Respiratory Paediatrics For GPs Dr Jennifer Townshend Consultant


- Slides: 63
Respiratory Paediatrics For GP’s Dr. Jennifer Townshend Consultant Paediatrician
Overview � Context � Some common presentations � Common complains ◦ Wheezy infant ◦ Wheezy child ◦ Chronic cough
Blue background slides Audience participation
Is it important? � Respiratory distress is the most common complaint for which children seek medical care. � Up to 10% of children have a persistent cough at any one time � 1/3 of 1 -5 year olds suffer recurrent wheeze
A familiar case? � 9 year old boy � Diagnosed with asthma 4 years ago � Never free from symptoms � Ends up in hospital about once per year � Nothing seems to be working
What are your thoughts? � What do you want to know? � What else could be going on?
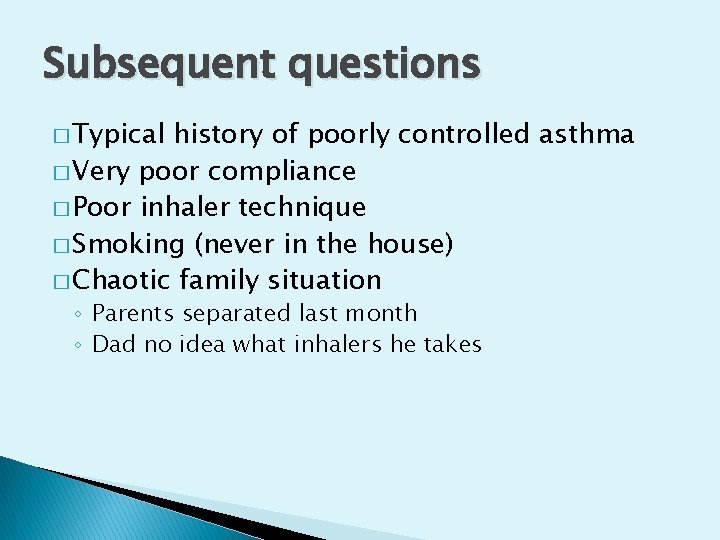
Subsequent questions � Typical history of poorly controlled asthma � Very poor compliance � Poor inhaler technique � Smoking (never in the house) � Chaotic family situation ◦ Parents separated last month ◦ Dad no idea what inhalers he takes
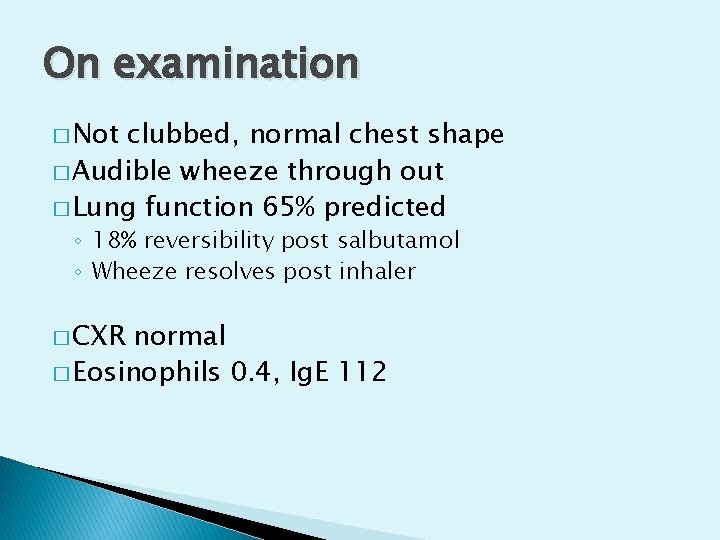
On examination � Not clubbed, normal chest shape � Audible wheeze through out � Lung function 65% predicted ◦ 18% reversibility post salbutamol ◦ Wheeze resolves post inhaler � CXR normal � Eosinophils 0. 4, Ig. E 112
What is the likely diagnosis? � Poorly controlled atopic asthma
Are you concerned? � RF ◦ ◦ for life threatening disease Poor compliance Poor technique Chaotic social situation Parental smoking, risk of child smoking
Another familiar case? � 18 month old girl ‘There’s something wrong with my child – she picks up everything. I think its her immune system’ ‘She’s always chesty, and pants with her breathing’ ‘This has been going on for as long as I can remember…. . ’
What do you think? � What else do you want to know? � What could be going on?
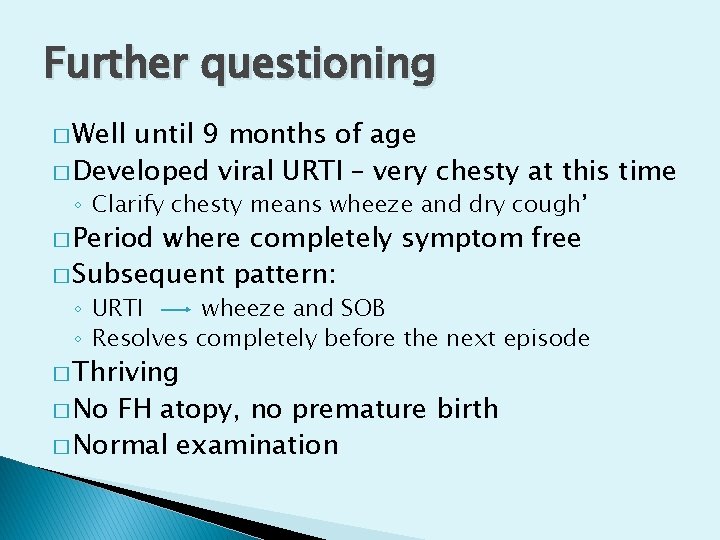
Further questioning � Well until 9 months of age � Developed viral URTI – very chesty at this time ◦ Clarify chesty means wheeze and dry cough’ � Period where completely symptom free � Subsequent pattern: ◦ URTI wheeze and SOB ◦ Resolves completely before the next episode � Thriving � No FH atopy, no premature birth � Normal examination
What is the likely diagnosis? � Episodic viral wheeze
Wheeze
Wheeze � What is it?
