Current Use and Documentation of Incentive Spirometry and


- Slides: 11
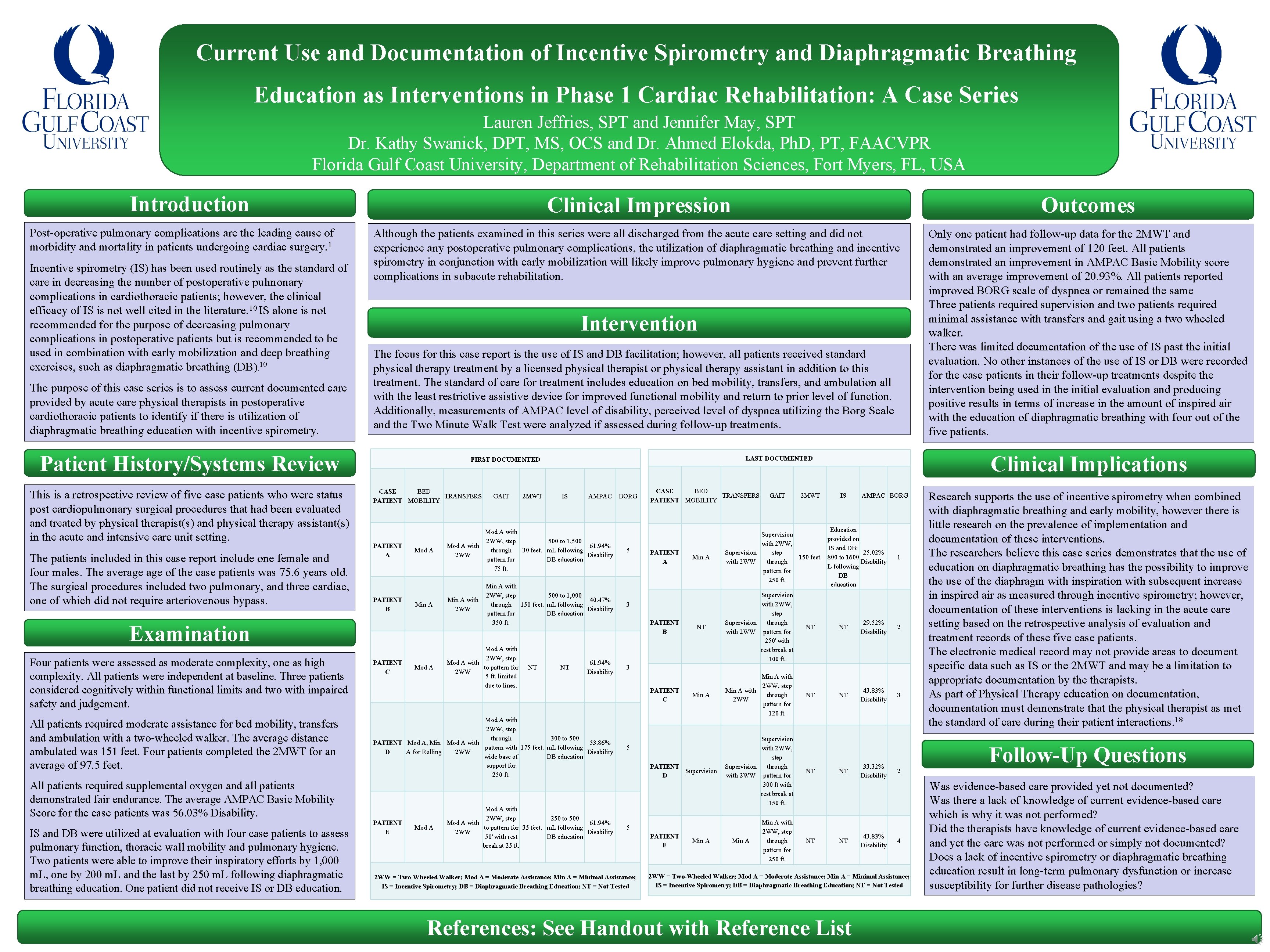
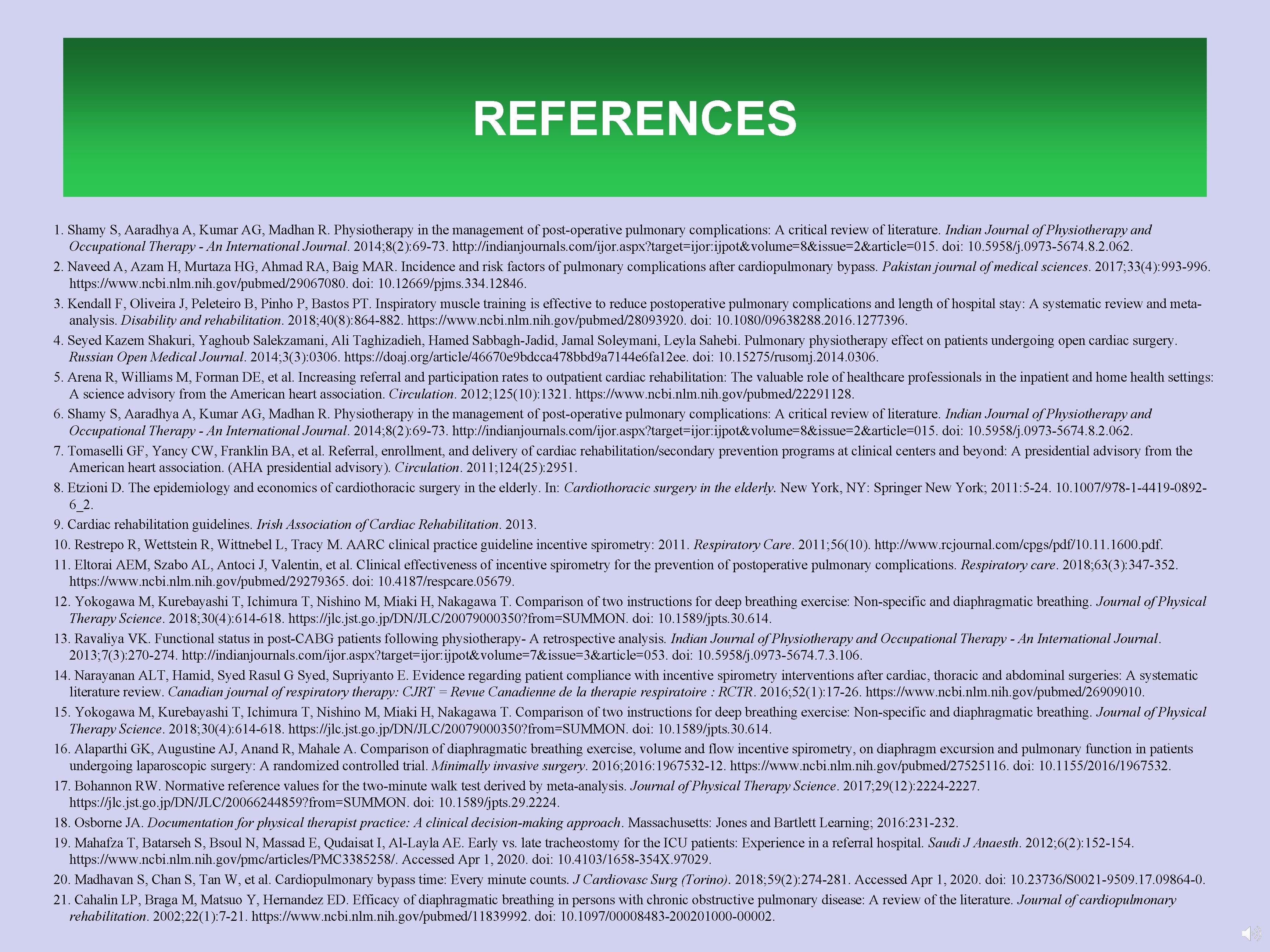
Current Use and Documentation of Incentive Spirometry and Diaphragmatic Breathing Education as Interventions in Phase 1 Cardiac Rehabilitation: A Case Series Lauren Jeffries, SPT and Jennifer May, SPT Dr. Kathy Swanick, DPT, MS, OCS and Dr. Ahmed Elokda, Ph. D, PT, FAACVPR Florida Gulf Coast University, Department of Rehabilitation Sciences, Fort Myers, FL, USA Introduction Post-operative pulmonary complications are the leading cause of morbidity and mortality in patients undergoing cardiac surgery. 1 Incentive spirometry (IS) has been used routinely as the standard of care in decreasing the number of postoperative pulmonary complications in cardiothoracic patients; however, the clinical efficacy of IS is not well cited in the literature. 10 IS alone is not recommended for the purpose of decreasing pulmonary complications in postoperative patients but is recommended to be used in combination with early mobilization and deep breathing exercises, such as diaphragmatic breathing (DB). 10 The purpose of this case series is to assess current documented care provided by acute care physical therapists in postoperative cardiothoracic patients to identify if there is utilization of diaphragmatic breathing education with incentive spirometry. Clinical Impression Outcomes Although the patients examined in this series were all discharged from the acute care setting and did not experience any postoperative pulmonary complications, the utilization of diaphragmatic breathing and incentive spirometry in conjunction with early mobilization will likely improve pulmonary hygiene and prevent further complications in subacute rehabilitation. Only one patient had follow-up data for the 2 MWT and demonstrated an improvement of 120 feet. All patients demonstrated an improvement in AMPAC Basic Mobility score with an average improvement of 20. 93%. All patients reported improved BORG scale of dyspnea or remained the same Three patients required supervision and two patients required minimal assistance with transfers and gait using a two wheeled walker. There was limited documentation of the use of IS past the initial evaluation. No other instances of the use of IS or DB were recorded for the case patients in their follow-up treatments despite the intervention being used in the initial evaluation and producing positive results in terms of increase in the amount of inspired air with the education of diaphragmatic breathing with four out of the five patients. Intervention The focus for this case report is the use of IS and DB facilitation; however, all patients received standard physical therapy treatment by a licensed physical therapist or physical therapy assistant in addition to this treatment. The standard of care for treatment includes education on bed mobility, transfers, and ambulation all with the least restrictive assistive device for improved functional mobility and return to prior level of function. Additionally, measurements of AMPAC level of disability, perceived level of dyspnea utilizing the Borg Scale and the Two Minute Walk Test were analyzed if assessed during follow-up treatments. Patient History/Systems Review This is a retrospective review of five case patients who were status post cardiopulmonary surgical procedures that had been evaluated and treated by physical therapist(s) and physical therapy assistant(s) in the acute and intensive care unit setting. The patients included in this case report include one female and four males. The average of the case patients was 75. 