Cardiovascular Emergencies Amy Gutman MD Amy Gutmanuc edu







- Slides: 70
Cardiovascular Emergencies Amy Gutman MD Amy. Gutman@uc. edu
Overview n Myocardial Infarction n Stroke
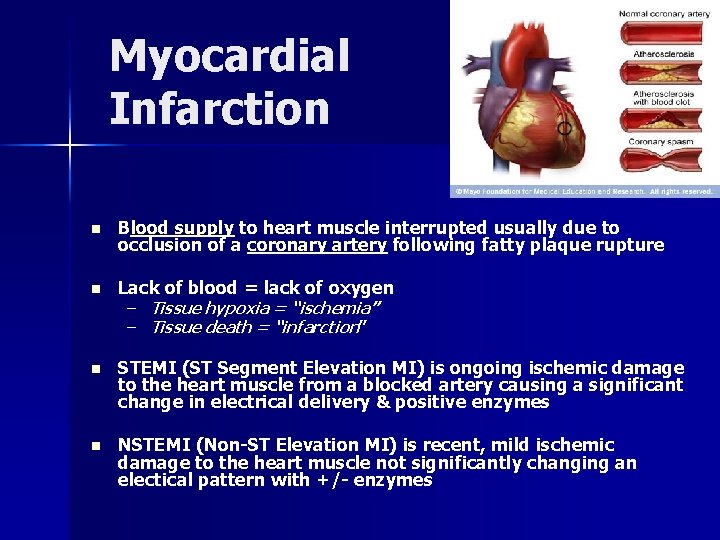
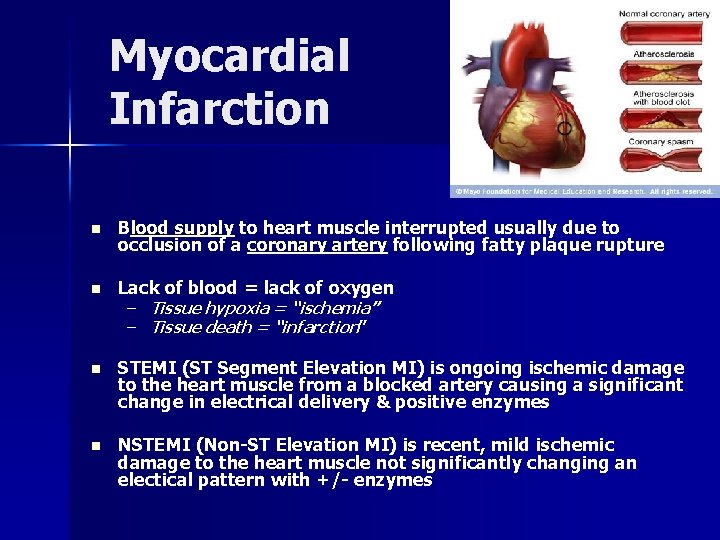
Myocardial Infarction n Blood supply to heart muscle interrupted usually due to occlusion of a coronary artery following fatty plaque rupture n Lack of blood = lack of oxygen n STEMI (ST Segment Elevation MI) is ongoing ischemic damage to the heart muscle from a blocked artery causing a significant change in electrical delivery & positive enzymes n NSTEMI (Non-ST Elevation MI) is recent, mild ischemic damage to the heart muscle not significantly changing an electical pattern with +/- enzymes – Tissue hypoxia = “ischemia” – Tissue death = “infarction”
Epidemiology n Coronary artery disease (CAD) is the #1 cause of death in developed countries – #3 rd to AIDS & respiratory infections in developing countries n In the US: – – – 1 in 5 deaths 7, 200, 000 men & 6, 000 women have CAD 1, 200, 000 people suffer a an MI annually 40% die as a result of the attack within 90 days Every 65 secs, an American dies of a coronary event

Risk Factors n Cardiovascular disease n Older age – Men >40 – Women >50 n Tobacco smoking n High lipids (triglycerides, LDLs) & low HDLs n Diabetes n HTN n Obesity n Kidney disease n CHF n Excessive alcohol consumption n Cocaine / stimulant usage n Chronic high stress levels n Male gender
Socioeconomic & Genetic Risk Factors n Shorter education n Inflammatary diseases n Lower income (particularly in women) n Periodontal disease n Baldness & hair greying n Diagonal earlobe crease n Living with a partner n Birth control pills n Nicotine usage
Triggers n Intense psychological or physical exertion n Intense exercise & subsequent recovery associated with a 6 x higher MI rate for people who are physically very fit – For those in poor condition, the rate is 35 x higher n Increased incidence in the morning hours (0300 -0600) – – – Cortisol spike Increased platelet aggregation Increased inflammation
Symptoms n “Angina” is most common – Sensation of tightness, pressure, or squeezing – Radiates & may mimic heartburn n Dyspnea occurs when heart damage limits cardiac output causing heart failure & pulmonary edema n Loss of consciousness due to inadequate cerebral perfusion or cardiogenic shock n Other ssx from nervous system catecholamine surge – Diaphoresis – Weakness – Vertigo – Palpitations
Atypical Symptoms n Women & geriatrics often experience atypical symptoms n The most common symptoms of MI in women include dyspnea, insomnia & fatigue – “Angina” less predictive of ischemia than in men – 50% experience warning ssx prior to infarction, often weeks earlier n 25% of all MIs are “silent” – Discovered later on ECG or at autopsy – Common in the elderly, diabetes, post heart transplantation
Differential Diagnosis n Pulmonary embolism n Aortic dissection n Pericardial effusion n Cardiac tamponade n Tension pneumothorax n Esophageal rupture
