EMS Laws The Legal Process Amy Gutman MD


- Slides: 56
EMS Laws & The Legal Process Amy Gutman MD prehospitalmd@gmail. com
Objectives • Review National EMS Standard Competencies for Laws & Ethics • Review concepts integral to EMS including: – – Civil vs Criminal Laws Mandated reporting Good Samaritan laws HIPPA & PHI
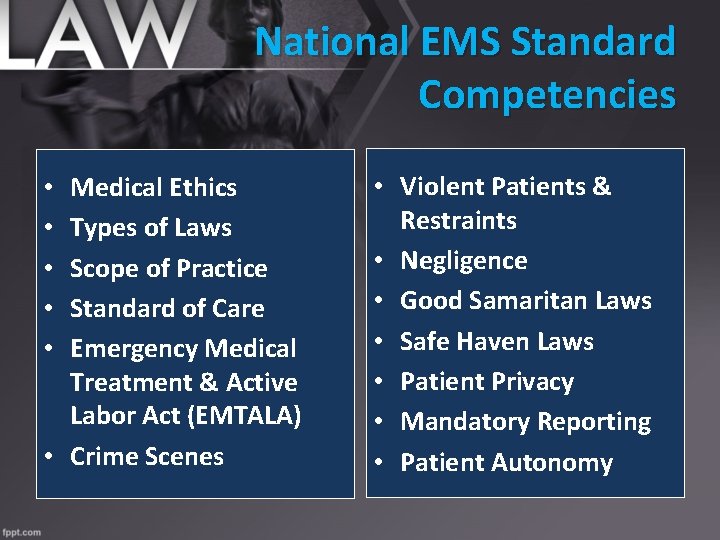
National EMS Standard Competencies Medical Ethics Types of Laws Scope of Practice Standard of Care Emergency Medical Treatment & Active Labor Act (EMTALA) • Crime Scenes • • • Violent Patients & Restraints • Negligence • Good Samaritan Laws • Safe Haven Laws • Patient Privacy • Mandatory Reporting • Patient Autonomy
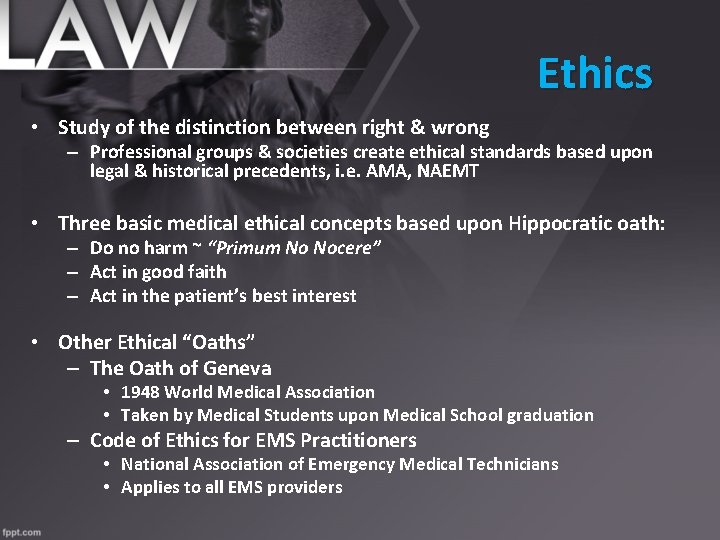
Ethics • Study of the distinction between right & wrong – Professional groups & societies create ethical standards based upon legal & historical precedents, i. e. AMA, NAEMT • Three basic medical ethical concepts based upon Hippocratic oath: – Do no harm ~ “Primum No Nocere” – Act in good faith – Act in the patient’s best interest • Other Ethical “Oaths” – The Oath of Geneva • 1948 World Medical Association • Taken by Medical Students upon Medical School graduation – Code of Ethics for EMS Practitioners • National Association of Emergency Medical Technicians • Applies to all EMS providers
What Are Laws? • Written expectations reflecting societal standards • US Law based upon: – – – The Constitution Bill of Rights Statues Administrative Law Common Law Case Law • Constitutional law is the standard by which all laws are measured
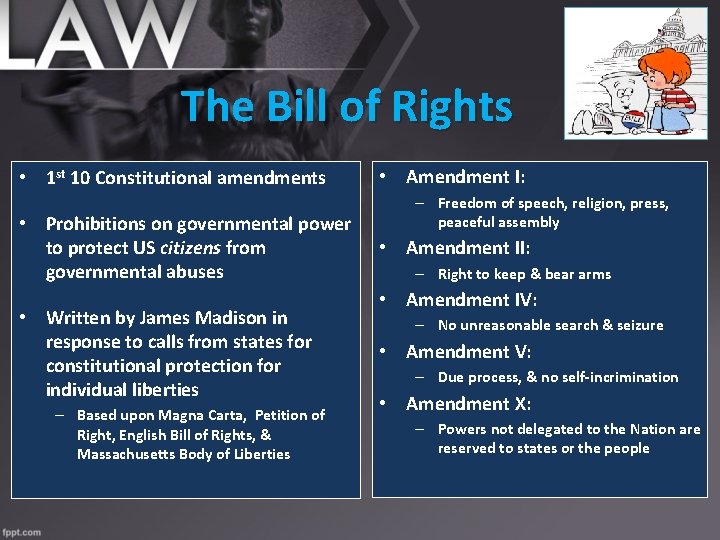
The Bill of Rights • 1 st 10 Constitutional amendments • Prohibitions on governmental power to protect US citizens from governmental abuses • Written by James Madison in response to calls from states for constitutional protection for individual liberties – Based upon Magna Carta, Petition of Right, English Bill of Rights, & Massachusetts Body of Liberties • Amendment I: – Freedom of speech, religion, press, peaceful assembly • Amendment II: – Right to keep & bear arms • Amendment IV: – No unreasonable search & seizure • Amendment V: – Due process, & no self-incrimination • Amendment X: – Powers not delegated to the Nation are reserved to states or the people
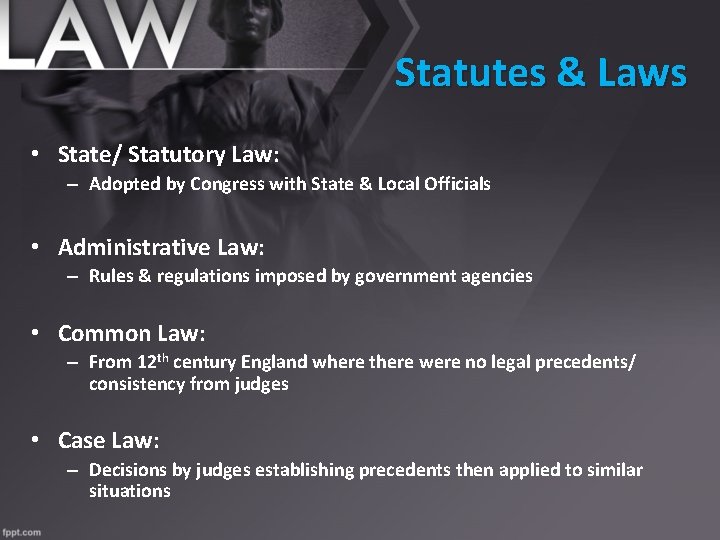
Statutes & Laws • State/ Statutory Law: – Adopted by Congress with State & Local Officials • Administrative Law: – Rules & regulations imposed by government agencies • Common Law: – From 12 th century England where there were no legal precedents/ consistency from judges • Case Law: – Decisions by judges establishing precedents then applied to similar situations
