Key Performance Indicators for Revenue Cycle Management National
















- Slides: 95

Key Performance Indicators for Revenue Cycle Management National Family Planning and Reproductive Health Association - Regional Meeting Tampa, Florida January 12, 2015 presenter: Nancy Smit, MBA, RPT, RRT President and CEO SHR ASSOCIATES, INC.
Since 1981, SHR Associates, Inc. (SHR) has been dedicated to providing physicians and practice managers with the business tools and resources necessary to operate successfully in today’s ever-changing health care environment. 2 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
“What gets measured, gets managed” Peter F. Drucker writer, professor, management consultant and self-described “social ecologist” 3 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Outline of Today’s Presentation Overview of the Revenue Cycle Management Process Key Performance Indicators to Ensure Peak Financial Performance Using Key Performance Indicators for Process Improvement Additional References and Resources 4 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

K P I 5 Performance improvement, particularly within the revenue cycle, is dependent upon consistent monitoring of Key Performance Indicators (KPI) along with effective management that includes accountability throughout the organization. www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
K P I 6 To assure successful and compliant billing, everyone involved in the billing cycle process needs to be familiar with each step of the encounter. Billing requires a “team effort”. www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Encounter An encounter should be created for each client visit. The flow of the encounter begins at the time of scheduling and flows through the billing and collection process. 7 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Encounter The encounter is not complete until the charges have been reconciled by posting the associated payments and/or adjustments. 8 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process The Components of Revenue Cycle Process Front-end Operations § § § § 9 Appointment scheduling Pre-registration and authorization Reminder call Registration/check-in Eligibility verification Visit: Charge capture and coding Check-out Reconciliation processes www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process The Components of Revenue Cycle Process Back-end Operations § § § 10 Claim submission Clearinghouse Remittance/Payment posting Claims Follow-up and A/R management Patient bill Benchmarking/KPI www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Appointment Scheduling The first step of the encounter involves making the appointment and setting up the account to prepare for billing and patient contact. If the appointment is scheduled incorrectly, the patient may be dissatisfied and revenue may be lost. 11 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Overview of the Revenue Cycle Management Process Appointment Scheduling Electronic systems for appointments greatly facilitate the appointment scheduling process and help to ensure that complete demographic and insurance information is obtained. If possible, assigning staff to collect detailed information from the patient prior to the appointment will greatly facilitate the check-in process. 12 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Pre-registration and Authorization Using the information collected at the time of scheduling to verify eligibility and obtain authorization for the appointment (or specific services) helps to identify missing or inaccurate information and ensure that services requiring pre-authorization are covered and paid. 13 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Pre-registration and Authorization Pre-authorization and eligibility for most payers today can be accomplished online and most state-of- the-art practice management (PM) systems have the capability for automated pre-authorization and eligibility verification. 14 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Reminder Calls Contacting the patients to remind them of their upcoming appointment greatly reduces the chances for a no-show and provides an opportunity to discuss payment issues. Most PM systems today have the capability to automate patient reminder and follow-up calls. 