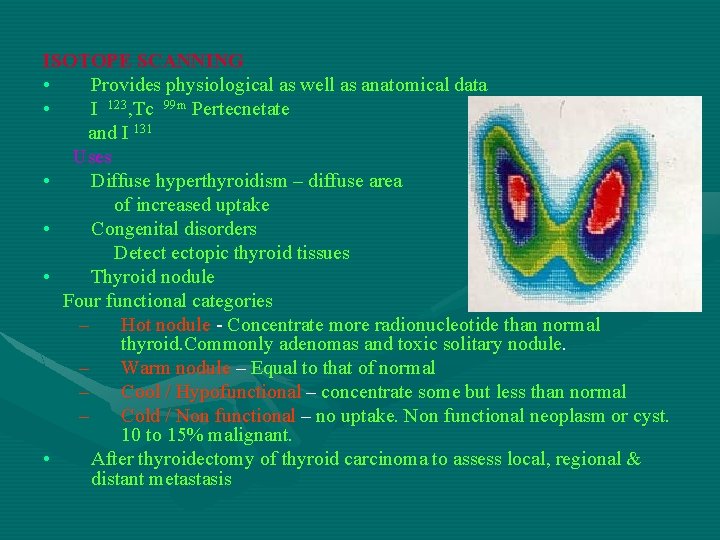
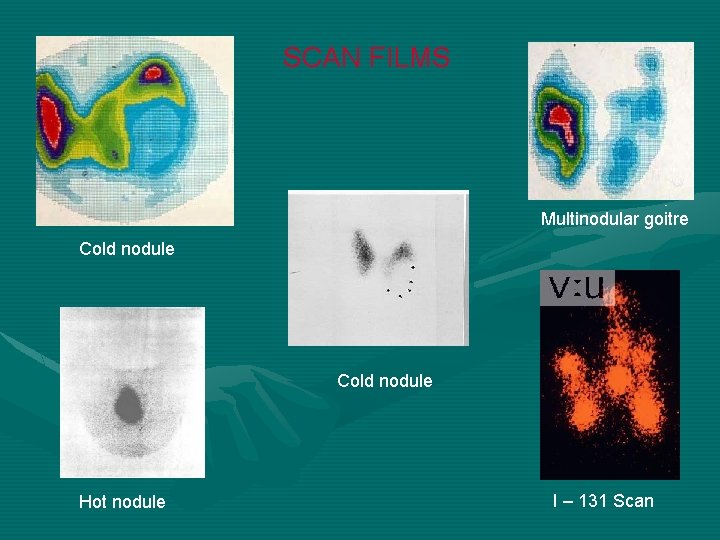
ISOTOPE SCANNING • Provides physiological as well as anatomical data • I 123, Tc 99 m Pertecnetate and I 131 Uses • Diffuse hyperthyroidism – diffuse area of increased uptake • Congenital disorders Detect ectopic thyroid tissues • Thyroid nodule Four functional categories – Hot nodule - Concentrate more radionucleotide than normal thyroid. Commonly adenomas and toxic solitary nodule. – Warm nodule – Equal to that of normal – Cool / Hypofunctional – concentrate some but less than normal – Cold / Non functional – no uptake. Non functional neoplasm or cyst. 10 to 15% malignant. • After thyroidectomy of thyroid carcinoma to assess local, regional & distant metastasis
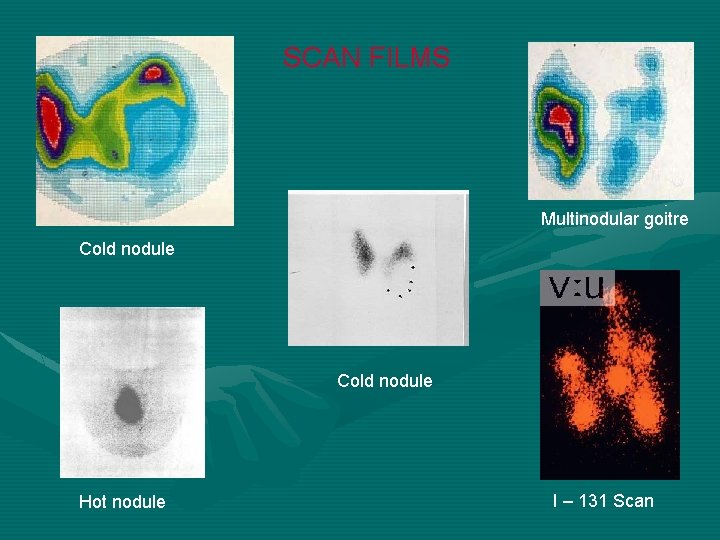
SCAN FILMS Multinodular goitre Cold nodule Hot nodule I – 131 Scan
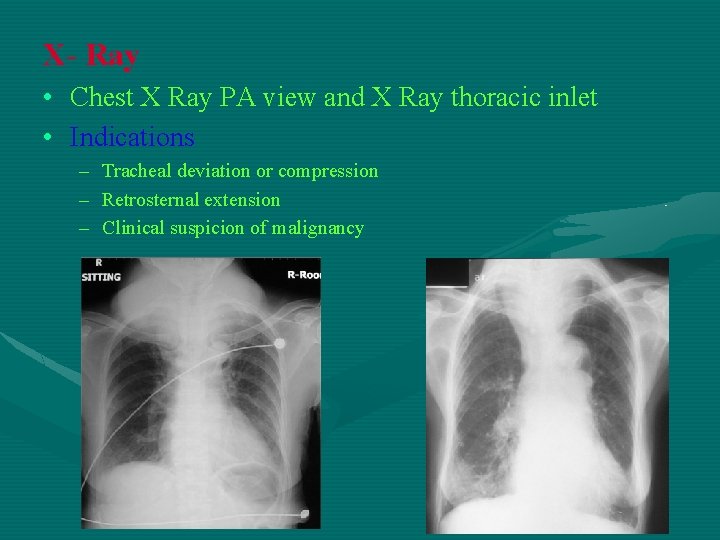
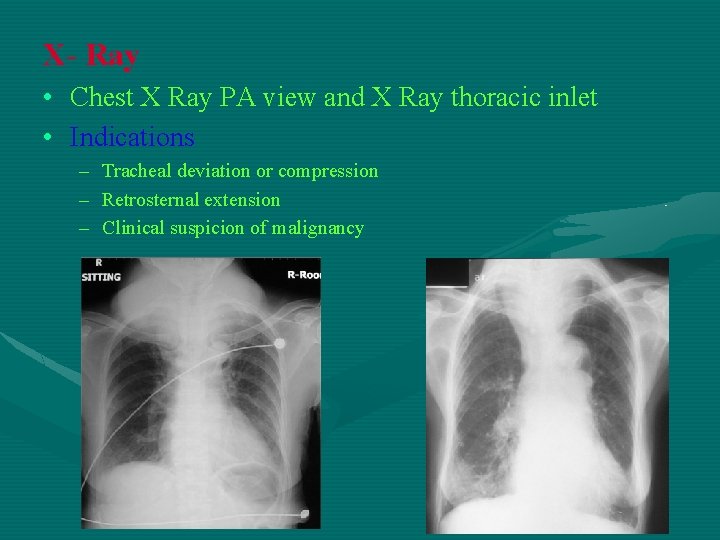
X- Ray • Chest X Ray PA view and X Ray thoracic inlet • Indications – Tracheal deviation or compression – Retrosternal extension – Clinical suspicion of malignancy
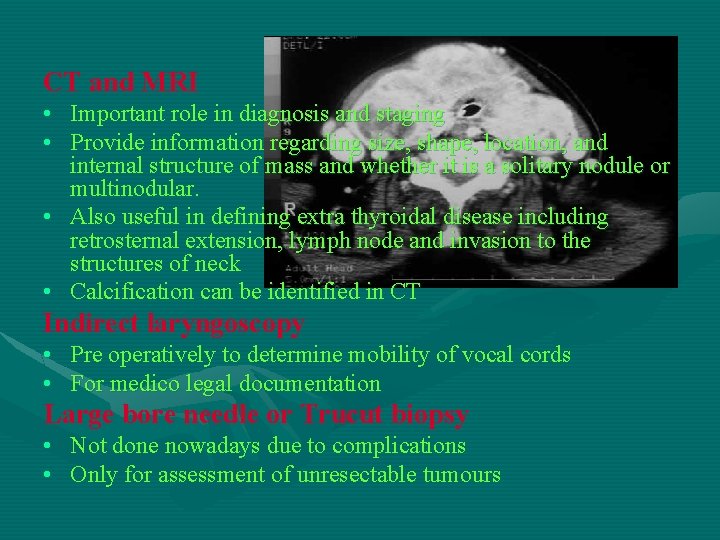
CT and MRI • Important role in diagnosis and staging • Provide information regarding size, shape, location, and internal structure of mass and whether it is a solitary nodule or multinodular. • Also useful in defining extra thyroidal disease including retrosternal extension, lymph node and invasion to the structures of neck • Calcification can be identified in CT Indirect laryngoscopy • Pre operatively to determine mobility of vocal cords • For medico legal documentation Large bore needle or Trucut biopsy • Not done nowadays due to complications • Only for assessment of unresectable tumours
