Pulmonary Function Tests Spirometer A device that measures







- Slides: 82

Pulmonary Function Tests
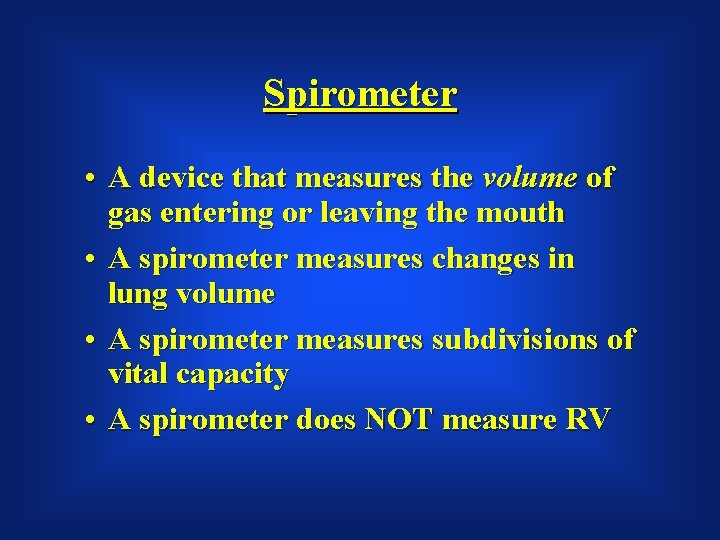
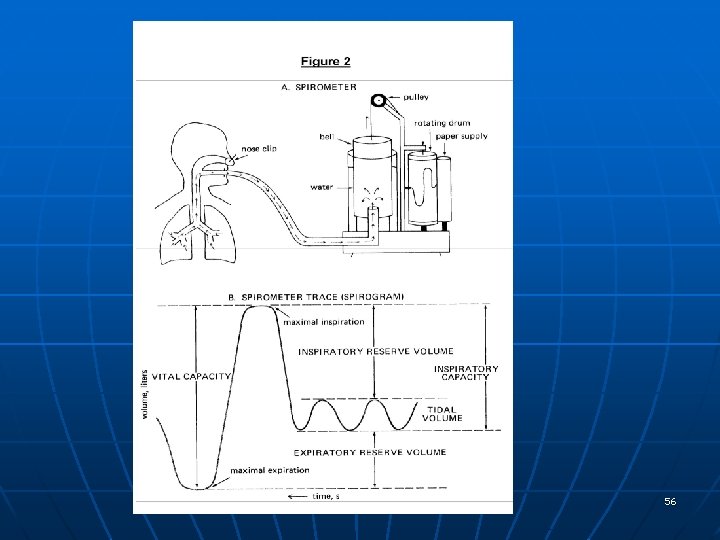
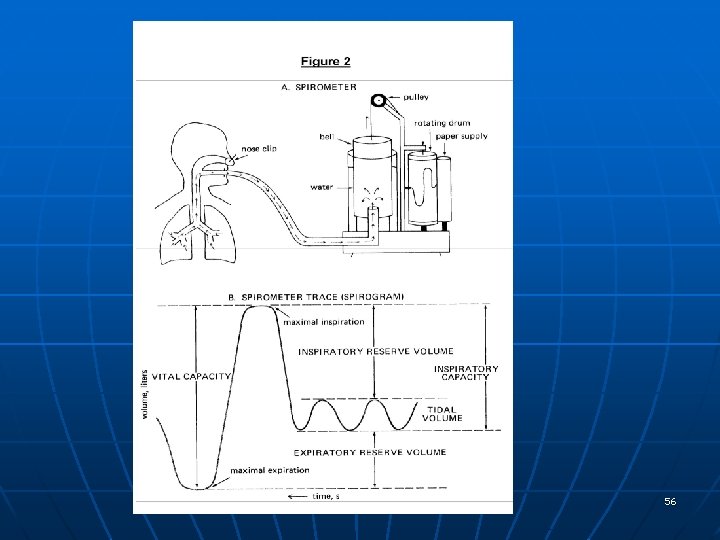
Spirometer • A device that measures the volume of gas entering or leaving the mouth • A spirometer measures changes in lung volume • A spirometer measures subdivisions of vital capacity • A spirometer does NOT measure RV
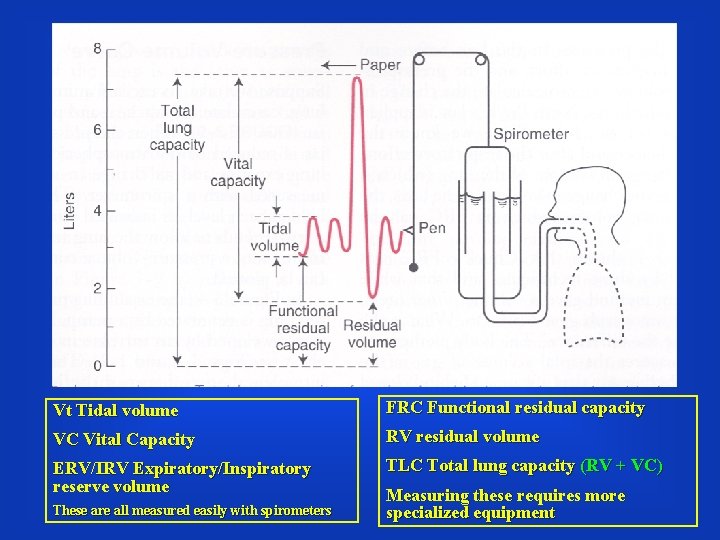
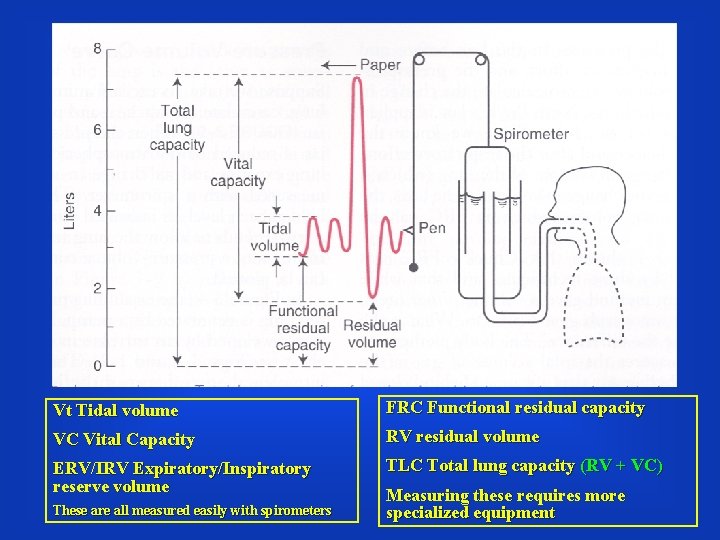
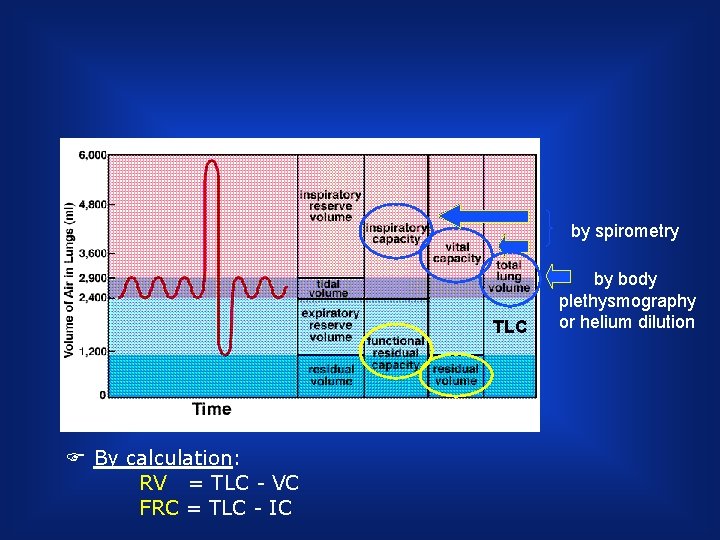
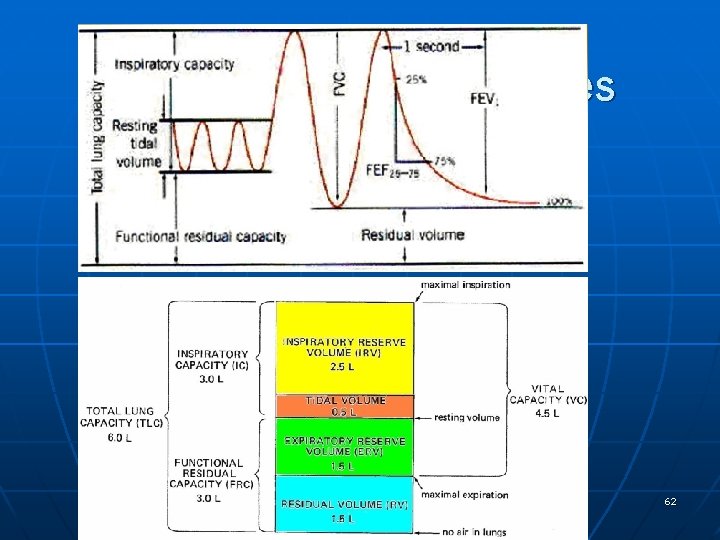
Vt Tidal volume FRC Functional residual capacity VC Vital Capacity RV residual volume ERV/IRV Expiratory/Inspiratory reserve volume TLC Total lung capacity (RV + VC) These are all measured easily with spirometers Measuring these requires more specialized equipment
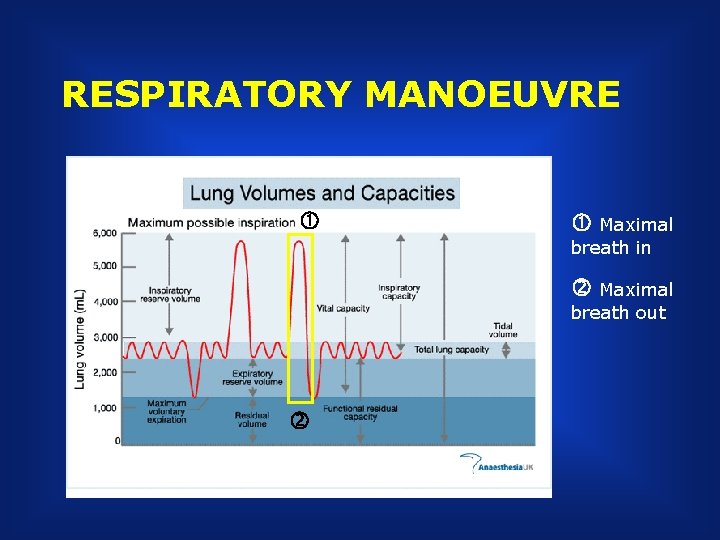
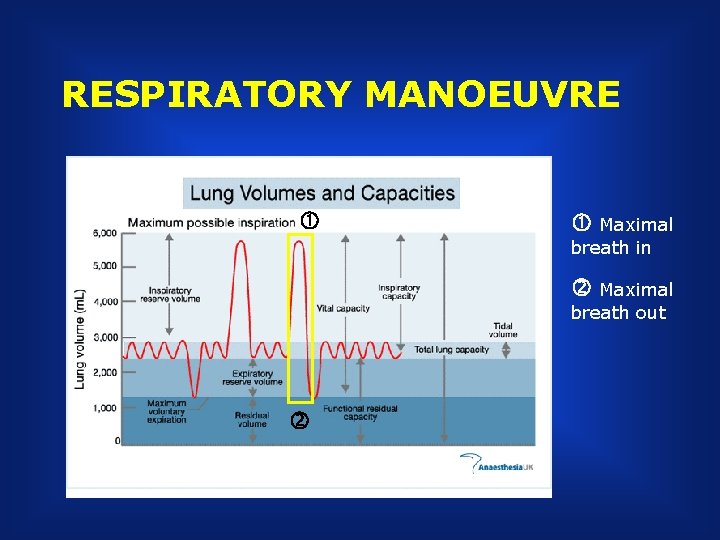
RESPIRATORY MANOEUVRE Maximal breath in Maximal breath out
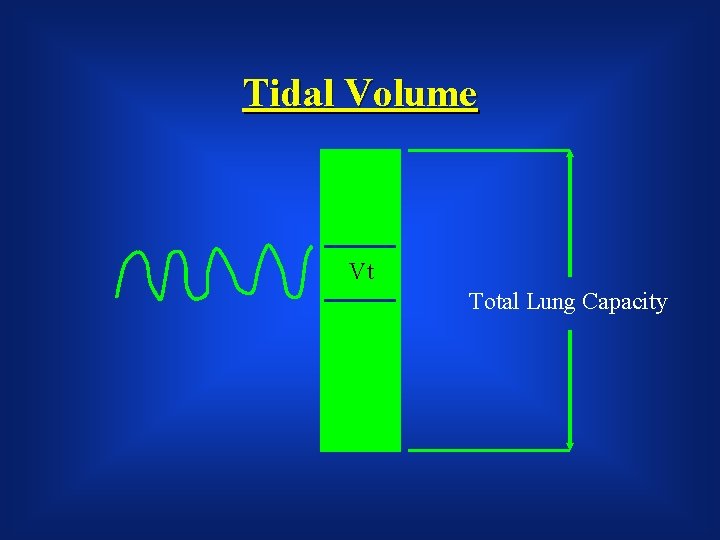
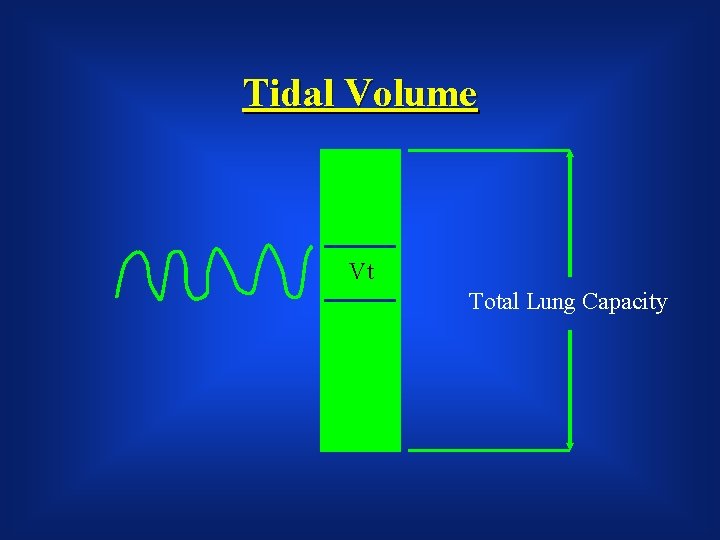
Tidal Volume Vt Total Lung Capacity
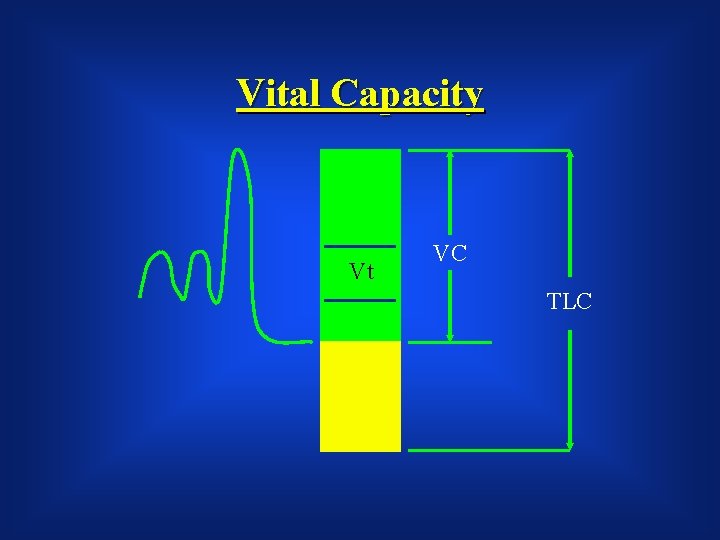
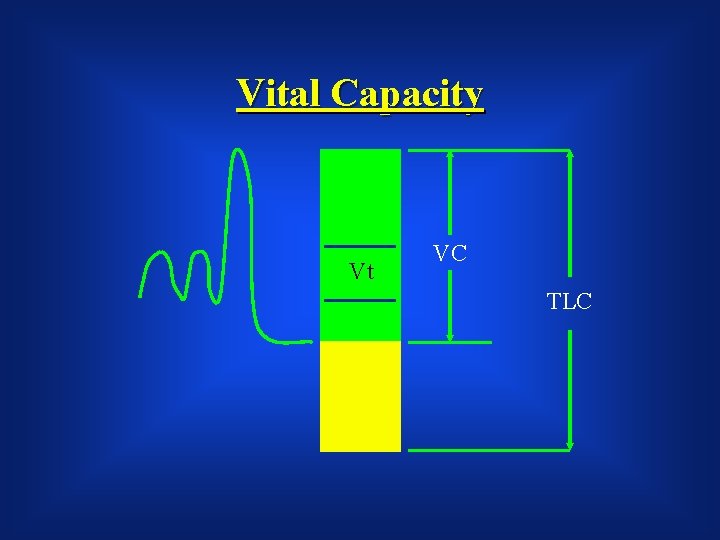
Vital Capacity Vt VC TLC
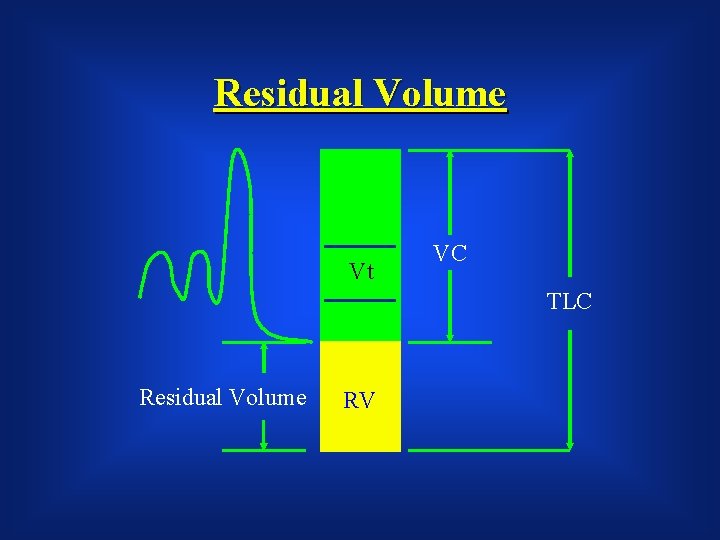
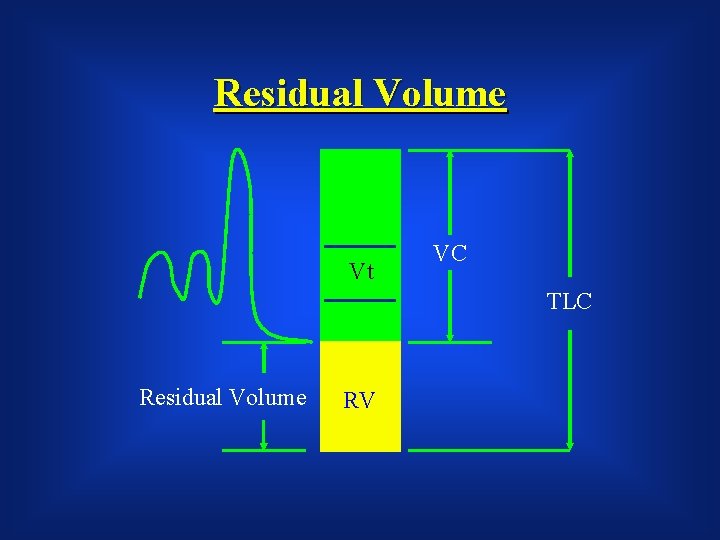
Residual Volume Vt VC TLC Residual Volume RV
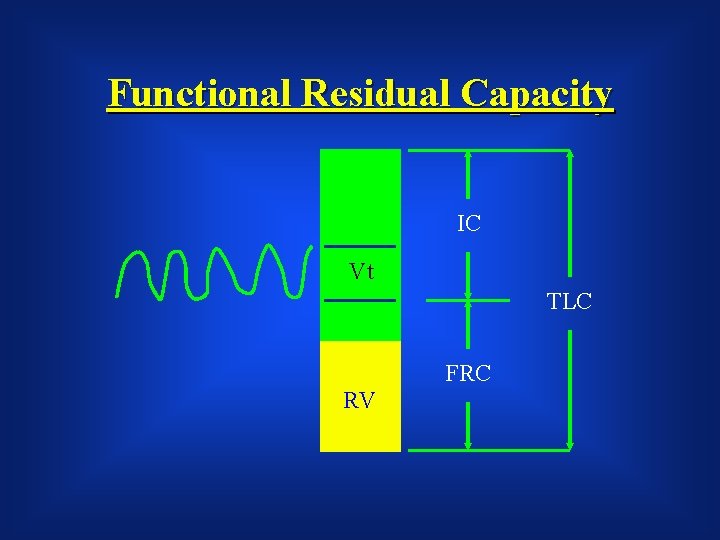
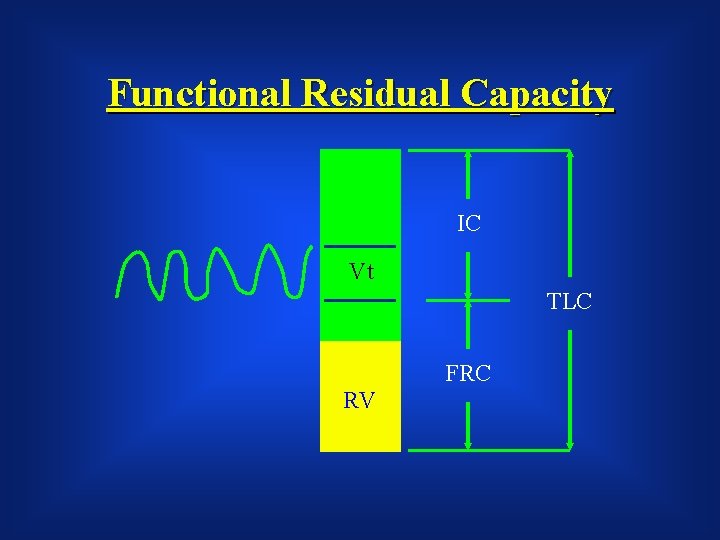
Functional Residual Capacity IC Vt TLC FRC RV
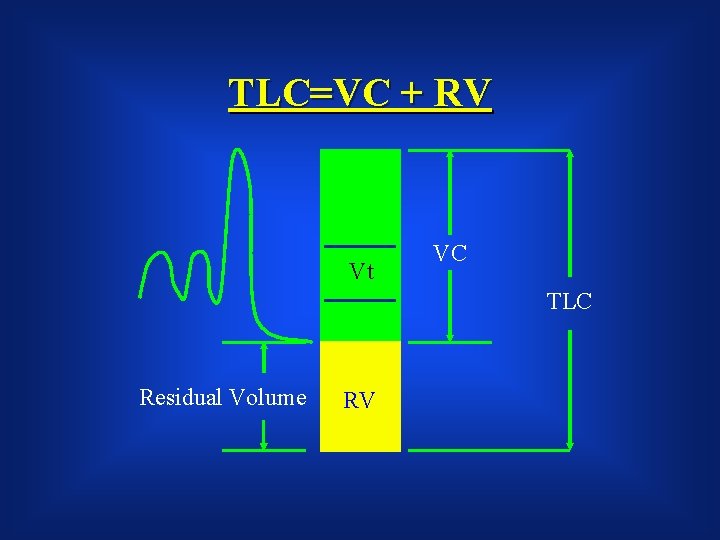
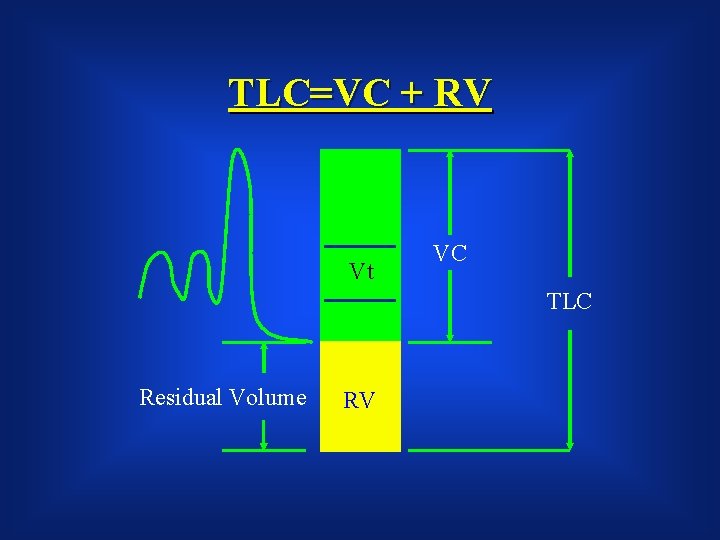
TLC=VC + RV Vt VC TLC Residual Volume RV
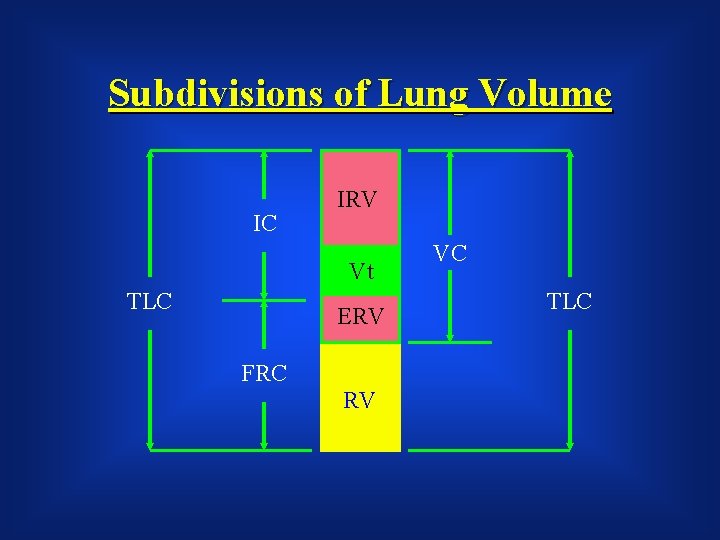
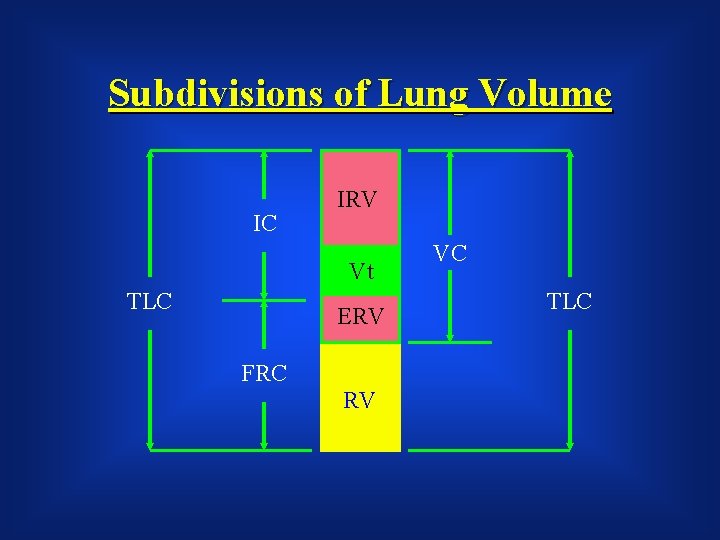
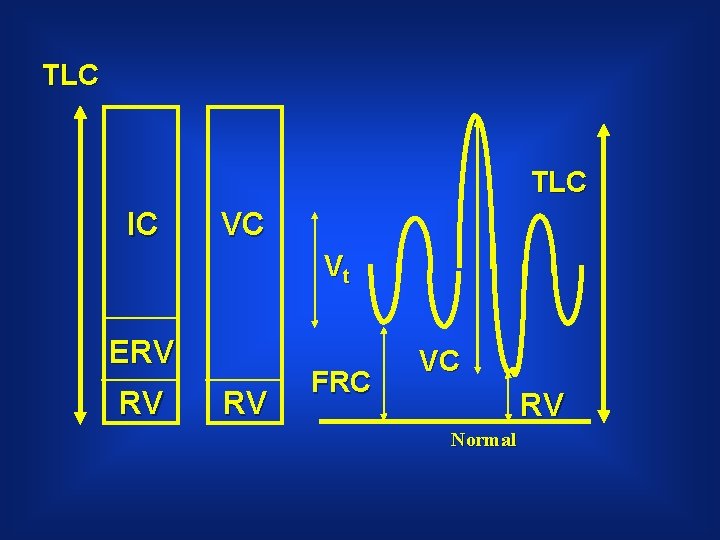
Subdivisions of Lung Volume IC IRV Vt TLC ERV FRC RV VC TLC
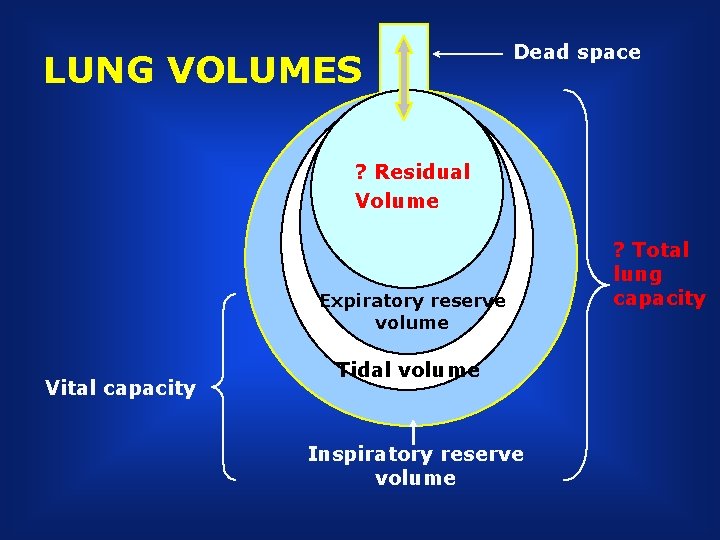
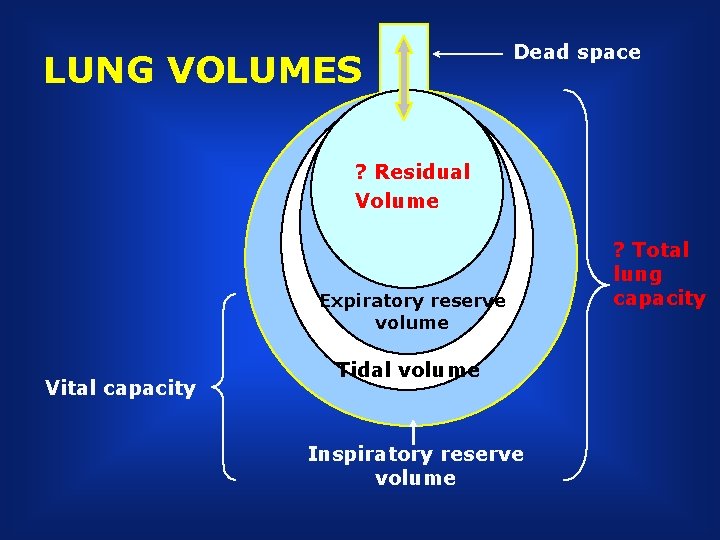