15 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Overview of the Revenue Cycle Management Process Registration/Check-in The registration/check-in process provides the opportunity to verify the patient’s identity and insurance information and confirm the reason for the visit. Due to the complexities of the various insurance plan requirements and coverage, front office staff need to be well-trained and provided with quick reference materials on all insurance plans in which the organization participates. 16 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Key Steps for Time of Service Registration § Complete patient registration forms § Complete HIPAA forms § Copy/scan insurance cards and photo ID § Collect copayment and any outstanding balances 17 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Eligibility Verification The information provided at check-in should be used to verify eligibility. Even if this process has been done prior to the visit, this step is important to verify that the coverage is active at the time of service. 18 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Eligibility Verification This process also identifies the amount that the patient is obligated to pay for deductibles, co-payments or co-insurance. Arranging for collecting these payments from the patient at check-in greatly improves the ability of the clinic to obtain those funds. Eligibility verification can now be done directly through most PM systems. If your system does not have this capability, eligibility can be verified through the payer websites. 19 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
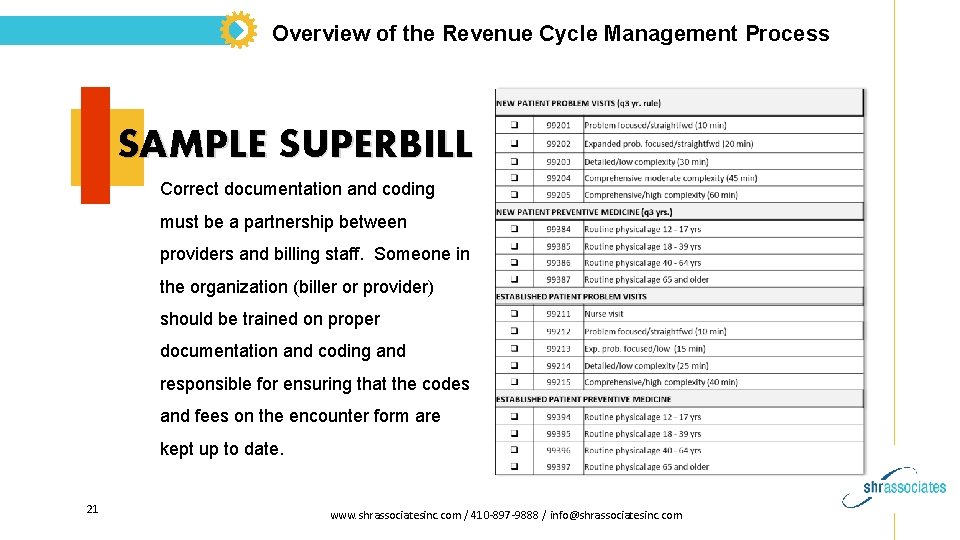
Overview of the Revenue Cycle Management Process Charge Capture and Coding All clinical services need to be properly documented, coded and captured as charges for billing. Organizations should utilize an encounter form/superbill/charge ticket in either a paper or electronic format. 20 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
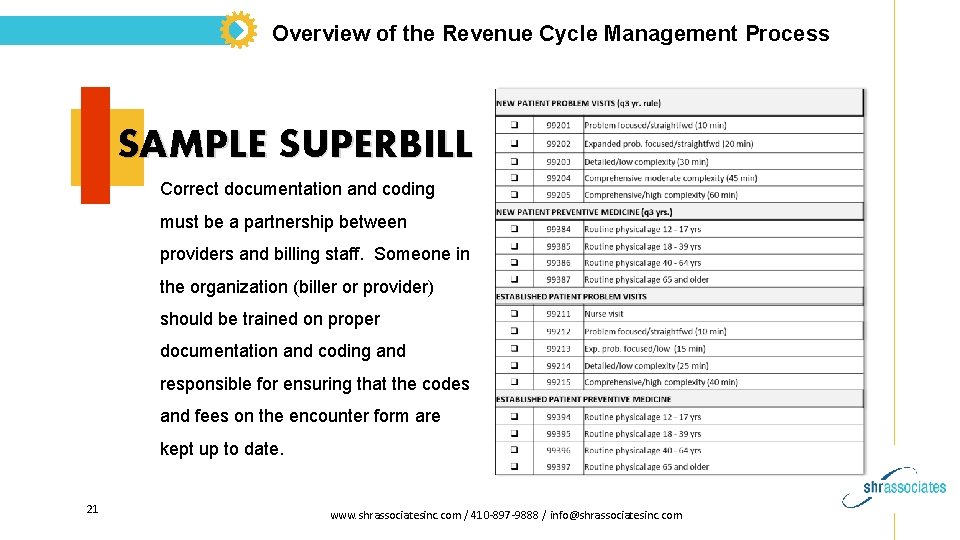
Overview of the Revenue Cycle Management Process SAMPLE SUPERBILL Correct documentation and coding must be a partnership between providers and billing staff. Someone in the organization (biller or provider) should be trained on proper documentation and coding and responsible for ensuring that the codes and fees on the encounter form are kept up to date. 21 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Charge Capture & Reconciliation § Use visit tracking reports to identify no-shows, missed charges. § Reconcile posted charges to source documents, e. g. , encounter forms (superbills). § Reconcile encounters to patient sign-in sheets. § Reconcile service volumes to external resources, e. g. , lab logs. § Reconcile to inventory control for injectables and other billable supplies. § Post charges within 24 hours of service. 22 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Claims Submission This is the process of preparing and submitting the claim to a clearinghouse or directly to the payers. All charges and codes should be reviewed to verify that charges are captured and posted correctly. Most PM systems have a “review” feature that identifies errors or omissions on the claims prior to submission (claims scrubbers or edit functions). The organization should have a written procedure for claims submission that includes a schedule for the timing of claims submission (i. e. daily, weekly). 23 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Clearing House A clearing house is a private company that provides connectivity between physicians, billing entities, health insurers and other health care partners for transmission and translation of claims (primarily electronic). Information is changed into the specific format that health insurer requires. 