Chapter 20 The Heart Location and Size of
- Slides: 59
Chapter 20 - The Heart
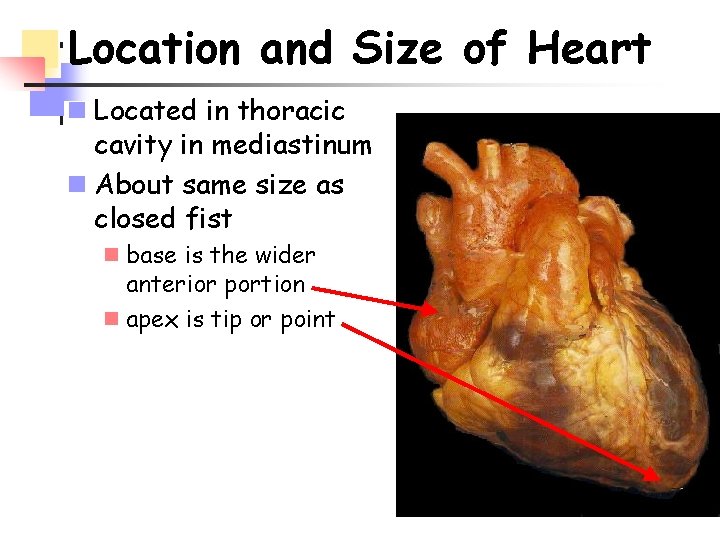
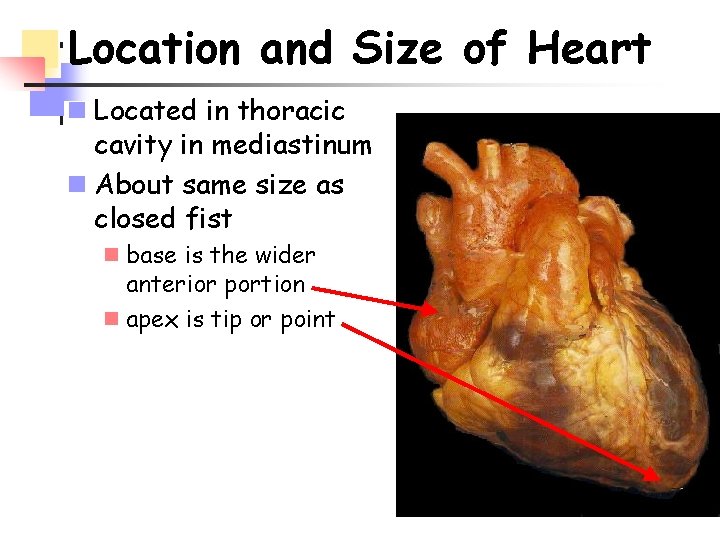
Location and Size of Heart n Located in thoracic cavity in mediastinum n About same size as closed fist n base is the wider anterior portion n apex is tip or point
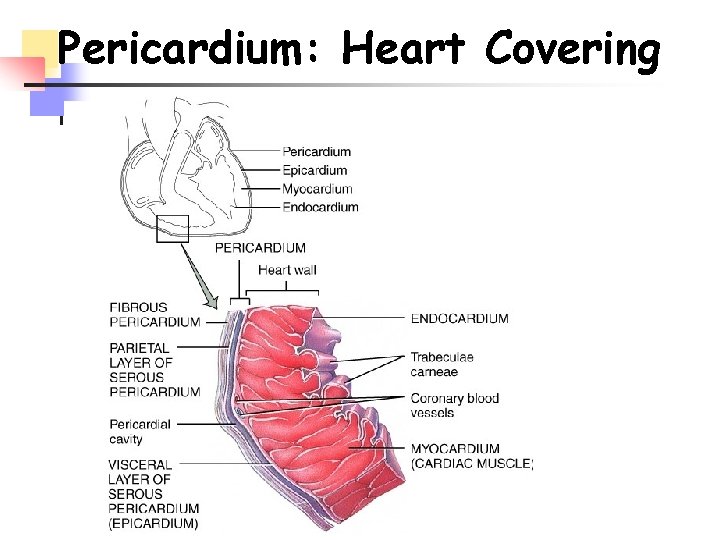
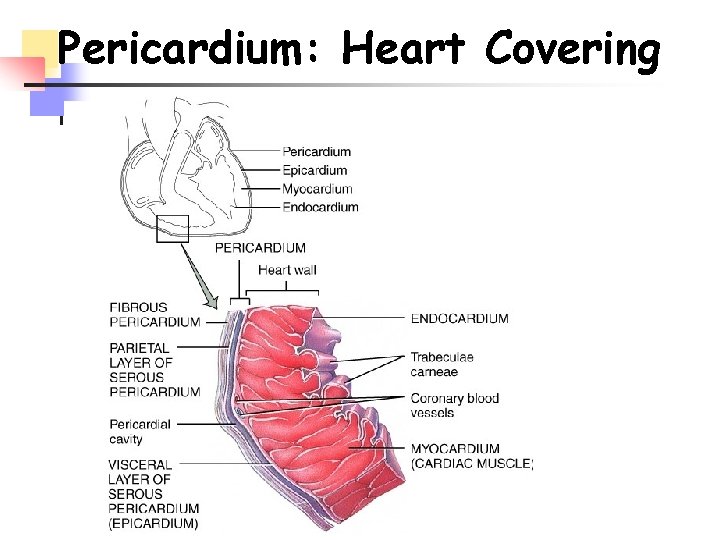
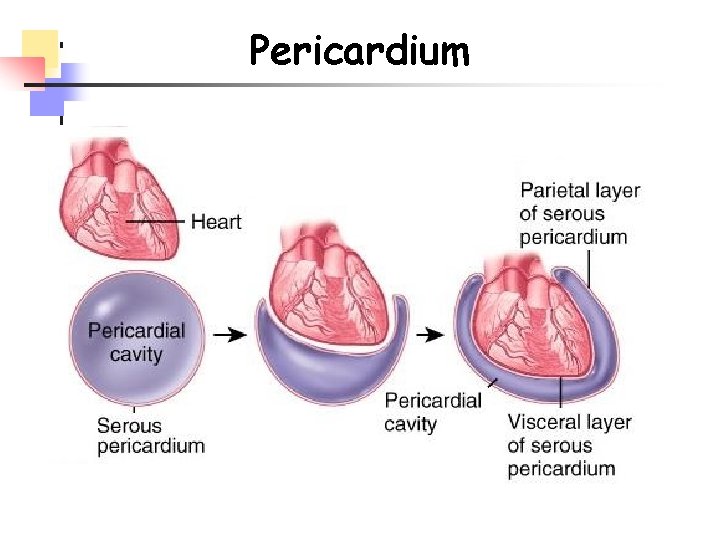
Pericardium: Heart Covering
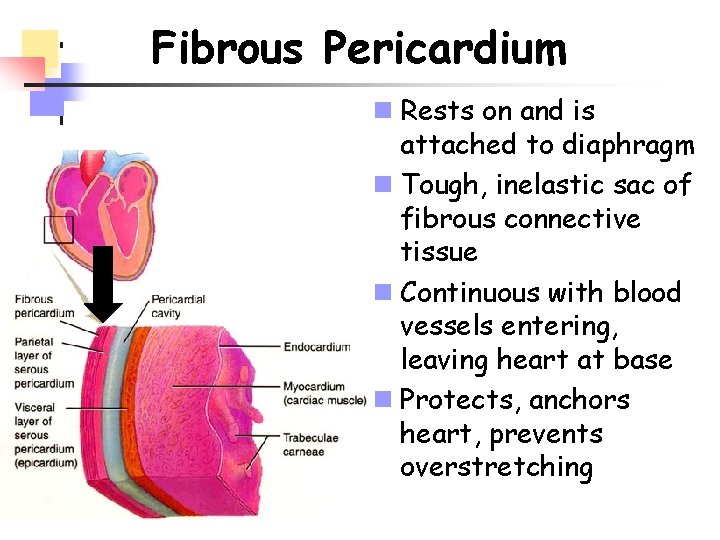
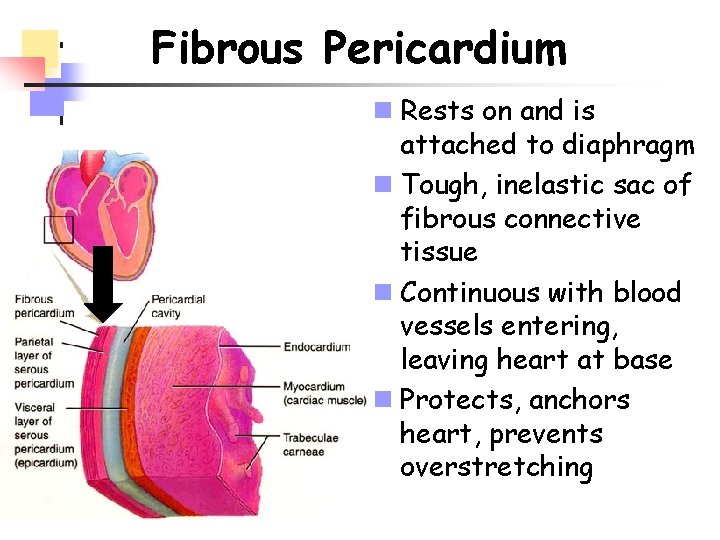
Fibrous Pericardium n Rests on and is attached to diaphragm n Tough, inelastic sac of fibrous connective tissue n Continuous with blood vessels entering, leaving heart at base n Protects, anchors heart, prevents overstretching
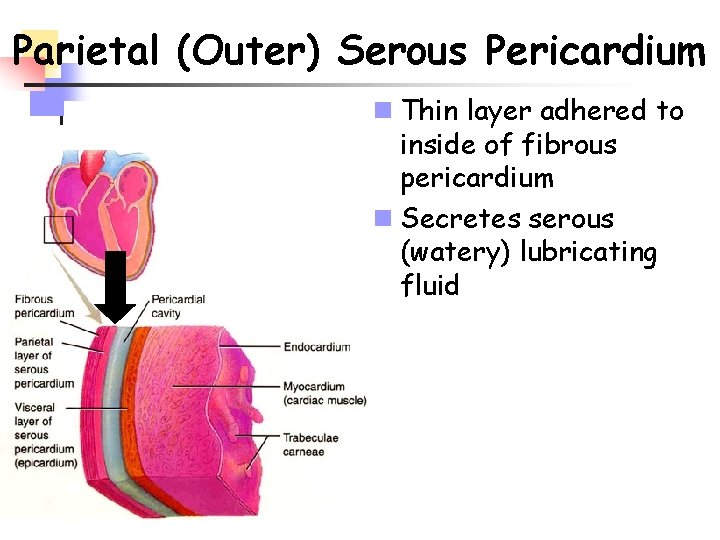
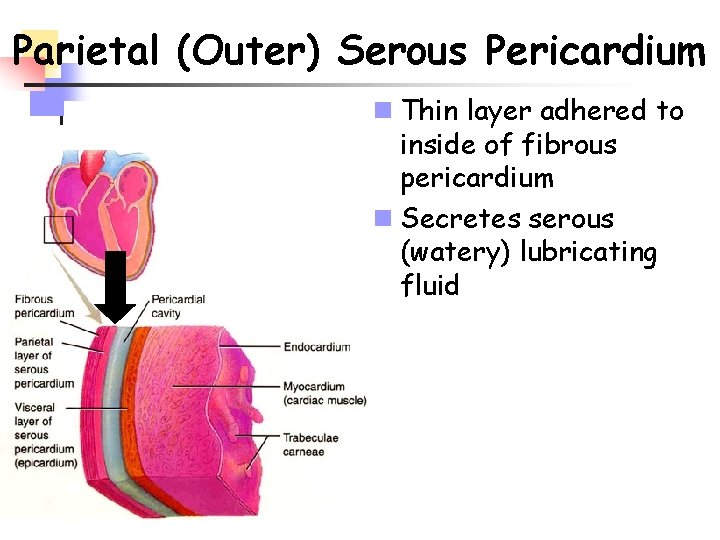