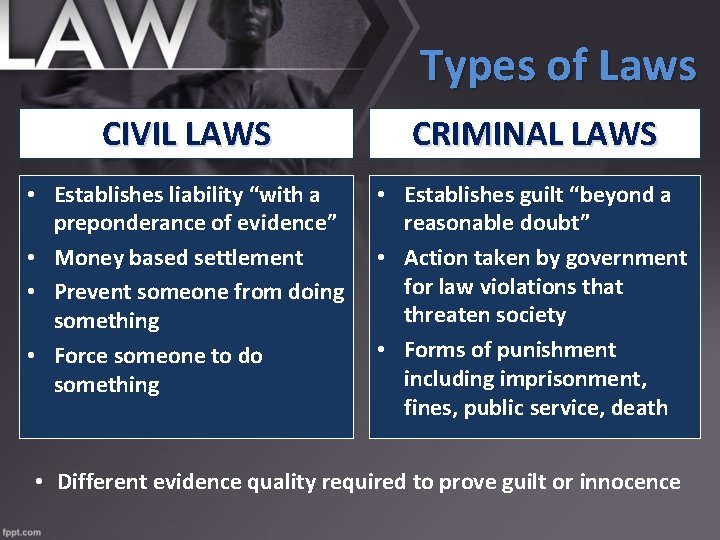
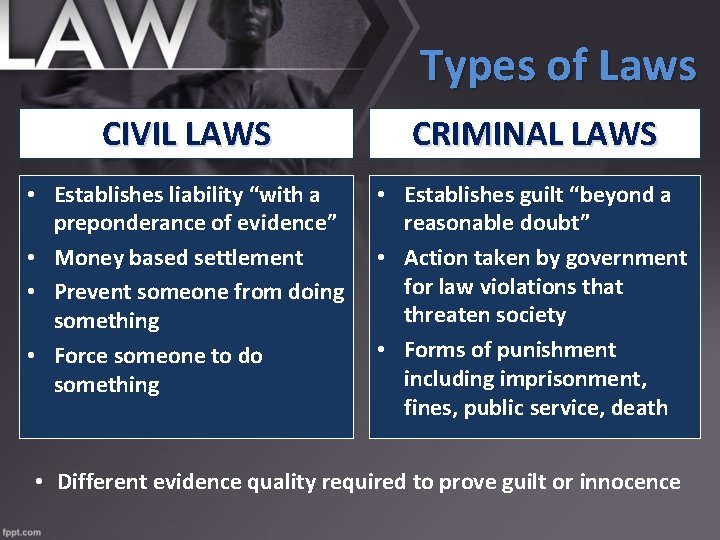
Types of Laws CIVIL LAWS CRIMINAL LAWS • Establishes liability “with a preponderance of evidence” • Money based settlement • Prevent someone from doing something • Force someone to do something • Establishes guilt “beyond a reasonable doubt” • Action taken by government for law violations that threaten society • Forms of punishment including imprisonment, fines, public service, death • Different evidence quality required to prove guilt or innocence
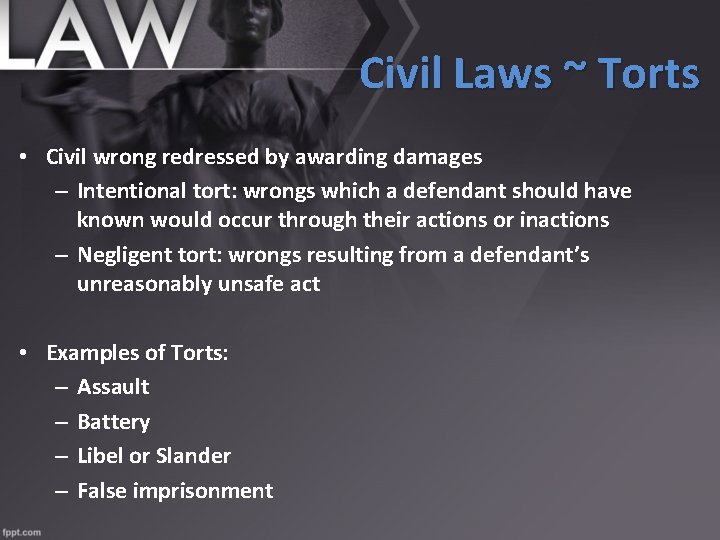
Civil Laws ~ Torts • Civil wrong redressed by awarding damages – Intentional tort: wrongs which a defendant should have known would occur through their actions or inactions – Negligent tort: wrongs resulting from a defendant’s unreasonably unsafe act • Examples of Torts: – Assault – Battery – Libel or Slander – False imprisonment
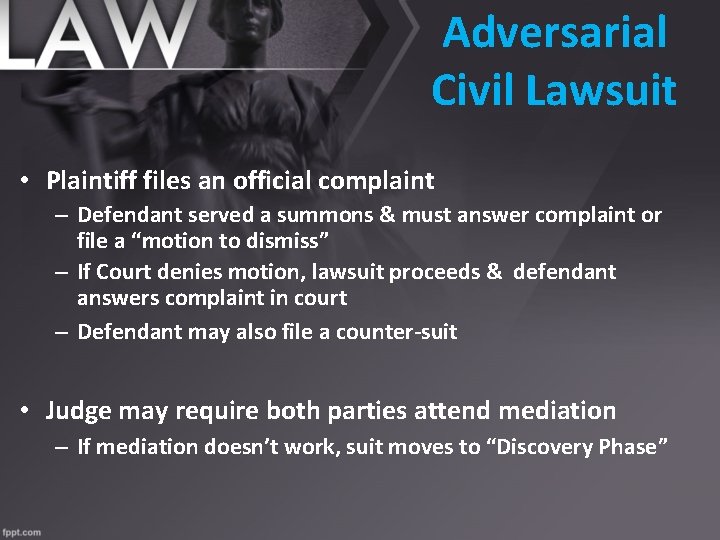
Adversarial Civil Lawsuit • Plaintiff files an official complaint – Defendant served a summons & must answer complaint or file a “motion to dismiss” – If Court denies motion, lawsuit proceeds & defendant answers complaint in court – Defendant may also file a counter-suit • Judge may require both parties attend mediation – If mediation doesn’t work, suit moves to “Discovery Phase”
Discovery • Interrogatories / Depositions – List of questions traded between the two sides – Both parties agree to answer all questions from opposition • Motions to produce documents – Both parties may be asked to forward information pertinent to the case, i. e. PCRs, emails, employment records • Requests to admit – Both sides agree or disagree on certain facts of the case to avoid arguing all issues in court
Courtroom • Two options regarding how trial decided: – Jury Trial ~ Peers – Bench Trial ~ Judge only, with right to jury trial waived • Cannot appeal decision based on the fact that you disagree – Only can appeal if you or attorney believe there were errors in court procedure or testimony unfair to one party other
State Courts • Municipal courts • Justice of the Peace • County Courts • Circuit Courts • Superior Courts • District Courts • Regional Trial Courts
3 Levels of State Jurisdiction Limited Jurisdiction • – – – Civil suits Juvenile crime Minor criminal infractions (i. e. traffic violations) General Jurisdiction • – Civil suits involving large sums of money &/or serious crimes Specialized Trial Courts • – – – Probate Family Law Small Claims