24 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Clearing House Clearinghouses may contract with or act on behalf of one of a number of health insurers or may contract with medical practices to transmit and/or translate claims information. Sample Clearinghouses: Emdeon (Web. MD), Payer. Path, Mc. Kesson 25 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Remittance Advice and Payment Posting Clean claims will be either be paid, applied to co-insurance or deductibles, or denied. The Remittance Advice (RA) or Explanation of Benefits (EOB) sent from the payer explains how payments or denials were applied. Whenever possible, arrangements should be made with the payer for electronic remittance (ERA) and electronic funds transfer (EFT). 26 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Electronic EOB/RAs are obtained by: 1. Going to the insurance carrier’s website and printing the EOB/RA 2. Electronic Remittance Advice (ERA) which download into the Practice’s medical billing software and is posted electronically to the patient account 27 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Insurance Reimbursement: Payment is either: § Mailed check § EFT - electronic funds transfer: electronically sent to the bank § Credit Card Voucher is mailed to the Practice 28 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Insurance Reimbursement: Failing to post payments and denials in a timely manner results in the clinic’s inability to effectively manage the accounts receivable (AR) and reconcile billing. 29 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Claims Follow-up and A/R Management This is the process of tracking claims that have been submitted to ensure that proper payment is received. Appropriate action (resubmission, appeal or write-off) must be taken on claims that are either denied, not paid in full or not responded to by the payer. 30 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Claims Follow-up and A/R Management Many denied claims contain easily corrected errors. Those claims should be modified and resubmitted for approval and payment. Correcting and resubmitting claims in a timely manner will reduce “days in A/R” and help to avoid denials due to untimely filing limits. 31 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Patient Billing Patients may need to be billed after their insurance has responded and/or if they are uninsured or do not wish to bill their insurance. It is very important to ensure compliance with payer requirements before billing patients. 32 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Patient Billing Statements should be generated on a regular basis (weekly, 2 – 3 times/month). With many PM systems today, patient statements can be generated electronically which can be very cost-effective and allows the clinic to use their internal staff for other tasks. 33 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Patient Billing There should be clear, written policies and procedures for the patient billing and collection process, including when balances should be billed to patients and how many statement should be sent before sending the account to collections, if appropriate. 34 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Overview of the Revenue Cycle Management Process Benchmarking and KPI Establishing benchmarks and tracking key performance indicators helps the organization establish goals, monitor performance and make improvements. If you don’t monitor your revenue cycle management process, you don’t know where you stand or if your processes are effective. 35 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Cash flow is just one factor in the financial health of a health care organization. To determine how effective your revenue cycle process is, there are other important metrics that should be measured and monitored. Management should determine what the Key Performance Indicators are for their organizations and monitor them on monthly basis. In most cases, many of these metrics can obtained directly from your PM/billing system. 36 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
A standard set of monthly management reports should be identified and consistently run at each month-end. The monthly results should be reported and compared to prior months and year-to-date. They should also be compared to benchmarks and goals set by the organization, as appropriate. 37 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
