Acute and Chronic Pancreatitis The Pancreas one hard
- Slides: 61
Acute (and Chronic) Pancreatitis:
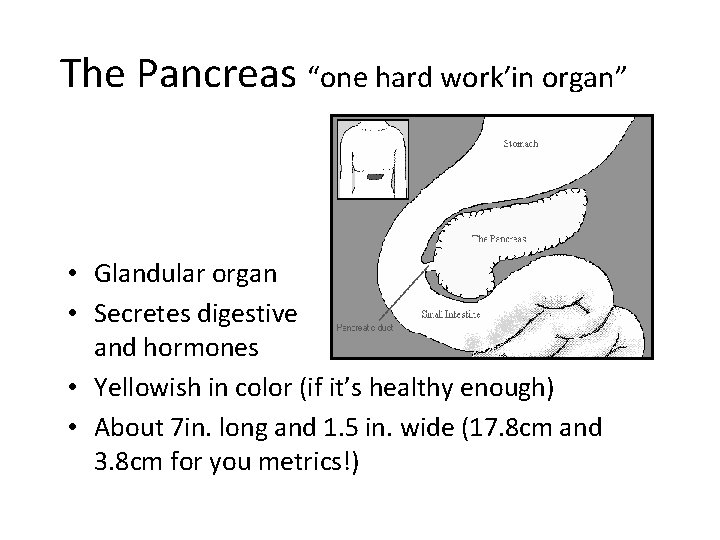
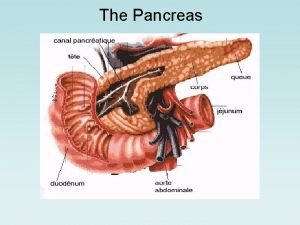
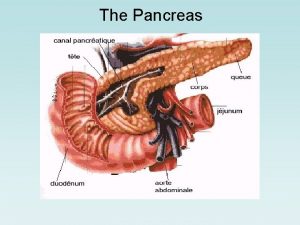
The Pancreas “one hard work’in organ” • Glandular organ • Secretes digestive enzymes and hormones • Yellowish in color (if it’s healthy enough) • About 7 in. long and 1. 5 in. wide (17. 8 cm and 3. 8 cm for you metrics!)
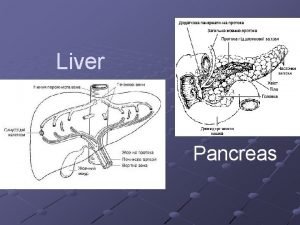
Location • Sits outside the posterior curve of stomach behind the duodenum and the spleen stomach • Located in retro peritoneal space, mostly behind stomach • Divided into head, body, and tail portions • Connected to the small intestine at the duodenum
Pancreas • A major mixed gland – Has both endocrine and exocrine functions • 98% exocrine – Secretion of digestive enzymes and bicarbonate by pancreatic acini and ducts • 2% endocrine – Peptide hormones vital in regulating carbohydrate metabolism and blood sugar • “Detects” levels of nutrients absorbed from intestine via hepatic portal vein
– Islets of Langerhans’ cells • throughout pancreas • Alpha cells which secrete glucagon – Increase glucose concentration in blood • Beta cells which secrete insulin – Lower blood glucose • Delta cells which secrete somatostatin – Regulate other pancreatic hormones
Somatostatin Facts • 3 rd peptide secreted from pancreas • Tends to dampen rise in both insulin and glucagon, preventing roller-coaster rides with the blood sugar! • May inhibit GH secretion from pituitary, since GH has anti-insulin effects
So, what are those enzymes? • Pancreatic Acinar cells secrete pancreatic enzymes • Produce digestive enzymes and bicarbonate. Secretes about 1, 500 -2, 000 cc of digestive solution per day • Lipase • Amylase • Trypsin Main • Phospholipase (PLA 2) ones