Parietal (Outer) Serous Pericardium n Thin layer adhered to inside of fibrous pericardium n Secretes serous (watery) lubricating fluid
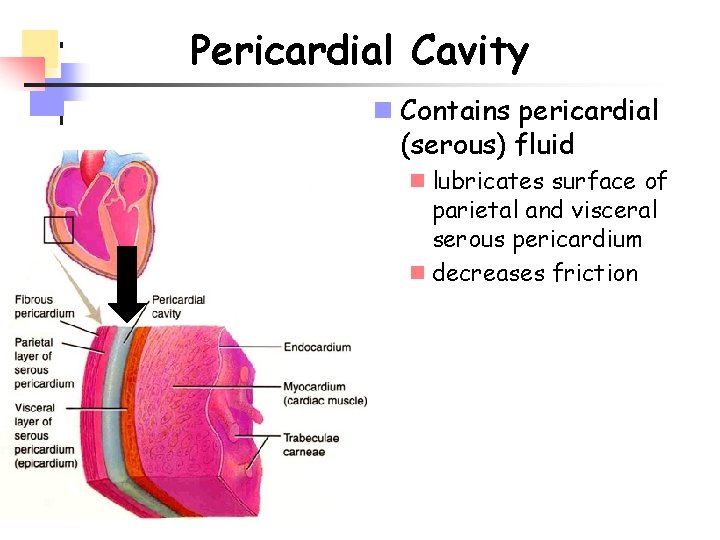
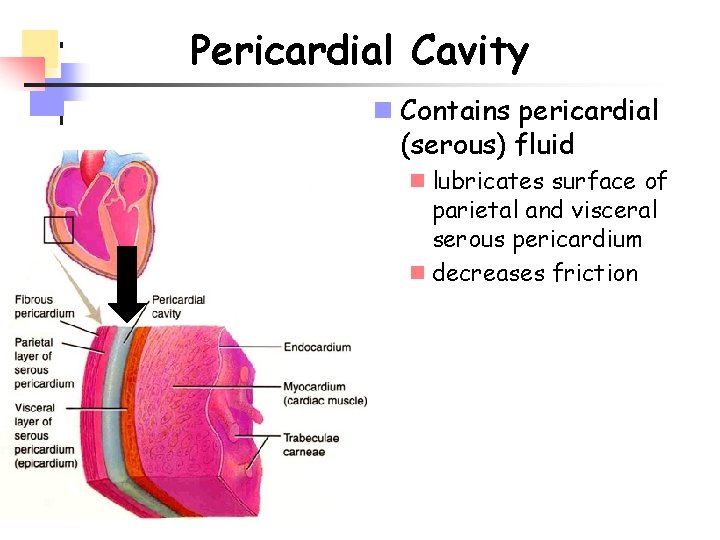
Pericardial Cavity n Contains pericardial (serous) fluid n lubricates surface of parietal and visceral serous pericardium n decreases friction
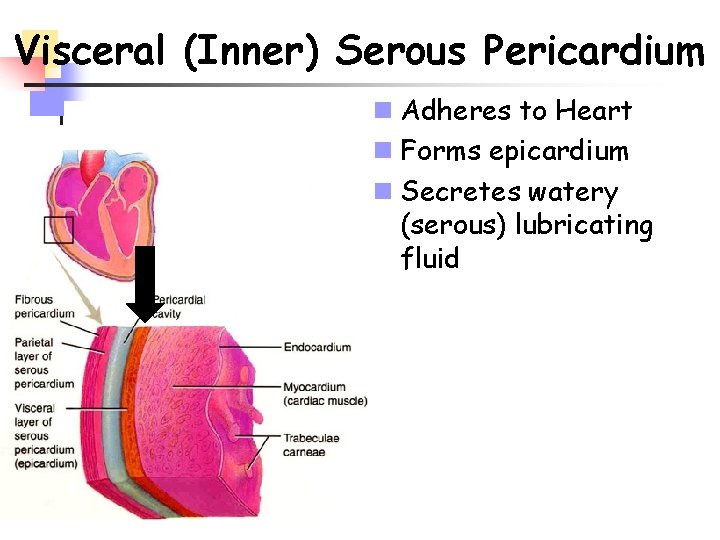
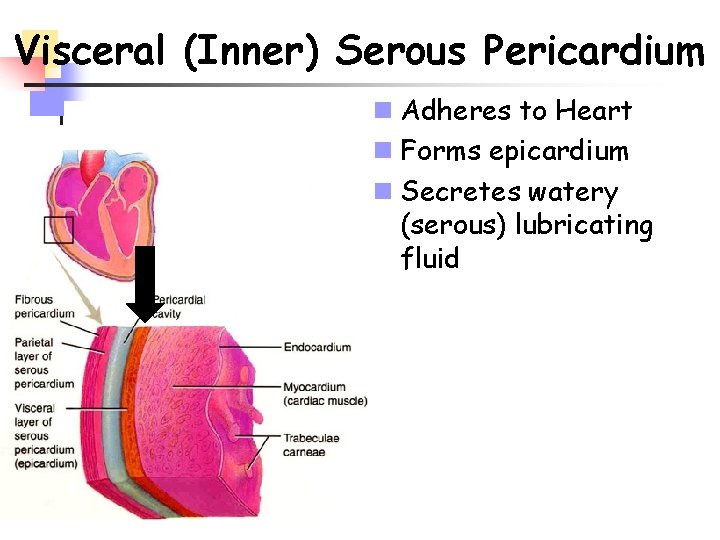
Visceral (Inner) Serous Pericardium n Adheres to Heart n Forms epicardium n Secretes watery (serous) lubricating fluid
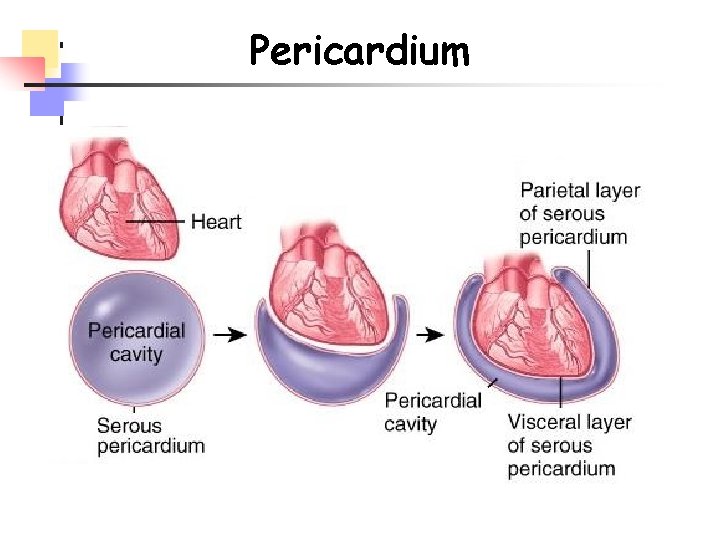
Pericardium
Homeostatic Imbalances n. Pericarditis ninflammation of pericardium npainful, rubbing of tissues ncan damage myocardium n. Cardiac tamponade na buildup of pericardial fluid nbleeding into pericardial cavity nmay result in cardiac failure
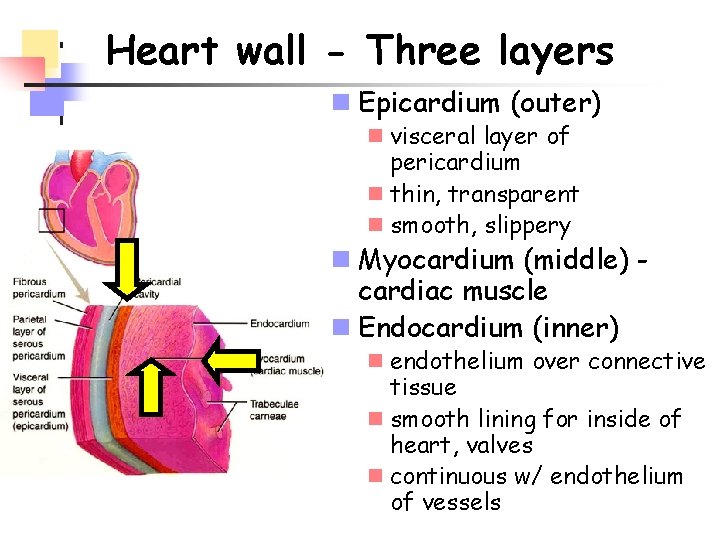
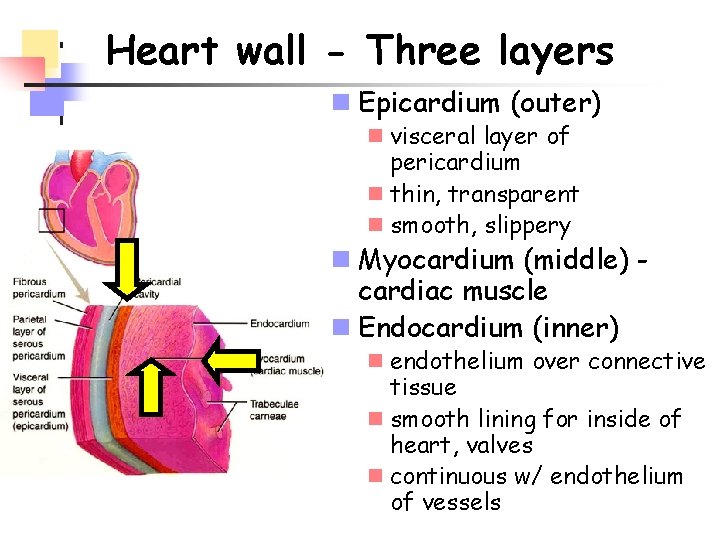
