Differential diagnosis of nephrotic syndrome Tactics of GP
- Slides: 47
Differential diagnosis of nephrotic syndrome Tactics of GP
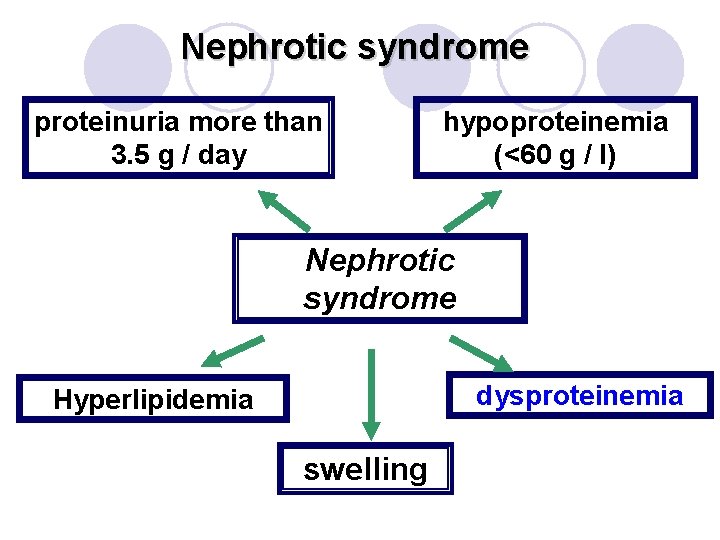
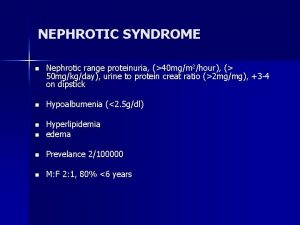
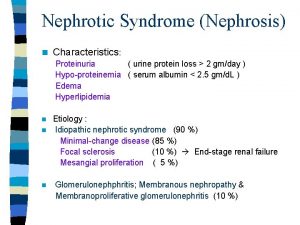
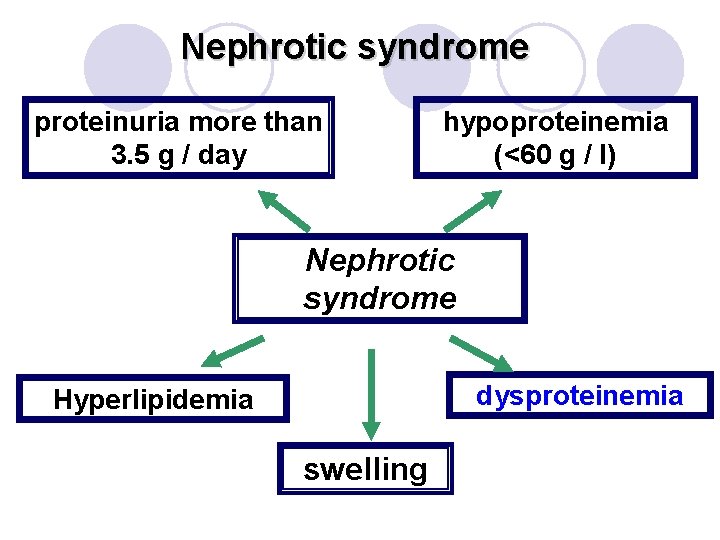
Nephrotic syndrome proteinuria more than 3. 5 g / day hypoproteinemia (<60 g / l) Nephrotic syndrome dysproteinemia Hyperlipidemia swelling
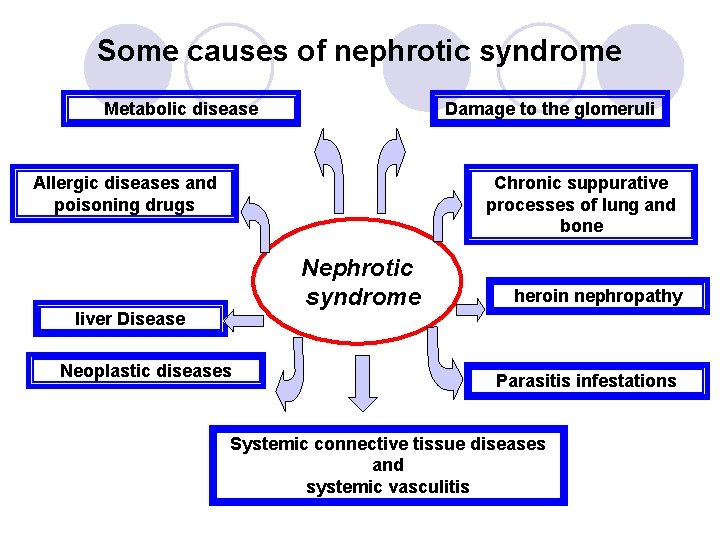
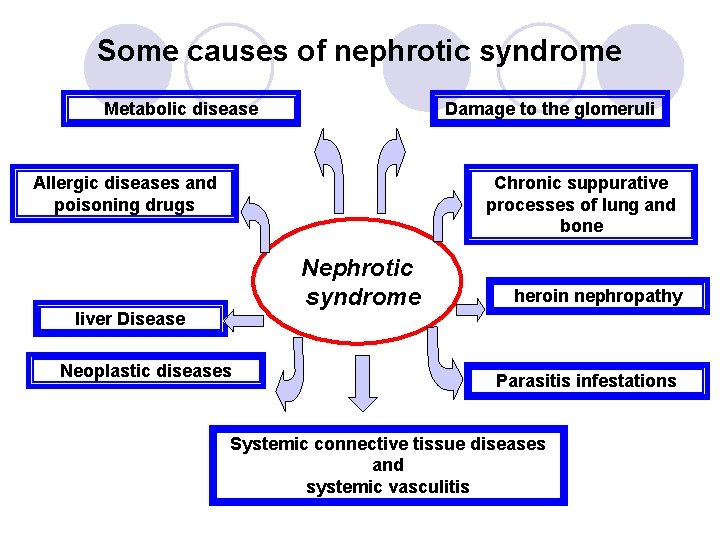
Some causes of nephrotic syndrome Metabolic disease Damage to the glomeruli Allergic diseases and poisoning drugs Chronic suppurative processes of lung and bone Nephrotic syndrome liver Disease Neoplastic diseases heroin nephropathy Parasitis infestations Systemic connective tissue diseases and systemic vasculitis
When all of the above cases of nephrotic syndrome It manifested as clinics kidney damage in glomerulonephritis or amyloidosis
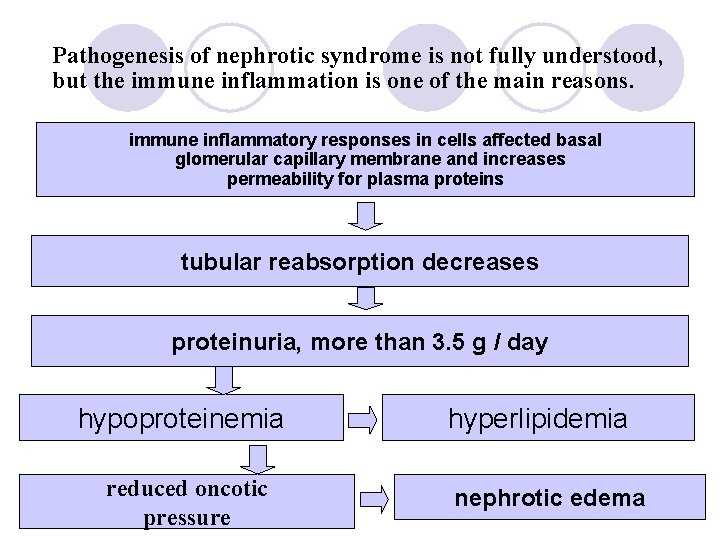
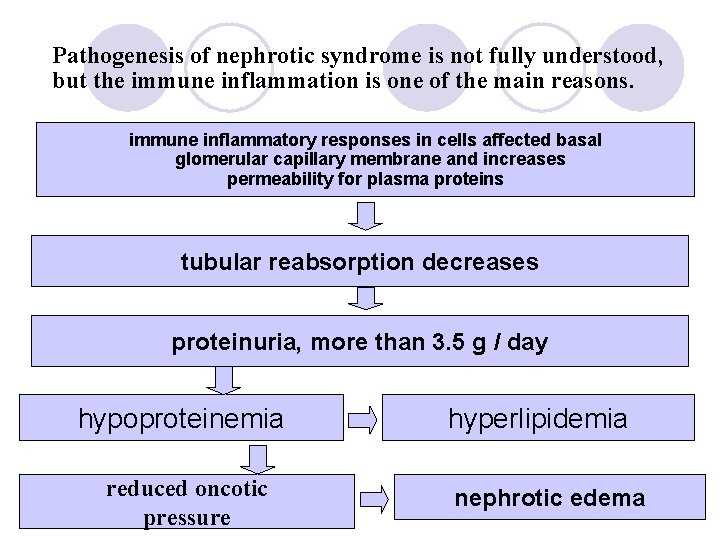
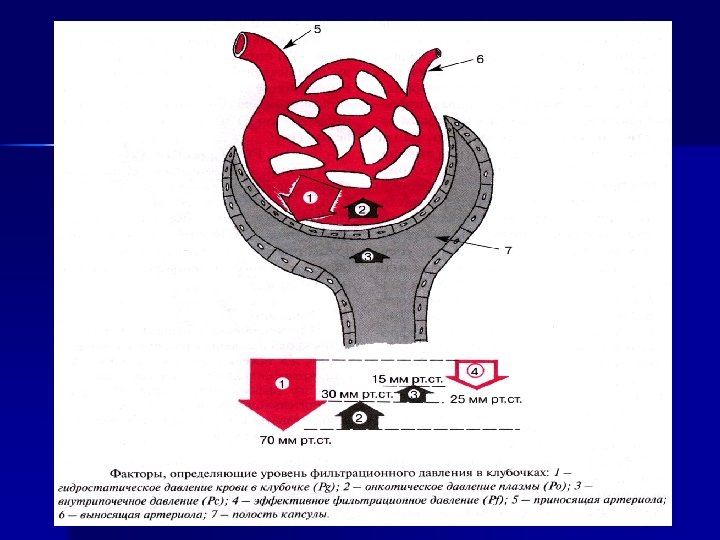
Pathogenesis of nephrotic syndrome is not fully understood, but the immune inflammation is one of the main reasons. immune inflammatory responses in cells affected basal glomerular capillary membrane and increases permeability for plasma proteins tubular reabsorption decreases proteinuria, more than 3. 5 g / day hypoproteinemia reduced oncotic pressure hyperlipidemia nephrotic edema
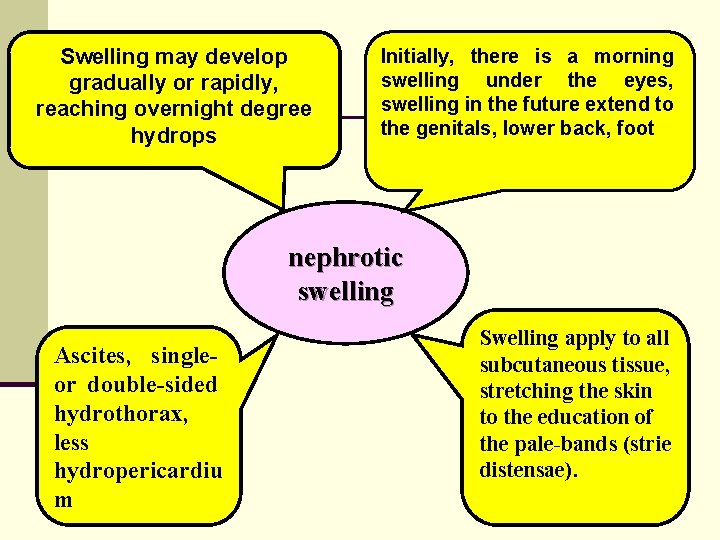
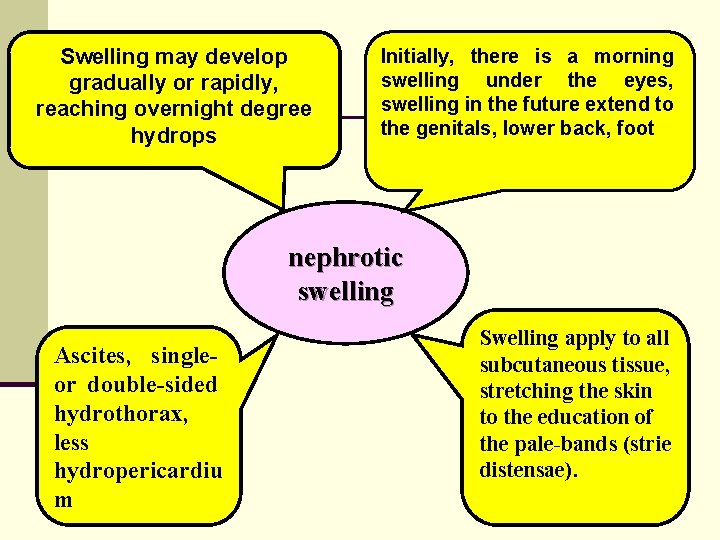
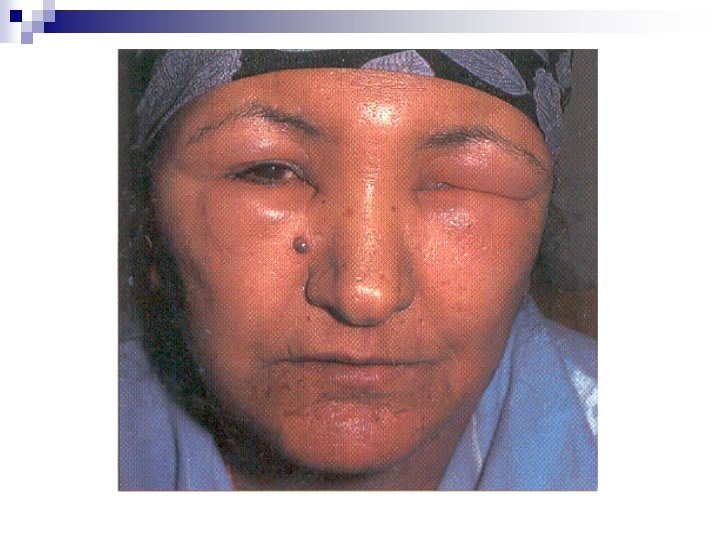
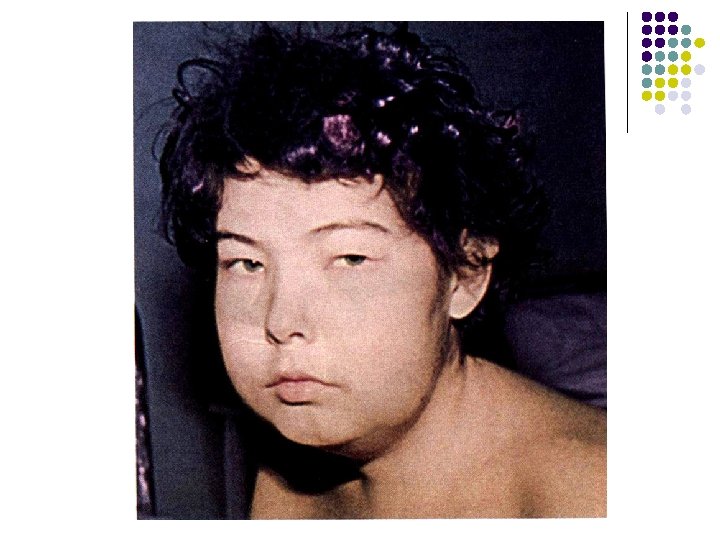
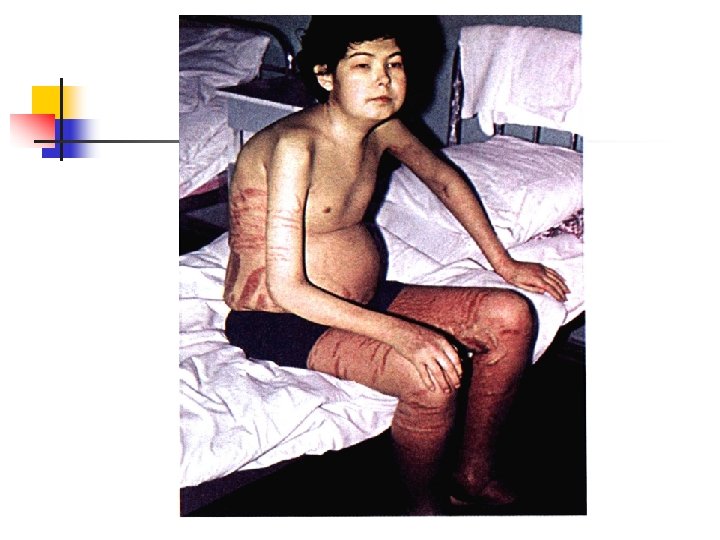
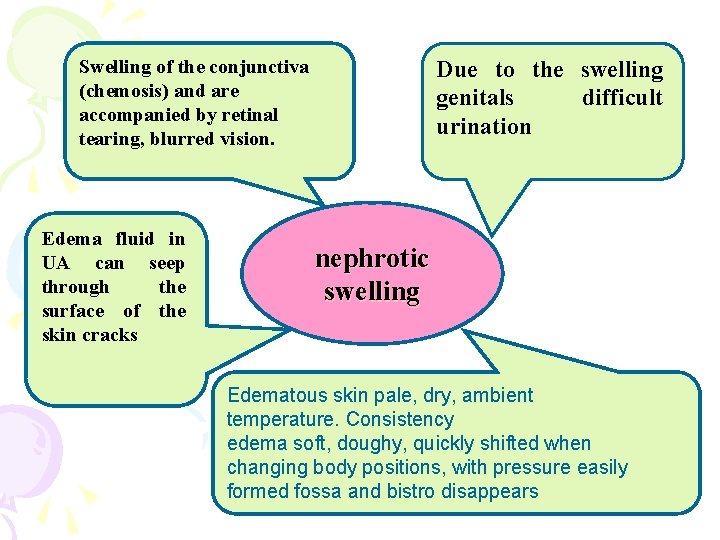
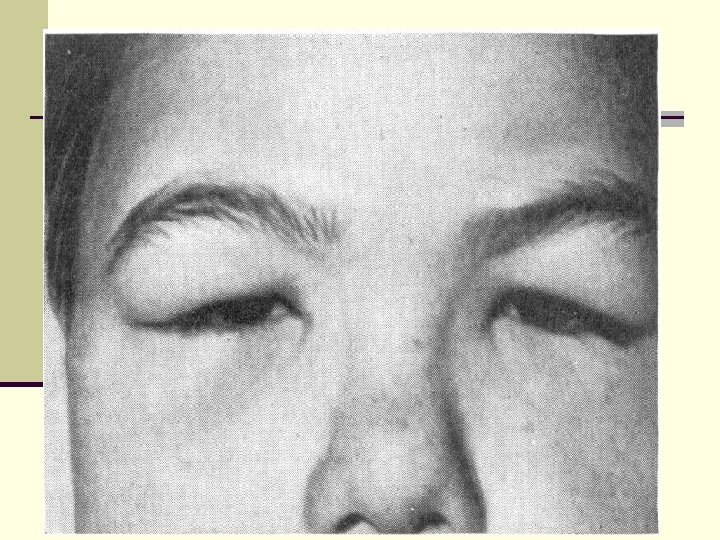
