Pancreas Anatomy Acute Pancreatitis Chronic Pancreatitis Pancreatic Neoplasm

- Slides: 41
Pancreas Anatomy Acute Pancreatitis Chronic Pancreatitis Pancreatic Neoplasm Hanna Tahmasebi Sagharlou
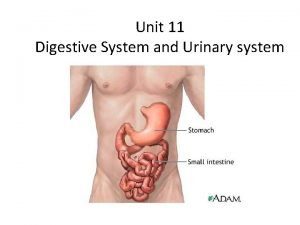
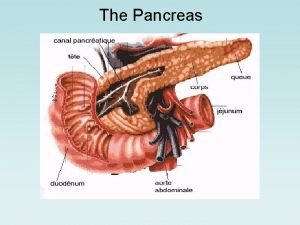
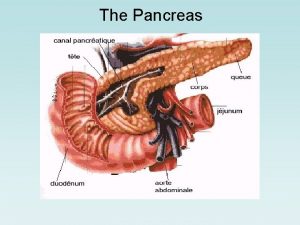
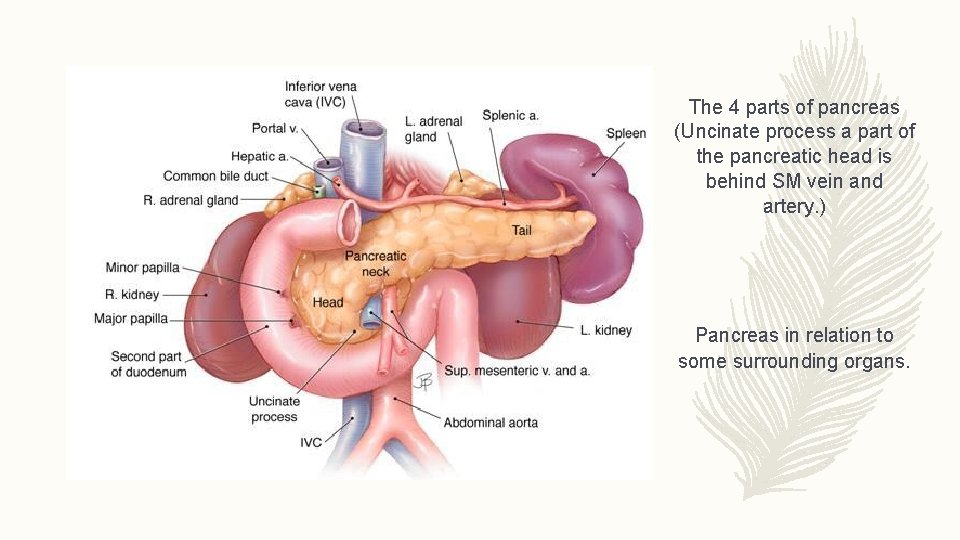
Anatomy overview • A gland with both endocrine and exocrine function present in all vertebrates. • Situated in the retro peritoneum (tail excluded) in level of the 2 nd lumbar vertebrae. • 15 -25 cm long. • Weights about 60 -100 g. • 4 parts: head, neck, body and tail ( some say 3). • Blood supply from many major arteries. • Inervation by vagus nerve and plexuses around its arteries • Venous drainage into splenic, SMV and portal veins. • Lymphatic drainage to pancreaticoduodenal and pancreaticosplenic nodules. • Lacks capsule, inflammation can spread quite fast to the immediate vicinity of the pancreas.
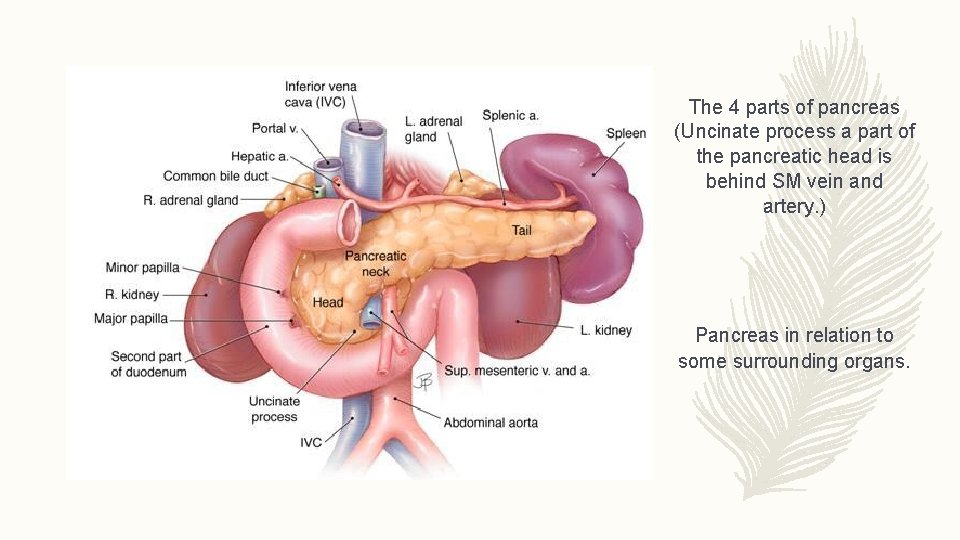
The 4 parts of pancreas (Uncinate process a part of the pancreatic head is behind SM vein and artery. ) Pancreas in relation to some surrounding organs.
Head of Pancreas • Approximately 2 -3 cm. • Include Unicate process. • Attached to the 2 nd and 3 rd parts of duodenum on the right , and on the left it emerges into the neck. • The border between the head and neck is at the insertion of gastroduodenal artery. • Superior and inferior pancreatoduodenal artery anastomose between duodenum and the left border of pancreas.
Neck of Pancreas • 2. 5 cm in length. • At the anterosuperior surface we find the pylorus. • Superior mesenteric vessels emerge from its inferior border. • Behind the neck, Superior mesenteric artery join with Splenic vein to form Portal vein.
Body of pancreas • Elongated, long structure • Anterior surface is separated from stomach by lesser omentum. • On the posterior surface we can find the aorta, left adrenal gland, renal vessels and upper part of the kidney. • Splenic vein also runs posteriorly to the body of pancreas. • Inferior surface is covered by transverse mesocolon.
