Pancreas Acute pancreatitis The term pancreatitis implies the



































- Slides: 68

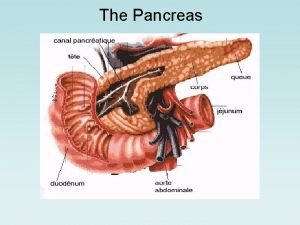
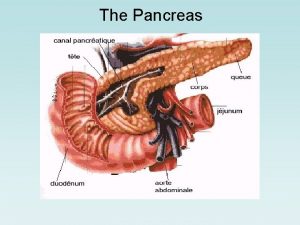
Pancreas






Acute pancreatitis The term pancreatitis implies the presence of pancreatic inflammation and autodigestion It is classified into n Acute (reversible no residue) form, which is either Acute pancreatitis Recurrent acute pancreatitis n Chronic (progressive damage) form, which is either Chronic pancreatitis Chronic relapsing pancreatitis
Acute pancreatitis Pathogenesis Common channel (biliary) Pan-obstruction &hyper-secretion (Alcohol) Back diffusion Duodenal reflux
Acute pancreatitis acute attack may ~>chronic pancreatitis if residual damage is left behind) Each acute attack is classified as n n n Edematous (completely reversible) Persistent (subsequent development of complications) Hemorrhagic (fatal)
Acute pancreatitis (Etiology) Idiopathic Obstruction n n Choledocolithiasis Ampullary or pancreatic tumors Pancreatic structural anomalies Toxins n n Alcohol Drugs - salicylates, azathioprine, cimetidine Trauma n n Accidental Iatrogenic Metabolic abnormalities (hypercalcemia) Infection Vascular anomalies
Acute pancreatitis (Etiology) From the practical point of view the two conditions most commonly associated with acute pancreatitis are Alcoholism (recurrent disease, the first attack is usually very severe getting less severe with recurrence and merging into chronic pancreatitis) Biliary tract stone disease (older than 60, tends to be severe, frequently accompanied with complications and recurrence is preventable).

Clinical picture (Symptoms) The cardinal symptom of acute pancreatitis is abdominal pain, n n n Most often, it is located in the upper abdomen, usually epigastric, but may be perceived more on the left or right side, depending on which portion of the pancreas is involved. which characteristically is dull, boring, and steady in quality. The pain radiates to the back in approximately one half of the cases. Associated symptoms such as anorexia, nausea, and vomiting are common, and some patients experience diarrhea
Clinical picture (Sings) The findings on physical examination that follow are variable, depending on the severity of the disease. General n Pulse------ Tachycardia are common abnormal vital sign. n Temp----- Fever are common abnormal vital sign. n Respiratory rate--- Few patients experience dyspnea (10%), which may be caused by irritation of the diaphragm, resulting from inflammation, or a more serious condition, such as respiratory distress syndrome. n BP------In severe cases, hemodynamic instability is evident (10%), n A minority of patients exhibits jaundice n Profound shock and cyanosis
Clinical picture (Sings) Local n n Abdominal tenderness, muscular guarding, and distension are observed in most patients. Bowel sounds often are hypoactive. Sometimes, hematemesis or melena develops (5%).
Clinical picture (Sings) A few local uncommon physical findings are associated with severe necrotizing pancreatitis. n n n The Cullen sign is a bluish discoloration around the umbilicus, resulting from hemoperitoneum. The Grey-Turner sign is a reddish-brown discoloration along the flanks, resulting from retroperitoneal blood dissecting along tissue planes. Erythematous skin nodules may result from focal subcutaneous fat necrosis
Diagnostic procedures Nonspecific investigations CBC n n increased hematocrit due to hemoconcentration Leucocytosis X ray chest n n n elevation of copulae, basal atalectasis, left sided or bilateral effusions ECG will show transient signs of ischemia
Diagnostic procedures Laboratory investigations Serum amylase (elevated for 3 days mainly) n n n Attain 5 times the normal or more If persistently elevated >10 days it means complication Other diseases can give elevations (acute cholecystitis, and perforated DU) Urine amylase Serum lipase Serum bilirubin Hyperglycemia and glucosuria Hypocalcemia (can cause tetany, is due to saponification of omentum) CBC Leucocytosis and anaemia Immunoreactive trypsin and elastase
Diagnostic procedures Radiological investigations Plain abdomen, standing n n Sentinel jujenal loop, or paralytic ileus Granular calcification of chronic pancratitis Radio-opaque gall stones Colon cut off sign Abdominal ultrasound n n This is the most useful initial test in determining the etiology of pancreatitis and is the technique of choice for detecting gallstones. In the setting of acute pancreatitis, sensitivity is reduced to 70 -80%. CT scan