Appellate Courts • Uphold previous judges’ decision(s) • Reverse a previous decision – “De Novo” = “Anew” or “Start over” • Modify a previous decision – i. e. amount awarded in a civil trial
State Supreme Court • Court of “almost last” resort after an appeal has been exhausted • Only review decisions, do not hold “trials”
Federal Courts • Districts • Circuits • Supreme Court – – Highest court Does not hold trials Review prior rulings & provide a final decision “Final” decision can be overturned by a new case precedent
Rules & Regulations Pertaining to Health Care Providers
Protect Yourself • Comply with SOPs • Heed standard of care for level of training – Attend con ed! • Accurate & thorough documentation • Kind & professional attitude
Duty To Act • “Duty to Act” refers to: – Provide reasonable care to prevent harm – Person has a duty to do a specific thing, & if they fail to act, may be found liable • Duty to act? – – Provider on duty Provider stops to assist at an incident EMS unit traveling where it could render care No unreasonable threat to provider safety • A breach of duty is a violation of Standard of Care or Scope of Practice – Failure to act or acted inappropriately
Negligence • Failure to act as a prudent & similarly trained health care provider would given the same circumstances – Based upon a “Duty to Act”, which is a legal obligation to provide care • Must prove four things: – – There was a duty to act There was a breach of that duty Damage or injury occurred because of failure to act Proximate cause: injury caused by the breech of duty • Liability – Legal responsibility for an act – Negligence is a Tort, therefore monetary penalties may apply – May also be a criminal charge • Action may be taken by the Department, review boards or court system – Reprimand, Retraining, Suspension, Revocation of License – Civil or Criminal court
Negligence Protection • Some states offer protection against negligence liability claims • Must show evidence that the HCP was not willful & wanton in actions • Behavior did not demonstrate "a deliberate or reckless disregard for the safety of others"
Negligence Can Lead To Criminal Charges • A California doctor was convicted of murder in connection with the OD deaths of 3 patients & sentenced to 30 years to life • Over the course of 3 years, Tseng wrote over 27, 000 narcotic prescriptions – 25 a day, with appointments lasting 3 -5 minutes
