Pancreatitis PANCREATITIS Pancreatitis is an inflammation of the

















- Slides: 53
Pancreatitis
PANCREATITIS • Pancreatitis is an inflammation of the pancreas. • The pancreas secretes digestive enzymes into the small intestine through a tube called the pancreatic duct. • These enzymes help digest fats, proteins, and carbohydrates in food. • The pancreas also releases the hormones insulin and glucagon into the bloodstream. These hormones help the body use the glucose it takes from food for energy. Normally, digestive enzymes do not become active until they reach the small intestine, where they begin digesting food. But in pancreatitis these enzymes become active inside the pancreas, &start "digesting" the pancreas itself.


Pancreatitis is classified as: § Acute pancreatitis § Chronic pancreatitis
Acute pancreatitis: is a condition that develops when the pancreas is damaged by an inflammation that leads to swelling and sometimes to Necrosis of parts of the pancreas. In about 85% of patients, acute pancreatitis is mild disease and is associated with a rapid recovery within a few days of onset of the illness In about 15 -20% of patients, acute pancreatitis can lead to severe damage of the pancreas associated with the developments of pancreatic necrosis. Patients with severe acute pancreatitis are at the risk of developing following complications: § Failure of multiple body organ systems such as heart, lungs, liver and kidney. § Pancreatitis necrosis( part of pancreas becomes dead) § Infected pancreatic necrosis( infection of the dead pancreas) § Pancreatic abscess § Pseudocyts § Pancreatic fistula
Chronic pancreatitis: is a condition associated with widespread scarring and destruction of pancreatic tissue. The condition is most frequently associated with alcohol abuse and excessive smoking. Chronic pancreatitis is a slowly progressive disease that takes many years to develop. Patients with severe chronic pancreatitis are at the risk of developing following complications: • • Severe chronic pain Diabetes mellitus Poor absorption of nutrients from the digestive tract especially fats Cancer of pancreas Blockage of bile ducts Pseudocysts Bleeding from the stomach
Causes of pancreatitis are: • • Alcohol Gallstone Medications, Hereditary disease, Exposure to certain chemicals High fat levels in the blood. Infections such as mumps (not common), Surgery and other medical procedures, Trauma, • Abnormalities of the pancreas or intestine • Auto digestion Other factors that lead to pancreatitis are: • • Structural abnormalities of the pancreas Viral infections like hepatitis Pancreatic cancer, which can obstruct the flow of pancreatic enzymes Inherited diseases, especially cystic fibrosis
Signs and symptoms of Pancreatitis § Acute pancreatitis occurs abruptly, generally with gentle to harsh pain in your upper abdomen that may spread out to your back and rarely to your chest. The pain may become worse when you have alcohol. Other signs and symptoms of acute pancreatitis are: § Swollen, tender abdomen § Rapid pulse § Fever § Nausea and vomiting § Dehydration and low blood pressure, internal bleeding, and shock

DIAGNOSIS Diagnosing acute pancreatitis is often difficult because of the deep location of the pancreas. The doctor will likely order one or more of the following tests: • Abdominal ultrasound • Computerized tomography (CT) scan. • Endoscopic ultrasound (EUS). • Magnetic resonance cholangiopancreatography (MRCP).
Treatment of Acute Pancreatitis • Treatment depends on the severity of the attack. If no kidney or lung complications occur, acute pancreatitis usually improves on its own. • A hospital stay will be necessary so that fluids can be replaced intravenously. • Unless the pancreatic duct or bile duct is blocked by gallstones, an acute attack usually lasts only a few days. • Medication for pain and nausea are provided to ease these symptoms and food is withheld until these symptoms have subsided considerably. • Antibiotics are often prescribed in cases of severe acute pancreatitis or if infection occurs.
If pancreatic necrosis occur and are considered large enough to interfere with the pancreas's healing, your doctor may drain or surgically remove them.
What is pancreatic necrosis? • Severe pancreatitis causes death of parts of the pancreas. • The injured and dying pancreas releases digestive enzymes in the pancreas, which causes extensive death of fatty tissue in the abdomen. • This dead pancreas tissue is called pancreatic necrosis and the dead fat around the pancreas is called peripancreatic necrosis.
Types of necrosis • When the dead pancreas is not infected, it is called sterile necrosis. • When the dead pancreas is infected then it is called infected necrosis.
• Surgery in patients with sterile necrosis is conducted when patients condition appears not be improving and or continue to deteriorate due to infection of necrotic cells. • Surgery is done usually after two weeks, as by the time the dead pancreatic tissue is demarcated (separated) from the live tissue and can be easily removed.
Surgery for acute pancreatitis • The surgery that is performed remove all the dead pancreas is called Debridement of pancreatic necrosis. The term debridement means removal of all dead or necrotic tissue. • In this surgery all dead or necrotic pancreas and any dead tissue outside of the pancreas is removed. • The CT scan is very useful for planning surgery and all areas identified on CT scan of having necrotic or dead tissue are opened up and the dead areas are removed.
LONG TERM OUTCOME AFTER SURGICAL TREATMENT FOR PANCREATIC NECROSIS Many patients often require multiple surgeries to remove all the necrotic tissue. Patients often remain critically ill for a long period after their surgery until the infection subsides. The long-term complications after surgical treatment of acute pancreatitis are : • Pancreatic Fistula: • Pancreatic Pseudo cyst • Diabetes: • Chronic Pancreatitis
Nutritional Management Nutrition prior to surgery • Good nutrition prior to surgery ensures fewer post operative complications, better wound healing, short convalescence and lower mortality. • Patients who have lost much weight prior to surgery benefit considerably by ingesting a high calorie, high protein diet for even a week or two prior to surgery. • Foods which provide a maximum amount of nutrients in a minimum volume are essential • Foods and fluids are generally allowed until midnight just proceeding the day of operation.
It is essential that the stomach is empty prior to administering the anesthesia so as to reduce the incidence of vomiting. The patient should not be operated in a state of dehydration, since the dangers of acidosis are great, parenteral fluids must be administered if the patient is unable to ingest sufficient liquid by mouth.