Physical Exam n Diaphoresis – Cool & pale skin due to vasoconstriction n Dyspnea / Evidence of CHF – Elevated JVD, LE swelling & decreased cardiac output n Anxiety or irritability n Abnormal &/or irregular pulse rate n Hypo / Hypertension n Nausea or vomiting n Auscultation abnormalitites: – S 3 & S 4, systolic murmurs, pericardiac friction rub
EKG n Detects electrical abnormalities n Limitations: – A “normal” EKG does not rule out acute MI – Represents a brief period of time – Difficult for evaluating posterior & lateral heart – Mistakes in interpretation are relatively common n STEMI requires >1 mm ST elevation in contiguous limb leads & >2 mm elevation in precordial leads n ECG mimics of acute MI include: LVH, LBBB, paced rhythms, early repolarization, pericarditis, hypo/erkalemia, ventricular aneurysm
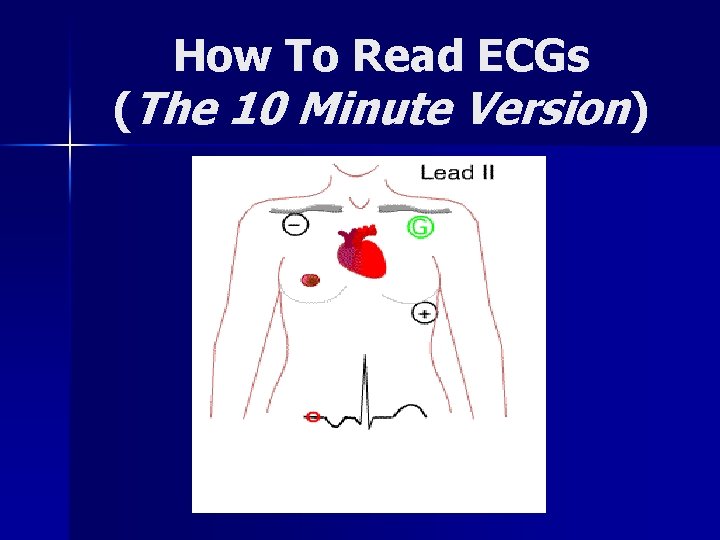
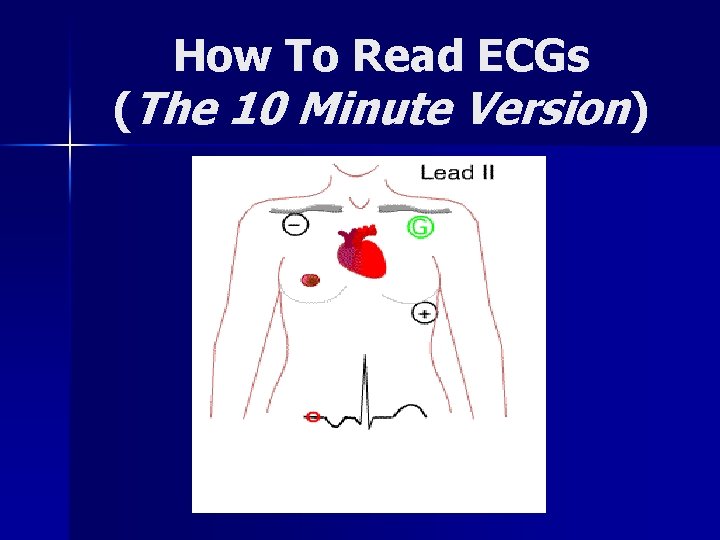
How To Read ECGs (The 10 Minute Version)
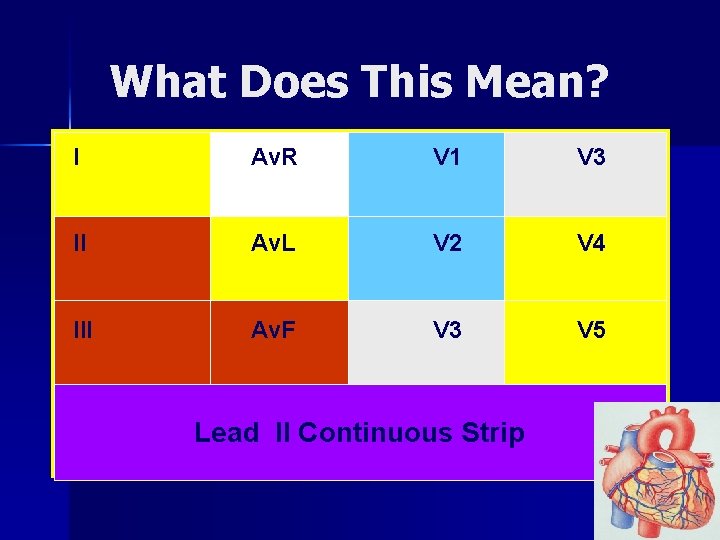
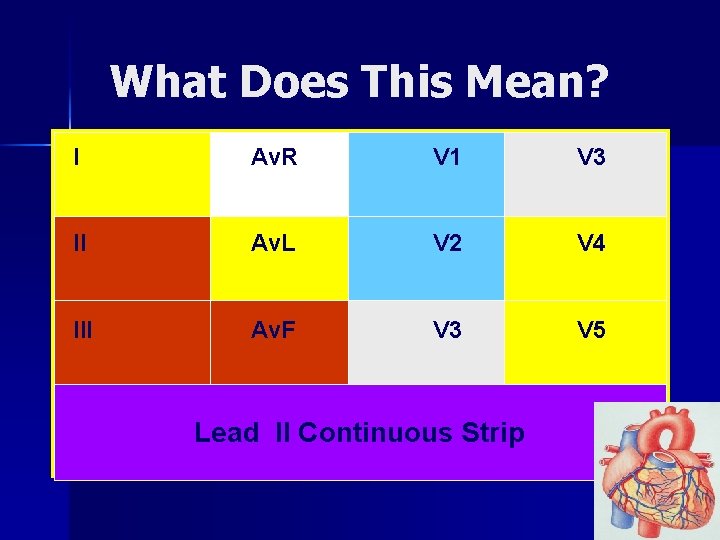
What Does This Mean? I Av. R V 1 V 3 II Av. L V 2 V 4 III Av. F V 3 V 5 Lead II Continuous Strip
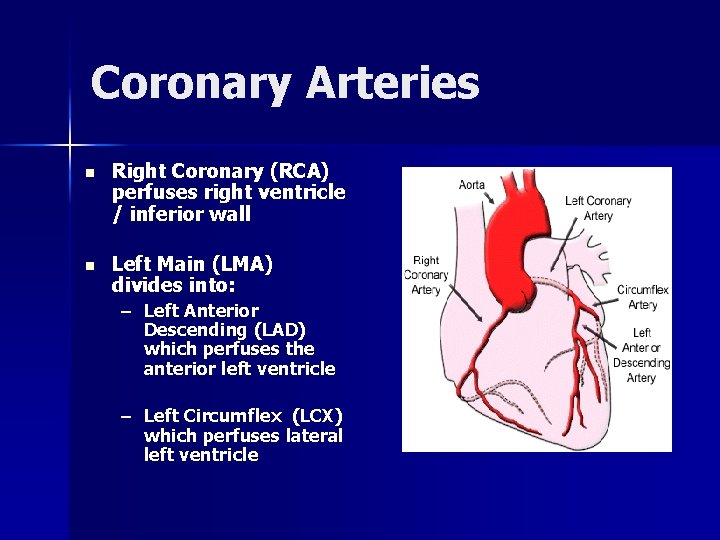
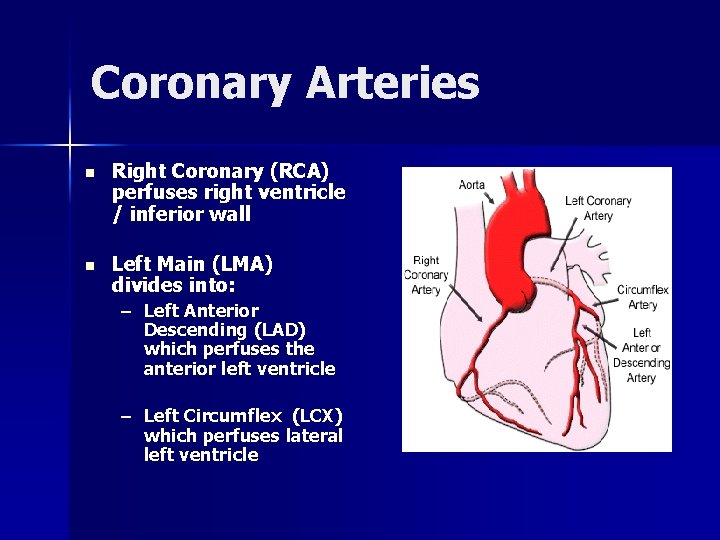
Coronary Arteries n Right Coronary (RCA) perfuses right ventricle / inferior wall n Left Main (LMA) divides into: – Left Anterior Descending (LAD) which perfuses the anterior left ventricle – Left Circumflex (LCX) which perfuses lateral left ventricle

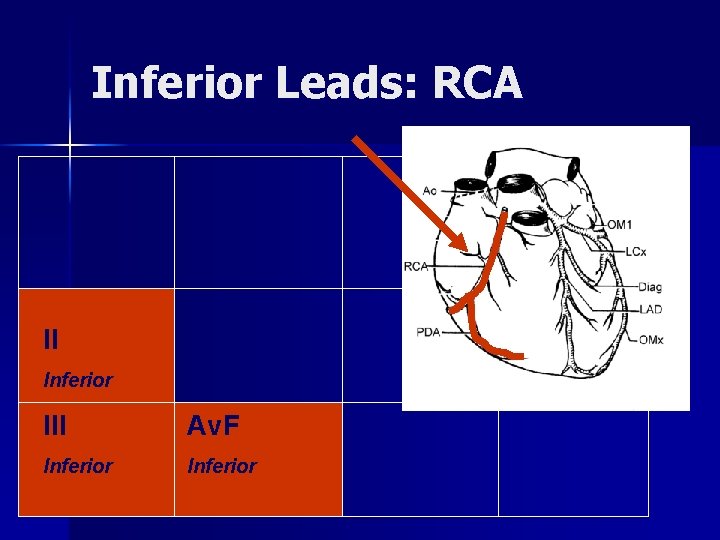
Inferior = Right Coronary Artery II, III, Av. F n Right ventricle positioned down & inferior n Perfused by RCA n Innervated by same nerve as stomach: – Inferior wall MIs cause nausea & vomiting
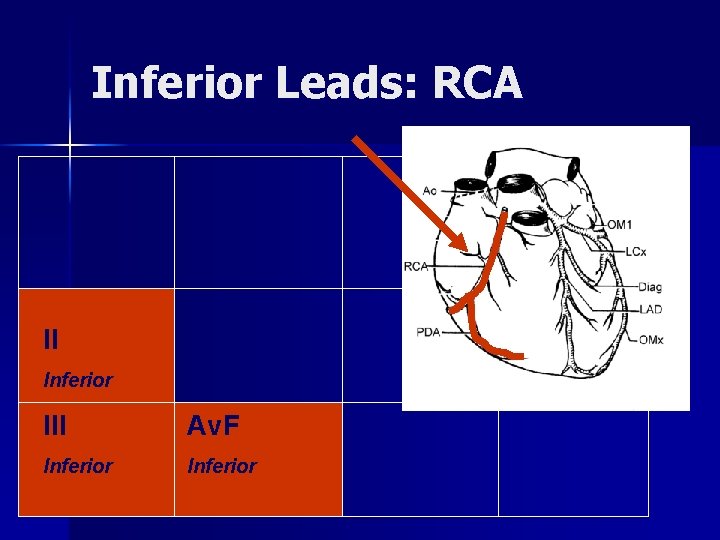
Inferior Leads: RCA II Inferior III Av. F Inferior
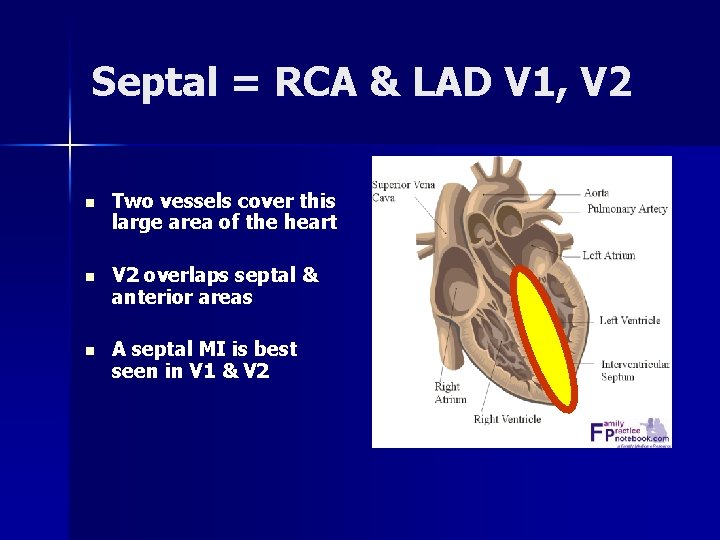
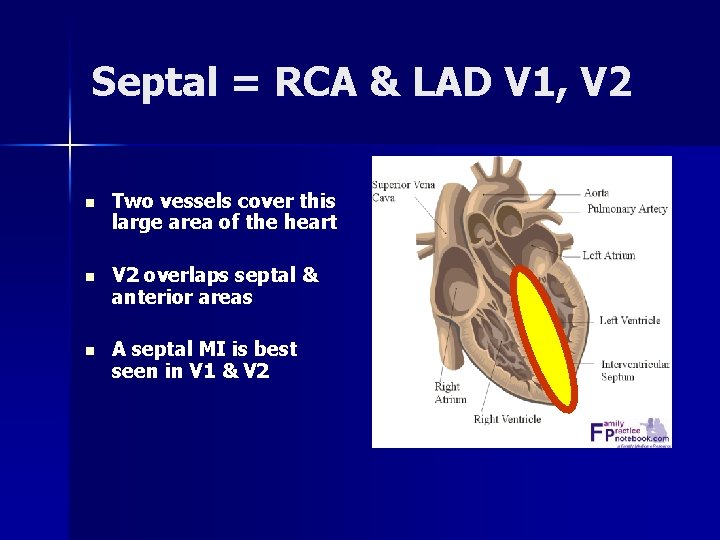
Septal = RCA & LAD V 1, V 2 n Two vessels cover this large area of the heart n V 2 overlaps septal & anterior areas n A septal MI is best seen in V 1 & V 2

Septal Leads V 1 Septal V 2 Septal
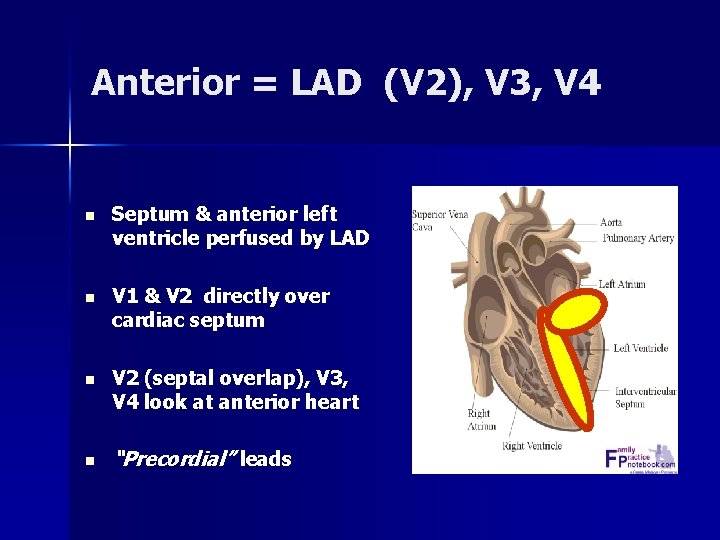
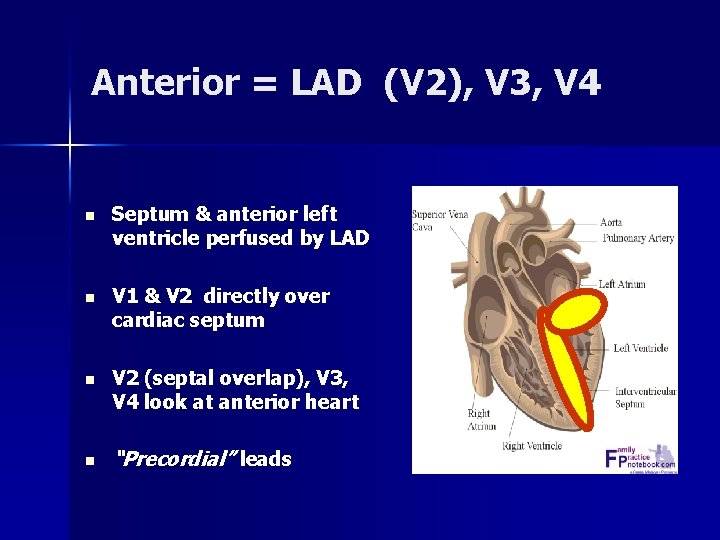
Anterior = LAD (V 2), V 3, V 4 n Septum & anterior left ventricle perfused by LAD n V 1 & V 2 directly over cardiac septum n V 2 (septal overlap), V 3, V 4 look at anterior heart n “Precordial” leads
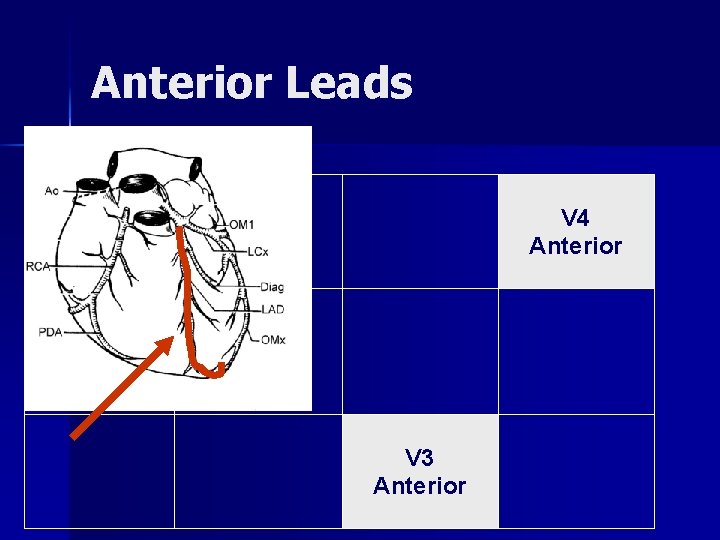
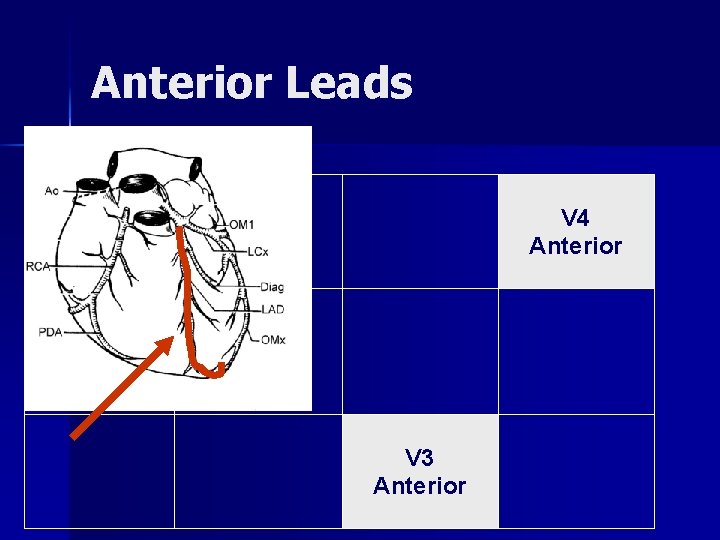
Anterior Leads V 4 Anterior V 3 Anterior

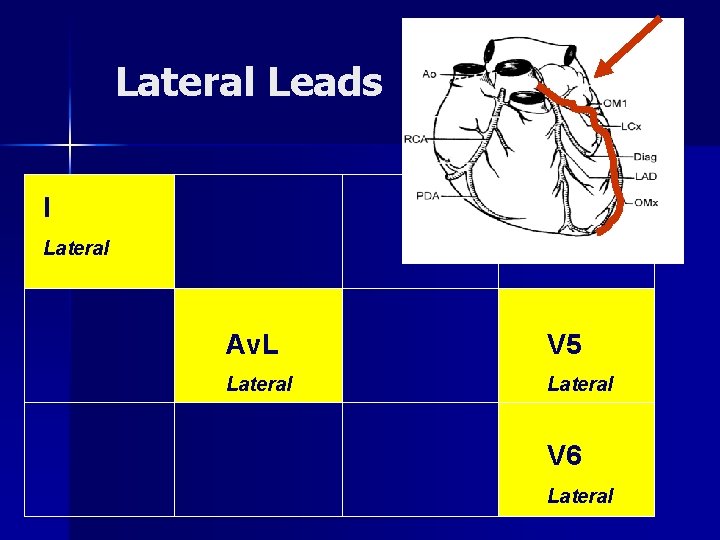
Lateral: LMA & LCX I, Av. L, V 5, V 6 n Winds around left chest & lateral left ventricle n LMA “Widow Maker”: – Divides into LAD & LCX – LMA occlusion causes a massive antero-lateral MI
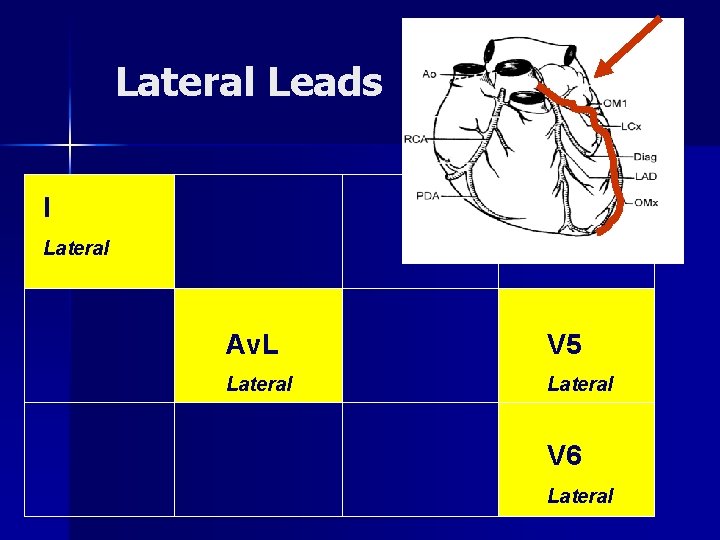
Lateral Leads I Lateral Av. L V 5 Lateral V 6 Lateral
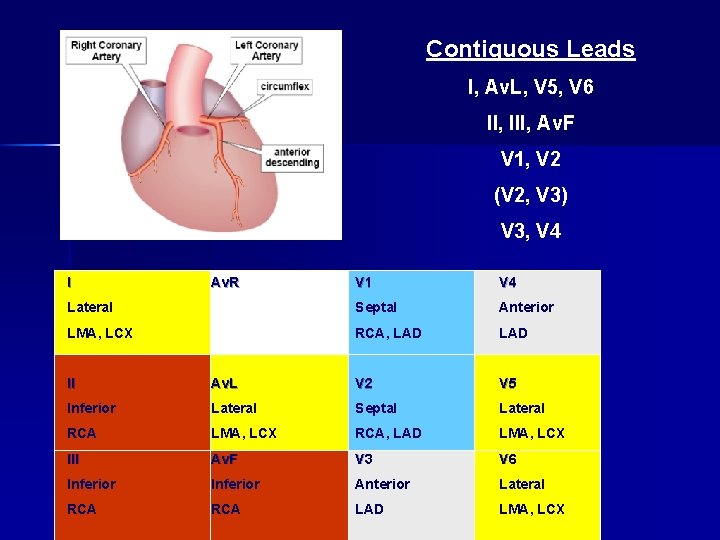
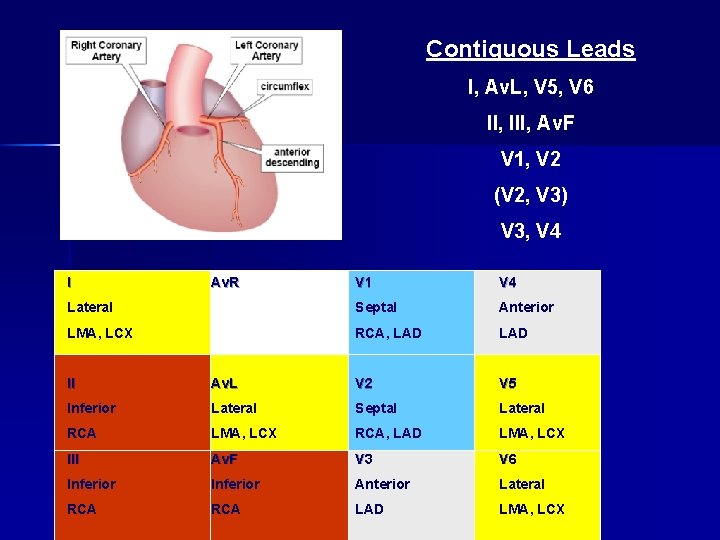
Contiguous Leads I, Av. L, V 5, V 6 II, III, Av. F V 1, V 2 (V 2, V 3) V 3, V 4 I Av. R V 1 V 4 Lateral Septal Anterior LMA, LCX RCA, LAD II Av. L V 2 V 5 Inferior Lateral Septal Lateral RCA LMA, LCX RCA, LAD LMA, LCX III Av. F V 3 V 6 Inferior Anterior Lateral RCA LAD LMA, LCX
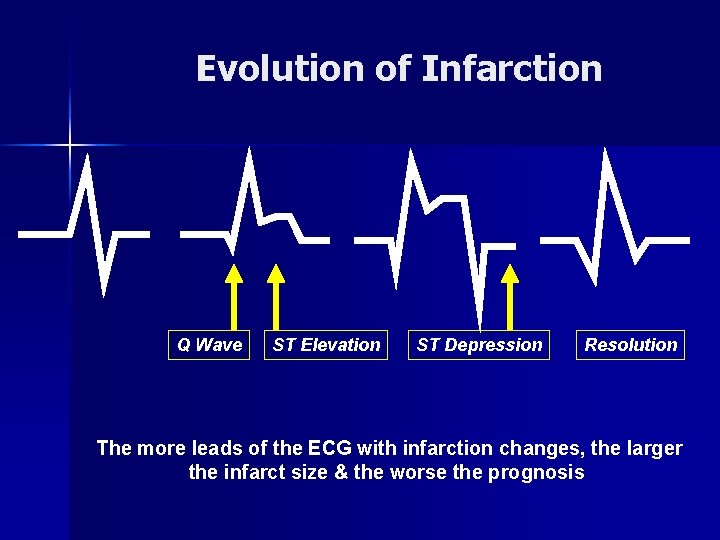
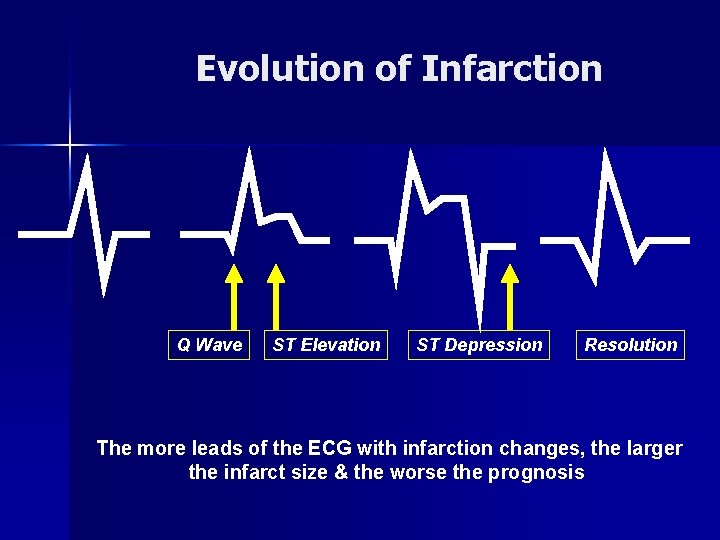
Evolution of Infarction Q Wave ST Elevation ST Depression Resolution The more leads of the ECG with infarction changes, the larger the infarct size & the worse the prognosis
