Pain Assessment and Management in Palliative are Pain
- Slides: 36
Pain Assessment and Management in Palliative are ��. ������������������������
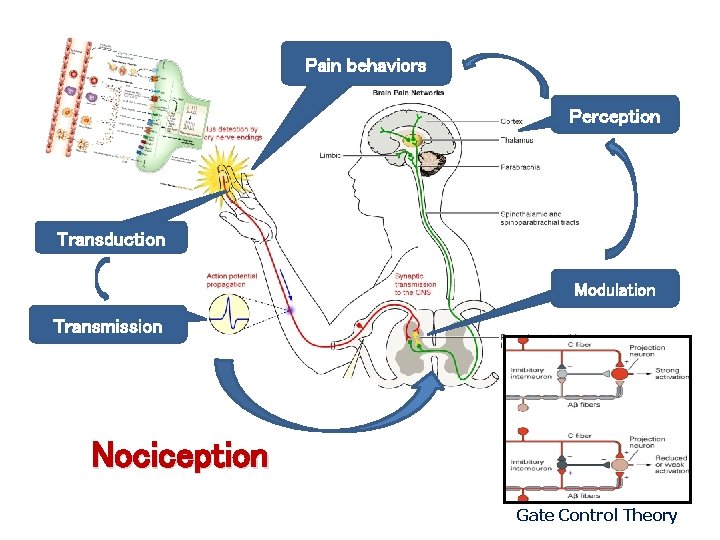
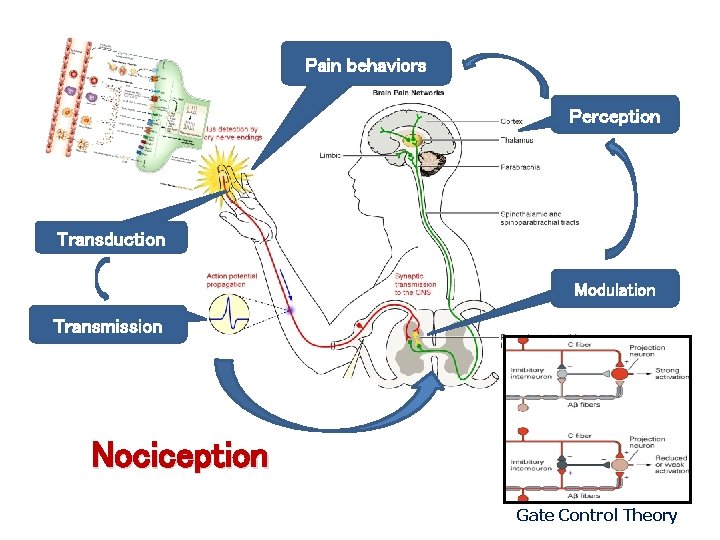
Pain behaviors Perception Transduction Modulation Transmission Nociception Gate Control Theory
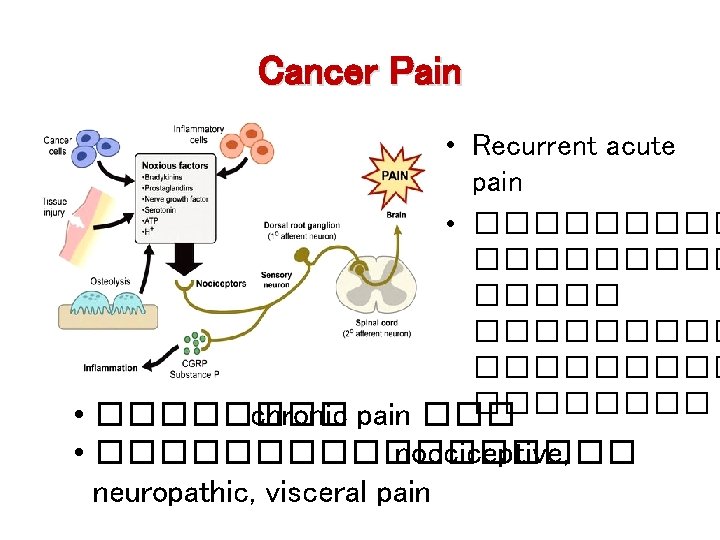
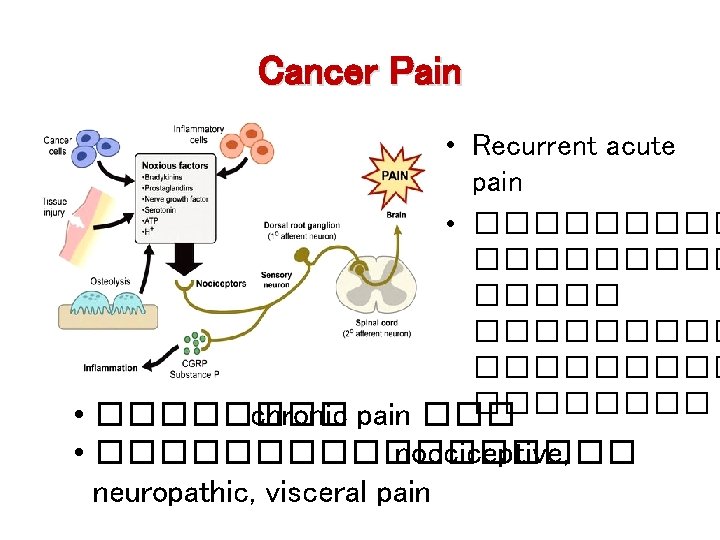
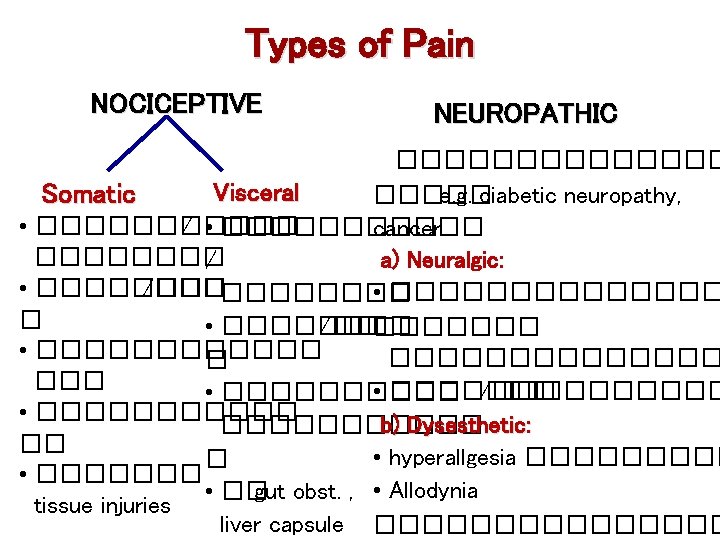
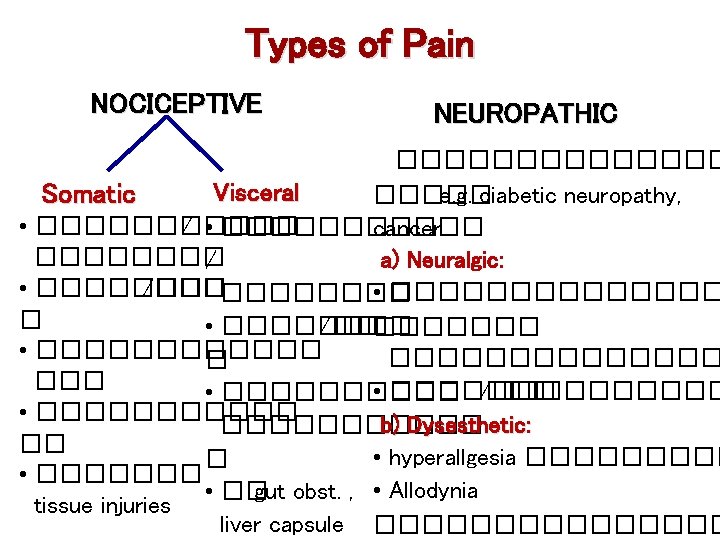
Cancer Pain • Recurrent acute pain • ��������� �������� • ���� chronic pain ��� • ��������� nocciceptive, neuropathic, visceral pain
�������� Pain is what a person says “ it hurts”.
