Pain Assessment Management M 3 Palliative Medicine Curriculum



- Slides: 55
Pain Assessment & Management M 3 Palliative Medicine Curriculum Seema S. Limaye, MD University of Chicago
GOALS 1. 2. 3. 4. Describe methods of pain assessment in cognitively impaired older adults. Understand various types of pain. Describe the basic pharmacology of opioids Understand how to initiate and titrate opioids.
Self-Directed Learning Modules Basics of Neuropathic pain n Side Effects of Opiods and Management Options n Treatment of Pain in Persons with h/o Substance Abuse n
Mrs. P 70 y. o. female h/o Paget’s disease, renal insufficiency, osteoporosis presents to clinic with new back pain. What do you want to obtain from the history?
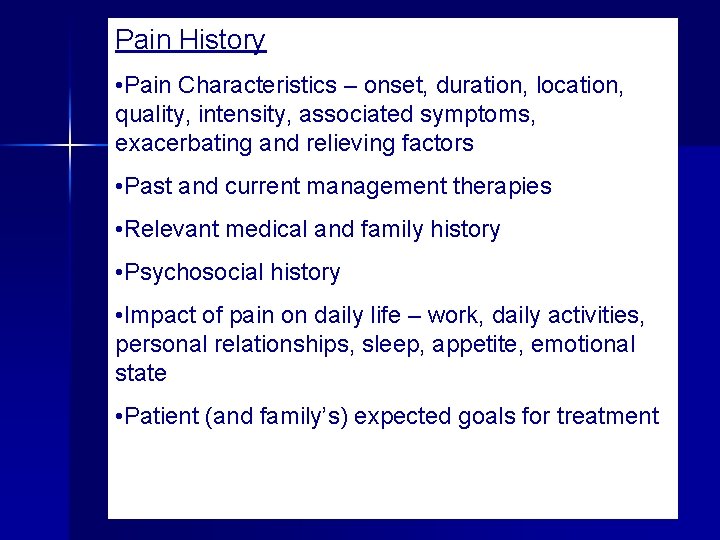
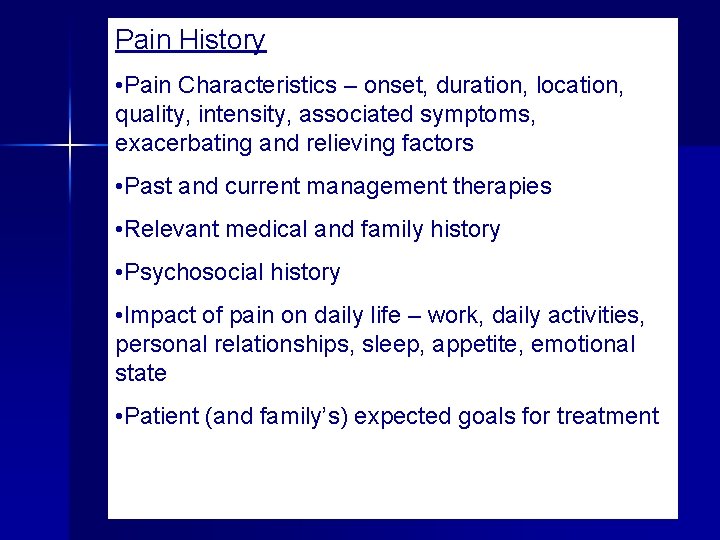
Pain History • Pain Characteristics – onset, duration, location, quality, intensity, associated symptoms, exacerbating and relieving factors • Past and current management therapies • Relevant medical and family history • Psychosocial history • Impact of pain on daily life – work, daily activities, personal relationships, sleep, appetite, emotional state • Patient (and family’s) expected goals for treatment
Pain: A Complex Phenomenon n Pain – Sensory stimuli and/or neurologic injury modified by an individual’s memory, expectations, emotions n Biocultural Model of Pain: – Society also influences an individual’s pain experiences

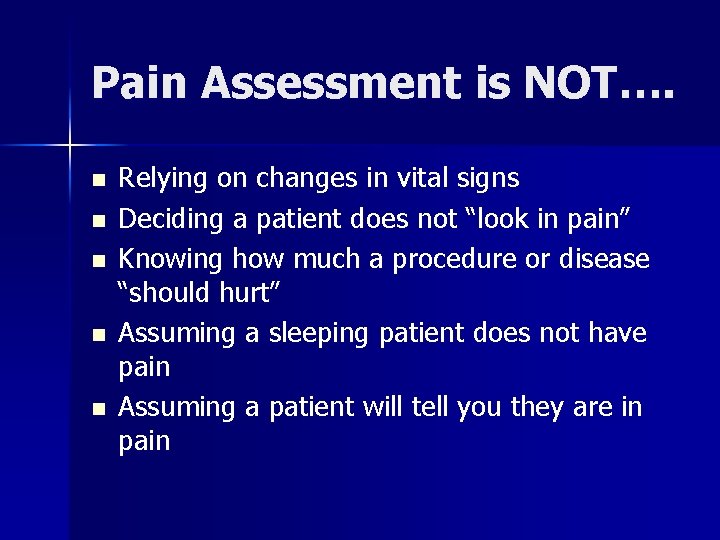
Pain Assessment is NOT…. n n n Relying on changes in vital signs Deciding a patient does not “look in pain” Knowing how much a procedure or disease “should hurt” Assuming a sleeping patient does not have pain Assuming a patient will tell you they are in pain
Consequences of Untreated Pain n Acute pain: – increase metabolic rate and blood clotting, – impair immune function – induce negative emotions n Without intervention, pain receptors become sensitive and may have long lasting changes in the neurons
Consequences of Untreated Pain n Chronic pain may lead to: – fatigue, – anxiety, – depression, – confusion, – increased falls, – impaired sleep, and – decreased physical functioning/deconditioning
Bedside Assessment n ASK the patient about pain – Asking about ADL’s and IADL’s – Asking about physical activity, mood, sleep, appetite, energy level n Identify preferred pain terminology -hurting, aching, stabbing, discomfort, soreness n Use a pain scale that works for the individual -Insure understanding of its use -Modify sensory deficits Ferrell et al. J Pain Symptom Manage 1995. Chinball and Tait Pain 2001. Herr and Garand. Pain Management in the Elderly 2001
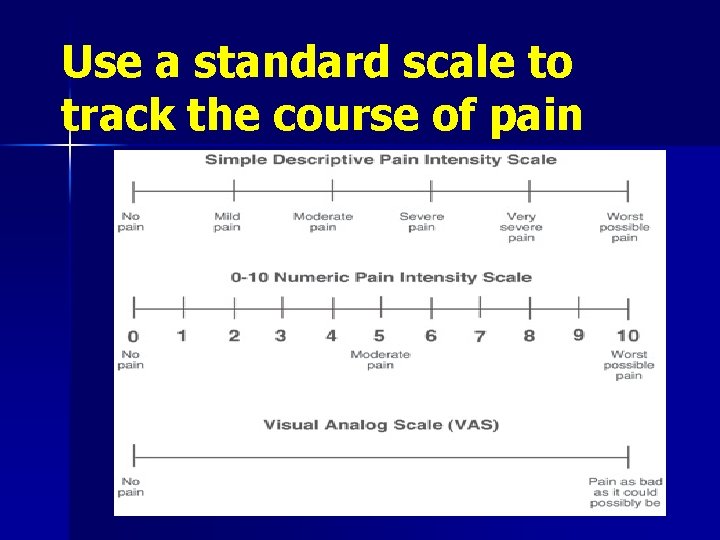
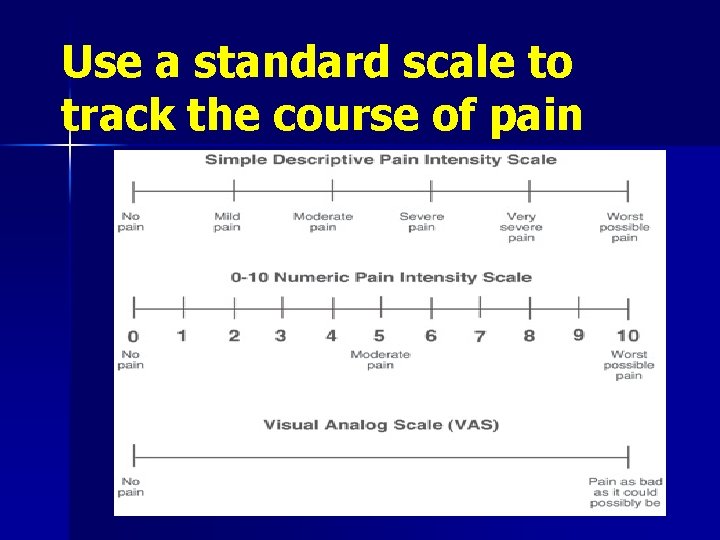
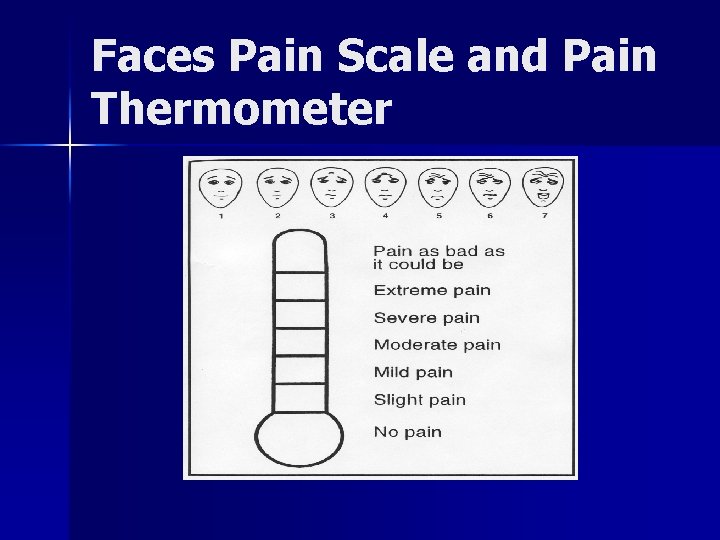
Use a standard scale to track the course of pain
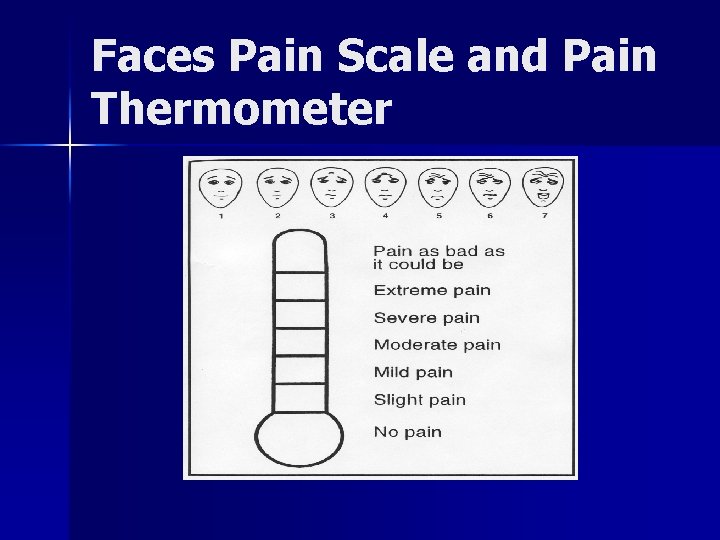
Faces Pain Scale and Pain Thermometer
What are some common barriers to pain treatment?