6 years old. The surgical procedures included two pulmonary, and three cardiac, one of which did not require arteriovenous bypass. CASE BED TRANSFERS PATIENT MOBILITY PATIENT A PATIENT B GAIT 2 MWT IS AMPAC Mod A with 2 WW, step 500 to 1, 500 Mod A with 61. 94% through 30 feet. m. L following 2 WW Disability pattern for DB education 75 ft. Min A with 2 WW, step 500 to 1, 000 40. 47% through 150 feet. m. L following Disability pattern for DB education 350 ft. Examination Min A with 2 WW Mod A with 2 WW, step Mod A with to pattern for 2 WW 5 ft. limited due to lines. Four patients were assessed as moderate complexity, one as high complexity. All patients were independent at baseline. Three patients considered cognitively within functional limits and two with impaired safety and judgement. PATIENT C All patients required moderate assistance for bed mobility, transfers and ambulation with a two-wheeled walker. The average distance ambulated was 151 feet. Four patients completed the 2 MWT for an average of 97. 5 feet. Mod A with 2 WW, step through 300 to 500 PATIENT Mod A, Min Mod A with 53. 86% pattern with 175 feet. m. L following D A for Rolling 2 WW Disability DB education wide base of support for 250 ft. Mod A All patients required supplemental oxygen and all patients demonstrated fair endurance. The average AMPAC Basic Mobility Score for the case patients was 56. 03% Disability. IS and DB were utilized at evaluation with four case patients to assess pulmonary function, thoracic wall mobility and pulmonary hygiene. Two patients were able to improve their inspiratory efforts by 1, 000 m. L, one by 200 m. L and the last by 250 m. L following diaphragmatic breathing education. One patient did not receive IS or DB education. PATIENT E Mod A NT Clinical Implications LAST DOCUMENTED FIRST DOCUMENTED NT 61. 94% Disability Mod A with 2 WW, step 250 to 500 Mod A with 61. 94% to pattern for 35 feet. m. L following 2 WW Disability 50' with rest DB education break at 25 ft. BORG 5 CASE BED TRANSFERS PATIENT MOBILITY PATIENT A 2 MWT IS AMPAC BORG Education Supervision provided on with 2 WW, IS and DB: Supervision step 25. 02% 150 feet. 800 to 1600 with 2 WW Disability through L following pattern for DB 250 ft. education 1 NT Supervision with 2 WW, step Supervision through with 2 WW pattern for 250' with rest break at 100 ft. NT NT 29. 52% Disability 2 Min A with 2 WW, step Min A with through 2 WW pattern for 120 ft. NT NT 43. 83% Disability 3 Min A 3 PATIENT B GAIT 3 PATIENT C 5 PATIENT Supervision D Supervision with 2 WW, step Supervision through with 2 WW pattern for 300 ft with rest break at 150 ft. NT Min A with 2 WW, step through pattern for 250 ft. NT 5 2 WW = Two-Wheeled Walker; Mod A = Moderate Assistance; Min A = Minimal Assistance; IS = Incentive Spirometry; DB = Diaphragmatic Breathing Education; NT = Not Tested PATIENT E Min A NT NT 33. 