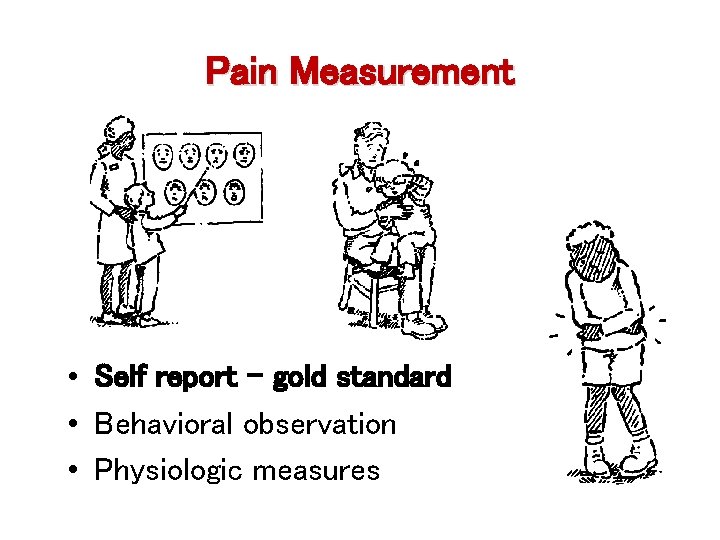
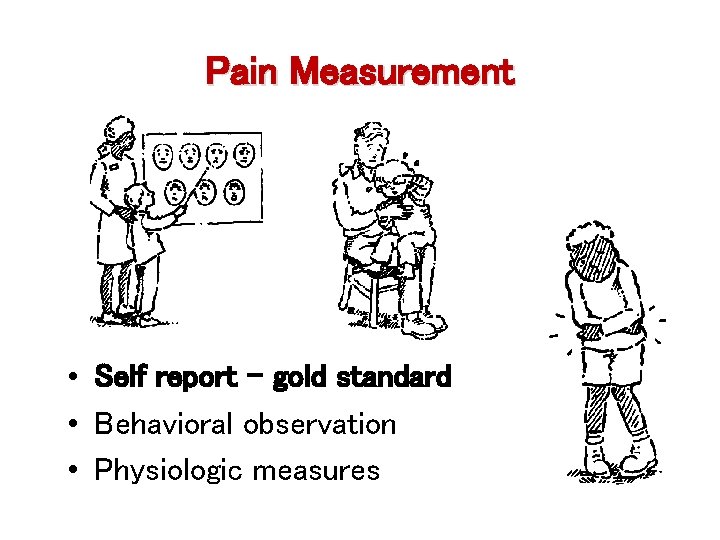
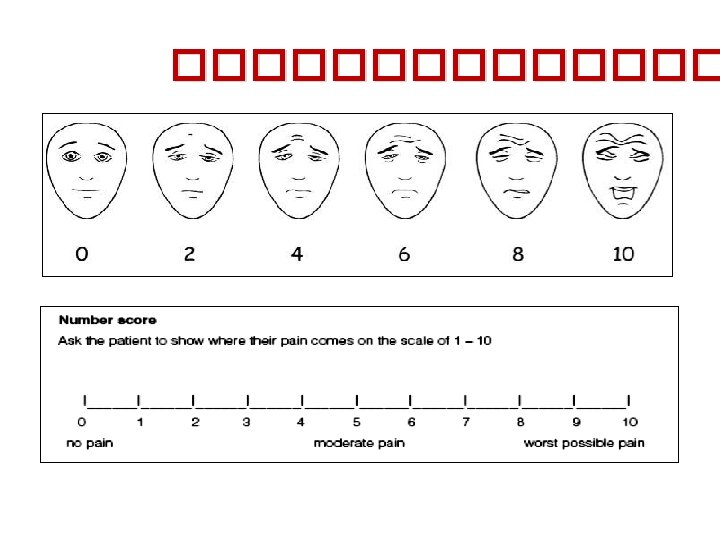
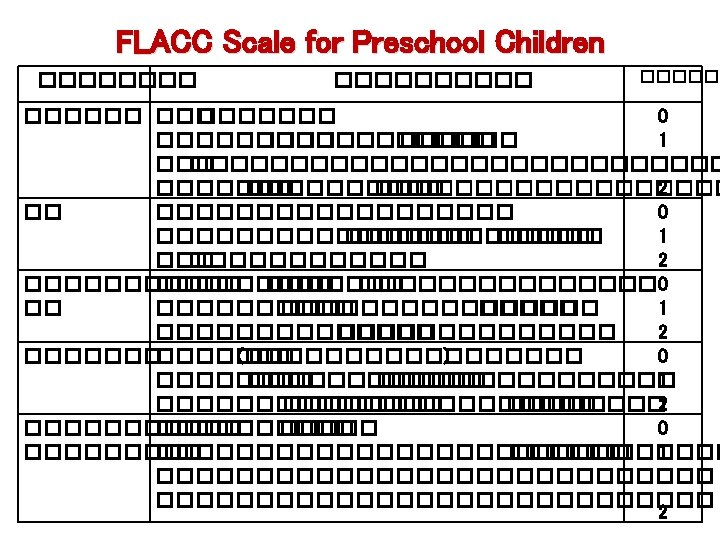
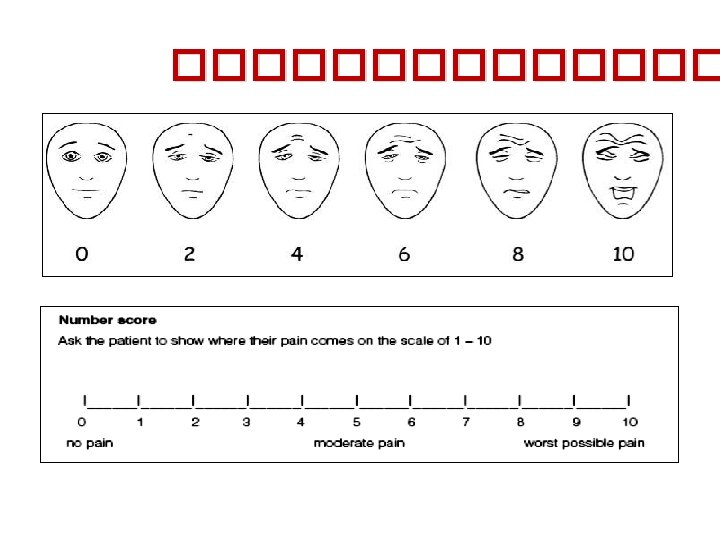
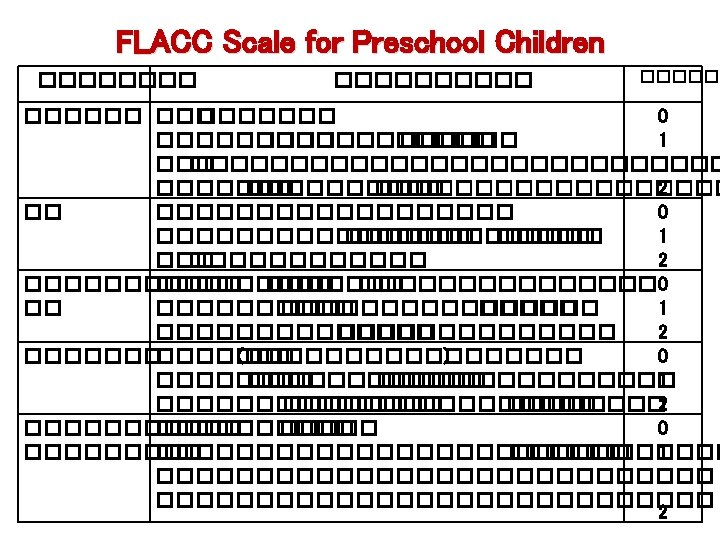
Pain Measurement • Self report – gold standard • Behavioral observation • Physiologic measures
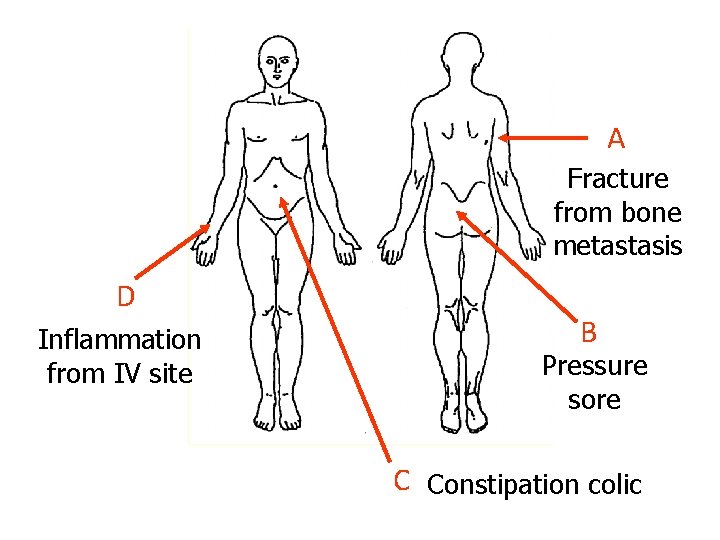
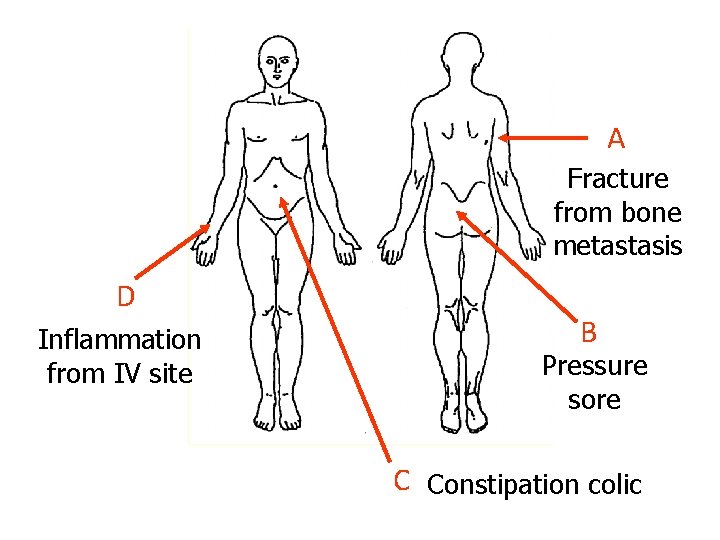
A Fracture from bone metastasis D Inflammation from IV site B Pressure sore C Constipation colic
Management of Chronic Pain • By the clock • By the mouth • By the patient
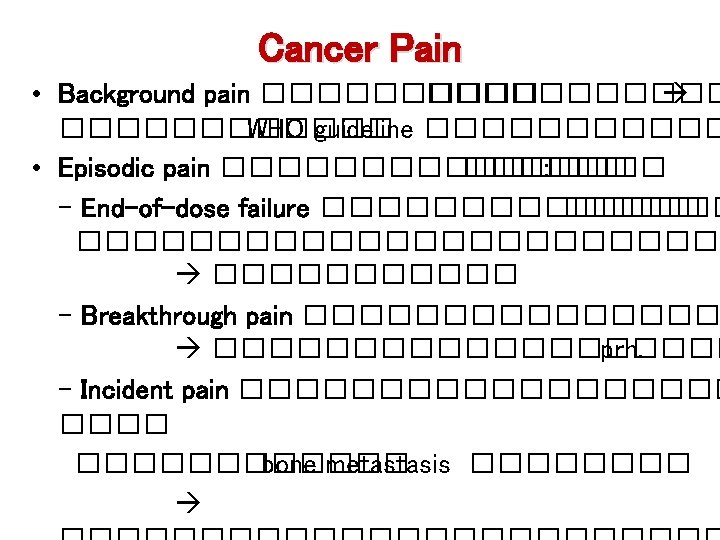
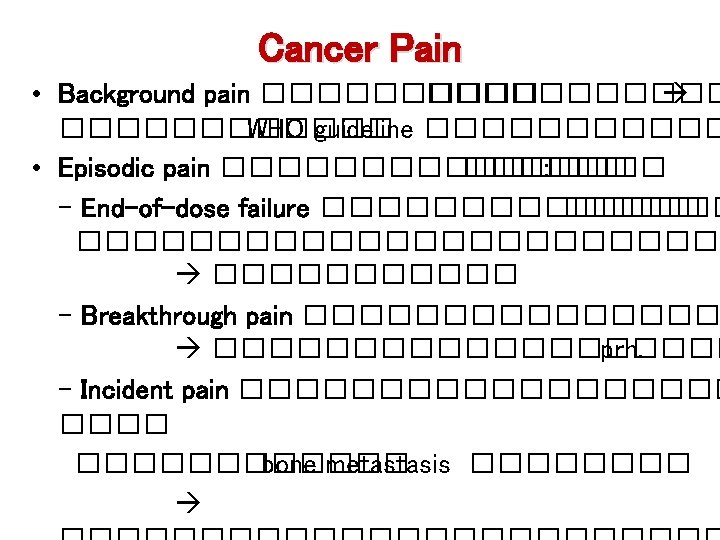
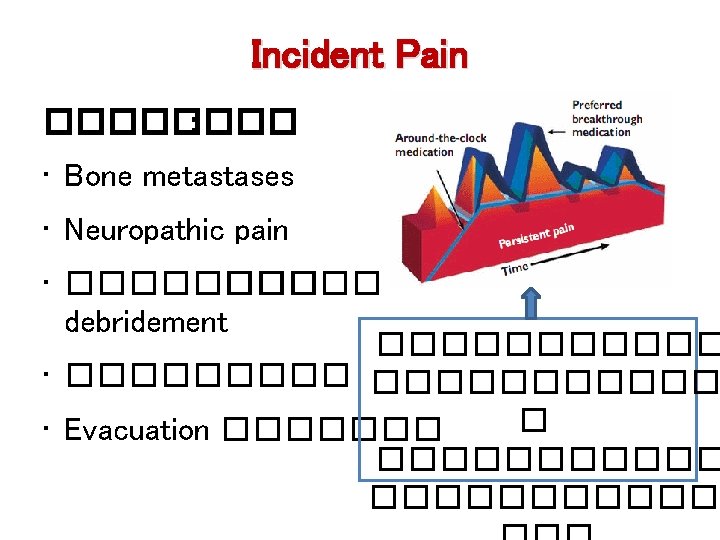
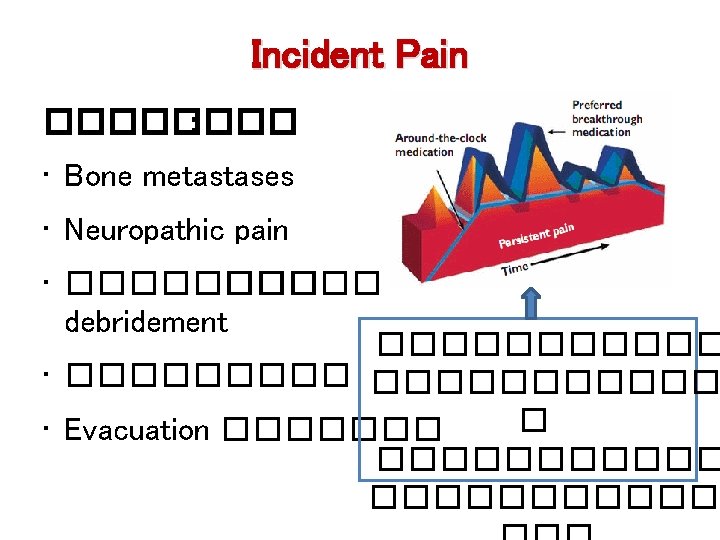
Cancer Pain • Background pain ����������� WHO guideline ������ • Episodic pain �������� : - End-of-dose failure �������������� - Breakthrough pain ���������� prn. - Incident pain ��������� bone metastasis ����
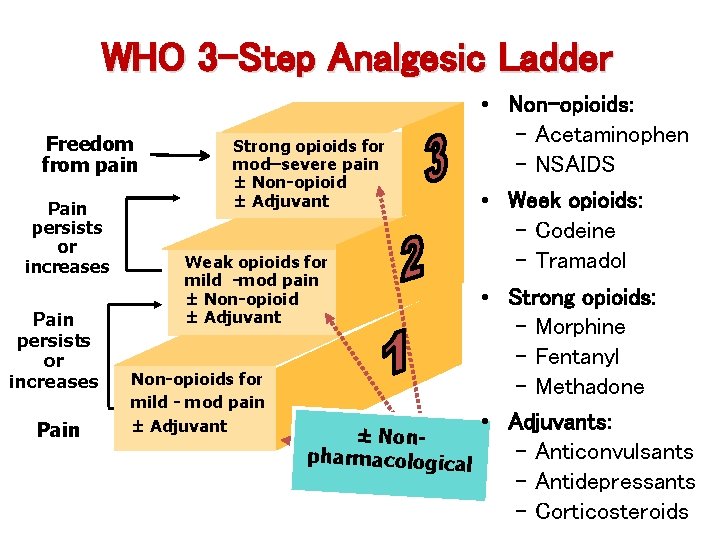
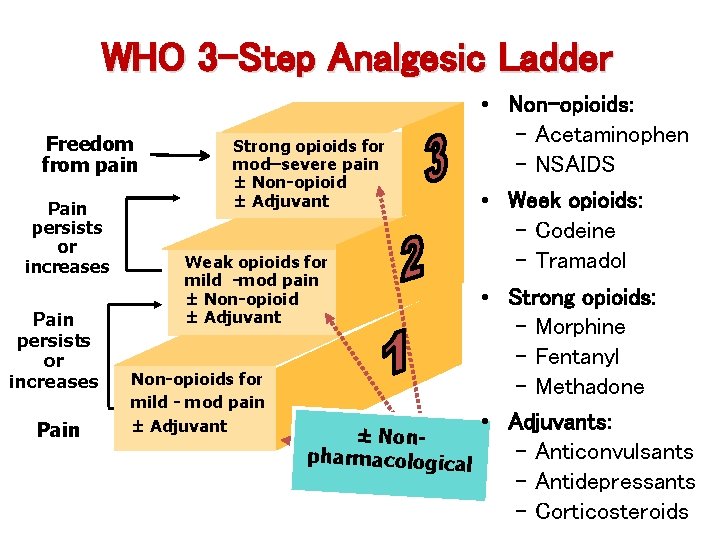