Wheeze � What is it? ‘a continuous high pitched musical sound emitting from the chest in expiration as a result of narrowing of the small airways’
Wheeze � Where does it come from? ◦ Closed cavity ◦ Relationship between pressure and volume
Wheeze � What causes it? • All that wheezes is not asthma……. .
Alerting symptom/Sign Possible diagnosis Clinical Clue
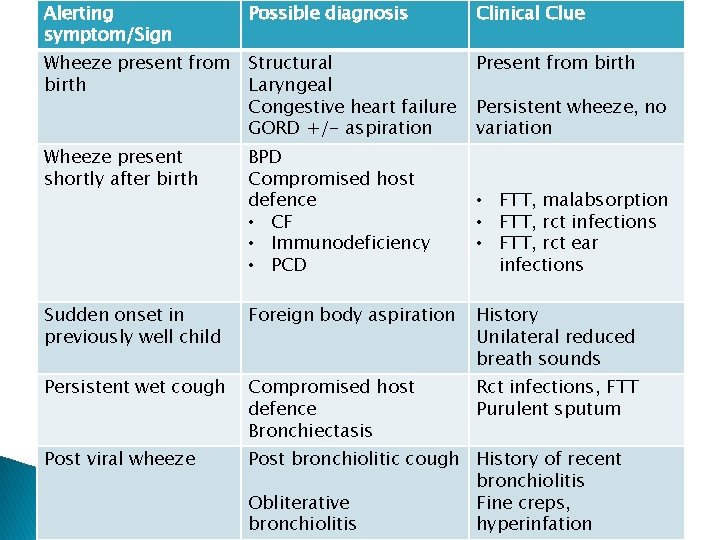
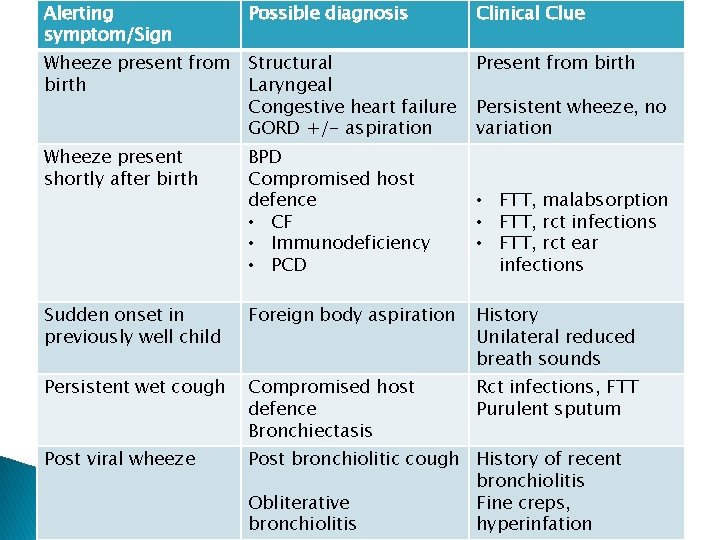
Alerting symptom/Sign Possible diagnosis Clinical Clue Wheeze present from birth Structural Laryngeal Congestive heart failure GORD +/- aspiration Present from birth Wheeze present shortly after birth BPD Compromised host defence • CF • Immunodeficiency • PCD Sudden onset in previously well child Foreign body aspiration History Unilateral reduced breath sounds Persistent wet cough Compromised host defence Bronchiectasis Rct infections, FTT Purulent sputum Post viral wheeze Post bronchiolitic cough History of recent bronchiolitis Obliterative Fine creps, bronchiolitis hyperinfation Persistent wheeze, no variation • FTT, malabsorption • FTT, rct infections • FTT, rct ear infections
Asthma phenotypes � Asthma more complex, especially in children � Different patterns of illness having different underlying pathogenesis � Different phenotypes have different management strategies and different prognosis
Atopic Asthma � Most commonly recognised phenotype � Classical characteristics
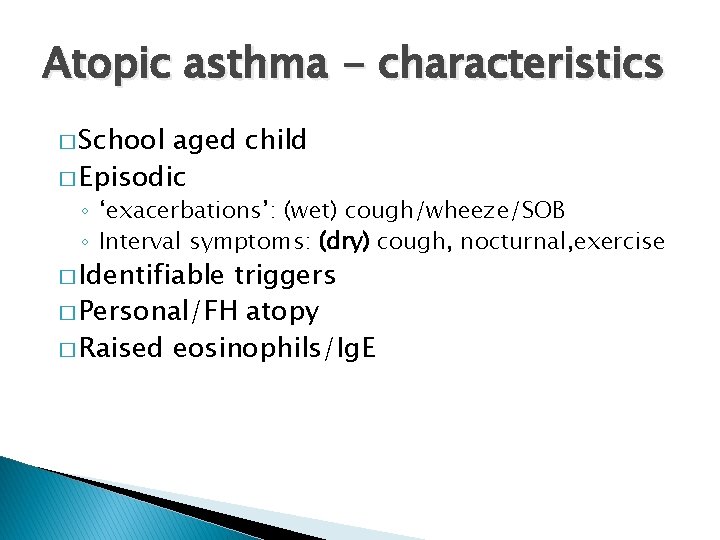
Atopic asthma - characteristics � School aged child � Episodic ◦ ‘exacerbations’: (wet) cough/wheeze/SOB ◦ Interval symptoms: (dry) cough, nocturnal, exercise � Identifiable triggers � Personal/FH atopy � Raised eosinophils/Ig. E
What about cough varient asthma? � Very rare to (Mc. Kenzie, 1994) cough without wheeze in asthma � More likely to be a marker for another condition � But, does exist – consider trial of asthma therapy if all other conditions excluded
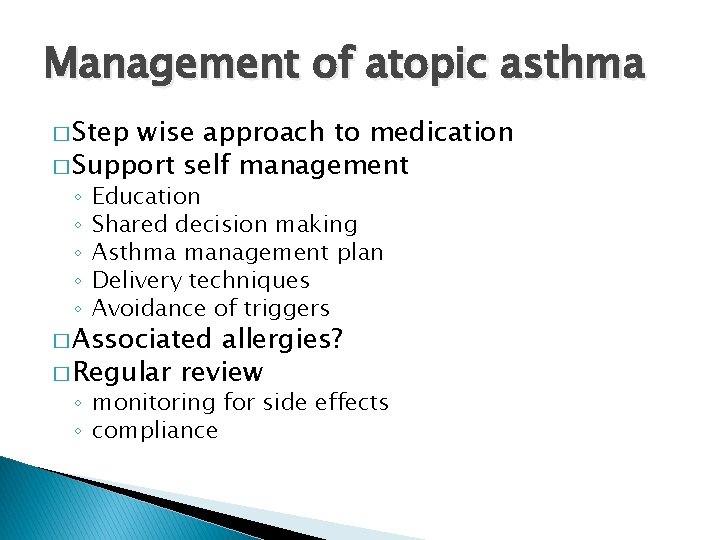
Management of atopic asthma � Step wise approach to medication � Support self management ◦ ◦ ◦ Education Shared decision making Asthma management plan Delivery techniques Avoidance of triggers � Associated allergies? � Regular review ◦ monitoring for side effects ◦ compliance
A few things to mention � Inhaled corticosteroids ◦ Friend? Foe? Practically? � Long acting beta agonists ◦ Better then doubling dose of ICS ◦ But safe? ?