Heart wall - Three layers n Epicardium (outer) n visceral layer of pericardium n thin, transparent n smooth, slippery n Myocardium (middle) cardiac muscle n Endocardium (inner) n endothelium over connective tissue n smooth lining for inside of heart, valves n continuous w/ endothelium of vessels
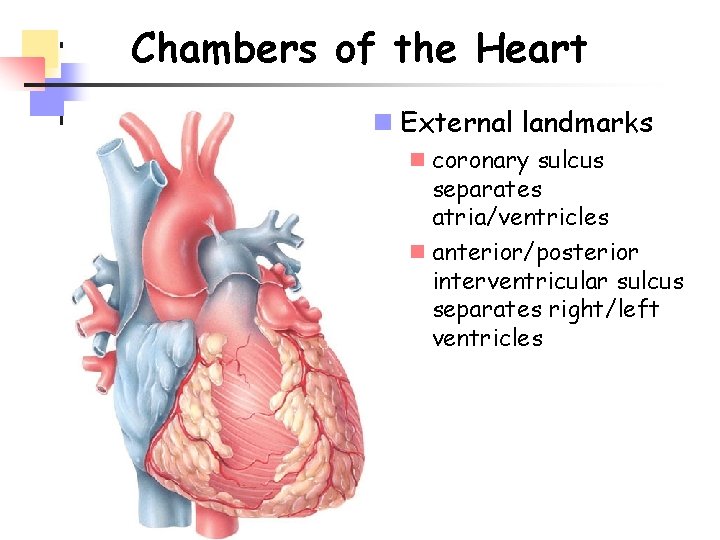
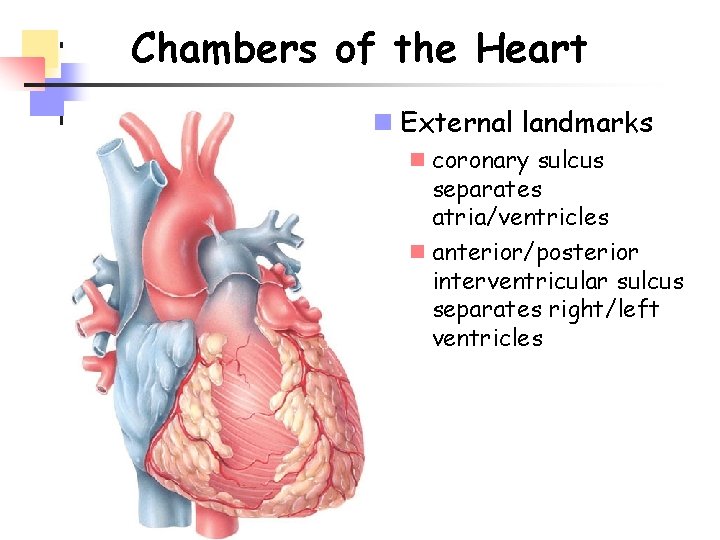
Chambers of the Heart n External landmarks n coronary sulcus separates atria/ventricles n anterior/posterior interventricular sulcus separates right/left ventricles
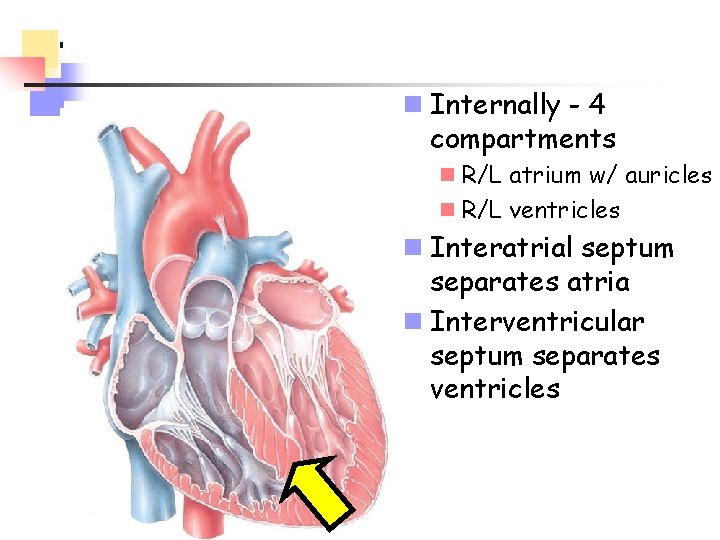
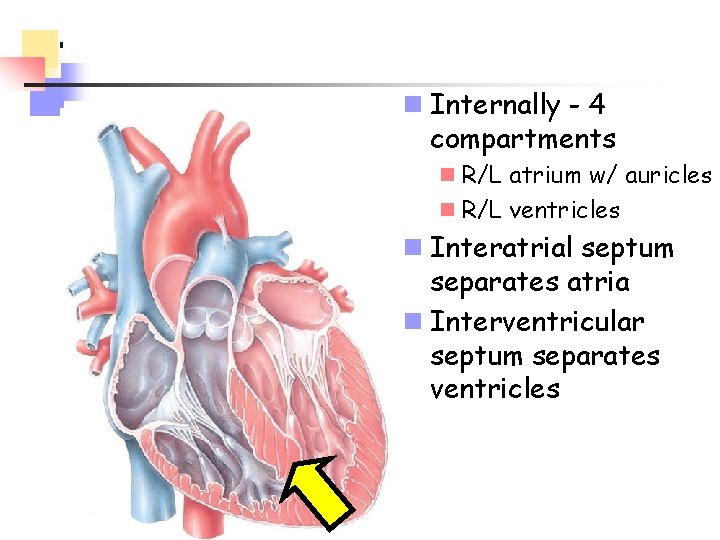
n Internally - 4 compartments n R/L atrium w/ auricles n R/L ventricles n Interatrial septum separates atria n Interventricular septum separates ventricles
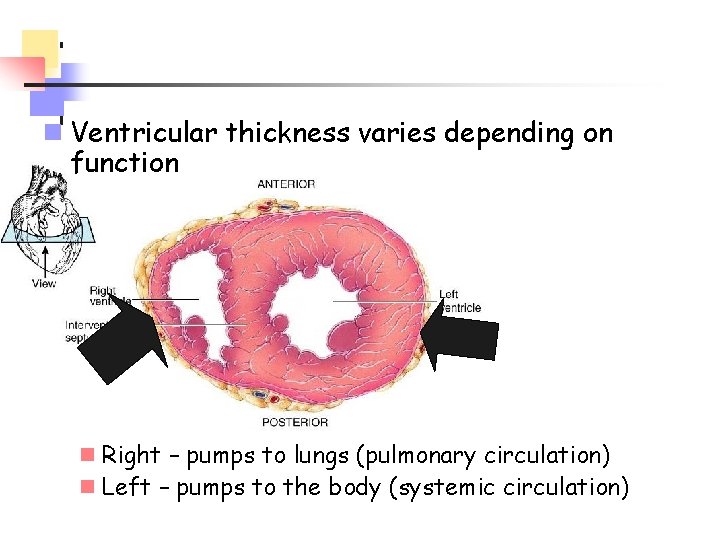
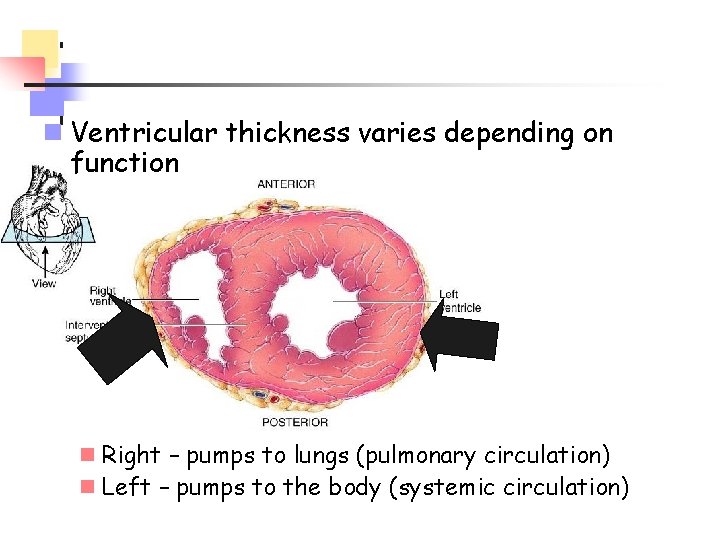