Acute pancreatitis • Pathophys- insult leads to leakage of pancreatic enzymes into pancreatic and peripancreatic tissue leading to acute inflammatory reaction • Inflammation of the pancreas • Pancreatic enzymes activated prematurely (before reaching intestines) • Activates inflammatory mediators to area • Increasing vascular permeability • Leads to edema and fluid shifts from intravascular spaces to the interstitum • Vasodilation occurs, increased capillary leakage and pooling of fluid in the venous system can result in shock and reduced cardiac function • Destruction of connective tissue in the vascular wall and causes microemboli can lead to DIC and bleeding
Acute pancreatitis • Phospholipase A irritates pancreatic tissue and causes tissue necrosis • Lipase overflowing into the tissues and systemic circulation leads to fat necrosis of the pancreas and surrounding areas • Risk of mortality increases with development of infection or pulmonary, cardiac, and renal complications
Causes of Acute Pancreatitis • Obstruction – Cholelithiasis – Ampullary or pancreatic tumor – Duodenal obstruction – Papillary obstruction – Hypertensive Oddi’s sphincter – Ampullary stenosis – Biliary disease
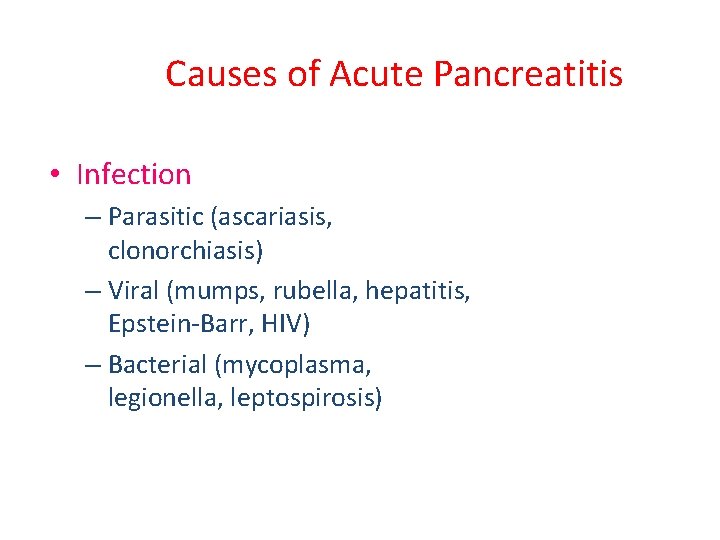
Causes of Acute Pancreatitis • Infection – Parasitic (ascariasis, clonorchiasis) – Viral (mumps, rubella, hepatitis, Epstein-Barr, HIV) – Bacterial (mycoplasma, legionella, leptospirosis)
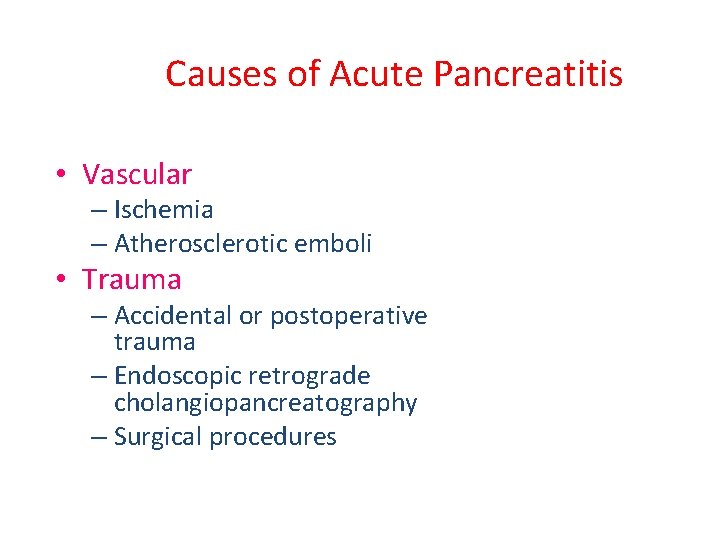
Causes of Acute Pancreatitis • Vascular – Ischemia – Atherosclerotic emboli • Trauma – Accidental or postoperative trauma – Endoscopic retrograde cholangiopancreatography – Surgical procedures
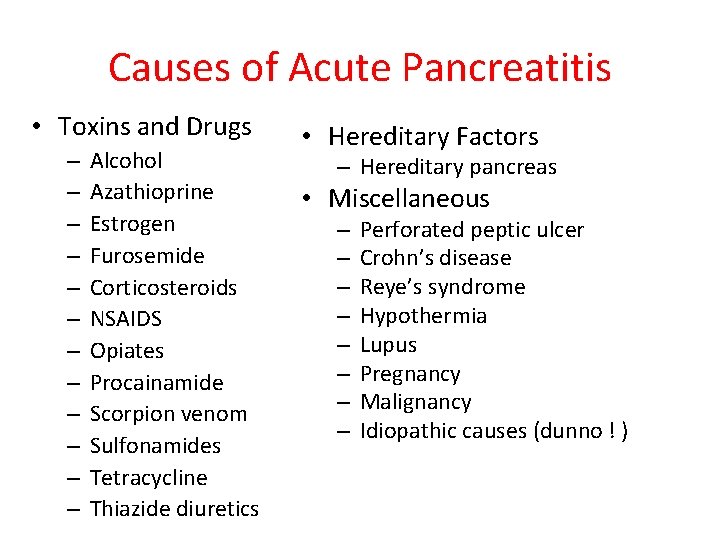
Causes of Acute Pancreatitis • Toxins and Drugs – – – Alcohol Azathioprine Estrogen Furosemide Corticosteroids NSAIDS Opiates Procainamide Scorpion venom Sulfonamides Tetracycline Thiazide diuretics • Hereditary Factors – Hereditary pancreas • Miscellaneous – – – – Perforated peptic ulcer Crohn’s disease Reye’s syndrome Hypothermia Lupus Pregnancy Malignancy Idiopathic causes (dunno ! )