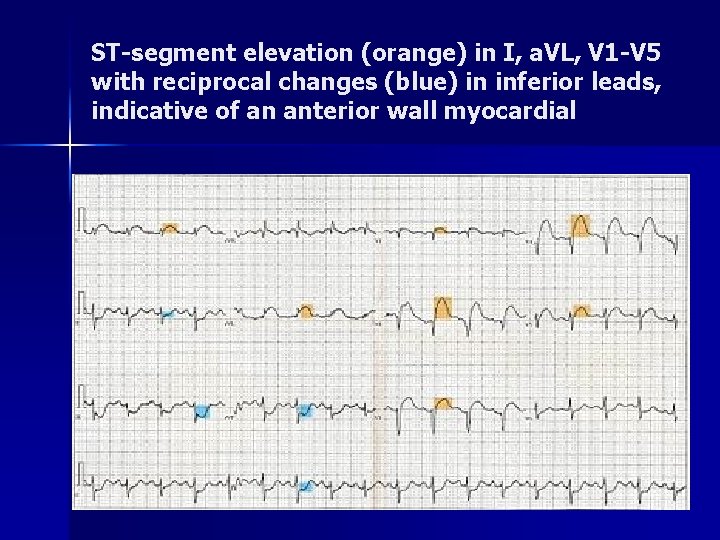
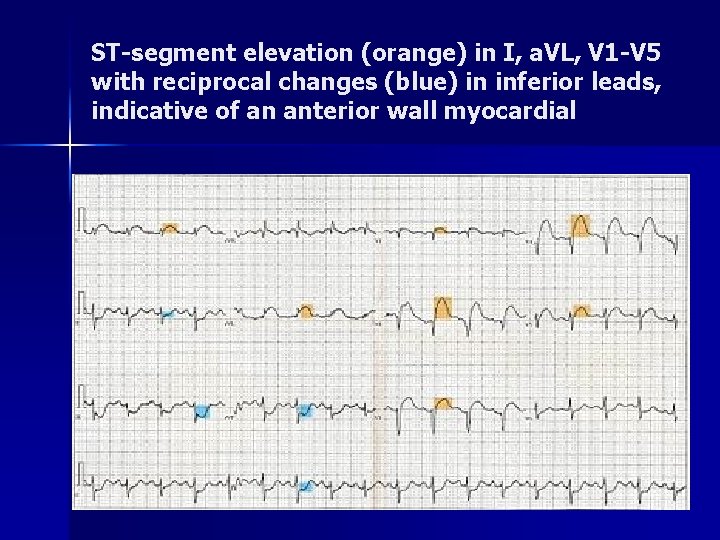
ST-segment elevation (orange) in I, a. VL, V 1 -V 5 with reciprocal changes (blue) in inferior leads, indicative of an anterior wall myocardial
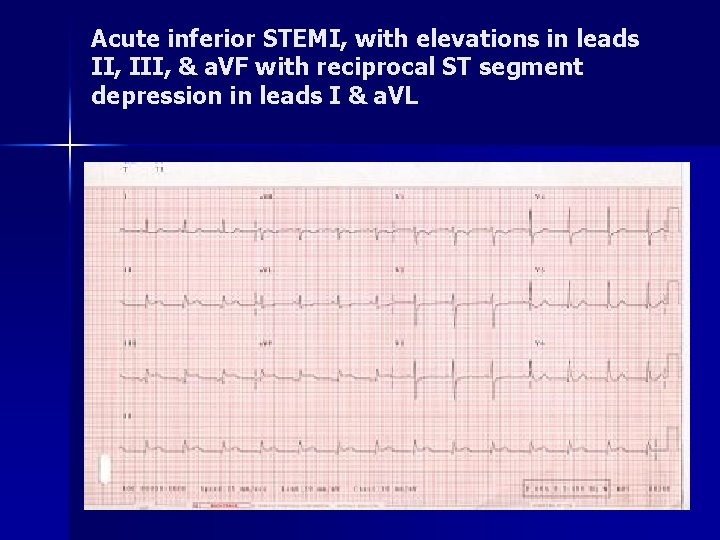
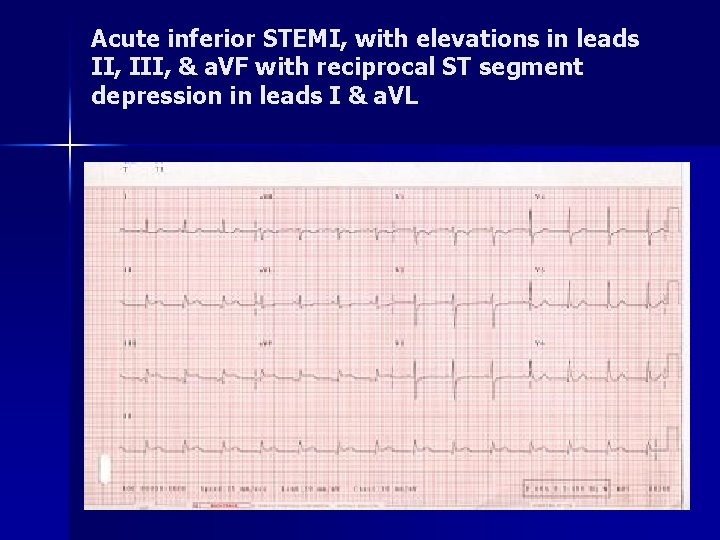
Acute inferior STEMI, with elevations in leads II, III, & a. VF with reciprocal ST segment depression in leads I & a. VL
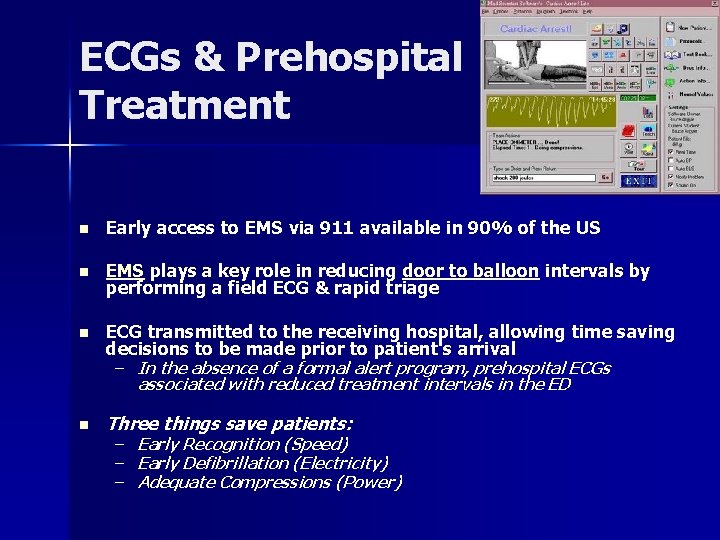
ECGs & Prehospital Treatment n Early access to EMS via 911 available in 90% of the US n EMS plays a key role in reducing door to balloon intervals by performing a field ECG & rapid triage n ECG transmitted to the receiving hospital, allowing time saving decisions to be made prior to patient's arrival – In the absence of a formal alert program, prehospital ECGs associated with reduced treatment intervals in the ED n Three things save patients: – Early Recognition (Speed) – Early Defibrillation (Electricity) – Adequate Compressions (Power)

Prehospital Management (Adopted from AOM) n BSI / PPE n Place patient in a position of comfort while performing a focused history & physical examination n Obtain & serially monitor vitals n Maintain airway & provide O 2 if <94% n Initiate early transport – Request ALS back-up if available
Prehospital Management ~ Medications n Administer 4 baby aspirins n Ask if patient has personal NTG; if no contraindications give 0. 4 under the tongue every 5 mins if in pain – Ask if patient has taken Viagra, Levitra, Cialis in past 24 - 72 hrs n Reassess q 3 - 5 minutes or if any chest discomfort, lightheadedness, dizzy, &/or hypotension n If patient is symptomatic after administration of NTG, place patient flat or Trandelenberg n If the patient experiences no relief & SBP remains > 100 mm Hg contact medical control for further direction n Continue serial assessments
Cardiac Arrest Management n Unresponsive, with apneic or agonal respirations & pulseless n BSI / PPE / ABCs n Start CPR – If CPR started prior to your arrival, stop & confirm apnea & pulselessness n Request ALS back-up or intercept n Continue CPR x 2 minutes then apply AED
Cardiac Arrest Protocol n If pulse present: – Assess ABCs – If respirations adequate, administer high flow O 2 via NRB – If respirations not adequate, assist with BVM at 8 -10 BPM & prepare to provide an advanced airway n If pulse absent: – Assist ventilations with BVM at 8 -10 BPM & prepare to provide an advanced airway – Stop CPR, ensure people are clear of patient & again press "Analyze" on the AED – Follow AED directions for "Deliver Shock" or "No Shock“ – Resume CPR immediately after shock without pulse check
Cardiac Arrest Protocol n If indicated by the AED, provide up to a total of 3 shocks (not stacked) n Contact medical control after the 3 rd shock or after three consecutive "No Shock" advisories are obtained n Advanced airway should be performed after the second shock or after the second "No Shock“
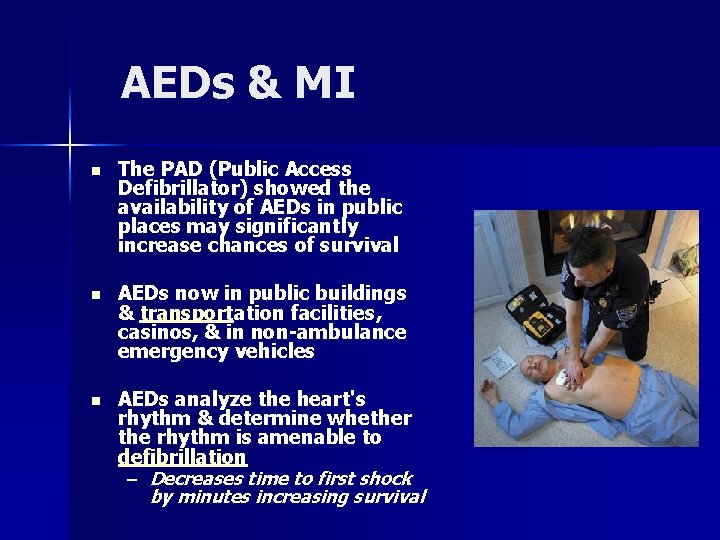
