Approach to myopathy 1 The first goal in











- Slides: 83
Approach to myopathy
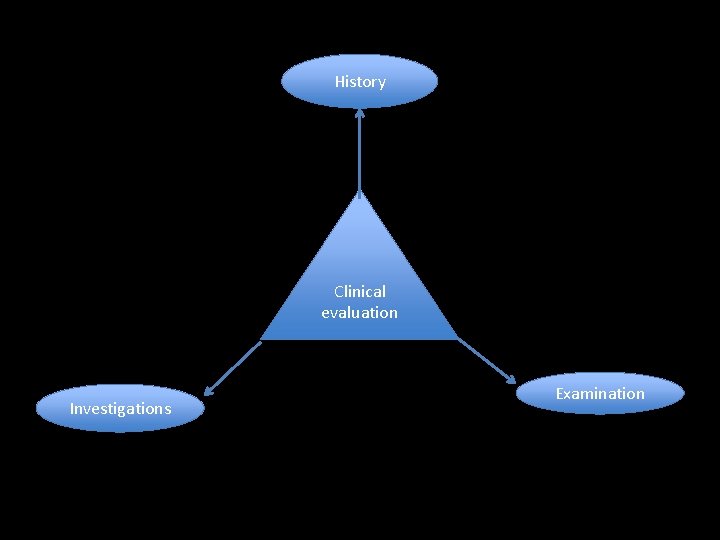
1. The first goal in approaching a patient with a suspected muscle disease is to determine the correct site of the lesion. 1. The second goal is to determine the cause of the myopathy. 1. The third goal is to determine whether a specific treatment is available and if not, to optimally manage the patient’s symptoms to maximize his or her functional abilities and enhance quality of life.

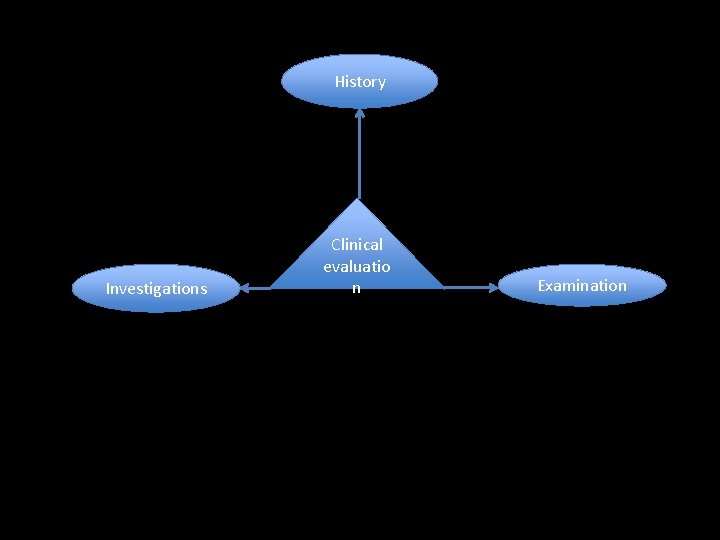
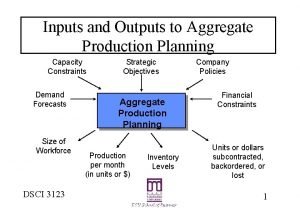
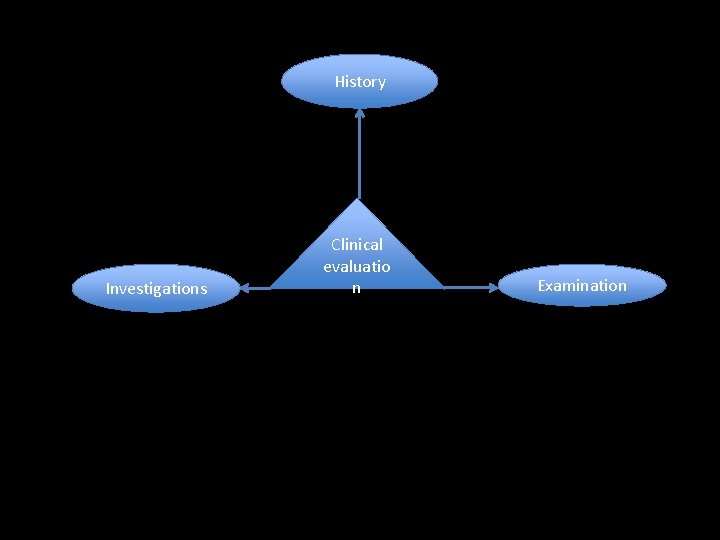
History Investigations Clinical evaluatio n Examination
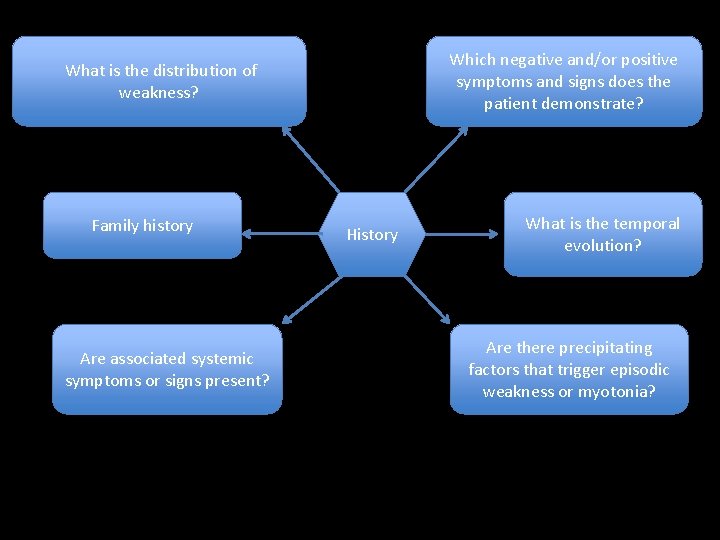
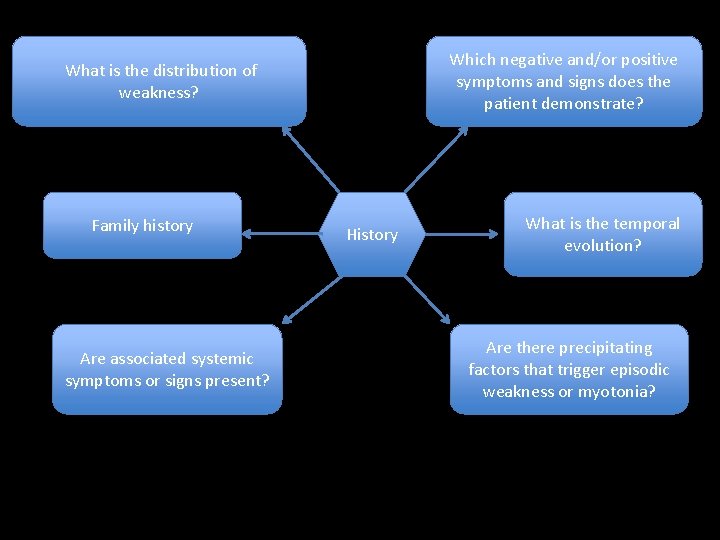
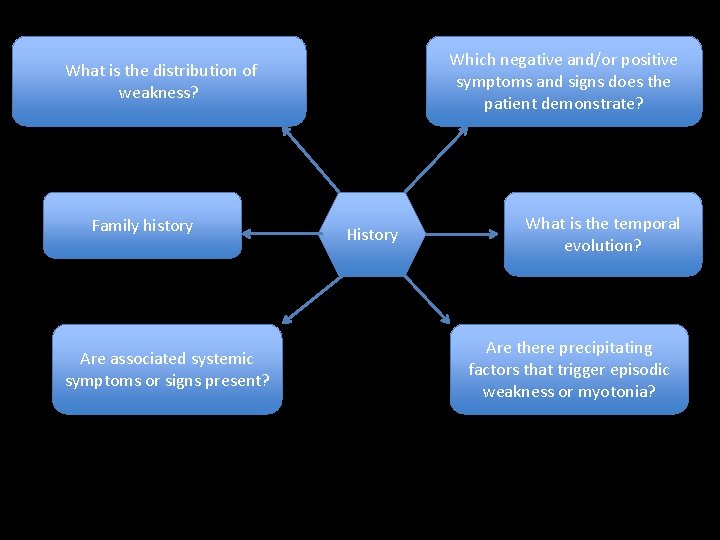
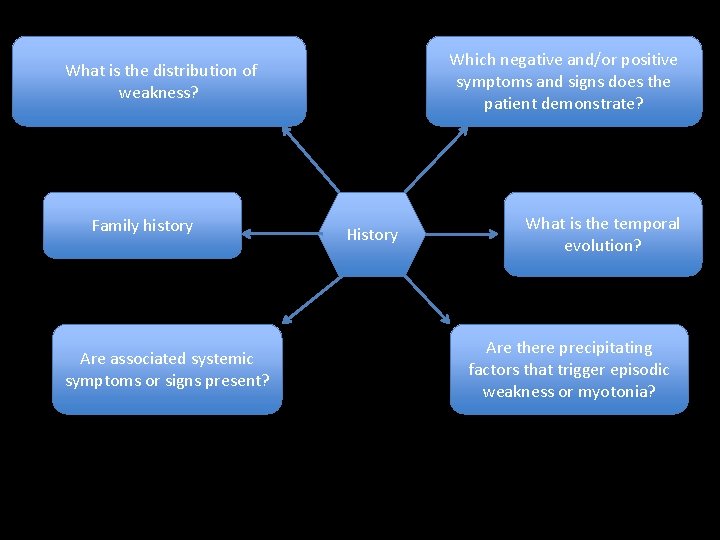
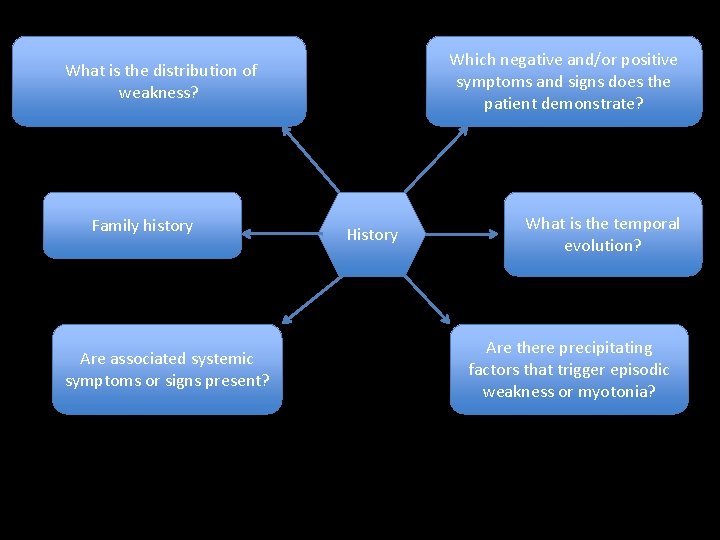
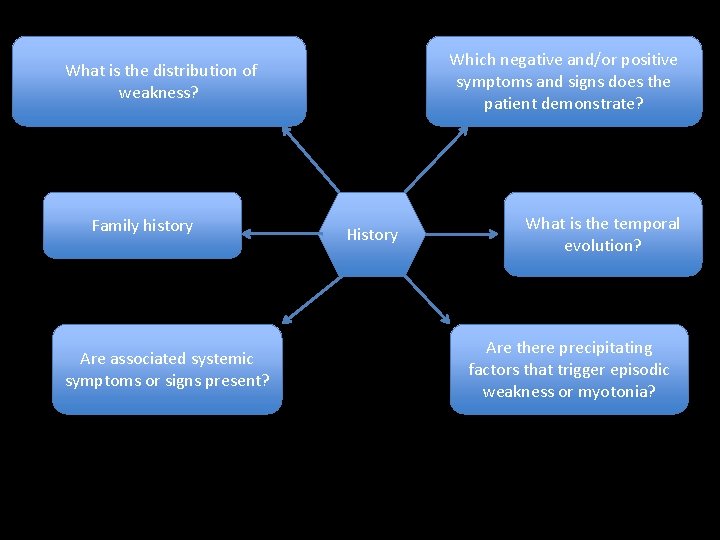
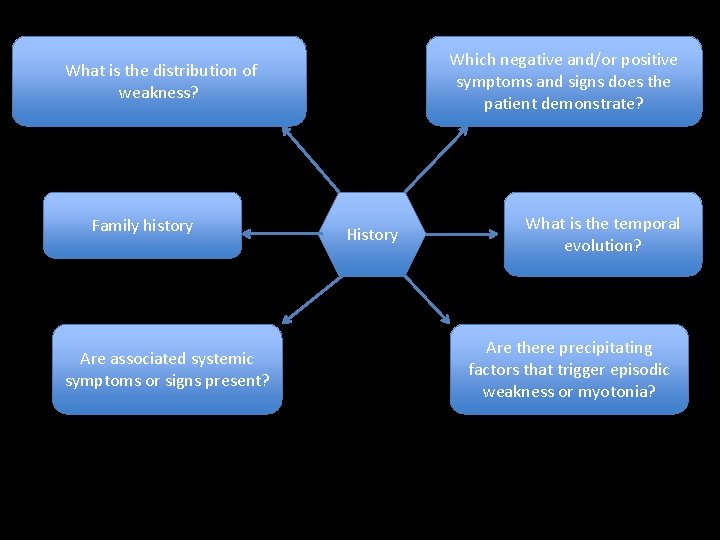
Which negative and/or positive symptoms and signs does the patient demonstrate? What is the distribution of weakness? Family history Are associated systemic symptoms or signs present? History What is the temporal evolution? Are there precipitating factors that trigger episodic weakness or myotonia?
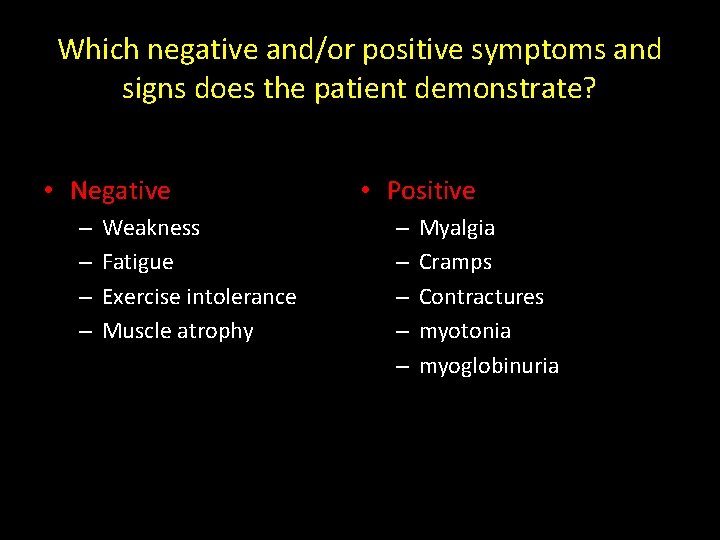
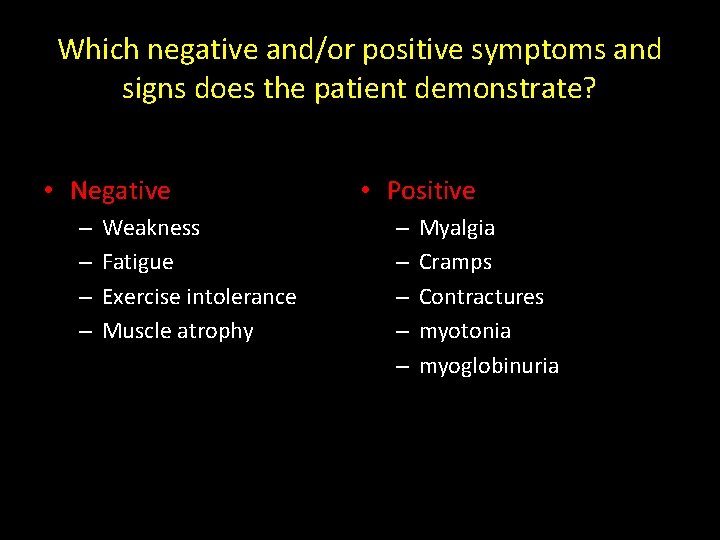
Which negative and/or positive symptoms and signs does the patient demonstrate? • Negative – – Weakness Fatigue Exercise intolerance Muscle atrophy • Positive – – – Myalgia Cramps Contractures myotonia myoglobinuria
1. Weakness: a) Proximal lower extremities: • difficulty climbing stairs, arising from a low chair or toilet, or getting up from a squatted position. b) Proximal upper extremities: • trouble lifting objects over their head and brushing their hair. c) Distal upper extremities: • difficulty opening jars, inability to turn a key in the ignition. d) Distal lower extremities: • tripping due to footdrop. e) Cranial muscle weakness, • dysarthria, dysphagia, or ptosis.
2. Fatigue • • • less useful negative symptom Nonspecific abnormal fatigability after exercise can result from certain metabolic and mitochondrial myopathies, and it is important to define the duration and intensity of exercise that provokes the fatigue.