Atopic asthma – when to refer � Many variables � Secondary or tertiary?
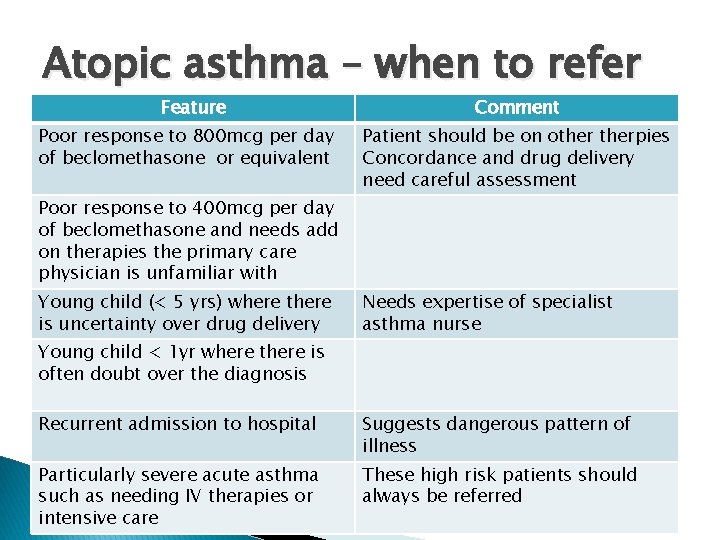
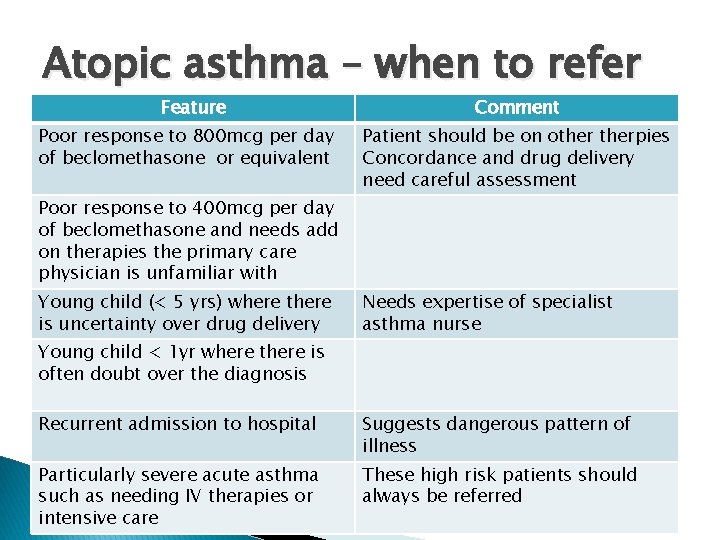
Atopic asthma – when to refer Feature Poor response to 800 mcg per day of beclomethasone or equivalent Comment Patient should be on otherpies Concordance and drug delivery need careful assessment Poor response to 400 mcg per day of beclomethasone and needs add on therapies the primary care physician is unfamiliar with Young child (< 5 yrs) where there is uncertainty over drug delivery Needs expertise of specialist asthma nurse Young child < 1 yr where there is often doubt over the diagnosis Recurrent admission to hospital Suggests dangerous pattern of illness Particularly severe acute asthma such as needing IV therapies or intensive care These high risk patients should always be referred
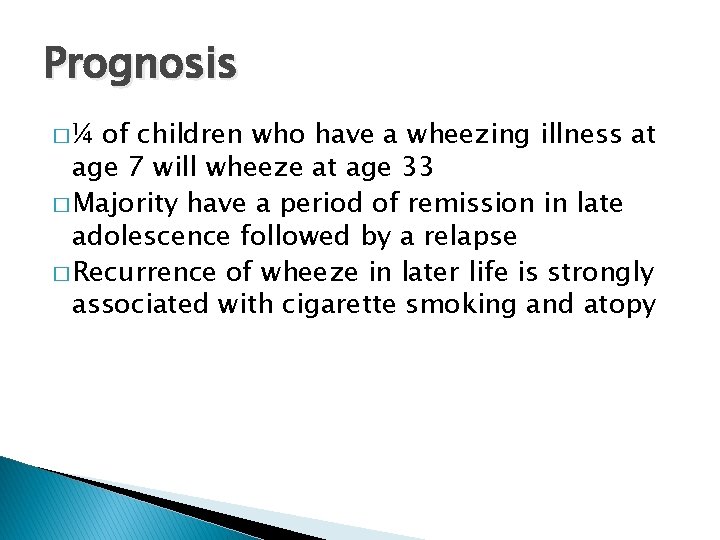
Prognosis �¼ of children who have a wheezing illness at age 7 will wheeze at age 33 � Majority have a period of remission in late adolescence followed by a relapse � Recurrence of wheeze in later life is strongly associated with cigarette smoking and atopy
Asthma phenotypes (2) � Atopic Asthma � Episodic viral wheeze ‘the wheezing infant’
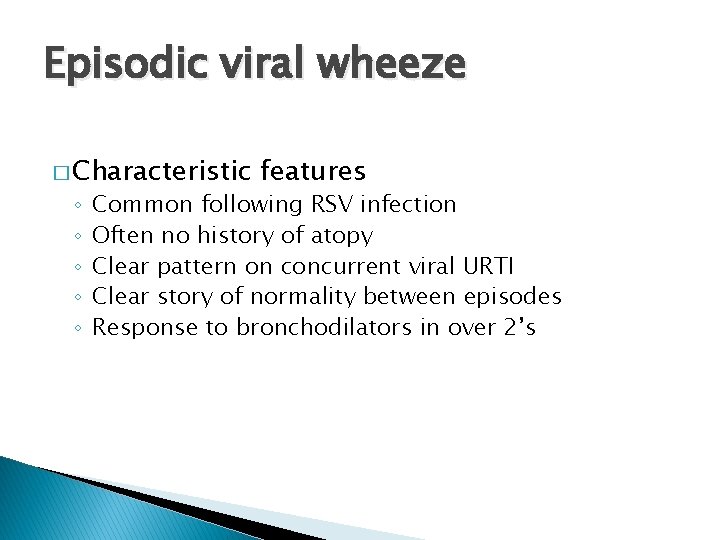