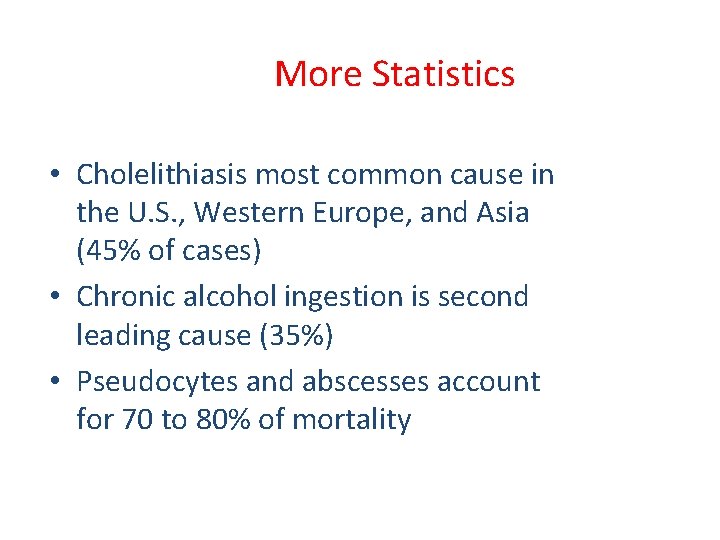
More Statistics • Cholelithiasis most common cause in the U. S. , Western Europe, and Asia (45% of cases) • Chronic alcohol ingestion is second leading cause (35%) • Pseudocytes and abscesses account for 70 to 80% of mortality
Signs & Symptoms • Severe epigastric abdominal pain - abrupt onset (may radiate to back) • Nausea & Vomiting • Weakness • Tachycardia • +/- Fever; +/- Hypotension or shock – Grey Turner sign - flank discoloration due to retroperitoneal bleed in pt. with pancreatic necrosis (rare) – Cullen’s sign - periumbilical discoloration (rare)
Acute Pancreatitis • Clinical Manifestations – Epigastric or midabdominal pain – May radiate to back – Fever, leukocytosis – Nausea and vomiting – Abdominal distention – Hypotension and shock, DIC – ATN, ARDS – Formation of pancreatic fluid collections (pseudocytes and abscesses)
Clinical Manifestations (continued) – Atelectasis, Pneumonia, Pleural Effusions, Pulmonary edema, – Tetany may develop as a result of deposition of calcium in areas of fat necrosis or decreased parathorome – Transient hyperglycemia – Lleus, colonic obstruction – CNS hypoperfusion with confusion
Differential Diagnosis • • Biliary colic Perforated hollow viscus Mesenteric ischemia Closed-loop intestinal obstruction Inferior wall MI Dissecting aneurysm Ectopic pregnancy
Diagnosis • Based on clinical presentation, history, physical and labs • Amylase and lipase levels • Amylase elevated in 80% – More sensitive early on • Lipase is more sensitive if symptoms have been present for more than 24 hours
Diagnosis • Both amylase and lipase levels may be normal with CT proved pancreatitis • Ultrasonography or CT is definitive • Radiography may reveal a “sentinel loop” – Localized ileus in midepigastric region – Pleural effusions may also be present • MRI, abdominal plain films, Chest X-ray Upright