32% Disability 43. 83% Disability Follow-Up Questions 2 4 2 WW = Two-Wheeled Walker; Mod A = Moderate Assistance; Min A = Minimal Assistance; IS = Incentive Spirometry; DB = Diaphragmatic Breathing Education; NT = Not Tested References: See Handout with Reference List Research supports the use of incentive spirometry when combined with diaphragmatic breathing and early mobility, however there is little research on the prevalence of implementation and documentation of these interventions. The researchers believe this case series demonstrates that the use of education on diaphragmatic breathing has the possibility to improve the use of the diaphragm with inspiration with subsequent increase in inspired air as measured through incentive spirometry; however, documentation of these interventions is lacking in the acute care setting based on the retrospective analysis of evaluation and treatment records of these five case patients. The electronic medical record may not provide areas to document specific data such as IS or the 2 MWT and may be a limitation to appropriate documentation by therapists. As part of Physical Therapy education on documentation, documentation must demonstrate that the physical therapist as met the standard of care during their patient interactions. 18 Was evidence-based care provided yet not documented? Was there a lack of knowledge of current evidence-based care which is why it was not performed? Did therapists have knowledge of current evidence-based care and yet the care was not performed or simply not documented? Does a lack of incentive spirometry or diaphragmatic breathing education result in long-term pulmonary dysfunction or increase susceptibility for further disease pathologies?
INTRODUCTION • Post-operative pulmonary complications are the leading cause of morbidity 1 and mortality in patients undergoing cardiac surgery. • Incentive spirometry (IS) has been used routinely as the standard of care in decreasing the number of postoperative pulmonary complications in cardiothoracic patients; however, the clinical efficacy of IS is not well cited 10 in the literature. IS alone is not recommended for the purpose of decreasing pulmonary complications in postoperative patients but is recommended to be used in combination with early mobilization and deep breathing 10 exercises, such as diaphragmatic breathing (DB). • The purpose of this case series is to assess current documented care provided by acute care physical therapists in postoperative cardiothoracic patients to identify if there is utilization of diaphragmatic breathing education with incentive spirometry.
PATIENT HISTORY/SYSTEMS REVIEW • This is a retrospective review of five case patients who were status post cardiopulmonary surgical procedures that had been evaluated and treated by physical therapist(s) and physical therapy assistant(s) in the acute and intensive care unit setting. • The patients included in this case report include one female and four males. The average of the case patients was 75. 6 years old. The surgical procedures included two pulmonary, and three cardiac, one of which did not require arteriovenous bypass.
