1 pain assessment The importance of pain assessment



- Slides: 57
1
pain assessment • The importance of pain assessment was identified as a necessary first step in improving the effectiveness of pain Management. 4
Principles of Assessment • Assess and reassess. • Reassess Intensity, Relief, And Side Effects. • Use verbal report whenever possible. • Document in a visible place. • Include the family. 5
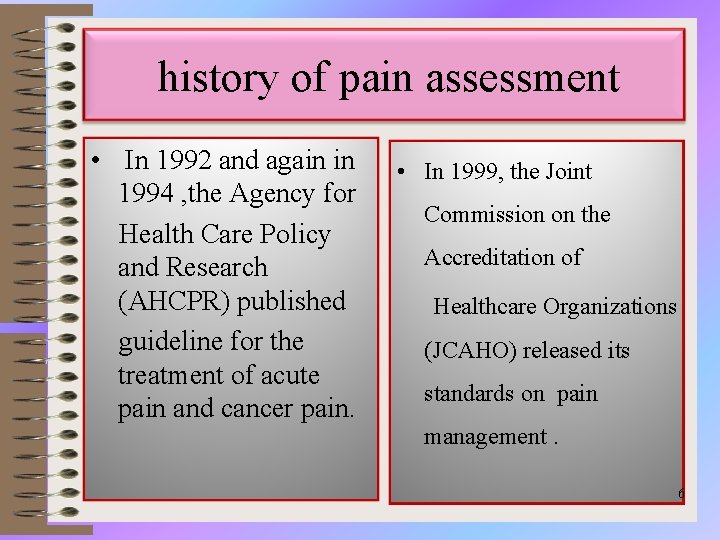
history of pain assessment • In 1992 and again in 1994 , the Agency for Health Care Policy and Research (AHCPR) published guideline for the treatment of acute pain and cancer pain. • In 1999, the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) released its standards on pain management. 6
The Role of Nursing in Pain assessment ü Onset ü Location ü Duration ü Radiation ü Influence of pain in daily and quality of life 7
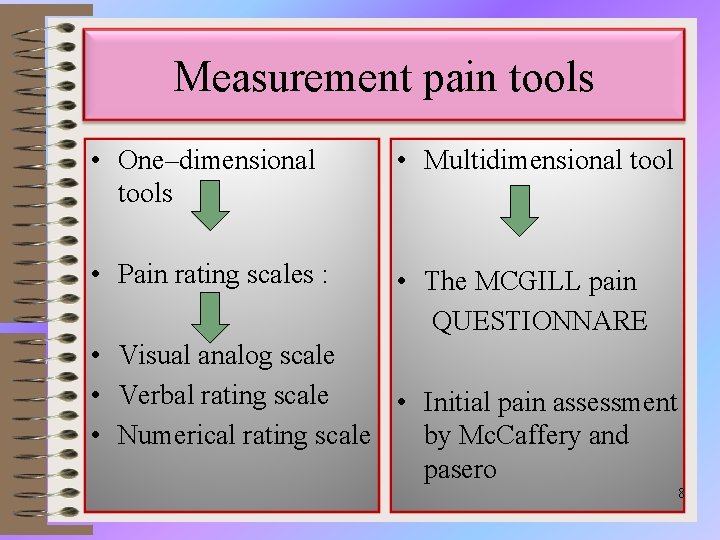
Measurement pain tools • One–dimensional tools • Multidimensional tool • Pain rating scales : • The MCGILL pain QUESTIONNARE • Visual analog scale • Verbal rating scale • Initial pain assessment • Numerical rating scale by Mc. Caffery and pasero 8