Remember the common patientrelated barriers to pain management n Drugs. . – are addicting – should be saved for when it is really needed – have unpleasant or dangerous side effects – pills are not as effective as a shot – narcotics are only for dying people
Pain assessment in a vulnerable group: Cognitively Impaired Older Adults
Assessing pain: Nonverbal, Moderate to Severe Impairment n Formal assessment tools available but not necessarily useful in routine clinical settings n Unique Pain Signature n Nonverbal Pain Indicators Kaasalainen et al Perspectives 1998. Herr and Garand Clinics in Geriatric Medicine 2000
Unique Pain Signature How does the patient usually act? n What changes are seen when they are in pain? – family members – nursing staff n Communication across caregiver settings is key! n Kovach et al. J Pain Symptom Manage 1999. Feldt et al. JAGS 1998. Weiner et al. Aging 1998.
Nonverbal Pain Indicators n n n Facial expressions (grimacing) -Less obvious: slight frown, rapid blinking, sad/frightened, any distortion Vocalizations (crying, moaning, groaning) -Less obvious: grunting, chanting, calling out, noisy breathing, asking for help Body movements (guarding) -Less obvious: rigid, tense posture, fidgeting, pacing, rocking, limping, resistance to moving Kaasalainen et al Perspectives 1998. Herr and Garand Clinics in Geriatric Medicine 2000
Selection of pain meds Source/type of pain n Duration/timing/frequency n History of medication use n Impact on quality of life n Presence of associated factors n
Types of Pain: A Brief Review n Nociceptive Pain – Visceral – Somatic Neuropathic Pain n Mixed/Unspecified Pain n Psychologic cause n
Quality: Visceral Pain n Descriptors: cramping, squeezing, n Distribution/Examples: pressure – Referred n heart attack, kidney stone – Colicky n Bowel obstruction, gallstone – Diffuse n n Peritonitis Analgesics: opioids; acetaminophen

Quality: Somatic pain Descriptors: aching, deep, dull, gnawing n Distribution/Examples: n – Well localized—patients can often point with one finger to the location of their pain • bone mets, strained ankle, toothache n Analgesics: NSAIDS, acetaminophen opioids
General Principles of Management Set a goal of reduction of pain to tolerable levels, not a goal of complete relief n “Start low and go slow” n Make sure patient and family are aware of goals n Frequent clinic visits at first for assurance, validation, and monitoring of titration n
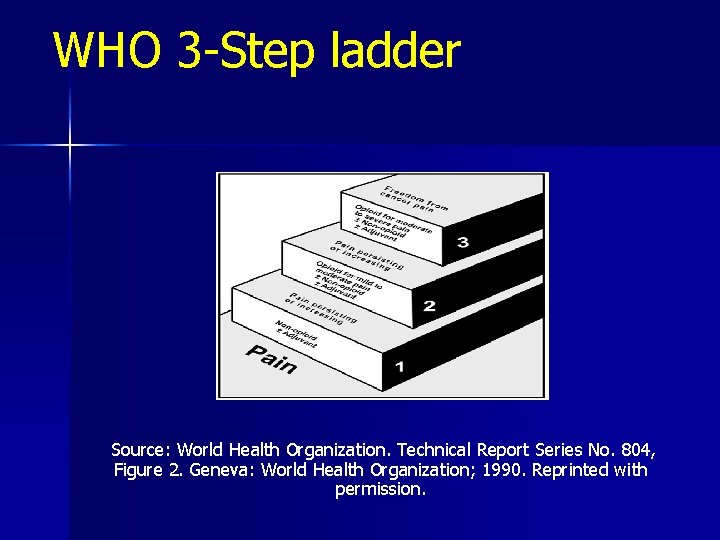
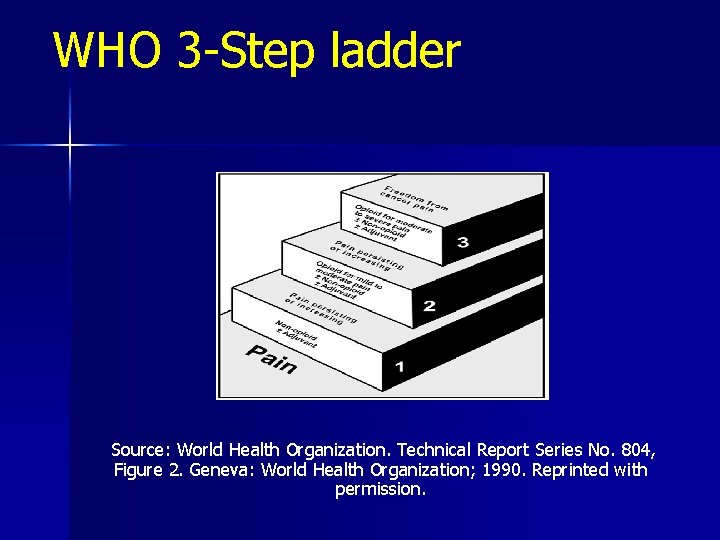
WHO 3 -Step ladder Source: World Health Organization. Technical Report Series No. 804, Figure 2. Geneva: World Health Organization; 1990. Reprinted with permission.

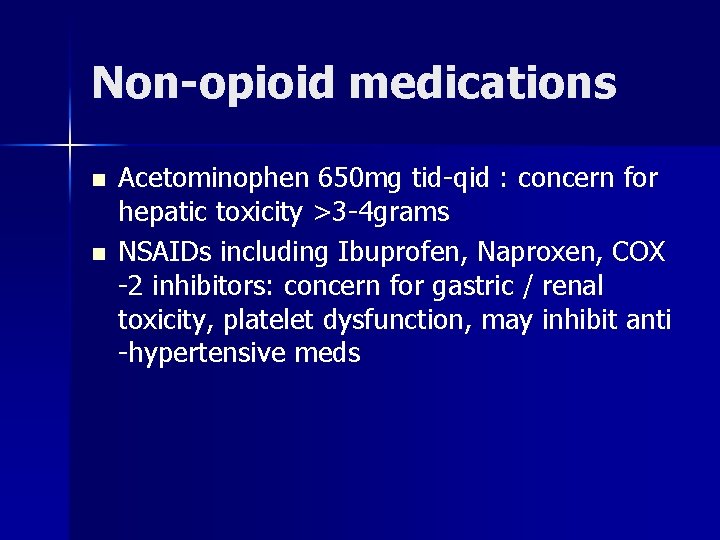
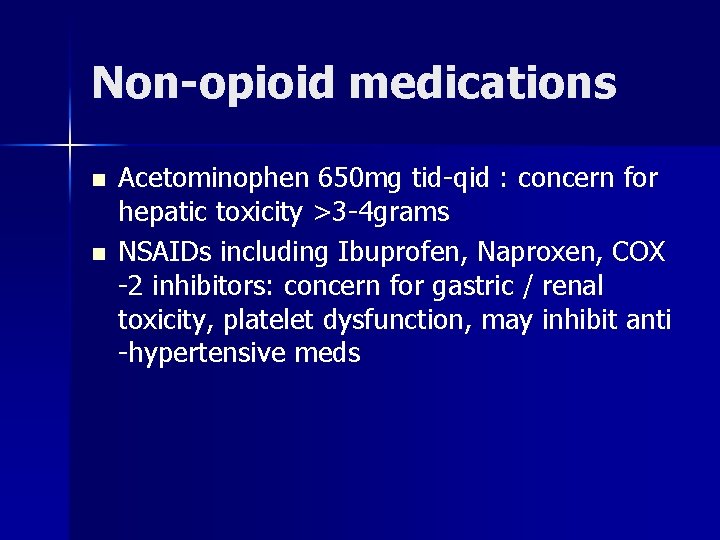
Non-opioid medications n n Acetominophen 650 mg tid-qid : concern for hepatic toxicity >3 -4 grams NSAIDs including Ibuprofen, Naproxen, COX -2 inhibitors: concern for gastric / renal toxicity, platelet dysfunction, may inhibit anti -hypertensive meds
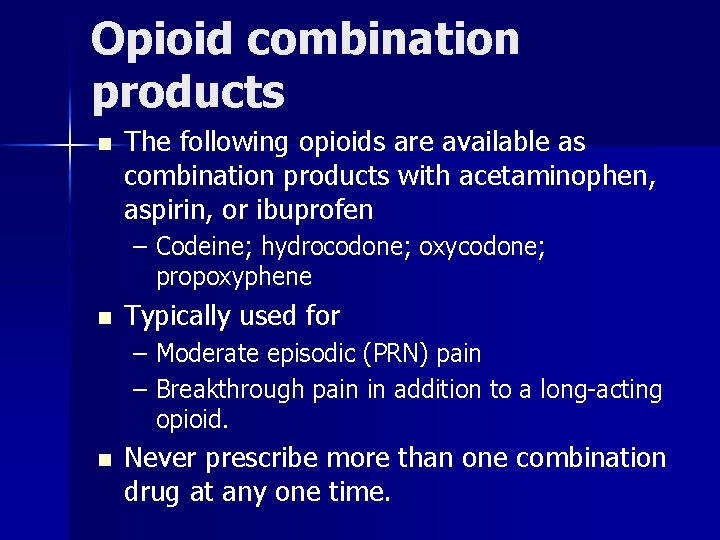
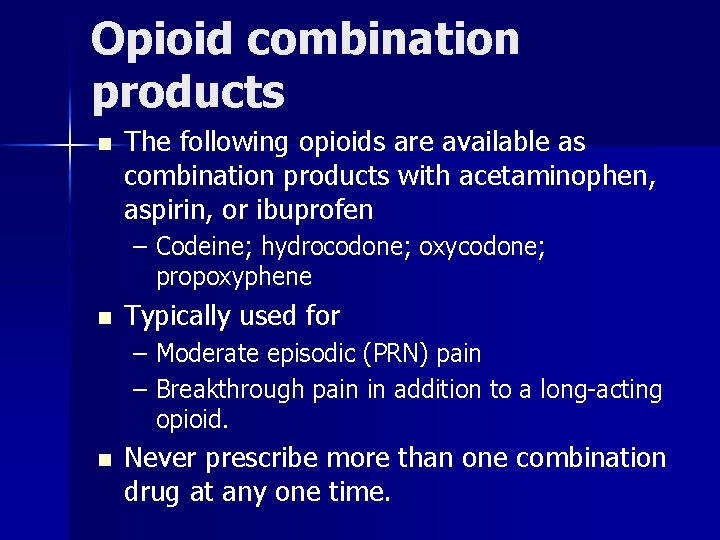
Opioid combination products n The following opioids are available as combination products with acetaminophen, aspirin, or ibuprofen – Codeine; hydrocodone; oxycodone; propoxyphene n Typically used for – Moderate episodic (PRN) pain – Breakthrough pain in addition to a long-acting opioid. n Never prescribe more than one combination drug at any one time.