Tail of pancreas • Narrow, short segment • Lies at the level of the 12 vertebrae. • Ends within the splenic hilum. • Lies in the splenophrenic ligament. • Anteriorly, it's related to splenic flexure of colon. • May be injured during splenectomy (fistula)
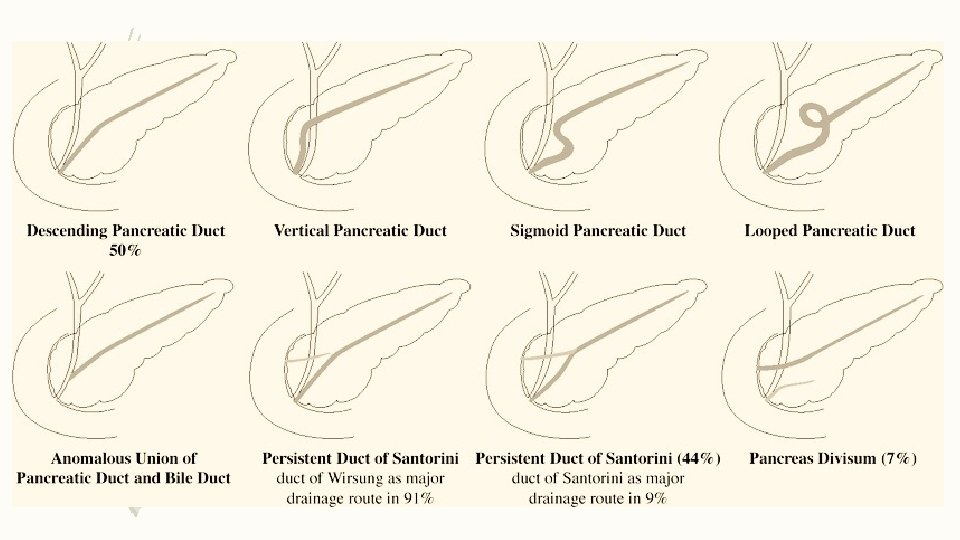
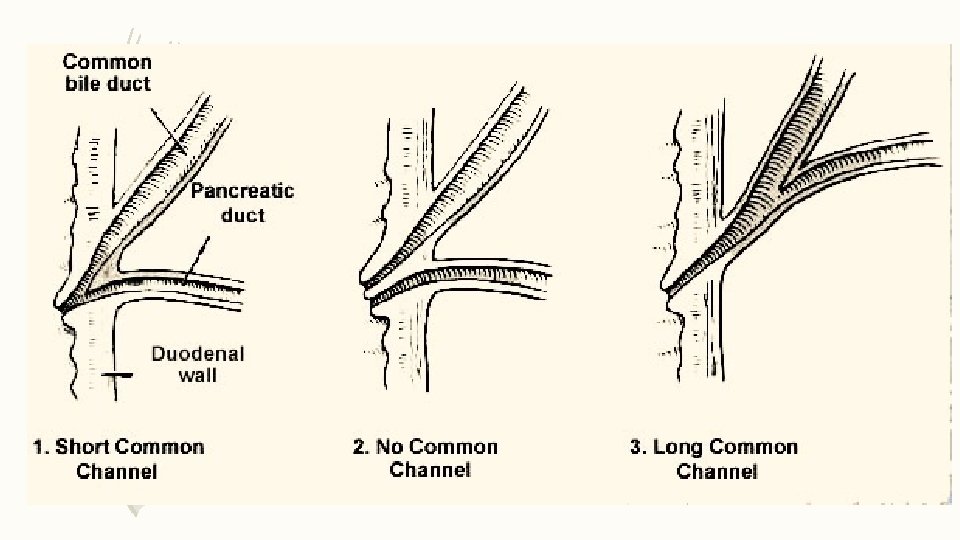
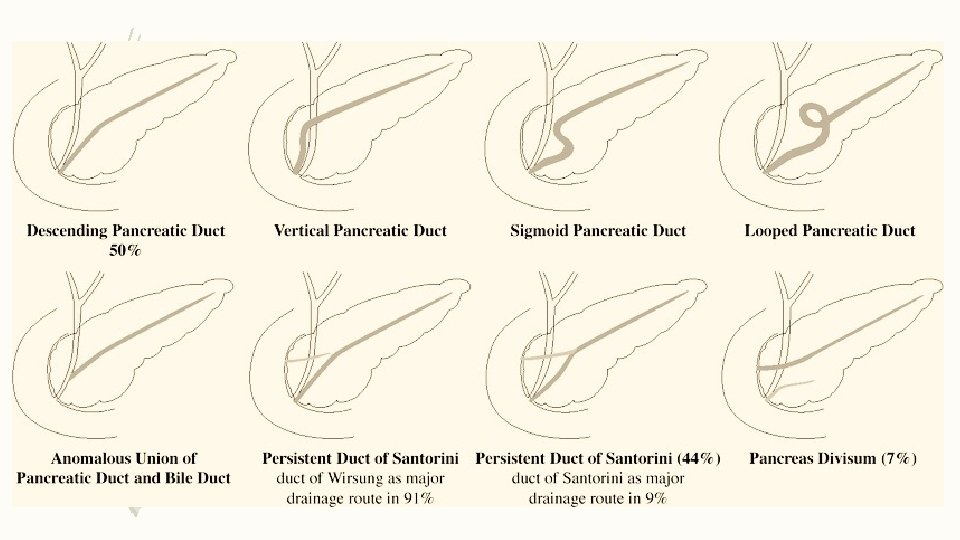
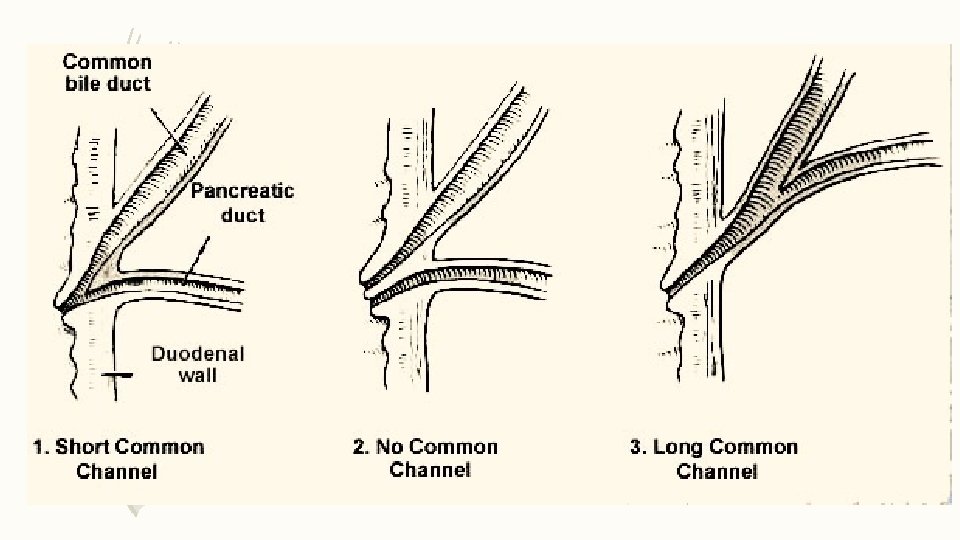
Duct of pancreas • Main duct (Wirsung) runs the entire length of pancreas. • It usually joins the Common bile duct at the ampulla of Vater ( variations do occur). • Around 2 – 4 mm in diameter, with approximately 20 secondary branches • Ductal pressure is higher than in the Common Bile Duct, hus preventing damage to pancreatic duct • Acsessory duct (Santorini) drains superior portion of head and usually empties separately into 2 nd portion of duodenum.
