Chapter 43 Pain Management NRS105320Collings Importance Pain management

![Physiological Response to Pain • Mild – moderate pain [1 -6] superficial → autonomic Physiological Response to Pain • Mild – moderate pain [1 -6] superficial → autonomic](https://slidetodoc.com/presentation_image/bf05f3b3fb19efe6935f945671c381a3/image-8.jpg)
![Types of Pain • Chronic pain – Serves no purpose [not protective] – Lasts Types of Pain • Chronic pain – Serves no purpose [not protective] – Lasts](https://slidetodoc.com/presentation_image/bf05f3b3fb19efe6935f945671c381a3/image-11.jpg)
![Factors Influencing Pain • Psychological – Anxiety – Coping style • Control [PCA] • Factors Influencing Pain • Psychological – Anxiety – Coping style • Control [PCA] •](https://slidetodoc.com/presentation_image/bf05f3b3fb19efe6935f945671c381a3/image-17.jpg)



![Implementation Pain Management • Barriers to effective pain management [pts, nurses, doctors, system…] – Implementation Pain Management • Barriers to effective pain management [pts, nurses, doctors, system…] –](https://slidetodoc.com/presentation_image/bf05f3b3fb19efe6935f945671c381a3/image-28.jpg)

- Slides: 32
Chapter 43 Pain Management NRS_105/320_Collings
Importance • Pain management is a primary nursing responsibility • Nurse have a legal and ethical duty to control/relieve pain • Pain relief is a basic human right • Patients need to know we CAN and WILL relieve their pain NRS_105/320_Collings
Why? • Effective pain management: – Improves quality of life – Reduces disability – Promotes early mobility and return to work – Results in less hospital / office visits – Reduces length of stay, complications – Reduces health care cost – Improves patient satisfaction NRS_105/320_Collings