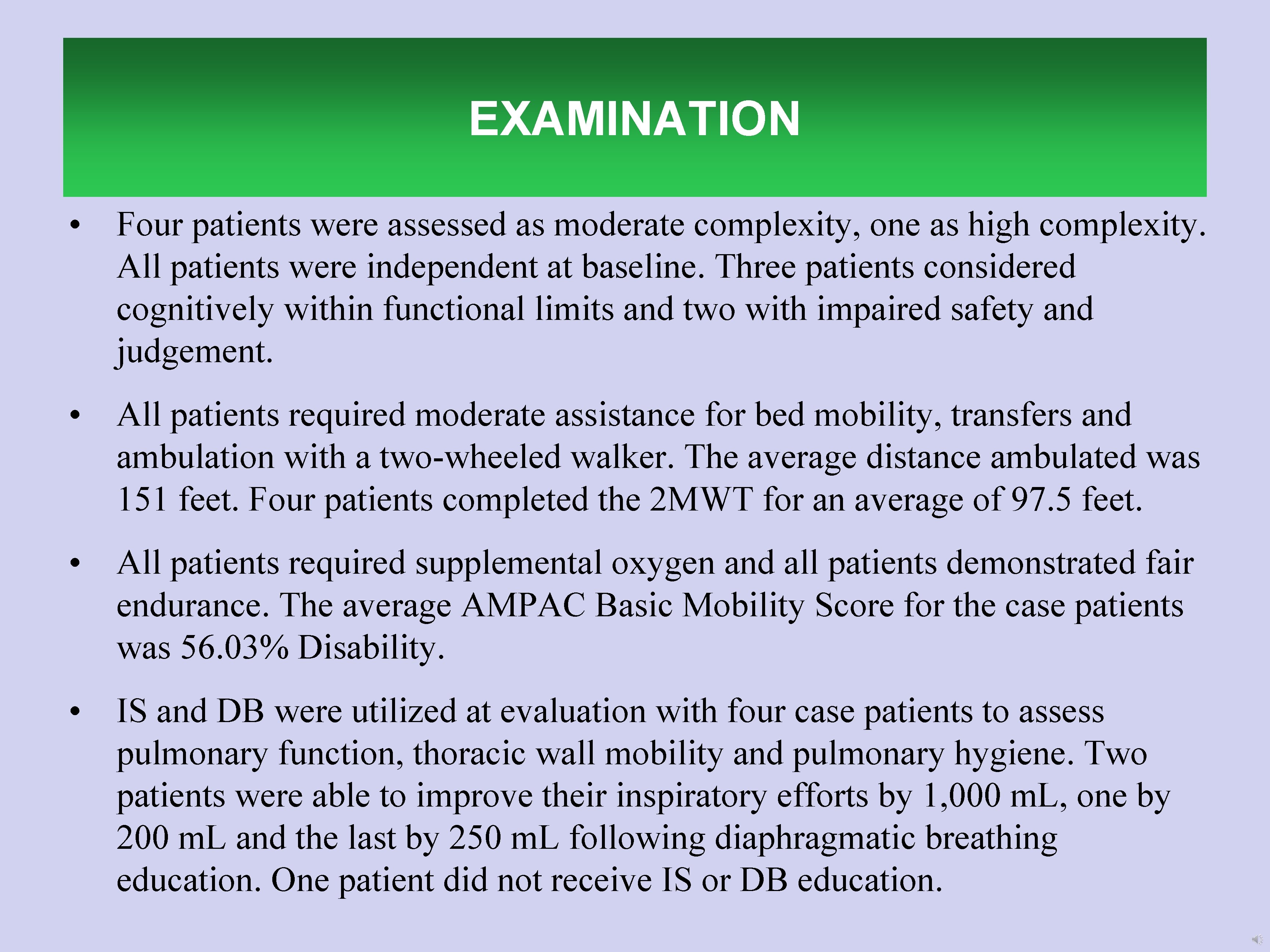
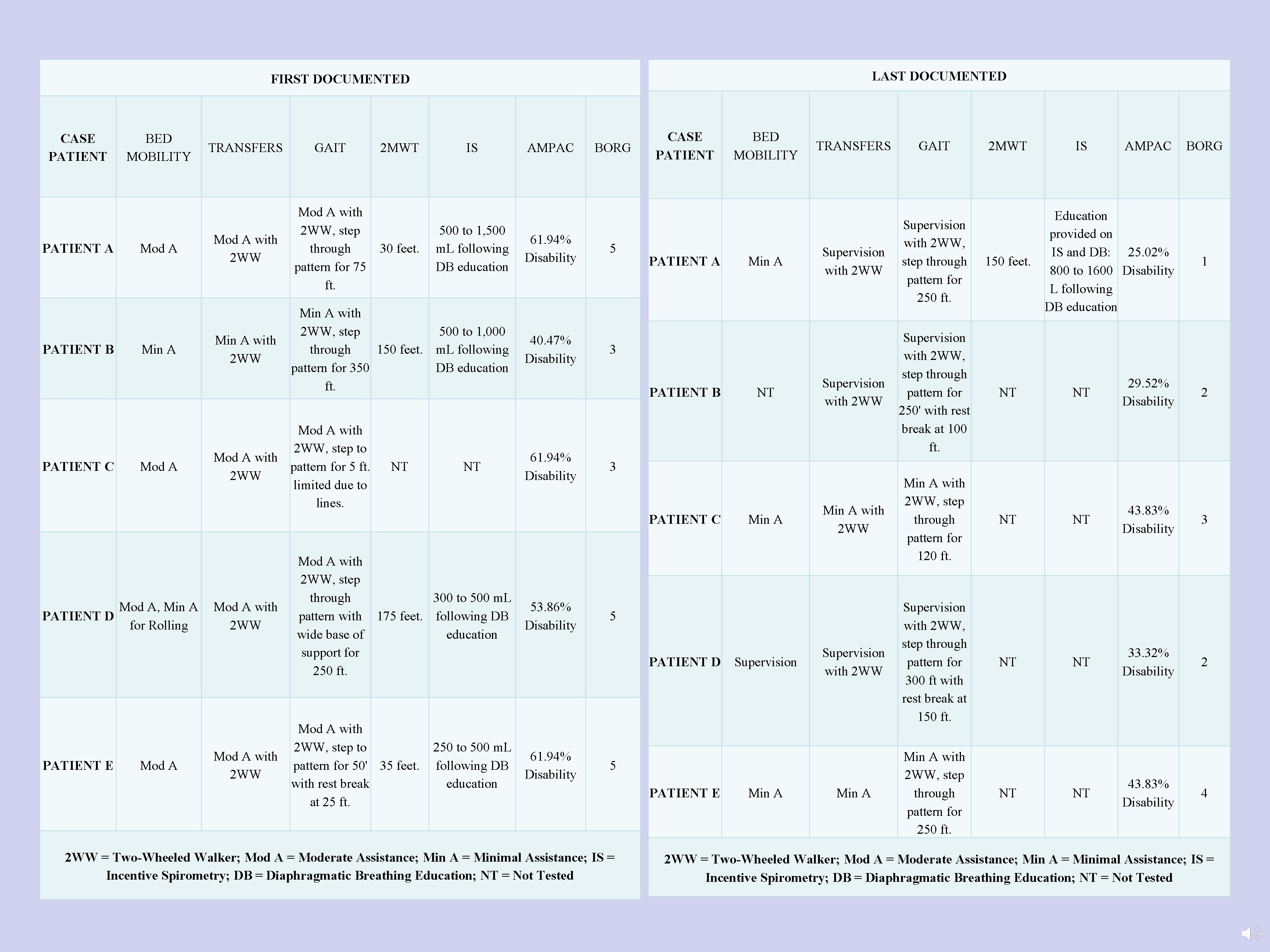
EXAMINATION • Four patients were assessed as moderate complexity, one as high complexity. All patients were independent at baseline. Three patients considered cognitively within functional limits and two with impaired safety and judgement. • All patients required moderate assistance for bed mobility, transfers and ambulation with a two-wheeled walker. The average distance ambulated was 151 feet. Four patients completed the 2 MWT for an average of 97. 5 feet. • All patients required supplemental oxygen and all patients demonstrated fair endurance. The average AMPAC Basic Mobility Score for the case patients was 56. 03% Disability. • IS and DB were utilized at evaluation with four case patients to assess pulmonary function, thoracic wall mobility and pulmonary hygiene. Two patients were able to improve their inspiratory efforts by 1, 000 m. L, one by 200 m. L and the last by 250 m. L following diaphragmatic breathing education. One patient did not receive IS or DB education.

CLINICAL IMPRESSION • Although the patients examined in this series were all discharged from the acute care setting and did not experience any postoperative pulmonary complications, the utilization of diaphragmatic breathing and incentive spirometry in conjunction with early mobilization will likely improve pulmonary hygiene and prevent further complications in subacute rehabilitation.