Civil Rights Violations • It is not uncommon that a HCP is sued for negligence & violation of patient’s civil rights at the same time • Do not withhold ANY treatment based on religion, race, gender or national origin – With very few exceptions, your personal rights or beliefs are held to a less valuable legal standard than your patients • Do not withhold treatment from those with communicable diseases such as TB or HIV
Patient Autonomy • A patient has the right to direct their own care • Providers must respect & honor the patient’s rights, including consent of treatment & refusal of care • Express consent & refusal expressed by: – Living Wills – Advanced Directives – Healthcare Power of Attorney – Do Not Resuscitate (DNR) Orders – Medical Orders for Life Sustaining Treatment (MOLST)
Consent • HCPs required to obtain consent before treatment • Implied Consent – Reasonable person believes consent would be granted even though agreement was “not direct, express, or explicit”
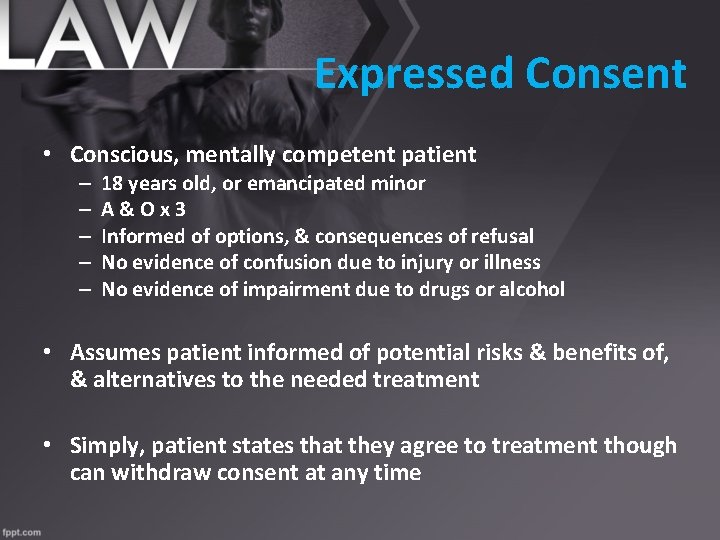
Expressed Consent • Conscious, mentally competent patient – – – 18 years old, or emancipated minor A&Ox 3 Informed of options, & consequences of refusal No evidence of confusion due to injury or illness No evidence of impairment due to drugs or alcohol • Assumes patient informed of potential risks & benefits of, & alternatives to the needed treatment • Simply, patient states that they agree to treatment though can withdraw consent at any time
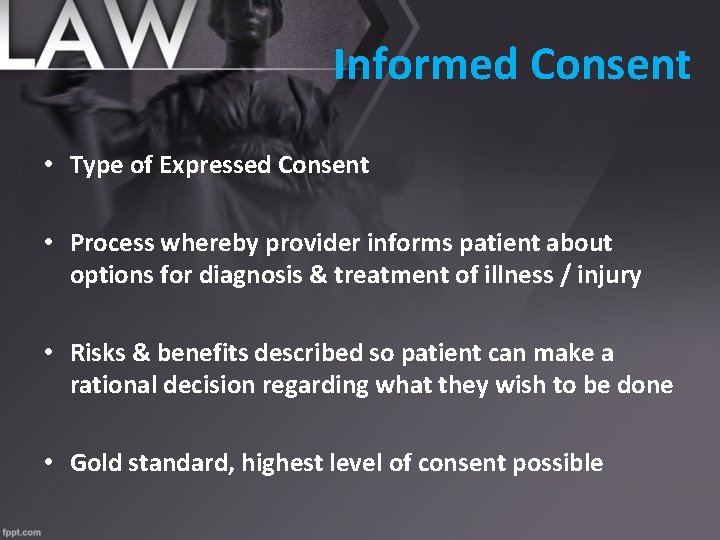
Informed Consent • Type of Expressed Consent • Process whereby provider informs patient about options for diagnosis & treatment of illness / injury • Risks & benefits described so patient can make a rational decision regarding what they wish to be done • Gold standard, highest level of consent possible
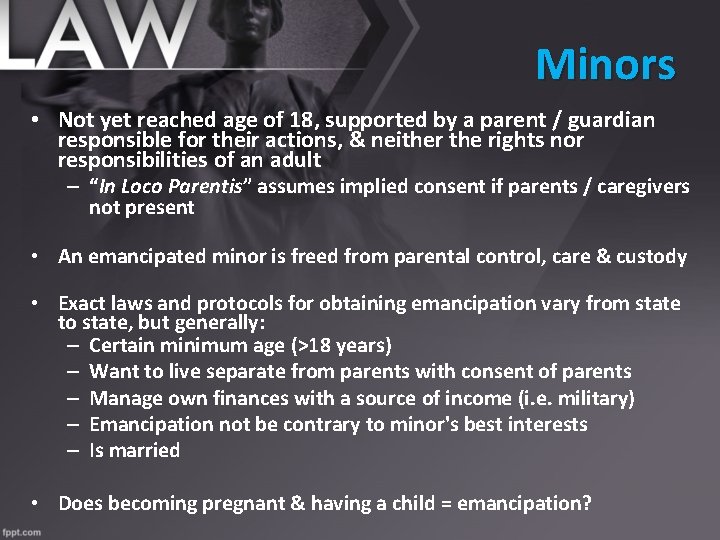
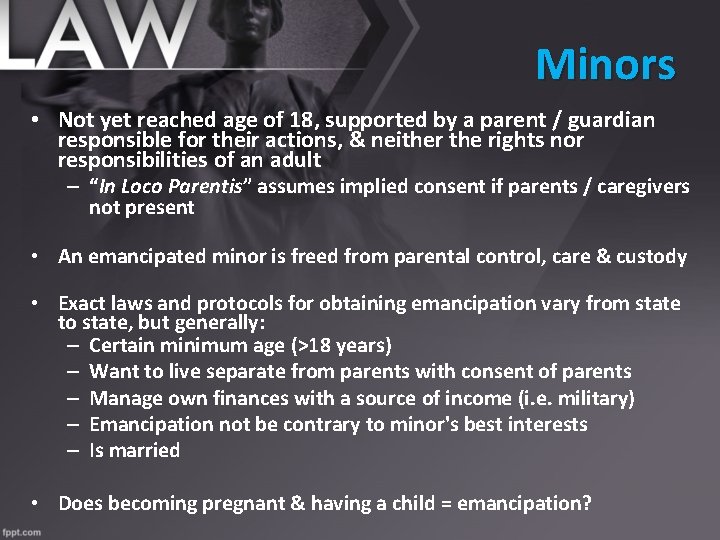
Minors • Not yet reached age of 18, supported by a parent / guardian responsible for their actions, & neither the rights nor responsibilities of an adult – “In Loco Parentis” assumes implied consent if parents / caregivers not present • An emancipated minor is freed from parental control, care & custody • Exact laws and protocols for obtaining emancipation vary from state to state, but generally: – Certain minimum age (>18 years) – Want to live separate from parents with consent of parents – Manage own finances with a source of income (i. e. military) – Emancipation not be contrary to minor's best interests – Is married • Does becoming pregnant & having a child = emancipation?