PROGNOSTIC STAGING OF THYROID MALIGNANCIES
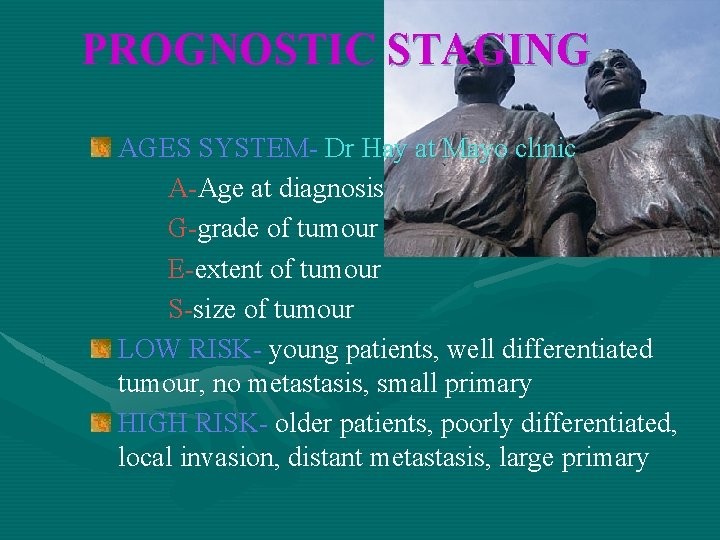
PROGNOSTIC STAGING AGES SYSTEM- Dr Hay at Mayo clinic A-Age at diagnosis G-grade of tumour E-extent of tumour S-size of tumour LOW RISK- young patients, well differentiated tumour, no metastasis, small primary HIGH RISK- older patients, poorly differentiated, local invasion, distant metastasis, large primary
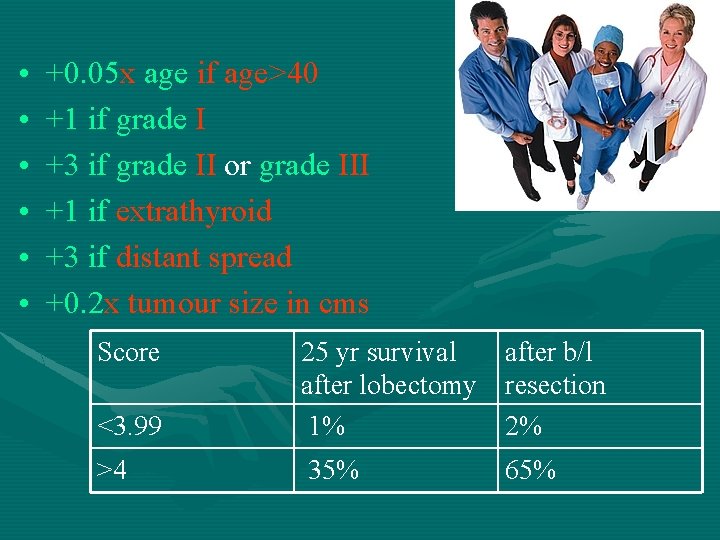
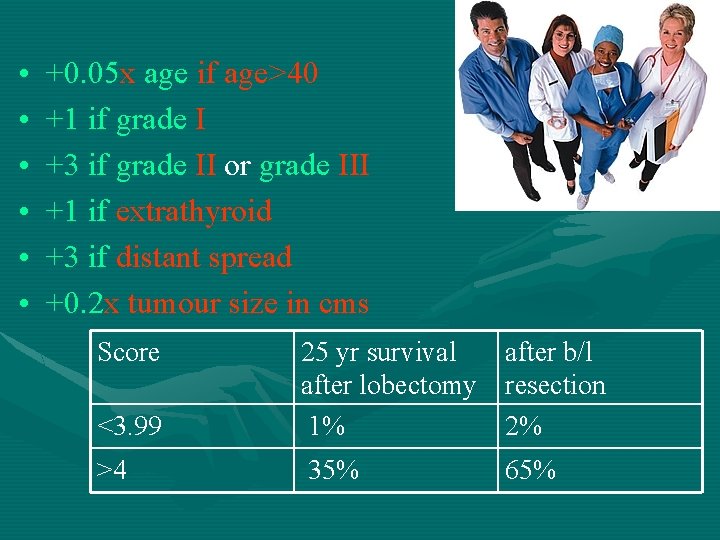
• • • +0. 05 x age if age>40 +1 if grade I +3 if grade II or grade III +1 if extrathyroid +3 if distant spread +0. 2 x tumour size in cms Score <3. 99 25 yr survival after lobectomy 1% after b/l resection 2% >4 35% 65%
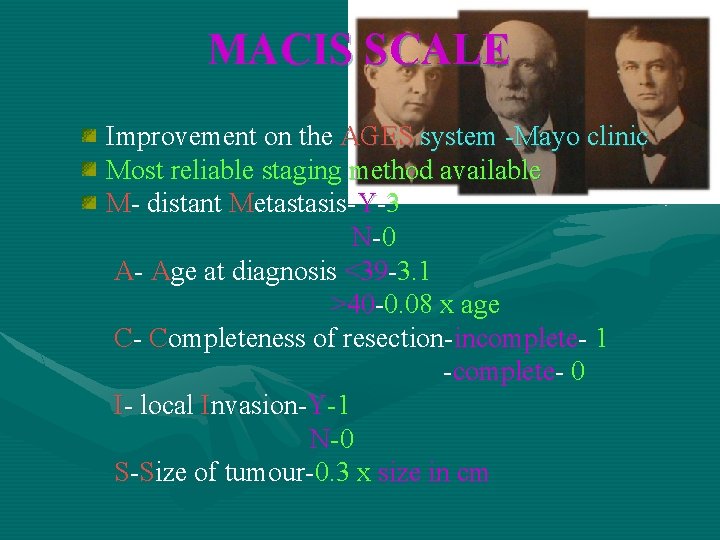
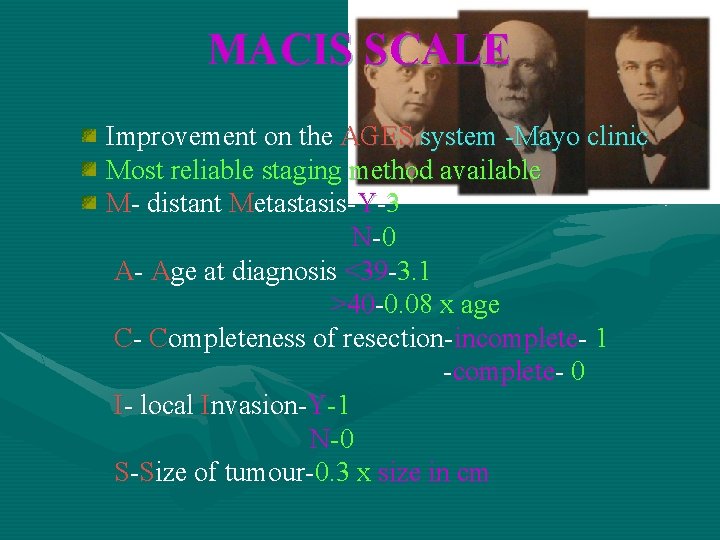
MACIS SCALE Improvement on the AGES system -Mayo clinic Most reliable staging method available M- distant Metastasis-Y-3 N -0 A- Age at diagnosis <39 -3. 1 >40 -0. 08 x age C- Completeness of resection-incomplete- 1 -complete- 0 I- local Invasion-Y-1 N-0 S-Size of tumour-0. 3 x size in cm

20 YEAR SURVIVAL RATE <6 MACIS 20 YR 99% SURVIV AL RATE 6 -6. 99 7 -7. 99 >8 89% 56% 24%
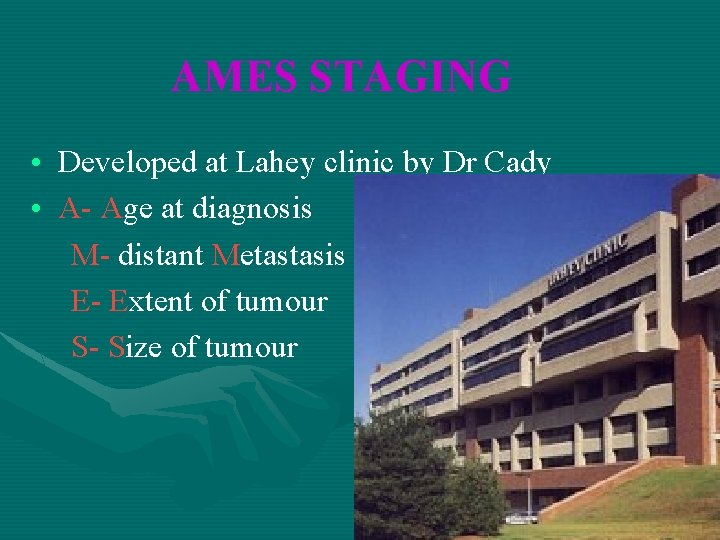
AMES STAGING • Developed at Lahey clinic by Dr Cady • A- Age at diagnosis M- distant Metastasis E- Extent of tumour S- Size of tumour

Low Risk Men < 40 yrs, women<50 yrs, without distant metastasis All older pts with intrathyroid pap ca, foll ca with minor capsular invol, Tumour<5 cm, no dist metastasis 20 yr mortality= 1% High risk All pts with distant metastasis All older pts with extrathyroid pap ca, foll ca with major capsular invol, tumour>5 cm 30 -40%
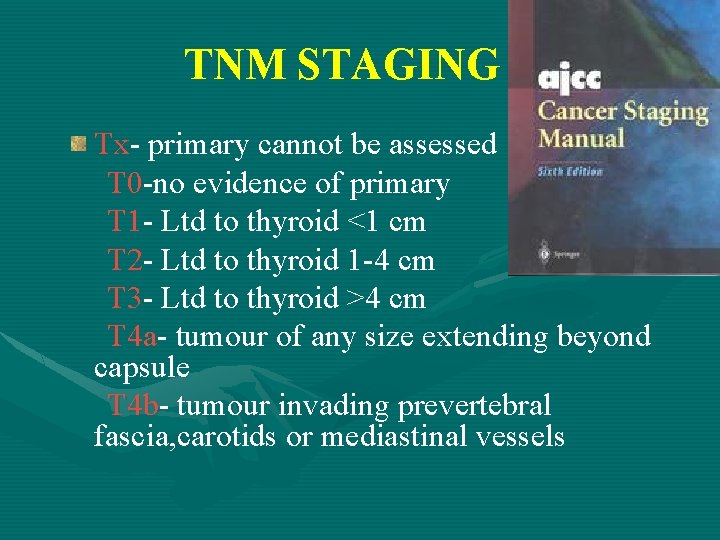