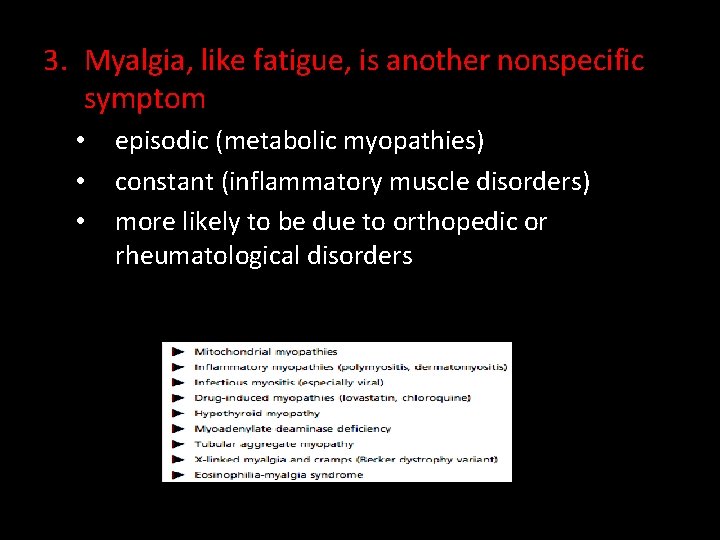
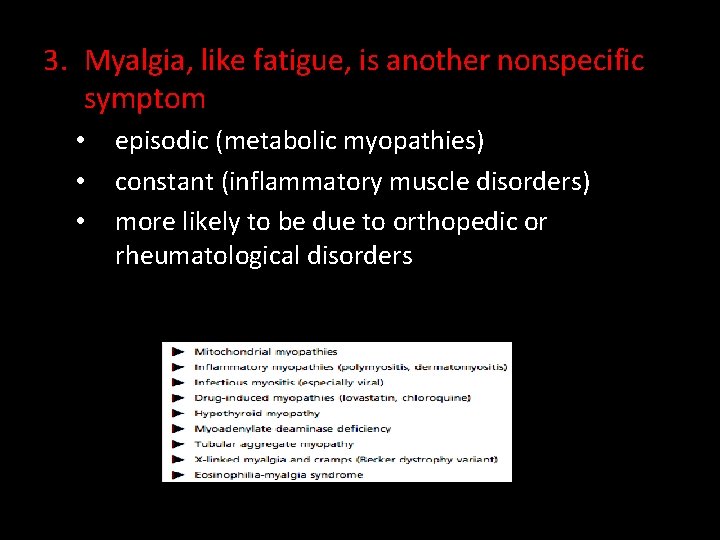
3. Myalgia, like fatigue, is another nonspecific symptom • • • episodic (metabolic myopathies) constant (inflammatory muscle disorders) more likely to be due to orthopedic or rheumatological disorders
4. Muscle cramp – They are typically benign, occurring frequently in normal individuals, and are seldom a feature of a primary myopathy – Cramps can occur with: • • • dehydration, hyponatremia, azotemia, myxedema disorders of the nerve or motor neuron (especially amyotrophic lateral sclerosis).
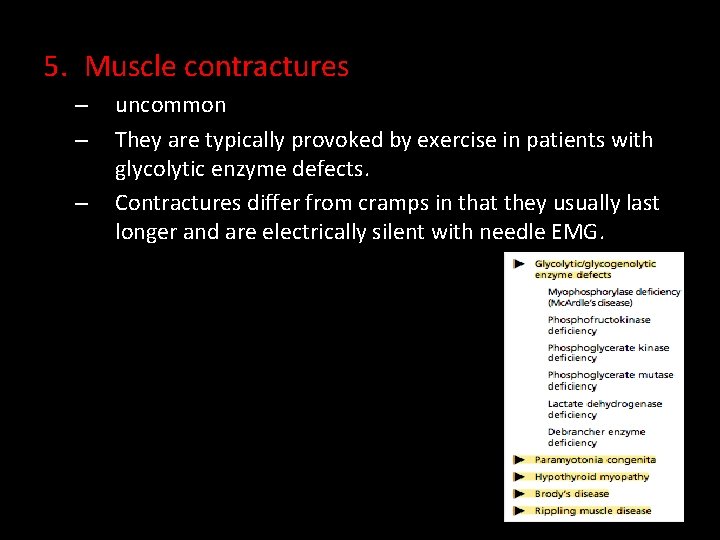
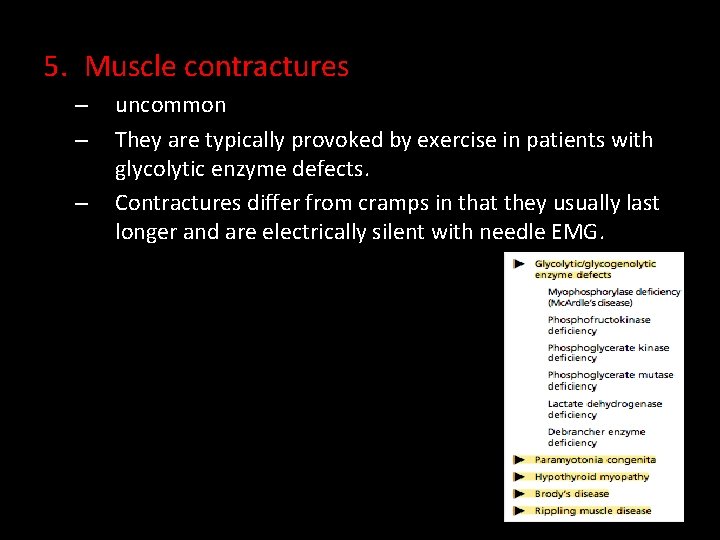
5. Muscle contractures – – – uncommon They are typically provoked by exercise in patients with glycolytic enzyme defects. Contractures differ from cramps in that they usually last longer and are electrically silent with needle EMG.
6. Myotonia is the phenomenon of impaired relaxation of muscle after forceful voluntary contraction and most commonly involves the hands and eyelids. – – – Myotonia is due to repetitive depolarization of the muscle membrane. Patients may complain of muscle stiffness or tightness resulting in difficulty releasing their handgrip after a handshake, unscrewing a bottle top, or opening their eyelids if they forcefully shut their eyes. Myotonia classically improves with repeated exercise.
6. paramyotonia congenita: ‘‘paradoxical myotonia’’ in that symptoms are typically worsened by exercise or repeated muscle contractions. • Exposure to cold results in worsening of both myotonia and paramyotonia.
• Myopathies associated with muscle stiffness: – Myotonic dystrophy – Proxymal myotonic dystrophy – Myotonia congenita – Paramyotonia congenita – Hyperkalemic periodic paralysis – Hypothyroid myopathy
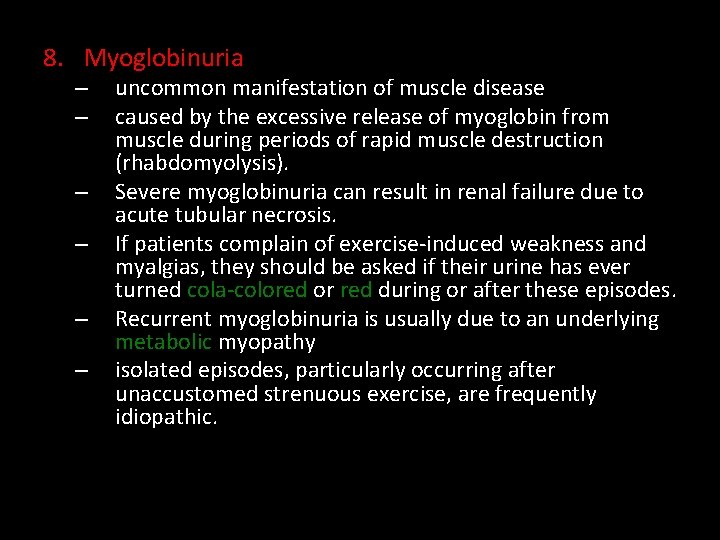
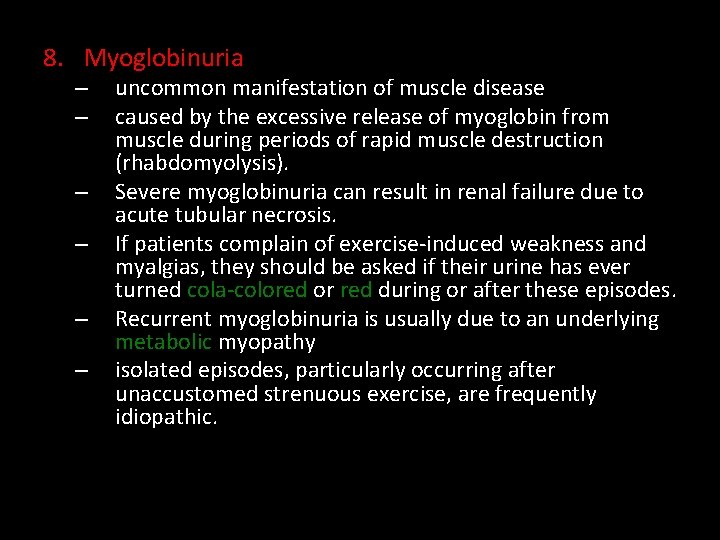
8. Myoglobinuria – – – uncommon manifestation of muscle disease caused by the excessive release of myoglobin from muscle during periods of rapid muscle destruction (rhabdomyolysis). Severe myoglobinuria can result in renal failure due to acute tubular necrosis. If patients complain of exercise-induced weakness and myalgias, they should be asked if their urine has ever turned cola-colored or red during or after these episodes. Recurrent myoglobinuria is usually due to an underlying metabolic myopathy isolated episodes, particularly occurring after unaccustomed strenuous exercise, are frequently idiopathic.

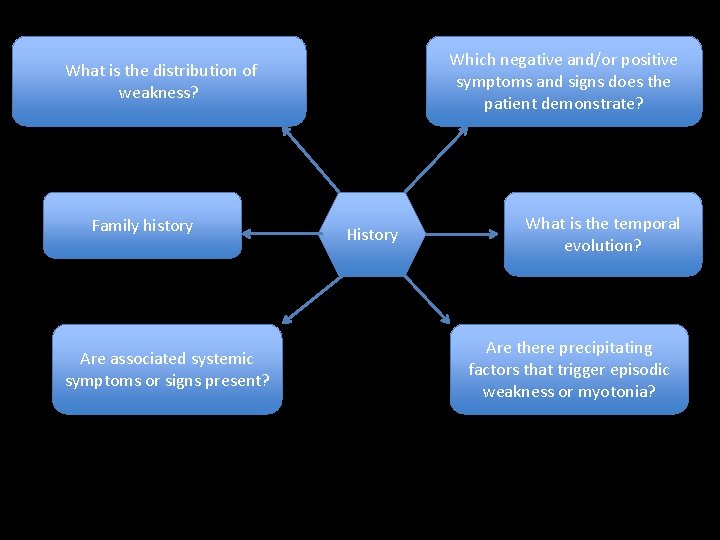
Which negative and/or positive symptoms and signs does the patient demonstrate? What is the distribution of weakness? Family history Are associated systemic symptoms or signs present? History What is the temporal evolution? Are there precipitating factors that trigger episodic weakness or myotonia?
What is the temporal evolution? • onset, • duration, and • evolution of the patient’s symptoms
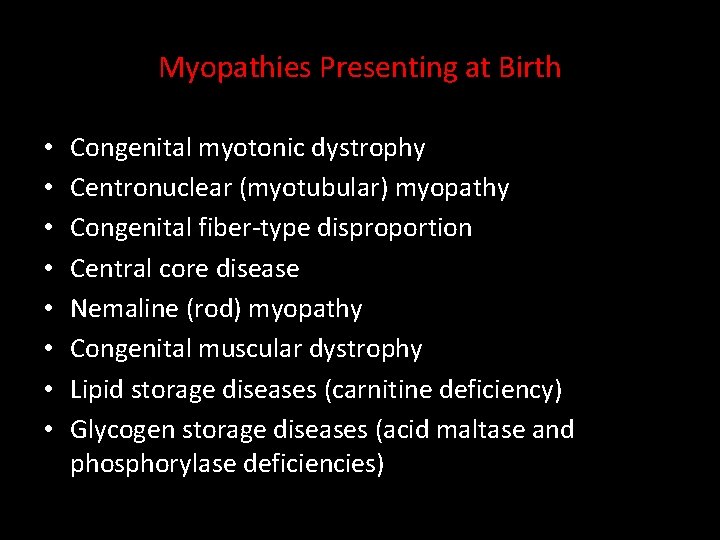
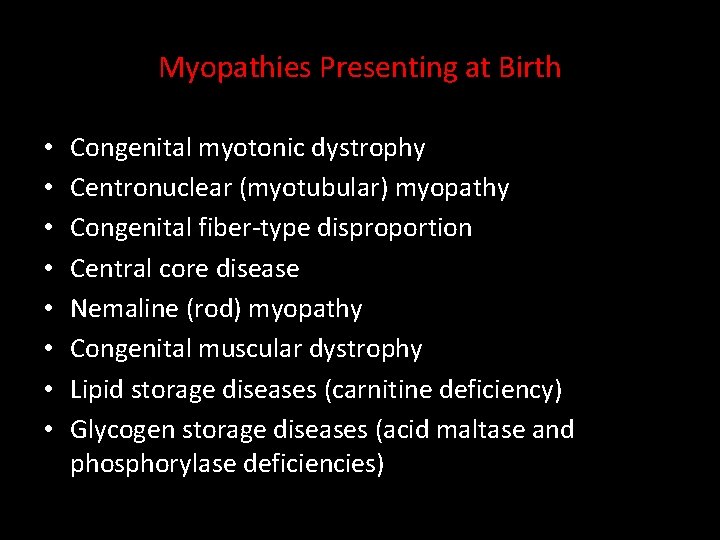
Myopathies Presenting at Birth • • Congenital myotonic dystrophy Centronuclear (myotubular) myopathy Congenital fiber-type disproportion Central core disease Nemaline (rod) myopathy Congenital muscular dystrophy Lipid storage diseases (carnitine deficiency) Glycogen storage diseases (acid maltase and phosphorylase deficiencies)
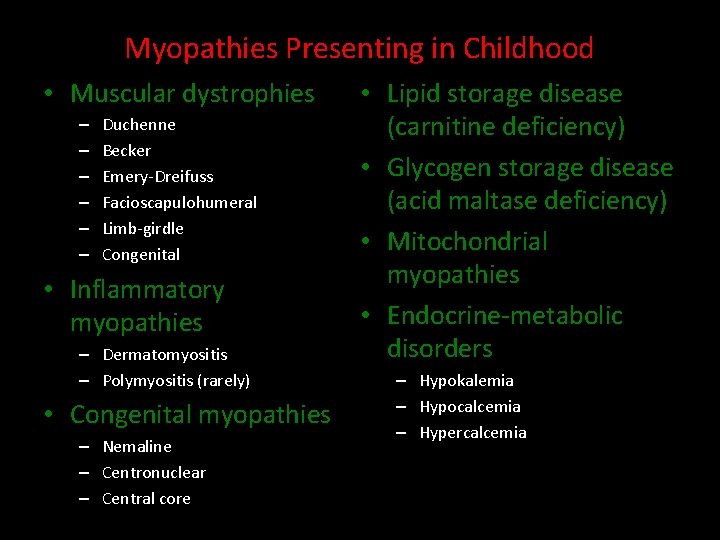
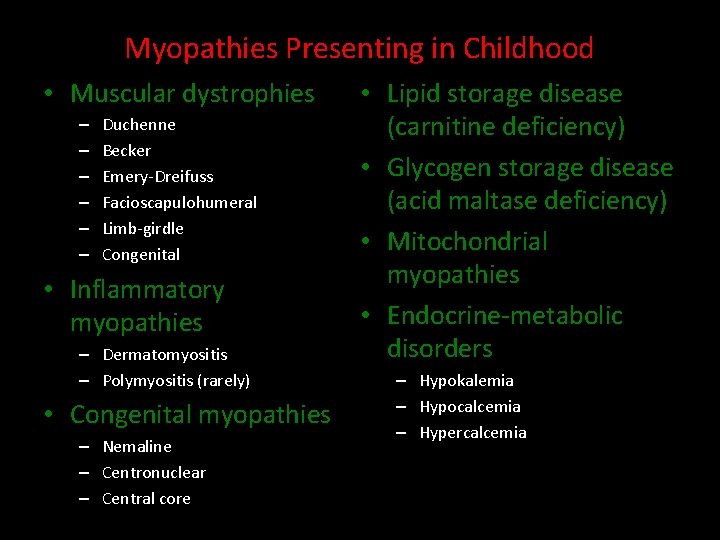
Myopathies Presenting in Childhood • Muscular dystrophies – – – Duchenne Becker Emery-Dreifuss Facioscapulohumeral Limb-girdle Congenital • Inflammatory myopathies – Dermatomyositis – Polymyositis (rarely) • Congenital myopathies – Nemaline – Centronuclear – Central core • Lipid storage disease (carnitine deficiency) • Glycogen storage disease (acid maltase deficiency) • Mitochondrial myopathies • Endocrine-metabolic disorders – Hypokalemia – Hypocalcemia – Hypercalcemia
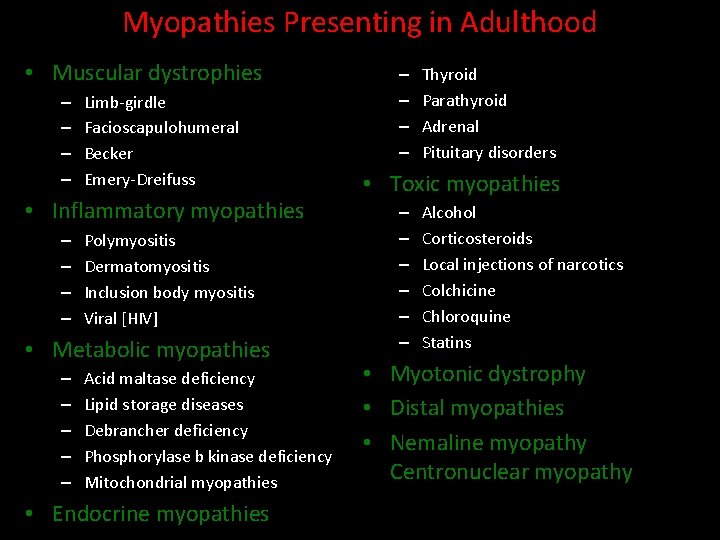
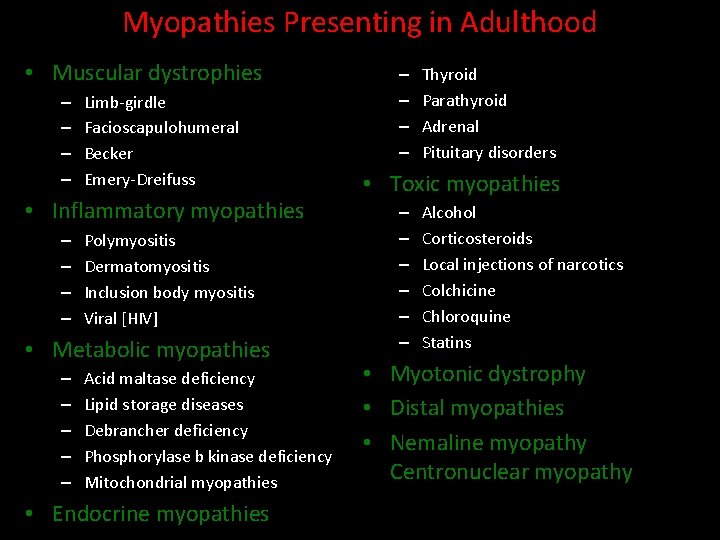
