Pearls of Precepting Translating Concepts of the PatientCentered



- Slides: 94
Pearls of Precepting Translating Concepts of the Patient-Centered Medical Home (PCMH) Into Teaching Opportunities Harald Lausen, DO, FACOFP American College of Osteopathic Family Physicians 47 th Annual Convention & Scientific Seminars Las Vegas, Nevada March 2010
Objectives • List the general principles and concepts of the PCMH. • Translate principles and concepts of the PCMH into student learning experiences. • Discuss and explore possible educational approaches for preceptors to teach and demonstrate principles and concepts of the PCMH. • Capture several educational approaches that could be implemented into their own practices as preceptors.
Power. Point Rules • • Forgive Me --- I Am Breaking the Rules! Designed for Future Reference Busy Slides Be Merciful
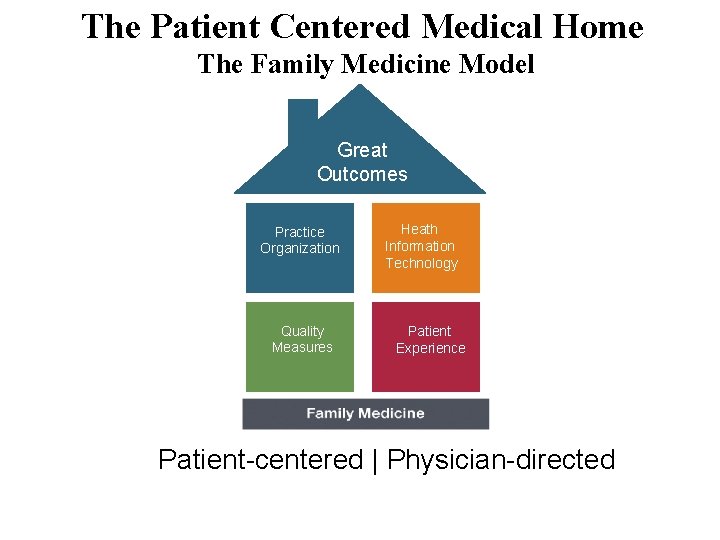
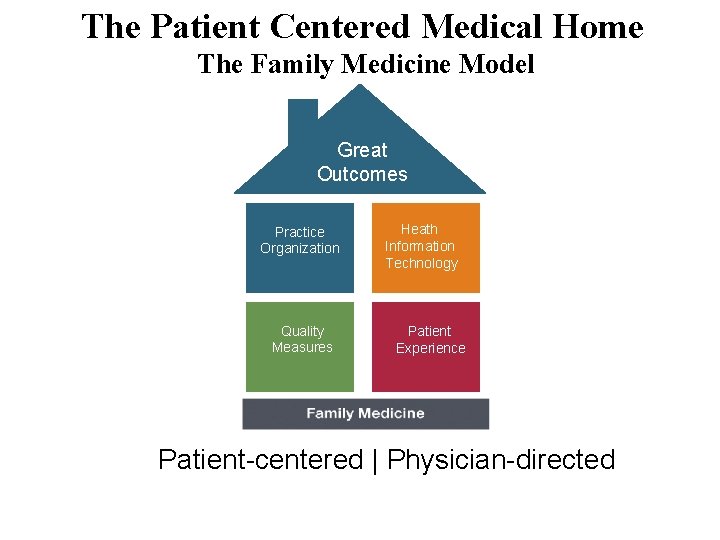
The Patient Centered Medical Home The Family Medicine Model Great Outcomes Practice Organization Health IT Quality Measures Heath Health IT Information Technology Patient Experience Family Medicine Foundation Patient-centered | Physician-directed
Foundation – Evidence & Facts Slides by Jerry Kruse, MD, MSPH
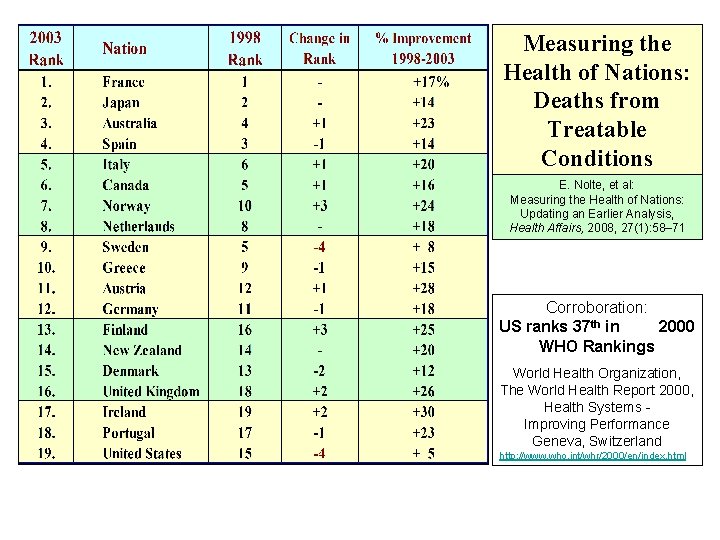
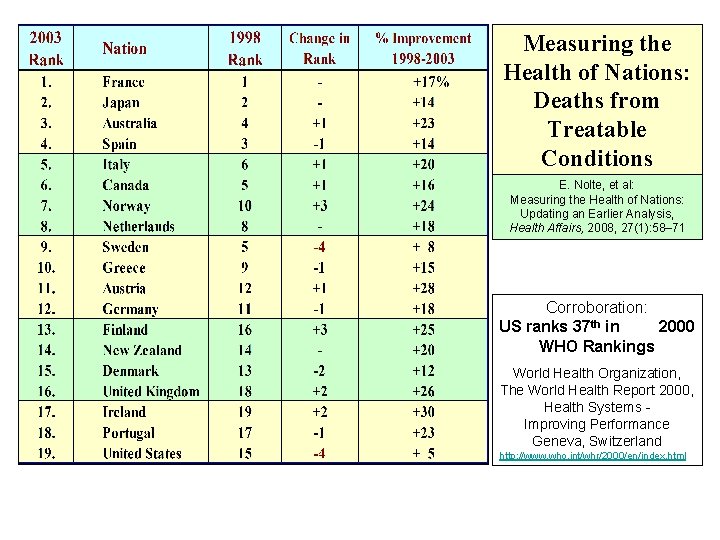
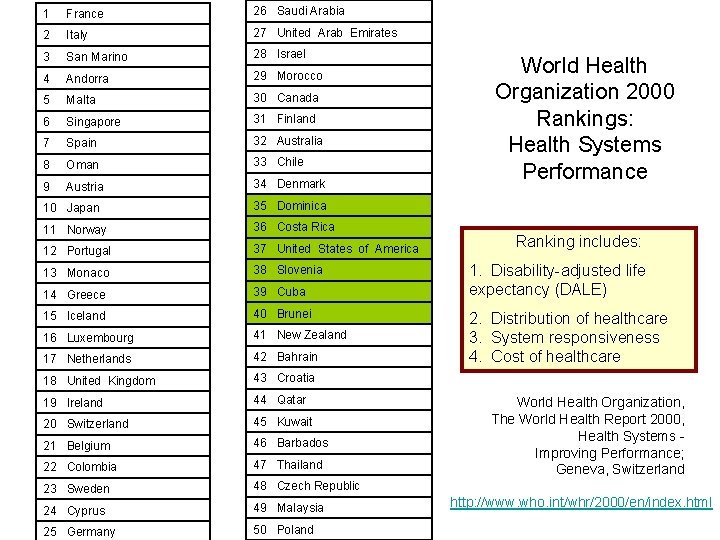
Measuring the Health of Nations: Deaths from Treatable Conditions E. Nolte, et al: Measuring the Health of Nations: Updating an Earlier Analysis, Health Affairs, 2008, 27(1): 58– 71 Corroboration: US ranks 37 th in 2000 WHO Rankings World Health Organization, The World Health Report 2000, Health Systems Improving Performance Geneva, Switzerland http: //www. who. int/whr/2000/en/index. html
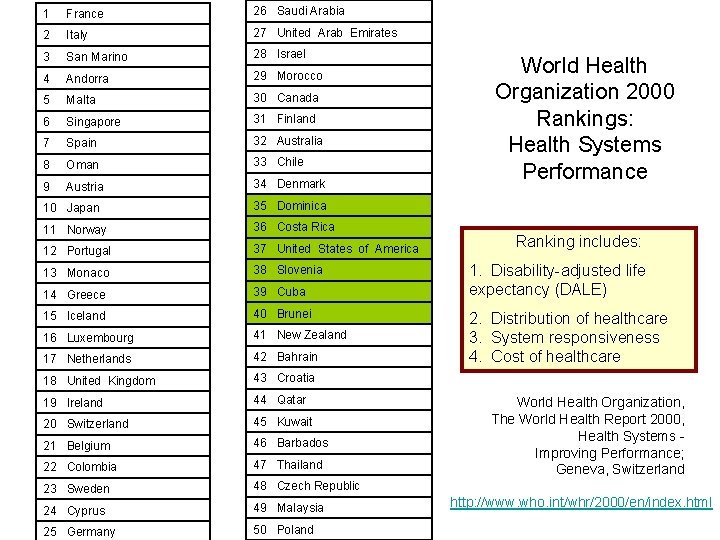
1 France 26 Saudi Arabia 2 Italy 27 United Arab Emirates 3 San Marino 28 Israel 4 Andorra 29 Morocco 5 Malta 30 Canada 6 Singapore 31 Finland 7 Spain 32 Australia 8 Oman 33 Chile 9 Austria 34 Denmark 10 Japan 35 Dominica 11 Norway 36 Costa Rica 12 Portugal 37 United States of America 13 Monaco 38 Slovenia 14 Greece 39 Cuba 15 Iceland 40 Brunei 16 Luxembourg 41 New Zealand 17 Netherlands 42 Bahrain 18 United Kingdom 43 Croatia 19 Ireland 44 Qatar 20 Switzerland 45 Kuwait 21 Belgium 46 Barbados 22 Colombia 47 Thailand 23 Sweden 48 Czech Republic 24 Cyprus 49 Malaysia 25 Germany 50 Poland World Health Organization 2000 Rankings: Health Systems Performance Ranking includes: 1. Disability-adjusted life expectancy (DALE) 2. Distribution of healthcare 3. System responsiveness 4. Cost of healthcare World Health Organization, The World Health Report 2000, Health Systems Improving Performance; Geneva, Switzerland http: //www. who. int/whr/2000/en/index. html
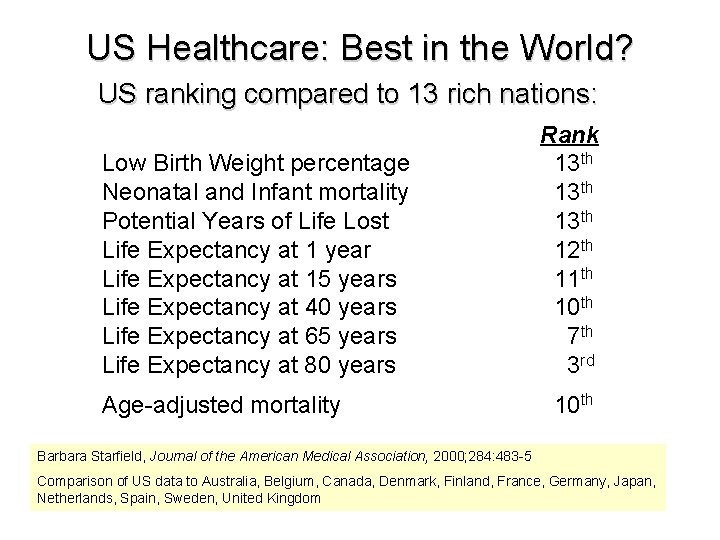
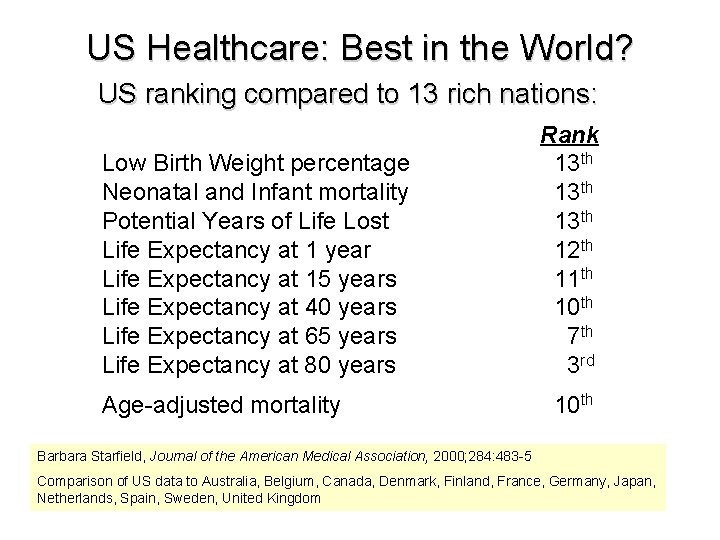
US Healthcare: Best in the World? US ranking compared to 13 rich nations: Low Birth Weight percentage Neonatal and Infant mortality Potential Years of Life Lost Life Expectancy at 1 year Life Expectancy at 15 years Life Expectancy at 40 years Life Expectancy at 65 years Life Expectancy at 80 years Age-adjusted mortality Rank 13 th 12 th 11 th 10 th 7 th 3 rd 10 th Barbara Starfield, Journal of the American Medical Association, 2000; 284: 483 -5 Comparison of US data to Australia, Belgium, Canada, Denmark, Finland, France, Germany, Japan, Netherlands, Spain, Sweden, United Kingdom
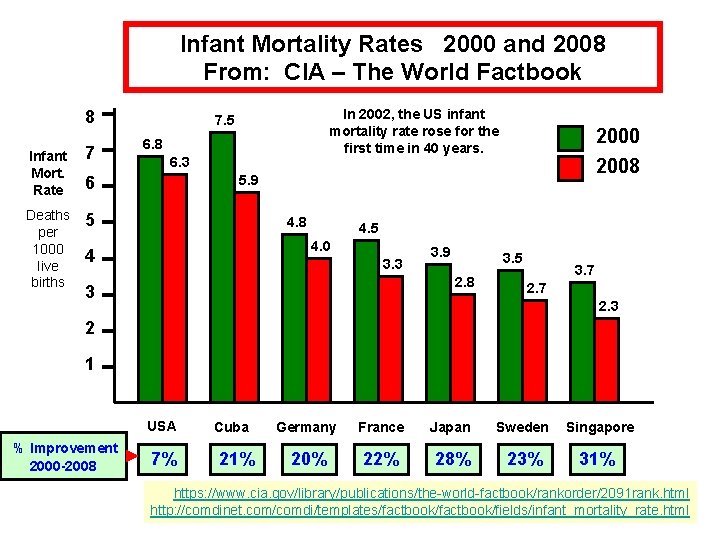
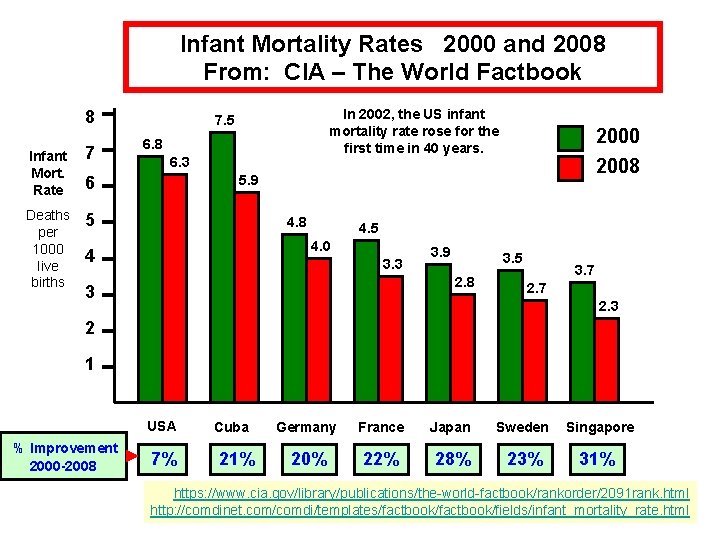
Infant Mortality Rates 2000 and 2008 From: CIA – The World Factbook 8 Infant Mort. Rate 7 Deaths per 1000 live births 5 In 2002, the US infant mortality rate rose for the first time in 40 years. 7. 5 6. 8 6. 3 2000 2008 5. 9 6 4. 8 4. 5 4. 0 4 3. 3 3. 9 3. 5 2. 8 3 3. 7 2. 3 2 1 USA % Improvement 2000 -2008 7% Cuba 21% Germany France Japan Sweden Singapore 20% 22% 28% 23% 31% https: //www. cia. gov/library/publications/the-world-factbook/rankorder/2091 rank. html http: //comdinet. com/comdi/templates/factbook/fields/infant_mortality_rate. html
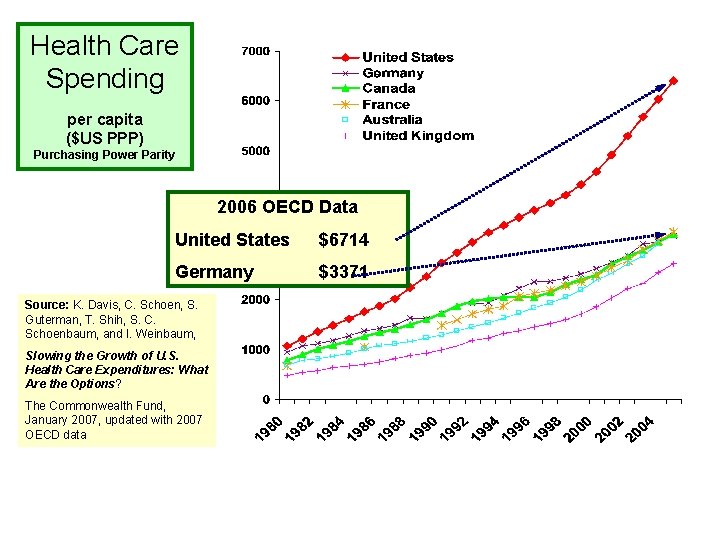
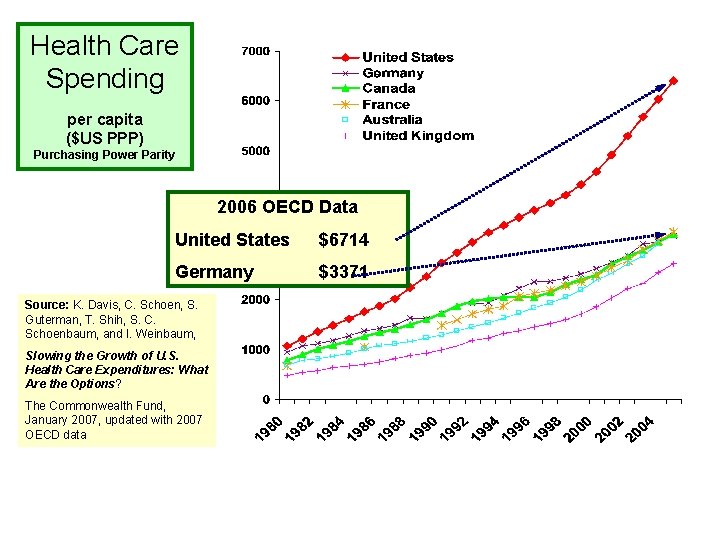
Health Care Spending per capita ($US PPP) Purchasing Power Parity 2006 OECD Data United States $6714 Germany $3371 Source: K. Davis, C. Schoen, S. Guterman, T. Shih, S. C. Schoenbaum, and I. Weinbaum, Slowing the Growth of U. S. Health Care Expenditures: What Are the Options? The Commonwealth Fund, January 2007, updated with 2007 OECD data
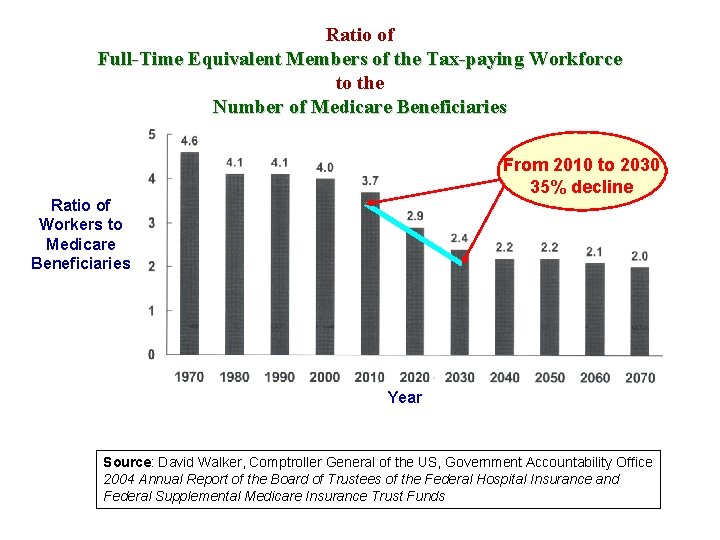
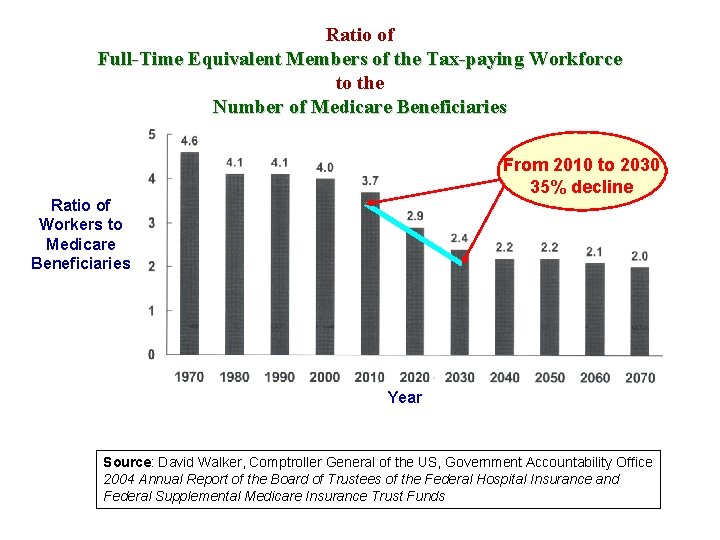
Ratio of Full-Time Equivalent Members of the Tax-paying Workforce to the Number of Medicare Beneficiaries From 2010 to 2030 35% decline Ratio of Workers to Medicare Beneficiaries Year Source: David Walker, Comptroller General of the US, Government Accountability Office 2004 Annual Report of the Board of Trustees of the Federal Hospital Insurance and Federal Supplemental Medicare Insurance Trust Funds
The Patient-Centered Medical Home: The Evidence Johns Hopkins Bloomberg School of Public Health Examples: Starfield, Shi, Macinko. Contributions of Primary Care to Health Systems and Health: The Milbank Quarterly 83(3), 2005; 457 -502 Starfield & Shi. The Medical Home Access to Care, and Insurance, A Review of Evidence: Pediatrics, 2004; 113: 1493 -99 Dartmouth Center for Health Policy and Clinical Practice Formerly “The Center for Clinical Evaluative Sciences at Dartmouth”