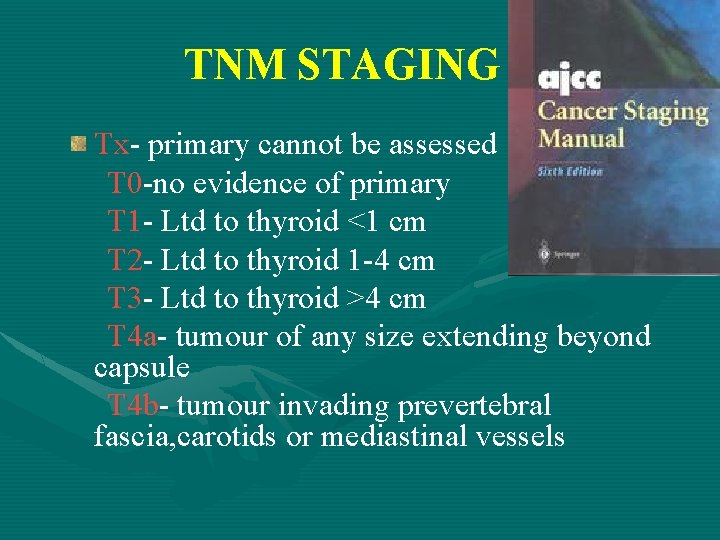
TNM STAGING Tx- primary cannot be assessed T 0 -no evidence of primary T 1 - Ltd to thyroid <1 cm T 2 - Ltd to thyroid 1 -4 cm T 3 - Ltd to thyroid >4 cm T 4 a- tumour of any size extending beyond capsule T 4 b- tumour invading prevertebral fascia, carotids or mediastinal vessels
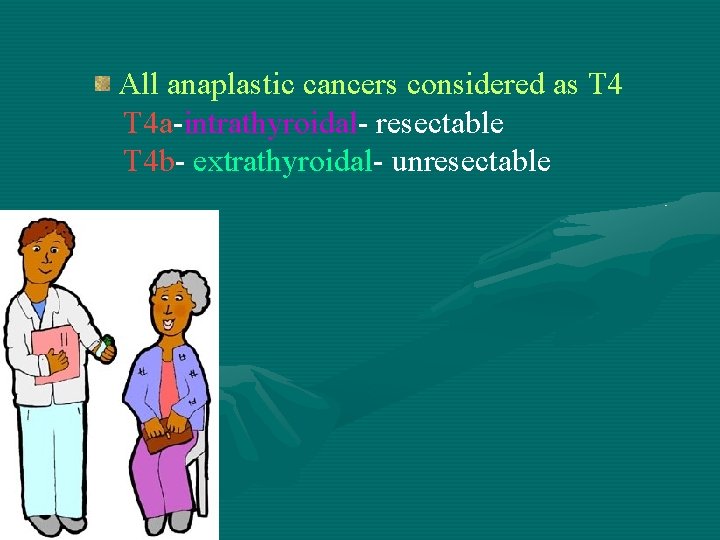
All anaplastic cancers considered as T 4 a-intrathyroidal- resectable T 4 b- extrathyroidal- unresectable
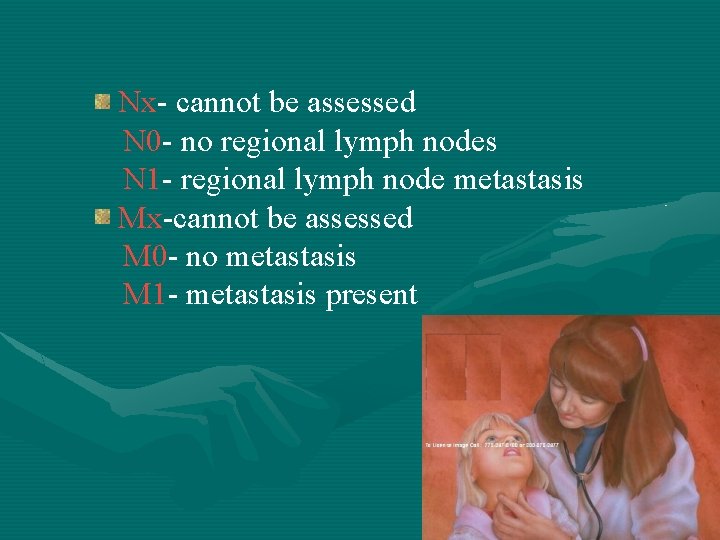
Nx- cannot be assessed N 0 - no regional lymph nodes N 1 - regional lymph node metastasis Mx-cannot be assessed M 0 - no metastasis M 1 - metastasis present

TNM STAGING CONTD STAGE 1 STAGE 2 STAGE 3 STAGE 4 <45 YRS Any T, Any N MO Any. T , Any N, M 1 >45 YRS T 1 N 0 MO T 2 NOMO T 3 NOMO T 4 NOMO Any TN 1 MO Any T, N, M

TREATMENT
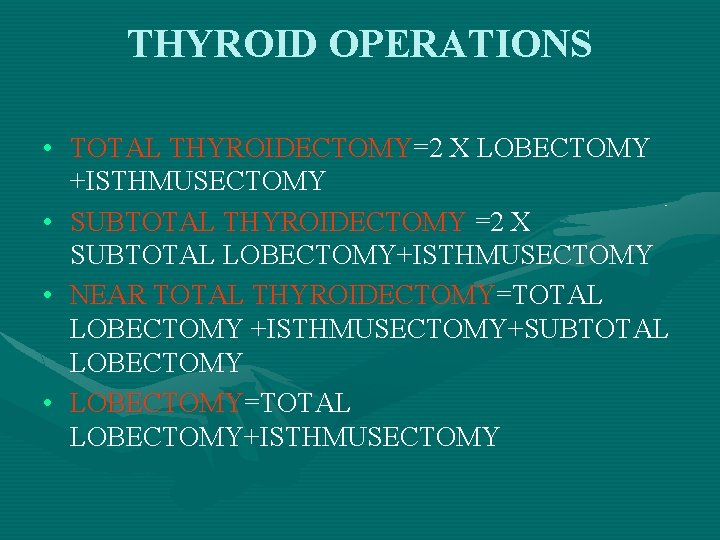
THYROID OPERATIONS • TOTAL THYROIDECTOMY=2 X LOBECTOMY +ISTHMUSECTOMY • SUBTOTAL THYROIDECTOMY =2 X SUBTOTAL LOBECTOMY+ISTHMUSECTOMY • NEAR TOTAL THYROIDECTOMY=TOTAL LOBECTOMY +ISTHMUSECTOMY+SUBTOTAL LOBECTOMY • LOBECTOMY=TOTAL LOBECTOMY+ISTHMUSECTOMY
PAPILLARY CARCINOMA • Total thyroidectomy done routinely
Advantages of Total Thyroidectomy • Multifocal tumours removed • Risk of anaplastic change in residual tissue excluded • Post op surveillance by serial thyroglobulin • Radioiodine screening for micro metastasis possible
Disadvantages • Greater risk of recurrent laryngeal N injury • Risk of permanent hypoparathyroidism
THYROXINE • Most tumours are TSH dependent • Dose-0. 1 -0. 2 mg/day • Thyroid hormone replacement necessary after total thyroidectomy or near total thyroidectomy in majority of patients
