Myopathies The term myopathy encompasses a heterogeneous group








- Slides: 41
Myopathies The term myopathy encompasses a heterogeneous group of disorders, both morphologically and clinically.
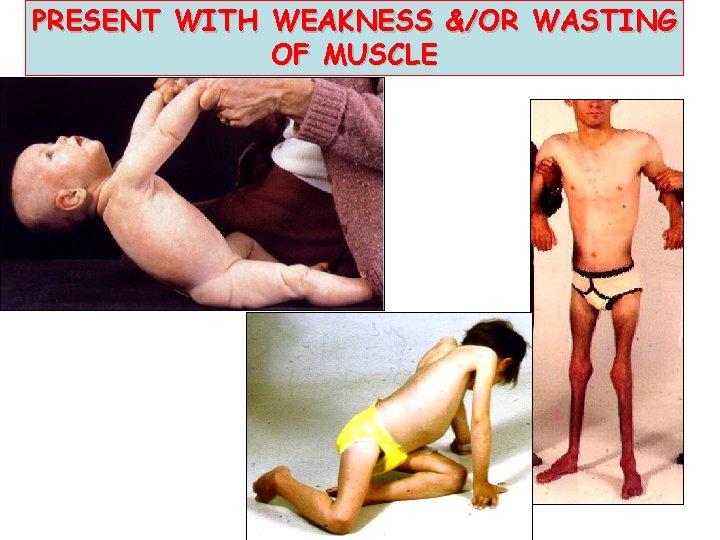
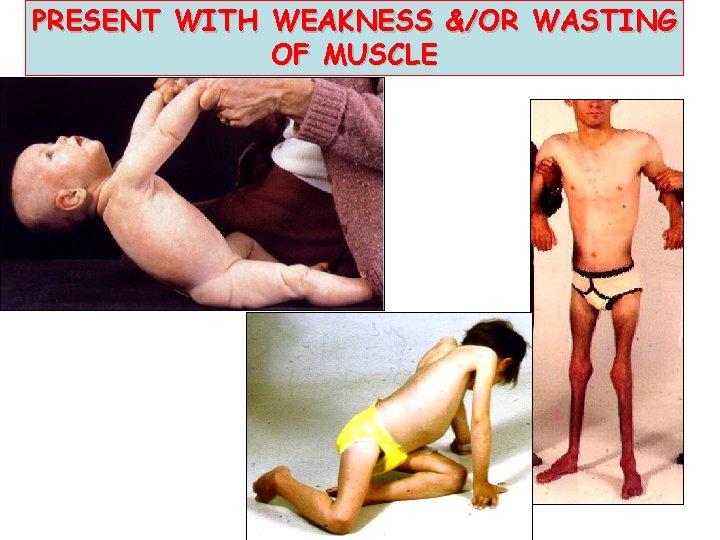
PRESENT WITH WEAKNESS &/OR WASTING OF MUSCLE
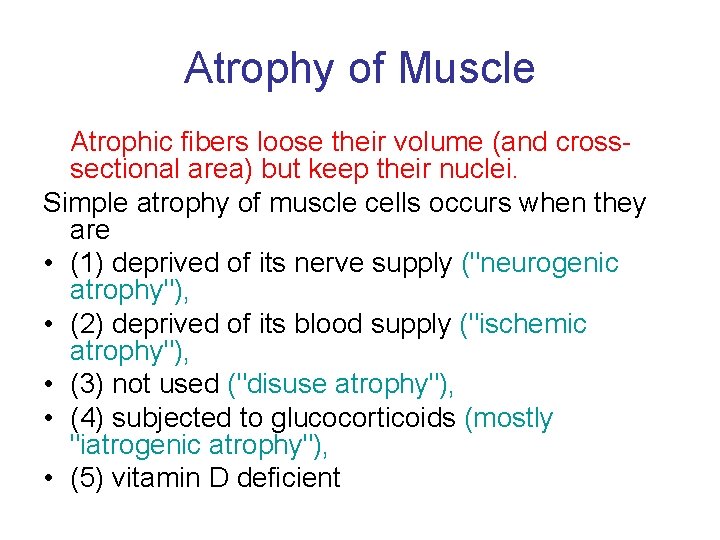
Atrophy of Muscle Atrophic fibers loose their volume (and crosssectional area) but keep their nuclei. Simple atrophy of muscle cells occurs when they are • (1) deprived of its nerve supply ("neurogenic atrophy"), • (2) deprived of its blood supply ("ischemic atrophy"), • (3) not used ("disuse atrophy"), • (4) subjected to glucocorticoids (mostly "iatrogenic atrophy"), • (5) vitamin D deficient



PRIMARY MYOPATHIES • • • In this broad group of disorders the abnormality is within the muscle fiber. A number of these disorders may microscopically resemble one another closely, making precise histological classification difficult. Consequently a detailed clinical and family history is essential. Some of these conditions are genetically determined (hereditary) although the exact abnormality may be unknown. In others, there is an identifiable metabolic abnormality.
• Unknown etiology: Occasionally they appear to be the result of an error at some stage of muscle development and present as congenital disorders, while some are associated with prominent inflammation and a disturbance of the immune system. • Classification of primary myopathies: – – 1. Dystrophic myopathies 2. Congenital myopathies 3. Metabolic myopathies 4. Inflammatory myopathy
1. Dystrophic myopathies • A group of genetically determined (hereditary) myopathies, • largely of unknown etiology, • characterised by progressive degeneration of muscle fibres, resulting clinically in progressive weakness and wasting of muscle. • The 4 major patterns are: – a. Duchenne muscular dystrophy: males, death by 20 yrs age. Now known to be due to a genetic abnormality resulting in a deficiency of dystrophin (a large structural protein playing a role in maintaining integrity of muscle fibres) – b. Myotonic dystrophy – c. Limb-girdle dystrophy (proximal limb muscles) – d. Fascioscapulohumeral dystrophy.