Episodic viral wheeze � Characteristic ◦ ◦ ◦ features Common following RSV infection Often no history of atopy Clear pattern on concurrent viral URTI Clear story of normality between episodes Response to bronchodilators in over 2’s
Episodic viral wheeze � Risk factors for development into atopic phenotype ◦ ◦ FH/personal history of atopy Premature birth/low birth weight Smoking Bronchiolitis as an infant
Different phenotypes – so what? � Acute management ◦ Salbutamol in under 2’s ◦ Corticosteroids � Long term management � Prognosis
Episodic Viral Wheeze – prognosis � 30 -50% of children have one episode � 66% out grow their symptoms before school age � Atopic asthma can start with EVW but often have atopic phenotype and/or FH
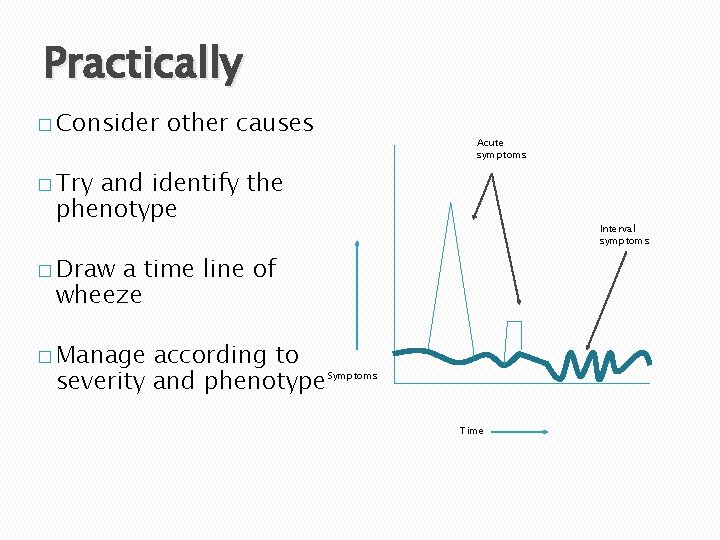
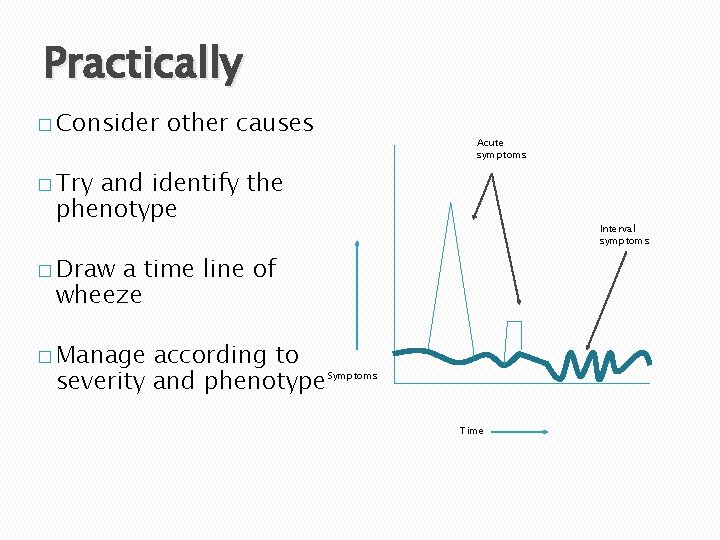
Practically � Consider other causes Acute symptoms � Try and identify the phenotype Interval symptoms � Draw a time line of wheeze � Manage according to severity and phenotype Symptoms Time
Some more cases…. . � 11 year old boy � Presented ‘exacerbation of asthma’ � Difficult to control asthma for years � Primary symptom is cough ◦ Wet ◦ Every day ◦ No real relief from inhalers � Some mild SOB, no real wheeze
What are your thoughts? � What else do you want to know?