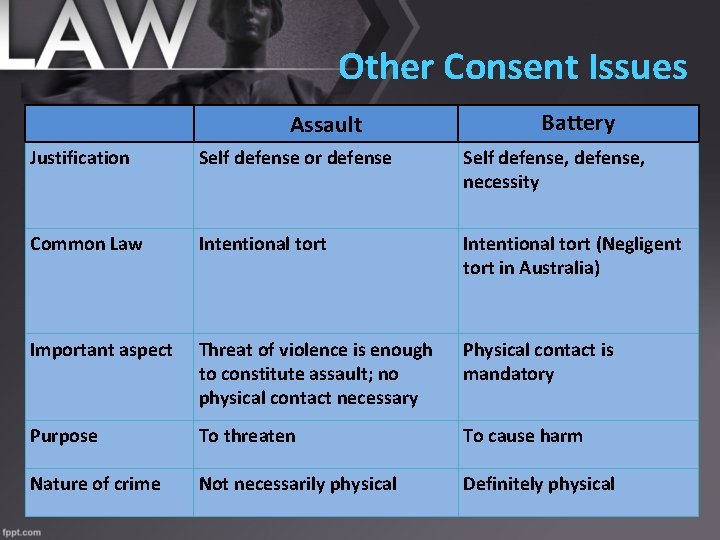
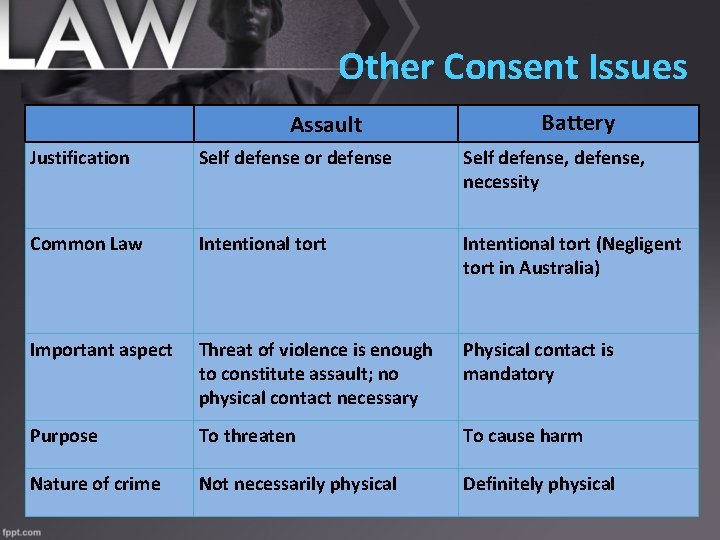
Other Consent Issues Assault • If you touch Self a patient Justification defensethat or defense has not given you permission for treatment you can be charged with Common Law Intentional tort assault & / or battery • Simply, assault is the threat to commit Important aspect battery Threat of violence is enough to constitute assault; no physical contact necessary Battery Self defense, necessity Intentional tort (Negligent tort in Australia) Physical contact is mandatory Purpose To threaten To cause harm Nature of crime Not necessarily physical Definitely physical
Patient Autonomy • Transportation Decisions – Patient has right to be transported to facility of their choice “within reason” in accordance with protocols • Refusals – Must be informed – If AMA, consider contacting Medical Control – You are the patient’s & your best advocate – Do not judge any patient refusing care based on their personal beliefs – Document!
Who Can Refuse Care? • Patient’s medical power of attorney • Patient’s legal guardian or custodian of a mentally incompetent patient – “Health Care Proxy” • In the event a parent or guardian not present, or not located, treat patient under implied consent
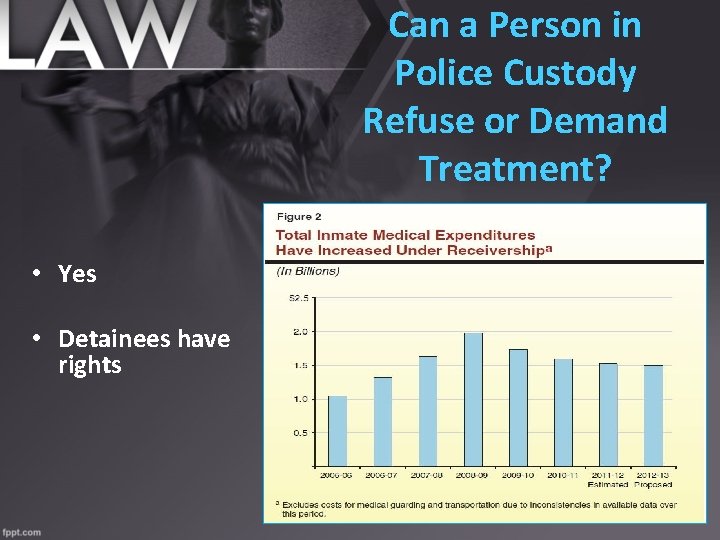
Can a Person in Police Custody Refuse or Demand Treatment? • Yes • Detainees have rights
Safe Haven Laws: Legally Abandonment of an Infant • Any infant turned in under the Safe Haven Law must have a medical evaluation being turned over to social services • Laws vary from state-to-state – Ohio: <3 days old with EMS, medical facility or police – Indiana: Up to 30 days old with any EMS provider – Utah: Up to age 17 years, 364 days to medical facility or police – Maryland: Any infant up to and including 10 days old
Mandated Reporters • Persons with intermittent responsibility for care of “vulnerable” population legally required report or suspected abuse – Educators, Health Practitioners, Human Service Workers, Public Safety • Abuse in many forms: – – – Child, elder or “special population” abuse / neglect Domestic abuse Sexual assault Stab / Gunshot wounds Animal attacks Financial • Reports made to appropriate personnel & documented in report – Anyone who makes a report in “good faith” immune from civil liability or criminal penalties
Good Samaritan Laws • Anyone voluntarily rendering aid in an emergency – A person is not legally obligated to perform 1 st aid in most states unless it's part of a job description – Some states consider it an act of negligence if a person doesn't at least call for help • Immunity for lay persons attempting to provide “good faith” assistance – Statutes do not exempt acting in a willful, wanton or reckless manner in providing care, advice, or assistance • Limited protection for off duty EMS personnel – Does not apply to on duty EMS personnel