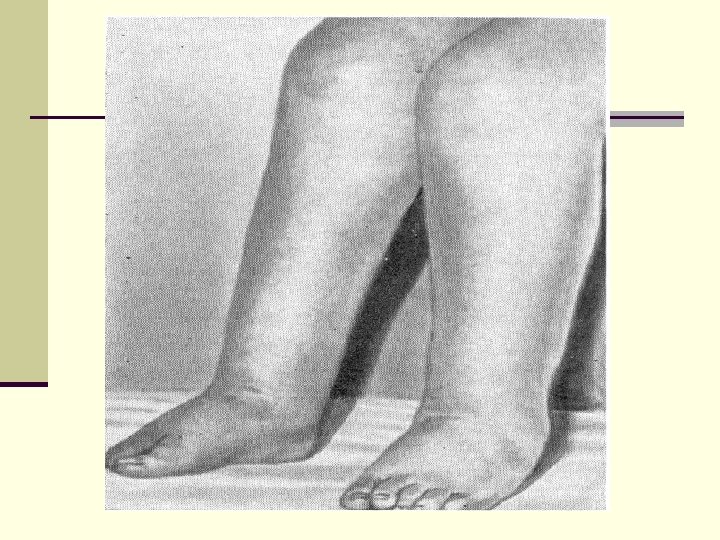
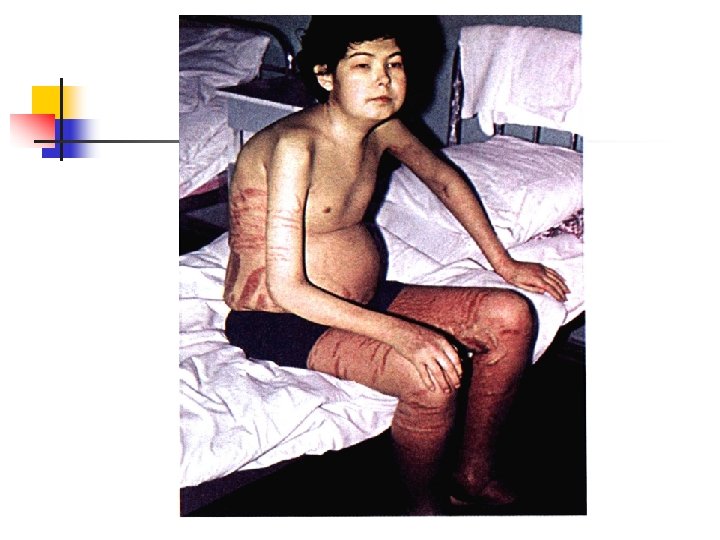
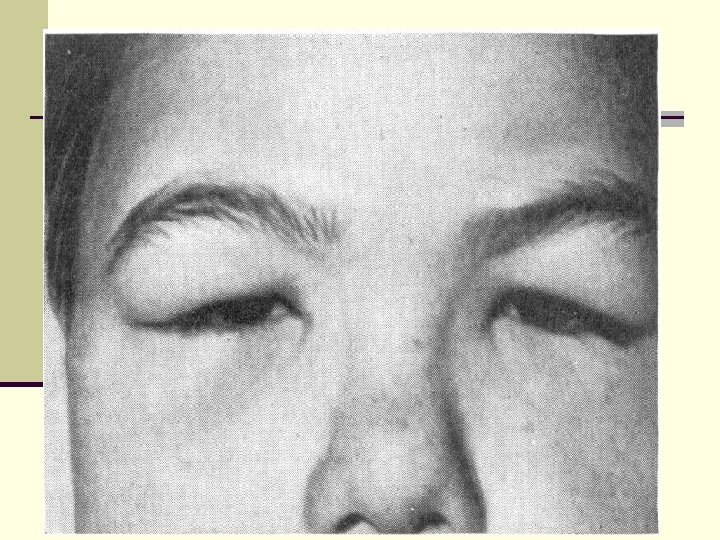
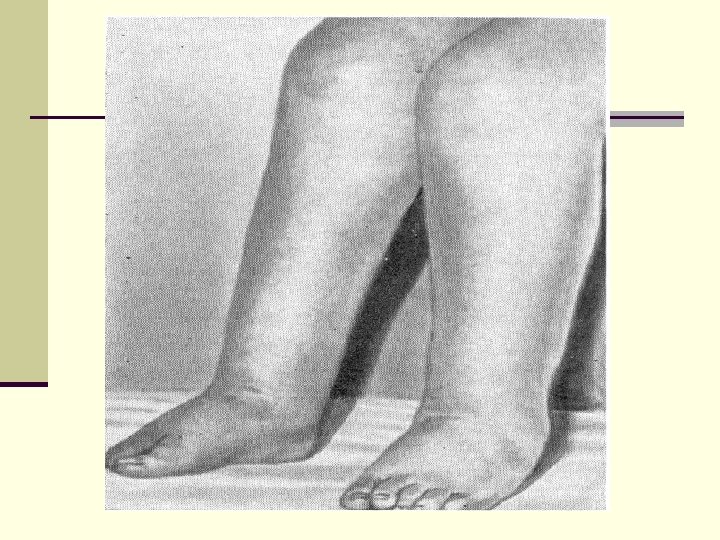
Swelling may develop gradually or rapidly, reaching overnight degree hydrops Initially, there is a morning swelling under the eyes, swelling in the future extend to the genitals, lower back, foot nephrotic swelling Ascites, single- or double-sided hydrothorax, less hydropericardiu m Swelling apply to all subcutaneous tissue, stretching the skin to the education of the pale-bands (strie distensae).
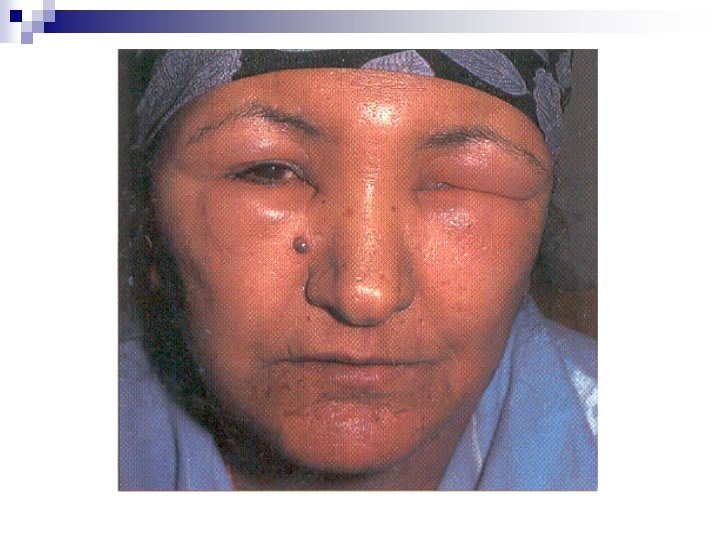
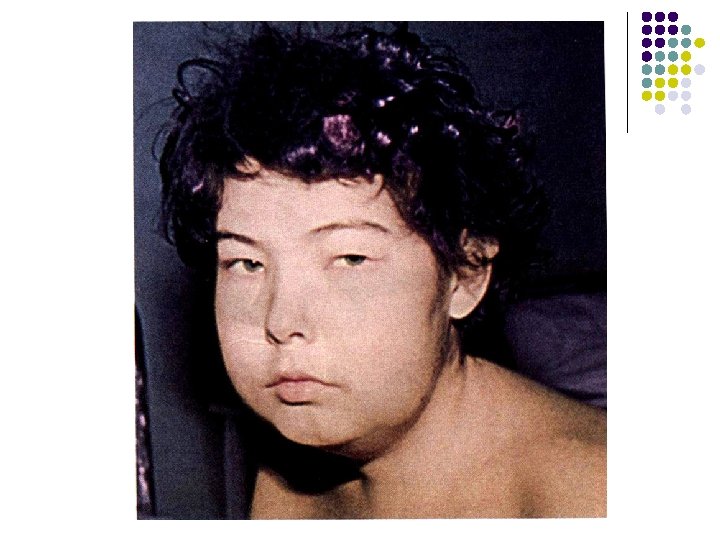
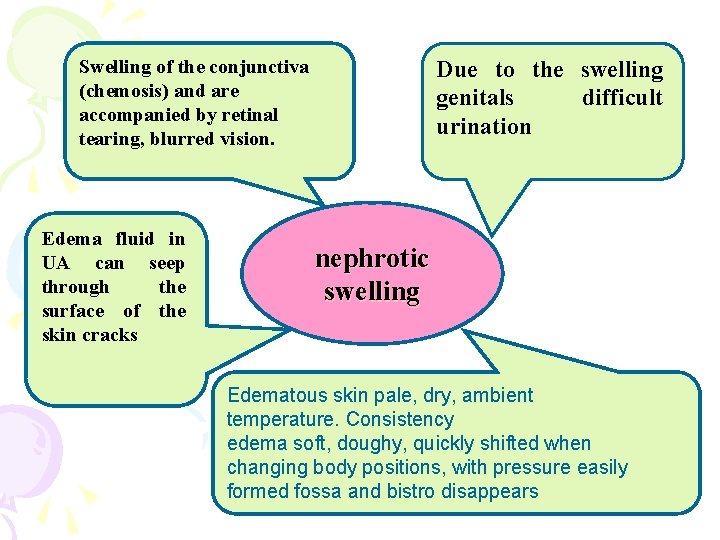
Swelling of the conjunctiva (chemosis) and are accompanied by retinal tearing, blurred vision. Edema fluid in UA can seep through the surface of the skin cracks Due to the swelling genitals difficult urination nephrotic swelling Edematous skin pale, dry, ambient temperature. Consistency edema soft, doughy, quickly shifted when changing body positions, with pressure easily formed fossa and bistro disappears
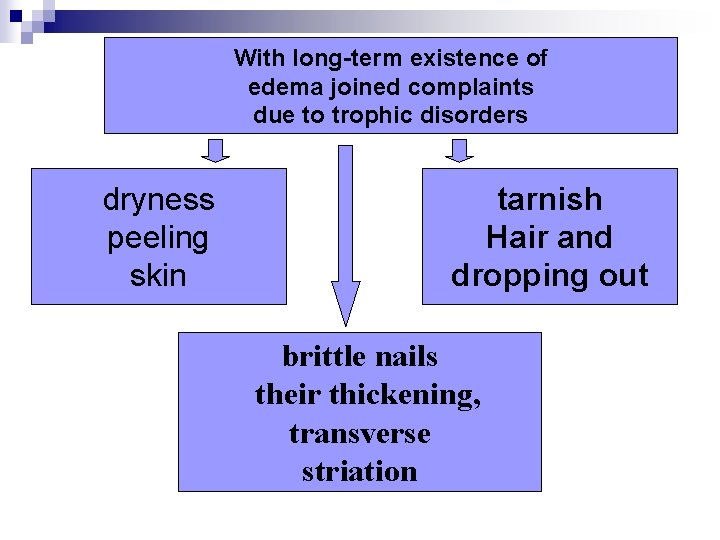
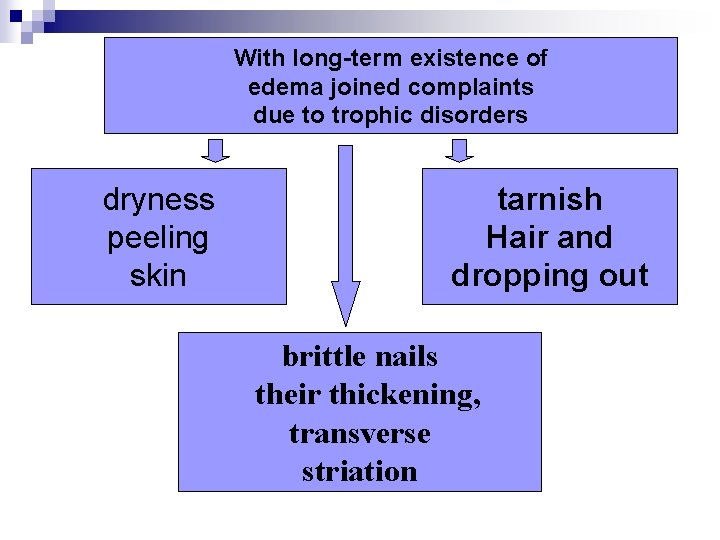
With long-term existence of edema joined complaints due to trophic disorders dryness peeling skin tarnish Hair and dropping out brittle nails their thickening, transverse striation
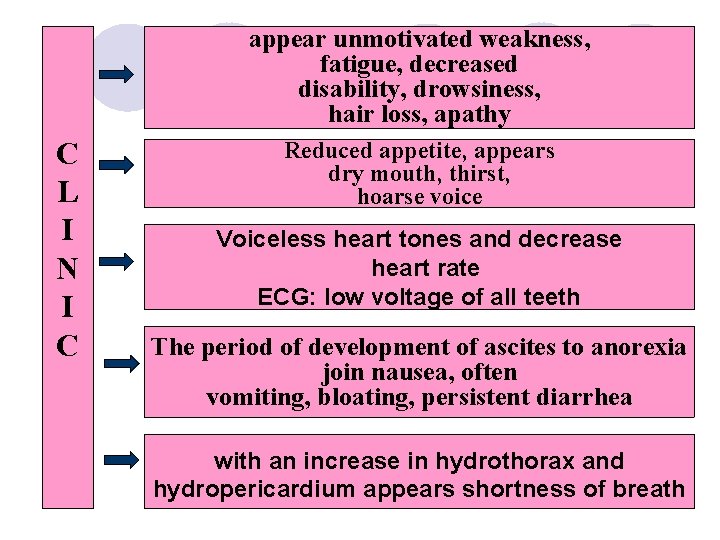
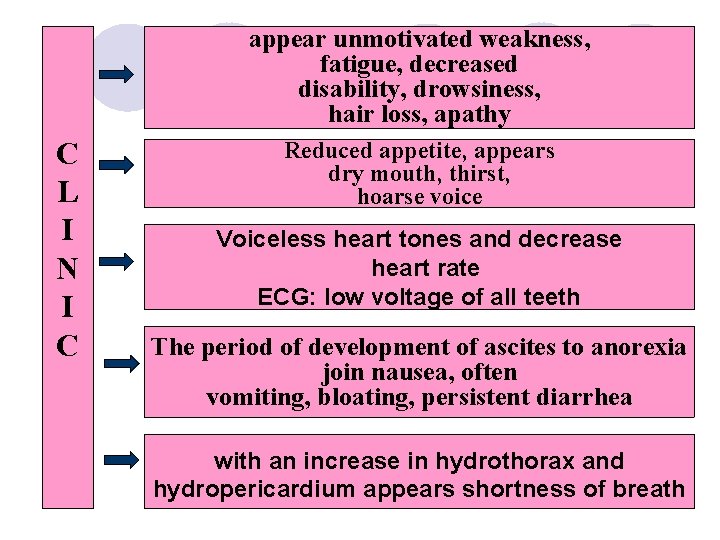
appear unmotivated weakness, fatigue, decreased disability, drowsiness, hair loss, apathy C L I N I С Reduced appetite, appears dry mouth, thirst, hoarse voice Voiceless heart tones and decrease heart rate ECG: low voltage of all teeth The period of development of ascites to anorexia join nausea, often vomiting, bloating, persistent diarrhea with an increase in hydrothorax and hydropericardium appears shortness of breath
