ational Hospice and Palliative Care Organizations N Palliative






- Slides: 23
�ational Hospice and Palliative Care Organization’s N Palliative Care Resource Series Metrics and Measurement for Palliative Care Kathleen Kerr Principal, PC-Insights
OBJECTIVES • Review a five-step process for selecting a balanced portfolio of feasible measures for your palliative care (PC) program • Introduce a framework for determining how many of which types of metrics your service might track • Review which practices to adopt and which to avoid, and some useful resources
What You Are Aiming for When You Are Measuring Being able to describe your program, what is does, and its impact on outcomes of interest (to leaders, decision-makers and other stakeholders)
5 Steps for Selecting Palliative Care Metrics 1. 2. 3. 4. Review best practices in the PC field Elicit and appreciate stakeholder priorities Identify potential structure, process and outcome metrics Assess feasibility – consider data collection burden and data accessibility 5. Pick your portfolio of feasible measures
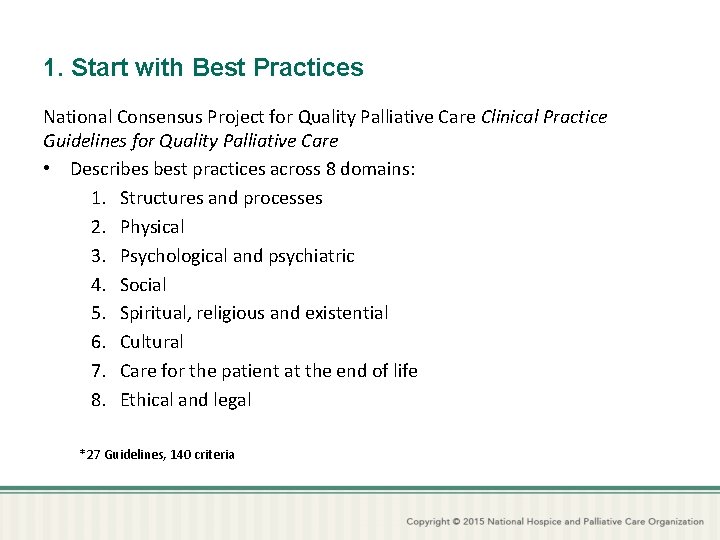
1. Start with Best Practices National Consensus Project for Quality Palliative Care Clinical Practice Guidelines for Quality Palliative Care • Describes best practices across 8 domains: 1. Structures and processes 2. Physical 3. Psychological and psychiatric 4. Social 5. Spiritual, religious and existential 6. Cultural 7. Care for the patient at the end of life 8. Ethical and legal *27 Guidelines, 140 criteria
2. Elicit Stakeholder Interests and Priorities • • • Patients and families Organizational leadership Payers Important donors Referring providers Your team
3. Identify Potential Metrics Look for measures that: – Speak to your goals – Are appropriate for your patients – Demonstrate adherence to best practices – Capture the impact your intervention has on outcomes you hope to achieve

Three Types of Metrics The Donabedian Model: • Structures (What’s in place) – The context of healthcare facilities, personnel, organizational characteristics. • Processes (Who gets it done) – Actions in healthcare including those of patients and families • Outcomes (How it turns out) – Effects on health status, quality of life, knowledge, behavior, satisfaction. Donabedian A, Wheeler JR, Wyszewianski L. Quality, cost, and health: an integrative model. Med Care. 1982 Oct; 20(10): 975 -92.

PC Program Structure Metrics • What you have in place to serve patients and families, team composition, training, availability and scope. – Sample Structure Metrics • Program staffing • Services offered • Locations/settings/availability