WHO 3 -Step Analgesic Ladder Freedom from pain Pain persists or increases Pain Strong opioids for mod–severe pain ± Non-opioid ± Adjuvant Weak opioids for mild -mod pain ± Non-opioid ± Adjuvant Non-opioids for mild - mod pain ± Adjuvant • Non-opioids: - Acetaminophen - NSAIDS • Week opioids: - Codeine - Tramadol • Strong opioids: - Morphine - Fentanyl - Methadone • Adjuvants: ± Non- Anticonvulsants pharmacological - Antidepressants - Corticosteroids
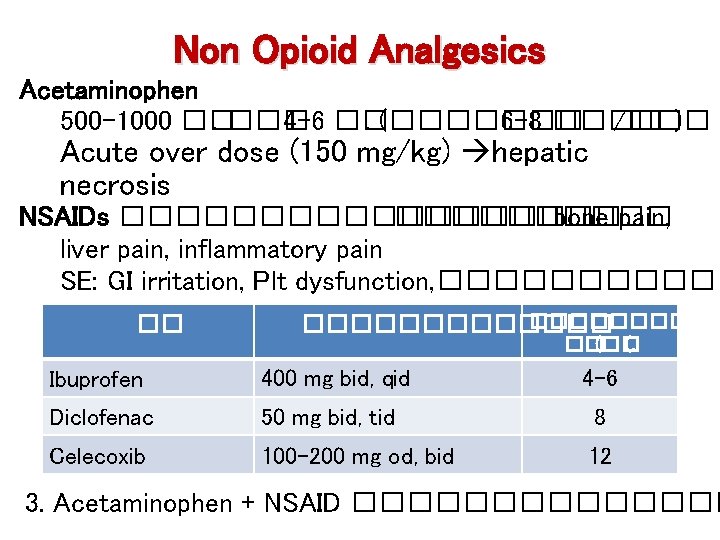
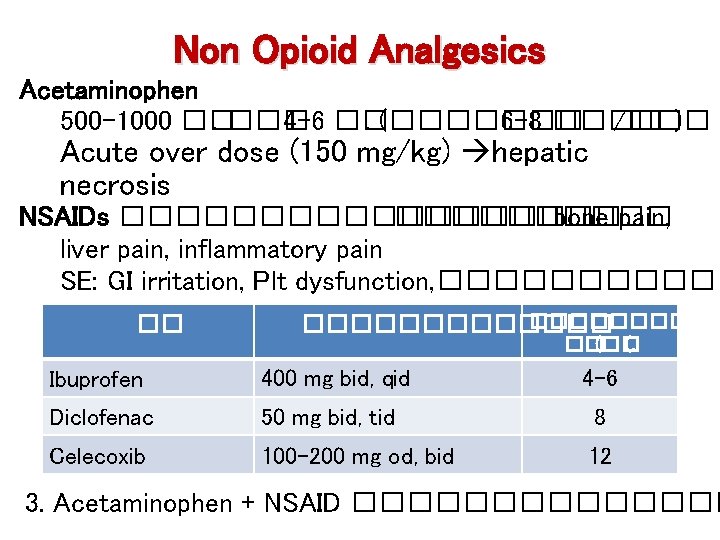
Non Opioid Analgesics Acetaminophen 500 -1000 ��. ��� 4 -6 ��. (������� 6 -8 ���� /��� ) Acute over dose (150 mg/kg) hepatic necrosis NSAIDs ��������� bone pain, liver pain, inflammatory pain SE: GI irritation, Plt dysfunction, ���������� �� ������� ��(�� (. Ibuprofen 400 mg bid, qid 4 -6 Diclofenac 50 mg bid, tid 8 Celecoxib 100 -200 mg od, bid 12 3. Acetaminophen + NSAID �������
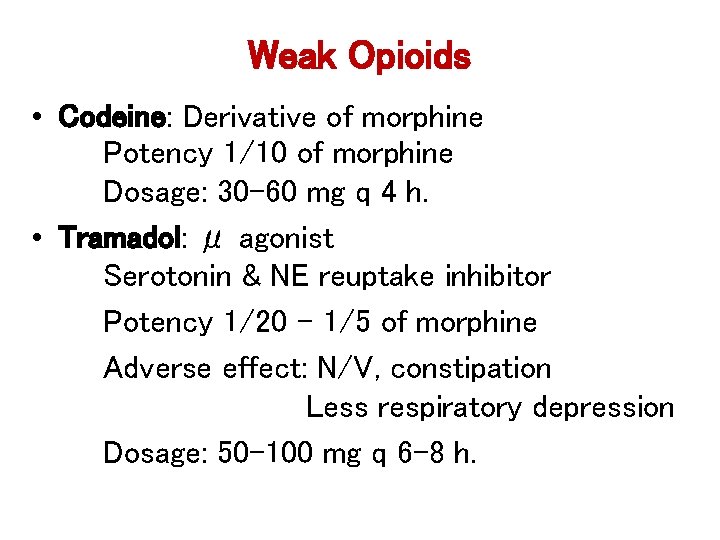
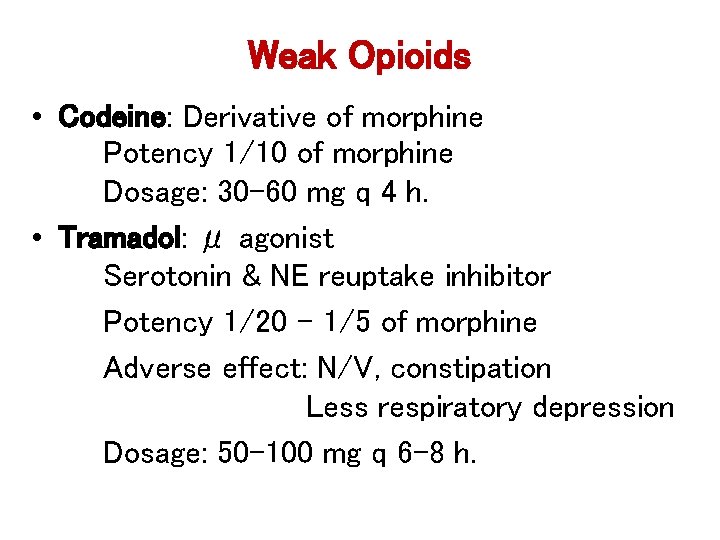
Weak Opioids • Codeine: Derivative of morphine Potency 1/10 of morphine Dosage: 30– 60 mg q 4 h. • Tramadol: μ agonist Serotonin & NE reuptake inhibitor Potency 1/20 – 1/5 of morphine Adverse effect: N/V, constipation Less respiratory depression Dosage: 50 -100 mg q 6 -8 h.