Nutritional management after surgery • The need for nutrients is greatly increased as a result of loss of blood , plasma or pus from the wound surface , hemorrhage from the gastrointestinal tract , vomiting and fever. • High calorie , high protein , low fat and high carbohydrate diet should be the goal.

ENERGY • Calorie requirement must be increased to restore weight status & maintain ideal weight. • An intake of 40 -50 K Cal/KG body weight is recommended if the patient is underweight. • Calories should be increased gradually to avoid digestive disturbances
PROTEIN – A satisfactory state of protein nutrition ensures: • A rapid wound healing. • Increases the resistance to infection. • Exerts a protective action upon the liver against the toxic effects of anesthesia. • Reduces possibility of oedema at the site of wound. • Intake of 1. 5 – 2. 5 gm/ kg body weight or about 100 gm of protein is necessary as a rule.

• FAT – About 20% of calories should be from fat. MCT are preferred as they are easily digested • Usual foods which contain fat are permitted but not fried foods. As they may cause nausea & feeling of satiety. • Intake of 20 gm visible fat is recommended. Intake can exceed the requirement as per tolerance.
CARBOHYDRATES • 50 -60% of energy should come from carbohydrates. • Carbohydratess are Easily absorbable source of energy. • Sugars & Starches can make the increased calorie intake. VITAMINS • Needed for healing process & utilization of proteins & calories. • Ascorbic acid is important for wound healing & should be provided in increased amounts. • Vitamin “K” must be incorporated in diet to avoid bleeding.
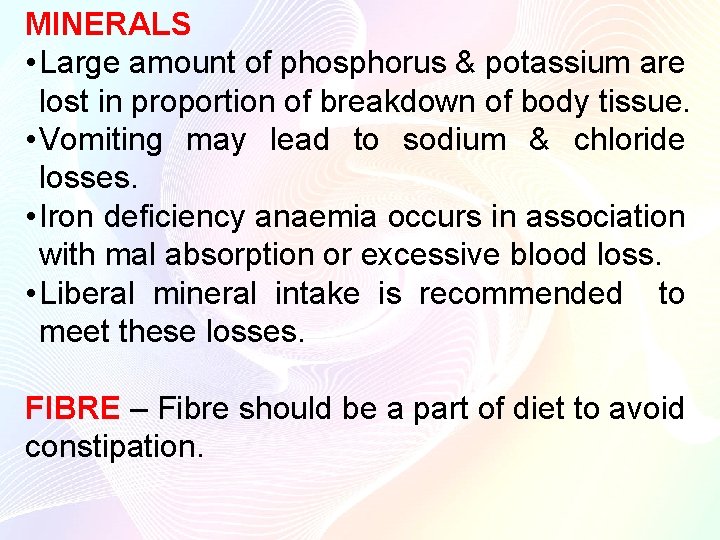
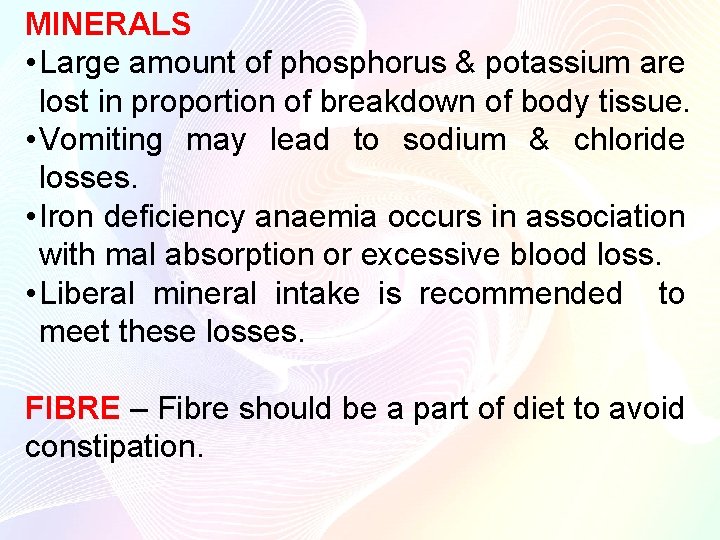
MINERALS • Large amount of phosphorus & potassium are lost in proportion of breakdown of body tissue. • Vomiting may lead to sodium & chloride losses. • Iron deficiency anaemia occurs in association with mal absorption or excessive blood loss. • Liberal mineral intake is recommended to meet these losses. FIBRE – Fibre should be a part of diet to avoid constipation.