Comprehensive Review of the Effectiveness of Primary Care Contribution of Primary Care to Health Systems and Health Barbara Starfield, Leiyu Shi and James Macinko Johns Hopkins University, New York University The Milbank Quarterly, Volume 83, No. 3, 2005 Pages 457 - 502
Institute of Medicine Definition of Primary Care “… (1) the provision of integrated, accessible health care services (2) by clinicians who are accountable for addressing a large majority of health care needs, (3) developing sustained partnerships with patients, and (4) practicing within the context of the family and community…” General Pediatrics: The Medical Home (1967) Family Medicine: The Personal Medical Home (2002) Internal Medicine: The Advanced Medical Home (2006) General Now: The Patient-Centered Medical Home (2007) Donaldson, IOM Report, Primary Care: America’s Health in a New Era, 1996 IOM Report, 1978
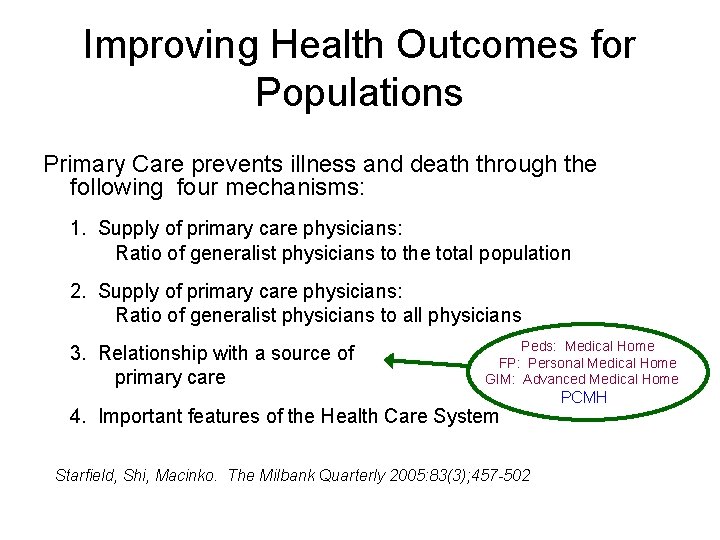
Improving Health Outcomes for Populations Primary Care prevents illness and death through the following four mechanisms: 1. Supply of primary care physicians: Ratio of generalist physicians to the total population 2. Supply of primary care physicians: Ratio of generalist physicians to all physicians 3. Relationship with a source of primary care Peds: Medical Home FP: Personal Medical Home GIM: Advanced Medical Home 4. Important features of the Health Care System Starfield, Shi, Macinko. The Milbank Quarterly 2005: 83(3); 457 -502 PCMH
Health System and Policy Characteristics Associated With Improved Health Outcomes • Attempts to distribute health services equitably with respect to regional health care needs • Universal or near-universal financial assistance guaranteed by a publicly accountable body • Low or no co-pay for health services • Percentage of physicians who are generalists • Professional earnings of primary care physicians relative to other specialties Starfield, Shi, Macinko. The Milbank Quarterly 2005: 83(3); 457 -502
Social Health Disparities and Primary Care • Social deprivation is accurately measured by levels of income inequality (Gini Coefficient), and is associated with very poor health outcomes • A high supply of Primary Care Physicians eliminates the adverse health effect of income inequality • A high supply of Primary Care Physicians eliminates racial disparities in health outcomes in rural and suburban populations Data from multiple studies in the United States, United Kingdom, Mexico, Costa Rica, and 7 African nations. Summarized in Starfield B, et al. Contribution of Primary Care to Health Systems and Health, The Milbank Quarterly, 2005; 83: 457 -502. Most important data is in: Shi L et al: Journal of Family Practice, April 1999, p 275 -283
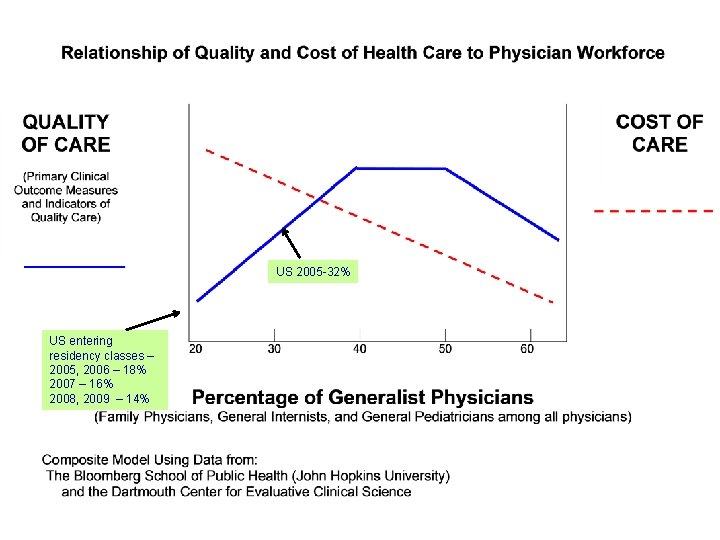
Population-Based Health Outcomes, Equity and Cost • The nations and regions that emphasize these things consistently have better health outcomes, more equitable systems, and substantially lower costs. a. Public health and preventive medicine b. Usual sources of comprehensive care (Primary Care Physicians) c. First-contact care with effective systems of care (PCMH) • Health outcomes are optimized when 40 -50% of the physician workforce is made up of primary care physicians • Socioeconomic and racial disparities in healthcare outcomes are dramatically reduced when there is an appropriate primary care workforce
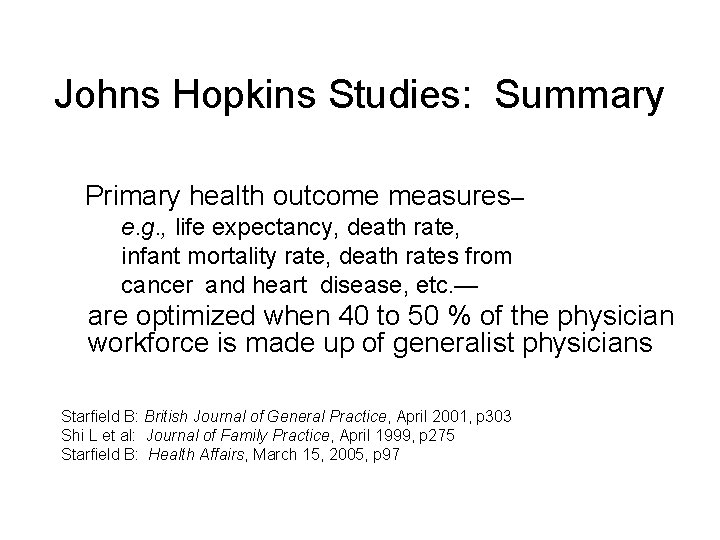
Johns Hopkins Studies: Summary Primary health outcome measures– e. g. , life expectancy, death rate, infant mortality rate, death rates from cancer and heart disease, etc. — are optimized when 40 to 50 % of the physician workforce is made up of generalist physicians Starfield B: British Journal of General Practice, April 2001, p 303 Shi L et al: Journal of Family Practice, April 1999, p 275 Starfield B: Health Affairs, March 15, 2005, p 97
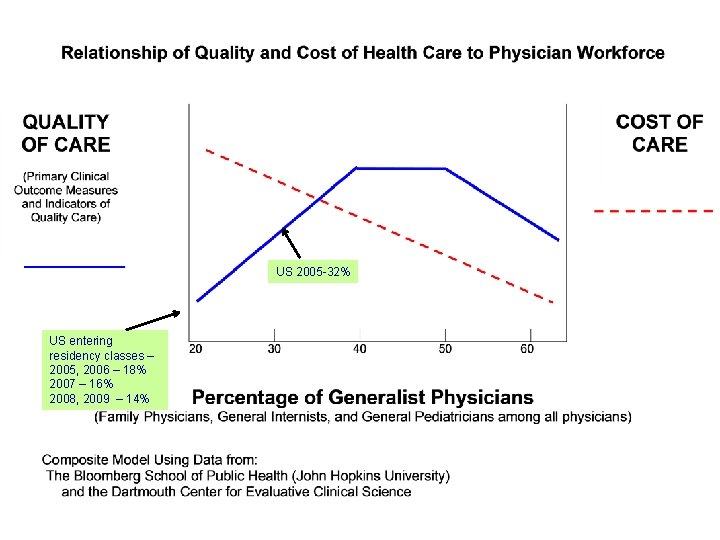
US 2005 -32% US entering residency classes – 2005, 2006 – 18% 2007 – 16% 2008, 2009 – 14%
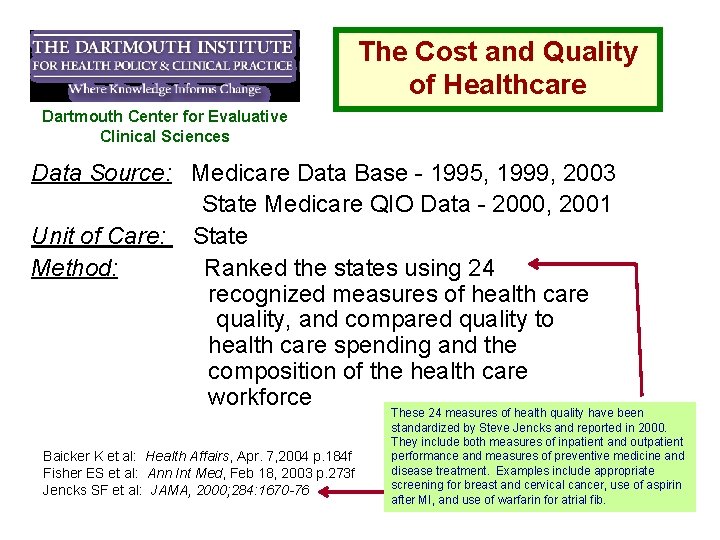
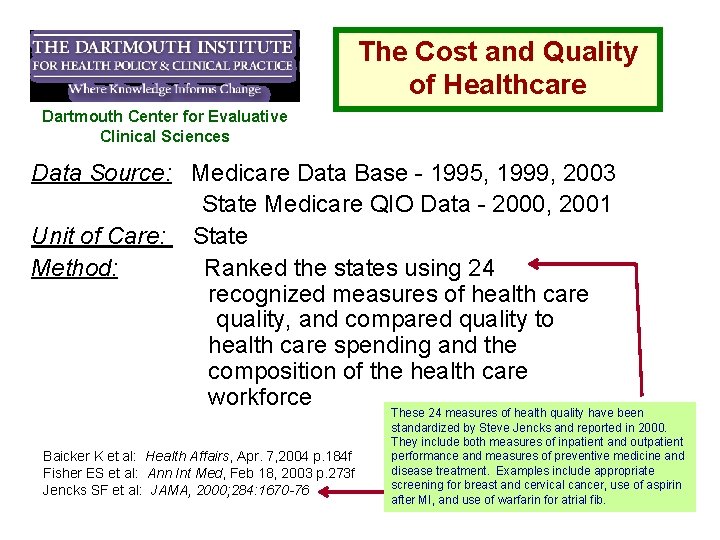
The Cost and Quality of Healthcare Dartmouth Center for Evaluative Clinical Sciences Data Source: Medicare Data Base - 1995, 1999, 2003 State Medicare QIO Data - 2000, 2001 Unit of Care: State Method: Ranked the states using 24 recognized measures of health care quality, and compared quality to health care spending and the composition of the health care workforce Baicker K et al: Health Affairs, Apr. 7, 2004 p. 184 f Fisher ES et al: Ann Int Med, Feb 18, 2003 p. 273 f Jencks SF et al: JAMA, 2000; 284: 1670 -76 These 24 measures of health quality have been standardized by Steve Jencks and reported in 2000. They include both measures of inpatient and outpatient performance and measures of preventive medicine and disease treatment. Examples include appropriate screening for breast and cervical cancer, use of aspirin after MI, and use of warfarin for atrial fib.
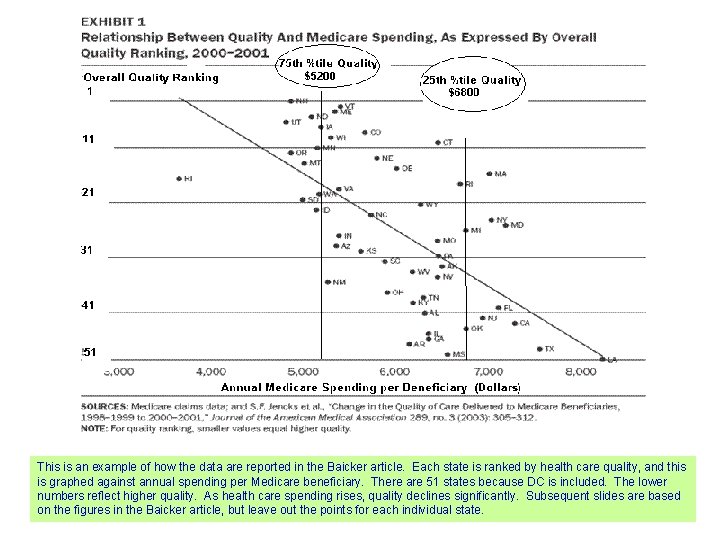
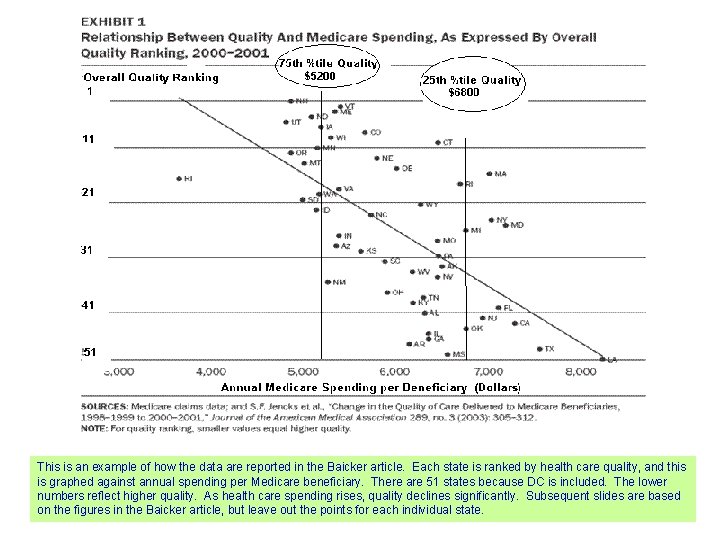
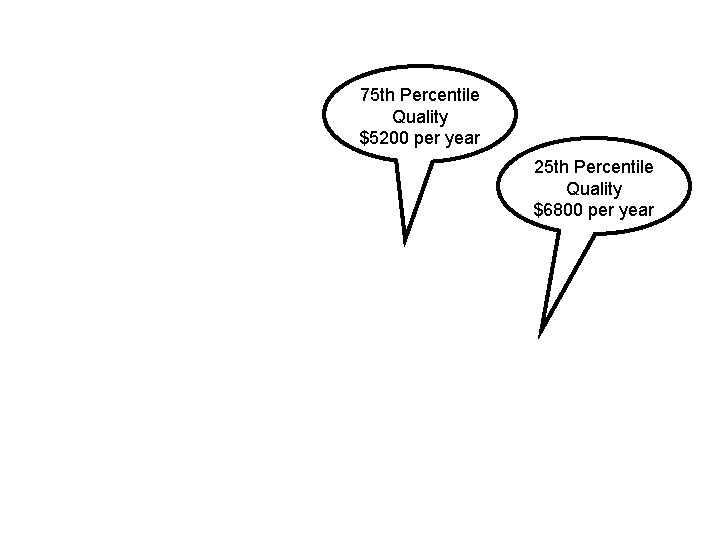
This is an example of how the data are reported in the Baicker article. Each state is ranked by health care quality, and this is graphed against annual spending per Medicare beneficiary. There are 51 states because DC is included. The lower numbers reflect higher quality. As health care spending rises, quality declines significantly. Subsequent slides are based on the figures in the Baicker article, but leave out the points for each individual state.