Acute Pancreatitis • Lab studies – CBC, electrolytes, liver enzymes, calcium, magnesium, PT/PTT – May have hemoconcentration due to third spacing of fluid – May have hypocalcemia caused by “soap” formation • Saponification of triglycerides and calcium – Frequently have hypomagnesemia – WBC usually elevated – Liver enzymes may be elevated from biliary obstruction
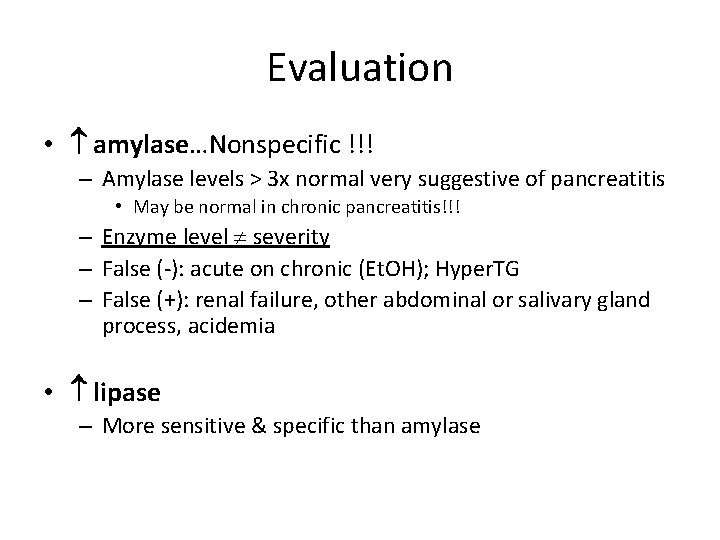
Evaluation • amylase…Nonspecific !!! – Amylase levels > 3 x normal very suggestive of pancreatitis • May be normal in chronic pancreatitis!!! – Enzyme level severity – False (-): acute on chronic (Et. OH); Hyper. TG – False (+): renal failure, other abdominal or salivary gland process, acidemia • lipase – More sensitive & specific than amylase
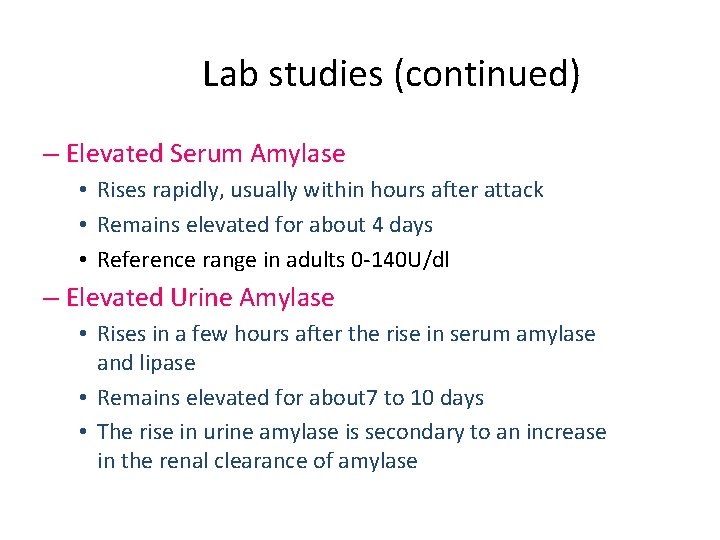
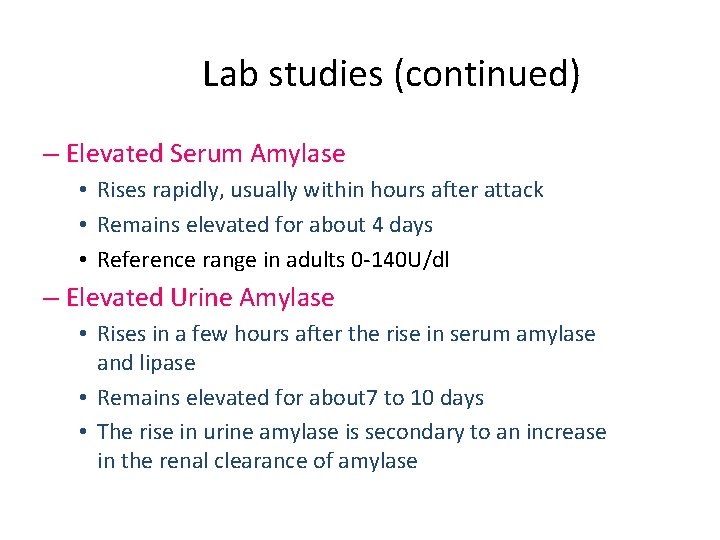
Lab studies (continued) – Elevated Serum Amylase • Rises rapidly, usually within hours after attack • Remains elevated for about 4 days • Reference range in adults 0 -140 U/dl – Elevated Urine Amylase • Rises in a few hours after the rise in serum amylase and lipase • Remains elevated for about 7 to 10 days • The rise in urine amylase is secondary to an increase in the renal clearance of amylase
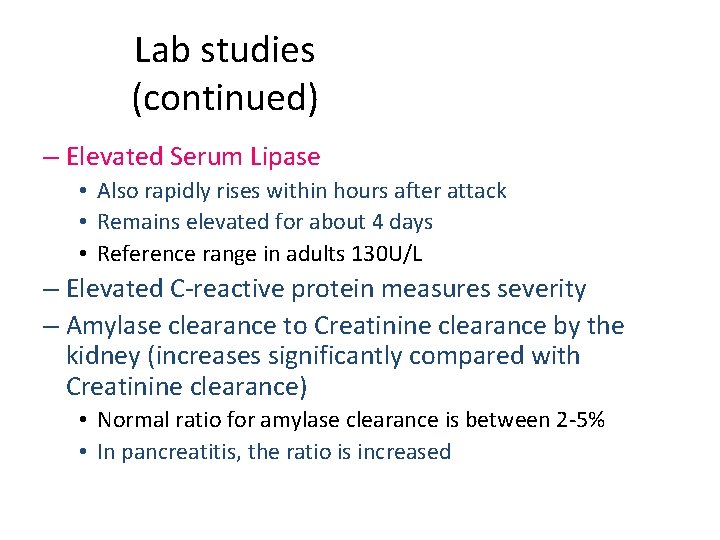
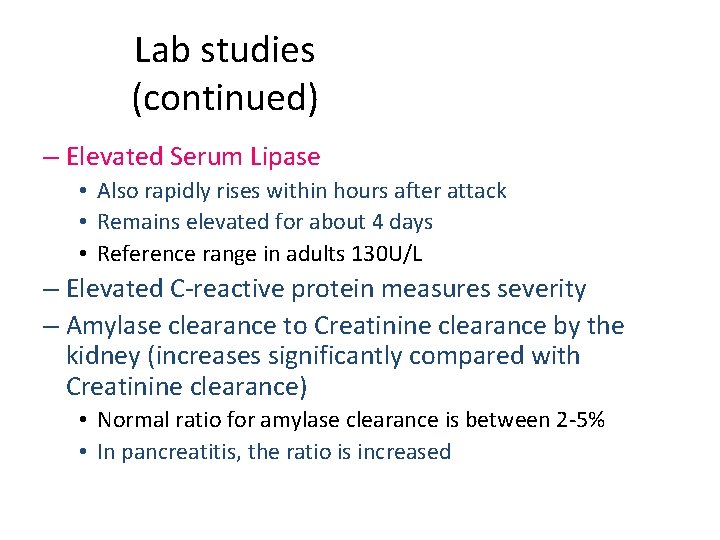
Lab studies (continued) – Elevated Serum Lipase • Also rapidly rises within hours after attack • Remains elevated for about 4 days • Reference range in adults 130 U/L – Elevated C-reactive protein measures severity – Amylase clearance to Creatinine clearance by the kidney (increases significantly compared with Creatinine clearance) • Normal ratio for amylase clearance is between 2 -5% • In pancreatitis, the ratio is increased