Myopathies Presenting in Adulthood • Muscular dystrophies – – Limb-girdle Facioscapulohumeral Becker Emery-Dreifuss • Inflammatory myopathies – – Polymyositis Dermatomyositis Inclusion body myositis Viral [HIV] • Metabolic myopathies – – – Acid maltase deficiency Lipid storage diseases Debrancher deficiency Phosphorylase b kinase deficiency Mitochondrial myopathies • Endocrine myopathies – – Thyroid Parathyroid Adrenal Pituitary disorders • Toxic myopathies – – – Alcohol Corticosteroids Local injections of narcotics Colchicine Chloroquine Statins • Myotonic dystrophy • Distal myopathies • Nemaline myopathy Centronuclear myopathy
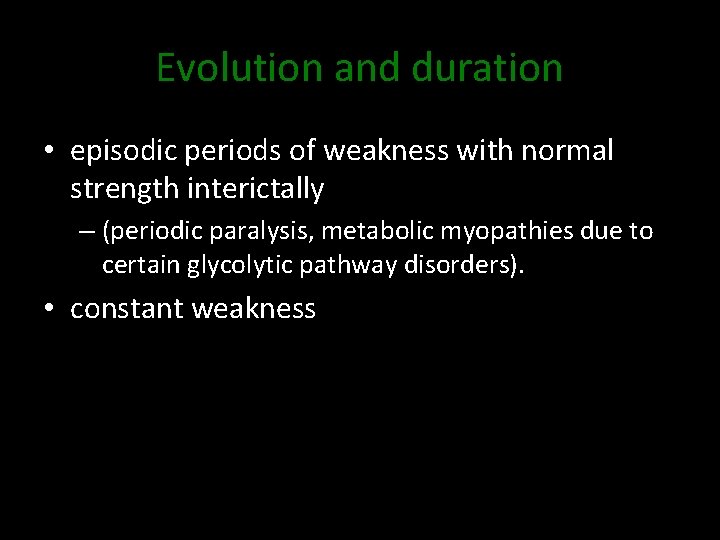
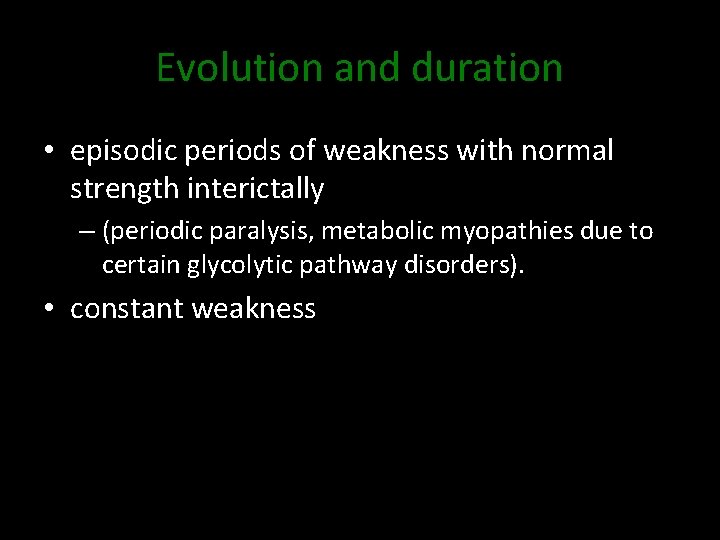
Evolution and duration • episodic periods of weakness with normal strength interictally – (periodic paralysis, metabolic myopathies due to certain glycolytic pathway disorders). • constant weakness
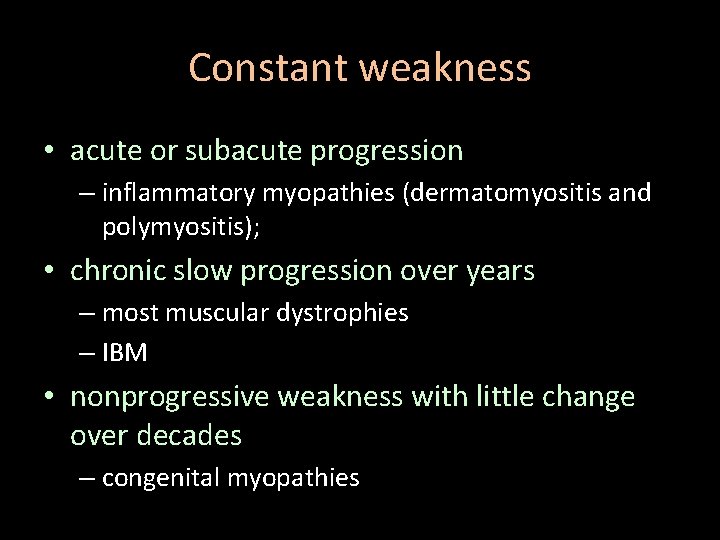
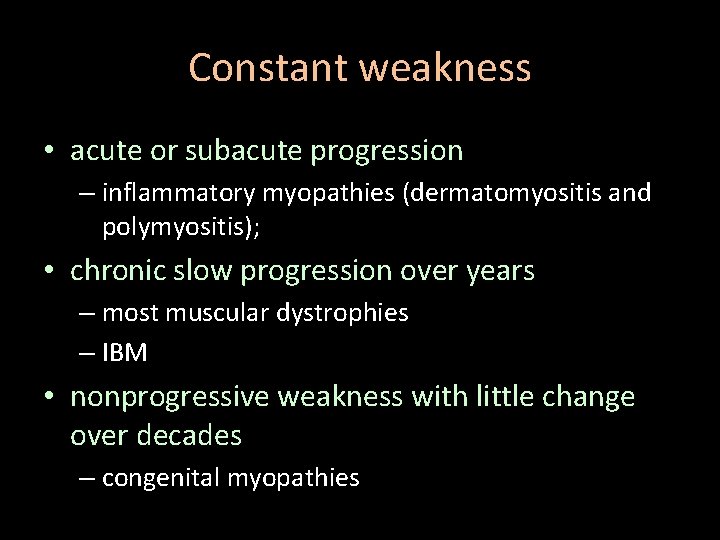
Constant weakness • acute or subacute progression – inflammatory myopathies (dermatomyositis and polymyositis); • chronic slow progression over years – most muscular dystrophies – IBM • nonprogressive weakness with little change over decades – congenital myopathies
Monophasic or relapsing • polymyositis can occasionally have an acute monophasic course with complete resolution of strength within weeks or months. • Patients with periodic paralysis or metabolic myopathies can have recurrent attacks of weakness over many years, • a patient with acute rhabdomyolysis due to cocaine may have a single episode.
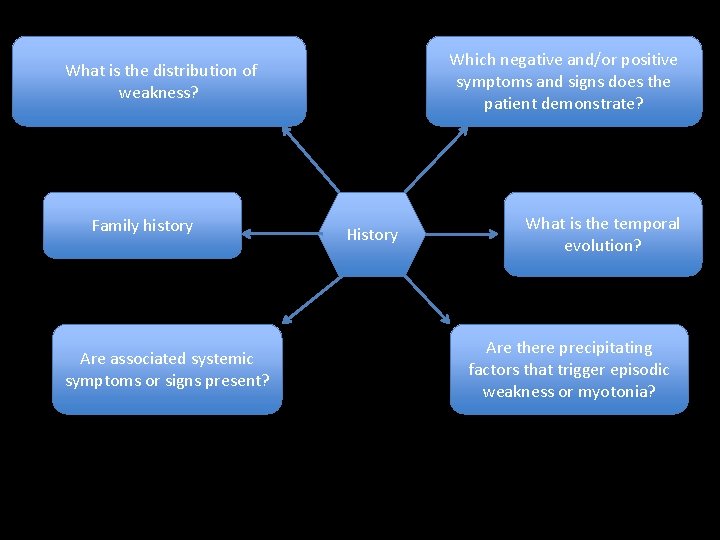
Which negative and/or positive symptoms and signs does the patient demonstrate? What is the distribution of weakness? Family history Are associated systemic symptoms or signs present? History What is the temporal evolution? Are there precipitating factors that trigger episodic weakness or myotonia?
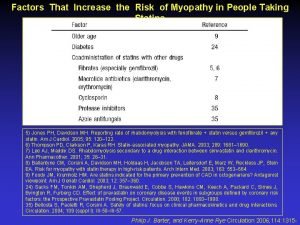
Precipitating factors • illegal drug or prescription medication use that might produce a myopathy. • weakness, pain, and/or myoglobinuria provoked by exercise – a glycolytic pathway defect. • Episodes of weakness with a fever – carnitine palmityl transferase deficiency. • Periodic paralysis is characteristically provoked by exercise or ingestion of a carbohydrate meal followed by a period of rest. • Patients with paramyotonia congenita frequently report that cold exposure may precipitate their symptoms of muscle stiffness.
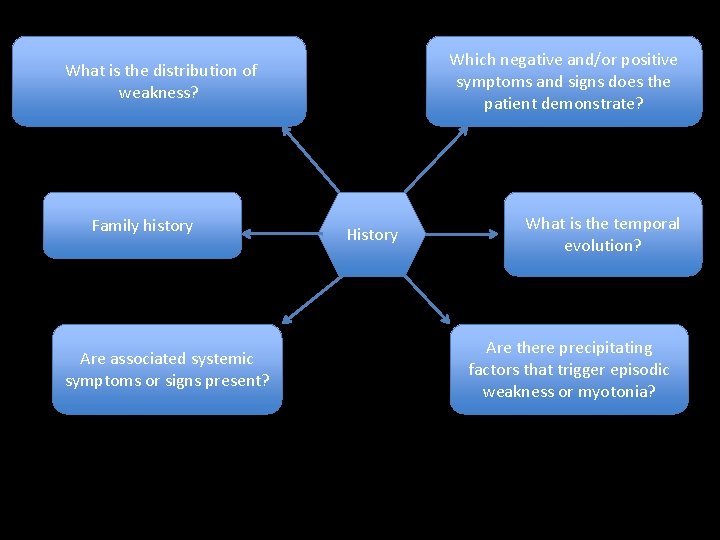
Which negative and/or positive symptoms and signs does the patient demonstrate? What is the distribution of weakness? Family history Are associated systemic symptoms or signs present? History What is the temporal evolution? Are there precipitating factors that trigger episodic weakness or myotonia?
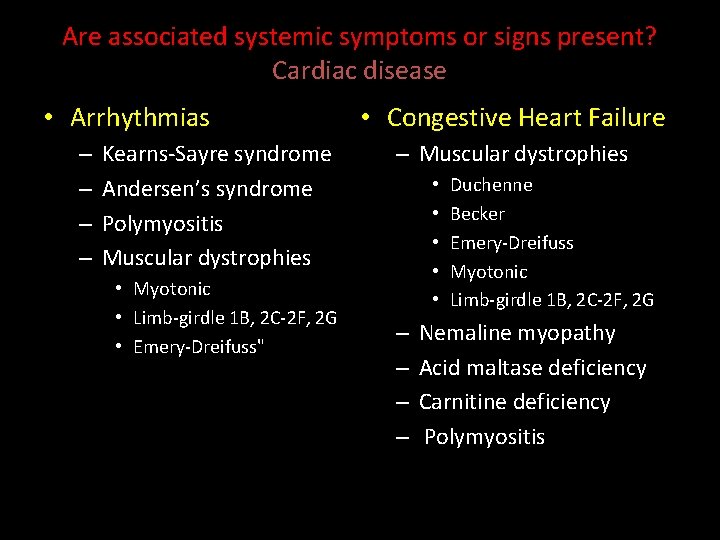
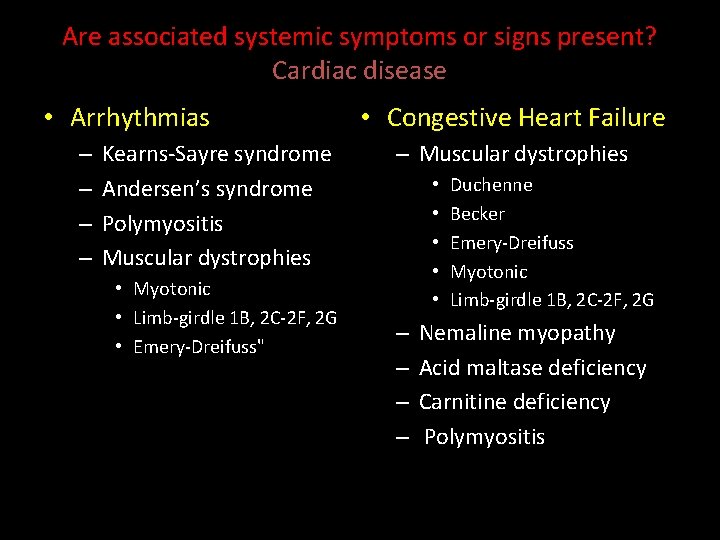
Are associated systemic symptoms or signs present? Cardiac disease • Arrhythmias – – Kearns-Sayre syndrome Andersen’s syndrome Polymyositis Muscular dystrophies • Myotonic • Limb-girdle 1 B, 2 C-2 F, 2 G • Emery-Dreifuss" • Congestive Heart Failure – Muscular dystrophies • • • – – Duchenne Becker Emery-Dreifuss Myotonic Limb-girdle 1 B, 2 C-2 F, 2 G Nemaline myopathy Acid maltase deficiency Carnitine deficiency Polymyositis
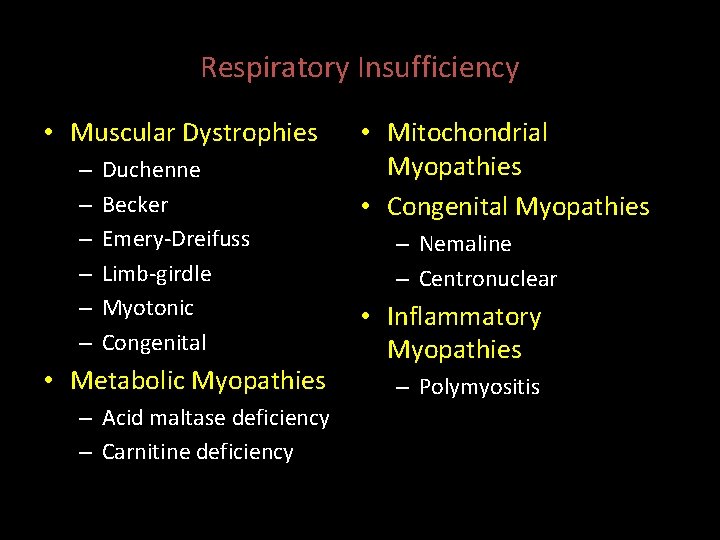
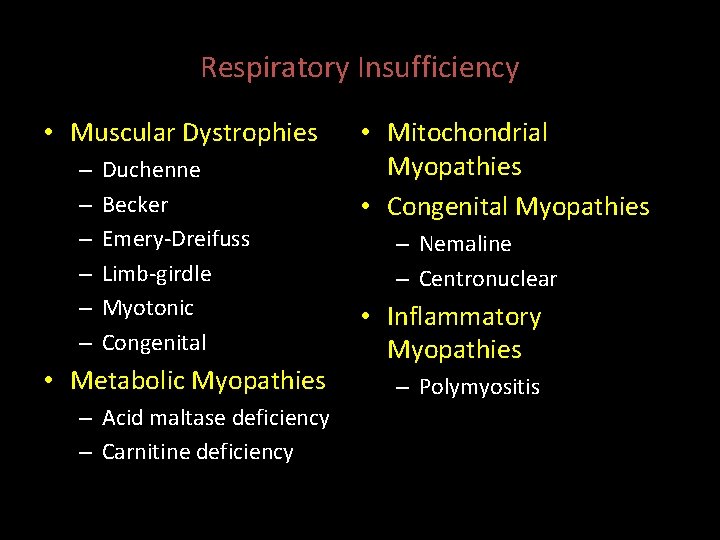
Respiratory Insufficiency • Muscular Dystrophies – – – Duchenne Becker Emery-Dreifuss Limb-girdle Myotonic Congenital • Metabolic Myopathies – Acid maltase deficiency – Carnitine deficiency • Mitochondrial Myopathies • Congenital Myopathies – Nemaline – Centronuclear • Inflammatory Myopathies – Polymyositis
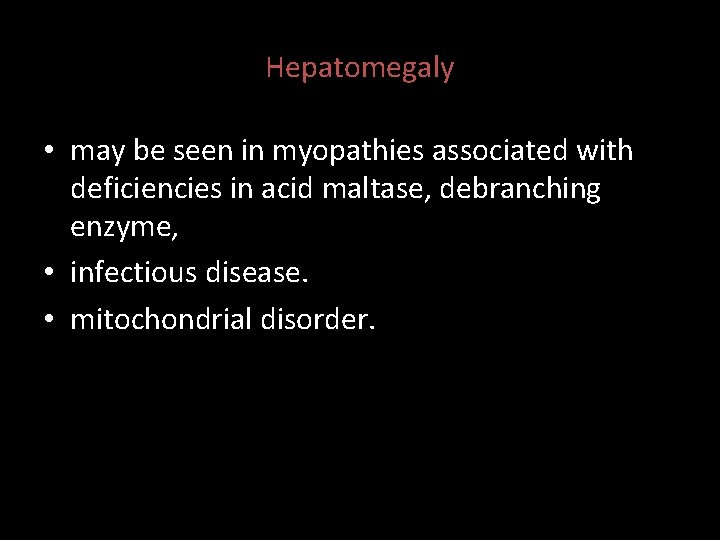
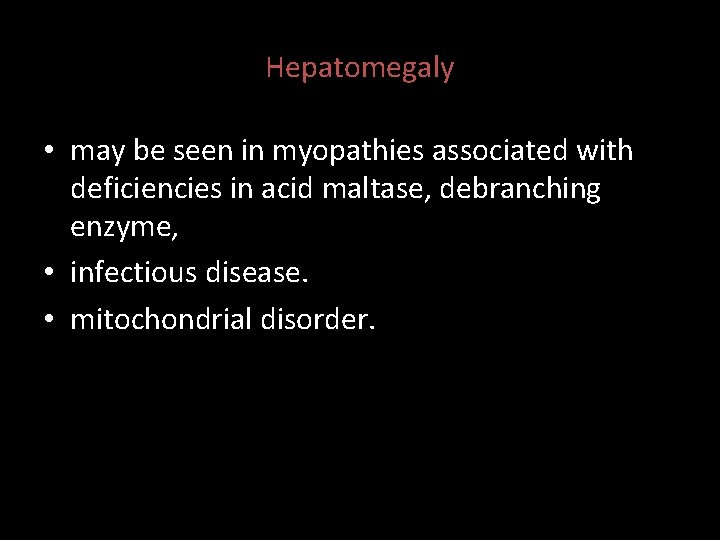
Hepatomegaly • may be seen in myopathies associated with deficiencies in acid maltase, debranching enzyme, • infectious disease. • mitochondrial disorder.