RADIOIODINE THERAPY • Standard management in high risk group • 4 weeks after total or near total thyroidectomy, after TSH levels have risen to 50 IU-ablative dose of 3 GBq • 4 months after first dose, thyroglobulin measured and total body scan, after stopping T 3 for 10 days • Remnant ablation at 6 -12 months

• Primarily surgical management FOLLICULAR NEOPLASM • Diagnosis cannot be made by FNAC alone • MAGNETIC RESONANCE SPECTROSCOPY- To distinguish between follicular adenoma and carcinoma • 100% sensitivity and 99% accuracy

• Surgery depending on score • Lesion <2 cm, well contained in one lobe-lobectomy with isthmectomy 2 -4 cm- grey area-decision of surgery depends on surgeon >4 cm- total or near total thyroidectomy • Completion thyroidectomy
FOLLOW UP • Low risk patients-USG evaluation every 6 months • High risk patients-radio ablation
ANAPLASTIC CARCINOMA • Very poor prognosis, survival for more than 2 yrs rare • Optimise the quality of life • Maintain the integrity of aero digestive tract • Adequate hydration and nutrition
SURGERY • No extra thyroidal spread- total thyroidectomy with central neck dissection • Most cases-advanced • Impending airway obstruction-central thyroid resection with freeing of trachea- Isthmectomytissue for histopathology • Tracheostomy if possible
• RADIOTHERAPY- external beam radiation • CHEMOTHERAPY- Doxorubicin -Most effective -Radiosensitiser -down staging or post op MUCOMYCIN -Blocks RAS proto-oncogene
POSTOPERATIVE COMPLICATIONS HAEMORRHAGE- usually reactionary, within 24 hrs Features-pallor, respiratory distress, stridor, swelling of wound Treatment-evacuation, intubation/tracheostomy
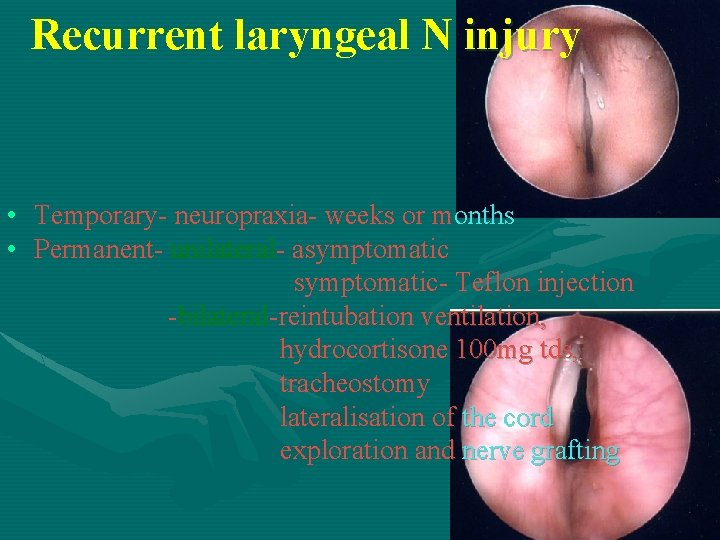
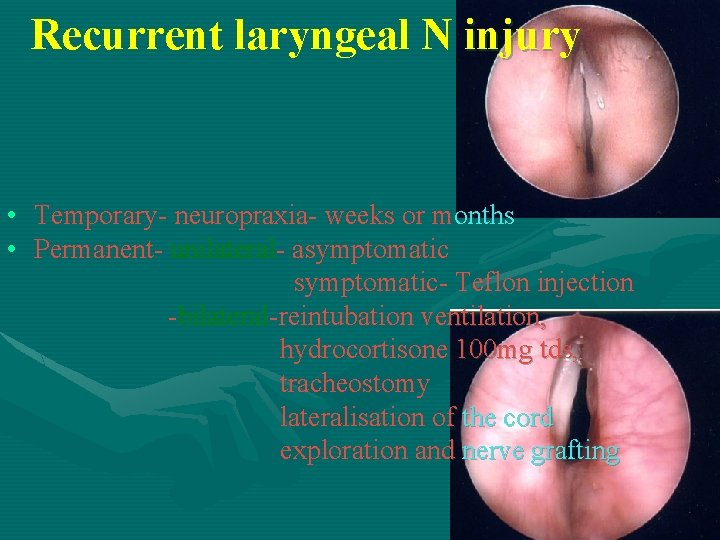
