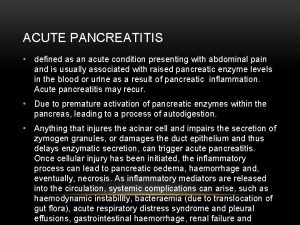
ACUTE PANCREATITIS Dr Prajwala Reddy Definition Acute Pancreatitis

- Slides: 36
ACUTE PANCREATITIS Dr. Prajwala Reddy
Definition � Acute Pancreatitis is an inflammatory process of Pancreas that may be associated with varying degrees of auto digestion, edema, necrosis & hemorrhage of pancreatic tissue. Function: � 1. Exocrine -Insulin production. � 2. Endocrine-Manufacturing and secretion of � digestive enzymes.
Pathophysiology v AP occurs as a consequence of premature activation of Zymogen granules & due to injury to Acinar cells releasing protease which digest the pancreas &the surrounding tissue. v It may occur when factors involved in maintaining cellular homeostasis are out of balance. v The initiating event may be any thing that injures the acinar cells& impairs them(eg : alcohol , gall stones , Drugs , etc. , )
v It is unclear exactly what pathophysiologic event triggers the onset. v Its believed that both extracellular factors& intracellular factors play a role. v In addition AP can develop when ductal cell injury leads to delayed or absent enzymatic secretions , as seen in pts with CRTF gene mutation.
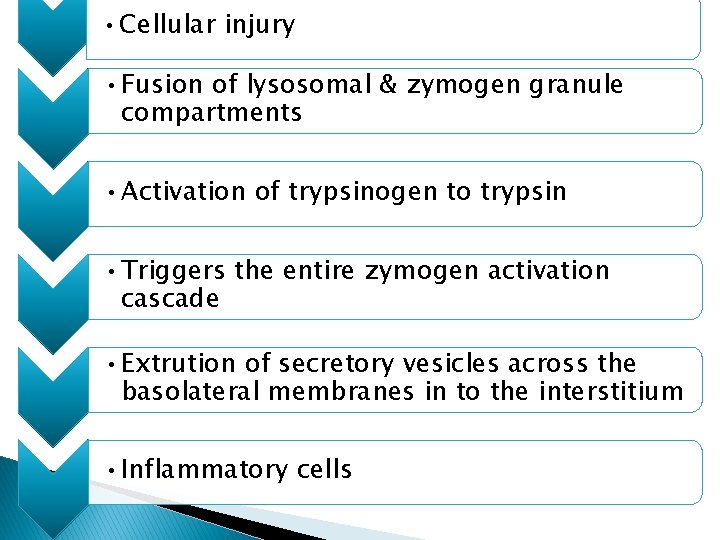
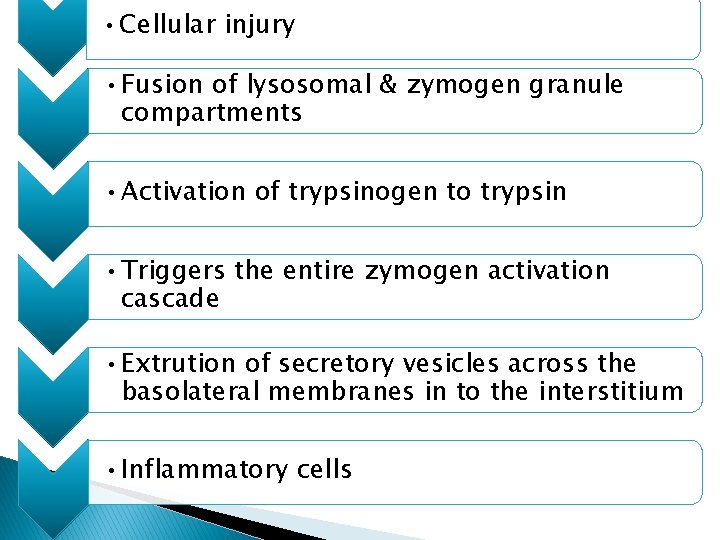
• Cellular injury • Fusion of lysosomal & zymogen granule compartments • Activation of trypsinogen to trypsin • Triggers the entire zymogen activation cascade • Extrution of secretory vesicles across the basolateral membranes in to the interstitium • Inflammatory cells
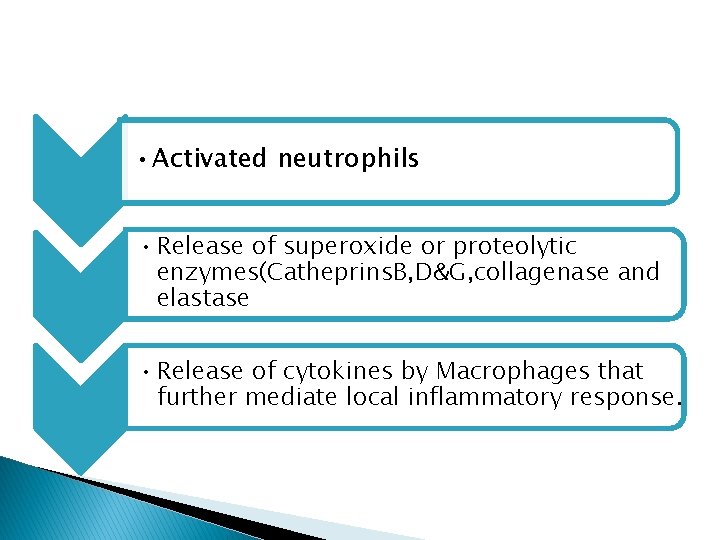
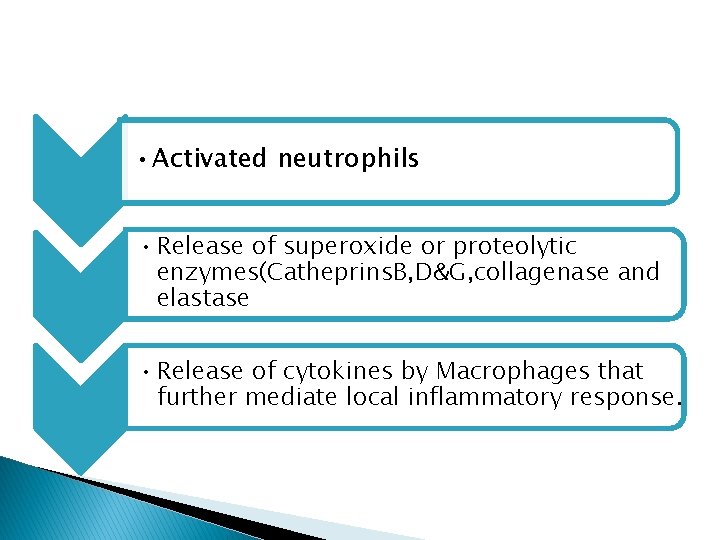
• Activated neutrophils • Release of superoxide or proteolytic enzymes(Catheprins. B, D&G, collagenase and elastase • Release of cytokines by Macrophages that further mediate local inflammatory response.