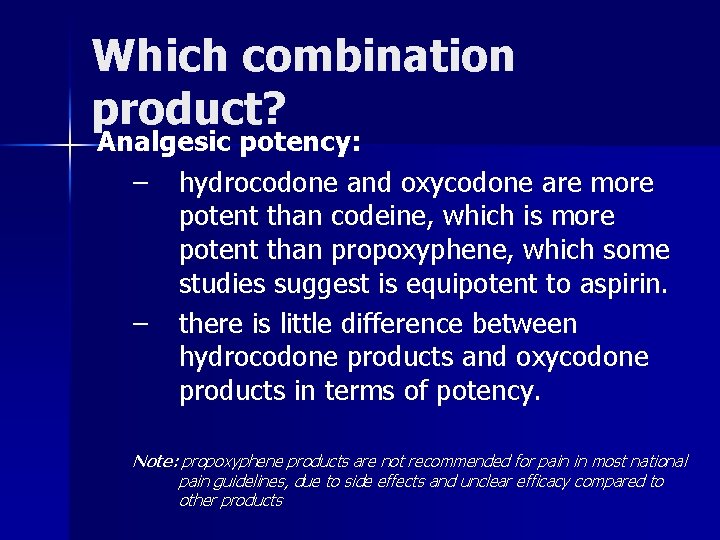
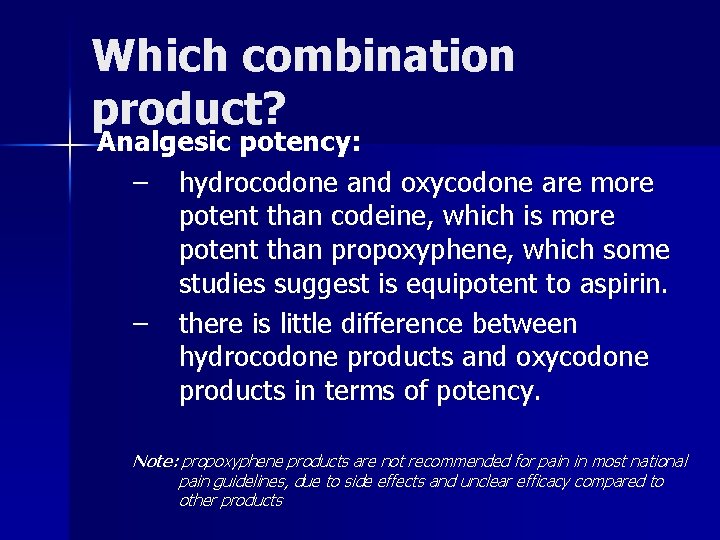
Which combination product? Analgesic potency: – hydrocodone and oxycodone are more potent than codeine, which is more potent than propoxyphene, which some studies suggest is equipotent to aspirin. – there is little difference between hydrocodone products and oxycodone products in terms of potency. Note: propoxyphene products are not recommended for pain in most national pain guidelines, due to side effects and unclear efficacy compared to other products
Adjuvants n n n n Non-pharmacologic Topicals Tylenol NSAIDS, Celecoxib, steroids Anticonvulsants Antidepressants Antiarrhythmics
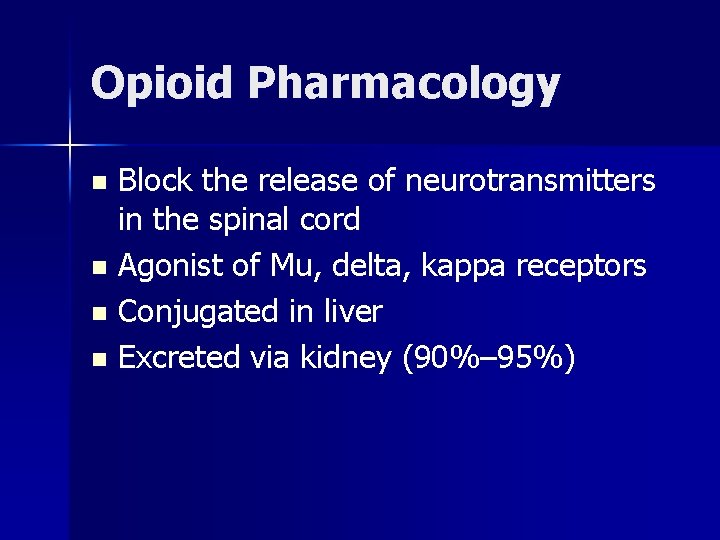
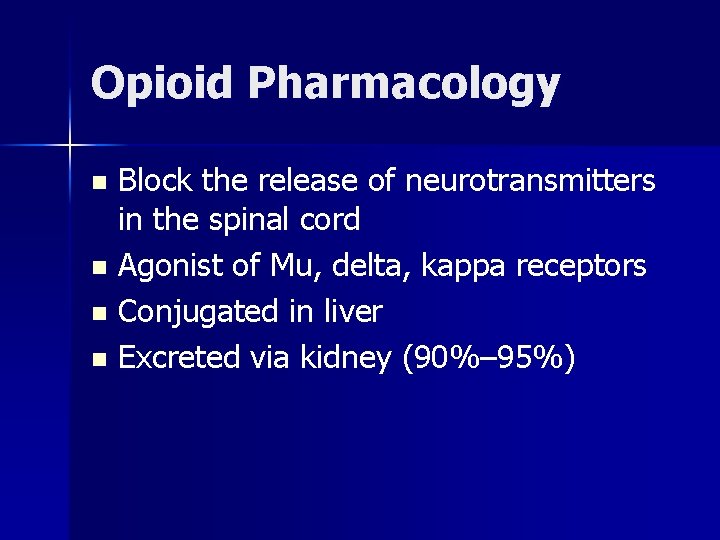
Opioid Pharmacology Block the release of neurotransmitters in the spinal cord n Agonist of Mu, delta, kappa receptors n Conjugated in liver n Excreted via kidney (90%– 95%) n
Opioid pharmacology Central and peripheral effects of opioids n This leads to desired effects, as well as side effects n
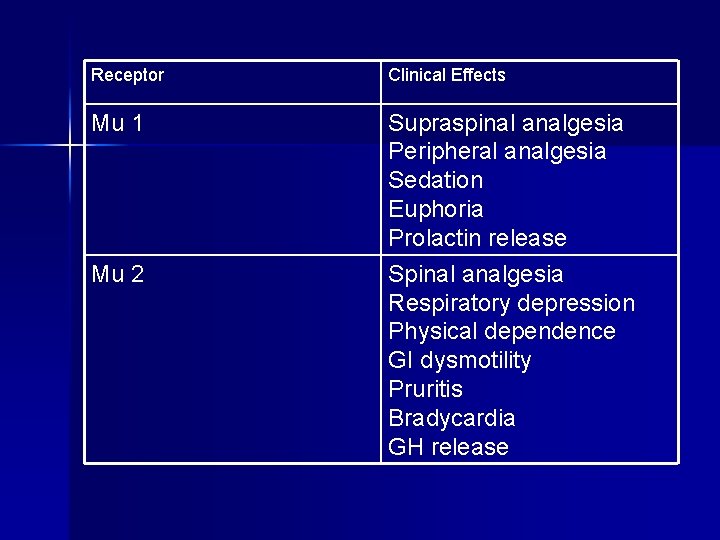
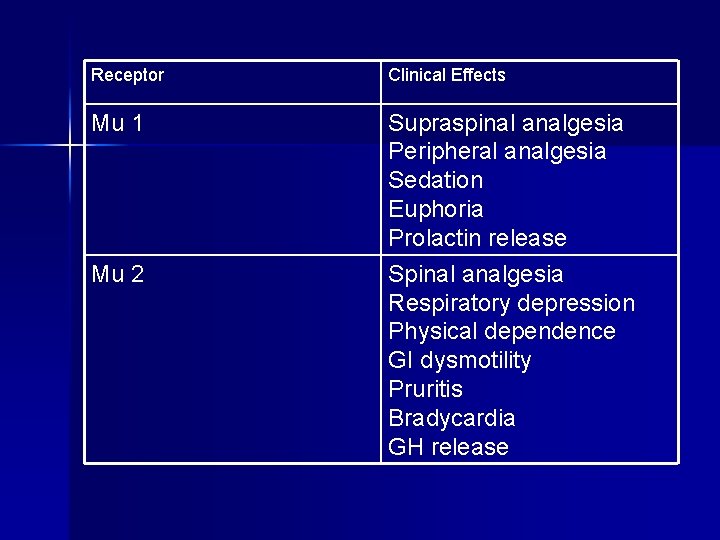
Receptor Clinical Effects Mu 1 Supraspinal analgesia Peripheral analgesia Sedation Euphoria Prolactin release Spinal analgesia Respiratory depression Physical dependence GI dysmotility Pruritis Bradycardia GH release Mu 2