LUNG VOLUMES Dead space ? Residual Volume Tidal volume Expiratory reserve volume Vital capacity Tidal volume Inspiratory reserve volume ? Total lung capacity
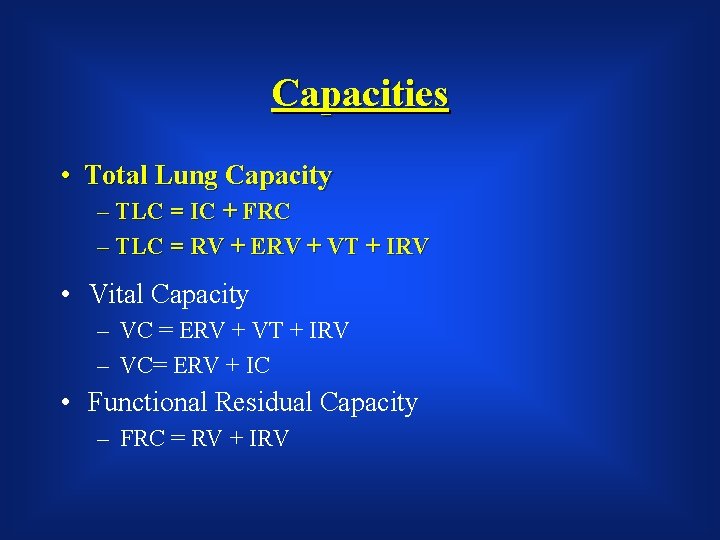
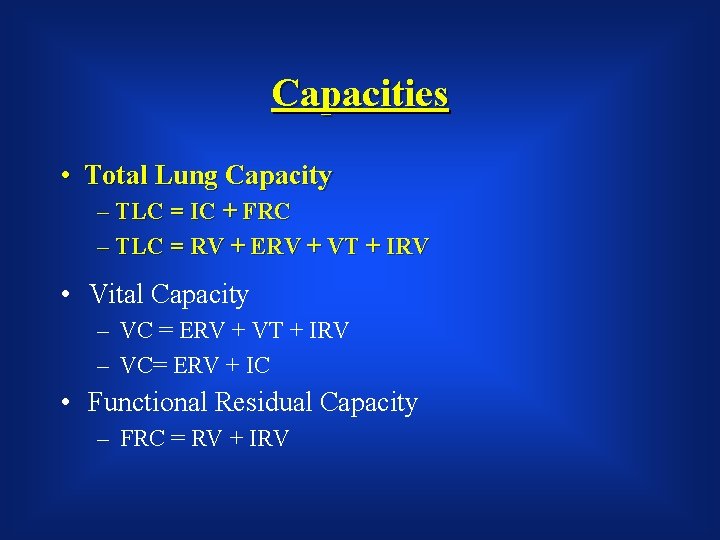
Capacities • Total Lung Capacity – TLC = IC + FRC – TLC = RV + ERV + VT + IRV • Vital Capacity – VC = ERV + VT + IRV – VC= ERV + IC • Functional Residual Capacity – FRC = RV + IRV
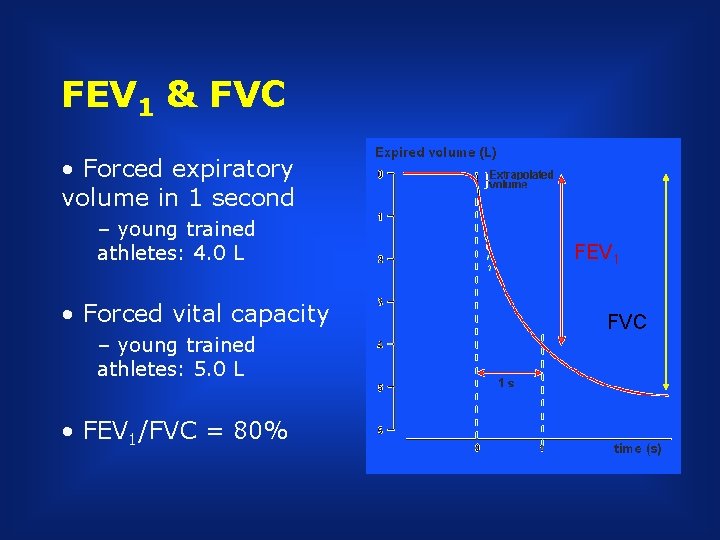
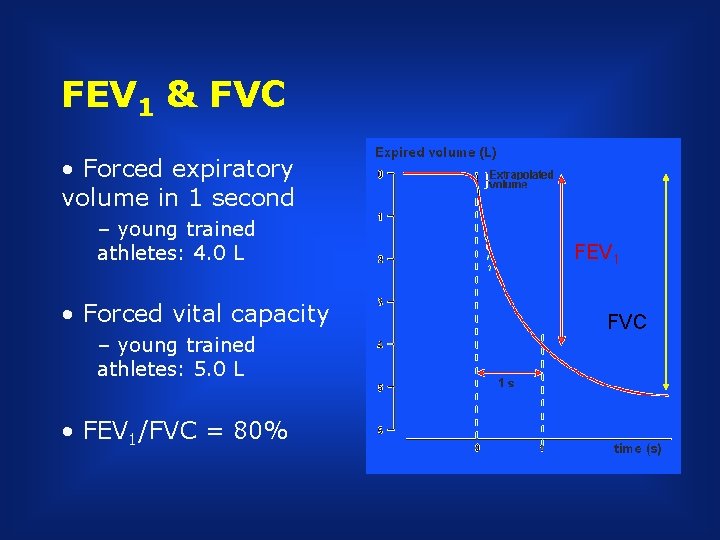
FEV 1 & FVC • Forced expiratory volume in 1 second – young trained athletes: 4. 0 L • Forced vital capacity – young trained athletes: 5. 0 L • FEV 1/FVC = 80% FEV 1 FVC
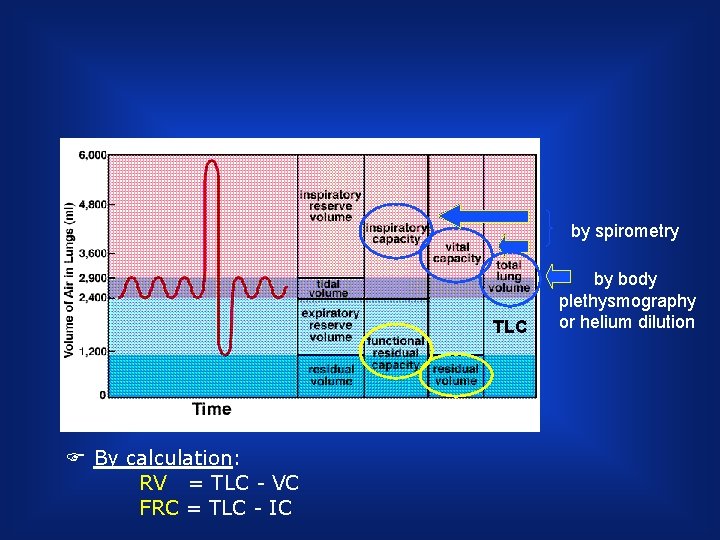
by spirometry TLC F By calculation: RV = TLC - VC FRC = TLC - IC by body plethysmography or helium dilution
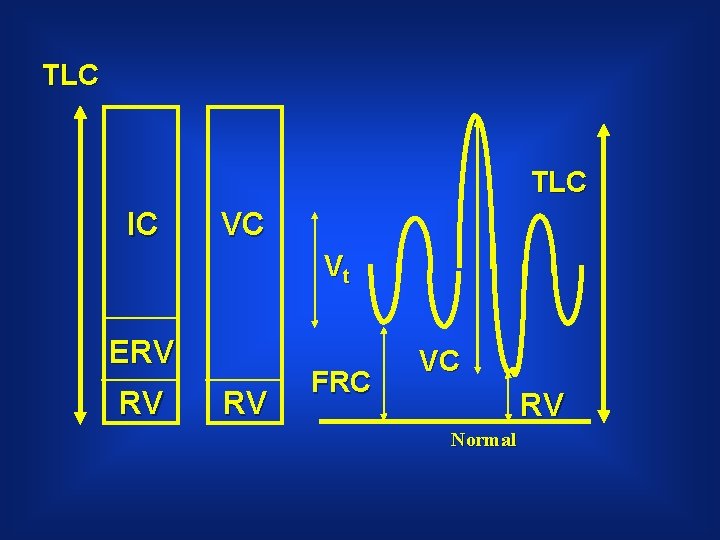
TLC IC VC Vt ERV RV RV FRC VC RV Normal
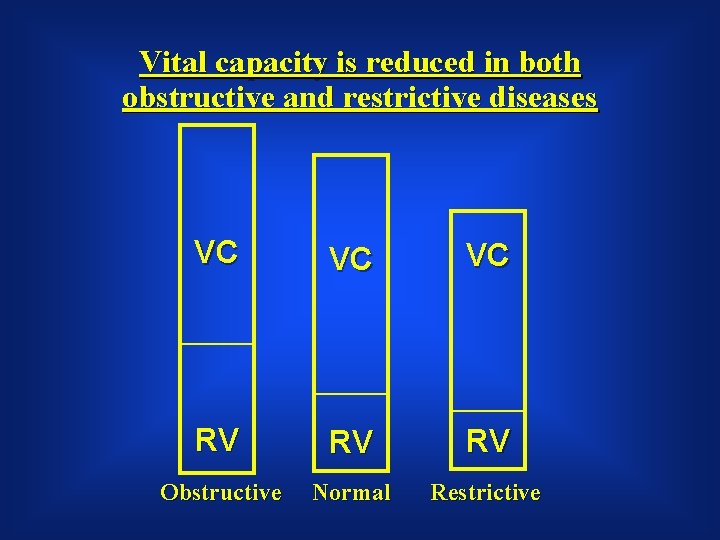
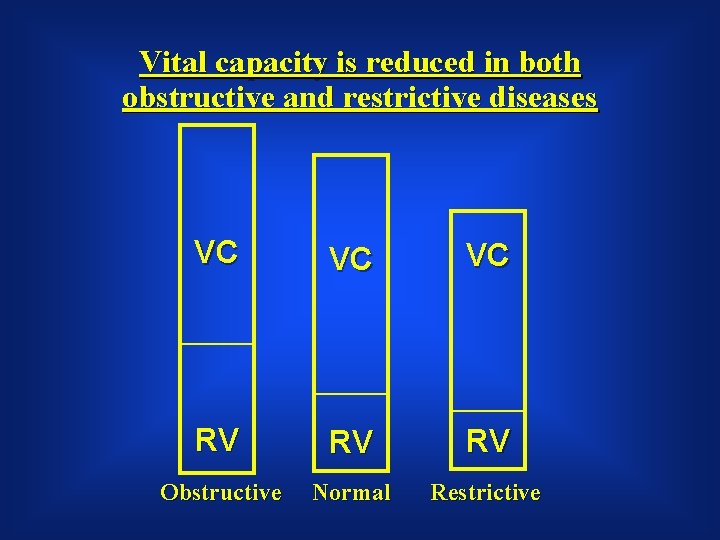
Vital capacity is reduced in both obstructive and restrictive diseases VC VC VC RV RV RV Obstructive Normal Restrictive
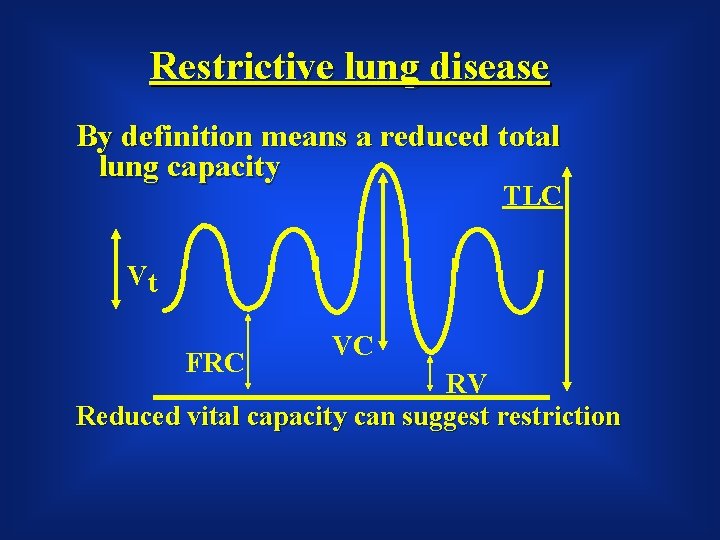
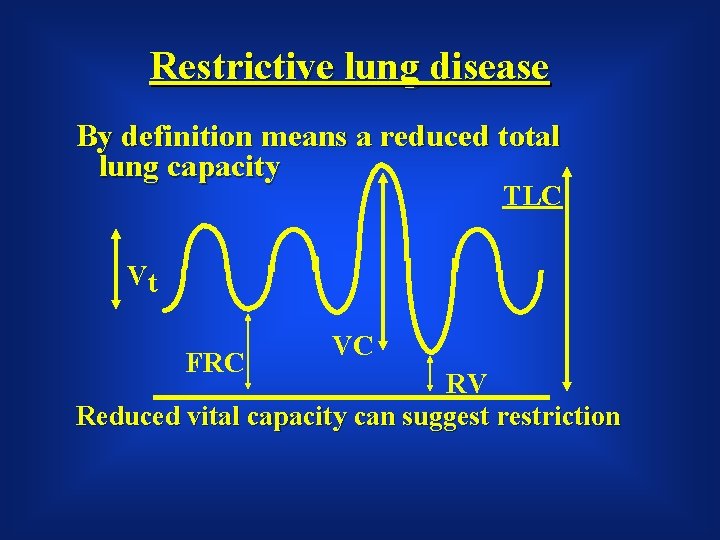
Restrictive lung disease By definition means a reduced total lung capacity TLC Vt FRC VC RV Reduced vital capacity can suggest restriction
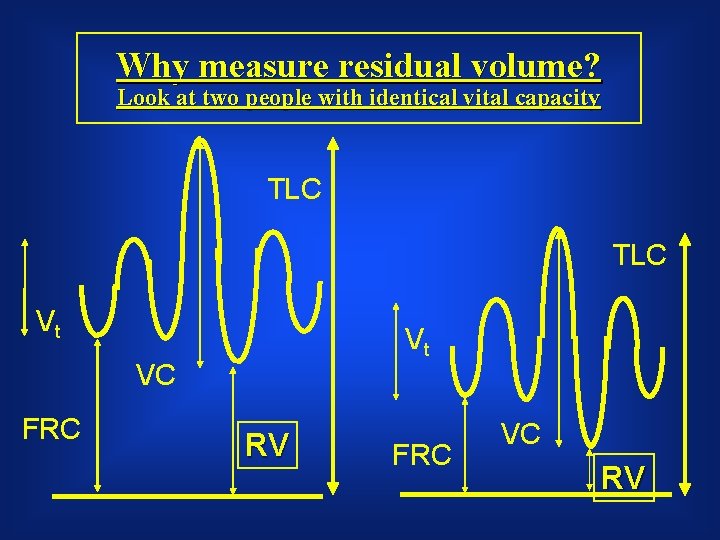
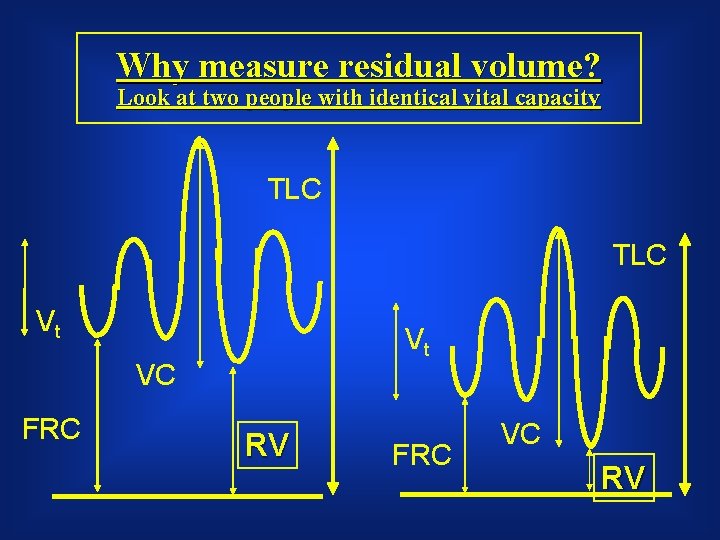
Why measure residual volume? Look at two people with identical vital capacity TLC Vt Vt VC FRC RV FRC VC RV
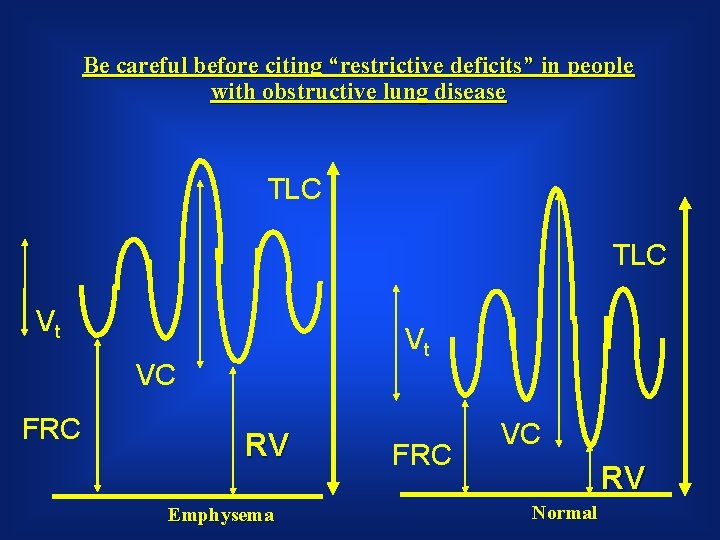
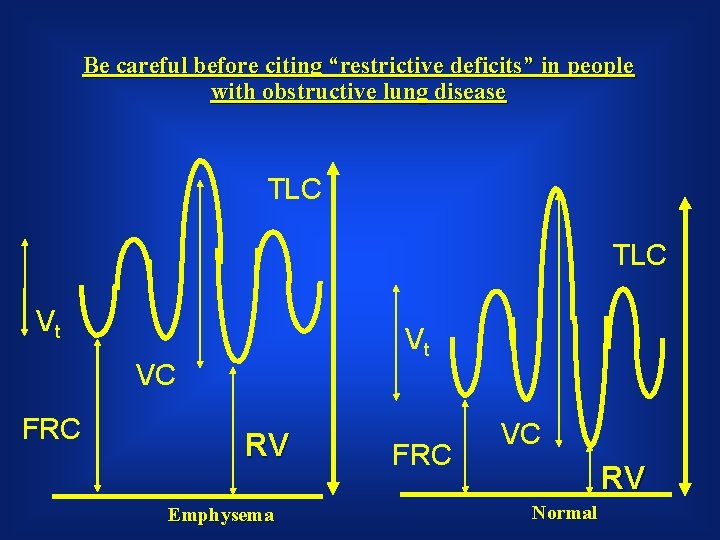
Be careful before citing “restrictive deficits” in people with obstructive lung disease TLC Vt Vt VC FRC RV Emphysema FRC VC RV Normal
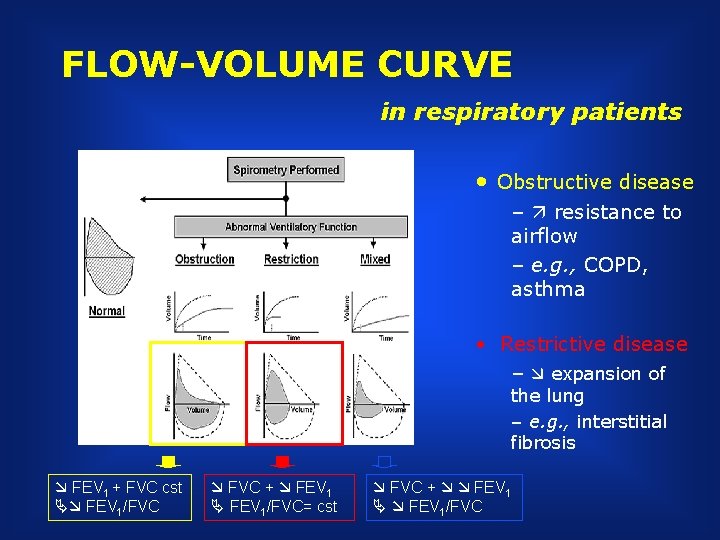
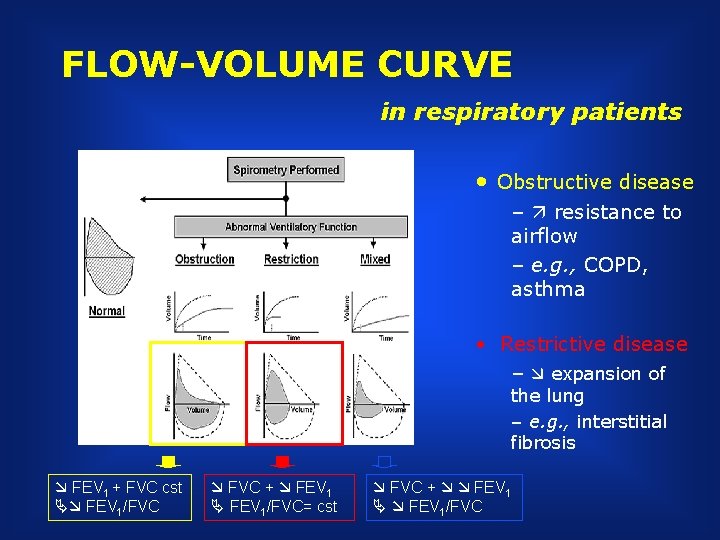
FLOW-VOLUME CURVE in respiratory patients • Obstructive disease – resistance to airflow – e. g. , COPD, asthma • Restrictive disease – expansion of the lung – e. g. , interstitial fibrosis FEV 1 + FVC cst FEV 1/FVC + FEV 1/FVC= cst FVC + FEV 1/FVC