Visual analogue scale (VAS) • A horizontal or vertical line for the patient to rate current pain level. • Patient can communicate by pointing • Simple, easy to use • Needs to understand concept of rating pain. • Dependent on patient's prior pain experiences 9
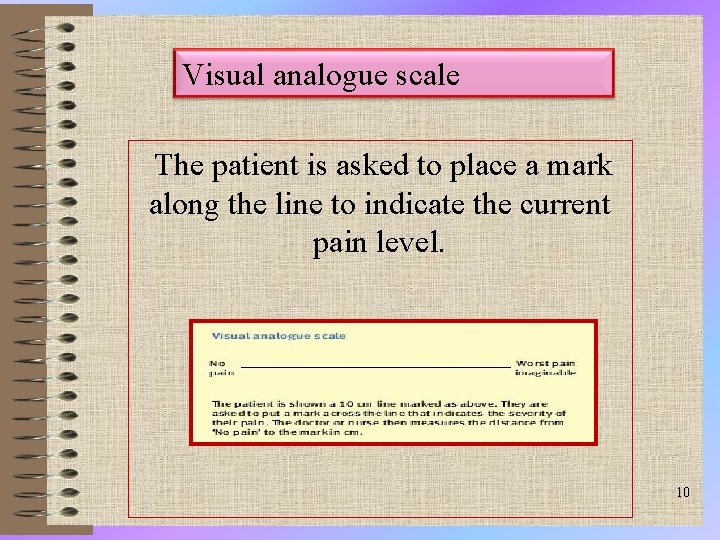
Visual analogue scale The patient is asked to place a mark along the line to indicate the current pain level. 10
Advantage of Visual analogue scale • Simple • quick to administer • and may be used before, during, and following treatment. • The scales may also be completed throughout the course of a day to assess change in pain intensity relative to activity or time of day. 11
limitation of visual analog scale • Difficultly with administration in patient who has perceptual-motor problems. • The major disadvantage of VAS is the assumption that pain is a unidimensional experience. 12
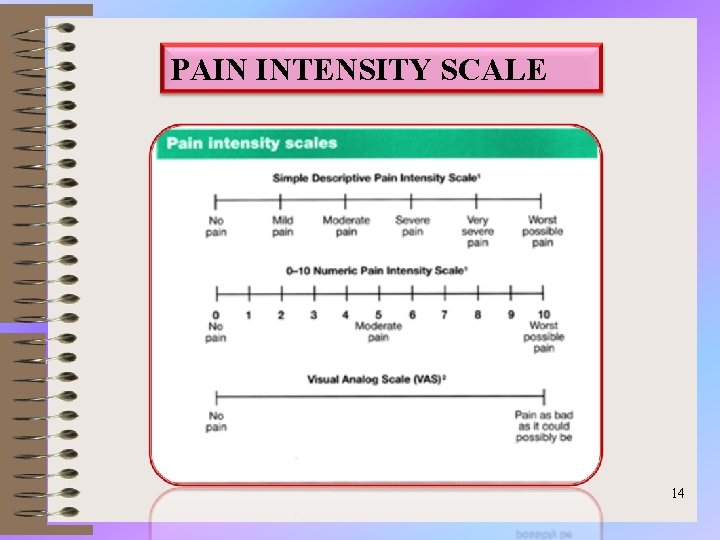
Verbal and Numeric Rating Scale • Verbal rating scales numeric rating scales 13
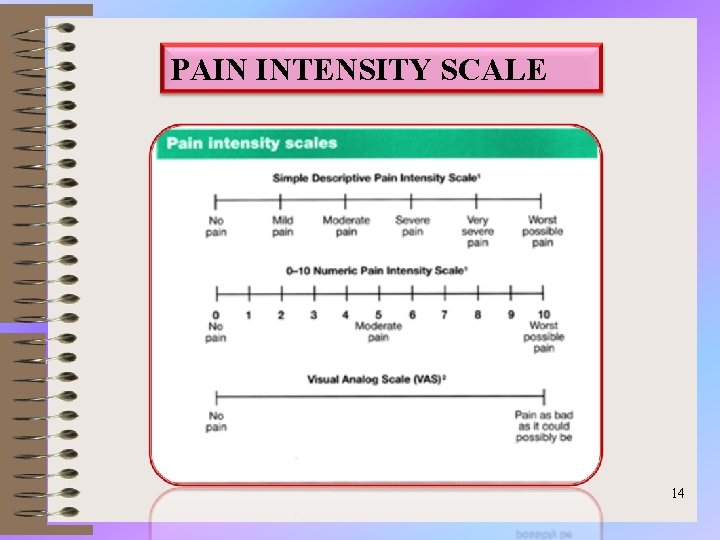
PAIN INTENSITY SCALE 14