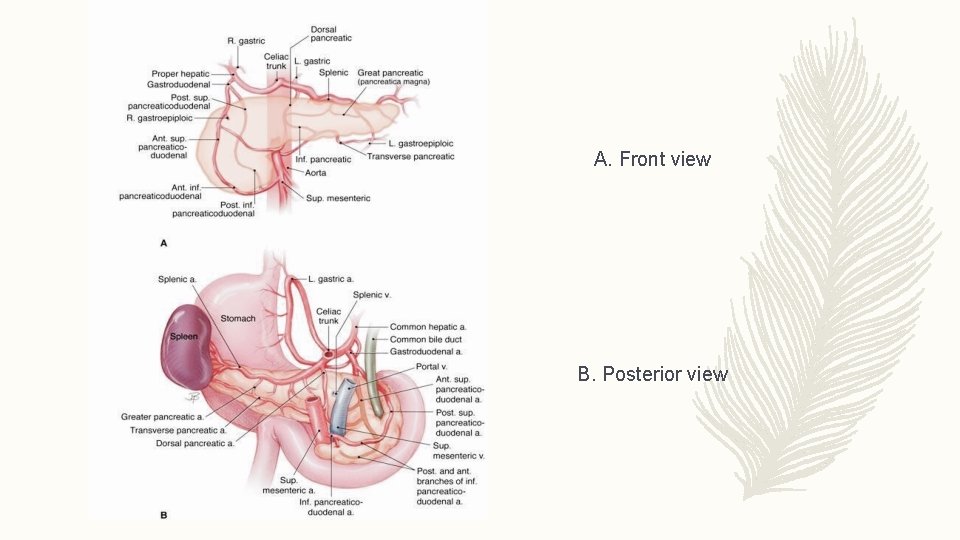
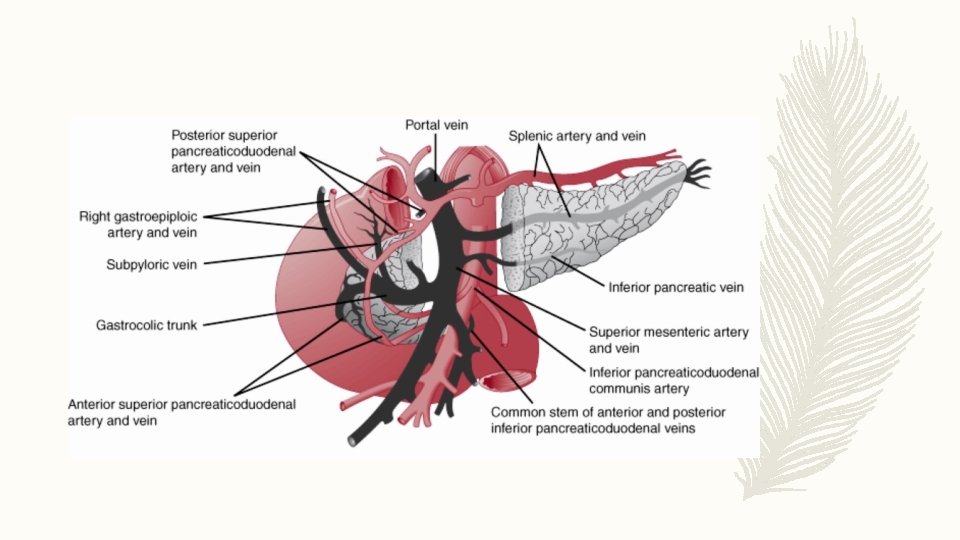
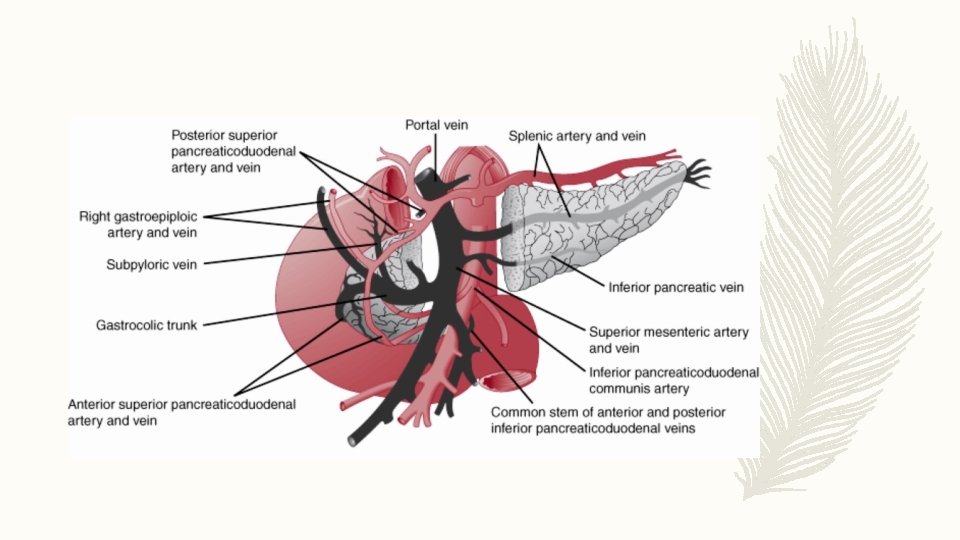
Blood supply • The blood supply of the pancreas is derived from branches of the celiac and superior mesenteric arteries. • The superior pancreaticoduodenal artery arises from the gastroduodenal artery, runs parallel to the duodenum, and eventually meets the inferior pancreaticoduodenal artery, a branch of the superior mesenteric artery, to form an arcade. • The splenic artery provides tributaries that supply the body and tail of the pancreas. The main branches are termed the dorsal pancreatic, pancreatica magna, and caudal pancreatic arteries. • The venous supply of the gland is parallel to the arterial supply. And as said before it is from the splenic , superior mesenteric and portal vein.
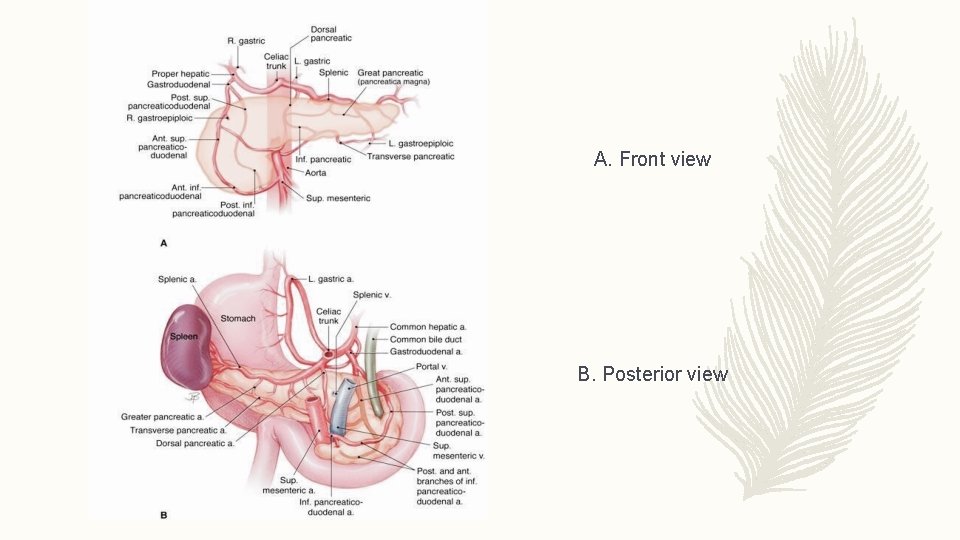
A. Front view B. Posterior view
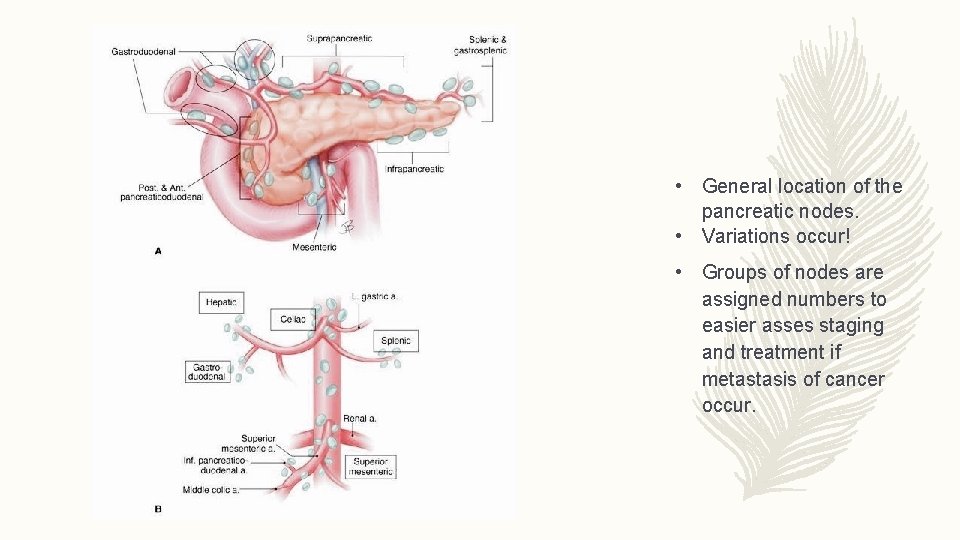
Innervation and lymphatic drainage • The innervation of the pancreas is derived from the vagal and splanchnic nerves. • The efferent fibers pass through the celiac plexus from the celiac branch of the right vagal nerve to terminate in ganglia located in the interlobular septa of the pancreas. Postganglionic fibers from these synapses innervate the acini, the islets, and the ducts. • The visceral afferent fibers from the pancreas also travel in the vagal and splanchnic nerves, but those that mediate pain are confined to the latter. • Sympathetic fibers to the pancreas pass from the splanchnic nerves through the celiac plexus and innervate the pancreatic vasculature • Lymphatic drainage is into the peripancreatic nodes located along the veins.