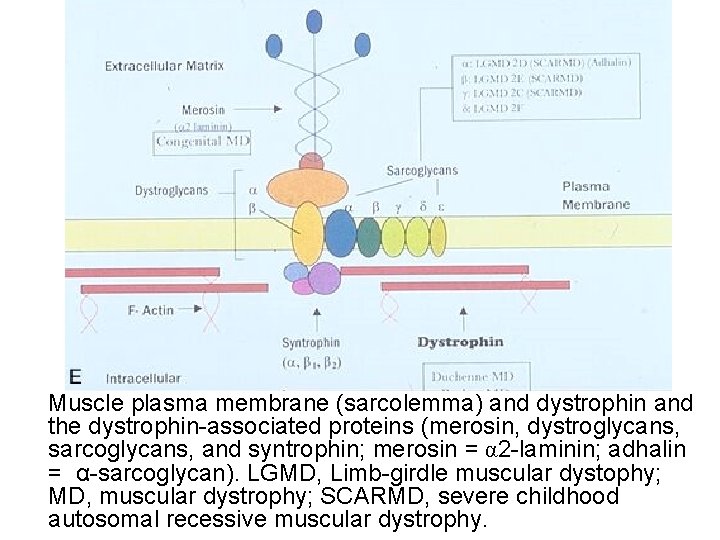
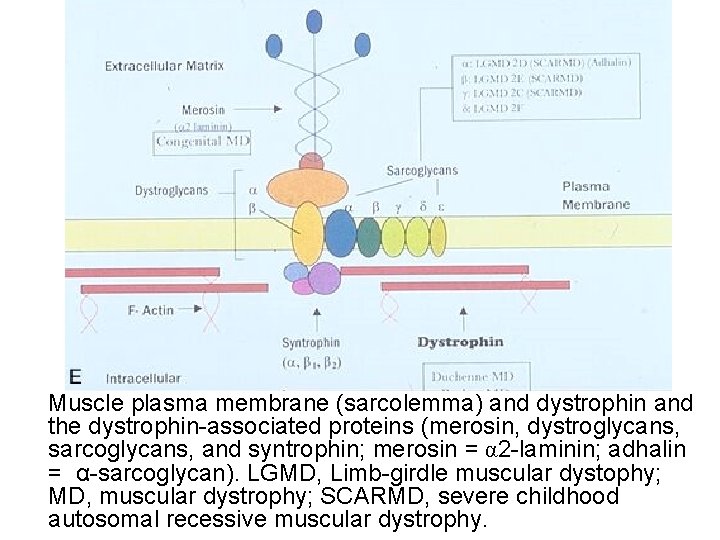
Muscle plasma membrane (sarcolemma) and dystrophin and the dystrophin-associated proteins (merosin, dystroglycans, sarcoglycans, and syntrophin; merosin = α 2 -laminin; adhalin = α-sarcoglycan). LGMD, Limb-girdle muscular dystophy; MD, muscular dystrophy; SCARMD, severe childhood autosomal recessive muscular dystrophy.
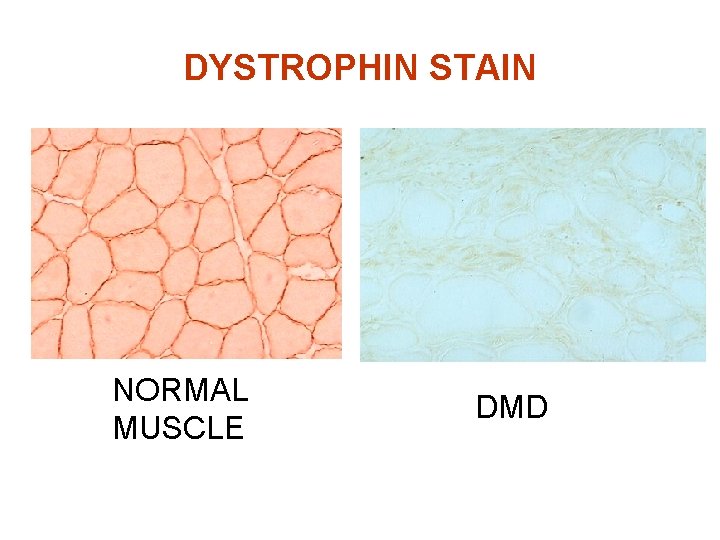
DUCHENNE DYSTROPHY • Genetically determined (X-linked) • Deficiency of DYSTROPHIN (normally present in muscle cell membrane) - Raised CPK • Presents males 2 -4 years • Weakness • Pseudohypertophy of the calves • Die by age 20 years
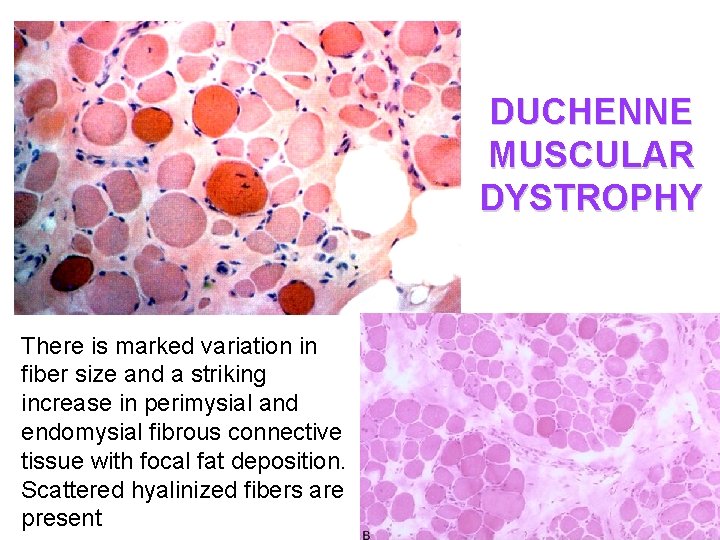
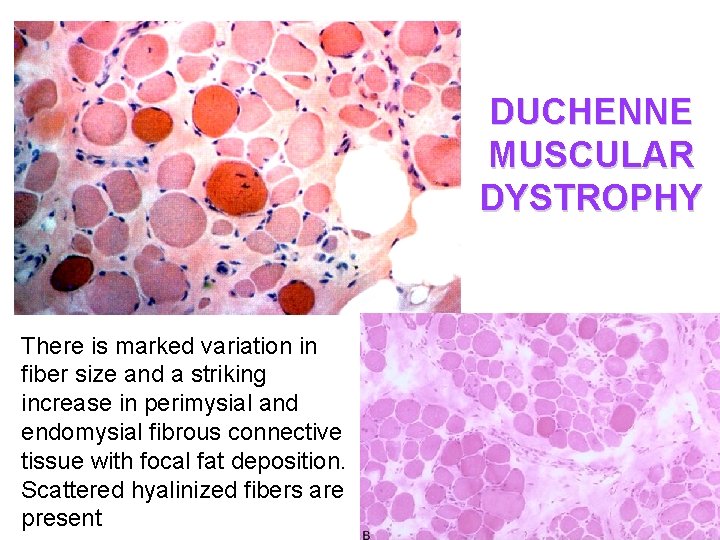
DUCHENNE MUSCULAR DYSTROPHY There is marked variation in fiber size and a striking increase in perimysial and endomysial fibrous connective tissue with focal fat deposition. Scattered hyalinized fibers are present
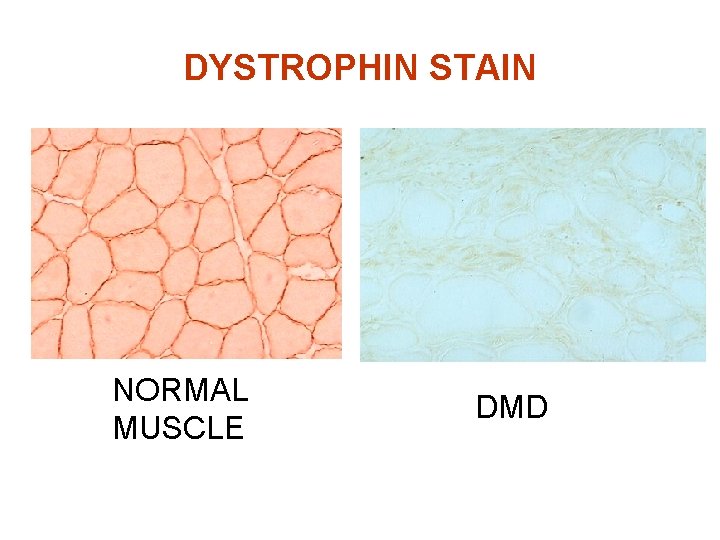
DYSTROPHIN STAIN NORMAL MUSCLE DMD
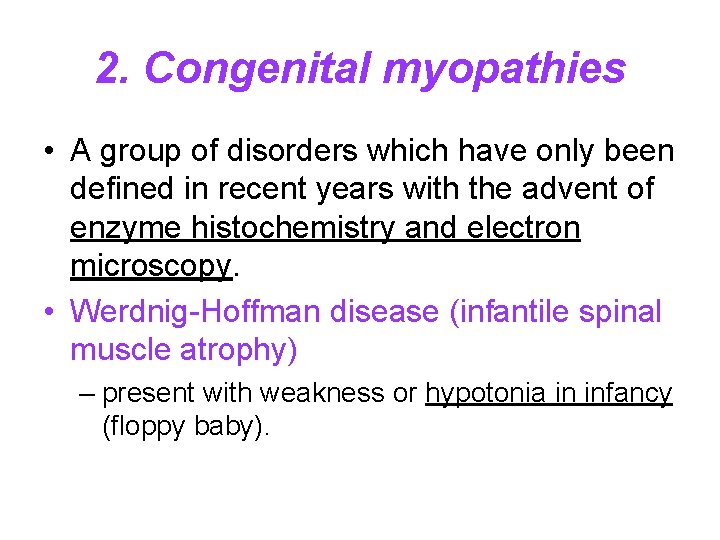
