Prehospital Documentation Amy Gutman MD prehospitalmdgmail com amy











- Slides: 45
Prehospital Documentation Amy Gutman MD prehospitalmd@gmail. com / amy. gutman@hahv. org
Why Is It Important? Patient Care Reports (PCRs) serve as: n Patient care record (continuity of care) n Legal document n Billing resource n Administrative tool
The PCR as a Record of Patient Care n n n Continuity of care Describes condition before & after EMS contact Establishes provider credibility & competency
The PCR “Serves as the ‘official record’ of the care you provided… The purpose of the PCR is to provide the reader with a ‘picture’ of the continuum of care that was provided to the patient from the arrival of first responders to the transfer of care in the hospital. It becomes your ‘substituted’ memory. ” Courtesy : Good Documentation is Your Best Defense: Steve Worth, Esquire
Legal Document n n n A report must be generated for any patient contact No exception for non-transports, patients “missing” on arrival, or situations in which there was minimal contact &/or no treatment provided Local standards on documentation may be viewed under NY EMS website
Billing Tool n Poorly written, incomplete or missing PCRs are billing obstacles
Administrative Tool n n Establishes need for EMS services in a particular area Protects your job
Narratives

DCHARTE D= C= H= A= R= T= E= Dispatch CC History Assessment Rx at scene Treatment Enroute Exemptions