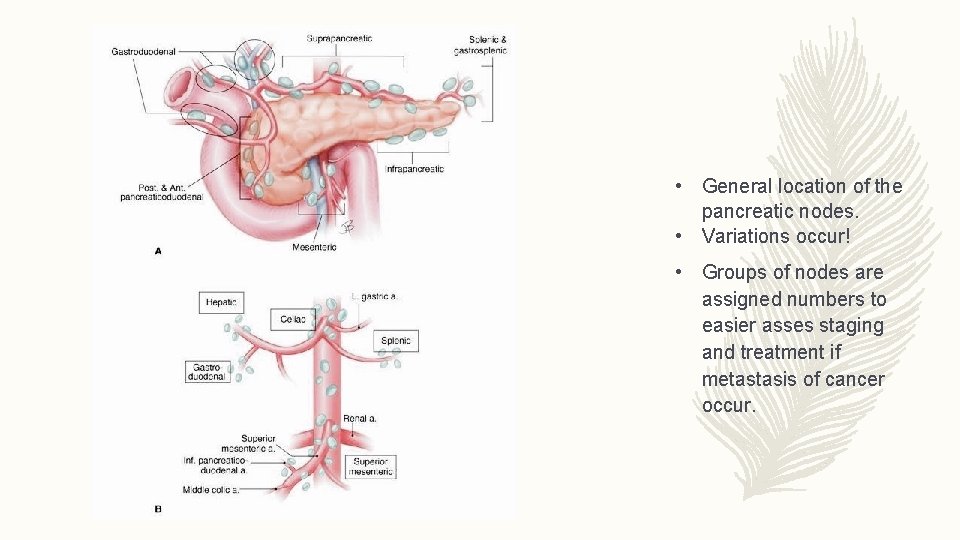
• General location of the pancreatic nodes. • Variations occur! • Groups of nodes are assigned numbers to easier asses staging and treatment if metastasis of cancer occur.
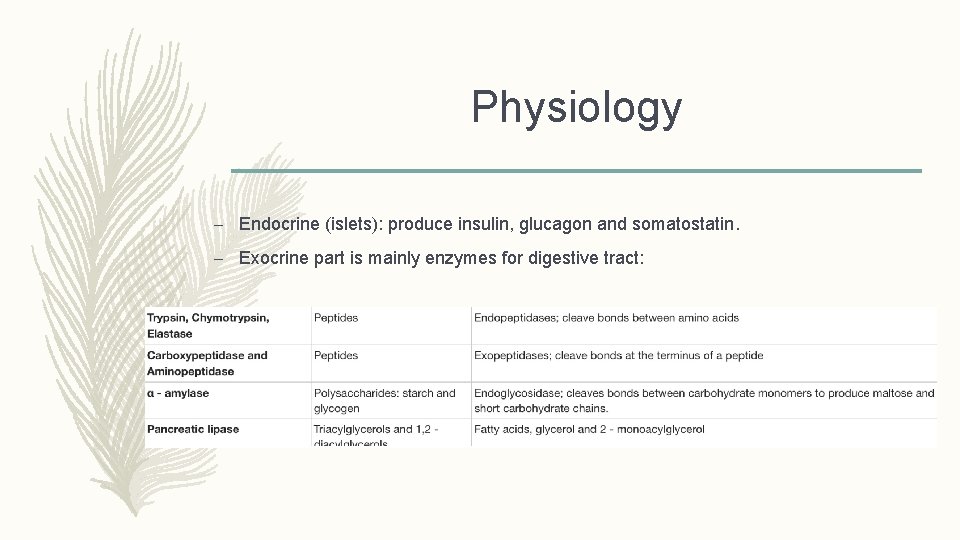
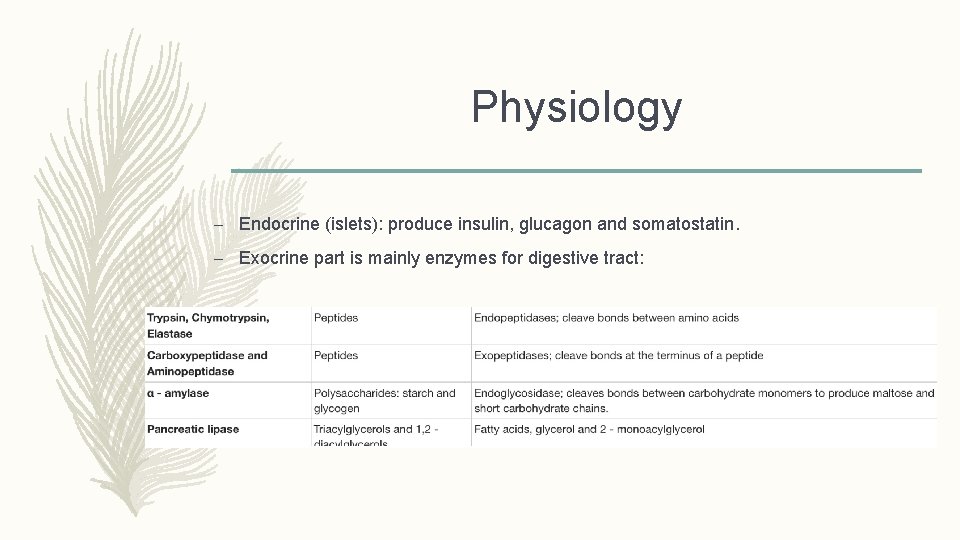
Physiology – Endocrine (islets): produce insulin, glucagon and somatostatin. – Exocrine part is mainly enzymes for digestive tract:
Pancreatitis • Pancreatitis is a inflammatory disease, usually nonbacterial, caused by activation, interstitial liberation, and autodigestion of the pancreas by its own enzymes. • The process may cause permanent morphologic and functional changes. • Much is known about the causes of pancreatitis but understanding of the pathogenesis of this disorder is still incomplete in some cases.
Acute Pancreatitis: Causes • Most common causes are: Alcohol, Gallstones (80% together), and idiopathic. • Realatively common causes: Metabolic disorders (hereditary pancreatitis, hypercalcemia, hyperlipidemia, malnutrition), Post-ERCP, Abdominal trauma, Penetrating ulcers, Carcinoma of the head of pancreas, and other cancer, Drugs, Infections (specially viral, eg. mumps, viral hepatitis), Structural abnormalities (pancreas divisum and autoimmune pancreatitis. • The mnemonic GETSMASHED is often used to remember the common causes of Pancreatitis: G—Gall stones E—Ethanol T—Trauma S—Steroids M—Mumps A—Autoimmune Pancreatitis S—Scorpion sting H—Hyperlipidaemia, Hypothermia, Hyperparathyroidism E—Endoscopic retrograde cholangiopancreatography D—Drugs commonly azathioprine, valproic acid • - Less common causes may be fat necrosis, pregnancy, other viral infections than mumps ( eg varicella zoster) etc.