2. Congenital myopathies • A group of disorders which have only been defined in recent years with the advent of enzyme histochemistry and electron microscopy. • Werdnig-Hoffman disease (infantile spinal muscle atrophy) – present with weakness or hypotonia in infancy (floppy baby).

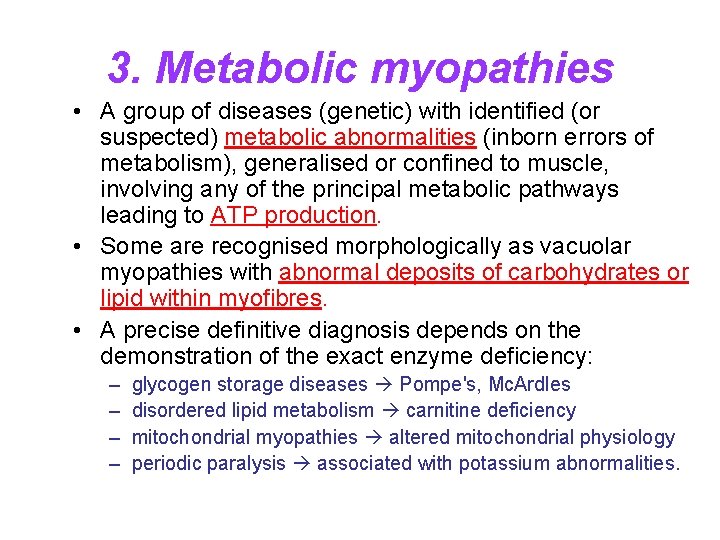
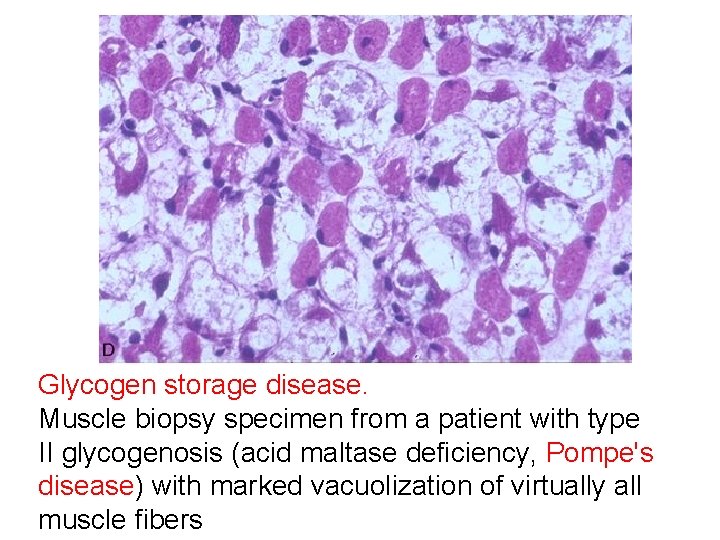
3. Metabolic myopathies • A group of diseases (genetic) with identified (or suspected) metabolic abnormalities (inborn errors of metabolism), generalised or confined to muscle, involving any of the principal metabolic pathways leading to ATP production. • Some are recognised morphologically as vacuolar myopathies with abnormal deposits of carbohydrates or lipid within myofibres. • A precise definitive diagnosis depends on the demonstration of the exact enzyme deficiency: – – glycogen storage diseases Pompe's, Mc. Ardles disordered lipid metabolism carnitine deficiency mitochondrial myopathies altered mitochondrial physiology periodic paralysis associated with potassium abnormalities.