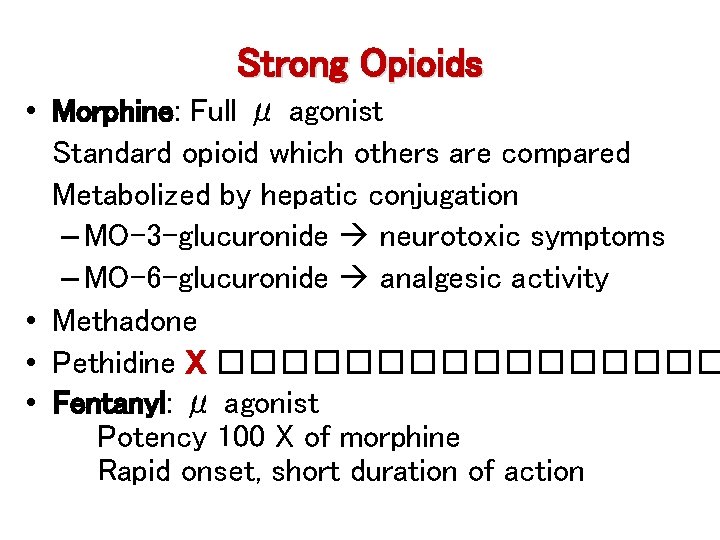
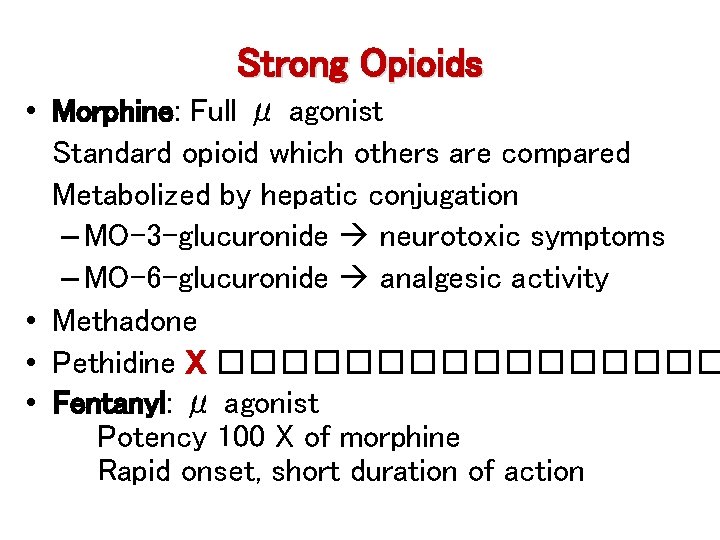
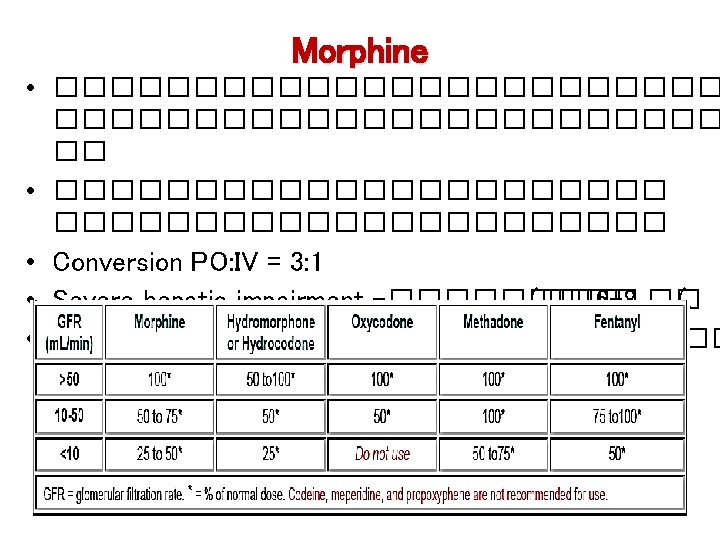
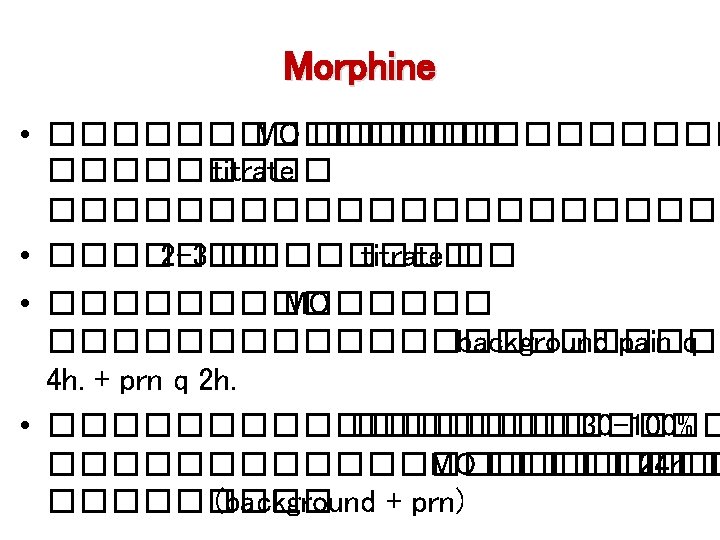
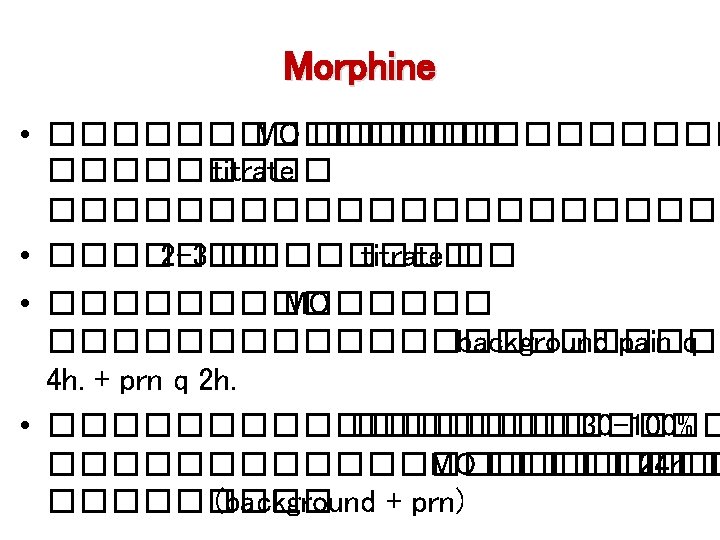
Strong Opioids • Morphine: Full μ agonist Standard opioid which others are compared Metabolized by hepatic conjugation – MO-3 -glucuronide neurotoxic symptoms – MO-6 -glucuronide analgesic activity • Methadone • Pethidine X �������� • Fentanyl: μ agonist Potency 100 X of morphine Rapid onset, short duration of action
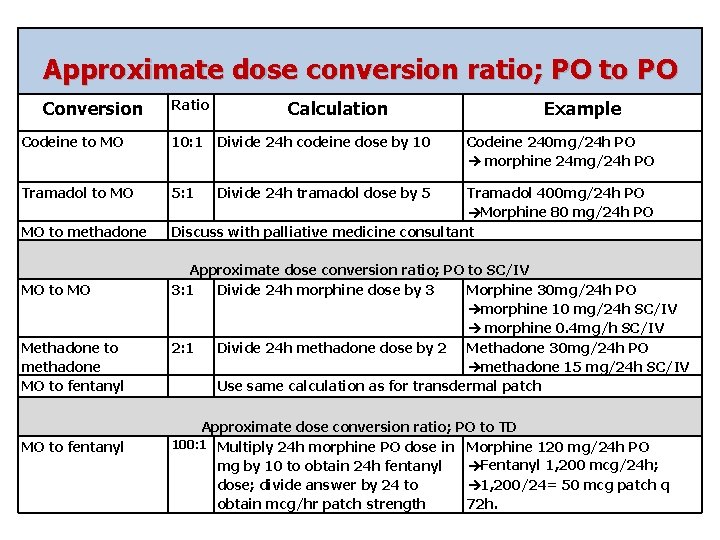
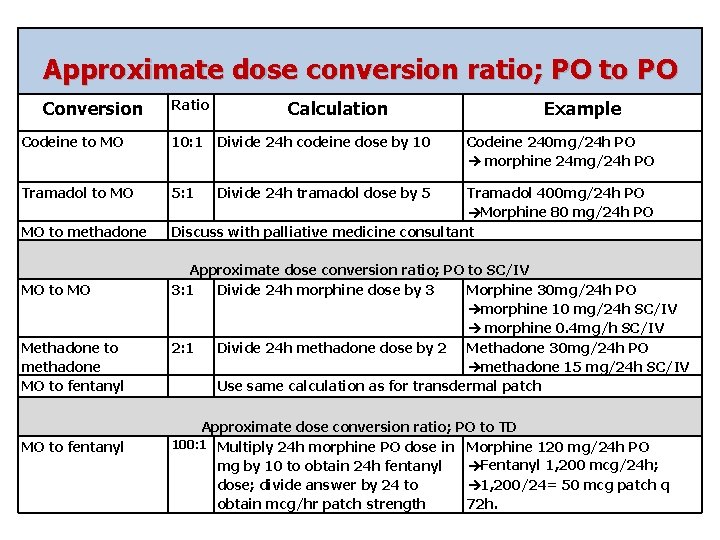
Approximate dose conversion ratio; PO to PO Conversion Ratio Calculation Codeine to MO 10: 1 Divide 24 h codeine dose by 10 Tramadol to MO 5: 1 Divide 24 h tramadol dose by 5 MO to methadone MO to MO Methadone to methadone MO to fentanyl Example Codeine 240 mg/24 h PO morphine 24 mg/24 h PO Tramadol 400 mg/24 h PO Morphine 80 mg/24 h PO Discuss with palliative medicine consultant Approximate dose conversion ratio; PO to SC/IV 3: 1 Divide 24 h morphine dose by 3 Morphine 30 mg/24 h PO morphine 10 mg/24 h SC/IV morphine 0. 4 mg/h SC/IV 2: 1 Divide 24 h methadone dose by 2 Methadone 30 mg/24 h PO methadone 15 mg/24 h SC/IV Use same calculation as for transdermal patch Approximate dose conversion ratio; PO to TD 100: 1 Multiply 24 h morphine PO dose in Morphine 120 mg/24 h PO Fentanyl 1, 200 mcg/24 h; mg by 10 to obtain 24 h fentanyl 1, 200/24= 50 mcg patch q dose; divide answer by 24 to obtain mcg/hr patch strength 72 h.