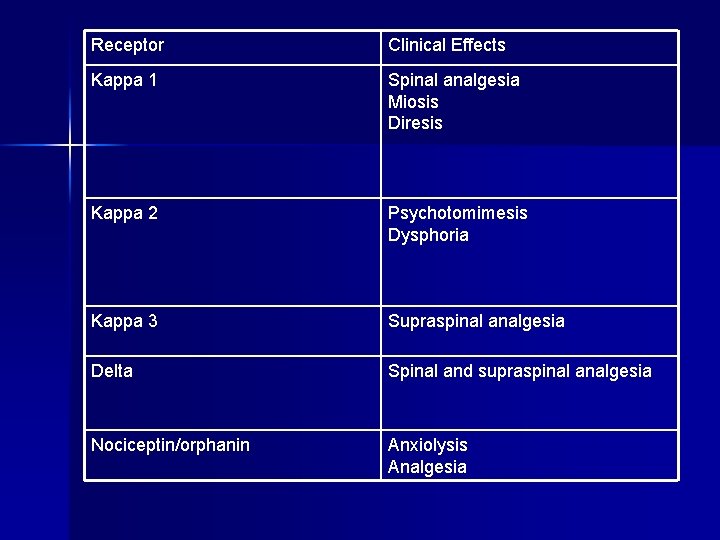
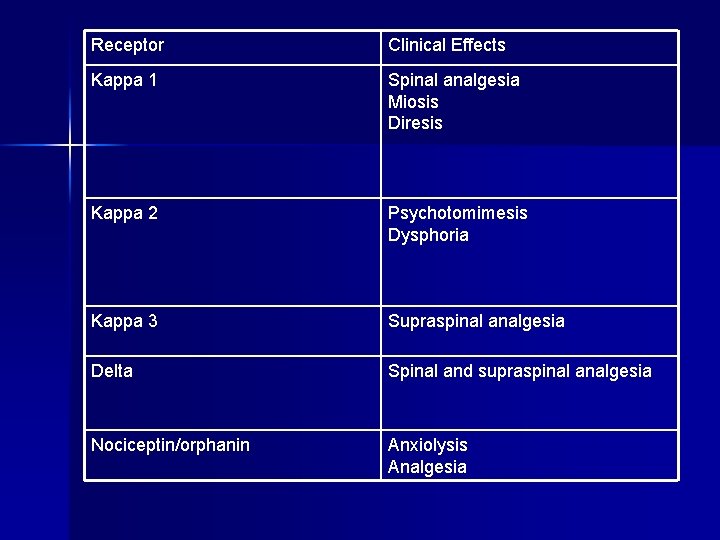
Receptor Clinical Effects Kappa 1 Spinal analgesia Miosis Diresis Kappa 2 Psychotomimesis Dysphoria Kappa 3 Supraspinal analgesia Delta Spinal and supraspinal analgesia Nociceptin/orphanin Anxiolysis Analgesia
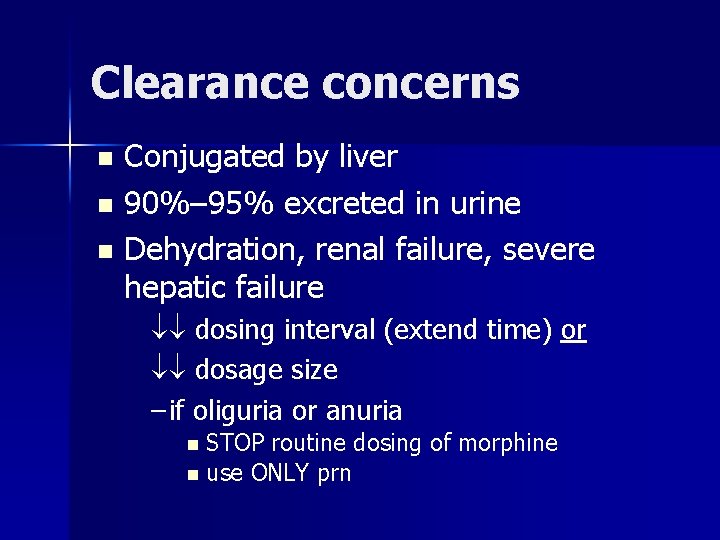
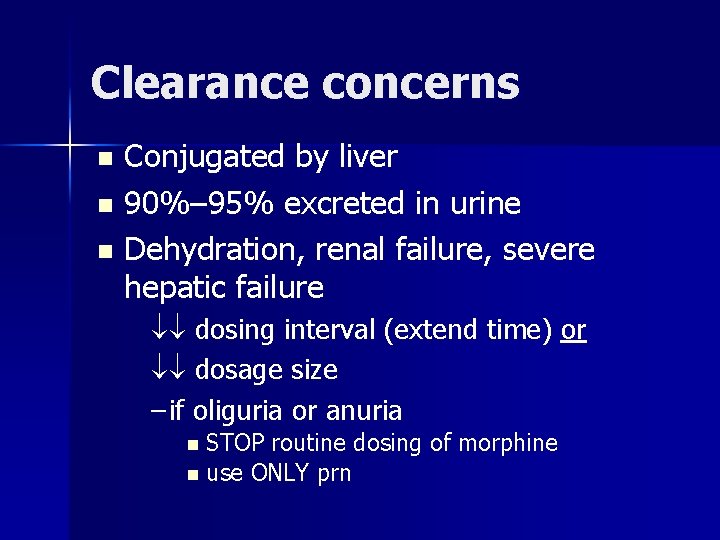
Clearance concerns Conjugated by liver n 90%– 95% excreted in urine n Dehydration, renal failure, severe hepatic failure n dosing interval (extend time) or dosage size – if oliguria or anuria STOP routine dosing of morphine n use ONLY prn n
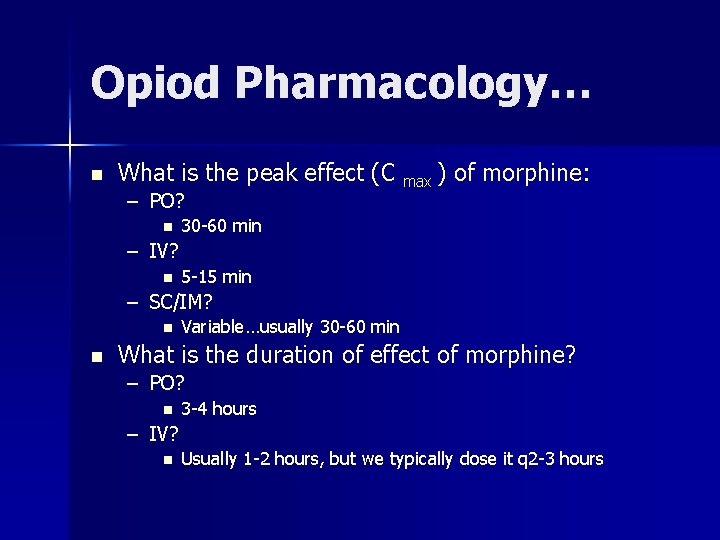
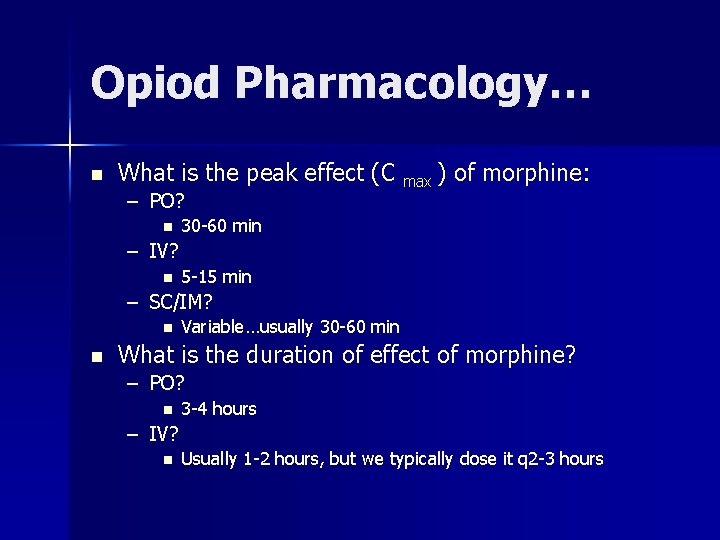
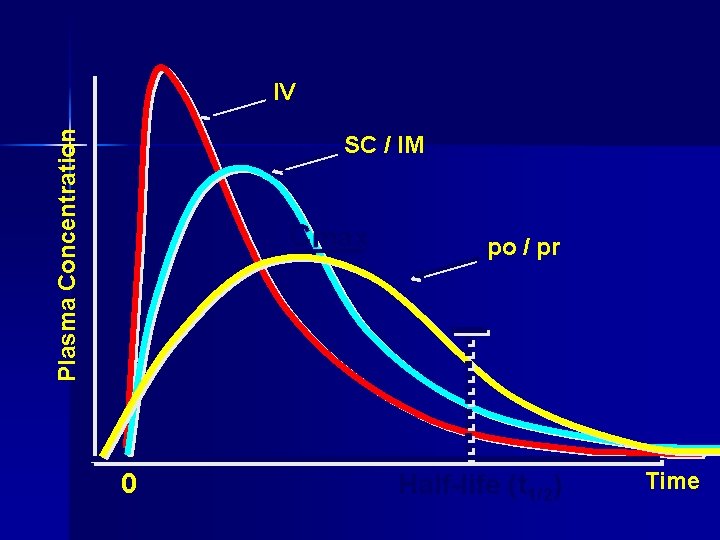
Opiod Pharmacology… n What is the peak effect (C max ) of morphine: – PO? n 30 -60 min – IV? n 5 -15 min – SC/IM? n n Variable…usually 30 -60 min What is the duration of effect of morphine? – PO? n 3 -4 hours – IV? n Usually 1 -2 hours, but we typically dose it q 2 -3 hours
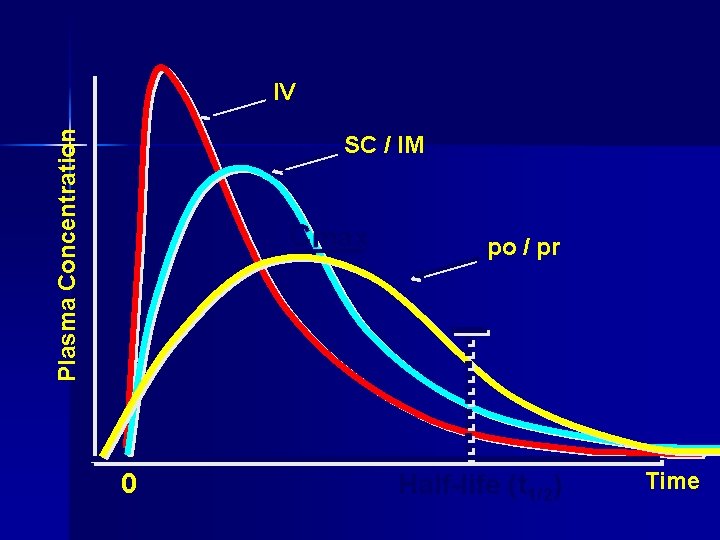
Plasma Concentration IV SC / IM Cmax 0 po / pr Half-life (t 1/2) Time
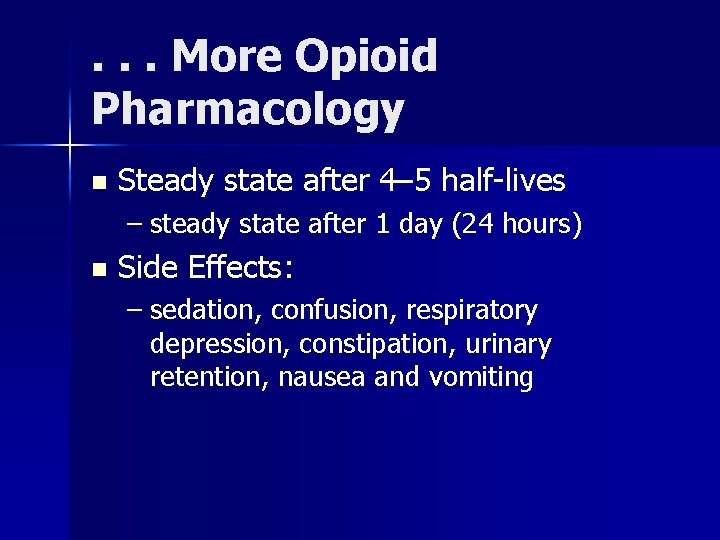
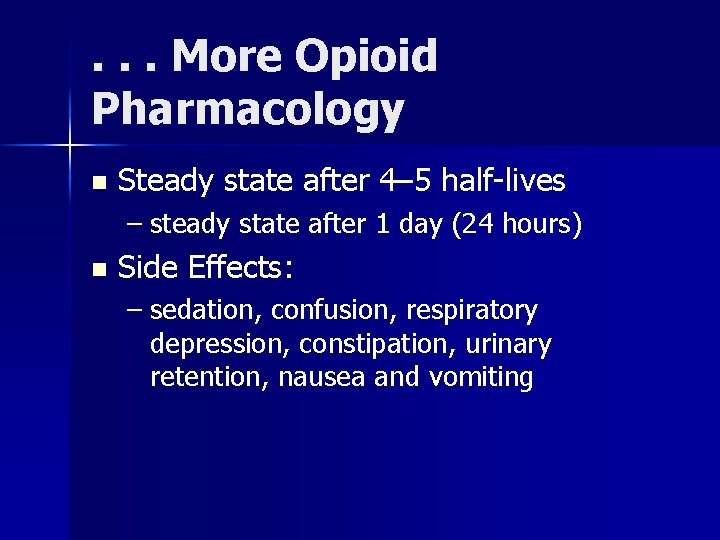