Further questioning � No FH of atopy � No personal history of atopy � No smoking in family � Always hungry, but still slim
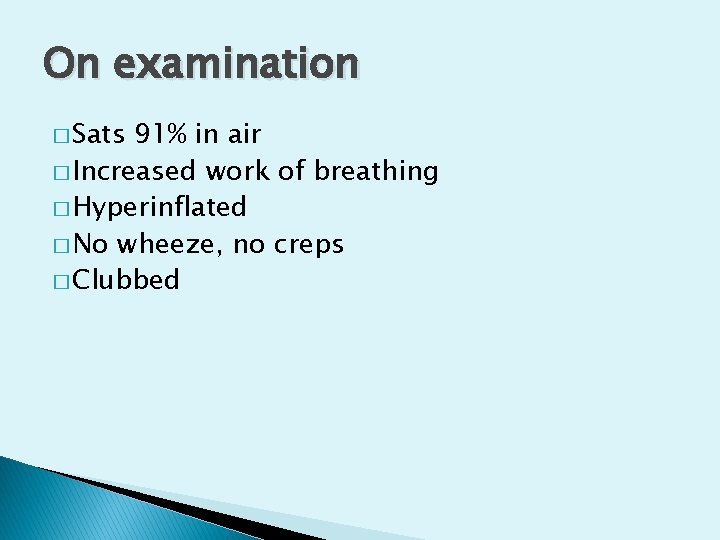
On examination � Sats 91% in air � Increased work of breathing � Hyperinflated � No wheeze, no creps � Clubbed
� CXR: chronic changes � Sweat test – confirmed Cystic fibrosis
Case 2 � 18 month old child � Well until 13 months � ‘Never been right since’ � Coughs every day, no break in between
Further questioning � Started nursery at 13 months � Recurrent episodes of runny nose � Wet cough associated with runny nose � Cough beginning to recede after a few weeks � Then further runny nose and cough starts again � Thriving
On examination � Well child � Nasal crusting � Wet cough � Normal chest shape � Chest clear to auscultation � Recurrent � Reassure � Reassess viral URTI’s in summer months

Cough � Important � Common � OTC physiological reflex (up to 10% children) medicine – cochrane review
Different cough types � Acute cough � Recurrent acute cough � Persistent none remitting cough
Acute cough (< 3 weeks ) � Vast majority viral URTI � History and examination important to rule out chronic illness � Consider ◦ ◦ Pertussis Allergy Inhaled foreign body Rarely – presenting feature of serious underlying disorder
When to consider CXR/Referral � Uncertainty � IFB � Possible about diagnosis of pneumonia chronic problem � Prolonged clinical course � True haemoptysis
How to manage acute cough � Antipyretics and fluids as required � Antibiotics not beneficial in absence of signs of pneumonia � Bronchodilators not helpful in children who don’t have asthma � OTC remedies not effective � Macrolide for pertussis � EXPLANATION – reduce future consultations
Chronic cough � Chronic cough > 8 weeks � 3 -8 weeks ‘grey area’ ◦ Subacute (post viral) ◦ Pertussis