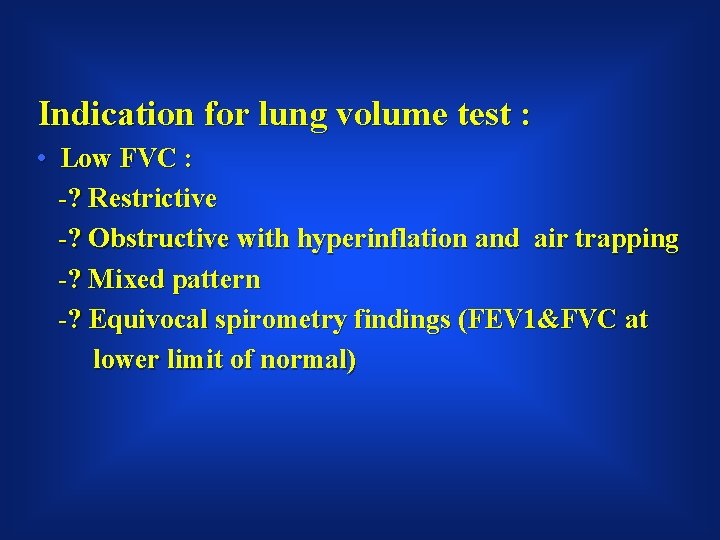
Indication for lung volume test : • Low FVC : -? Restrictive -? Obstructive with hyperinflation and air trapping -? Mixed pattern -? Equivocal spirometry findings (FEV 1&FVC at lower limit of normal)
Measuring TLC • To measure TLC or FRC, which include RV, spirometry is insufficient • Techniques: –Gas dilution –Plethysmography (body box)
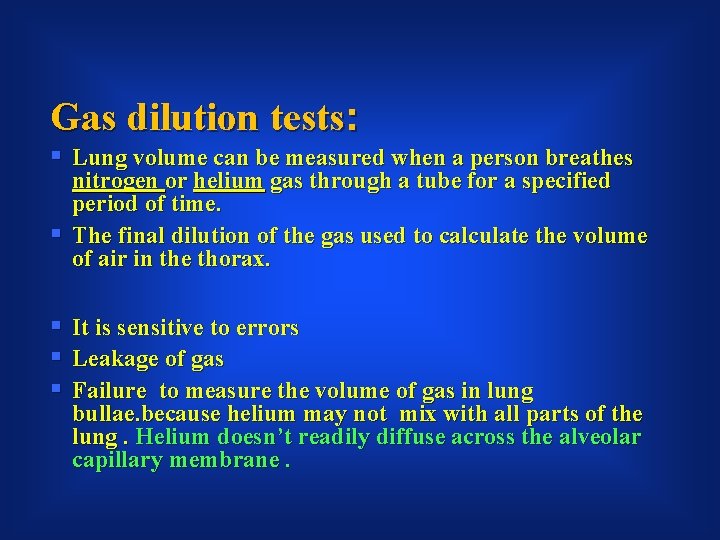
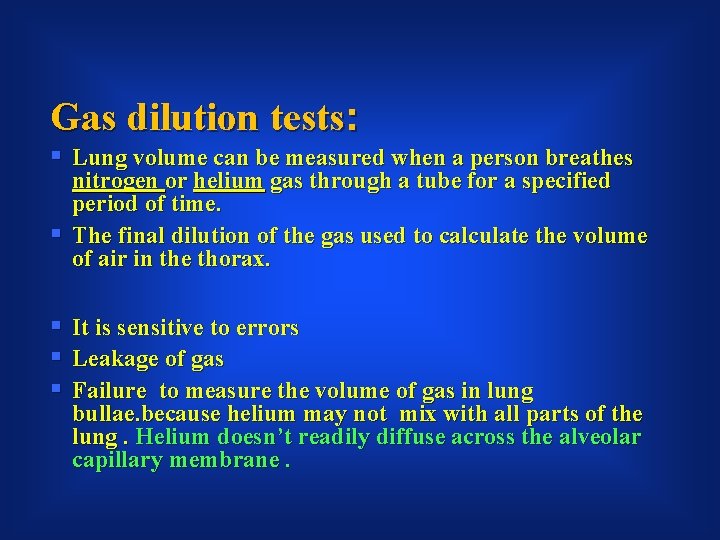
Gas dilution tests: § Lung volume can be measured when a person breathes nitrogen or helium gas through a tube for a specified period of time. § The final dilution of the gas used to calculate the volume of air in the thorax. § It is sensitive to errors § Leakage of gas § Failure to measure the volume of gas in lung bullae. because helium may not mix with all parts of the lung. Helium doesn’t readily diffuse across the alveolar capillary membrane.
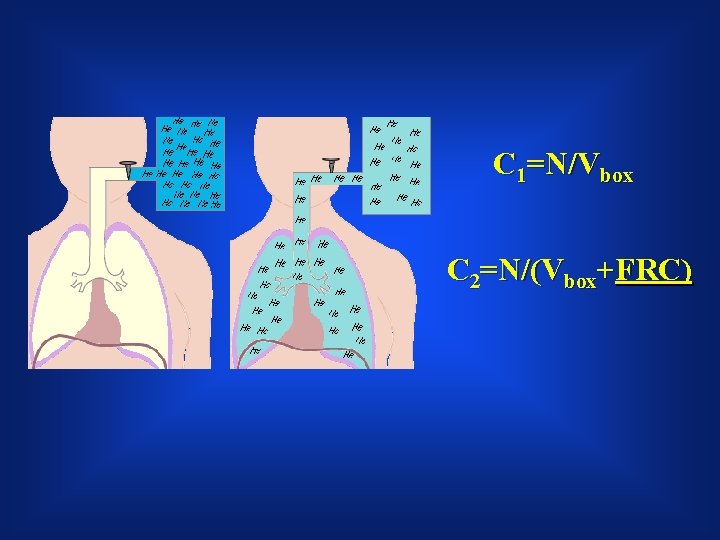
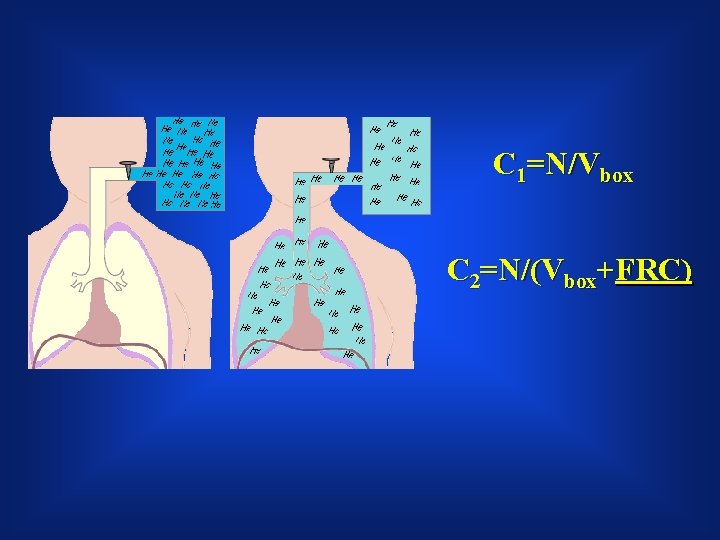
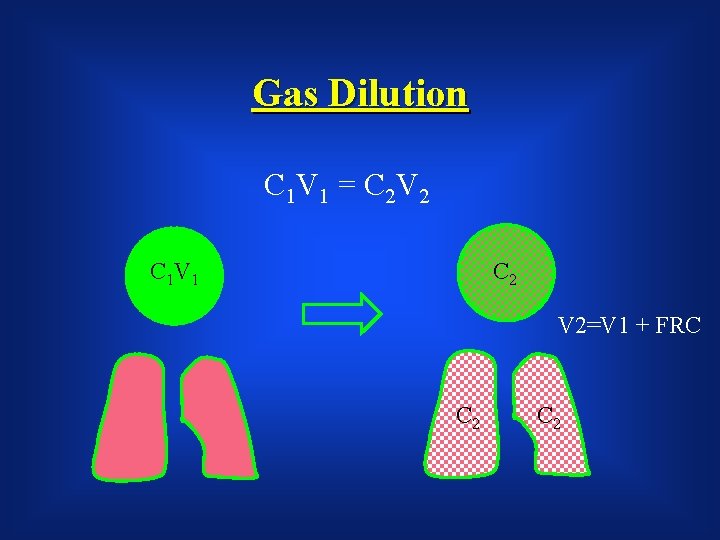
C 1=N/Vbox C 2=N/(Vbox+FRC)
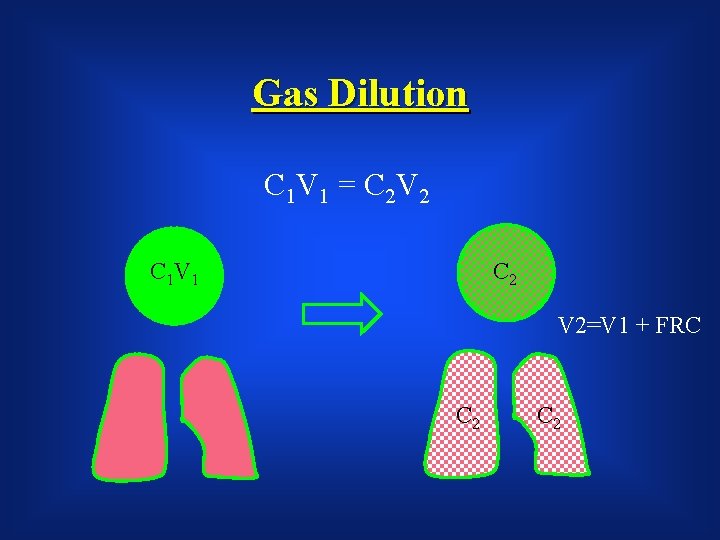
Gas Dilution C 1 V 1 = C 2 V 2 C 1 V 1 C 2 V 2=V 1 + FRC C 2
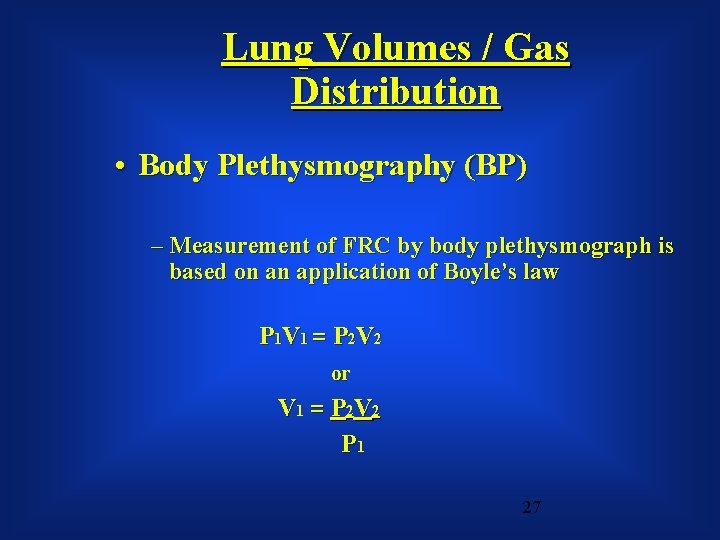
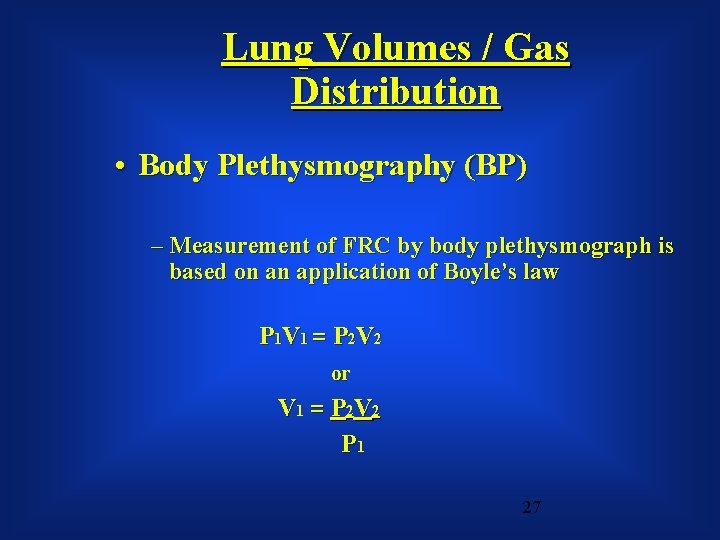
Lung Volumes / Gas Distribution • Body Plethysmography (BP) – Measurement of FRC by body plethysmograph is based on an application of Boyle’s law P 1 V 1 = P 2 V 2 or V 1 = P 2 V 2 P 1 27
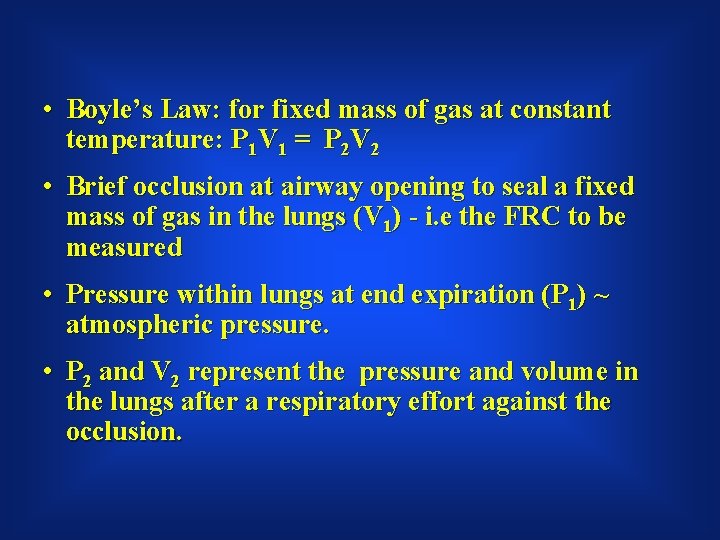
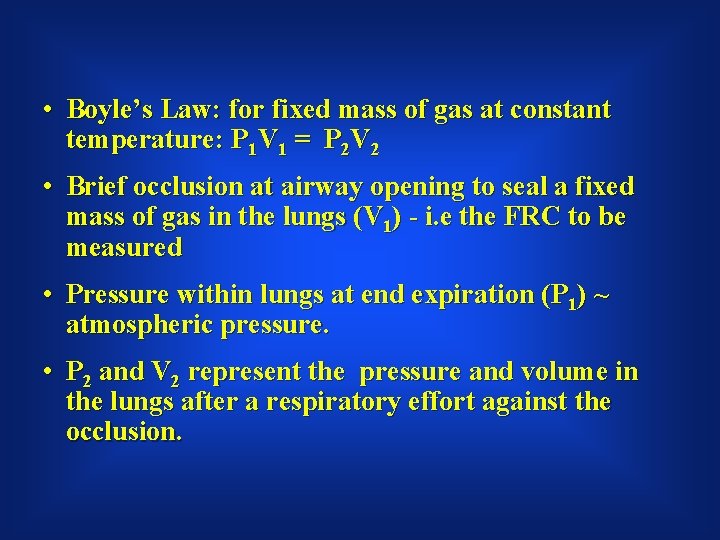
• Boyle’s Law: for fixed mass of gas at constant temperature: P 1 V 1 = P 2 V 2 • Brief occlusion at airway opening to seal a fixed mass of gas in the lungs (V 1) - i. e the FRC to be measured • Pressure within lungs at end expiration (P 1) ~ atmospheric pressure. • P 2 and V 2 represent the pressure and volume in the lungs after a respiratory effort against the occlusion.