. . . More Opioid Pharmacology n Steady state after 4– 5 half-lives – steady state after 1 day (24 hours) n Side Effects: – sedation, confusion, respiratory depression, constipation, urinary retention, nausea and vomiting
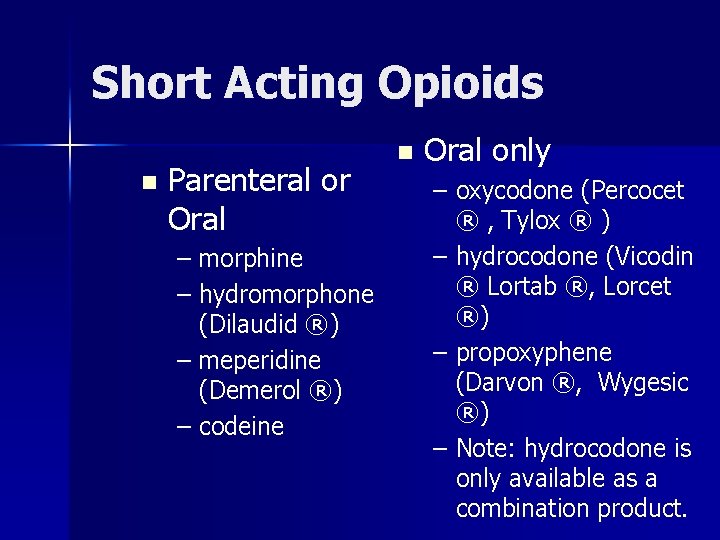
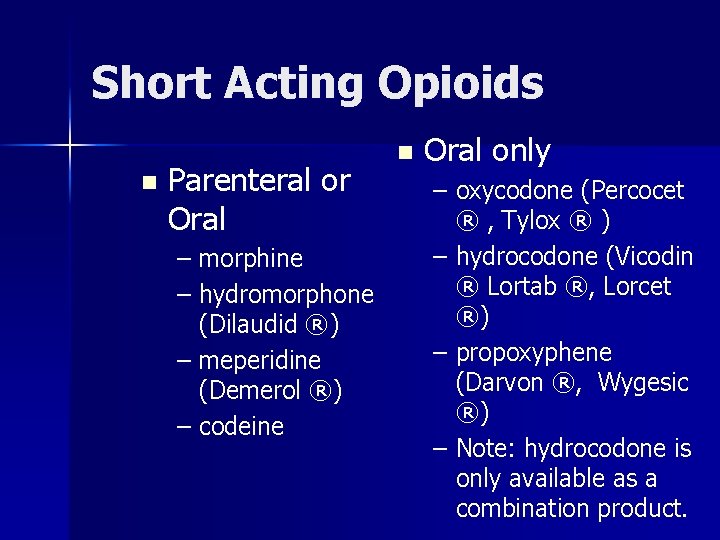
Short Acting Opioids n Parenteral or Oral – morphine – hydromorphone (Dilaudid ®) – meperidine (Demerol ®) – codeine n Oral only – oxycodone (Percocet ® , Tylox ® ) – hydrocodone (Vicodin ® Lortab ®, Lorcet ®) – propoxyphene (Darvon ®, Wygesic ®) – Note: hydrocodone is only available as a combination product.
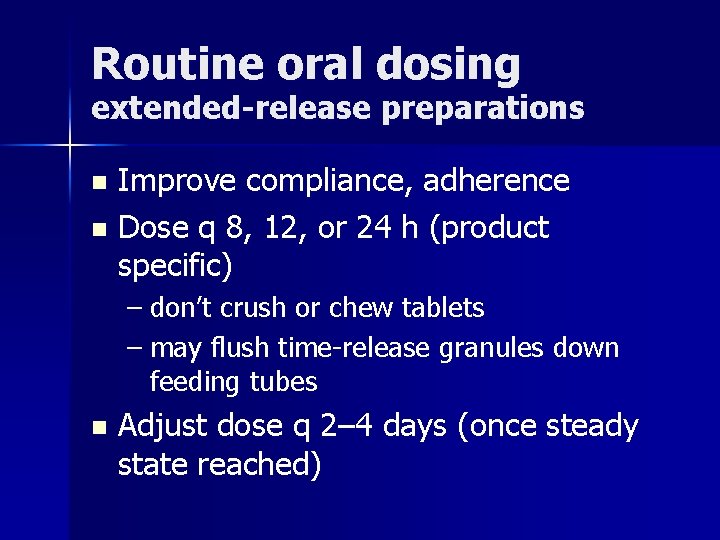
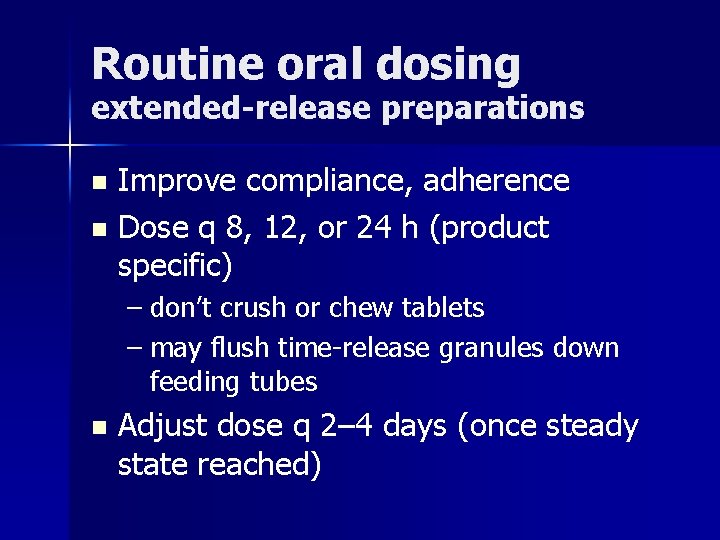
Routine oral dosing extended-release preparations Improve compliance, adherence n Dose q 8, 12, or 24 h (product specific) n – don’t crush or chew tablets – may flush time-release granules down feeding tubes n Adjust dose q 2– 4 days (once steady state reached)
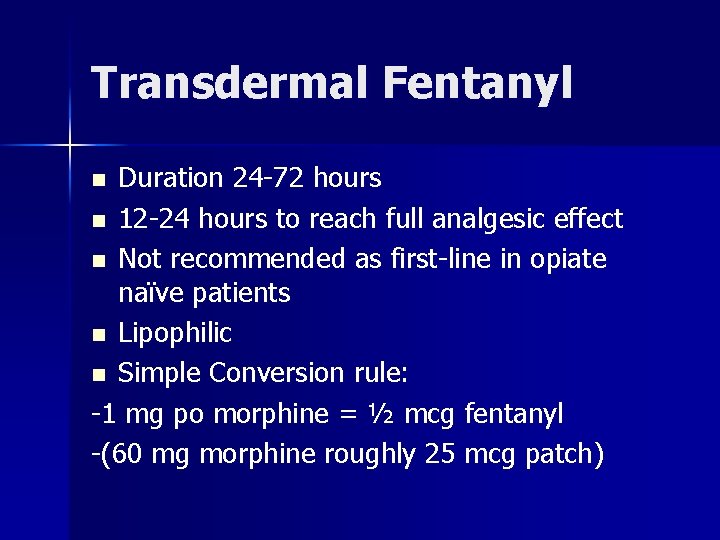
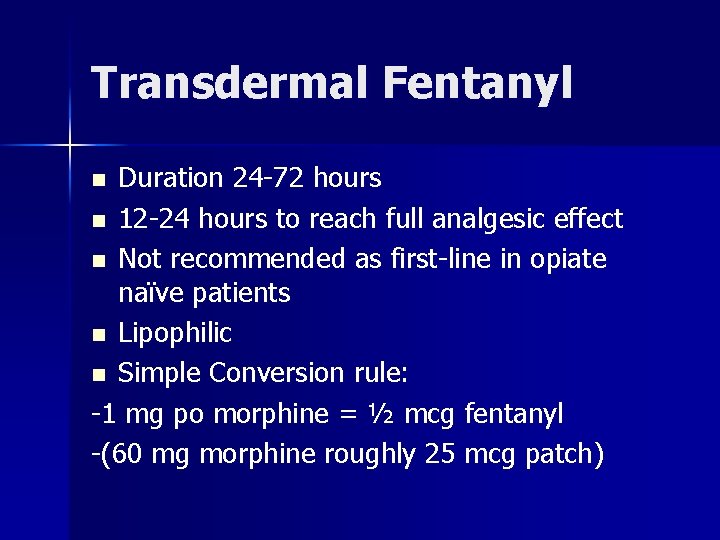
Transdermal Fentanyl Duration 24 -72 hours n 12 -24 hours to reach full analgesic effect n Not recommended as first-line in opiate naïve patients n Lipophilic n Simple Conversion rule: -1 mg po morphine = ½ mcg fentanyl -(60 mg morphine roughly 25 mcg patch) n
DOSE FINDING
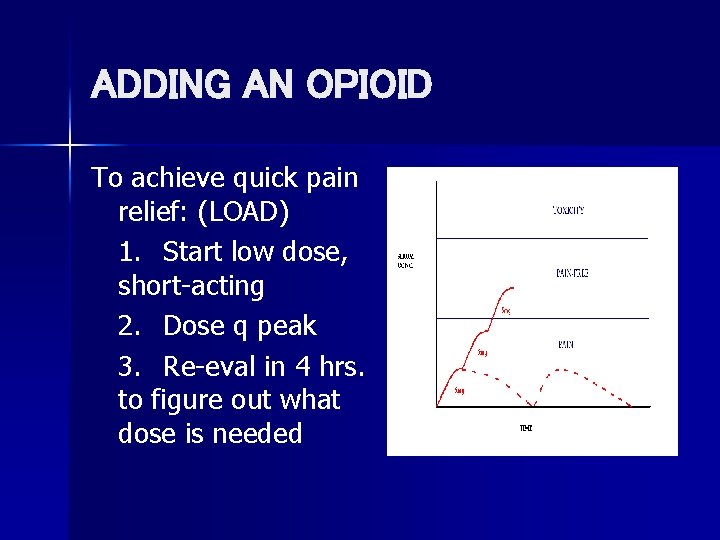
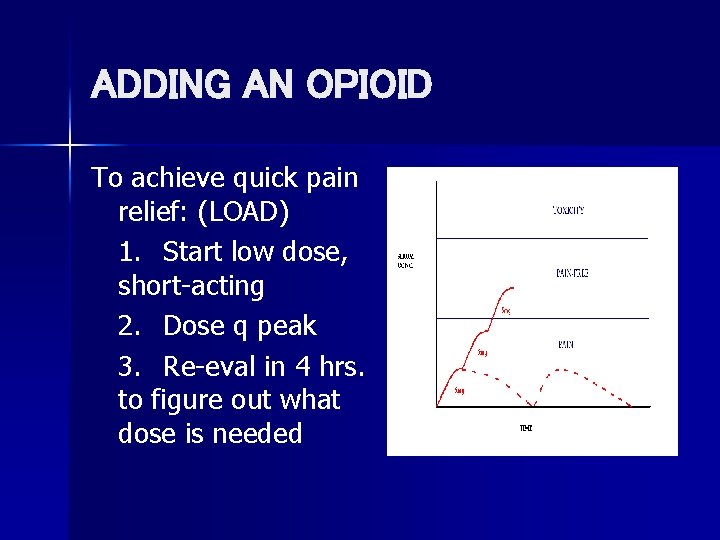