Nature of Pain • • Physical Emotional Cognitive Subjective NRS_105/320_Collings
Physiology of Pain • Transduction • Thermal, chemical, mechanical stimulation • → electrical impulse in nerve fiber • Transmission • A fibers: sharp, localized, distinct sensation • C fibers: generalized, persistent sensation – E. g. Burn finger – spot pain → ache • Peripheral → spinal → brain NRS_105/320_Collings
Physiology of Pain • Perception – Brain interprets impulse, perceives as pain – Experience, memory, context, knowledge – Ascribes meaning to sensation • Modulation – Body response • Endogenous opiods, serotonin, norepinephrine, GABA • ↓ transmission of impulse, analgesic effect – These deplete over time with continued pain NRS_105/320_Collings
Gate-Control Theory of Pain • Gating mechanisms along the CNS – Can block transmission of impulses • Pain relief measures to close the gate – Light touch [effleurage] • Pain threshold – Level at which you feel pain • Genetic, learned, • Runner’s high, endogenous opiods • Individual – not transferrable! NRS_105/320_Collings
![Physiological Response to Pain Mild moderate pain 1 6 superficial autonomic Physiological Response to Pain • Mild – moderate pain [1 -6] superficial → autonomic](https://slidetodoc.com/presentation_image/bf05f3b3fb19efe6935f945671c381a3/image-8.jpg)
Physiological Response to Pain • Mild – moderate pain [1 -6] superficial → autonomic response [sympathetic]; • fight or flight, general adaptation • ↑HR, RR, B/P, BG, diaphoresis, peripheral vasoconstriction • Severe or deep [7 -10], visceral pain → parasympathetic response • ↓ HR, B/P, muscle tension, immobility, irreg resp • may cause harm – Physiologic response [VS] is short-term; – VS are not reliable pain indicators over time NRS_105/320_Collings
Behavioral responses to Pain • Dependent on context, meaning, culture, pain tolerance – It is supposed to hurt – Men don’t cry – I don’t want to be a complainer, bother • Nonverbal indicators – Body movements; restless or still, holding, guarding – Facial expression; grimace, frown, clenched teeth, posture, • Lack of expression of pain does not mean it isn’t there! NRS_105/320_Collings
Types of Pain • Acute pain – Protective, identifiable cause, short duration, limited tissue damage, ↓ emotional response – Causes harm by ↓ mobility, energy Goal is to control pain so patient can participate in recovery ↓ Pain → ↑Mobility → decreased complications, decreased length of stay NRS_105/320_Collings
![Types of Pain Chronic pain Serves no purpose not protective Lasts Types of Pain • Chronic pain – Serves no purpose [not protective] – Lasts](https://slidetodoc.com/presentation_image/bf05f3b3fb19efe6935f945671c381a3/image-11.jpg)
Types of Pain • Chronic pain – Serves no purpose [not protective] – Lasts longer than anticipated – May or may not have an identifiable cause – Impacts every part of patient’s life – Depression, Suicide – Disability, isolation, energy drain, ADL’s • Pseudoaddiction: seeking pain relief – not drug-seeking NRS_105/320_Collings
Types of Pain • Cancer pain – May be acute or chronic, constant or episodic, mild to severe – Up to 90% of Ca pts have pain • Pain by inferred pathology – Known cause = characteristic pain [neuropathic] • Idiopathic pain – No known cause BUT still pain – “Excessive” pain for a condition NRS_105/320_Collings
Knowledge, Attitudes, and Beliefs • Subjective nature of pain – Pain is what the patient says it is, not what the nurse thinks it should be – Same procedure, different pain – Expectations, context, culture affect perception and expression of pain NRS_105/320_Collings
Knowledge, Attitudes, and Beliefs • Nurse’s Response to Pain • Bias – ‘I go to work with 5/10 pain every day’ – ‘Its only a minor surgery’ – ‘I had three kids and didn’t scream’ • Fallacies – Infants don’t feel pain like we do – Regular pain med use causes addiction – Older people all are in pain NRS_105/320_Collings
Factors Influencing Pain • Physiological – Age – interpretation/communication – Fatigue • increases pain, • sleep not sign pain is relieved – Genes • Pain threshold – Neurological function • Interpretation, communication, reflex NRS_105/320_Collings
Factors Influencing Pain • Social – Attention/ distraction – Previous experience • May increase or decrease tolerance – Family and social support • Spiritual – Meaning of pain, suffering – Support system NRS_105/320_Collings
![Factors Influencing Pain Psychological Anxiety Coping style Control PCA Factors Influencing Pain • Psychological – Anxiety – Coping style • Control [PCA] •](https://slidetodoc.com/presentation_image/bf05f3b3fb19efe6935f945671c381a3/image-17.jpg)
Factors Influencing Pain • Psychological – Anxiety – Coping style • Control [PCA] • Cultural – – Meaning of pain Expression of pain Role in Family Ethnicity NRS_105/320_Collings
Assessment of Pain • Client’s expression of pain – Description is most valid indicator • Characteristics of pain – Onset and duration – Location – Intensity – Quality – Pattern NRS_105/320_Collings
Assessment of Pain • Characteristics of pain (cont'd) – – Relief measures Contributing symptoms Behavioral effects on the client Influences on ADLs • Client expectations – What pain level would allow you to function well? • [walk the hall, do ADL’s, resume job…] NRS_105/320_Collings
Assessment • Can we do a full assessment of pain when the client is in severe pain? • No! • Alleviate severe [7 -10] pain before talking it to death • Pain rated >7 needs immediate attention NRS_105/320_Collings
Nursing Diagnoses • • Anxiety Ineffective coping Fatigue Acute pain Chronic pain Ineffective role performance Disturbed sleep pattern NRS_105/320_Collings
Planning • Goals and outcomes – Client is using pain relief measures safely – Pain level reported at </=___ and congruent nonverbal behaviors seen – Demonstrate understanding of need to premedicate before activity – Splint abdomen with cough • Setting priorities – What is important for the client? What does he need to do? • Control pain enough to eat, sleep? Be mobile to prevent complications? Work? PT? Maintain dignity, relationships while dying? – Maslow: Pain relief is basic need NRS_105/320_Collings

Implementation: Health Promotion • Client education – Expectations, when to seek treatment – Preparation before pain • Holistic care – Whole self; physical, emotional, spiritual – Education, rest, exercise, nutrition, relationships NRS_105/320_Collings
Nonpharmacological Pain Relief • • Relaxation and guided imagery Distraction Biofeedback Cutaneous stimulation—massage, application of hot/cold, TENS • Herbals • Reducing painful stimuli and perception NRS_105/320_Collings
Controlling Painful Stimuli • Managing the client’s environment— bed, linens, temperature • Positioning • Changing wet clothes and dressings • Monitoring equipment, bandages, hot and cold applications • Preventing urinary retention and constipation NRS_105/320_Collings

Implementation Pain Management • Pharmacological pain relief • … Administer analgesics as ordered/ reassess pain in 30 minutes and hourly – Analgesics: NSAIDs and nonopioids, adjuvants – Patient-controlled analgesia (PCA) – Local analgesic infusion pump – Topical analgesics and anesthetics – Local and regional anesthetics NRS_105/320_Collings