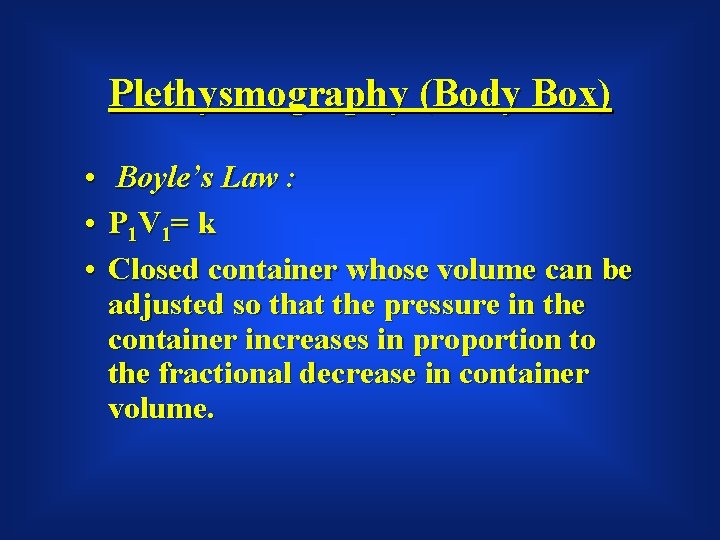
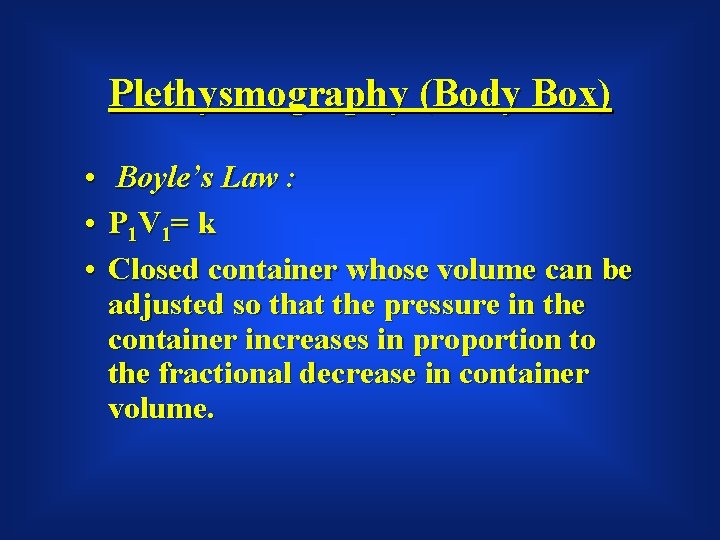
Plethysmography (Body Box) • • • Boyle’s Law : P 1 V 1= k Closed container whose volume can be adjusted so that the pressure in the container increases in proportion to the fractional decrease in container volume.
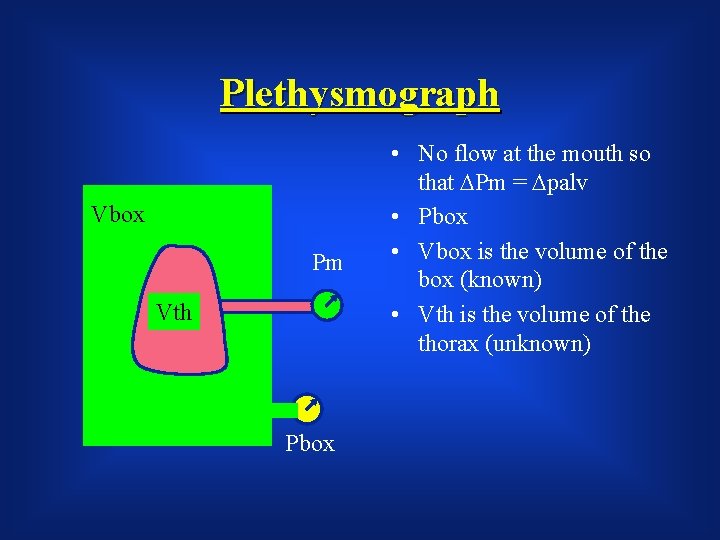
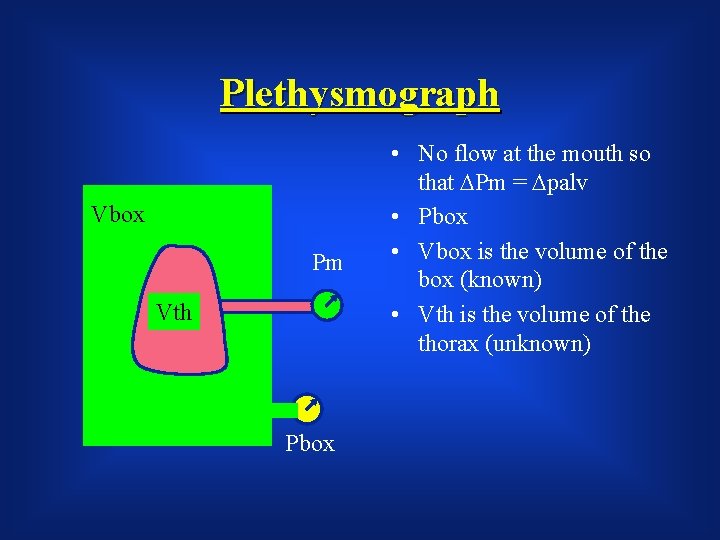
Plethysmograph Vbox Pm Vth Pbox • No flow at the mouth so that DPm = Dpalv • Pbox • Vbox is the volume of the box (known) • Vth is the volume of the thorax (unknown)
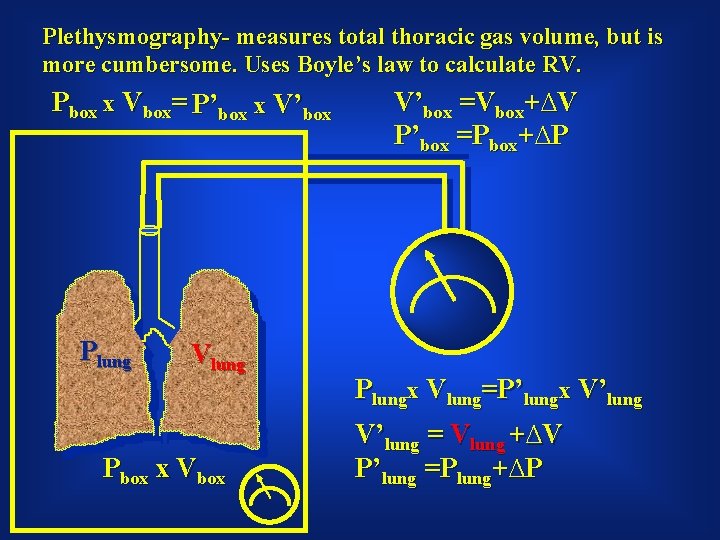
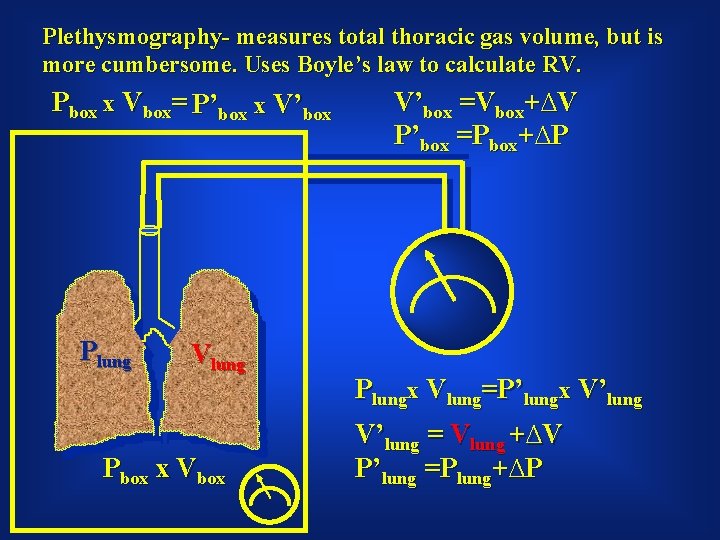
Plethysmography- measures total thoracic gas volume, but is more cumbersome. Uses Boyle’s law to calculate RV. Pbox x Vbox= P’box x V’box Plung Vlung Pbox x Vbox V’box =Vbox+∆V P’box =Pbox+∆P Plungx Vlung=P’lungx V’lung = Vlung +∆V P’lung =Plung+∆P

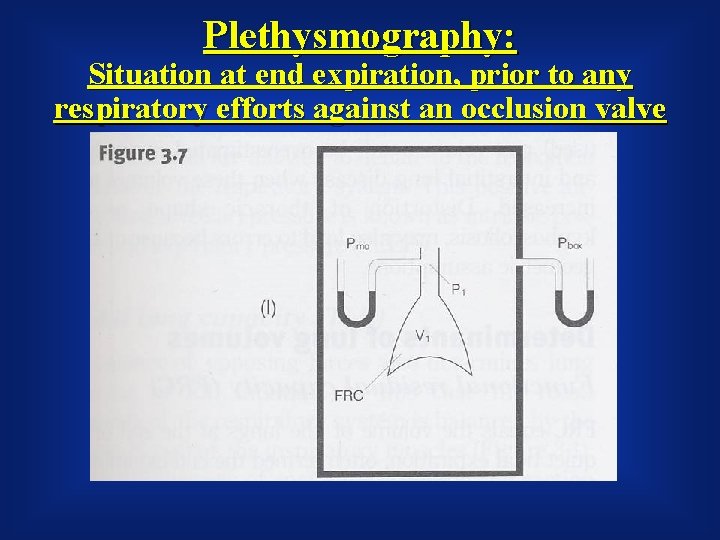
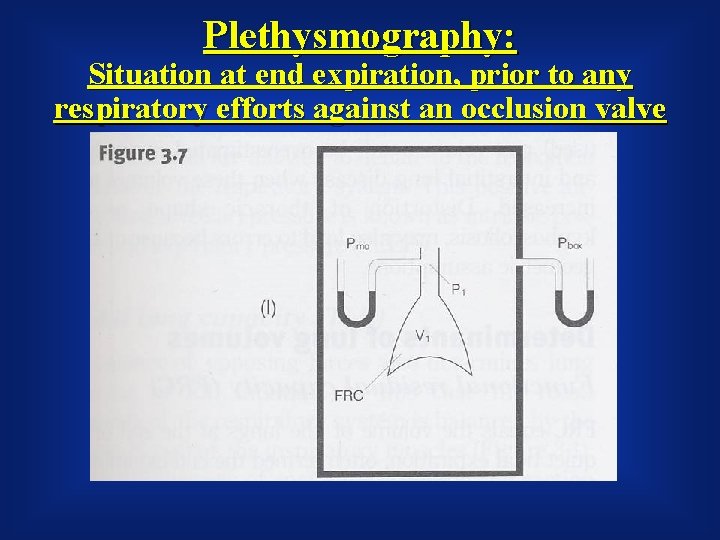
Plethysmography: Situation at end expiration, prior to any respiratory efforts against an occlusion valve
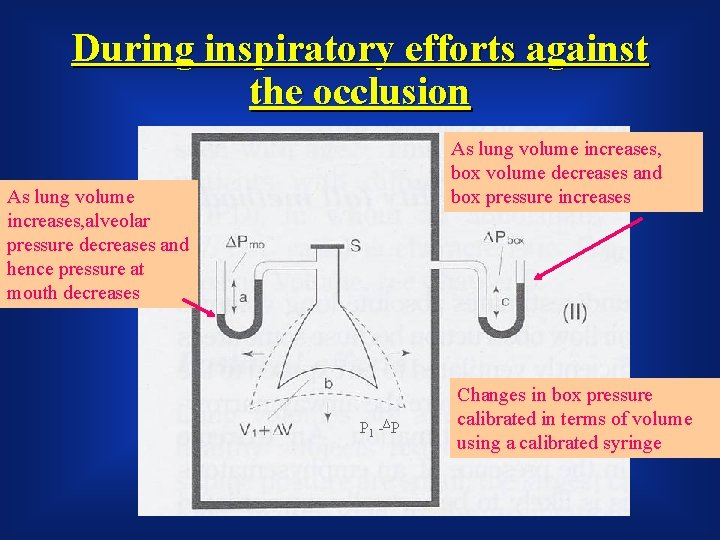
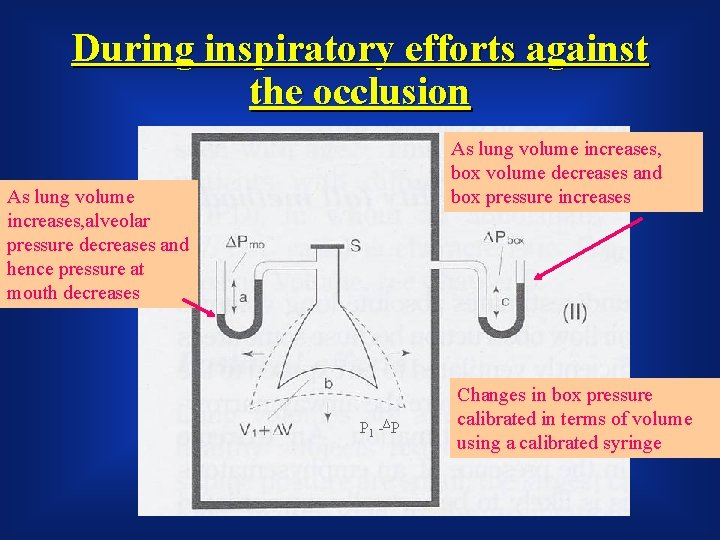
During inspiratory efforts against the occlusion As lung volume increases, box volume decreases and box pressure increases As lung volume increases, alveolar pressure decreases and hence pressure at mouth decreases P 1 -ΔP Changes in box pressure calibrated in terms of volume using a calibrated syringe
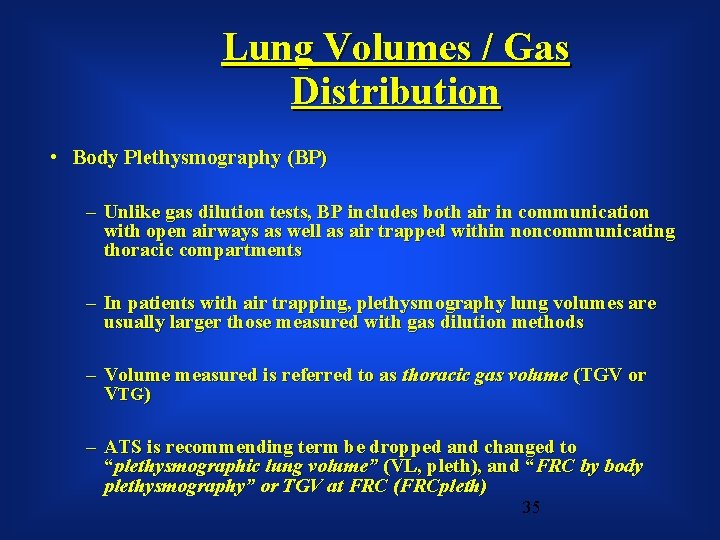
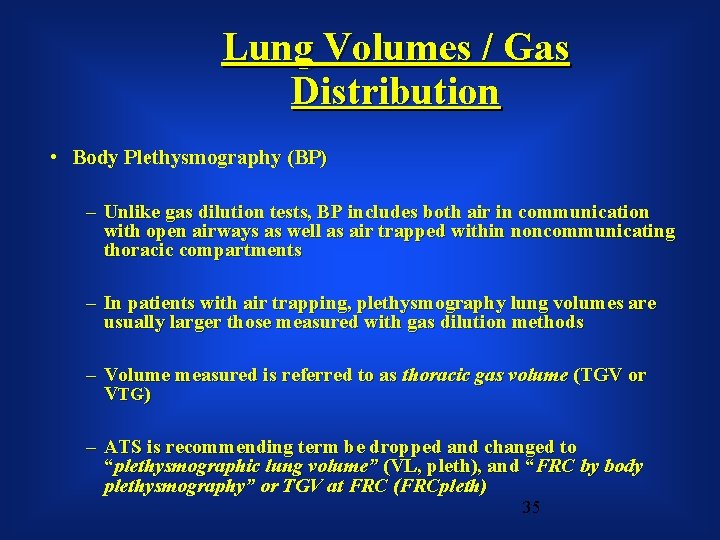
Lung Volumes / Gas Distribution • Body Plethysmography (BP) – Unlike gas dilution tests, BP includes both air in communication with open airways as well as air trapped within noncommunicating thoracic compartments – In patients with air trapping, plethysmography lung volumes are usually larger those measured with gas dilution methods – Volume measured is referred to as thoracic gas volume (TGV or VTG) – ATS is recommending term be dropped and changed to “plethysmographic lung volume” (VL, pleth), and “FRC by body plethysmography” or TGV at FRC (FRCpleth) 35
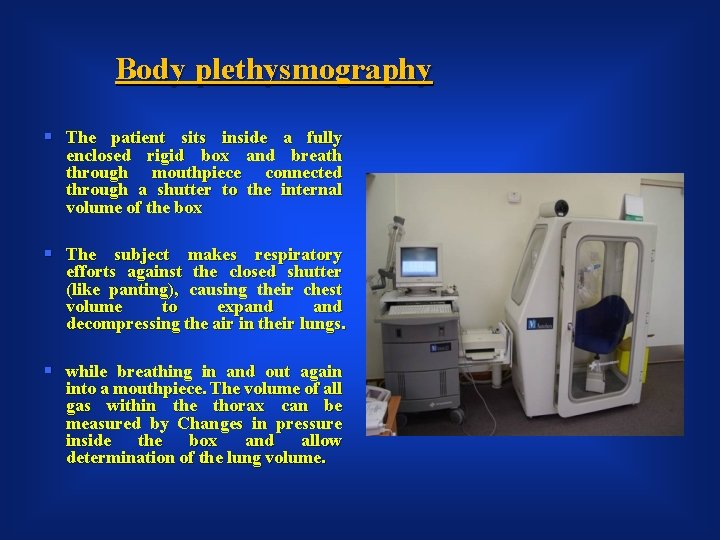
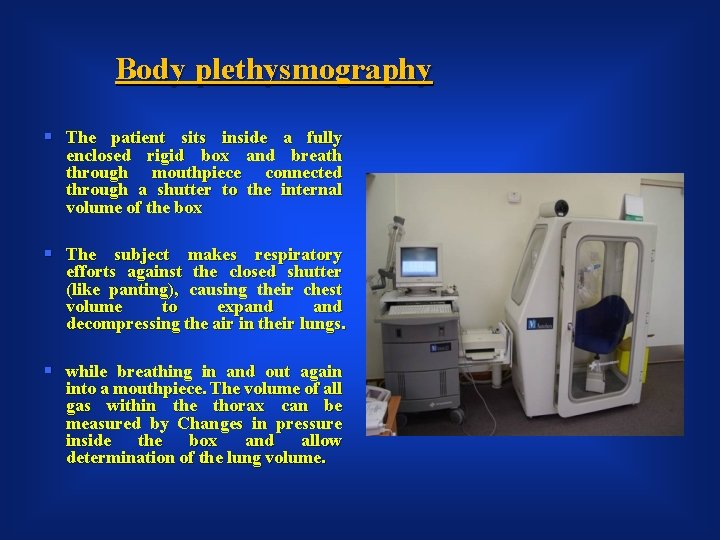
Body plethysmography § The patient sits inside a fully enclosed rigid box and breath through mouthpiece connected through a shutter to the internal volume of the box § The subject makes respiratory efforts against the closed shutter (like panting), causing their chest volume to expand decompressing the air in their lungs. § while breathing in and out again into a mouthpiece. The volume of all gas within the thorax can be measured by Changes in pressure inside the box and allow determination of the lung volume.