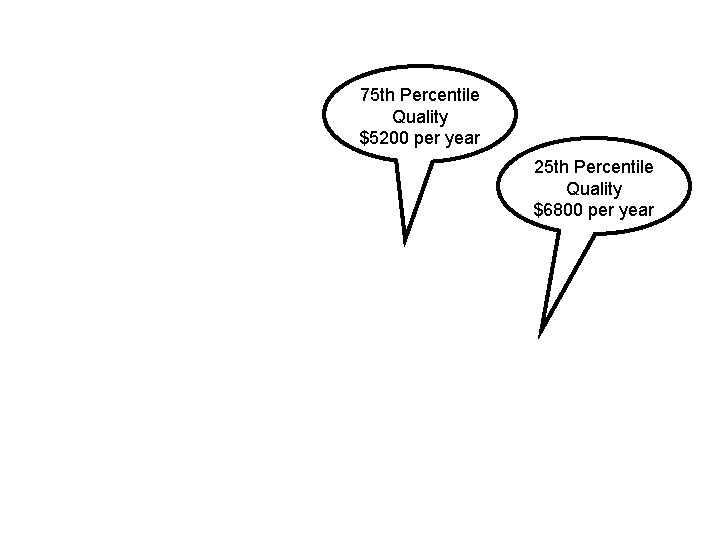
75 th Percentile Quality $5200 per year 25 th Percentile Quality $6800 per year
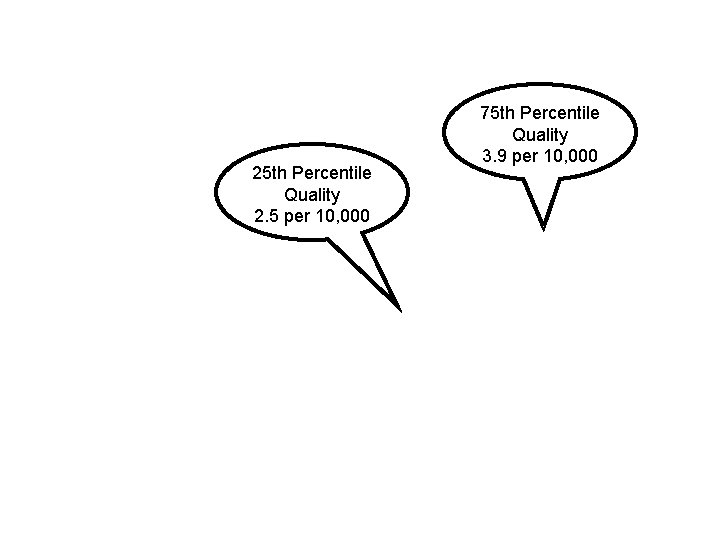
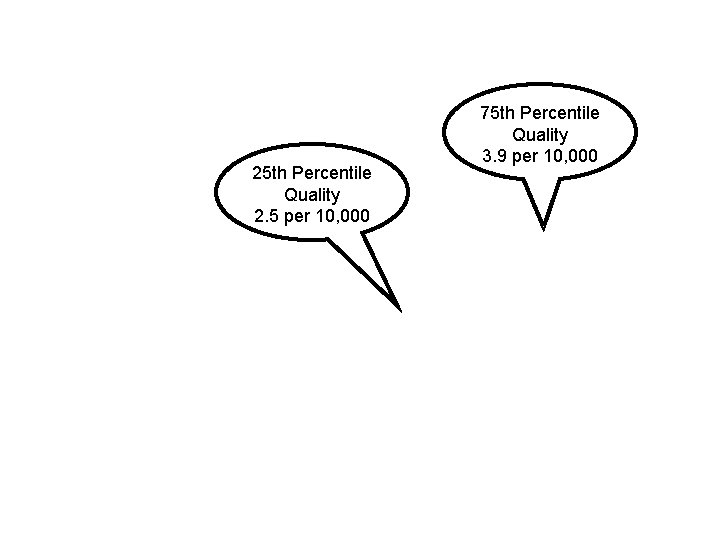
25 th Percentile Quality 2. 5 per 10, 000 75 th Percentile Quality 3. 9 per 10, 000
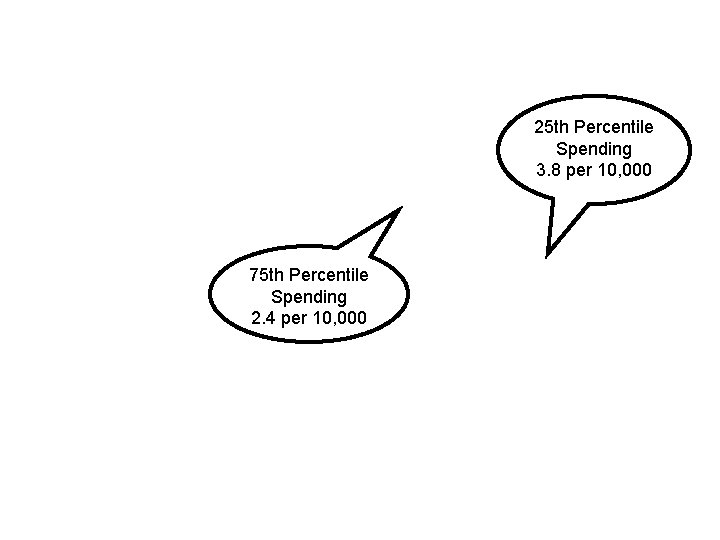
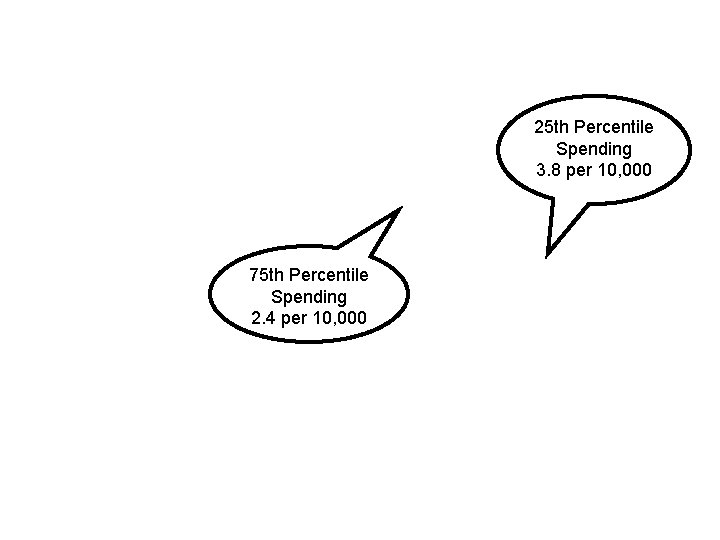
25 th Percentile Spending 3. 8 per 10, 000 75 th Percentile Spending 2. 4 per 10, 000
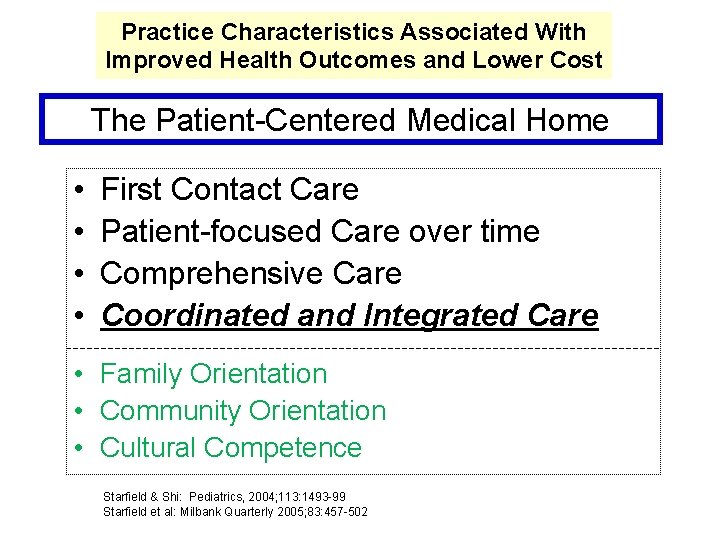
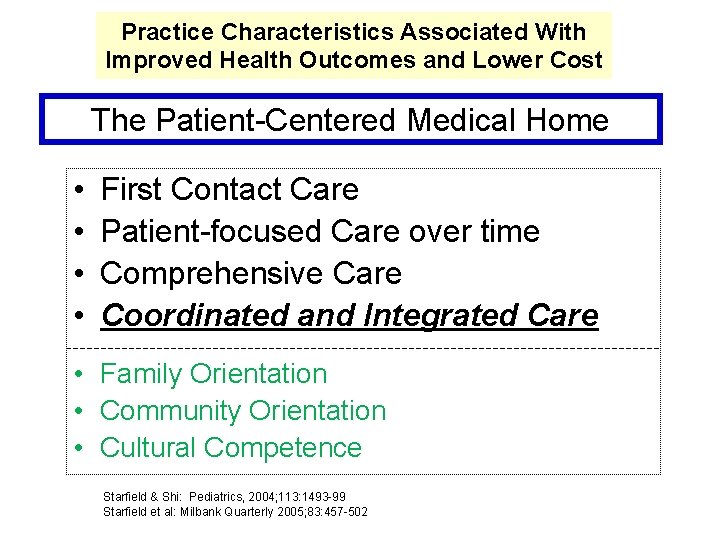
Practice Characteristics Associated With Improved Health Outcomes and Lower Cost The Patient-Centered Medical Home • • First Contact Care Patient-focused Care over time Comprehensive Care Coordinated and Integrated Care • Family Orientation • Community Orientation • Cultural Competence Starfield & Shi: Pediatrics, 2004; 113: 1493 -99 Starfield et al: Milbank Quarterly 2005; 83: 457 -502
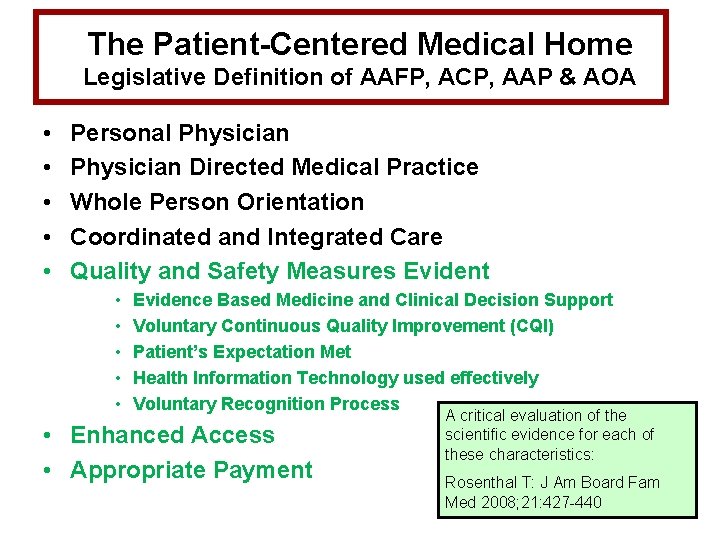
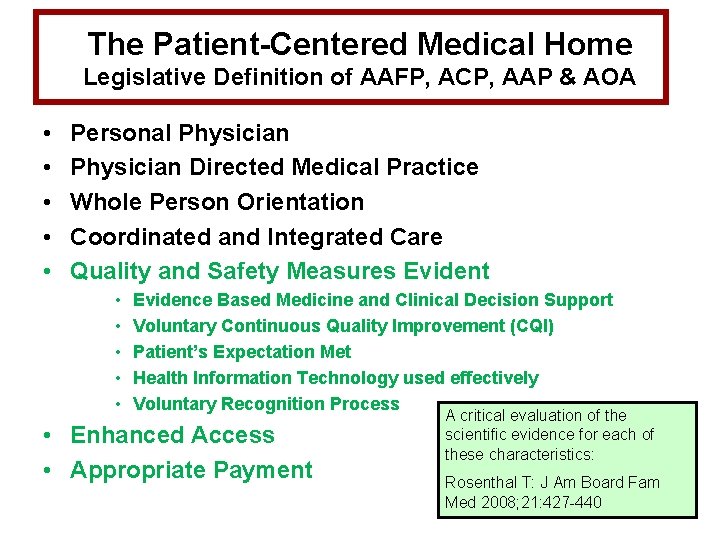
The Patient-Centered Medical Home Legislative Definition of AAFP, ACP, AAP & AOA • • • Personal Physician Directed Medical Practice Whole Person Orientation Coordinated and Integrated Care Quality and Safety Measures Evident • • • Evidence Based Medicine and Clinical Decision Support Voluntary Continuous Quality Improvement (CQI) Patient’s Expectation Met Health Information Technology used effectively Voluntary Recognition Process • Enhanced Access • Appropriate Payment A critical evaluation of the scientific evidence for each of these characteristics: Rosenthal T: J Am Board Fam Med 2008; 21: 427 -440
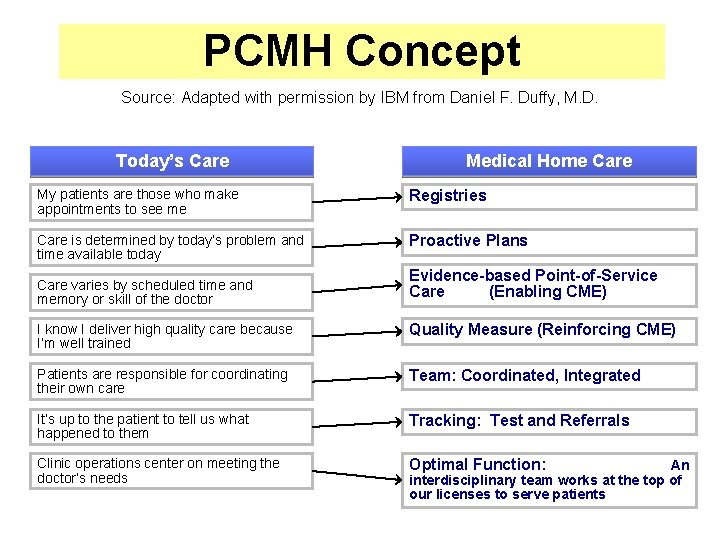
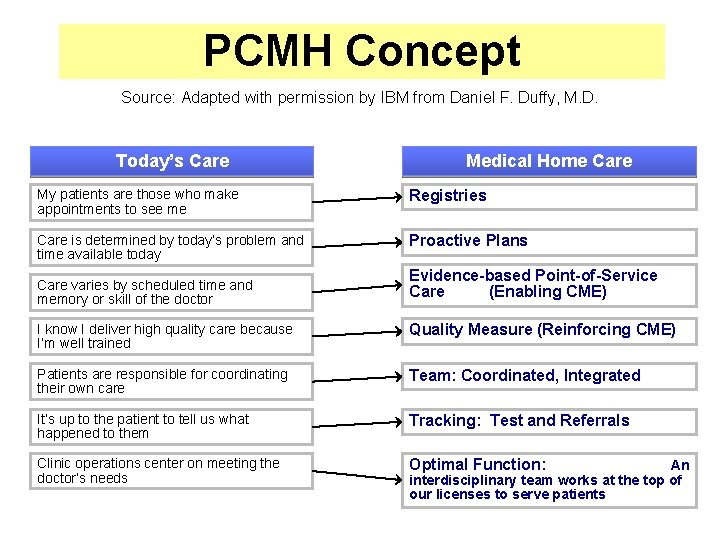
PCMH Concept Source: Adapted with permission by IBM from Daniel F. Duffy, M. D. Today’s Care Medical Home Care My patients are those who make appointments to see me Registries Care is determined by today’s problem and time available today Proactive Plans Care varies by scheduled time and memory or skill of the doctor Evidence-based Point-of-Service Care (Enabling CME) I know I deliver high quality care because I’m well trained Quality Measure (Reinforcing CME) Patients are responsible for coordinating their own care Team: Coordinated, Integrated It’s up to the patient to tell us what happened to them Tracking: Test and Referrals Clinic operations center on meeting the doctor’s needs Optimal Function: 28 An interdisciplinary team works at the top of our licenses to serve patients
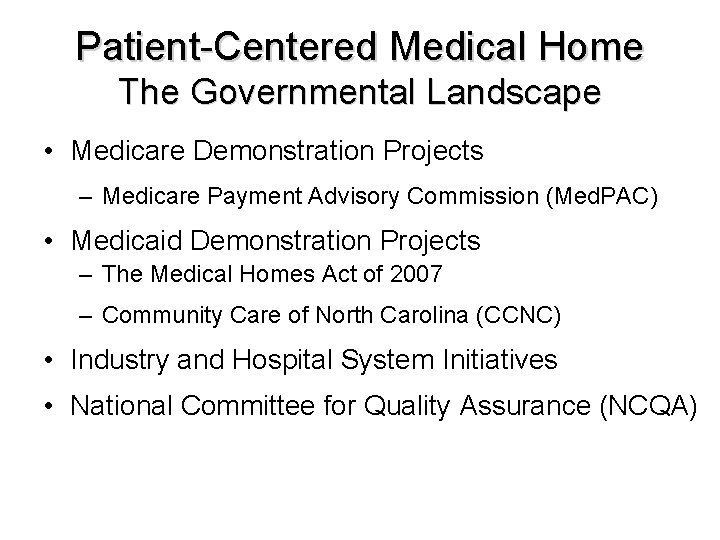
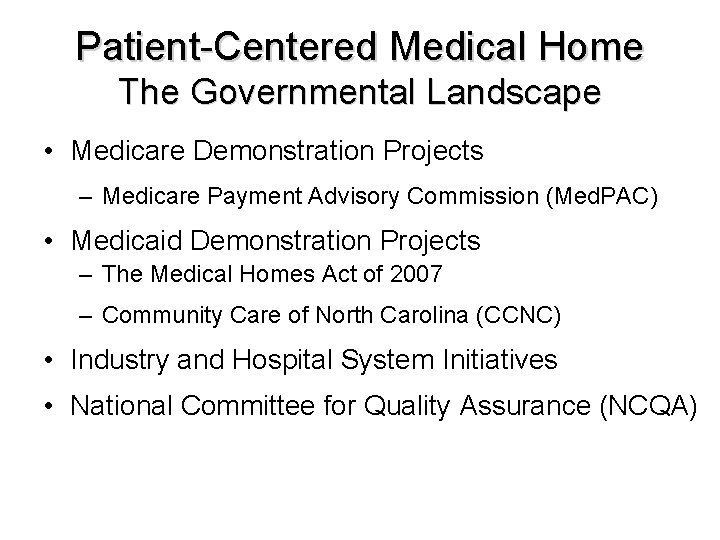
Patient-Centered Medical Home The Governmental Landscape • Medicare Demonstration Projects – Medicare Payment Advisory Commission (Med. PAC) • Medicaid Demonstration Projects – The Medical Homes Act of 2007 – Community Care of North Carolina (CCNC) • Industry and Hospital System Initiatives • National Committee for Quality Assurance (NCQA)
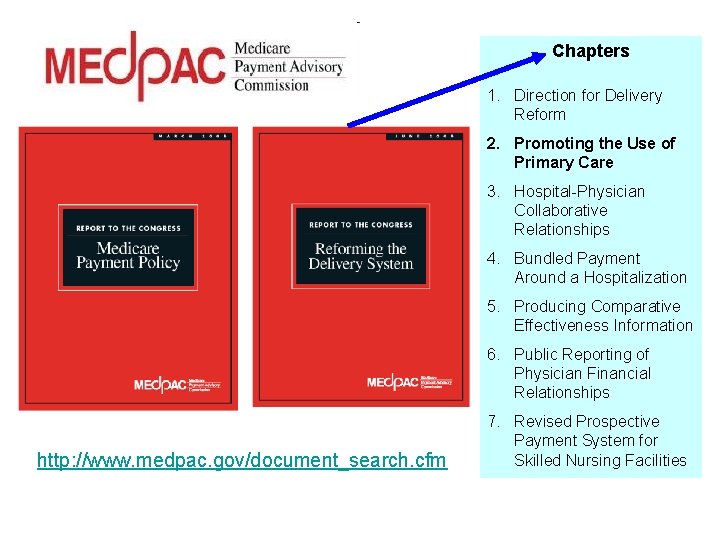
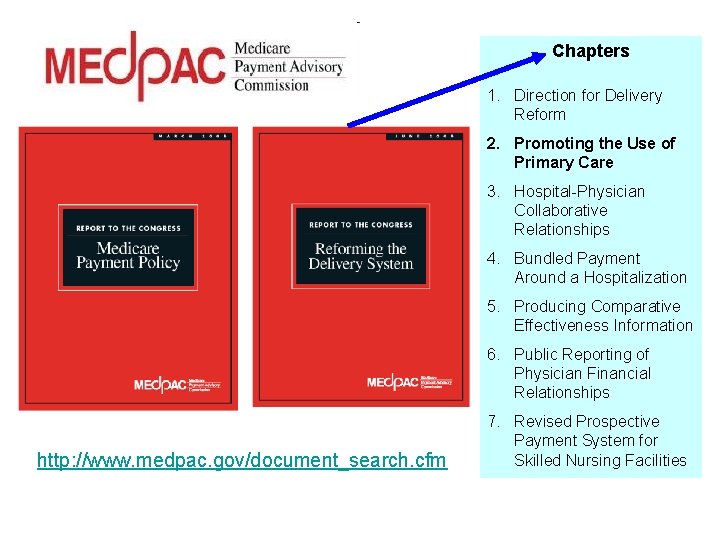
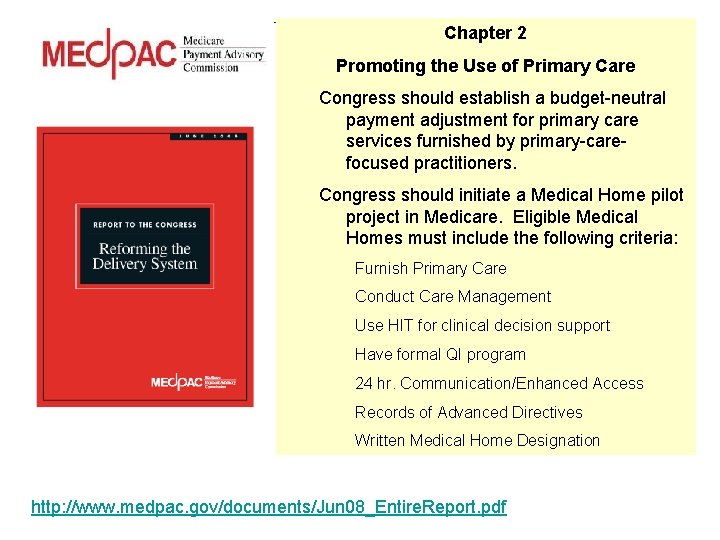
Chapters 1. Direction for Delivery Reform 2. Promoting the Use of Primary Care 3. Hospital-Physician Collaborative Relationships 4. Bundled Payment Around a Hospitalization 5. Producing Comparative Effectiveness Information 6. Public Reporting of Physician Financial Relationships http: //www. medpac. gov/document_search. cfm 7. Revised Prospective Payment System for Skilled Nursing Facilities
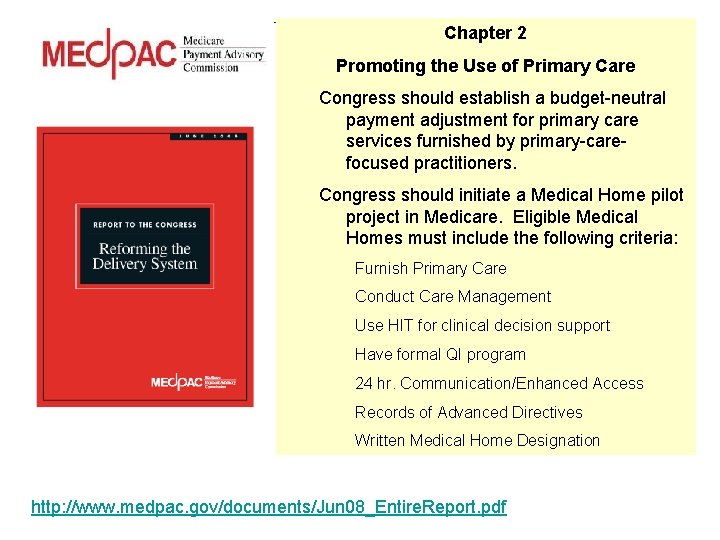
Chapter 2 Promoting the Use of Primary Care Congress should establish a budget-neutral payment adjustment for primary care services furnished by primary-carefocused practitioners. Congress should initiate a Medical Home pilot project in Medicare. Eligible Medical Homes must include the following criteria: Furnish Primary Care Conduct Care Management Use HIT for clinical decision support Have formal QI program 24 hr. Communication/Enhanced Access Records of Advanced Directives Written Medical Home Designation http: //www. medpac. gov/documents/Jun 08_Entire. Report. pdf
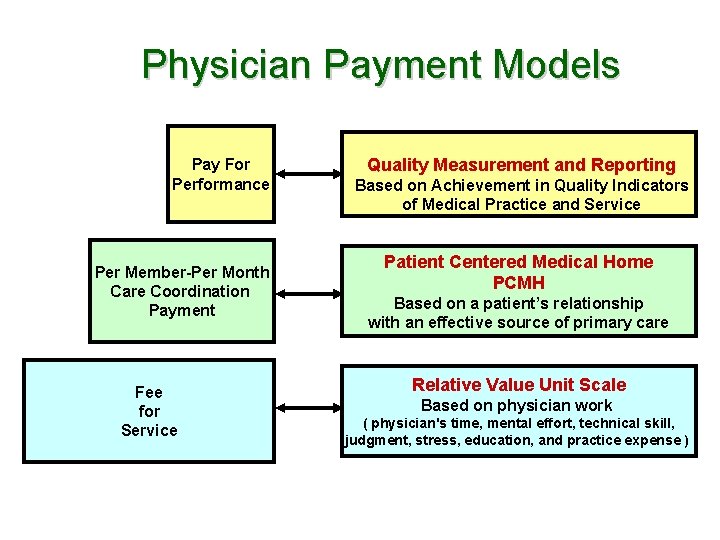
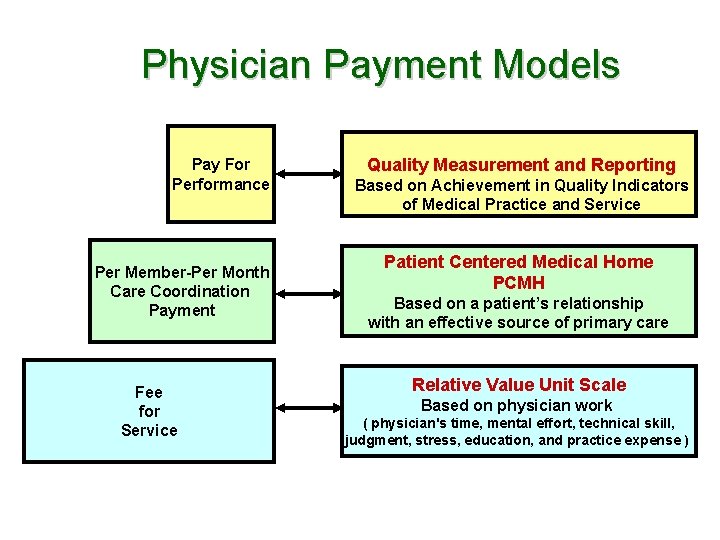
Physician Payment Models Pay For Performance Per Member-Per Month Care Coordination Payment Fee for Service Quality Measurement and Reporting Based on Achievement in Quality Indicators of Medical Practice and Service Patient Centered Medical Home PCMH Based on a patient’s relationship with an effective source of primary care Relative Value Unit Scale Based on physician work ( physician's time, mental effort, technical skill, judgment, stress, education, and practice expense )
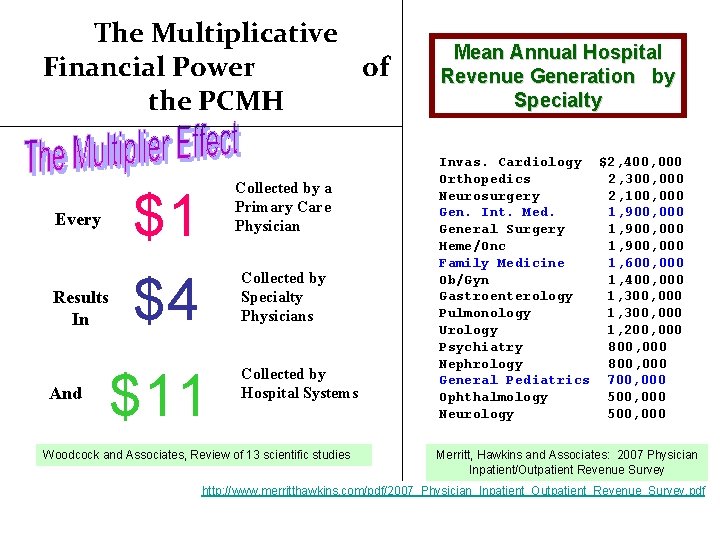
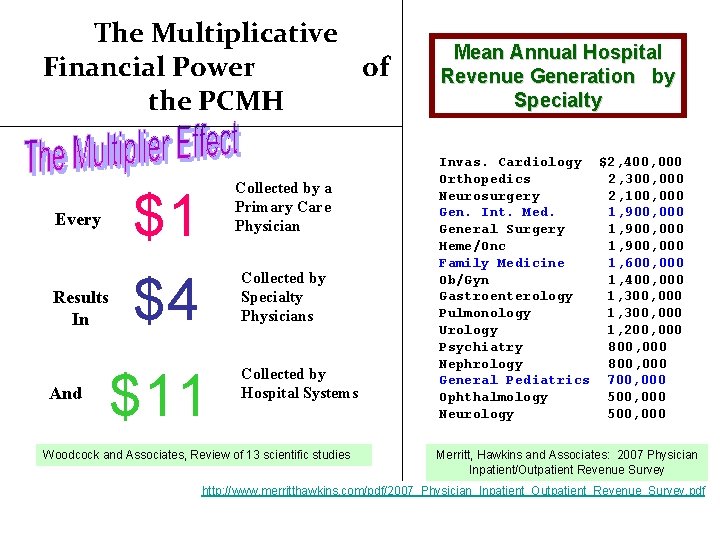
The Multiplicative Financial Power of the PCMH Every Results In And Collected by a Primary Care Physician $1 $4 Collected by Specialty Physicians $11 Collected by Hospital Systems Woodcock and Associates, Review of 13 scientific studies Mean Annual Hospital Revenue Generation by Specialty Invas. Cardiology $2, 400, 000 Orthopedics 2, 300, 000 Neurosurgery 2, 100, 000 Gen. Int. Med. 1, 900, 000 General Surgery 1, 900, 000 Heme/Onc 1, 900, 000 Family Medicine 1, 600, 000 Ob/Gyn 1, 400, 000 Gastroenterology 1, 300, 000 Pulmonology 1, 300, 000 Urology 1, 200, 000 Psychiatry 800, 000 Nephrology 800, 000 General Pediatrics 700, 000 Ophthalmology 500, 000 Neurology 500, 000 Merritt, Hawkins and Associates: 2007 Physician Inpatient/Outpatient Revenue Survey http: //www. merritthawkins. com/pdf/2007_Physician_Inpatient_Outpatient_Revenue_Survey. pdf
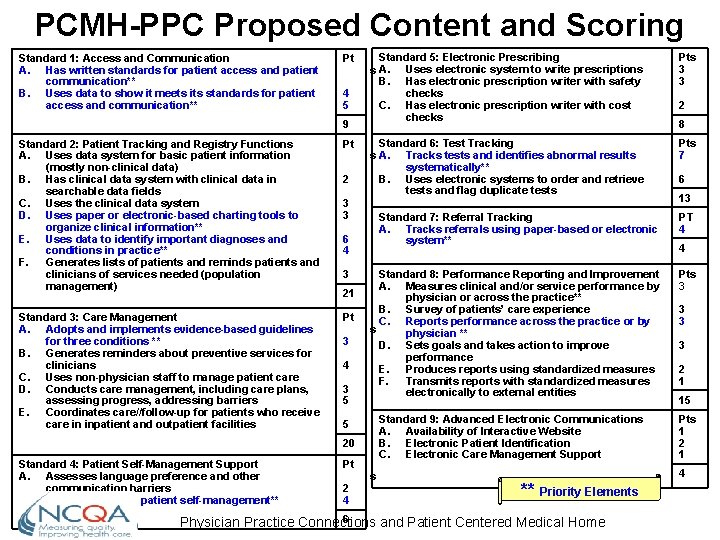
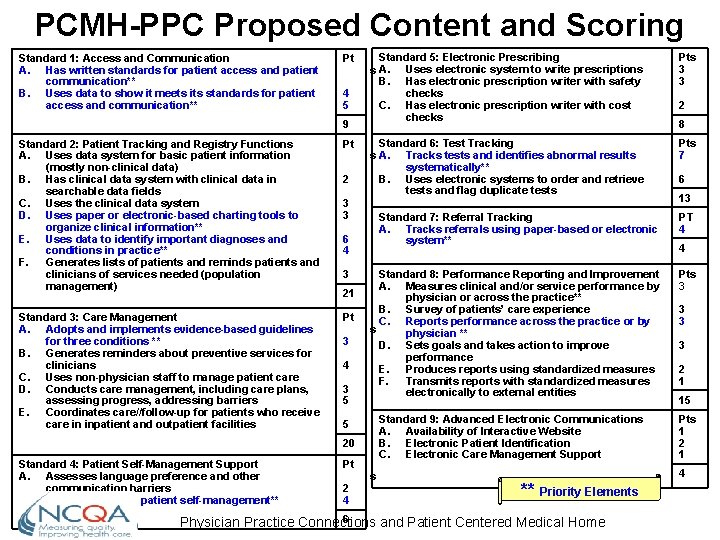
PCMH-PPC Proposed Content and Scoring Standard 1: Access and Communication A. Has written standards for patient access and patient communication** B. Uses data to show it meets its standards for patient access and communication** Pt 4 5 9 Standard 2: Patient Tracking and Registry Functions A. Uses data system for basic patient information (mostly non-clinical data) B. Has clinical data system with clinical data in searchable data fields C. Uses the clinical data system D. Uses paper or electronic-based charting tools to organize clinical information** E. Uses data to identify important diagnoses and conditions in practice** F. Generates lists of patients and reminds patients and clinicians of services needed (population management) Pt Standard 3: Care Management A. Adopts and implements evidence-based guidelines for three conditions ** B. Generates reminders about preventive services for clinicians C. Uses non-physician staff to manage patient care D. Conducts care management, including care plans, assessing progress, addressing barriers E. Coordinates