Dispatch n What is the nature of the call? n Updates provided enroute n i. e. CPR in progress, police on scene

Chief Complaint n Why did patient call 911? n n Or who called & why? Described in patient’s own words, quotations if possible EMS should indicate reason patient was unable to speak Document who provided history
Examples n Upon arrival found 54 year old female seated on couch. Patient reports “pressure in chest” describes as “feels like someone is sitting on my chest” n Vs n “Possible heart attack”
What If Patient Curses? n Quote em! n “My chest f_c_ing hurts. ”
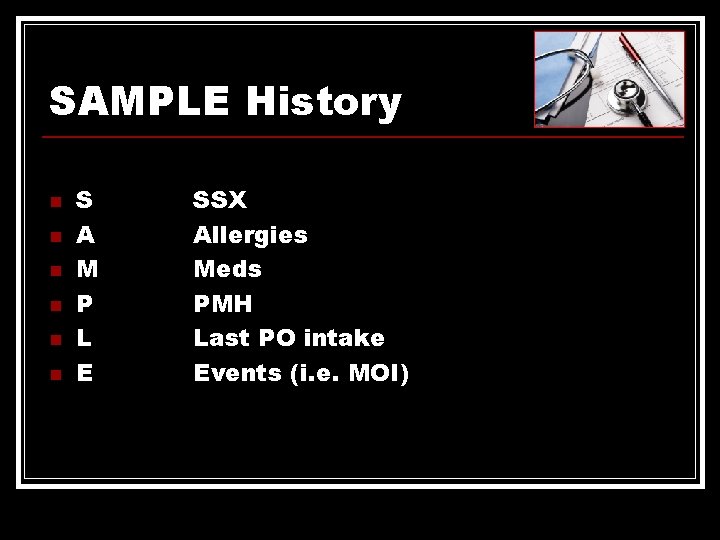
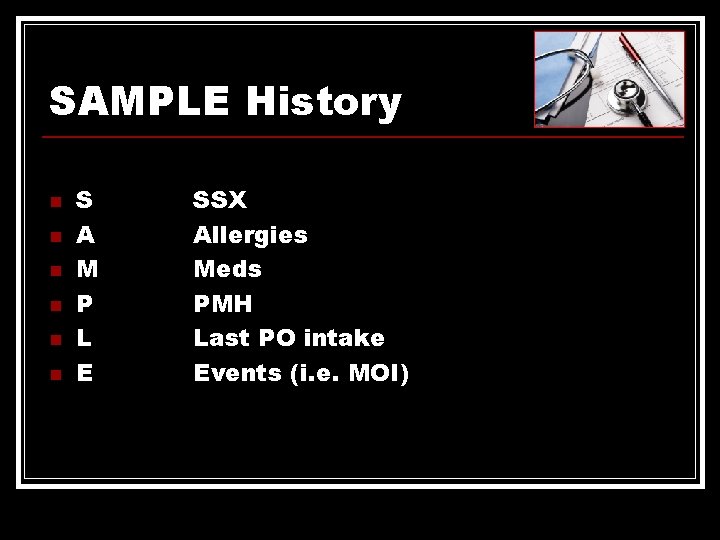
SAMPLE History n n n S A M P L E SSX Allergies Meds PMH Last PO intake Events (i. e. MOI)
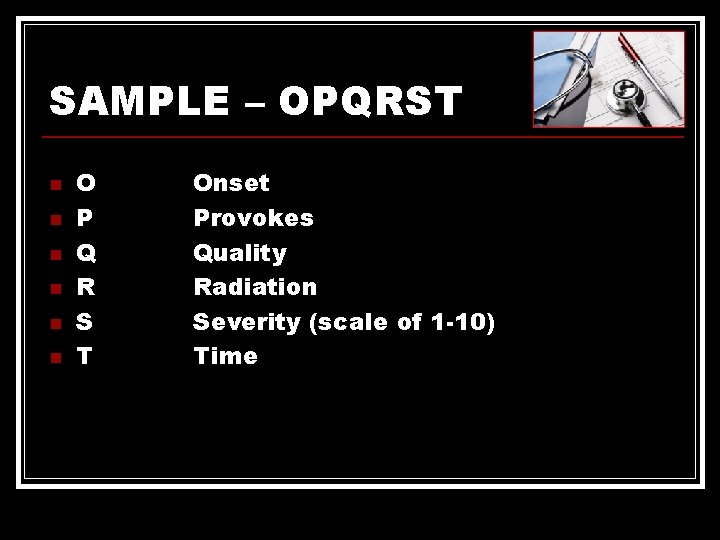
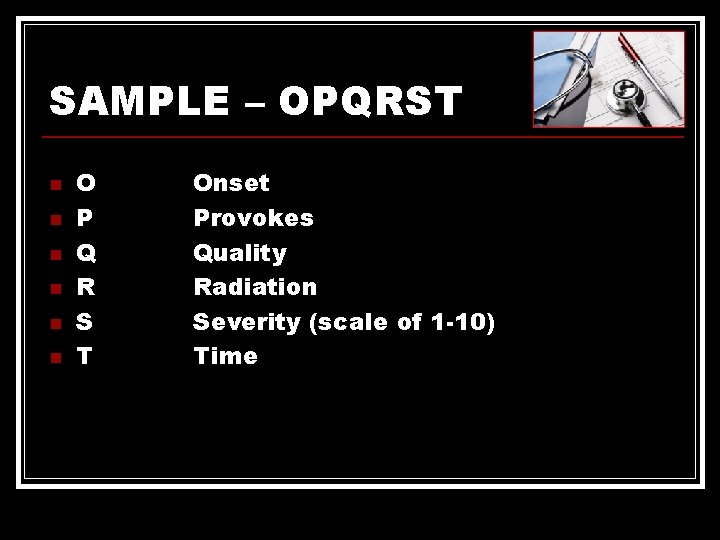
SAMPLE – OPQRST n n n O P Q R S T Onset Provokes Quality Radiation Severity (scale of 1 -10) Time
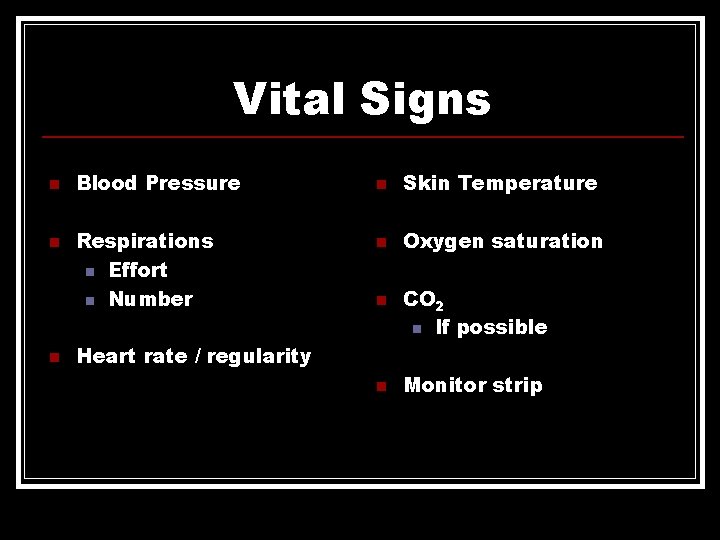
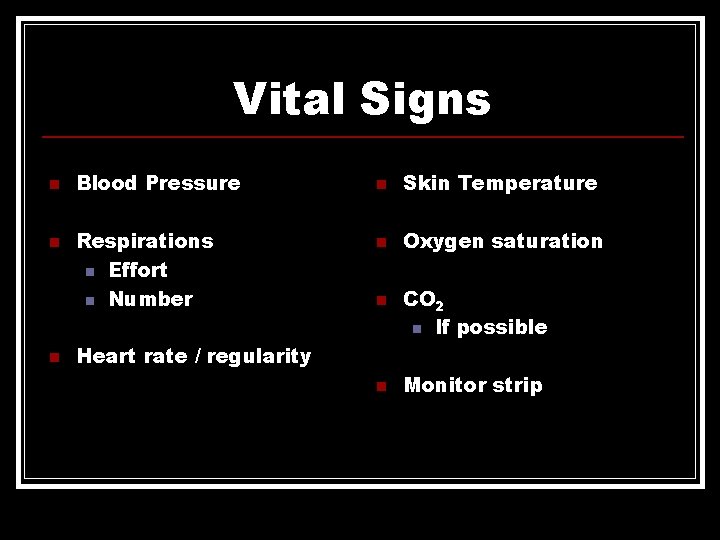
Vital Signs n n n Blood Pressure Respirations n Effort n Number n Skin Temperature n Oxygen saturation n CO 2 n If possible Heart rate / regularity n Monitor strip

Treatment n All interventions n Includes: n n Interventions by bystanders prior to your arrival Your interventions Response to treatment Document telemetry or notification calls as part of treatment
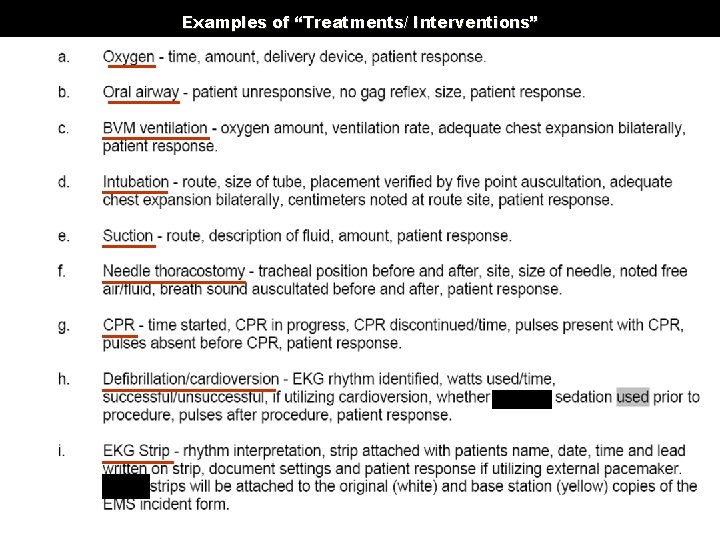