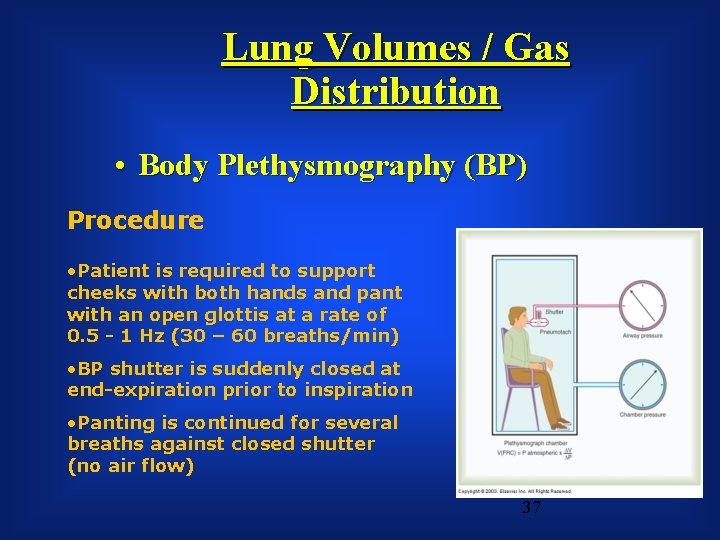
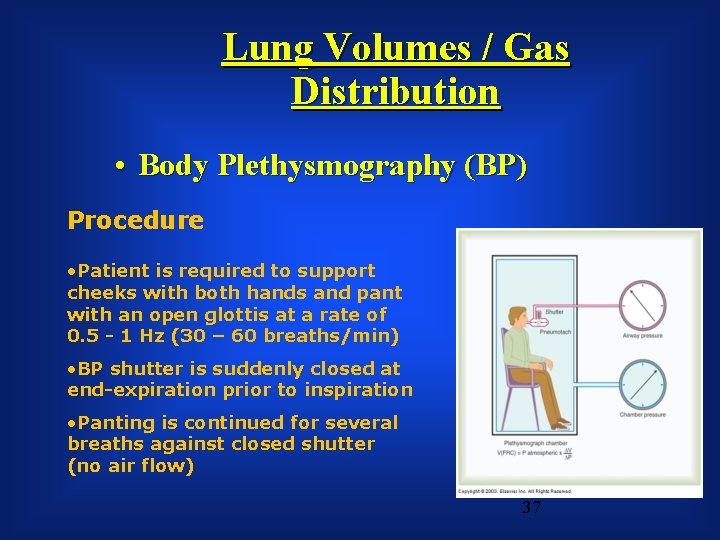
Lung Volumes / Gas Distribution • Body Plethysmography (BP) Procedure • Patient is required to support cheeks with both hands and pant with an open glottis at a rate of 0. 5 - 1 Hz (30 – 60 breaths/min) • BP shutter is suddenly closed at end-expiration prior to inspiration • Panting is continued for several breaths against closed shutter (no air flow) 37
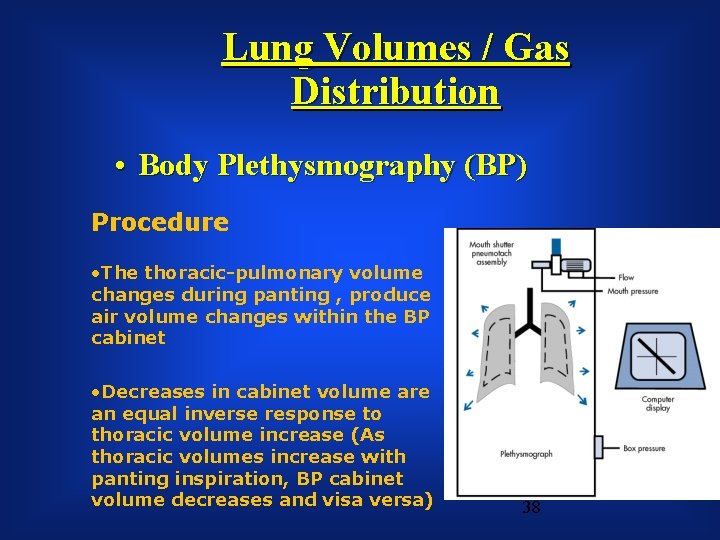
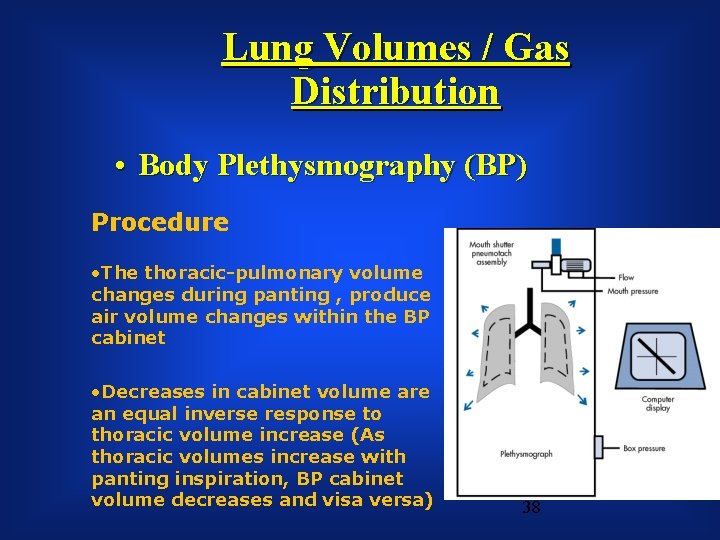
Lung Volumes / Gas Distribution • Body Plethysmography (BP) Procedure • The thoracic-pulmonary volume changes during panting , produce air volume changes within the BP cabinet • Decreases in cabinet volume are an equal inverse response to thoracic volume increase (As thoracic volumes increase with panting inspiration, BP cabinet volume decreases and visa versa) 38
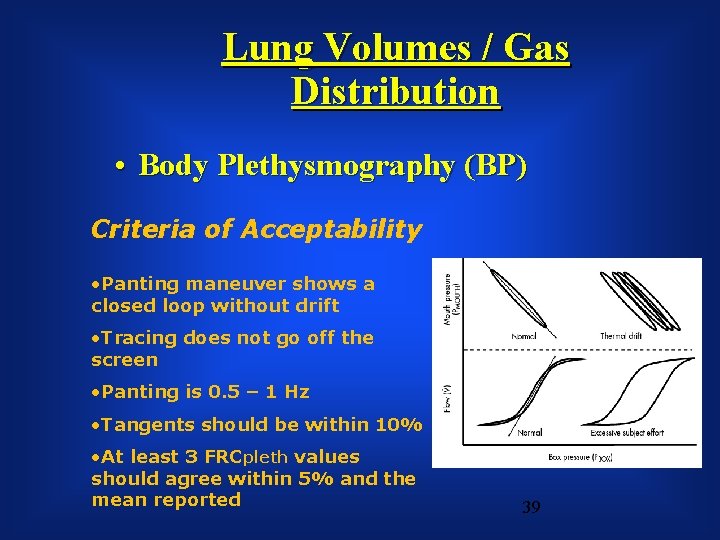
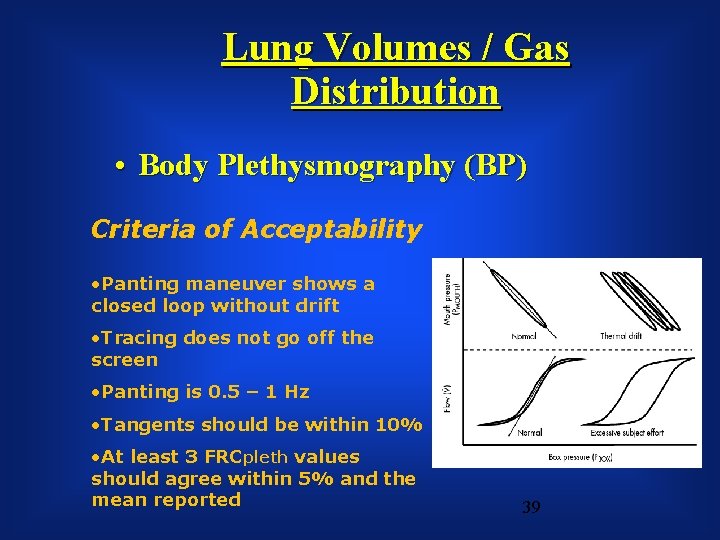
Lung Volumes / Gas Distribution • Body Plethysmography (BP) Criteria of Acceptability • Panting maneuver shows a closed loop without drift • Tracing does not go off the screen • Panting is 0. 5 – 1 Hz • Tangents should be within 10% • At least 3 FRCpleth values should agree within 5% and the mean reported 39

The history of clinical whole body plethysmography l l 1790 Menzies „Dissertation on Respiration“ 1881/2 Gad und Pflüger, „Residualvolumen“ • 1923 - 1959 Verzar, Du Bois, Mead etc • 1972, 2005 Matthys „Historische Entwicklung der klinischen Ganzkörperplethysmographie“ Atemw. u. Lungenkrkh. 31/4, 204211


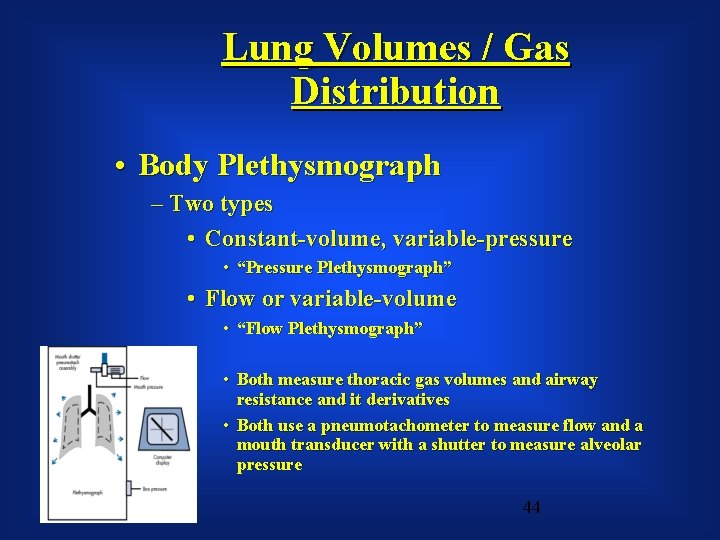
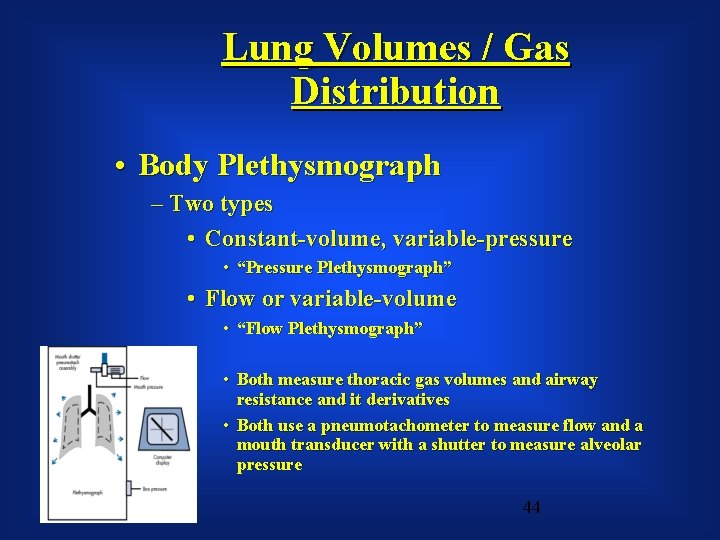
Lung Volumes / Gas Distribution • Body Plethysmograph – Two types • Constant-volume, variable-pressure • “Pressure Plethysmograph” • Flow or variable-volume • “Flow Plethysmograph” • Both measure thoracic gas volumes and airway resistance and it derivatives • Both use a pneumotachometer to measure flow and a mouth transducer with a shutter to measure alveolar pressure 44
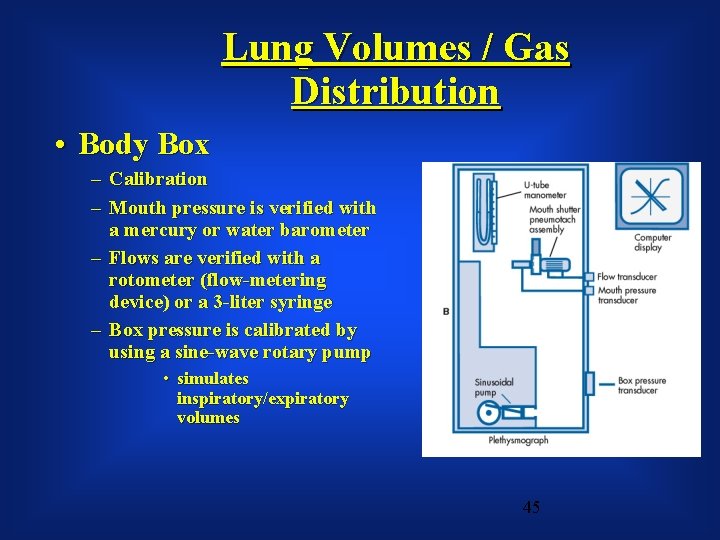
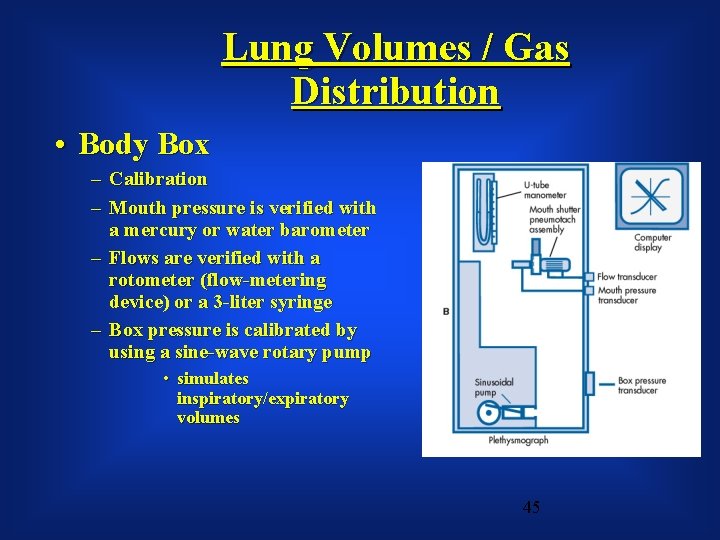
Lung Volumes / Gas Distribution • Body Box – Calibration – Mouth pressure is verified with a mercury or water barometer – Flows are verified with a rotometer (flow-metering device) or a 3 -liter syringe – Box pressure is calibrated by using a sine-wave rotary pump • simulates inspiratory/expiratory volumes 45
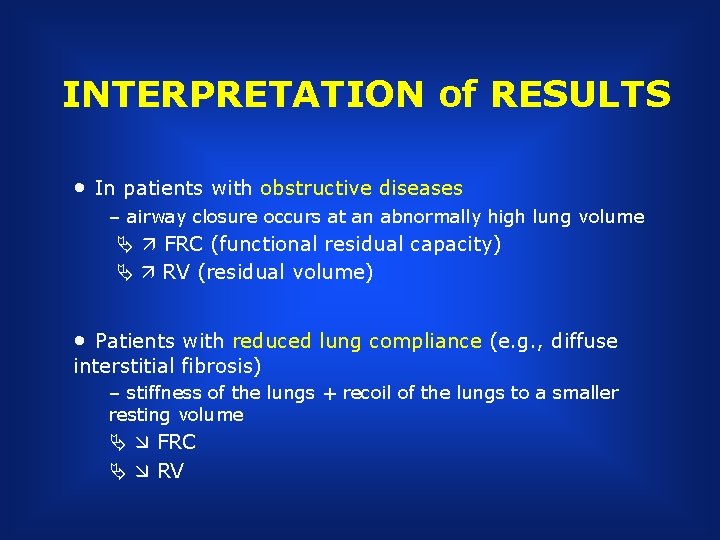
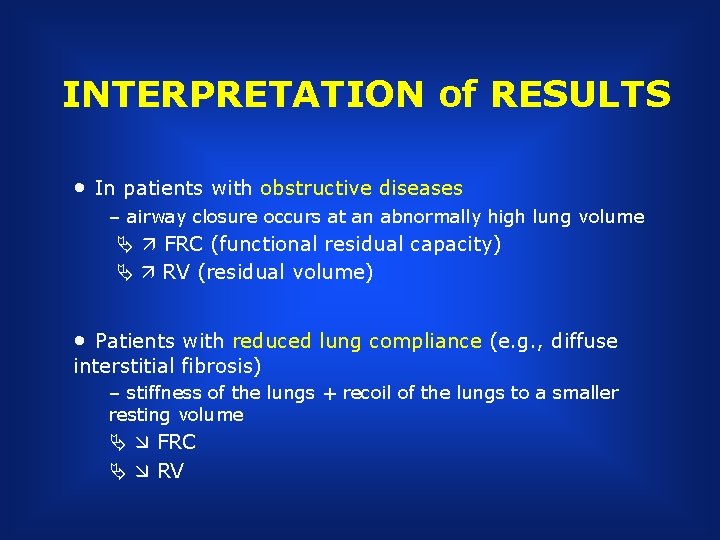
INTERPRETATION of RESULTS • In patients with obstructive diseases – airway closure occurs at an abnormally high lung volume FRC (functional residual capacity) RV (residual volume) • Patients with reduced lung compliance (e. g. , diffuse interstitial fibrosis) – stiffness of the lungs + recoil of the lungs to a smaller resting volume FRC RV
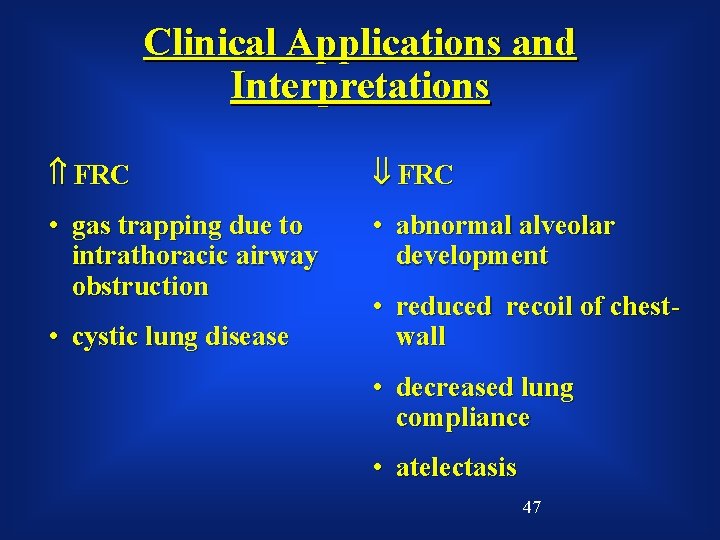
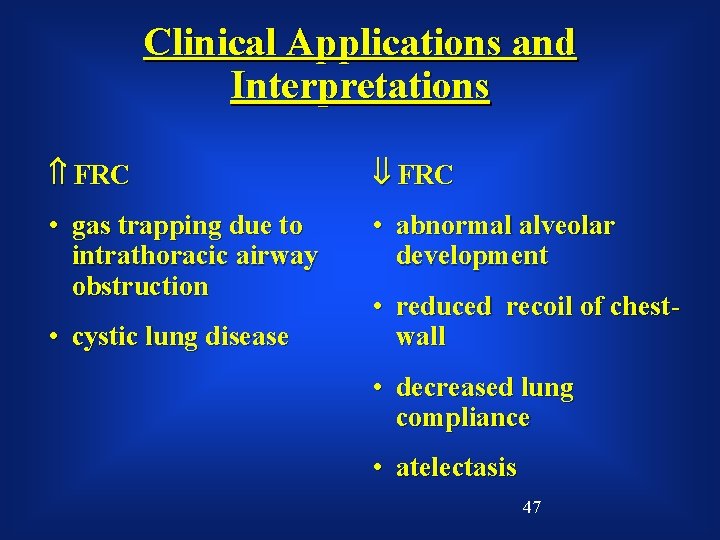
Clinical Applications and Interpretations FRC • gas trapping due to intrathoracic airway obstruction • abnormal alveolar development • cystic lung disease • reduced recoil of chestwall • decreased lung compliance • atelectasis 47
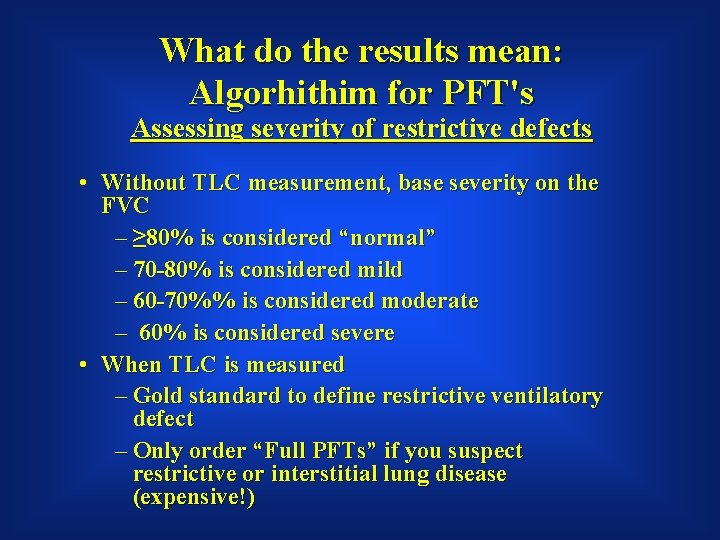
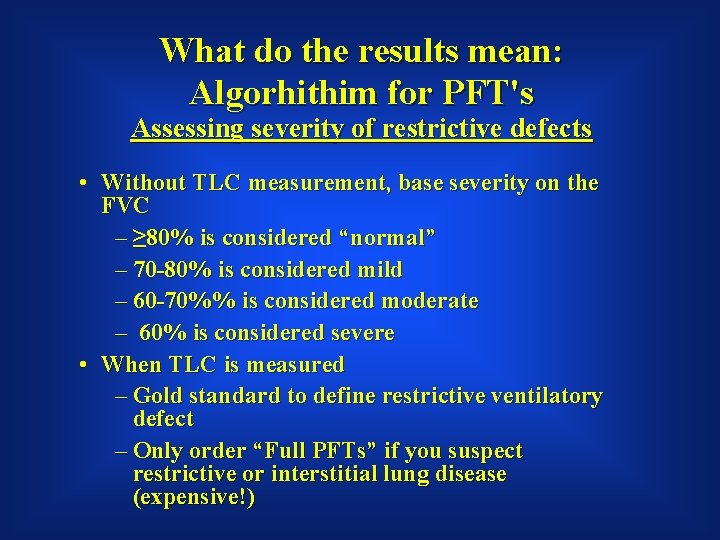
What do the results mean: Algorhithim for PFT's Assessing severity of restrictive defects • Without TLC measurement, base severity on the FVC – ≥ 80% is considered “normal” – 70 -80% is considered mild – 60 -70%% is considered moderate – 60% is considered severe • When TLC is measured – Gold standard to define restrictive ventilatory defect – Only order “Full PFTs” if you suspect restrictive or interstitial lung disease (expensive!)