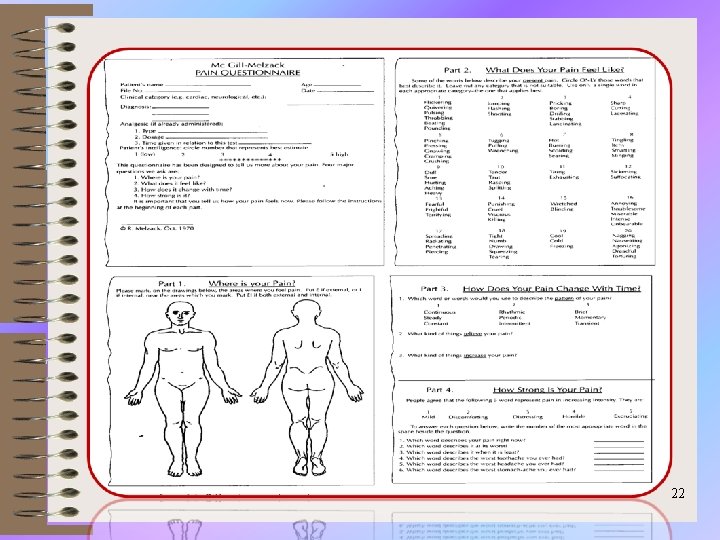
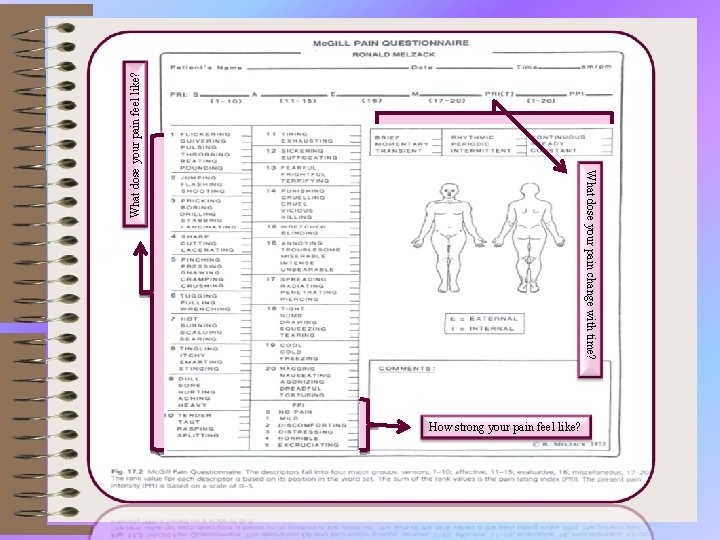
Mc. Gill Pain Questionnaire (MPQ) • The Mc. Gill Pain Questionnaire, developed by Melzack (1975), was the first proper multidimensional self-report pain measuring instrument and is still the most widely used today. 15
Mc. Gill Pain Questionnaire (MPQ) • sensory: what the pain feels like physically where it is located, how intense it is, its duration and its quality (for example, burning, ‘throbbing). • affective: what the pain feels like emotionally —whether it is frightening, worrying and so on. • evaluative: what the subjective overall intensity of the pain experience is (for example, unbearable, distressing). 16
Mc. Gill Pain Questionnaire (MPQ) • Each of the three main classes was divided into a number of sub-classes (sixteen in total). 17
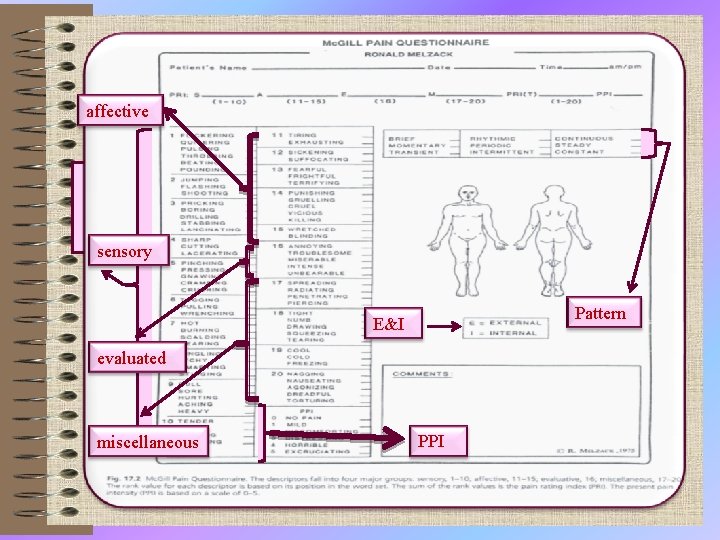
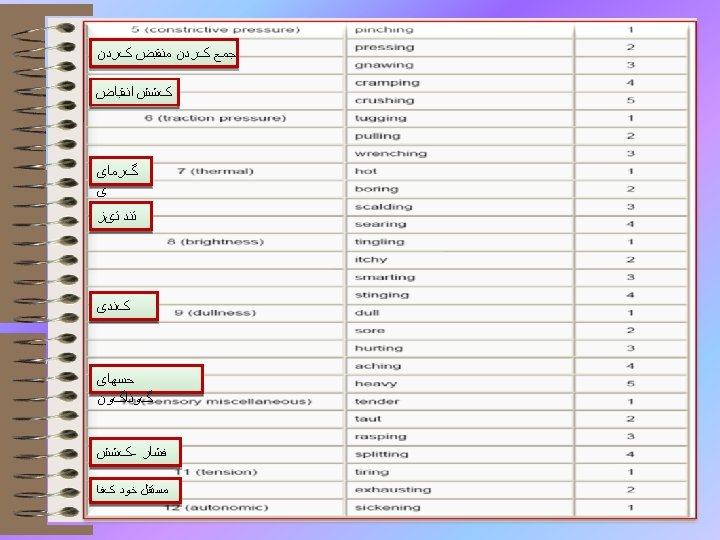
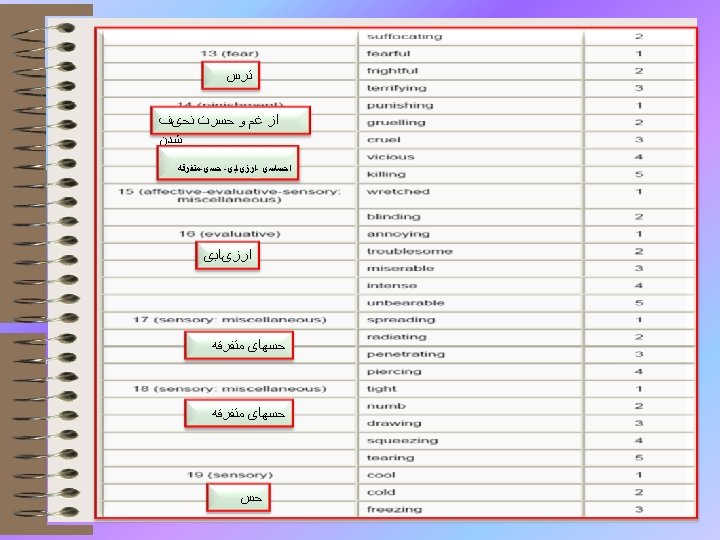
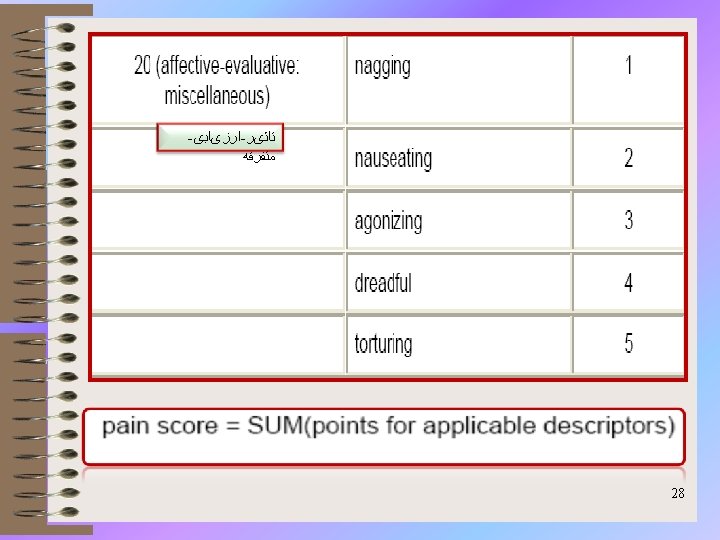
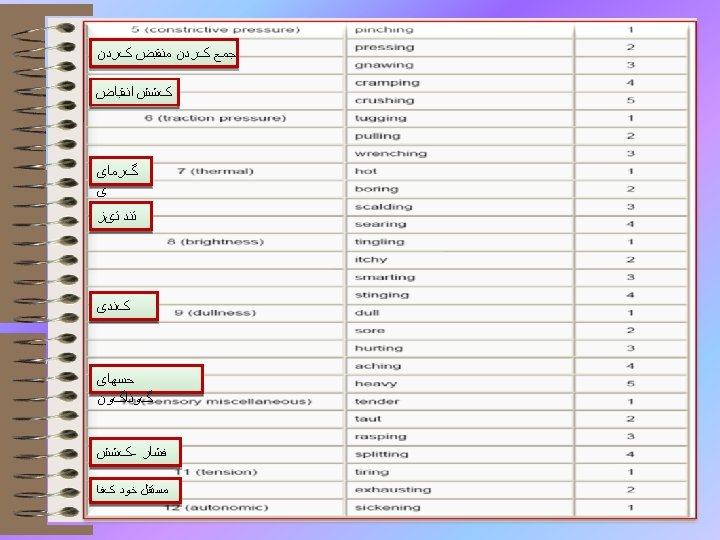
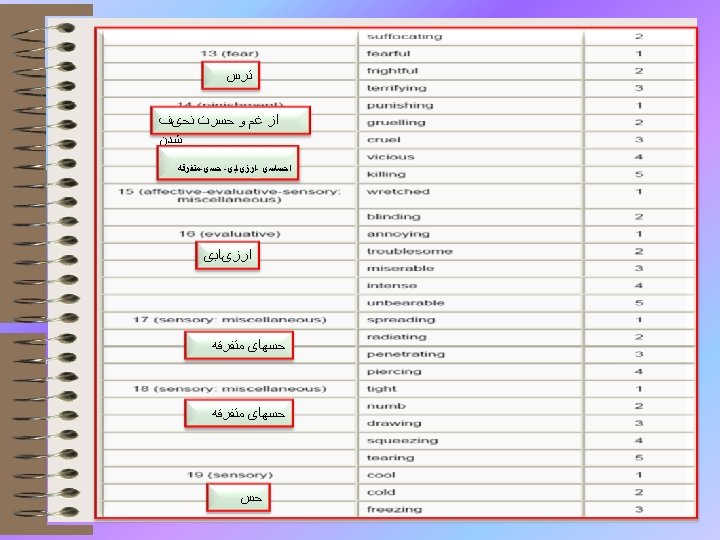