PC Program Process Metrics • • • Who –characteristics of patients seen What – what did the palliative care team do? Where – where were services provided? When – when were services provided? Why – what were the reasons that PC was asked to help? How much – what was the “dose” of PC provided? – Sample Process Metrics • What was addressed? • Timing of first contact relative to diagnosis and/or death • Proportion of patients receiving a comprehensive assessment
Outcomes of PC Programs • Describe the impact of clinical contacts – On patients: the impact of palliative care on pain scores or impact on care goals and trajectory. – On families and care teams: how satisfied were families or referring providers with the services provided? – On institutions: what impact does palliative care have on hospital use? Are costs reduced? Are there fewer inhospital deaths?
Sources for Potential Metrics • • Professional Organizations The literature Case Studies National Quality Forum National Palliative Care Research Center AHRQ Health Care Innovations Exchange Measuring What Matters
National Quality Forum Endorsed Measures • NQF: a nonprofit, nonpartisan, public service organization that reviews, endorses, and recommends use of standardized healthcare performance measures • Expert committees made up of varied stakeholders use rigorous process for evaluating evidence-base and utility of proposed measures • The federal government and many private sector entities use NQF-endorsed measures in payment and public reporting programs; broad national use • Currently there are 20+ measures that address cancer EOL care and palliative care generally