BREAK 38 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Key Performance Indicators (KPI) For Peak Financial Performance Benchmarking and KPI Establishing benchmarks and tracking key performance indicators helps the organization establish goals, monitor performance and make improvements. If you don’t monitor your revenue cycle management process, you don’t know where you stand or if your processes are effective. 39 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance Summary of Key Performance Indicators (KPI) Total charges overall and by provider Total new and established patient visits Days in accounts receivable (A/R) Aged accounts receivable (A/R) Collection rate/ratio Claims denial rate 40 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance Once your organization has determined what KPIs to measure, it may be helpful to meet with your PM vendor and/or IT support to determine which reports to run and how best to obtain this information from your system. 41 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
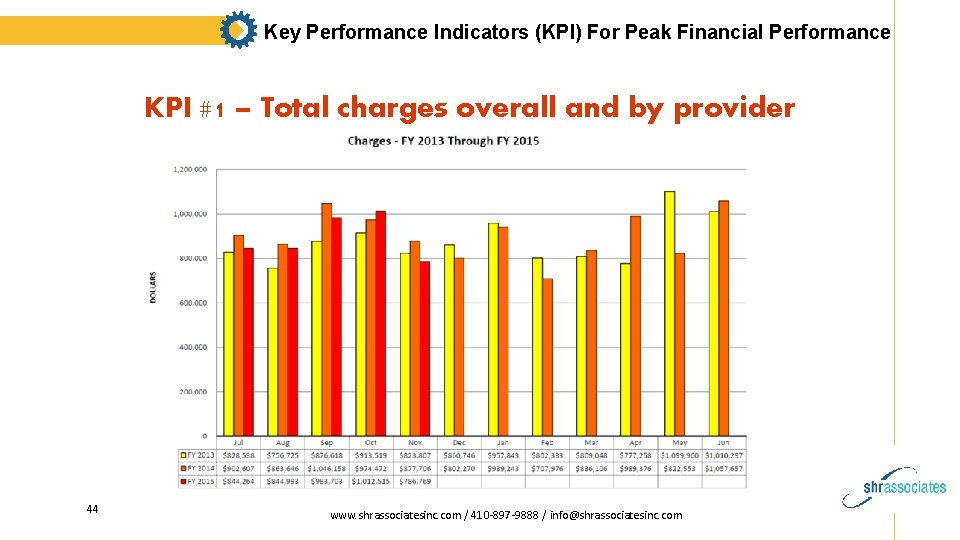
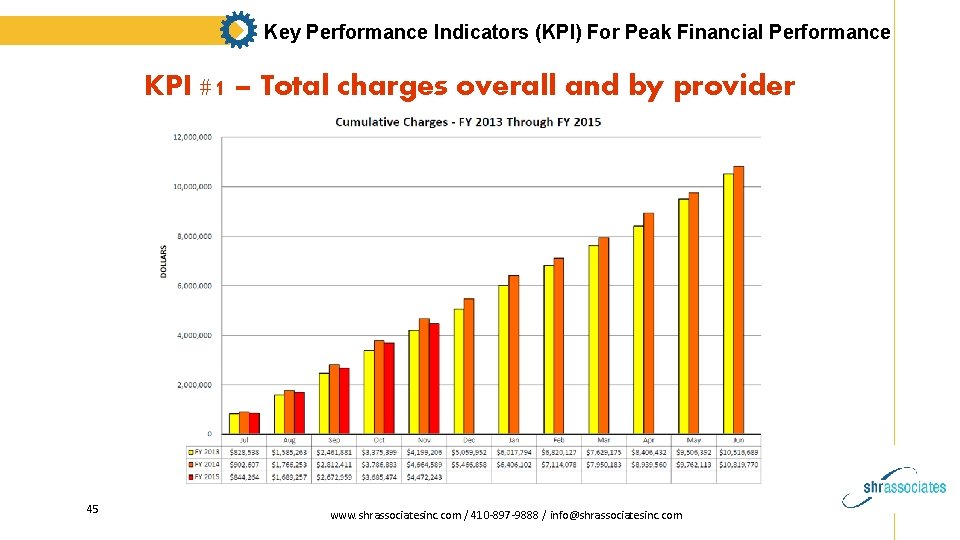
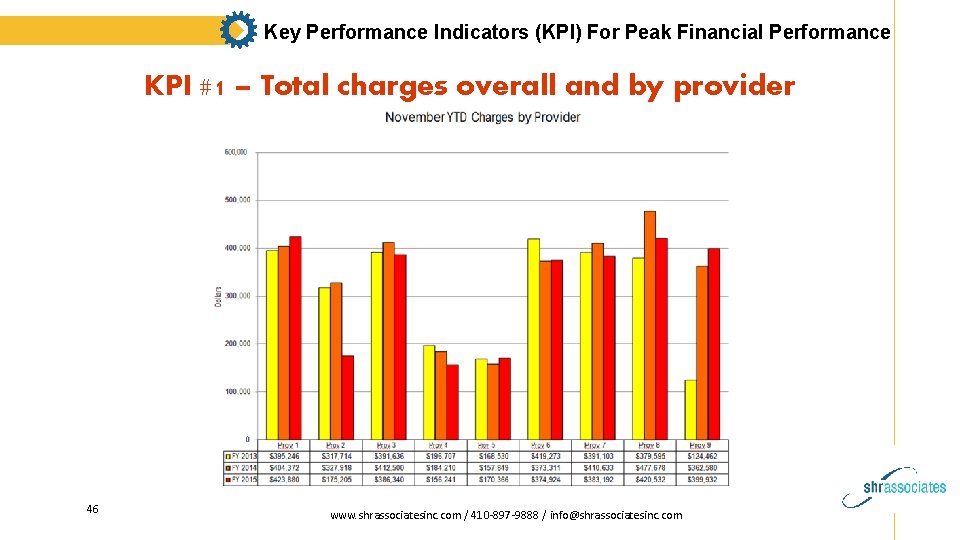
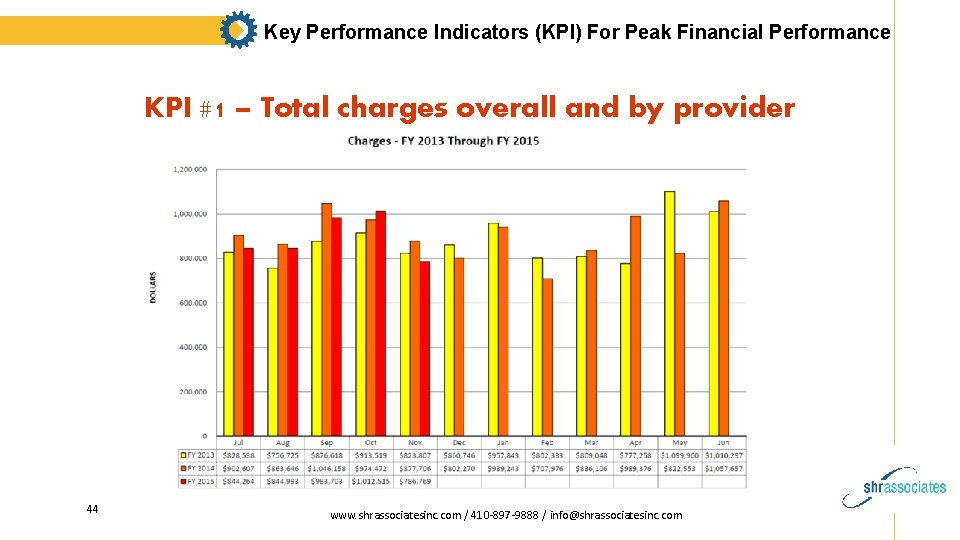
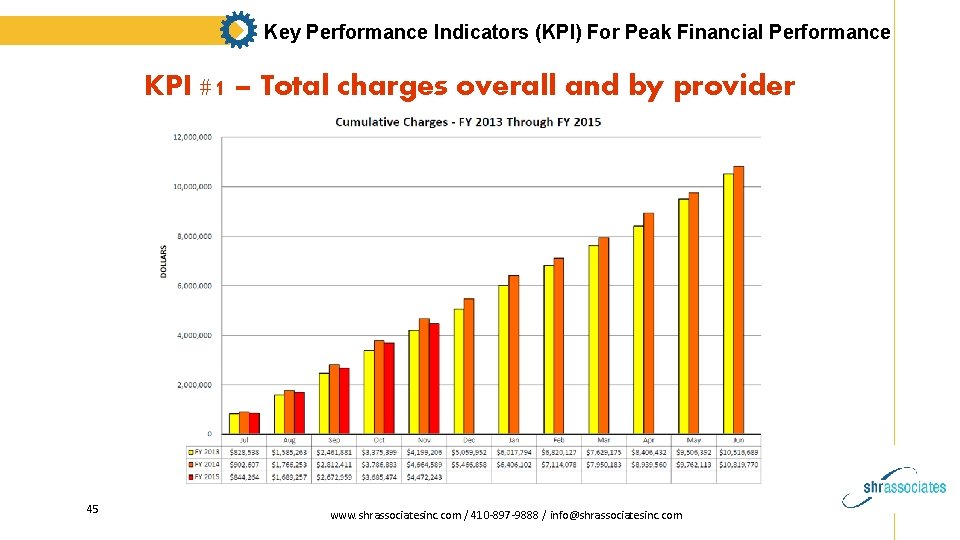
Key Performance Indicators (KPI) For Peak Financial Performance KPI #1 – Total charges overall and by provider Total monthly charges will be reported in most PM systems as long as each month’s activity is formally closed at month-end. If the internal files of your PM system have been set up properly, total charges by provider should also be available 42 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
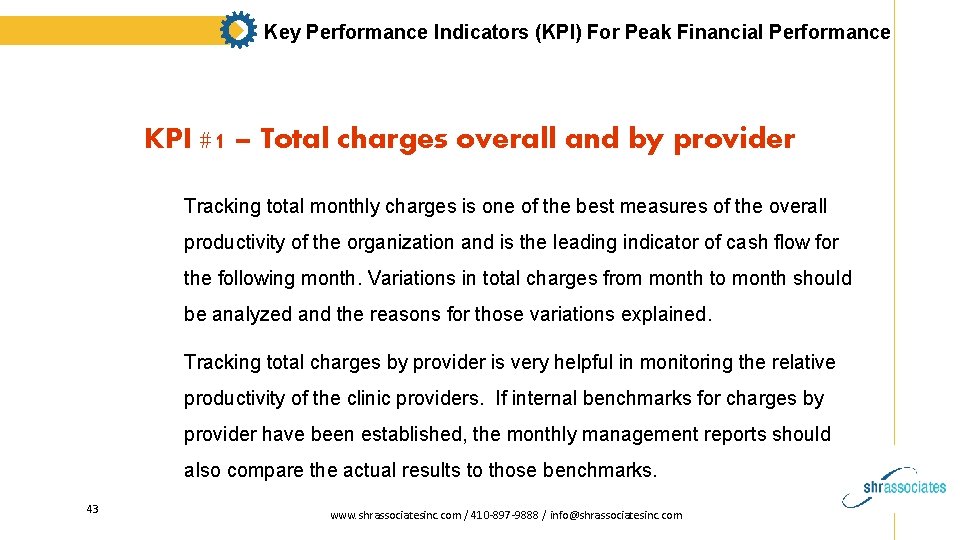
Key Performance Indicators (KPI) For Peak Financial Performance KPI #1 – Total charges overall and by provider Tracking total monthly charges is one of the best measures of the overall productivity of the organization and is the leading indicator of cash flow for the following month. Variations in total charges from month to month should be analyzed and the reasons for those variations explained. Tracking total charges by provider is very helpful in monitoring the relative productivity of the clinic providers. If internal benchmarks for charges by provider have been established, the monthly management reports should also compare the actual results to those benchmarks. 43 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #1 – Total charges overall and by provider 44 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #1 – Total charges overall and by provider 45 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #1 – Total charges overall and by provider 46 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #2 - Total new and established patient visits Although it is not considered a metric for the effectiveness of your revenue cycle and billing process, tracking new and established patient visits on a consistent and comparative basis will help your organization project both current and future demand for services. 47 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Key Performance Indicators (KPI) For Peak Financial Performance KPI #2 - Total new and established patient visits Most organizations have internal benchmarks for monthly visit volumes and use the actual results to discuss marketing strategies and make important management decisions if the goals are not being achieved. 48 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #3 – Days in Accounts Receivable (A/R) Days in accounts receivable measures how long it takes for a service to be paid. It is perhaps the single most important revenue cycle metric. There are three simple steps to calculating days in A/R: Step 1: Determine the total amount of the organization’s accounts receivable. Subtract from that total any credits/funds owed by the clinic to others. 49 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Key Performance Indicators (KPI) For Peak Financial Performance KPI #3 – Days in Accounts Receivable (A/R) Step 2: Determine the average daily charge by dividing the total charges for the past 12 months by 365 days. This measure should be recalculated on a quarterly basis to account for any changes in volume and/or productivity. 