care//follow-up for patients who receive care in inpatient and outpatient facilities Pt 2 Standard 5: Electronic Prescribing s A. Uses electronic system to write prescriptions B. Has electronic prescription writer with safety checks C. Has electronic prescription writer with cost checks Pts 3 3 Standard 6: Test Tracking s A. Tracks tests and identifies abnormal results systematically** B. Uses electronic systems to order and retrieve tests and flag duplicate tests Pts 7 3 3 21 3 4 3 5 2 4 13 Standard 8: Performance Reporting and Improvement A. Measures clinical and/or service performance by physician or across the practice** B. Survey of patients’ care experience C. Reports performance across the practice or by s physician ** D. Sets goals and takes action to improve performance E. Produces reports using standardized measures F. Transmits reports with standardized measures electronically to external entities Pts 3 Standard 9: Advanced Electronic Communications A. Availability of Interactive Website B. Electronic Patient Identification C. Electronic Care Management Support 5 Pt 6 PT 4 20 Standard 4: Patient Self-Management Support A. Assesses language preference and other communication barriers B. Actively supports patient self-management** 8 Standard 7: Referral Tracking A. Tracks referrals using paper-based or electronic system** 6 4 3 2 s ** Priority Elements 6 Physician Practice Connections and Patient Centered Medical Home 4 3 3 3 2 1 15 Pts 1 2 1 4
Framework – Application Slides from AAFP
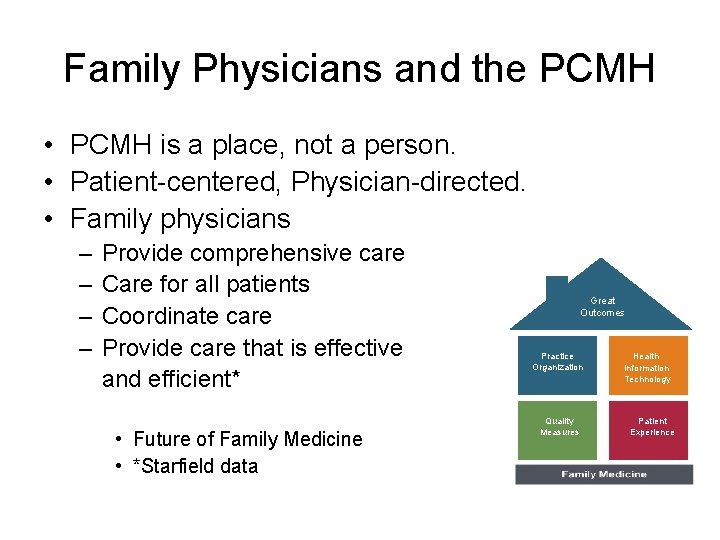
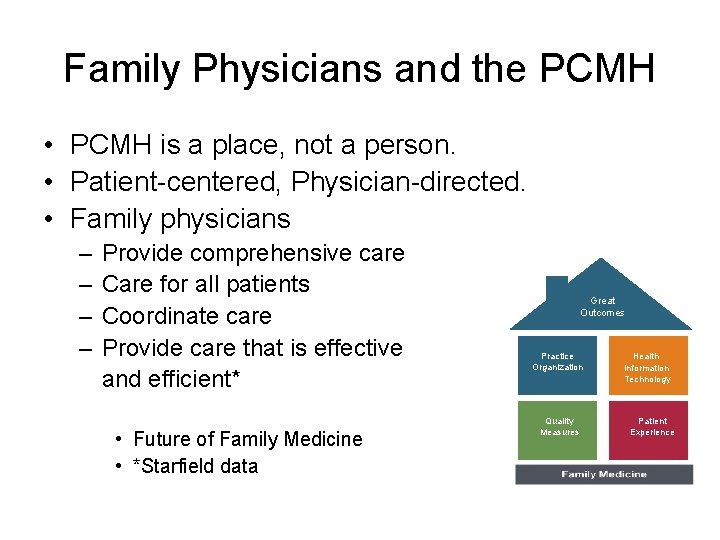
Family Physicians and the PCMH • PCMH is a place, not a person. • Patient-centered, Physician-directed. • Family physicians – – Provide comprehensive care Care for all patients Coordinate care Provide care that is effective and efficient* • Future of Family Medicine • *Starfield data Great Outcomes Practice Organization Quality Measures Health Information Technology Patient Experience
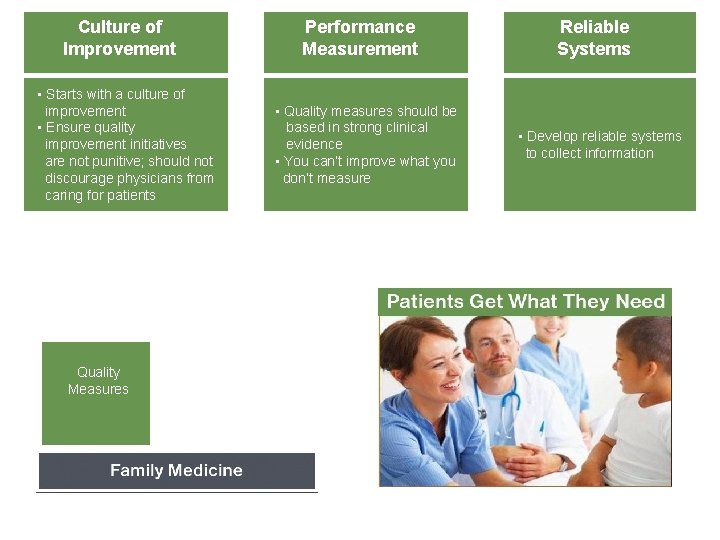
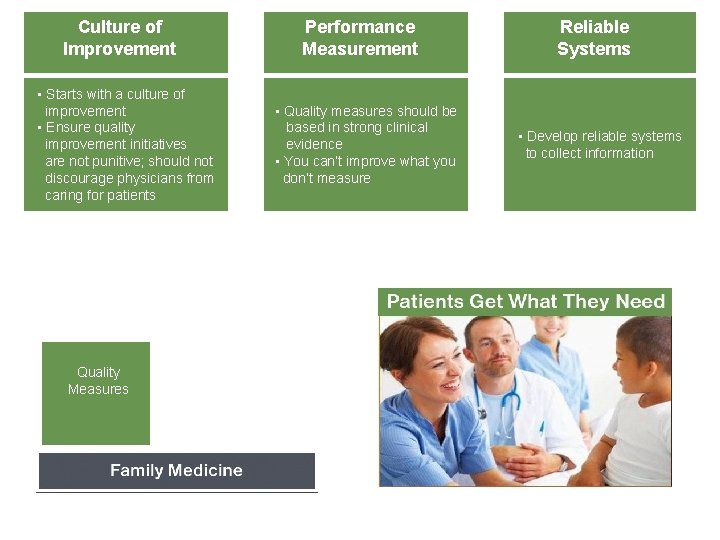
Culture of Improvement • Starts with a culture of improvement • Ensure quality improvement initiatives are not punitive; should not discourage physicians from caring for patients Quality Measures Performance Measurement • Quality measures should be based in strong clinical evidence • You can’t improve what you don’t measure Reliable Systems • Develop reliable systems to collect information
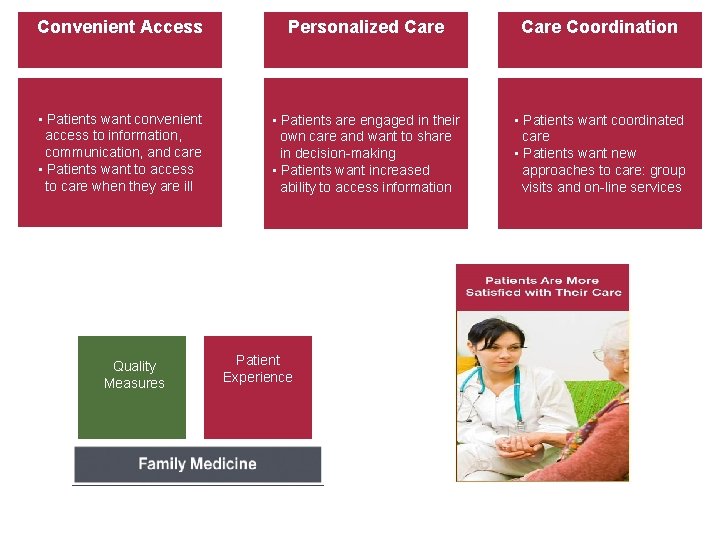
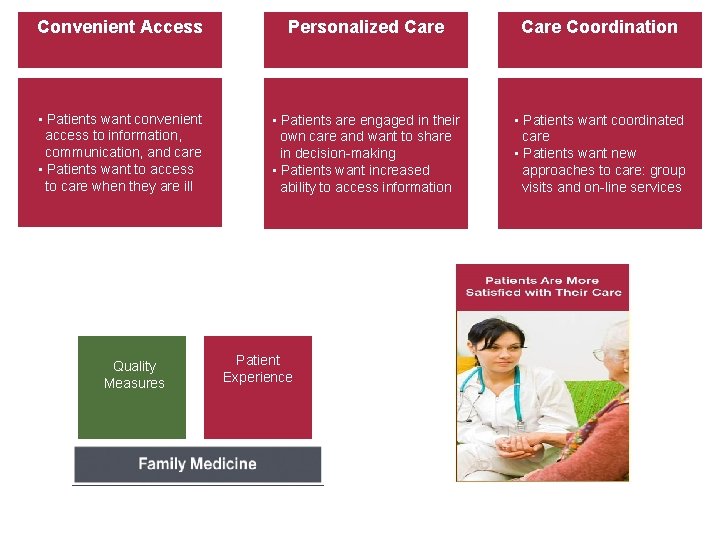
Convenient Access Personalized Care Coordination • Patients want convenient access to information, communication, and care • Patients want to access to care when they are ill • Patients are engaged in their own care and want to share in decision-making • Patients want increased ability to access information • Patients want coordinated care • Patients want new approaches to care: group visits and on-line services Quality Measures Patient Experience
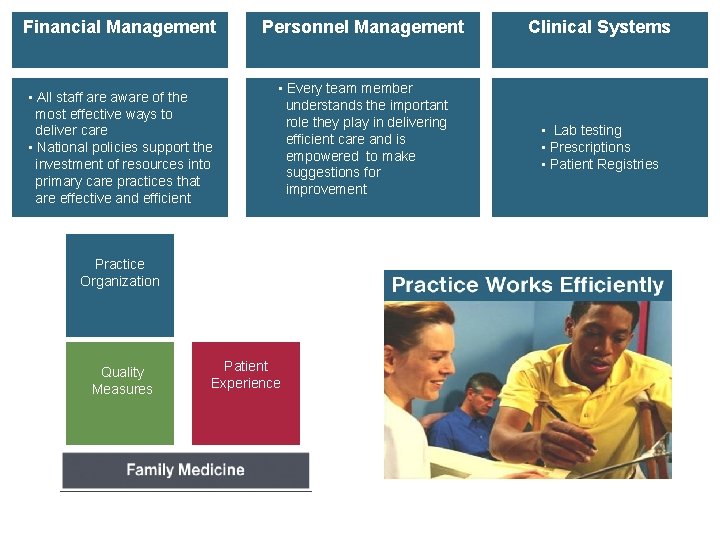
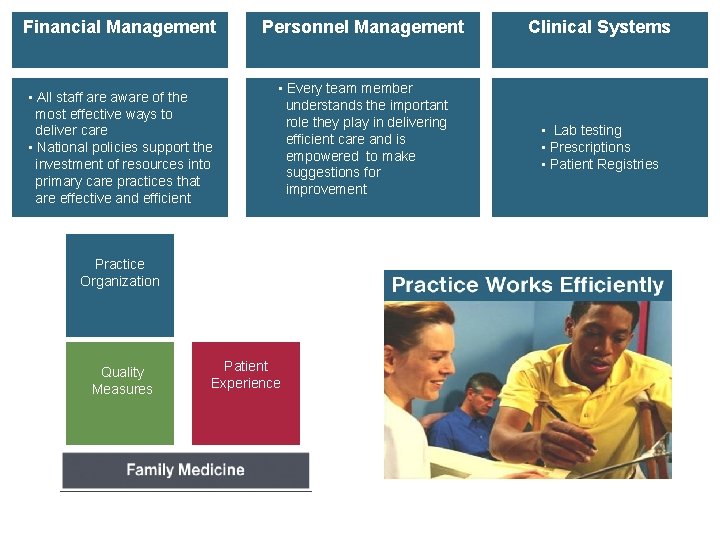
Financial Management • All staff are aware of the most effective ways to deliver care • National policies support the investment of resources into primary care practices that are effective and efficient Personnel Management • Every team member understands the important role they play in delivering efficient care and is empowered to make suggestions for improvement Practice Organization Quality Measures Patient Experience Clinical Systems • Lab testing • Prescriptions • Registries • Lab testing • Prescriptions • Patient Registries
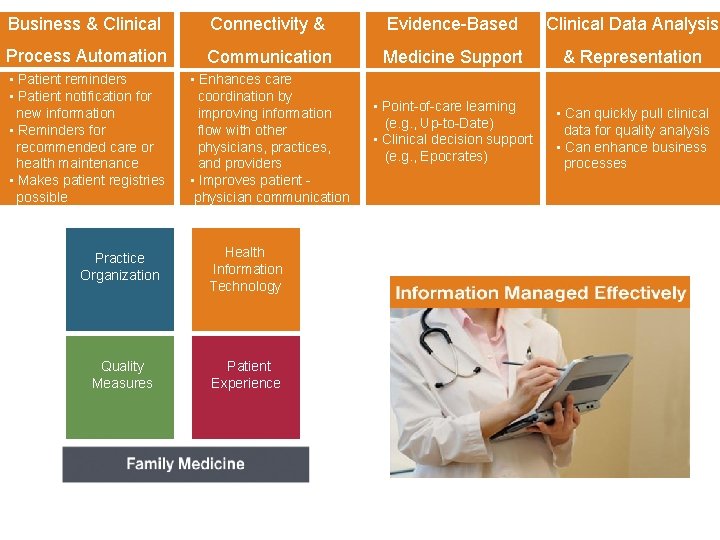
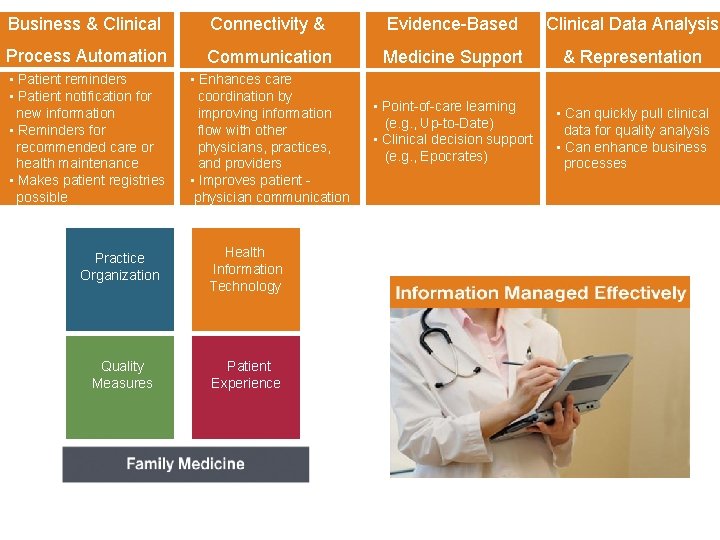
Business & Clinical Connectivity & Evidence-Based Clinical Data Analysis Process Automation Communication Medicine Support & Representation • Patient reminders • Patient notification for new information • Reminders for recommended care or health maintenance • Makes patient registries possible • Enhances care coordination by improving information flow with other physicians, practices, and providers • Improves patient physician communication • Point-of-care learning (e. g. , Up-to-Date) • Clinical decision support (e. g. , Epocrates) • Can quickly pull clinical data for quality analysis • Can enhance business processes Practice Organization Health Information Technology Quality Measures Patient Experience Family Medicine Foundation
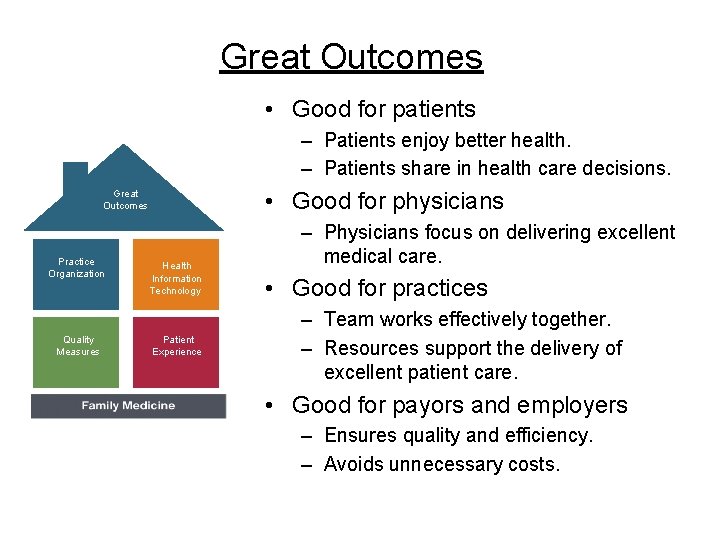
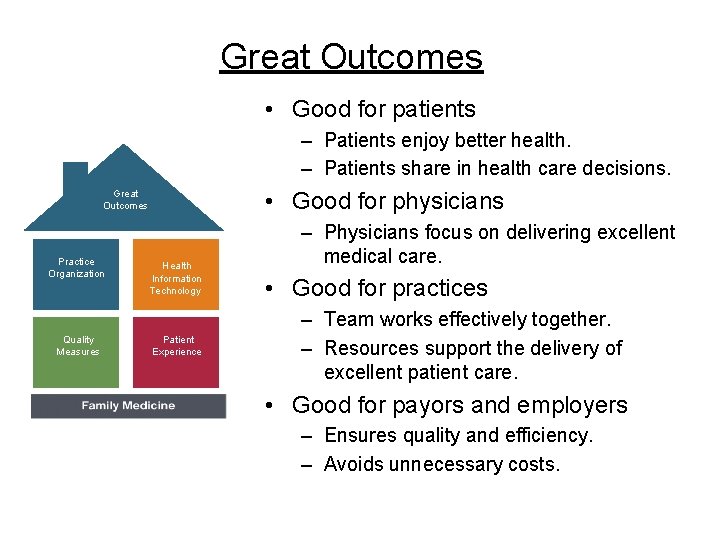
Great Outcomes • Good for patients – Patients enjoy better health. – Patients share in health care decisions. • Good for physicians Great Outcomes Practice Organization Quality Measures Health Information Technology Patient Experience Family Medicine Foundation – Physicians focus on delivering excellent medical care. • Good for practices – Team works effectively together. – Resources support the delivery of excellent patient care. • Good for payors and employers – Ensures quality and efficiency. – Avoids unnecessary costs.
Goals – Education & Recruitment
Teaching Opportunities • • • Rotation – How Many Weeks? Curriculum – Existing Assignments? Experience – Patient Care? Teaching – Frequency / Format? Today’s Presentation – Framing Concepts of the PCMH
Family Medicine Digital Resource Library • • http: //www. fmdrl. org Open to Everyone Search Lausen Resources, Power. Points, Documents
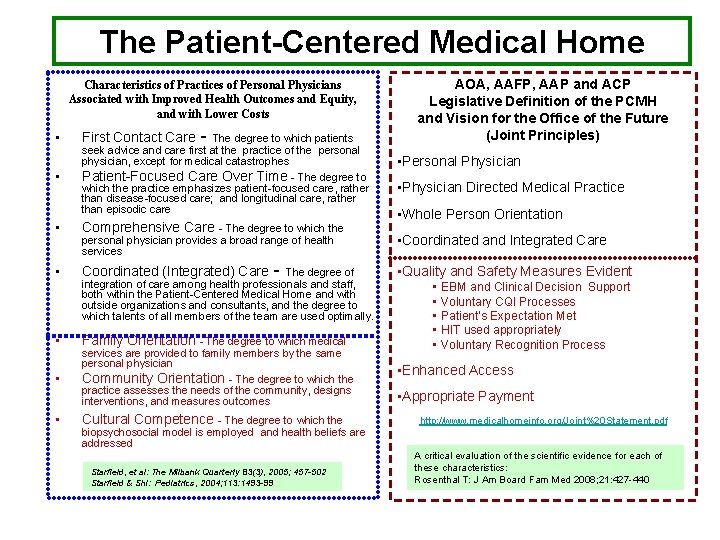
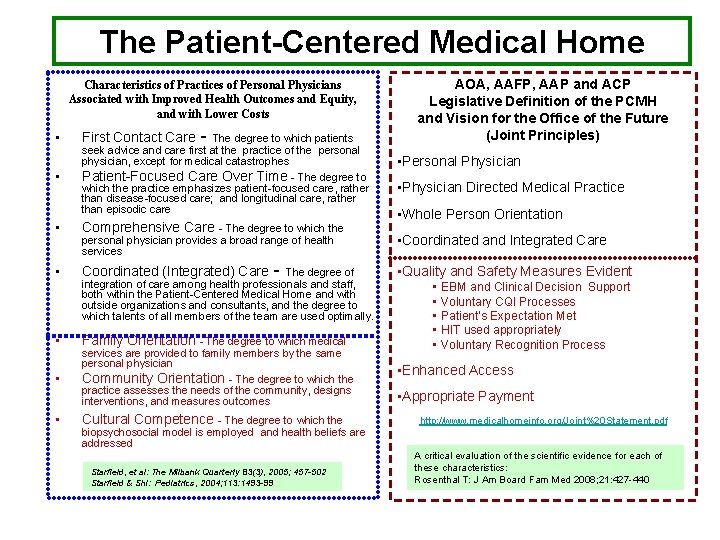
The Patient-Centered Medical Home Characteristics of Practices of Personal Physicians Associated with Improved Health Outcomes and Equity, and with Lower Costs • • First Contact Care - The degree to which patients seek advice and care first at the practice of the personal physician, except for medical catastrophes Patient-Focused Care Over Time - The degree to which the practice emphasizes patient-focused care, rather than disease-focused care; and longitudinal care, rather than episodic care • Comprehensive Care • Coordinated (Integrated) Care • • • - The degree to which the personal physician provides a broad range of health services - The degree of integration of care among health professionals and staff, both within the Patient-Centered Medical Home and with outside organizations and consultants, and the degree to which talents of all members of the team are used optimally. Family Orientation - The degree to which medical services are provided to family members by the same personal physician Community Orientation - The degree to which the practice assesses the needs of the community, designs interventions, and measures outcomes Cultural Competence - The degree to which the biopsychosocial model is employed and health beliefs are addressed Starfield, et al: The Milbank Quarterly 83(3), 2005; 457 -502 Starfield & Shi: Pediatrics, 2004; 113: 1493 -99 AOA, AAFP, AAP and ACP Legislative Definition of the PCMH and Vision for the Office of the Future (Joint Principles) • Personal Physician • Physician Directed Medical Practice • Whole Person Orientation • Coordinated and Integrated Care • Quality and Safety Measures Evident • EBM and Clinical Decision Support • Voluntary CQI Processes • Patient’s Expectation Met • HIT used appropriately • Voluntary Recognition Process • Enhanced Access • Appropriate Payment http: //www. medicalhomeinfo. org/Joint%20 Statement. pdf A critical evaluation of the scientific evidence for each of these characteristics: Rosenthal T: J Am Board Fam Med 2008; 21: 427 -440