10 gm albumin care provides Energy- 29. 4 kcal and Protein-6. 5 gm
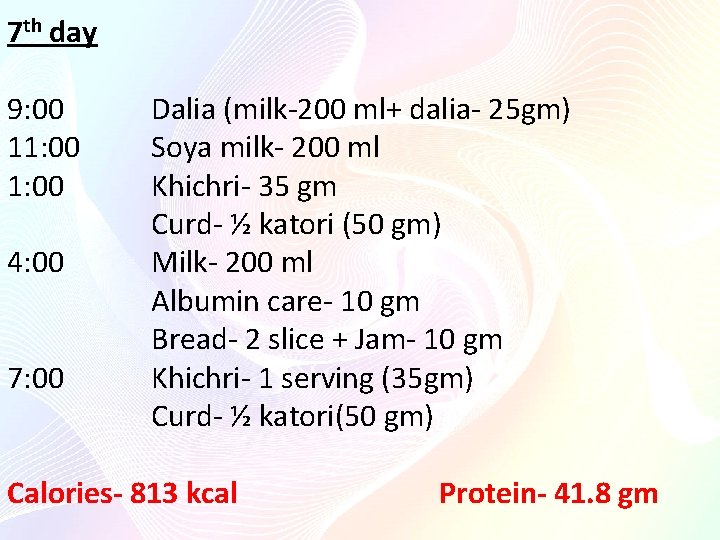
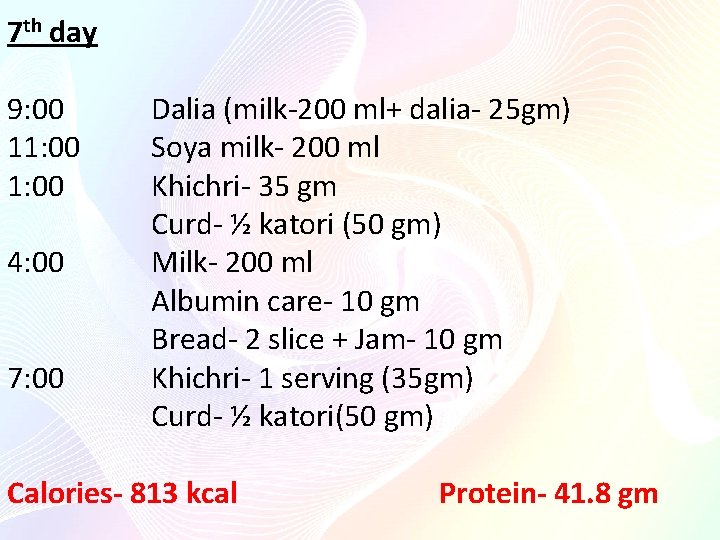
7 th day 9: 00 Dalia (milk-200 ml+ dalia- 25 gm) 11: 00 Soya milk- 200 ml 1: 00 Khichri- 35 gm Curd- ½ katori (50 gm) 4: 00 Milk- 200 ml Albumin care- 10 gm Bread- 2 slice + Jam- 10 gm 7: 00 Khichri- 1 serving (35 gm) Curd- ½ katori(50 gm) Calories- 813 kcal Protein- 41. 8 gm
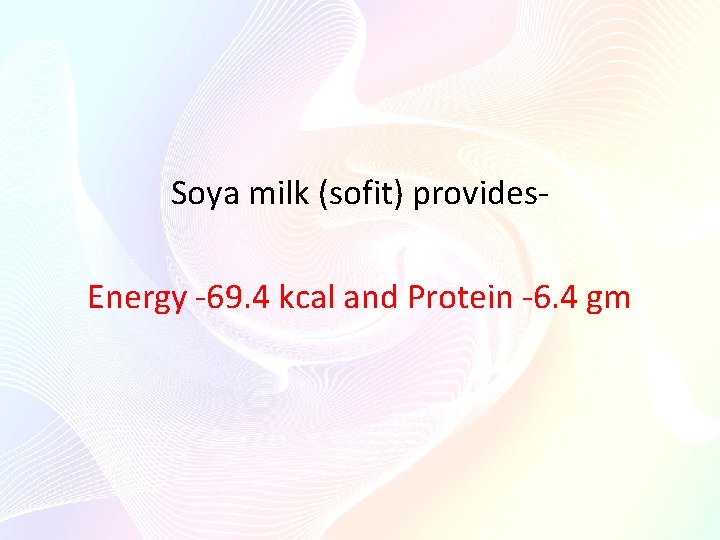
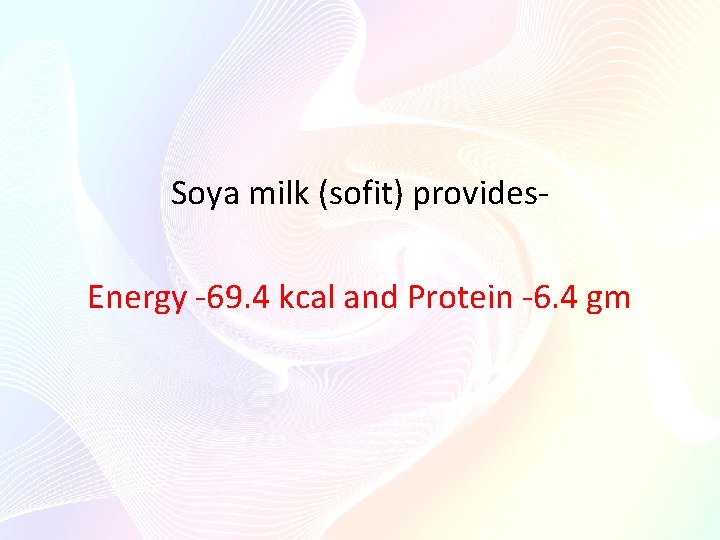
Soya milk (sofit) provides- Energy -69. 4 kcal and Protein -6. 4 gm
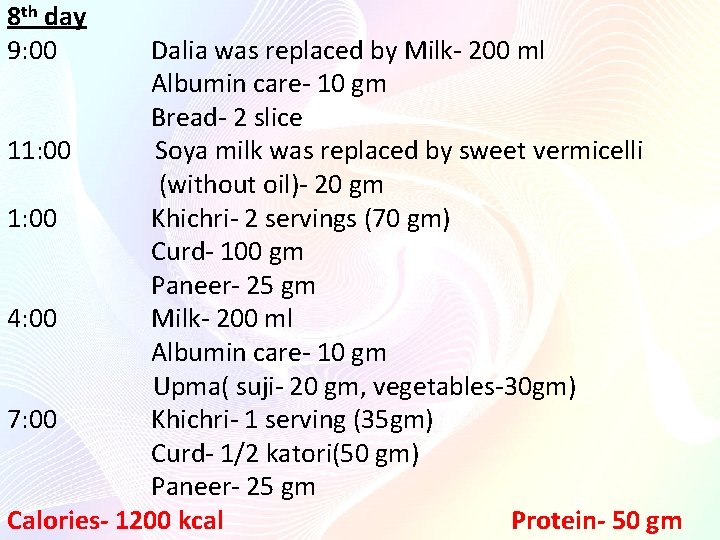
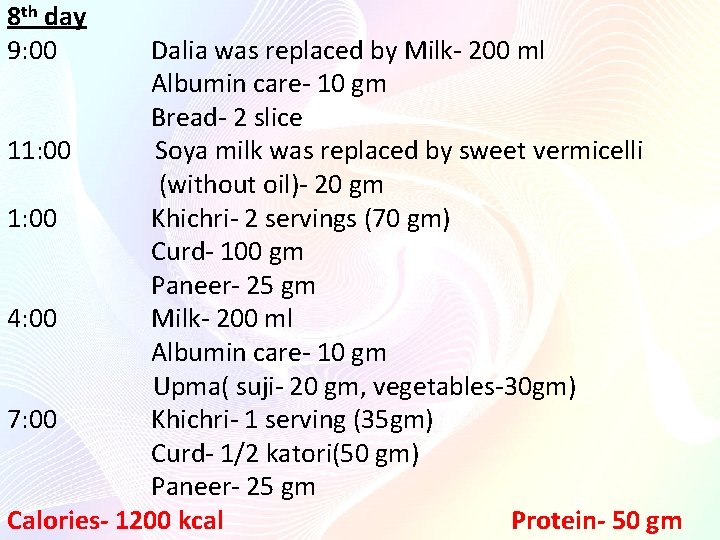
8 th day 9: 00 Dalia was replaced by Milk- 200 ml Albumin care- 10 gm Bread- 2 slice 11: 00 Soya milk was replaced by sweet vermicelli (without oil)- 20 gm 1: 00 Khichri- 2 servings (70 gm) Curd- 100 gm Paneer- 25 gm 4: 00 Milk- 200 ml Albumin care- 10 gm Upma( suji- 20 gm, vegetables-30 gm) 7: 00 Khichri- 1 serving (35 gm) Curd- 1/2 katori(50 gm) Paneer- 25 gm Calories- 1200 kcal Protein- 50 gm

Sweet vermicilli provides Energy -150 kcal and Protein-1. 6 gm Upma provides Energy -81. 5 kcal and Protein-3. 8 gm
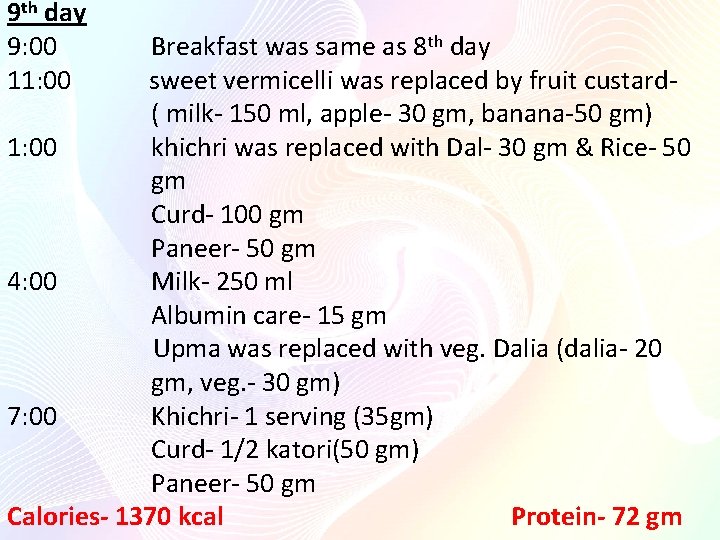
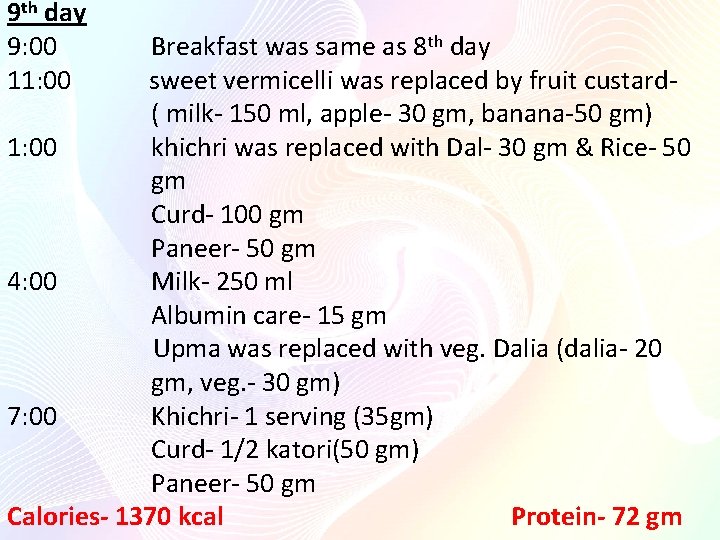