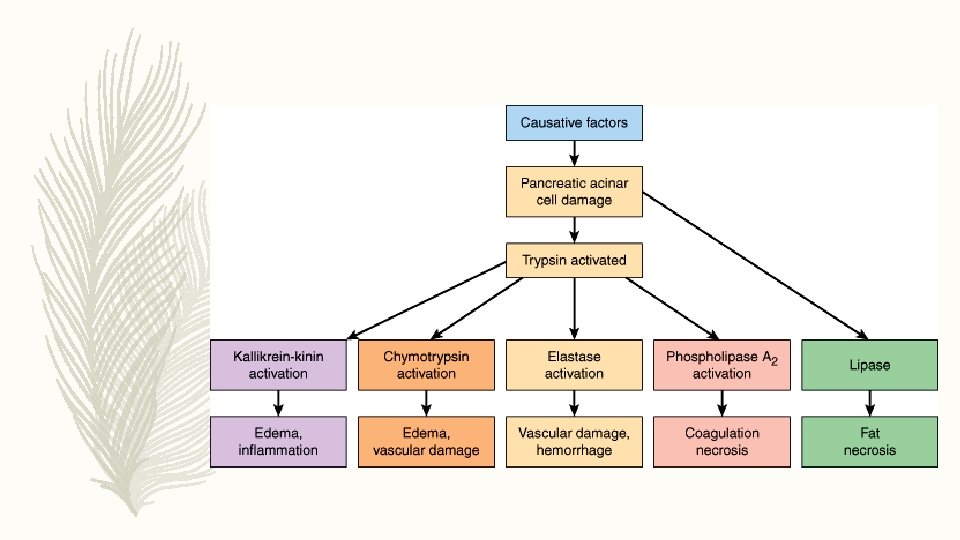
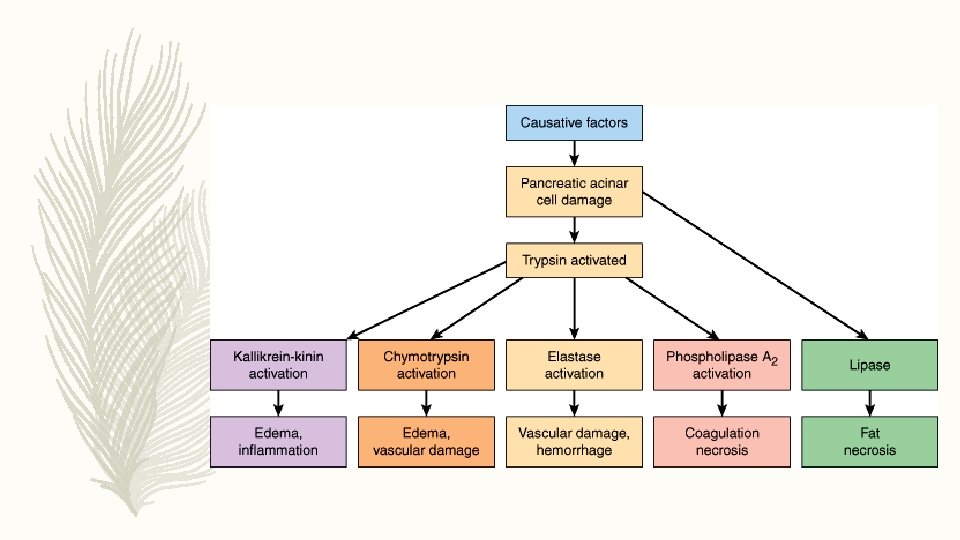
Acute Pancreatitis: Pathogenesis • There are mainly two types of pancreatitis, mild and severe. These are separated based on the predominant cell response. In mild pancreatitis it is inflammation restricted to the pancreas and in severe type it is necrosis with some secondary damage to extra pancreatic tissues/organs. E. g. Saponification of the surrounding fatty tissue. • Both types are to abnormal inhibition, activation or secretion of the zymogens (proenzymes) produced by the pancreas. • Normally the pancreas protects itself from autodigestion by following mechanisms: producing inactive proenzymes, low ph and calcium levels in the storage granules that prevent premature activation, proteolytic inhibitors and a feedback system that limit excessive enzyme activation. • Initiation of acute pancreatitis may occur when factors involving maintaining homeostasis fails. It may be anything that cause injury of the acinar cells, impair the secretion of zymogens granules or inappropriate enzyme activation. • Ones this cellular injury pattern is initiated following destructive events take place: lysosomal and zymogen granules fuse and enables conversion of trypsinogen to trypsin -> trypsin triggers zymogen activation cascade -> inappropriate enzyme activation -> autodigestion. • Secretory vesicles may migrate to the interstitium where the molecular fragments produced by the enzymes may act as chemo attractants for inflammatory cells. Neutrophils exacerbate the problem by releasing superoxide (causing respiratory burst) and/or proteolytic enzymes (cathepsins, collagenase, elastase etc). Macrophages release cytokines that further provoke systemic and local inflammatory responses. The most important that we know today are TNF-a, IL-6, IL-8 och IL-1.
Cytokine storm • These may cause something known as a cytokine storm with is responsible for most of the systemic signs seen during the disease. • The symptoms include: high fever, edema and redness, loss of appetite, vomiting, extreme fatigue and tachycardia. • If the situation progress SIRS, DIC, sepsis, ARDS, myocardial depression, renal insufficiency and gastric stress ulcer, hemodynamics instability including shock, peritonitis is some of the possible complications that may happen.
Local signs/ symptoms • Local signs are severe epigastric pain (cardinal sign !)which can be located on left or right depending on which part of the pancreas that is affected. Pain is usually of sudden onset after a meal and may radiate to the back. A supine position may relive the pain. This + vomiting and nausea, elevated serum or urinary amylase +tachycardia + risk factor is usually enough to diagnose acute pancreatitis. Assessment of severity and cause must still be done! • There also some signs which are less common and more characteristic of a severe disease: The Cullen sign is a bluish discoloration around the umbilicus resulting from hemoperitoneum The Grey-Turner sign is a reddish-brown discoloration along the flanks resulting from retroperitoneal blood dissecting along tissue planes; more commonly, patients may have a ruddy erythema in the flanks secondary to extravasated pancreatic exudate Erythematous skin nodules may result from focal subcutaneous fat necrosis; these are usually not more than 1 cm in size and are typically located on extensor skin surfaces; in addition, polyarthritis is occasionally seen.
Diagnosis • Laboratory tests can help establish the severity of the disease and If it affects the function of other organs. • Blood Investigations - Full blood count, Renal function tests, Liver Function, serum calcium, serum amylase and lipase (lipase is considered better by most, but not all studies), Arterial blood gas, Trypsin-Selective test. • However CT combined with ultrasonography is considered the golden standard.
