INFLAMMATION Comprehensive Approach Inflammation and repair Inflammation is








- Slides: 50
INFLAMMATION Comprehensive Approach
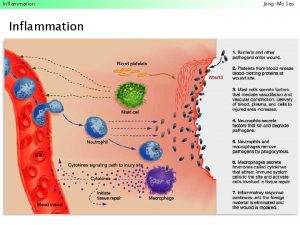
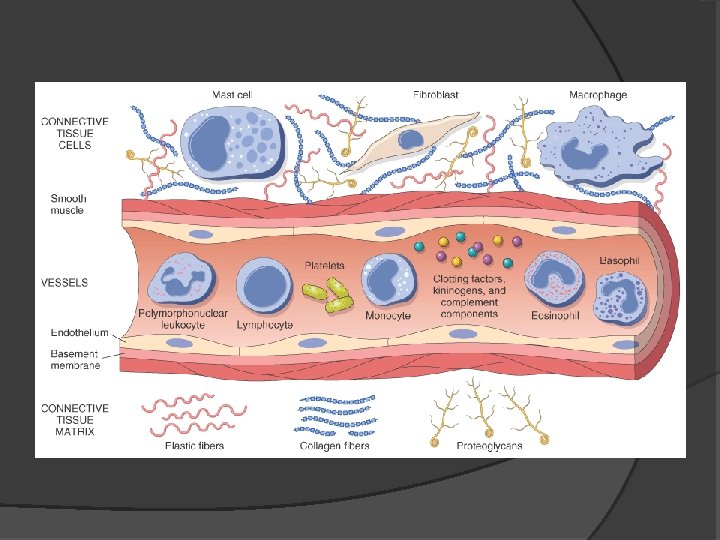
Inflammation and repair � Inflammation is fundamentally a protective response � Inflammation and repair may be potentially harmful � The inflammatory response consists of two main components, a vascular reaction and a cellular reaction
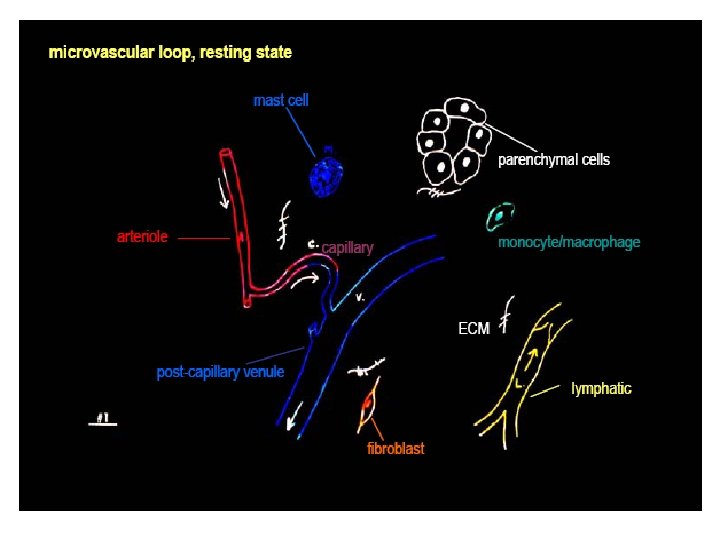
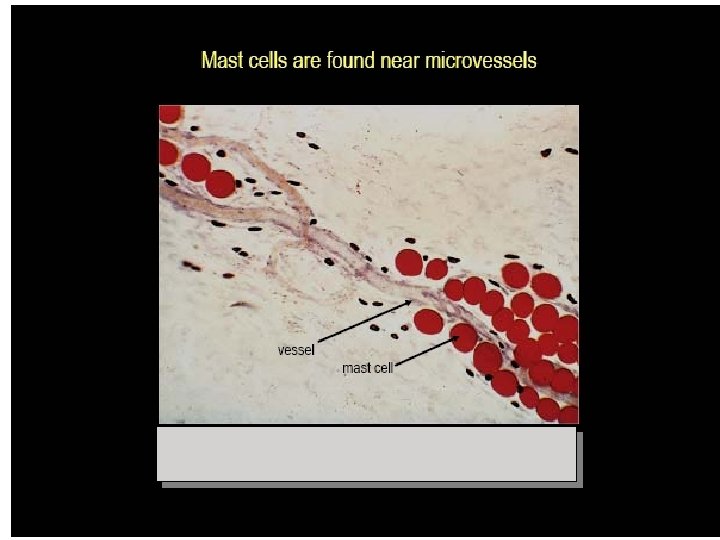
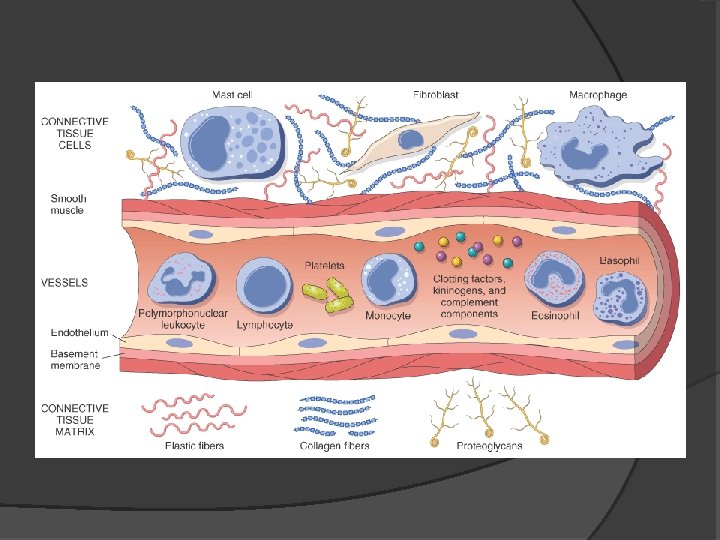
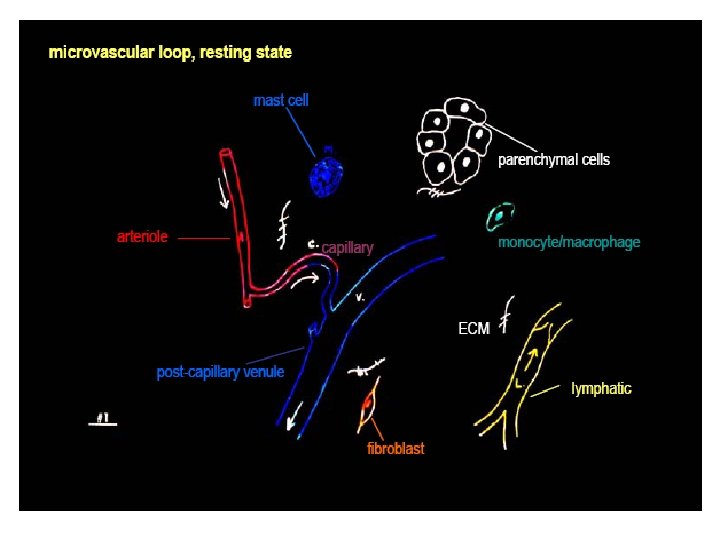
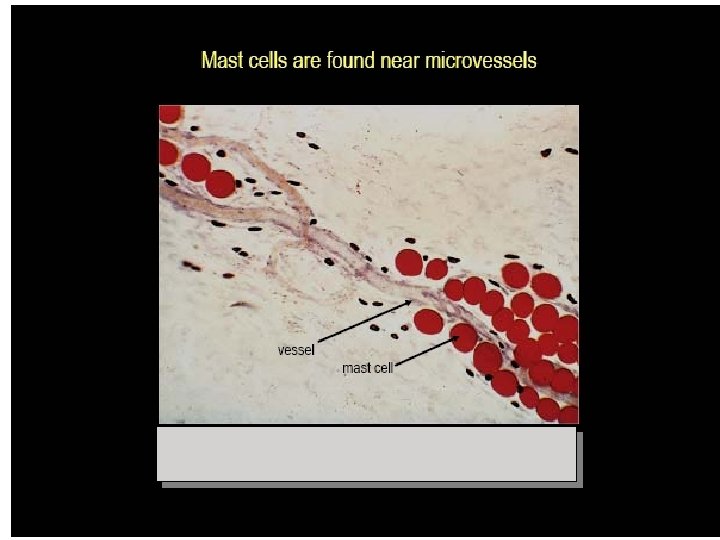
Inflammation and repair � Neutrophils, monocytes, eosinophils, lymphocytes, basophils, and platelets. � Mast cells, fibroblasts, resident macrophages and lymphocytes. � The extracellular matrix
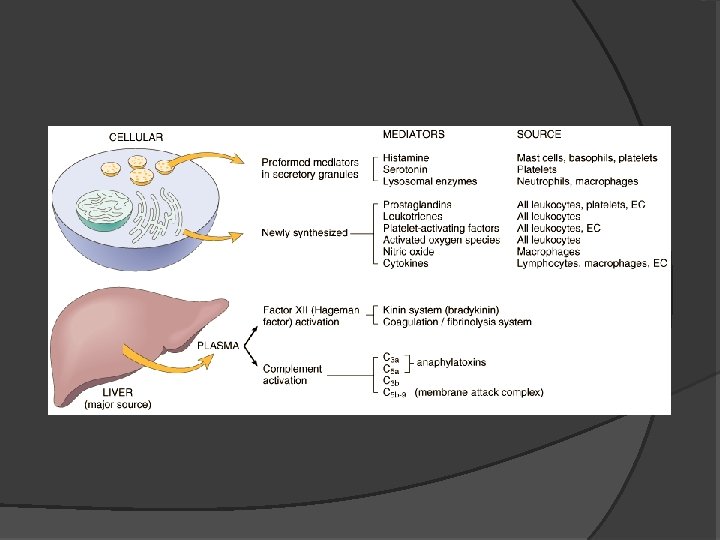
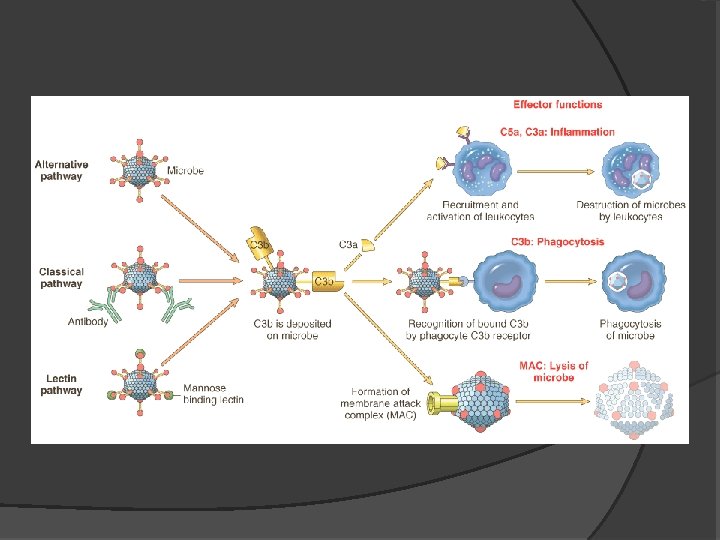
Inflammation and repair � Acute inflammation � Chronic inflammation � The vascular and cellular reactions of both acute and chronic inflammation are mediated by chemical factors
Inflammation and repair Historical Perspective: � (Latin, inflamatio, to set on fire) � The word "inflammation" goes back at least to ancient Egyptian times. “Shem-e -met " : Inflammation and ends in a symbol called a determinative, a "flaming brazier". This brazier is a device heated with fire.