AEDs & MI n The PAD (Public Access Defibrillator) showed the availability of AEDs in public places may significantly increase chances of survival n AEDs now in public buildings & transportation facilities, casinos, & in non-ambulance emergency vehicles n AEDs analyze the heart's rhythm & determine whether the rhythm is amenable to defibrillation – Decreases time to first shock by minutes increasing survival
MI Arrhythmia Pathophysiology n Injured heart tissue conducts electrical impulses more slowly than normal tissue n The difference in conduction velocities triggers a feedback loop causing lethal arrhythmias n The most serious of these arrhythmias is ventricular fibrillation, the leading cause of sudden cardiac death n Ventricular tachycardia usually results in rapid heart rates that prevent the effective pumping of blood, droping cardiac output & BP, leading to further coronary ischemia & extension of the infarction
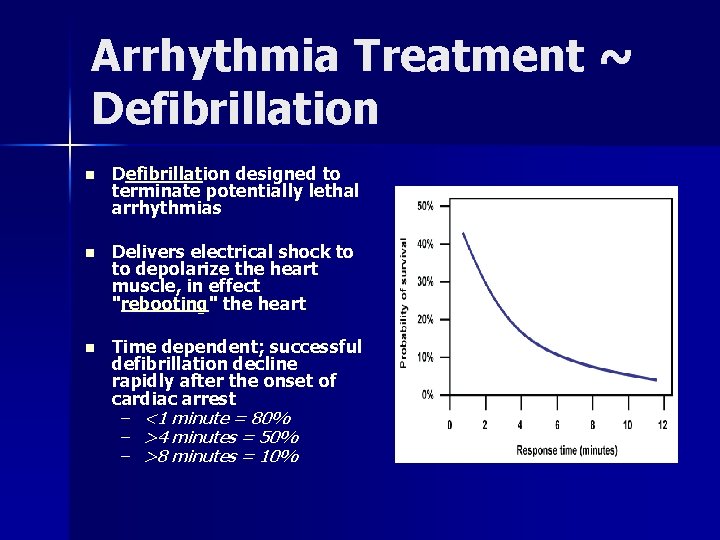
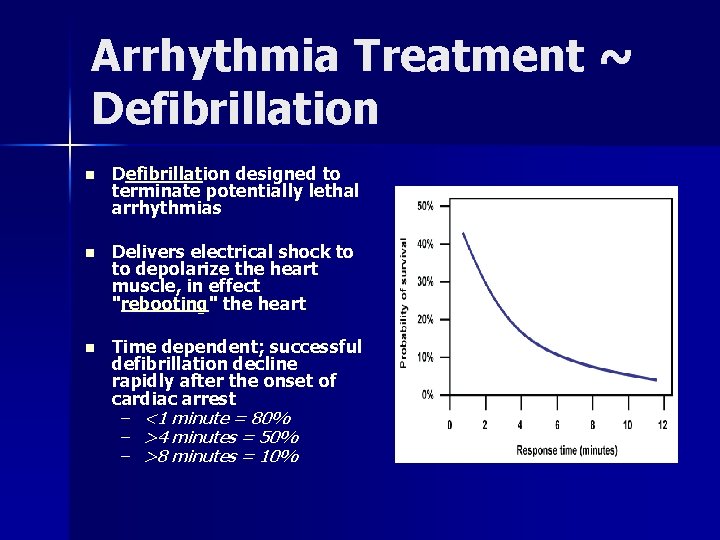
Arrhythmia Treatment ~ Defibrillation n Defibrillation designed to terminate potentially lethal arrhythmias n Delivers electrical shock to to depolarize the heart muscle, in effect "rebooting" the heart n Time dependent; successful defibrillation decline rapidly after the onset of cardiac arrest – <1 minute = 80% – >4 minutes = 50% – >8 minutes = 10%
Cardiac Arrest Important Points ~ Peds, Trauma, AEDs n Weight not age used for AED as cardiac injury can occur at 10 joules/kg – AEDs cannot provide low energy required for pediatric defibrillation n In traumatic arrest the AED may not be helpful as condition is result of blood loss requiring surgical intervention rather than electricity n When using the AED during transport, stop the vehicle to analyze the rhythm or deliver shocks n If patient is successfully defibrillated, has a pulse, & rearrests, continue rhythm analysis & follow directions of the AED for "Deliver Shock" or "No Shock" advisories
MI Hospital Management Strategies
Thrombolysis n Treatment of STEMI within 12 hours of the onset of symptoms & primary PCI is immediately available – Effectiveness highest in the first 2 hours – Failure rates >20% n Thrombolytics contraindicated in treatment of unstable angina, NSTEMI, & treatment of individuals with evidence of cardiogenic shock n Intracranial hemorrhage & stroke are serious side effects – Previous ICH, age, & thrombolytic regimen being used – Complications are significantly higher with rescue PCI than with primary PCI due to the action of the thrombolytic agent
Coronary Artery Bypass Surgery (CABG) n Emergency bypass surgery for MI less common then PCI or medical management n CABG with intra-aortic balloon pumps simultaneously treats a mechanical complication (i. e. valvular defect) & cardiogenic shock – Uses an artery or vein from the patient being implanted to bypass coronary artery occlusions n There is a higher mortality rate than in PCI of performed immediately following infarction n In patients with >2 arteries affected, CABG associated with higher long-term survival compared to PCI
Primary Percutaneous Coronary Intervention (PCI) n Primary PCI restores flow in 95% of patients with STEMI n Goal is to open artery <90 mins after symptom onset – “Symptoms-to-balloon” n Angiogram determines anatomical location of blocked, followed by balloon angioplasty +/- stenting – Stents decrease rates of vessel restenosis compared to balloon angioplasty