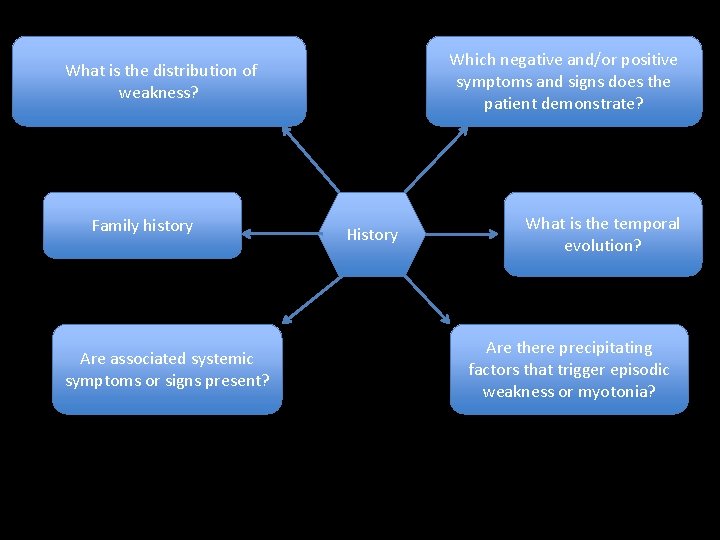
Which negative and/or positive symptoms and signs does the patient demonstrate? What is the distribution of weakness? Family history Are associated systemic symptoms or signs present? History What is the temporal evolution? Are there precipitating factors that trigger episodic weakness or myotonia?
Family history • A thorough family history is clearly of great importance in making a correct diagnosis. • Questions regarding family members’ use of canes or wheelchairs, skeletal deformities, or functional limitations are usually more informative than questions such as, ‘‘Does any member of your family have a muscle disease? ’’
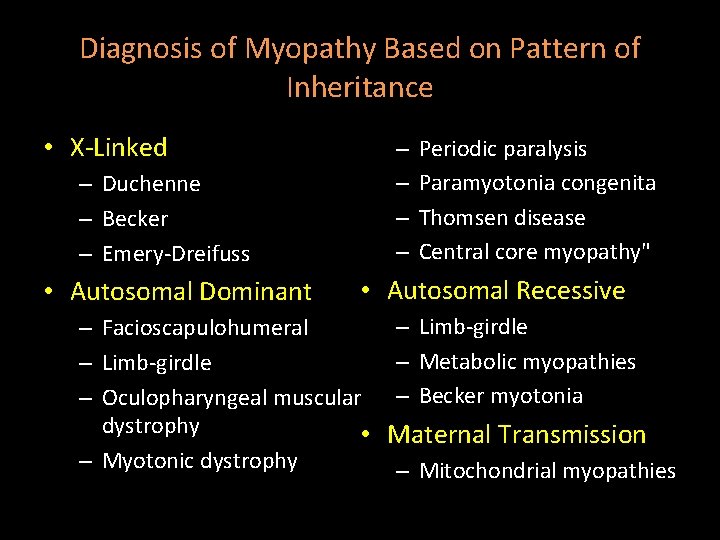
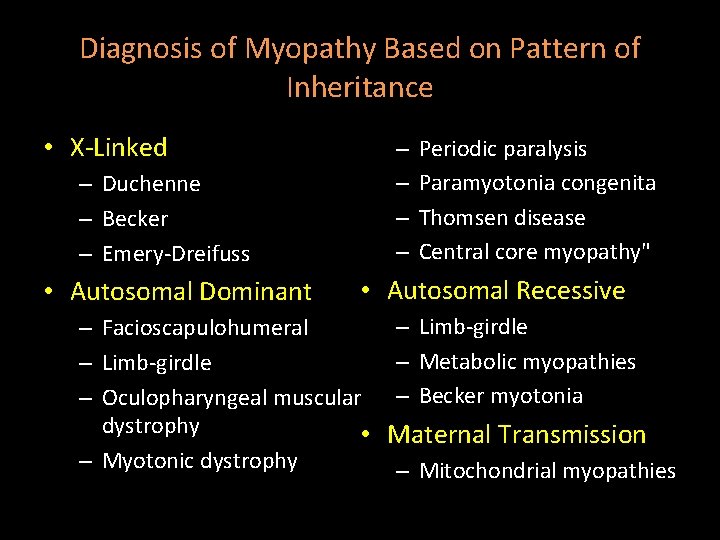
Diagnosis of Myopathy Based on Pattern of Inheritance • X-Linked – Duchenne – Becker – Emery-Dreifuss • Autosomal Dominant – – Periodic paralysis Paramyotonia congenita Thomsen disease Central core myopathy" • Autosomal Recessive – Limb-girdle – Facioscapulohumeral – Metabolic myopathies – Limb-girdle – Oculopharyngeal muscular – Becker myotonia dystrophy • Maternal Transmission – Myotonic dystrophy – Mitochondrial myopathies
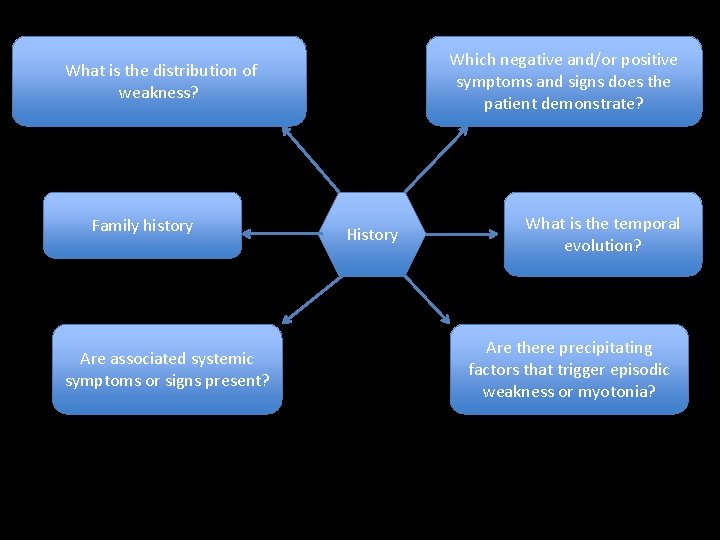
Which negative and/or positive symptoms and signs does the patient demonstrate? What is the distribution of weakness? Family history Are associated systemic symptoms or signs present? History What is the temporal evolution? Are there precipitating factors that trigger episodic weakness or myotonia?
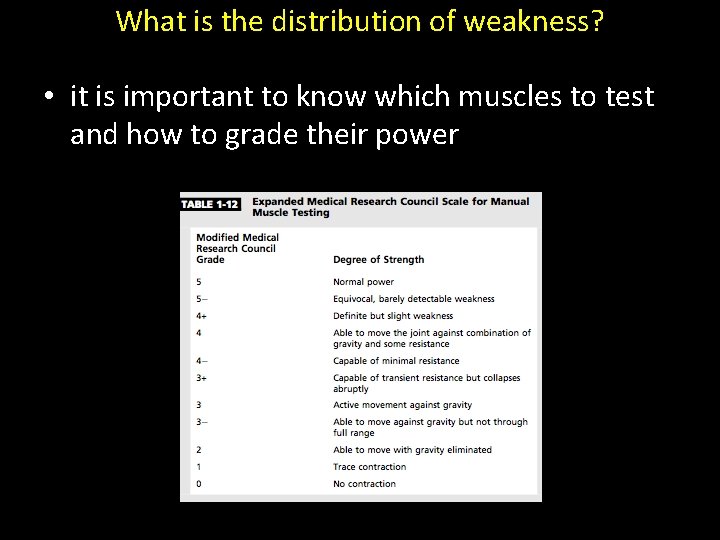
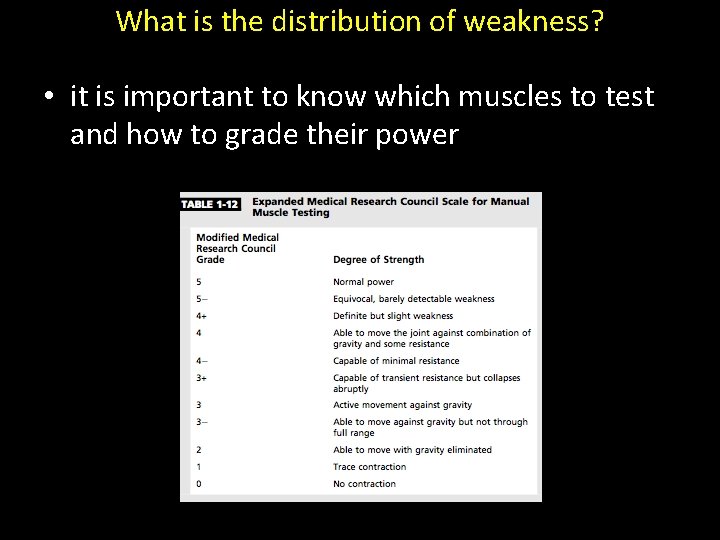
What is the distribution of weakness? • it is important to know which muscles to test and how to grade their power
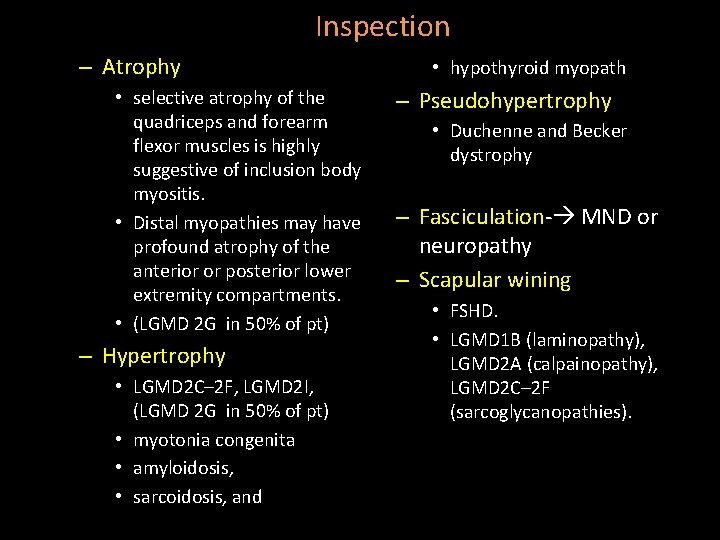
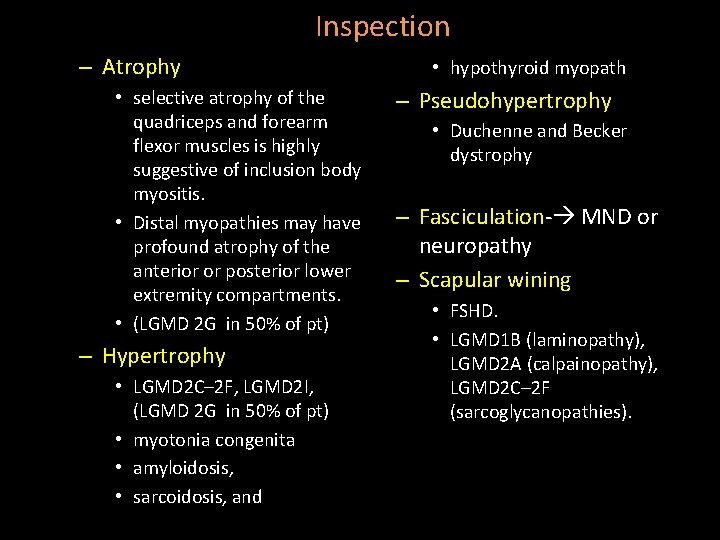
Inspection – Atrophy • selective atrophy of the quadriceps and forearm flexor muscles is highly suggestive of inclusion body myositis. • Distal myopathies may have profound atrophy of the anterior or posterior lower extremity compartments. • (LGMD 2 G in 50% of pt) – Hypertrophy • LGMD 2 C– 2 F, LGMD 2 I, (LGMD 2 G in 50% of pt) • myotonia congenita • amyloidosis, • sarcoidosis, and • hypothyroid myopath – Pseudohypertrophy • Duchenne and Becker dystrophy – Fasciculation- MND or neuropathy – Scapular wining • FSHD. • LGMD 1 B (laminopathy), LGMD 2 A (calpainopathy), LGMD 2 C– 2 F (sarcoglycanopathies).