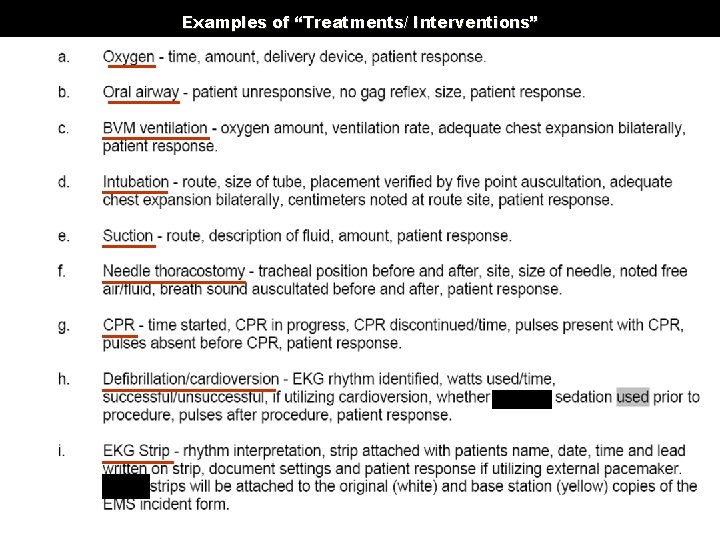
Examples of “Treatments/ Interventions”

Other Treatments/ Interventions
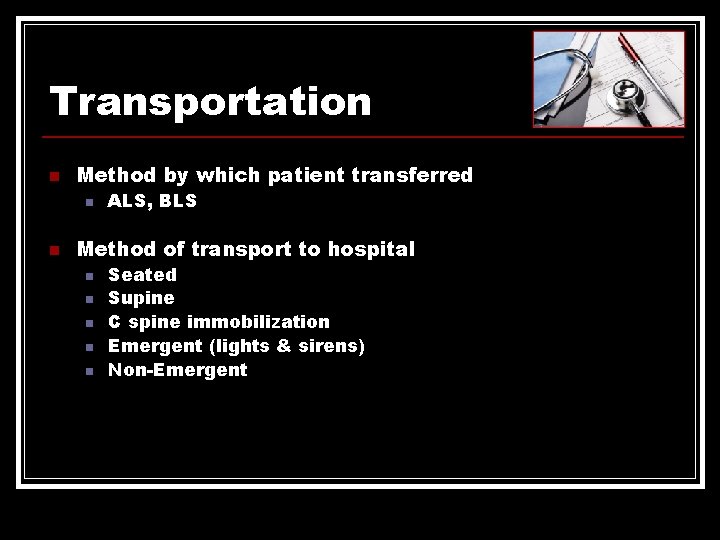
Transportation n Method by which patient transferred n n ALS, BLS Method of transport to hospital n n n Seated Supine C spine immobilization Emergent (lights & sirens) Non-Emergent
Transportation n n Description of treatment initiated / continued n “VS reassessed q 15 mins. O 2 10 LPM via NRB due to decreased pulse ox from 99% RA to 90% RA” Also: n n Changes in condition upon ED arrival Document name / title of person care transferred to at ED
“Exceptions” n Anything that is an “exception” from the norm n i. e. “Patient refused aspirin due to known allergy” n All treatment must be consistent with protocols n Through CQI process, PCRs reviewed n Document everything that was done, & if a standard treatment was not done, why not?
Exceptions: Trauma Patients n n Principles of trauma triage suggest EMS providers document if patient meets criteria for transportation to a trauma center i. e. “Patient unconscious following MVC. Transported to a Level 1 trauma center due to bilateral femur fractures”
Alternative Methods: “SOAP” n n S O A P Subjective Observations Assessment Plan
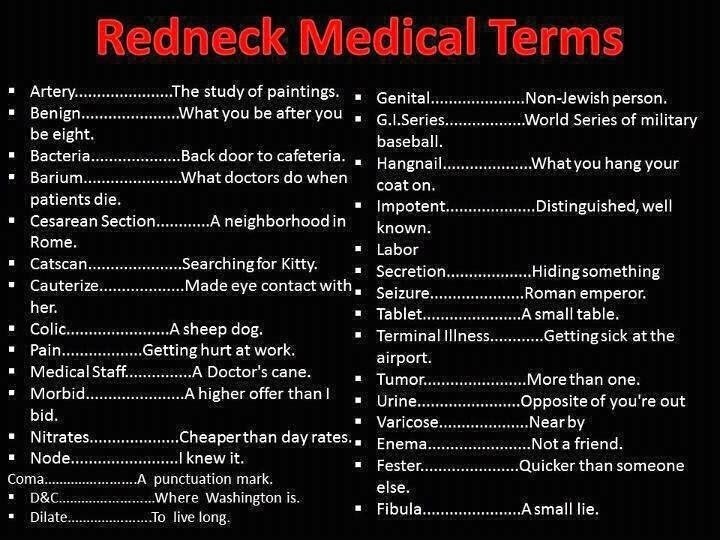
Abbreviations n No home-grown abbreviations n n n DRT, BFN Only accepted abbreviations Spelling counts n If a jury looks at your errorfilled chart they may conclude that you are as sloppy at patient care as you are at documentation