9 th day 9: 00 Breakfast was same as 8 th day 11: 00 sweet vermicelli was replaced by fruit custard- ( milk- 150 ml, apple- 30 gm, banana-50 gm) 1: 00 khichri was replaced with Dal- 30 gm & Rice- 50 gm Curd- 100 gm Paneer- 50 gm 4: 00 Milk- 250 ml Albumin care- 15 gm Upma was replaced with veg. Dalia (dalia- 20 gm, veg. - 30 gm) 7: 00 Khichri- 1 serving (35 gm) Curd- 1/2 katori(50 gm) Paneer- 50 gm Calories- 1370 kcal Protein- 72 gm

Fruit custard provides Energy- 230 kcal and protein- 5. 8 gm Veg. Dalia provides Energy- 80 kcal and protein- 3. 6 gm
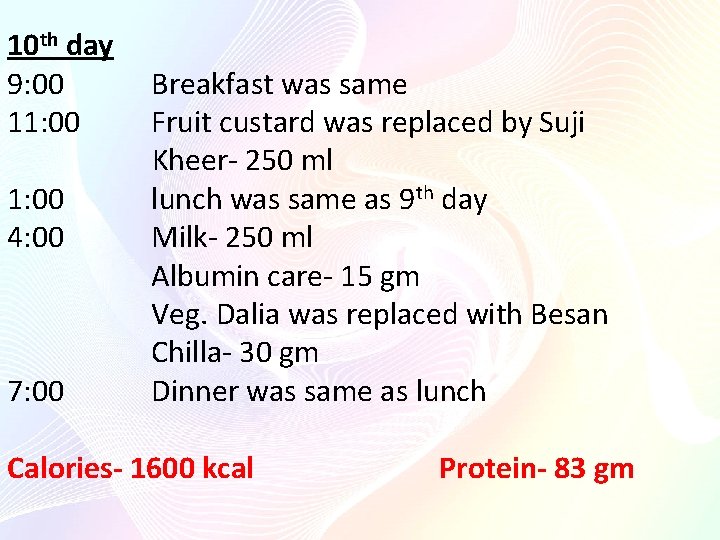
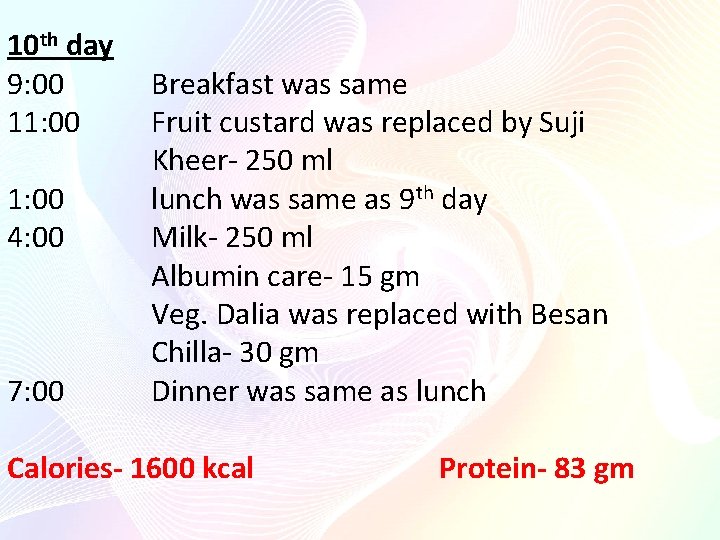
10 th day 9: 00 Breakfast was same 11: 00 Fruit custard was replaced by Suji Kheer- 250 ml 1: 00 lunch was same as 9 th day 4: 00 Milk- 250 ml Albumin care- 15 gm Veg. Dalia was replaced with Besan Chilla- 30 gm 7: 00 Dinner was same as lunch Calories- 1600 kcal Protein- 83 gm

Suji kheer provides Energy- 237 kcal and Protein- 9. 8 Besan Chilla provides Energy-165. 5 kcal and protein- 7. 1
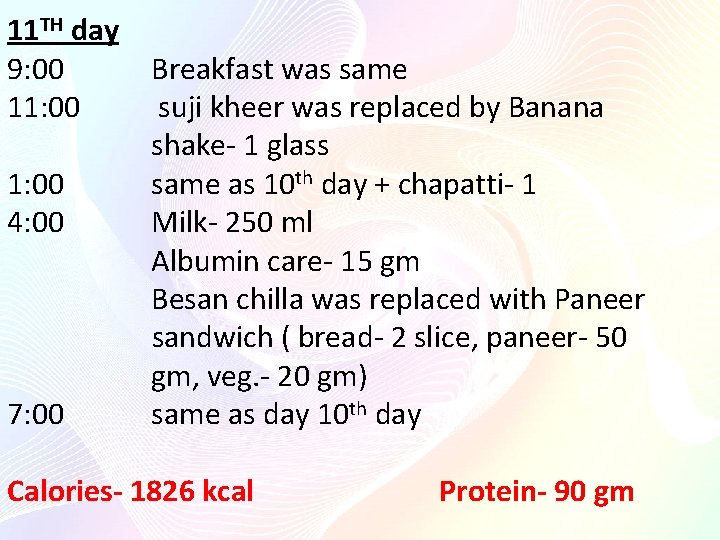
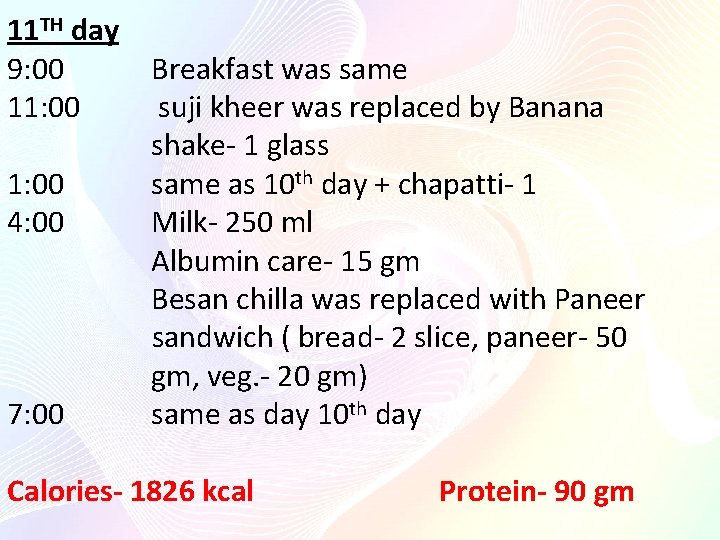
11 TH day 9: 00 11: 00 Breakfast was same suji kheer was replaced by Banana shake- 1 glass 1: 00 same as 10 th day + chapatti- 1 4: 00 Milk- 250 ml Albumin care- 15 gm Besan chilla was replaced with Paneer sandwich ( bread- 2 slice, paneer- 50 gm, veg. - 20 gm) 7: 00 same as day 10 th day Calories- 1826 kcal Protein- 90 gm
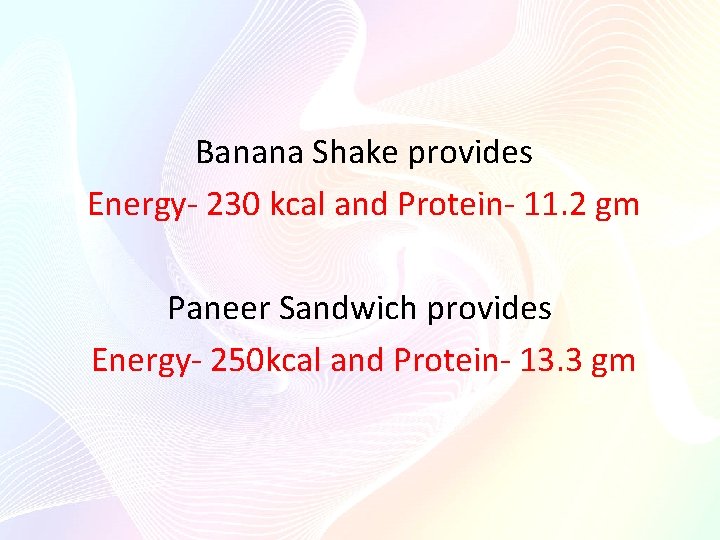