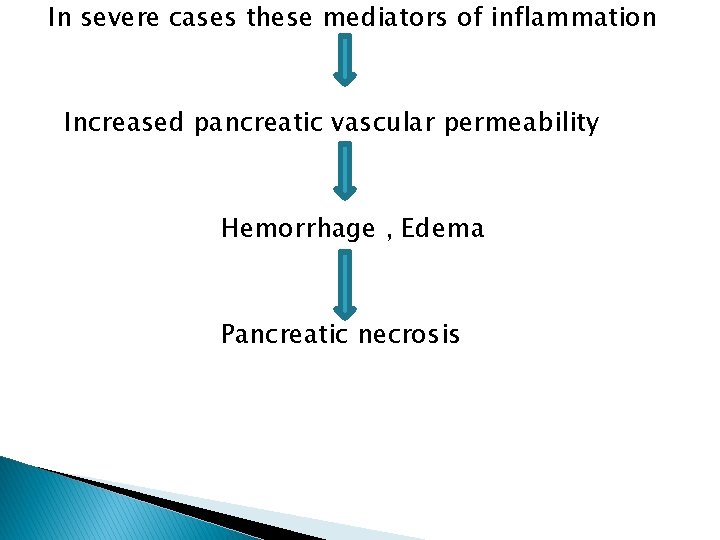
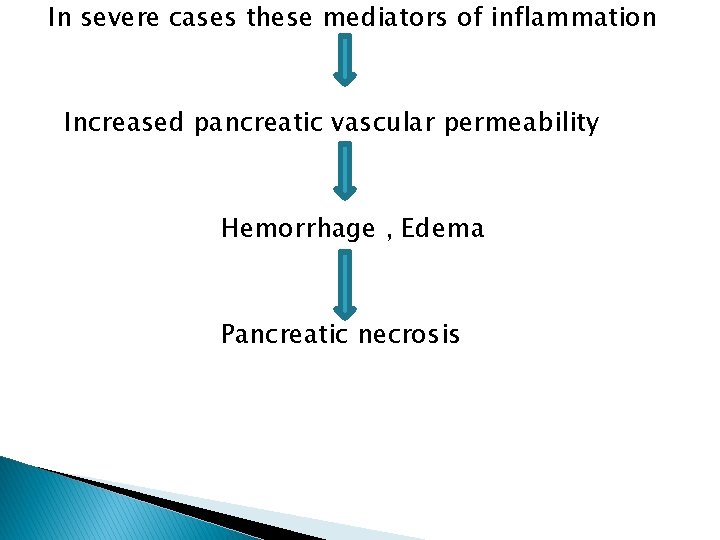
In severe cases these mediators of inflammation Increased pancreatic vascular permeability Hemorrhage , Edema Pancreatic necrosis
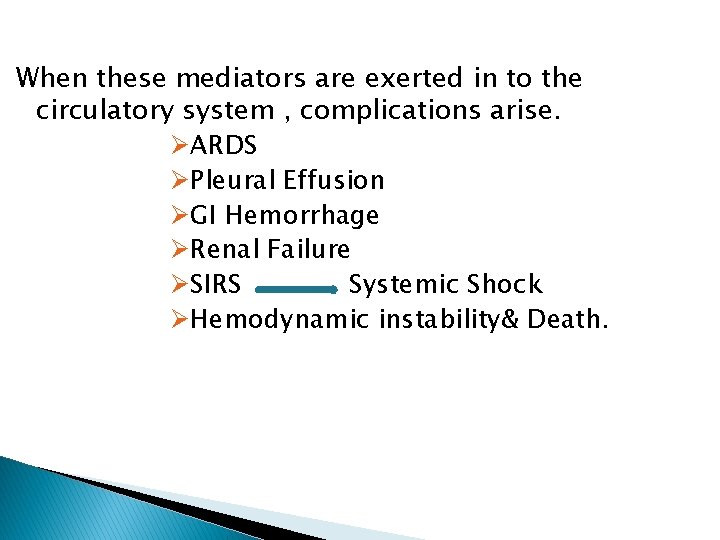
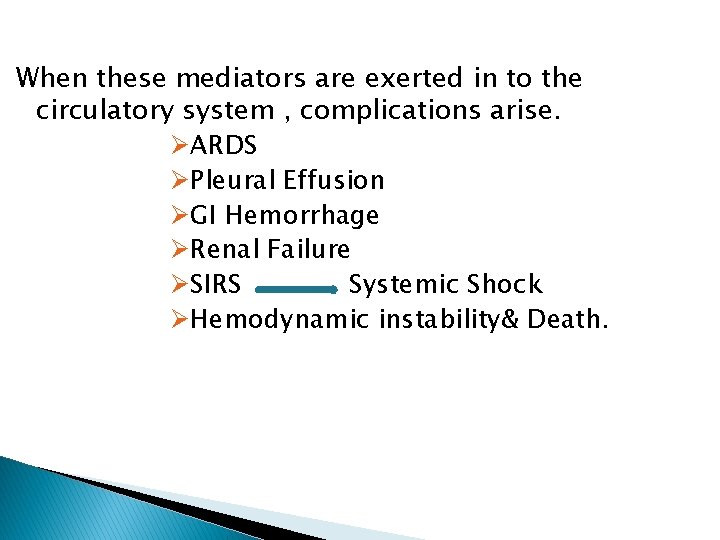
When these mediators are exerted in to the circulatory system , complications arise. ØARDS ØPleural Effusion ØGI Hemorrhage ØRenal Failure ØSIRS Systemic Shock ØHemodynamic instability& Death.