Dr. Maha Arafah:

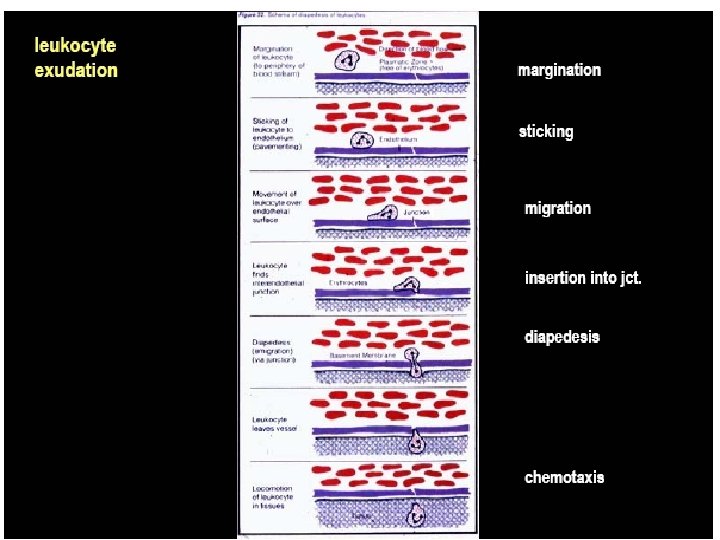


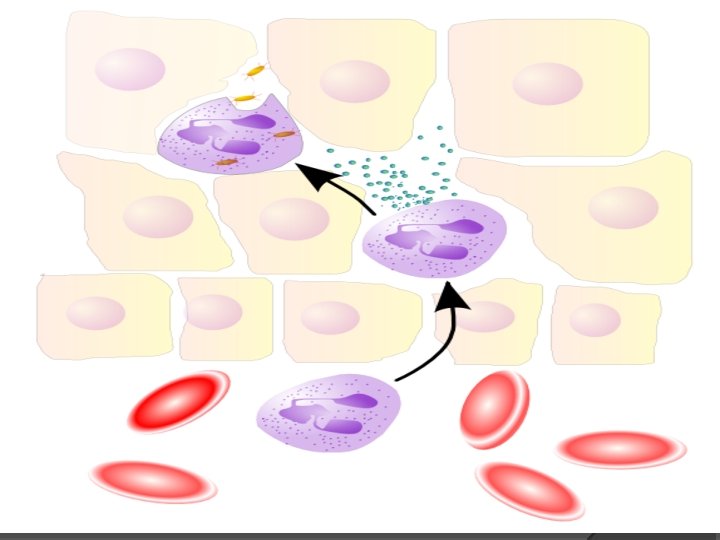

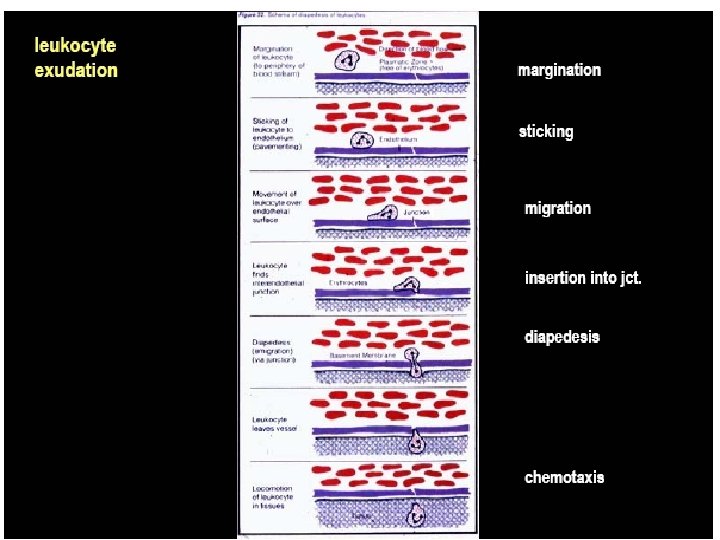
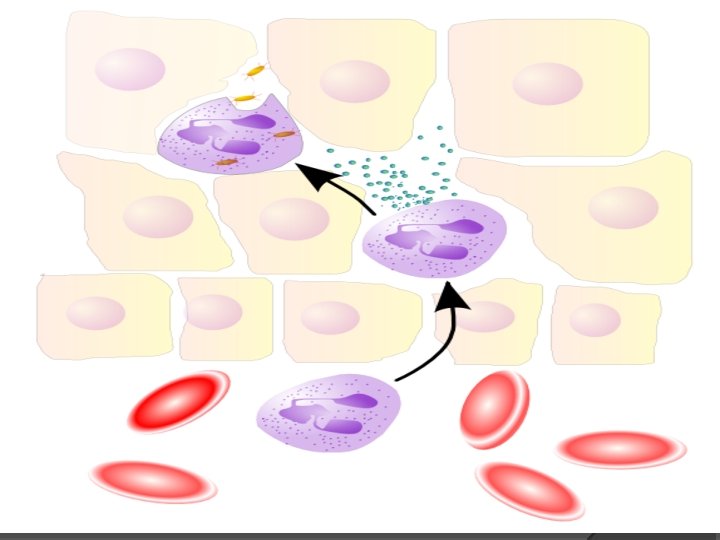
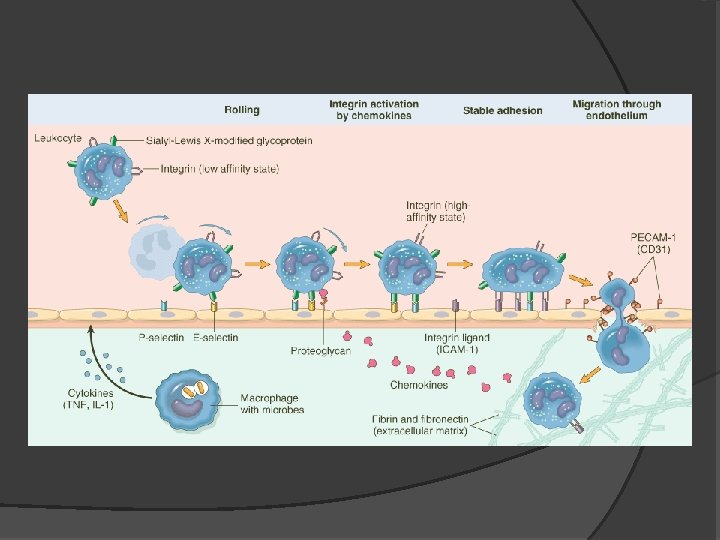
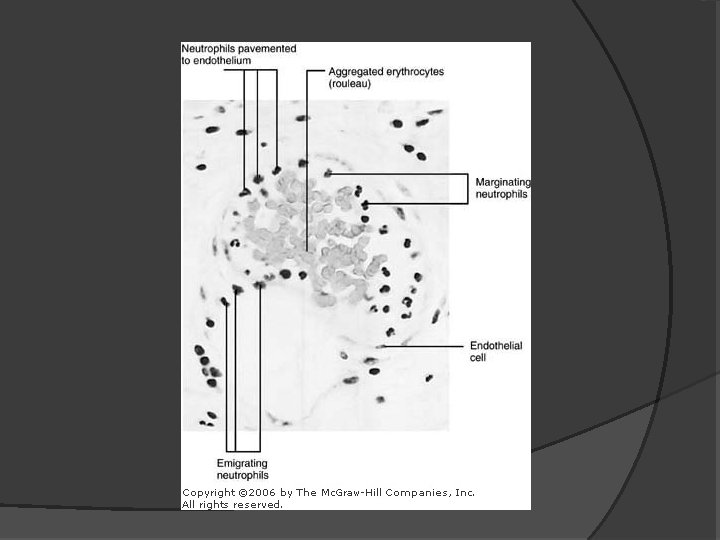
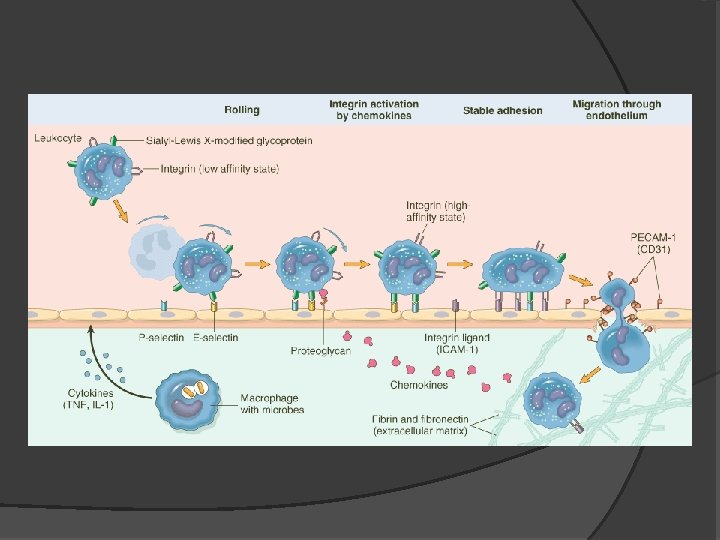
Inflammation and repair Leukocyte extravasation � Leukocyte localisation and recruitment to the endothelium local to the site of inflammation – involving margination and adhesion to the endothelial cells �
Inflammation and repair � Greek for flame, and indeed an inflamed body part may feel ‘on fire’. In its traditional clinical description, inflammation has four characteristics: calor (heat), rubor (redness), tumor (swelling and dolor (pain).