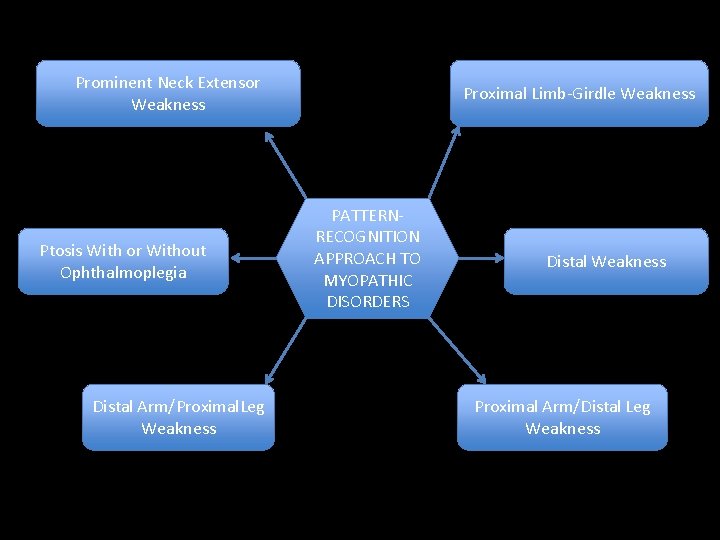
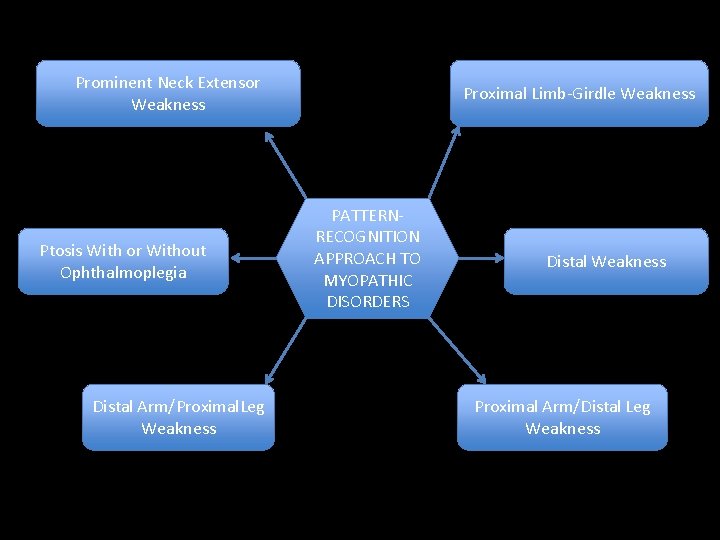
Prominent Neck Extensor Weakness Ptosis With or Without Ophthalmoplegia Distal Arm/Proximal. Leg Weakness Proximal Limb-Girdle Weakness PATTERNRECOGNITION APPROACH TO MYOPATHIC DISORDERS Distal Weakness Proximal Arm/Distal Leg Weakness

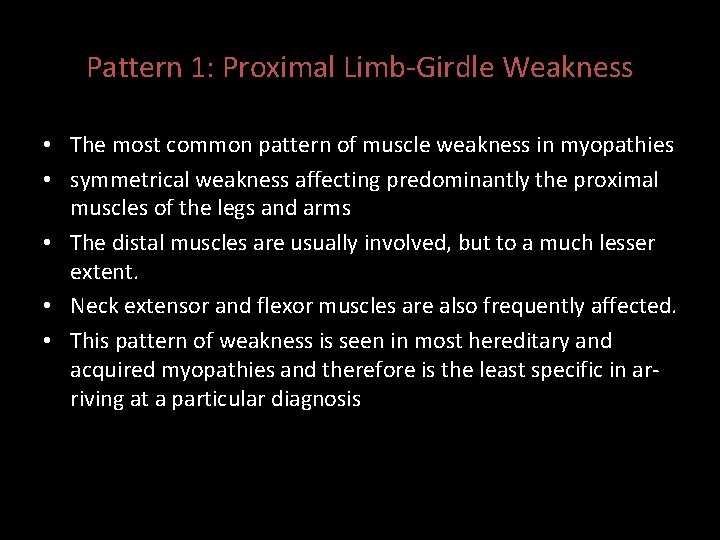
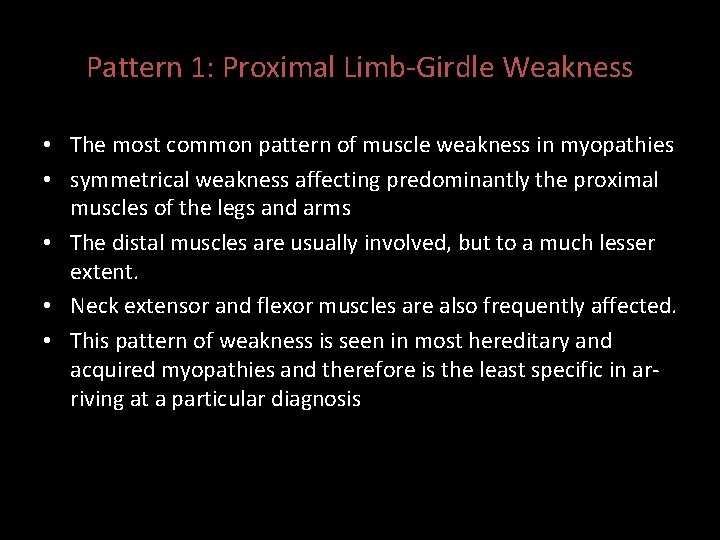
Pattern 1: Proximal Limb-Girdle Weakness • The most common pattern of muscle weakness in myopathies • symmetrical weakness affecting predominantly the proximal muscles of the legs and arms • The distal muscles are usually involved, but to a much lesser extent. • Neck extensor and flexor muscles are also frequently affected. • This pattern of weakness is seen in most hereditary and acquired myopathies and therefore is the least specific in arriving at a particular diagnosis
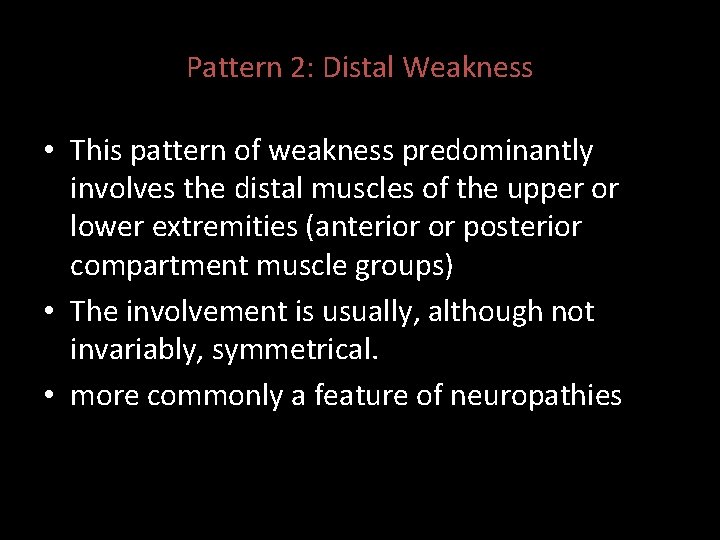
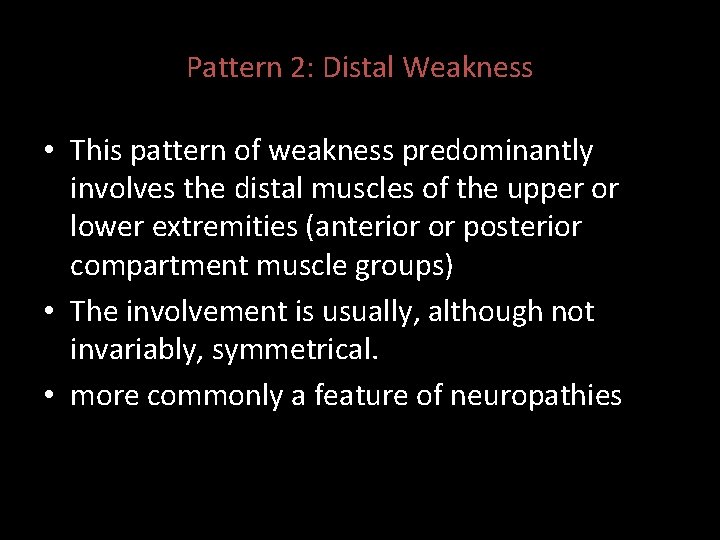
Pattern 2: Distal Weakness • This pattern of weakness predominantly involves the distal muscles of the upper or lower extremities (anterior or posterior compartment muscle groups) • The involvement is usually, although not invariably, symmetrical. • more commonly a feature of neuropathies
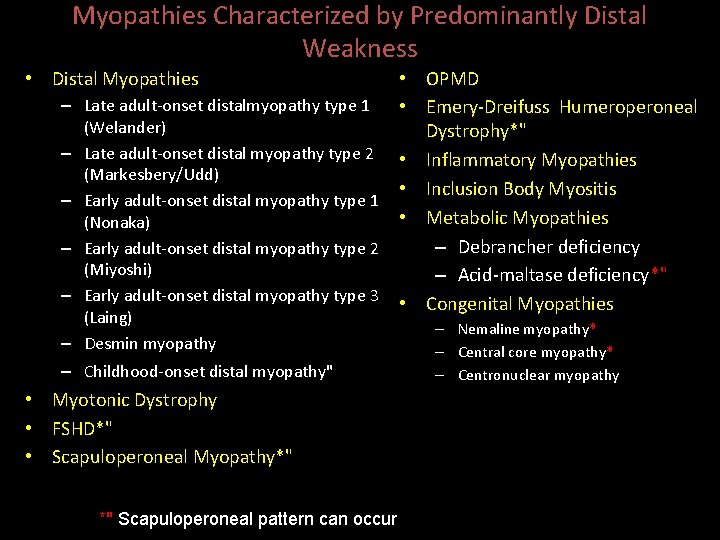
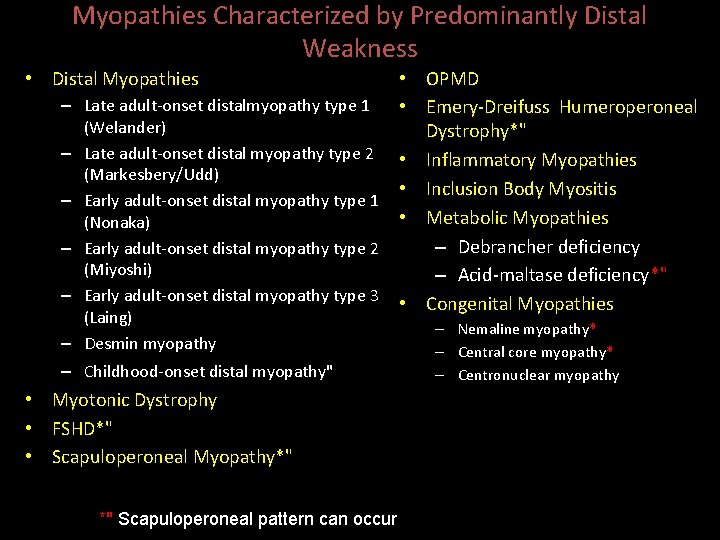
Myopathies Characterized by Predominantly Distal Weakness • Distal Myopathies – – – • OPMD Late adult-onset distalmyopathy type 1 • Emery-Dreifuss Humeroperoneal (Welander) Dystrophy*" Late adult-onset distal myopathy type 2 • Inflammatory Myopathies (Markesbery/Udd) • Inclusion Body Myositis Early adult-onset distal myopathy type 1 • Metabolic Myopathies (Nonaka) – Debrancher deficiency Early adult-onset distal myopathy type 2 (Miyoshi) – Acid-maltase deficiency*" Early adult-onset distal myopathy type 3 • Congenital Myopathies (Laing) – Desmin myopathy – Childhood-onset distal myopathy" • Myotonic Dystrophy • FSHD*" • Scapuloperoneal Myopathy*" *" Scapuloperoneal pattern can occur – Nemaline myopathy* – Central core myopathy* – Centronuclear myopathy
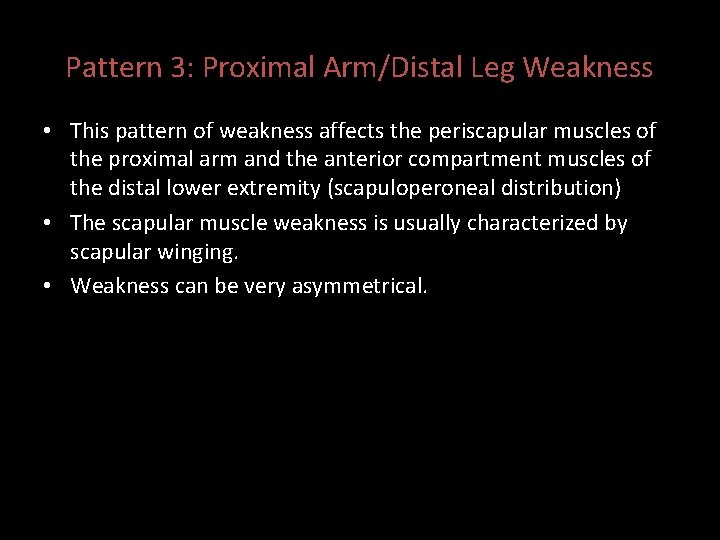
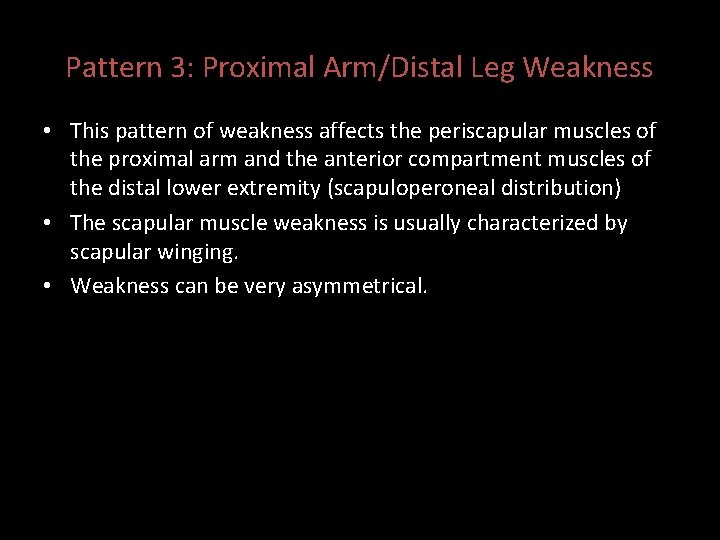
Pattern 3: Proximal Arm/Distal Leg Weakness • This pattern of weakness affects the periscapular muscles of the proximal arm and the anterior compartment muscles of the distal lower extremity (scapuloperoneal distribution) • The scapular muscle weakness is usually characterized by scapular winging. • Weakness can be very asymmetrical.
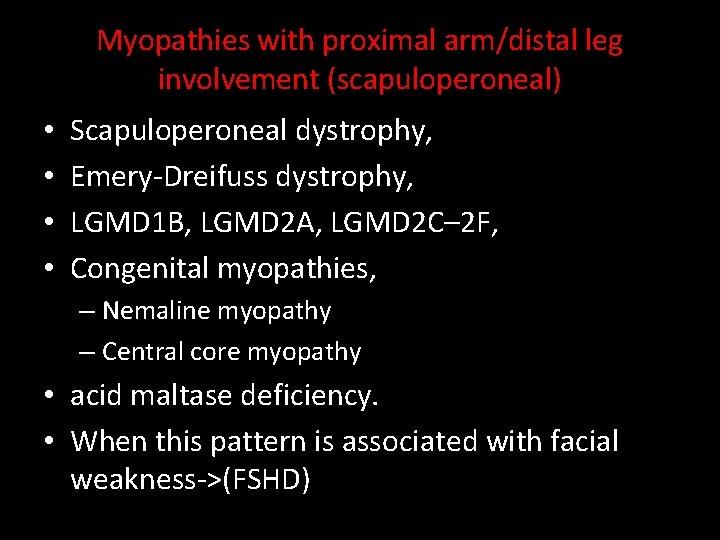
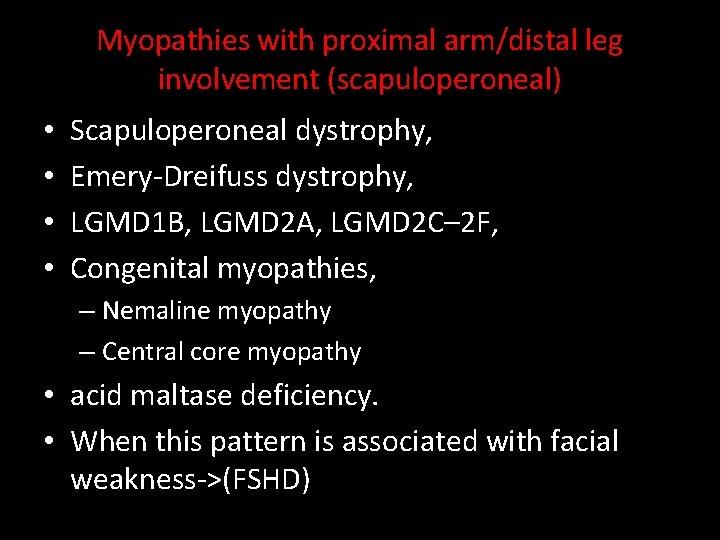
Myopathies with proximal arm/distal leg involvement (scapuloperoneal) • • Scapuloperoneal dystrophy, Emery-Dreifuss dystrophy, LGMD 1 B, LGMD 2 A, LGMD 2 C– 2 F, Congenital myopathies, – Nemaline myopathy – Central core myopathy • acid maltase deficiency. • When this pattern is associated with facial weakness->(FSHD)
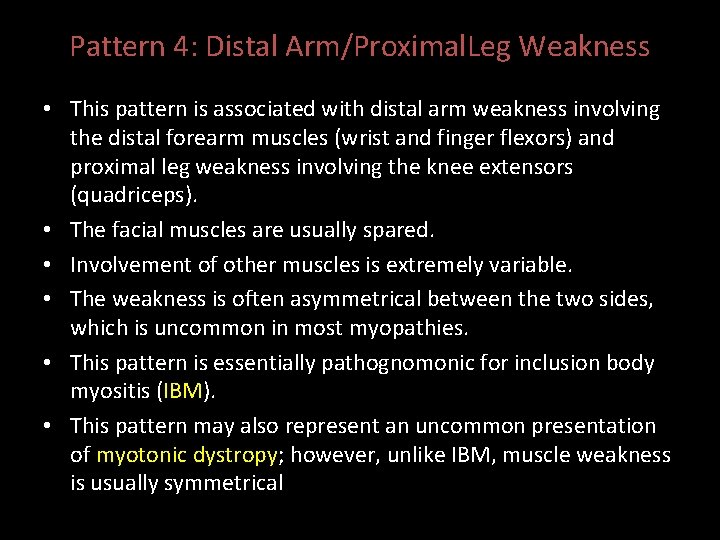
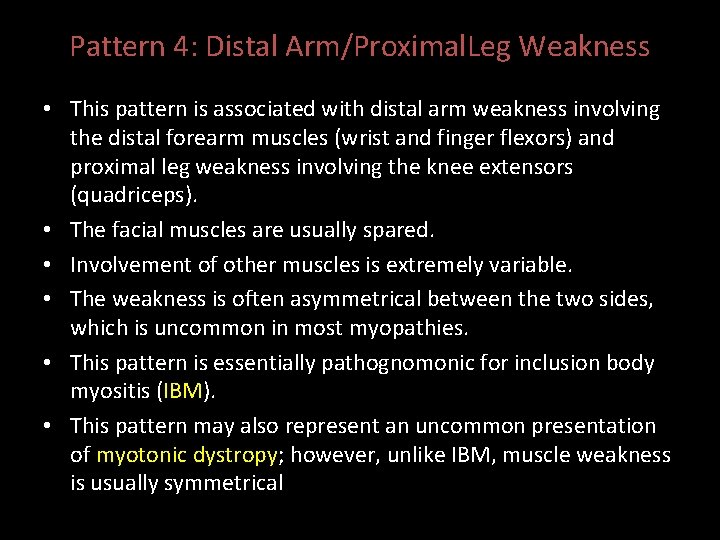
Pattern 4: Distal Arm/Proximal. Leg Weakness • This pattern is associated with distal arm weakness involving the distal forearm muscles (wrist and finger flexors) and proximal leg weakness involving the knee extensors (quadriceps). • The facial muscles are usually spared. • Involvement of other muscles is extremely variable. • The weakness is often asymmetrical between the two sides, which is uncommon in most myopathies. • This pattern is essentially pathognomonic for inclusion body myositis (IBM). • This pattern may also represent an uncommon presentation of myotonic dystropy; however, unlike IBM, muscle weakness is usually symmetrical
Pattern 5: Ptosis With or Without Ophthalmoplegia • usually, although not always, occurs without symptoms of diplopia. • Facial weakness is not uncommon, • extremity weakness is extremely variable, depending on the diagnosis.
• The combination of ptosis, ophthalmoplegia (without diplopia), and dysphagia should suggest the diagnosis of oculopharyngeal dystrophy, especially if the onset is in middle age or later. • Ptosis and ophthalmoplegia without prominent pharyngeal involvement is a hallmark of many of the mitochondrial myopathies. • Ptosis and facial weakness without ophthalmoplegia is a common feature of myotonic dystrophy.