Key Prehospital Points n Early recognition n Aspirin / O 2 / AED saves lives n Goal is in the catherization lab < 90 mins post onset of symptoms
Stroke n Loss of brain function from a cerebralvascular abnormality – WHO: "neurological deficit of cerebrovascular cause persisting >24 hrs or causing death within 24 hrs“ n Causes from a lack of blood flow (ischemic), or an interrupted blood flow (hemorrhagic) n Hippocrates (460 BC) termed stroke “Apoplexy”, which is Greek for "struck down with violence”
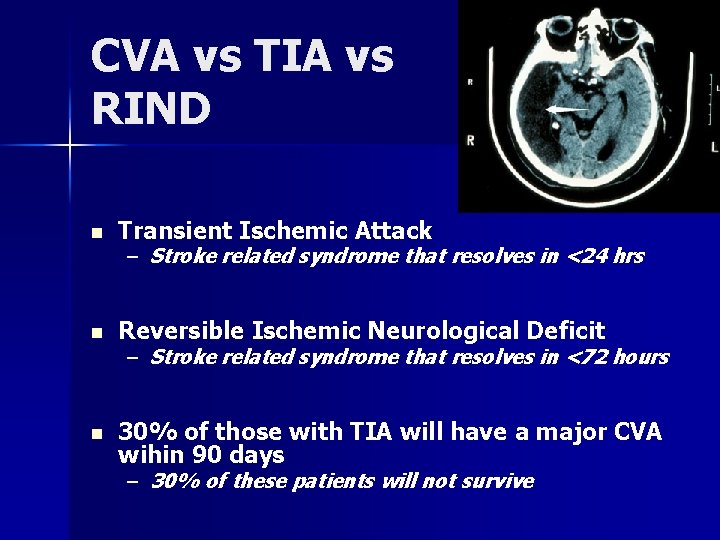
CVA vs TIA vs RIND n Transient Ischemic Attack n Reversible Ischemic Neurological Deficit n 30% of those with TIA will have a major CVA wihin 90 days – Stroke related syndrome that resolves in <24 hrs – Stroke related syndrome that resolves in <72 hours – 30% of these patients will not survive
Epidemiology n Disability affects 75% of survivors – #1 cause of adult disability in the US & Europe – #3 cause of death worldwide after CAD & cancer – Causes 10% of deaths worldwide n Management costs $43 billion annually in the US n Incidence increases exponentially >30 yrs – Etiology varies by age – 95% of strokes occur in people >45 yo – 75% of strokes occur in people >65 yo
Gender Differences n Men 1. 25 x more likely to suffer strokes than women n However, 60% of deaths from stroke occur in women n Since women live longer than men, they are older on average when they have their strokes & therefore more often killed n Some risk factors for stroke apply only to women: – Pregnancy – Childbirth – Menopause – HRT
Stroke Risk Factors n Advanced age n Previous stroke or TIA n Diabetes n High cholesterol n Cigarette smoking n Atrial fibrillation n HRT n Migraines n Thrombophilia n Patent foramen ovale n HTN – Mst important & modifiable
CVA History n AMS n Altered speech, sensory, or motor function without suspected trauma – Trauma can cause an intracerebral bleed, but is treated differently than a CVA n Possible history of prior stroke or TIA
Stroke Symptoms n Fairly rapid development n Symptoms related to anatomical location of damage n Ischemic: – Affect regional areas of brain perfused by blocked artery n Hemorrhagic: – Affect local or global symptoms due to bleeding & increased ICP n By history & neurological examination, as well as the presence of risk factors, the anatomical nature of the stroke can often be identified
Stroke Mimics n Seizure n Infection – Meningitis – Sepsis – Endocarditis n Hypoglycemia n Syncope n Brain abscess or tumor n Drug overdose n Head trauma n Migraine n Vascular lesions n Hypertensive encephalopathy – Arteriovenous malformation
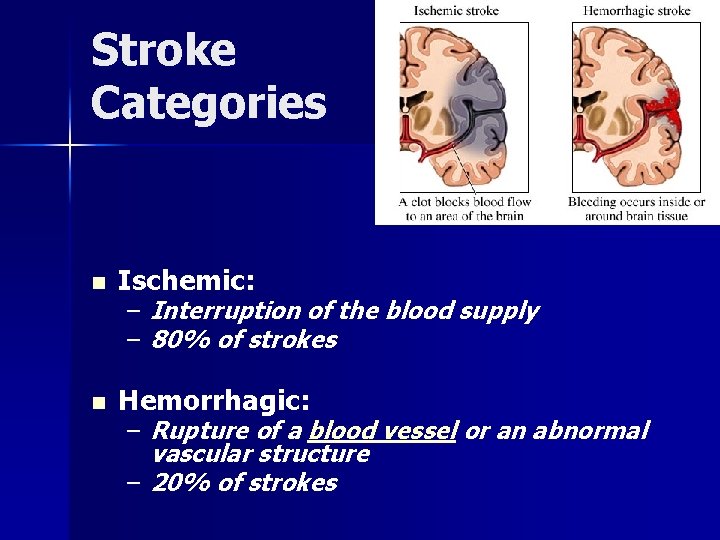
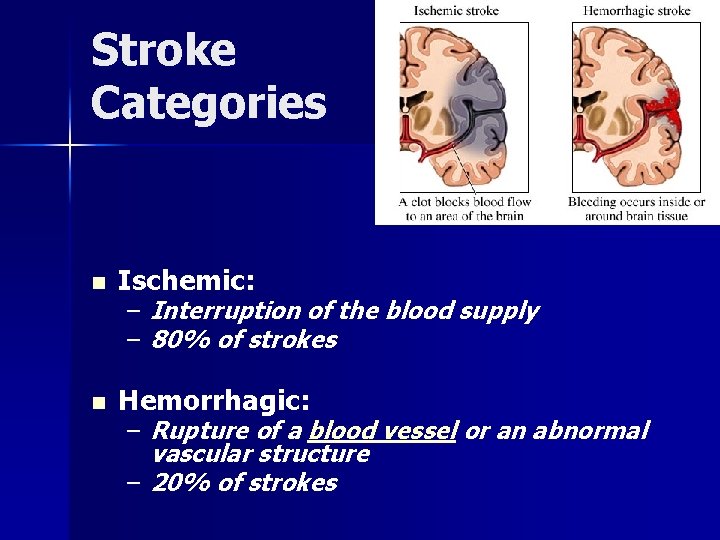
Stroke Categories n Ischemic: n Hemorrhagic: – Interruption of the blood supply – 80% of strokes – Rupture of a blood vessel or an abnormal vascular structure – 20% of strokes
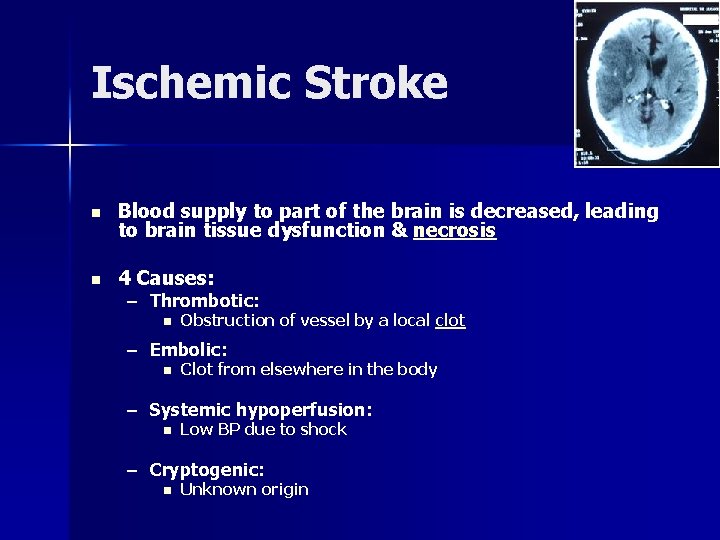
Ischemic Stroke n Blood supply to part of the brain is decreased, leading to brain tissue dysfunction & necrosis n 4 Causes: – Thrombotic: n Obstruction of vessel by a local clot – Embolic: n Clot from elsewhere in the body – Systemic hypoperfusion: n Low BP due to shock – Cryptogenic: n Unknown origin