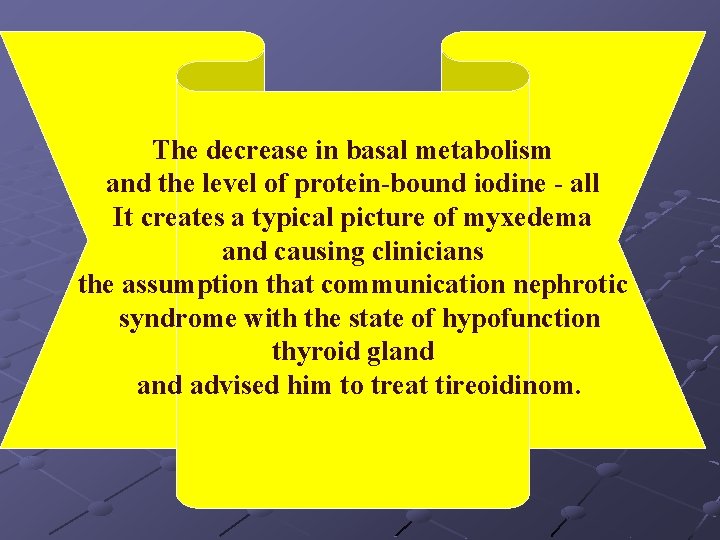
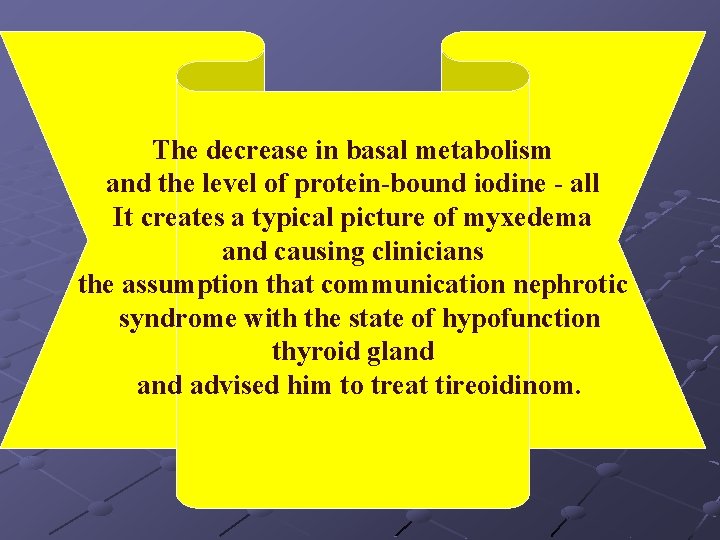
The decrease in basal metabolism and the level of protein-bound iodine - all It creates a typical picture of myxedema and causing clinicians the assumption that communication nephrotic syndrome with the state of hypofunction thyroid gland advised him to treat tireoidinom.
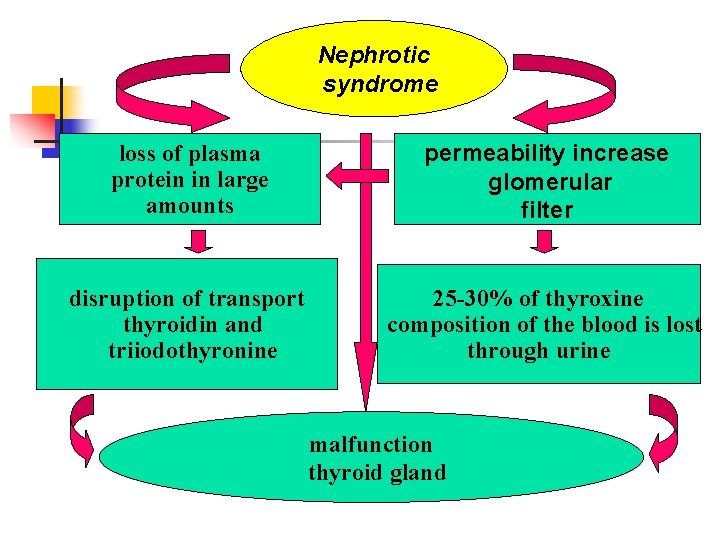
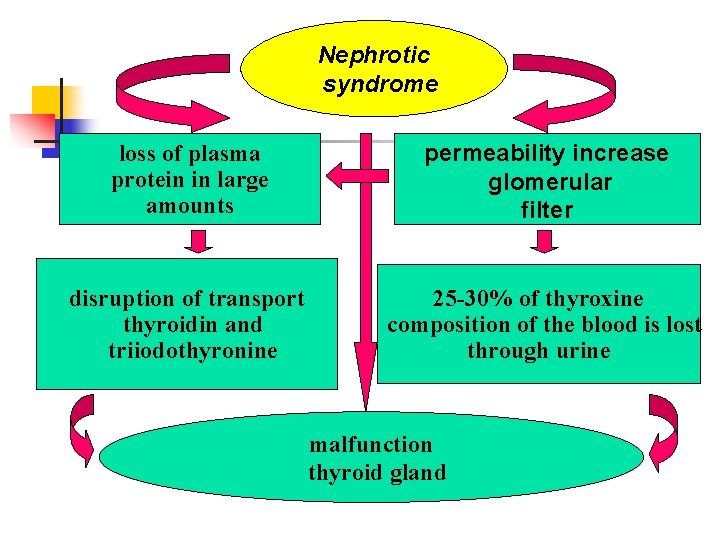
Nephrotic syndrome permeability increase glomerular filter loss of plasma protein in large amounts disruption of transport thyroidin and triiodothyronine 25 -30% of thyroxine composition of the blood is lost through urine malfunction thyroid gland
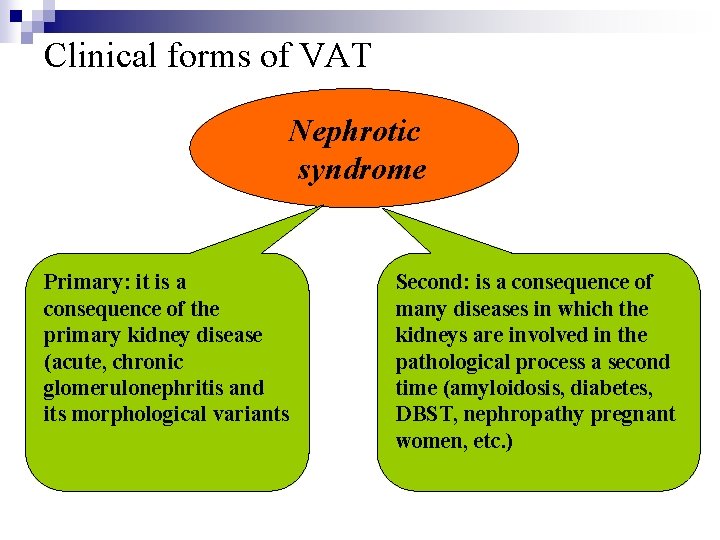
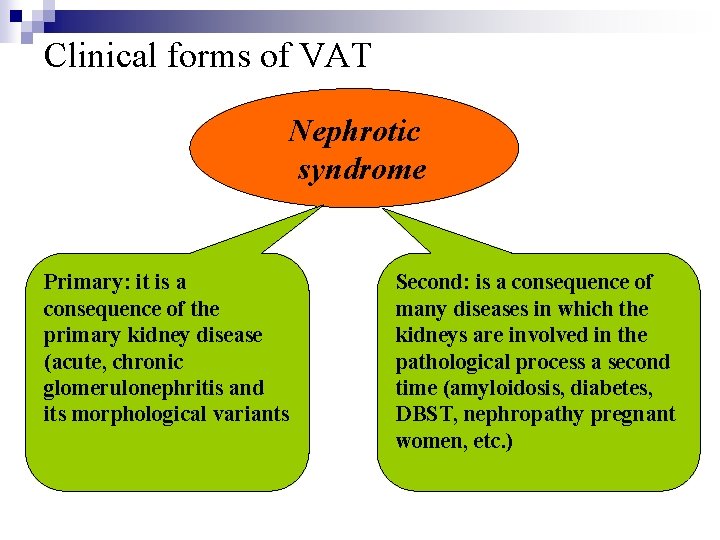
Clinical forms of VAT Nephrotic syndrome Primary: it is a consequence of the primary kidney disease (acute, chronic glomerulonephritis and its morphological variants Second: is a consequence of many diseases in which the kidneys are involved in the pathological process a second time (amyloidosis, diabetes, DBST, nephropathy pregnant women, etc. )
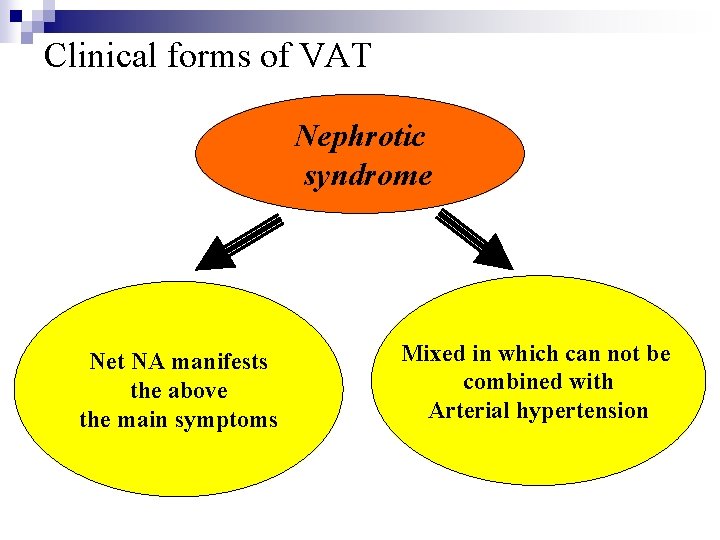
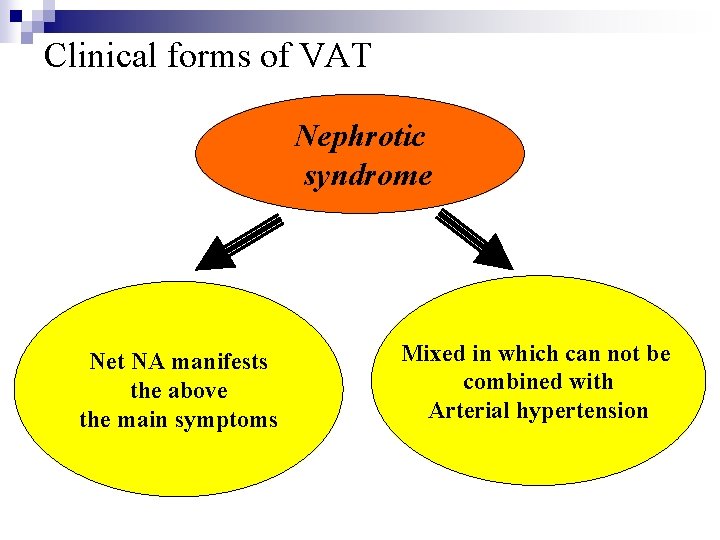
Clinical forms of VAT Nephrotic syndrome Net NA manifests the above the main symptoms Mixed in which can not be combined with Arterial hypertension
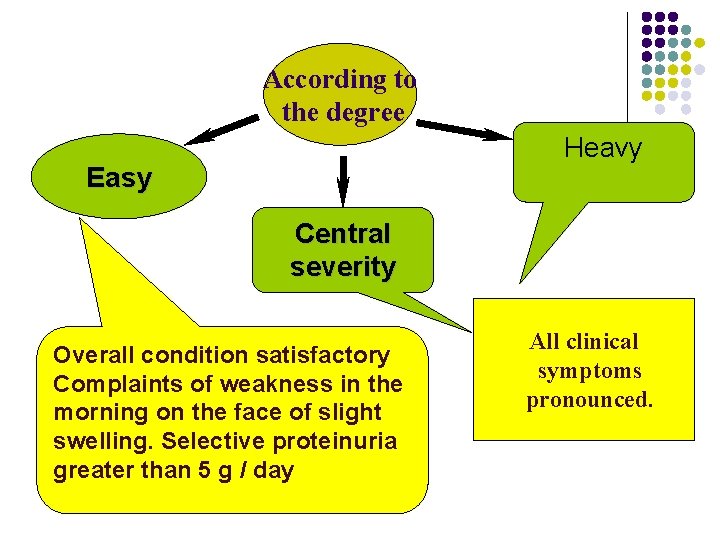
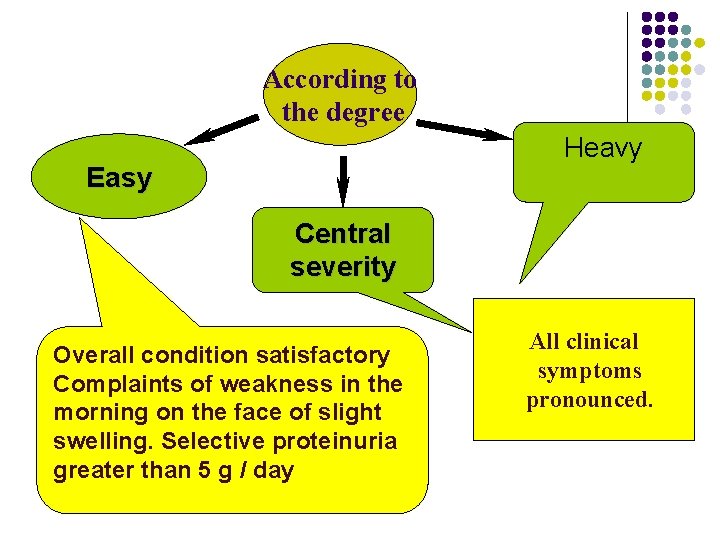
According to the degree Heavy Easy Central severity Overall condition satisfactory Complaints of weakness in the morning on the face of slight swelling. Selective proteinuria greater than 5 g / day All clinical symptoms pronounced.