Differential � Structural � Immunodeficiency � Suppurative (PBB, bronchiectasis) � Recurrent aspiration � Pertussis � Retained IFB � TB � Bronchcospasm � Intersitial lung disease/cardiac
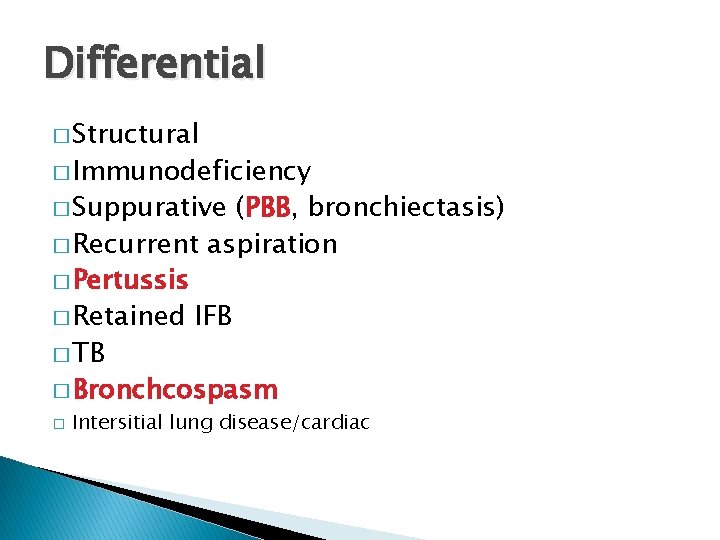
Differential � Structural � Immunodeficiency � Suppurative (PBB, bronchiectasis) � Recurrent aspiration � Pertussis � Retained IFB � TB � Bronchcospasm � Intersitial lung disease/cardiac
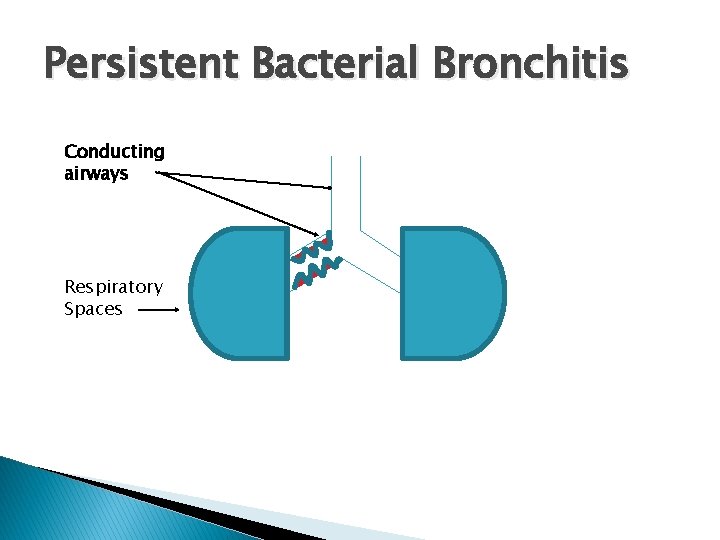
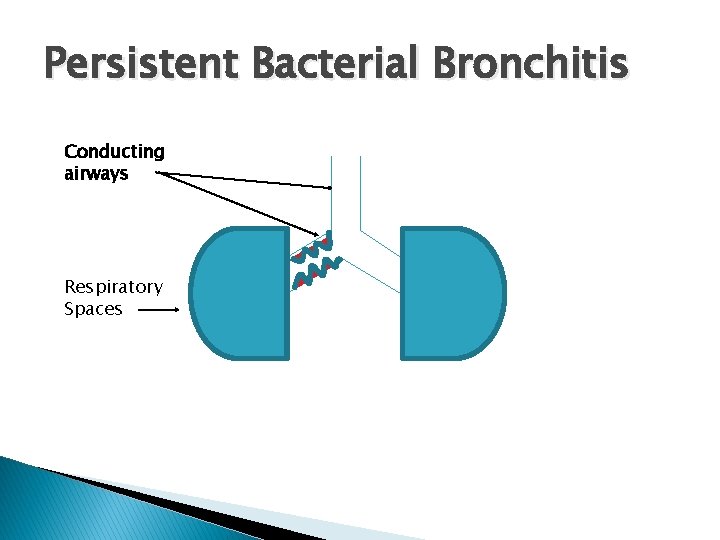
Persistent Bacterial Bronchitis Conducting airways Respiratory Spaces
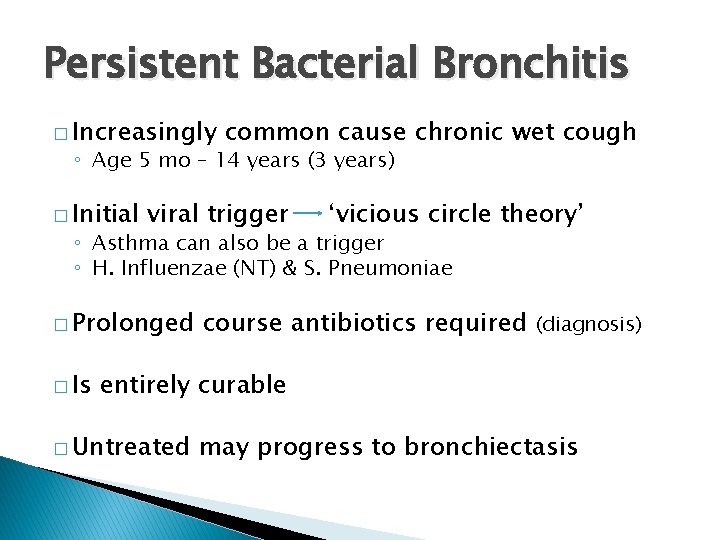
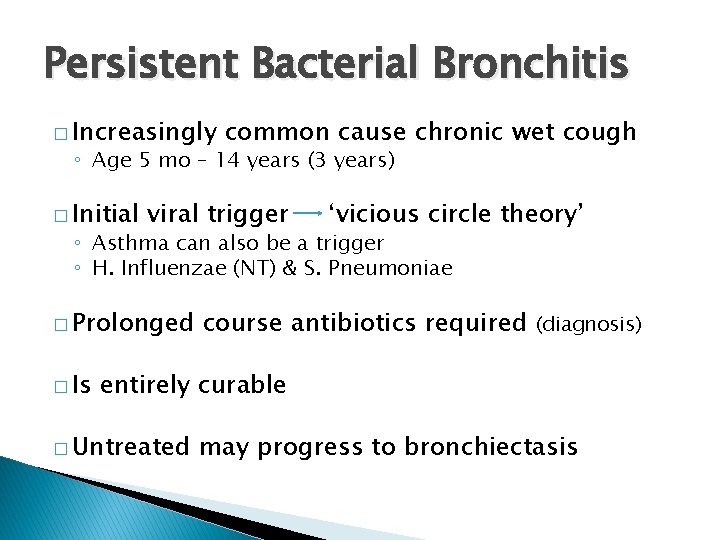
Persistent Bacterial Bronchitis � Increasingly common cause chronic wet cough ◦ Age 5 mo – 14 years (3 years) � Initial viral trigger ‘vicious circle theory’ ◦ Asthma can also be a trigger ◦ H. Influenzae (NT) & S. Pneumoniae � Prolonged � Is course antibiotics required (diagnosis) entirely curable � Untreated may progress to bronchiectasis
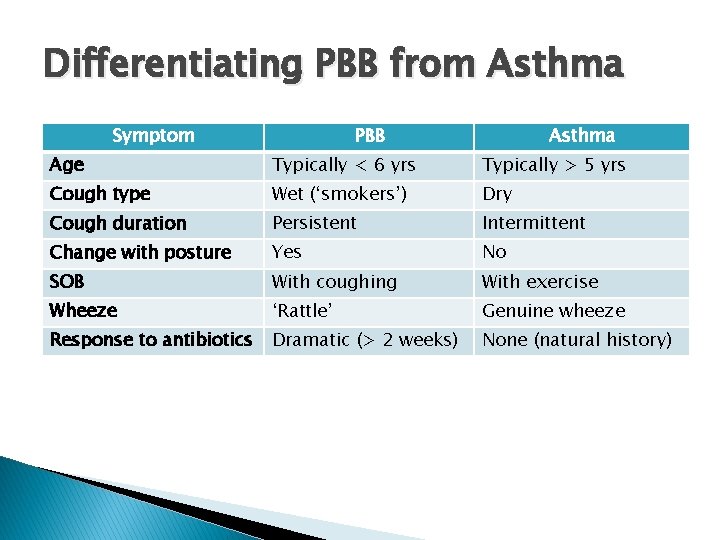
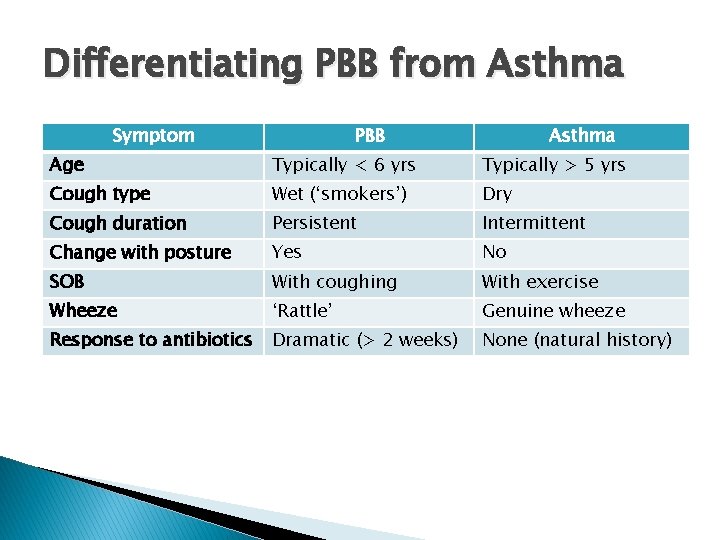
Differentiating PBB from Asthma Symptom PBB Asthma Age Typically < 6 yrs Typically > 5 yrs Cough type Wet (‘smokers’) Dry Cough duration Persistent Intermittent Change with posture Yes No SOB With coughing With exercise Wheeze ‘Rattle’ Genuine wheeze Response to antibiotics Dramatic (> 2 weeks) None (natural history)
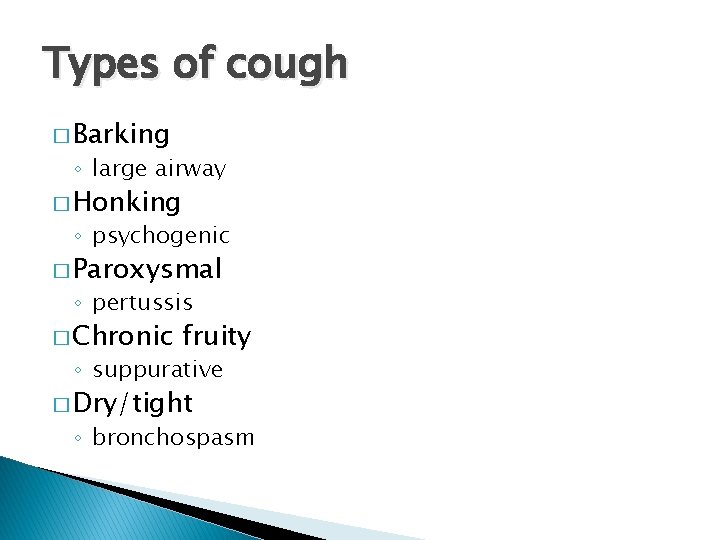
Assessment � Consider different types of cough
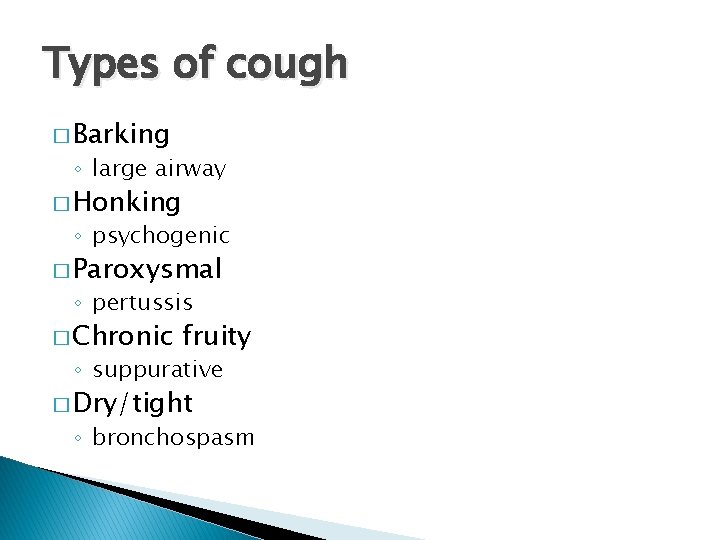
Types of cough � Barking ◦ large airway � Honking ◦ psychogenic � Paroxysmal ◦ pertussis � Chronic fruity ◦ suppurative � Dry/tight ◦ bronchospasm
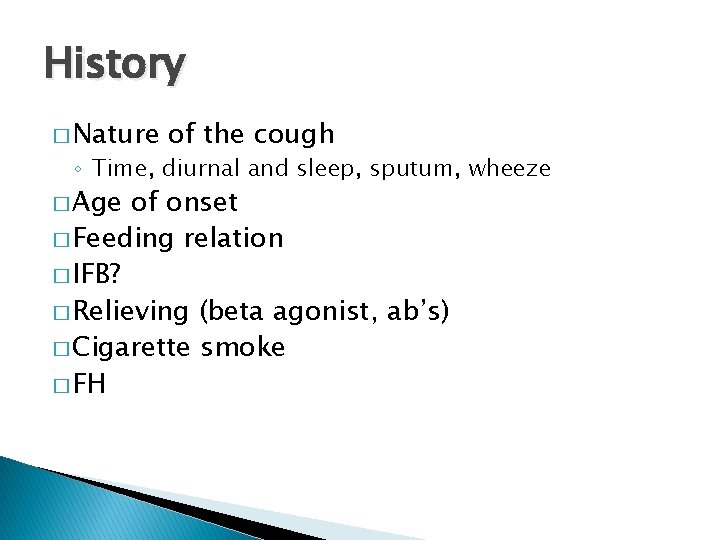
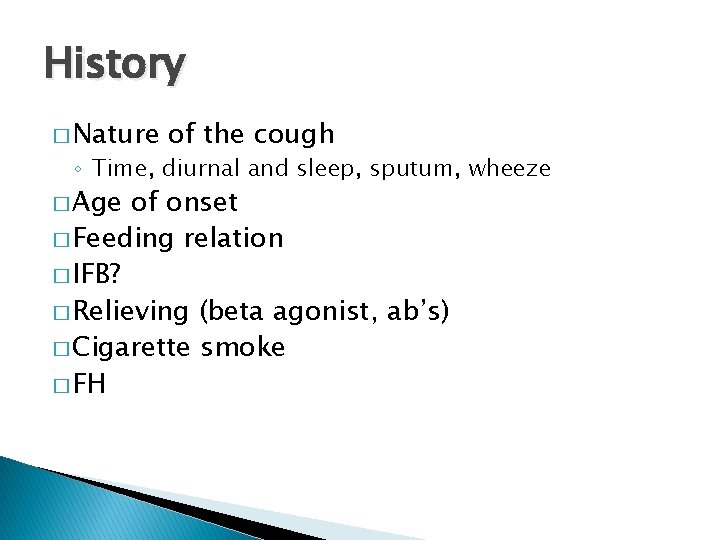
History � Nature of the cough ◦ Time, diurnal and sleep, sputum, wheeze � Age of onset � Feeding relation � IFB? � Relieving (beta agonist, ab’s) � Cigarette smoke � FH