Contrast-enhanced CT scoring system A-----Normal B-----Focal or diffuse glandular enlargement or small intra-pancreatic fluid collection C-----Peripancreatic inflammatory changes or less than 25% gland necrosis (concentration of contrast dye) D------Single extrapancreatic fluid collection, or 25 -50% gland necrosis, or extensive extrapancreatic fluid collection. E----Pancreatic abscess, or more than 50% gland necrosis
Other imaging techniques Endoscopic ultrasonography n Endoscopic ultrasonography (EUS) is an endoscopic procedure that allows a highfrequency ultrasound transducer to be inserted into the gastrointestinal tract to visualize the pancreas and biliary tract. Magnetic resonance cholangiopancreatography n (MRCP) has an emerging role in the diagnosis of suspected biliary and pancreatic duct obstruction in the setting of pancreatitis.
Differential diagnosis (DD) Early 2 to 3 h acute cholecystitis After 6 to 8 h perforated DU or acute appendicitis After 2 to 3 days intestinal obstruction If presentation is with profound shock the DD is myocardial infarction, aortic dissection, ruptured aortic aneurysm, or mesentric infarction
Natural history 80% of patients have mild pancreatitis with good recovery Mild disease accounts for less than 5% of the mortality from pancreatitis Mortality from pancreatitis due to: n n Early multiple organ failure Late infected pancreatic necrosis Hemorrhage Associated co-morbidity Aim of prognostic scores is to identify patients with severe pancreatitis

Bad prognostic markers (Ranson) On admission AGLS Age>55 n Fasting blood gulcose >200 mg% n Leucocytosis (WBC >16, 000) n LDH in serum >350 iu/L n SGOT>250 units% n
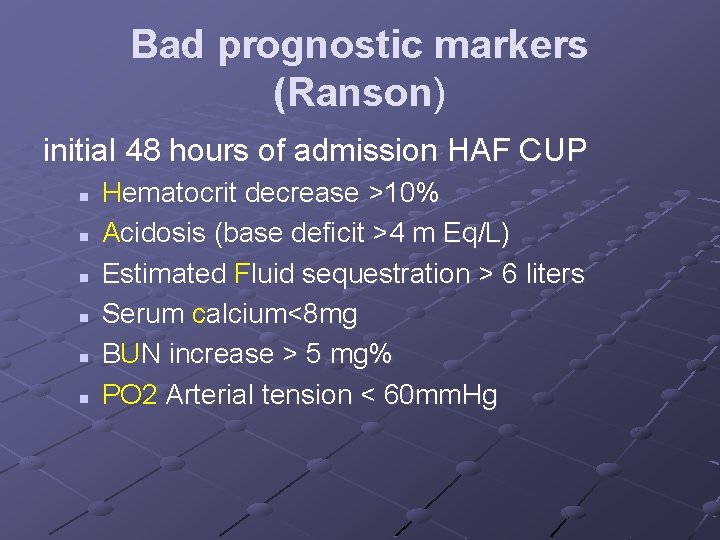
Bad prognostic markers (Ranson) initial 48 hours of admission HAF CUP n n n Hematocrit decrease >10% Acidosis (base deficit >4 m Eq/L) Estimated Fluid sequestration > 6 liters Serum calcium<8 mg BUN increase > 5 mg% PO 2 Arterial tension < 60 mm. Hg

Bad prognostic markers (Ranson) > 3~> mortality < 1% 3 -4~> mortality 18%, 5 -6~> mortality 50%, >6~> mortality 90%

Medical treatment (Acute management): Treat shock. Invasive hemodynamic monitoring may be required. May need up to 6 -8 liters of fluid per day. An NG tube useful for those with vomiting. However, NG tubes have not been shown to reduce the duration of hospitalization nor do they decrease pain intensity associated with pancreatitis. Keep the patient NPO until pain resolves and analgesia is no longer required. n n n NPO for 7 days in mild and 14 days in severe is a must. TPN can be used as a nutritional support.
Medical treatment (Acute management): Prevent hypocalcemia and hypomagnesemia. Manage pain with parenteral patient-controlled narcotics. Meperidine is preferred in the case of a common duct stone. Morphine is otherwise a good choice. (Adequate analgesia - opiate or epidural) Keep stomach p. H close to neutral by using prentral proton pump inhibitors. Octreotide has not been shown to be useful in treating pancreatitis. However Lexipafant – A platelet activating factor antagonist can be useful