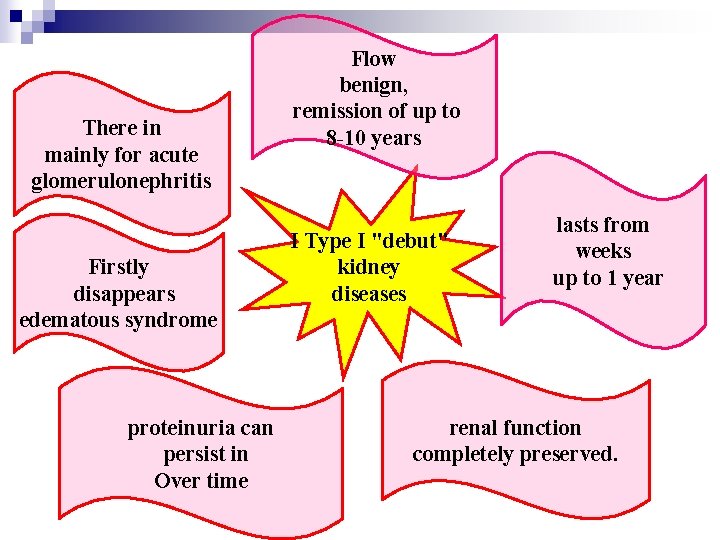
There are four types of flow
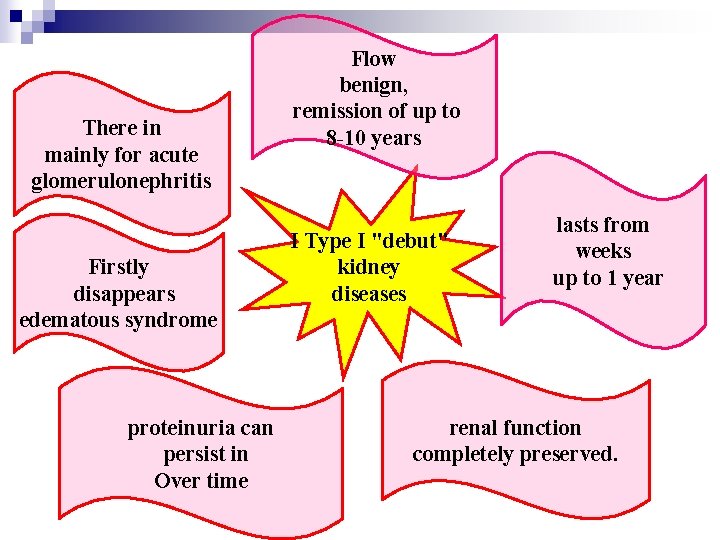
There in mainly for acute glomerulonephritis Firstly disappears edematous syndrome proteinuria can persist in Over time Flow benign, remission of up to 8 -10 years I Type I "debut" kidney diseases lasts from weeks up to 1 year renal function completely preserved.
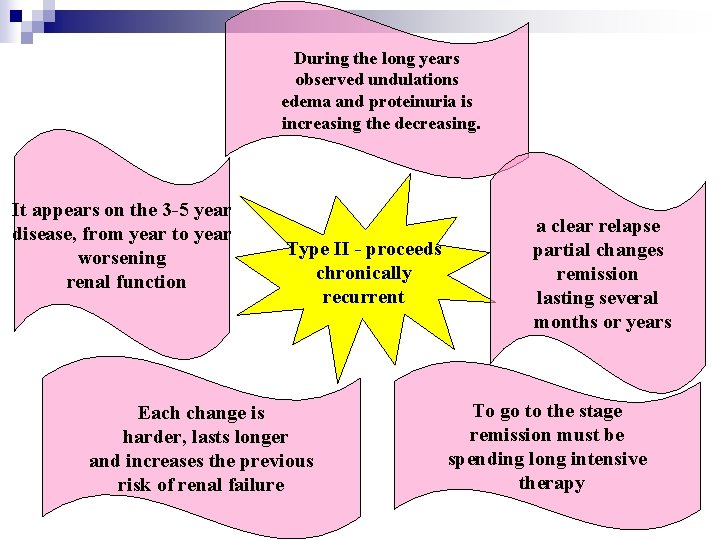
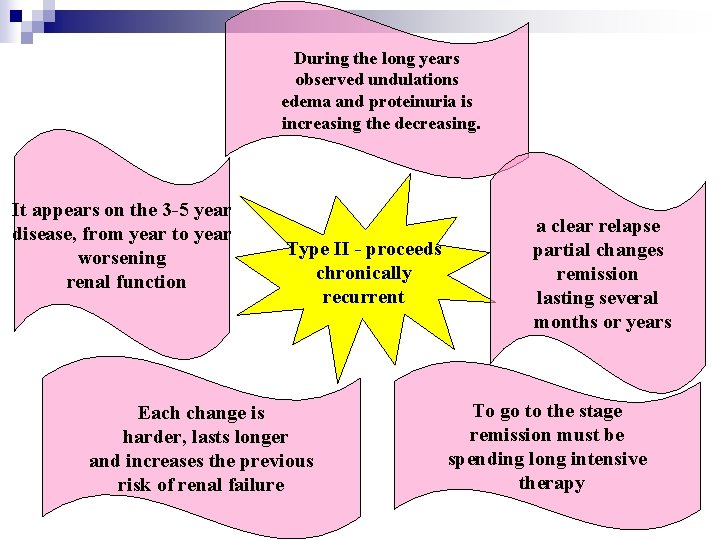
During the long years observed undulations edema and proteinuria is increasing the decreasing. It appears on the 3 -5 year disease, from year to year worsening renal function Type II - proceeds chronically recurrent Each change is harder, lasts longer and increases the previous risk of renal failure a clear relapse partial changes remission lasting several months or years To go to the stage remission must be spending long intensive therapy
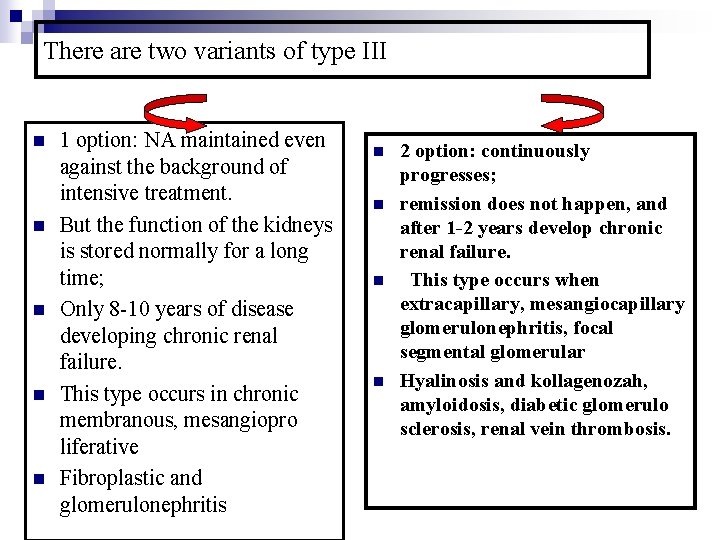
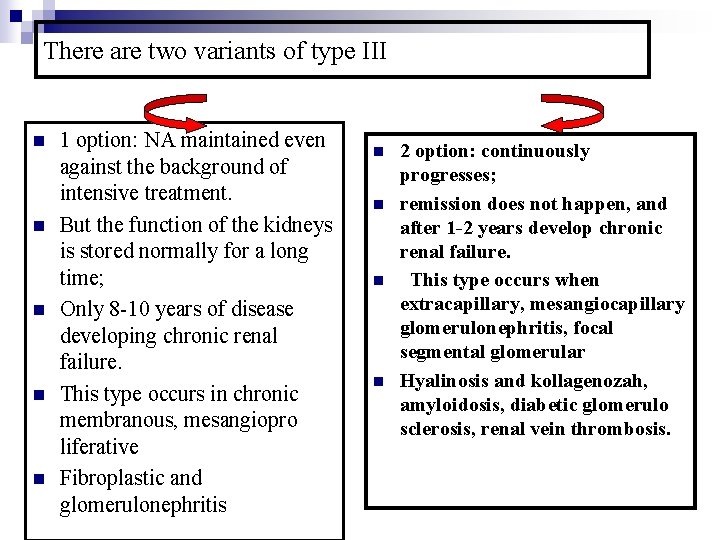
There are two variants of type III n n n 1 option: NA maintained even against the background of intensive treatment. But the function of the kidneys is stored normally for a long time; Only 8 -10 years of disease developing chronic renal failure. This type occurs in chronic membranous, mesangiopro liferative Fibroplastic and glomerulonephritis n n 2 option: continuously progresses; remission does not happen, and after 1 -2 years develop chronic renal failure. This type occurs when extracapillary, mesangiocapillary glomerulonephritis, focal segmental glomerular Hyalinosis and kollagenozah, amyloidosis, diabetic glomerulo sclerosis, renal vein thrombosis.
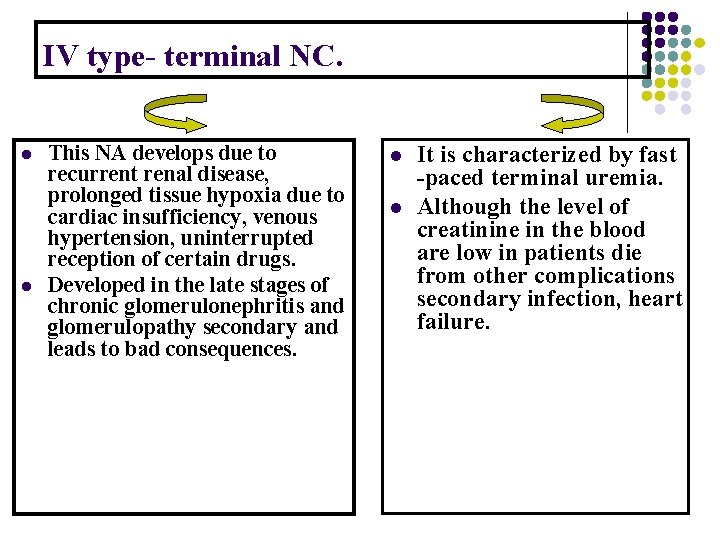
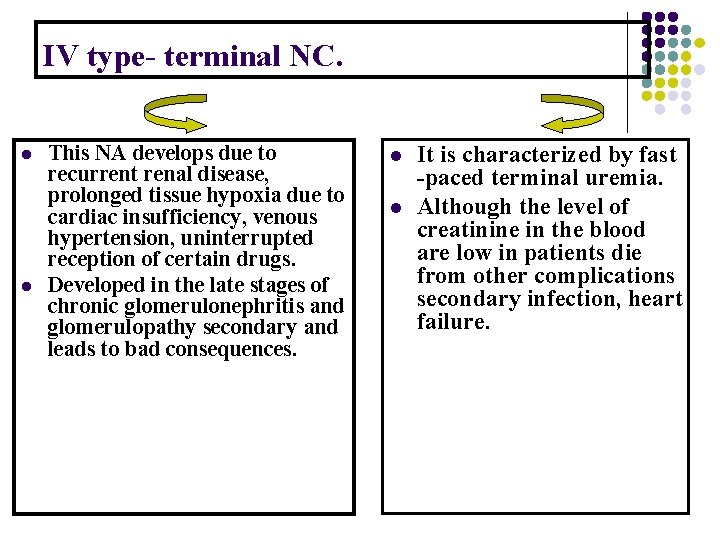
IV type- terminal NC. l l This NA develops due to recurrent renal disease, prolonged tissue hypoxia due to cardiac insufficiency, venous hypertension, uninterrupted reception of certain drugs. Developed in the late stages of chronic glomerulonephritis and glomerulopathy secondary and leads to bad consequences. l l It is characterized by fast -paced terminal uremia. Although the level of creatinine in the blood are low in patients die from other complications secondary infection, heart failure.