ADDING AN OPIOID To achieve quick pain relief: (LOAD) 1. Start low dose, short-acting 2. Dose q peak 3. Re-eval in 4 hrs. to figure out what dose is needed
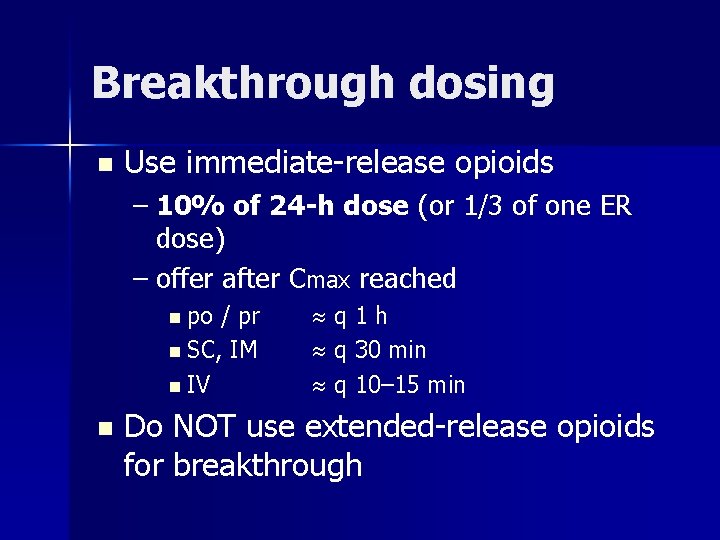
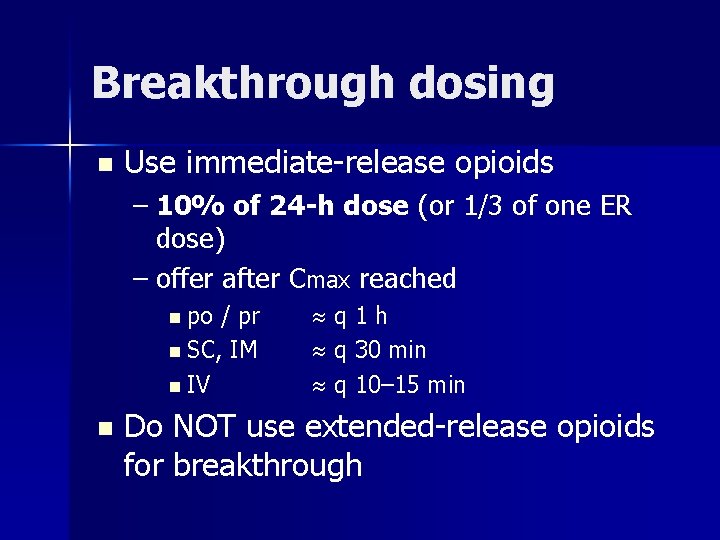
Breakthrough dosing n Use immediate-release opioids – 10% of 24 -h dose (or 1/3 of one ER dose) – offer after Cmax reached n po / pr n SC, IM n IV n q 1 h q 30 min q 10– 15 min Do NOT use extended-release opioids for breakthrough
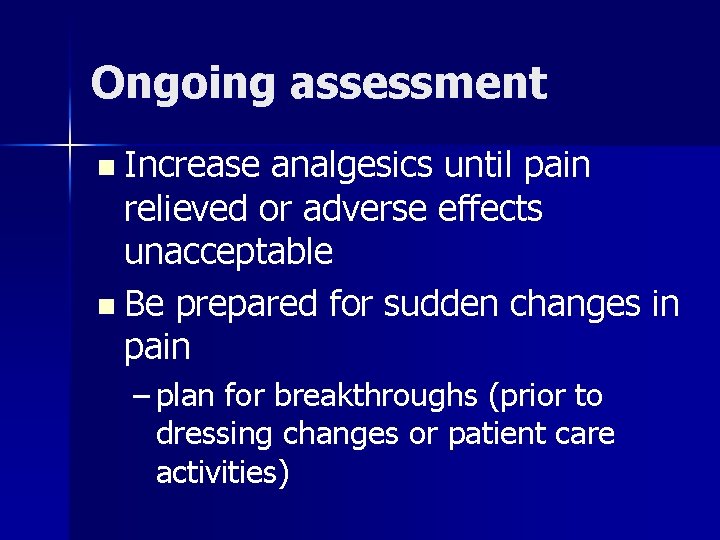
Ongoing assessment n Increase analgesics until pain relieved or adverse effects unacceptable n Be prepared for sudden changes in pain – plan for breakthroughs (prior to dressing changes or patient care activities)
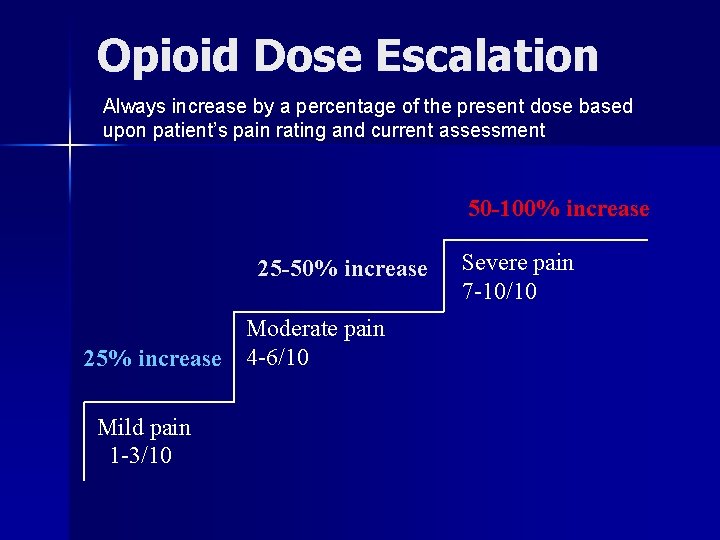
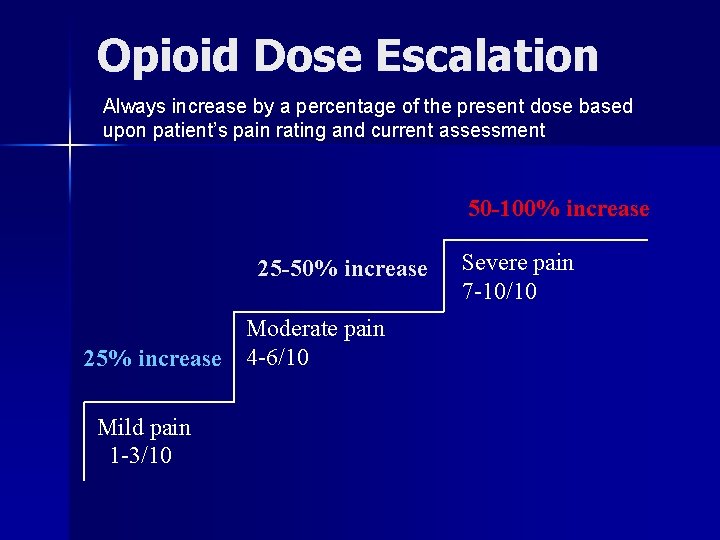
Opioid Dose Escalation Always increase by a percentage of the present dose based upon patient’s pain rating and current assessment 50 -100% increase 25 -50% increase 25% increase Mild pain 1 -3/10 Moderate pain 4 -6/10 Severe pain 7 -10/10
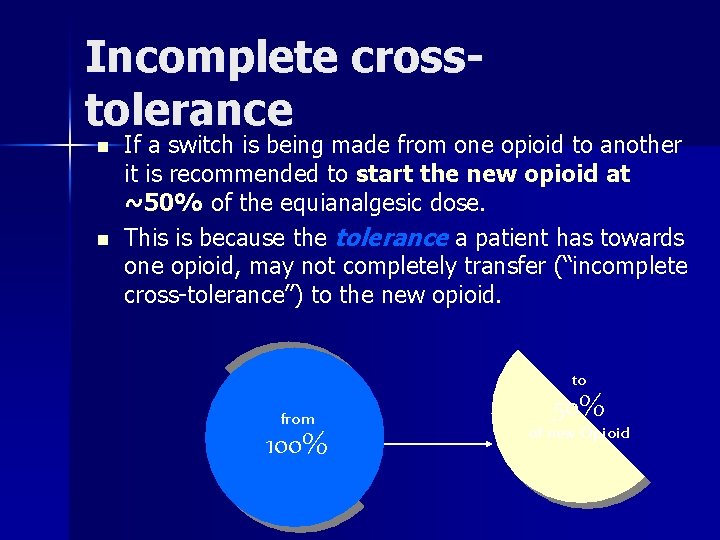
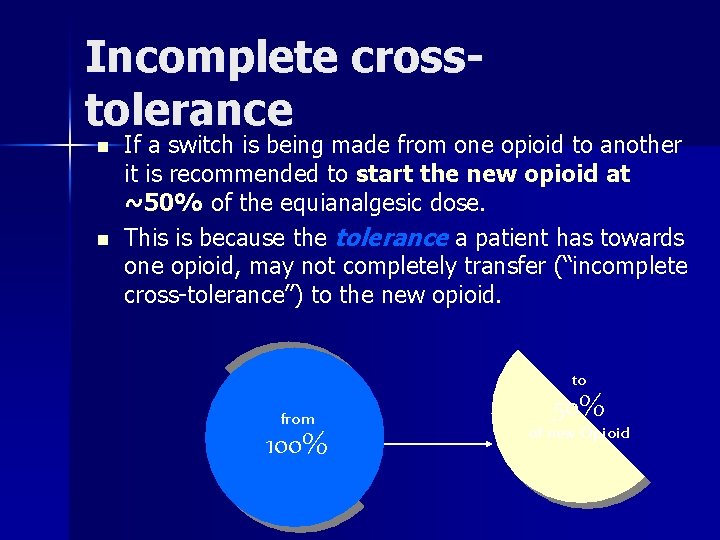
Incomplete crosstolerance n n If a switch is being made from one opioid to another it is recommended to start the new opioid at ~50% of the equianalgesic dose. This is because the tolerance a patient has towards one opioid, may not completely transfer (“incomplete cross-tolerance”) to the new opioid. to from 100% 50% of new Opioid