n Ventricular thickness varies depending on function n Right – pumps to lungs (pulmonary circulation) n Left – pumps to the body (systemic circulation)
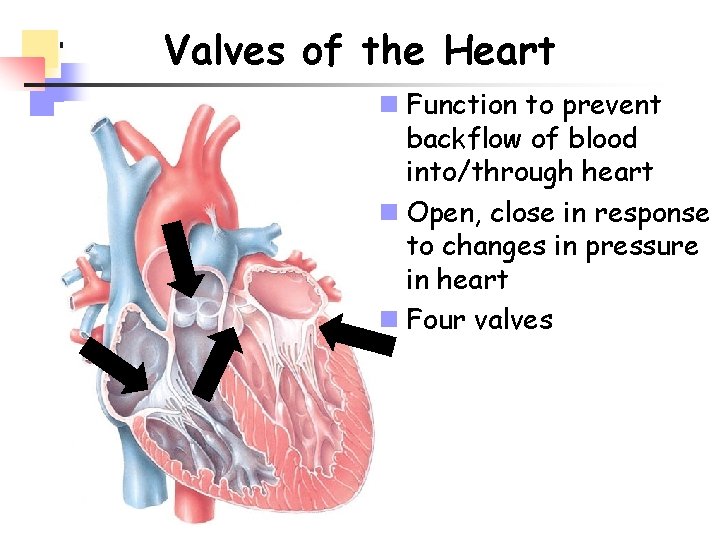
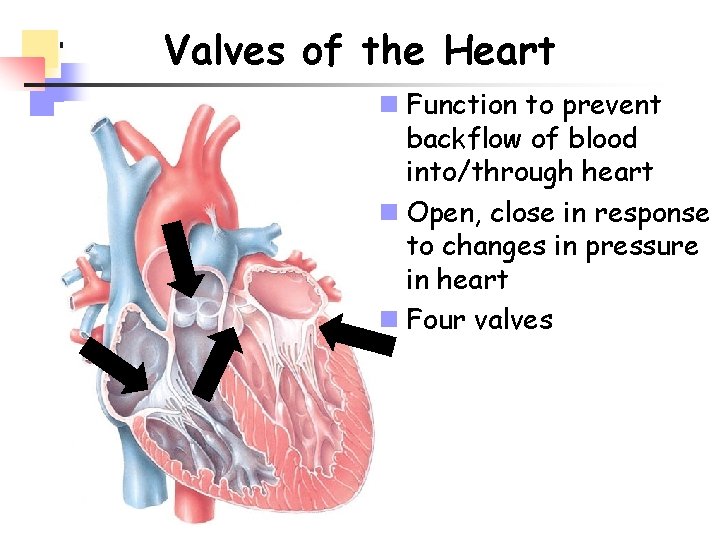
Valves of the Heart n Function to prevent backflow of blood into/through heart n Open, close in response to changes in pressure in heart n Four valves
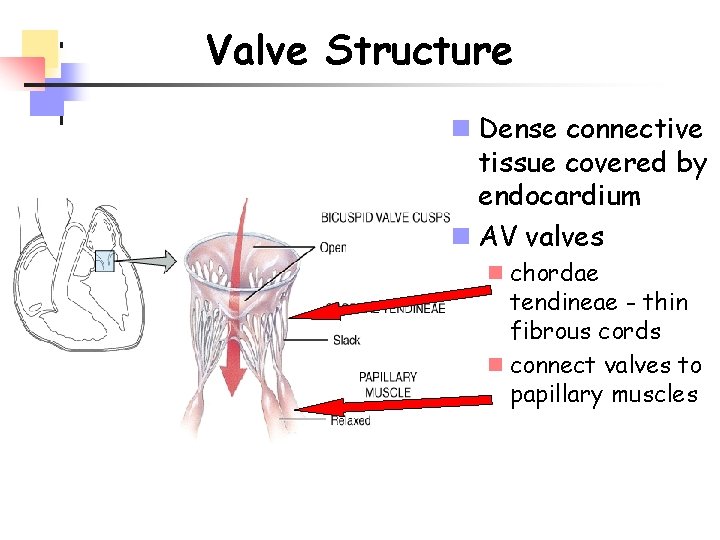
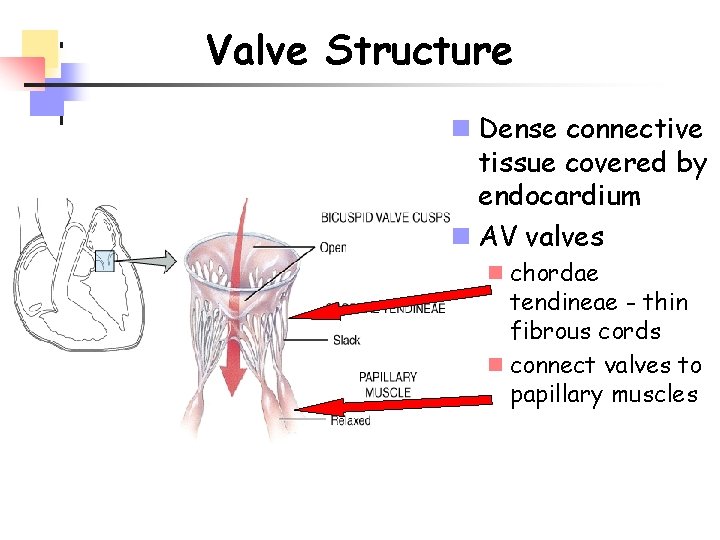
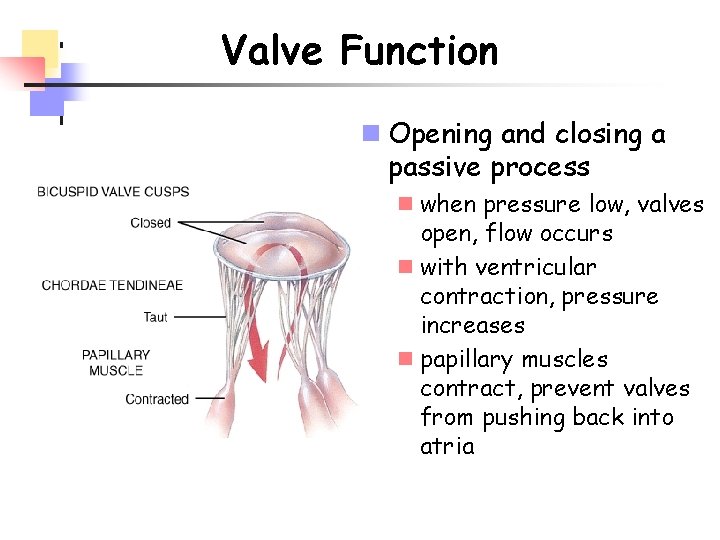
Valve Structure n Dense connective tissue covered by endocardium n AV valves n chordae tendineae - thin fibrous cords n connect valves to papillary muscles
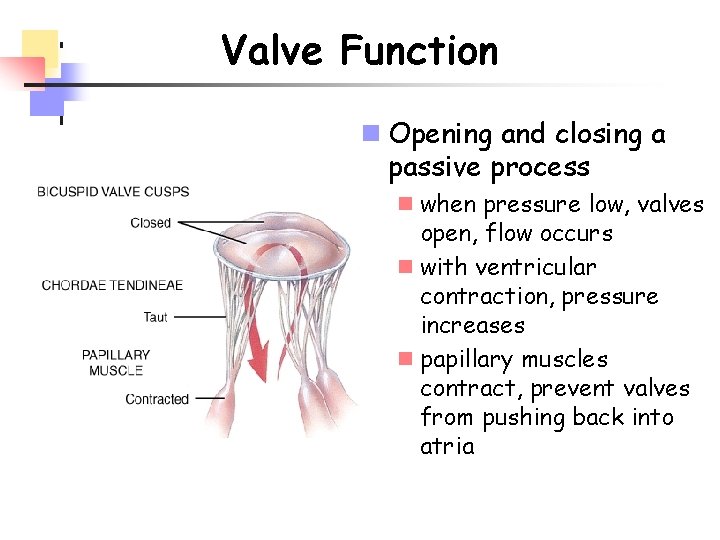
Valve Function n Opening and closing a passive process n when pressure low, valves open, flow occurs n with ventricular contraction, pressure increases n papillary muscles contract, prevent valves from pushing back into atria
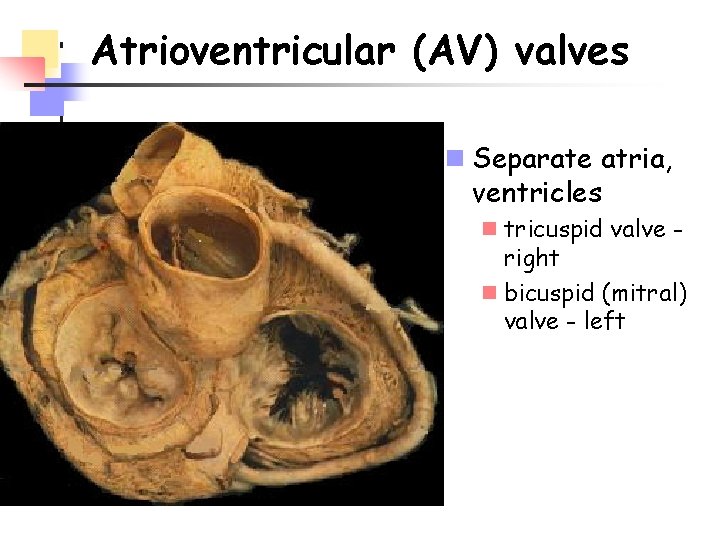