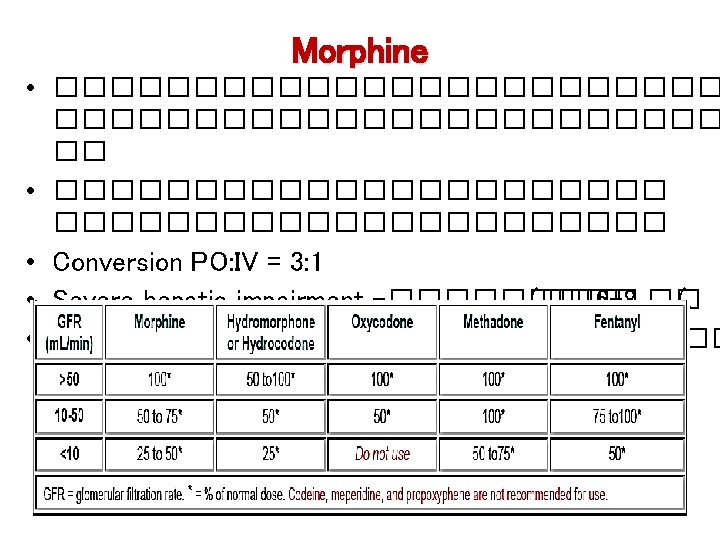
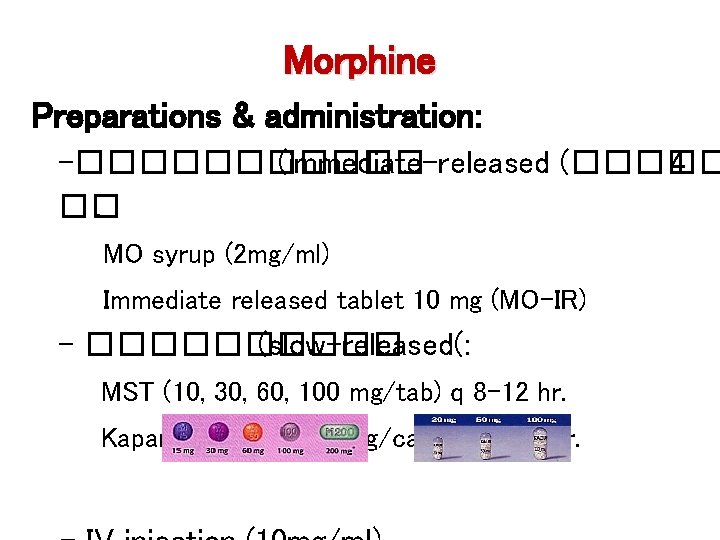
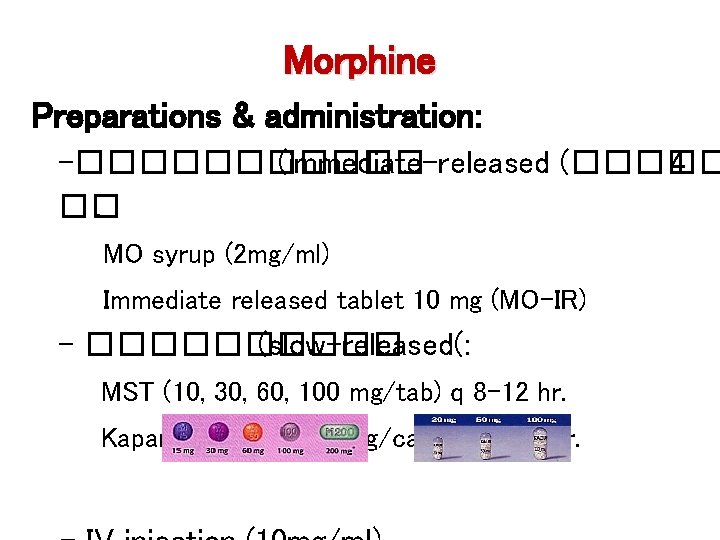
Morphine Preparations & administration: -������ (immediate-released (����� 4 ��. MO syrup (2 mg/ml) Immediate released tablet 10 mg (MO-IR) - ����� (slow-released(: MST (10, 30, 60, 100 mg/tab) q 8 -12 hr. Kapanol (20, 50, 100 mg/cap) q 12 -24 hr.
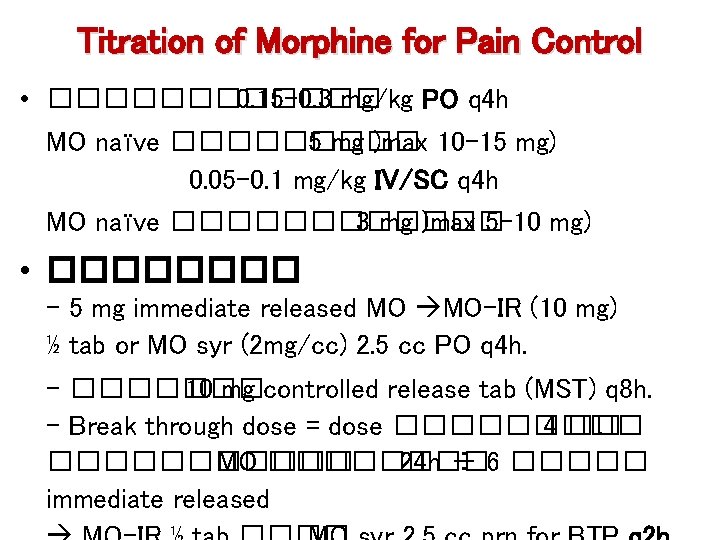
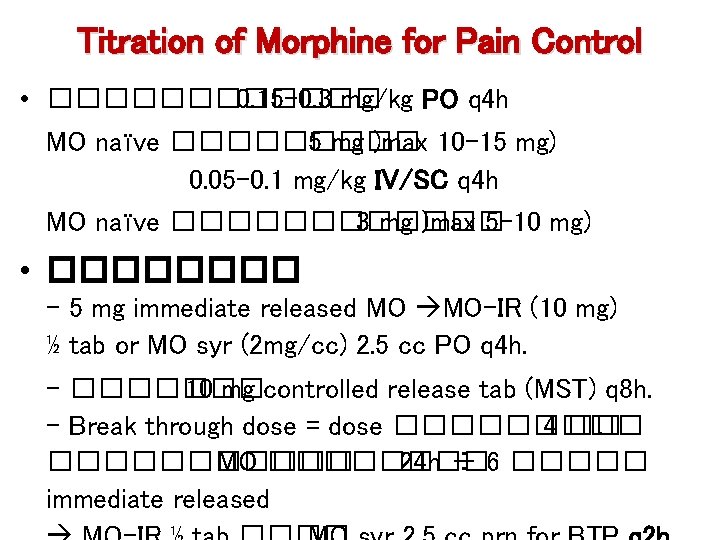
Titration of Morphine for Pain Control • ������ 0. 15 -0. 3 mg/kg PO q 4 h MO naïve ����� 5 mg )max 10 -15 mg) 0. 05 -0. 1 mg/kg IV/SC q 4 h MO naïve ������ 3 mg )max 5 -10 mg) • ���� - 5 mg immediate released MO MO-IR (10 mg) ½ tab or MO syr (2 mg/cc) 2. 5 cc PO q 4 h. - ������� 10 mg controlled release tab (MST) q 8 h. - Break through dose = dose ����� 4 ��. ������ MO ���� 24 h ÷ 6 ����� immediate released
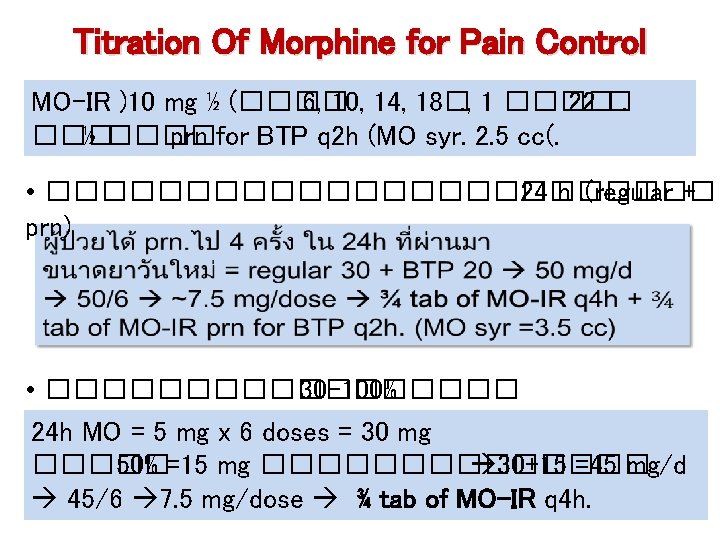
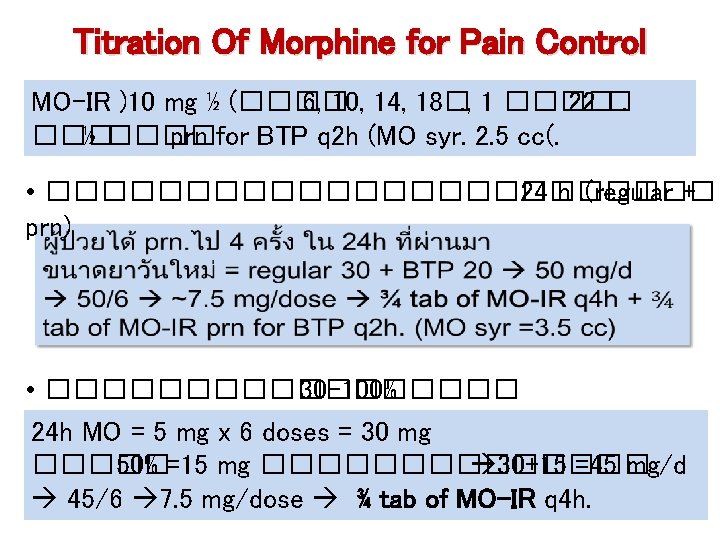
Titration Of Morphine for Pain Control MO-IR )10 mg ½ (���� 6, 10, 14, 18�. , 1 ���� 22 �. ��� ½ ���� prn for BTP q 2 h (MO syr. 2. 5 cc(. • ������������� 24 h. (regular + prn) • ��������� 30 -100% 24 h MO = 5 mg x 6 doses = 30 mg ����� 50% =15 mg ������� 30+15 =45 mg/d 45/6 7. 5 mg/dose ¾ tab of MO-IR q 4 h.