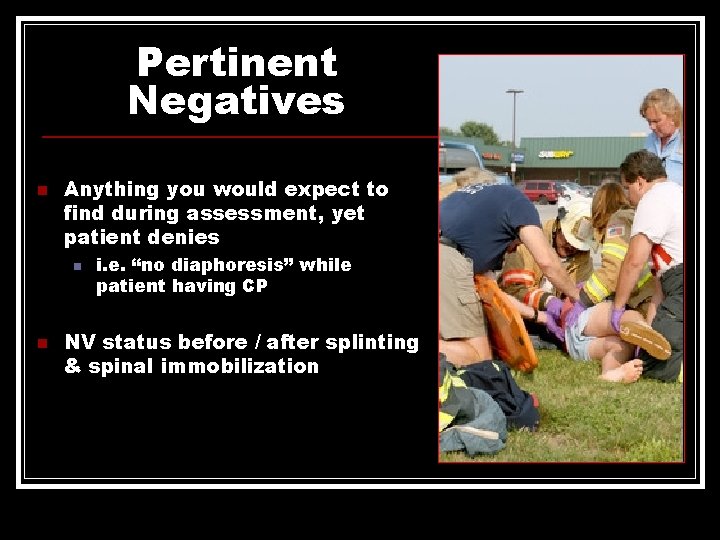
Pertinent Negatives n Anything you would expect to find during assessment, yet patient denies n n i. e. “no diaphoresis” while patient having CP NV status before / after splinting & spinal immobilization

Utstein OOHCA Documentation n Date/ Time n n Incident Number n n Accepting Hospital n Age/ DOB n n Gender n n Past Medical History n Down Time n ROSC n Time to Patient Contact n HPI Narrative n Witnessed Arrest n Bystander CPR Initial & Serial Rhythms Initial & Serial Vitals (ventilation rates!) Initial & Serial ETCO 2 Any Interventions (meds, defibrillation)
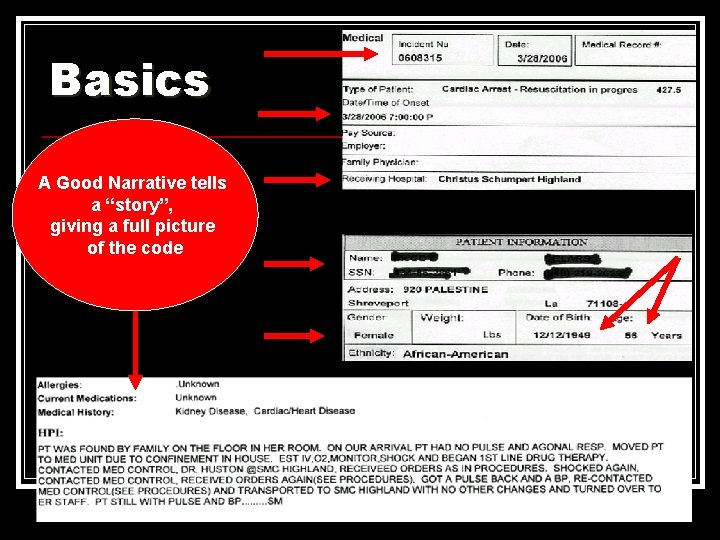
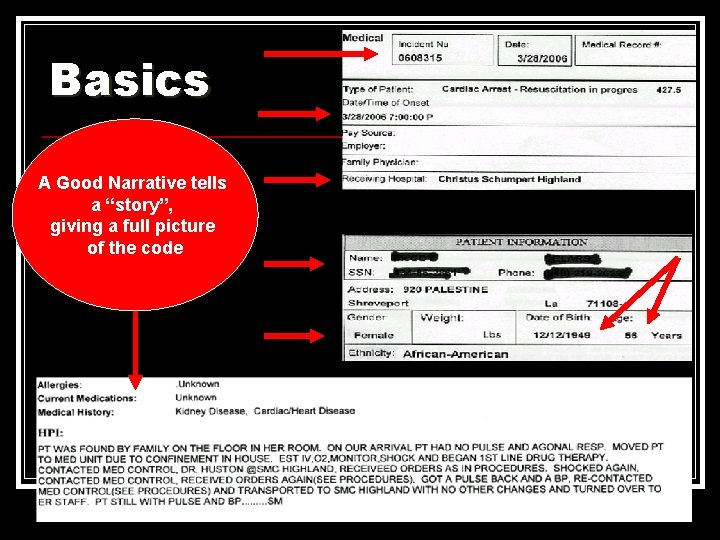
Basics A Good Narrative tells a “story”, giving a full picture of the code

Down Time n Best estimate based upon “story” received on scene n Quantify as: n n n <10 mins 11 -15 mins 16 -30 mins 31 -60 mins > 60/ unk mins
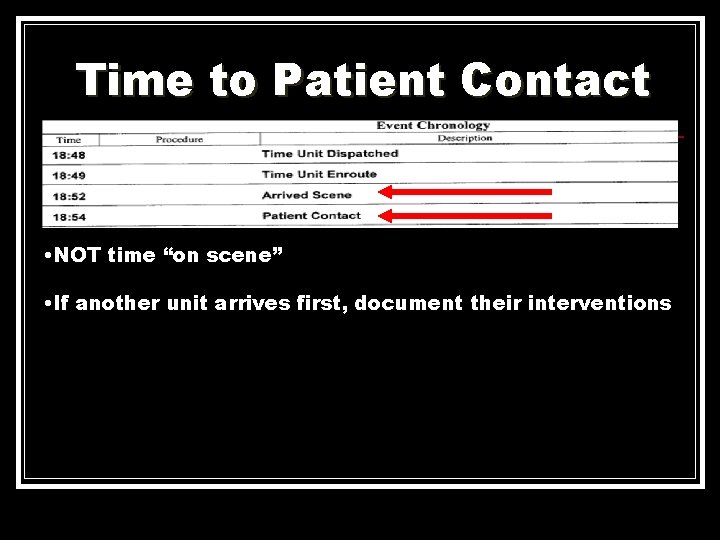
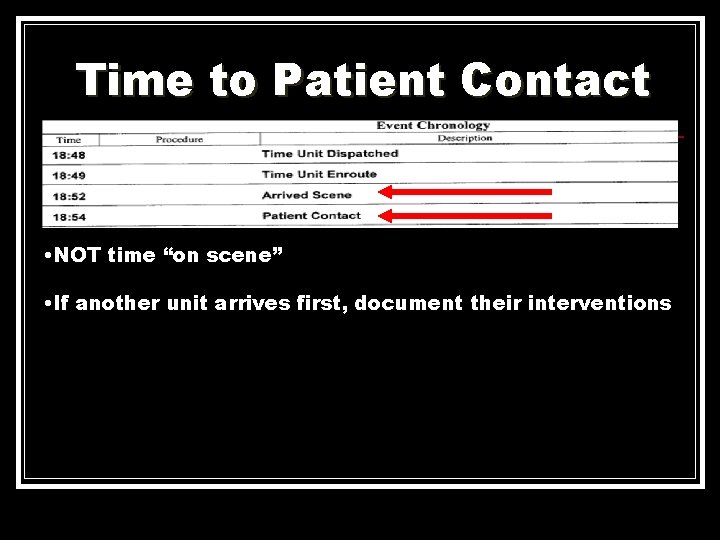
Time to Patient Contact • NOT time “on scene” • If another unit arrives first, document their interventions
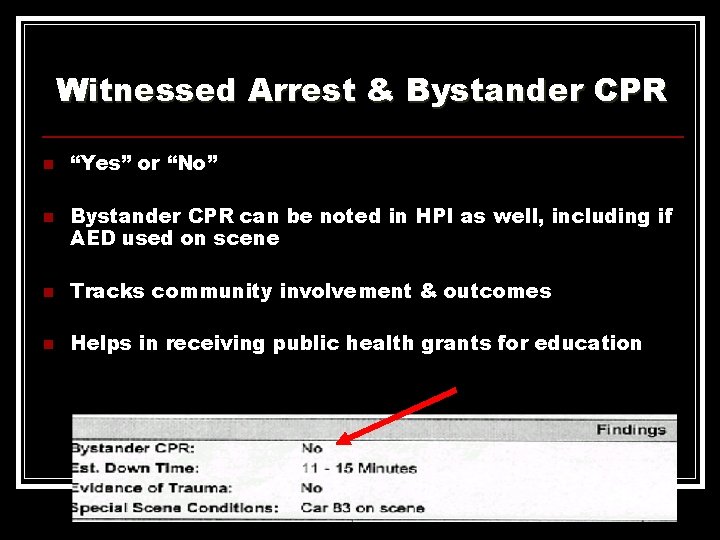
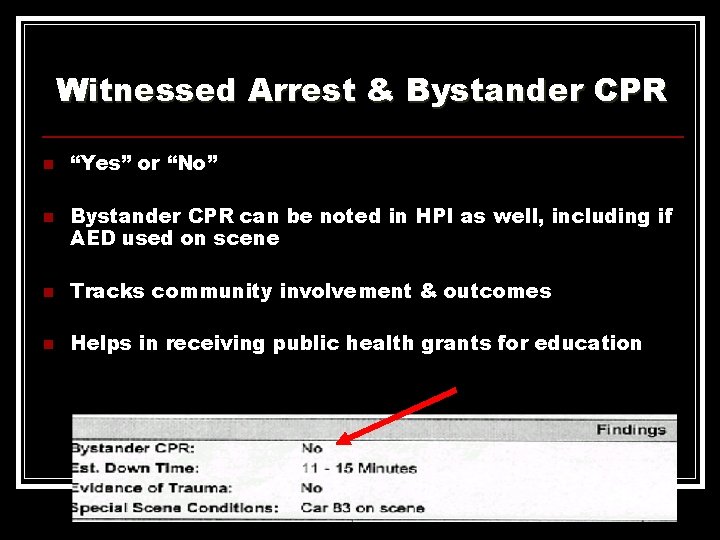
Witnessed Arrest & Bystander CPR n n “Yes” or “No” Bystander CPR can be noted in HPI as well, including if AED used on scene n Tracks community involvement & outcomes n Helps in receiving public health grants for education