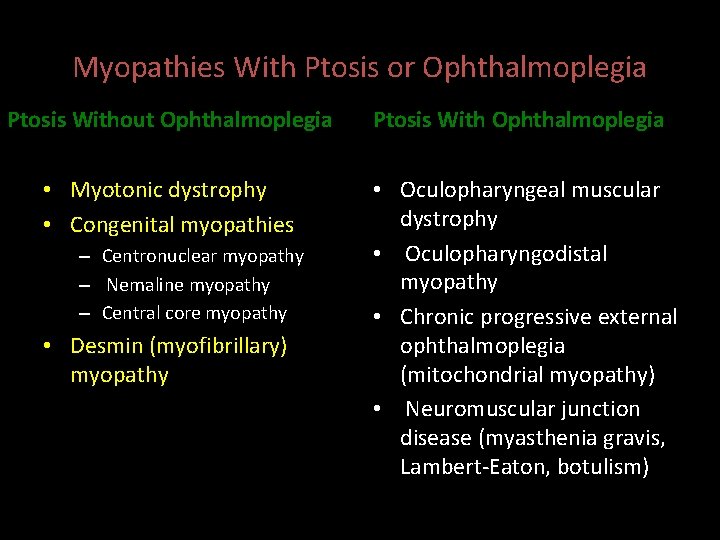
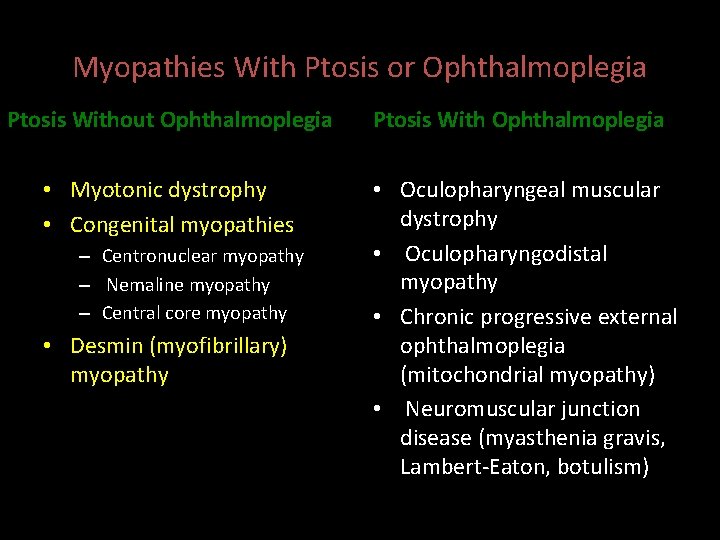
Myopathies With Ptosis or Ophthalmoplegia Ptosis Without Ophthalmoplegia Ptosis With Ophthalmoplegia • Myotonic dystrophy • Congenital myopathies • Oculopharyngeal muscular dystrophy • Oculopharyngodistal myopathy • Chronic progressive external ophthalmoplegia (mitochondrial myopathy) • Neuromuscular junction disease (myasthenia gravis, Lambert-Eaton, botulism) – Centronuclear myopathy – Nemaline myopathy – Central core myopathy • Desmin (myofibrillary) myopathy
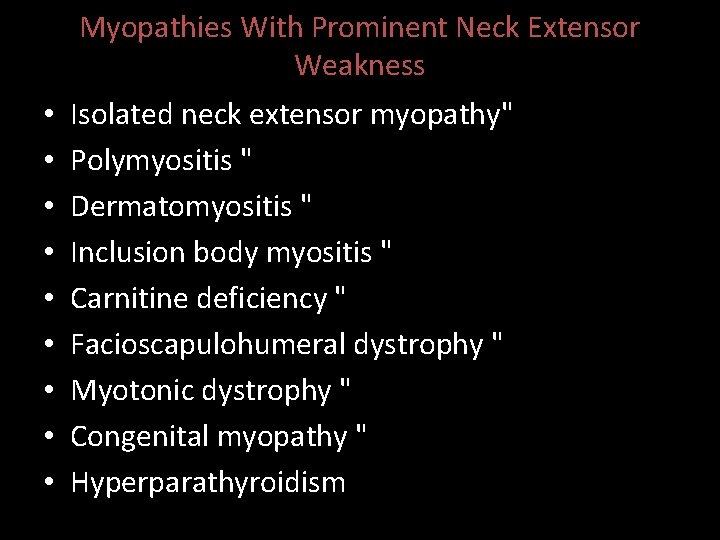
Pattern 6: Prominent Neck Extensor Weakness • ‘‘dropped head syndrome’’ • Involvement of the neck flexors is variable. • Isolated neck extension weakness represents a distinct muscle disorder called isolated neck extensor myopathy. • Prominent neck extensor weakness: – amyotrophic lateral sclerosis and – myasthenia gravis.
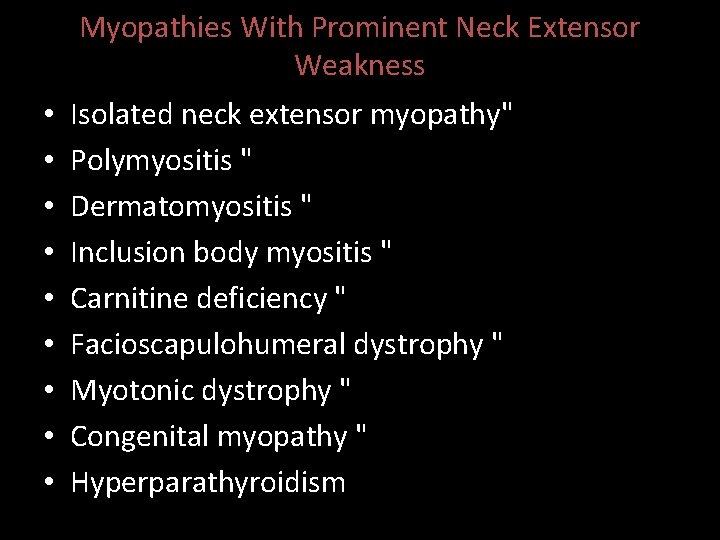
Myopathies With Prominent Neck Extensor Weakness • • • Isolated neck extensor myopathy" Polymyositis " Dermatomyositis " Inclusion body myositis " Carnitine deficiency " Facioscapulohumeral dystrophy " Myotonic dystrophy " Congenital myopathy " Hyperparathyroidism
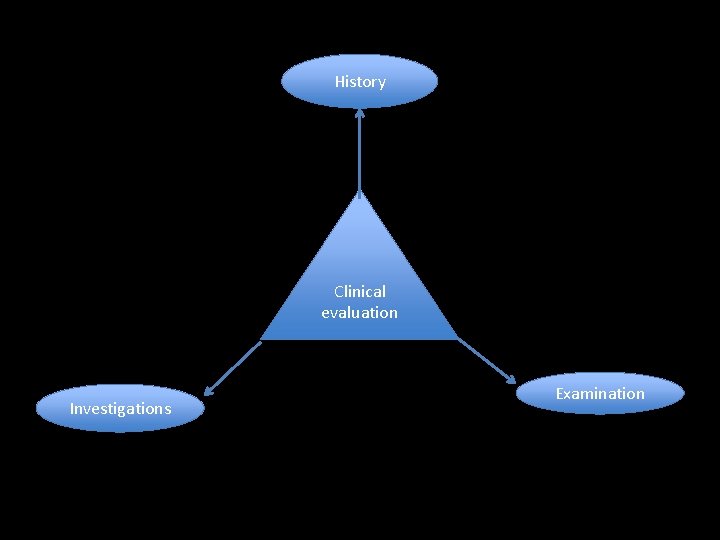
History Clinical evaluation Investigations Examination
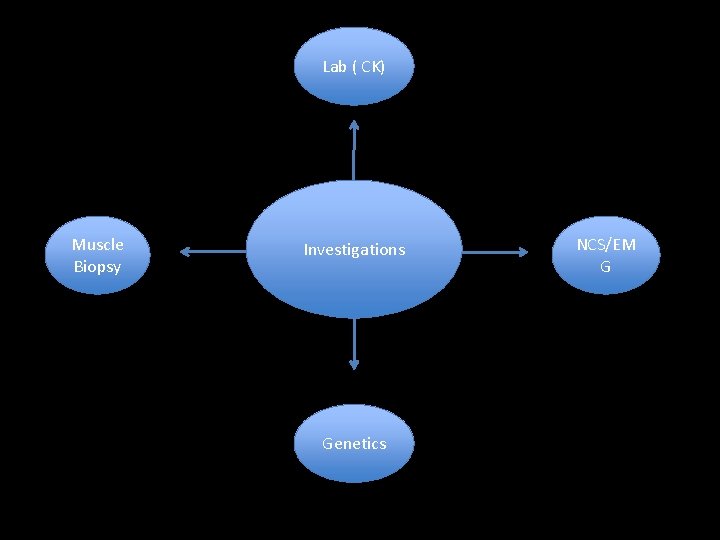
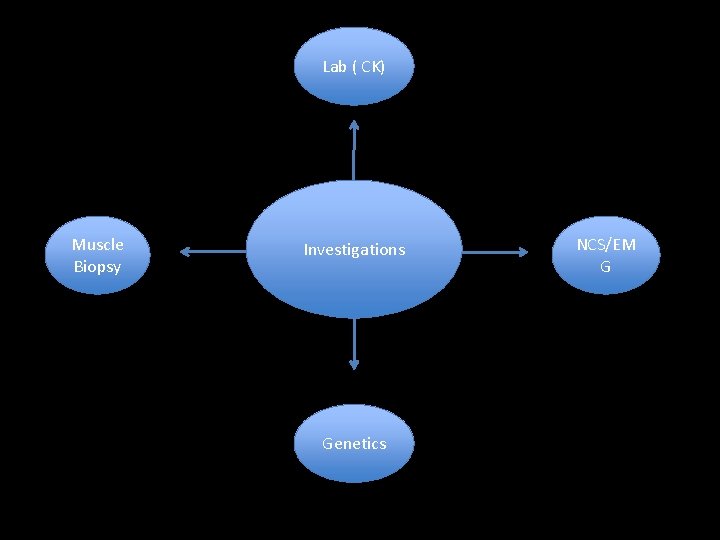
Lab ( CK) Muscle Biopsy Investigations Genetics NCS/EM G
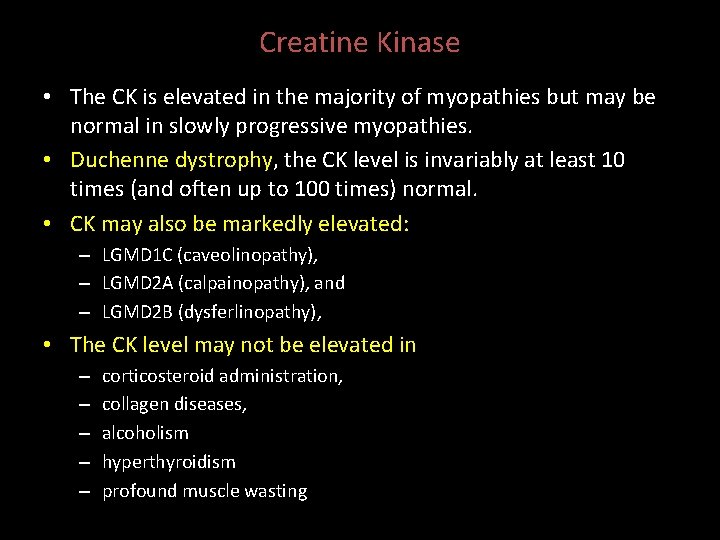
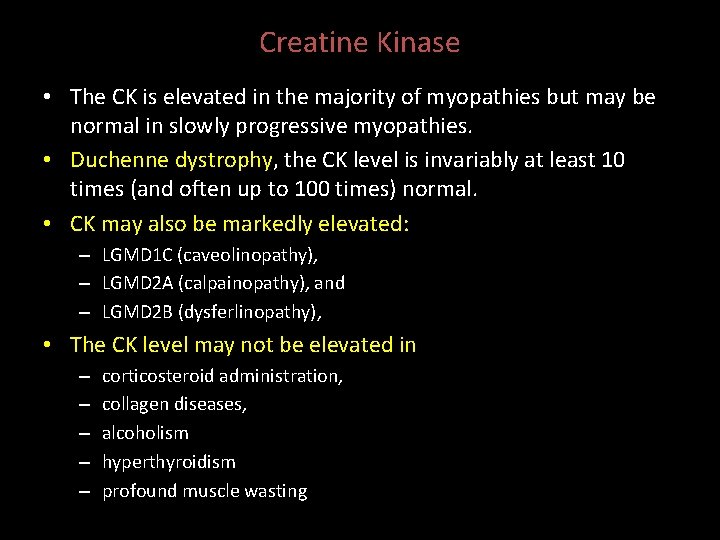
Creatine Kinase • The CK is elevated in the majority of myopathies but may be normal in slowly progressive myopathies. • Duchenne dystrophy, the CK level is invariably at least 10 times (and often up to 100 times) normal. • CK may also be markedly elevated: – LGMD 1 C (caveolinopathy), – LGMD 2 A (calpainopathy), and – LGMD 2 B (dysferlinopathy), • The CK level may not be elevated in – – – corticosteroid administration, collagen diseases, alcoholism hyperthyroidism profound muscle wasting
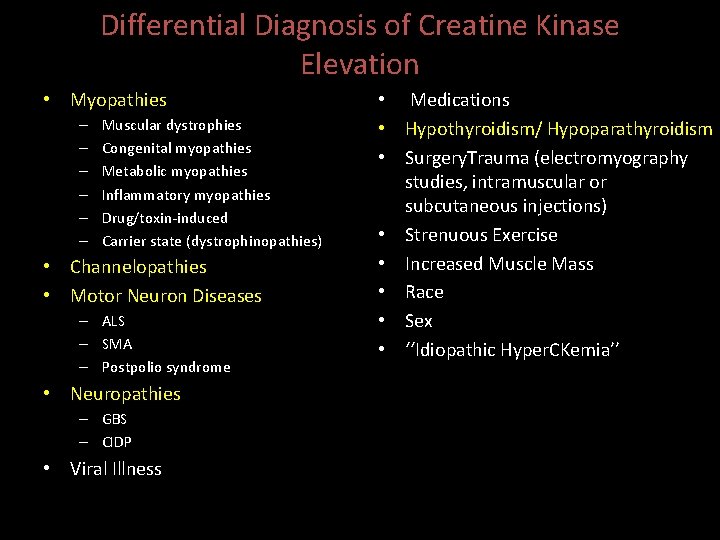
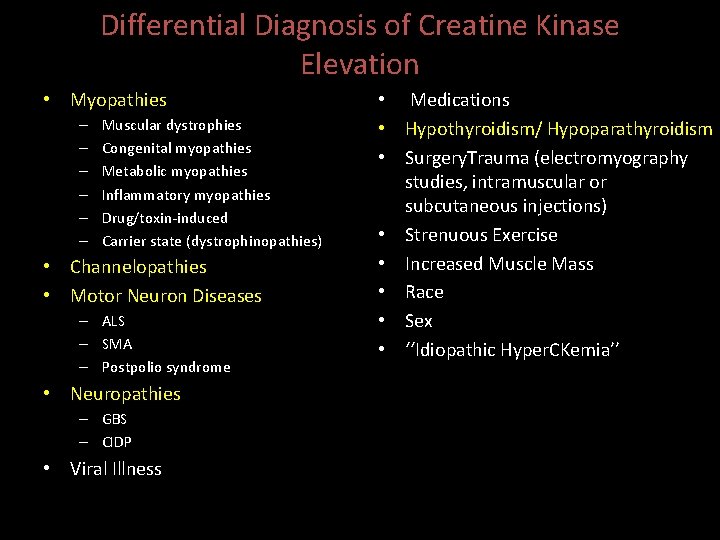
Differential Diagnosis of Creatine Kinase Elevation • Myopathies – – – Muscular dystrophies Congenital myopathies Metabolic myopathies Inflammatory myopathies Drug/toxin-induced Carrier state (dystrophinopathies) • Channelopathies • Motor Neuron Diseases – ALS – SMA – Postpolio syndrome • Neuropathies – GBS – CIDP • Viral Illness • Medications • Hypothyroidism/ Hypoparathyroidism • Surgery. Trauma (electromyography studies, intramuscular or subcutaneous injections) • Strenuous Exercise • Increased Muscle Mass • Race • Sex • ‘‘Idiopathic Hyper. CKemia’’
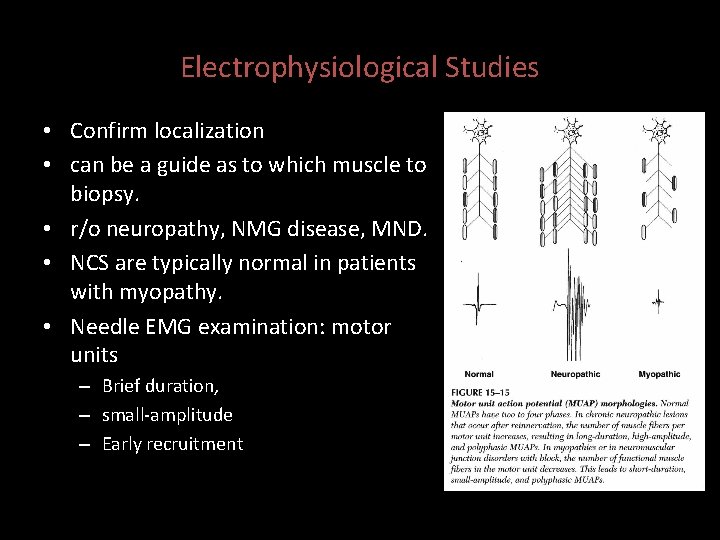
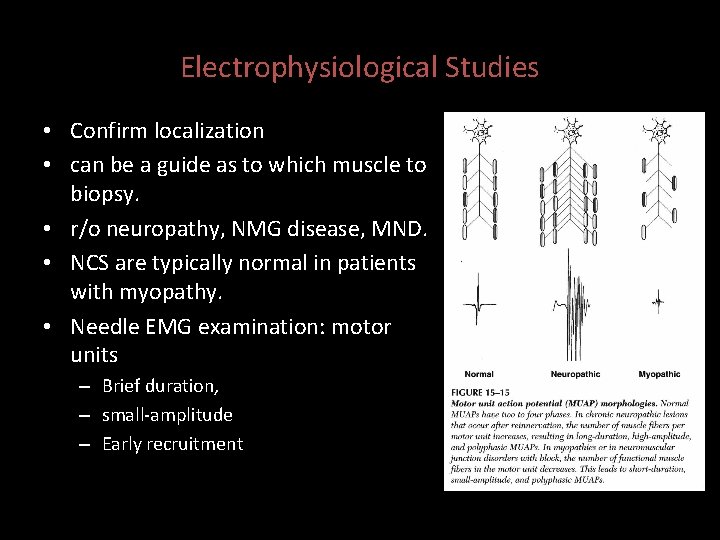
Electrophysiological Studies • Confirm localization • can be a guide as to which muscle to biopsy. • r/o neuropathy, NMG disease, MND. • NCS are typically normal in patients with myopathy. • Needle EMG examination: motor units – Brief duration, – small-amplitude – Early recruitment
Muscle biopsy • Selection of the appropriate muscle to biopsy is critical. • Muscles that are severely weak (MRC grade 3 or less) should not be biopsied, since the results are likely to show only evidence of end stage muscle disease • muscles that have recently been studied by needle EMG should be avoided because of the possibility of artifacts created by needle insertion.