Medical treatment (Acute management): Urgent ERCP to clear the biliary tract has been shown to reduce morbidity and mortality in severe acute biliary pancreatitis. Antibiotics (for the associated ascending cholangitis) are indicated. n n In several trials, imipenem has been shown to have good penetration into pancreatic tissue, and it has a good activity against all likely pathogens. Other antibiotics that have been shown to be efficacious in acute necrotizing pancreatitis include cefuroxime and a regimen of ceftazidime, amikacin, and metronidazole.
Medical treatment (Acute management): Close monitoring of n n Hemocynamics blood gases local condition by repeated CT or less efficiently U/S and treat organ failure as indicated. e. g. dialysis in renal failure oxygen therapy and PEEP in ADRS etc.

Early surgery Indications When the diagnosis is in doubt Failure of the patient to improve on medical treatment. Patients with known biliary stone disease with no improvement within 48 to 72 hours For patients who improve, they should undergo operation for cholelithiasis as soon as the pancreatitis subsides (preferably during same hospitalization)

Surgical procedures in early intervention Inspection only Placement of catheters for peritoneal lavage Biliary decompression via cholecystostomy or T tube in CBD Cholecystectomy, CBD exploration for stone extraction Decompressing gastrostomy and feeding jujenostomy For pancreatic abscess or extensive necrosis n n Total or subtotal pancreatic necrosectomy Pancreatic and retroperitoneal debridement and drainage

Complications of acute pancreatitis Local Necrosis +/- infection (pancreatic abscess) Pancreatic fluid collections (pseudocyst of the pancreas) Colonic necrosis Gastrointestinal hemorrhage Splenic rupture
Complications of acute pancreatitis Systemic Hypovolaemia and shock Coagulopathy Respiratory failure Renal Failure Hyperglycaemia Hypocalcaemia

Complications of acute pancreatitis Pseudocyst formation Is a collection of fluid, serum and hematoma in the lesser sac with a connection at some point with glandular tissue or ductal system? Abscess formation (usually after second week) It implies the presence of extensive pancreatic and peripancreatic necrosis with secondary infection (not merely infected pseudocyst) Hemorrhage From pseudoaneurysm of splenic artery or left sided portal hypertension due to splenic V thrombosis
Pseudocyst Surgery depends on five items Size (<5 cm is likely to resolve, while >7. 5 will need drainage) Development of symptoms (will indicate complications, rupture, infection or hemorrhage) Maturity (4 to 6 weeks for acute cysts to mature for better internal drainage) Vascular complications associated with pseudocyst (pseudoaneurysm is an indication for resection rather than drainage, and left sided portal hypertension is an indication of splenectomy) Site n n n retrogastric ~>cystogastrostomy, head ~>cystoduodenostomy, and inferior~>cystojujenostomy by Roux en Y)
Pseudocyst Internal drainage (cyst-enterostomy) is the rule. External drainage n n Infected or ruptured or acute cysts~> drain externally using sump drain the resulting pancreatic fistula will spontaneously close CT or U/S guided external drainage has special indications where the patient cannot tolerate surgery in infected or acute cysts with rapid enlargement

Cancer Pancreas
Cancer Pancreas In clinical practice, pancreatic cancer is synonymous with pancreatic ductal adenocarcinoma, which constitutes 90% of all primary malignant tumors arising from the gland. When cancer originates in the head of the pancreas (70%) it must also be differentiated from cancer originating from the ampulla, duodenum or lower common bile duct which has a much better prognosis than true pancreatic cancer

Risk factors Diabetes Chronic pancreatitis, and alcoholism Tobacco, coffee Previous radiation Genetics. Approximately 5 -10% of patients with pancreatic carcinoma have some genetic predisposition to developing the disease.