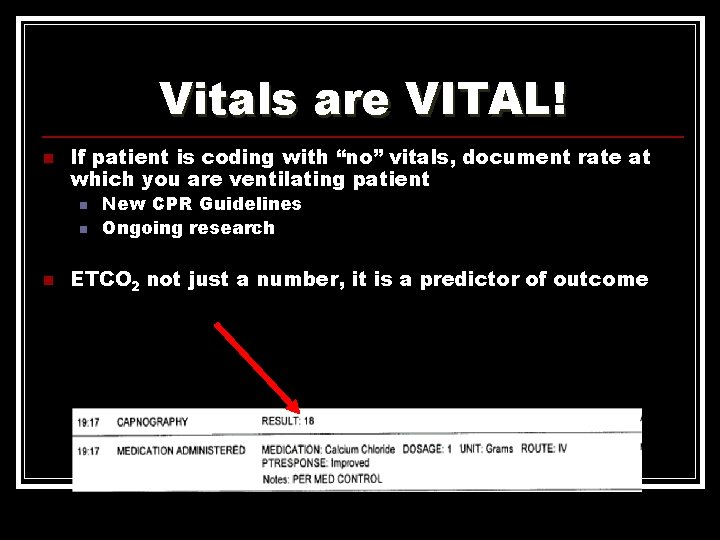
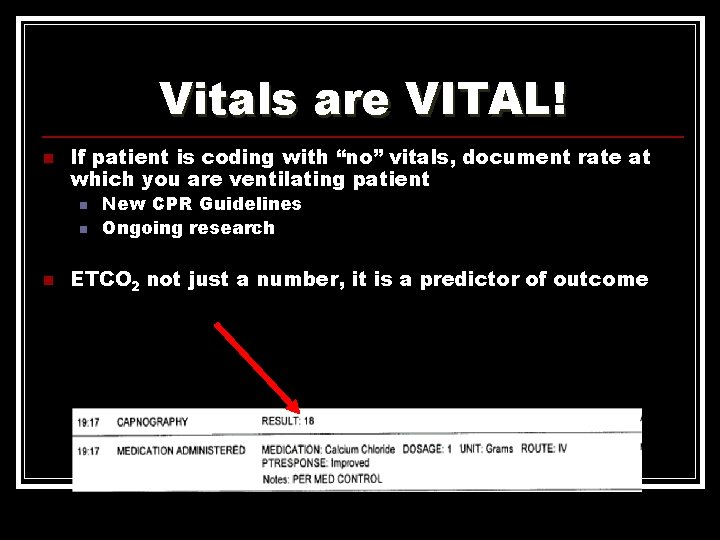
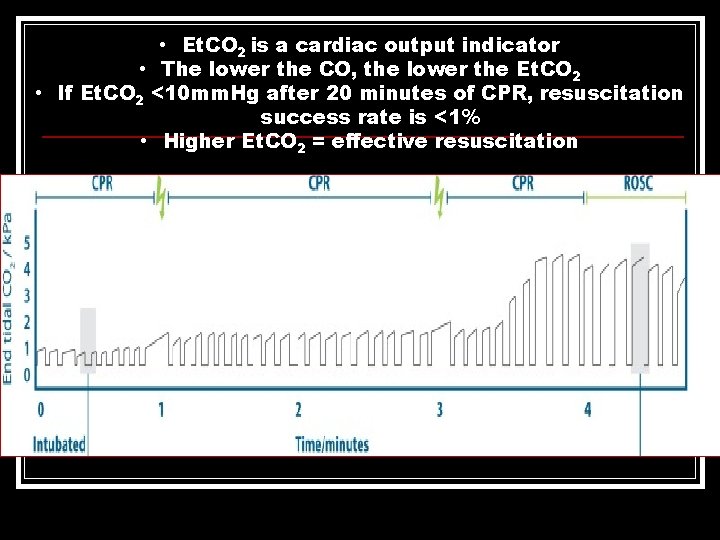
Vitals are VITAL! n If patient is coding with “no” vitals, document rate at which you are ventilating patient n n n New CPR Guidelines Ongoing research ETCO 2 not just a number, it is a predictor of outcome
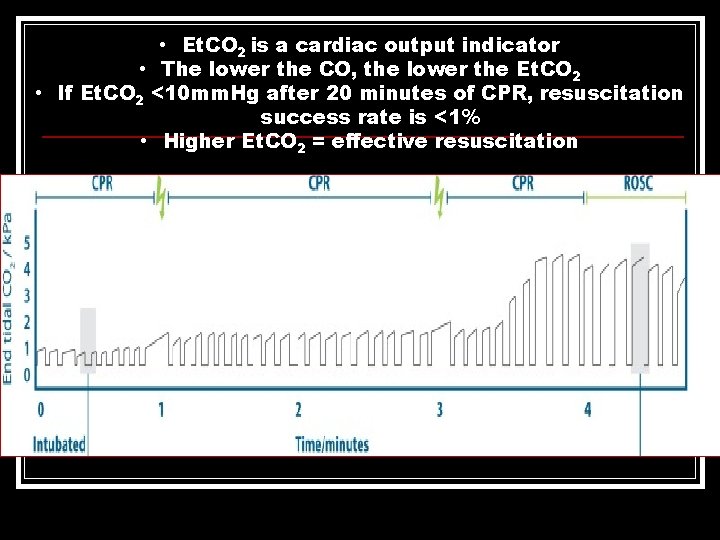
• Et. CO 2 is a cardiac output indicator • The lower the CO, the lower the Et. CO 2 • If Et. CO 2 <10 mm. Hg after 20 minutes of CPR, resuscitation success rate is <1% • Higher Et. CO 2 = effective resuscitation
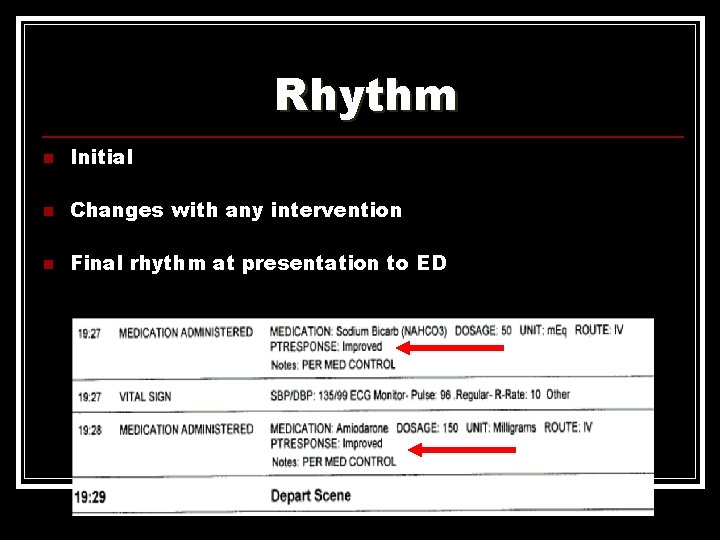
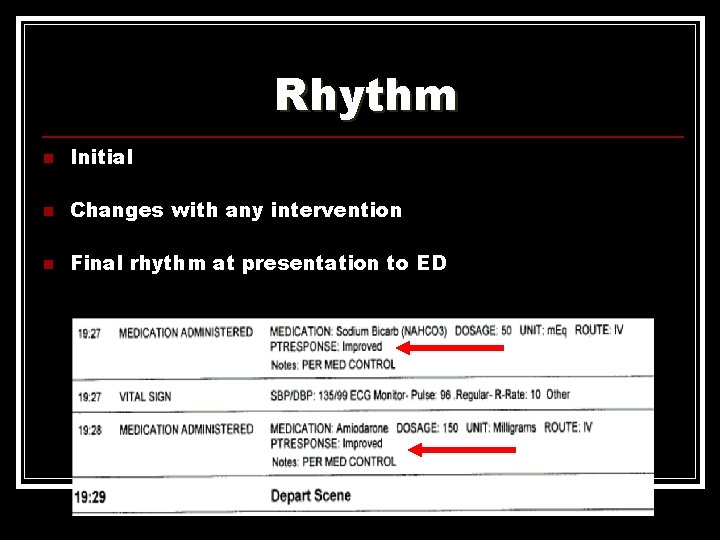
Rhythm n Initial n Changes with any intervention n Final rhythm at presentation to ED
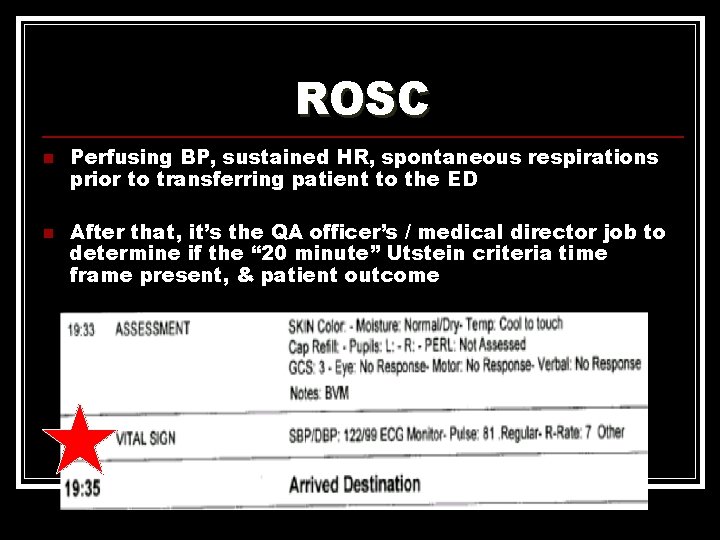
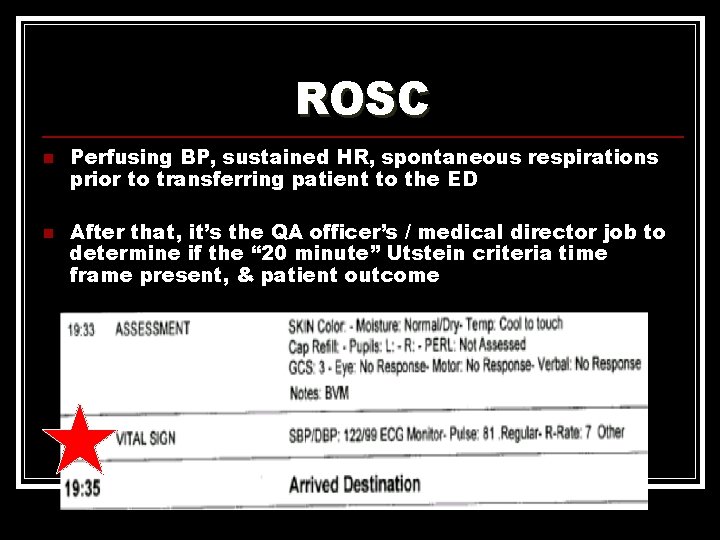
ROSC n n Perfusing BP, sustained HR, spontaneous respirations prior to transferring patient to the ED After that, it’s the QA officer’s / medical director job to determine if the “ 20 minute” Utstein criteria time frame present, & patient outcome
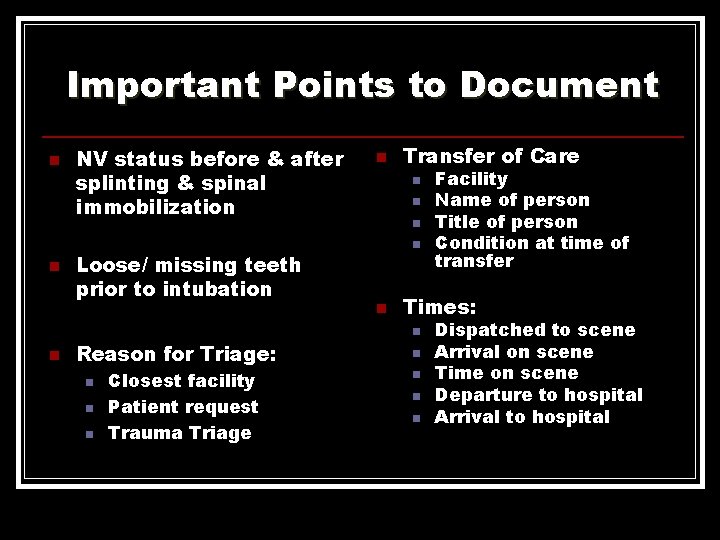
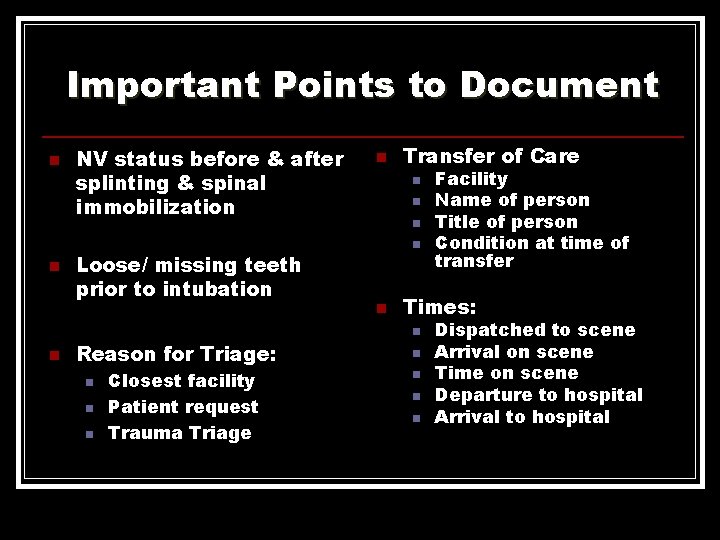
Important Points to Document n n n NV status before & after splinting & spinal immobilization Loose/ missing teeth prior to intubation Reason for Triage: n n n Closest facility Patient request Trauma Triage n Transfer of Care n n n Facility Name of person Title of person Condition at time of transfer Times: n n n Dispatched to scene Arrival on scene Time on scene Departure to hospital Arrival to hospital