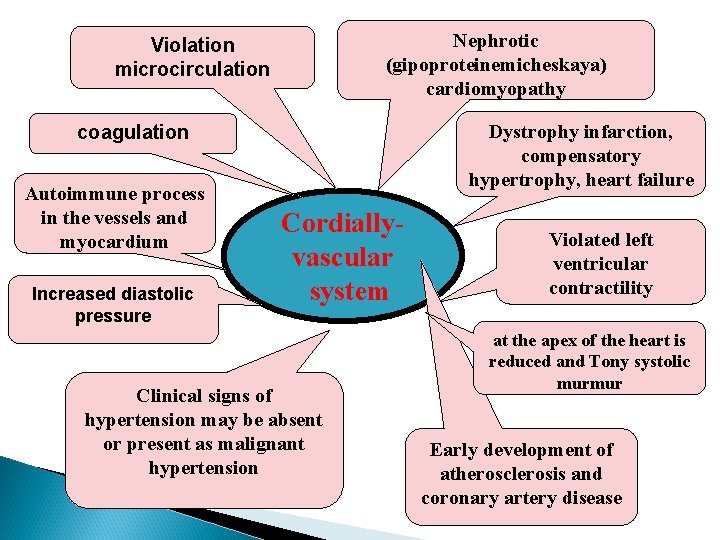
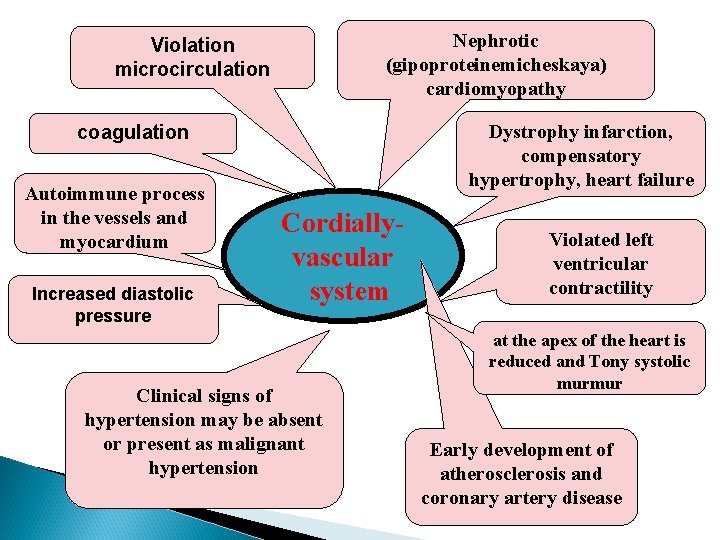
Nephrotic (gipoproteinemicheskaya) cardiomyopathy Violation microcirculation Dystrophy infarction, compensatory hypertrophy, heart failure coagulation Autoimmune process in the vessels and myocardium Increased diastolic pressure Cordiallyvascular system Clinical signs of hypertension may be absent or present as malignant hypertension Violated left ventricular contractility at the apex of the heart is reduced and Tony systolic murmur Early development of atherosclerosis and coronary artery disease
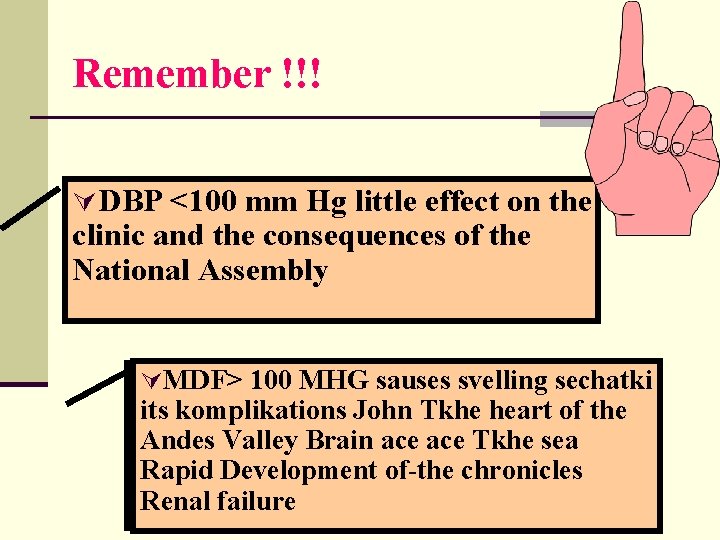
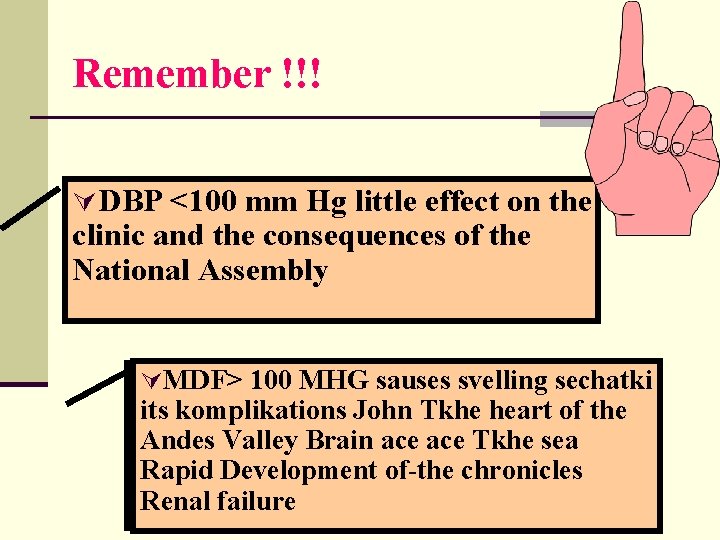
Remember !!! ÚDBP <100 mm Hg little effect on the clinic and the consequences of the National Assembly ÚMDF> 100 MHG sauses svelling sechatki its komplikations John Tkhe heart of the Andes Valley Brain ace Tkhe sea Rapid Development of-the chronicles Renal failure
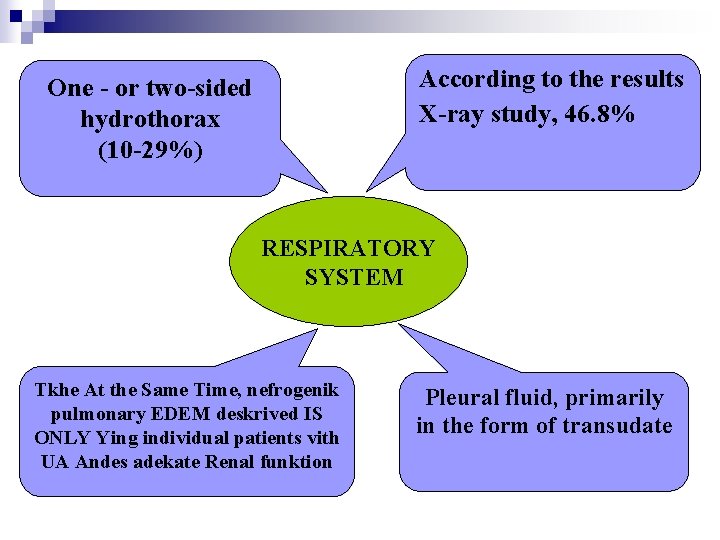
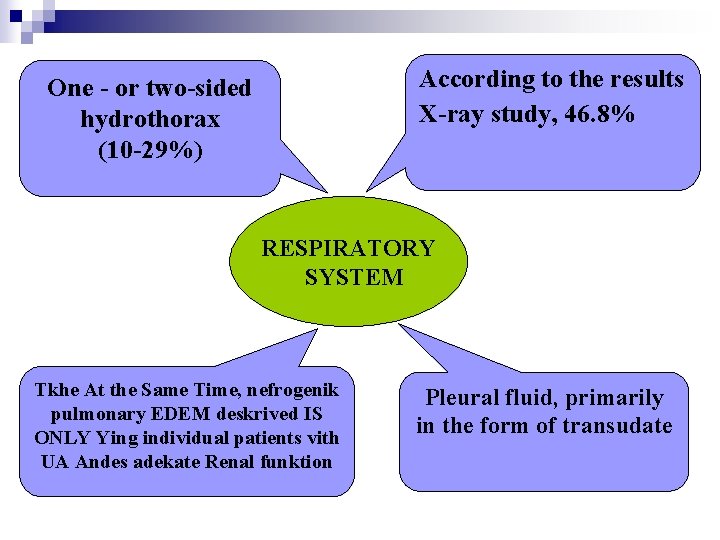
According to the results X-ray study, 46. 8% One - or two-sided hydrothorax (10 -29%) RESPIRATORY SYSTEM Tkhe At the Same Time, nefrogenik pulmonary EDEM deskrived IS ONLY Ying individual patients vith UA Andes adekate Renal funktion Pleural fluid, primarily in the form of transudate
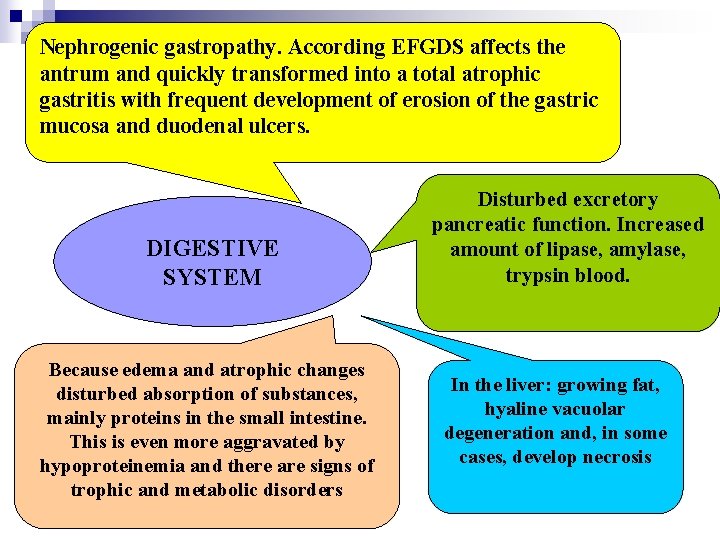
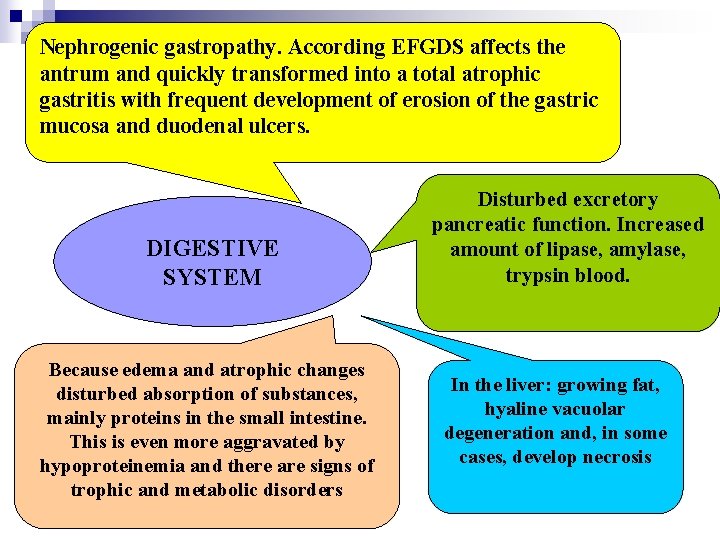
Nephrogenic gastropathy. According EFGDS affects the antrum and quickly transformed into a total atrophic gastritis with frequent development of erosion of the gastric mucosa and duodenal ulcers. DIGESTIVE SYSTEM Because edema and atrophic changes disturbed absorption of substances, mainly proteins in the small intestine. This is even more aggravated by hypoproteinemia and there are signs of trophic and metabolic disorders Disturbed excretory pancreatic function. Increased amount of lipase, amylase, trypsin blood. In the liver: growing fat, hyaline vacuolar degeneration and, in some cases, develop necrosis
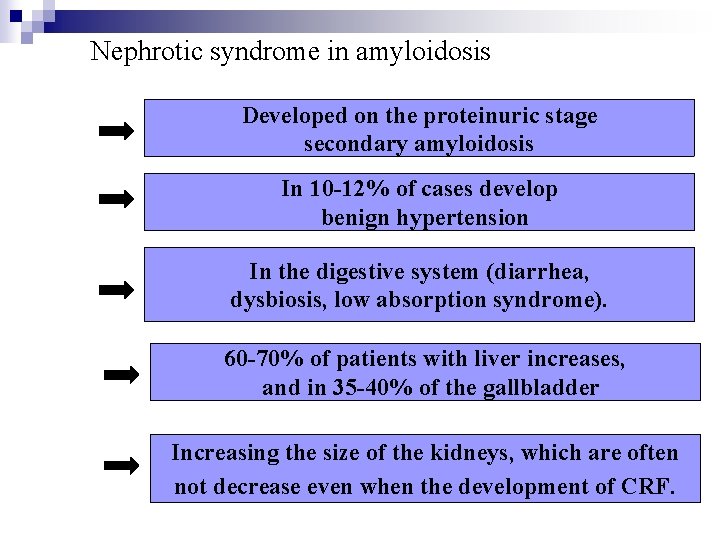
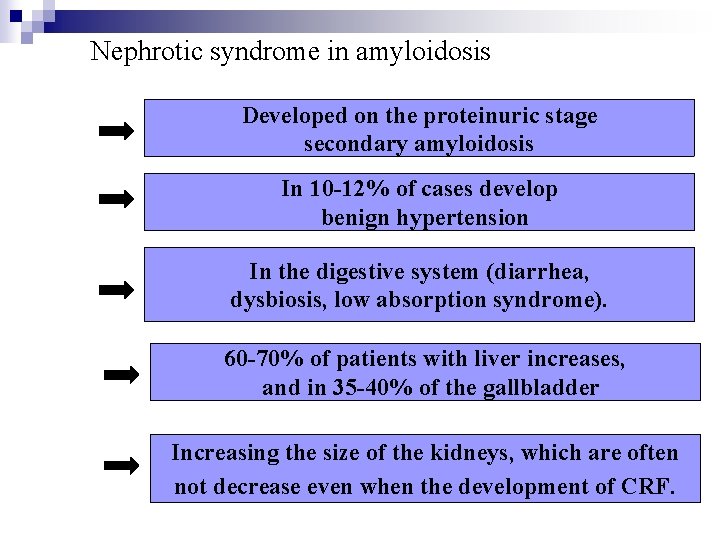
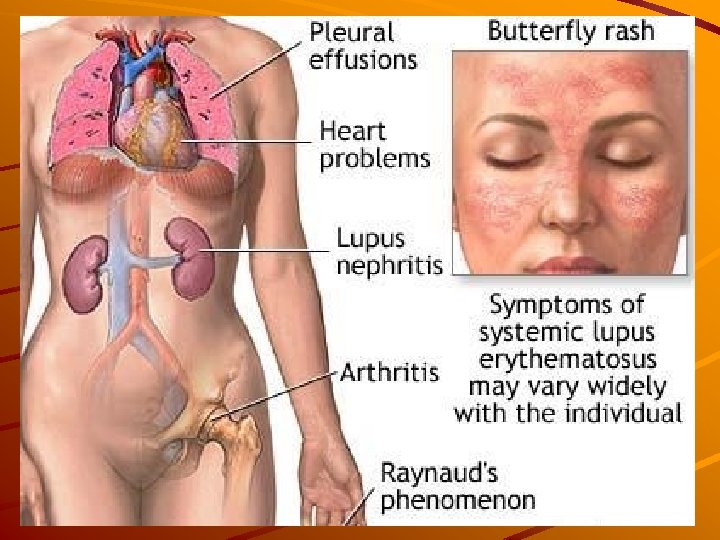
Nephrotic syndrome in amyloidosis Developed on the proteinuric stage secondary amyloidosis In 10 -12% of cases develop benign hypertension In the digestive system (diarrhea, dysbiosis, low absorption syndrome). 60 -70% of patients with liver increases, and in 35 -40% of the gallbladder Increasing the size of the kidneys, which are often not decrease even when the development of CRF.
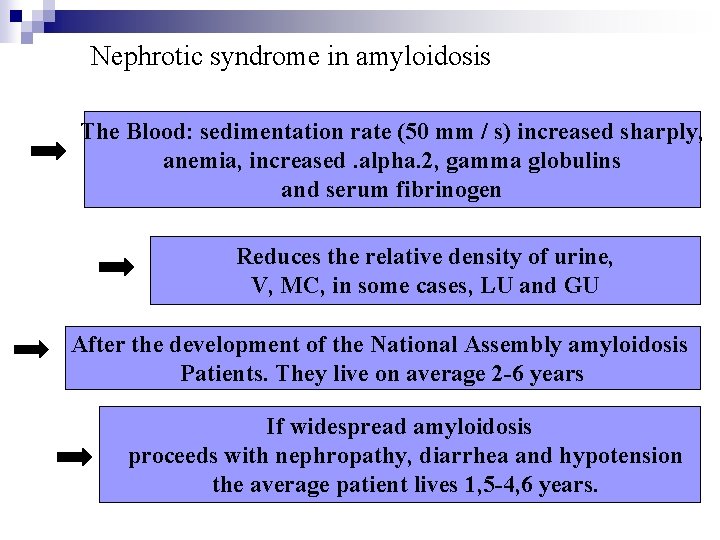
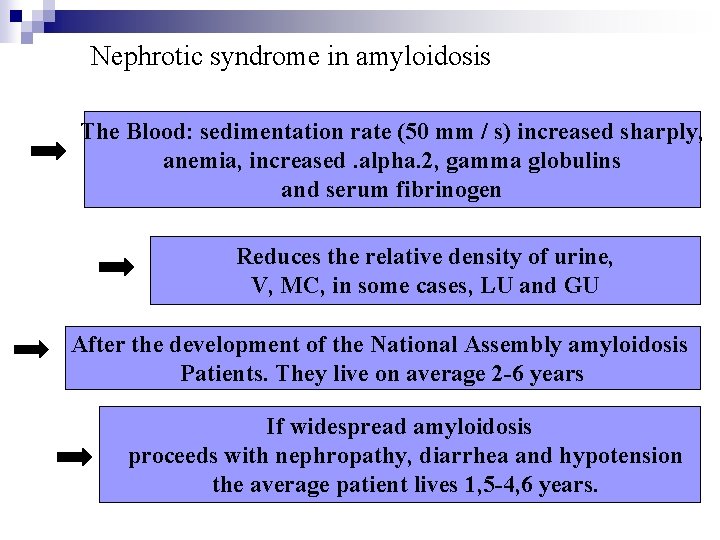
Nephrotic syndrome in amyloidosis The Blood: sedimentation rate (50 mm / s) increased sharply, anemia, increased. alpha. 2, gamma globulins and serum fibrinogen Reduces the relative density of urine, V, MC, in some cases, LU and GU After the development of the National Assembly amyloidosis Patients. They live on average 2 -6 years If widespread amyloidosis proceeds with nephropathy, diarrhea and hypotension the average patient lives 1, 5 -4, 6 years.