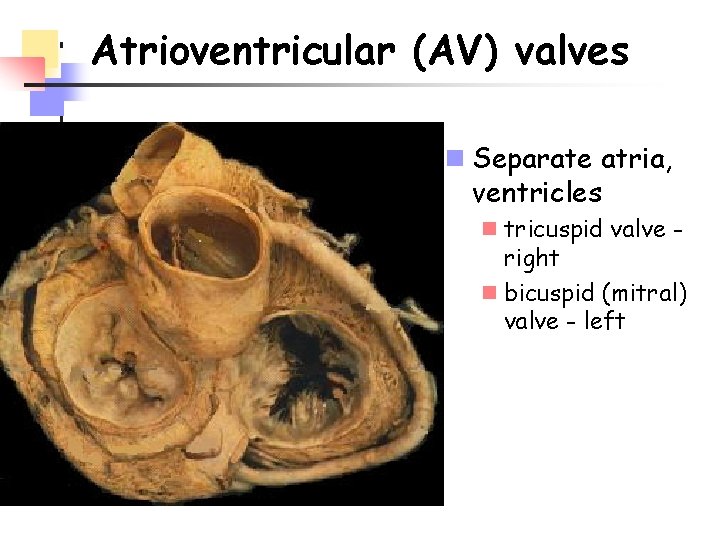
Atrioventricular (AV) valves n Separate atria, ventricles n tricuspid valve right n bicuspid (mitral) valve - left
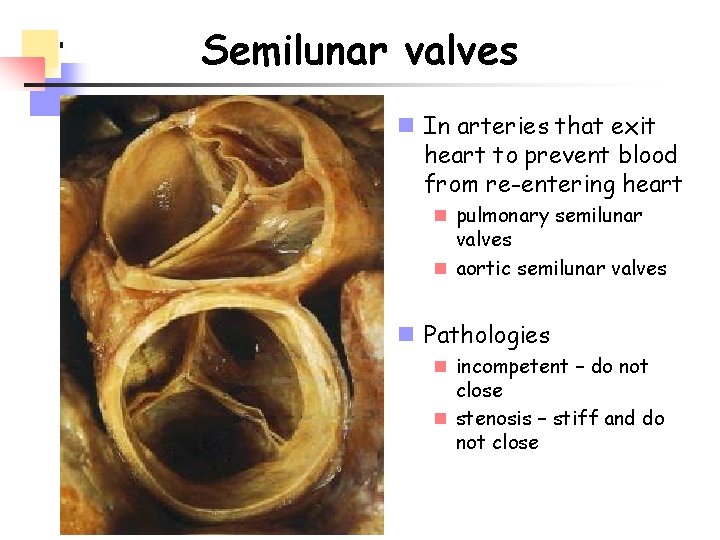
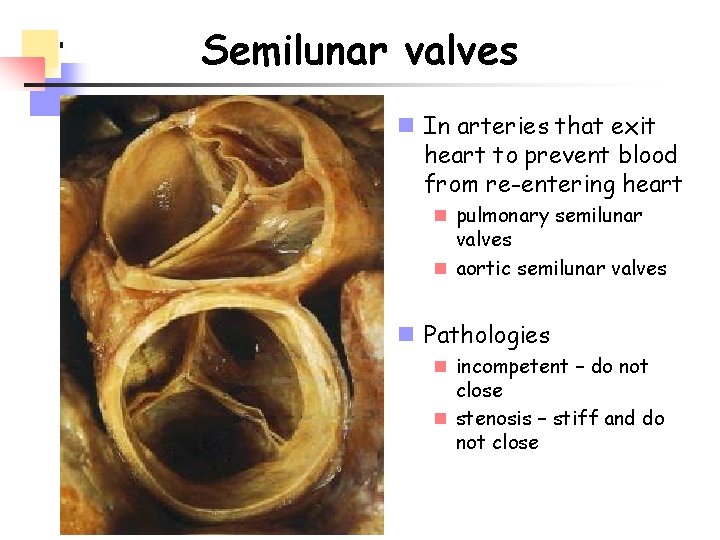
Semilunar valves n In arteries that exit heart to prevent blood from re-entering heart n pulmonary semilunar valves n aortic semilunar valves n Pathologies n incompetent – do not close n stenosis – stiff and do not close
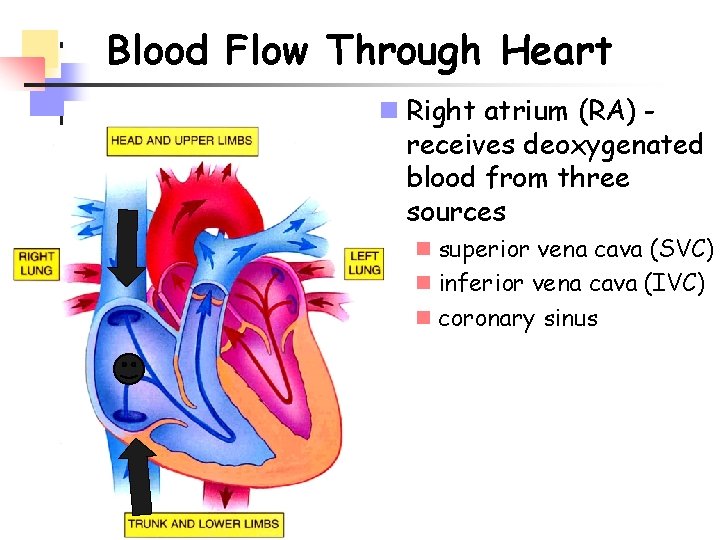
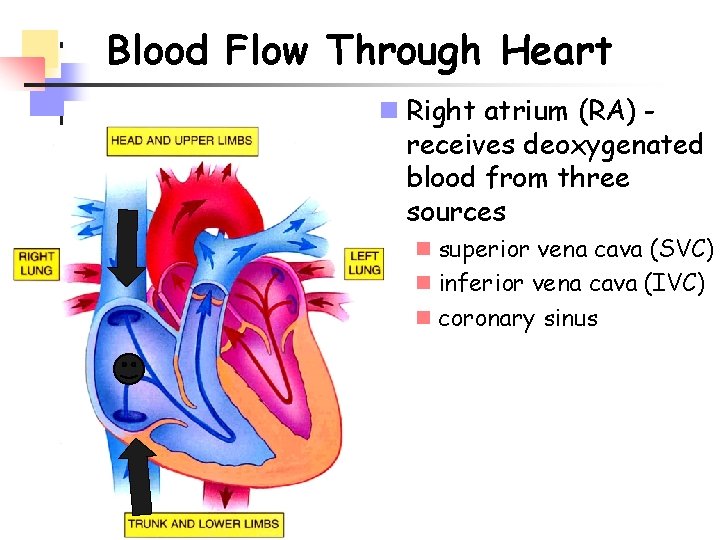
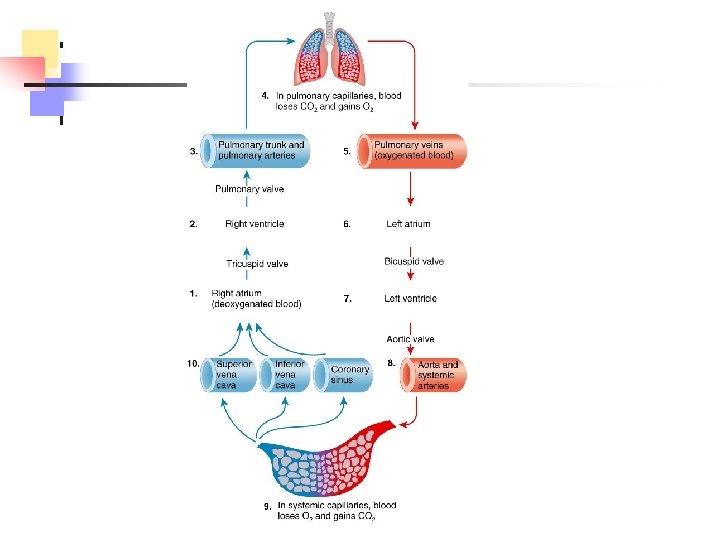
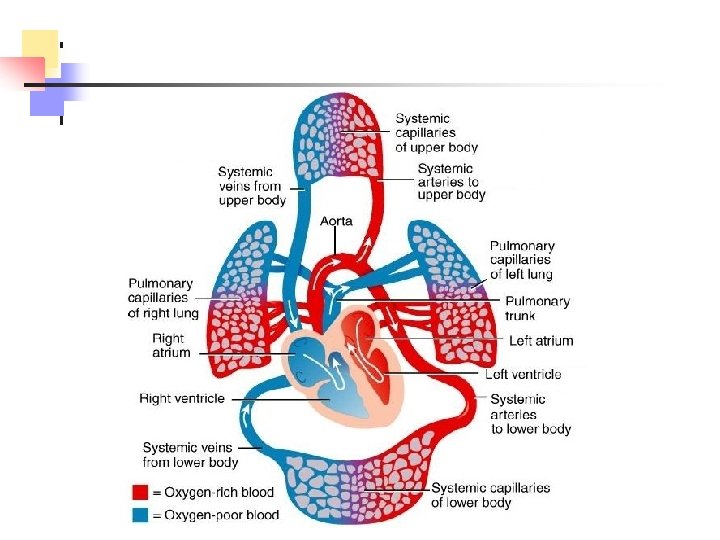
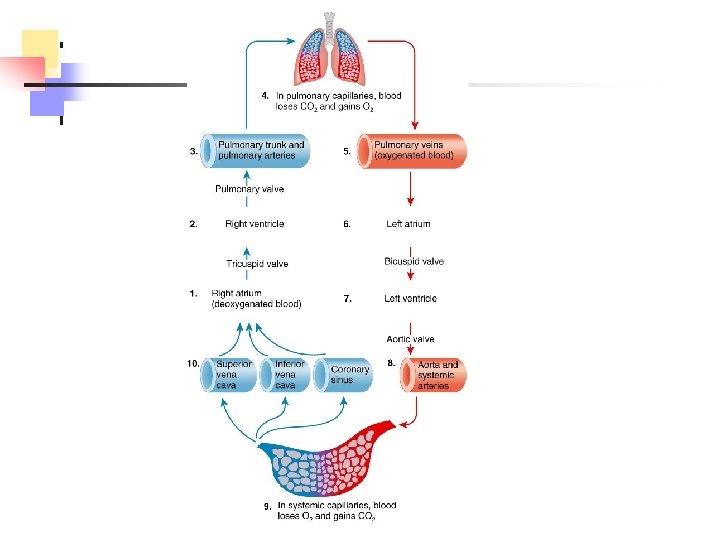
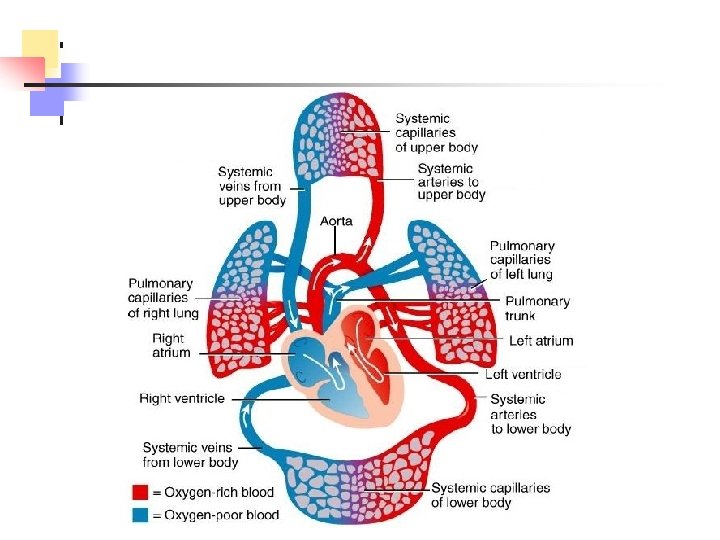
Blood Flow Through Heart n Right atrium (RA) receives deoxygenated blood from three sources n superior vena cava (SVC) n inferior vena cava (IVC) n coronary sinus
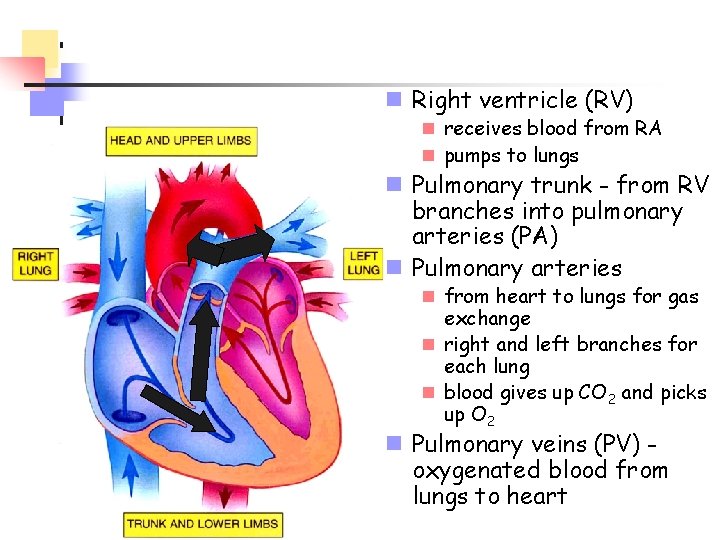