Recurrent laryngeal N injury • Temporary- neuropraxia- weeks or months • Permanent- unilateral- asymptomatic- Teflon injection -bilateral-reintubation ventilation, hydrocortisone 100 mg tds, tracheostomy lateralisation of the cord exploration and nerve grafting

– SUPERIOR LARYNGEAL N PALSYTeflon injection – HYPOPARATHYROIDISM-CHVOSTEK-WEISS SIGN -TROUSSEAU'S SIGN TREATMENT- iv 10 ml 10% calcium gluconate -oral effervescent calcium -calciferol 25000 -100000 U -2 -3 g oral calcium/day until normal level reached
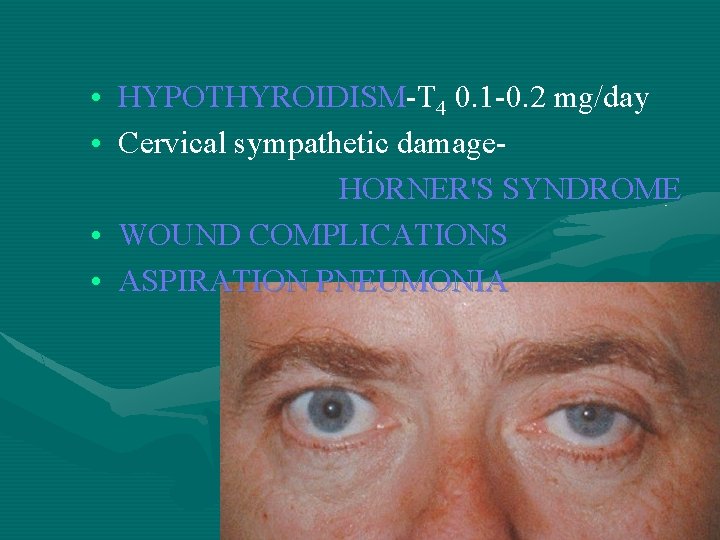
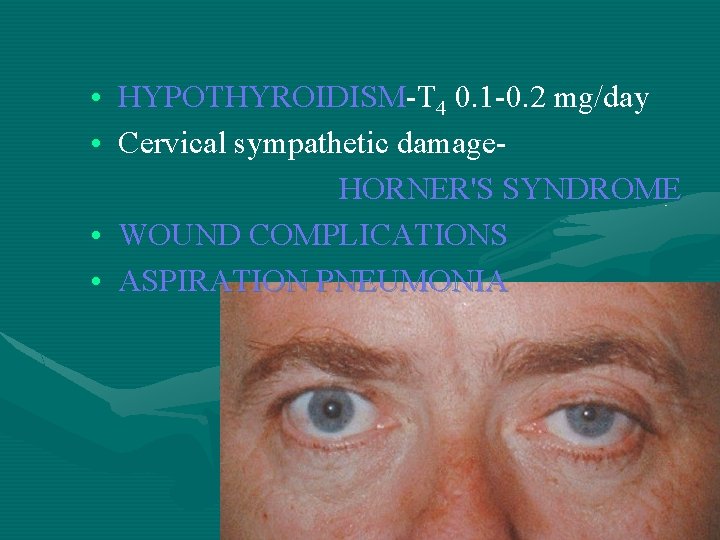
• HYPOTHYROIDISM-T 4 0. 1 -0. 2 mg/day • Cervical sympathetic damage. HORNER'S SYNDROME • WOUND COMPLICATIONS • ASPIRATION PNEUMONIA
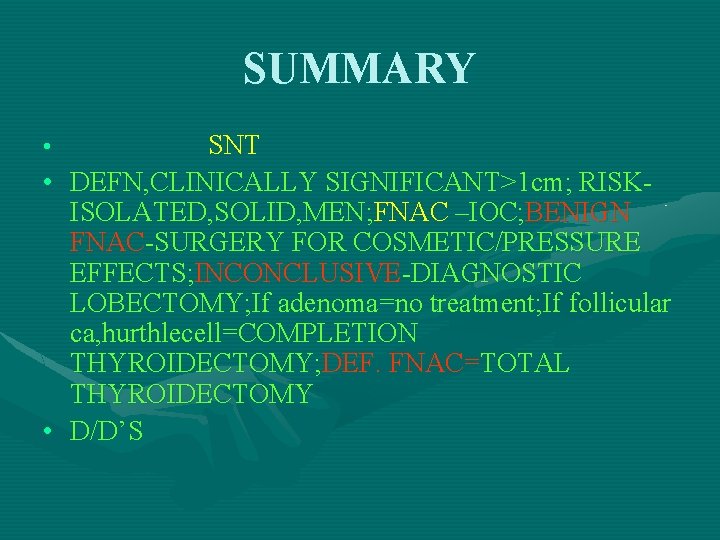
SUMMARY • • • SNT DEFN, CLINICALLY SIGNIFICANT>1 cm; RISKISOLATED, SOLID, MEN; FNAC –IOC; BENIGN FNAC-SURGERY FOR COSMETIC/PRESSURE EFFECTS; INCONCLUSIVE-DIAGNOSTIC LOBECTOMY; If adenoma=no treatment; If follicular ca, hurthlecell=COMPLETION THYROIDECTOMY; DEF. FNAC=TOTAL THYROIDECTOMY D/D’S
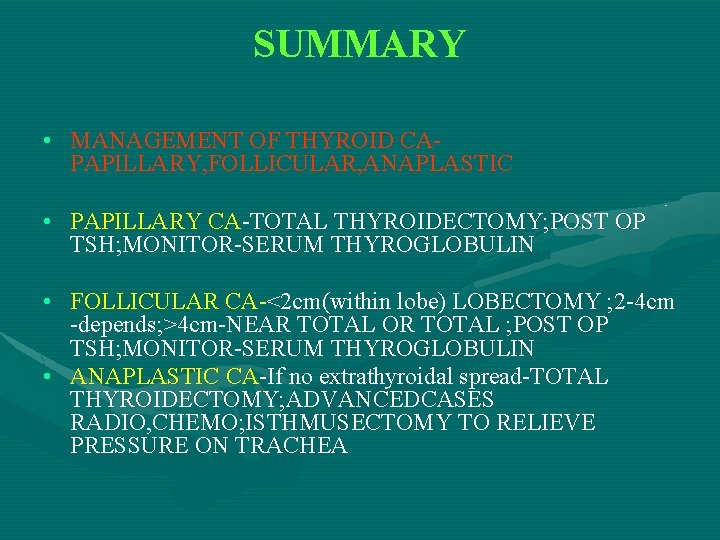
SUMMARY • MANAGEMENT OF THYROID CAPAPILLARY, FOLLICULAR, ANAPLASTIC • PAPILLARY CA-TOTAL THYROIDECTOMY; POST OP TSH; MONITOR-SERUM THYROGLOBULIN • FOLLICULAR CA-<2 cm(within lobe) LOBECTOMY ; 2 -4 cm -depends; >4 cm-NEAR TOTAL OR TOTAL ; POST OP TSH; MONITOR-SERUM THYROGLOBULIN • ANAPLASTIC CA-If no extrathyroidal spread-TOTAL THYROIDECTOMY; ADVANCEDCASES RADIO, CHEMO; ISTHMUSECTOMY TO RELIEVE PRESSURE ON TRACHEA

 Solitary nodule thyroid
Solitary nodule thyroid Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Hot thyroid nodule
Hot thyroid nodule Reidels thyroiditis
Reidels thyroiditis Palak choksi
Palak choksi Lieberkuhn