• Biopsies should generally be taken from muscles that demonstrate MRC grade 4 strength. • The muscle of choice: – biceps. – vastus lateralis. • The gastrocnemius should be avoided, since its tendon insertion extends throughout the muscle and inadvertent sampling of a myotendinous junction may cause difficulty with interpretation.
• Typical myopathic abnormalities include: – central nuclei, – both small and large hypertrophic round fibers, – split fibers, and – degenerating and regenerating fibers. – Chronic myopathies frequently show evidence of increased connective tissue and fat.
Inflammatory myopathies • characterized by: – the presence of mononuclear inflammatory cells in the endomysial and perimysial connective tissue between fibers and occasionally around blood vessels ( perivascular)
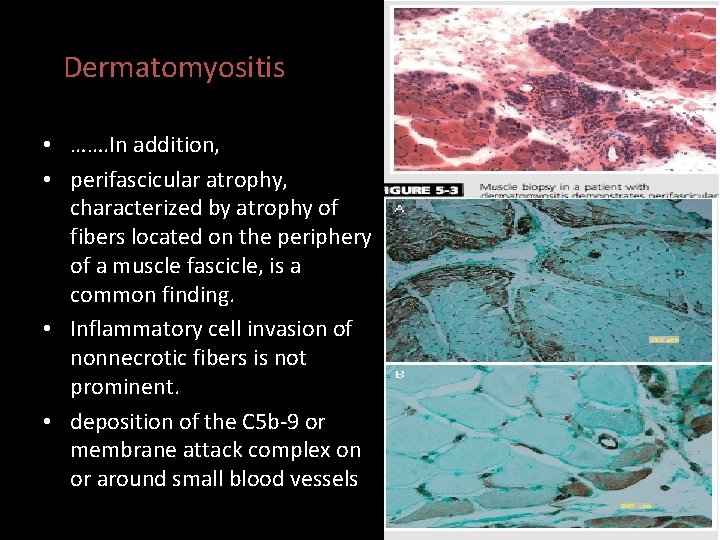
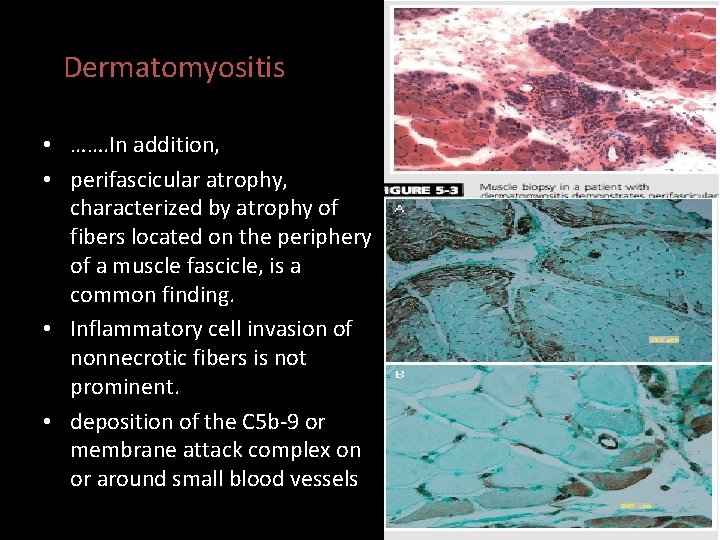
Dermatomyositis • ……. In addition, • perifascicular atrophy, characterized by atrophy of fibers located on the periphery of a muscle fascicle, is a common finding. • Inflammatory cell invasion of nonnecrotic fibers is not prominent. • deposition of the C 5 b-9 or membrane attack complex on or around small blood vessels
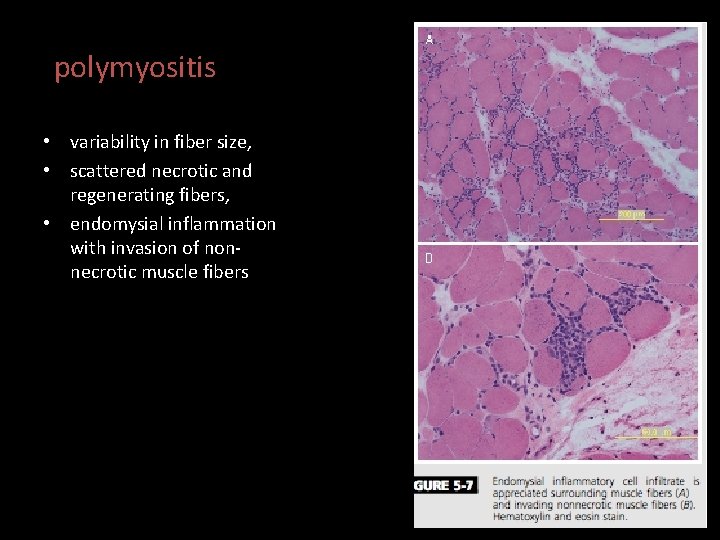
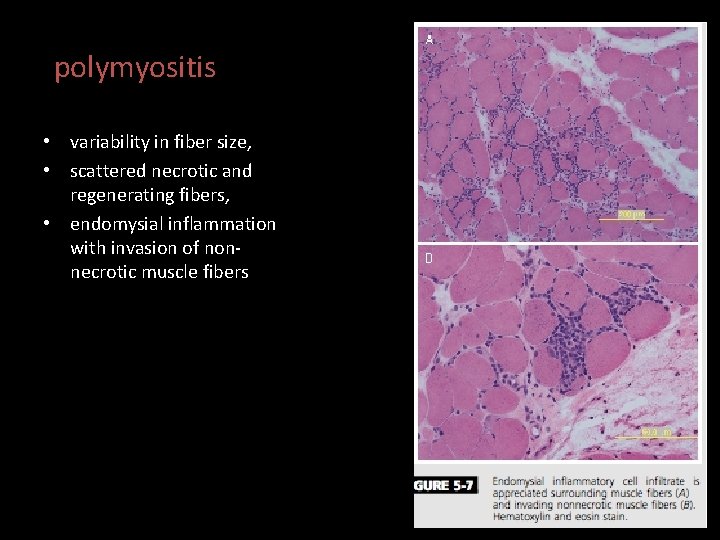
polymyositis • variability in fiber size, • scattered necrotic and regenerating fibers, • endomysial inflammation with invasion of nonnecrotic muscle fibers
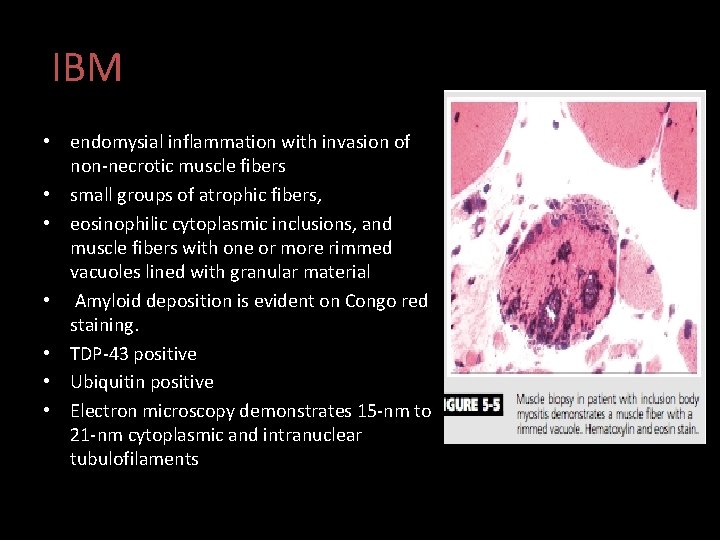
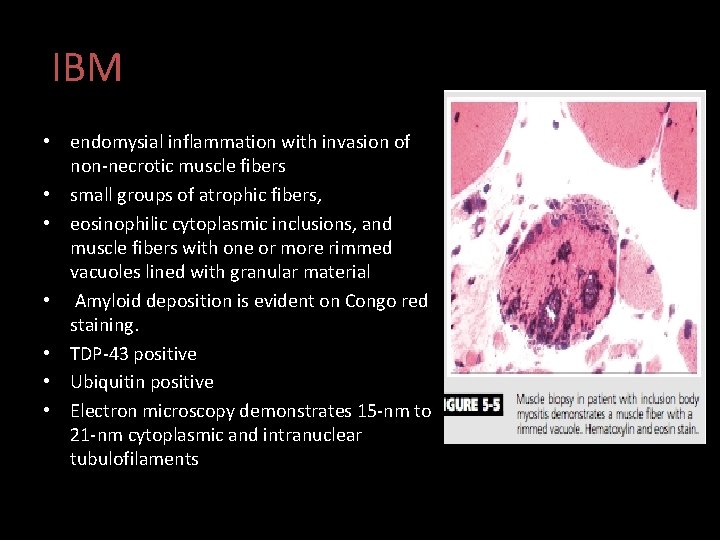
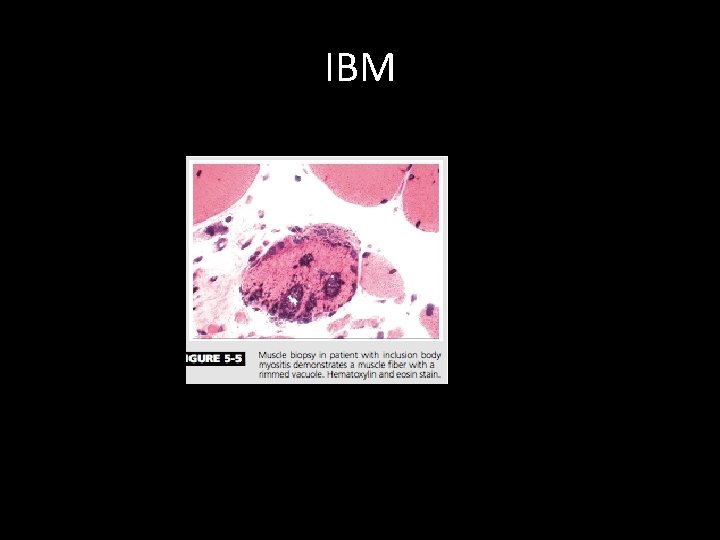
IBM • endomysial inflammation with invasion of non-necrotic muscle fibers • small groups of atrophic fibers, • eosinophilic cytoplasmic inclusions, and muscle fibers with one or more rimmed vacuoles lined with granular material • Amyloid deposition is evident on Congo red staining. • TDP-43 positive • Ubiquitin positive • Electron microscopy demonstrates 15 -nm to 21 -nm cytoplasmic and intranuclear tubulofilaments

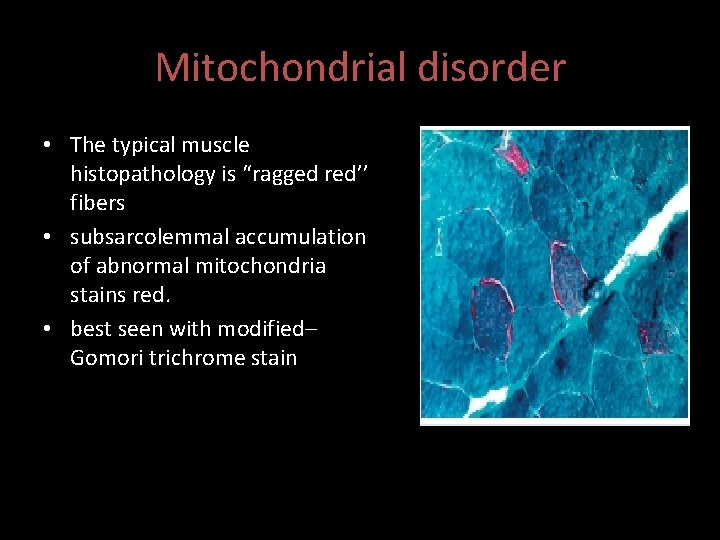
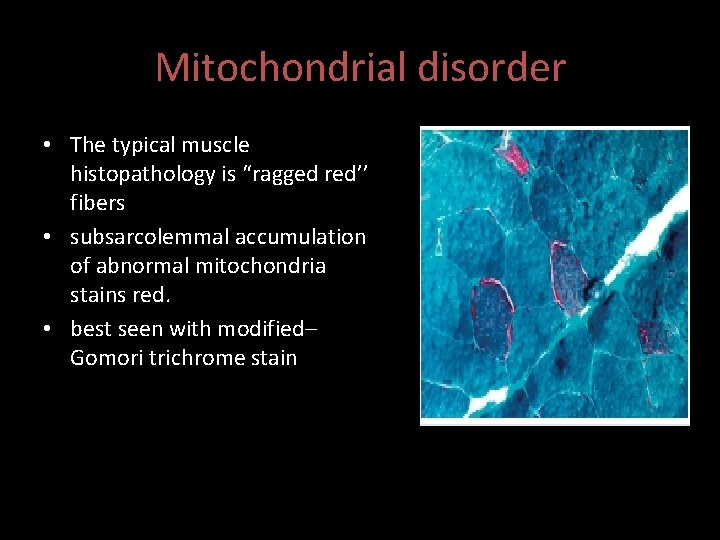
Mitochondrial disorder • The typical muscle histopathology is “ragged red’’ fibers • subsarcolemmal accumulation of abnormal mitochondria stains red. • best seen with modified– Gomori trichrome stain
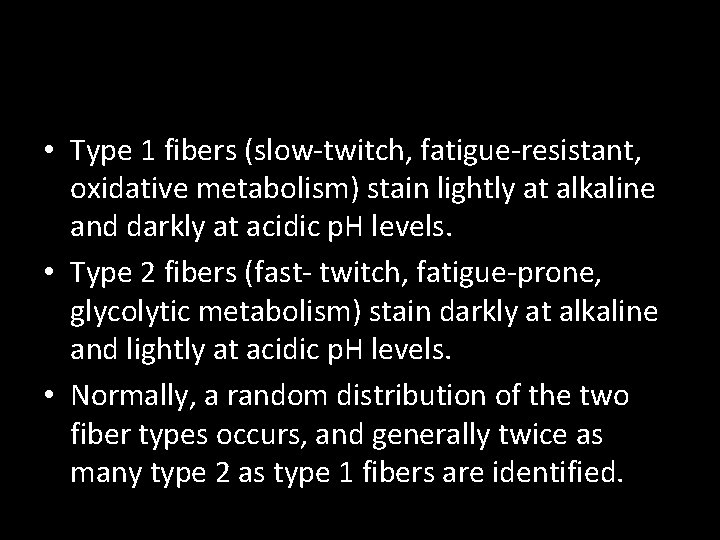
• Type 1 fibers (slow-twitch, fatigue-resistant, oxidative metabolism) stain lightly at alkaline and darkly at acidic p. H levels. • Type 2 fibers (fast- twitch, fatigue-prone, glycolytic metabolism) stain darkly at alkaline and lightly at acidic p. H levels. • Normally, a random distribution of the two fiber types occurs, and generally twice as many type 2 as type 1 fibers are identified.