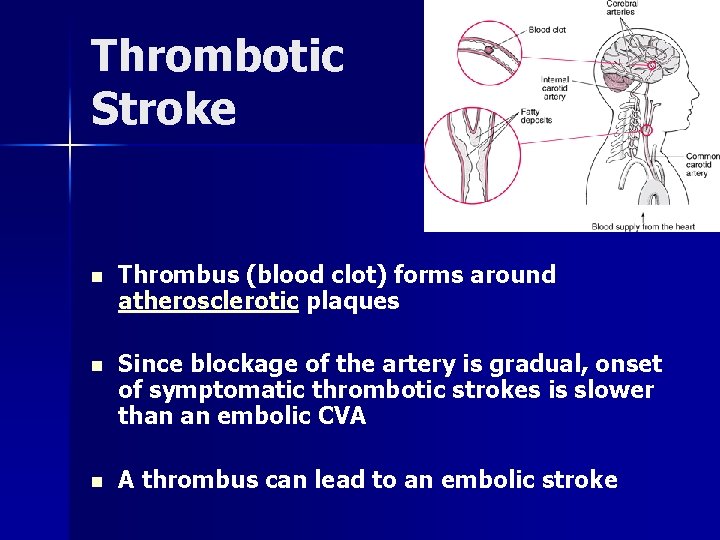
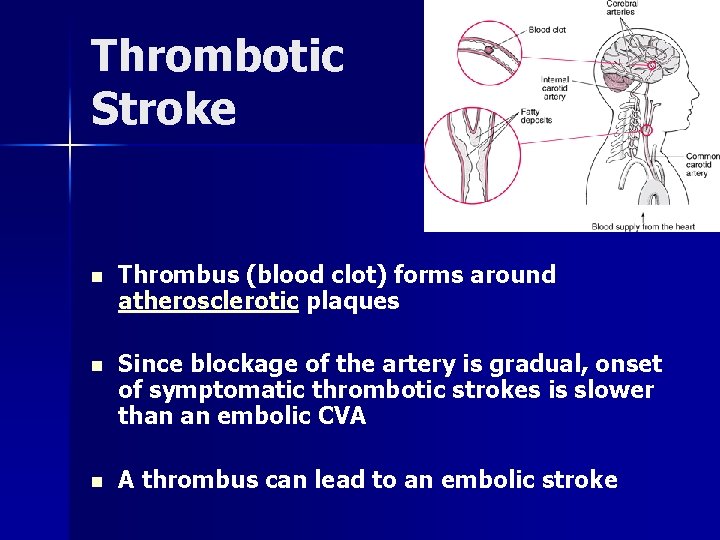
Thrombotic Stroke n Thrombus (blood clot) forms around atherosclerotic plaques n Since blockage of the artery is gradual, onset of symptomatic thrombotic strokes is slower than an embolic CVA n A thrombus can lead to an embolic stroke
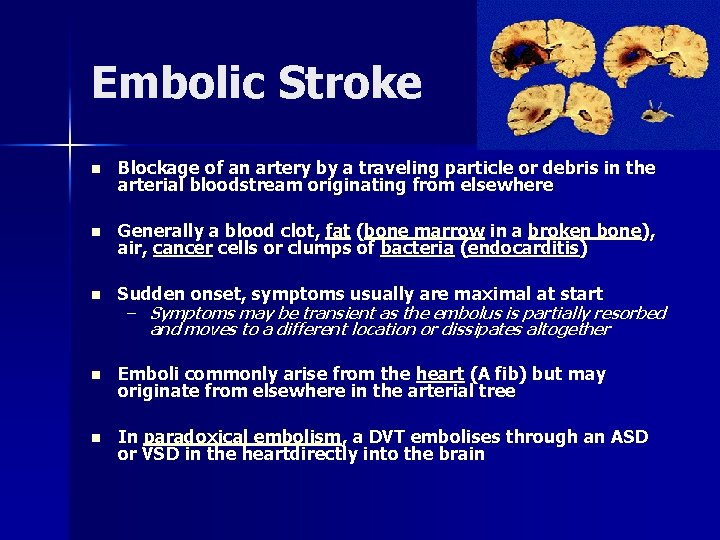
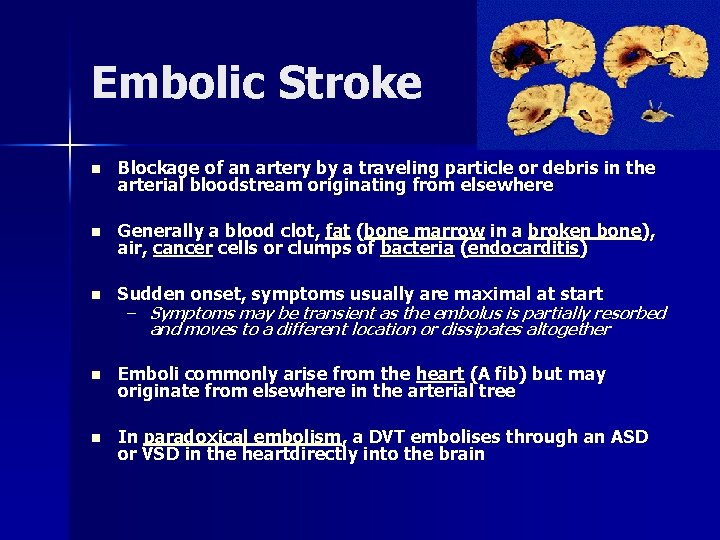
Embolic Stroke n Blockage of an artery by a traveling particle or debris in the arterial bloodstream originating from elsewhere n Generally a blood clot, fat (bone marrow in a broken bone), air, cancer cells or clumps of bacteria (endocarditis) n Sudden onset, symptoms usually are maximal at start n Emboli commonly arise from the heart (A fib) but may originate from elsewhere in the arterial tree n In paradoxical embolism, a DVT embolises through an ASD or VSD in the heartdirectly into the brain – Symptoms may be transient as the embolus is partially resorbed and moves to a different location or dissipates altogether
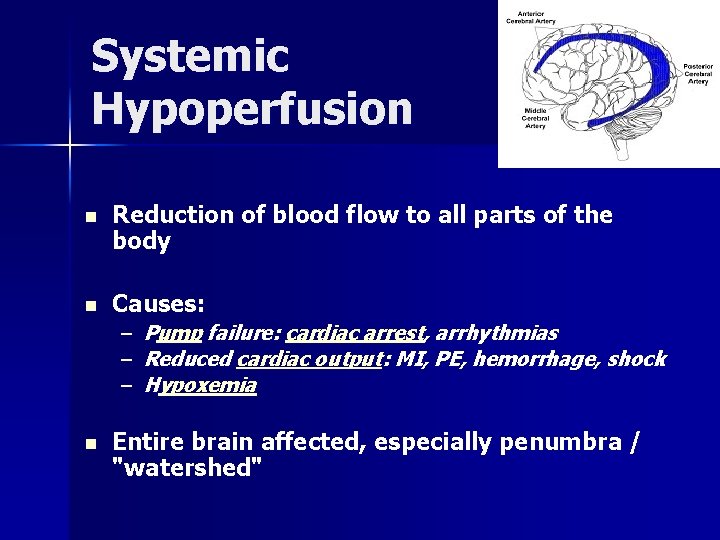
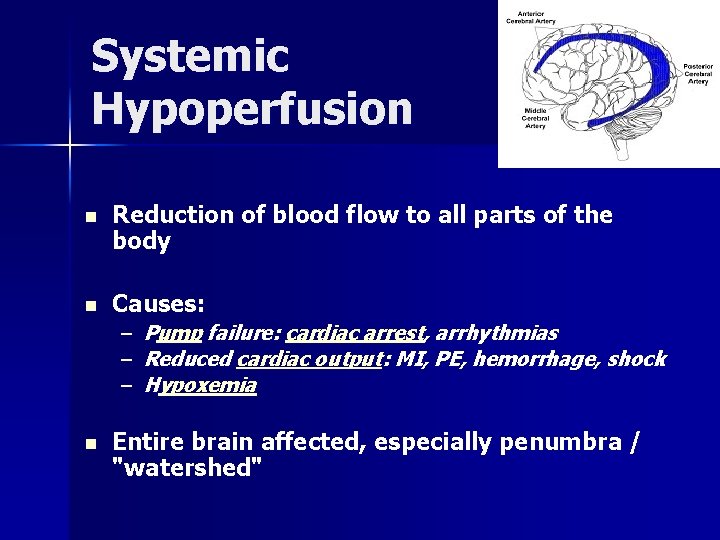
Systemic Hypoperfusion n Reduction of blood flow to all parts of the body n Causes: – – – n Pump failure: cardiac arrest, arrhythmias Reduced cardiac output: MI, PE, hemorrhage, shock Hypoxemia Entire brain affected, especially penumbra / "watershed"
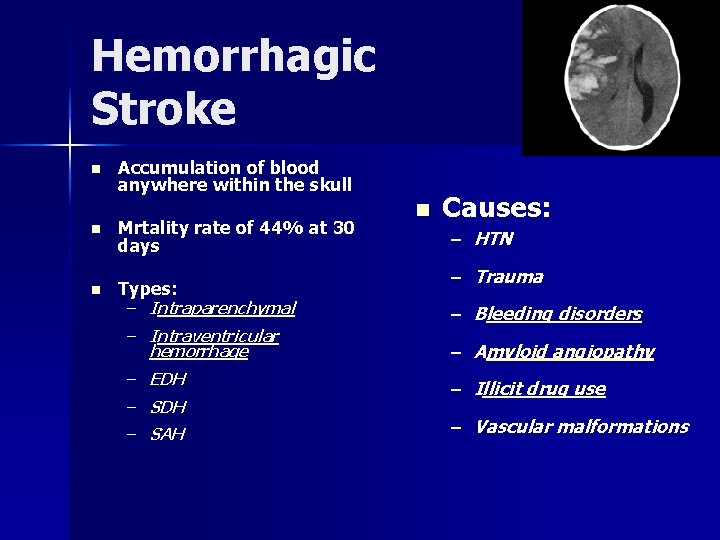
Hemorrhagic Stroke n Accumulation of blood anywhere within the skull n Mrtality rate of 44% at 30 days n Types: n Causes: – HTN – Trauma – Intraparenchymal – Bleeding disorders – Intraventricular hemorrhage – Amyloid angiopathy – EDH – SAH – Illicit drug use – Vascular malformations
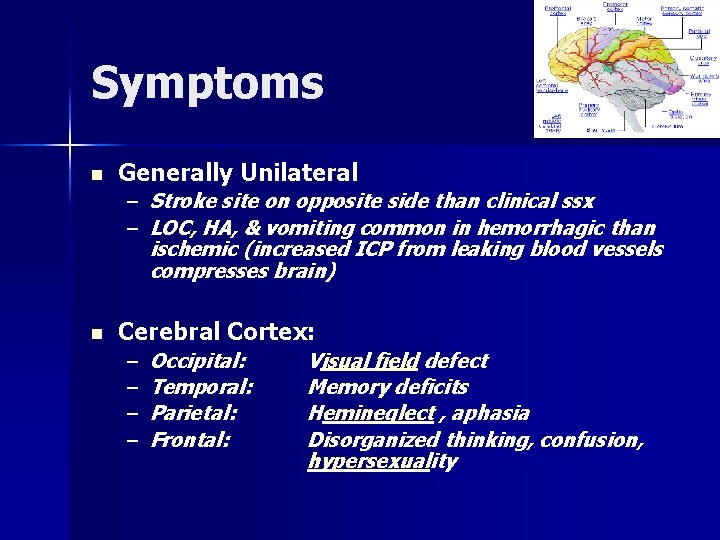
Symptoms n Generally Unilateral – Stroke site on opposite side than clinical ssx – LOC, HA, & vomiting common in hemorrhagic than ischemic (increased ICP from leaking blood vessels compresses brain) n Cerebral Cortex: – – Occipital: Temporal: Parietal: Frontal: Visual field defect Memory deficits Hemineglect , aphasia Disorganized thinking, confusion, hypersexuality
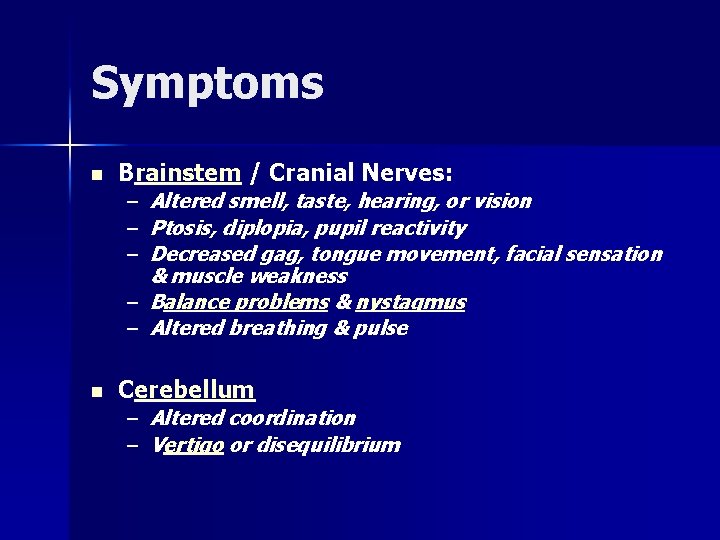
Symptoms n Brainstem / Cranial Nerves: – Altered smell, taste, hearing, or vision – Ptosis, diplopia, pupil reactivity – Decreased gag, tongue movement, facial sensation & muscle weakness – Balance problems & nystagmus – Altered breathing & pulse n Cerebellum – Altered coordination – Vertigo or disequilibrium
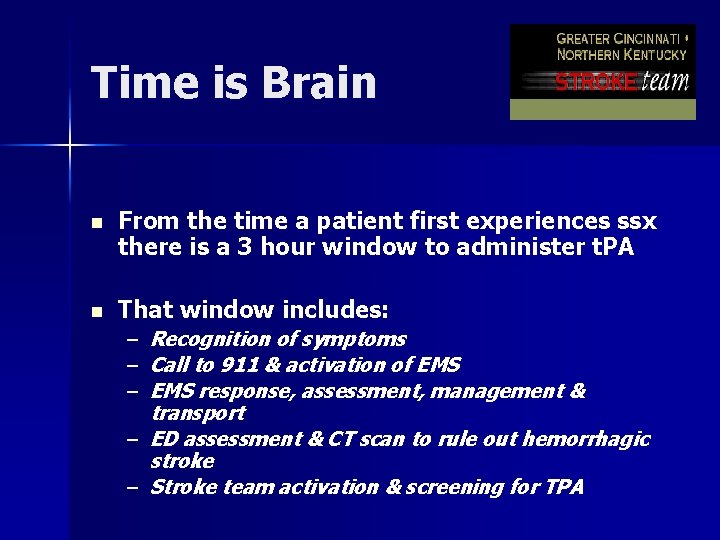
Time is Brain n From the time a patient first experiences ssx there is a 3 hour window to administer t. PA n That window includes: Recognition of symptoms Call to 911 & activation of EMS response, assessment, management & transport – ED assessment & CT scan to rule out hemorrhagic stroke – Stroke team activation & screening for TPA – – –


MEND Examination Miami Emergency Neurological Deficit Exam n Based on the NIH Stroke Scale, incorporates the Cincinnati Prehospital Stroke Scale (CPSS), takes < 3 mins to perform n ABCD n En route, perform full MEND Exam – D = CPSS
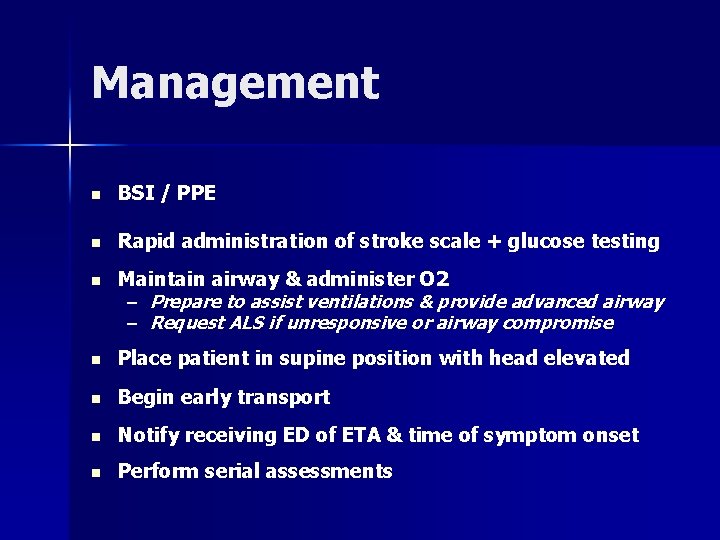