Good Samaritan Act ~ National Standards “When medical personnel gratuitously & in good faith render first aid or emergency care at the scene of an accident, casualty, or disaster to a person injured therein, he or she shall not be liable for any civil damages as a result of his or her acts or omissions in rendering first aid or emergency care, nor shall he or she be liable for any civil damages as a result of any act or failure to act to provide or arrange for further medical treatment or care for the injured person”
DNR vs Do Not Treat • Patient receives all the appropriate medical treatment, including resuscitation, until they have a cardiac or pulmonary arrest • At this point only comfort care provided – Nutrition &/or hydration to diminish pain or discomfort but not postpone death – All medical care administered to diminish pain or discomfort that does not postpone death – Patient may reject other life-sustaining measures such as antiarrhythmic, central line, vasopressors
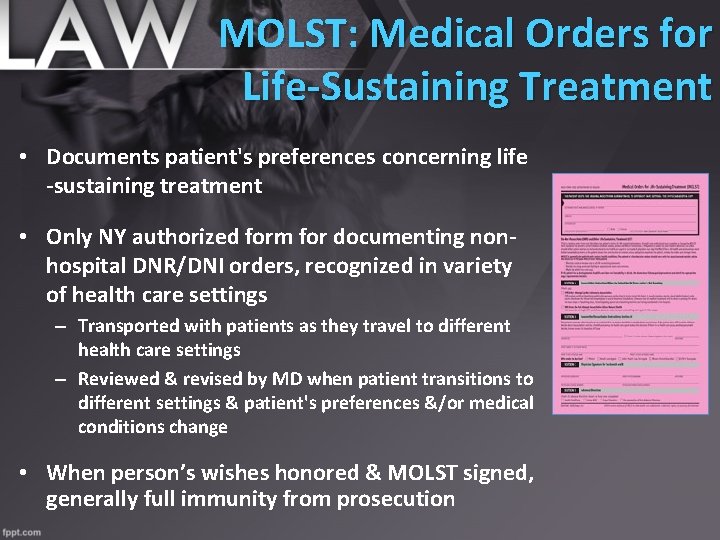
MOLST: Medical Orders for Life-Sustaining Treatment • Documents patient's preferences concerning life -sustaining treatment • Only NY authorized form for documenting nonhospital DNR/DNI orders, recognized in variety of health care settings – Transported with patients as they travel to different health care settings – Reviewed & revised by MD when patient transitions to different settings & patient's preferences &/or medical conditions change • When person’s wishes honored & MOLST signed, generally full immunity from prosecution
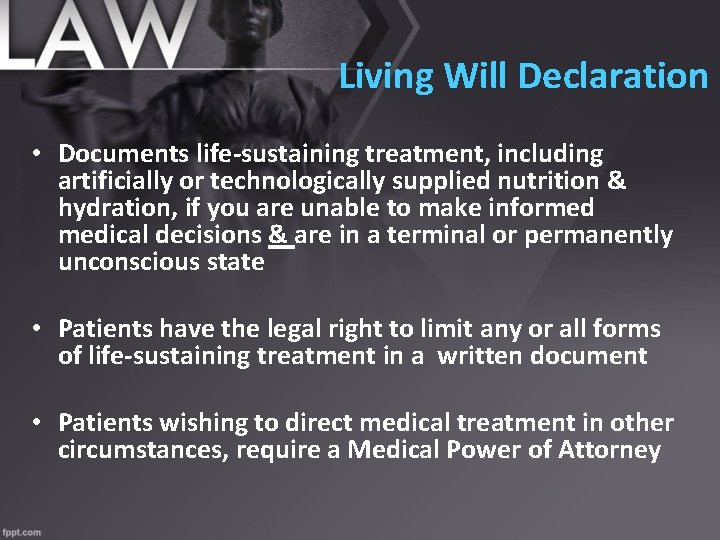
Living Will Declaration • Documents life-sustaining treatment, including artificially or technologically supplied nutrition & hydration, if you are unable to make informed medical decisions & are in a terminal or permanently unconscious state • Patients have the legal right to limit any or all forms of life-sustaining treatment in a written document • Patients wishing to direct medical treatment in other circumstances, require a Medical Power of Attorney
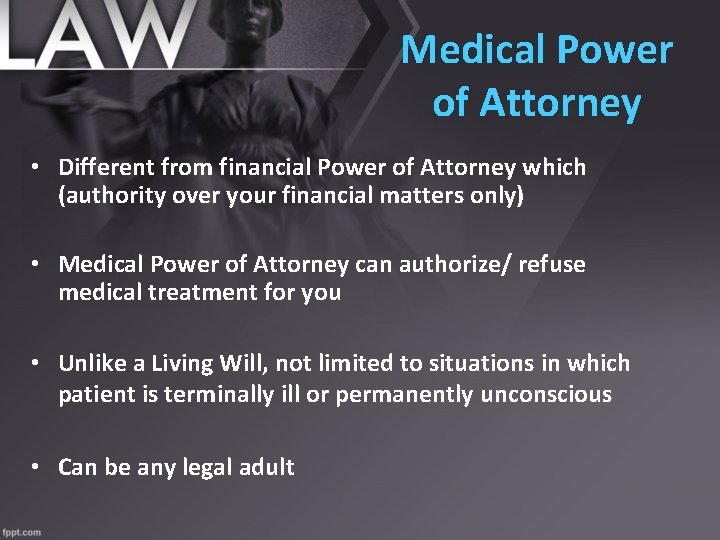
Medical Power of Attorney • Different from financial Power of Attorney which (authority over your financial matters only) • Medical Power of Attorney can authorize/ refuse medical treatment for you • Unlike a Living Will, not limited to situations in which patient is terminally ill or permanently unconscious • Can be any legal adult
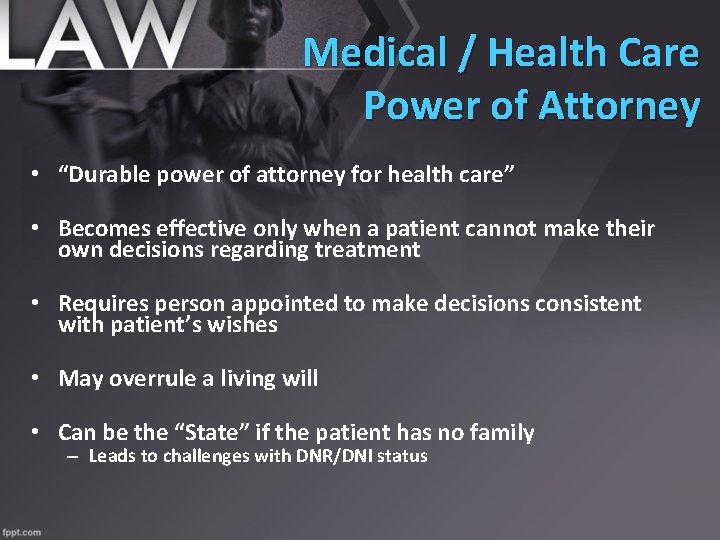
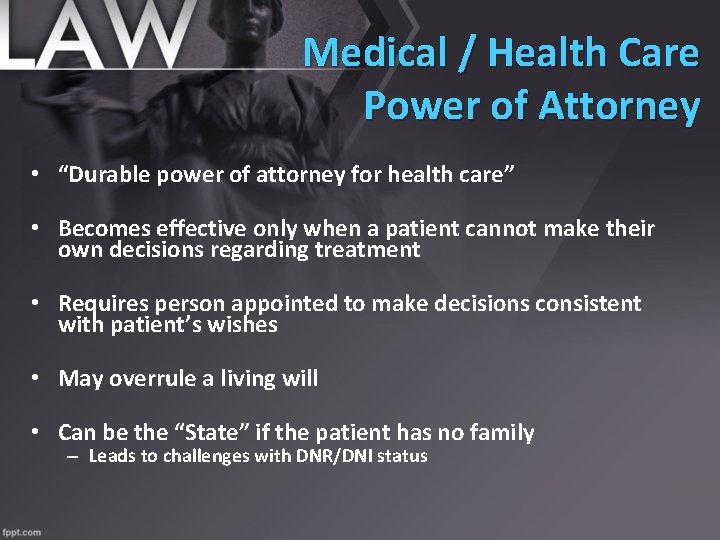
Medical / Health Care Power of Attorney • “Durable power of attorney for health care” • Becomes effective only when a patient cannot make their own decisions regarding treatment • Requires person appointed to make decisions consistent with patient’s wishes • May overrule a living will • Can be the “State” if the patient has no family – Leads to challenges with DNR/DNI status
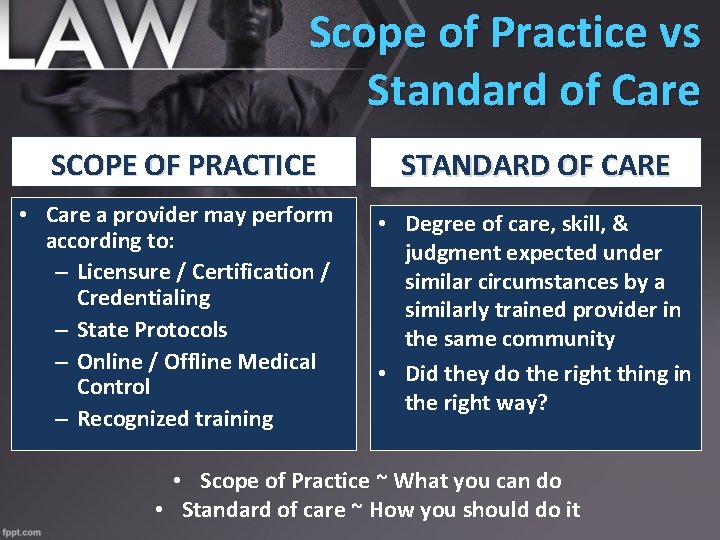
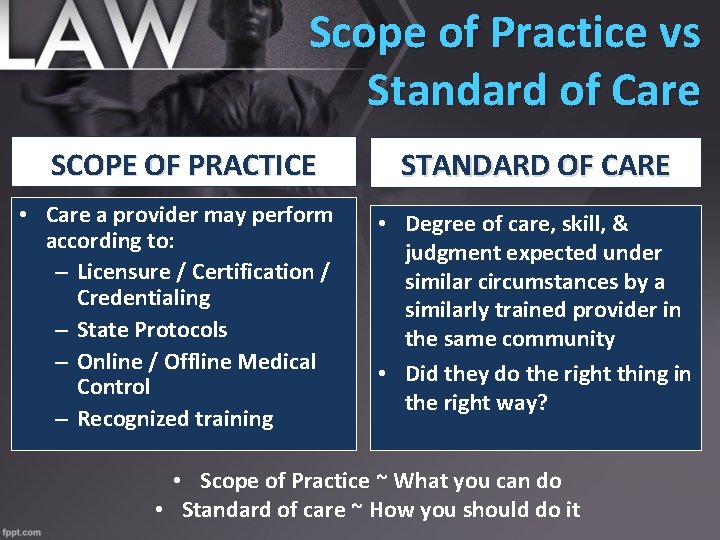
Scope of Practice vs Standard of Care SCOPE OF PRACTICE • Care a provider may perform according to: – Licensure / Certification / Credentialing – State Protocols – Online / Offline Medical Control – Recognized training STANDARD OF CARE • Degree of care, skill, & judgment expected under similar circumstances by a similarly trained provider in the same community • Did they do the right thing in the right way? • Scope of Practice ~ What you can do • Standard of care ~ How you should do it