Inflammation and repair
Inflammation Overview of Cellular Mechanisms Involved in Acute Inflammation � Chemical Mediators of Acute Inflammation � Examples of Acute Inflammatory Responses � Differences Between Acute and Chronic Inflammation � Examples of Chronic Inflammation � Discussion of Potential Roles of Nutrition in Inflammation �
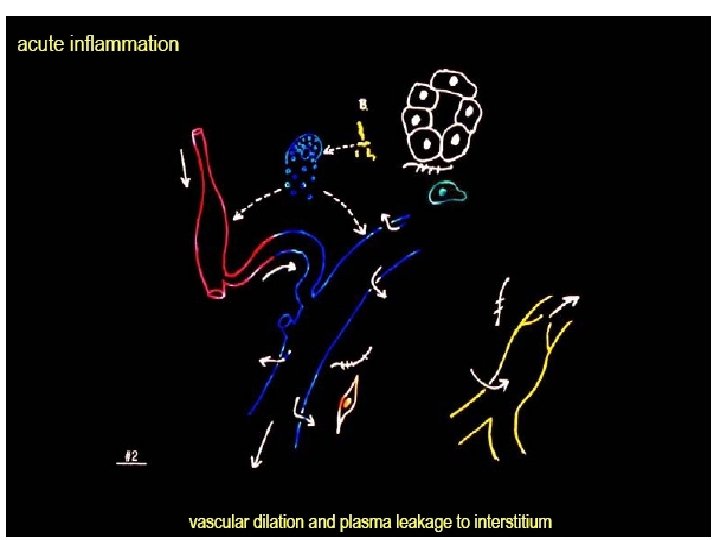
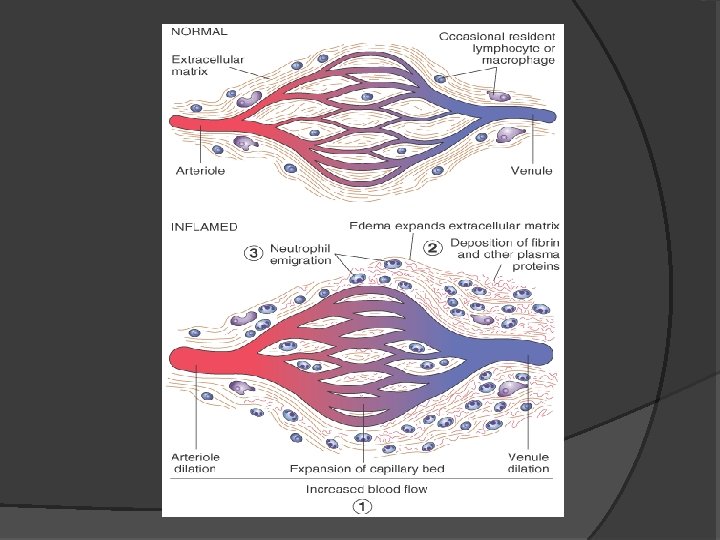
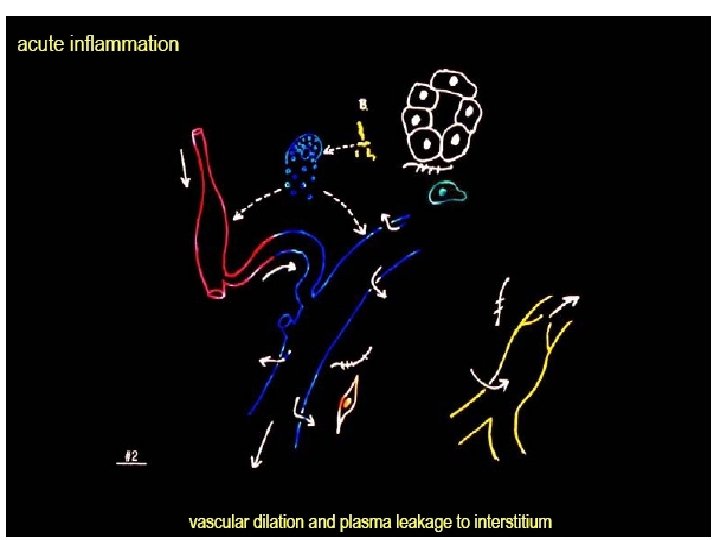
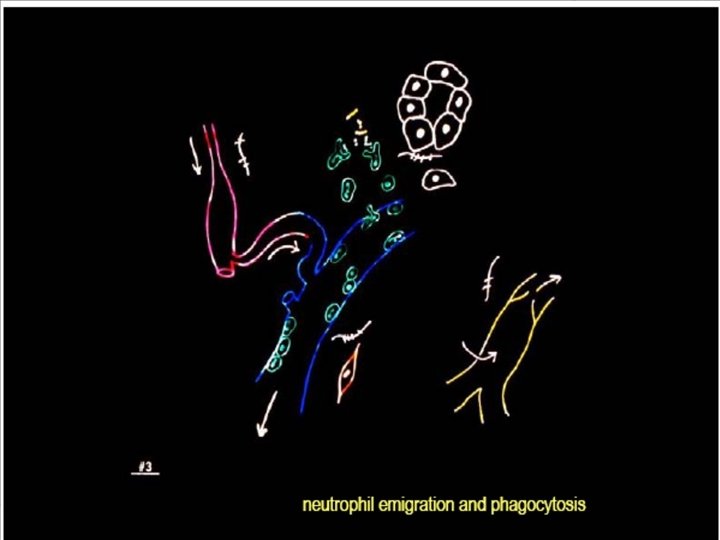
Acute Inflammation Acute inflammation is a rapid response to an injurious agent that serves to deliver mediators of host defense— leukocytes and plasma proteins—to the site of injury. Acute inflammation has three major components: (1) alterations in vascular caliber that lead to an increase in blood flow; (2) structural changes in the microvasculature that permit plasma proteins and leukocytes to leave the circulation; and (3) emigration of the leukocytes from the microcirculation, their accumulation in the focus of injury, and their activation to eliminate the offending agent
Acute inflammatory reactions are triggered by a variety of stimuli: • Infections (bacterial, viral, parasitic) and microbial toxins • Trauma (blunt and penetrating) • Physical and chemical agents (thermal injury, e. g. , burns or frostbite; irradiation; some environmental chemicals) • Tissue necrosis (from any cause) • Foreign bodies (splinters, dirt, sutures) • Immune reactions (also called hypersensitivity reactions)