Mc. Gill Pain Questionnaire (MPQ) • Melzack and Torgerson (1971) then asked a sample of doctors, patients and students to rate the words in each sub-class for intensity. The first 20 questions on the Mc. Gill Pain Questionnaire consist of adjectives set out within their sub-classes, in order of intensity. Questions 1 to 10 are sensory, 11 to 15 affective, 16 is evaluative and 17 to 20 are miscellaneous. 18
Mc. Gill Pain Questionnaire (MPQ) • • codes E for pain on the surface of the body codes I for internal pain Codes and EI for both external and internal) indicate present pain intensity (PPI) on a 6 -point verbal rating scale. • Finally, patients complete a set of three verbal rating scales describing the pattern of the pain. 19
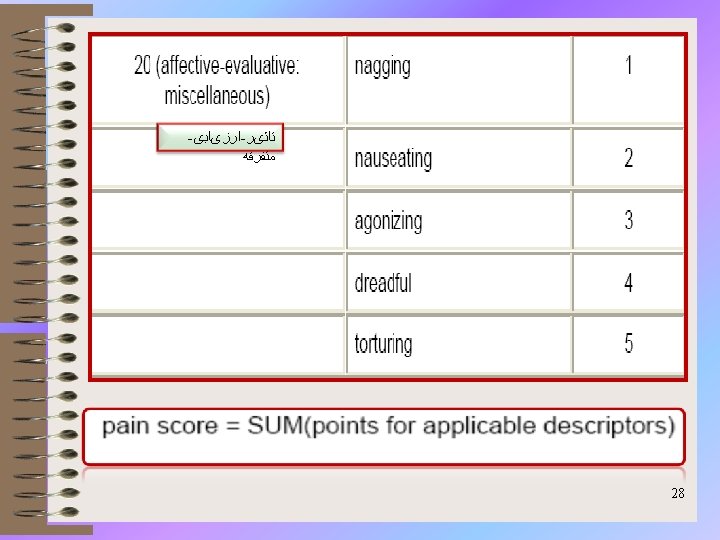
Mc. Gill Pain Questionnaire (MPQ) • Scores are given for the different classes (sensory, affective, evaluative and miscellaneous), and also a total score for all the sub-classes. • Based on this, a pain rating index (PRI) is calculated 20
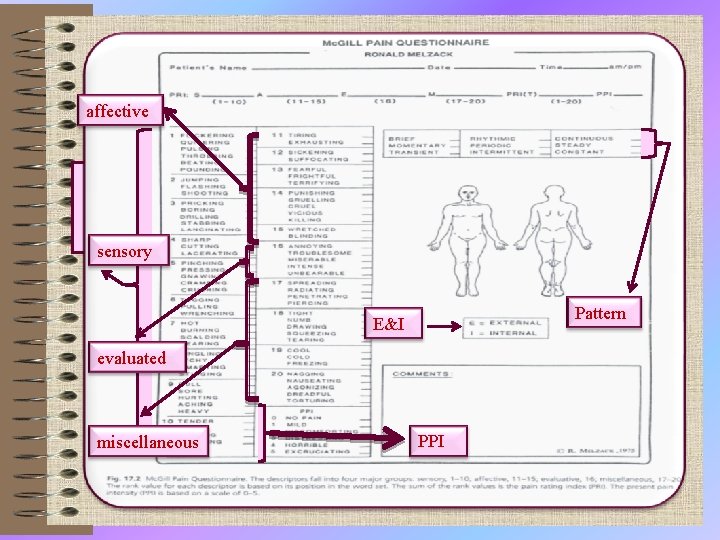
affective sensory Pattern E&I evaluated miscellaneous PPI
22
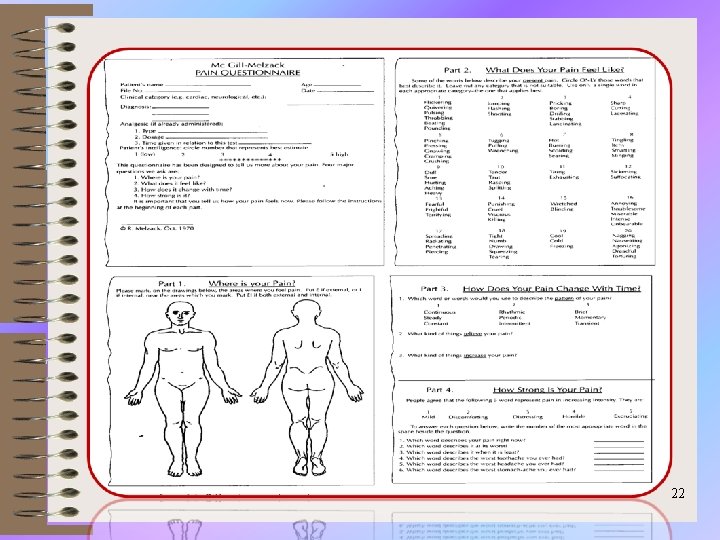