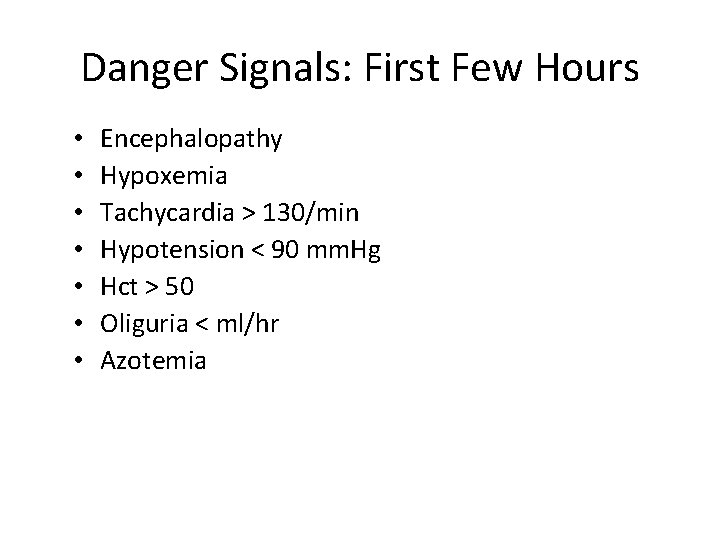
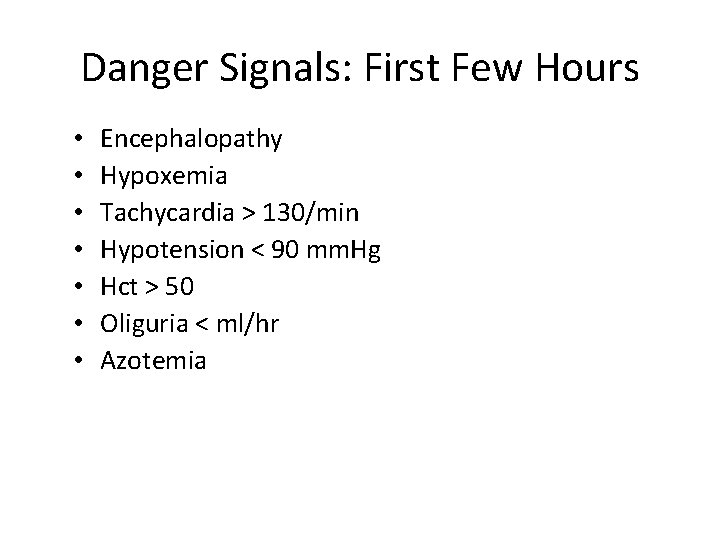
Danger Signals: First Few Hours • • Encephalopathy Hypoxemia Tachycardia > 130/min Hypotension < 90 mm. Hg Hct > 50 Oliguria < ml/hr Azotemia
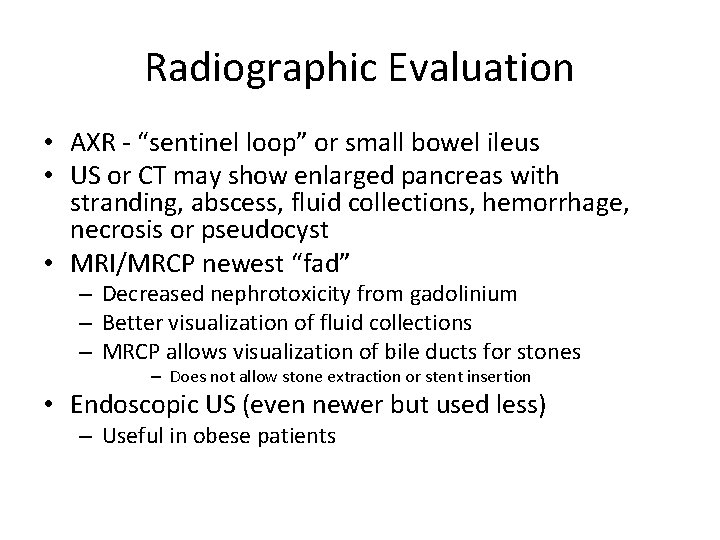
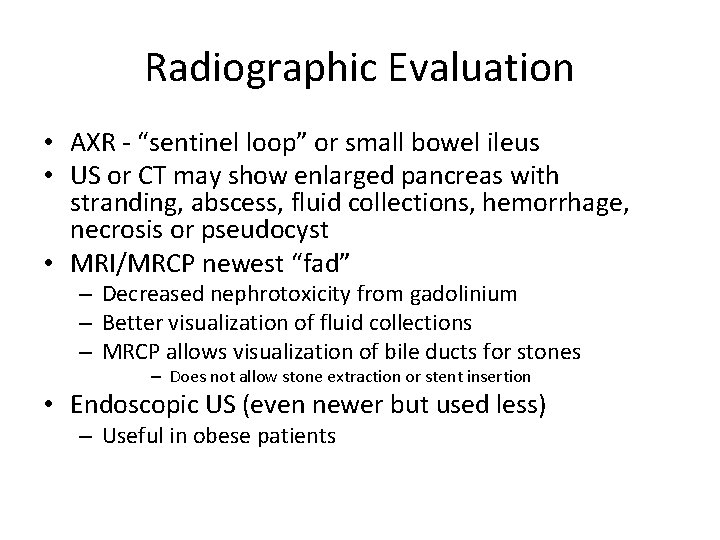
Radiographic Evaluation • AXR - “sentinel loop” or small bowel ileus • US or CT may show enlarged pancreas with stranding, abscess, fluid collections, hemorrhage, necrosis or pseudocyst • MRI/MRCP newest “fad” – Decreased nephrotoxicity from gadolinium – Better visualization of fluid collections – MRCP allows visualization of bile ducts for stones – Does not allow stone extraction or stent insertion • Endoscopic US (even newer but used less) – Useful in obese patients
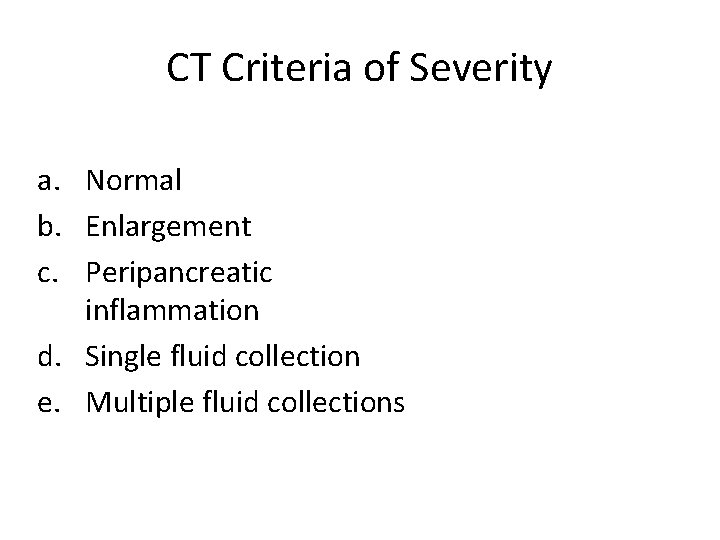
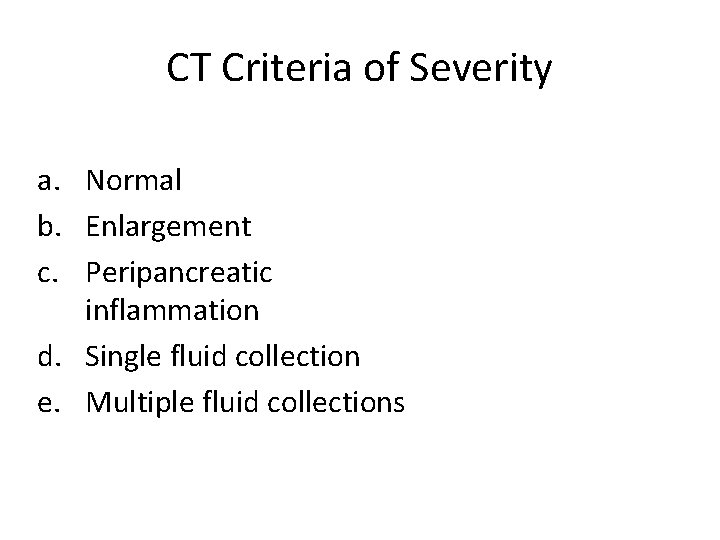
CT Criteria of Severity a. Normal b. Enlargement c. Peripancreatic inflammation d. Single fluid collection e. Multiple fluid collections
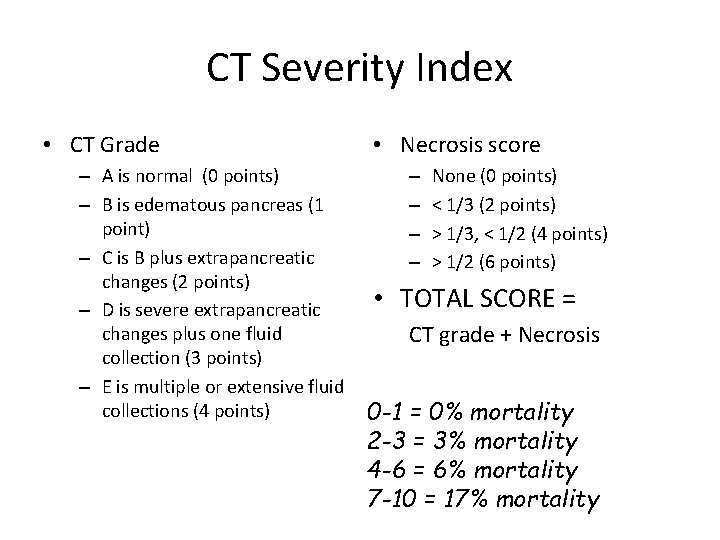
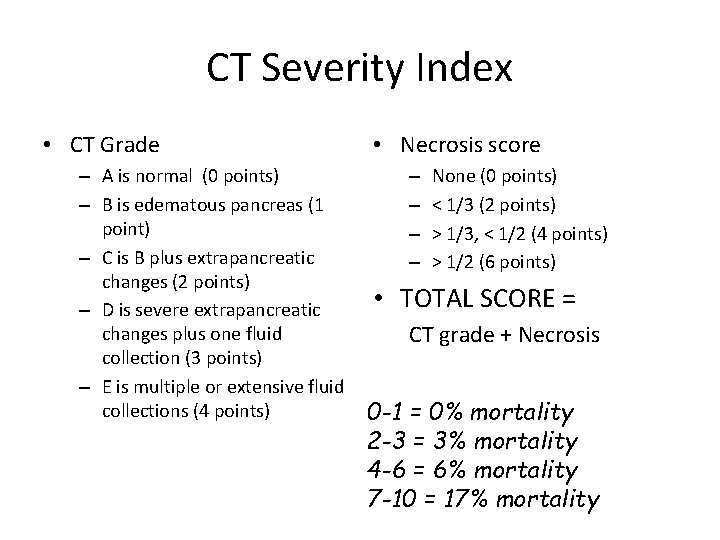
CT Severity Index • CT Grade – A is normal (0 points) – B is edematous pancreas (1 point) – C is B plus extrapancreatic changes (2 points) – D is severe extrapancreatic changes plus one fluid collection (3 points) – E is multiple or extensive fluid collections (4 points) • Necrosis score – – None (0 points) < 1/3 (2 points) > 1/3, < 1/2 (4 points) > 1/2 (6 points) • TOTAL SCORE = CT grade + Necrosis 0 -1 = 0% mortality 2 -3 = 3% mortality 4 -6 = 6% mortality 7 -10 = 17% mortality
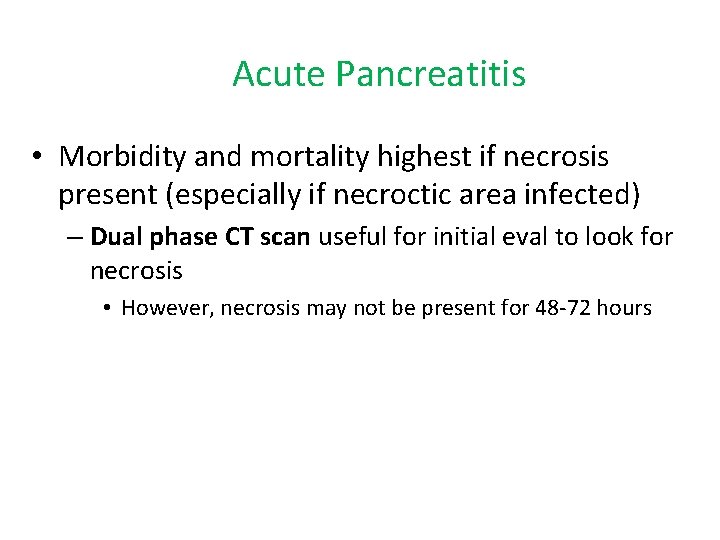
Acute Pancreatitis • Morbidity and mortality highest if necrosis present (especially if necroctic area infected) – Dual phase CT scan useful for initial eval to look for necrosis • However, necrosis may not be present for 48 -72 hours
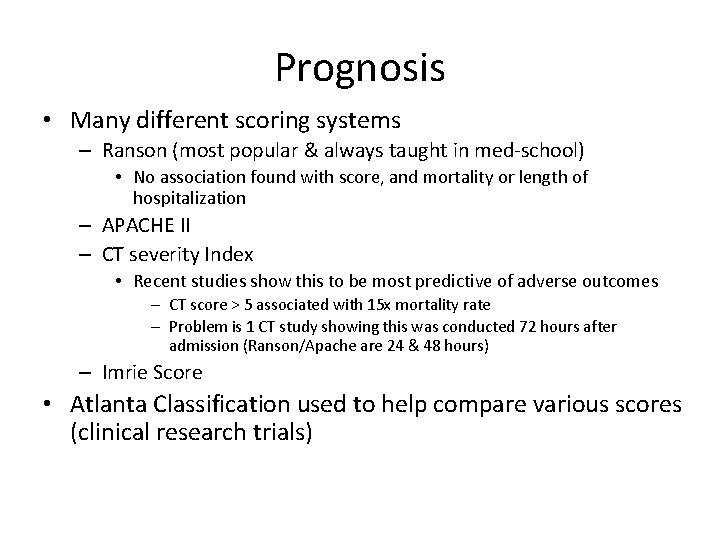
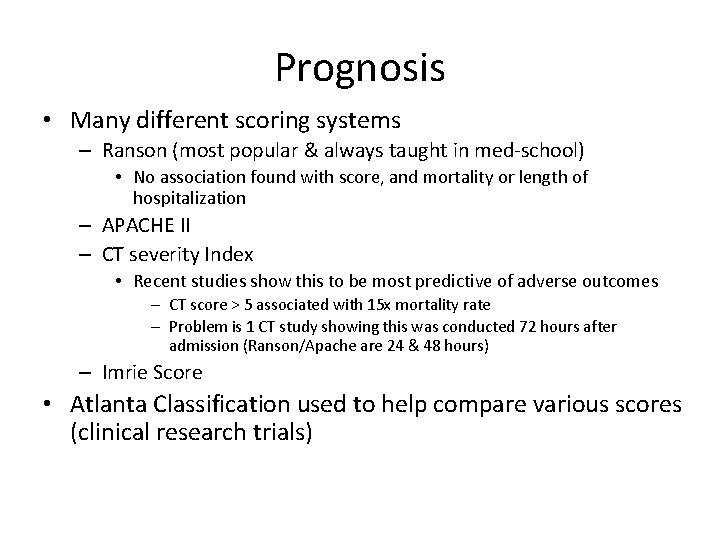