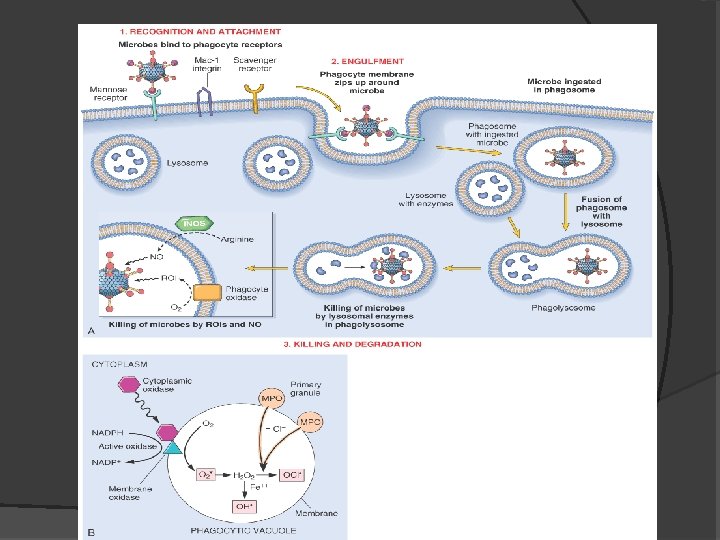
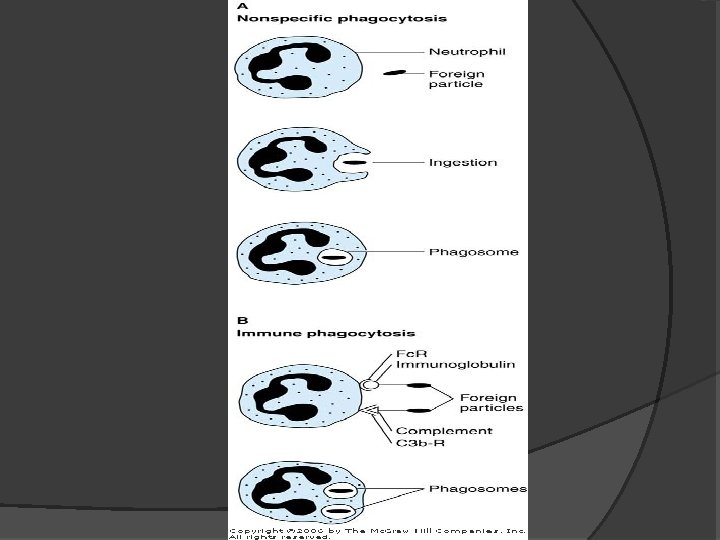
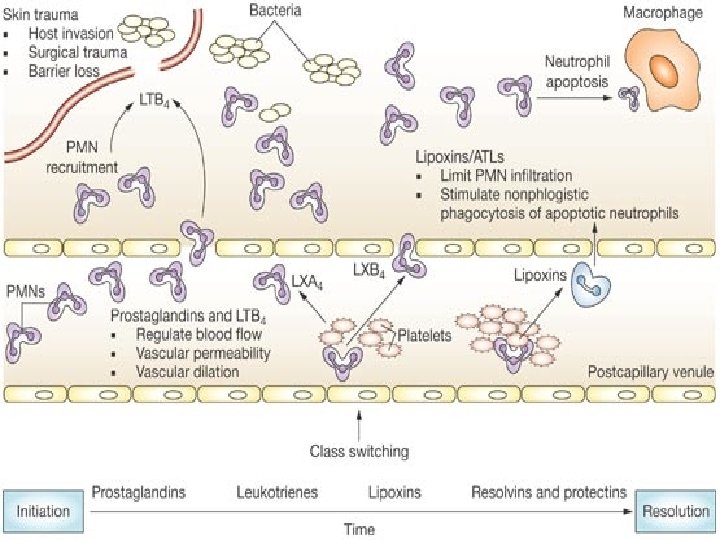
Acute Inflammation When a host encounters an injurious agent, such as an infectious microbe or dead cells, phagocytes that reside in all tissues try to get rid of these agents. At the same time, phagocytes and other host cells react to the presence of the foreign or abnormal substance by liberating cytokines, lipid messengers, and the various other mediators of inflammation. Some of these mediators act on endothelial cells in the vicinity and promote the efflux of plasma and the recruitment of circulating leukocytes to the site where the offending agent is located.
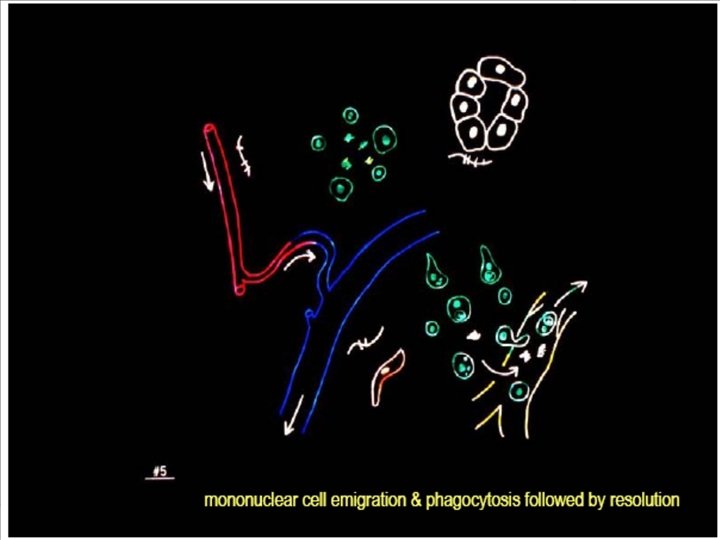
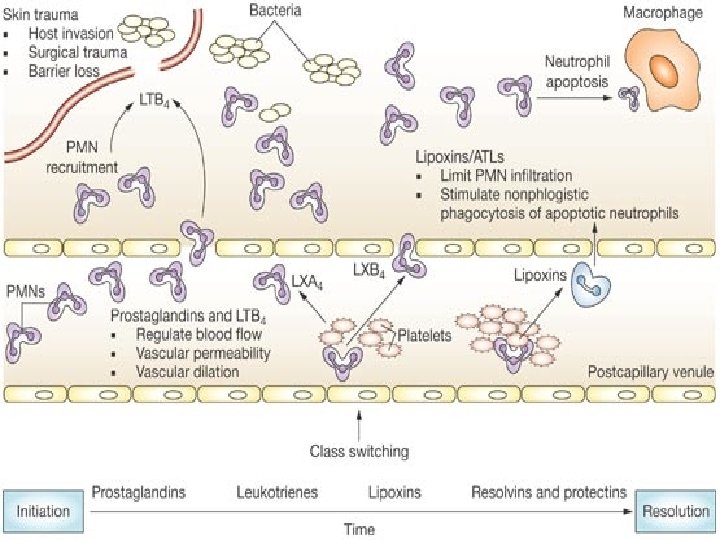
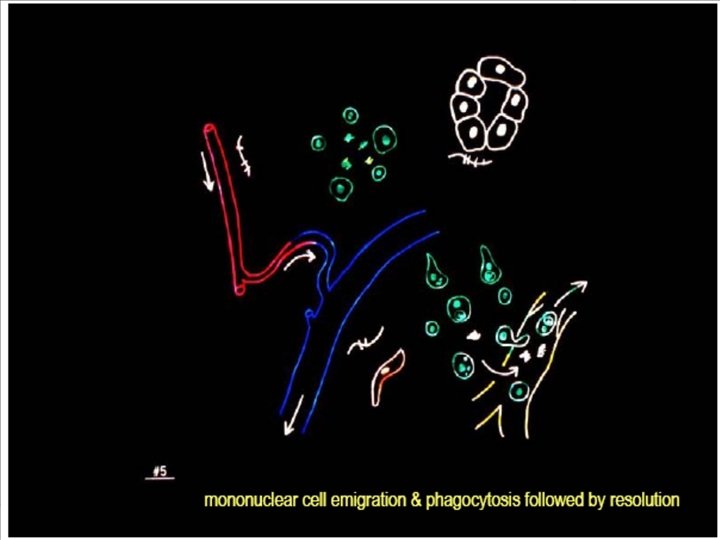
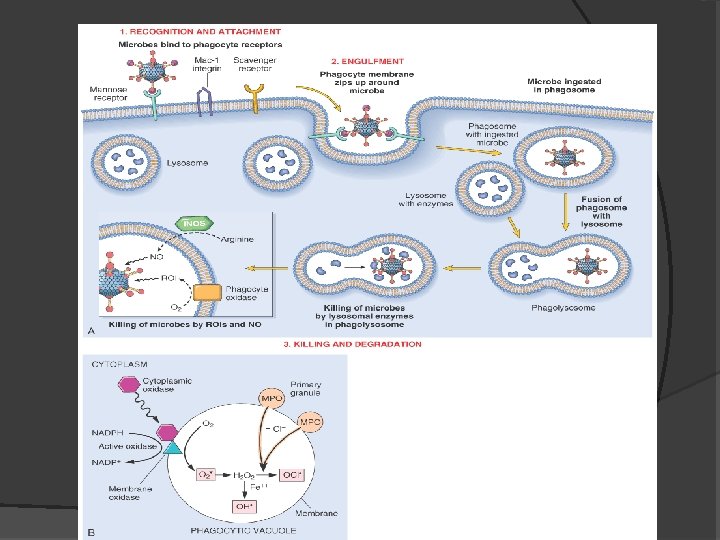
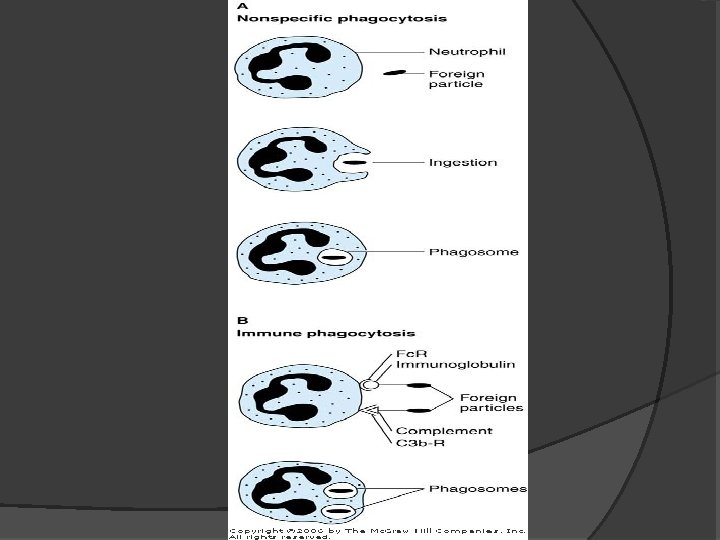
Acute Inflammation - continued As the injurious agent is eliminated anti-inflammatory mechanisms become active, the process subsides and the host returns to a normal state of health. If the injurious agent cannot be quickly eliminated, the result may be chronic inflammation. The recruited leukocytes are activated by the injurious agent and by locally produced mediators, and the activated leukocytes try to remove the offending agent by phagocytosis.