Management n BSI / PPE n Rapid administration of stroke scale + glucose testing n Maintain airway & administer O 2 – Prepare to assist ventilations & provide advanced airway – Request ALS if unresponsive or airway compromise n Place patient in supine position with head elevated n Begin early transport n Notify receiving ED of ETA & time of symptom onset n Perform serial assessments
Prehospital Treatment n Transport to a hospital with a stroke management team n Aggressive airway management n Treatment should be aimed at maintaining O 2 saturation > 95% & CO 2 between 28 – 35 mm. Hg – Patients with a GCS <8 , loss of gag, or failure to maintain adequate oxygenation or ventilation – If O 2 sat falls below 95%, there is a 150% increase in mortality n Prophylactic hyperventilation of the head-injured patient is no longer recommended n Elevate the head of the bed 30 - 35 degrees to reduce ICP n Thrombolysis ("clot-busters") both in the field & in the ED
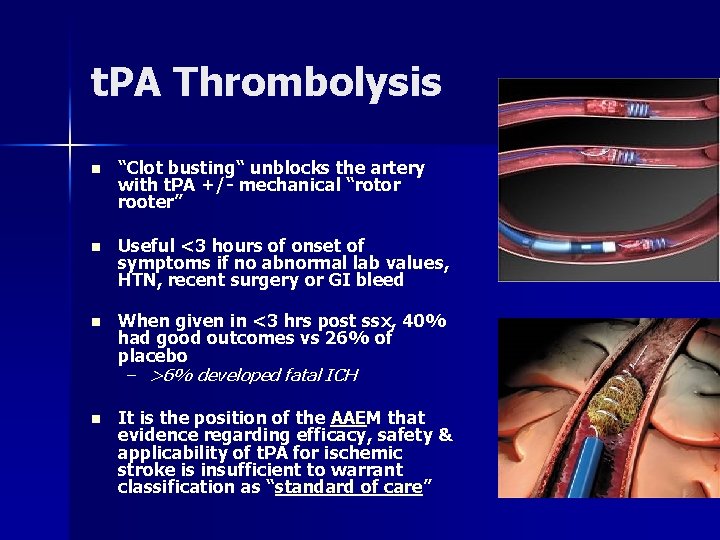
t. PA Thrombolysis n “Clot busting“ unblocks the artery with t. PA +/- mechanical “rotor rooter” n Useful <3 hours of onset of symptoms if no abnormal lab values, HTN, recent surgery or GI bleed n When given in <3 hrs post ssx, 40% had good outcomes vs 26% of placebo – >6% developed fatal ICH n It is the position of the AAEM that evidence regarding efficacy, safety & applicability of t. PA for ischemic stroke is insufficient to warrant classification as “standard of care”
Hypertension Management n Prehospital management of hypertension is now considered dangerous for “cerebral resuscitation” n There is no evidence that emergent HTN improves neurological outcome – Numerous studies report neurological deterioration in strokes immediately following BP reduction n In the first 48 hrs post stroke, if the SBP drops <100 or O 2 sat falls <95%, there is a 150% increase in mortality n Rapid & dramatically lowered BP reduces blood flow to ischemic tissue & vulnerable but viable penumbra
Prevention n Primary prevention less effective than secondary n Determine patient's risk for other cardiovascular diseases n The most important modifiable risk factor are HTN n Medication is the most common method of prevention n Carotid endarterectomy is a surgical prevention method – Comprehensive medical management includes diet, exercise, & cessation of smoking & alcohol use – – – Statins Aspirin Antihypertensives
Key Prehospital Points n Early symptom recognition n Early hospital notification n Maintain hemodynamic stability
Summary n Cardiovascular diseases are among the top killers worldwide n Early recognition, treatment & transport are keys to good outcome
Questions? Amy. Gutman@uc. edu
 Dcharte example
Dcharte example Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies Skala gutman
Skala gutman Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies Psychiatric emergencies
Psychiatric emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Chapter 13 handling emergencies
Chapter 13 handling emergencies During a psychiatric emergency the emt should be able to
During a psychiatric emergency the emt should be able to Qut security contact number for emergencies
Qut security contact number for emergencies Chapter 28 first aid and emergencies