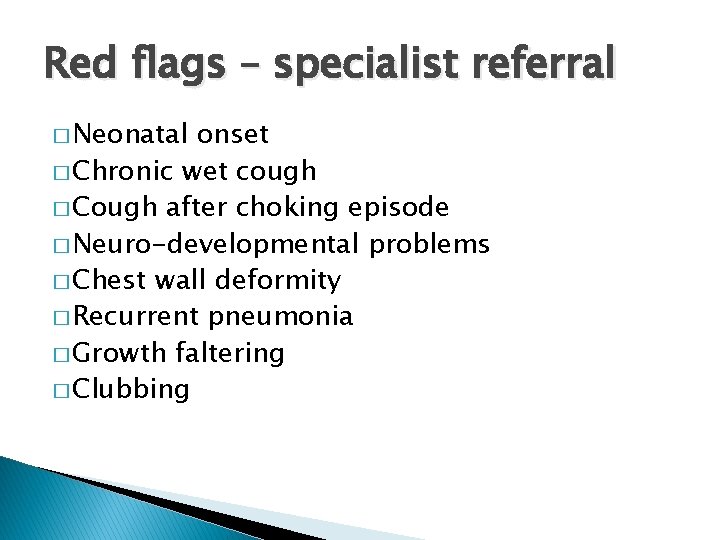
Red flags � When would you refer (when have you referred? )
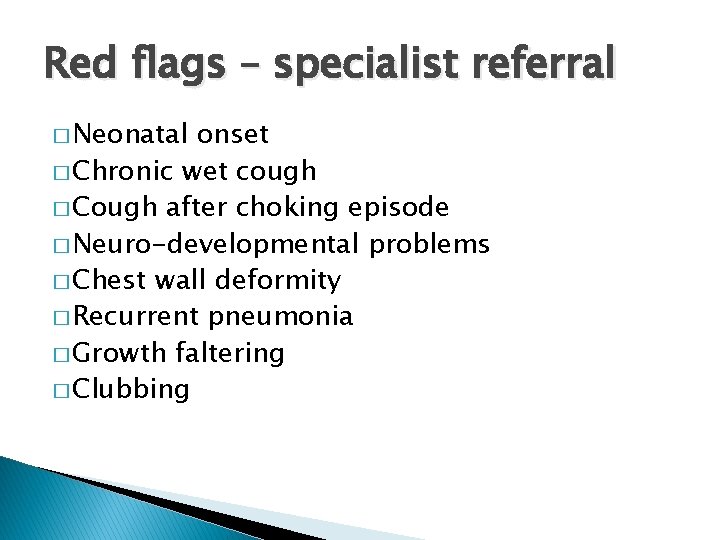
Red flags – specialist referral � Neonatal onset � Chronic wet cough � Cough after choking episode � Neuro-developmental problems � Chest wall deformity � Recurrent pneumonia � Growth faltering � Clubbing
Approach to management � Watchful waiting – 6 -8 weeks � Removal of aeroallergens � Trial anti-asthma treatment � Trial antibiotics for PBB
Summary � Respiratory paediatrics is fascinating! � …. . and relevant to everyday practice � Think of other causes of wheeze � Identify asthma phenotypes � Classify different cough types � Consider PBB � Refer if unsure
Thank you.
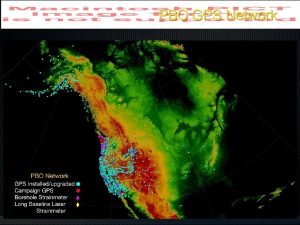
 Gps gps gps
Gps gps gps How does gps work
How does gps work Paed
Paed Neonatology lectures
Neonatology lectures Royal college of paediatrics developmental milestones
Royal college of paediatrics developmental milestones London school of paediatrics
London school of paediatrics History taking paediatrics
History taking paediatrics Where did the townshend act take place
Where did the townshend act take place Townshend act
Townshend act Townshend acts
Townshend acts Townshend act clipart
Townshend act clipart Why did the colonists hate the proclamation of 1763
Why did the colonists hate the proclamation of 1763 Bernard l shaw
Bernard l shaw What is the conducting zone of the respiratory system
What is the conducting zone of the respiratory system En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Egg för emanuel
Egg för emanuel Tack för att ni har lyssnat
Tack för att ni har lyssnat Meios steg för steg
Meios steg för steg Byggprocessen steg för steg
Byggprocessen steg för steg Rådet för byggkompetens