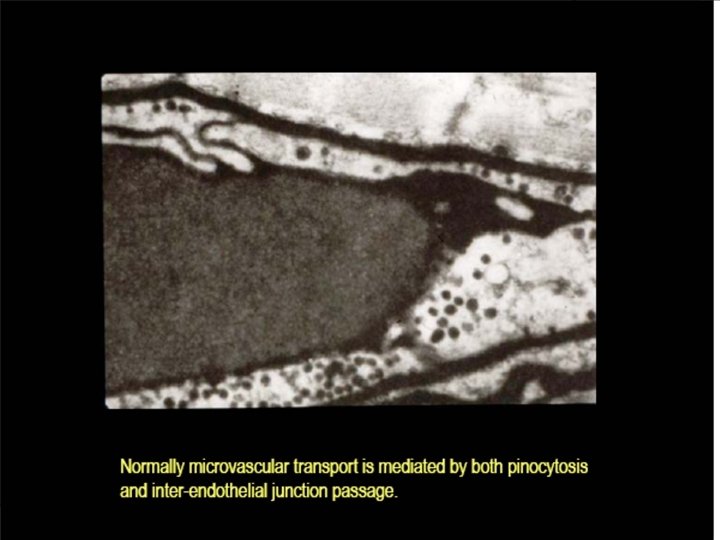
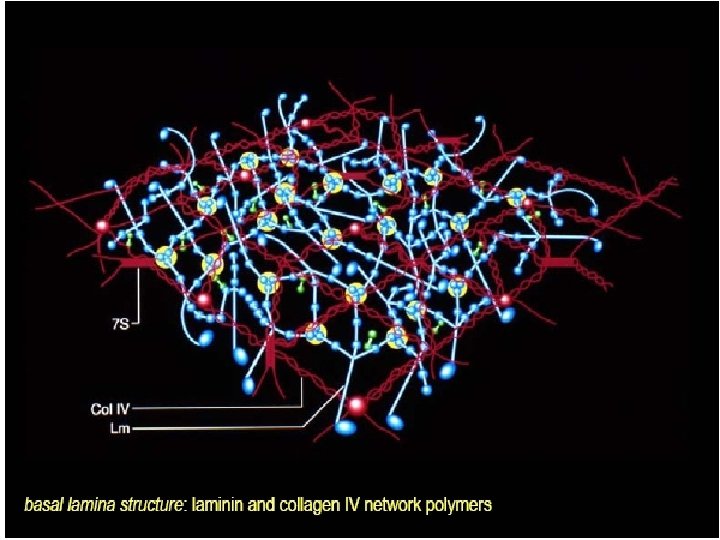
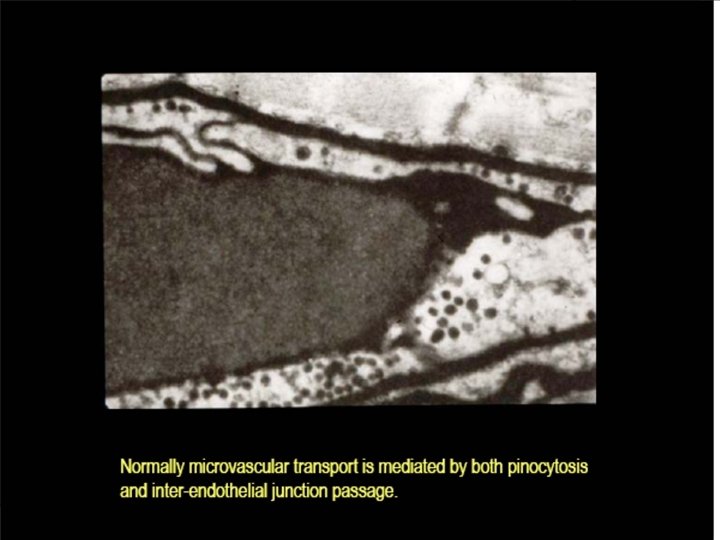
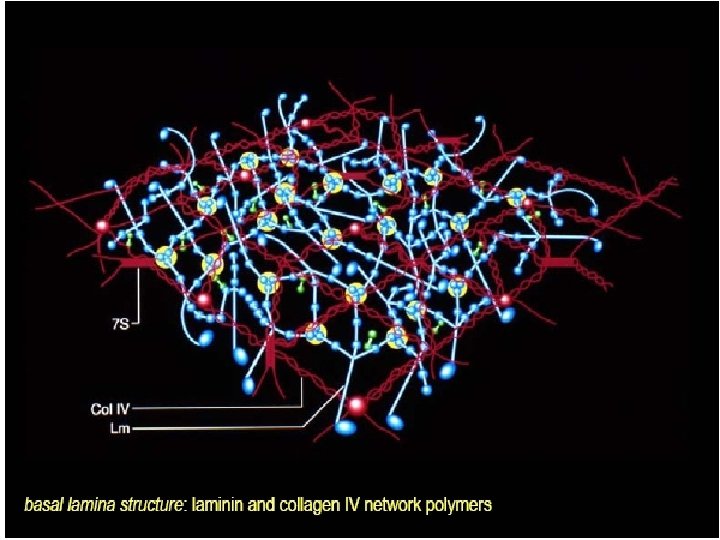
The vascular phenomena of acute inflammation are characterized by increased blood flow to the injured area, resulting mainly from arteriolar dilation and opening of capillary beds induced by mediators such as histamine. Increased vascular permeability results in the accumulation of proteinrich extravascular fluid, which forms the exudate. Plasma proteins leave the vessels, most commonly through widened interendothelial cell junctions of the venules. The redness (rubor), warmth (calor), and swelling (tumor) of acute inflammation are caused by the increased blood flow and edema.
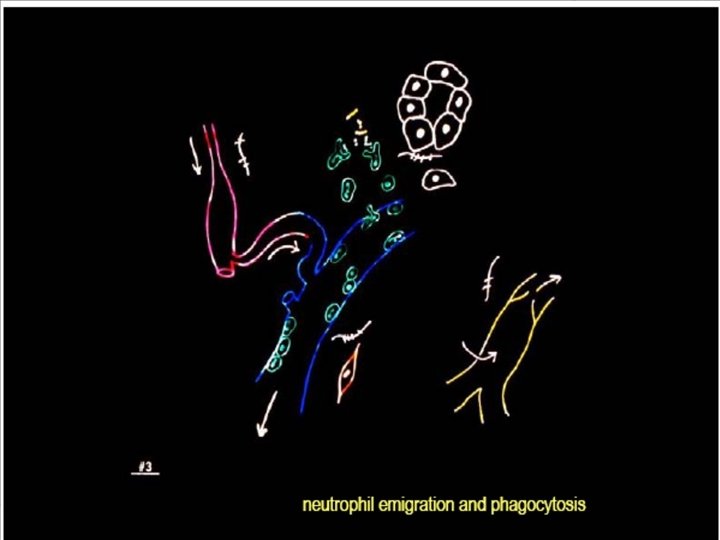
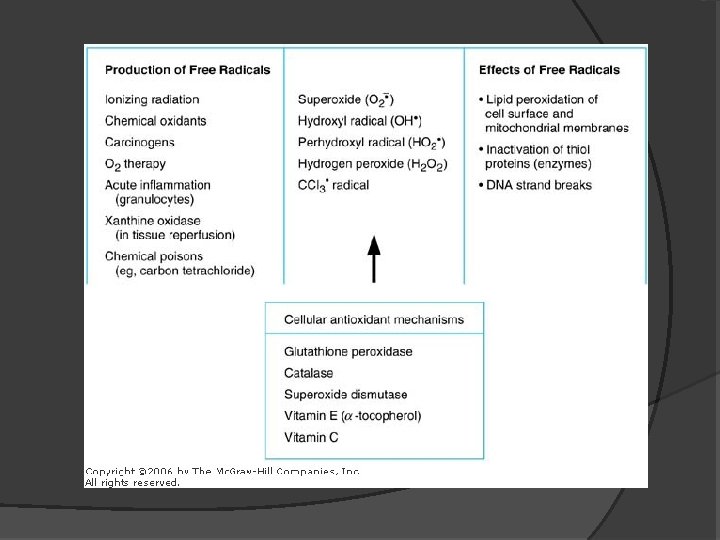
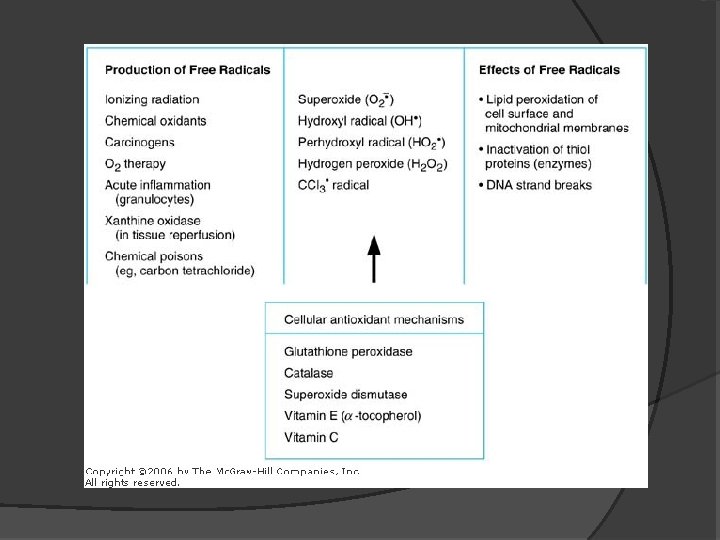
Circulating leukocytes, initially predominantly neutrophils, adhere to the endothelium via adhesion molecules, transmigrate across the endothelium, and migrate to the site of injury under the influence of chemotactic agents. Leukocytes that are activated by the offending agent and by endogenous mediators may release toxic metabolites and proteases extracellularly, causing tissue damage. During the damage, and in part as a result of the liberation of prostaglandins, neuropeptides, and cytokines, one of the local symptoms is pain (dolor).