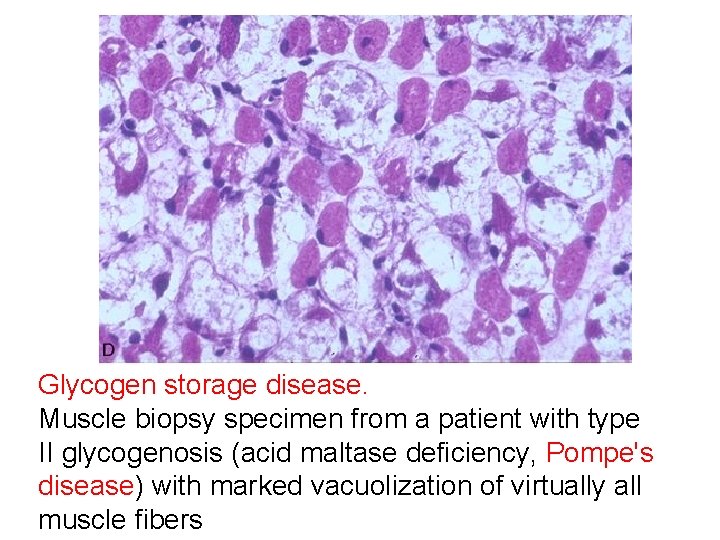
Glycogen storage disease. Muscle biopsy specimen from a patient with type II glycogenosis (acid maltase deficiency, Pompe's disease) with marked vacuolization of virtually all muscle fibers

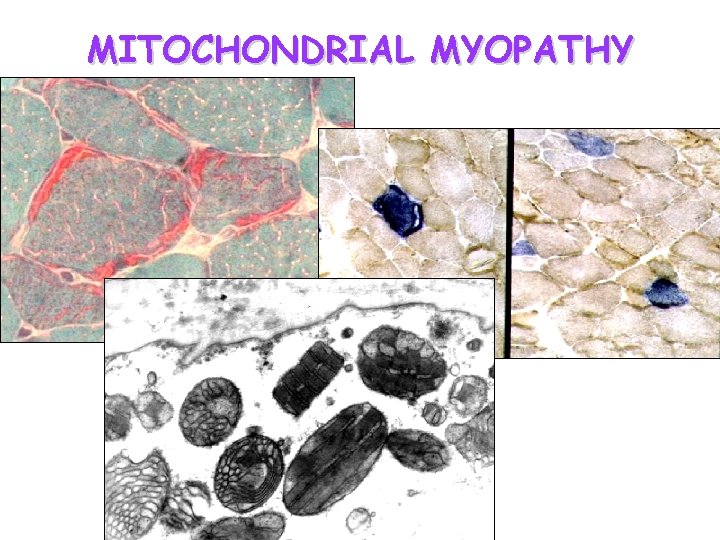
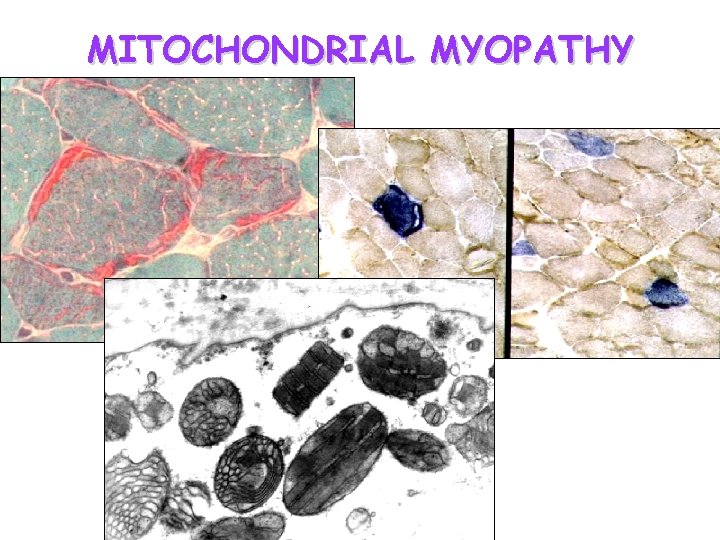
MITOCHONDRIAL MYOPATHY
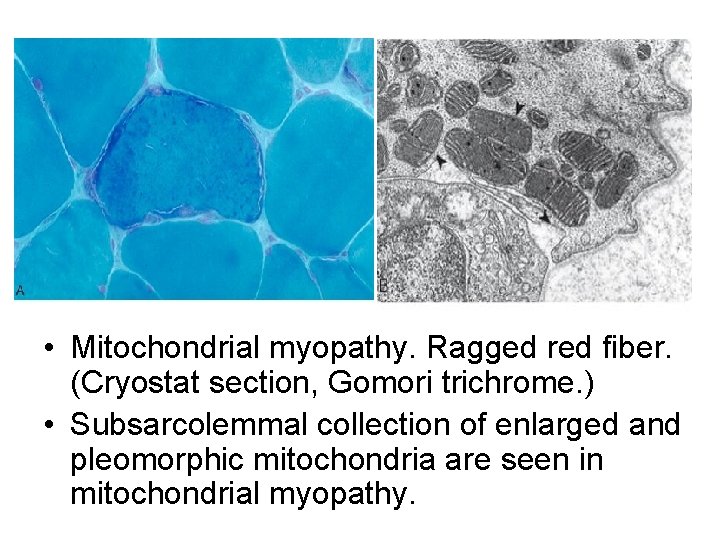
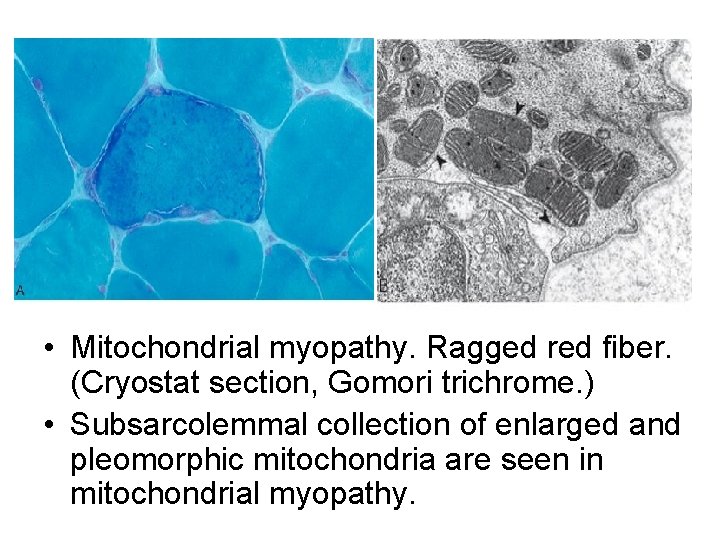
• Mitochondrial myopathy. Ragged red fiber. (Cryostat section, Gomori trichrome. ) • Subsarcolemmal collection of enlarged and pleomorphic mitochondria are seen in mitochondrial myopathy.