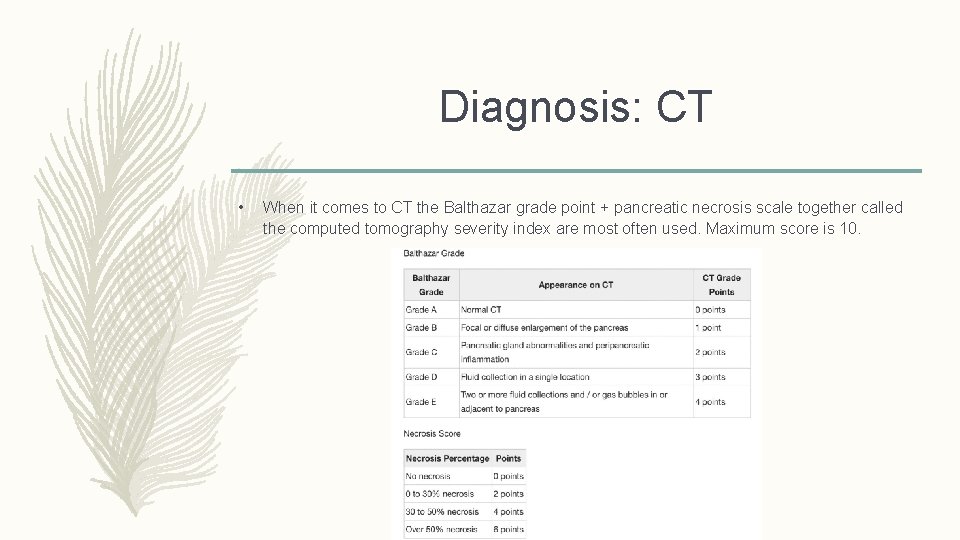
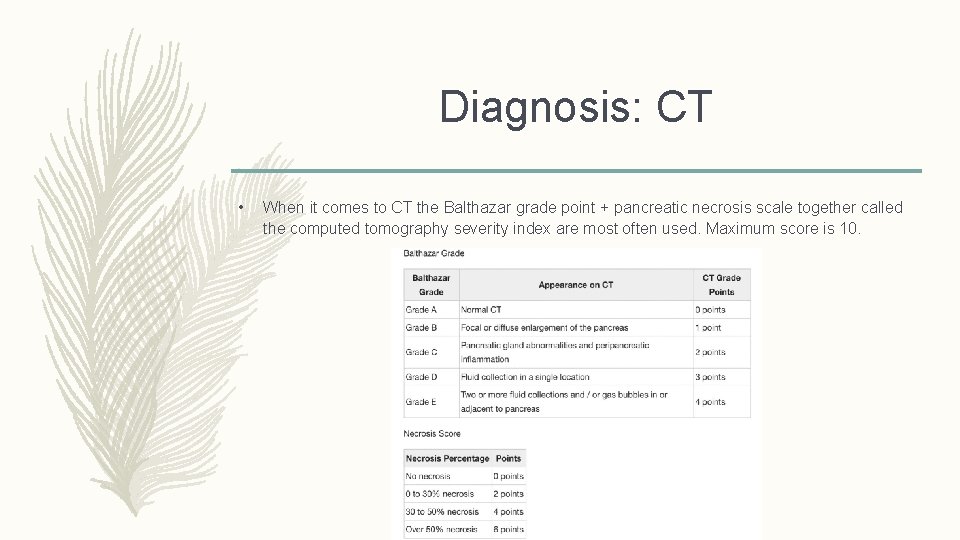
Diagnosis: CT • When it comes to CT the Balthazar grade point + pancreatic necrosis scale together called the computed tomography severity index are most often used. Maximum score is 10.
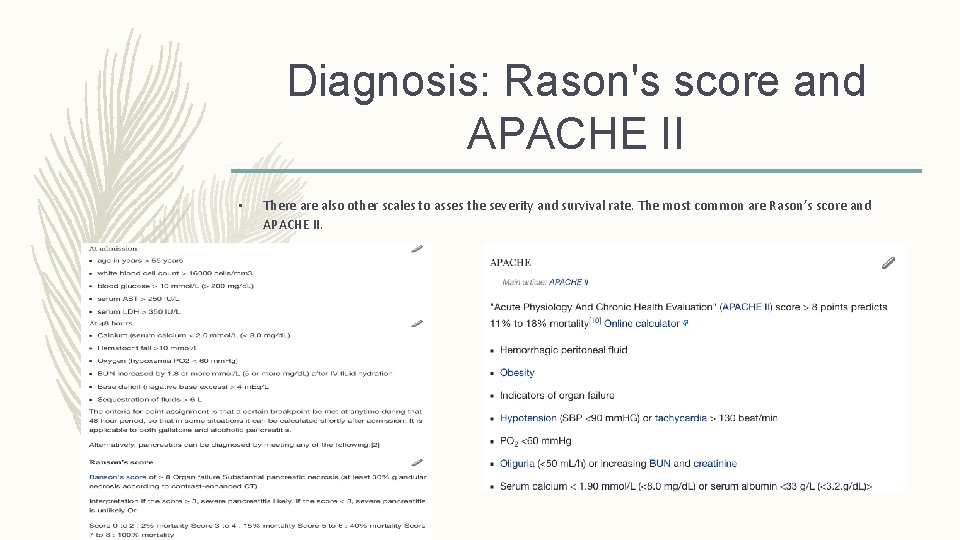
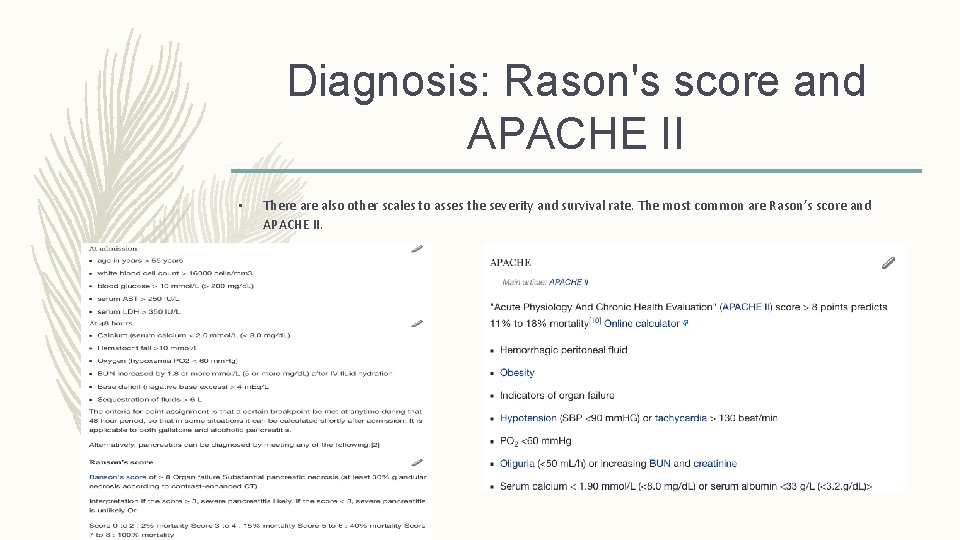
Diagnosis: Rason's score and APACHE II • There also other scales to asses the severity and survival rate. The most common are Rason’s score and APACHE II.
Treatment • The chocie of treatment depends on severity of the disease, condition of the patient, comorbidities and on any other that may have already occurred (eg. Infections). • One of the primary therapies for acute pancreatitis is adequate early fluid resuscitation, especially within the first 24 hours of onset. Pancreatitis is associated with a lot of swelling and inflammation. Giving fluids intravenously prevents dehydration and ensures that the rest of the organs of the body get adequate blood flow to support the healing process. Usually saline or ringers formula is given. • Initially, the patient is kept NPO (nil per os—that is, nothing by mouth) so no nutrition is given to rest the pancreas and bowels during the first 24 to 48 hours. After 48 hours, a plan to provide nutrition should be implemented because acute pancreatitis is a highly active state of inflammation and injury that requires a lot of calories to support the healing process. • Medication for pain and nausea is also given- but these symptoms usually relieves as the inflammations is reduced. There are some controversies about using morphine as pain reliever since it constricts the sphincter of Oddi which may worsen the problem. • In addition to providing supportive care, underlying causes need to be promptly evaluated. For example, if the cause is gallstones, medication, high triglycerides, or high calcium levels within the patient’s body , directed therapy can be given.