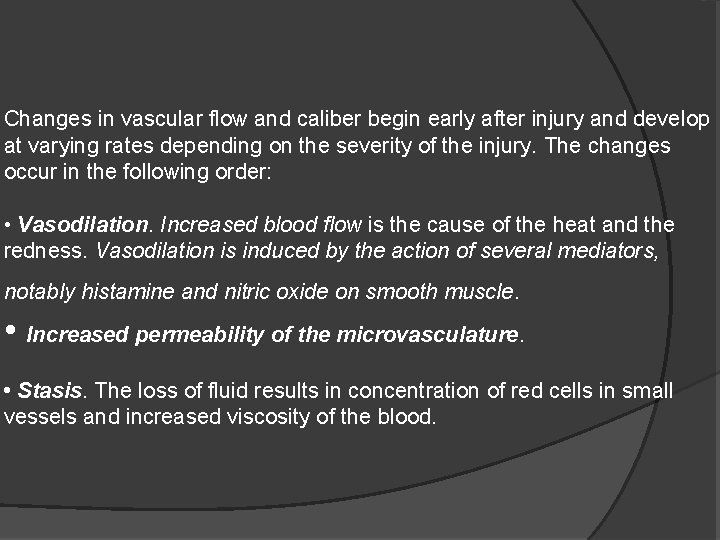
Changes in vascular flow and caliber begin early after injury and develop at varying rates depending on the severity of the injury. The changes occur in the following order: • Vasodilation. Increased blood flow is the cause of the heat and the redness. Vasodilation is induced by the action of several mediators, notably histamine and nitric oxide on smooth muscle. • Increased permeability of the microvasculature. • Stasis. The loss of fluid results in concentration of red cells in small vessels and increased viscosity of the blood.
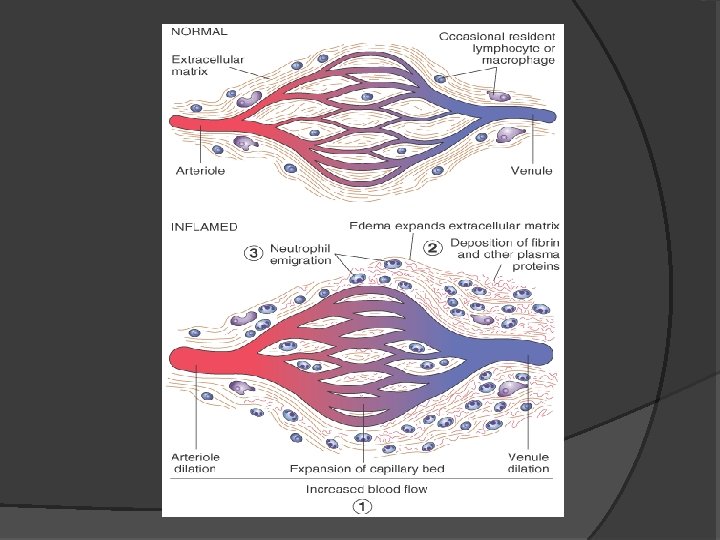
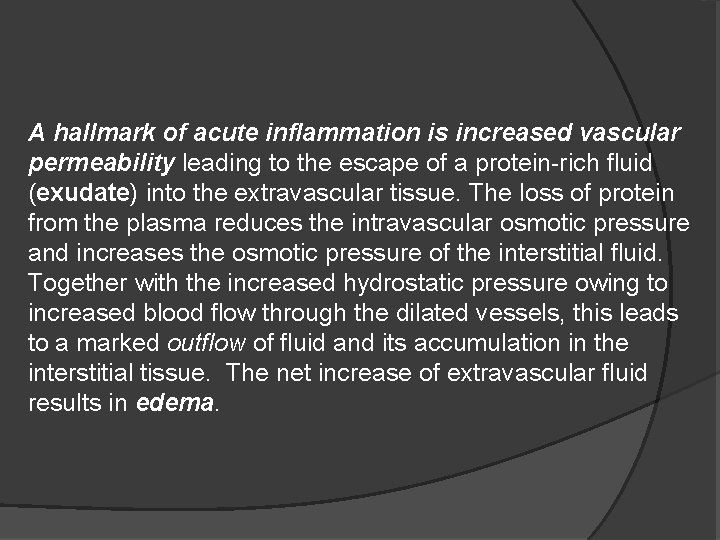
A hallmark of acute inflammation is increased vascular permeability leading to the escape of a protein-rich fluid (exudate) into the extravascular tissue. The loss of protein from the plasma reduces the intravascular osmotic pressure and increases the osmotic pressure of the interstitial fluid. Together with the increased hydrostatic pressure owing to increased blood flow through the dilated vessels, this leads to a marked outflow of fluid and its accumulation in the interstitial tissue. The net increase of extravascular fluid results in edema.