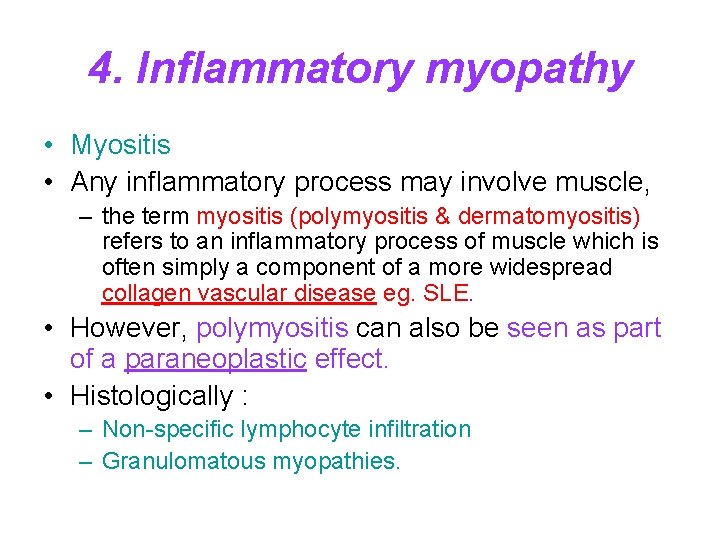
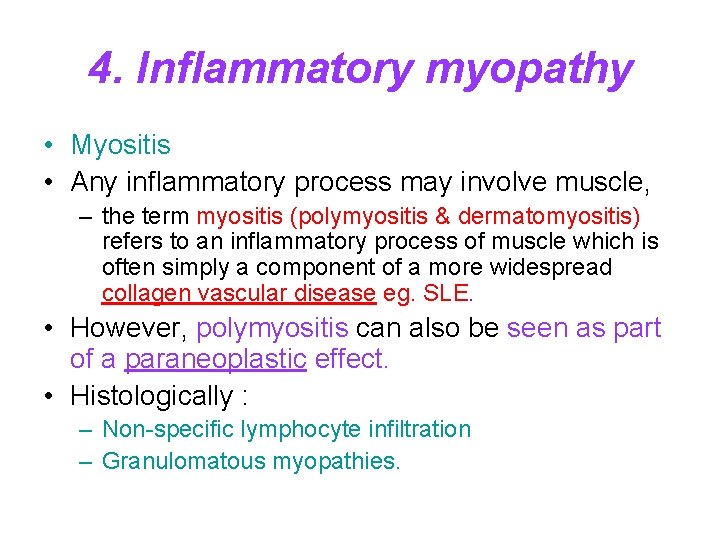
4. Inflammatory myopathy • Myositis • Any inflammatory process may involve muscle, – the term myositis (polymyositis & dermatomyositis) refers to an inflammatory process of muscle which is often simply a component of a more widespread collagen vascular disease eg. SLE. • However, polymyositis can also be seen as part of a paraneoplastic effect. • Histologically : – Non-specific lymphocyte infiltration – Granulomatous myopathies.
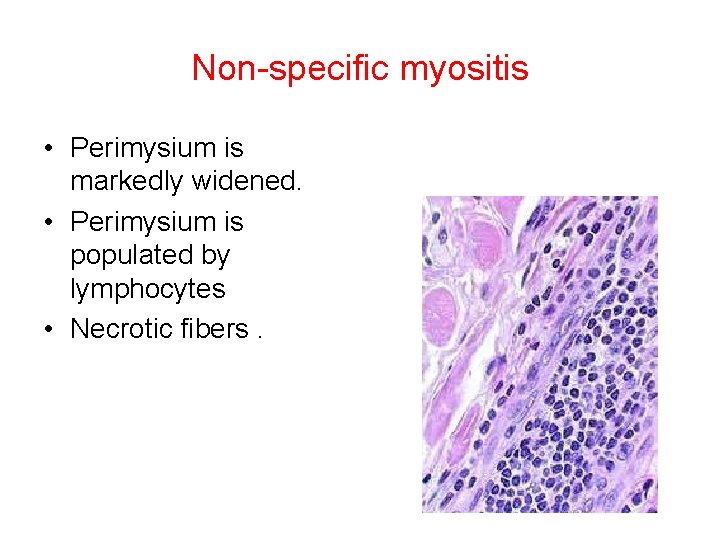
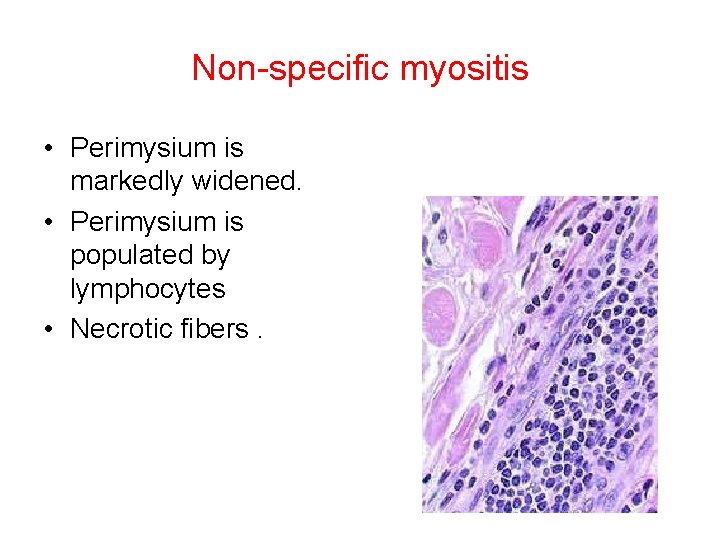
Non-specific myositis • Perimysium is markedly widened. • Perimysium is populated by lymphocytes • Necrotic fibers.