Bystanders n Include name, level of training & license number of ANY non-EMS personnel who assist during assessment or management

Just The Facts, Please n n n Avoid name calling, i. e. “frequent flyer” If an error was made, document what happened & what you did to correct it Report delays in care, & how it affected treatment: n “Police did not secure the scene for 15 minutes, resulting in a delay of care”
Refusals n NEVER accepted by any pediatric patient or adult with AMS / not competent to make decisions n Document attempts to convince patient transport is recommended n n n Include potential consequences explained to patient Potential consequences always includes DEATH All refusals must be signed, including signatures by the patient/ guardian / health care agent, provider & witness n If police or an adult family member not available, your partner’s signature is appropriate
DNR / MOLST n n n DNR/ MOLST? Competent patient / health care agent can change mind at any time Include statement regarding DNR / MOLST in your report n n ? Date ? Signed Physically present at scene DNR does not equal “Do Not Treat”
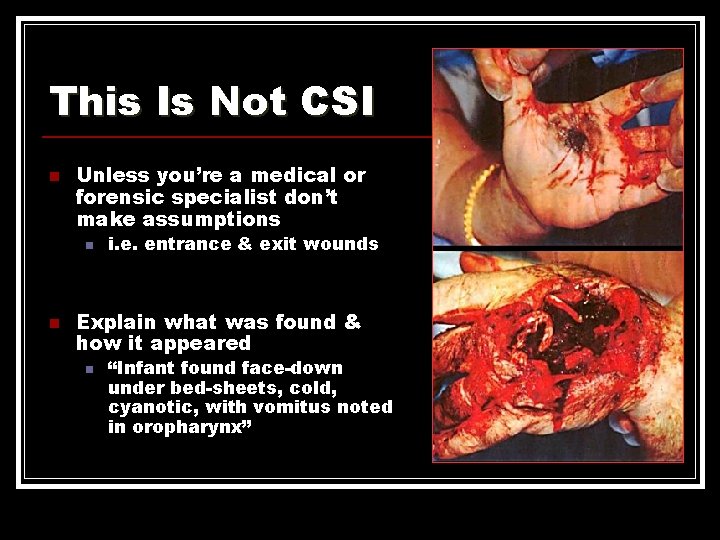
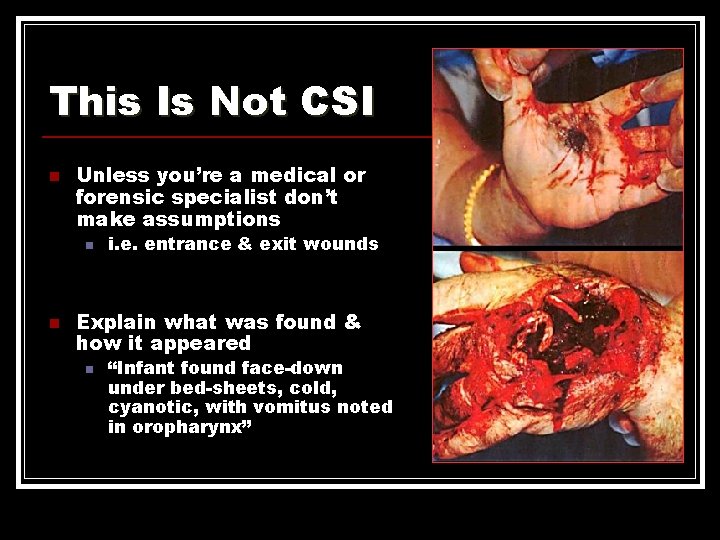