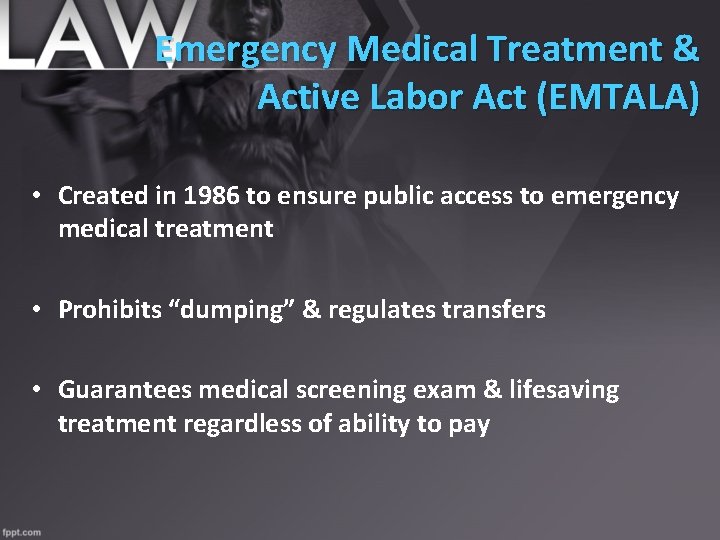
Emergency Medical Treatment & Active Labor Act (EMTALA) • Created in 1986 to ensure public access to emergency medical treatment • Prohibits “dumping” & regulates transfers • Guarantees medical screening exam & lifesaving treatment regardless of ability to pay
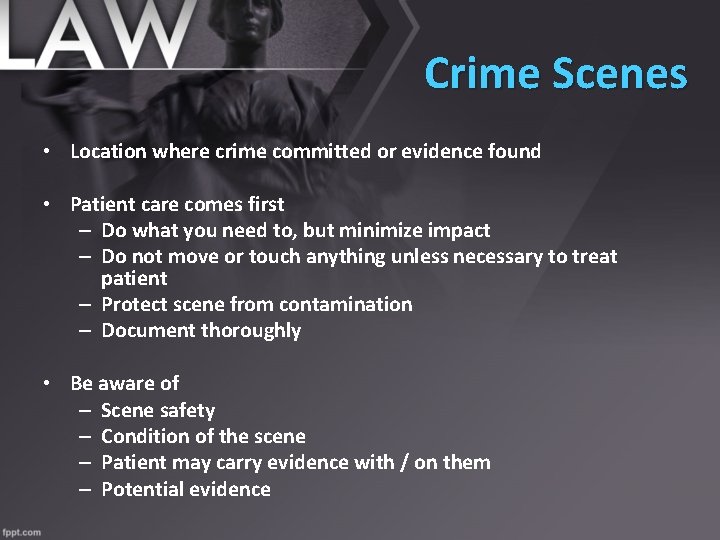
Crime Scenes • Location where crime committed or evidence found • Patient care comes first – Do what you need to, but minimize impact – Do not move or touch anything unless necessary to treat patient – Protect scene from contamination – Document thoroughly • Be aware of – Scene safety – Condition of the scene – Patient may carry evidence with / on them – Potential evidence

Violent Patients & Restraints • Scene and Provider safety comes first – Wait for law enforcement to secure scene • You can only use force in response to force used against you – Your use of force must be reasonable to situation – Minimum force necessary to restrain a combative patient • Patients who are a danger to themselves or others may be restrained – If a patient restrained you are liable for their safety – Attempt to have law enforcement perform restraint • False Imprisonment? – Detaining person without proper consent – Document well all circumstances surrounding any restraint
Abandonment • Failure to continue care once started • Transferring patient care to lesser trained person • Termination of care without patient’s consent • General rule of thumb: – Once you make patient contact, you cannot leave until a provider of equal or higher training accepts responsibility of the patient – Required to give report to the accepting provider – Special circumstances do apply i. e. MCIs
Patient Privacy / HIPAA • 1996 Health Insurance Portability & Accountability Act which applies to all health care providers • Specifies what is Protected Health Information (PHI) – Individually identifiable information dealing with past, present, or future physical or mental health care or payment created by or received by a health care provider • Forms of PHI include: – Oral – Written – Photographic – Electronic / Digital
HIPAA Provider Obligations • Respect privacy of patient’s information as you would your own • Do not share PHI with those not involved in patient care except as permitted • Keep disclosures to “minimum amount necessary” • Violation of Patient Privacy is a Tort – Fines may be in the tens of thousands of dollars.
Permitted PHI Use • Treatment – Shared with other providers responsible for treating patient – Minimum necessary rule does not apply to treatment related disclosures • Payment – PHI used to file claims for reimbursement with insurances • Health Care Operations – QA / CQI or training following minimum necessary rule