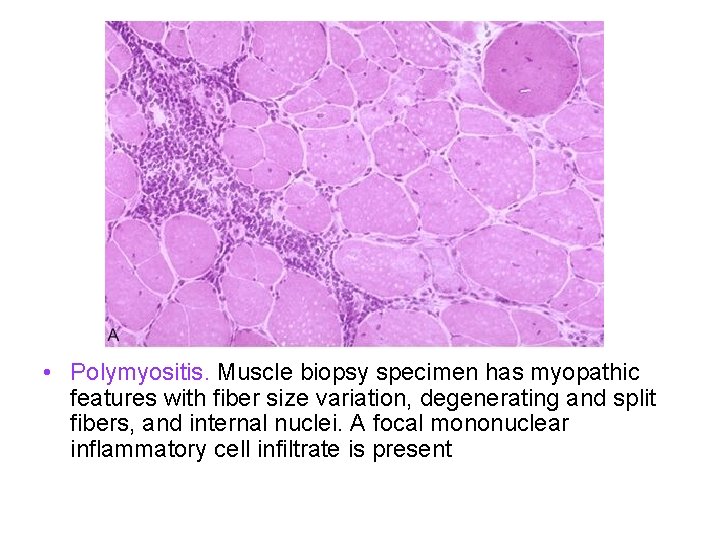
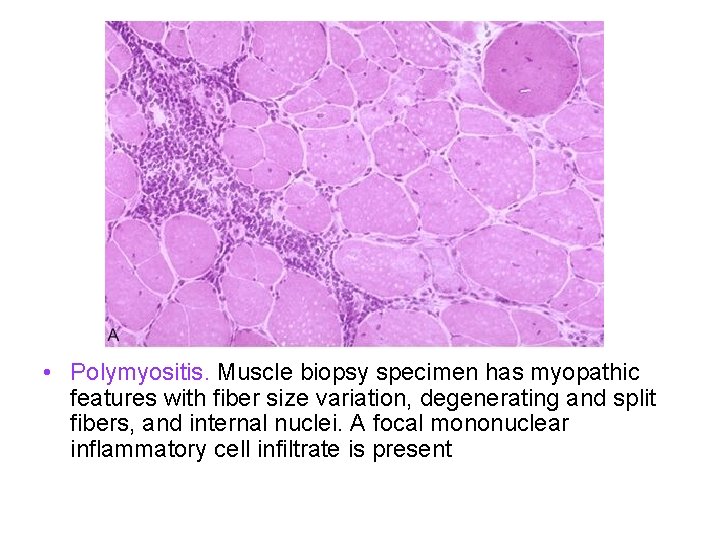
• Polymyositis. Muscle biopsy specimen has myopathic features with fiber size variation, degenerating and split fibers, and internal nuclei. A focal mononuclear inflammatory cell infiltrate is present
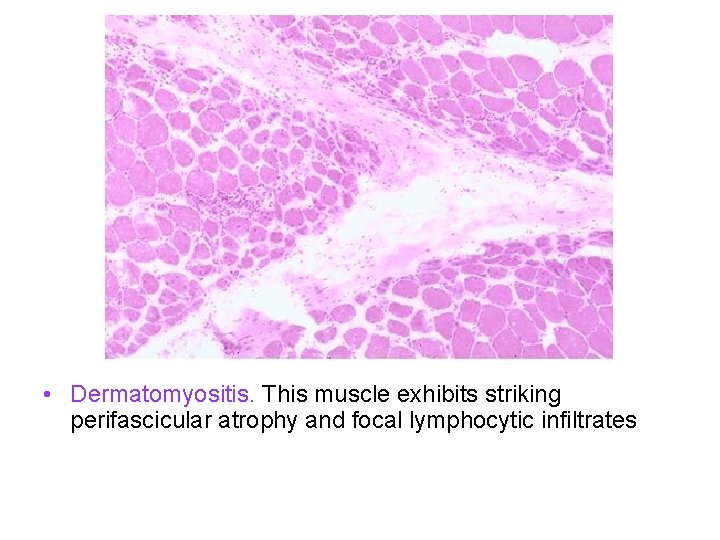
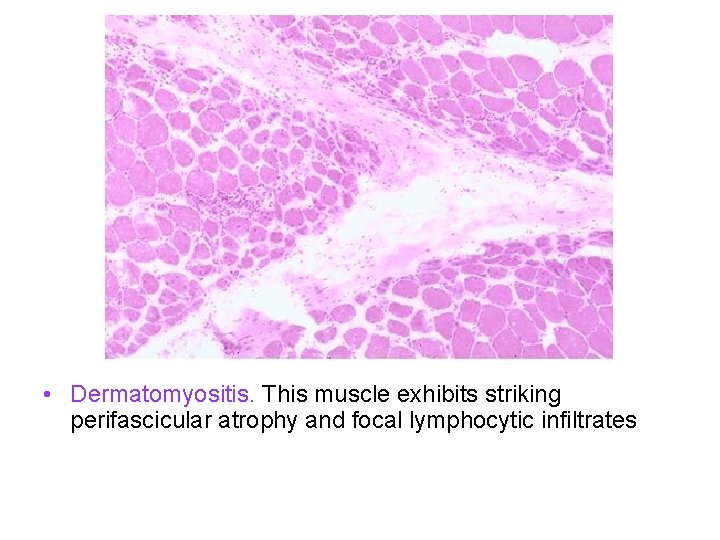
• Dermatomyositis. This muscle exhibits striking perifascicular atrophy and focal lymphocytic infiltrates
Granulomatous myopathies • Clinical features – Dysphagia – Muscle hypertrophy – Post-menopausal females. • Pathology – Granulomas • Non-caseating • Location in muscle.