INTERVENTION • The focus for this case report is the use of IS and DB facilitation; however, all patients received standard physical therapy treatment by a licensed physical therapist or physical therapy assistant in addition to this treatment. The standard of care for treatment includes education on bed mobility, transfers, and ambulation all with the least restrictive assistive device for improved functional mobility and return to prior level of function. Additionally, measurements of AMPAC level of disability, perceived level of dyspnea utilizing the Borg Scale and the Two Minute Walk Test were analyzed if assessed during follow-up treatments.
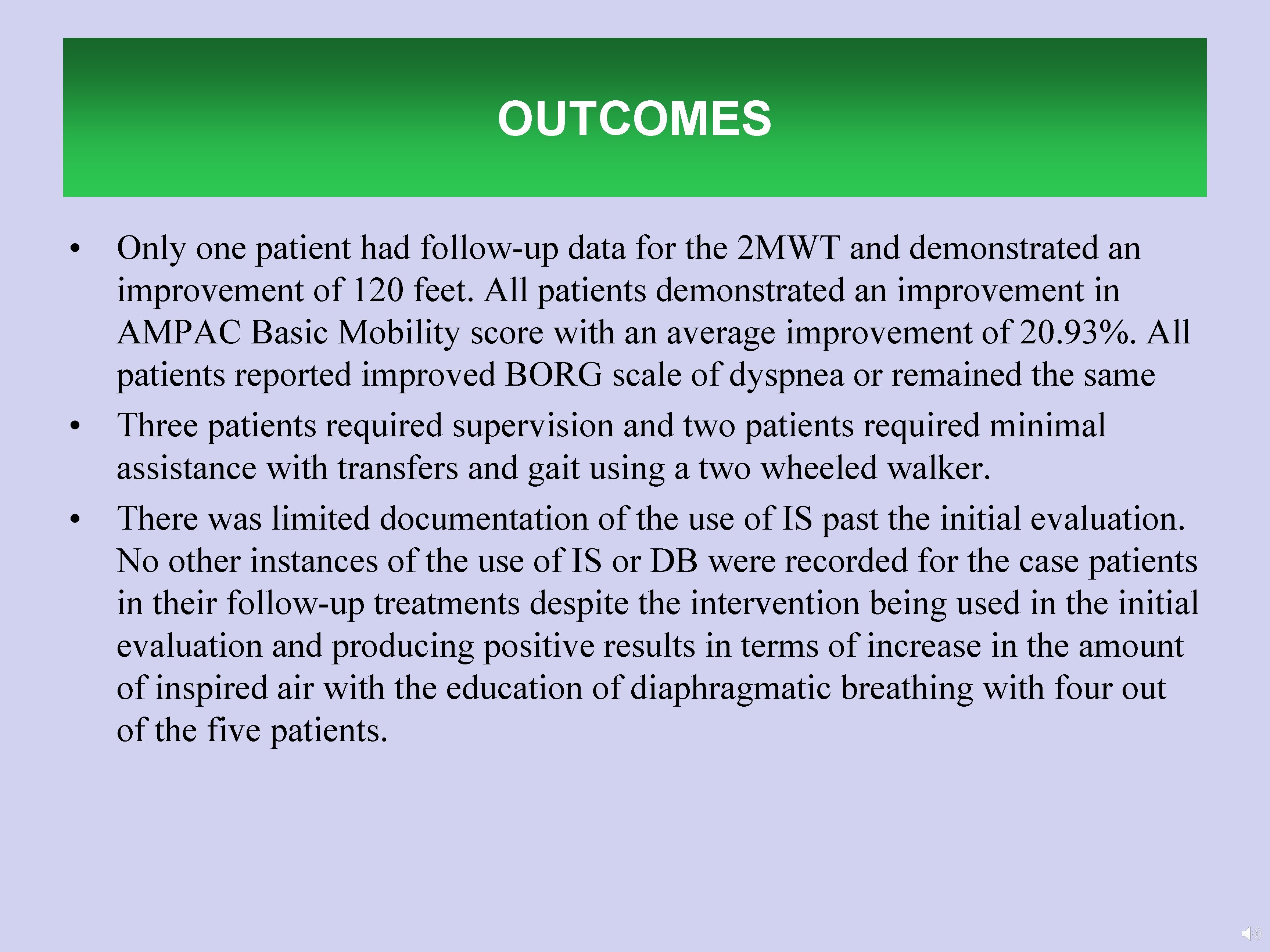
OUTCOMES • Only one patient had follow-up data for the 2 MWT and demonstrated an improvement of 120 feet. All patients demonstrated an improvement in AMPAC Basic Mobility score with an average improvement of 20. 93%. All patients reported improved BORG scale of dyspnea or remained the same • Three patients required supervision and two patients required minimal assistance with transfers and gait using a two wheeled walker. • There was limited documentation of the use of IS past the initial evaluation. No other instances of the use of IS or DB were recorded for the case patients in their follow-up treatments despite the intervention being used in the initial evaluation and producing positive results in terms of increase in the amount of inspired air with the education of diaphragmatic breathing with four out of the five patients.
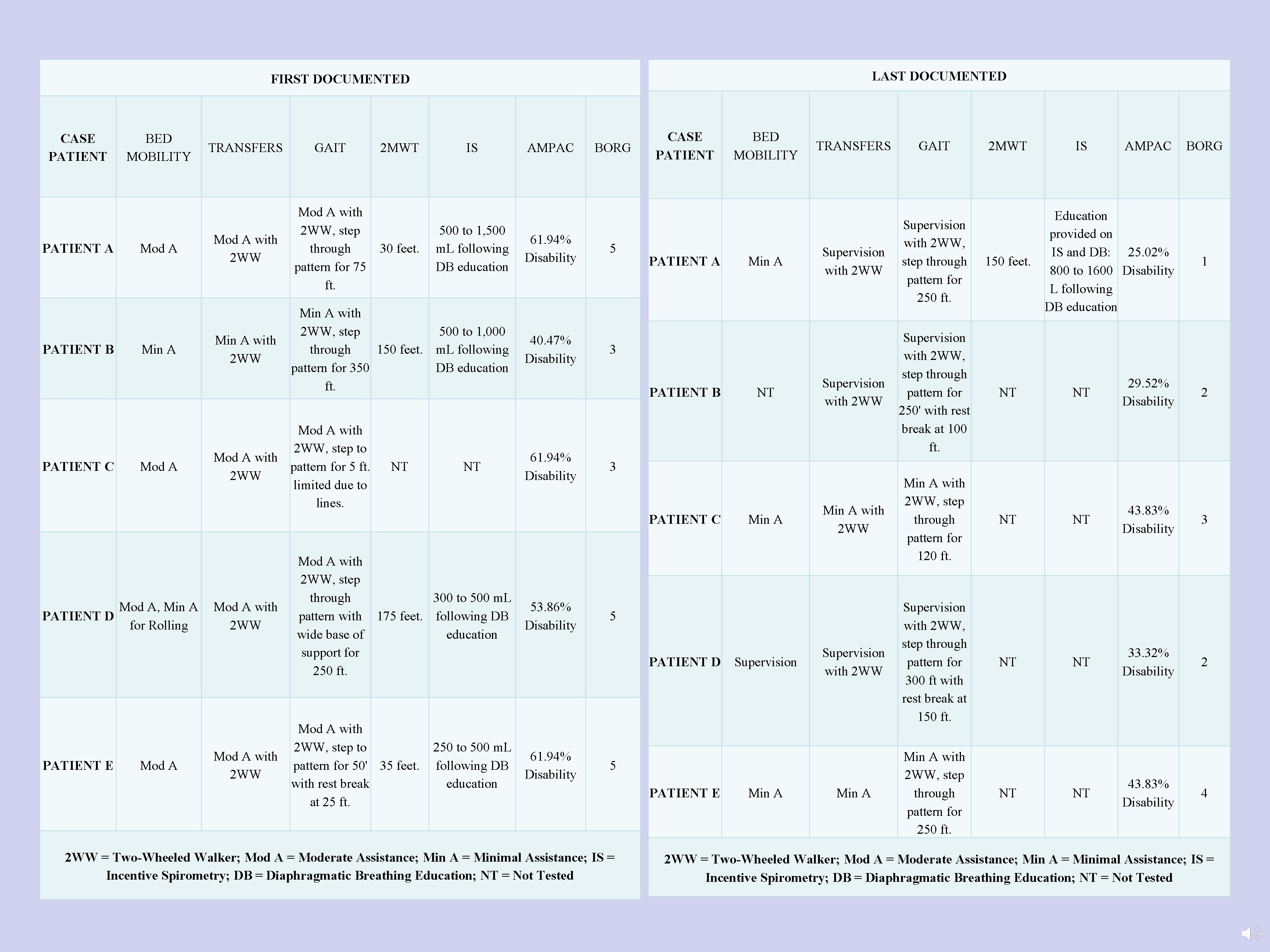