Sections: • (1) What Does Your Pain Feel Like? • (2) How Does Your Pain Change with Time? • (3) How Strong is Your Pain? 23
What Does Your Pain Feel Like? Some of the following words below describe your present pain. ü Circle ONLY those words that best describe it. ü Leave out any category that is not suitable. ü Use only a single word in each appropriate category - the one that applies best. 24

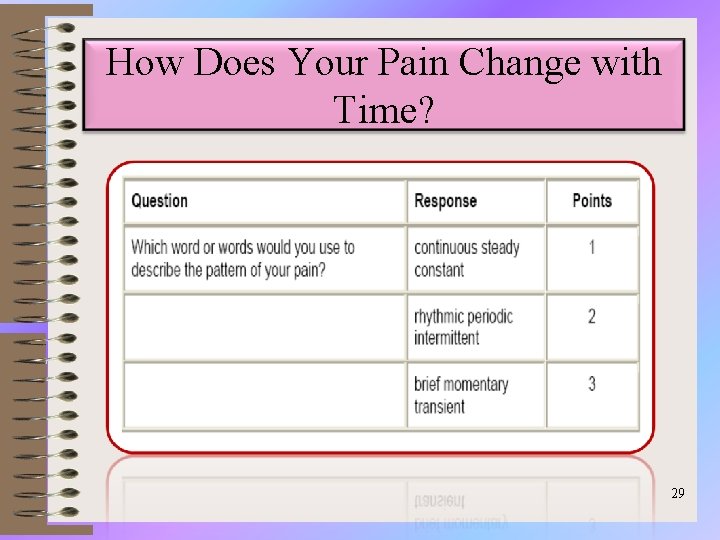
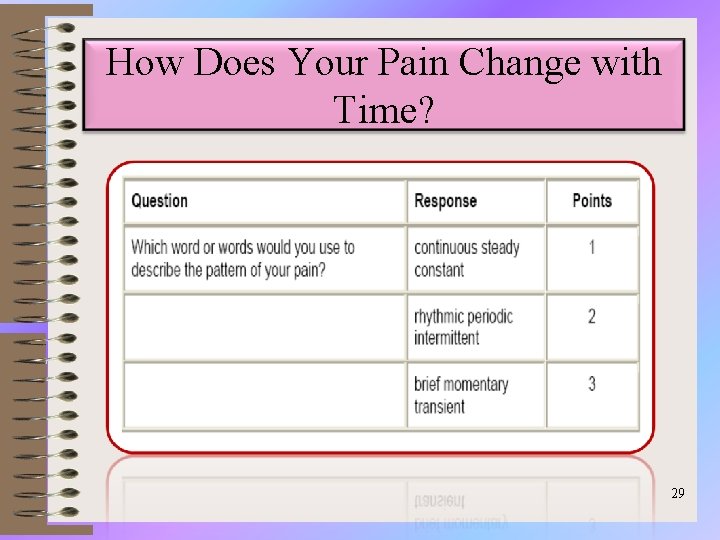
How Does Your Pain Change with Time? 29
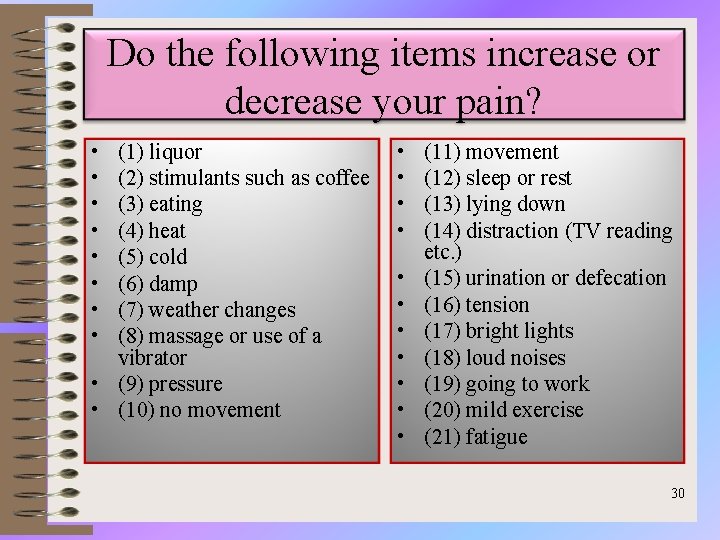
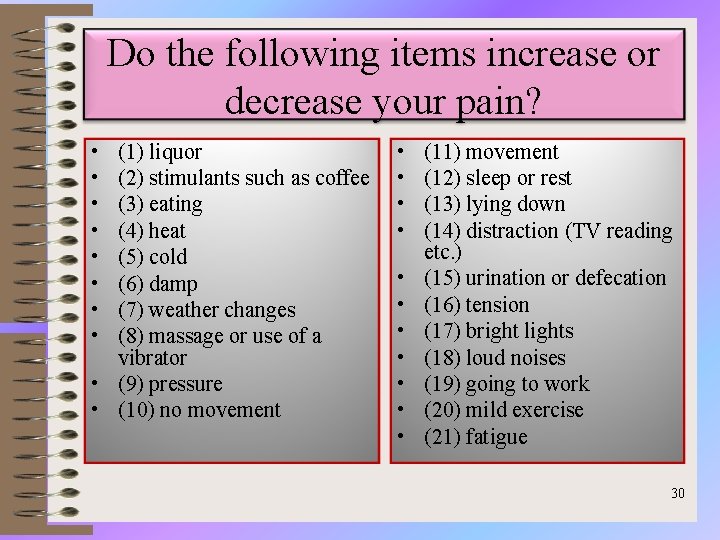
Do the following items increase or decrease your pain? • • (1) liquor (2) stimulants such as coffee (3) eating (4) heat (5) cold (6) damp (7) weather changes (8) massage or use of a vibrator • (9) pressure • (10) no movement • • • (11) movement (12) sleep or rest (13) lying down (14) distraction (TV reading etc. ) (15) urination or defecation (16) tension (17) bright lights (18) loud noises (19) going to work (20) mild exercise (21) fatigue 30
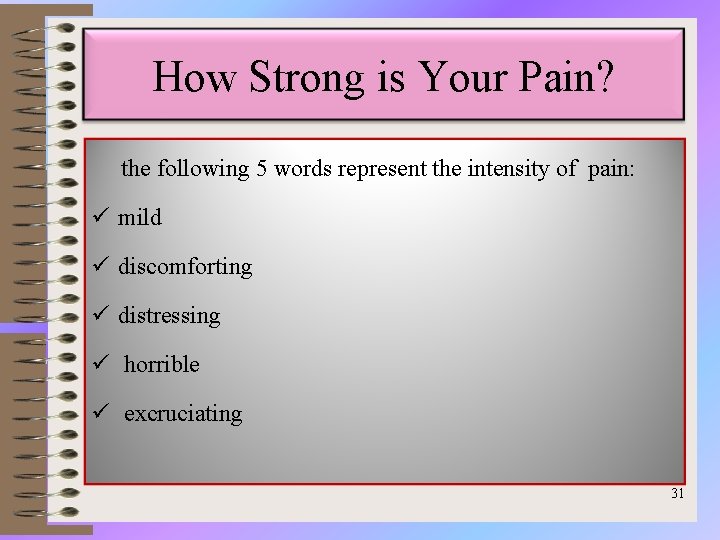
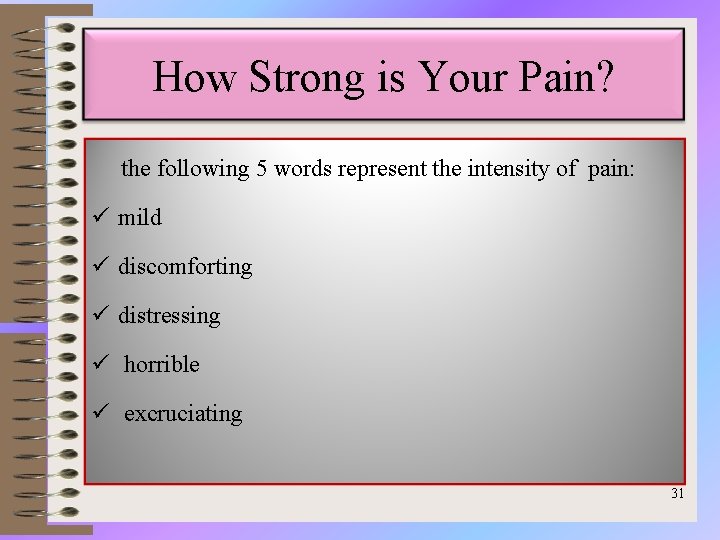