Chapter 28 first aid and emergencies Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies Besides being required for diver training
Besides being required for diver training Immunologic emergencies
Immunologic emergencies Dic labs
Dic labs Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Environmental emergencies emt
Environmental emergencies emt Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies A 41 year old man presents with slow irregular breathing
A 41 year old man presents with slow irregular breathing Gems diamond geriatric assessment
Gems diamond geriatric assessment Edu.sharif.edu
Edu.sharif.edu Anatomy blood vessels
Anatomy blood vessels Pequena e grande circulação
Pequena e grande circulação Battiti ectopici ventricolari forum
Battiti ectopici ventricolari forum Chapter 26 the child with a cardiovascular disorder
Chapter 26 the child with a cardiovascular disorder Maniobra de azoulay
Maniobra de azoulay Pithed model
Pithed model Blood vessels
Blood vessels Chapter 8 cardiovascular system
Chapter 8 cardiovascular system What are the components of fitness?
What are the components of fitness? How does intrathoracic pressure affect venous return
How does intrathoracic pressure affect venous return Cardiovascular drugs
Cardiovascular drugs Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Coronary circulation of heart
Coronary circulation of heart True capillaries
True capillaries Salud cardiovascular
Salud cardiovascular Veias
Veias Isotonic exercise physiology
Isotonic exercise physiology Caracteristicas de las venas
Caracteristicas de las venas Wheezing
Wheezing Wolters kluwer
Wolters kluwer Fresenius national cardiovascular partners
Fresenius national cardiovascular partners What makes up the circulatory system
What makes up the circulatory system Onda p
Onda p Chapter 7 cardiovascular fitness
Chapter 7 cardiovascular fitness Sistolw
Sistolw Cardiovascular system
Cardiovascular system Aparato cardiovascular
Aparato cardiovascular Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Receptores sensoriales
Receptores sensoriales Medical terminology chapter 5 learning exercises answers
Medical terminology chapter 5 learning exercises answers Cmqcc cardiovascular toolkit
Cmqcc cardiovascular toolkit Capillary bed
Capillary bed Sistema cardiovascular
Sistema cardiovascular Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Quiz sistema cardiovascular
Quiz sistema cardiovascular Cardiovascular research institute basel
Cardiovascular research institute basel Prairie cardiovascular consultants springfield il
Prairie cardiovascular consultants springfield il Figure 11-8 arteries
Figure 11-8 arteries Cardiovascular/lymphatic system it's totally tubular
Cardiovascular/lymphatic system it's totally tubular Rias hipertension arterial
Rias hipertension arterial Bhf glasgow cardiovascular research centre
Bhf glasgow cardiovascular research centre Salud cardiovascular
Salud cardiovascular Chapter 11 the cardiovascular system figure 11-2
Chapter 11 the cardiovascular system figure 11-2 Tissue in cardiovascular system
Tissue in cardiovascular system Pequena circulacao
Pequena circulacao American board of cardiovascular medicine
American board of cardiovascular medicine