LAST DOCUMENTED FIRST DOCUMENTED CASE PATIENT A PATIENT B PATIENT C BED MOBILITY Mod A Min A Mod A TRANSFERS GAIT 2 MWT IS AMPAC Mod A with 2 WW, step through pattern for 75 ft. 500 to 1, 500 m. L following DB education 61. 94% Disability Min A with 2 WW, step 500 to 1, 000 through 150 feet. m. L following pattern for 350 DB education ft. 40. 47% Disability Mod A with 2 WW, step to Mod A with pattern for 5 ft. 2 WW limited due to lines. 30 feet. NT NT BORG 5 CASE PATIENT A Mod A, Min A PATIENT D for Rolling PATIENT E Mod A with 2 WW, step to Mod A with pattern for 50' 35 feet. 2 WW with rest break at 25 ft. 250 to 500 m. L 61. 94% following DB Disability education NT GAIT Supervision with 2 WW, step through pattern for 250 ft. Supervision with 2 WW, step through pattern for 250' with rest break at 100 ft. Min A with 2 WW, step through pattern for 120 ft. Supervision with 2 WW, step through pattern for 300 ft with rest break at 150 ft. Min A with 2 WW, step through pattern for 250 ft. 2 MWT 150 feet. NT IS AMPAC BORG Education provided on IS and DB: 25. 02% 800 to 1600 Disability L following DB education 1 NT 29. 52% Disability 2 NT 43. 83% Disability 3 NT 33. 32% Disability 2 NT 43. 83% Disability 4 3 PATIENT C Mod A with 2 WW, step through 300 to 500 m. L 53. 86% pattern with 175 feet. following DB Disability wide base of education support for 250 ft. Min A TRANSFERS 3 PATIENT B 61. 94% Disability BED MOBILITY Min A 5 PATIENT D Supervision 5 2 WW = Two-Wheeled Walker; Mod A = Moderate Assistance; Min A = Minimal Assistance; IS = Incentive Spirometry; DB = Diaphragmatic Breathing Education; NT = Not Tested PATIENT E Min A NT NT NT 2 WW = Two-Wheeled Walker; Mod A = Moderate Assistance; Min A = Minimal Assistance; IS = Incentive Spirometry; DB = Diaphragmatic Breathing Education; NT = Not Tested

CLINICAL IMPLICATIONS • Research supports the use of incentive spirometry when combined with diaphragmatic breathing and early mobility, however there is little research on the prevalence of implementation and documentation of these interventions. • The researchers believe this case series demonstrates that the use of education on diaphragmatic breathing has the possibility to improve the use of the diaphragm with inspiration with subsequent increase in inspired air as measured through incentive spirometry; however, documentation of these interventions is lacking in the acute care setting based on the retrospective analysis of evaluation and treatment records of these five case patients. • The electronic medical record may not provide areas to document specific data such as IS or the 2 MWT and may be a limitation to appropriate documentation by therapists. • As part of Physical Therapy education on documentation, documentation must demonstrate that the physical therapist as met the standard of care 18 during their patient interactions.
FOLLOW-UP QUESTIONS • Was evidence-based care provided yet not documented? • Was there a lack of knowledge of current evidence-based care which is why it was not performed? • Did therapists have knowledge of current evidence-based care and yet the care was not performed or simply not documented? • Does a lack of incentive spirometry or diaphragmatic breathing education result in long-term pulmonary dysfunction or increase susceptibility for further disease pathologies?