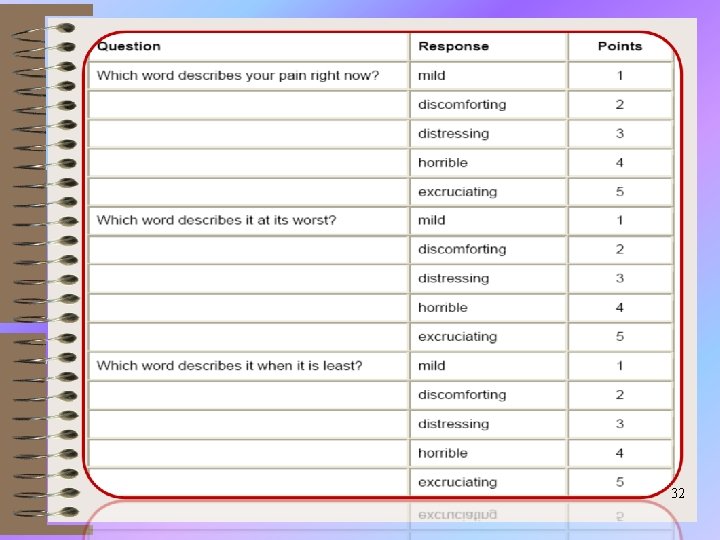
How Strong is Your Pain? the following 5 words represent the intensity of pain: ü mild ü discomforting ü distressing ü horrible ü excruciating 31
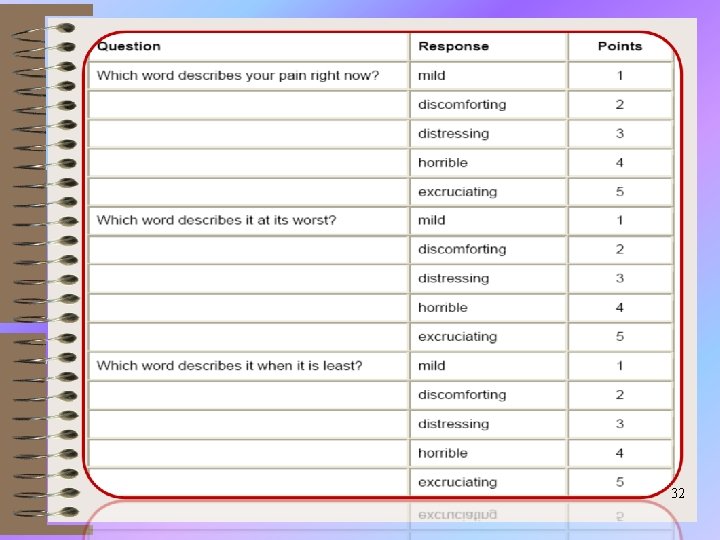
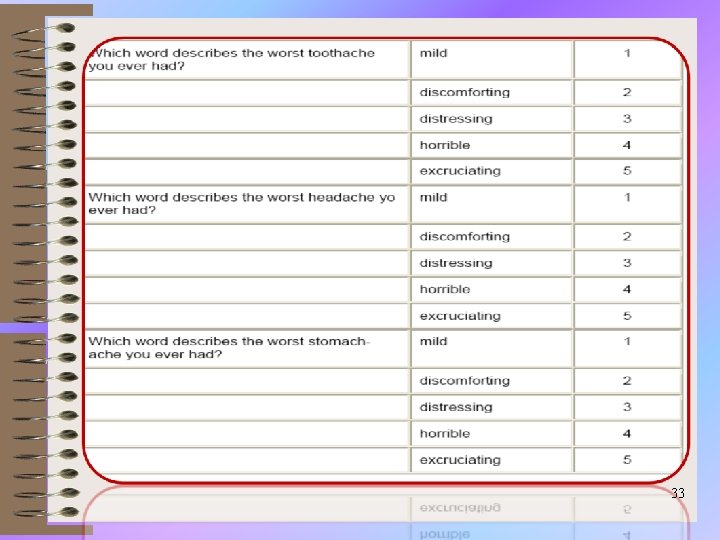
32
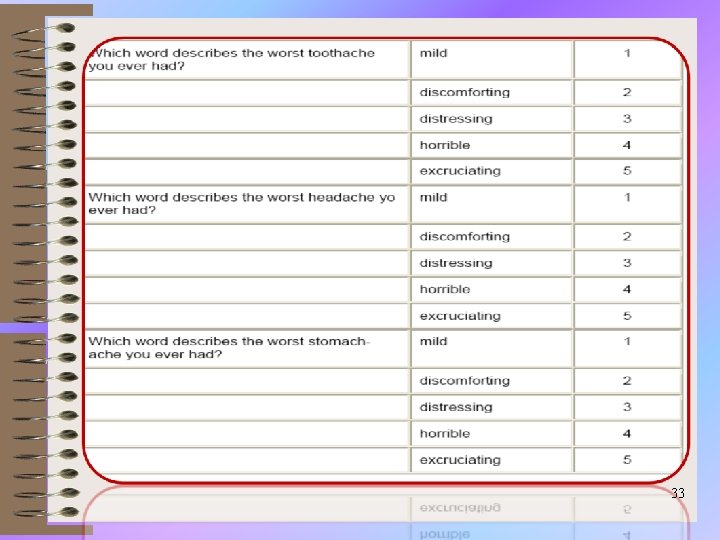
33
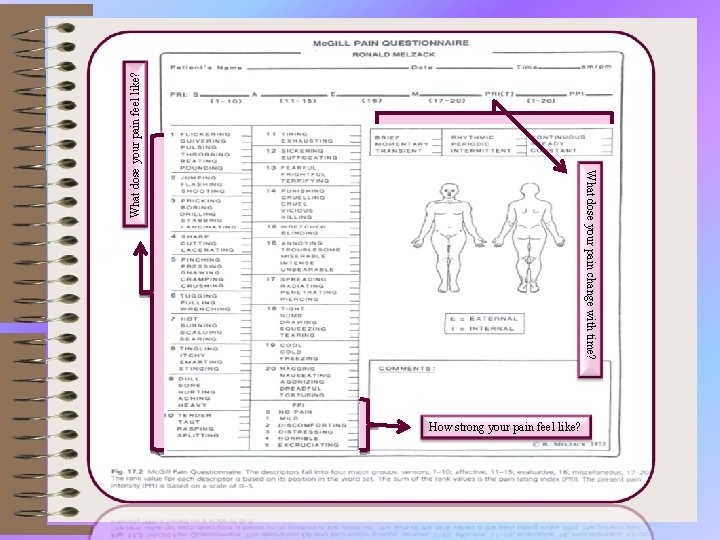
What dose your pain feel like? What dose your pain change with time? How strong your pain feel like?
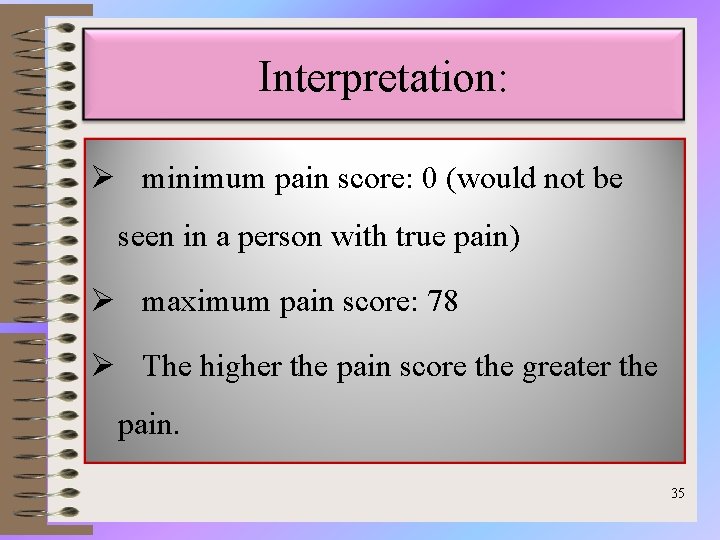
Interpretation: Ø minimum pain score: 0 (would not be seen in a person with true pain) Ø maximum pain score: 78 Ø The higher the pain score the greater the pain. 35
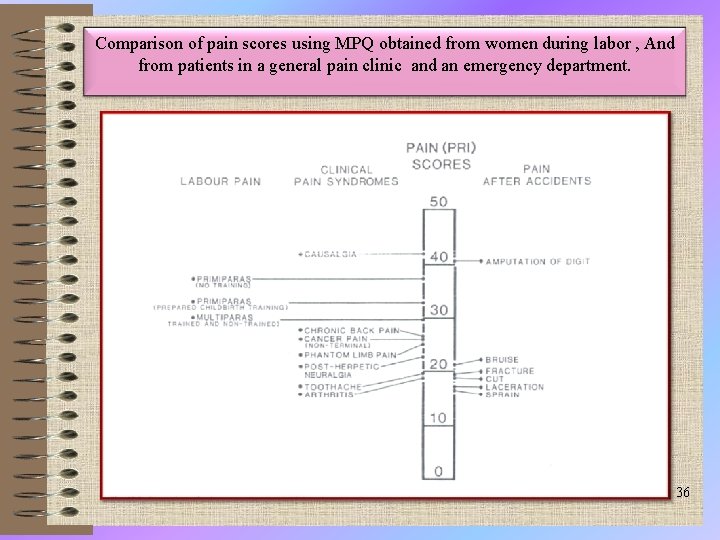
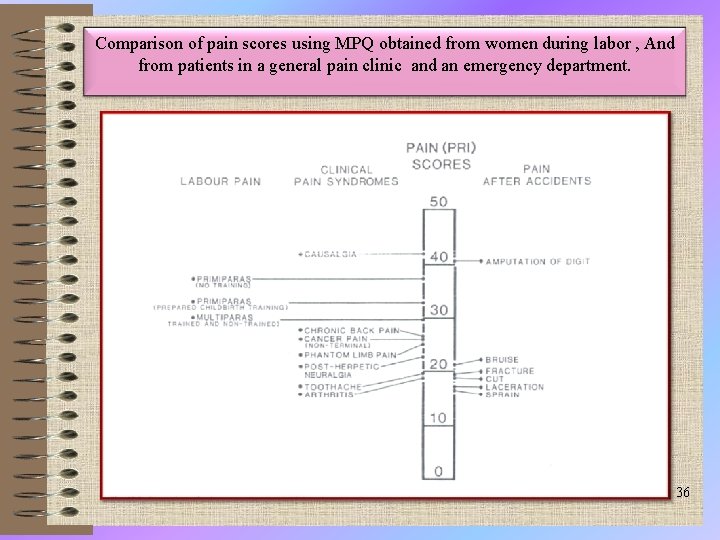
Comparison of pain scores using MPQ obtained from women during labor , And from patients in a general pain clinic and an emergency department. 36
Criticisms ü the need to have extensive understanding of the English language. ü Need to time consuming ü sufficient attention span ü normal cognitive state. 37
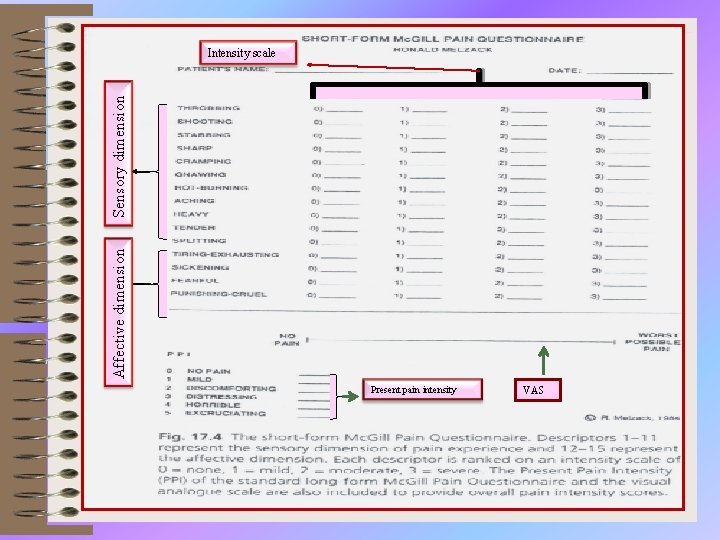