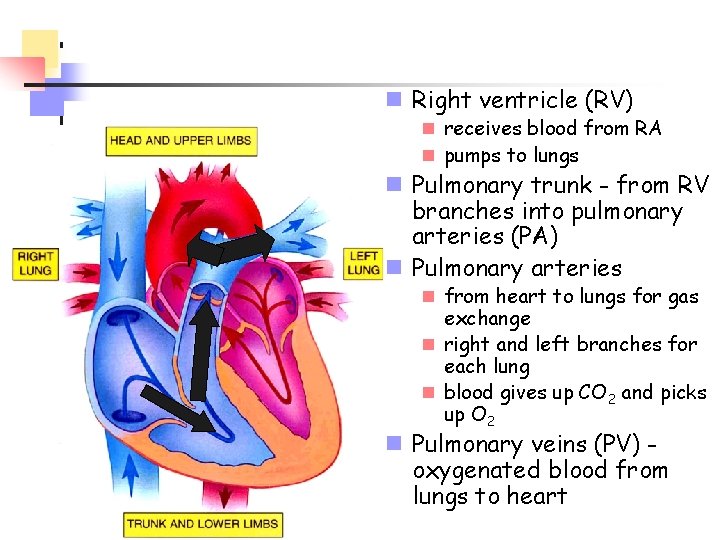
n Right ventricle (RV) n receives blood from RA n pumps to lungs n Pulmonary trunk - from RV branches into pulmonary arteries (PA) n Pulmonary arteries n from heart to lungs for gas exchange n right and left branches for each lung n blood gives up CO 2 and picks up O 2 n Pulmonary veins (PV) oxygenated blood from lungs to heart
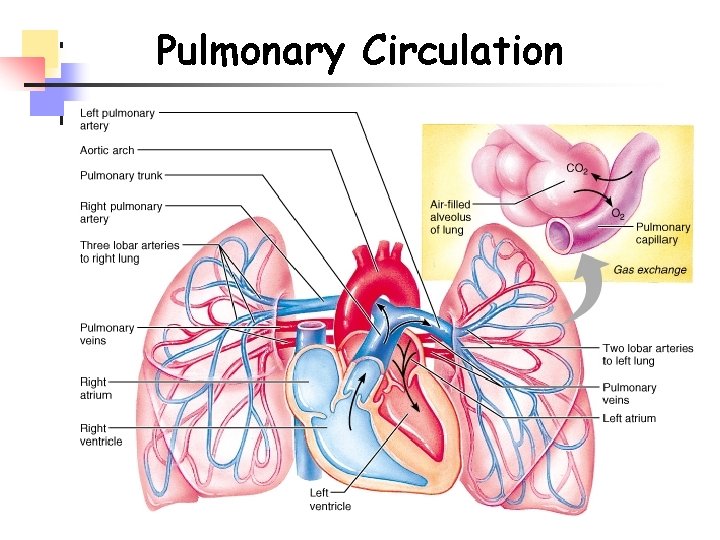
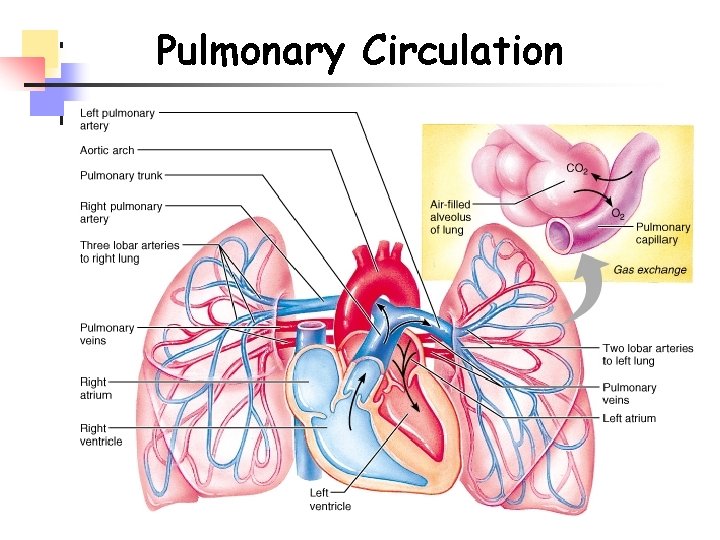
Pulmonary Circulation
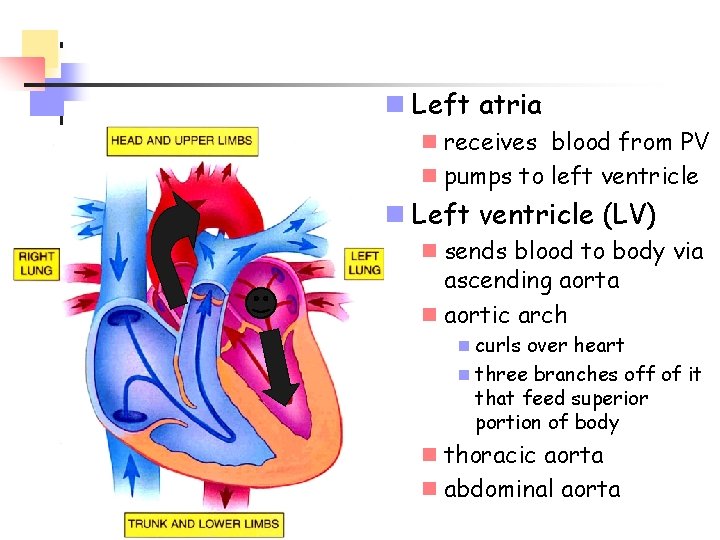
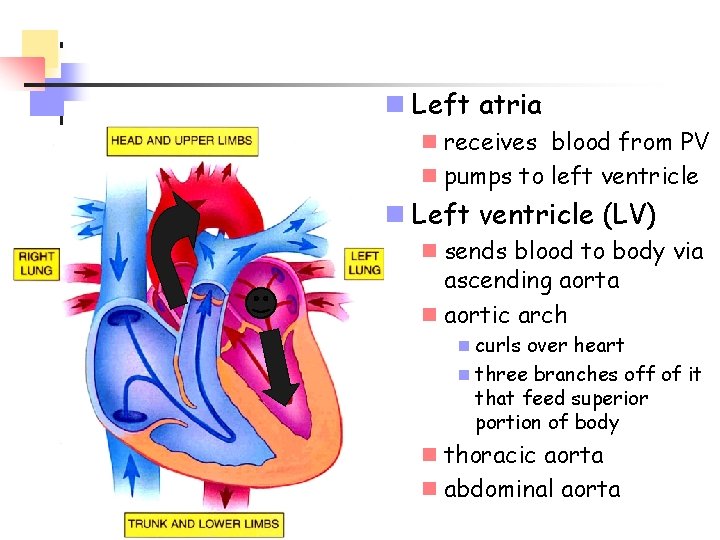
n Left atria n receives blood from PV n pumps to left ventricle n Left ventricle (LV) n sends blood to body via ascending aorta n aortic arch n curls over heart n three branches off of it that feed superior portion of body n thoracic aorta n abdominal aorta
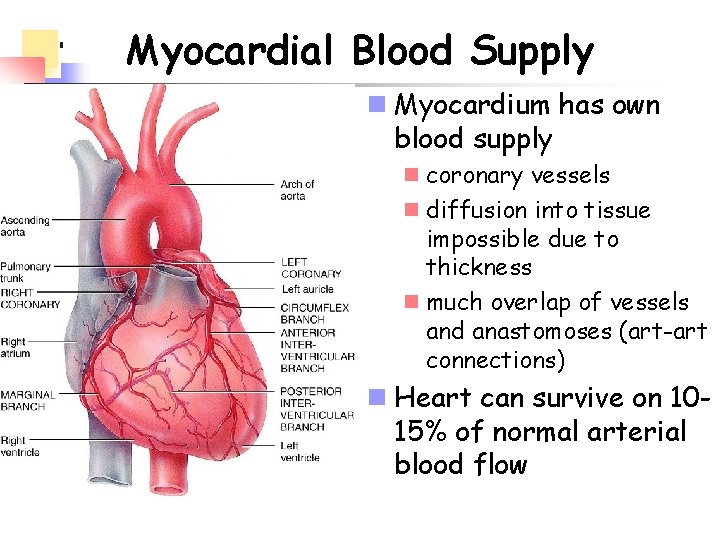
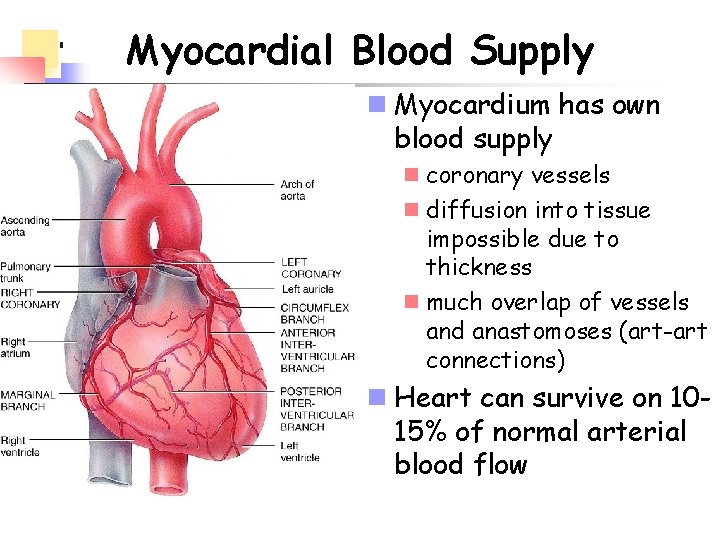