Educational Approaches • 10 Concepts from PCMH Descriptions • Reframe the Context • Approaches – Discussion – Reflective Writing – Worksheet / Exercise – Assignment – Real Clinic Examples
Be Interactive • • Share Your Ideas Discuss As We Go Ask Questions Comments & Concerns
Our 10 - Today • • • Personal Physician / Longitudinal Care Longitudinal Patient-Focused Care Cultural Competence Coordinated / Integrated Care Community Orientation Comprehensive Whole-Person Care Enhanced Access Evidence-Based Medicine Quality Improvement Clinical Decision Support
Personal Physician / Longitudinal Care • Longitudinal Patient-Focused Care (the degree to which the practice emphasizes patient-focused care, rather than disease-focused care; and longitudinal care, rather than episodic care) • • Biopsychosocial Model Personal Knowledge of Patient Medical / Personal Health History Social Context of the Patient – Socioeconomics – Health Belief System – Health Literacy
PC-MH Reflection • Introduction: The purpose of this assignment is to promote the recognition of a specific characteristic of the Patient-Centered Medical Home that has been associated with improved health outcomes and lower costs. • Longitudinal Patient-Focused Care (the degree to which the practice emphasizes patient-focused care, rather than diseasefocused care; and longitudinal care, rather than episodic care) • Instructions: Reflect or Discuss your specific experience regarding an established patient of the clinic. How did the relationship with and prior knowledge of the patient affect the office visit, information discussed, treatment plan, and future care / studies / labs?
Longitudinal Patient-Focused Care • Longitudinal Patient-Focused Care (the degree to which the practice emphasizes patient-focused care, rather than disease-focused care; and longitudinal care, rather than episodic care) • Health Literacy • Patient Education
Health Literacy • Knowing Your Patients – Education Level – Reading Ability – Comprehension • Health Literacy Assessment Tool – http: //www. pfizerhealthliteracy. com/physicians -providers/default. html#


Health Literacy Exercise • Mr. Stone is 57 and often is a “difficult” patient because he doesn’t seem to adhere to your management recommendations. His BMI is 37 and his BP is 148/78. He is not diabetic, leads a sedentary lifestyle, and prefers to eat meat and potatoes. You perform the Newest Vital Sign health literacy assessment on him and find he scores a 3 which indicates the possibility of limited literacy. You are talking to him about his hypertension. You begin to discuss diet and activity with him as a ways of controlling his weight. As you are talking he asks you what this has to do with hyperactive? He says for the past couple of years you have been telling him he is hyperactive and giving him a pill to take and told him to watch his diet and to exercise more but he can’t see what that has to do with being hyperactive. In fact he says he stopped taking his pill because he wasn’t hyperactive. • What do you think just happened? • What are some ways to approach management discussion with Mr. Stone? (discuss 3 different approaches) – Use simple words, pictures, teach back • Use the Personal Health Prescription supplied and write out a management goal for either nutrition or activity that you would provide to Mr. Stone. - make sure the recommendations are written in measurable goals- i. e. not walk more but walk 15 minutes per day
Patient Education Points • • • • Educates Patient on Diet / Weight Educates Patient on Medication Changes Educates Patient on Importance of Regular Physician Visits Educates Patient on Diabetes / Hypertension Management Educates Patient on Drug / Tobacco / Alcohol Use Assesses Barriers to Compliance / Understanding Assesses Readiness for Change Determines Patient Level of Understanding Avoids Medical Jargon Communicates with the Patient Clearly and Effectively Clearly Identifies Issues / Problems Utilizes Shared Decision-Making Develops Appropriate Patient Education Strategies Displays Understanding of Disease Pathophysiology
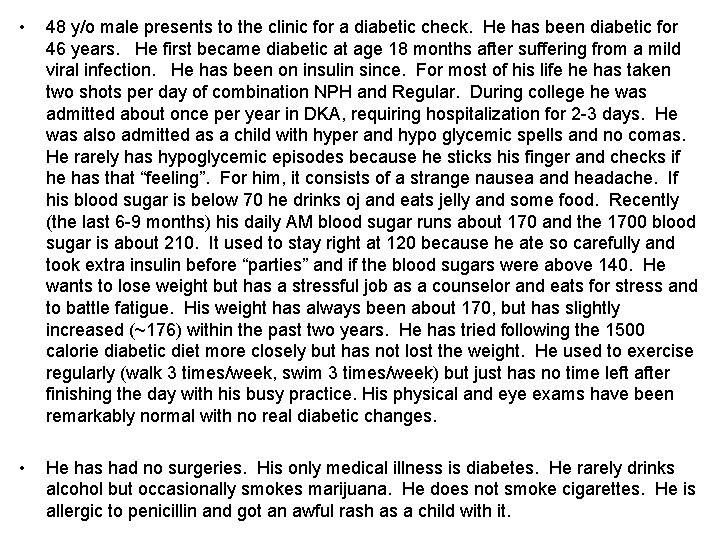
• 48 y/o male presents to the clinic for a diabetic check. He has been diabetic for 46 years. He first became diabetic at age 18 months after suffering from a mild viral infection. He has been on insulin since. For most of his life he has taken two shots per day of combination NPH and Regular. During college he was admitted about once per year in DKA, requiring hospitalization for 2 -3 days. He was also admitted as a child with hyper and hypo glycemic spells and no comas. He rarely has hypoglycemic episodes because he sticks his finger and checks if he has that “feeling”. For him, it consists of a strange nausea and headache. If his blood sugar is below 70 he drinks oj and eats jelly and some food. Recently (the last 6 -9 months) his daily AM blood sugar runs about 170 and the 1700 blood sugar is about 210. It used to stay right at 120 because he ate so carefully and took extra insulin before “parties” and if the blood sugars were above 140. He wants to lose weight but has a stressful job as a counselor and eats for stress and to battle fatigue. His weight has always been about 170, but has slightly increased (~176) within the past two years. He has tried following the 1500 calorie diabetic diet more closely but has not lost the weight. He used to exercise regularly (walk 3 times/week, swim 3 times/week) but just has no time left after finishing the day with his busy practice. His physical and eye exams have been remarkably normal with no real diabetic changes. • He has had no surgeries. His only medical illness is diabetes. He rarely drinks alcohol but occasionally smokes marijuana. He does not smoke cigarettes. He is allergic to penicillin and got an awful rash as a child with it.