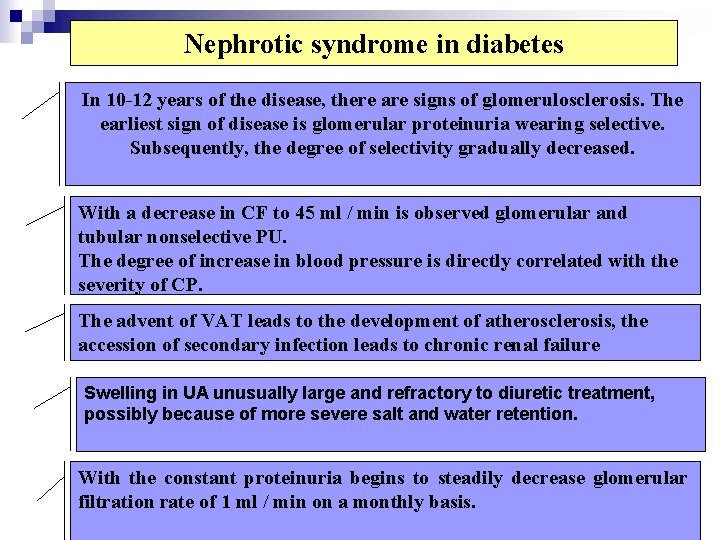
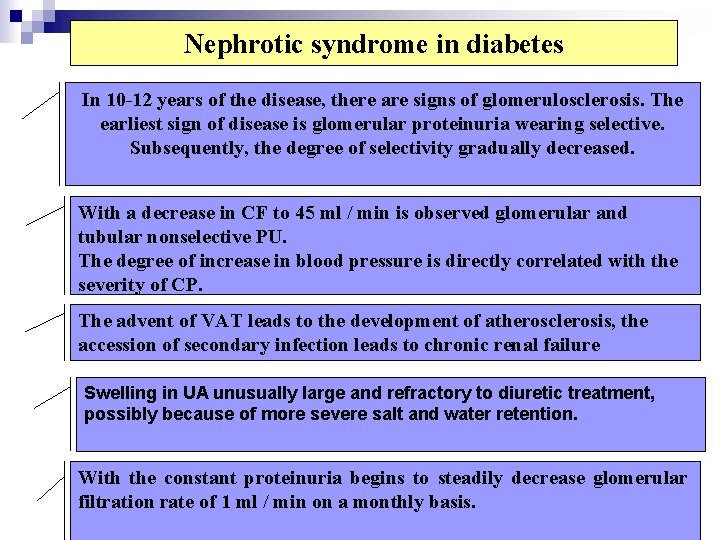
Nephrotic syndrome in diabetes In 10 -12 years of the disease, there are signs of glomerulosclerosis. The earliest sign of disease is glomerular proteinuria wearing selective. Subsequently, the degree of selectivity gradually decreased. With a decrease in CF to 45 ml / min is observed glomerular and tubular nonselective PU. The degree of increase in blood pressure is directly correlated with the severity of CP. The advent of VAT leads to the development of atherosclerosis, the accession of secondary infection leads to chronic renal failure Swelling in UA unusually large and refractory to diuretic treatment, possibly because of more severe salt and water retention. With the constant proteinuria begins to steadily decrease glomerular filtration rate of 1 ml / min on a monthly basis.
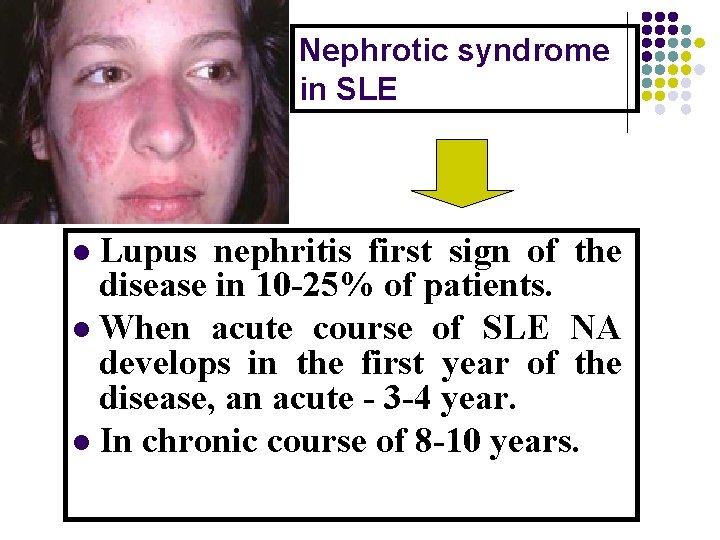
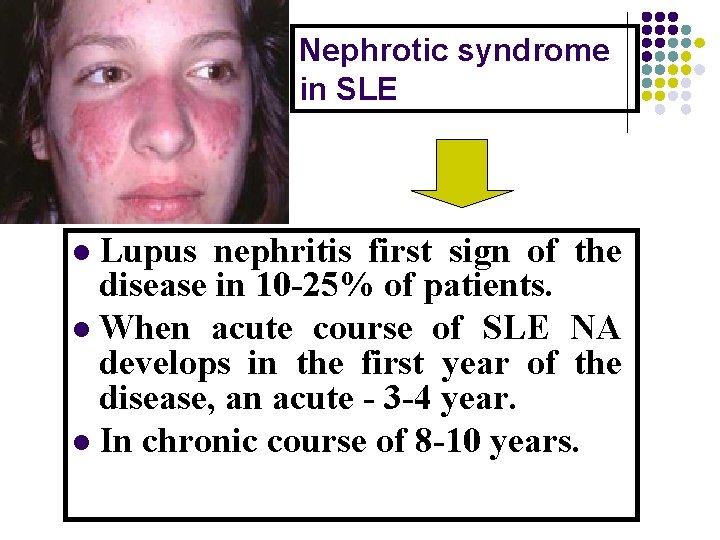
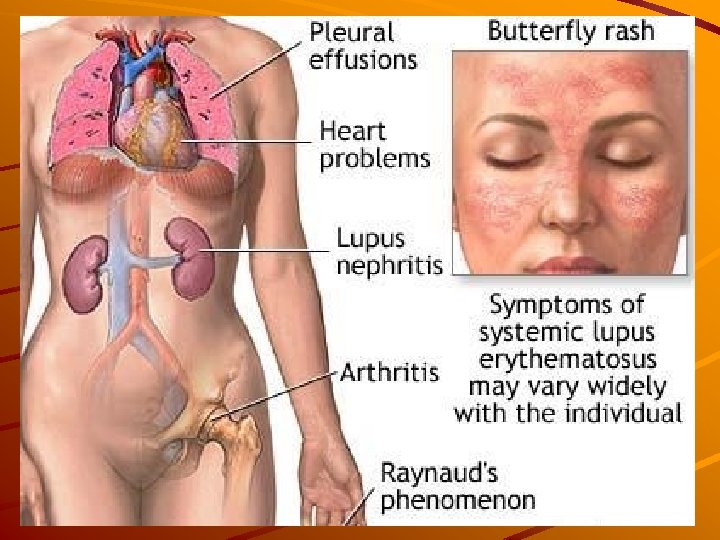
Nephrotic syndrome in SLE Lupus nephritis first sign of the disease in 10 -25% of patients. l When acute course of SLE NA develops in the first year of the disease, an acute - 3 -4 year. l In chronic course of 8 -10 years. l
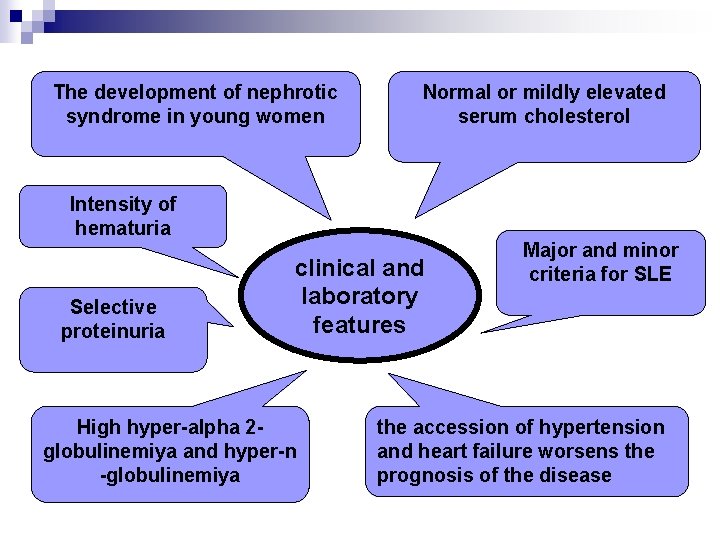
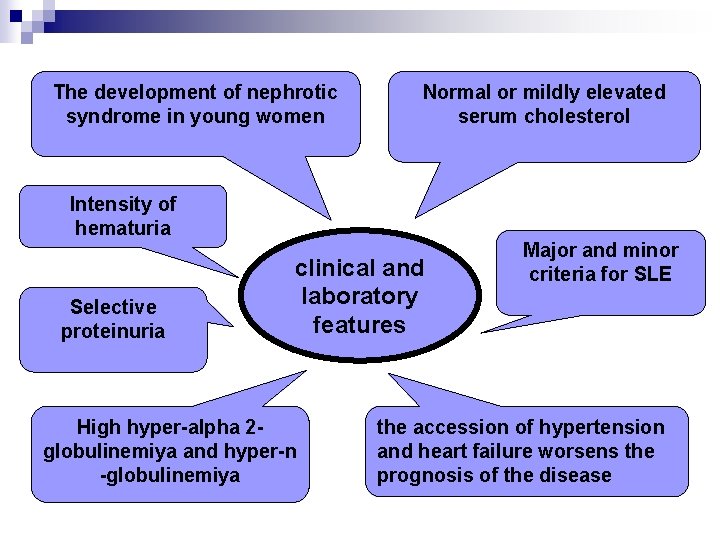
The development of nephrotic syndrome in young women Normal or mildly elevated serum cholesterol Intensity of hematuria Selective proteinuria clinical and laboratory features High hyper-alpha 2 globulinemiya and hyper-n -globulinemiya Major and minor criteria for SLE the accession of hypertension and heart failure worsens the prognosis of the disease
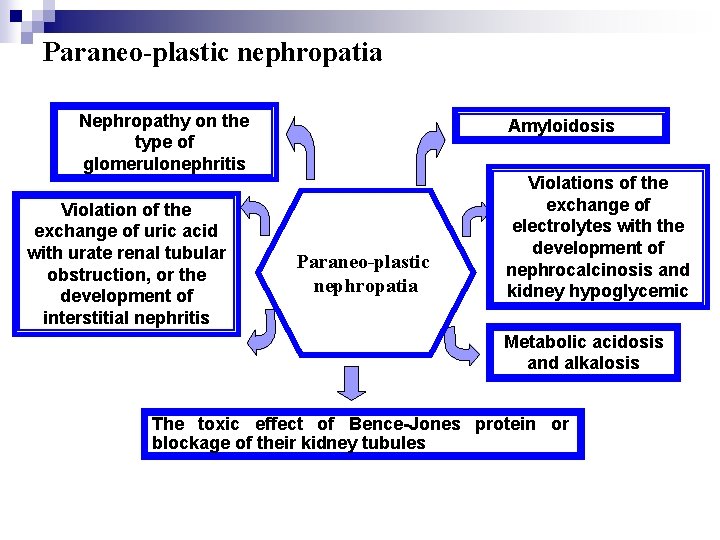
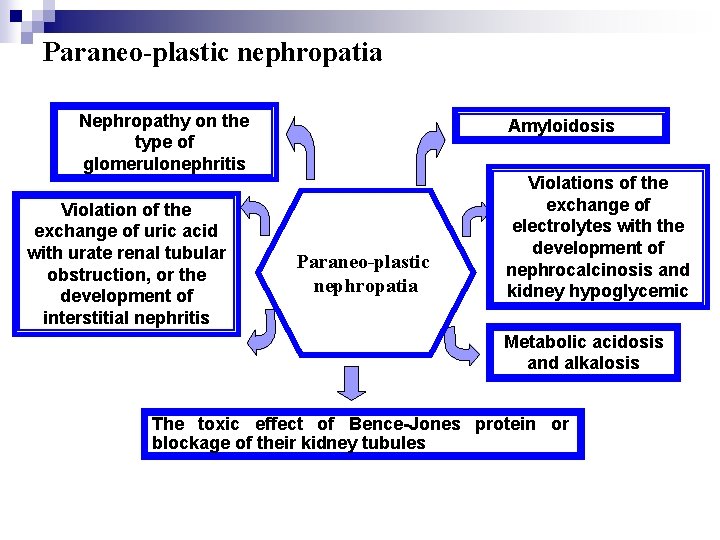
Paraneo-plastic nephropatia Nephropathy on the type of glomerulonephritis Violation of the exchange of uric acid with urate renal tubular obstruction, or the development of interstitial nephritis Amyloidosis Paraneo-plastic nephropatia Violations of the exchange of electrolytes with the development of nephrocalcinosis and kidney hypoglycemic Metabolic acidosis and alkalosis The toxic effect of Bence-Jones protein or blockage of their kidney tubules
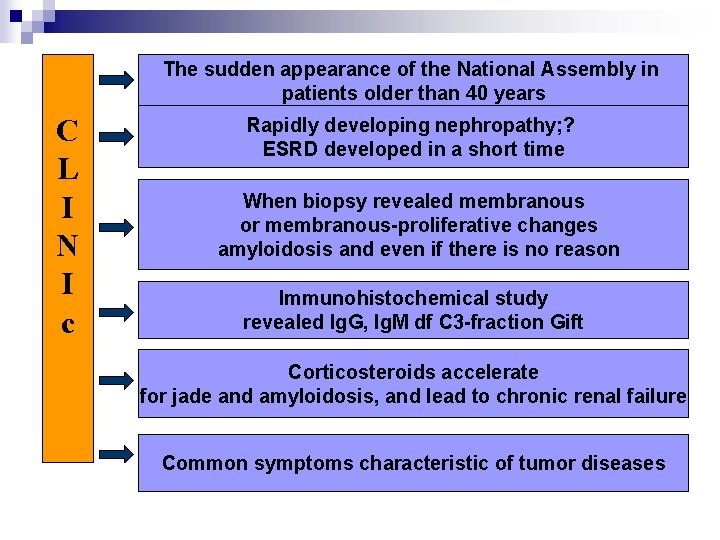
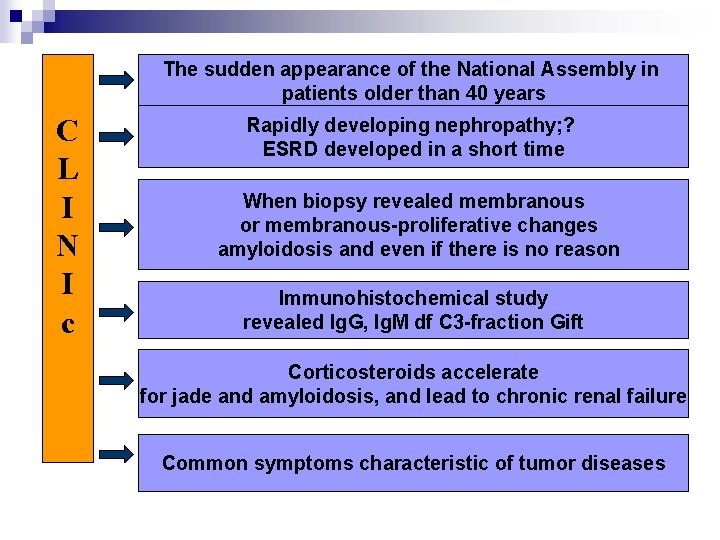
The sudden appearance of the National Assembly in patients older than 40 years C L I N I c Rapidly developing nephropathy; ? ESRD developed in a short time When biopsy revealed membranous or membranous-proliferative changes amyloidosis and even if there is no reason Immunohistochemical study revealed Ig. G, Ig. M df C 3 -fraction Gift Corticosteroids accelerate for jade and amyloidosis, and lead to chronic renal failure Common symptoms characteristic of tumor diseases
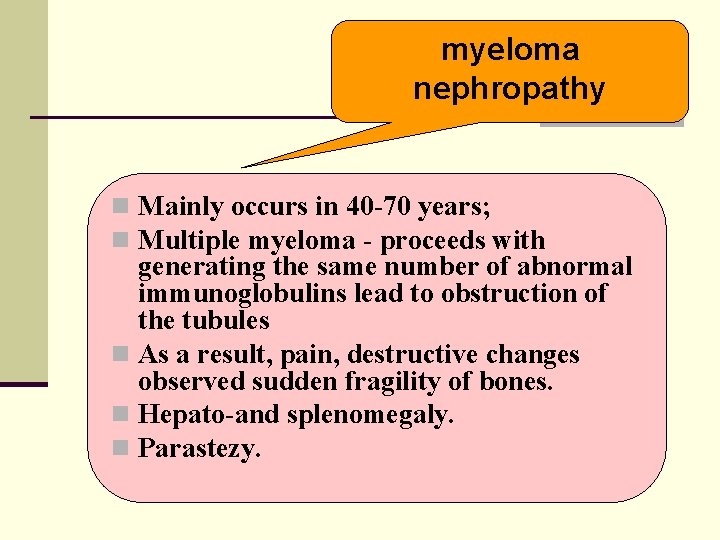
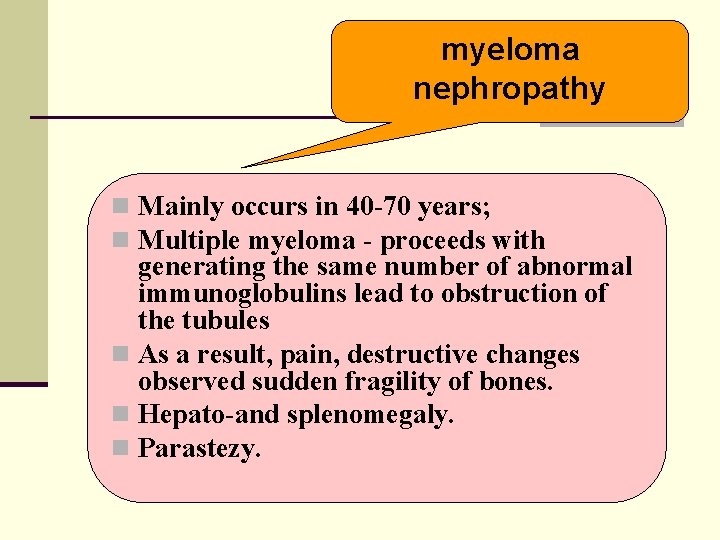
myeloma nephropathy n Mainly occurs in 40 -70 years; n Multiple myeloma - proceeds with generating the same number of abnormal immunoglobulins lead to obstruction of the tubules n As a result, pain, destructive changes observed sudden fragility of bones. n Hepato-and splenomegaly. n Parastezy.