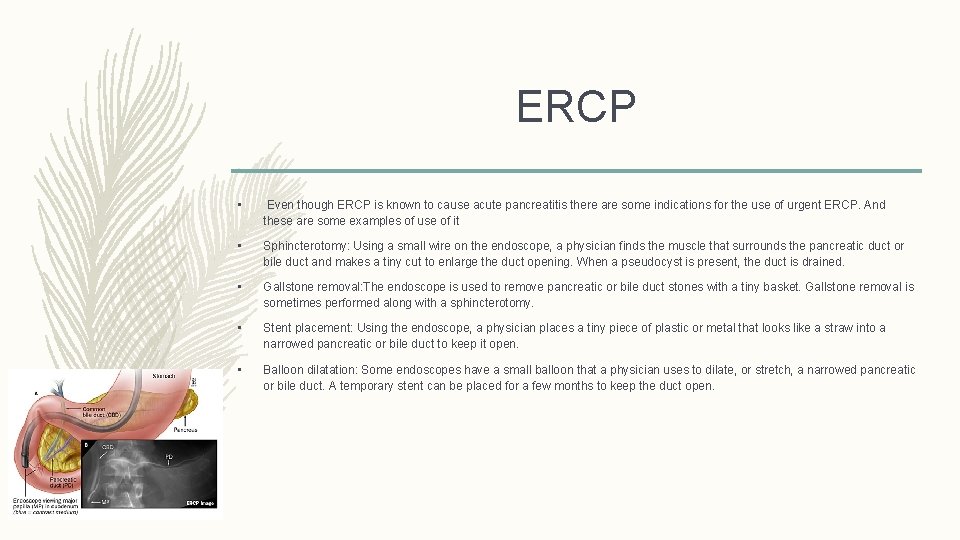
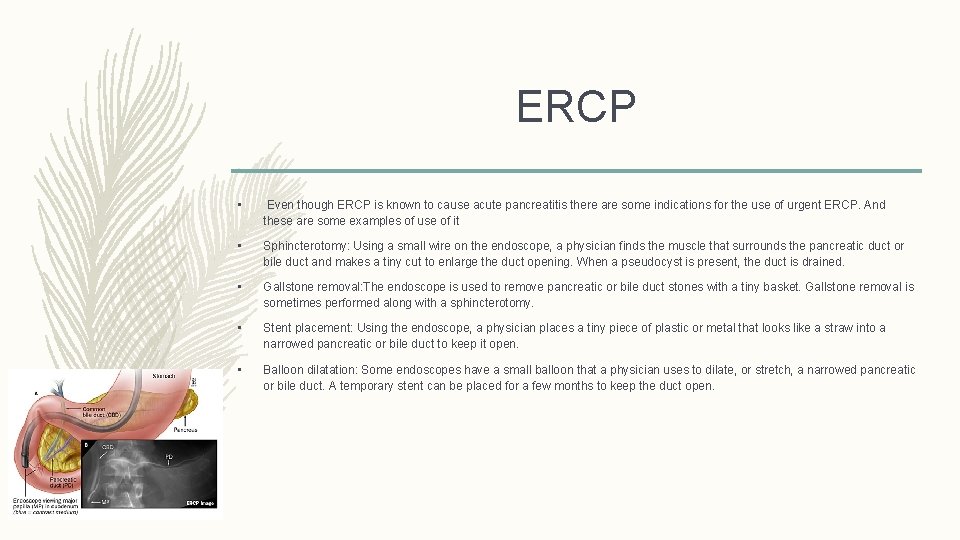
ERCP • Even though ERCP is known to cause acute pancreatitis there are some indications for the use of urgent ERCP. And these are some examples of use of it • Sphincterotomy: Using a small wire on the endoscope, a physician finds the muscle that surrounds the pancreatic duct or bile duct and makes a tiny cut to enlarge the duct opening. When a pseudocyst is present, the duct is drained. • Gallstone removal: The endoscope is used to remove pancreatic or bile duct stones with a tiny basket. Gallstone removal is sometimes performed along with a sphincterotomy. • Stent placement: Using the endoscope, a physician places a tiny piece of plastic or metal that looks like a straw into a narrowed pancreatic or bile duct to keep it open. • Balloon dilatation: Some endoscopes have a small balloon that a physician uses to dilate, or stretch, a narrowed pancreatic or bile duct. A temporary stent can be placed for a few months to keep the duct open.
Surgery • If one were to have severe acute pancreatitis (necrotizing pancreatitis). It is important to remember that in some cases, this dead tissue can become a source of infection. When infection is suspected, diagnosis can be made by needle biopsy, and if confirmed, medical treatment with antibiotics is required along with consideration of drainage or surgical recesction of those parts. • Also as I mentioned before there is an increase of cytokines which one must take into account before performing surgery. Waiting approximately one week or/and give anticytokine therapy during this time to reduce the cytokine levels is ideal but maybe not always possible.
Chronic pancreatitis • Chronic pancreatitis is characterized by irreversible change. It can present as episodes of acute inflammation in a previously injured pancreas, or as chronic damage with persistent pain or malabsorption. • Patient often have persistent abdominal pain and steatohrrea due to impairment of fat digestion. • Diabetes can is also a common finding due to damage of the islets. • Weight loss and malnutrition can be found in patient with a long time disease.

Causes/ Risk Factors The correlation between risk/ causes and chronic inflammation is hard because it's very variable in nature. However following things are strongly connected with the disease. • Alcohol • Smoking • Malnutrition • Trypsinogen, and inhibitory protein defects • Cystic fibrosis • Idiopathic (unknown) • Trauma • Hypercalcemia • Calcific stones.
Diagnosis • Diagnosis is mainly based on structure and function of pancreas. • Direct biopsy is generally considered excessively risky. • Laboratory tests: Serum amylase and lipase – hard to interpret. May be increased or normal/low if pancreatic function is reduced. Secretin is the golden standard but not commonly used clinically. Bicarbonate production Fecal elastase • Imaging (calcifications and altered density) : CT, MRI, US, X-ray
Treatment • Treatment is usually directed to the cause of the pancreatitis as well as supportive • Diet – low fat and proteins • Pancreatic enzyme replacement – decrease malabsorption, insulin etc. • Pain relieve • Resection and drainage and endoscopic procedures • Transplantation.
Pancreatic tumors • About 85 percent of tumors in pancreas are adenocarcinoma with a poor prognosis. The remaining 15% are usually either benign (adenomas mostly) or non- malignant neoplasms like : • cystic tumors or neoplasms including mucinous cystadenoma and serous cyst adenoma • islet cell tumors also called neuroendocrine tumors • papillary cystic neoplasms • lymphoma of the pancreas • acinar cell tumors of the pancreas • metastatic tumors to the pancreas
Symptoms • Malignant tumors often has a poor prognosis, even when diagnosed early. The 5 year survival rate is at best around 10% in case of adenocarcinoma. . Pancreatic cancer typically spreads rapidly and is seldom detected in its early stages, which is a major reason why it's one of the leading causes of cancer mortality. • Symptoms that finally arise is related to the mass effect, tissue destruction, functional loss or overexpression and cahexia for example: Upper abdominal pain that may radiate to your back Yellowing of your skin and sclera (jaundice) Loss of appetite and prostprandial vomiting Weight loss Depression Blood clots Enzyme related symptoms.
Causes/ Risk Factors • Excess body weight • Chronic inflammation of the pancreas (pancreatitis) • Diabetes • Family history of genetic syndromes that can increase cancer risk, including a BRCA 2 gene mutation, Lynch syndrome and familial atypical mole-malignant melanoma (FAMMM). • Gallstones • Personal or family history of pancreatic cancer • Smoking
Diagnosis • Diagnosis is based on imaging techniques such as: CT MRI EUS ( endoscopic ultrasound), ERCP or/and biopsy. • One tumor marker test used in pancreatic cancer is called CA 19 -9. But the test isn't always reliable, and it isn't clear how best to use the CA 19 -9 test results.