REFERENCES 1. Shamy S, Aaradhya A, Kumar AG, Madhan R. Physiotherapy in the management of post-operative pulmonary complications: A critical review of literature. Indian Journal of Physiotherapy and Occupational Therapy - An International Journal. 2014; 8(2): 69 -73. http: //indianjournals. com/ijor. aspx? target=ijor: ijpot&volume=8&issue=2&article=015. doi: 10. 5958/j. 0973 -5674. 8. 2. 062. 2. Naveed A, Azam H, Murtaza HG, Ahmad RA, Baig MAR. Incidence and risk factors of pulmonary complications after cardiopulmonary bypass. Pakistan journal of medical sciences. 2017; 33(4): 993 -996. https: //www. ncbi. nlm. nih. gov/pubmed/29067080. doi: 10. 12669/pjms. 334. 12846. 3. Kendall F, Oliveira J, Peleteiro B, Pinho P, Bastos PT. Inspiratory muscle training is effective to reduce postoperative pulmonary complications and length of hospital stay: A systematic review and metaanalysis. Disability and rehabilitation. 2018; 40(8): 864 -882. https: //www. ncbi. nlm. nih. gov/pubmed/28093920. doi: 10. 1080/09638288. 2016. 1277396. 4. Seyed Kazem Shakuri, Yaghoub Salekzamani, Ali Taghizadieh, Hamed Sabbagh-Jadid, Jamal Soleymani, Leyla Sahebi. Pulmonary physiotherapy effect on patients undergoing open cardiac surgery. Russian Open Medical Journal. 2014; 3(3): 0306. https: //doaj. org/article/46670 e 9 bdcca 478 bbd 9 a 7144 e 6 fa 12 ee. doi: 10. 15275/rusomj. 2014. 0306. 5. Arena R, Williams M, Forman DE, et al. Increasing referral and participation rates to outpatient cardiac rehabilitation: The valuable role of healthcare professionals in the inpatient and home health settings: A science advisory from the American heart association. Circulation. 2012; 125(10): 1321. https: //www. ncbi. nlm. nih. gov/pubmed/22291128. 6. Shamy S, Aaradhya A, Kumar AG, Madhan R. Physiotherapy in the management of post-operative pulmonary complications: A critical review of literature. Indian Journal of Physiotherapy and Occupational Therapy - An International Journal. 2014; 8(2): 69 -73. http: //indianjournals. com/ijor. aspx? target=ijor: ijpot&volume=8&issue=2&article=015. doi: 10. 5958/j. 0973 -5674. 8. 2. 062. 7. Tomaselli GF, Yancy CW, Franklin BA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: A presidential advisory from the American heart association. (AHA presidential advisory). Circulation. 2011; 124(25): 2951. 8. Etzioni D. The epidemiology and economics of cardiothoracic surgery in the elderly. In: Cardiothoracic surgery in the elderly. New York, NY: Springer New York; 2011: 5 -24. 1007/978 -1 -4419 -08926_2. 9. Cardiac rehabilitation guidelines. Irish Association of Cardiac Rehabilitation. 2013. 10. Restrepo R, Wettstein R, Wittnebel L, Tracy M. AARC clinical practice guideline incentive spirometry: 2011. Respiratory Care. 2011; 56(10). http: //www. rcjournal. com/cpgs/pdf/10. 11. 1600. pdf. 11. Eltorai AEM, Szabo AL, Antoci J, Valentin, et al. Clinical effectiveness of incentive spirometry for the prevention of postoperative pulmonary complications. Respiratory care. 2018; 63(3): 347 -352. https: //www. ncbi. nlm. nih. gov/pubmed/29279365. doi: 10. 4187/respcare. 05679. 12. Yokogawa M, Kurebayashi T, Ichimura T, Nishino M, Miaki H, Nakagawa T. Comparison of two instructions for deep breathing exercise: Non-specific and diaphragmatic breathing. Journal of Physical Therapy Science. 2018; 30(4): 614 -618. https: //jlc. jst. go. jp/DN/JLC/20079000350? from=SUMMON. doi: 10. 1589/jpts. 30. 614. 13. Ravaliya VK. Functional status in post-CABG patients following physiotherapy- A retrospective analysis. Indian Journal of Physiotherapy and Occupational Therapy - An International Journal. 2013; 7(3): 270 -274. http: //indianjournals. com/ijor. aspx? target=ijor: ijpot&volume=7&issue=3&article=053. doi: 10. 5958/j. 0973 -5674. 7. 3. 106. 14. Narayanan ALT, Hamid, Syed Rasul G Syed, Supriyanto E. Evidence regarding patient compliance with incentive spirometry interventions after cardiac, thoracic and abdominal surgeries: A systematic literature review. Canadian journal of respiratory therapy: CJRT = Revue Canadienne de la therapie respiratoire : RCTR. 2016; 52(1): 17 -26. https: //www. ncbi. nlm. nih. gov/pubmed/26909010. 15. Yokogawa M, Kurebayashi T, Ichimura T, Nishino M, Miaki H, Nakagawa T. Comparison of two instructions for deep breathing exercise: Non-specific and diaphragmatic breathing. Journal of Physical Therapy Science. 2018; 30(4): 614 -618. https: //jlc. jst. go. jp/DN/JLC/20079000350? from=SUMMON. doi: 10. 1589/jpts. 30. 614. 16. Alaparthi GK, Augustine AJ, Anand R, Mahale A. Comparison of diaphragmatic breathing exercise, volume and flow incentive spirometry, on diaphragm excursion and pulmonary function in patients undergoing laparoscopic surgery: A randomized controlled trial. Minimally invasive surgery. 2016; 2016: 1967532 -12. https: //www. ncbi. nlm. nih. gov/pubmed/27525116. doi: 10. 1155/2016/1967532. 17. Bohannon RW. Normative reference values for the two-minute walk test derived by meta-analysis. Journal of Physical Therapy Science. 2017; 29(12): 2224 -2227. https: //jlc. jst. go. jp/DN/JLC/20066244859? from=SUMMON. doi: 10. 1589/jpts. 29. 2224. 18. Osborne JA. Documentation for physical therapist practice: A clinical decision-making approach. Massachusetts: Jones and Bartlett Learning; 2016: 231 -232. 19. Mahafza T, Batarseh S, Bsoul N, Massad E, Qudaisat I, Al-Layla AE. Early vs. late tracheostomy for the ICU patients: Experience in a referral hospital. Saudi J Anaesth. 2012; 6(2): 152 -154. https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 3385258/. Accessed Apr 1, 2020. doi: 10. 4103/1658 -354 X. 97029. 20. Madhavan S, Chan S, Tan W, et al. Cardiopulmonary bypass time: Every minute counts. J Cardiovasc Surg (Torino). 2018; 59(2): 274 -281. Accessed Apr 1, 2020. doi: 10. 23736/S 0021 -9509. 17. 09864 -0. 21. Cahalin LP, Braga M, Matsuo Y, Hernandez ED. Efficacy of diaphragmatic breathing in persons with chronic obstructive pulmonary disease: A review of the literature. Journal of cardiopulmonary rehabilitation. 2002; 22(1): 7 -21. https: //www. ncbi. nlm. nih. gov/pubmed/11839992. doi: 10. 1097/00008483 -200201000 -00002.