SECONDARY MYOPATHIES • The muscle is secondarily affected by disease processes outside the neuro- muscular system: – 1. Cachetic atrophy - seen in many wasting conditions eg. chronic infection, cancer, malabsorption, old age. – 2. Endocrine disorders - eg. acromegaly, hyper and hypothyroidism, hyperaldosteronism (K+), hyperparathyroidism, corticosteroid excess. – 3. Alcohol and other drugs - may produce a "necrotising, inflammatory myopathy". – 4. Vit D deficiency.
MYASTHENIA GRAVIS • A disorder of the neuromuscular strength that occurs during sustained or repetitive muscle contraction. • In obtaining the history it is essential to document that loss of muscle power occurs in association with continuous effort. • It is also necessary to inquire about common signs and symptoms, such as ptosis, diplopia, dysarthria or dysphagia. • Improvement with rest is an important feature of the disease.
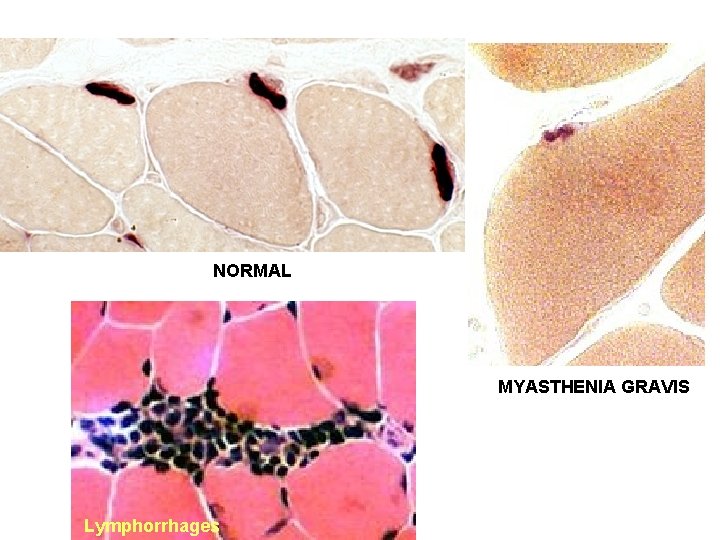
• Young women • Polyclonal antibodies attack the acetylcholine receptor of the post-synaptic membrane of the neuromuscular junction. • This is not an anatomic pathologist's disease. – In a minority of patients clusters of lymphocytes ("lymphorrhages") appear around the motor end plates. Anti-skeletal muscle antibody titer: Elevated in 95% of patients with thymoma.

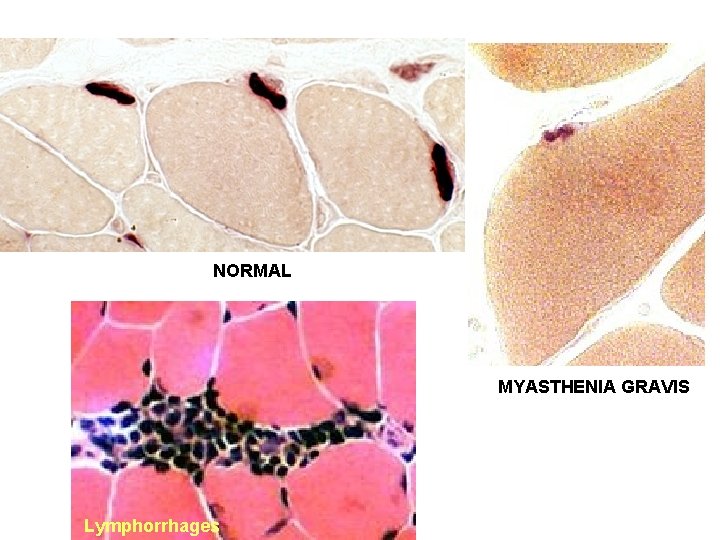
NORMAL MYASTHENIA GRAVIS Lymphorrhages
Types of MG • 1. Autoimmune ocular: Many patients present with ocular involvement. Some have disease restricted to ocular musculature and never have generalized MG. • 2. Autoimmune generalized: – a. Many patients present with ocular symptoms. – b. Most patients have generalized weakness within 13 months of clinical onset. – c. 40% improve. – d. 15% develop irreversible weakness and atrophy.
• 3. Transient neonatal MG: is produced by passive transfer of maternal antibodies from a mother with MG. • 4. Congenital MG: Multiple forms occur with different pathophysiological mechanisms such as structural and/or electrophysiologic defects of the neuromuscular junction. These are congenital syndromes and not related to autoimmunity. • 5. Drug Induced MG: Antibody mediated MG is sometimes caused by the drug Penicillamine. • 6. Neuromuscular Junction Blockade (NJM): Gentamicin and other Aminoglycoside antibiotics can cause a pharmacologic block of the NJM which has clinical features similar to MG without autoimmunity.
Autoimmune diseases associated with MG • • • Autoimmune Thyroid Diseases Systemic Lupus Erythematosus (SLE) Rheumatoid arthritis Pernicious anemia Pemphigus vulgaris (an autoimmune skin disease)
MYASTHENIC SYNDROMES • CONGENITAL MYASTHENIC SYNDROMES – not associated with antibody or autoimmunity • LAMBERT-EATON MYASTHENIC SYNDROME – Weakness and fatigue of proximal muscles – relative sparing of ocular and bulbar muscles. – common association with carcinoma • specifically oat cell carcinoma of the lung.
BOTULISM • A food-borne illness caused by the exotoxin of clostridium botulinum. • Canned vegetables are the most frequent source of poisoning. • Symptoms frequently begin 12 to 36 hours after ingestion of the contaminated food.
Symptoms and clinical findings of Botulism 1. Blurred vision and diplopia 2. Ptosis 3. Extraocular muscle palsies 4. Dysarthria and dysphagia 5. Progressive generalized weakness with respiratory failure. 6. Dilated pupils 7. Constipation
AMYOTROPHIC LATERAL SCLEROSIS • A progressive disorder involving lower and upper motor systems. • Clinical features: Wasting and weakness of muscles with visible fasciculations in scattered muscles. – The disease frequently presents in the upper extremities but may initially involve lower extremities or bulbar muscles. – Hyper-reflexia and spasticity may be observed.