Lieberkuhn Nodule isoéchogène tirads 3
Nodule isoéchogène tirads 3 Vestibular reflex
Vestibular reflex Nodule de sœur marie-joseph scanner
Nodule de sœur marie-joseph scanner Down syndrome ears
Down syndrome ears Criteres de jones
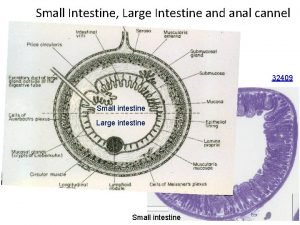
Criteres de jones Anal canal tissue
Anal canal tissue Reticulation pulmonaire
Reticulation pulmonaire Hypothyrodic
Hypothyrodic Nodule pulmonaire en verre dépoli taux de malignité
Nodule pulmonaire en verre dépoli taux de malignité Esophageal varices
Esophageal varices Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Second phase of nursing process
Second phase of nursing process Objectives of nursing process
Objectives of nursing process Nursing process
Nursing process Trifoliate duodenum
Trifoliate duodenum Differential diagnosis of hydrocephalus
Differential diagnosis of hydrocephalus Acute productive cough differential diagnosis
Acute productive cough differential diagnosis Differential diagnosis of osmf
Differential diagnosis of osmf Carpal tunnel
Carpal tunnel Myelopathy vs radiculopathy
Myelopathy vs radiculopathy Broadbent sign in constrictive pericarditis
Broadbent sign in constrictive pericarditis Fairy skin
Fairy skin Vitamin c differential diagnosis mnemonic
Vitamin c differential diagnosis mnemonic Conjunctivitis differential diagnosis
Conjunctivitis differential diagnosis Differential diagnosis of jaundice in pediatrics
Differential diagnosis of jaundice in pediatrics Differential diagnosis leukocoria
Differential diagnosis leukocoria Osteochondrosis
Osteochondrosis Differential diagnosis of stroke
Differential diagnosis of stroke Tnm staging of breast cancer
Tnm staging of breast cancer Differential diagnosis of otitis externa