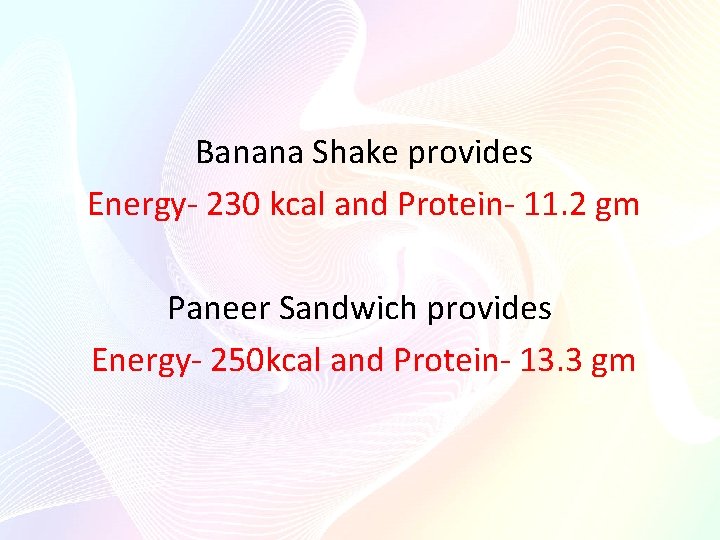
Banana Shake provides Energy- 230 kcal and Protein- 11. 2 gm Paneer Sandwich provides Energy- 250 kcal and Protein- 13. 3 gm

12 th day 9: 00 Breakfast was same 11: 00 Banana shake was replaced with H. P Feed 1: 00 same as 11 th day + chapatti- 2 4: 00 Milk- 250 ml Albumin care- 15 gm Paneer sandwich was replaced with veg. omelet ( eggs- 2, veg. - 30 gm) 7: 00 same as day 10 + 1 chapatti Calories- 1950 kcal Protein-102 gm
High protein feed provides Energy- 240 kcal and protein- 11 gm Veg. omelet provides Energy- 251 kcal and Protein- 13. 5
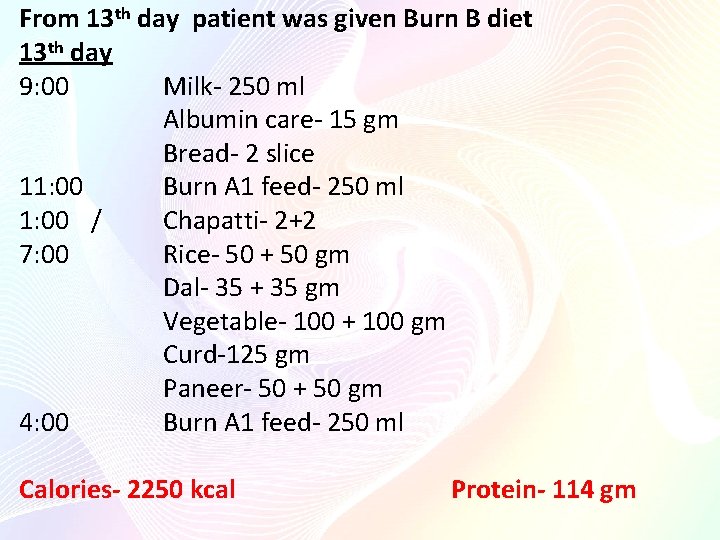
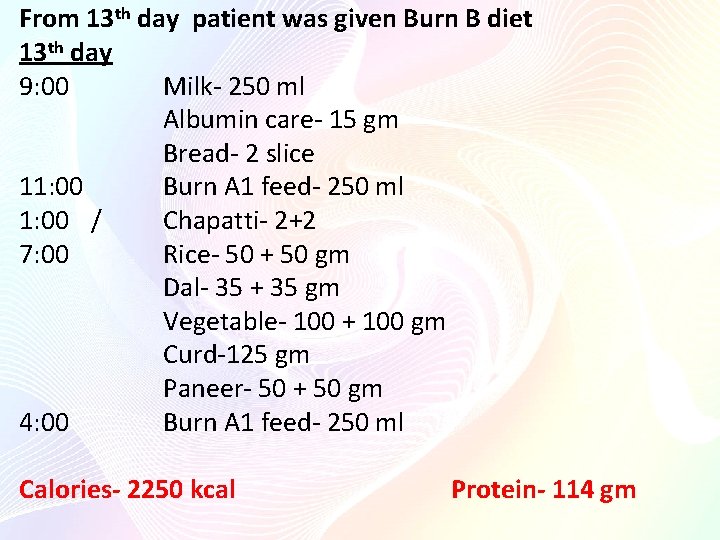
From 13 th day patient was given Burn B diet 13 th day 9: 00 Milk- 250 ml Albumin care- 15 gm Bread- 2 slice 11: 00 Burn A 1 feed- 250 ml 1: 00 / Chapatti- 2+2 7: 00 Rice- 50 + 50 gm Dal- 35 + 35 gm Vegetable- 100 + 100 gm Curd-125 gm Paneer- 50 + 50 gm 4: 00 Burn A 1 feed- 250 ml Calories- 2250 kcal Protein- 114 gm
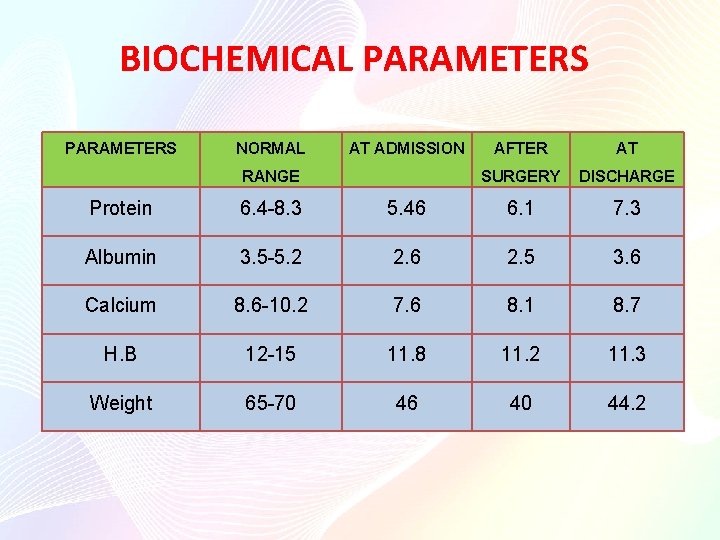
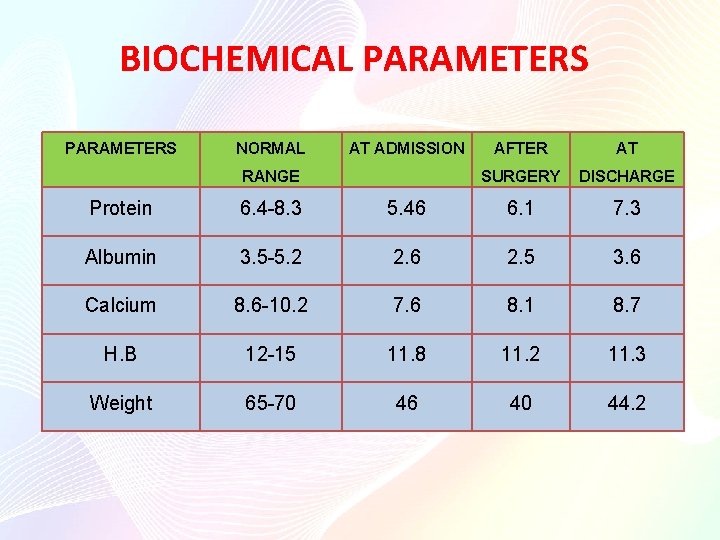
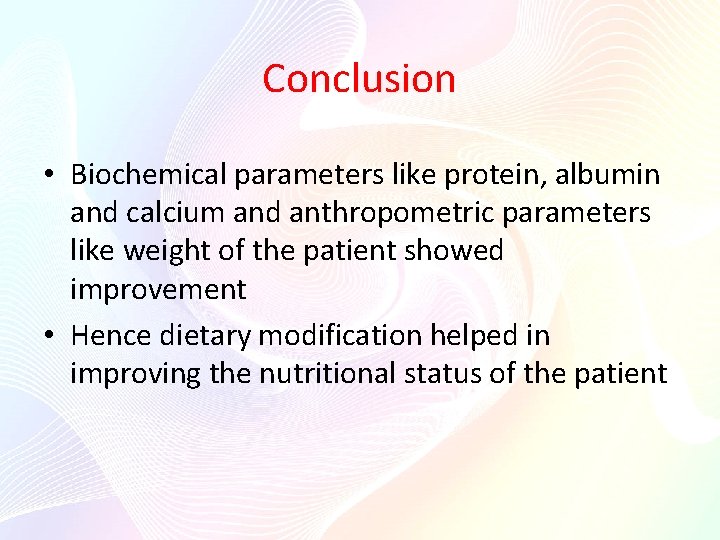
BIOCHEMICAL PARAMETERS NORMAL AT ADMISSION RANGE AFTER AT SURGERY DISCHARGE Protein 6. 4 -8. 3 5. 46 6. 1 7. 3 Albumin 3. 5 -5. 2 2. 6 2. 5 3. 6 Calcium 8. 6 -10. 2 7. 6 8. 1 8. 7 H. B 12 -15 11. 8 11. 2 11. 3 Weight 65 -70 46 40 44. 2
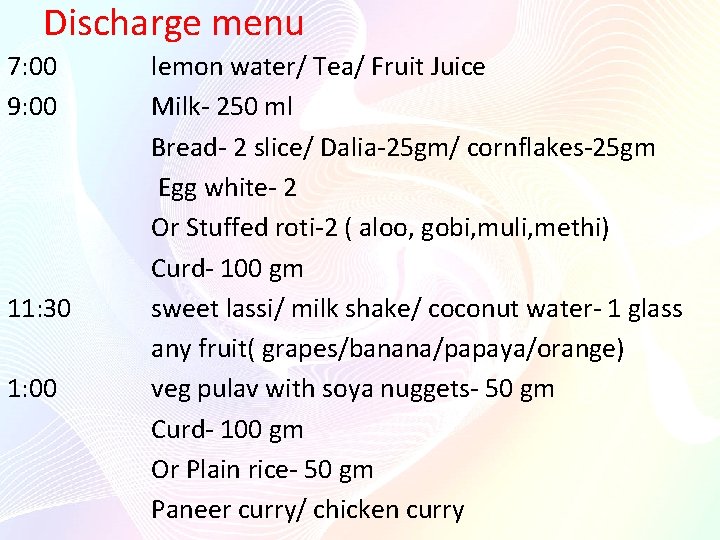