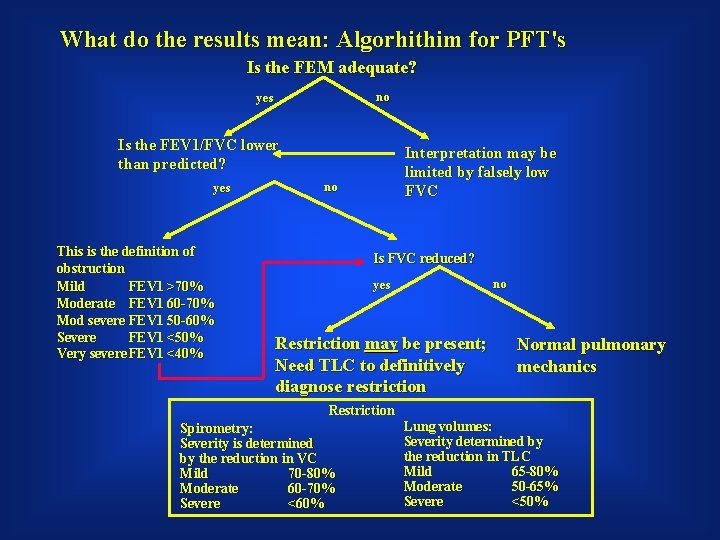
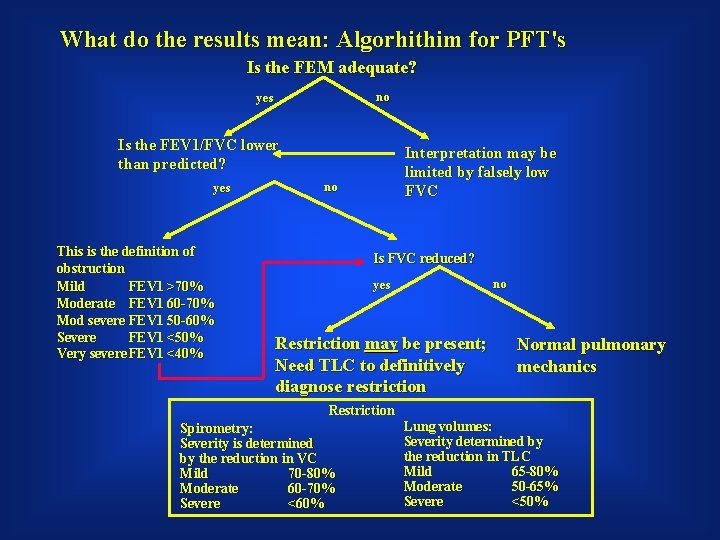
What do the results mean: Algorhithim for PFT's Is the FEM adequate? no y es Is the FEV 1/FVC lower than predicted? y es This is the definition of obstruction Mild FEV 1 >70% Moderate FEV 1 60 -70% Mod severe FEV 1 50 -60% Severe FEV 1 <50% Very severe FEV 1 <40% Interpretation may be limited by falsely low FVC no Is FVC reduced? no y es Restriction may be present; Need TLC to definitively diagnose restriction Normal pulmonary mechanics Restriction Spirometry: Severity is determined by the reduction in VC Mild 70 -80% Moderate 60 -70% Severe <60% Lung volumes: Severity determined by the reduction in TLC Mild 65 -80% Moderate 50 -65% Severe <50%
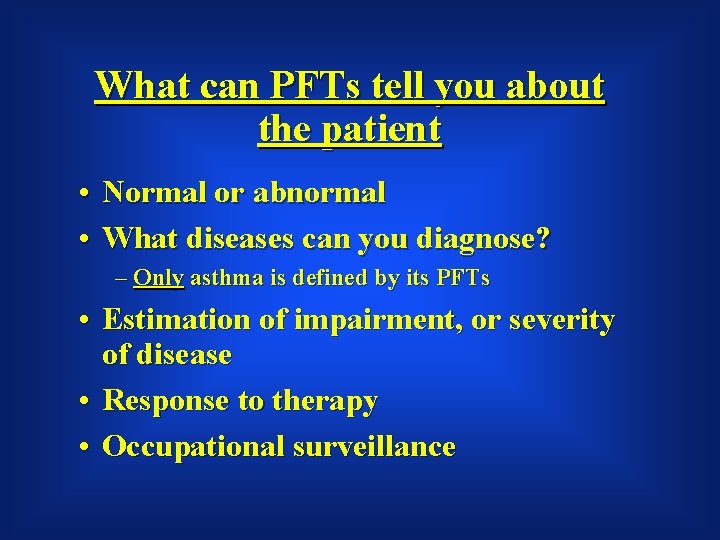
What can PFTs tell you about the patient • Normal or abnormal • What diseases can you diagnose? – Only asthma is defined by its PFTs • Estimation of impairment, or severity of disease • Response to therapy • Occupational surveillance
What PFTs cannot tell you • Does the degree of abnormality explain the patients symptoms? • “Normality” does not exclude the presence of disease • Abnormal test may not reflect loss of lung function
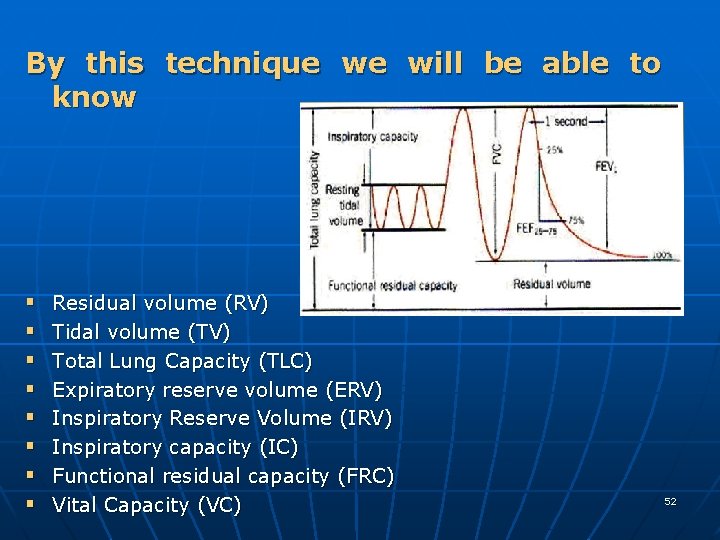
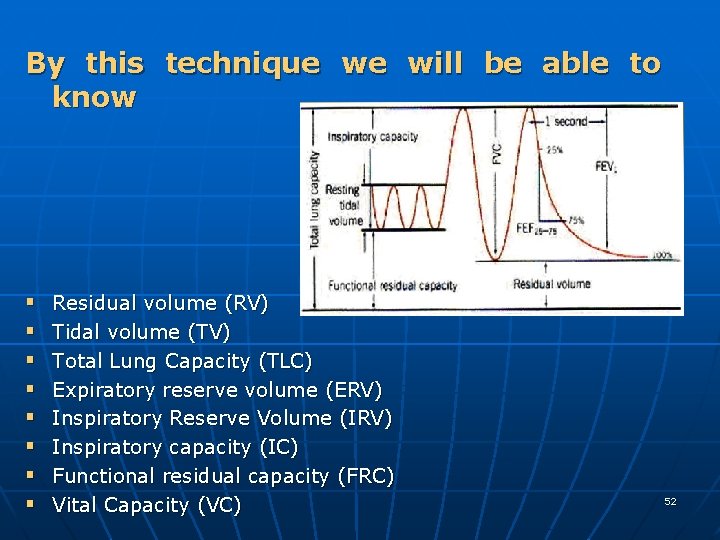
By this technique we will be able to know § § § § Residual volume (RV) Tidal volume (TV) Total Lung Capacity (TLC) Expiratory reserve volume (ERV) Inspiratory Reserve Volume (IRV) Inspiratory capacity (IC) Functional residual capacity (FRC) Vital Capacity (VC) 52
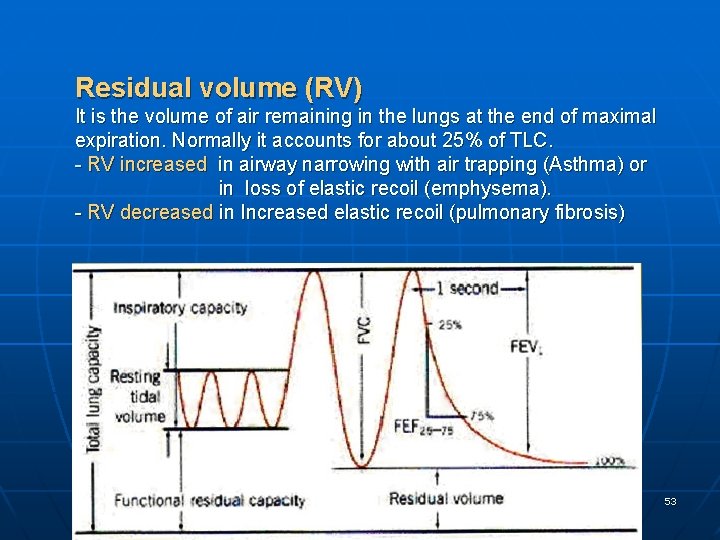
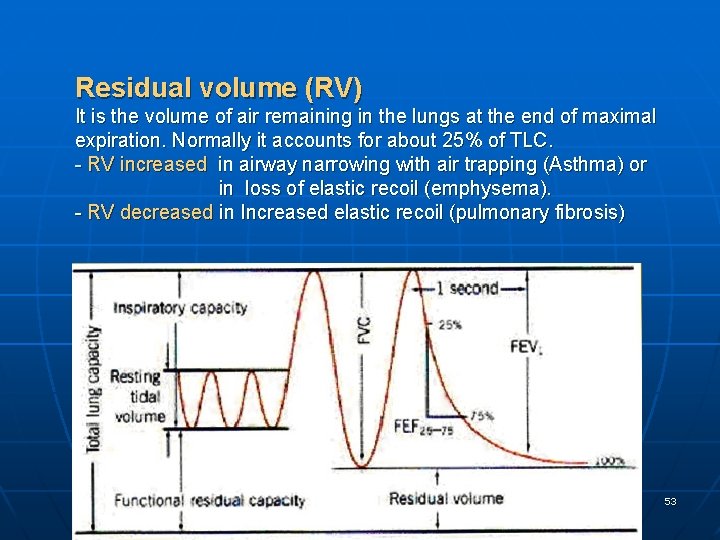
Residual volume (RV) It is the volume of air remaining in the lungs at the end of maximal expiration. Normally it accounts for about 25% of TLC. - RV increased in airway narrowing with air trapping (Asthma) or in loss of elastic recoil (emphysema). - RV decreased in Increased elastic recoil (pulmonary fibrosis) 53
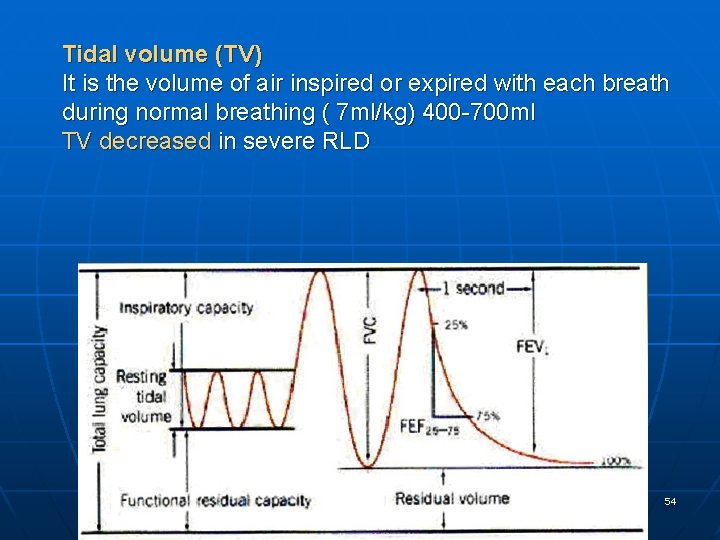
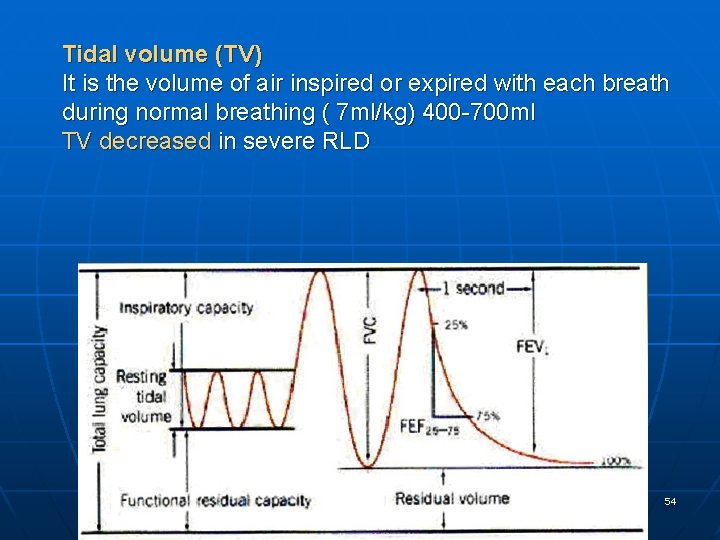
Tidal volume (TV) It is the volume of air inspired or expired with each breath during normal breathing ( 7 ml/kg) 400 -700 ml TV decreased in severe RLD 54
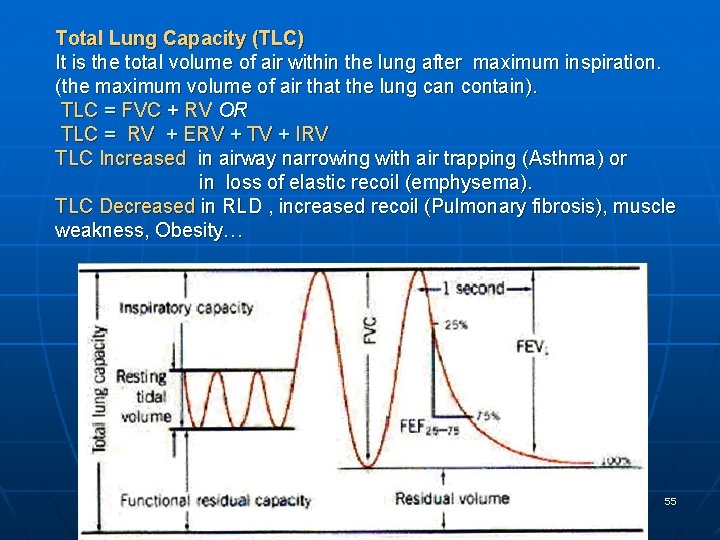
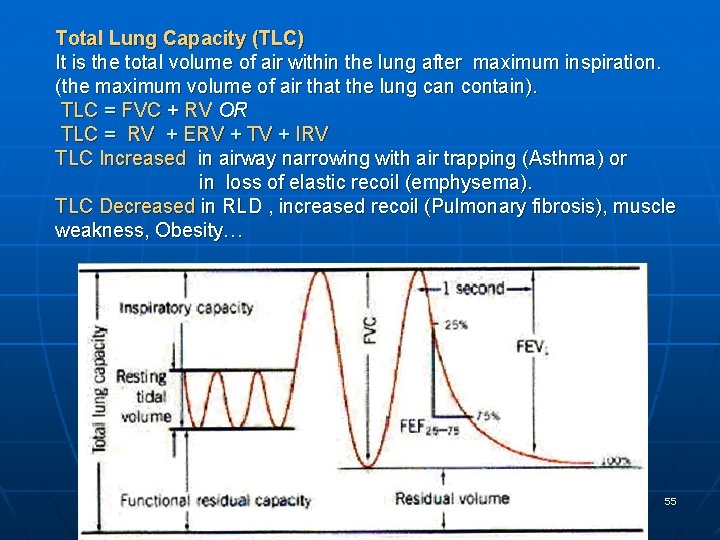
Total Lung Capacity (TLC) It is the total volume of air within the lung after maximum inspiration. (the maximum volume of air that the lung can contain). TLC = FVC + RV OR TLC = RV + ERV + TV + IRV TLC Increased in airway narrowing with air trapping (Asthma) or in loss of elastic recoil (emphysema). TLC Decreased in RLD , increased recoil (Pulmonary fibrosis), muscle weakness, Obesity… 55
56
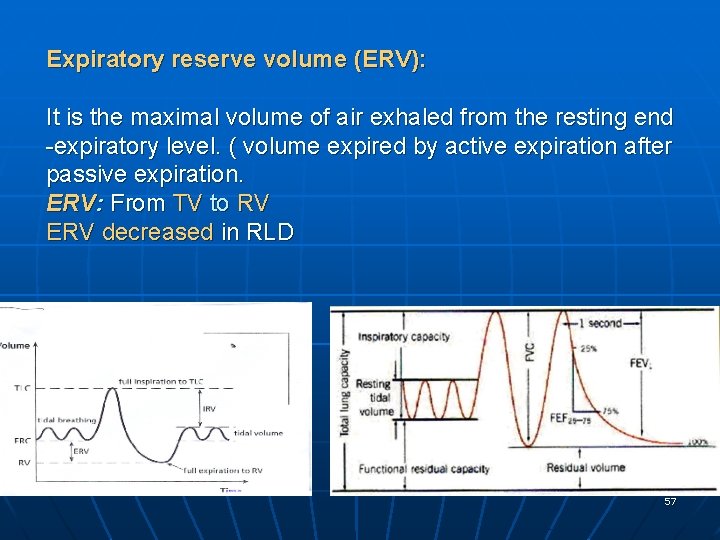
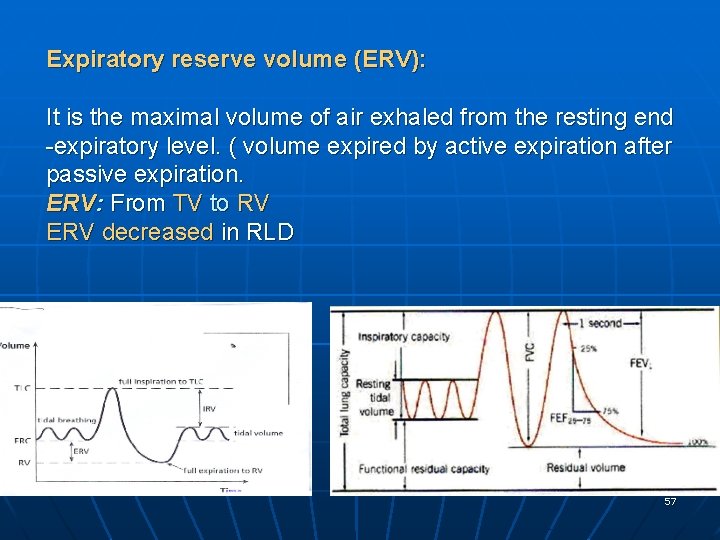
Expiratory reserve volume (ERV): It is the maximal volume of air exhaled from the resting end -expiratory level. ( volume expired by active expiration after passive expiration. ERV: From TV to RV ERV decreased in RLD 57