• W • Increased variability in muscle fiber size • degeneration, regeneration, isolated ‘‘opaque’’ hypertrophic fibers, and significant replacement of muscle by fat and connective tissue. • Central nuclei are present in 2% to 4% of the fibers. • Type 1 fiber predominance is seen in most patients. • Inflammatory cell infiltrates in the perimysium, endomysium, and perivascular spaces and consist mostly of mononuclear cells, especially macrophages. • endomysial and perimysial fibrosis with disease progression


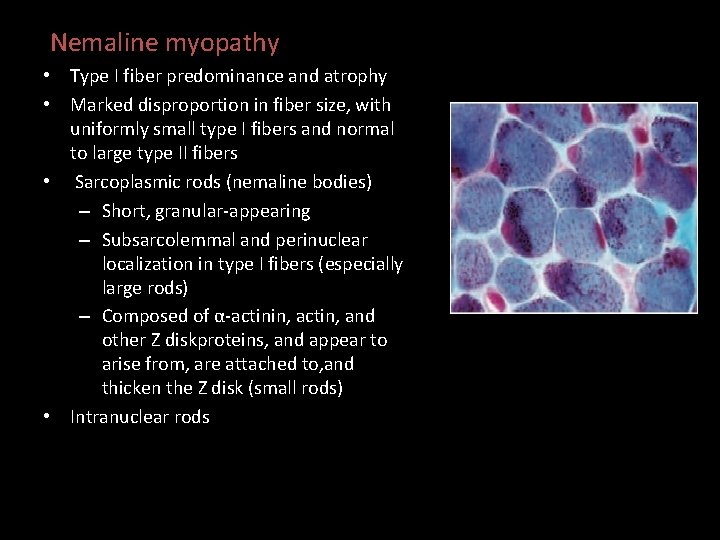
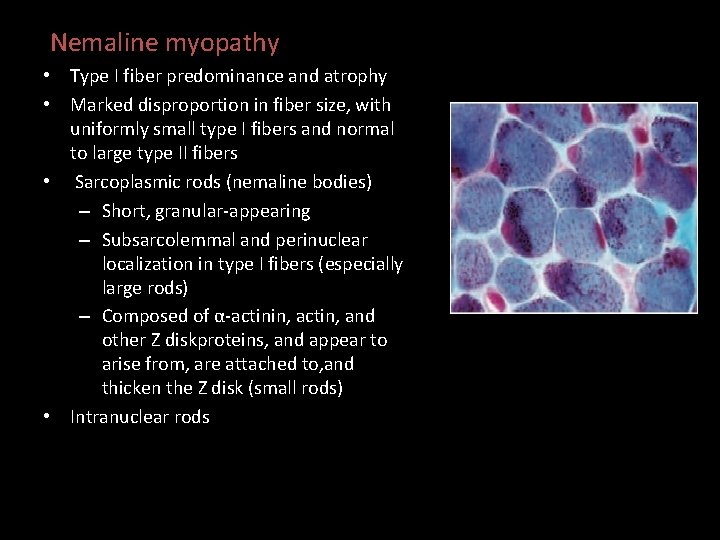
Nemaline myopathy • Type I fiber predominance and atrophy • Marked disproportion in fiber size, with uniformly small type I fibers and normal to large type II fibers • Sarcoplasmic rods (nemaline bodies) – Short, granular-appearing – Subsarcolemmal and perinuclear localization in type I fibers (especially large rods) – Composed of α-actinin, actin, and other Z diskproteins, and appear to arise from, are attached to, and thicken the Z disk (small rods) • Intranuclear rods
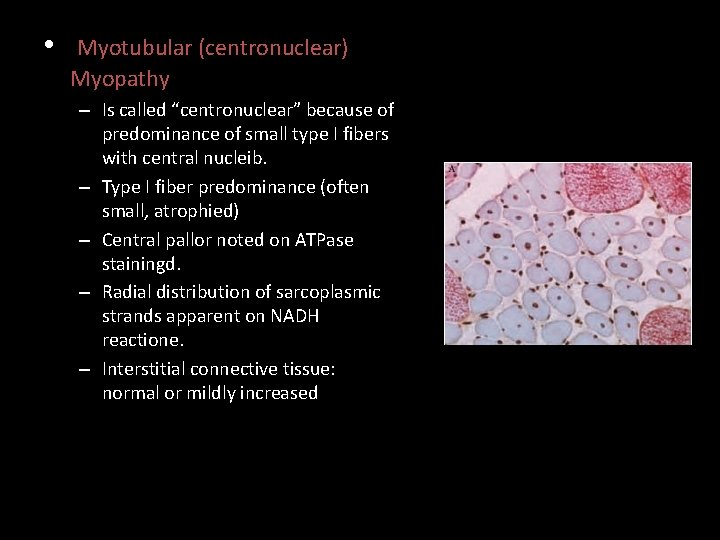
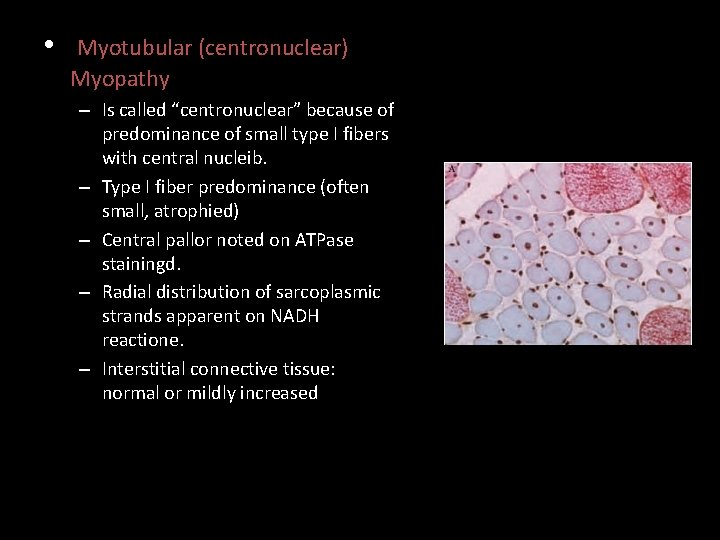
• Myotubular (centronuclear) Myopathy – Is called “centronuclear” because of predominance of small type I fibers with central nucleib. – Type I fiber predominance (often small, atrophied) – Central pallor noted on ATPase stainingd. – Radial distribution of sarcoplasmic strands apparent on NADH reactione. – Interstitial connective tissue: normal or mildly increased
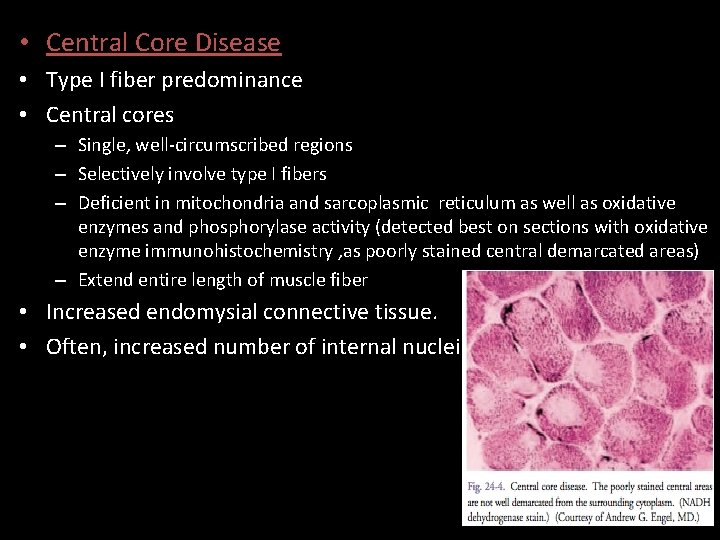
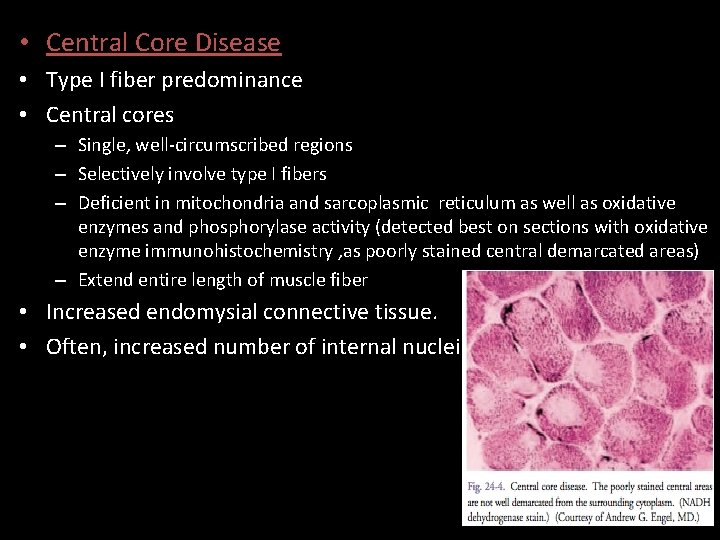
• Central Core Disease • Type I fiber predominance • Central cores – Single, well-circumscribed regions – Selectively involve type I fibers – Deficient in mitochondria and sarcoplasmic reticulum as well as oxidative enzymes and phosphorylase activity (detected best on sections with oxidative enzyme immunohistochemistry , as poorly stained central demarcated areas) – Extend entire length of muscle fiber • Increased endomysial connective tissue. • Often, increased number of internal nuclei

Molecular Genetic Studies • Disorders With Commercially Available Molecular Genetic Studies Performed With Peripheral Blood Samples – – – Duchenne and Becker muscular dystrophies ” FSHD MD (types 1 and 2) " OPMD LGMD 1 B, 2 A, 2 C– 2 F, and 2 I " Congenital muscular dystrophy (FKRP, FCMD, MEB, and POMT 1 mutations) " Nonaka myopathy/inclusion body myopathy type 2 " Nemaline myopathy (ACTA 1 mutations) " Myotubular myopathy (MTM 1 mutations) " MERRF MELAS

Case 1 • A 51 -year-old man without significant past medical • Slowly progressive muscle weakness for the past 7 years. • His symptoms initially began with difficulty walking down stairs because his left knee would ‘‘give out. ’’ • He currently has difficulty arising from a chair and grasping objects with his right hand.

• Current examination reveals intact cranial nerves, sensation, and muscle stretch reflexes. • Motor examination in the right upper extremity shows MRC grade 5 shoulder abduction, grade 5 elbow flexion/extension, grade 4 wrist flexion, grade 5 wrist extension, and grade 3 finger flexion. • Strength in the left upper extremity is normal except for grade 4+ finger flexion. • In the left lower extremity, the patient exhibits grade 4+ hip flexion, grade 3+ knee extension, and grade 4+ ankle dorsiflexion. • In the right lower extremity, strength is normal except for grade 4+ knee extension.
• The chronic onset, asymmetrical distribution of weakness, and selective involvement of wrist/finger flexion and knee extension • CK= 500 • EMG= myopathy • Muscle biopsy
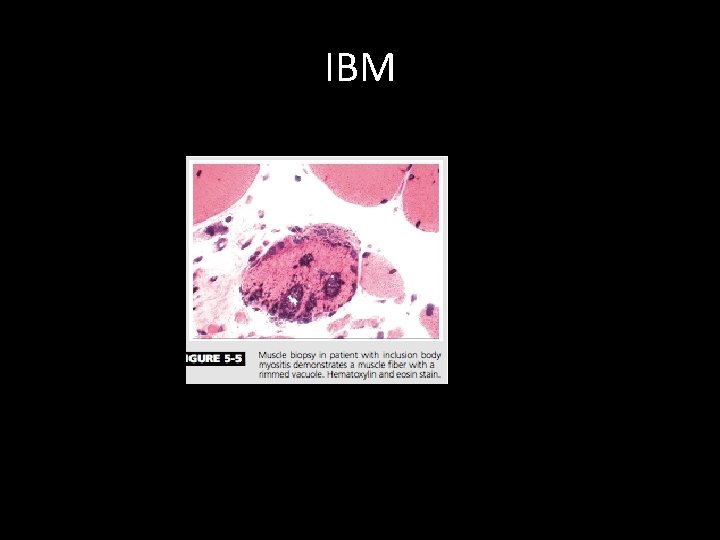
IBM
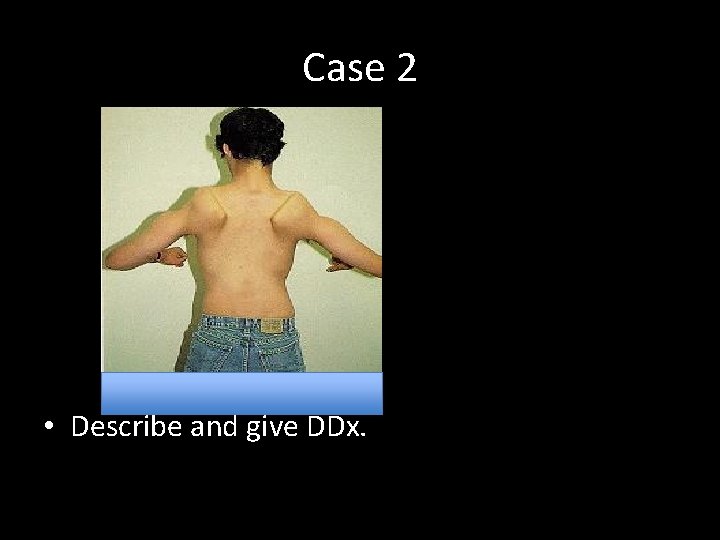
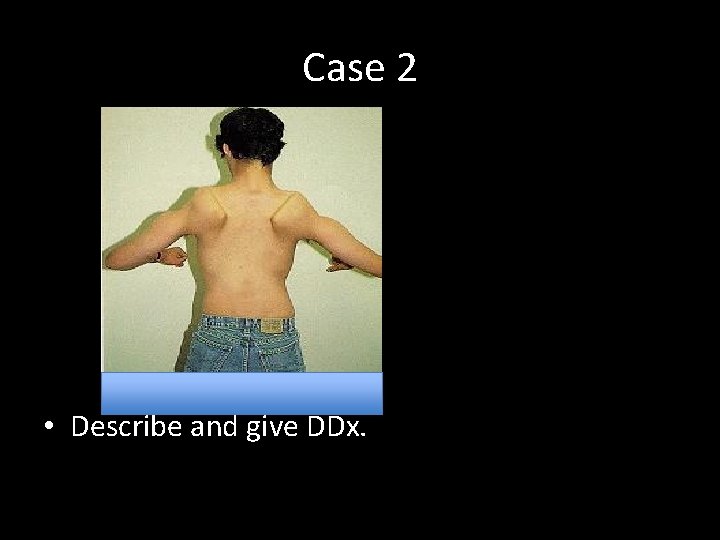
Case 2 • Describe and give DDx.
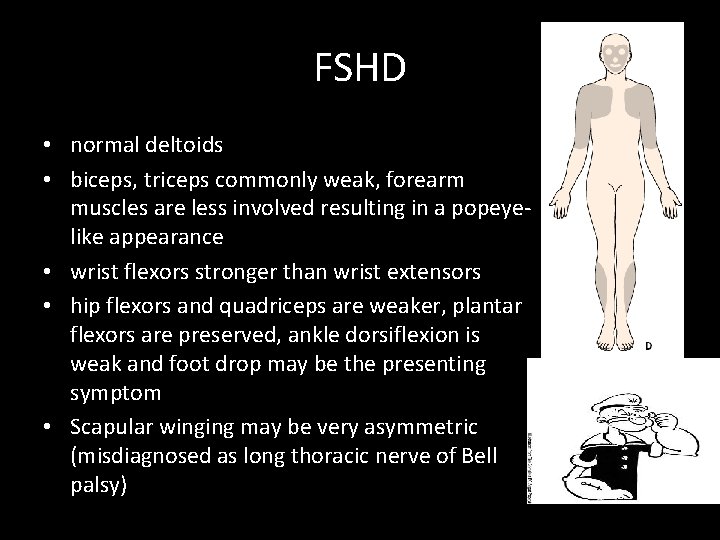
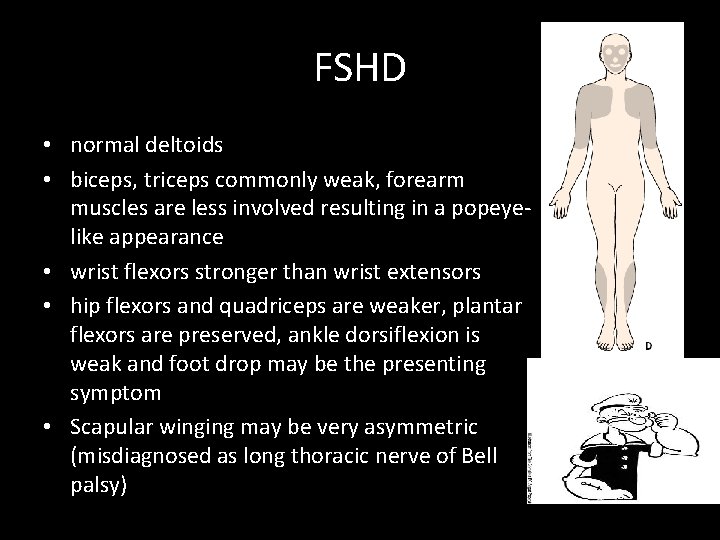
FSHD • normal deltoids • biceps, triceps commonly weak, forearm muscles are less involved resulting in a popeyelike appearance • wrist flexors stronger than wrist extensors • hip flexors and quadriceps are weaker, plantar flexors are preserved, ankle dorsiflexion is weak and foot drop may be the presenting symptom • Scapular winging may be very asymmetric (misdiagnosed as long thoracic nerve of Bell palsy)
• Thanks!
 Myopathy
Myopathy Physiology of muscle contraction
Physiology of muscle contraction Steroid myopathy
Steroid myopathy Difference between code first and database first approach
Difference between code first and database first approach First aid for fainting with pictures
First aid for fainting with pictures What was the goal of the first continental congress?
What was the goal of the first continental congress? Explain virtual circuit and datagram network
Explain virtual circuit and datagram network Theoretical models of counseling
Theoretical models of counseling Michael treacy and fred wiersema
Michael treacy and fred wiersema Multiple approach-avoidance conflict
Multiple approach-avoidance conflict Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Research approach definition
Research approach definition Traditional approach to systems implementation
Traditional approach to systems implementation Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Glasgow thang điểm
Glasgow thang điểm Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Các số nguyên tố là gì
Các số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Assumptions of psychodynamic theory
Assumptions of psychodynamic theory Customer first approach
Customer first approach To approach and speak to first
To approach and speak to first Coverdale systematic approach steps
Coverdale systematic approach steps Cash flow adjustments
Cash flow adjustments Stages of maturity 7 habits
Stages of maturity 7 habits Breadth vs depth search
Breadth vs depth search Sdl first vs code first
Sdl first vs code first Habit 3 lesson plans
Habit 3 lesson plans Put first things first
Put first things first First to file vs first to invent
First to file vs first to invent Stack declaration
Stack declaration Diketahui suatu stack dgn max_stack = 6
Diketahui suatu stack dgn max_stack = 6 First in first out
First in first out First come first serve
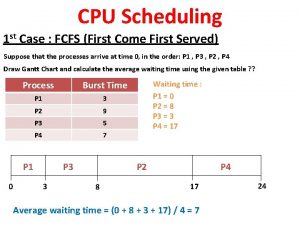
First come first serve Put first things first definition
Put first things first definition Gantt chart first come first serve
Gantt chart first come first serve See do get model
See do get model Habit number 3
Habit number 3 Put first things first video
Put first things first video Put first things first activities
Put first things first activities First aid merit badge first aid kit
First aid merit badge first aid kit Which is an objective of first aid
Which is an objective of first aid 7 habits promise
7 habits promise Zero safety incidents
Zero safety incidents Pci goal
Pci goal What was the goal of stalin's 5 year plan
What was the goal of stalin's 5 year plan Sbp goal
Sbp goal