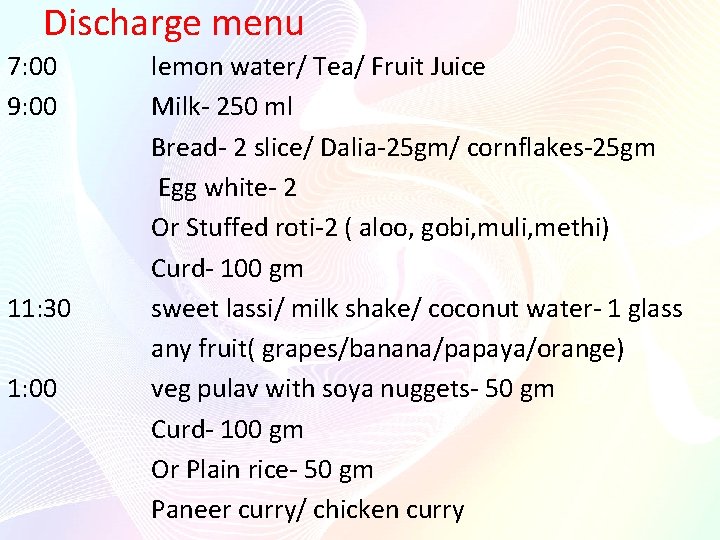
Discharge menu 7: 00 9: 00 11: 30 1: 00 lemon water/ Tea/ Fruit Juice Milk- 250 ml Bread- 2 slice/ Dalia-25 gm/ cornflakes-25 gm Egg white- 2 Or Stuffed roti-2 ( aloo, gobi, muli, methi) Curd- 100 gm sweet lassi/ milk shake/ coconut water- 1 glass any fruit( grapes/banana/papaya/orange) veg pulav with soya nuggets- 50 gm Curd- 100 gm Or Plain rice- 50 gm Paneer curry/ chicken curry
4: 00 7: 30 Milk/Tea/ Fruit juice Rusk-2/ poha-30 gm/veg dalia 30 gm/ Besan chilla- 30 gm/ omlete/ veg sandwich veg. soup- 1 bowl Chapatti- 3 Seasonal veg. - 150 gm Curd/ dal- 100 gm/ 35 gm Calories-2200 kcal Proteins- 75 gm
Do’s and Don’t, s • Quit alcohol and nicotine. This is because they stimulate the pancreas to a great extent. Stop smoking and chewing tobacco also. • Maintain a low fat diet consisting of 15% fat. • Try to eat food that is high in carbohydrates and proteins as they reduce the work pressure of your pancreas. • Stop eating rich and spicy food to reduce the chance of another attack Don’t try to eat large meals at a time. Rather go for small frequent meals. • Avoid concentrated sweets and desserts that are very sweet if your blood glucose level is high or above normal. • Caffeine and gas-forming food items stimulate pancreas. So avoid these type of food. • Margarine, butter etc. , should also be avoided • Quit red meat. Rather