Mc. Gill short pain questionnaire • Measures quality of pain • Uses 15 descriptor words to measure sensory and affective dimension of pain. • Can be used in conjunction with a pain intensity scale Gives more information about the patient's pain. 38
THE SHORT-FORM Mc. Gill PAIN QUESTIONNAIRE When it use? . ü when the time to obtain information from patients is limited ü when more information is desired than that provided by intensity measures such as the VAS or NRS. 39
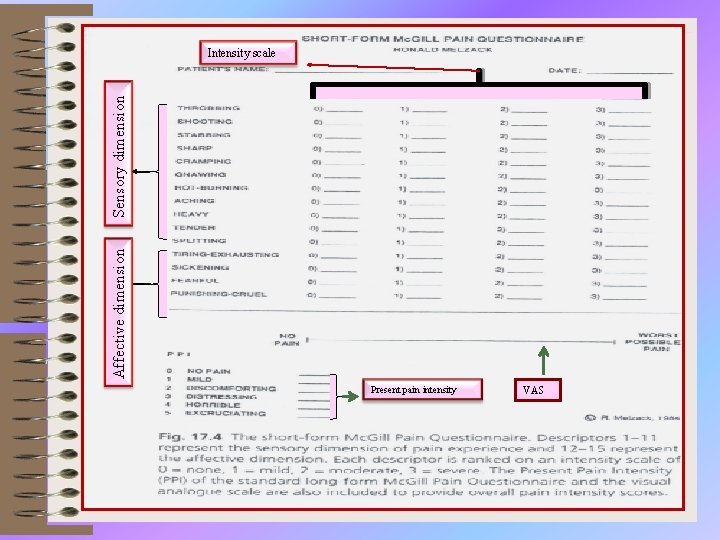
Affective dimension Sensory dimension Intensity scale Present pain intensity VAS
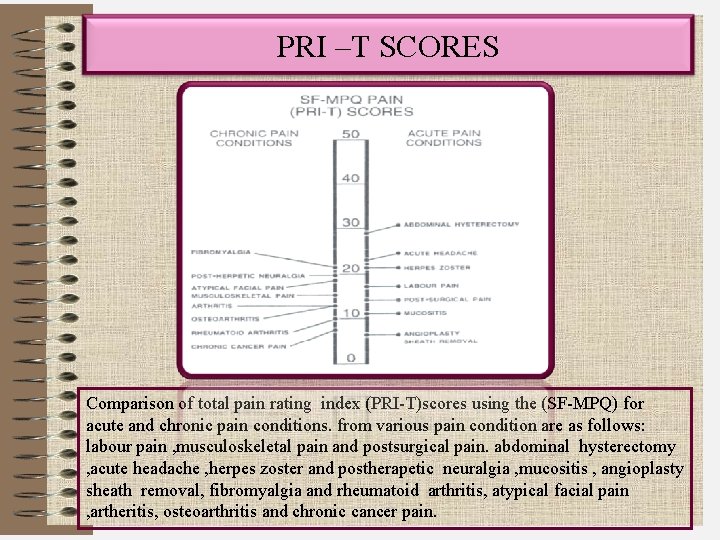
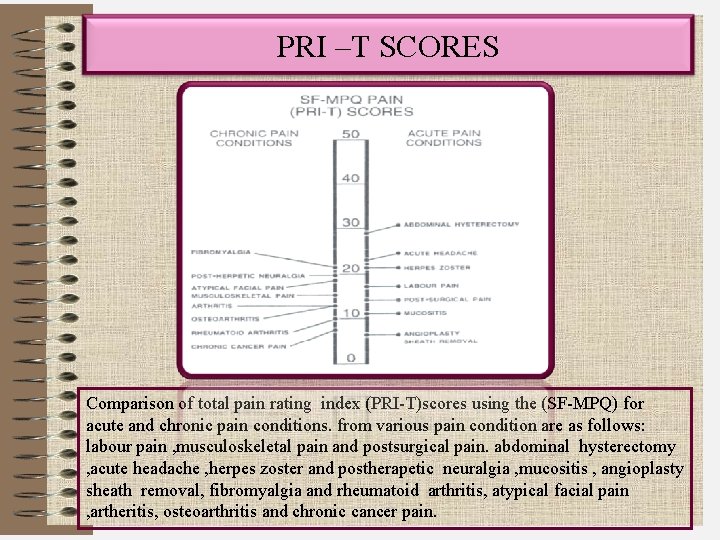
PRI –T SCORES Comparison of total pain rating index (PRI-T)scores using the (SF-MPQ) for acute and chronic pain conditions. from various pain condition are as follows: labour pain , musculoskeletal pain and postsurgical pain. abdominal hysterectomy , acute headache , herpes zoster and postherapetic neuralgia , mucositis , angioplasty sheath removal, fibromyalgia and rheumatoid arthritis, atypical facial pain , artheritis, osteoarthritis and chronic cancer pain.