Pain Problem #1 n You started Mrs. T on 10 mg morphine every 4 hrs around the clock for her cancer pain with good effect. She says she’s tired of taking a pill every 4 hours. Convert her to long-acting morphine with appropriate prn doses.
Pain Problem #1: Answer n 24 hour use: 10 mg PO morphine x 6 = 60 mg PO morphine n Convert to long-acting twice a day dosing: 60 mg PO morphine / 2 = 30 mg PO morphine SR BID n Calculate prn dosing of morphine sulfateimmediate release: 60 mg PO morphine in 24 h x 10% = 6 mg PO morphine q 3 h prn breakthrough pain
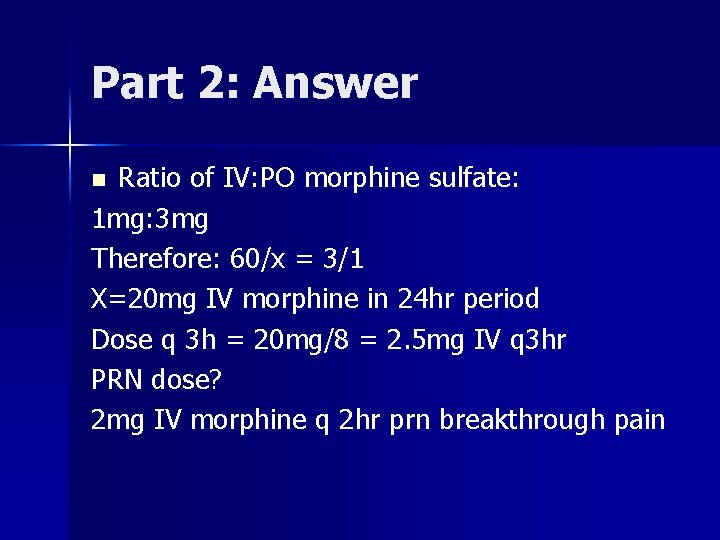
Part 2 n She is admitted to the hospital and unable to take oral medications-convert Mrs. T to: IV morphine
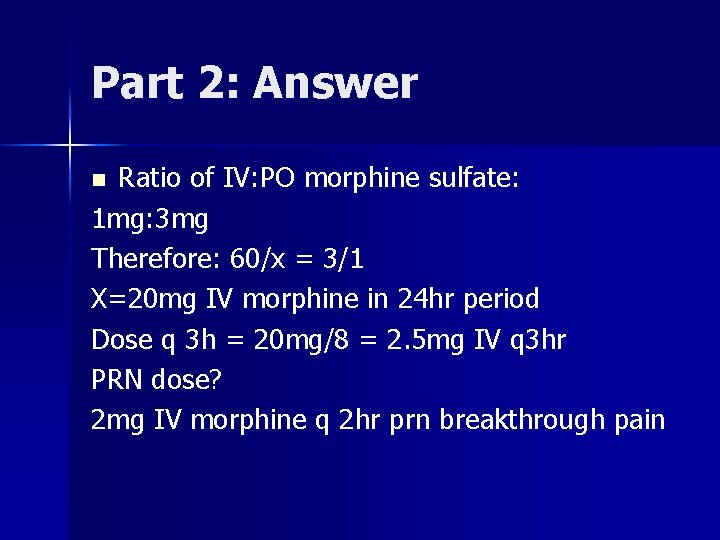
Part 2: Answer Ratio of IV: PO morphine sulfate: 1 mg: 3 mg Therefore: 60/x = 3/1 X=20 mg IV morphine in 24 hr period Dose q 3 h = 20 mg/8 = 2. 5 mg IV q 3 hr PRN dose? 2 mg IV morphine q 2 hr prn breakthrough pain n
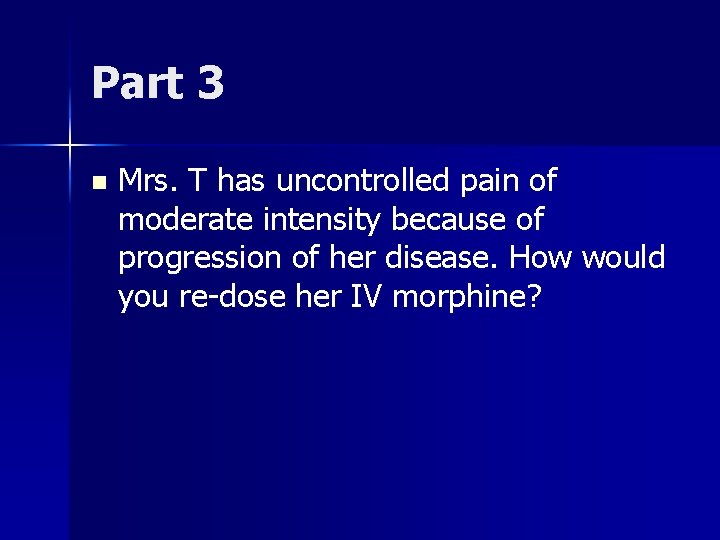
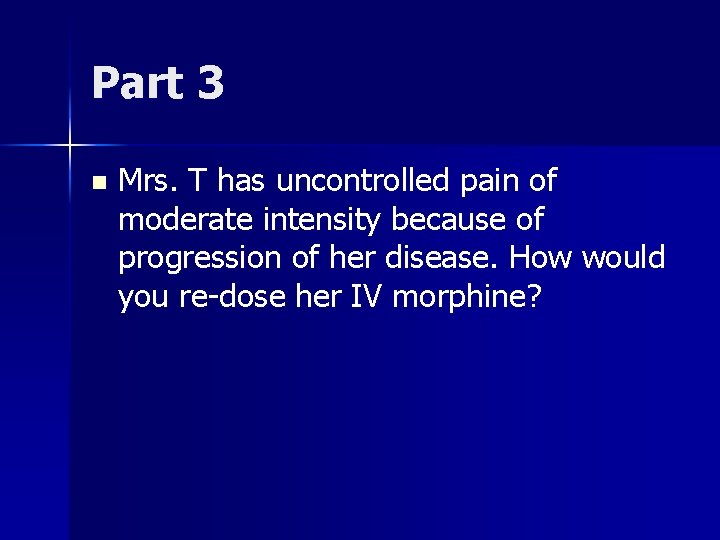
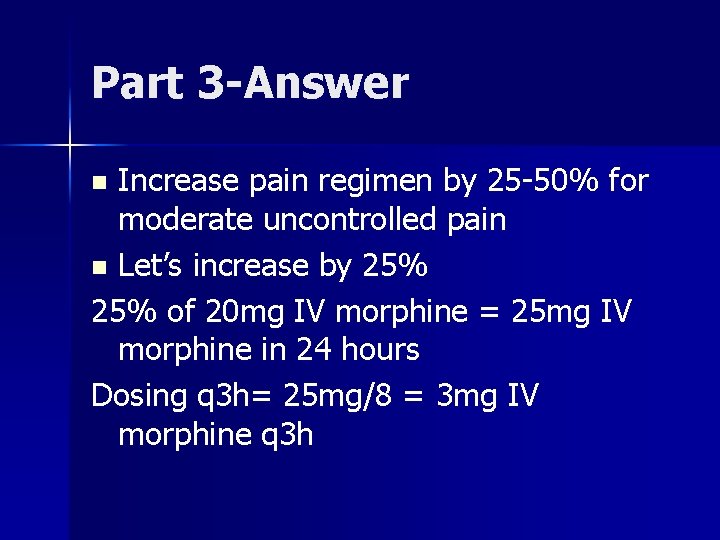
Part 3 n Mrs. T has uncontrolled pain of moderate intensity because of progression of her disease. How would you re-dose her IV morphine?