Prognosis • Many different scoring systems – Ranson (most popular & always taught in med-school) • No association found with score, and mortality or length of hospitalization – APACHE II – CT severity Index • Recent studies show this to be most predictive of adverse outcomes – CT score > 5 associated with 15 x mortality rate – Problem is 1 CT study showing this was conducted 72 hours after admission (Ranson/Apache are 24 & 48 hours) – Imrie Score • Atlanta Classification used to help compare various scores (clinical research trials)
Assessment of Severity • Ranson Criteria • Modified Glasgow Criteria • APACHE II • SAPS • Clinical Staging System
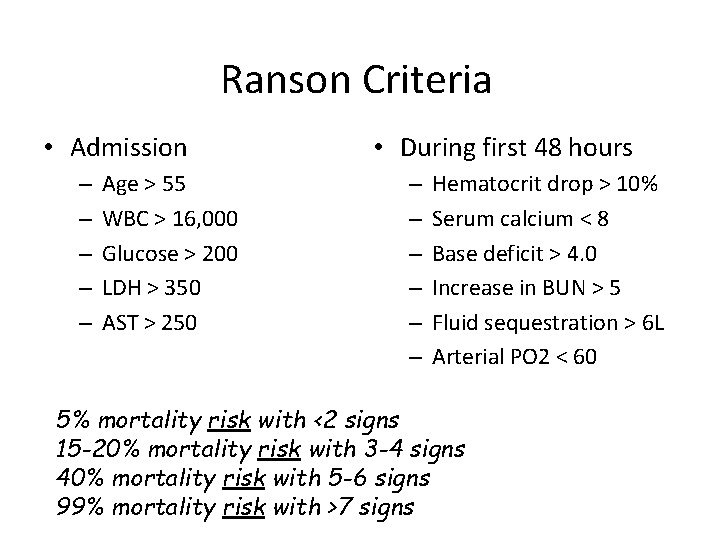
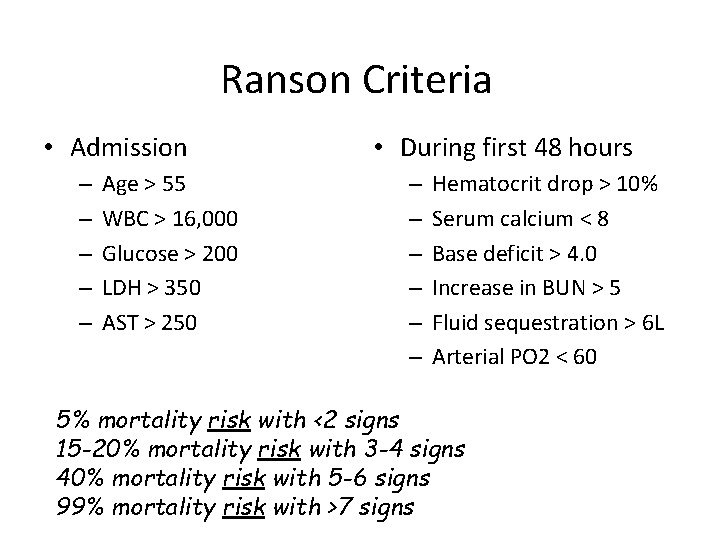
Ranson Criteria • Admission – – – Age > 55 WBC > 16, 000 Glucose > 200 LDH > 350 AST > 250 • During first 48 hours – – – Hematocrit drop > 10% Serum calcium < 8 Base deficit > 4. 0 Increase in BUN > 5 Fluid sequestration > 6 L Arterial PO 2 < 60 5% mortality risk with <2 signs 15 -20% mortality risk with 3 -4 signs 40% mortality risk with 5 -6 signs 99% mortality risk with >7 signs
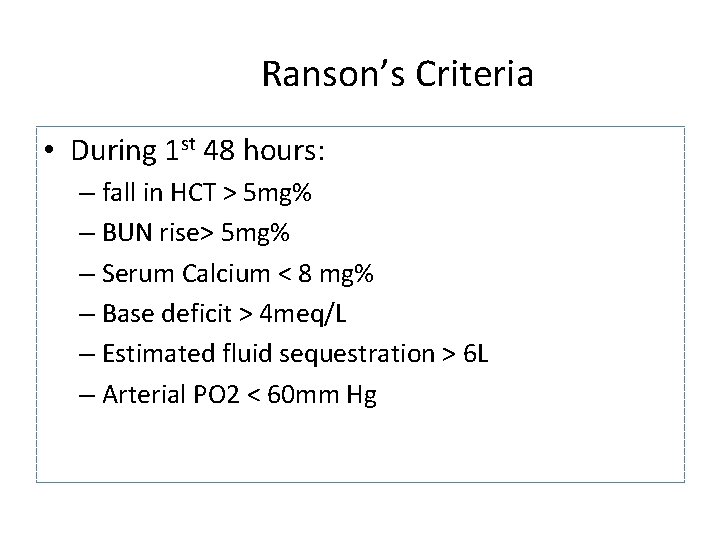
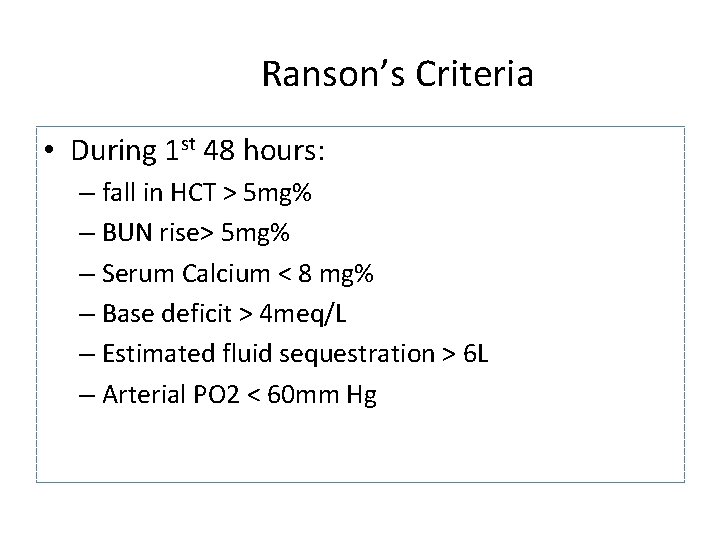
Ranson’s Criteria • During 1 st 48 hours: – fall in HCT > 5 mg% – BUN rise> 5 mg% – Serum Calcium < 8 mg% – Base deficit > 4 meq/L – Estimated fluid sequestration > 6 L – Arterial PO 2 < 60 mm Hg
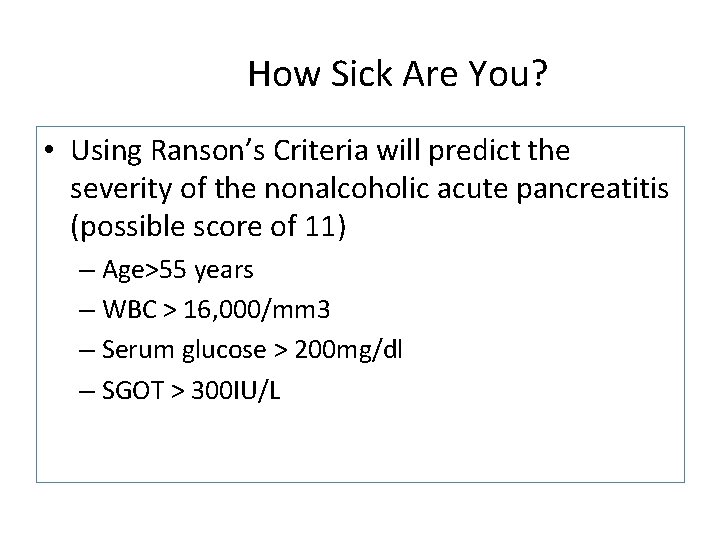
How Sick Are You? • Using Ranson’s Criteria will predict the severity of the nonalcoholic acute pancreatitis (possible score of 11) – Age>55 years – WBC > 16, 000/mm 3 – Serum glucose > 200 mg/dl – SGOT > 300 IU/L
Ranson’s Criteria • Relation to morbidity/mortality – 2 or fewer signs: 1% mortality – 3 signs: severe pancreatitis – 3 -4 signs: 15% mortality – 5 -6 signs: 40% mortality – More than 6 signs: better ask for the priest for fire proofing!!