50 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #3 – Days in Accounts Receivable (A/R) Step 3: Divide the total A/R (Step 1) by the average daily charge amount (Step 2) 51 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #3 – Days in Accounts Receivable (A/R) The formula looks like this: Total current A/R minus credits divided by the average daily charge amount = Days in A/R On average, an A/R greater than 50 days generally indicates the need for improvement. Practices typically see A/R of 35 – 50 days, with top performing practices with A/R of less than 35 days. 52 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #3 – Days in Accounts Receivable (A/R) Some organizations prefer to track this A/R metric in average months rather than average days. Monthly charges are typically already tracked and easy to compute. If average monthly charges are divided into the total A/R, the industry benchmark is 1. 5 Months in A/R or less. 53 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #3 – Days in Accounts Receivable (A/R) Again, remember to recalculate your organization’s average daily or average monthly charges at least quarterly to account for fluctuations in the demand for services (up or down). 54 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #3 – Days in Accounts Receivable (A/R) Measuring and monitoring days in A/R can help signal several areas of underperformance that should be watched including: - Payer specific delays - Delays in follow-up on the A/R by the billing team Payer specific delays means that the overall days in A/R may be 45 days, but Medicaid claims might average 75 days and warn of a problem that needs attention 55 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Key Performance Indicators (KPI) For Peak Financial Performance KPI #3 – Days in Accounts Receivable (A/R) Delays in follow-up on the A/R by the billing team are common. A/R follow-up is often the area of least attention (after charge entry, claim submission and payment posting) when staffing is limited or the organization has not established structured procedures for the working of the A/R. 56 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #4 – Aged Accounts Receivable (A/R) This KPI is an equally important measure to days in A/R because good overall days in A/R can hide elevated amount in the older aging buckets (e. g. , 90 – 120 days or older). Tracking the aged accounts receivable monthly will help the organization determine if it is receiving timely payment. This report is a standard report in most PM systems and should be run overall and by payer, including patient pay. 57 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
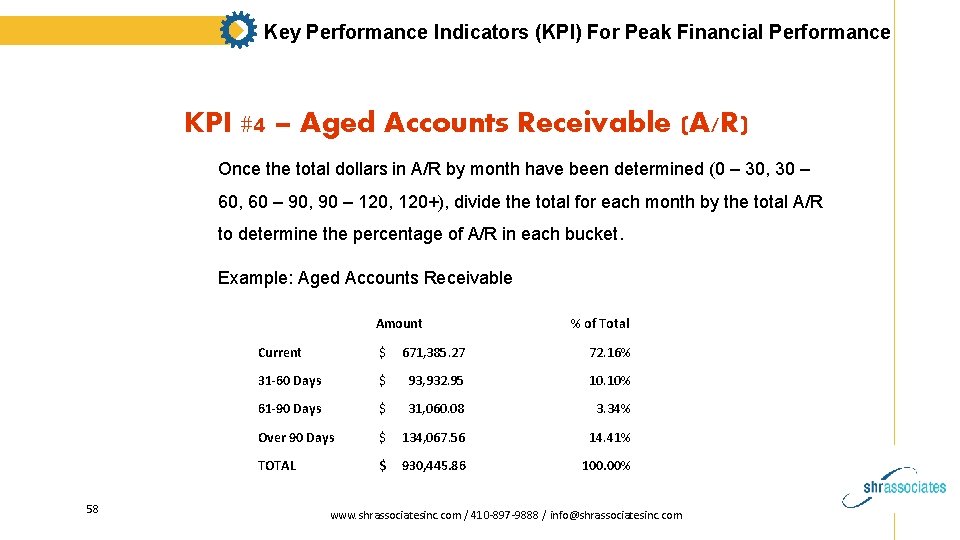
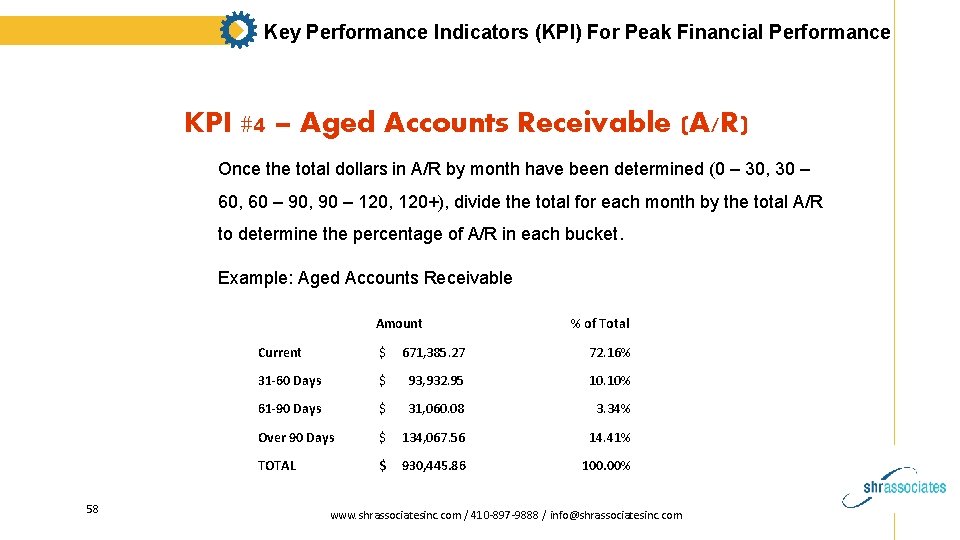
Key Performance Indicators (KPI) For Peak Financial Performance KPI #4 – Aged Accounts Receivable (A/R) Once the total dollars in A/R by month have been determined (0 – 30, 30 – 60, 60 – 90, 90 – 120, 120+), divide the total for each month by the total A/R to determine the percentage of A/R in each bucket. Example: Aged Accounts Receivable Amount 58 % of Total Current $ 671, 385. 27 72. 16% 31 -60 Days $ 93, 932. 95 10. 10% 61 -90 Days $ 31, 060. 08 3. 34% Over 90 Days $ 134, 067. 56 14. 41% TOTAL $ 930, 445. 86 100. 00% www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #4 – Aged Accounts Receivable (A/R) On average, if a practice has more than 20% of the total A/R 90 days or older, it signals a problem. The detail of the accounts in the over 90 day A/R should be printed so that the source and nature of the accounts can be analyzed and action taken. The longer a receivable remains on the books, the more likely it will be uncollected and turn into a bad debt. 59 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #4 – Aged Accounts Receivable (A/R) Important tip: Make sure that your aged A/R reports are run based on the date of service (DOS) and NOT on the date last submitted. Otherwise, if a claim is “re-aged” to “zero” every time it is resubmitted or moved to another payer, the organization will have a falsely positive impression of performance. 