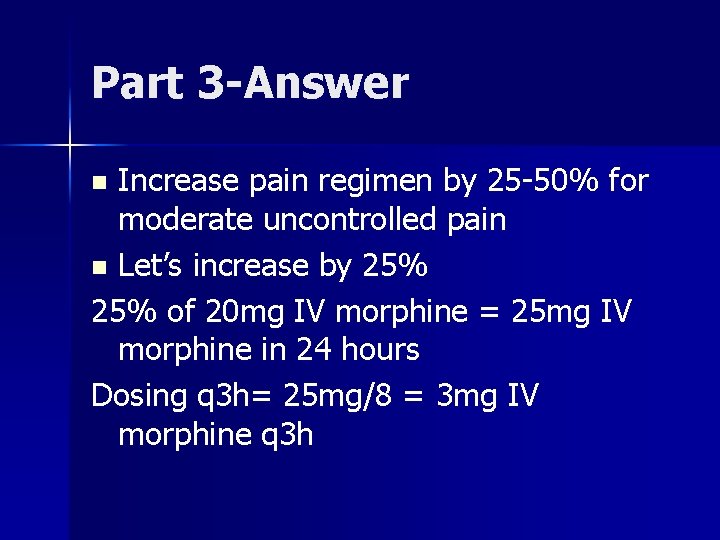
Part 3 -Answer Increase pain regimen by 25 -50% for moderate uncontrolled pain n Let’s increase by 25% of 20 mg IV morphine = 25 mg IV morphine in 24 hours Dosing q 3 h= 25 mg/8 = 3 mg IV morphine q 3 h n
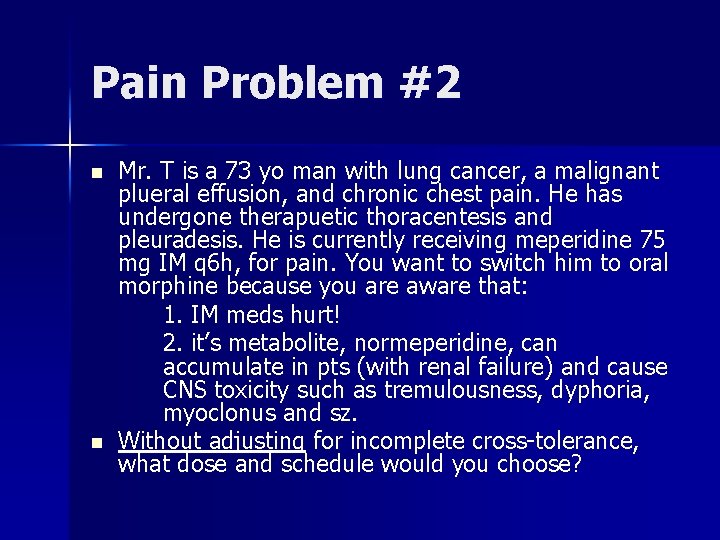
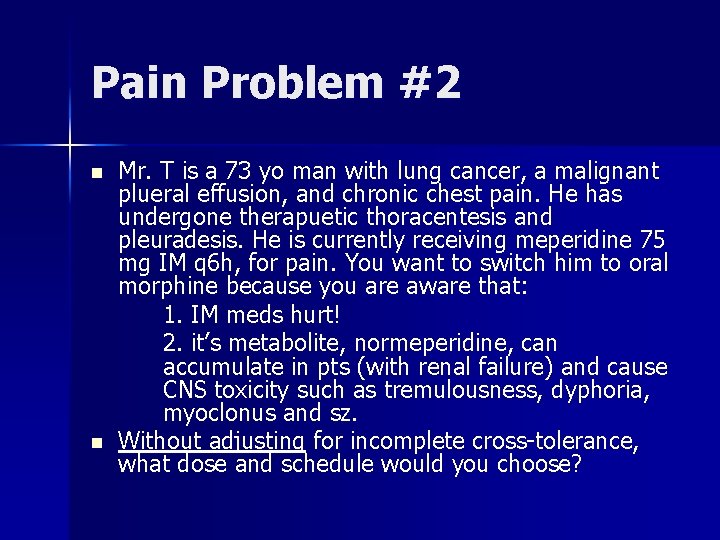
Pain Problem #2 n n Mr. T is a 73 yo man with lung cancer, a malignant plueral effusion, and chronic chest pain. He has undergone therapuetic thoracentesis and pleuradesis. He is currently receiving meperidine 75 mg IM q 6 h, for pain. You want to switch him to oral morphine because you are aware that: 1. IM meds hurt! 2. it’s metabolite, normeperidine, can accumulate in pts (with renal failure) and cause CNS toxicity such as tremulousness, dyphoria, myoclonus and sz. Without adjusting for incomplete cross-tolerance, what dose and schedule would you choose?
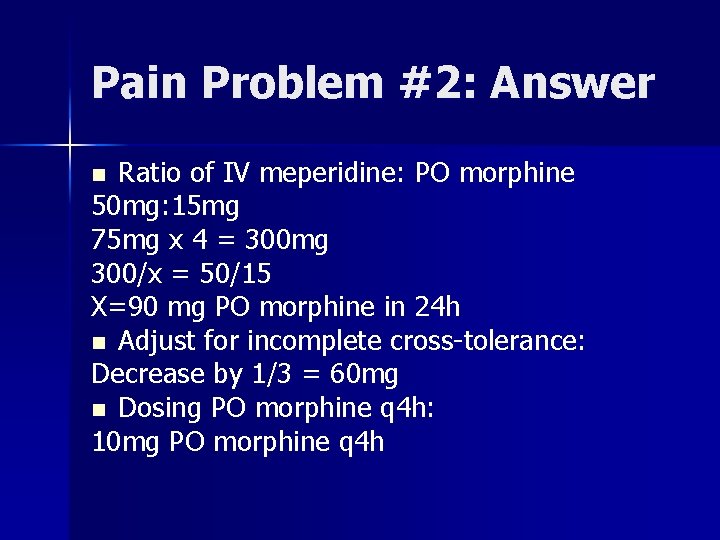
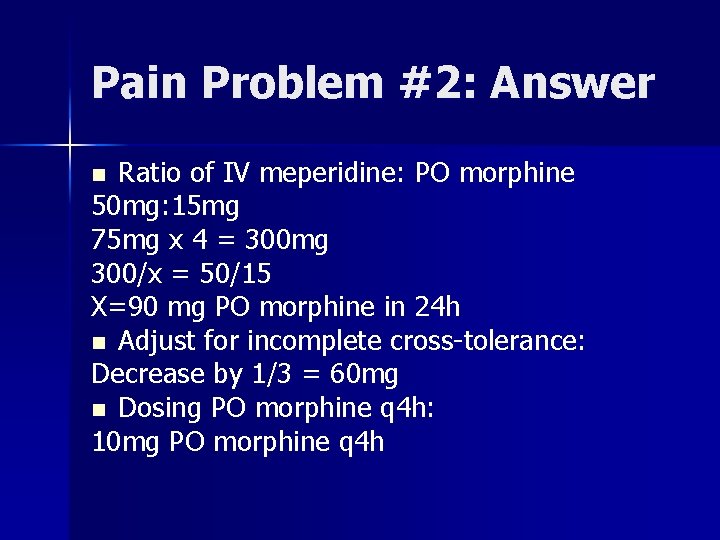
Pain Problem #2: Answer Ratio of IV meperidine: PO morphine 50 mg: 15 mg 75 mg x 4 = 300 mg 300/x = 50/15 X=90 mg PO morphine in 24 h n Adjust for incomplete cross-tolerance: Decrease by 1/3 = 60 mg n Dosing PO morphine q 4 h: 10 mg PO morphine q 4 h n
 Sas scale
Sas scale Madpain
Madpain Can you feel like your period is coming and be pregnant
Can you feel like your period is coming and be pregnant Period vs pregnancy
Period vs pregnancy Pqrst pain assessment
Pqrst pain assessment Painad
Painad Pqrstu pain
Pqrstu pain Capa pain assessment tool
Capa pain assessment tool Unpleasant sensory and emotional experience
Unpleasant sensory and emotional experience Neonatal infant pain scale
Neonatal infant pain scale Comprehensive pain assessment
Comprehensive pain assessment Comprehensive pain assessment
Comprehensive pain assessment Pqrstu pain assessment
Pqrstu pain assessment Oldcart
Oldcart Jarvis chapter 11 pain assessment
Jarvis chapter 11 pain assessment Palliative care programme
Palliative care programme Akps score
Akps score Palliative care programme
Palliative care programme Principles of palliative care
Principles of palliative care Palliative care versus hospice care
Palliative care versus hospice care Palliative care in nepal
Palliative care in nepal Pps scale hospice
Pps scale hospice Criterios de terminalidad
Criterios de terminalidad Palliative care assistant
Palliative care assistant European certificate in essential palliative care
European certificate in essential palliative care Parallel planning palliative care
Parallel planning palliative care Adjuvant neoadjuvant palliative
Adjuvant neoadjuvant palliative Franciscan palliative care
Franciscan palliative care Traduzione
Traduzione Nucot cos'è
Nucot cos'è Pcqc
Pcqc Antiemetic pediatric dose
Antiemetic pediatric dose Just in case bag palliative care
Just in case bag palliative care Amber care bundle nice
Amber care bundle nice Goscote palliative care centre
Goscote palliative care centre Palliative care at home barry
Palliative care at home barry Palliative prognostic index
Palliative prognostic index Hospice of the bluegrass frankfort ky
Hospice of the bluegrass frankfort ky Provocative/palliative
Provocative/palliative Calvary palliative care kogarah
Calvary palliative care kogarah Anorexia, nausea and vomiting
Anorexia, nausea and vomiting Palliative care matters
Palliative care matters Anorexia cachexia palliative care
Anorexia cachexia palliative care Goc palliative care
Goc palliative care Npcrc
Npcrc European delirium association
European delirium association Palliative fase
Palliative fase Anergia definition
Anergia definition Textbook of palliative care communication
Textbook of palliative care communication Palliative xrt definition
Palliative xrt definition Oacc palliative care
Oacc palliative care Ethical issues in palliative care
Ethical issues in palliative care Pam document for hod
Pam document for hod Pain management okc soonercare
Pain management okc soonercare Pico format question
Pico format question Pain management stony brook
Pain management stony brook