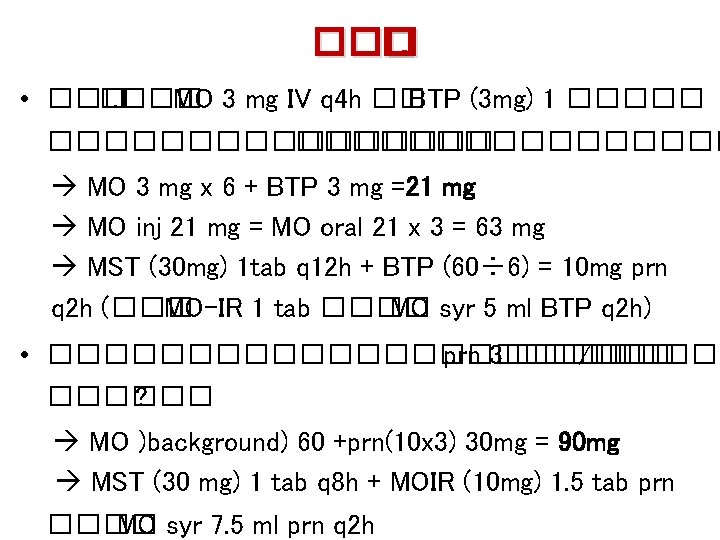
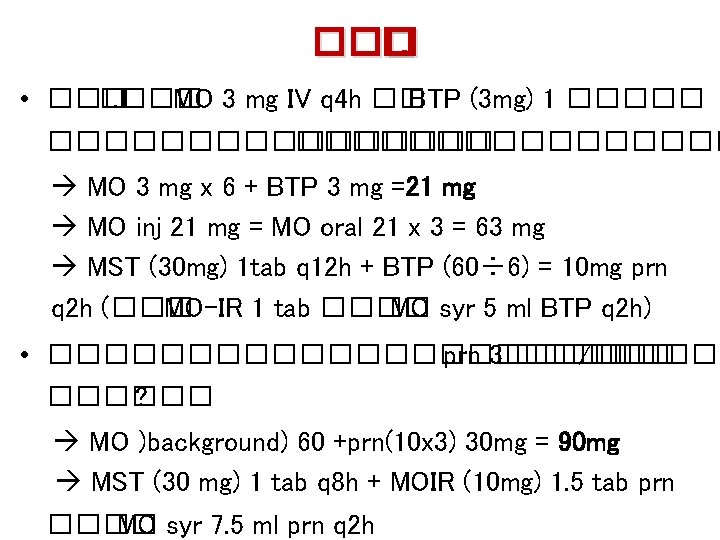
��� �. • ��� �. ��� MO 3 mg IV q 4 h �� BTP (3 mg) 1 ����������� MO 3 mg x 6 + BTP 3 mg =21 mg MO inj 21 mg = MO oral 21 x 3 = 63 mg MST (30 mg) 1 tab q 12 h + BTP (60÷ 6) = 10 mg prn q 2 h (��� MO-IR 1 tab ���� MO syr 5 ml BTP q 2 h) • ������������� prn 3����� /��� ������ ? MO )background) 60 +prn(10 x 3) 30 mg = 90 mg MST (30 mg) 1 tab q 8 h + MOIR (10 mg) 1. 5 tab prn ���� MO syr 7. 5 ml prn q 2 h
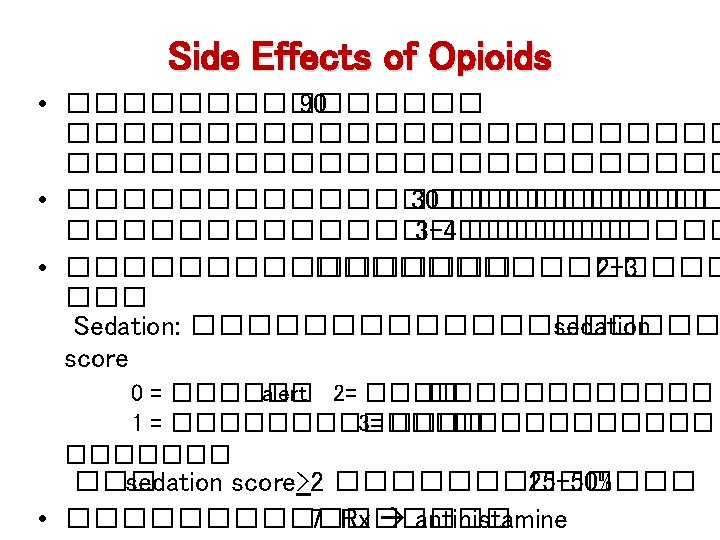
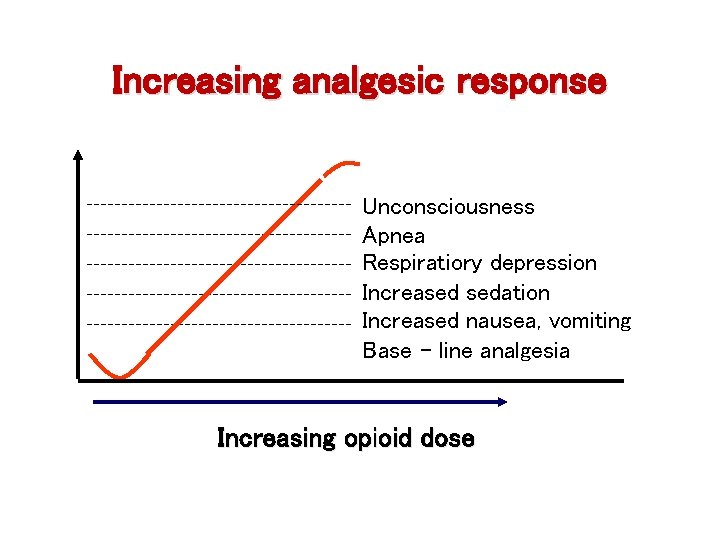
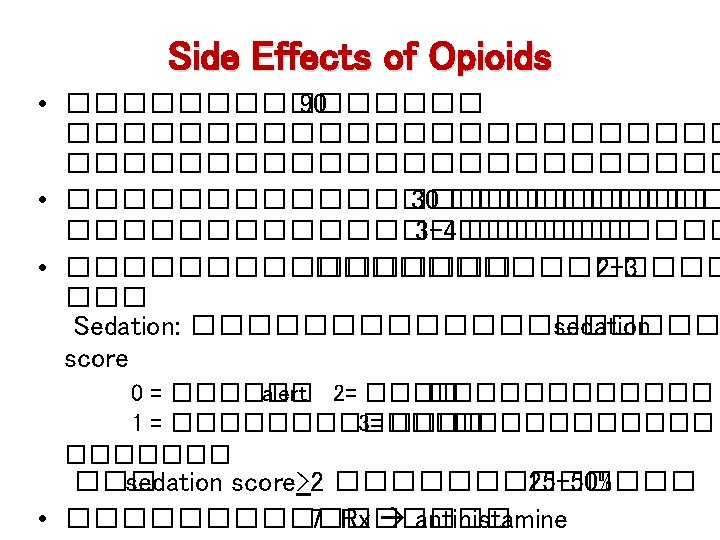
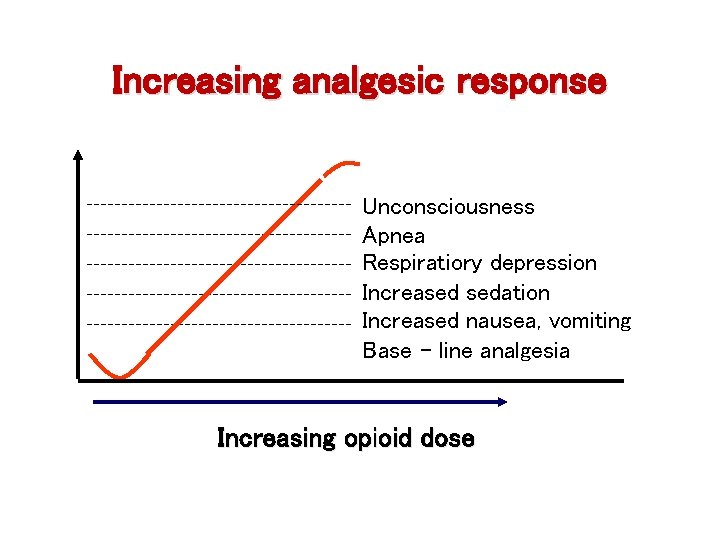
Increasing analgesic response Unconsciousness Apnea Respiratiory depression Increased sedation Increased nausea, vomiting Base - line analgesia Increasing opioid dose
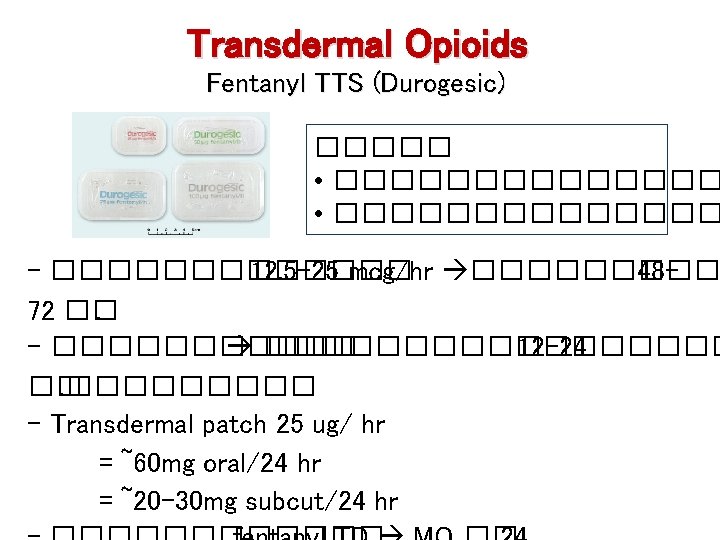
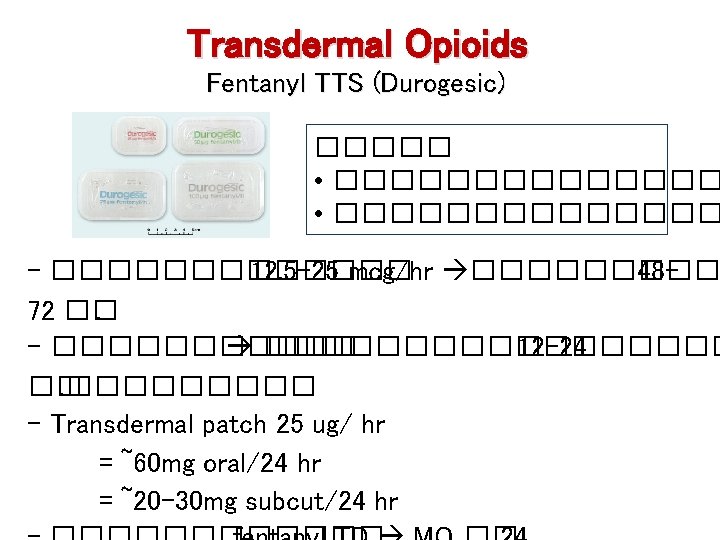
Transdermal Opioids Fentanyl TTS (Durogesic) ����� • �������������� - ������� 12. 5 -25 mcg/hr ����� 4872 ��. - ��������� 12 -24 ��. ����� - Transdermal patch 25 ug/ hr = ~60 mg oral/24 hr = ~20 -30 mg subcut/24 hr
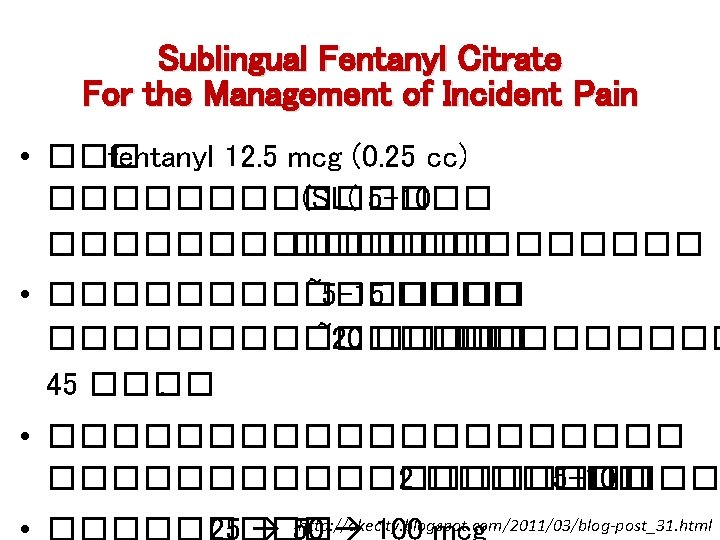
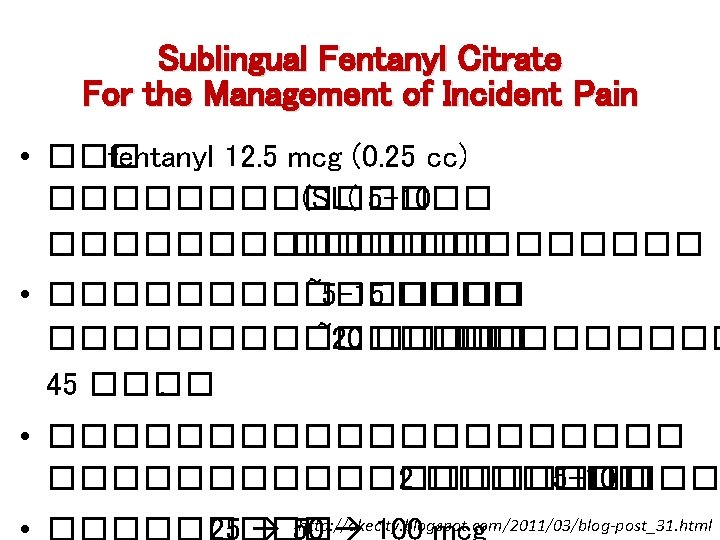
Sublingual Fentanyl Citrate For the Management of Incident Pain • ��� fentanyl 12. 5 mcg (0. 25 cc) ������� (SL( 5 -10 ������� • �������� ~5 -15 �������� ~20 ��������� 45 ����. • ���������� 2 ������� 5 -10 ��� http: //akecity. blogspot. com/2011/03/blog-post_31. html
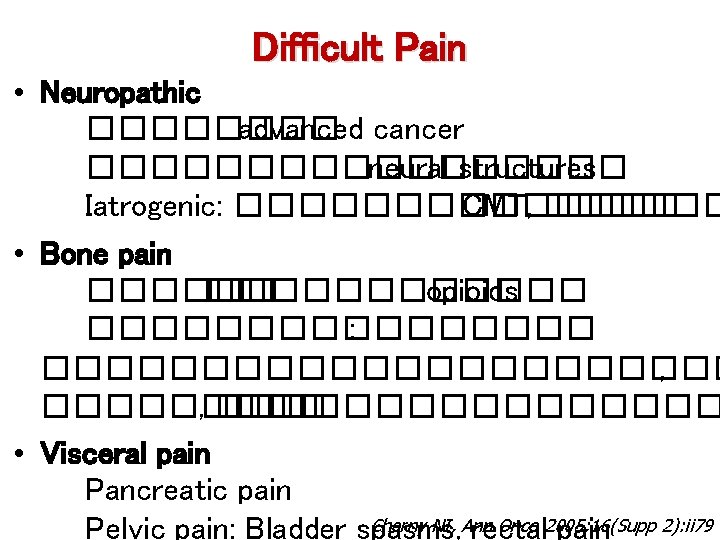
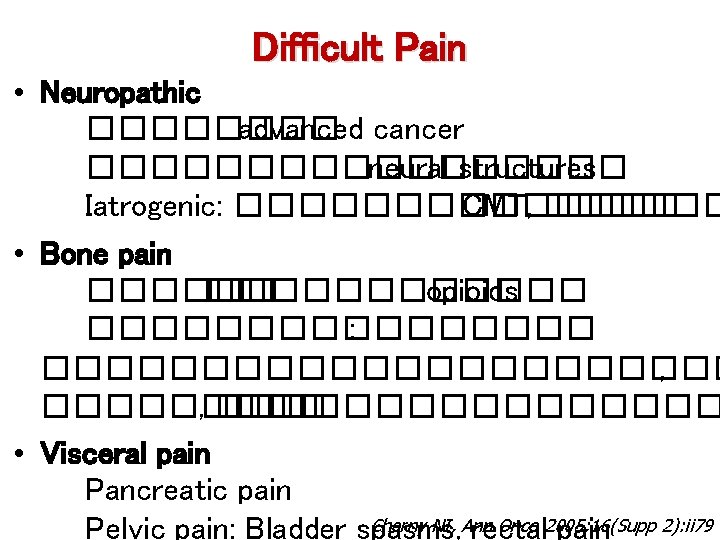