Differential diagnosis of otitis externa Hpilora
Hpilora Diabetic ketoacidosis anion gap
Diabetic ketoacidosis anion gap Differential diagnosis red eye
Differential diagnosis red eye Differential diagnosis for premature rupture of membranes
Differential diagnosis for premature rupture of membranes Epigastric pain differential diagnosis
Epigastric pain differential diagnosis What is podoconiosis
What is podoconiosis Mentzer index
Mentzer index Nephrotic syndrome differential diagnosis
Nephrotic syndrome differential diagnosis Differential diagnosis for atopic dermatitis
Differential diagnosis for atopic dermatitis Differential diagnosis of dysphagia
Differential diagnosis of dysphagia Mieloproliferative
Mieloproliferative Differential diagnosis of vitiligo
Differential diagnosis of vitiligo Differential diagnosis leukocytosis
Differential diagnosis leukocytosis Meningeal syndrome slideshare
Meningeal syndrome slideshare Folate deficiency symptoms
Folate deficiency symptoms Define demetia
Define demetia Submental lymph nodes
Submental lymph nodes Organs by quadrant
Organs by quadrant Peptic ulcer anatomy and physiology
Peptic ulcer anatomy and physiology Postmenopausal endometrial thickness
Postmenopausal endometrial thickness Gastric outlet obstruction differential diagnosis
Gastric outlet obstruction differential diagnosis Spotting differential diagnosis
Spotting differential diagnosis Tarry stool images
Tarry stool images Pulmonary hypertension differential diagnosis
Pulmonary hypertension differential diagnosis Osu lymphedema clinic
Osu lymphedema clinic Dd jaundice
Dd jaundice Differential diagnosis of molar pregnancy
Differential diagnosis of molar pregnancy Branchial cyst aspiration