go for chicken. • You can include soybeans in your diet as they are very good anti-oxidants. • You can eat light chicken soups or vegetable soups frequently. • Green leafy vegetables are also very good for pancretitis. • Keep some fruit juice with you and whenever you are tempted to have alcohol, sip it. • Drink plenty of fluids in the form of soups and juices.
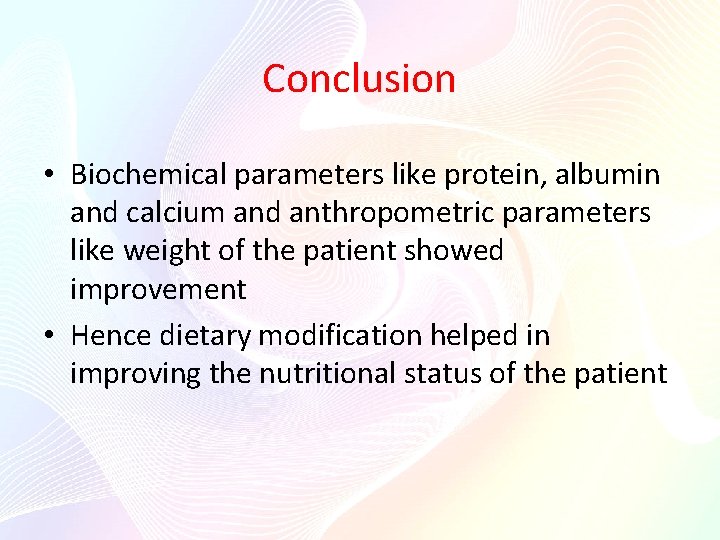
Conclusion • Biochemical parameters like protein, albumin and calcium and anthropometric parameters like weight of the patient showed improvement • Hence dietary modification helped in improving the nutritional status of the patient

References • • • Krause Food nutrition and diet therapy Clinical nutrition and dietetics by Antia Dietetics by B. Srilakshmi www. Wikipedia. com www. zadehsurgical. com www. surgery. usg. com
Thank you.
Pancreatitis
 Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Tư thế ngồi viết
Tư thế ngồi viết Thế nào là giọng cùng tên
Thế nào là giọng cùng tên Chó sói
Chó sói Thể thơ truyền thống
Thể thơ truyền thống Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu đại từ thay thế
đại từ thay thế Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Lp html
Lp html Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tư thế worm breton
Tư thế worm breton Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu điện thế nghỉ