PAIN ASSESSMENT in less responsive or unconscious With patients who are less responsive or unconscious the nurse must look to additional pain indicators. 42
üAltered body movements showing restlessness ü vocalizations (e. g. 'moaning and groaning) üand facial expressions (grimacing or clenched teeth) 43
Changes in physiological parameters ? ü The Changes occur in physiological parameters, including cardiovascular (elevated blood pressure and heart rate)and respiratory but are not always accurate due to the underlying or drug therapy, and should be used with other forms of assessment. 44
Factors contributing to pain and discomfort in the critically ill Physical Psychosocial Intensive Care Unit Environment or Routine Procedural 45
Factors contributing to pain and discomfort in the critically ill physical factor ü Wounds-post-trauma, postoperative, or post procedural ü Sleep disturbance and deprivation ü Immobility, inability to move to a comfortable position because of tubes, monitors, restraints 46
Factors contributing to pain and discomfort in the critically ill Psychosocial ü Anxiety and depression ü Impaired communication, inability to report and describe pain. üFear of pain, disability, or death üSeparation from family ü lack of pleasant distractions 47 47
Factors contributing to pain and discomfort in the critically ill Intensive Care Unit Environment Continuous noise from equipment and staff Continuous or unnatural patterns of light Awakening and physical manipulation every 1 -2 h for vital signs or positioning Continuous or frequent invasive, painful procedures Competing priorities in care: unstable vital signs, bleeding, dysrhythmias, poor ventilation-may take Precedence over pain management. 48
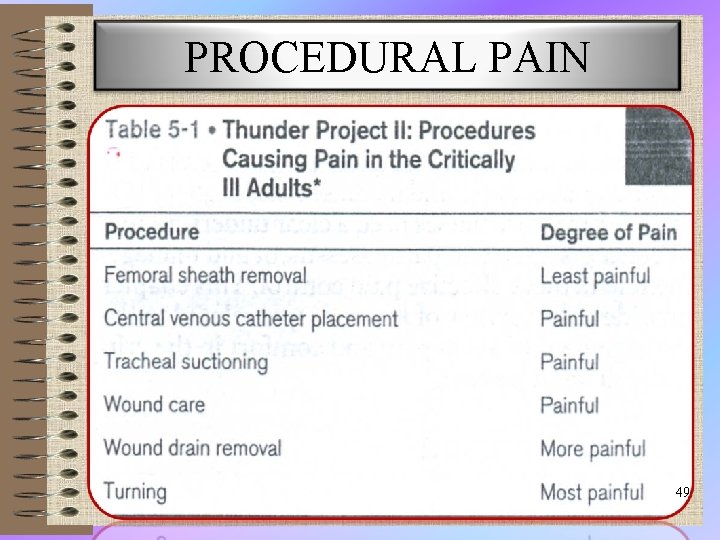
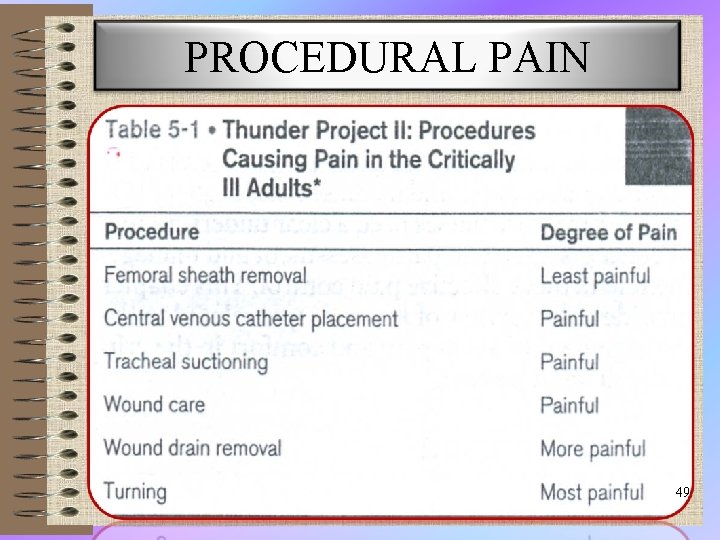
PROCEDURAL PAIN 49
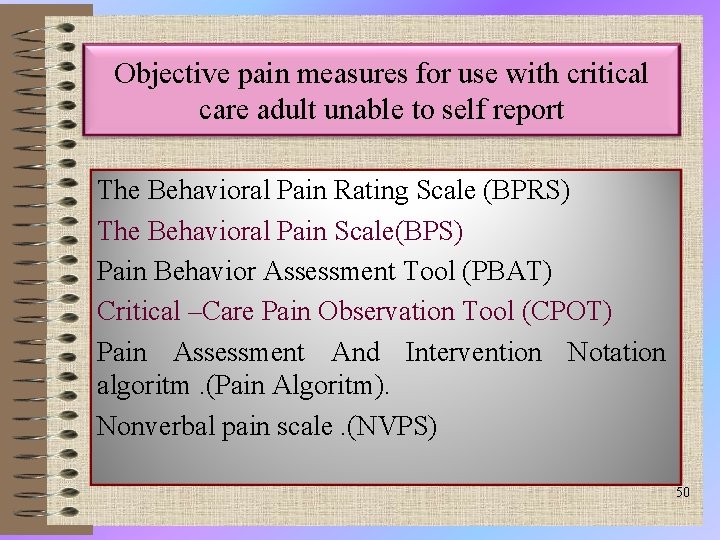
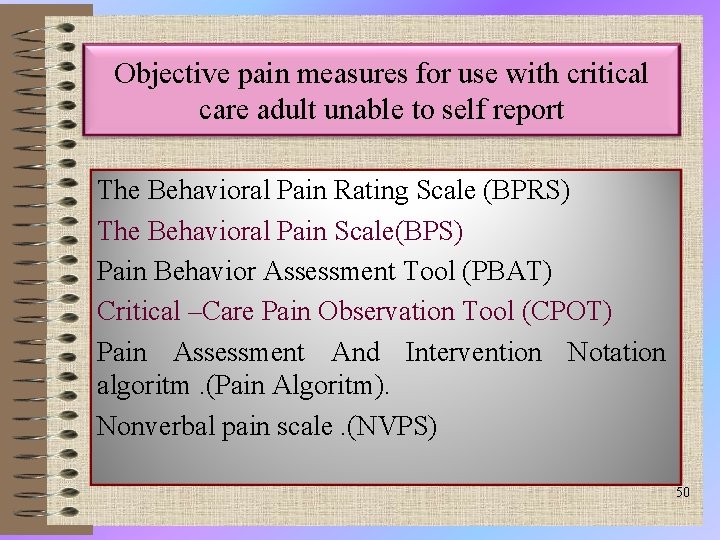
Objective pain measures for use with critical care adult unable to self report The Behavioral Pain Rating Scale (BPRS) The Behavioral Pain Scale(BPS) Pain Behavior Assessment Tool (PBAT) Critical –Care Pain Observation Tool (CPOT) Pain Assessment And Intervention Notation algoritm. (Pain Algoritm). Nonverbal pain scale. (NVPS) 50
Objective pain measures for use with critical care adult unable to self report Ø Research on the measurement of pain in critically ill adults who cannot self-report (referred to as nonverbal ICU patients) has emerged only within the past 2 decades. However , no measure of pain in nonverbal ICU patients is accepted as the “gold standard. ” 51
Abstract: Abstract • Critically ill patients experience significant levels of pain and discomfort from multiple intrinsic and extrinsic sources while in the intensive care unit (ICU). • The use of objective pain measures in nonverbal patients is an essential alternative approach for pain assessment when self-reports are unavailable. • This paper provides a critical review of the psychometric properties of 6 objective pain measures that were developed to assess pain in nonverbal adult patients in the ICU. 52
Although 2 of the 6 objective pain measures showed good evidence of validity and reliability, none has undergone vigorous validation or has been accepted as a standardized measure. 53

American Pain Foundation www. painfoundation. org or 1 -888 -615 -PAIN Alliance of State Pain Initiatives www. aspi. wisc. edu or 1 -608 -265 -4013 Maryland Pain Initiative: www. marylandpaininitiative. org or 1 -410 -783 -0199 (voicemail) American Pain Society www. ampainsoc. org or 1 -847 -375 -4715 American Society for Pain Management Nursing www. ASPMN. org or 1 -888 -342 -7766 American Chronic Pain Association www. theacpa. org or 1 -800 -533 -3231 55
Reference Text Book Of Pain Ronaid Melzack &Patrick D. Wall Critical Care Nursing Thelans 2008 Black &Hawks 2005 Pain Management 2006 Black Well 56

Thank you for your attention 11/22/2020
 Martian pain
Martian pain Can you feel like your period is coming and be pregnant
Can you feel like your period is coming and be pregnant Is pregnancy pain same as period pain
Is pregnancy pain same as period pain Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worms-breton
Tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V. c c
V. c c Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số nguyên là gì
Số nguyên là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Pqrst pain assessment
Pqrst pain assessment Pain school international
Pain school international Pqrstu pain
Pqrstu pain Capa pain assessment tool
Capa pain assessment tool Unpleasant sensory and emotional experience
Unpleasant sensory and emotional experience Pain scale 1-10 examples
Pain scale 1-10 examples Comprehensive pain assessment
Comprehensive pain assessment Comprehensive pain assessment
Comprehensive pain assessment Pqrst pain scale
Pqrst pain scale What is pain
What is pain Jarvis chapter 11 pain assessment
Jarvis chapter 11 pain assessment Chapter 3 the external assessment
Chapter 3 the external assessment Principles of portfolio assessment
Principles of portfolio assessment