Staging After diagnosis Staging must be done to choose appropriate treatment • Stage I. Cancer is confined to the pancreas. • Stage II. Cancer has spread beyond the pancreas to nearby tissues and organs and may have spread to the lymph nodes. • Stage III. Cancer has spread beyond the pancreas to the major blood vessels around the pancreas and may have spread to the lymph nodes. • Stage IV. Cancer has spread to distant sites beyond the pancreas, such as the liver, lungs and the lining that surrounds your abdominal organs (peritoneum).
Treatment is based on the stage, symptoms, comorbidities, age. • Surgical resection. • Chemotherapy • Radiation therapy • Palliative treatment: eg. reduce pain, stent may be placed in small intestine to hold it open or bypass surgery may be necessary to attach stomach to a lower point in intestines that isn't blocked by cancer. Insulin may be necessary (and other deficit enzymes).
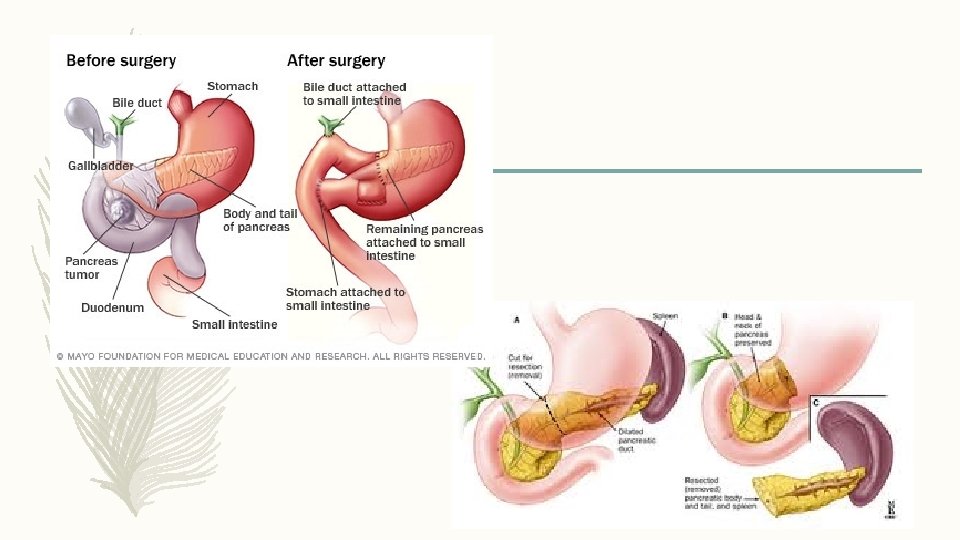
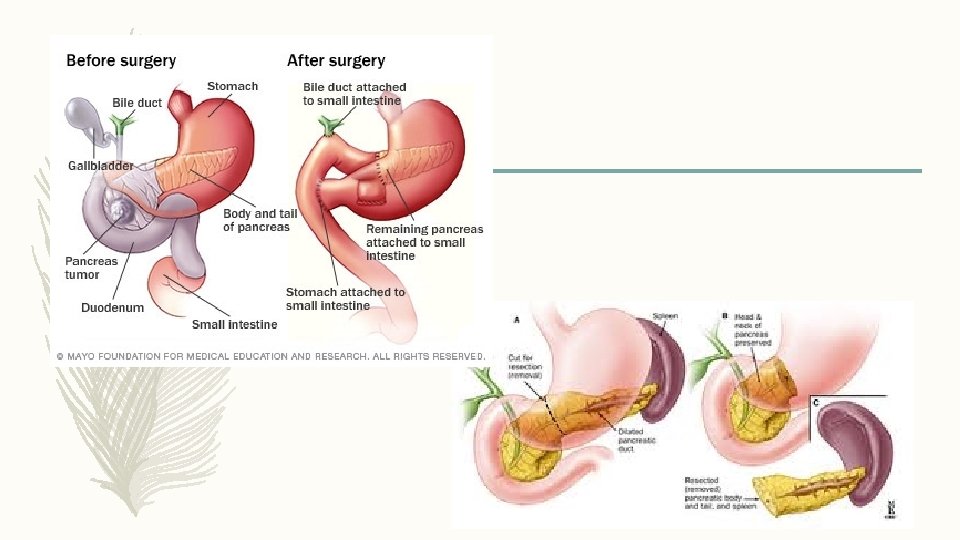
Surgical Techniques • The aim of surgery is to remove the entire tumor while preserving as much of pancreas as possible. • If the tumor is located in the head of pancreas the Whipple procedure can be done. It involves removing the head of pancreas, as well as a portion of duodenum, gallbladder and part of the bile duct. Part of stomach may be removed as well. Remaining parts of pancreas, stomach and intestines are then attached. • Surgery to remove the tail of the pancreas or the tail and a small portion of the body is called distal pancreatectomy • Laparoscopy (usually for benign tumors) • Open surgery
Sources • http: //www. pancreapedia. org/reviews/anatomy-and-histology-of-pancreas • http: //www. surgery. usc. edu/divisions/tumor/pancreasdiseases/web%20 pages/pancreas%20 cancer/surgical%20 tx%20 panc %20 canc. html • http: //www. webmd. com/digestive-disorders/tc/pancreatitis-treatment-overview • https: //www. pancan. org/section-facing-pancreatic-cancer/learn-about-pan-cancer/treatment/surgery/whipple-procedurepancreaticoduodenectomy/ • https: //www. pancreasfoundation. org/patient-information/acute-pancreatitis-risks-and-treatment/ • http: //www. mayoclinic. org/diseases-conditions/pancreatic-cancer/basics/treatment/con-20028153 • http: //www. surgery. usc. edu/divisions/tumor/pancreasdiseases/pancreas%20 cancer%20 overview. html
 Pancreatitis nursing
Pancreatitis nursing Chronic pancreatitis nursing care plan
Chronic pancreatitis nursing care plan Gallstonee
Gallstonee Chronic pancreatitis
Chronic pancreatitis Chronic pancreatitis guideline
Chronic pancreatitis guideline Common chronic and acute conditions chapter 18
Common chronic and acute conditions chapter 18 Periradicular disease classification
Periradicular disease classification Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Morphological types of inflammation
Morphological types of inflammation Acute subacute chronic
Acute subacute chronic Acute vs chronic heart failure
Acute vs chronic heart failure Gallbladder histology drawing
Gallbladder histology drawing Leukemia survival rate
Leukemia survival rate Cellular events of acute inflammation
Cellular events of acute inflammation Ranson
Ranson What activates trypsinogen
What activates trypsinogen Ranson criteria
Ranson criteria Criteria of acute pancreatitis
Criteria of acute pancreatitis Pancreatitis ct grade
Pancreatitis ct grade Acute pancreatitis pes statement
Acute pancreatitis pes statement Acute pancreatitis ct
Acute pancreatitis ct Acute pancreatitis treatment
Acute pancreatitis treatment Apendicolith
Apendicolith Myeloproliferative neoplasm
Myeloproliferative neoplasm Myeloproliferative syndrome
Myeloproliferative syndrome Osteosarcoma femur icd 10
Osteosarcoma femur icd 10 Bronchogenic neoplasm
Bronchogenic neoplasm Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Malignant neoplasm
Malignant neoplasm Plasma cell neoplasm
Plasma cell neoplasm Perdida de polaridad celular
Perdida de polaridad celular Intraductal papillary mucinous neoplasm
Intraductal papillary mucinous neoplasm Excessive and frequent artinya
Excessive and frequent artinya Cystic duct
Cystic duct Anatomy and physiology of pancreas
Anatomy and physiology of pancreas Gastric gland
Gastric gland Pancreas histology slide
Pancreas histology slide Pancreas anatomy
Pancreas anatomy Pancreatic calcification
Pancreatic calcification Carbohydrates in digestion
Carbohydrates in digestion Radiologix verdun
Radiologix verdun Pad sign in pancreatic carcinoma
Pad sign in pancreatic carcinoma