điện thế nghỉ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Dot
Dot Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Bổ thể
Bổ thể Phép trừ bù
Phép trừ bù Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Hát lên người ơi alleluia
Hát lên người ơi alleluia Fecboak
Fecboak Một số thể thơ truyền thống
Một số thể thơ truyền thống Hệ hô hấp
Hệ hô hấp Tư thế ngồi viết
Tư thế ngồi viết Công của trọng lực
Công của trọng lực Số.nguyên tố
Số.nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới độ dài liên kết
độ dài liên kết ưu thế lai là gì
ưu thế lai là gì Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thẻ vin
Thẻ vin Vascular response in acute inflammation
Vascular response in acute inflammation Dr el sabbagh
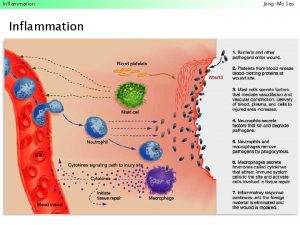
Dr el sabbagh Inflammation
Inflammation Radial articular surface
Radial articular surface Dlc blood smear
Dlc blood smear Cell injury and inflammation
Cell injury and inflammation Morphologic patterns of acute inflammation
Morphologic patterns of acute inflammation 5 cardinal signs of inflammation
5 cardinal signs of inflammation Middle meatus
Middle meatus Cardinal signs of inflammation
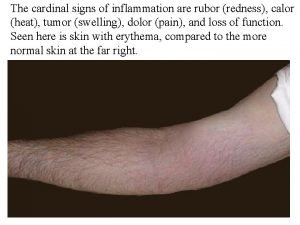
Cardinal signs of inflammation Morphological patterns of inflammation
Morphological patterns of inflammation Otitis media with effusion otoscopy
Otitis media with effusion otoscopy