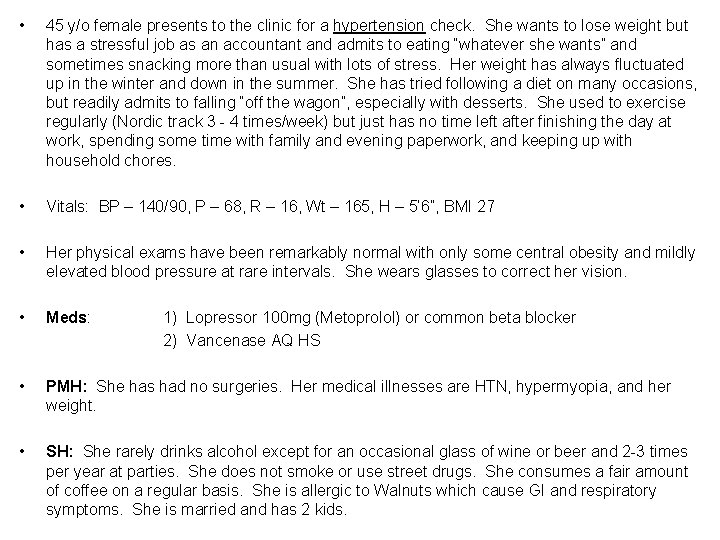
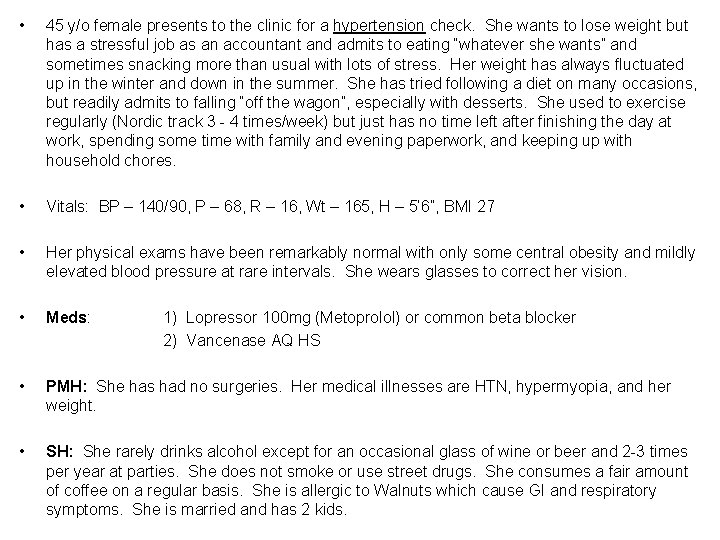
• 45 y/o female presents to the clinic for a hypertension check. She wants to lose weight but has a stressful job as an accountant and admits to eating “whatever she wants” and sometimes snacking more than usual with lots of stress. Her weight has always fluctuated up in the winter and down in the summer. She has tried following a diet on many occasions, but readily admits to falling “off the wagon”, especially with desserts. She used to exercise regularly (Nordic track 3 - 4 times/week) but just has no time left after finishing the day at work, spending some time with family and evening paperwork, and keeping up with household chores. • Vitals: BP – 140/90, P – 68, R – 16, Wt – 165, H – 5’ 6”, BMI 27 • Her physical exams have been remarkably normal with only some central obesity and mildly elevated blood pressure at rare intervals. She wears glasses to correct her vision. • Meds: • PMH: She has had no surgeries. Her medical illnesses are HTN, hypermyopia, and her weight. • SH: She rarely drinks alcohol except for an occasional glass of wine or beer and 2 -3 times per year at parties. She does not smoke or use street drugs. She consumes a fair amount of coffee on a regular basis. She is allergic to Walnuts which cause GI and respiratory symptoms. She is married and has 2 kids. 1) Lopressor 100 mg (Metoprolol) or common beta blocker 2) Vancenase AQ HS
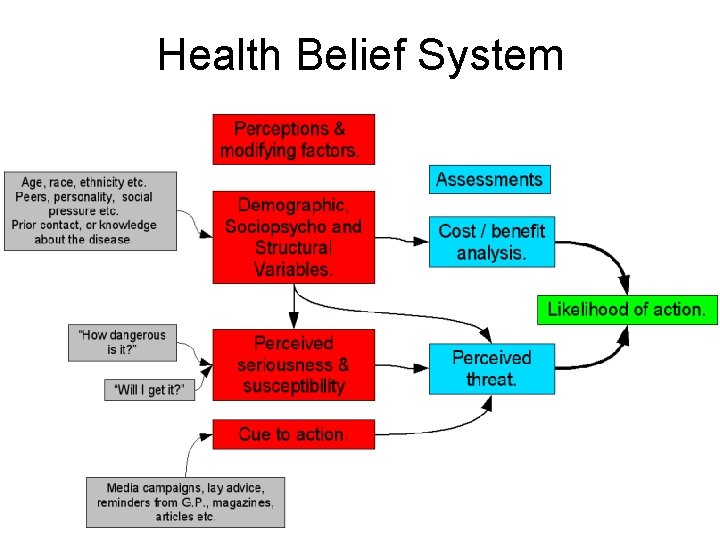
Cultural Competence • Cultural Competence (the degree to which the biopsychosocial model is employed and health beliefs are addressed) • Health Belief System • Shared Decision-Making
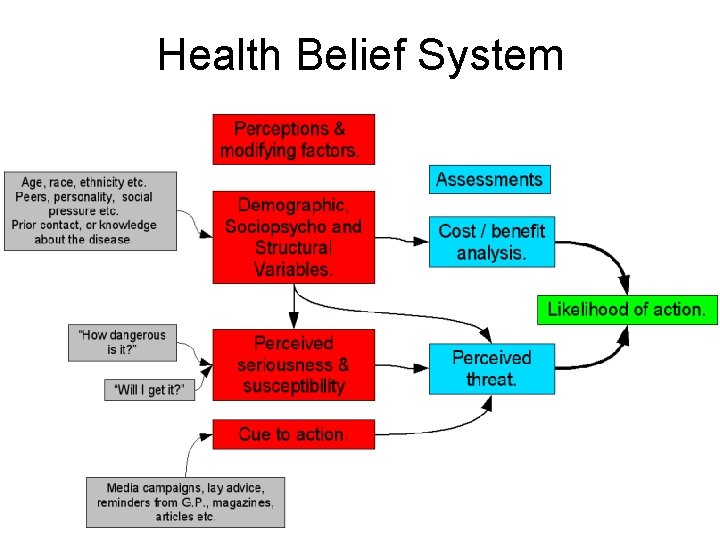
Health Belief System
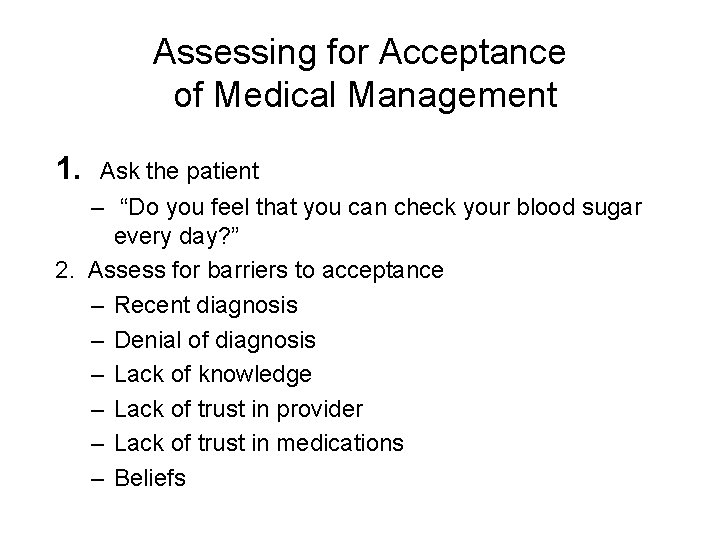
Assessing for Acceptance of Medical Management 1. Ask the patient – “Do you feel that you can check your blood sugar every day? ” 2. Assess for barriers to acceptance – Recent diagnosis – Denial of diagnosis – Lack of knowledge – Lack of trust in provider – Lack of trust in medications – Beliefs
Patient Ability & Adherence Assess for: 1. Barriers to adherence 2. Motivation for adherence 3. Skills needed for adherence
Medication Adherence What gets in the way of taking your medicine(s)? • Makes me feel sick • Cost • Can’t remember • Too many pills • Nothing • Other: Provider: remember to document asking the patient and the patient response!
Shared Decision-Making Rochester Participatory Decision-Making Scale http: //www. annfammed. org/cgi/reprint/3/5/436 Explain the clinical issue or nature of the decision Discussion of the uncertainties associated with the situation Clarification of agreement Examine barriers to follow-through with treatment plan Physician gives patient opportunity to ask questions and checks patients understanding of the treatment plan Physician’s medical language matches patient’s level of understanding **** Physician asks “Any questions? ” Physician asks open-ended questions Physician checks his/her understanding of patient’s point of view

Coordinated / Integrated Care • Coordinated/Integrated Care (the degree of integration of care among health professionals and staff, both within the PC-MH and with outside organizations and consultants) • • • Transitions of Care Specialty / Consultant Referrals Procedural / Treatment Referral Internal Referral Counseling / Education Community Services & Resources
PC-MH Reflection • Introduction: The purpose of this assignment is to promote the recognition of a specific characteristic of the Patient-Centered Medical Home that has been associated with improved health outcomes and lower costs. • Coordinated/Integrated Care (the degree of integration of care among health professionals and staff, both within the PC-MH and with outside organizations and consultants) • Instructions: Reflect or Discuss your specific experience regarding an established patient of the clinic. How did the provider / practice assist the patient with coordinating care to consultants, allied health professionals, community resources, and/or care transitions? How does the practice track these activities?
Community Orientation • Community Orientation (the degree to which the practice assesses the needs of the community, designs interventions, and measures outcomes) • Your Role In the Community – Roles – Services – Procedures • COPC Process – Evaluate Need for Community – http: //www. mcg. edu/som/fmfacdev/fd_copc. htm
COPC Process • Community-Oriented Primary Care (COPC) is an approach to health care delivery that undertakes responsibility for the health of a defined population. COPC is practiced by combining epidemiologic study and social interventions with clinical care of individual patients, so that the primary care practice itself becomes a community medicine program. Both the individual patient and the community or population are the foci of diagnosis, treatment and ongoing surveillance. • What does COPC offer me, as a physician? The concept of COPC offers physicians the opportunity to impact significantly larger populations and ultimately alter a community's health. A change in the overall health in the community is reflected in better health for each individual patient the physician treats on a daily basis. • How do I implement COPC in my practice? There are basically four steps you will need to follow to transform your primary care practice into a community medicine program: Define the population. Assess the defined population's health needs. Organize an effective intervention strategy. Evaluate the success of the intervention.
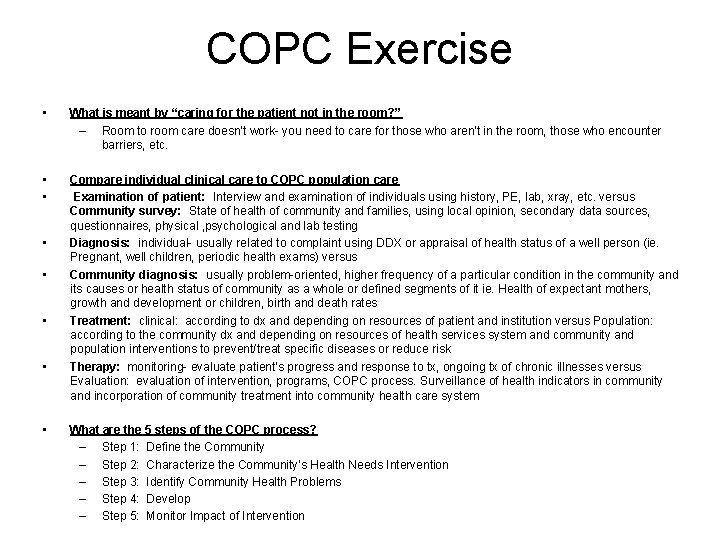
COPC Exercise • What is meant by “caring for the patient not in the room? ” – Room to room care doesn’t work- you need to care for those who aren’t in the room, those who encounter barriers, etc. • • Compare individual clinical care to COPC population care Examination of patient: Interview and examination of individuals using history, PE, lab, xray, etc. versus Community survey: State of health of community and families, using local opinion, secondary data sources, questionnaires, physical , psychological and lab testing Diagnosis: individual- usually related to complaint using DDX or appraisal of health status of a well person (ie. Pregnant, well children, periodic health exams) versus Community diagnosis: usually problem-oriented, higher frequency of a particular condition in the community and its causes or health status of community as a whole or defined segments of it ie. Health of expectant mothers, growth and development or children, birth and death rates Treatment: clinical: according to dx and depending on resources of patient and institution versus Population: according to the community dx and depending on resources of health services system and community and population interventions to prevent/treat specific diseases or reduce risk Therapy: monitoring- evaluate patient’s progress and response to tx, ongoing tx of chronic illnesses versus Evaluation: evaluation of intervention, programs, COPC process. Surveillance of health indicators in community and incorporation of community treatment into community health care system • • • What are the 5 steps of the COPC process? – Step 1: Define the Community – Step 2: Characterize the Community’s Health Needs Intervention – Step 3: Identify Community Health Problems – Step 4: Develop – Step 5: Monitor Impact of Intervention
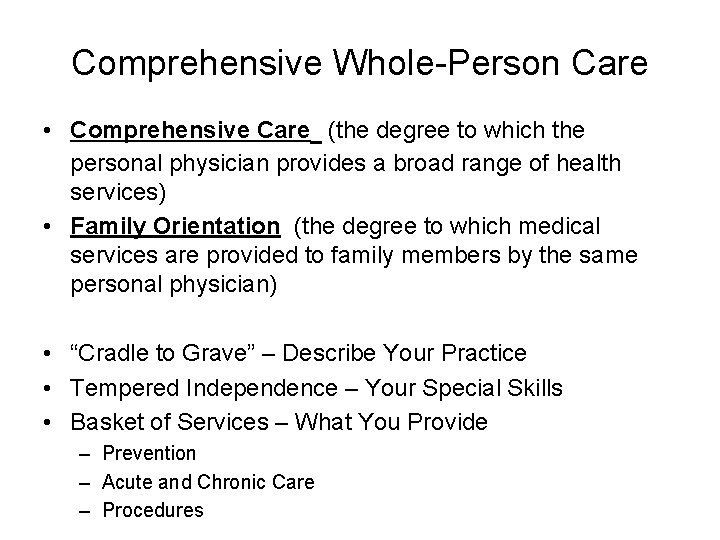
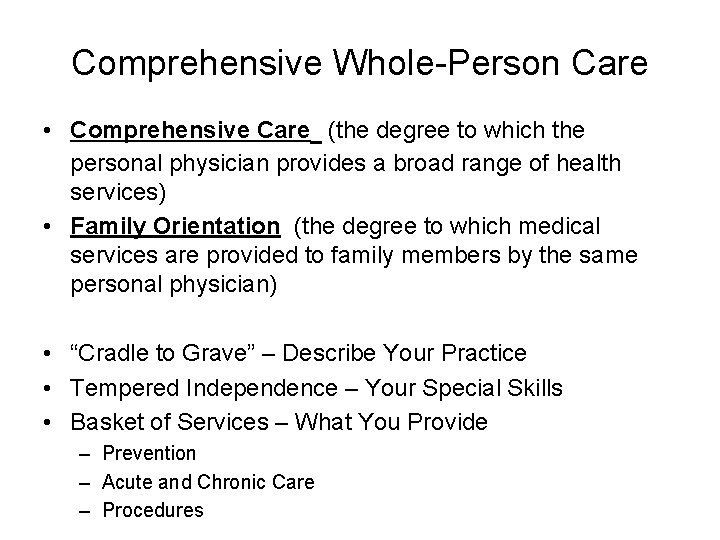
Comprehensive Whole-Person Care • Comprehensive Care (the degree to which the personal physician provides a broad range of health services) • Family Orientation (the degree to which medical services are provided to family members by the same personal physician) • “Cradle to Grave” – Describe Your Practice • Tempered Independence – Your Special Skills • Basket of Services – What You Provide – Prevention – Acute and Chronic Care – Procedures