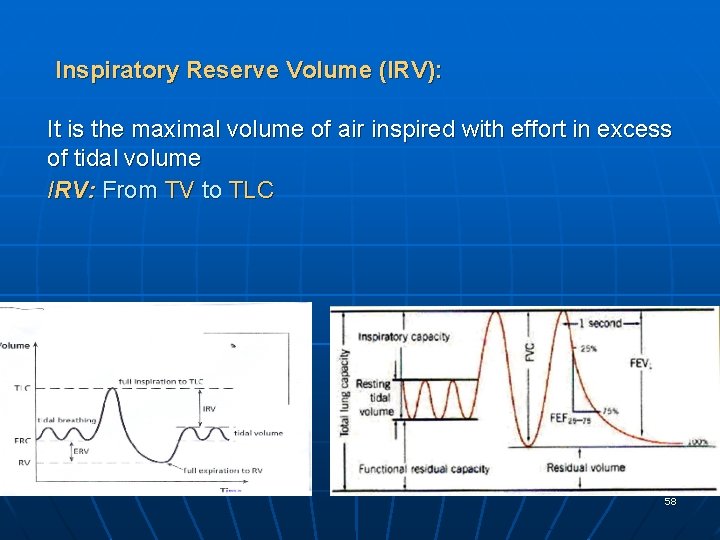
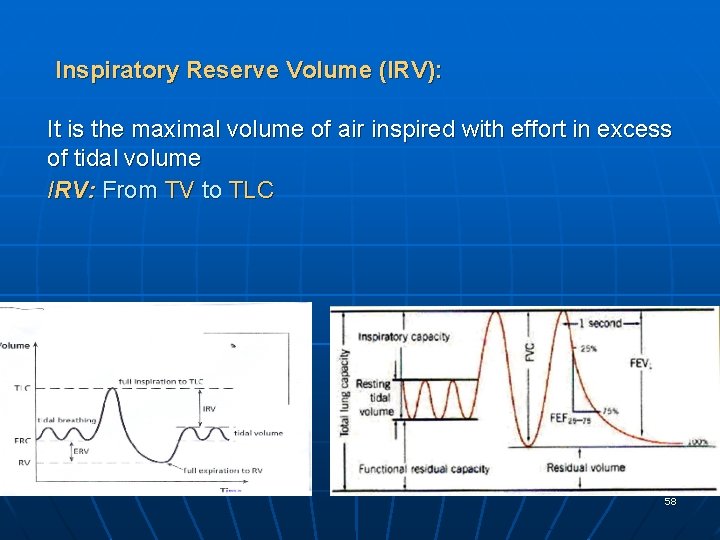
Inspiratory Reserve Volume (IRV): It is the maximal volume of air inspired with effort in excess of tidal volume IRV: From TV to TLC 58
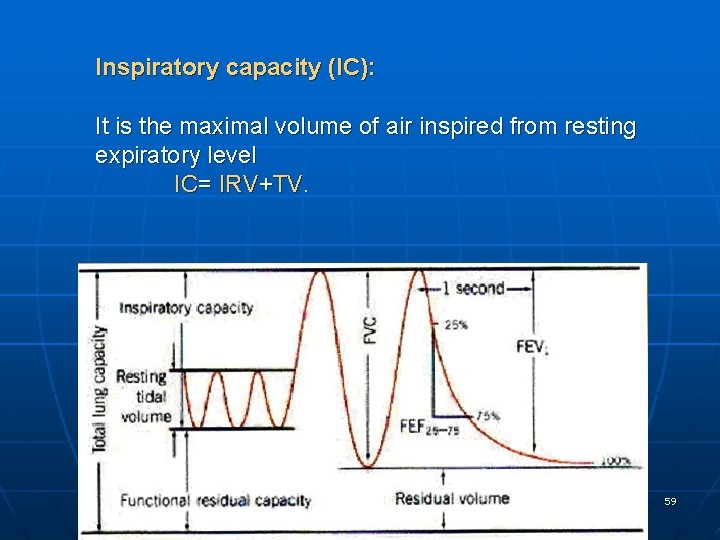
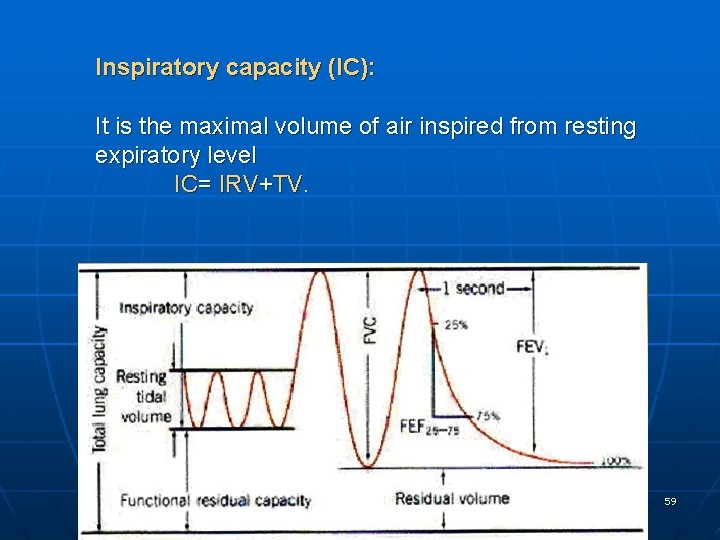
Inspiratory capacity (IC): It is the maximal volume of air inspired from resting expiratory level IC= IRV+TV. 59
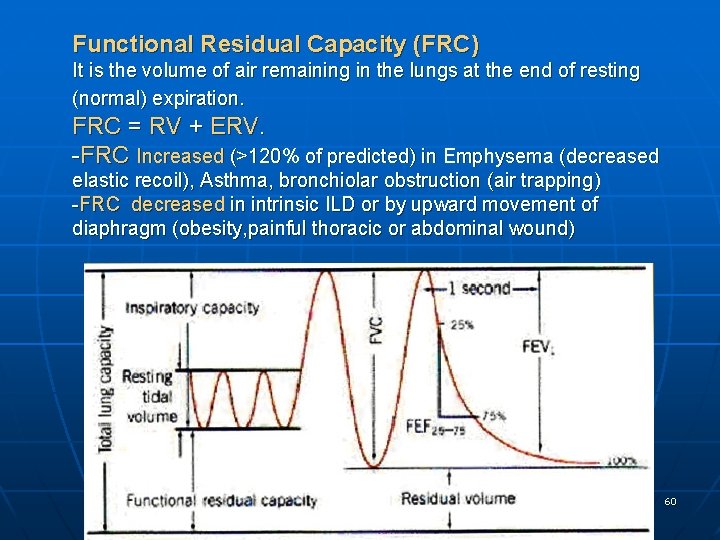
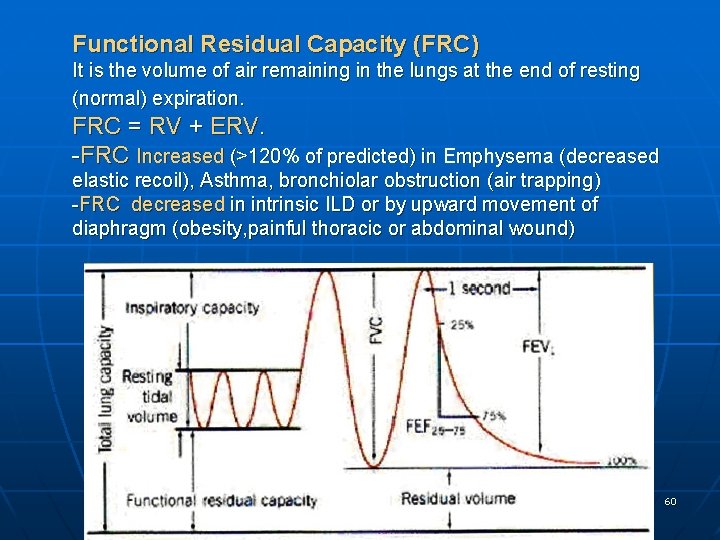
Functional Residual Capacity (FRC) It is the volume of air remaining in the lungs at the end of resting (normal) expiration. FRC = RV + ERV. -FRC Increased (>120% of predicted) in Emphysema (decreased elastic recoil), Asthma, bronchiolar obstruction (air trapping) -FRC decreased in intrinsic ILD or by upward movement of diaphragm (obesity, painful thoracic or abdominal wound) 60
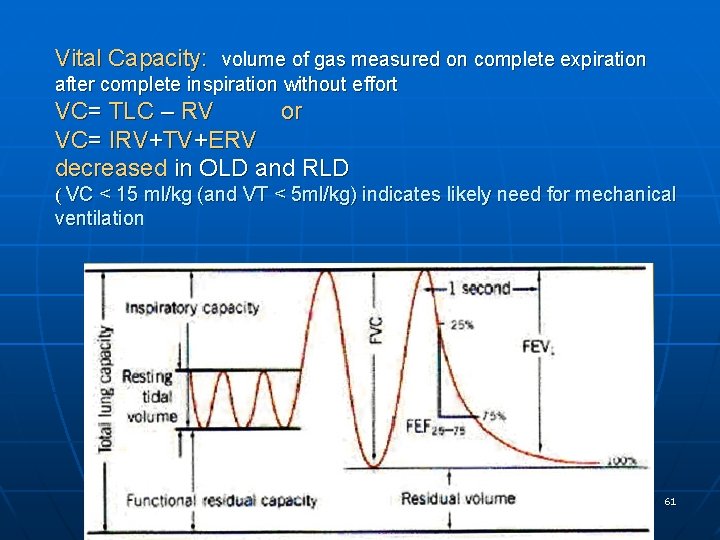
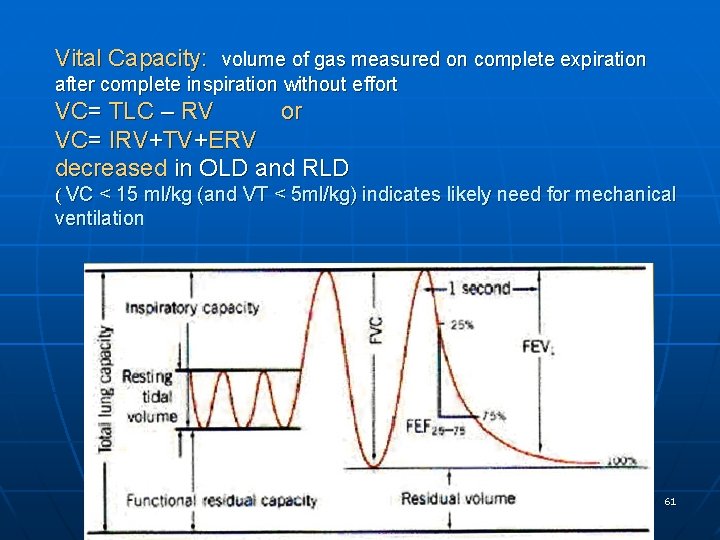
Vital Capacity: volume of gas measured on complete expiration after complete inspiration without effort VC= TLC – RV or VC= IRV+TV+ERV decreased in OLD and RLD ( VC < 15 ml/kg (and VT < 5 ml/kg) indicates likely need for mechanical ventilation 61
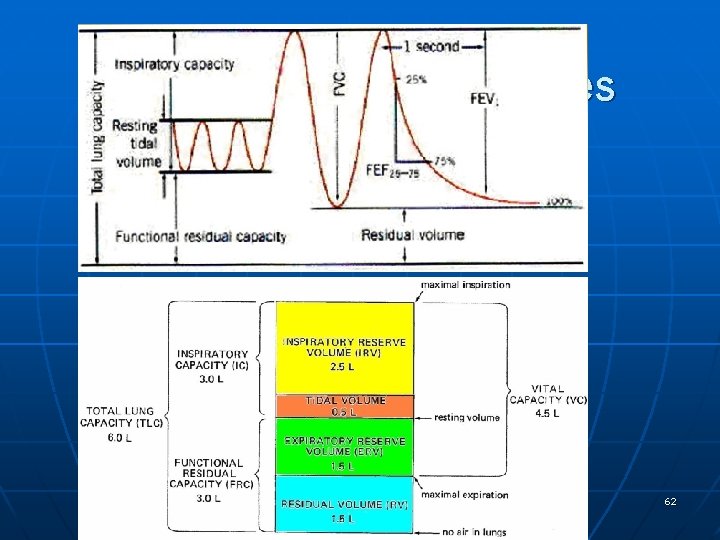
Lung volumes & capacities 62
Lung Volume in Obstructive Lung Disease 63
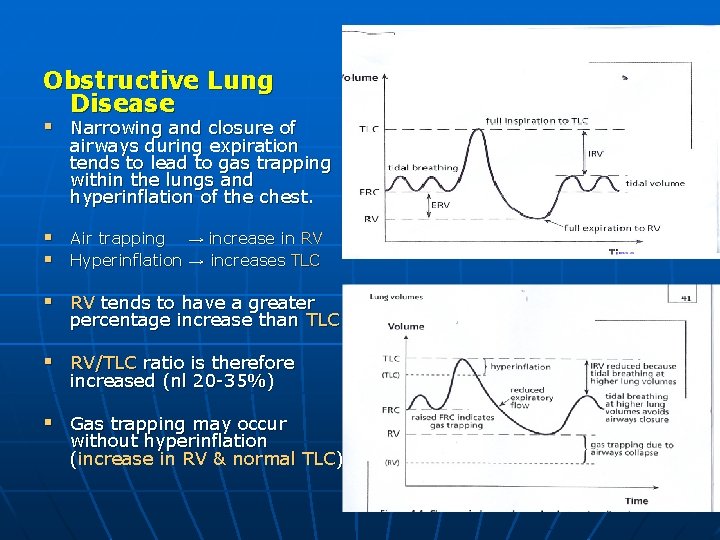
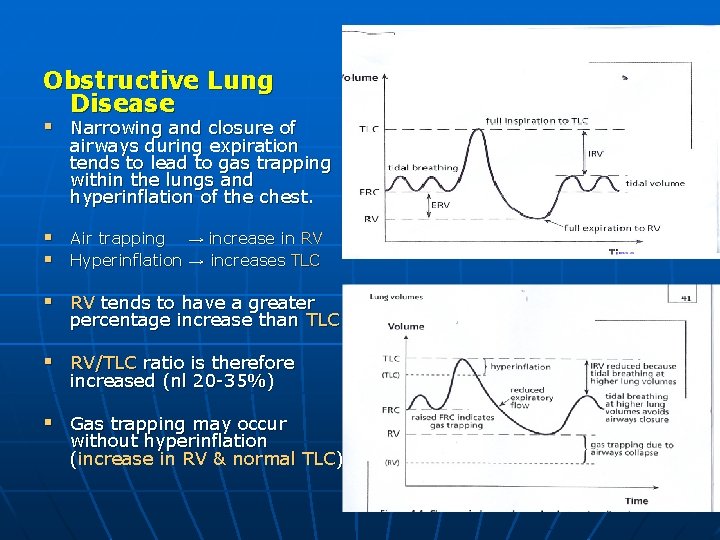
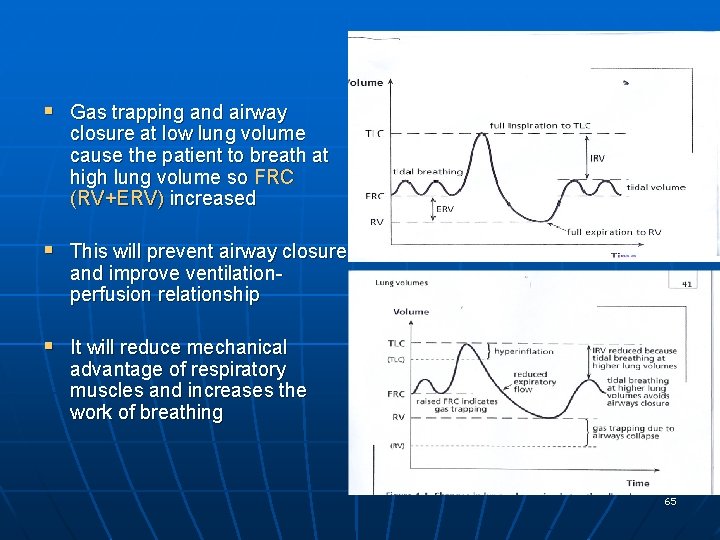
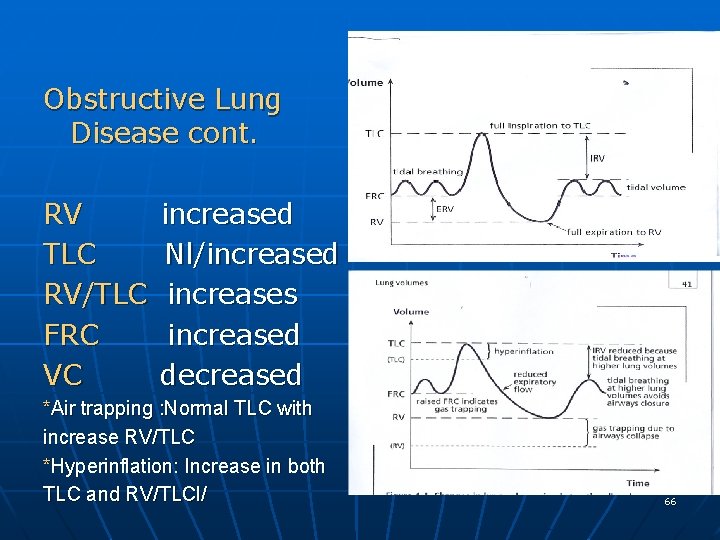
Obstructive Lung Disease § Narrowing and closure of airways during expiration tends to lead to gas trapping within the lungs and hyperinflation of the chest. § Air trapping → increase in RV § Hyperinflation → increases TLC § RV tends to have a greater percentage increase than TLC § RV/TLC ratio is therefore increased (nl 20 -35%) § Gas trapping may occur without hyperinflation (increase in RV & normal TLC) 64
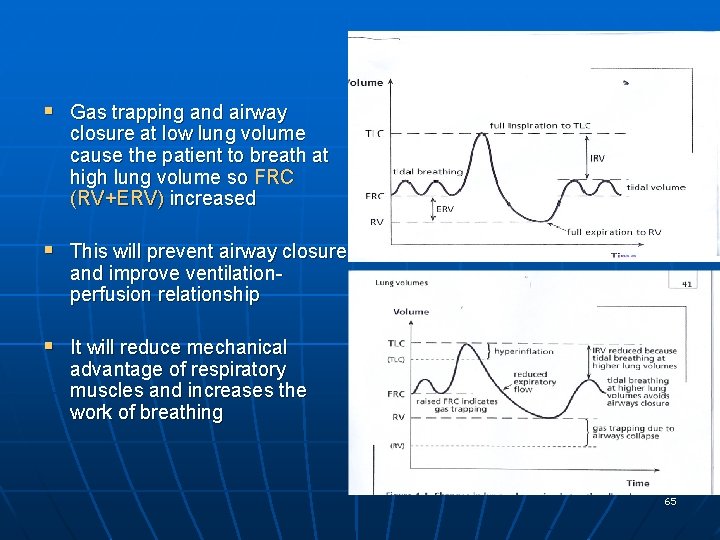
§ Gas trapping and airway closure at low lung volume cause the patient to breath at high lung volume so FRC (RV+ERV) increased § This will prevent airway closure and improve ventilationperfusion relationship § It will reduce mechanical advantage of respiratory muscles and increases the work of breathing 65
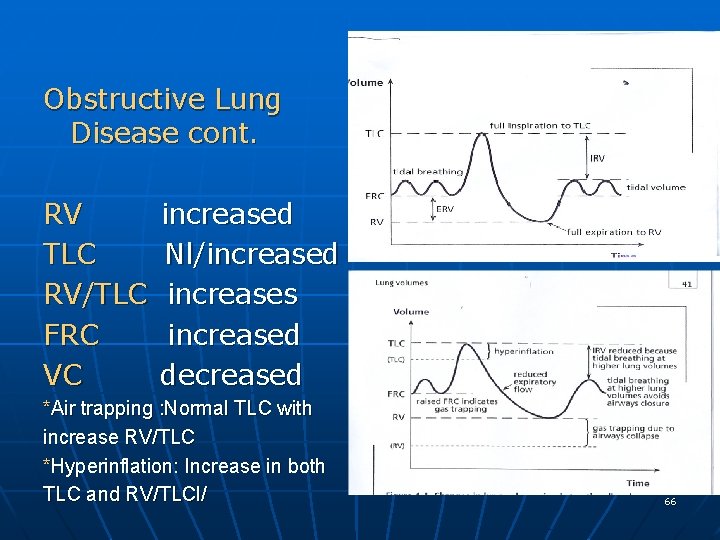
Obstructive Lung Disease cont. RV TLC RV/TLC FRC VC increased Nl/increased increases increased decreased *Air trapping : Normal TLC with increase RV/TLC *Hyperinflation: Increase in both TLC and RV/TLCl/ 66
Lung Volume in Restrictive Lung Disease 67
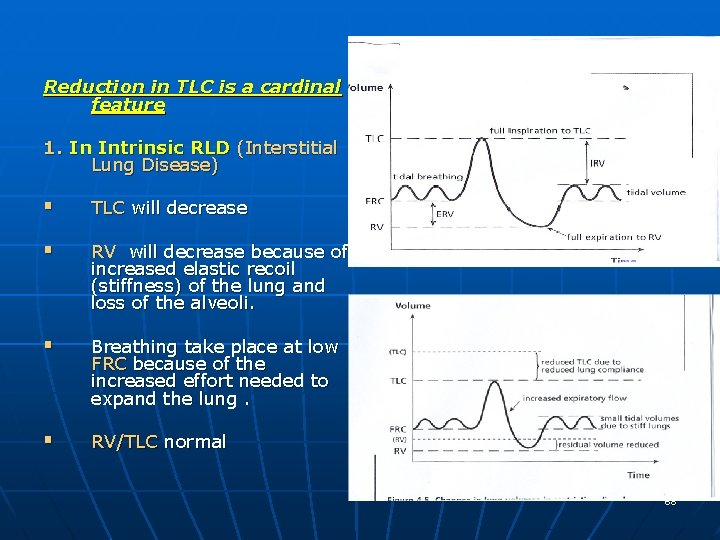
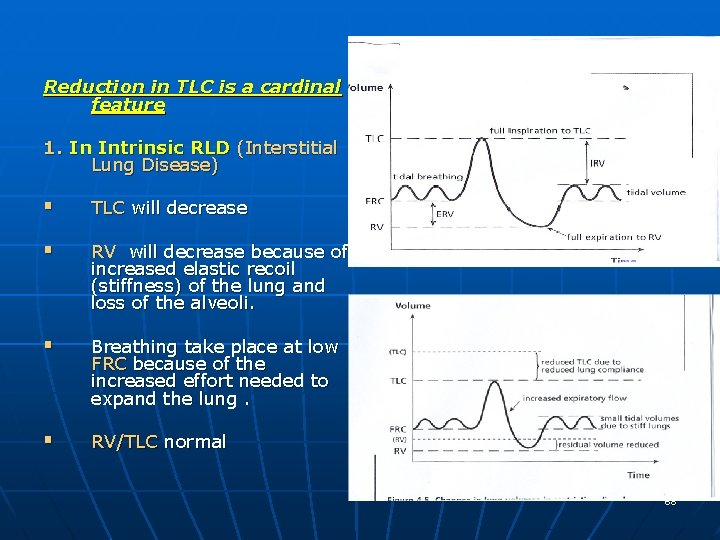