Branchial cyst aspiration Parkinson differential diagnosis
Parkinson differential diagnosis Polycythemia differential diagnosis
Polycythemia differential diagnosis Describe
Describe Differential diagnosis for premature rupture of membranes
Differential diagnosis for premature rupture of membranes Ivor lewis surgery
Ivor lewis surgery Alexander's law nystagmus
Alexander's law nystagmus Odd diagnosis
Odd diagnosis General appearance physical exam
General appearance physical exam Osgood schlatter vs patellar tendonitis
Osgood schlatter vs patellar tendonitis Dyslexia differential diagnosis
Dyslexia differential diagnosis Implantation spotting
Implantation spotting Bakers cyst differential diagnosis
Bakers cyst differential diagnosis Scalp swelling differential diagnosis
Scalp swelling differential diagnosis Papulovesicular rash differential diagnosis
Papulovesicular rash differential diagnosis Yap göster söyle yaz örnekleri
Yap göster söyle yaz örnekleri Differential diagnosis of stroke
Differential diagnosis of stroke The outsiders gangs
The outsiders gangs Tiffany mathews
Tiffany mathews Talle tonge mathews phosa
Talle tonge mathews phosa The mathews practice
The mathews practice Erin ledbetter
Erin ledbetter Mathew v eldridge
Mathew v eldridge The mathews practice
The mathews practice Roy mathews bainbridge
Roy mathews bainbridge Elizabeth mathews
Elizabeth mathews Cherry valance description
Cherry valance description Talle tonge gedig
Talle tonge gedig Tj mathews
Tj mathews Exposition in the outsiders
Exposition in the outsiders Mathews practice
Mathews practice Hibiscus inflorescence name
Hibiscus inflorescence name Solitary as an oyster pee paragraph
Solitary as an oyster pee paragraph