Acute Pancreatitis • Goal of treatment is to stop autodigestion • Prevent systemic complications – Maintain hemodynamic stability • Monitor BP, urine output, and peripheral circulation • PA catheter if needed • Parenteral fluids, fluid resuscitation if needed (Crystalloids, colloids, blood if needed) • May require vasoactive drugs (Dopamine) to increase SVR
Therapy • Remove offending agent (if possible) • Supportive !!! • #1 - NPO (until pain free) – NG suction for patients with ileus or emesis – TPN may be needed • #2 - Aggressive volume repletion with IVF – Keep an eye on fluid balance/sequestration and electrolyte disturbances
Therapy continued • #3 - Narcotic analgesics usually necessary for pain relief…textbooks say Meperidine… – NO conclusive evidence that morphine has deleterious effect on sphincter of Oddi pressure • #4 - Urgent ERCP and biliary sphincterotomy within 72 hours improves outcome of severe gallstone pancreatitis – Reduced biliary sepsis, not actual improvement of pancreatic inflammation • #5 - Don’t forget PPI to prevent stress ulcer
Acute Pancreatitis – Improve oxygenation • Supplemental oxygen • May need mechanical ventilation (ARDS) • Monitor Sp. O 2 via pulse ox • Monitor lung sounds • Suction if rhonchi present • Assume Fowler’s position if in compromise – Promotes maximum lung expansion • Watch for atelectasis or hypoxia • Encourage cough and deep breath, walk to maintain lung function
Acute Pancreatitis – Maintain metabolic balance • Monitor for electrolyte imbalances such as hypokalemia and hypocalcemia (assess for Chvostek’s and Trousseau’s sign) • Watch for arrhythmias • Watch glucose, may need insulin • Monitor BUN and Creatinine • Follow amylase and lipase levels • Obtain daily albumin levels
Acute Pancreatitis – Pain management • Narcotics to relieve pain around the clock • Demerol not MSO 4, but morphine lasts longer so. .