Myocardial Blood Supply n Myocardium has own blood supply n coronary vessels n diffusion into tissue impossible due to thickness n much overlap of vessels and anastomoses (art-art connections) n Heart can survive on 1015% of normal arterial blood flow
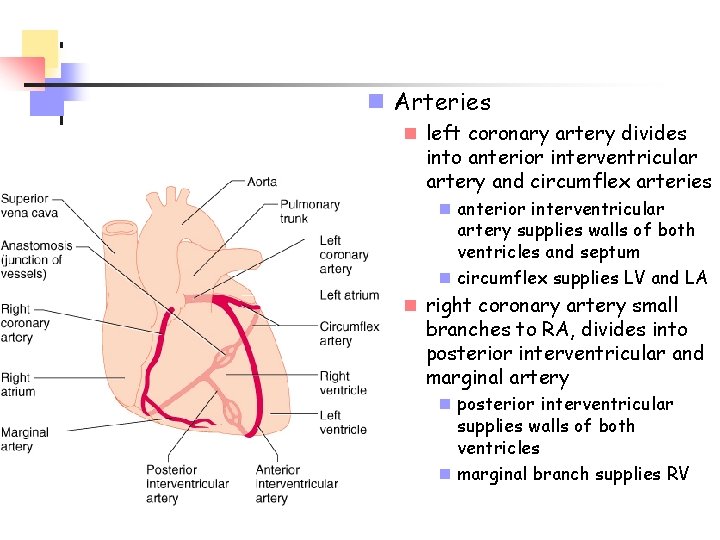
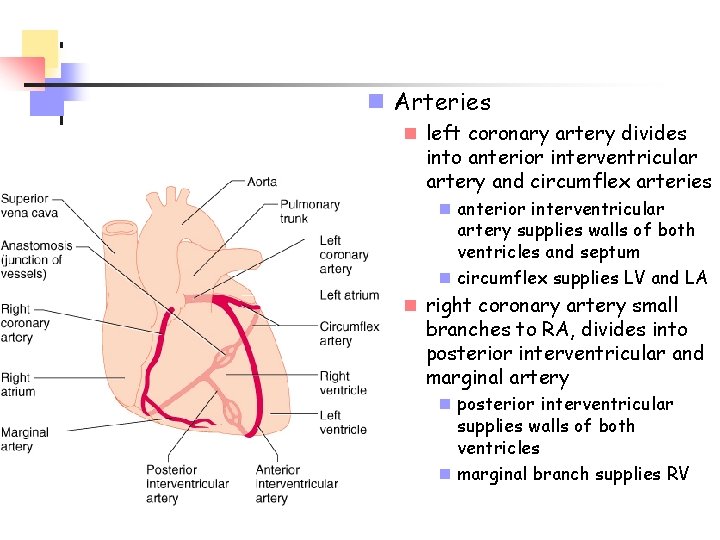
n Arteries n left coronary artery divides into anterior interventricular artery and circumflex arteries n anterior interventricular artery supplies walls of both ventricles and septum n circumflex supplies LV and LA n right coronary artery small branches to RA, divides into posterior interventricular and marginal artery n posterior interventricular supplies walls of both ventricles n marginal branch supplies RV
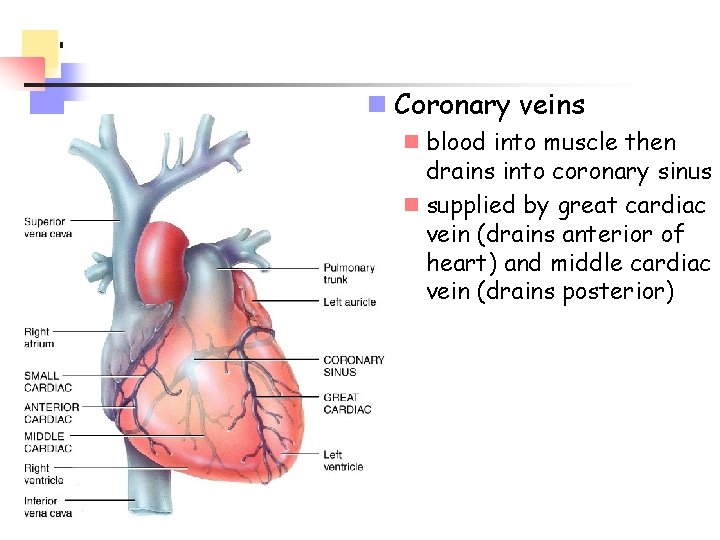
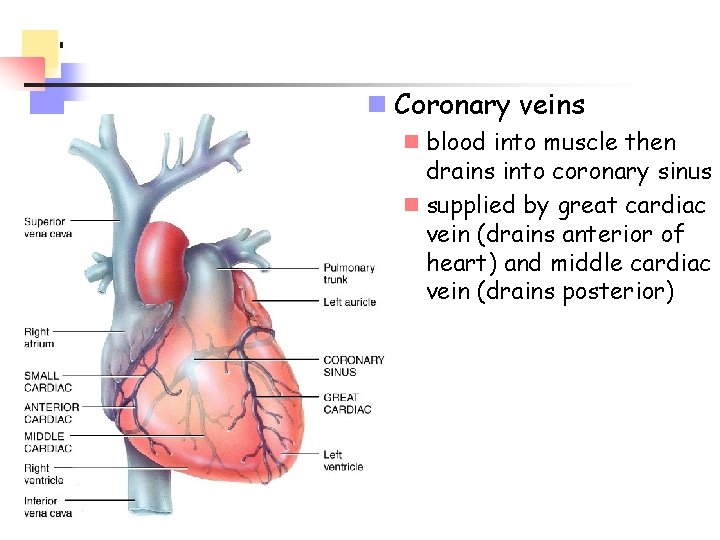
n Coronary veins n blood into muscle then drains into coronary sinus n supplied by great cardiac vein (drains anterior of heart) and middle cardiac vein (drains posterior)