Protecting PHI • Dispatch & Response – Shared over radio with responding agencies as needed for appropriate treatment purposes – Use secure communication when available • On Scene – Discussed with on-scene providers – Limited discussion with family & friends – Do not discuss with third parties – Minimize incidental disclosures
Protecting PHI • At Hospital – Verbal report & PCR may be given to staff involved in caring for the patient • After the call – Discussions in the station, QI activities, & CISD permissible – Minimum necessary rule applies – limit disclosures • Mass Casualty Incidents – Disclosed to entities involved in relief efforts, i. e. Red Cross for purpose of notifying family or personal representative of the location, condition, or death of a patient
Protecting PHI ~ Law Enforcement • HIPAA limits disclosures by EMS to law enforcement – EMS personnel are patient care advocates – not law enforcement “agents” • Permitted disclosure: – Officer who is a 1 st Responder on scene assisting with patient care & needs additional information to complete their PCR – Mandatory reporting cases • Restricted disclosure: – Officer stops by station & asks for PCR from vehicle crash – Law enforcement have channels to request required information
Safeguarding Written PHI • PCRs should not be left unattended – Including fax machines that may receive PHI • PCRs maintained in a locked cabinet with limited, role based access • Any notes, call intake records, physician certification, or other documents which contain PHI must be secured • PCRs cannot be posted as examples unless PHI removed • Implementation of password protection to computers, networks, or websites where PHI is maintained – Encryption technology should be used if available
Patient Privacy / HIPAA • Patient Rights – Patients have right to inspect & copy their records – Patients have right to request amendments to their medical records if information is incorrect – Requests directed through the company privacy officer • Company Policies – Policy on Confidentiality of Patient Information – Policy on PHI Security, Access, Use & Disclosure – Role Based access – Incidental Disclosures
REFERENCES Questions? prehospitalmd@gmail. com • Jones & Bartlett EMS Textbook, chapter 34: EMS Law & Ethics • NAEMT Standards of Care • NAEMSP Medical Directors Textbook • The. Law. Dictionary. Com • Wikipedia “Ethics”
 Amy gutman
Amy gutman Skala gutman
Skala gutman Amy taylor legal
Amy taylor legal Facts about montesquieu
Facts about montesquieu Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worm breton
Tư thế worm breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Các số nguyên tố là gì
Các số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Government legal trainee scheme application process
Government legal trainee scheme application process Wi ems wards
Wi ems wards Student business services uc merced
Student business services uc merced Ems felvételre kijelölt posták
Ems felvételre kijelölt posták Verdant thermostat
Verdant thermostat Ssv ems protocols
Ssv ems protocols Ems equipment repair
Ems equipment repair Northern virginia ems council
Northern virginia ems council Ems latlit
Ems latlit Ems report writing
Ems report writing Ems meaning
Ems meaning