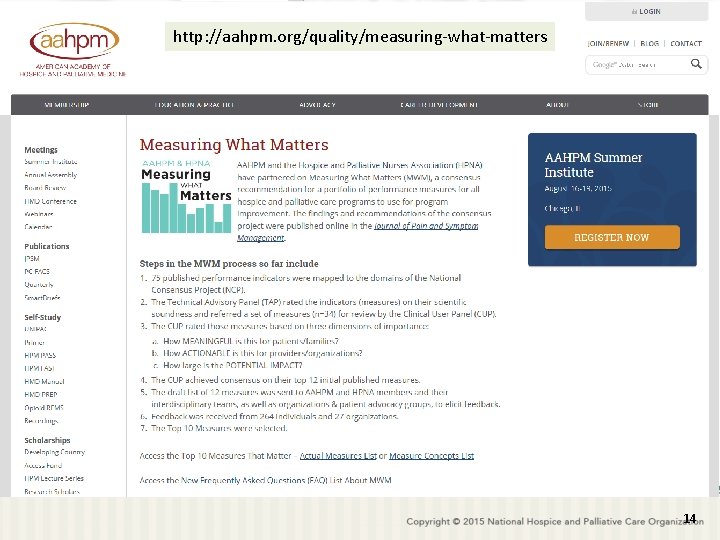
http: //aahpm. org/quality/measuring-what-matters 14
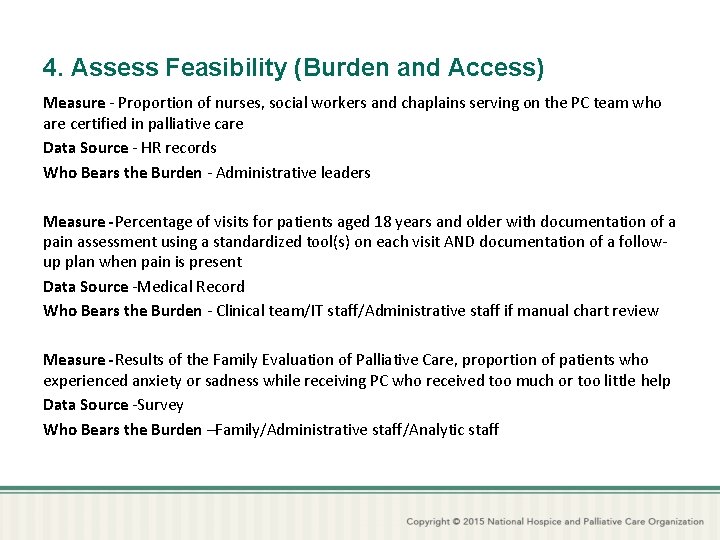
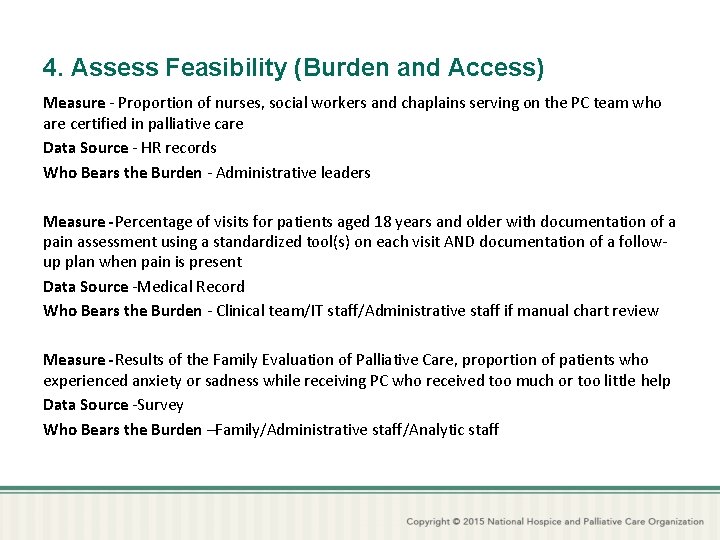
4. Assess Feasibility (Burden and Access) Measure - Proportion of nurses, social workers and chaplains serving on the PC team who are certified in palliative care Data Source - HR records Who Bears the Burden - Administrative leaders Measure -Percentage of visits for patients aged 18 years and older with documentation of a pain assessment using a standardized tool(s) on each visit AND documentation of a followup plan when pain is present Data Source -Medical Record Who Bears the Burden - Clinical team/IT staff/Administrative staff if manual chart review Measure -Results of the Family Evaluation of Palliative Care, proportion of patients who experienced anxiety or sadness while receiving PC who received too much or too little help Data Source -Survey Who Bears the Burden –Family/Administrative staff/Analytic staff
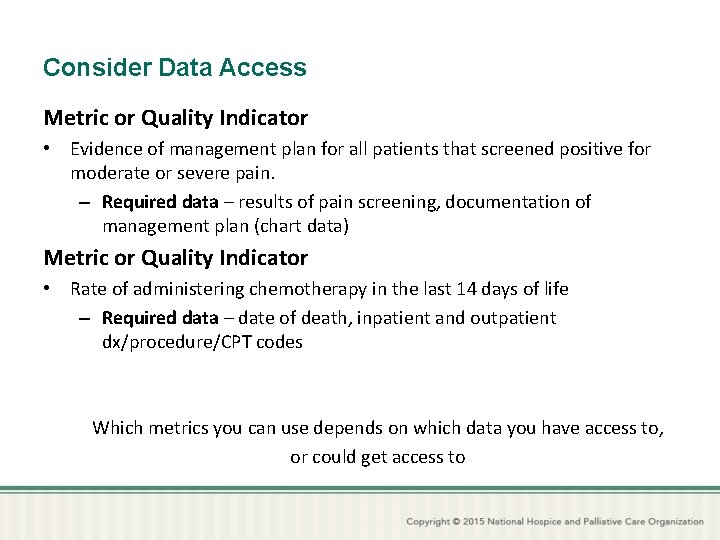
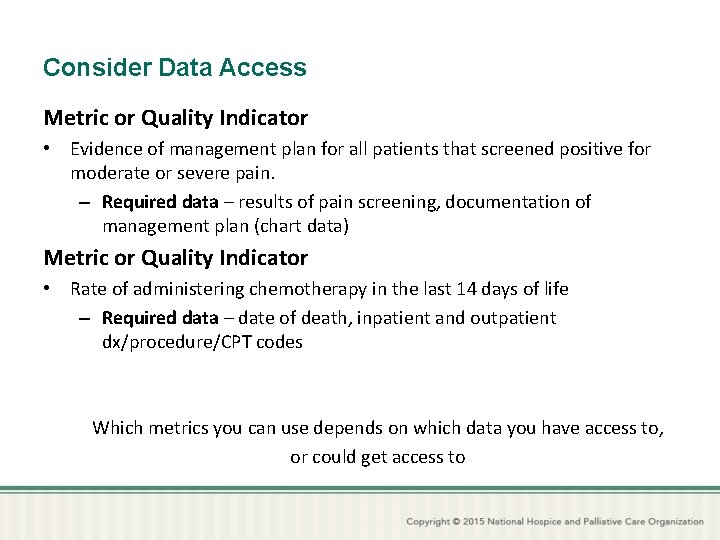
Consider Data Access Metric or Quality Indicator • Evidence of management plan for all patients that screened positive for moderate or severe pain. – Required data – results of pain screening, documentation of management plan (chart data) Metric or Quality Indicator • Rate of administering chemotherapy in the last 14 days of life – Required data – date of death, inpatient and outpatient dx/procedure/CPT codes Which metrics you can use depends on which data you have access to, or could get access to