Pancreatitis • Nursing Interventions – Administer analgesics, antacids, anticholinergics as ordered, monitor effects – Withhold food/fluid and eliminate odor and sight of food from environment to decrease pancreatic stimulations – Maintain NG tube and assess for drainage
Pancreatitis • Nursing Interventions (continued) – Institute nonpharmacologic measures to decrease pain • Assist patient to position of comfort (knee-chest; fetal position) – Teach relaxation techniques and provide a quiet, restful environment
Patient and Family Teaching • Talk about conditions which caused illness • Importance to sticking to a bland, low-fat, high carbohydrate diet avoiding large meals and caffeine • Make sure they know the symptoms of acute pancreatitis
Pancreatitis • Nursing Interventions (continued) – Provide patient teaching and discharge planning concerning • Dietary regimen when oral intake permitted – High-carbohydrate, high-protein, low-fat diet – Eating small, frequent meals instead of 3 large ones – Avoid caffeine products – Eliminate alcohol – Maintain relaxed atmosphere after meals
Pancreatitis • Nursing Interventions (continued) – Recognition and reporting of signs of complications • • • Continued nausea and vomiting Abdominal distention with increased fullness Persistent weight loss Severe epigastric or back pain Frothy/foul-smelling bowel movements Irritability, confusion, persistent elevation of temperature (2 days)
Acute Pancreatitis • Measure all Intake and Output – Vomit, blood loss, etc. • Auscultate bowel sounds – Initially will diminish or absent • Weigh daily • Measure abdominal girth if ascites is suspected • Check oral and nasal mucosa for signs of dryness and cracking
Acute Pancreatitis – Electrolyte replacement – Reduction of pancreatic secretions • “resting the pancreas” • NPO halts pancreatic enzymes • NG tube reduces HCL in stomach • Administer histamine 2 blockers to further reduce acid • Nutritional support via TPN – Renal support – Surgical therapies – Complications prevention (pulmonary, cardiac, and renal
After the acute phase • Once subsided, BS will resume, abdominal pain will diminish, and patient should report feeling hungry – May resume eating – Clear liquids – Small carbs – No spicy foods or caffeinated beverages – No fat or high protein – May need antispasmotics, anticholinergics and antacids to reduce gastric and pancreatic juices
Complications • Necrotizing pancreatitis – Significantly increases morbidity & mortality – Usually found on CT with IV contrast • Pseudocysts – Suggested by persistent pain or continued high amylase levels (may be present for 4 -6 wks afterward) – Cyst may become infected, rupture, hemorrhage or obstruct adjacent structures • Asymptomatic, non-enlarging pseudocysts can be watched and followed with imaging • Symptomatic, rapidly enlarging or complicated pseudocysts need to be decompressed
Complications continued #2 • Infection – Many areas for concern: abscess, pancreatic necrosis, infected pseudocyst, cholangitis, and aspiration pneumonia -> SEPSIS may occur – If concerned, obtain cultures and start broad-spectrum antimicrobials (appropriate for bowel flora) – In the absence of fever or other clinical evidence for infection, prophylactic antibiotics is not indicated • Renal failure – Severe intravascular volume depletion or acute tubular necrosis may lead to ARF
Complications continued #3 • Pulmonary – Atelectasis, pleural effusion, pneumonia and ARDS can develop in severe cases • Other – Metabolic disturbances • hypocalcemia, hypomagnesemia, hyperglycemia – GI bleeds • Stress gastritis – Fistula formation
Long-term Sequelae • Chronic Pancreatitis – Characterized by chronic and progressive loss of pancreatic parenchyma – Both endocrine (DM) and exocrine (steatorrhea, azotorrhea) insufficiency develop when 80% to 90% of gland is destroyed – Pancreatic calcification (from intraductal calcium carbonate deposits) may be apparent on plain abdominal x-ray – Patients may require insulin, pancreatic enzyme replacement (Creon), and medium-chain triglycerides
Long-term Sequelae • Pseudocyst Formation – Collection of enzyme-rich pancreatic fluid and tissue debris arising within areas of necrosis – Result from the formation of granulation tissue within the pancreas – May be asymptomatic and resolve spontaneously – Treatment • Drainage • Resection • Indicated if they persist for more than 6 weeks, are enlarging, or are symptomatic
Prognosis • 85 -90% mild, self-limited – Usually resolves in 3 -7 days • 10 -15% severe requiring ICU admission – Mortality may approach 50% in severe cases
Long-term Sequelae • Pleural Fistulas and Pancreatic Ascities – Result from pancreatic fluid entering pleural space or abdomen – Treatment includes: • Repeated aspiration • Diuretics • Carbonic anhydrase inhibitors • Surgical resection
Chronic pancreatitis • Pathophys - irreversible parenchymal destruction leading to pancreatic dysfunction • • • Persistent, recurrent episodes of severe pain Anorexia, nausea Constipation, flatulence Steatorrhea Diabetes
Chronic pancreatitis • #1 - etiology is chronic Et. OH abuse (90%) • Gallstones • Hyperparathyroidism • Congenital malformation (pancreas divisum) • Idiopathic • MRCP of pancreas divisum
Evaluation • or normal amylase and lipase • Plain AXR / CT may show calcified pancreas • Pain management critical – Et. OH cessation may improve pain – Narcotic dependency is common
Complications • Exocrine insufficiency typically manifests as weight loss and steatorrhea – If steatorrhea present, a trypsinogen level < 10 is diagnostic for chronic pancreatitis – Manage with low-fat diet and pancreatic enzyme supplements (Pancrease, Creon) • Endocrine insufficiency may result from islet cell destruction which leads to diabetes
Conclusion • Pancreatitis is common – YOU WILL SEE IT!!! • 10 -15% are severe = ICU admission – Mortality may approach 50% in severe cases • These are the cases where knowing future complications would be great (ie finding a marker that correlates with severity…and that’s what the clinical researchers are attempting to do)
 Cullen's sign
Cullen's sign Acg chronic pancreatitis
Acg chronic pancreatitis Pancreatitis nursing
Pancreatitis nursing Nursing care plan for acute pancreatitis
Nursing care plan for acute pancreatitis Chronic pancreatitis
Chronic pancreatitis 5 signs of inflammation
5 signs of inflammation Common chronic and acute conditions chapter 18
Common chronic and acute conditions chapter 18 Pattern of acute inflammation
Pattern of acute inflammation Leukemia death rate
Leukemia death rate Periradicular disease definition
Periradicular disease definition Pes statement for acute pancreatitis
Pes statement for acute pancreatitis What activates trypsinogen
What activates trypsinogen Criteria of acute pancreatitis
Criteria of acute pancreatitis Acute pancreatitis ct
Acute pancreatitis ct Dr rista
Dr rista Ranson criteria for acute pancreatitis
Ranson criteria for acute pancreatitis Carnett test
Carnett test Acute pancreatitis pathophysiology
Acute pancreatitis pathophysiology Topgl
Topgl Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Acute subacute chronic
Acute subacute chronic Gallbladder adenocarcinoma
Gallbladder adenocarcinoma Acute vs chronic heart failure
Acute vs chronic heart failure What makes hard water hard pre lab answers
What makes hard water hard pre lab answers Work hard play hard make history
Work hard play hard make history Hard times hard drive
Hard times hard drive Willow cabin speech
Willow cabin speech One god one empire one religion
One god one empire one religion One one one little dogs run
One one one little dogs run One king one law one faith
One king one law one faith Byzantine definition
Byzantine definition One ford behaviors
One ford behaviors See one do one teach one
See one do one teach one See one, do one, teach one
See one, do one, teach one Studiendekanat uni bonn
Studiendekanat uni bonn One vision one identity one community
One vision one identity one community One vision one identity one community
One vision one identity one community Uti and pancreatitis
Uti and pancreatitis Location of pancreas
Location of pancreas Liver and pancreas function
Liver and pancreas function Pharynx in digestive system
Pharynx in digestive system Pancreas anatomy and physiology
Pancreas anatomy and physiology Pancreasitis
Pancreasitis Liver lobules
Liver lobules Pancreas anatomy histology
Pancreas anatomy histology Pineal and pancreas glands
Pineal and pancreas glands Gastric gland
Gastric gland Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worm breton
Tư thế worm breton Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 101012 bằng
101012 bằng Phản ứng thế ankan
Phản ứng thế ankan