Clinical picture Cancer head Symptoms Triad of n n n jaundice (progressive and deep) with pain and loss of weight with anorexia is extremely common Vomiting, change in bowel habit and hematemesis and or melena occurs if the tumor invades or compresses the duodenum Signs General----Chills and fever and toxemia is due ascending cholangitis Local n n Palpable GB (Courvoisier’s sign), palpable liver (hydrohepatosis) are important signs
Clinical picture Cancer body and tail Symptoms Pain and weight loss are the two main symptoms. Pain is girdle like or in epigastrium with posterior radiation, with patient leaning forward, it may be related to meals Hematemesis, may be due to left sided portal hypertension Signs Trouseau’s signs, migrating thrombophlebitis Troisier’s signs (Virschow’s LN) Abdominal masses or malignant liver, ascites, Blummer shelf or
Coourvoisier”s law states that, if in a jaundiced patient, the gall bladder is enlarged, it is not a case of a stone impacted in the CBD for previous cholycystitis which existed when the stone was in the gall bladder, must have rendered the gall bladder fibrotic and incapable of dilatation.

Coourvoisier”s law Exceptions are Double stones, one in the CBD and another in the cystic duct, the later will force the gall bladder to distend Klatskin tumor, with carinal obstructin leaving the gal bladder not distended Ampullary tumor with no complete obstruction with intermittent relief of jaundice will not enforce the gall bladder to enlarge A gall bladder situated beneath the liver in an obese patient and cannot be palpated is another exception
Investigations Liver function Glucose tolerance curve Tumor markers n Carcinoembryonic antigen (CEA) It is a high molecular weight glycoprotein found normally in fetal tissues. The reference range is less than or equal to 2. 5 mg/m. L. Only 40 -45% of patients with pancreatic carcinoma have elevations in CEA levels. n Another tumor marker is carbohydrate antigen 19 -9 (CA 19 -9 )
Investigations Doppler ultrasound allows assessment of vascular invasion. Mesenteric angiography is now considered obsolete replaced by Doppler ultrasound CT completes the U/S especially as regards the pancreatic tumors Endoscopic ultrasound n EUS has detection rates of 99 -100% for all pancreatic carcinomas, including those smaller than 3 cm. EUS is as accurate as ERCP or MRCP for assessing the etiology of obstructive jaundice.
Investigations Endoscopic retrograde cholangiopancreatography n n n ERCP is highly sensitive for helping detect pancreatic carcinoma. Of patients with pancreatic adenocarcinoma, 90 -95% have abnormalities on ERCP findings. More recently, brush cytology and forceps biopsy at the time of ERCP have been used to histologically diagnose pancreatic carcinoma; ERCP does have the advantage of allowing for therapeutic palliation of obstructive jaundice with either a plastic or metal biliary stent.

Investigations Laparoscopy n Laparoscopy will identify liver or peritoneal metastases in 25% of patients deemed resectable after conventional imaging. Laparoscopic ultrasound has improved predictability of resection.

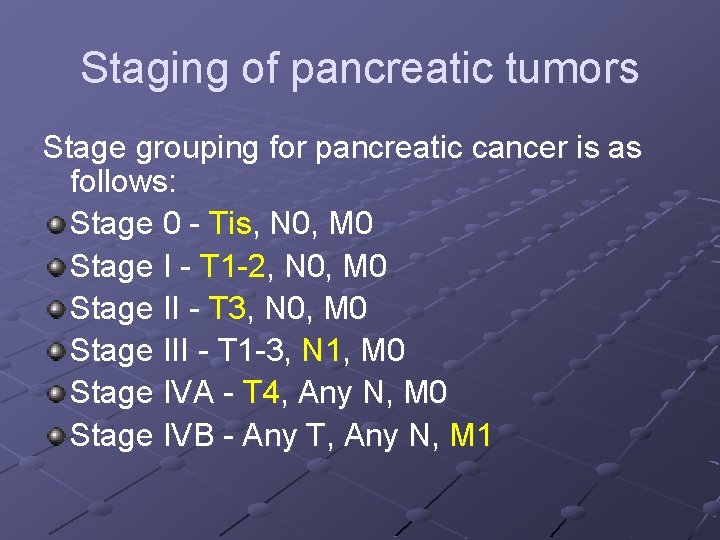
Staging of pancreatic tumors is as follows: Tumor (T) n n n n TX - Primary tumor cannot be assessed T 0 - No evidence of primary tumor Tis - Carcinoma in situ T 1 - Tumor limited to the pancreas, 2 cm or smaller in greatest dimension T 2 - Tumor limited to the pancreas, larger than 2 cm in greatest dimension T 3 - Tumor extension directly into duodenum, bile duct, or peripancreatic tissues T 4 - Tumor extension directly into stomach, spleen, colon, or adjacent large vessels