60 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate There are several ways to analyze your organization’s percentage of collected revenue. Some organizations make the comparison to the fee that was charged (Gross collection rate) while others calculate the adjusted (Net collection rate) based on the organization’s contractual fee schedule with the payers. Many organizations do both calculations, which we recommend. 61 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate 1) Calculating the Gross collection rate: To calculate the organization’s overall gross collection rate, at month-end, take the total payments received for the month and divide that by the sum of the total payments plus total adjustments (i. e. the charge associated with those payments. ) Collection Ratio= Total Payments for period / (Total Payments for period + Total Adjustments for period) 62 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate The formula for Gross collection rate looks like this: Monthly payments / (monthly payments + the adjustments on those payments) = Gross collection rate 63 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate Example: If an organization collects $75, 000 in total payments for a given month and the total adjustments for that month are $50, 000, then the Gross collection rate for the month will be 60%. 64 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate When this calculation is done by payer type, it will show who your best payers are and which your lowest reimbursing payers are. This information may then be useful for negotiating higher reimbursements with selected payers. 65 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate 2) Calculating the Net collection rate: In order to effectively calculate your organization’s net collection rate, it is helpful to have a PM system that allows you to enter the contracted rates for each payer. When the contracted payer information is readily available, the Net collection rate is an excellent measure of the clinic’s effectiveness in collecting all legitimate reimbursement. 66 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate Despite what one would believe, payers do not always pay the amount that they agreed to pay based on their contract and fee schedule with the organization. This metric is also helpful in identifying how much revenue is lost due to uncollectible bad debt, untimely filing or other non-contractual adjustments. 67 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate The formula for Net Collection Rate looks like this: Monthly payments divided by charges (net of approved contractual adjustments). Some PM systems can’t match payments with their originating charges. If this is the case, the calculation should be done on data dating back 4 – 6 months, giving the majority of the claims ample time to clear. 68 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate Example: Net collection rate for a 3 month period: Total payments for the 3 month period = $475, 000 Total payments for the 3 month period = $856, 000 Total write-offs for the 3 month period = $360, 000 $475, 000 / ($856, 000 – $360, 000) = 95. 8% Net collection ratio 69 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #5 – Collection rate Most practices average between 95 – 99%. A Net collection ratio below 95% usually signals a problem somewhere in your organization’s revenue cycle. 70 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate The denial rate is the percentage of claims denied by payers. The lower this number, the better your cash flow will be. Medicare and most payers have over 200 reasons why claims are denied or rejected. While most organizations think that the majority of claims are denied due to coding errors, the top reasons are actually due to front-end work flow failures. 71 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate Common Claim Denials Demographic errors Coding errors Billed to the wrong insurance Provider is non-par No out-of-network-benefits Lack of pre-authorization Missing NDC number or Units Duplicate claim Timely filing/appeal 72 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate Automating aspects of the billing process can dramatically lower the denial rate. Unfortunately, not all billing systems have the ability to obtain denial information in a meaningful way. Clinics that don’t track denials could be losing over 20% of their revenue. 