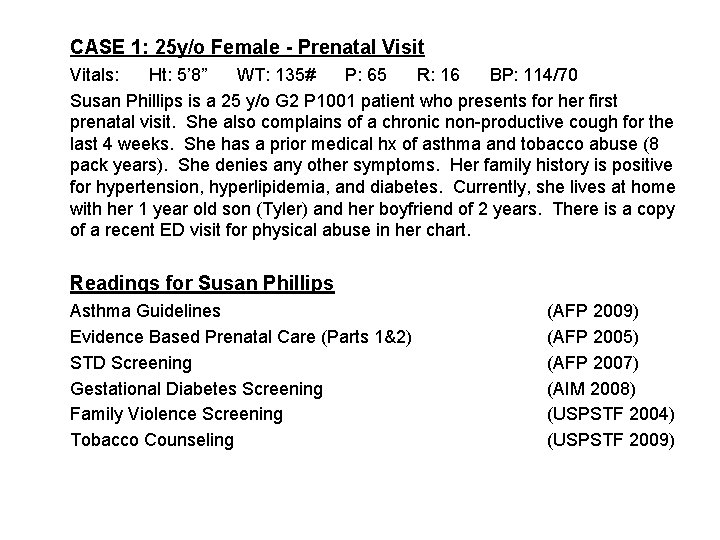
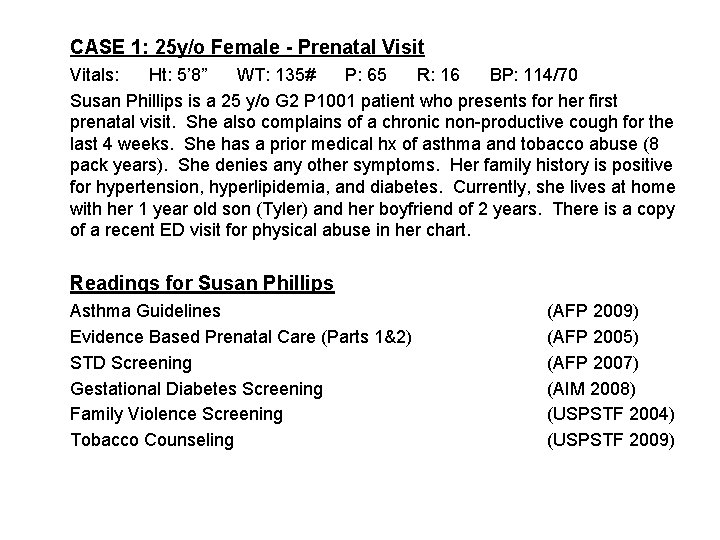
CASE 1: 25 y/o Female - Prenatal Visit Vitals: Ht: 5’ 8” WT: 135# P: 65 R: 16 BP: 114/70 Susan Phillips is a 25 y/o G 2 P 1001 patient who presents for her first prenatal visit. She also complains of a chronic non-productive cough for the last 4 weeks. She has a prior medical hx of asthma and tobacco abuse (8 pack years). She denies any other symptoms. Her family history is positive for hypertension, hyperlipidemia, and diabetes. Currently, she lives at home with her 1 year old son (Tyler) and her boyfriend of 2 years. There is a copy of a recent ED visit for physical abuse in her chart. Readings for Susan Phillips Asthma Guidelines Evidence Based Prenatal Care (Parts 1&2) STD Screening Gestational Diabetes Screening Family Violence Screening Tobacco Counseling (AFP 2009) (AFP 2005) (AFP 2007) (AIM 2008) (USPSTF 2004) (USPSTF 2009)
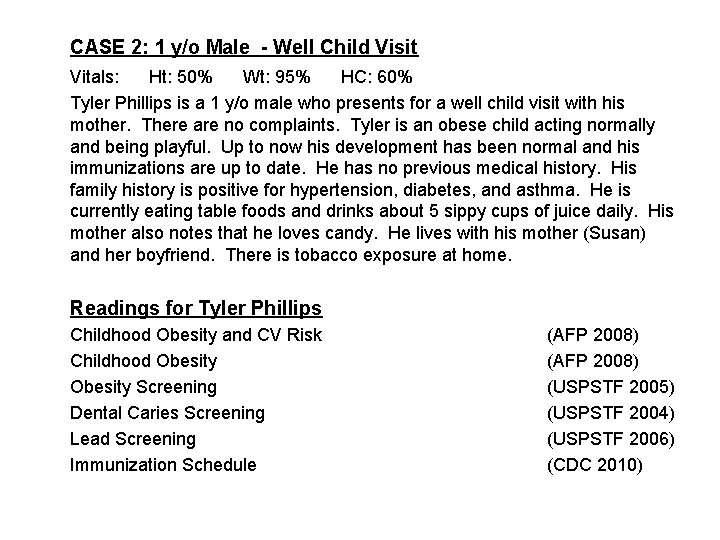
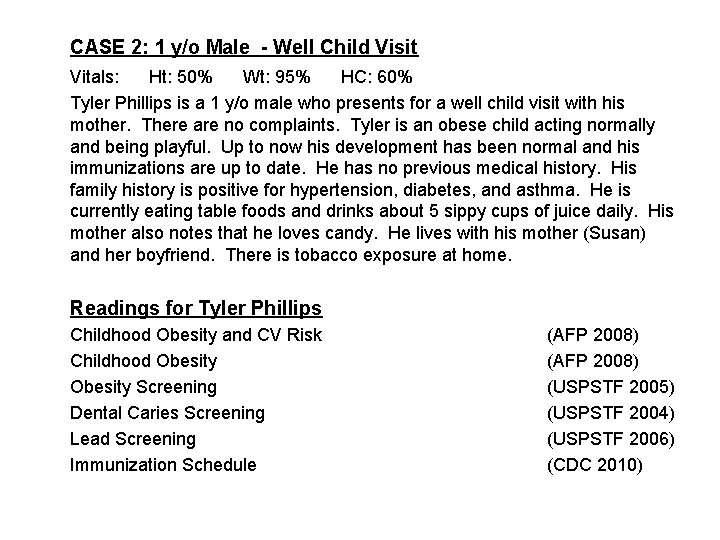
CASE 2: 1 y/o Male - Well Child Visit Vitals: Ht: 50% Wt: 95% HC: 60% Tyler Phillips is a 1 y/o male who presents for a well child visit with his mother. There are no complaints. Tyler is an obese child acting normally and being playful. Up to now his development has been normal and his immunizations are up to date. He has no previous medical history. His family history is positive for hypertension, diabetes, and asthma. He is currently eating table foods and drinks about 5 sippy cups of juice daily. His mother also notes that he loves candy. He lives with his mother (Susan) and her boyfriend. There is tobacco exposure at home. Readings for Tyler Phillips Childhood Obesity and CV Risk Childhood Obesity Screening Dental Caries Screening Lead Screening Immunization Schedule (AFP 2008) (USPSTF 2005) (USPSTF 2004) (USPSTF 2006) (CDC 2010)
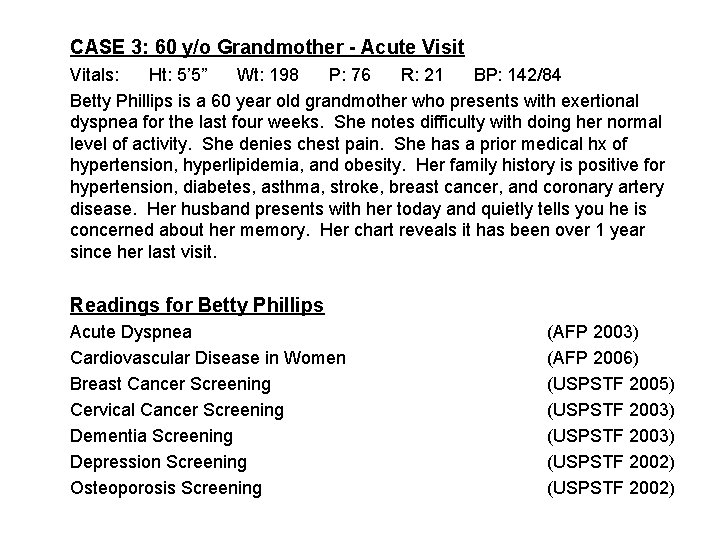
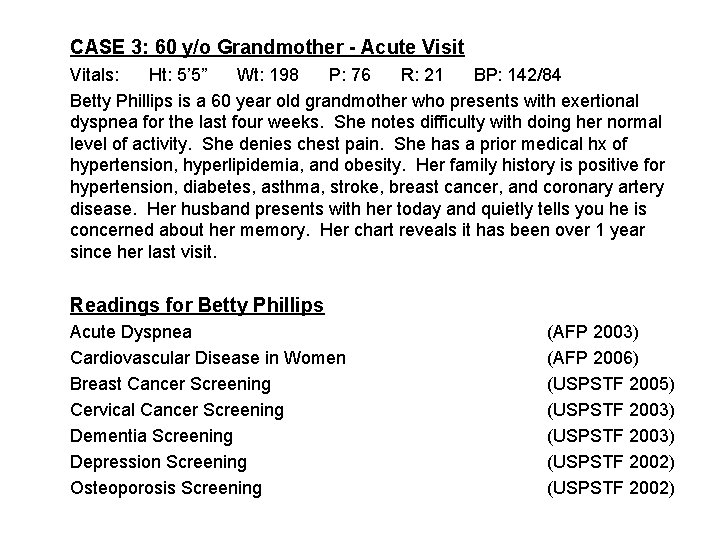
CASE 3: 60 y/o Grandmother - Acute Visit Vitals: Ht: 5’ 5” Wt: 198 P: 76 R: 21 BP: 142/84 Betty Phillips is a 60 year old grandmother who presents with exertional dyspnea for the last four weeks. She notes difficulty with doing her normal level of activity. She denies chest pain. She has a prior medical hx of hypertension, hyperlipidemia, and obesity. Her family history is positive for hypertension, diabetes, asthma, stroke, breast cancer, and coronary artery disease. Her husband presents with her today and quietly tells you he is concerned about her memory. Her chart reveals it has been over 1 year since her last visit. Readings for Betty Phillips Acute Dyspnea Cardiovascular Disease in Women Breast Cancer Screening Cervical Cancer Screening Dementia Screening Depression Screening Osteoporosis Screening (AFP 2003) (AFP 2006) (USPSTF 2005) (USPSTF 2003) (USPSTF 2002)
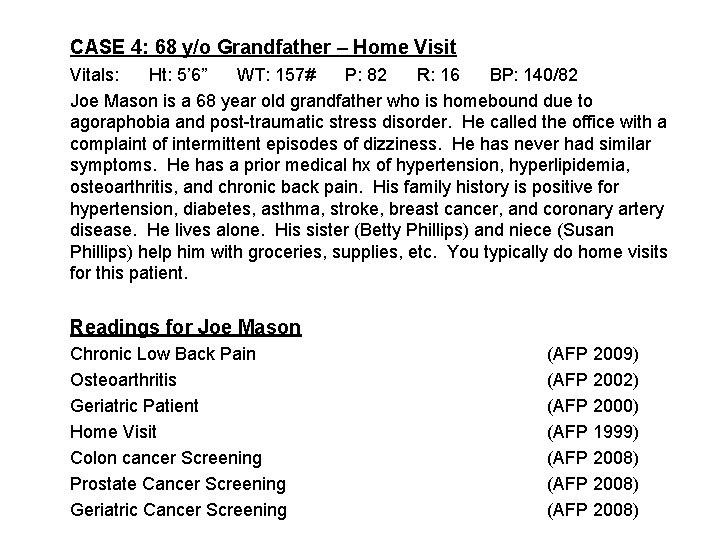
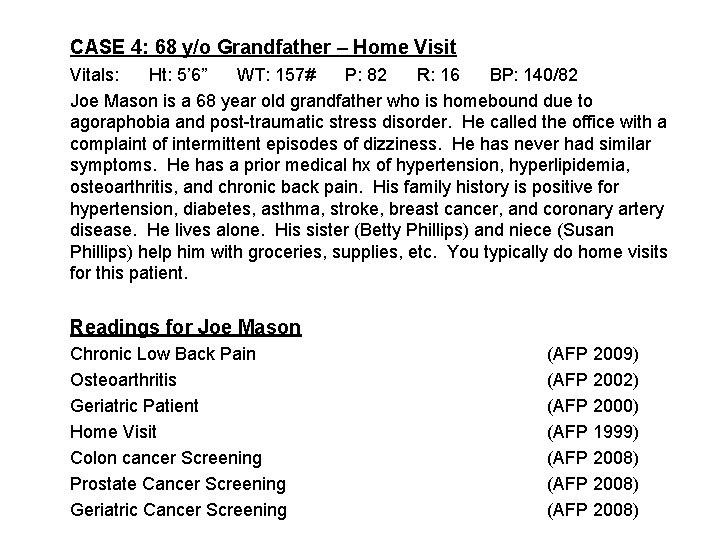
CASE 4: 68 y/o Grandfather – Home Visit Vitals: Ht: 5’ 6” WT: 157# P: 82 R: 16 BP: 140/82 Joe Mason is a 68 year old grandfather who is homebound due to agoraphobia and post-traumatic stress disorder. He called the office with a complaint of intermittent episodes of dizziness. He has never had similar symptoms. He has a prior medical hx of hypertension, hyperlipidemia, osteoarthritis, and chronic back pain. His family history is positive for hypertension, diabetes, asthma, stroke, breast cancer, and coronary artery disease. He lives alone. His sister (Betty Phillips) and niece (Susan Phillips) help him with groceries, supplies, etc. You typically do home visits for this patient. Readings for Joe Mason Chronic Low Back Pain Osteoarthritis Geriatric Patient Home Visit Colon cancer Screening Prostate Cancer Screening Geriatric Cancer Screening (AFP 2009) (AFP 2002) (AFP 2000) (AFP 1999) (AFP 2008)
Article References • American Academy of Family Physicians – http: //www. aafp. org/online/en/home/publicatio ns/journals/afp. html • USPSTF – http: //www. ahrq. gov/clinic/USpstfix. htm • Annals of Internal Medicine – http: //www. annals. org/content/by/year
Enhanced Access • What are Your Clinic Strategies? – Open Access Scheduling – Variable Office Hours – Electronic Patient Portal – Phone Visits / Tele-Health – Visit Options / Groups / Health Team • Patient Email Exercise – Specific Examples and Challenges – Scoring Rubric
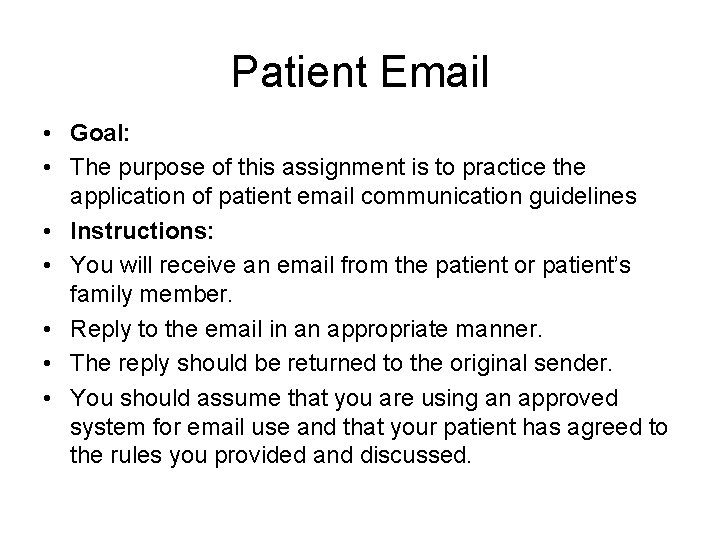
Patient Email • Goal: • The purpose of this assignment is to practice the application of patient email communication guidelines • Instructions: • You will receive an email from the patient or patient’s family member. • Reply to the email in an appropriate manner. • The reply should be returned to the original sender. • You should assume that you are using an approved system for email use and that your patient has agreed to the rules you provided and discussed.
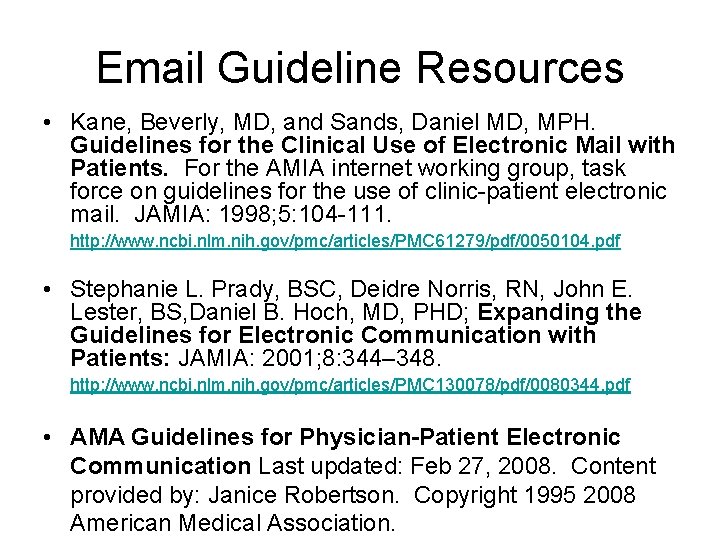
Email Guideline Resources • Kane, Beverly, MD, and Sands, Daniel MD, MPH. Guidelines for the Clinical Use of Electronic Mail with Patients. For the AMIA internet working group, task force on guidelines for the use of clinic-patient electronic mail. JAMIA: 1998; 5: 104 -111. http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 61279/pdf/0050104. pdf • Stephanie L. Prady, BSC, Deidre Norris, RN, John E. Lester, BS, Daniel B. Hoch, MD, PHD; Expanding the Guidelines for Electronic Communication with Patients: JAMIA: 2001; 8: 344– 348. http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 130078/pdf/0080344. pdf • AMA Guidelines for Physician-Patient Electronic Communication Last updated: Feb 27, 2008. Content provided by: Janice Robertson. Copyright 1995 2008 American Medical Association.
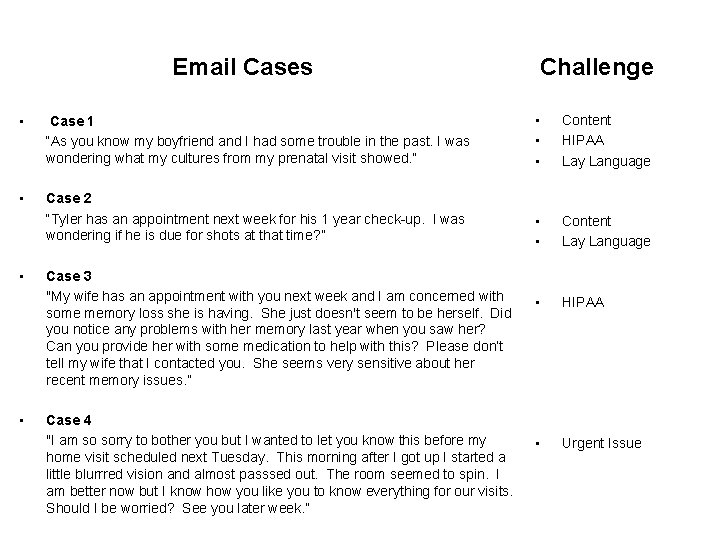
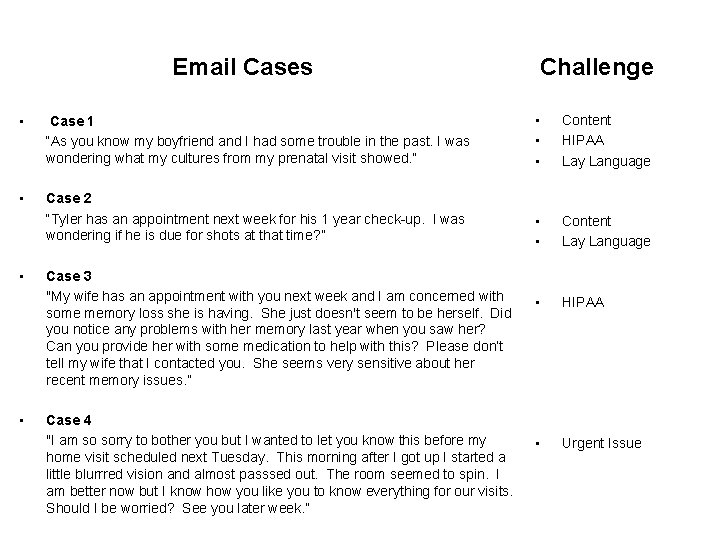
Email Cases Challenge • Case 1 “As you know my boyfriend and I had some trouble in the past. I was wondering what my cultures from my prenatal visit showed. ” • • • Content HIPAA Lay Language • Case 2 “Tyler has an appointment next week for his 1 year check-up. I was wondering if he is due for shots at that time? ” • • Content Lay Language • HIPAA • Urgent Issue • • Case 3 "My wife has an appointment with you next week and I am concerned with some memory loss she is having. She just doesn't seem to be herself. Did you notice any problems with her memory last year when you saw her? Can you provide her with some medication to help with this? Please don’t tell my wife that I contacted you. She seems very sensitive about her recent memory issues. ” Case 4 "I am so sorry to bother you but I wanted to let you know this before my home visit scheduled next Tuesday. This morning after I got up I started a little blurrred vision and almost passsed out. The room seemed to spin. I am better now but I know how you like you to know everything for our visits. Should I be worried? See you later week. ”
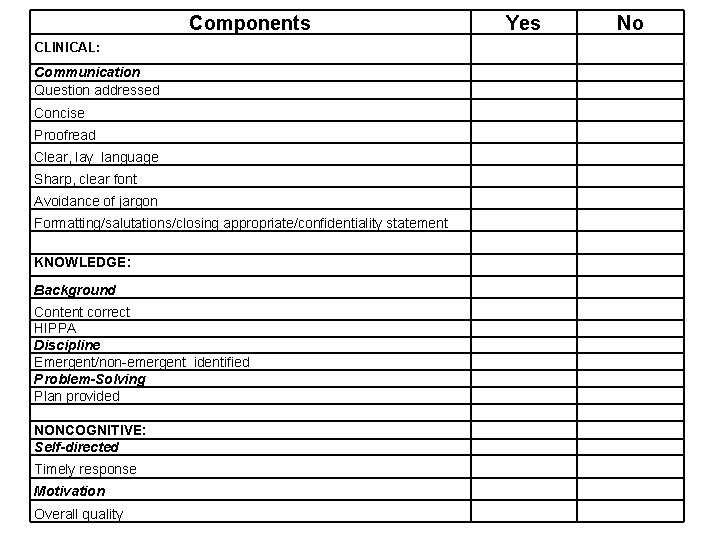
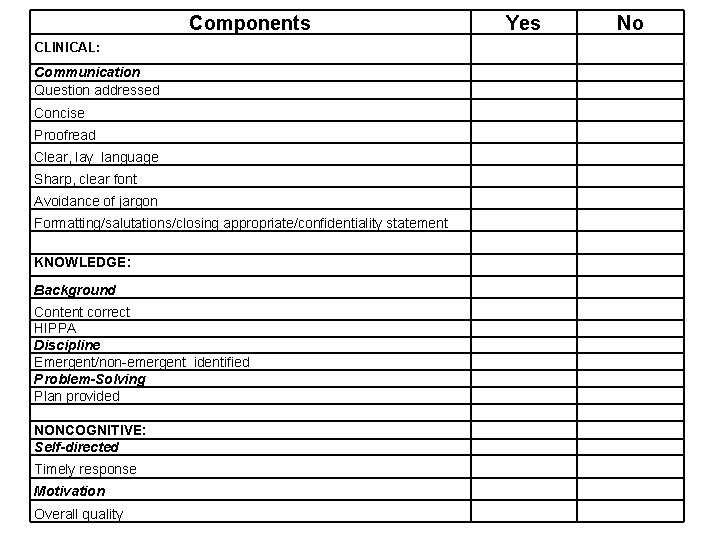
Components CLINICAL: Communication Question addressed Concise Proofread Clear, lay language Sharp, clear font Avoidance of jargon Formatting/salutations/closing appropriate/confidentiality statement KNOWLEDGE: Background Content correct HIPPA Discipline Emergent/non-emergent identified Problem-Solving Plan provided NONCOGNITIVE: Self-directed Timely response Motivation Overall quality Yes No
Quality Improvement • What Are Your Processes? – Clinical Assessment Program (AOA) – Maintenance of Certification (AAFP) – Physician Quality Reporting Initiative (CMS) – Private / Public Payors – Internal Quality Improvement Efforts
Quality Improvement Worksheet (Diabetes) • Goal: • The purpose of this assignment is to become familiar with the general approach of chart review as a fundamental step toward quality improvement. • Instructions: • Identify a patient with diabetes and perform a chart review. • Complete the Diabetes Quality Improvement Worksheet while you are doing the chart review.