Reduction in TLC is a cardinal feature 1. In Intrinsic RLD (Interstitial Lung Disease) § TLC will decrease § RV will decrease because of increased elastic recoil (stiffness) of the lung and loss of the alveoli. § Breathing take place at low FRC because of the increased effort needed to expand the lung. § RV/TLC normal 68
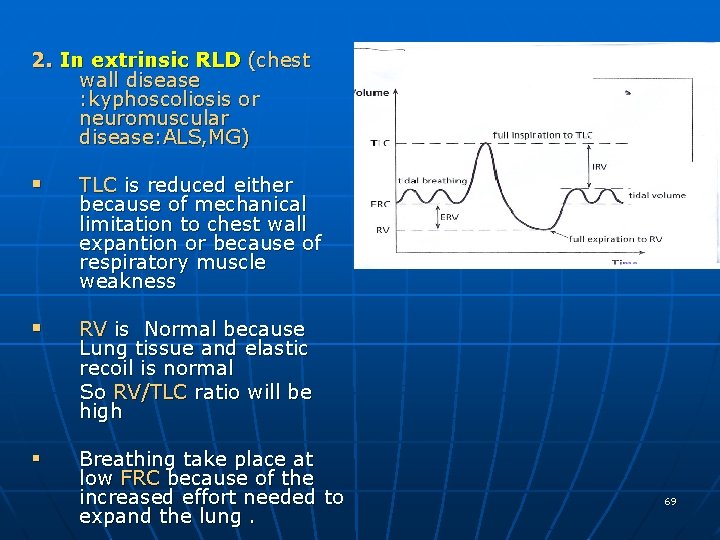
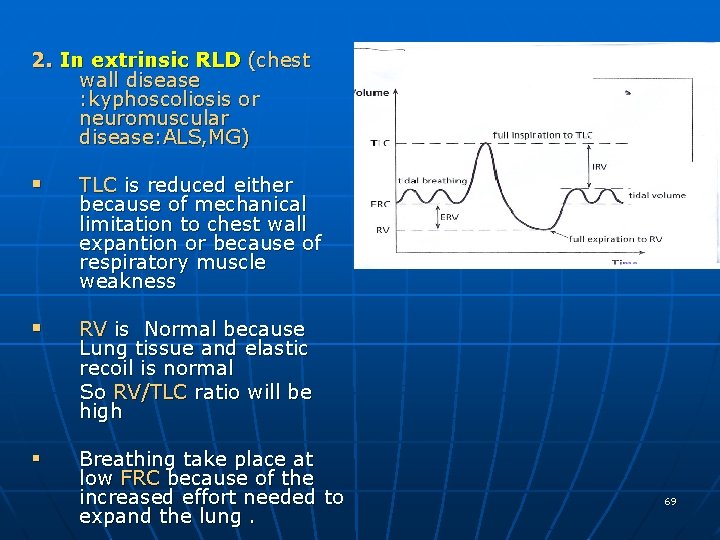
2. In extrinsic RLD (chest wall disease : kyphoscoliosis or neuromuscular disease: ALS, MG) § TLC is reduced either because of mechanical limitation to chest wall expantion or because of respiratory muscle weakness § RV is Normal because Lung tissue and elastic recoil is normal So RV/TLC ratio will be high § Breathing take place at low FRC because of the increased effort needed to expand the lung. 69
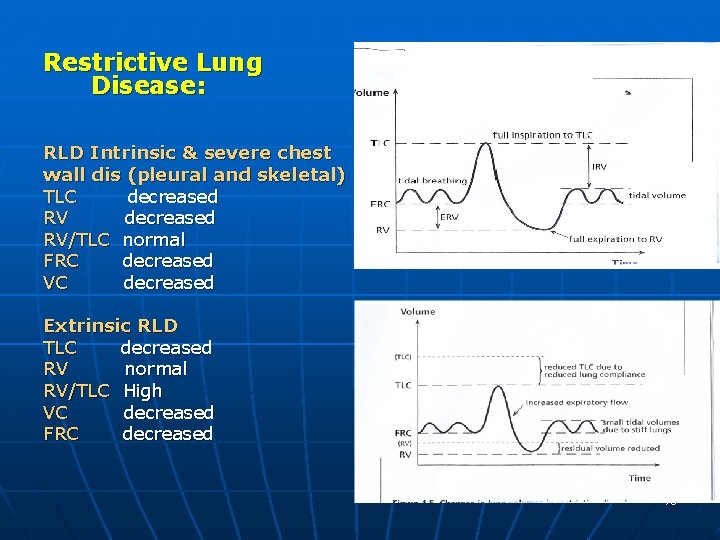
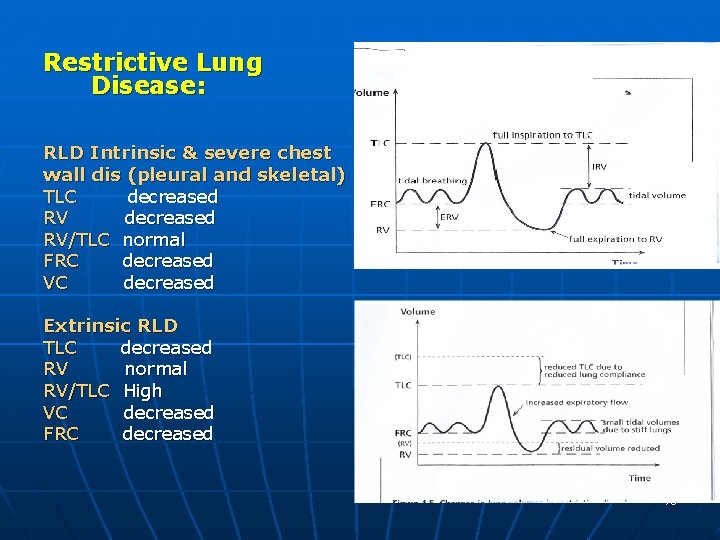
Restrictive Lung Disease: RLD Intrinsic & severe chest wall dis (pleural and skeletal) TLC decreased RV/TLC normal FRC decreased VC decreased Extrinsic RLD TLC decreased RV normal RV/TLC High VC decreased FRC decreased 70
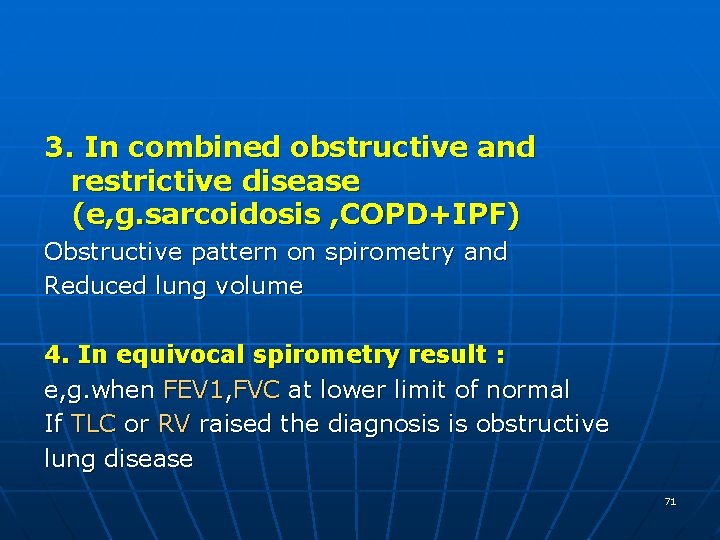
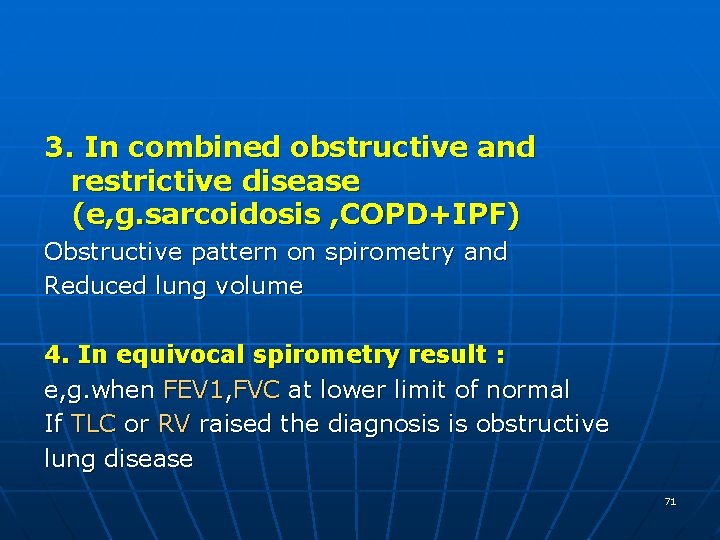
3. In combined obstructive and restrictive disease (e, g. sarcoidosis , COPD+IPF) Obstructive pattern on spirometry and Reduced lung volume 4. In equivocal spirometry result : e, g. when FEV 1, FVC at lower limit of normal If TLC or RV raised the diagnosis is obstructive lung disease 71
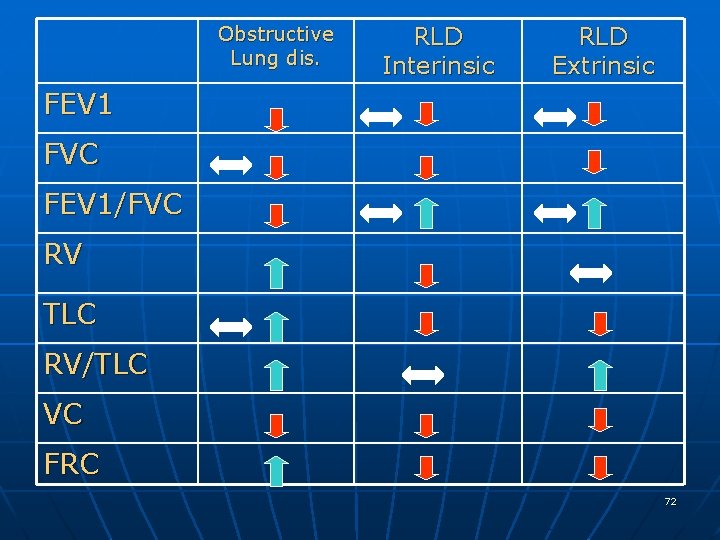
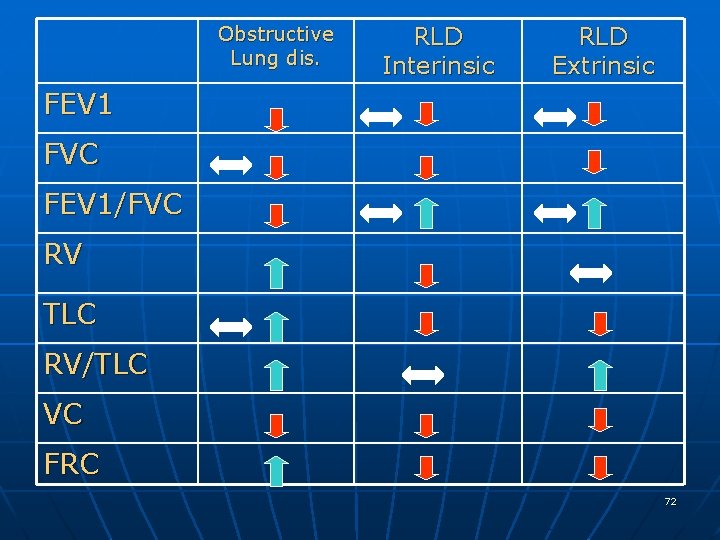
Obstructive Lung dis. RLD Interinsic RLD Extrinsic FEV 1 FVC FEV 1/FVC RV TLC RV/TLC VC FRC 72
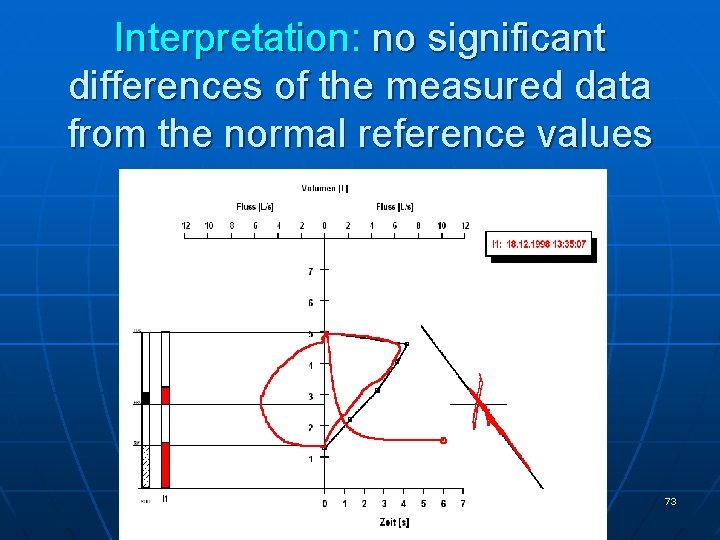
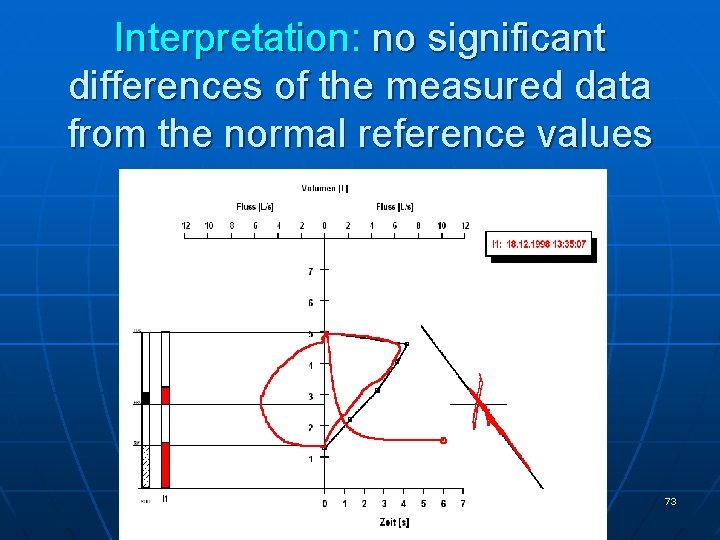
Interpretation: no significant differences of the measured data from the normal reference values 73
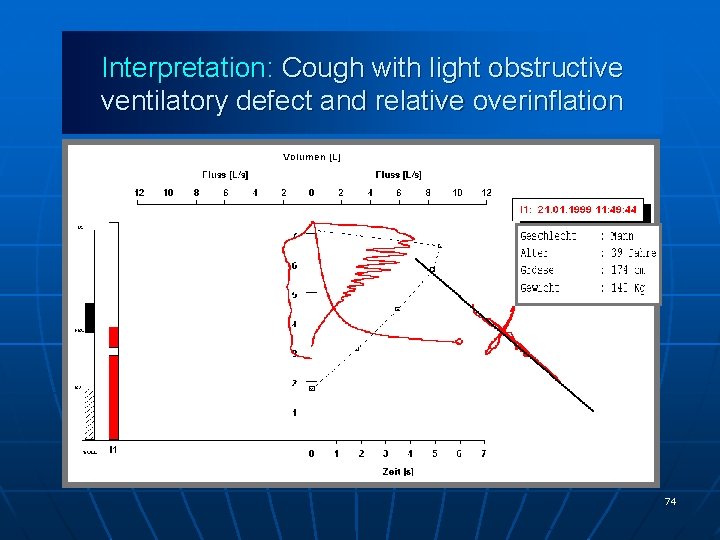
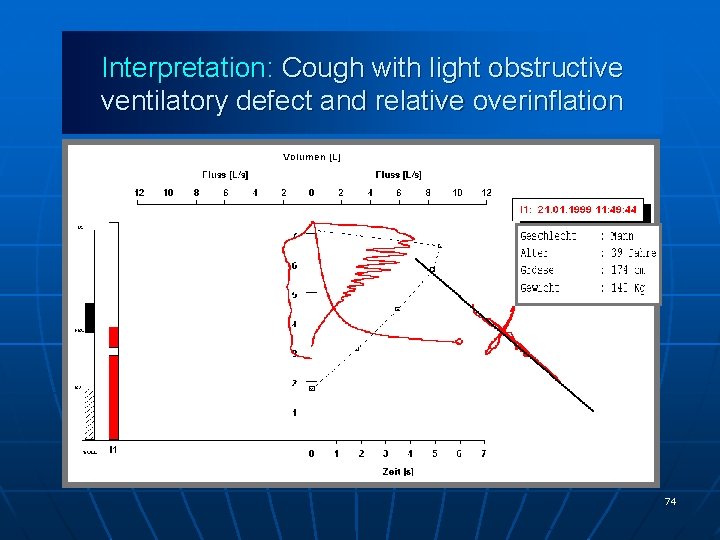
Interpretation: Cough with light obstructive ventilatory defect and relative overinflation 74
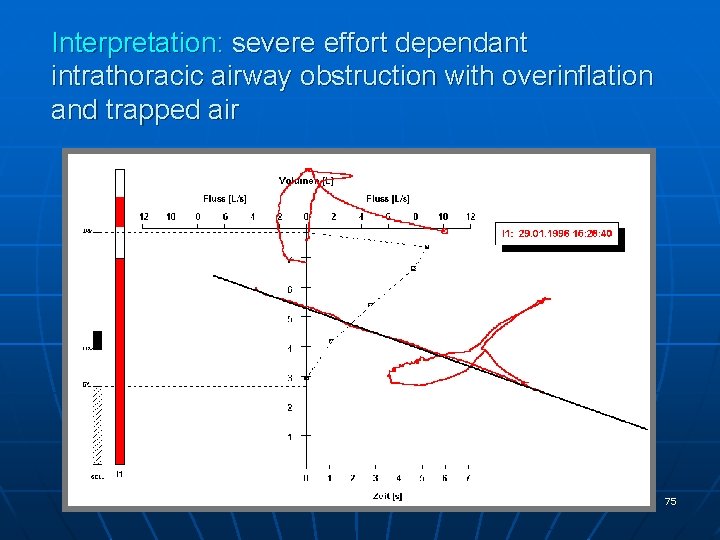
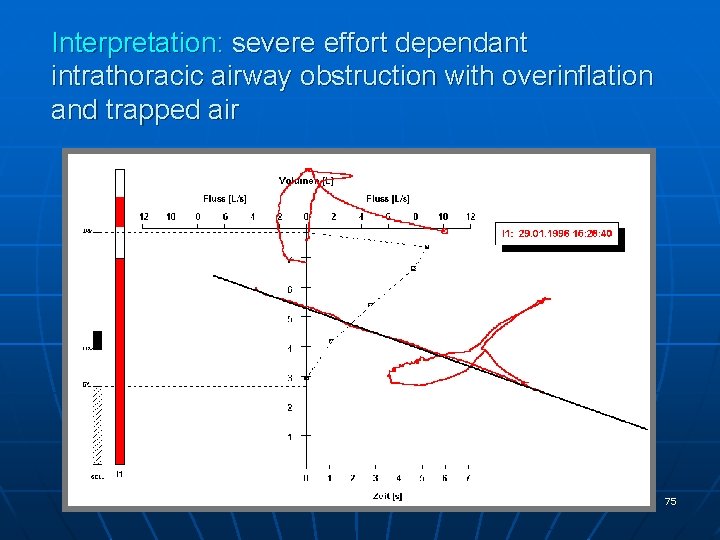
Interpretation: severe effort dependant intrathoracic airway obstruction with overinflation and trapped air 75
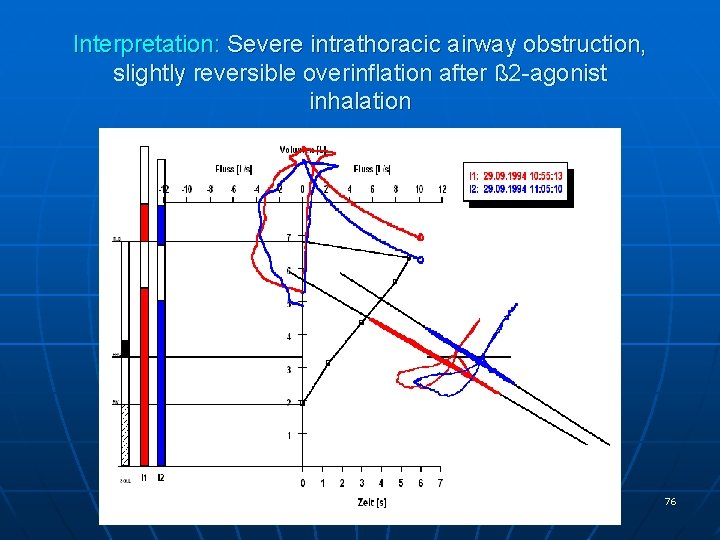
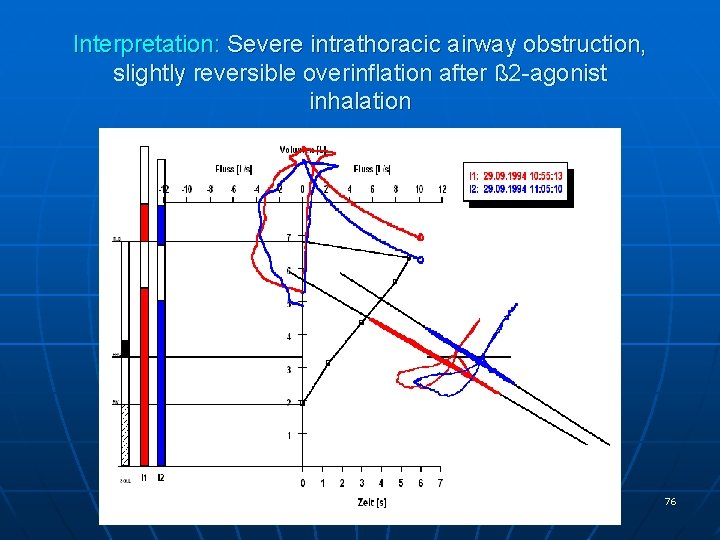
Interpretation: Severe intrathoracic airway obstruction, slightly reversible overinflation after ß 2 -agonist inhalation 76
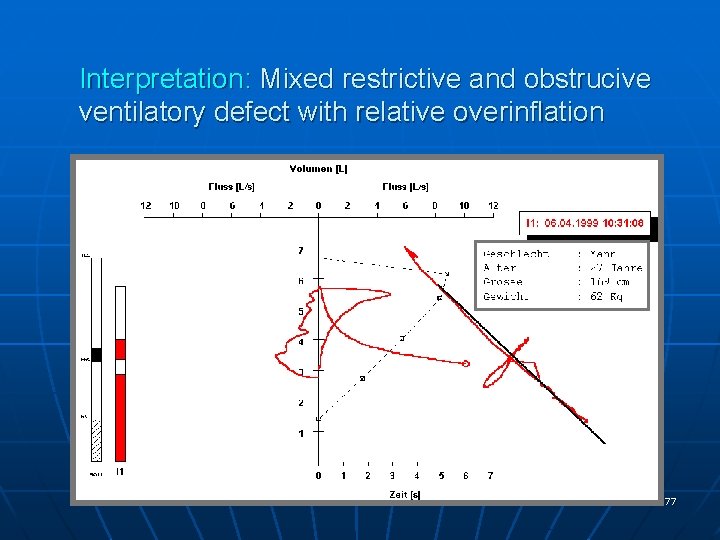
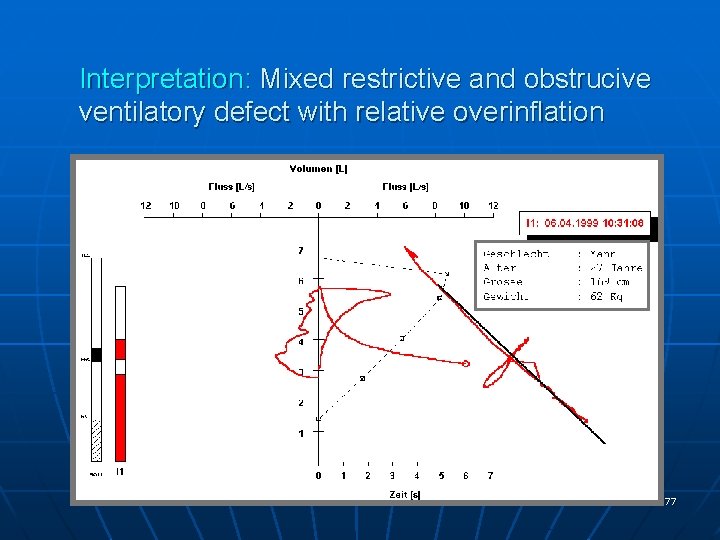
Interpretation: Mixed restrictive and obstrucive ventilatory defect with relative overinflation 77
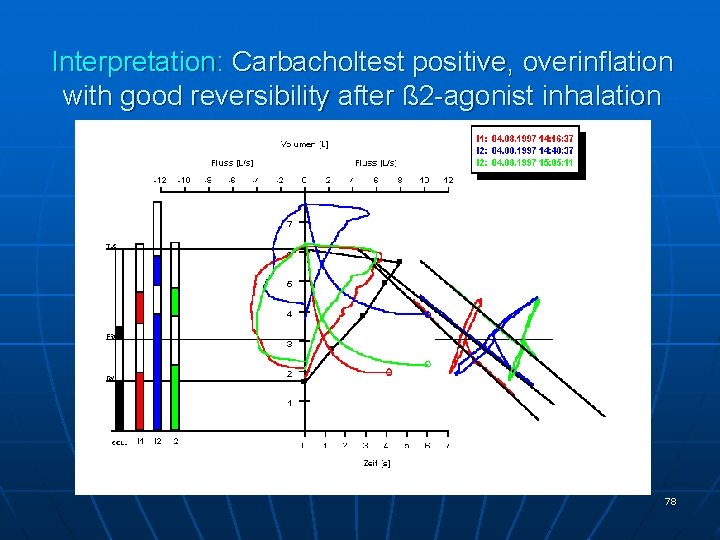
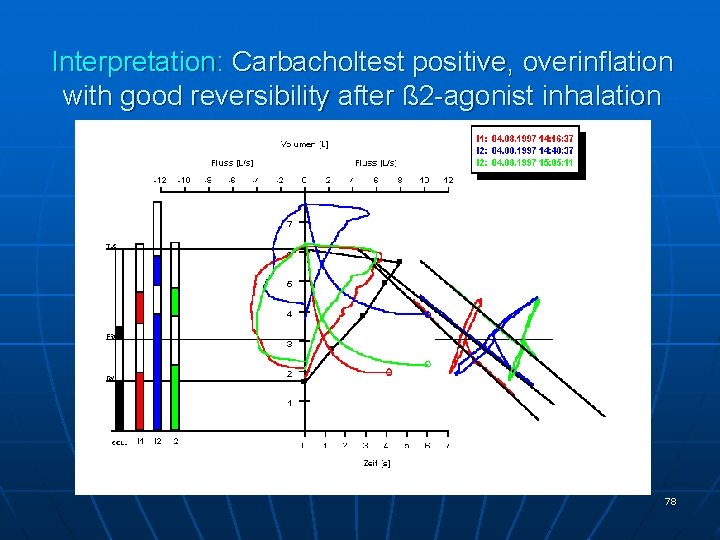
Interpretation: Carbacholtest positive, overinflation with good reversibility after ß 2 -agonist inhalation 78
The infant plethysmograph 79

Infant plethysmography 80
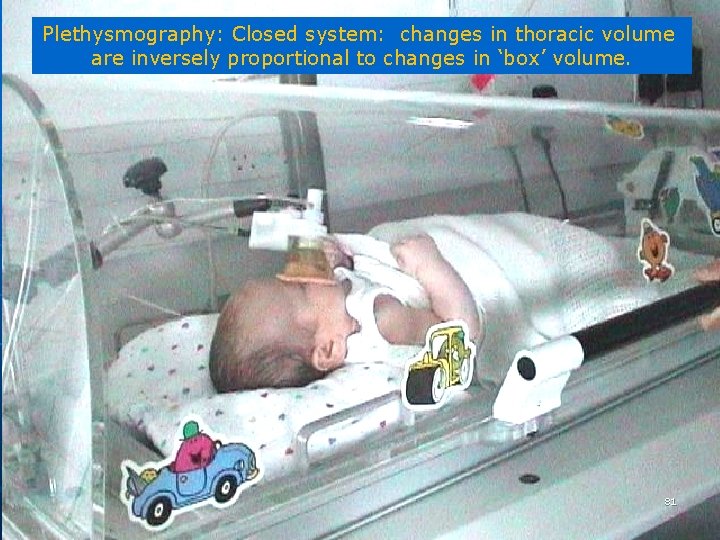
Plethysmography: Closed system: changes in thoracic volume are inversely proportional to changes in ‘box’ volume. 81

82