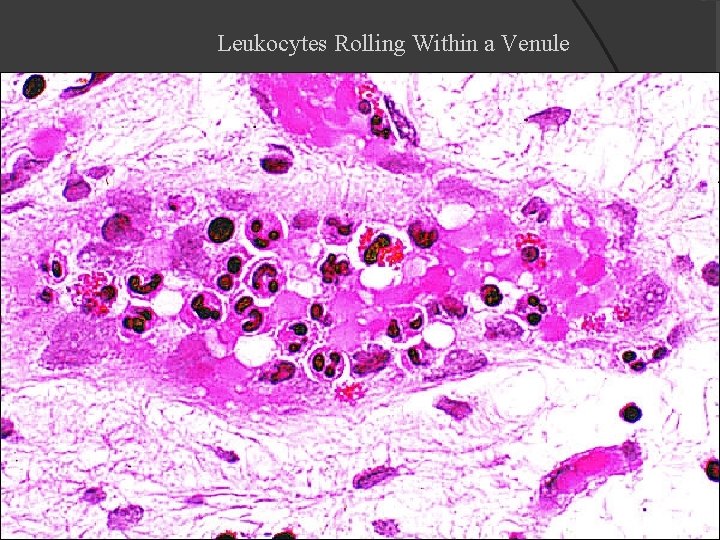
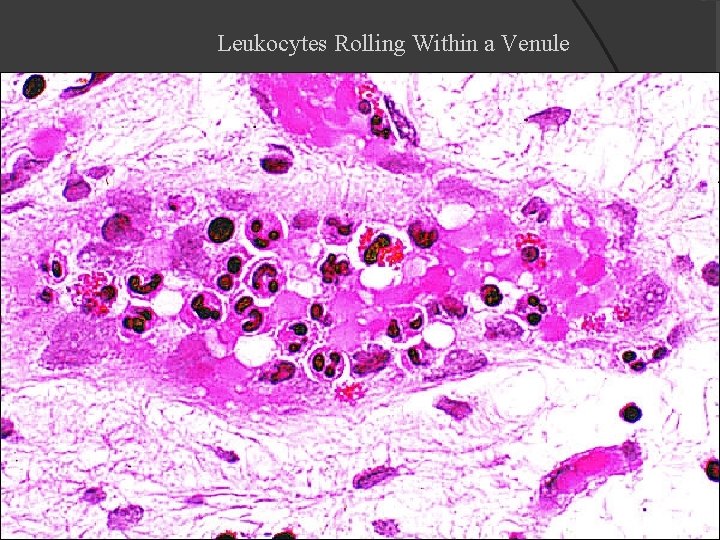
Leukocytes Rolling Within a Venule
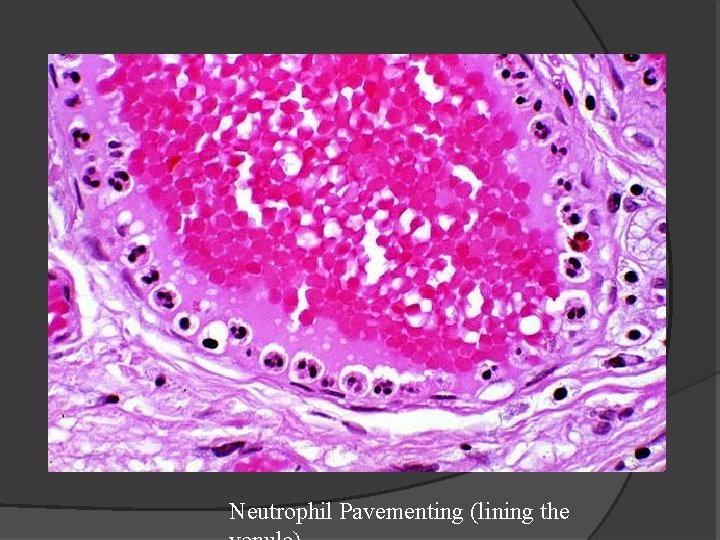
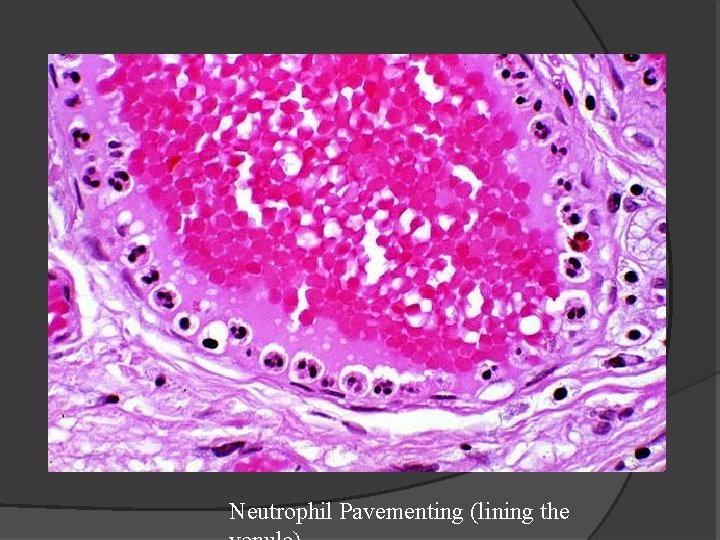
Neutrophil Pavementing (lining the
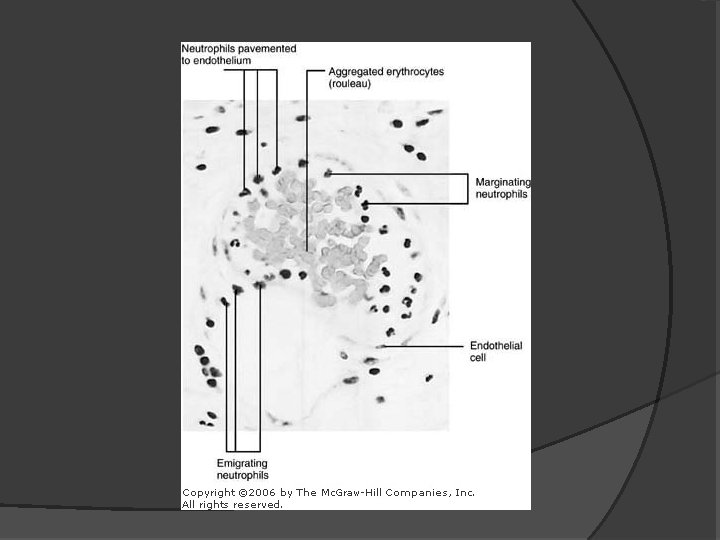
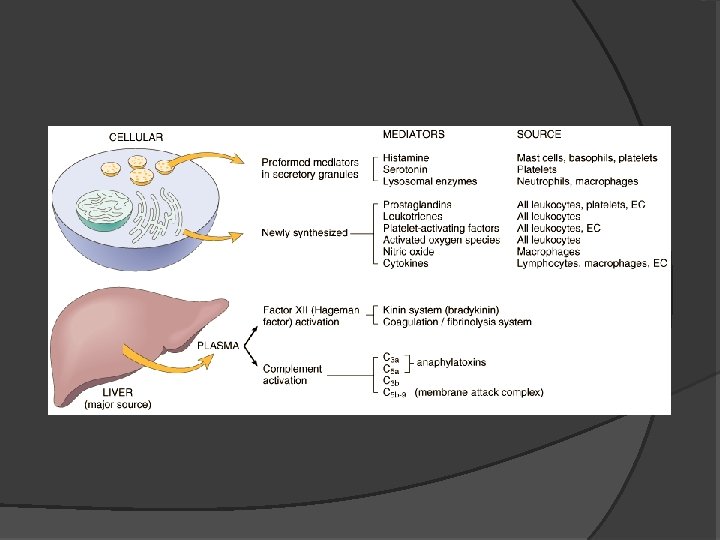
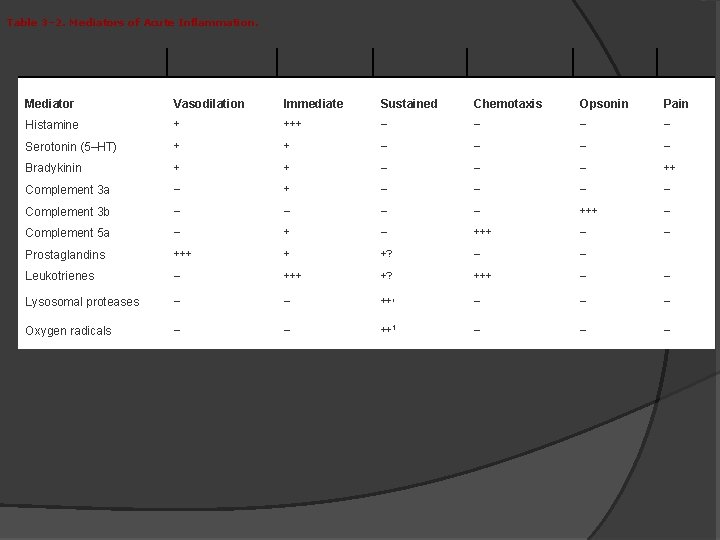
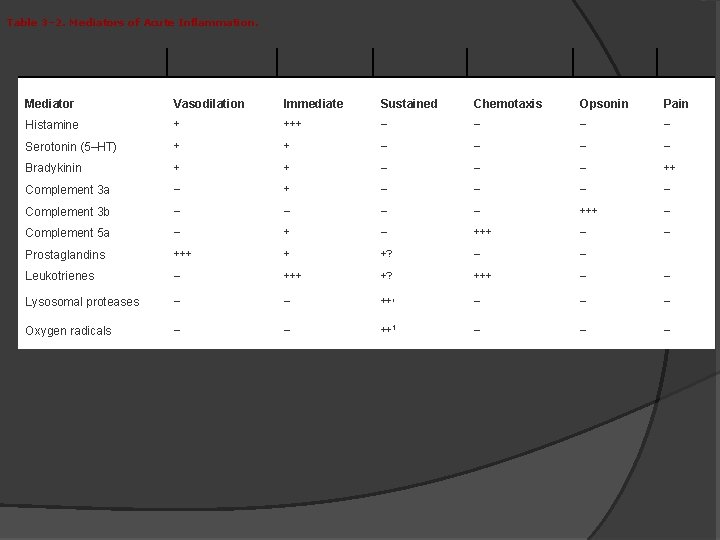
Table 3– 2. Mediators of Acute Inflammation. Mediator Vasodilation Immediate Sustained Chemotaxis Opsonin Pain Histamine + +++ – – Serotonin (5–HT) + + – – Bradykinin + + – – – ++ Complement 3 a – + – – Complement 3 b – – +++ – Complement 5 a – +++ – – Prostaglandins +++ + +? – – Leukotrienes – +++ +? +++ – – Lysosomal proteases – – ++1 – – – Oxygen radicals – – – ++1



Resolution of Acute Inflammation
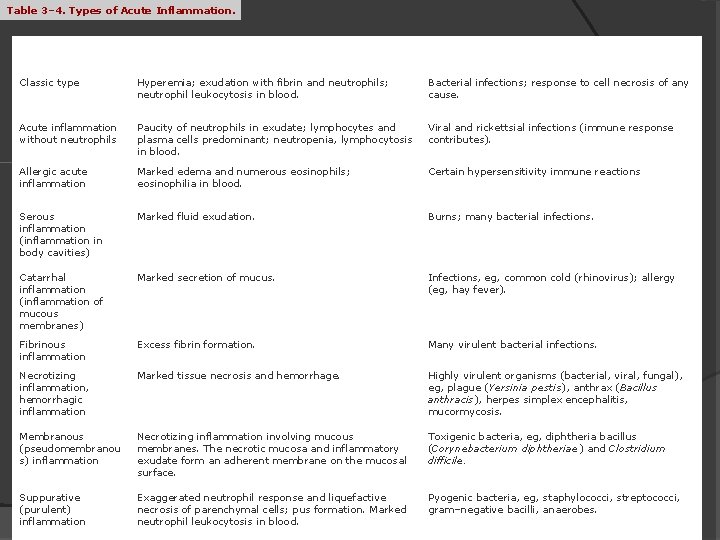
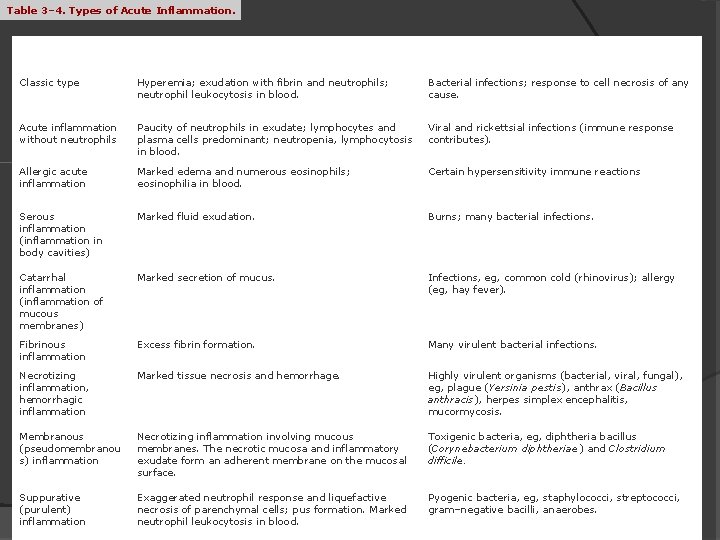
Table 3– 4. Types of Acute Inflammation. Type Features Common Causes Classic type Hyperemia; exudation with fibrin and neutrophils; neutrophil leukocytosis in blood. Bacterial infections; response to cell necrosis of any cause. Acute inflammation without neutrophils Paucity of neutrophils in exudate; lymphocytes and plasma cells predominant; neutropenia, lymphocytosis in blood. Viral and rickettsial infections (immune response contributes). Allergic acute inflammation Marked edema and numerous eosinophils; eosinophilia in blood. Certain hypersensitivity immune reactions Serous inflammation (inflammation in body cavities) Marked fluid exudation. Burns; many bacterial infections. Catarrhal inflammation (inflammation of mucous membranes) Marked secretion of mucus. Infections, eg, common cold (rhinovirus); allergy (eg, hay fever). Fibrinous inflammation Excess fibrin formation. Many virulent bacterial infections. Necrotizing inflammation, hemorrhagic inflammation Marked tissue necrosis and hemorrhage. Highly virulent organisms (bacterial, viral, fungal), eg, plague (Yersinia pestis), anthrax (Bacillus anthracis), herpes simplex encephalitis, mucormycosis. Membranous (pseudomembranou s) inflammation Necrotizing inflammation involving mucous membranes. The necrotic mucosa and inflammatory exudate form an adherent membrane on the mucosal surface. Toxigenic bacteria, eg, diphtheria bacillus (Corynebacterium diphtheriae) and Clostridium difficile. Suppurative (purulent) inflammation Exaggerated neutrophil response and liquefactive necrosis of parenchymal cells; pus formation. Marked neutrophil leukocytosis in blood. Pyogenic bacteria, eg, staphylococci, streptococci, gram–negative bacilli, anaerobes.
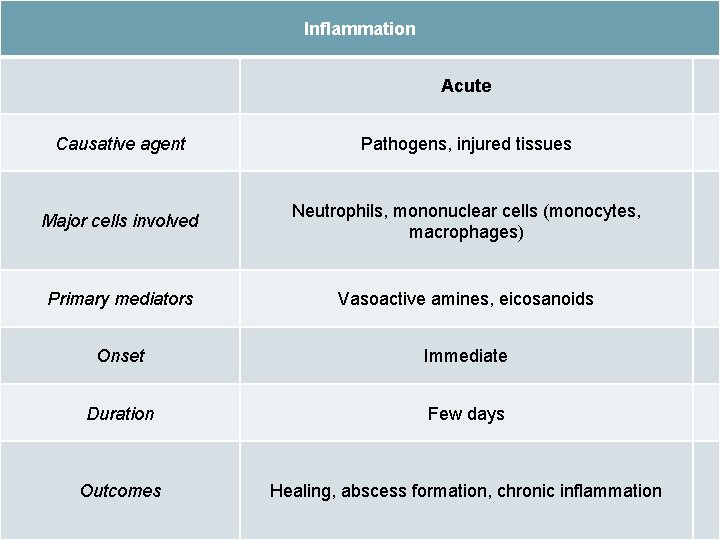
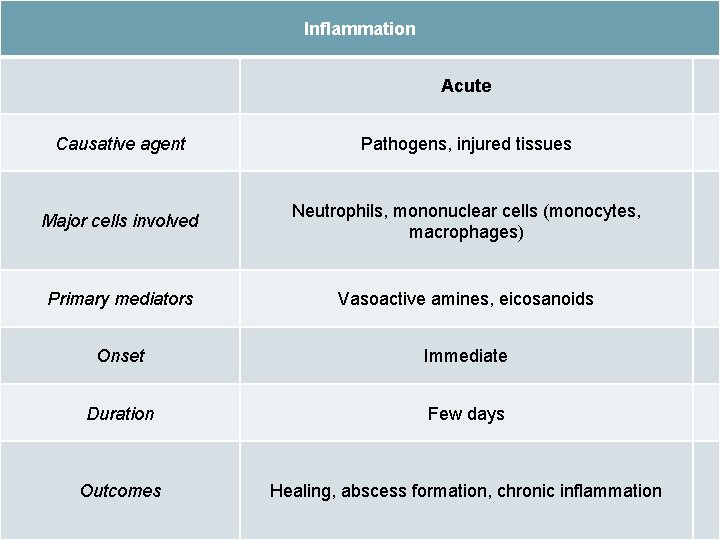
Inflammation Acute Causative agent Pathogens, injured tissues Major cells involved Neutrophils, mononuclear cells (monocytes, macrophages) Primary mediators Vasoactive amines, eicosanoids Onset Immediate Duration Few days Outcomes Healing, abscess formation, chronic inflammation
 Base excision repair
Base excision repair Mismatch repair
Mismatch repair Comprehensive approach to retaining employees