Difficult Pain • Neuropathic ���� advanced cancer ��������� neural structures Iatrogenic: ������� CMT, ������ • Bone pain ������������ opioids �������� : ����������� , ���������������� • Visceral pain Pancreatic pain Cherny NI, Ann Onco 2005; 16(Supp 2): ii 79 Pelvic pain: Bladder spasms, rectal pain
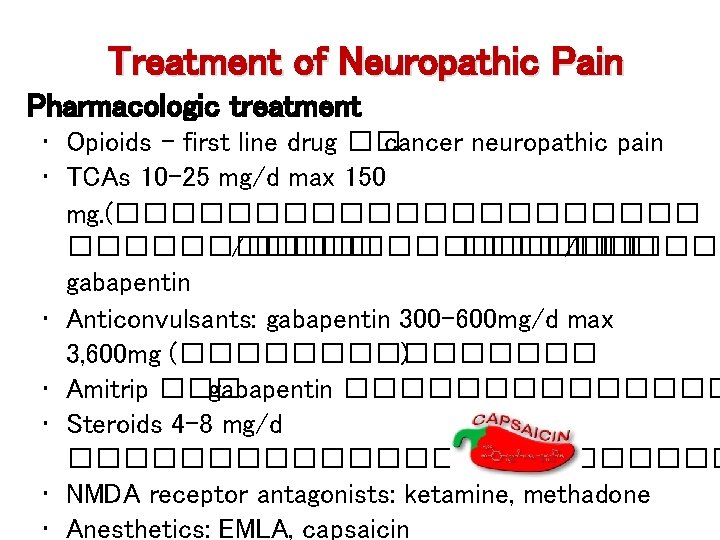
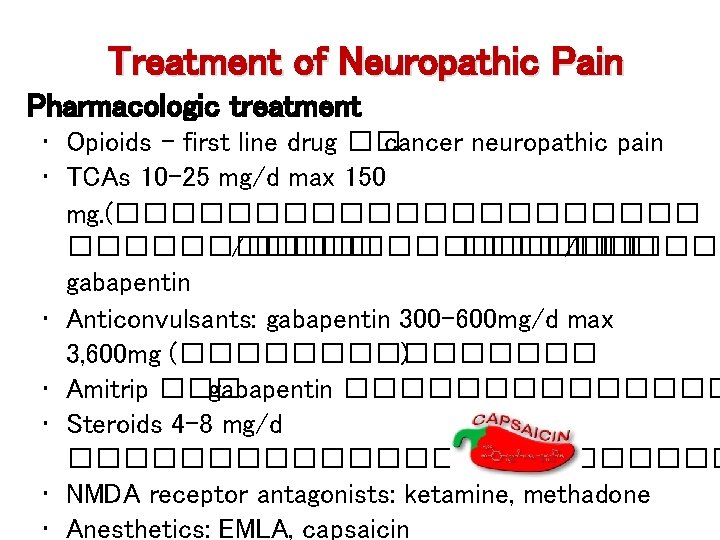
Treatment of Neuropathic Pain Pharmacologic treatment • Opioids - first line drug �� cancer neuropathic pain • TCAs 10 -25 mg/d max 150 mg. (����������� /������� /����� gabapentin • Anticonvulsants: gabapentin 300 -600 mg/d max 3, 600 mg (�������� ) • Amitrip ��� gabapentin ������� • Steroids 4 -8 mg/d ������������ • NMDA receptor antagonists: ketamine, methadone • Anesthetics: EMLA, capsaicin
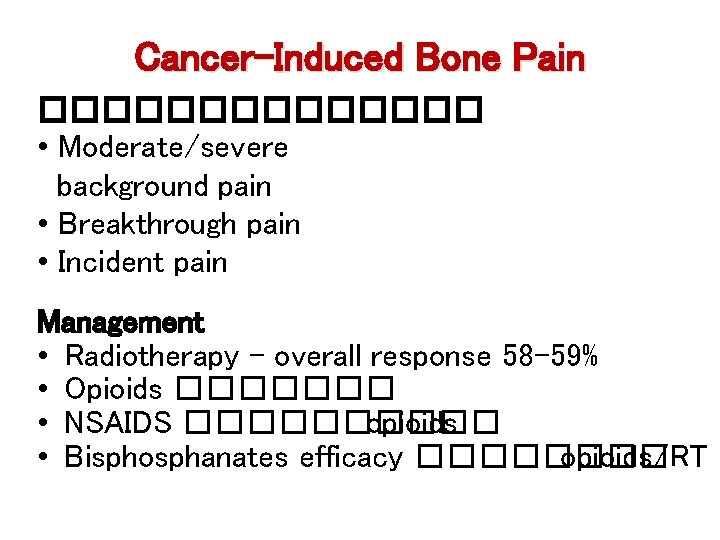
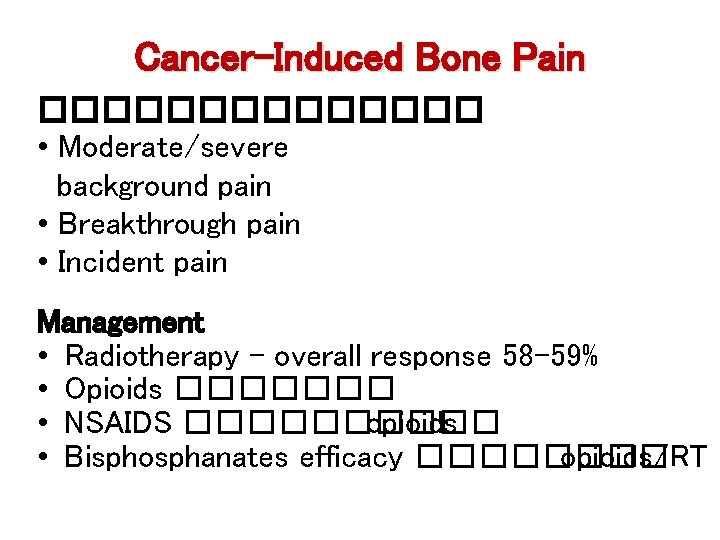
Cancer-Induced Bone Pain ������� • Moderate/severe background pain • Breakthrough pain • Incident pain Management • Radiotherapy - overall response 58 -59% • Opioids ������� • NSAIDS ����� opioids • Bisphosphanates efficacy ���� opioids/RT
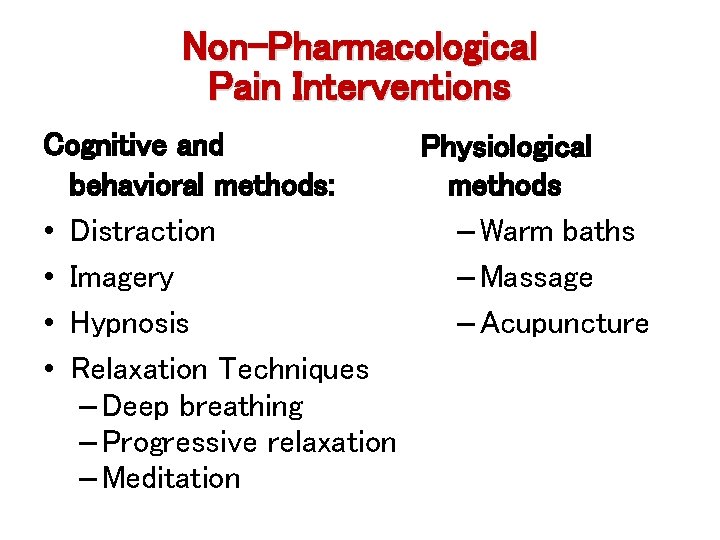
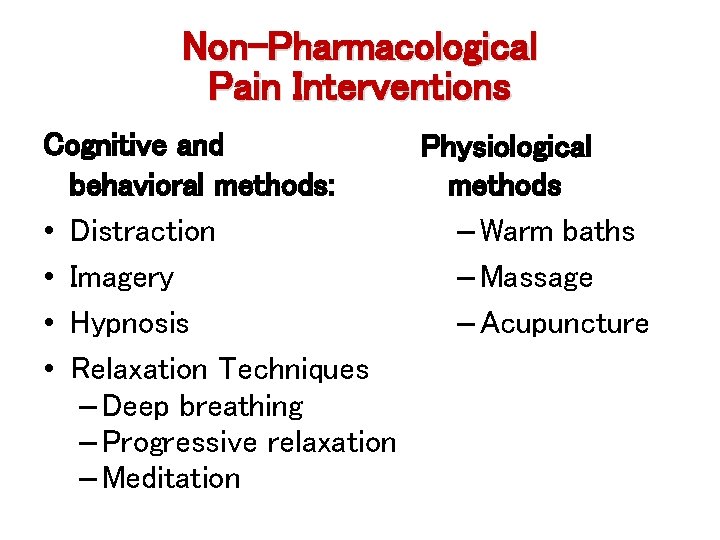
Non-Pharmacological Pain Interventions Cognitive and Physiological behavioral methods: methods • Distraction – Warm baths • Imagery – Massage • Hypnosis – Acupuncture • Relaxation Techniques – Deep breathing – Progressive relaxation – Meditation
 Antigentest åre
Antigentest åre Pcoc assessment tool kit
Pcoc assessment tool kit Martian pain
Martian pain Is tender breasts a sign of pregnancy
Is tender breasts a sign of pregnancy Franciscan palliative care