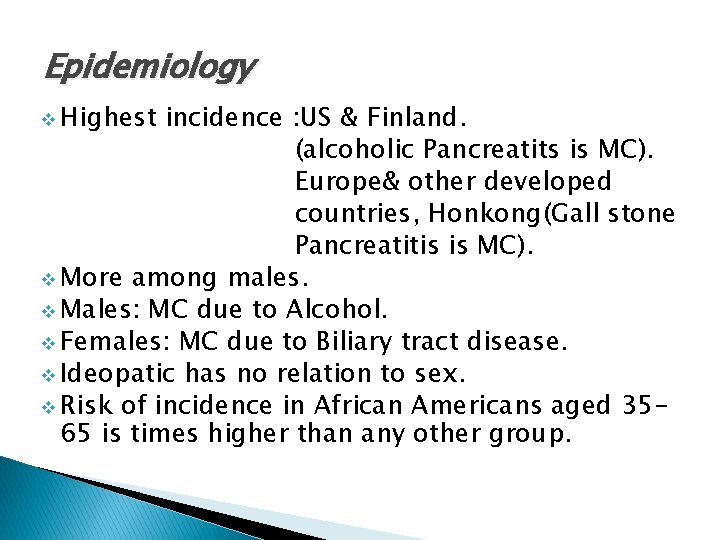
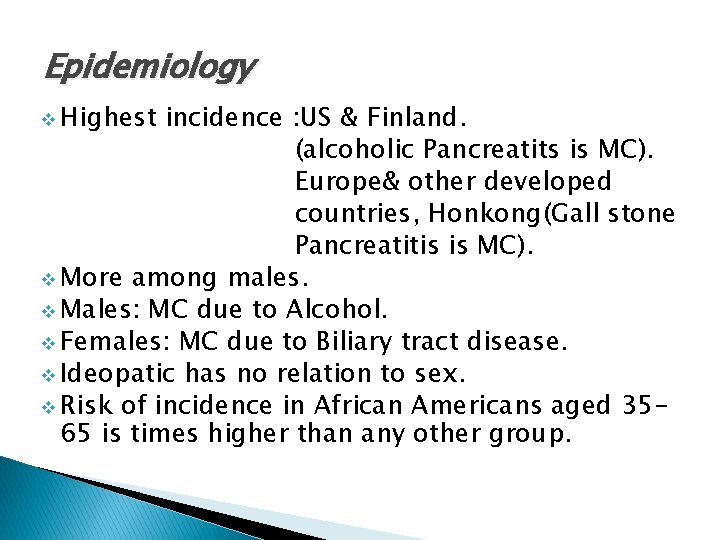
Epidemiology v Highest incidence : US & Finland. (alcoholic Pancreatits is MC). Europe& other developed countries, Honkong(Gall stone Pancreatitis is MC). v More among males. v Males: MC due to Alcohol. v Females: MC due to Biliary tract disease. v Ideopatic has no relation to sex. v Risk of incidence in African Americans aged 3565 is times higher than any other group.
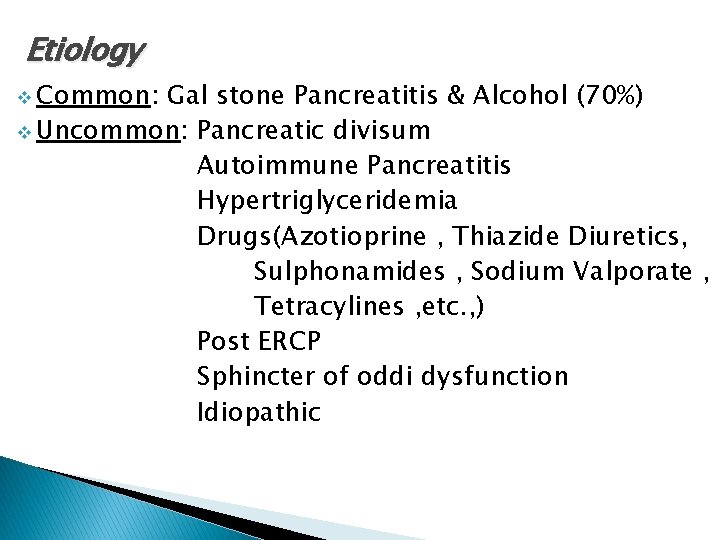
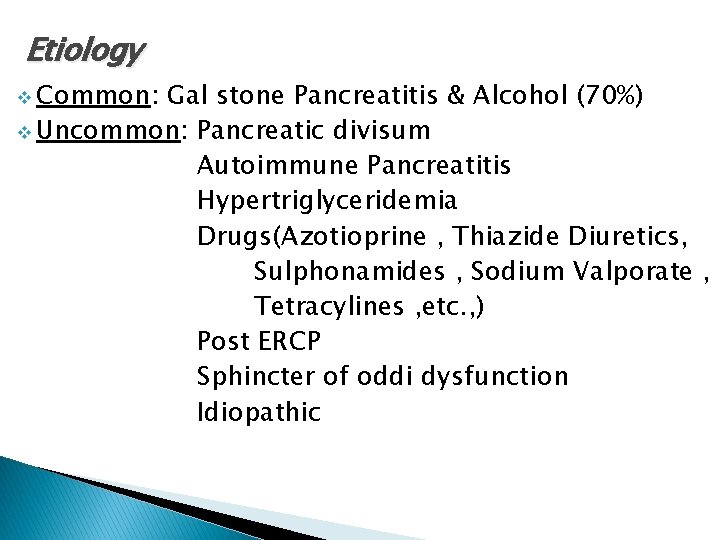
Etiology v Common: Gal stone Pancreatitis & Alcohol (70%) v Uncommon: Pancreatic divisum Autoimmune Pancreatitis Hypertriglyceridemia Drugs(Azotioprine , Thiazide Diuretics, Sulphonamides , Sodium Valporate , Tetracylines , etc. , ) Post ERCP Sphincter of oddi dysfunction Idiopathic
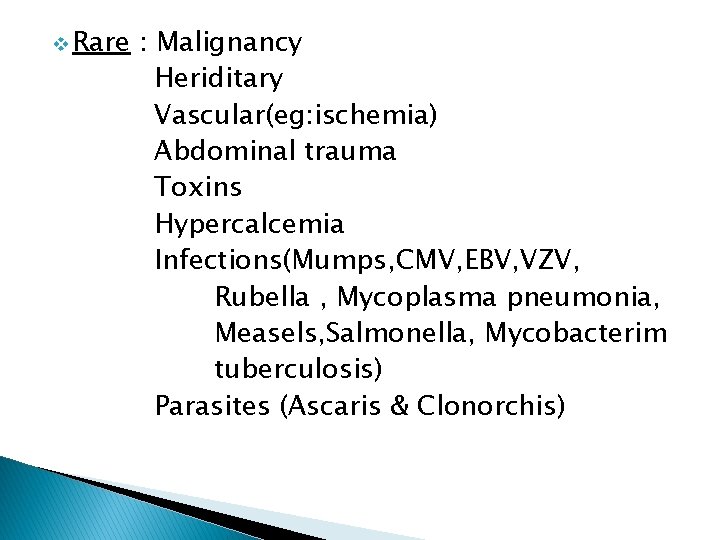
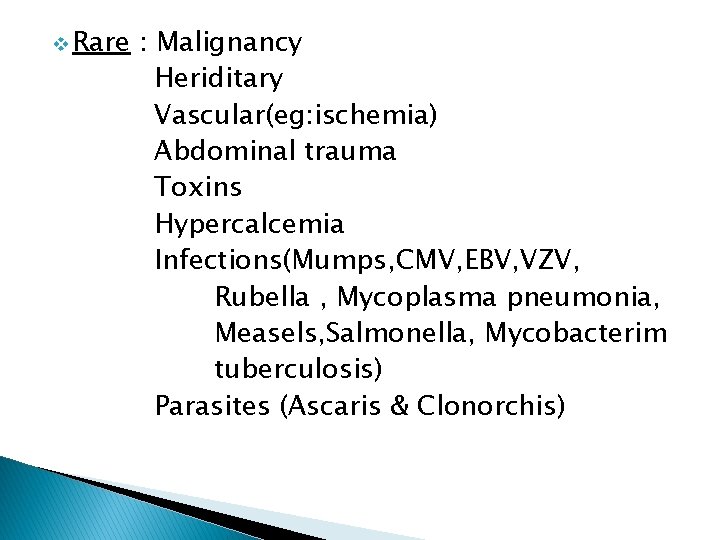
v Rare : Malignancy Heriditary Vascular(eg: ischemia) Abdominal trauma Toxins Hypercalcemia Infections(Mumps, CMV, EBV, VZV, Rubella , Mycoplasma pneumonia, Measels, Salmonella, Mycobacterim tuberculosis) Parasites (Ascaris & Clonorchis)
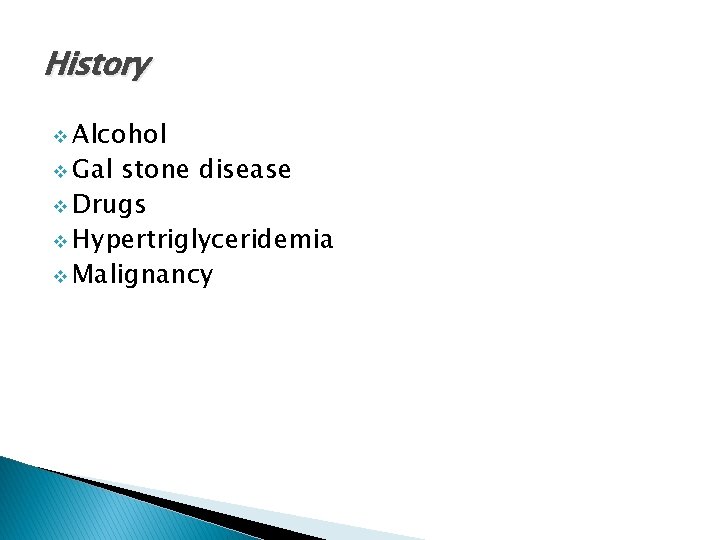
History v Alcohol v Gal stone disease v Drugs v Hypertriglyceridemia v Malignancy
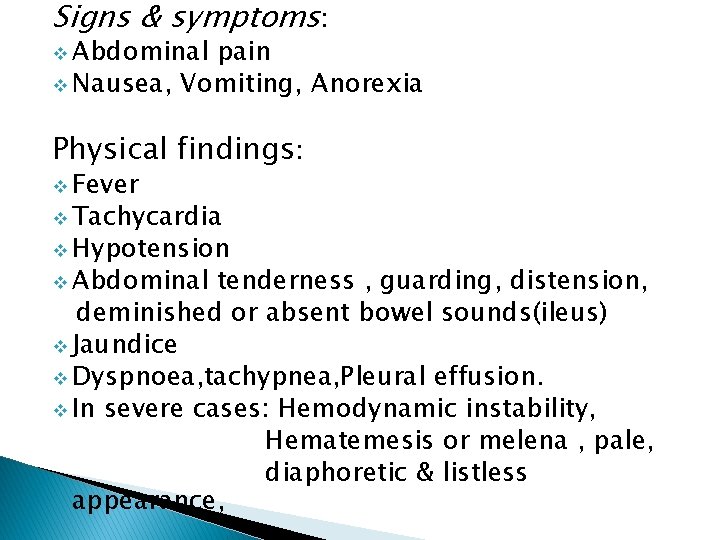
Signs & symptoms: v Abdominal pain v Nausea, Vomiting, Anorexia Physical findings: v Fever v Tachycardia v Hypotension v Abdominal tenderness , guarding, distension, deminished or absent bowel sounds(ileus) v Jaundice v Dyspnoea, tachypnea, Pleural effusion. v In severe cases: Hemodynamic instability, Hematemesis or melena , pale, diaphoretic & listless appearance,
Extremity muscle spasm secondary to hypocalcemia. v Uncommon Findings ass with severe Necrotizing Pancreatitis-Cullens Sign Grey Turner Sign Erythematous skin nodules.
Investigations Complete Hemogram Sr. Amylase& Sr. Lipase Sr. Calcium ABG, Electrolytes, Blood Glucose , Sr. Triglycerides RFT LFT CRP Blood c/s LDH Radiological : Chest & abdominal X-Rays , CT, MRI, MRCP, EUS.
Diagnosis As per the Atlanta Symposium, any 2 of the following: v Abdominal pain. v Amylase/lipase elevated>3 times upper limit of normal. v Pancreatic inflammation in cross sectional imaging
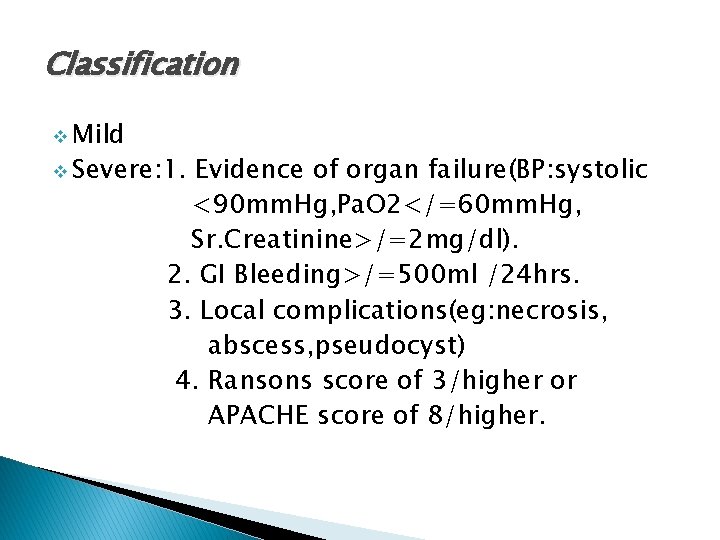
Classification v Mild v Severe: 1. Evidence of organ failure(BP: systolic <90 mm. Hg, Pa. O 2</=60 mm. Hg, Sr. Creatinine>/=2 mg/dl). 2. GI Bleeding>/=500 ml /24 hrs. 3. Local complications(eg: necrosis, abscess, pseudocyst) 4. Ransons score of 3/higher or APACHE score of 8/higher.
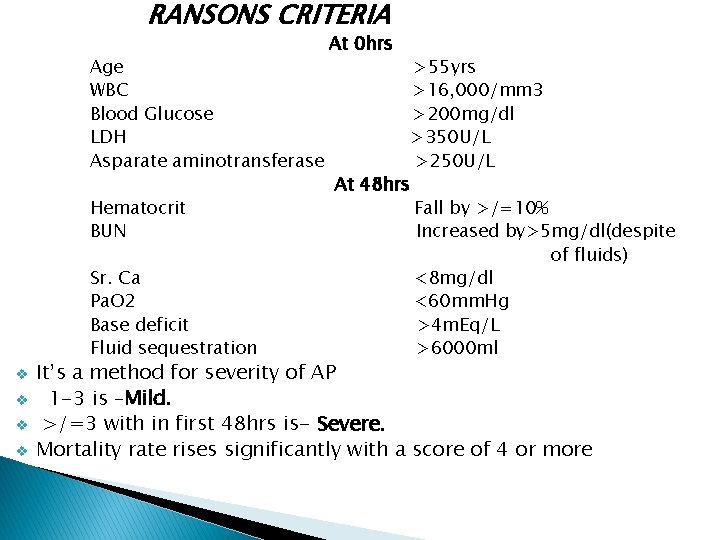
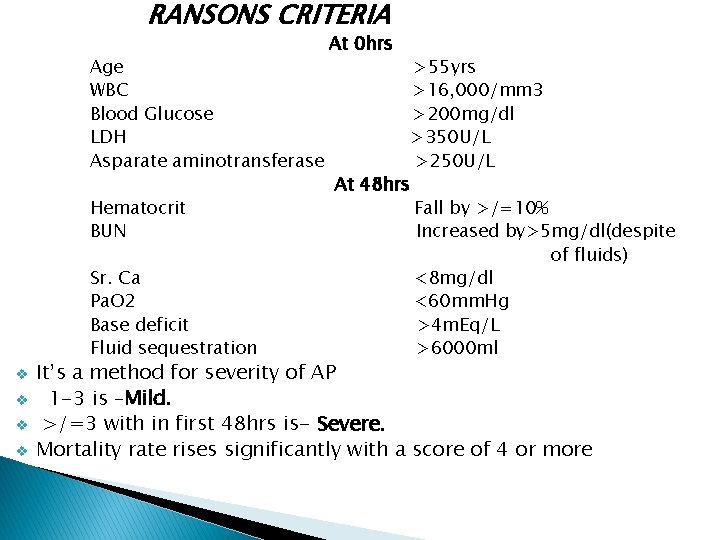
RANSONS CRITERIA Age WBC Blood Glucose LDH Asparate aminotransferase Hematocrit BUN Sr. Ca Pa. O 2 Base deficit Fluid sequestration v v At 0 hrs At 48 hrs >55 yrs >16, 000/mm 3 >200 mg/dl >350 U/L >250 U/L Fall by >/=10% Increased by>5 mg/dl(despite of fluids) <8 mg/dl <60 mm. Hg >4 m. Eq/L >6000 ml It’s a method for severity of AP 1 -3 is –Mild. >/=3 with in first 48 hrs is- Severe. Mortality rate rises significantly with a score of 4 or more
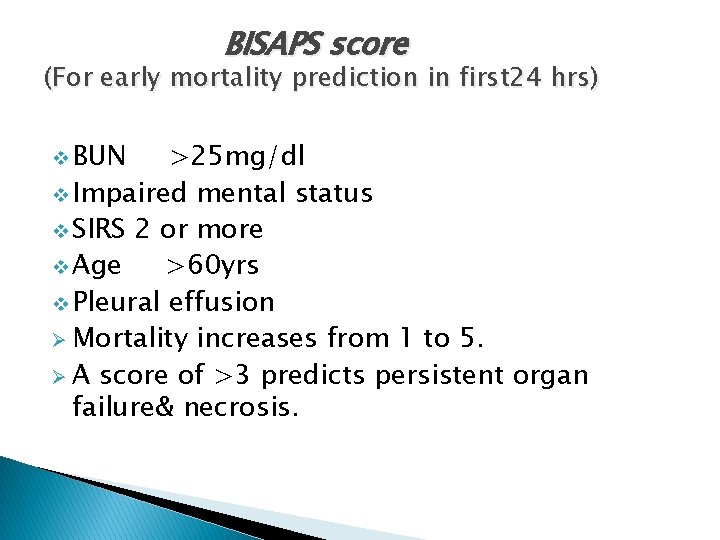
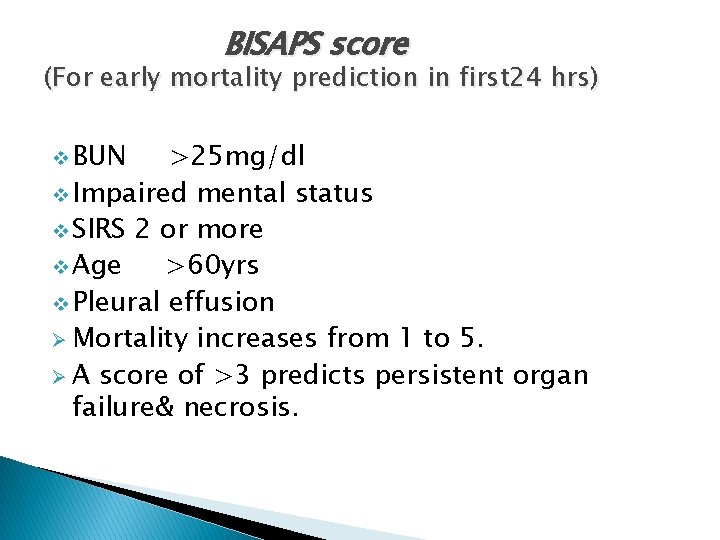
BISAPS score (For early mortality prediction in first 24 hrs) v BUN >25 mg/dl v Impaired mental status v SIRS 2 or more v Age >60 yrs v Pleural effusion Ø Mortality increases from 1 to 5. Ø A score of >3 predicts persistent organ failure& necrosis.
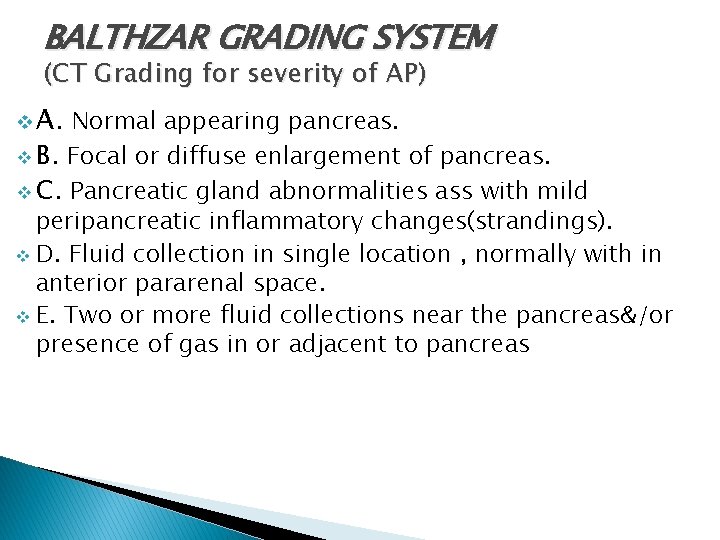
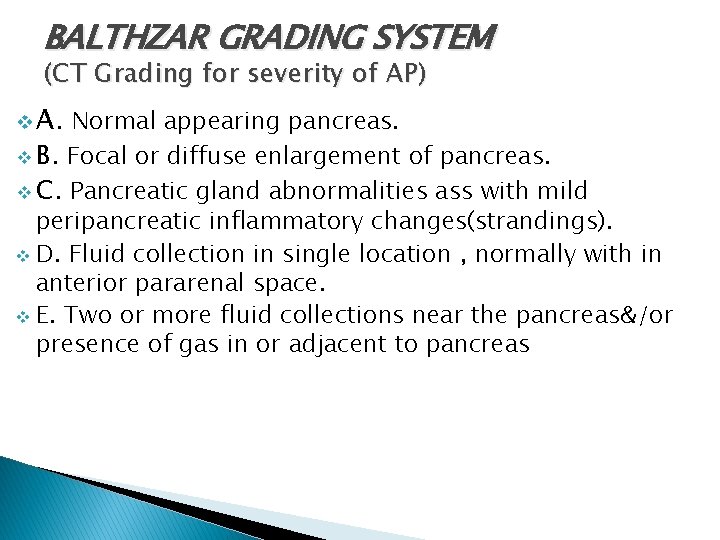
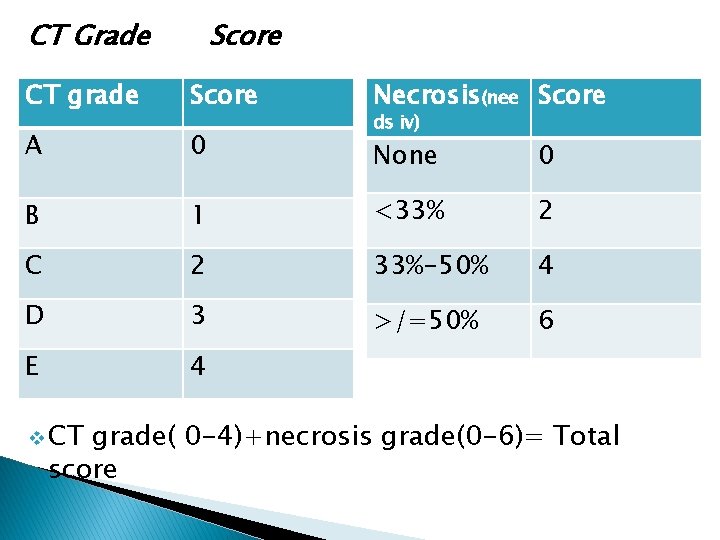
BALTHZAR GRADING SYSTEM (CT Grading for severity of AP) v A. Normal appearing pancreas. v B. Focal or diffuse enlargement of pancreas. v C. Pancreatic gland abnormalities ass with mild peripancreatic inflammatory changes(strandings). v D. Fluid collection in single location , normally with in anterior pararenal space. v E. Two or more fluid collections near the pancreas&/or presence of gas in or adjacent to pancreas
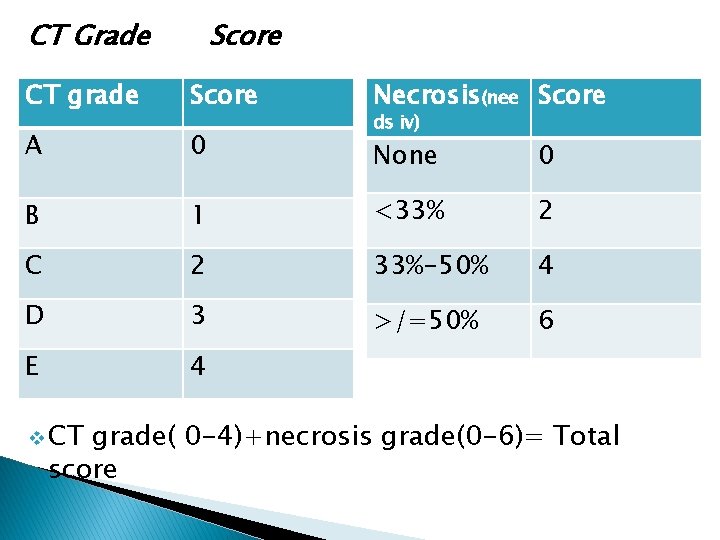
CT Grade Score CT grade Score Necrosis(nee Score A 0 None 0 B 1 <33% 2 C 2 33%-50% 4 D 3 >/=50% 6 E 4 v CT ds iv) grade( 0 -4)+necrosis grade(0 -6)= Total score
Management v All pts who have severe pain, vomitings, dehydration& raised amylase should be hospitalized. v Pts who is hemodynamically unstable& has tachycardia, hypoixia, decreased UOP indicates severe course and needs ICU admission. v General supportive care is the main stay of treatment. v Initial maintenace of ABC.
1. Fluids: v v v v These pts have huge fluid loss in to the third space , that increases the hemo-concentration & relative pancreatic bed ischemia, which increases the necrosis. Hence large amounts of fluids are required. Rapid restoration of fluids , Mc crystalloids. ~500 -1000 ml of fluid should be installed till organ hypo perfusion subsides. At very best at least 250 -350 ml/hr to maintain UOP@0. 5 ml/kg/hr. Vasopressors after adequate intravenous volume is achieved. Invasive hemodynamic monitoring(esply in poor Cardiac function, Chronic Renal failure, hemodynami unstability)to maintain UOP>0. 5 ml/kg/hr, hematocrit<30%& CVP@6 -8 cm. H 2 o
2. Pain: v v v Conventional analgesics by Iv route. Transdermal Fentanyl patch of 25 -50 mcg. Avoid NSAIDs 3. Nutrition: AP is a hypercatabolic state& can lead lo severe nutritional deficiencies. v Enteral /oral feeds should be started as early as possible. v Traditionally the only way of treating pancreatitis was to give rest to pancreas by not feeding& by NG tube aspiration. v Now NG tube aspiration is indicated only if pts has gastric ileus & repeated vomitings. v
v In mild uncomplicated AP, energy calories cam be received with IV Dextrose. v Enteral nutrition with NJ tube should be started as early as with in 48 hrs. v It helps in nutrition as well as prevention of sepsis. v Some recent studies show that NG feeding in pts who cannot tolerate oral feeds is as good as NJ feeds, but it still remains controversial. v Give enteral feeds as continuous 24 hrs infusion. v Start with 500 ml/day& increase gradually@250500 ml/day un till the targeted caloric needs are met. v If targets cannot be met after 5 -7 days trail with enteral route then consider TPN+EN. v Draw backs of only TPN usage : expensive , increase risk of line sepsis, fasting promotes gut atrophy with decreased mucosal lymphocytes & Ig. A, that predisposes bacterial translocation.
v Avoid over feeding& improve glucose tolerance by supplying some calories as lipids and maintain the triglyceride levels, 400 mg. v When pt can resume orally, should be initially fed with low calorie & low fat diet , which should gradually be increased. v This can be continued till pts start taking adequately orally(may b after 2 -3 wks). 4. Insilin: Monitor Sr. Glucose levels & iv insulin can be given if indicated.
5. Antibiotics: v Its use is quite controversial. v Initial phase clinical features are primarily of inflammation (SIRS)& do not require antibiotics. v Only definitive indication of therapeutic antibiotics is Cholangitis due to CBD Gram–ve pathogens such as E. coli &anaerobes are typical pathogens. Third generation Cephalosporins , Fluoroquinolones are good initial choice. v The other rationale is for prophylactic use to prevent infection of Pancreatic necrosis. v Imipenem class is used for Pancreatitis complicated by infected pancreatic necrosis. v Current guide lines do not recommend the use of prophylactic antibiotics.
v In practice , lot of pts with severe AP will be in ICU with CVC, urinary catheters, some on MV or Dialysis, thus they are prone to hospital acquired infections. v Antibiotics of choice for these pts depends on local epidemiology of infection in ICU with the sensitivities of these organisms. 6. IV calcium : v Only in pts with Hypocalcemia who have Tetany. 7. Somatostatin & octreotide: v There role is very small and there is insufficient evidences to support there use , there fore its effect is unlikely to have a significant effect in management of ANP
8. Protease inhibitors: v There use showed no significant reduction in mortality , length of stay or the need for surgery. Probably due to the time lag between the onset of pancreatitis and the administration. v Additionally derangement to the microvascular control of pancreas combined with increased vascular parmiability may contribute. v Continuos regional artery infusion or intraperitoneal administration may be more advantageous. v At present there is insufficient evidence to recommend them in ANP
9. Anti-inflammatory therapy: Pts with ANP exhibit a generalized uncontrolled inflammatory response. v Potentially there is a therapeutic window between the onset of symptoms and the development of organ failure , during which the anti-inflammatory therapy may be successful. v But currently there are not published trails of corticosterod therapy in ANP. v 10. Antifungal therapy: Antibiotic administration has been claimed to promote fungal infections ; how ever up to 25%of pts who do not receive antibiotics also develop fungal infections with an associated mortality up to 84%. One small randomized trail suggests that Fluconazole reduced the rate of fungal infection but had no effect on mortality.
CT: v. A CECT of abdomen is the first modality available to morphologically diagnose& quantify necrosis. v CT scan should be postponed till 72 hrs or more. v The only indication of early CT scan is when one I not clear about diagnosis , follow up CT scan if development of complications are suspected. 11. Early ERCP: (48 -72 hrs) v In Acute Biliary Pancreatitis with evidence of Cholangitis. v If in doubt EUS/MRCP can be done to decide if the stone is still in CBD
12. Management of complications Pseudocyst: v It’s a collection of pancreatic juice, which is enclosed by granulation tissue. v Takes at least 4 wks to form. v Drainage by percutaneous ultrasound guided, endoscopic or surgical is required in those with large&/or symptomatic pseudocyst. v MC complications include compression of adjacent structures , rupture, infection& bleeding(5%). v CT guided drainage of infected collection(multiple drains may be required)
13. Surgery: Indications: v In pts with Infected Pancreatic Necrosis not doing well. v When other techniques of draining in infected pancreatic necrosis is not possible. v Abdominal compartment syndrome in which percutaneous/other drainage techniques are not successful. v Surgery should be delayed to the 4 th wk as results before this are not good. v Local complications. v Bowel Infarction. v Pancreatic necrosis with pseudo-aneurism & massive intra-abdominal hemorrhage is best managed by Angiographic Embolization.
v Removal of GB: scheduled as early as possible to avoid the recurrence of biliary pancreatitis(30%). In severe attacks its recommended to wait up to 46 wks. Laparoscopic approach is feasible & safe even in cases where surgical debridement is required. Controversial indications: v Extensive(30%) sterile necrosis with persisting multi organ failure despite of intensive care therapy. v Most surgeons avoid surgery for this as the mortality rate is very high.
Prognosis v 10 -15% mortality. v About 80% of all cases are mild with a mortality of<5%. v 98% of deaths occur in the 20% of severe cases. v 1/3 rd occurs in first wk usually from multi organ failure. v After this the majority from sepsis, especially that complicate infected necrosis.

Thank u
 Pancreatitis pes statement
Pancreatitis pes statement Acute pancreatitis diagnosis criteria
Acute pancreatitis diagnosis criteria Ransons criteria
Ransons criteria Acute pancreatitis ct
Acute pancreatitis ct Cholecystitis nursing care plan
Cholecystitis nursing care plan Apendicolith
Apendicolith Pancreatitis nursing diagnosis
Pancreatitis nursing diagnosis Ranson criteria
Ranson criteria Acute pancreatitis ct severity index
Acute pancreatitis ct severity index Acute pancreatitis pathophysiology
Acute pancreatitis pathophysiology Ranson's criteria
Ranson's criteria Swarith
Swarith Jessica reddy x
Jessica reddy x Bheemarjuna reddy tamma
Bheemarjuna reddy tamma Michael reddy conduit metaphor
Michael reddy conduit metaphor Microtopography of gingival wall
Microtopography of gingival wall Ketan reddy
Ketan reddy Raj reddy inventions
Raj reddy inventions I am woman helen reddy lyrics meaning
I am woman helen reddy lyrics meaning Prof raj reddy
Prof raj reddy Konda madhava reddy
Konda madhava reddy Dr dn reddy
Dr dn reddy Pathophysiology of appendicitis
Pathophysiology of appendicitis Acute inflammation definition
Acute inflammation definition Acute responses to training definition
Acute responses to training definition Acute apical periodontitis definition
Acute apical periodontitis definition Acute scrotum definition
Acute scrotum definition Vacuple
Vacuple Congruent sides
Congruent sides Acute inflammation definition
Acute inflammation definition Cardinal sign of inflammation
Cardinal sign of inflammation Clasificaciones de pancreatitis
Clasificaciones de pancreatitis Cefotaxia
Cefotaxia Características de nutrición
Características de nutrición Criterios de cambridge pancreatitis cronica
Criterios de cambridge pancreatitis cronica Jaime es aguda
Jaime es aguda Marshall pancreatitis
Marshall pancreatitis