Staging of pancreatic tumors is as follows: Regional lymph nodes (N) n n n NX - Regional lymph nodes cannot be assessed N 0 - No regional lymph node metastasis N 1 - Regional lymph node metastasis p. N 1 a - Metastasis in a single regional lymph node p. N 1 b - Metastasis in multiple regional lymph nodes Distant metastasis (M) n n n MX - Distant metastasis cannot be assessed M 0 - No distant metastasis M 1 - Distant metastasis
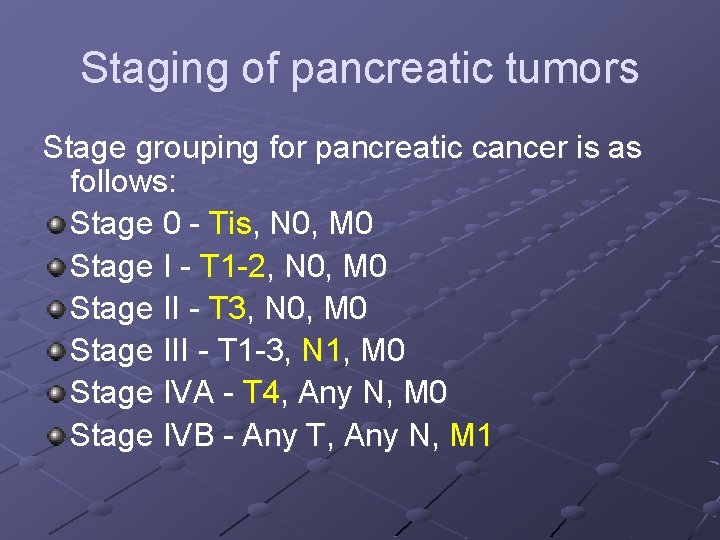
Staging of pancreatic tumors Stage grouping for pancreatic cancer is as follows: Stage 0 - Tis, N 0, M 0 Stage I - T 1 -2, N 0, M 0 Stage II - T 3, N 0, M 0 Stage III - T 1 -3, N 1, M 0 Stage IVA - T 4, Any N, M 0 Stage IVB - Any T, Any N, M 1
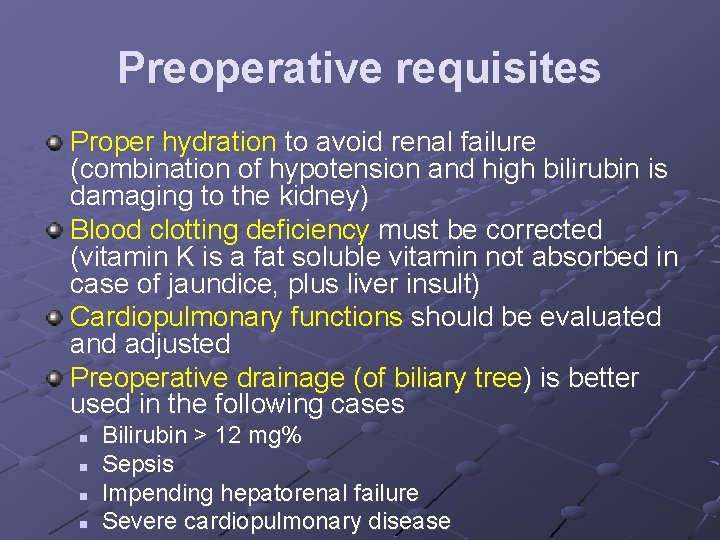
Preoperative requisites Proper hydration to avoid renal failure (combination of hypotension and high bilirubin is damaging to the kidney) Blood clotting deficiency must be corrected (vitamin K is a fat soluble vitamin not absorbed in case of jaundice, plus liver insult) Cardiopulmonary functions should be evaluated and adjusted Preoperative drainage (of biliary tree) is better used in the following cases n n Bilirubin > 12 mg% Sepsis Impending hepatorenal failure Severe cardiopulmonary disease

Resectional surgery Resection is the only hope of cure Only 15% tumors are deemed resectable Resectability assessed by: n Tumor size (<4 cm) n Invasion of SMA or portal vein n Presence of ascites, nodal, peritoneal or liver metastases

Resectional surgery Pre-operative biliary drainage of unproven benefit. It has not been shown to reduce post-operative morbidity or mortality Neoadjuvant chemoradiation: Some institutions use neoadjuvant chemotherapy and radiation therapy to try to improve the resectability potential of locally advanced cancers.