Franciscan palliative care Antiemetic drugs classification
Antiemetic drugs classification Period vs pregnancy
Period vs pregnancy Esasr
Esasr Rug adl
Rug adl Tarek mahdi md
Tarek mahdi md Principles of palliative care
Principles of palliative care Palliative care versus hospice care
Palliative care versus hospice care Palliative care in nepal
Palliative care in nepal Pps scale
Pps scale Criterio de terminalidad
Criterio de terminalidad Palliative care assistant
Palliative care assistant European certificate in essential palliative care
European certificate in essential palliative care Parallel planning palliative care
Parallel planning palliative care Adjuvant neoadjuvant palliative
Adjuvant neoadjuvant palliative Outcome measures traduzione
Outcome measures traduzione Log80 ausl romagna
Log80 ausl romagna Pcqc registry
Pcqc registry Just in case bag palliative care
Just in case bag palliative care Amber care bundle
Amber care bundle Goscote palliative care centre
Goscote palliative care centre Palliative care at home barry
Palliative care at home barry Palliative prognostic index
Palliative prognostic index Bluegrass care navigators hazard ky
Bluegrass care navigators hazard ky Provocative/palliative
Provocative/palliative Calvary palliative care kogarah
Calvary palliative care kogarah Anorexia, nausea and vomiting
Anorexia, nausea and vomiting Palliative care matters
Palliative care matters Anorexia cachexia palliative care
Anorexia cachexia palliative care Goc palliative care
Goc palliative care Npcrc
Npcrc European delirium association
European delirium association Palliative fase
Palliative fase