Implementation Pain Management • Surgical interventions • Procedural pain management • Chronic and cancer pain management NRS_105/320_Collings
![Implementation Pain Management Barriers to effective pain management pts nurses doctors system Implementation Pain Management • Barriers to effective pain management [pts, nurses, doctors, system…] –](https://slidetodoc.com/presentation_image/bf05f3b3fb19efe6935f945671c381a3/image-28.jpg)
Implementation Pain Management • Barriers to effective pain management [pts, nurses, doctors, system…] – Fear of addiction - #1 barrier – Terms: • Dependence: physical adaptation resulting in withdrawal symptoms • tolerance: physical adaptation resulting in diminished drug effect over time • Addiction: impaired control over use, use despite harm • pseudoaddiction: drug seeking behavior to relieve undertreated pain NRS_105/320_Collings
Implementation Pain Management • Nursing implications for pain management – Accurate safe medication administration – Assess effectiveness and side effects – Patient education [families too] – Use the appropriate drug when given a choice – Treat pain before it gets severe NRS_105/320_Collings

Implementation: Restorative Care • Pain clinics • Palliative care • Hospices NRS_105/320_Collings
Evaluation • Effectiveness – Assess at peak of drug effect • [30 minutes IV, 1 hour PO] – Add complementary therapies for partial effect – Talk with M. D. about options if approach is consistently ineffective • Side effects • Document and communicate – Most effective relief NRS_105/320_Collings
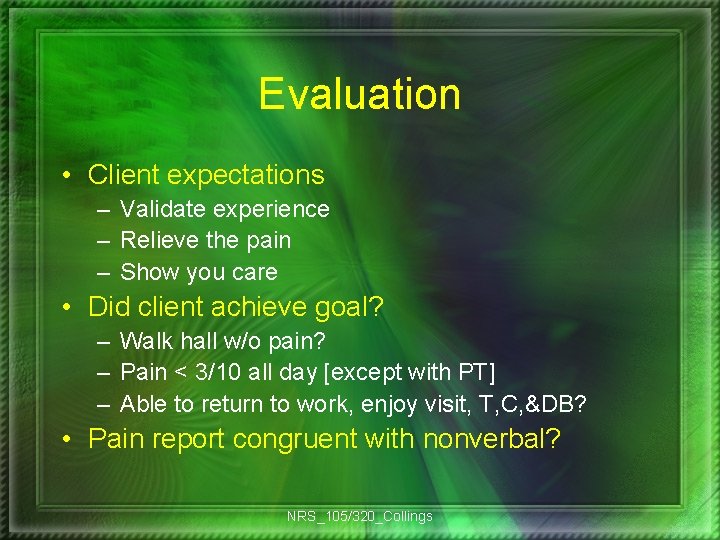
Evaluation • Client expectations – Validate experience – Relieve the pain – Show you care • Did client achieve goal? – Walk hall w/o pain? – Pain < 3/10 all day [except with PT] – Able to return to work, enjoy visit, T, C, &DB? • Pain report congruent with nonverbal? NRS_105/320_Collings
 David lewis mad pain and martian pain
David lewis mad pain and martian pain Can early pregnancy feel like period cramps
Can early pregnancy feel like period cramps Pms vs pregnancy
Pms vs pregnancy Chapter 7 nursing management of pain during labor and birth
Chapter 7 nursing management of pain during labor and birth Chapter 31 pain comfort and sleep
Chapter 31 pain comfort and sleep Jarvis chapter 11 pain assessment
Jarvis chapter 11 pain assessment Pain management okc soonercare
Pain management okc soonercare Pico question
Pico question Stony brook pain management
Stony brook pain management Iu pain management
Iu pain management Dr vallina gastroenterology
Dr vallina gastroenterology Nonpharmacologic pain management nursing
Nonpharmacologic pain management nursing Npass pain scale
Npass pain scale Matrifen
Matrifen Nursing goals for pain
Nursing goals for pain Dr danko pain management
Dr danko pain management Triangle conclusion paragraph
Triangle conclusion paragraph Dr. mehdi pain management
Dr. mehdi pain management Pain management ehr
Pain management ehr Chronic pain management irwin
Chronic pain management irwin Pain res manage
Pain res manage Dr lascarides pain management
Dr lascarides pain management Pain management synonym
Pain management synonym Ch 8 summary lord of the flies
Ch 8 summary lord of the flies Lesson 1 the importance of nutrition
Lesson 1 the importance of nutrition Characteristics of strategic management
Characteristics of strategic management Importance of project scope management
Importance of project scope management Importanceof hrm
Importanceof hrm Manajemen pengadaan proyek perangkat lunak
Manajemen pengadaan proyek perangkat lunak Importance of water sources
Importance of water sources Scope and importance of farm management
Scope and importance of farm management Staffing and directing in management
Staffing and directing in management Importance of project procurement management
Importance of project procurement management