Comprehensive approach to retaining employees Comprehensive approach to retaining employees
Comprehensive approach to retaining employees Comprehensive primary health care definition
Comprehensive primary health care definition Virtual circuit approach
Virtual circuit approach Tony wagner's seven survival skills
Tony wagner's seven survival skills Theoretical models of counseling
Theoretical models of counseling Waterfall and shower approach
Waterfall and shower approach Multiple approach avoidance
Multiple approach avoidance Bandura's reciprocal determinism
Bandura's reciprocal determinism Process of research definition
Process of research definition Traditional approach to systems implementation
Traditional approach to systems implementation Missouri counseling lessons
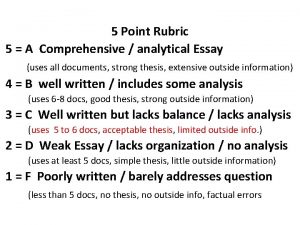
Missouri counseling lessons 5 point rubric for essay
5 point rubric for essay What is continuous and comprehensive evaluation
What is continuous and comprehensive evaluation Conclusion of continuous and comprehensive evaluation
Conclusion of continuous and comprehensive evaluation Missouri school counselor association
Missouri school counselor association Exonucleolytic proofreading
Exonucleolytic proofreading Power brake system
Power brake system Modified macpherson strut
Modified macpherson strut Pressure regulator
Pressure regulator Chapter 44 automotive wiring and wire repair
Chapter 44 automotive wiring and wire repair Bus garage repair dfd
Bus garage repair dfd Faa form 337 example
Faa form 337 example Pedal reserve distance
Pedal reserve distance Automotive maintenance and light repair answer key
Automotive maintenance and light repair answer key Repair and restoration theory of sleep
Repair and restoration theory of sleep Rrr of water bodies
Rrr of water bodies Repair theory of sleep
Repair theory of sleep Writing a comprehensive report in special education
Writing a comprehensive report in special education Comprehensive science major
Comprehensive science major Comprehensive care plan
Comprehensive care plan Wa.portal.cambiumast.com
Wa.portal.cambiumast.com Staxi-2 c/a
Staxi-2 c/a Comprehensive research definition
Comprehensive research definition Statement of other comprehensive income
Statement of other comprehensive income Comprehensive exams
Comprehensive exams Remedial teaching
Remedial teaching Penilaian klinis adalah
Penilaian klinis adalah School counseling responsive services
School counseling responsive services Statement of comprehensive income btec business
Statement of comprehensive income btec business Exploring microsoft office excel 2016 comprehensive
Exploring microsoft office excel 2016 comprehensive Diagnosing groups and jobs
Diagnosing groups and jobs Drdp comprehensive view
Drdp comprehensive view Ctopp-2 subtest descriptions
Ctopp-2 subtest descriptions Ctoni-2
Ctoni-2 Comprehensive safety analysis
Comprehensive safety analysis Explain in detail comprehensive interventions
Explain in detail comprehensive interventions Comprehensive classroom management
Comprehensive classroom management Comprehensive problem 1 part 8
Comprehensive problem 1 part 8