73 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate Even if your PM system does not track your denials and the reasons for those denials, you can set up a spreadsheet and track the type and frequency of your denials and address those errors with the appropriate personnel. 74 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate How to calculate your denial rate Using a designated period of time (monthly or at least quarterly), total the dollar amount of claims denied by the payers. Then divide that sum by the total dollar amount of claims submitted for that same period. 75 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate Denial rates of less than 5% indicate a strong, effective RCM process. Many practices average between 5 – 10%, and a denial rate of greater than 10% signals problems in your RCM process. 76 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate To fully understand what is driving your denial rate, you should do a denial rate analysis by payer, provider, remark code and category. Most clearing houses can provide these more detailed breakdowns. 77 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate Denial rate is one of the most crucial areas to focus on in advance of the transition to ICD-10. According to CMS, in the early stages of ICD-10 implementation, denial rates will increase by 100 – 200%! Practices will need to establish effective processes for appealing these claims or risk putting the financial health of their organizations at risk. 78 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Key Performance Indicators (KPI) For Peak Financial Performance KPI #6 – Claims denial rate Strategies & Tips to Reduce Payer Denials Monitor claim denials to identify trends. Use system analyzing reports indicating frequency of “Remark” codes. Tracking and categorizing denials by payer and provider. Monitor claim denials to identify trends. Correct the root denial problems and rejections. Follow-up on denials within 24 hours. Develop appeal letter templates. 79 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement Once your organization has identified what KPI to track and how to obtain that information, it is important to know the steps to take when there are unfavorable KPI results. 80 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement KPI #1 and 2 – Relating total charges by month to total visits, overall and by provider There should be a direct correlation each month between the number of patient s seen and the total charges billed. While the mix and type of visits may vary, there should still be a fairly predictable increase in charges in those months with increased patient visits. 81 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Using Your Key Performance Indicators for Process Improvement KPI #1 and 2 – Relating total charges by month to total visits, overall and by provider When charges do not reflect the variations in visit month to month, possible reasons may include providers not completing their charges in a timely way, providers not charging patients for certain services or charges missed entirely. 82 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement KPI #1 and 2 – Relating total charges by month to total visits, overall and by provider The daily charge reconciliation process should be helpful in identifying weaknesses in the charge capture process but tracking these metrics by physician may also reveal a particular provider who is delinquent in submitting charges. 83 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement KPI #3, #4 and #6– Days in A/R, Aged A/R and Denial rate These three KPIs are all directly affected by the “cleanliness” of the claims going out to the payers. The more effort that is put forth in obtaining accurate and complete information from the patients on the “front-end”, the less the effort that will required on the “back-end. ” 84 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement KPI #3, #4 and #6– Days in A/R, Aged A/R and Denial rate Well-run billing offices review and edit (reject) charges before they are sent to the clearing house or directly to the payer. Encouraging internal rejections (and having a system for correction) is an industry best practice. 