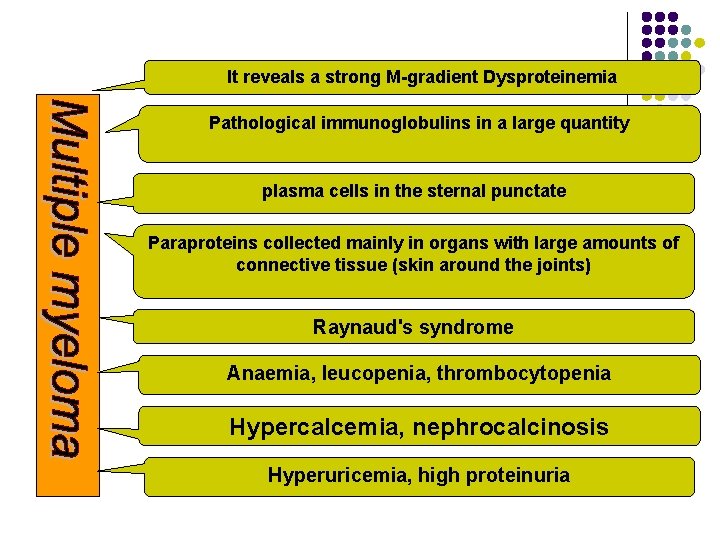
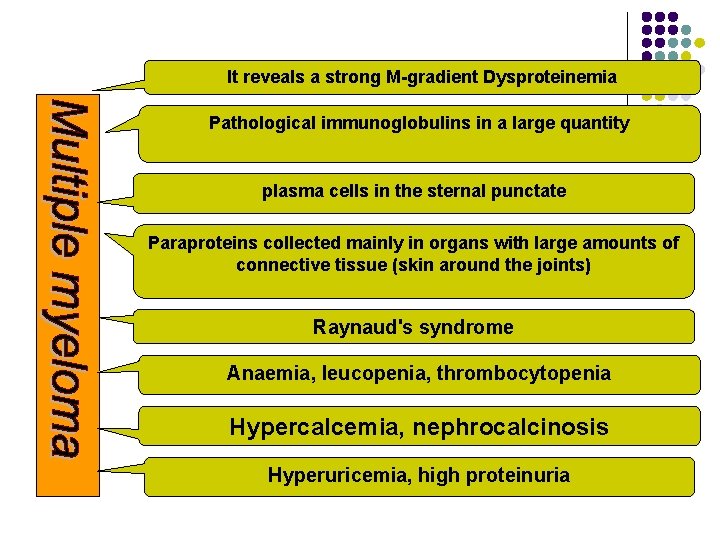
It reveals a strong M-gradient Dysproteinemia Pathological immunoglobulins in a large quantity plasma cells in the sternal punctate Paraproteins collected mainly in organs with large amounts of connective tissue (skin around the joints) Raynaud's syndrome Anaemia, leucopenia, thrombocytopenia Hypercalcemia, nephrocalcinosis Hyperuricemia, high proteinuria
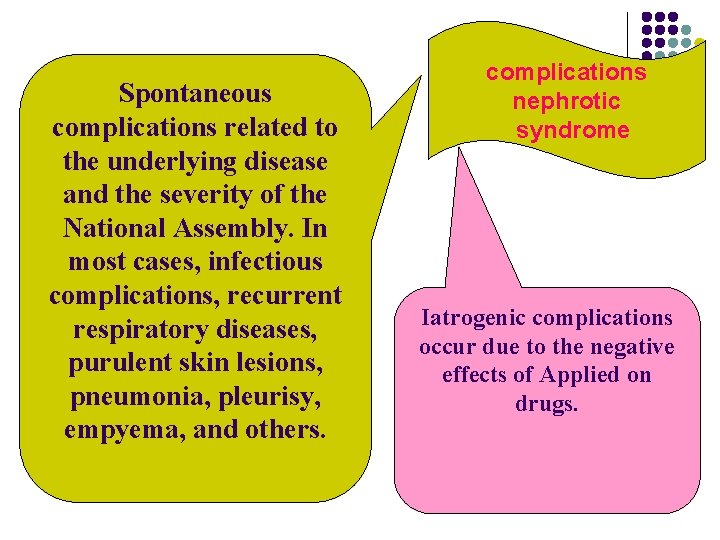
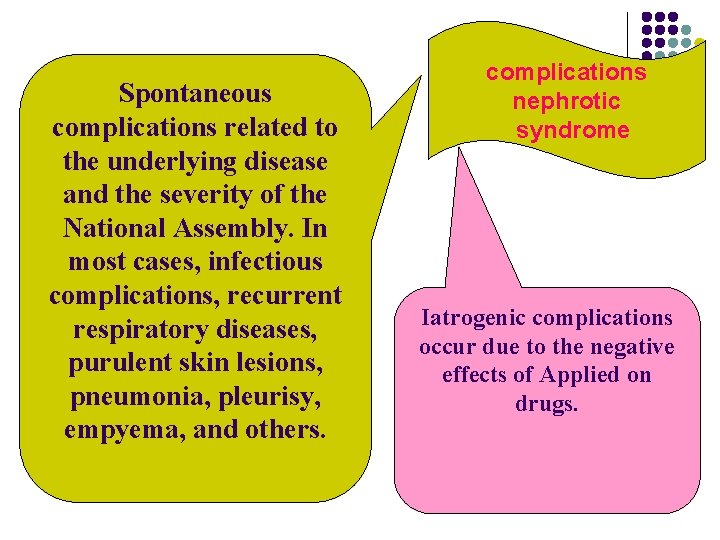
Spontaneous complications related to the underlying disease and the severity of the National Assembly. In most cases, infectious complications, recurrent respiratory diseases, purulent skin lesions, pneumonia, pleurisy, empyema, and others. complications nephrotic syndrome Iatrogenic complications occur due to the negative effects of Applied on drugs.
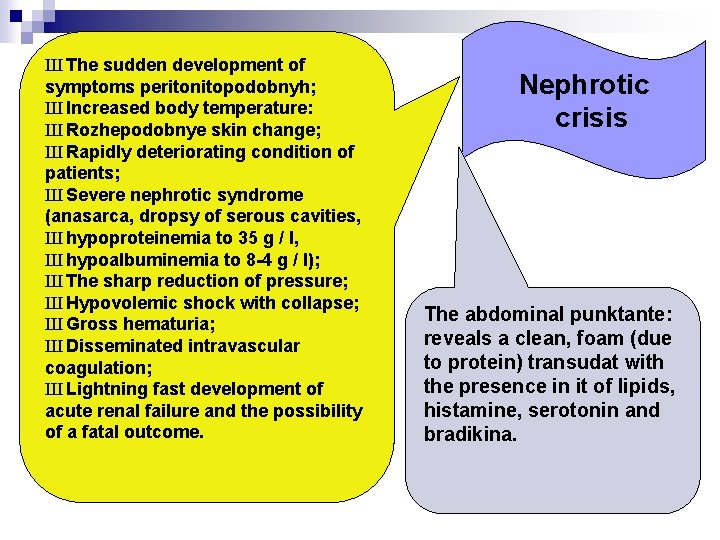
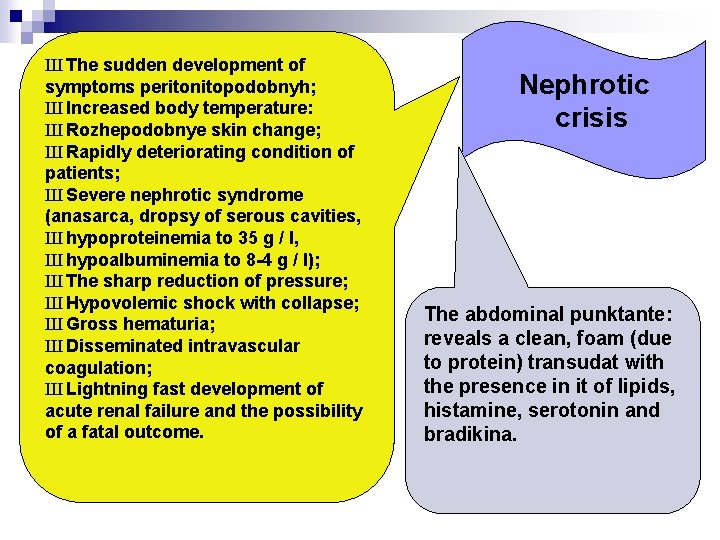
Ш The sudden development of symptoms peritonitopodobnyh; Ш Increased body temperature: Ш Rozhepodobnye skin change; Ш Rapidly deteriorating condition of patients; Ш Severe nephrotic syndrome (anasarca, dropsy of serous cavities, Ш hypoproteinemia to 35 g / l, Ш hypoalbuminemia to 8 -4 g / l); Ш The sharp reduction of pressure; Ш Hypovolemic shock with collapse; Ш Gross hematuria; Ш Disseminated intravascular coagulation; Ш Lightning fast development of acute renal failure and the possibility of a fatal outcome. Nephrotic crisis The abdominal punktante: reveals a clean, foam (due to protein) transudat with the presence in it of lipids, histamine, serotonin and bradikina.
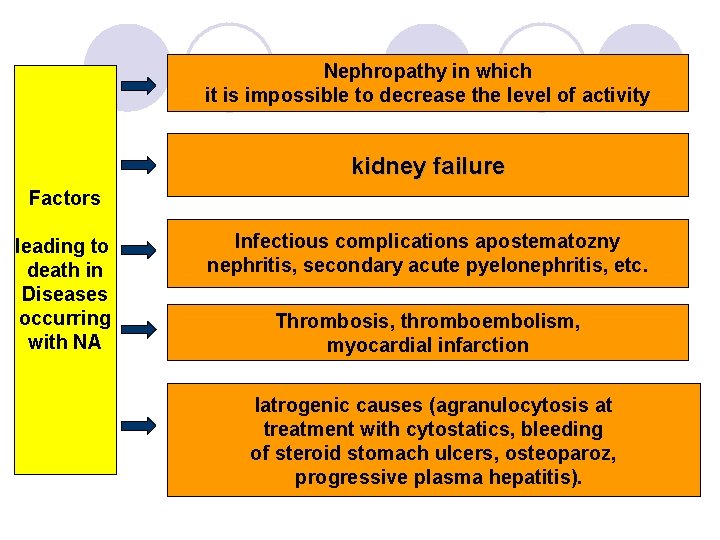
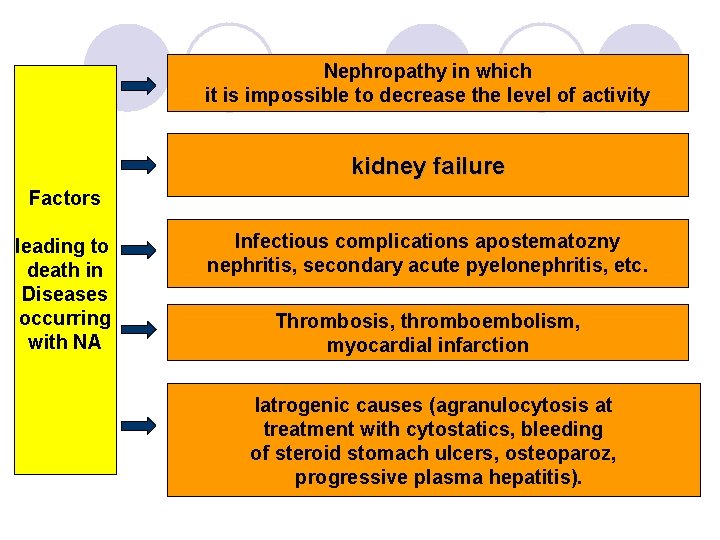
Nephropathy in which it is impossible to decrease the level of activity kidney failure Factors leading to death in Diseases occurring with NA Infectious complications apostematozny nephritis, secondary acute pyelonephritis, etc. Thrombosis, thromboembolism, myocardial infarction Iatrogenic causes (agranulocytosis at treatment with cytostatics, bleeding of steroid stomach ulcers, osteoparoz, progressive plasma hepatitis).