5. Make Your Choices Crawl, walk, run • The types and number of metrics in your portfolio will be dictated by: – The developmental stage of your program – The resources at your disposal to gather and analyze data • (Feasible) Minimal Measuring – New program or few resources • Maximal Measuring – Established program or abundant resources • Between Minimal and Maximal – Most programs will be somewhere on the continuum between “New/few resources” and “Established/lots of resources”

Minimal Measuring • Structure and Process Metrics – one structure or process metric for each of the 8 NCP PC Domains, including at least 2 process measures • Outcome Metrics – 4 -6 items including any combination of Clinical or patient reported outcome metrics, social (family/caregiver/provider) outcome metrics, and cost/utilization outcome metrics. • Operational Metrics – Items that describe the volume and timing of service delivery and are commonly reported to program sponsors, such as health system, payer or medical group. The number and type of metrics will be negotiated with stakeholders.
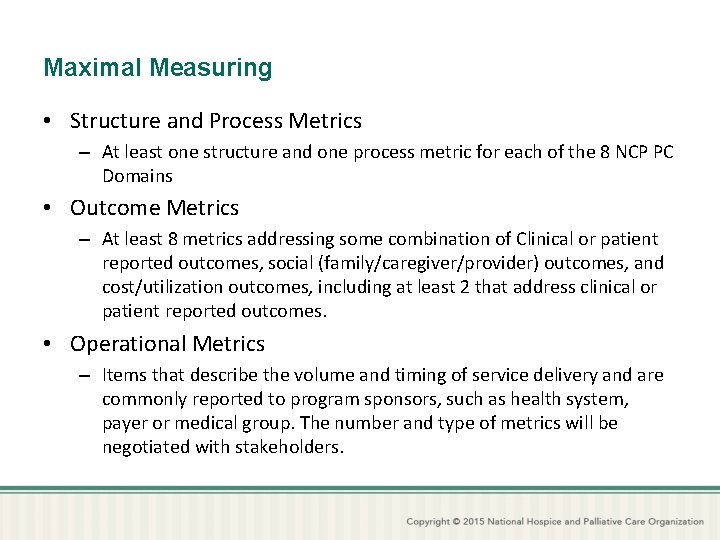
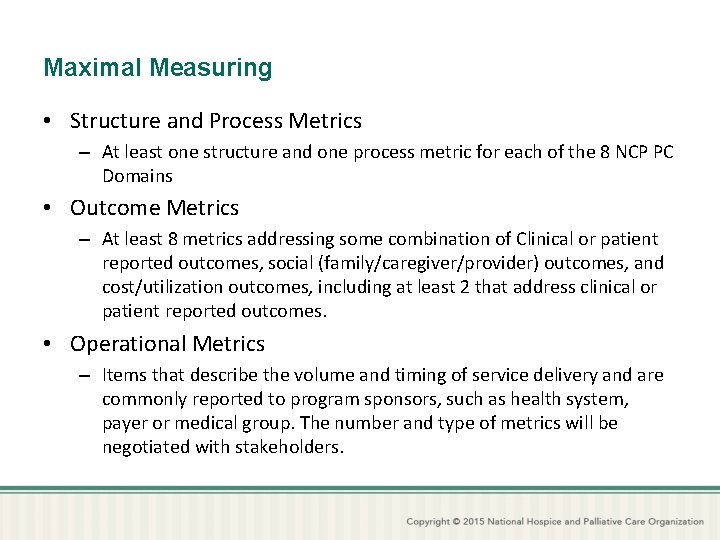
Maximal Measuring • Structure and Process Metrics – At least one structure and one process metric for each of the 8 NCP PC Domains • Outcome Metrics – At least 8 metrics addressing some combination of Clinical or patient reported outcomes, social (family/caregiver/provider) outcomes, and cost/utilization outcomes, including at least 2 that address clinical or patient reported outcomes. • Operational Metrics – Items that describe the volume and timing of service delivery and are commonly reported to program sponsors, such as health system, payer or medical group. The number and type of metrics will be negotiated with stakeholders.
5 Things Not To Do 1. Measure nothing 2. Gather lots of data … and never use it 3. Measure only one aspect of care, such as utilization and cost outcomes 4. Try to measure beyond your resources (time, expertise) 5. Measure things no one cares about
5 Things To Do 1. Anchor your program and your metrics portfolio in the core components of PC 2. Understand what you are trying to accomplish, and make sure you are set up to do those things 3. Understand what your stakeholders care about 4. Use structure, process and outcome metrics that map to your program’s goals, patients, priorities and resources 5. Remember that you are the expert, so be prepared to educate stakeholders about which metrics make sense to track, and why

Learn More! • Palliative Care Measure Menu – Web-based tool www. chcf. org/pcmenu • Metrics and Measurement for Palliative Care – California State University Institute for PC – Csupalliativecare. org/organizations/roadmap/metricsmeasurements/
Acknowledgements Co-developer of the concepts described in these slides: Brian Cassel, Ph. D jbcassel@vcu. edu / 804 -628 -1926 Assistant Professor, Hematology Oncology & Palliative Care Virginia Commonwealth University Richmond, Virginia The organizations that have supported our work: • The Coalition for Compassionate Care of California • The California Health Care Foundation • The CSU Institute for Palliative Care • The National Hospice and Palliative Care Organization
 Palliative care versus hospice care
Palliative care versus hospice care Franciscan palliative care
Franciscan palliative care Bluegrass hospice lexington ky
Bluegrass hospice lexington ky Traduzione
Traduzione Seamus hesney
Seamus hesney Esas-r
Esas-r Akps palliative
Akps palliative Palliative care programme
Palliative care programme Principles of palliative care
Principles of palliative care Palliative care in nepal
Palliative care in nepal Palliative care assistant
Palliative care assistant European certificate in essential palliative care
European certificate in essential palliative care Parallel planning palliative care
Parallel planning palliative care Pcpss
Pcpss Pcqc
Pcqc Just in case bag palliative care
Just in case bag palliative care What is amber care
What is amber care Goscote palliative care centre
Goscote palliative care centre Barry laird
Barry laird Calvary palliative care
Calvary palliative care Anorexia palliative care
Anorexia palliative care Palliative care matters
Palliative care matters Dr hong-phuc tran
Dr hong-phuc tran Goc palliative care
Goc palliative care