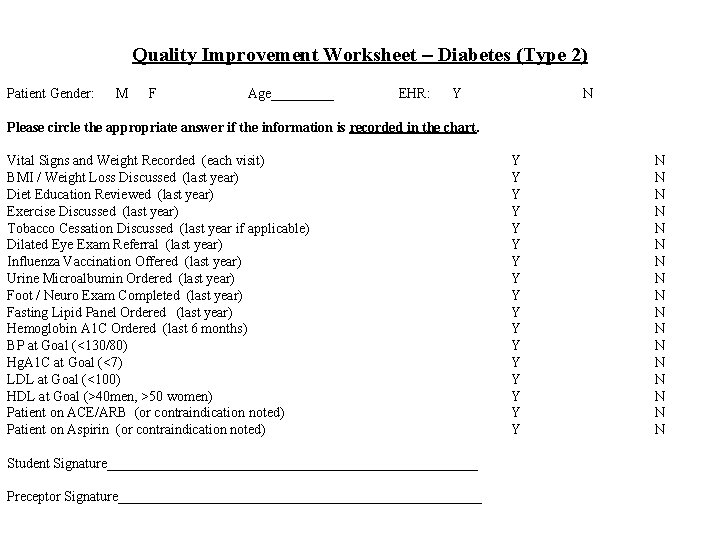
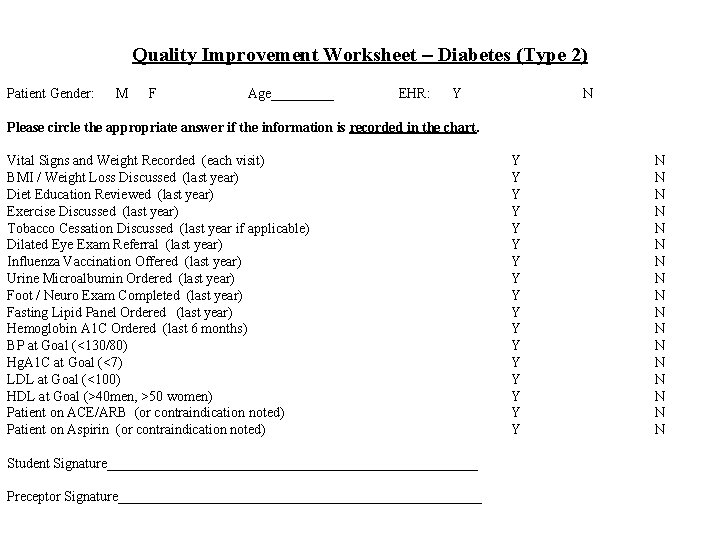
Quality Improvement Worksheet – Diabetes (Type 2) Patient Gender: M F Age_____ EHR: Y N Please circle the appropriate answer if the information is recorded in the chart. Vital Signs and Weight Recorded (each visit) BMI / Weight Loss Discussed (last year) Diet Education Reviewed (last year) Exercise Discussed (last year) Tobacco Cessation Discussed (last year if applicable) Dilated Eye Exam Referral (last year) Influenza Vaccination Offered (last year) Urine Microalbumin Ordered (last year) Foot / Neuro Exam Completed (last year) Fasting Lipid Panel Ordered (last year) Hemoglobin A 1 C Ordered (last 6 months) BP at Goal (<130/80) Hg. A 1 C at Goal (<7) LDL at Goal (<100) HDL at Goal (>40 men, >50 women) Patient on ACE/ARB (or contraindication noted) Patient on Aspirin (or contraindication noted) Student Signature___________________________ Preceptor Signature__________________________ Y Y Y Y Y N N N N N
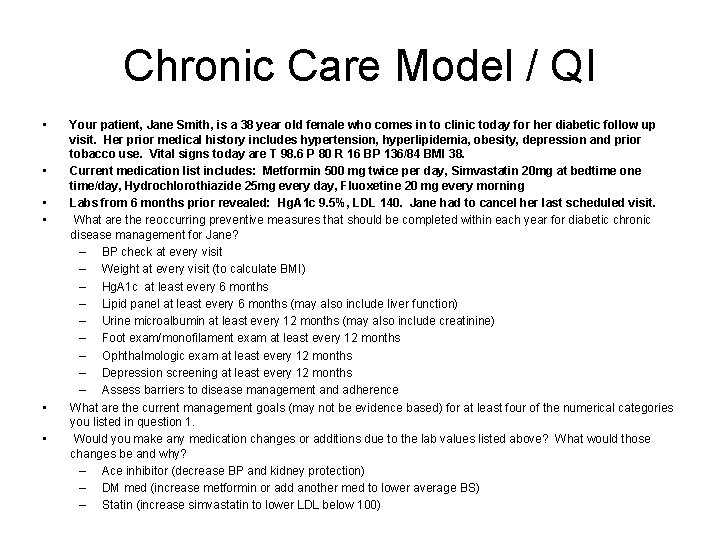
Chronic Care Model / QI • • • Your patient, Jane Smith, is a 38 year old female who comes in to clinic today for her diabetic follow up visit. Her prior medical history includes hypertension, hyperlipidemia, obesity, depression and prior tobacco use. Vital signs today are T 98. 6 P 80 R 16 BP 136/84 BMI 38. Current medication list includes: Metformin 500 mg twice per day, Simvastatin 20 mg at bedtime one time/day, Hydrochlorothiazide 25 mg every day, Fluoxetine 20 mg every morning Labs from 6 months prior revealed: Hg. A 1 c 9. 5%, LDL 140. Jane had to cancel her last scheduled visit. What are the reoccurring preventive measures that should be completed within each year for diabetic chronic disease management for Jane? – BP check at every visit – Weight at every visit (to calculate BMI) – Hg. A 1 c at least every 6 months – Lipid panel at least every 6 months (may also include liver function) – Urine microalbumin at least every 12 months (may also include creatinine) – Foot exam/monofilament exam at least every 12 months – Ophthalmologic exam at least every 12 months – Depression screening at least every 12 months – Assess barriers to disease management and adherence What are the current management goals (may not be evidence based) for at least four of the numerical categories you listed in question 1. Would you make any medication changes or additions due to the lab values listed above? What would those changes be and why? – Ace inhibitor (decrease BP and kidney protection) – DM med (increase metformin or add another med to lower average BS) – Statin (increase simvastatin to lower LDL below 100)
Evidence-Based Medicine • Primary Articles – Literature Search (Pub. Med) – Critical Appraisal • http: //www. fmdrl. org/ • Search – Lausen • The PCMH: Lessons Learned From A New Family Medicine Clerkship Curriculum • Select EBM Critical Appraisal of Lit. pdf • Clinical Decision Support – Point of Care Resources – “Quick & Dirty”
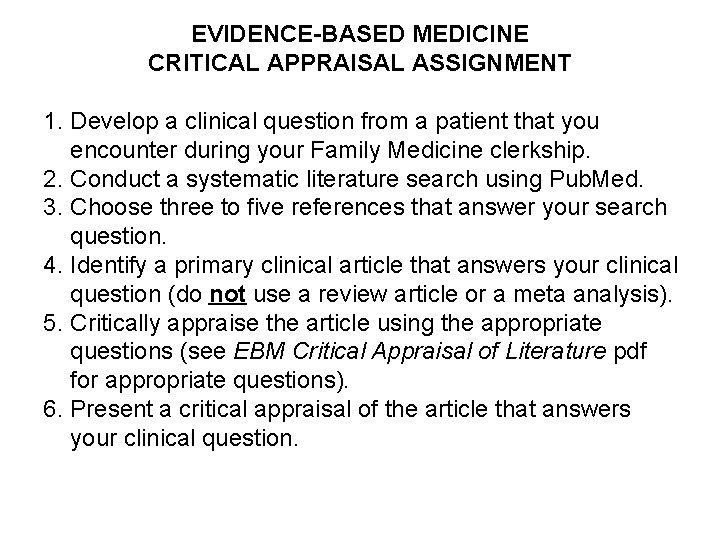
EVIDENCE-BASED MEDICINE CRITICAL APPRAISAL ASSIGNMENT 1. Develop a clinical question from a patient that you encounter during your Family Medicine clerkship. 2. Conduct a systematic literature search using Pub. Med. 3. Choose three to five references that answer your search question. 4. Identify a primary clinical article that answers your clinical question (do not use a review article or a meta analysis). 5. Critically appraise the article using the appropriate questions (see EBM Critical Appraisal of Literature pdf for appropriate questions). 6. Present a critical appraisal of the article that answers your clinical question.
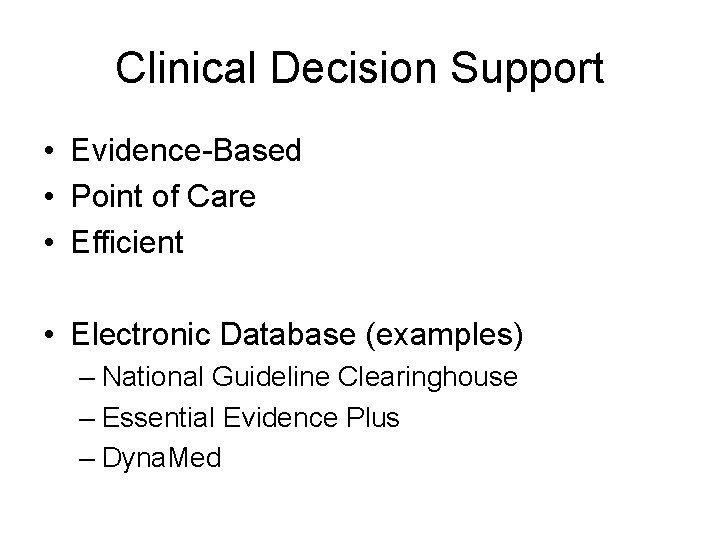
Clinical Decision Support • Evidence-Based • Point of Care • Efficient • Electronic Database (examples) – National Guideline Clearinghouse – Essential Evidence Plus – Dyna. Med
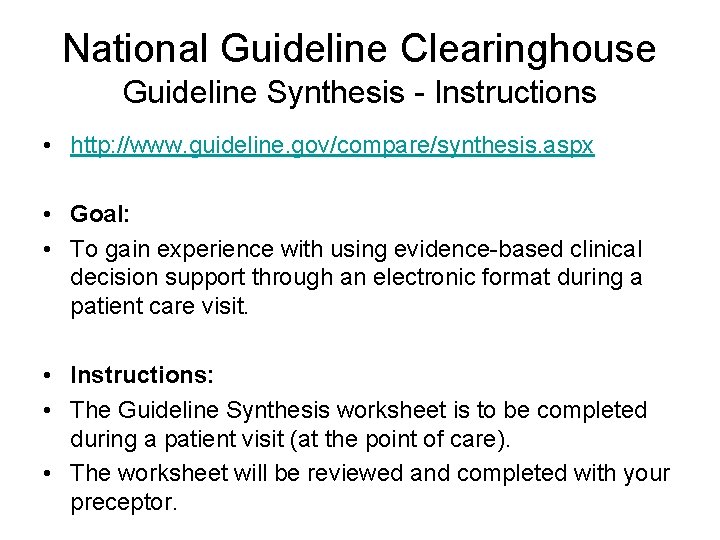
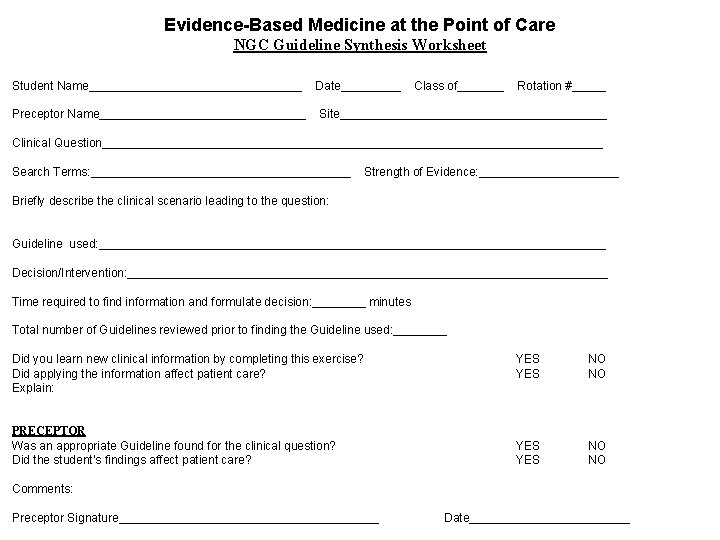
National Guideline Clearinghouse Guideline Synthesis - Instructions • http: //www. guideline. gov/compare/synthesis. aspx • Goal: • To gain experience with using evidence-based clinical decision support through an electronic format during a patient care visit. • Instructions: • The Guideline Synthesis worksheet is to be completed during a patient visit (at the point of care). • The worksheet will be reviewed and completed with your preceptor.
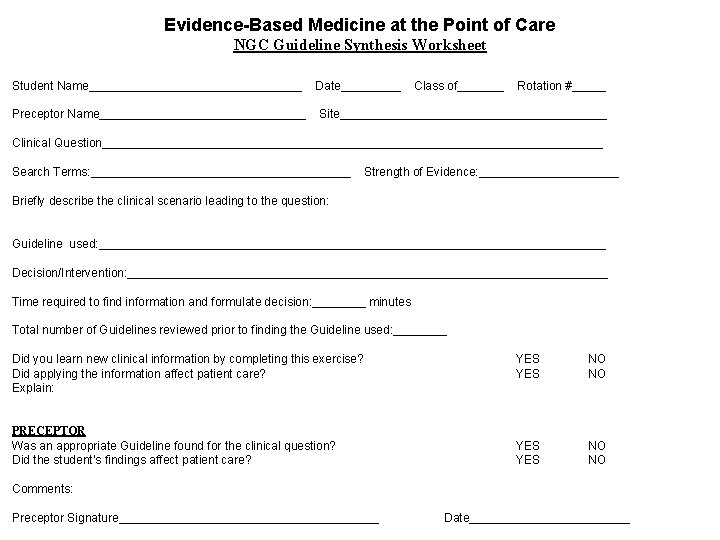
Evidence-Based Medicine at the Point of Care NGC Guideline Synthesis Worksheet Student Name________________ Preceptor Name________________ Date_____ Class of_______ Rotation #_____ Site____________________ Clinical Question______________________________________ Search Terms: ____________________ Strength of Evidence: ___________ Briefly describe the clinical scenario leading to the question: Guideline used: ______________________________________ Decision/Intervention: ____________________________________ Time required to find information and formulate decision: ____ minutes Total number of Guidelines reviewed prior to finding the Guideline used: ____ Did you learn new clinical information by completing this exercise? Did applying the information affect patient care? Explain: PRECEPTOR Was an appropriate Guideline found for the clinical question? Did the student’s findings affect patient care? YES YES NO NO Comments: Preceptor Signature____________________ Date____________
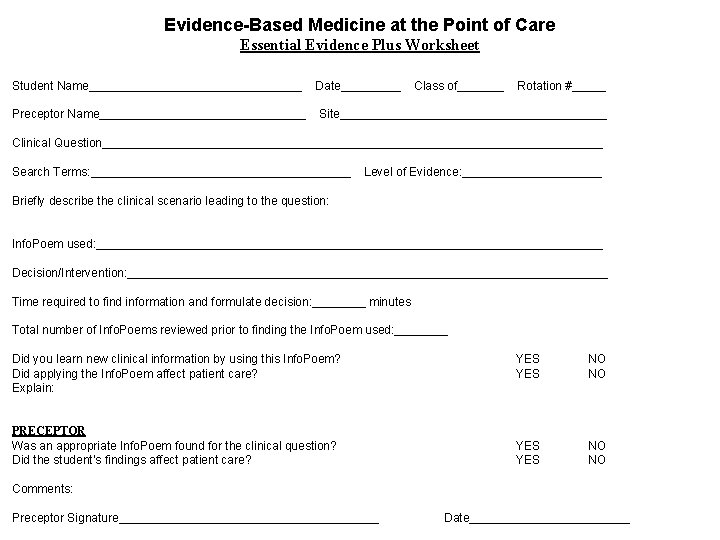
Essential Evidence Plus - Instructions • Goal: • To gain experience with using evidence-based clinical decision support through an electronic format during a patient care visit. • Instructions: • The Essential Evidence Plus worksheet is to be completed during a patient visit (at the point of care). • The worksheet will be reviewed and completed with your preceptor.
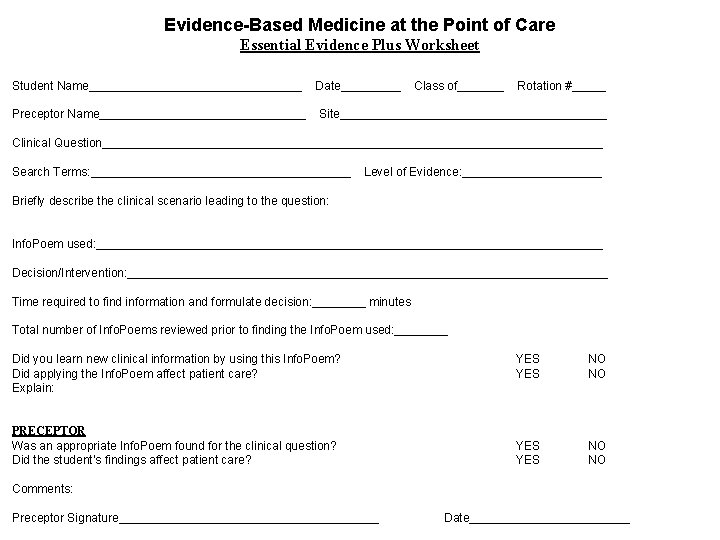
Evidence-Based Medicine at the Point of Care Essential Evidence Plus Worksheet Student Name________________ Preceptor Name________________ Date_____ Class of_______ Rotation #_____ Site____________________ Clinical Question______________________________________ Search Terms: ____________________ Level of Evidence: ___________ Briefly describe the clinical scenario leading to the question: Info. Poem used: ______________________________________ Decision/Intervention: ____________________________________ Time required to find information and formulate decision: ____ minutes Total number of Info. Poems reviewed prior to finding the Info. Poem used: ____ Did you learn new clinical information by using this Info. Poem? Did applying the Info. Poem affect patient care? Explain: PRECEPTOR Was an appropriate Info. Poem found for the clinical question? Did the student’s findings affect patient care? YES YES NO NO Comments: Preceptor Signature____________________ Date____________
Comments / Questions
Thank You! Harald Lausen, DO hlausen@siumed. edu
 Heucherella twilight
Heucherella twilight Obgyn pearls
Obgyn pearls Plastic packing pearls
Plastic packing pearls Analisa pearls
Analisa pearls Pearls of sicily lido di noto
Pearls of sicily lido di noto Mel.np
Mel.np Inrs
Inrs Taj mahal rabindranath tagore
Taj mahal rabindranath tagore Analisis pearls
Analisis pearls Trivselsvægt
Trivselsvægt Pharmacy clinical pearls
Pharmacy clinical pearls Stat pearls impact factor
Stat pearls impact factor The pearl symbols
The pearl symbols Natural pearls are found in which creature
Natural pearls are found in which creature Riddles on spices in english
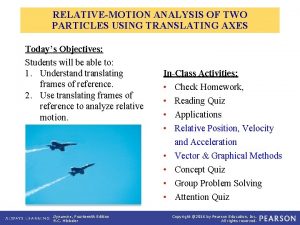
Riddles on spices in english Relative motion of two particles using translating axes
Relative motion of two particles using translating axes Translating phrases
Translating phrases Translating a sentence into a one step equation
Translating a sentence into a one step equation Translating quadratic functions
Translating quadratic functions Compound word waterfall
Compound word waterfall Translating graphs worksheet
Translating graphs worksheet Translating expressions and equations
Translating expressions and equations Translating between tables and expressions
Translating between tables and expressions The gym is 21 years newer than the auditorium
The gym is 21 years newer than the auditorium Translating quadratic functions
Translating quadratic functions Two less than a number
Two less than a number Translating chemical equations
Translating chemical equations Transformations of exponential functions
Transformations of exponential functions 1-5 translating sentences into equations answer key
1-5 translating sentences into equations answer key Translating linear inequalities
Translating linear inequalities Translating contracts
Translating contracts On the different methods of translating
On the different methods of translating Translating english into logical expressions
Translating english into logical expressions Sentence reverser
Sentence reverser Transformation of quadratic functions
Transformation of quadratic functions Translating conic sections
Translating conic sections Translating research findings to clinical nursing practice
Translating research findings to clinical nursing practice Horizontal stretch example
Horizontal stretch example Translate algebraic expressions
Translate algebraic expressions Cam definition
Cam definition How do thrust reversers work
How do thrust reversers work Translating verbal expressions
Translating verbal expressions Translating strategy into action
Translating strategy into action Translating ore polygons
Translating ore polygons Translation of financial statements
Translation of financial statements Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên 101012 bằng
101012 bằng Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con đại từ thay thế
đại từ thay thế Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công của trọng lực
Công của trọng lực Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi điện thế nghỉ
điện thế nghỉ Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Gấu đi như thế nào
Gấu đi như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Phối cảnh
Phối cảnh Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Ng-html
Ng-html Sơ đồ cơ thể người
Sơ đồ cơ thể người Số nguyên tố là gì
Số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Tư thế worm breton
Tư thế worm breton ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Geography: realms, regions, and concepts (doc or html) file
Geography: realms, regions, and concepts (doc or html) file Graph basic concepts
Graph basic concepts ñ
ñ Reviewing key concepts reproductive barriers
Reviewing key concepts reproductive barriers Chapter 7 motivation concepts
Chapter 7 motivation concepts Basic marketing concepts
Basic marketing concepts Origin of concepts
Origin of concepts Construction management concepts
Construction management concepts