Whipple's operation Involves a pancreatico-duodenal resection Initial assessment of resectability by n n dissection and Kocherization of the duodenum, with, most importantly a finger passing easily anterior to the superior mesenteric portal vein axis behind the neck of the pancreas. Head of pancreas and duodenum excised followed by: n n n End to side pancreaticojejunostomy End to side hepaticojejunostomy Gastroojejunostomy






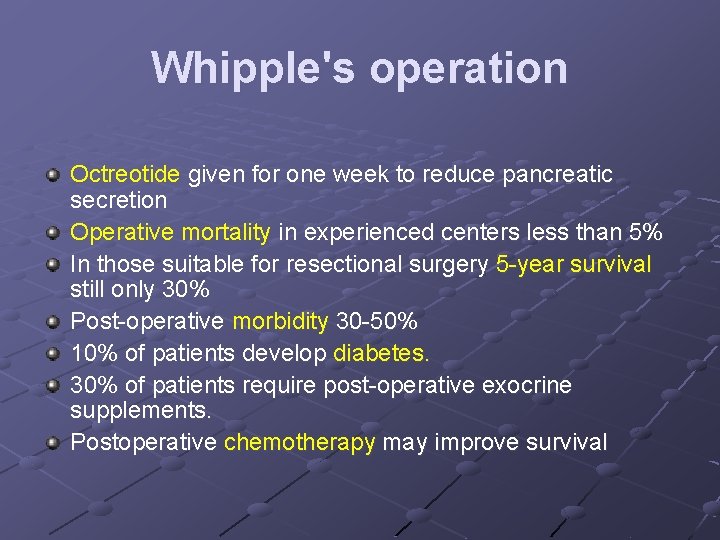
Whipple's operation Octreotide given for one week to reduce pancreatic secretion Operative mortality in experienced centers less than 5% In those suitable for resectional surgery 5 -year survival still only 30% Post-operative morbidity 30 -50% 10% of patients develop diabetes. 30% of patients require post-operative exocrine supplements. Postoperative chemotherapy may improve survival
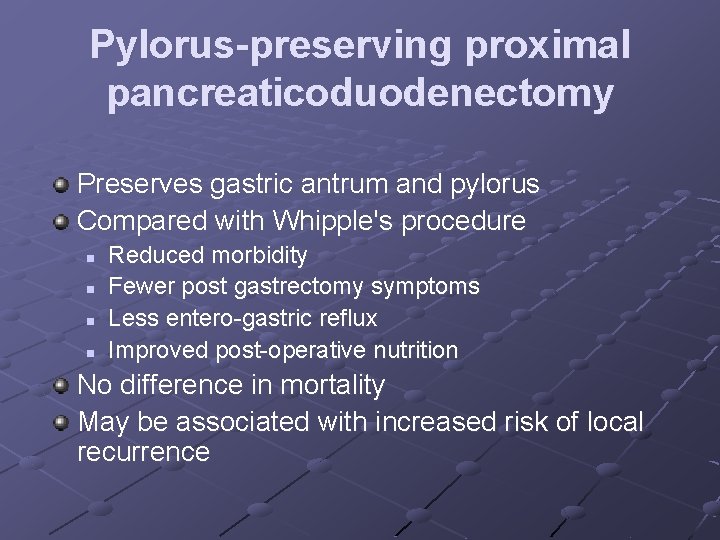
Pylorus-preserving proximal pancreaticoduodenectomy Preserves gastric antrum and pylorus Compared with Whipple's procedure n n Reduced morbidity Fewer post gastrectomy symptoms Less entero-gastric reflux Improved post-operative nutrition No difference in mortality May be associated with increased risk of local recurrence