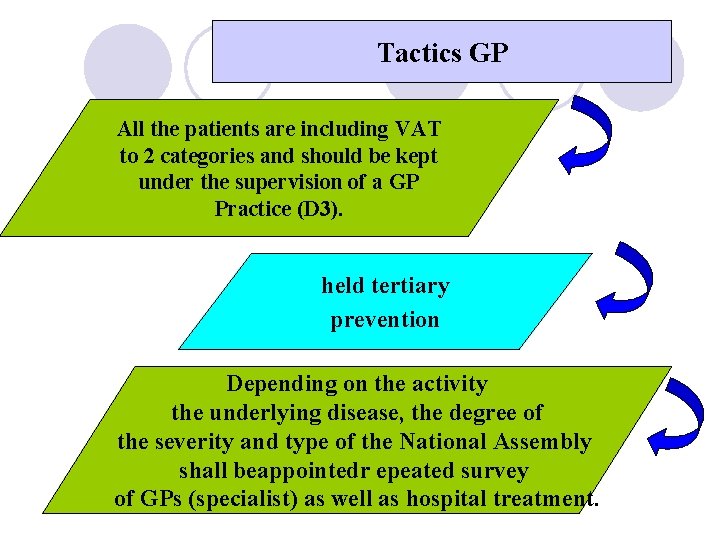
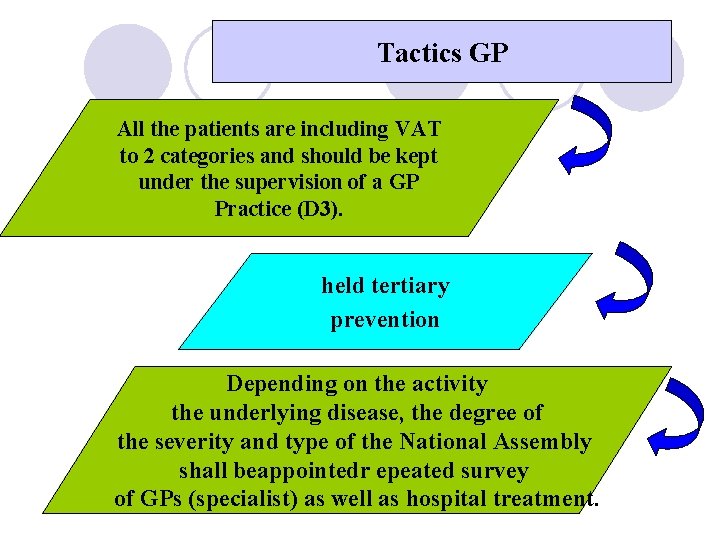
Tactics GP All the patients are including VAT to 2 categories and should be kept under the supervision of a GP Practice (D 3). held tertiary prevention Depending on the activity the underlying disease, the degree of the severity and type of the National Assembly shall beappointedr epeated survey of GPs (specialist) as well as hospital treatment.
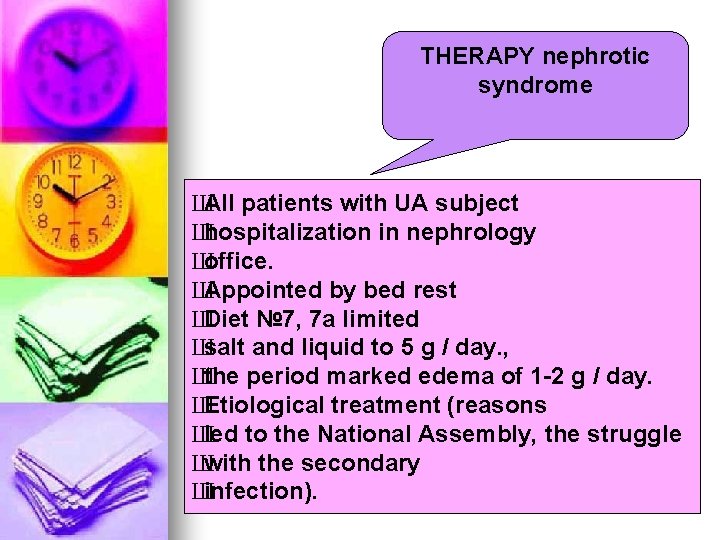
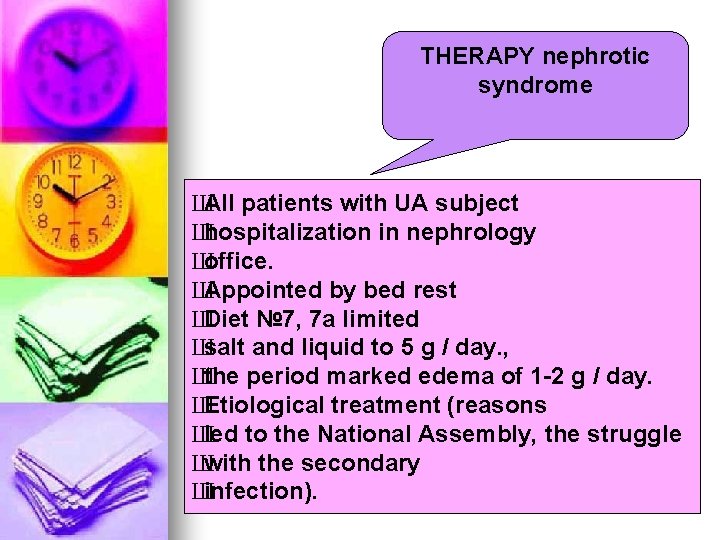
THERAPY nephrotic syndrome Ш All patients with UA subject Ш hospitalization in nephrology Ш office. Ш Appointed by bed rest Ш Diet № 7, 7 a limited Ш salt and liquid to 5 g / day. , Ш the period marked edema of 1 -2 g / day. Ш Etiological treatment (reasons Ш led to the National Assembly, the struggle Ш with the secondary Ш infection).
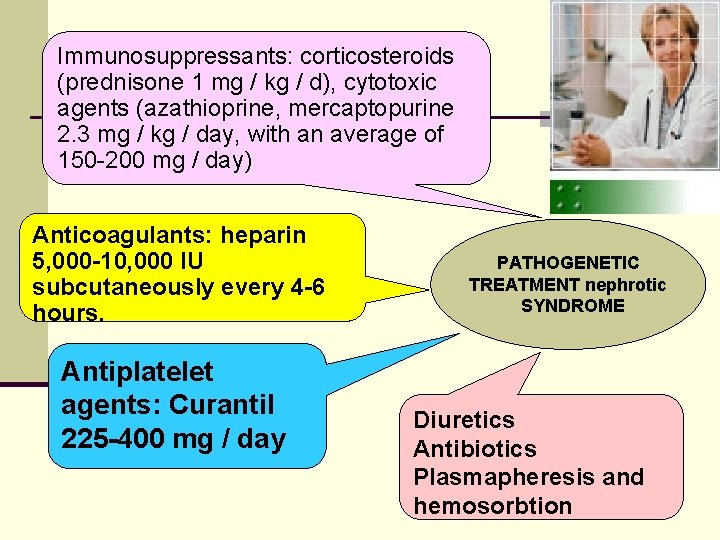
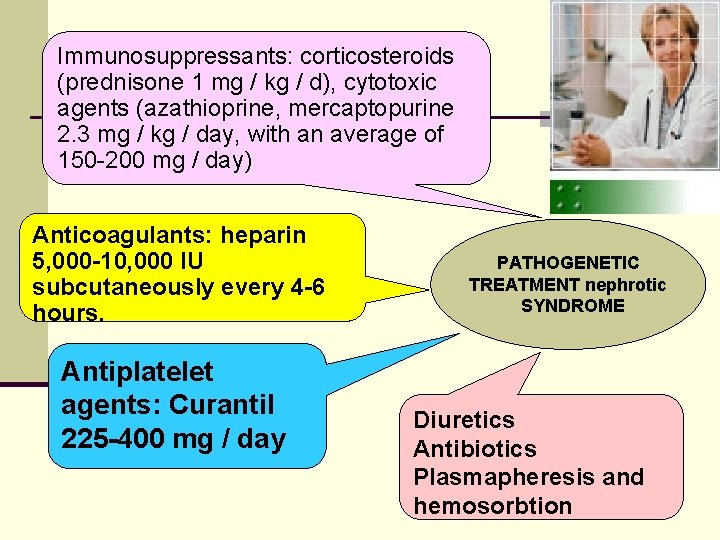
Immunosuppressants: corticosteroids (prednisone 1 mg / kg / d), cytotoxic agents (azathioprine, mercaptopurine 2. 3 mg / kg / day, with an average of 150 -200 mg / day) Anticoagulants: heparin 5, 000 -10, 000 IU subcutaneously every 4 -6 hours. Antiplatelet agents: Curantil 225 -400 mg / day PATHOGENETIC TREATMENT nephrotic SYNDROME Diuretics Antibiotics Plasmapheresis and hemosorbtion
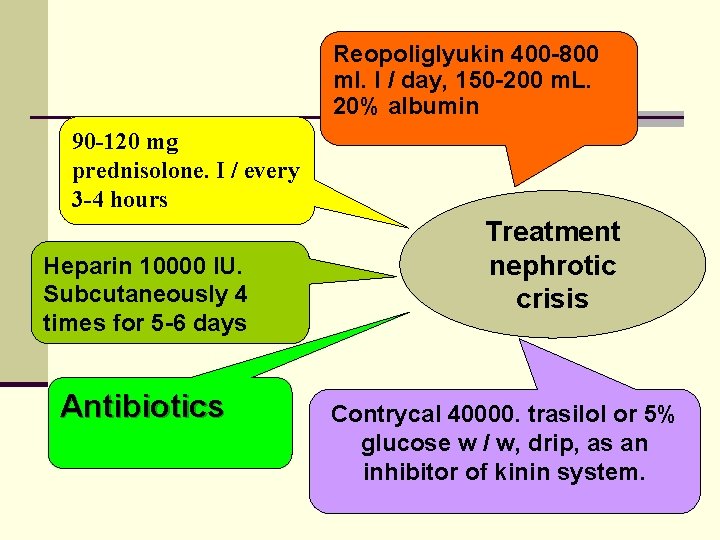
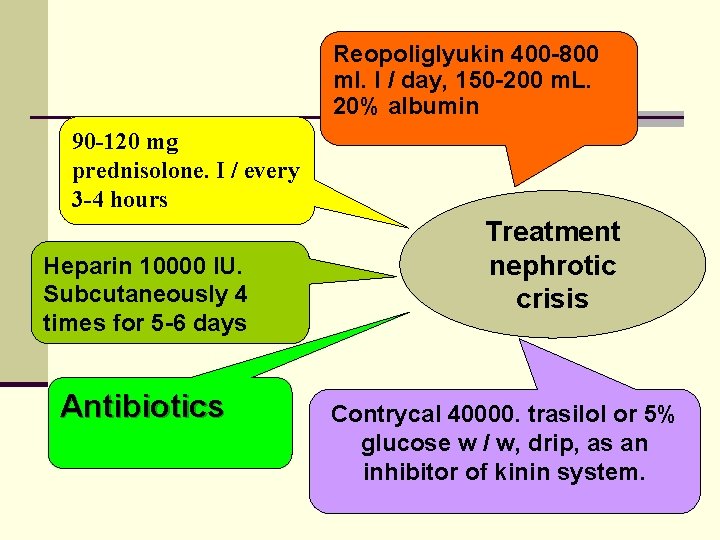
Reopoliglyukin 400 -800 ml. I / day, 150 -200 m. L. 20% albumin 90 -120 mg prednisolone. I / every 3 -4 hours Heparin 10000 IU. Subcutaneously 4 times for 5 -6 days Antibiotics Treatment nephrotic crisis Contrycal 40000. trasilol or 5% glucose w / w, drip, as an inhibitor of kinin system.
 Nephrotic syndrome differential diagnosis
Nephrotic syndrome differential diagnosis Kara potter
Kara potter Dr. kriti mohan
Dr. kriti mohan Primary and secondary causes of nephrotic syndrome
Primary and secondary causes of nephrotic syndrome Classes of corticosteroids
Classes of corticosteroids Why there is hyperlipidemia in nephrotic syndrome
Why there is hyperlipidemia in nephrotic syndrome Nephrotic syndrome
Nephrotic syndrome Nephrotic syndrome criteria
Nephrotic syndrome criteria Nephrotic syndrome
Nephrotic syndrome Nephrotic syndrome
Nephrotic syndrome Protein electrophoresis interpretation
Protein electrophoresis interpretation Nephrotic syndrome in child
Nephrotic syndrome in child Carpal tunnel
Carpal tunnel Osteochondrosis
Osteochondrosis Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Ongoing planning in nursing process
Ongoing planning in nursing process Types of nursing diagnosis
Types of nursing diagnosis Nursing process and critical thinking
Nursing process and critical thinking Early pregnancy pictures of spotting during pregnancy
Early pregnancy pictures of spotting during pregnancy Polycythemia differential diagnosis
Polycythemia differential diagnosis Differential diagnosis of learning disabilities
Differential diagnosis of learning disabilities Iron deficiency anemia differential diagnosis
Iron deficiency anemia differential diagnosis Brainstem stroke syndromes
Brainstem stroke syndromes Chicken pix los pinos menu
Chicken pix los pinos menu Yap göster söyle yaz örnekleri
Yap göster söyle yaz örnekleri Differential diagnosis of stroke
Differential diagnosis of stroke Osgood schlatter vs patellar tendonitis
Osgood schlatter vs patellar tendonitis Acute productive cough differential diagnosis
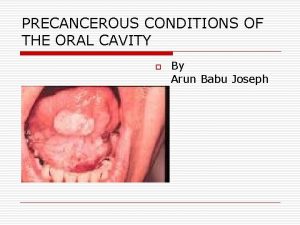
Acute productive cough differential diagnosis Osmf differential diagnosis
Osmf differential diagnosis Normocytic hypochromic anemia differential diagnosis
Normocytic hypochromic anemia differential diagnosis Differential diagnosis for pericarditis
Differential diagnosis for pericarditis Haemtemesis
Haemtemesis Vitamin c differential diagnosis mnemonic
Vitamin c differential diagnosis mnemonic Fairy skin
Fairy skin Obstructive jaundice differential diagnosis
Obstructive jaundice differential diagnosis Differentials of hydrocephalus
Differentials of hydrocephalus Ivor lewis surgery
Ivor lewis surgery Vitamin d differential diagnosis mnemonic
Vitamin d differential diagnosis mnemonic Phlebolymphedema
Phlebolymphedema Differential diagnosis of otitis externa
Differential diagnosis of otitis externa Breast cancer staging chart
Breast cancer staging chart Uveitis definition
Uveitis definition Differential diagnosis red eye
Differential diagnosis red eye Leukocoria differential diagnosis
Leukocoria differential diagnosis Lymphedema differential diagnosis
Lymphedema differential diagnosis Epigastric pain differential diagnosis
Epigastric pain differential diagnosis Pulmonary hypertension differential diagnosis
Pulmonary hypertension differential diagnosis