This Is Not CSI n Unless you’re a medical or forensic specialist don’t make assumptions n n i. e. entrance & exit wounds Explain what was found & how it appeared n “Infant found face-down under bed-sheets, cold, cyanotic, with vomitus noted in oropharynx”
Helpful Hints n Protect patient confidentiality n Follow HIPAA guidelines n Falsification of EMS report equals fraud n Any PCR CAN be subpoenaed without you being there to defend it

Of Course… n n n If it was not documented, it never happened If it was documented…it doesn’t mean it happened Always proofread
Questions? prehospitalmd@gmail. com / amy. gutman@hahv. org
 Dcharte
Dcharte Terstonova skala
Terstonova skala Dậy thổi cơm mua thịt cá
Dậy thổi cơm mua thịt cá Cơm
Cơm Peter bonadonna
Peter bonadonna Therapeutic communication techniques
Therapeutic communication techniques Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Cincinnati stroke scale
Cincinnati stroke scale Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Lams stroke scale
Lams stroke scale Cincinnati prehospital stroke scale
Cincinnati prehospital stroke scale Prehospital emergency care 10th edition
Prehospital emergency care 10th edition Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Discourse documentation
Discourse documentation Frida documentation
Frida documentation Omm in physical exam
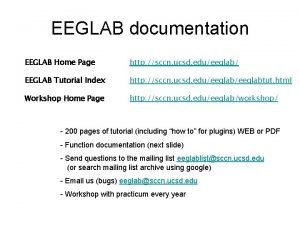
Omm in physical exam Eeglab
Eeglab Cmmi project management
Cmmi project management Internal audit documentation requirements
Internal audit documentation requirements Onap wiki
Onap wiki Production documentation
Production documentation Code documentation generator
Code documentation generator Adxstudio documentation
Adxstudio documentation Octopus rest api
Octopus rest api Network design documentation
Network design documentation Pcr documentation
Pcr documentation Google vision api docs
Google vision api docs Huawei documentation
Huawei documentation Nopcommerce github
Nopcommerce github Cardiac assessment documentation example
Cardiac assessment documentation example Continuous improvement documentation
Continuous improvement documentation Python documentation generator
Python documentation generator Apostol tnokovski
Apostol tnokovski Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Frisk letter of reprimand
Frisk letter of reprimand Language
Language What is documentation in computer
What is documentation in computer Types of medical documentation
Types of medical documentation Sequence diagram of gym management system
Sequence diagram of gym management system Documentation of specimen in laboratory
Documentation of specimen in laboratory Chirocredits
Chirocredits Documentation in accounting
Documentation in accounting Pattie maes sixth sense
Pattie maes sixth sense Documentation for graduation project computer science
Documentation for graduation project computer science Ibm igi documentation
Ibm igi documentation