Palliation of pancreatic cancer 85% of patients are not suitable for curative resection Palliation of symptoms can be achieved either surgically or endoscopically Surgical palliation has initially higher complication rate Produces better long-term symptom control.
Palliation of pancreatic cancer Palliative treatment should achieve: n n n Relief of jaundice by either endoscopic stenting or surgery Prevention of duodenal obstruction by gastrojejunostomy Relief of pain? By celiac plexus block External biliary drainage now rarely required Palliative chemotherapy (e. g. gemcitabine) controversia Radiation therapy for pancreatic cancer can palliate pain but does not affect the patient's survival.
 Apendicolith
Apendicolith Pancreatitis pathophysiology
Pancreatitis pathophysiology Ranson criteria
Ranson criteria Acute pancreatitis nursing management
Acute pancreatitis nursing management Ranson
Ranson Acute pancreatitis ct
Acute pancreatitis ct Ranson criteria
Ranson criteria Acute pancreatitis pes statement
Acute pancreatitis pes statement Patho
Patho Ct severity index
Ct severity index What activates trypsinogen
What activates trypsinogen Symptoms of overtrading
Symptoms of overtrading Implies in propositional logic
Implies in propositional logic A body will be in translational equilibrium if: phy101
A body will be in translational equilibrium if: phy101 Implies in propositional logic
Implies in propositional logic Logical connectives symbols
Logical connectives symbols Circular motion lab
Circular motion lab Job design definition
Job design definition Partitioning a directed line segment
Partitioning a directed line segment It implies emphasizing on specific message or goal at time
It implies emphasizing on specific message or goal at time Management implies
Management implies Absolute continuity implies uniform continuity
Absolute continuity implies uniform continuity In triangle pqr
In triangle pqr Contradiction formula
Contradiction formula Who implies something?
Who implies something? Clarity in effective communication
Clarity in effective communication Tangent line formula
Tangent line formula Absolute vs conditional convergence
Absolute vs conditional convergence Site:slidetodoc.com
Site:slidetodoc.com Andrew jackson found his greatest support among
Andrew jackson found his greatest support among What do the picture imply
What do the picture imply Term to term rule
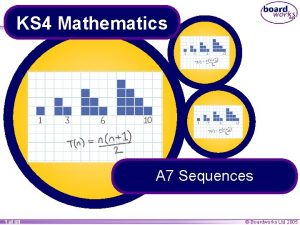
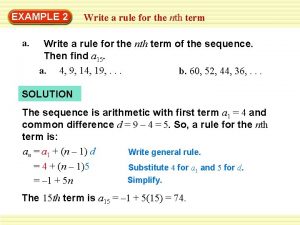
Term to term rule Nth term of ap
Nth term of ap Accounting for serial bonds
Accounting for serial bonds Short, medium and long term planning in education
Short, medium and long term planning in education Long term goal examples
Long term goal examples Short term human resources
Short term human resources Min term max term
Min term max term Term-to-term rule
Term-to-term rule Short term financial management
Short term financial management Position-to-term
Position-to-term Term to term rule example
Term to term rule example Long term memory vs short term memory
Long term memory vs short term memory Difference between long term and short term liabilities
Difference between long term and short term liabilities Rat diaphragm
Rat diaphragm Enterokinase enzyme function
Enterokinase enzyme function Glandula pancreas
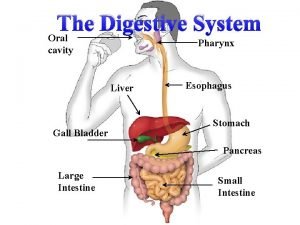
Glandula pancreas Liver and pancreas function
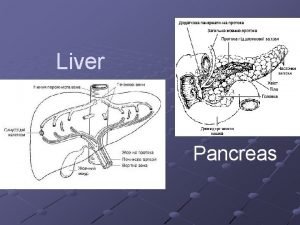
Liver and pancreas function Richtlijn pancreatitis
Richtlijn pancreatitis Ams pancreas
Ams pancreas Tuber omentale of pancreas
Tuber omentale of pancreas Pancreas non esplorabile per meteorismo
Pancreas non esplorabile per meteorismo Anatomy and physiology diabetes
Anatomy and physiology diabetes Pancreas anatomy
Pancreas anatomy Location
Location Glandula endocrino
Glandula endocrino Cells
Cells Cullen's sign
Cullen's sign Májlebenyke
Májlebenyke Ductus omfaloentericus
Ductus omfaloentericus Como es el proceso de la digestión
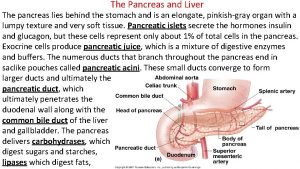
Como es el proceso de la digestión Pancreas lies
Pancreas lies Baylor
Baylor Pancréas
Pancréas Diagram of kidney pain
Diagram of kidney pain Fisiopatologia pancreas
Fisiopatologia pancreas Cwrm pancreas
Cwrm pancreas Pharynx digestion
Pharynx digestion Vena interlobularis
Vena interlobularis