Rådet för byggkompetens Presentera för publik crossboss
Presentera för publik crossboss Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Förklara densitet för barn
Förklara densitet för barn Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Tack för att ni har lyssnat
Tack för att ni har lyssnat Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Mall för referat
Mall för referat Frger
Frger Epiteltyper
Epiteltyper Autokratiskt ledarskap
Autokratiskt ledarskap Lufttryck formel
Lufttryck formel Avrunda decimaltal
Avrunda decimaltal Adressändring ideell förening
Adressändring ideell förening Toppslätskivling effekt
Toppslätskivling effekt Elektronik för barn
Elektronik för barn Borra hål för knoppar
Borra hål för knoppar Bra mat för unga idrottare
Bra mat för unga idrottare Bris för vuxna
Bris för vuxna Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Ledarskapsteorier
Ledarskapsteorier Trög för kemist
Trög för kemist Ellika andolf
Ellika andolf Datorkunskap för nybörjare
Datorkunskap för nybörjare Steg för steg rita
Steg för steg rita Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Redogör för vad psykologi är
Redogör för vad psykologi är Geometriska former i förskolan
Geometriska former i förskolan Bästa kameran för astrofoto
Bästa kameran för astrofoto Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Offentlig förvaltning
Offentlig förvaltning Dikt rim
Dikt rim Plagg i rom
Plagg i rom Tidbok för yrkesförare
Tidbok för yrkesförare Handledning reflektionsmodellen
Handledning reflektionsmodellen Orubbliga rättigheter
Orubbliga rättigheter Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Big brother rösta
Big brother rösta Vem räknas som jude
Vem räknas som jude Cellorov
Cellorov Tillitsbaserad ledning
Tillitsbaserad ledning Ro i rom pax
Ro i rom pax Boverket ka
Boverket ka