• Pathology: – Shrinkage with sclerosis in the corticospinal tracts – Degeneration of the large anterior horn neurons noted in spinal cord and brainstem – Degeneration of the large Betz cells of the motor cortex.
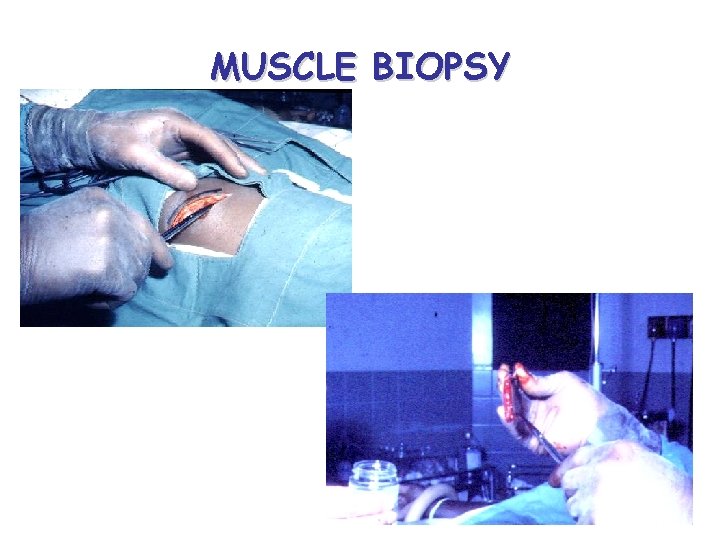
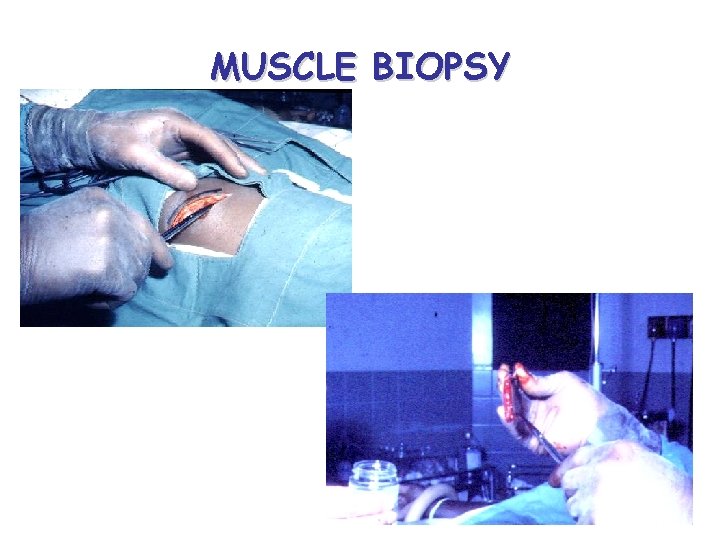
MUSCLE BIOPSY
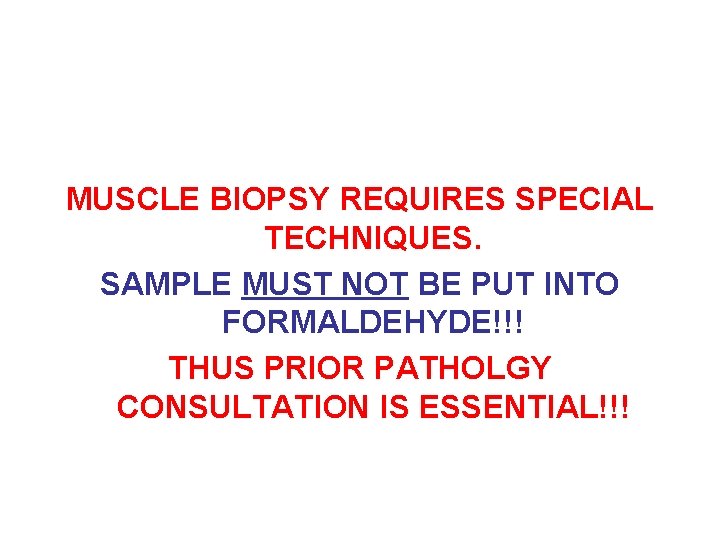
MUSCLE BIOPSY REQUIRES SPECIAL TECHNIQUES. SAMPLE MUST NOT BE PUT INTO FORMALDEHYDE!!! THUS PRIOR PATHOLGY CONSULTATION IS ESSENTIAL!!!

 Myopathy
Myopathy Terminal cisternae
Terminal cisternae Steroid myopathy
Steroid myopathy Crime scene vocabulary
Crime scene vocabulary V
V It encompasses several different aspects including
It encompasses several different aspects including What encompasses all activities associated with the flow
What encompasses all activities associated with the flow Medicated scalp lotion definition
Medicated scalp lotion definition English cuisine encompasses
English cuisine encompasses What encompasses all activities associated with the flow
What encompasses all activities associated with the flow Software encompasses
Software encompasses The biosphere encompasses all of the
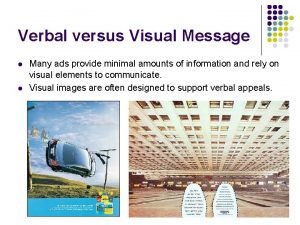
The biosphere encompasses all of the Verbal advertisement
Verbal advertisement Long medium and short term planning in primary schools
Long medium and short term planning in primary schools Term-to-term rule
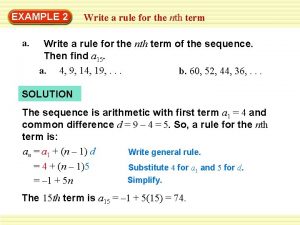
Term-to-term rule Long term memory vs short term memory
Long term memory vs short term memory Quadratic sequence formula
Quadratic sequence formula Example of short term human resources
Example of short term human resources Term to term rule
Term to term rule Difference between long term and short term liabilities
Difference between long term and short term liabilities Long term liabilities
Long term liabilities Minterm maxterm
Minterm maxterm Term to term rule example
Term to term rule example Term to term rule
Term to term rule Example of short term goal
Example of short term goal Short term finance planning
Short term finance planning Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Hát lên người ơi
Hát lên người ơi Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới