Inflammation Inflammation The response of living vascularised tissues





- Slides: 40

Inflammation
Inflammation The response of living vascularised tissues to injury 1 - Acute inflammation 2 - Chronic inflammation
Acute inflammation Early response of tissue to injury Vascular Non-specific Short duration
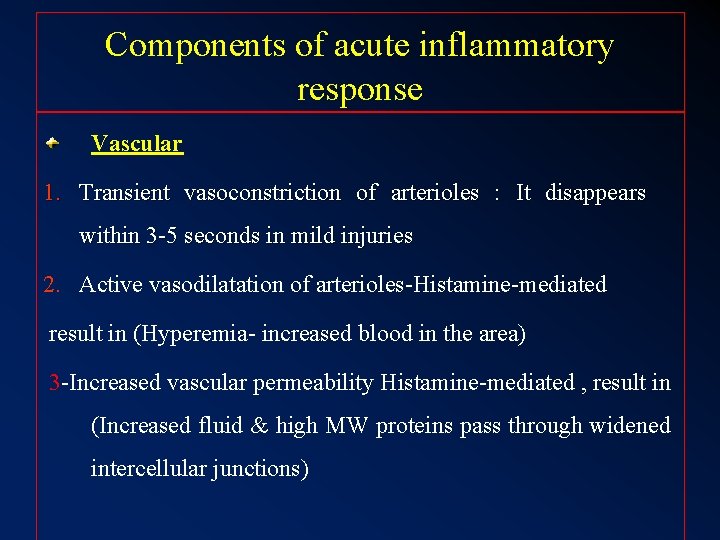
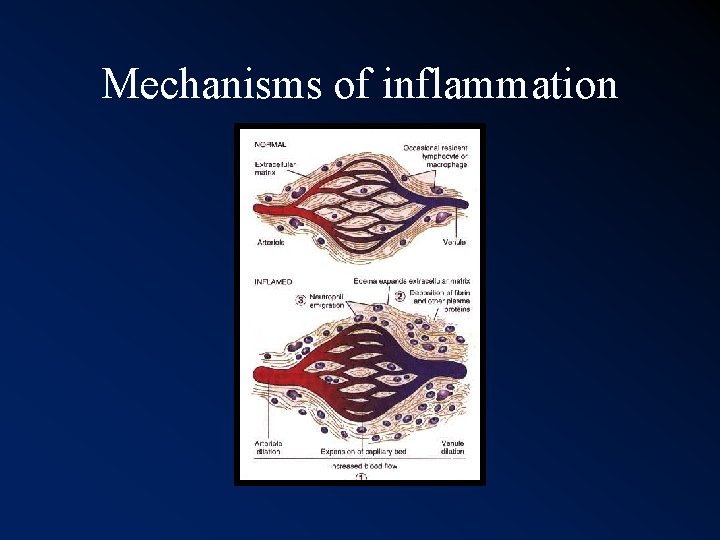
Components of acute inflammatory response Vascular 1. Transient vasoconstriction of arterioles : It disappears within 3 -5 seconds in mild injuries 2. Active vasodilatation of arterioles-Histamine-mediated result in (Hyperemia- increased blood in the area) 3 -Increased vascular permeability Histamine-mediated , result in (Increased fluid & high MW proteins pass through widened intercellular junctions)
- 4. Formation of fluid exudate, from circulation to the interstitial tissues. Fibrin-rich fluid - Contains plasma proteins including Ig, C’ and fibrinogen. - Helps combat the offending agent by diluting it, increase lymphatic flow and flooding the area with Ig+C’.
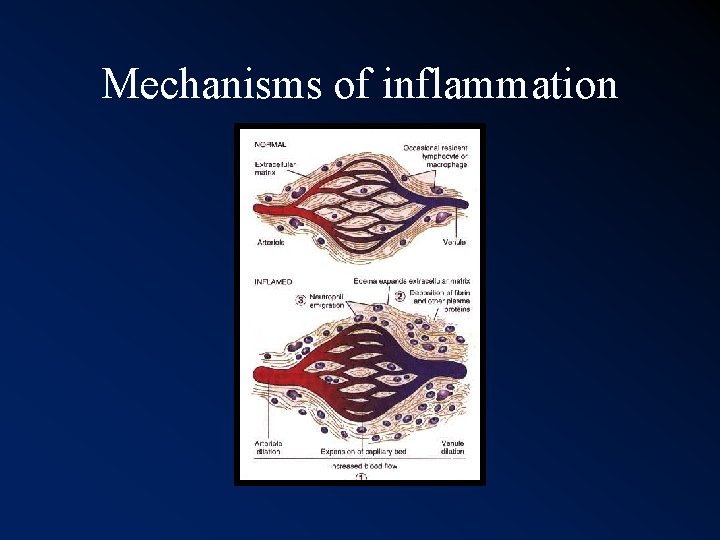
Mechanisms of inflammation
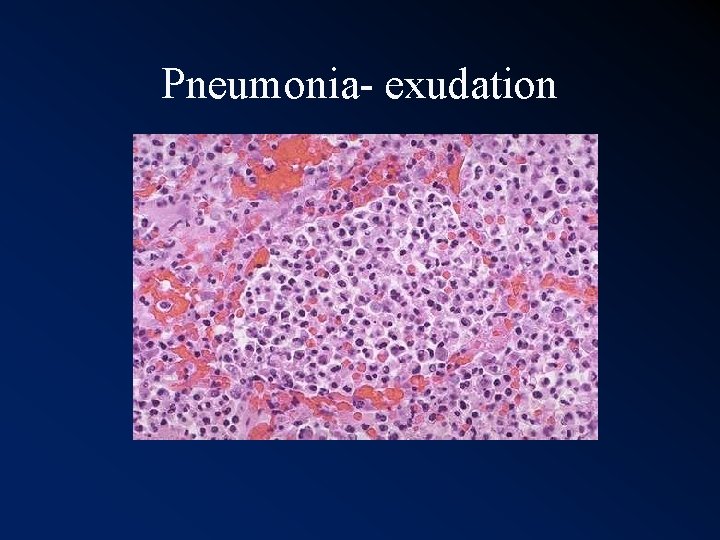
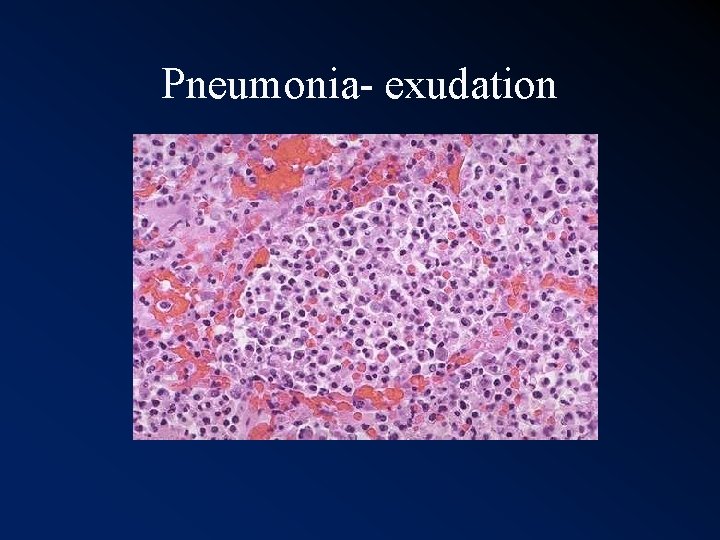
Pneumonia- exudation
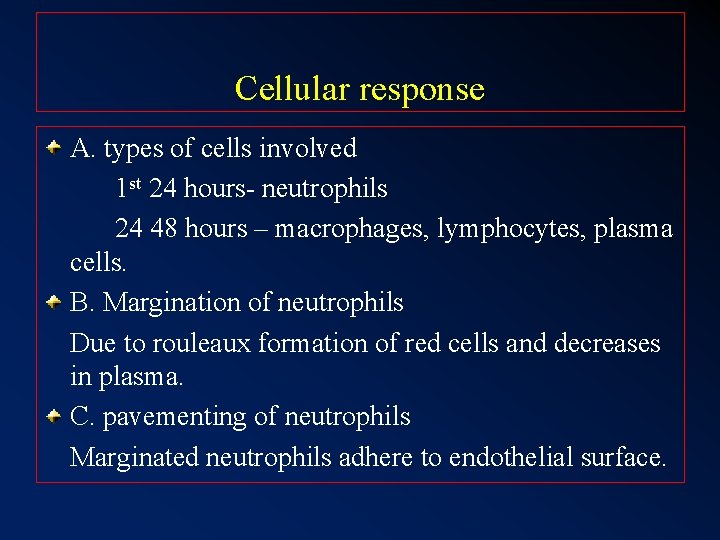
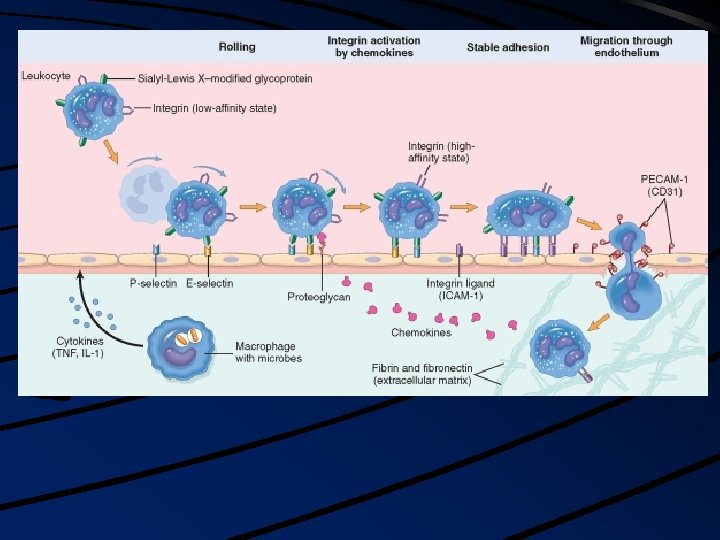
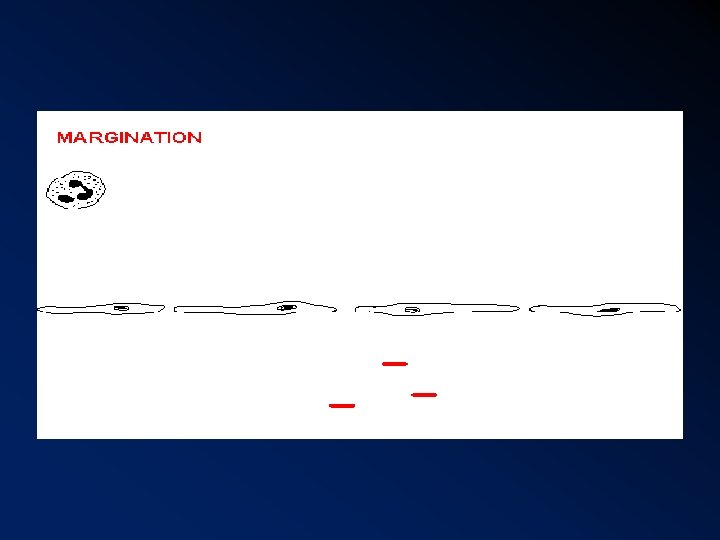
Cellular response A. types of cells involved 1 st 24 hours- neutrophils 24 48 hours – macrophages, lymphocytes, plasma cells. B. Margination of neutrophils Due to rouleaux formation of red cells and decreases in plasma. C. pavementing of neutrophils Marginated neutrophils adhere to endothelial surface.
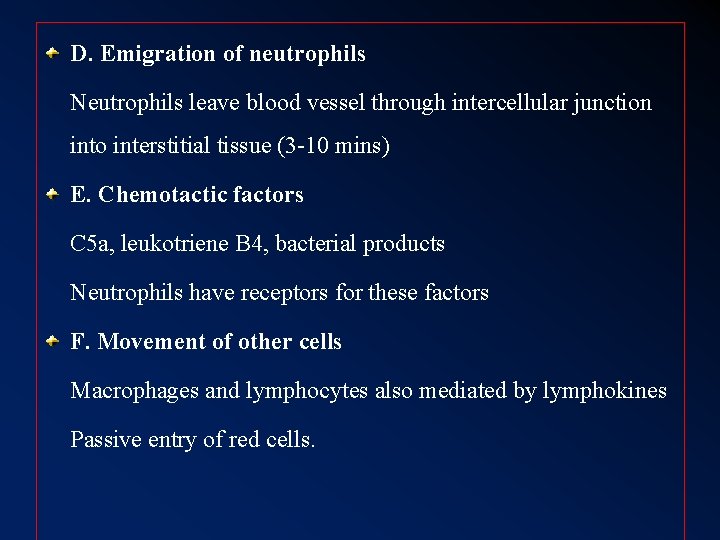
D. Emigration of neutrophils Neutrophils leave blood vessel through intercellular junction into interstitial tissue (3 -10 mins) E. Chemotactic factors C 5 a, leukotriene B 4, bacterial products Neutrophils have receptors for these factors F. Movement of other cells Macrophages and lymphocytes also mediated by lymphokines Passive entry of red cells.
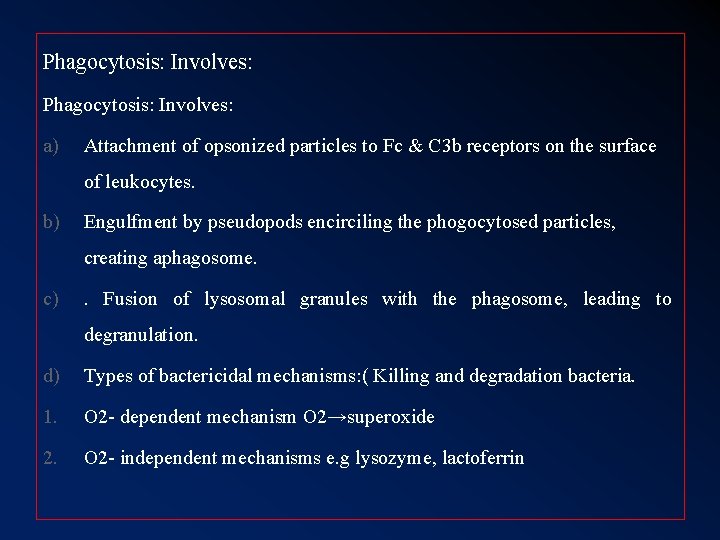
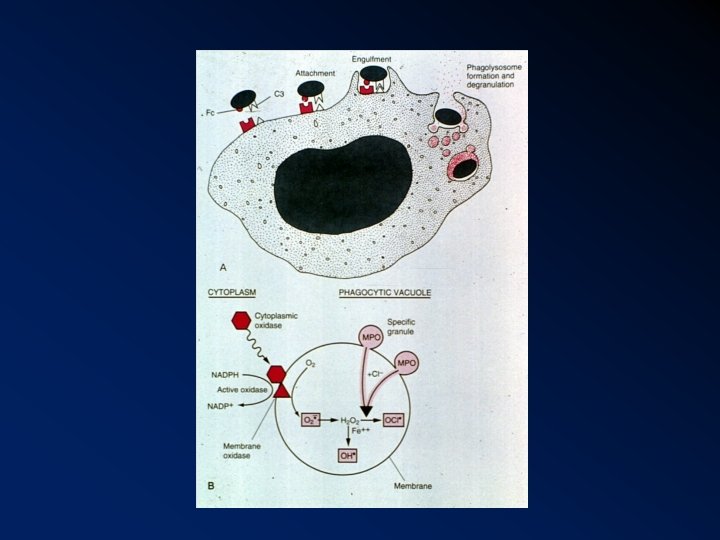
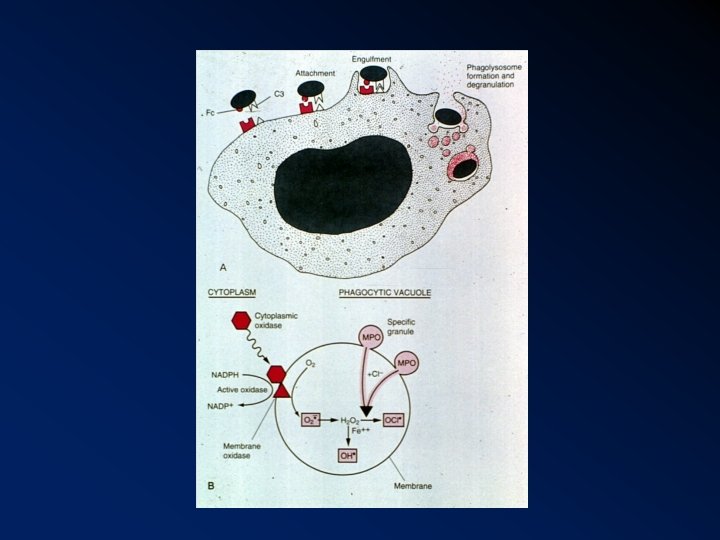
Phagocytosis: Involves: a) Attachment of opsonized particles to Fc & C 3 b receptors on the surface of leukocytes. b) Engulfment by pseudopods encirciling the phogocytosed particles, creating aphagosome. c) . Fusion of lysosomal granules with the phagosome, leading to degranulation. d) Types of bactericidal mechanisms: ( Killing and degradation bacteria. 1. O 2 - dependent mechanism O 2→superoxide 2. O 2 - independent mechanisms e. g lysozyme, lactoferrin
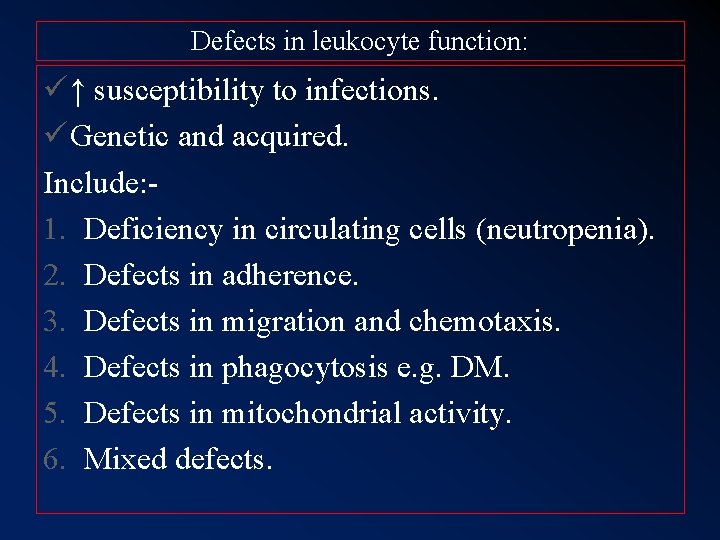
Defects in leukocyte function: ü ↑ susceptibility to infections. ü Genetic and acquired. Include: 1. Deficiency in circulating cells (neutropenia). 2. Defects in adherence. 3. Defects in migration and chemotaxis. 4. Defects in phagocytosis e. g. DM. 5. Defects in mitochondrial activity. 6. Mixed defects.
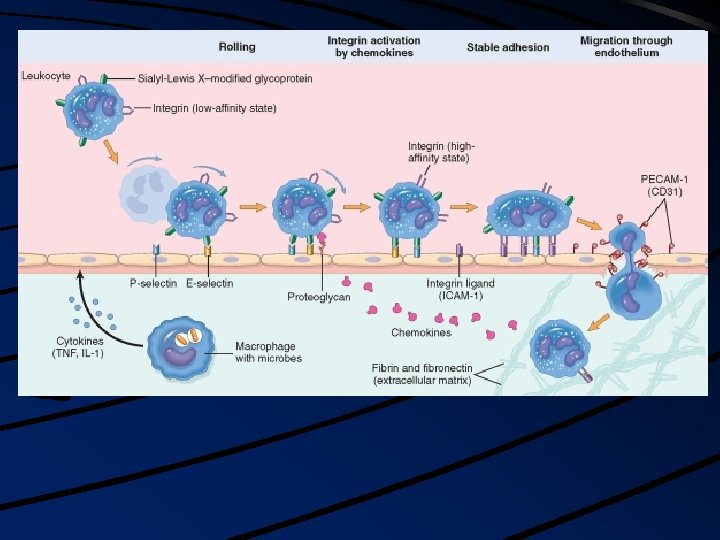
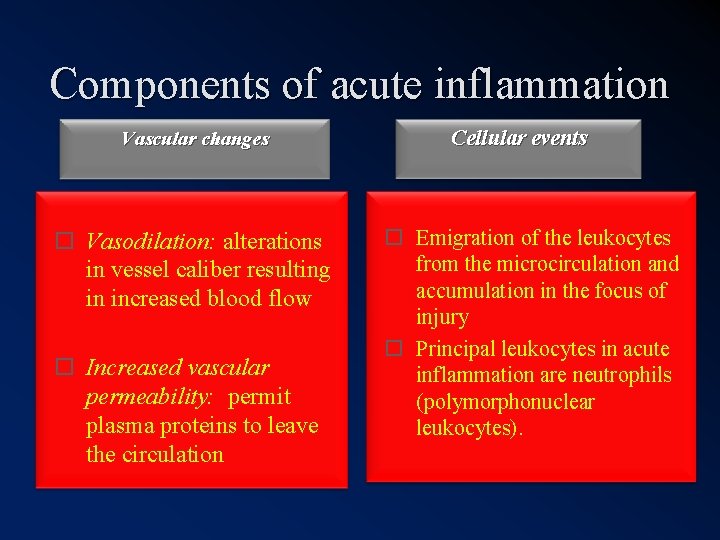
Components of acute inflammation Vascular changes Vasodilation: alterations in vessel caliber resulting in increased blood flow Increased vascular permeability: permit plasma proteins to leave the circulation Cellular events Emigration of the leukocytes from the microcirculation and accumulation in the focus of injury Principal leukocytes in acute inflammation are neutrophils (polymorphonuclear leukocytes).
Inflammation serves to destroy, dilute or isolate the injurious agent (microbes, toxins) and eliminate the necrotic cells and tissues.
The 5 cardinal signs of
Cardinal signs of acute inflammation Color—heat Rubor—redness Tumor—swelling Dolor—pain Functio laesa—loss of function
Redness/ Heat Increased rate and volume of blood flow into inflamed area Swelling Accumulation of exudate in the tissues Pain Accumulation of chemicals (prostaglandins) that stimulate nerve endings. Increased tissue tension

Redness

Swelling

Cardinal Signs of Inflammation

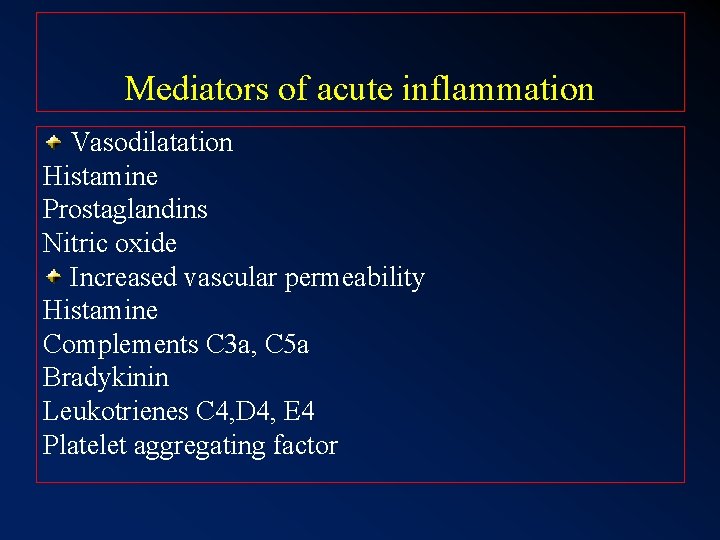
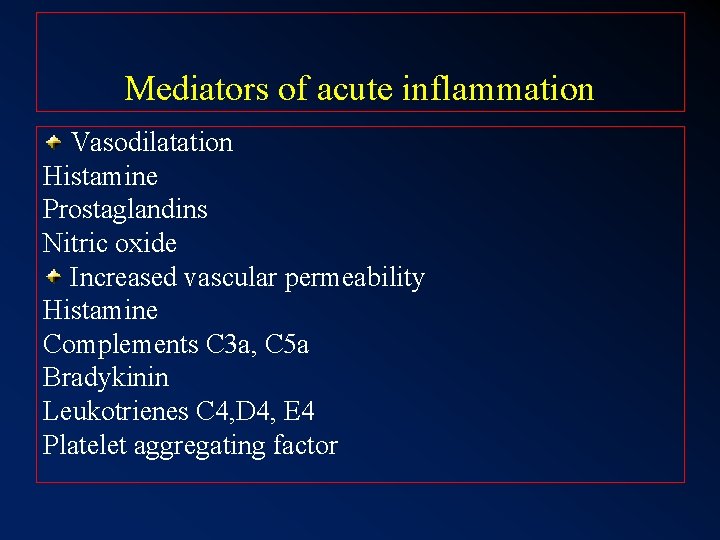
Mediators of acute inflammation Vasodilatation Histamine Prostaglandins Nitric oxide Increased vascular permeability Histamine Complements C 3 a, C 5 a Bradykinin Leukotrienes C 4, D 4, E 4 Platelet aggregating factor
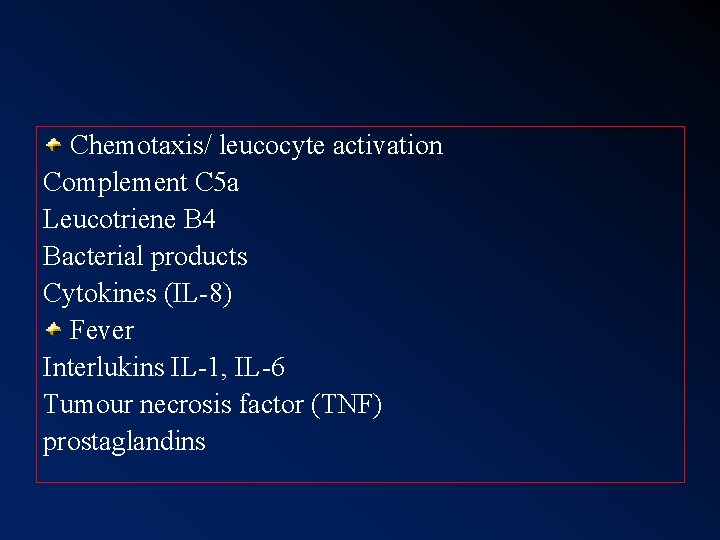
Chemotaxis/ leucocyte activation Complement C 5 a Leucotriene B 4 Bacterial products Cytokines (IL-8) Fever Interlukins IL-1, IL-6 Tumour necrosis factor (TNF) prostaglandins
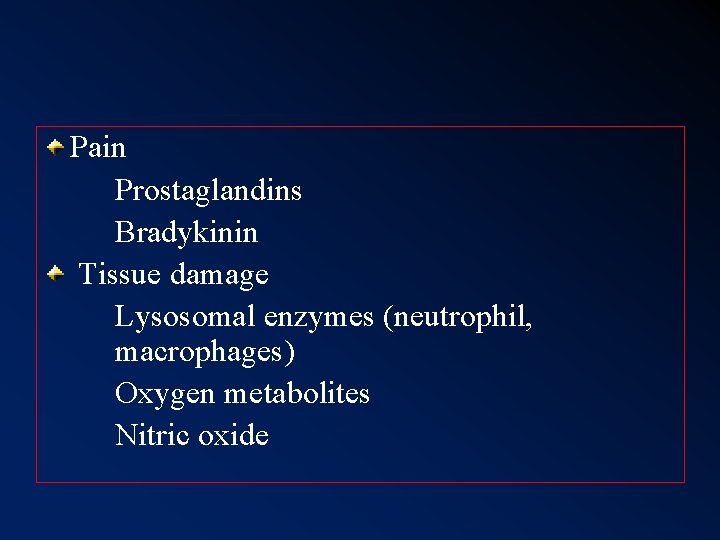
Pain Prostaglandins Bradykinin Tissue damage Lysosomal enzymes (neutrophil, macrophages) Oxygen metabolites Nitric oxide
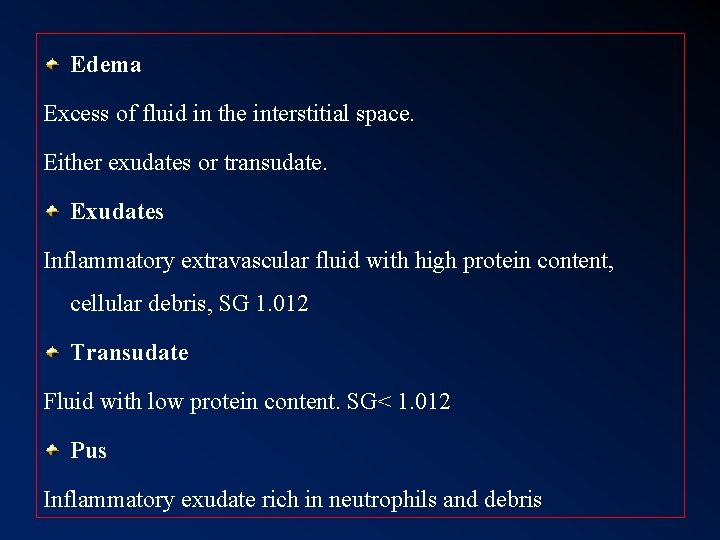
Edema Excess of fluid in the interstitial space. Either exudates or transudate. Exudates Inflammatory extravascular fluid with high protein content, cellular debris, SG 1. 012 Transudate Fluid with low protein content. SG< 1. 012 Pus Inflammatory exudate rich in neutrophils and debris
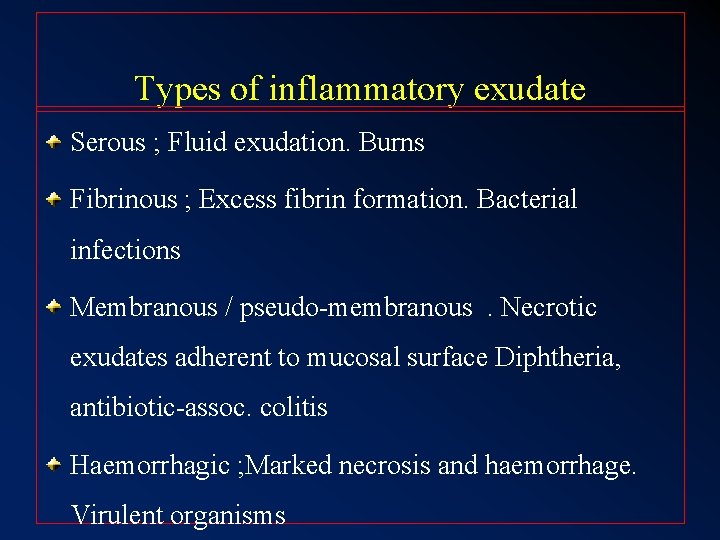
Types of inflammatory exudate Serous ; Fluid exudation. Burns Fibrinous ; Excess fibrin formation. Bacterial infections Membranous / pseudo-membranous. Necrotic exudates adherent to mucosal surface Diphtheria, antibiotic-assoc. colitis Haemorrhagic ; Marked necrosis and haemorrhage. Virulent organisms
Catarrhal ; Excess mucus, common cold Suppurative ; Marked neutrophils response with pus. Pyogenic infections Allergic : Marked edema. urticaria
Cellulitis Spreading inflammation with tissue necrosis Nitric oxide Soluble free radical gas Produced by Endothelial cells Macrophages
Outcome / Sequelae of acute inflammation Resolution : Return to normal structure and function Healing by fibrosis/ later fibrous scar Suppuration / abscess Chronic inflammation : Persistence of acute inflammation converts response to a chronic type
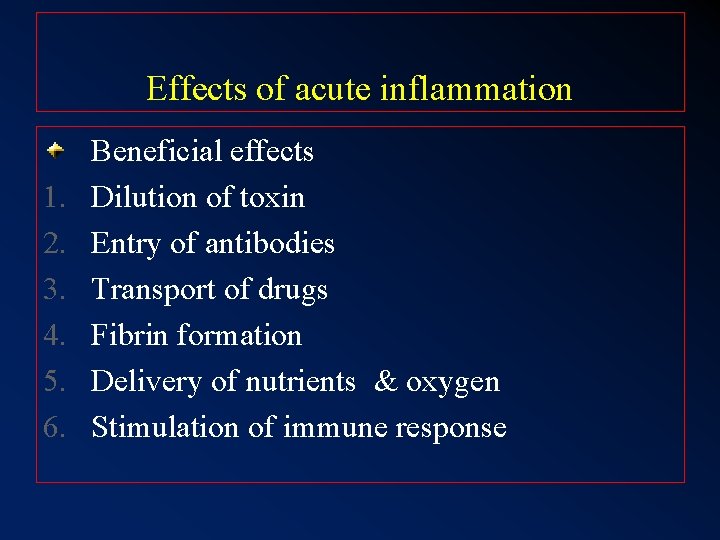
Effects of acute inflammation 1. 2. 3. 4. 5. 6. Beneficial effects Dilution of toxin Entry of antibodies Transport of drugs Fibrin formation Delivery of nutrients & oxygen Stimulation of immune response
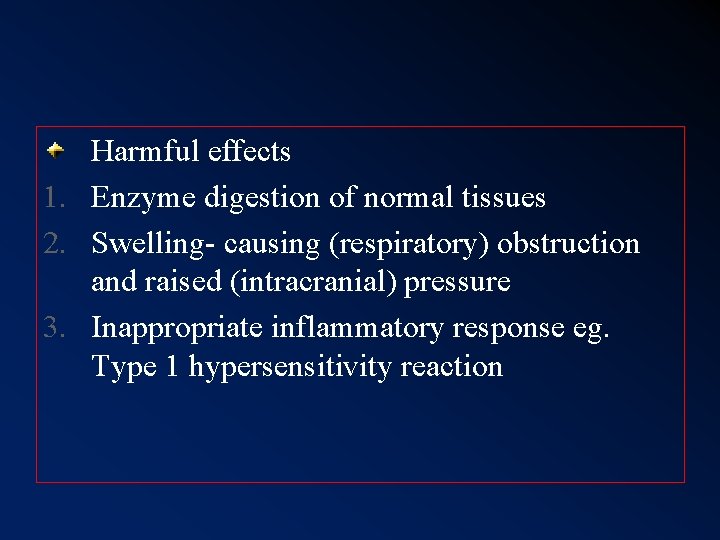
Harmful effects 1. Enzyme digestion of normal tissues 2. Swelling- causing (respiratory) obstruction and raised (intracranial) pressure 3. Inappropriate inflammatory response eg. Type 1 hypersensitivity reaction
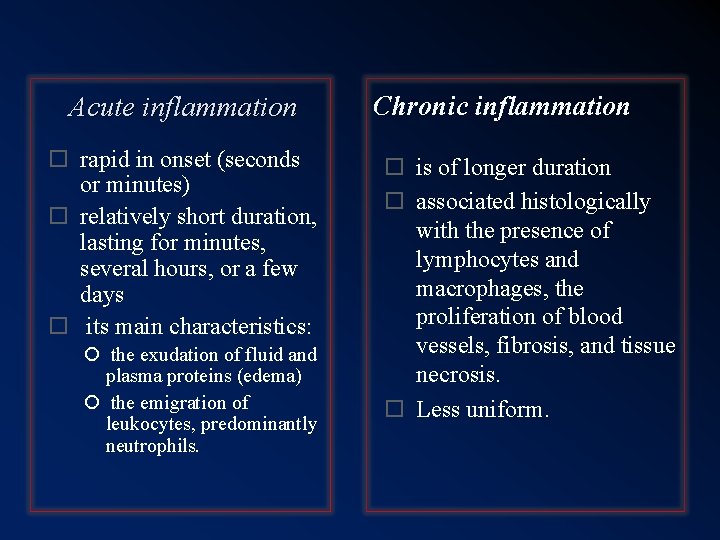
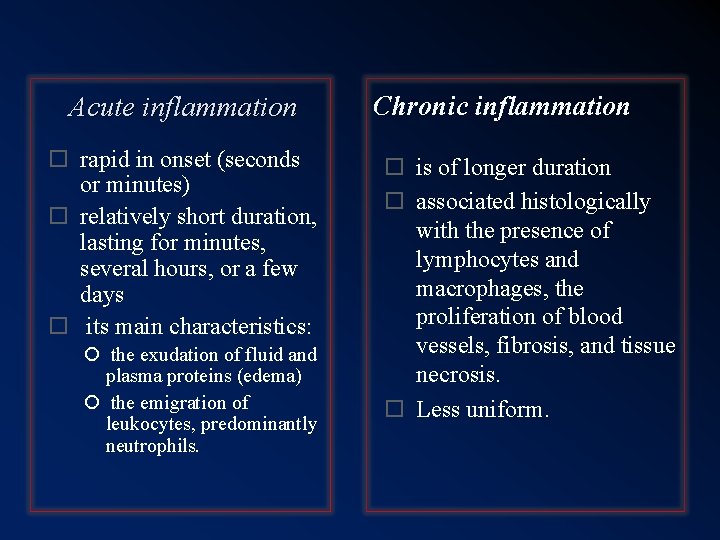
Acute inflammation rapid in onset (seconds or minutes) relatively short duration, lasting for minutes, several hours, or a few days its main characteristics: the exudation of fluid and plasma proteins (edema) the emigration of leukocytes, predominantly neutrophils. Chronic inflammation is of longer duration associated histologically with the presence of lymphocytes and macrophages, the proliferation of blood vessels, fibrosis, and tissue necrosis. Less uniform.
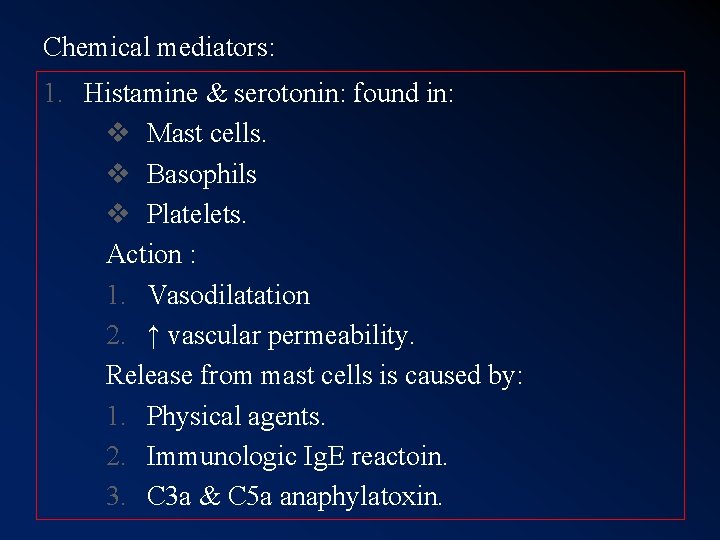
Chemical mediators: 1. Histamine & serotonin: found in: v Mast cells. v Basophils v Platelets. Action : 1. Vasodilatation 2. ↑ vascular permeability. Release from mast cells is caused by: 1. Physical agents. 2. Immunologic Ig. E reactoin. 3. C 3 a & C 5 a anaphylatoxin.
4. Interleukin-1. 5. Other histamine releasing factors. Release from platelets is stimulated by: a. Contact with collagen. b. Thrombin. c. ADP. d. Antigen- antibody complexes. e. Platelets activating factor (PAF). 2. Complement system: Activation of complement system occurs via : i. The classic pathway, initiated by antigen-antibody complexes.
ii. Alternate complement pathway, activated by: Ø Endotoxin Ø Complex polysaccharides Ø Aggregated globulins. Coplement components with inflammatory activity include: 1. C 3 a, which increase vascular permeability. 2. C 5 a, “ “ “ and leukocytes chemotaxis. 3. C 3 b, C 3 bi the opsonins important in phagocytosis.
4. C 5 b- 9 the membrane attack complex that a. Lyses cells b. Stimulate arachidonic acid metabolism. c. Production of reactive O 2 metabolities by leukocytes. 3. Kinin system: 1. bradykinin→↑ vasopermeability. 2. Kallikrein has chemotatic activity & causes neutrophil aggregation.
4. Clotting system: Fibrinogen → fibrinopeptides. 1. ↑vascular permeability. 2. Chemotatic. 5. Arachidonic acid metabolities: The inflammatory prostaglandins & leukotreines include: 1) Prostacyclin: PGI 2 &PGE 2→ vasoconstriction. 2) Leukotreines, C 4, D 4, & E 4, ↑permeability & vasoconstriction. 3) Thromboxane A 2: → vasoconstriction. 4) Leukotreine B 4 → chemotaxis.
6. Platelet activating factor (PAF) v↑ vascular permeability. v. Vasodilatation. v. Increase leukocytes adhesion. v. Leukocytes chemotaxis. 7. Cytokines: - Polypeptides. - Released by macrophages and lymphocytes. - Example, IL-1, TNF, IL-8
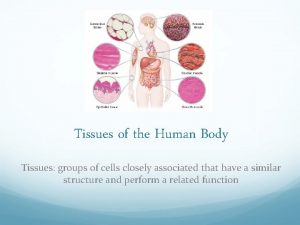
 Body tissues chapter 3 cells and tissues
Body tissues chapter 3 cells and tissues Eisonophil
Eisonophil Body tissue
Body tissue Anatomy chapter 3 cells and tissues
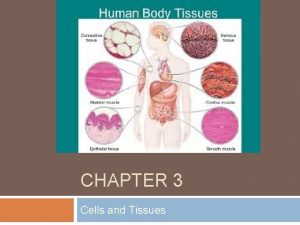
Anatomy chapter 3 cells and tissues The four major categories of tissues are
The four major categories of tissues are Cellular events of inflammation
Cellular events of inflammation Vascular response in acute inflammation
Vascular response in acute inflammation Living non living dead
Living non living dead Mitochondria information
Mitochondria information Venn diagram living and nonliving things
Venn diagram living and nonliving things Is tomato living or nonliving
Is tomato living or nonliving Natural response circuit
Natural response circuit A subsequent
A subsequent Natural and forced response
Natural and forced response Cells-tissues-organ-systems-organism
Cells-tissues-organ-systems-organism Dense connective tissue
Dense connective tissue Tissues are groups of similar cells working together to
Tissues are groups of similar cells working together to 3 tissues of a plant
3 tissues of a plant Plant tissues
Plant tissues Goblet cells cilia and microvilli
Goblet cells cilia and microvilli Zonula occludens
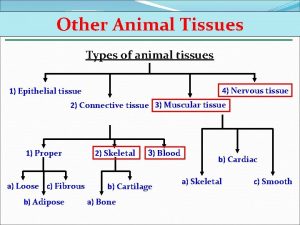
Zonula occludens Types of tissues
Types of tissues Connective tissue poem
Connective tissue poem Tissues causes of civil war
Tissues causes of civil war Meristematic tissue
Meristematic tissue Tissues in plants
Tissues in plants Chapter 3 cells and tissues figure 3-1
Chapter 3 cells and tissues figure 3-1 The circulatory system includes
The circulatory system includes Four major tissues
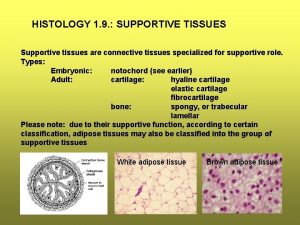
Four major tissues What are supportive tissues
What are supportive tissues Tissues group together to form
Tissues group together to form Genetic effects on gene expression across human tissues
Genetic effects on gene expression across human tissues Plant tissue and organs
Plant tissue and organs A tissues
A tissues Define periradicular disease
Define periradicular disease Chapter 3 cells and tissues
Chapter 3 cells and tissues Tissue
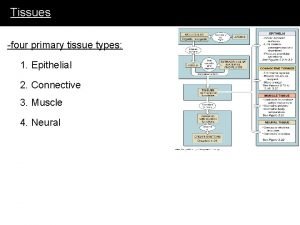
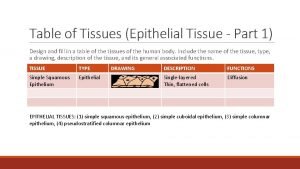
Tissue Types of tissues
Types of tissues Muscle tissue where is it found
Muscle tissue where is it found Table tissue design
Table tissue design What are the 4 types of tissues
What are the 4 types of tissues