85 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement KPI #3, #4 and #6– Days in A/R, Aged A/R and Denial rate A high internal claims rejection rate will typically result in a lower denial rate – and thus, improved cash flow. If the clearing house or claims scrubber in your PM system detects errors, such as your coder using an improper modifier, the payback will be two=fold: a denial will be prevented and a delay will be avoided in posting the paid claim. 86 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Using Your Key Performance Indicators for Process Improvement KPI #3, #4 and #6– Days in A/R, Aged A/R and Denial rate There also needs to be a good, effective process established internally for the reasons for rejection and denial to be shared with both front office staff and providers so that those errors can be corrected and reduced. 87 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement KPI #5 – Gross and Net Collection rates As we discussed, the Gross collection rate is a metric that is directly related to the contractual fee schedules established with your various payers. Depending upon the payer and the state in which you operate, those rates may or may not be negotiable. 88 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Using Your Key Performance Indicators for Process Improvement KPI #5 – Gross and Net Collection rates To ensure that your organization is receiving the amounts from each payer that have been agreed to in your contract, load each payer’s fee schedule into your PM system. If your billing system cannot accommodate that information, identify your top 10 – 20 CPT codes billed to the payers and create a spreadsheet with those codes and the amounts expected from each payer. 89 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement KPI #5 – Gross and Net Collection rates As payments are received, post the amounts paid to the spread sheet and compare to the expected reimbursement. If there is a discrepancy, the payer should be contacted. 90 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement KPI #5 – Gross and Net Collection rates The Net collection ratio is much more dependent on the effectiveness of your billing team. If the Net collection ratio for your organization falls below 95%, one of the key areas to investigate is “write-offs. ” 91 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com

Using Your Key Performance Indicators for Process Improvement KPI #5 – Gross and Net Collection rates Most PM systems will have a special “adjudication report” that provides all of the detail on the write-offs that have been done. Writing off a claim is certainly less work than correcting and/or appealing a claim but is certainly not in the best interest of the organization. 92 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement Summary of Best Practices for monitoring RCM metrics; § Hold monthly revenue cycle team meetings § Track and monitor key performance indicators (KPI) § Benchmark against industry standards and internally to trends over time § Use a dashboard to manage and measure revenue cycle improvement and goals. § Ongoing monitoring of these key metrics is essential to improved revenue cycle performance. With the right tools and information, your organization can experience fewer denials, faster payment and greater profitability. 93 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Using Your Key Performance Indicators for Process Improvement In summary, management must focus on each part of the revenue cycle process to ensure that value is delivered consistently and that revenue is maximized. KPI tracking and process improvement will contribute greatly to the success of the revenue cycle. Implementing these best practices will have a positive impact on your organization and the communities that you serve. 94 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com
Additional references and resources: AMA Glossary of terms AMA - How to select a practice management system RCM Action Plan 95 www. shrassociatesinc. com / 410 -897 -9888 / info@shrassociatesinc. com