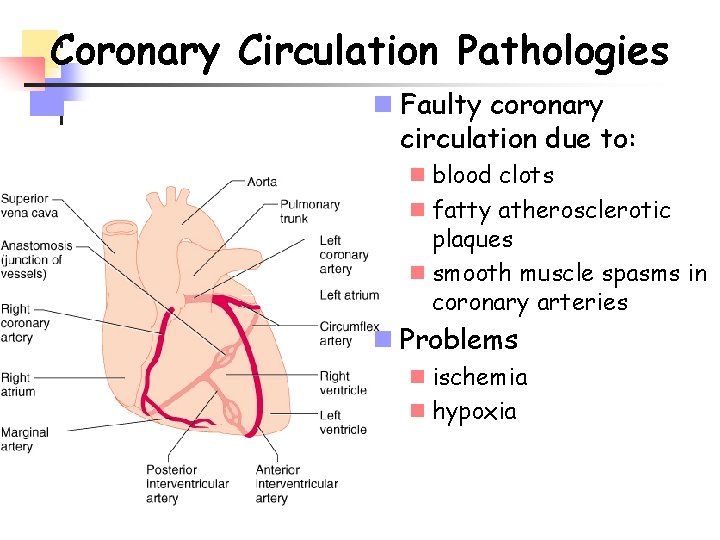
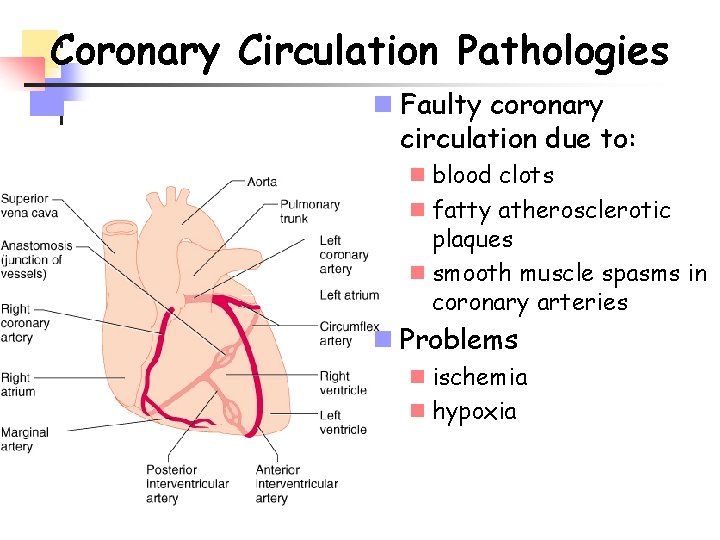
Coronary Circulation Pathologies n Faulty coronary circulation due to: n blood clots n fatty atherosclerotic plaques n smooth muscle spasms in coronary arteries n Problems n ischemia n hypoxia
Pathologies (cont. ) n Angina pectoris - "strangled chest" n pain w/ myocardial ischemia - referred pain! n tight/squeezing sensation in chest n labored breathing, weakness, dizziness, perspiration, foreboding n often during exertion - climbing stairs, etc n silent myocardial ischemia
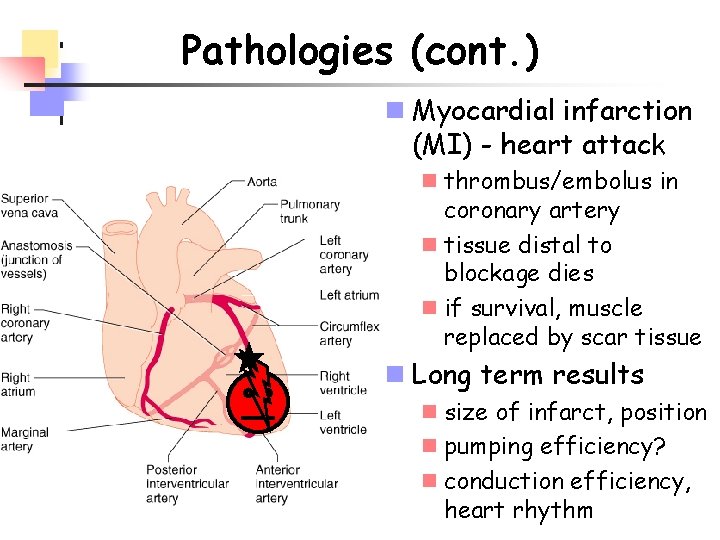
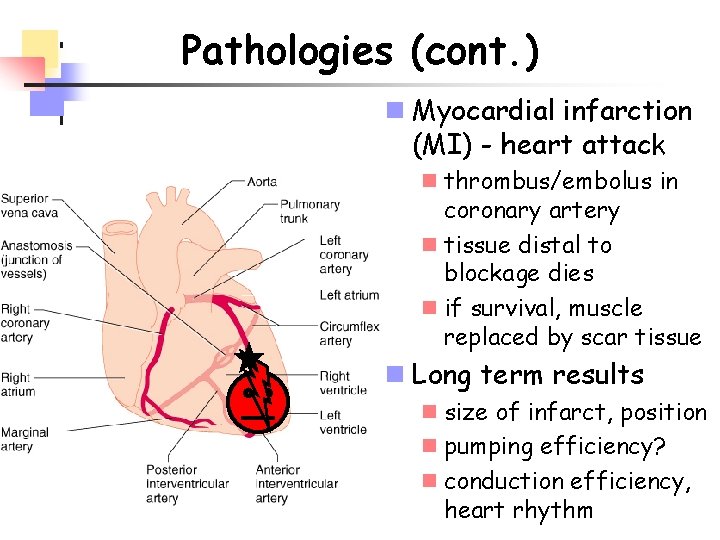
Pathologies (cont. ) n Myocardial infarction (MI) - heart attack n thrombus/embolus in coronary artery n tissue distal to blockage dies n if survival, muscle replaced by scar tissue n Long term results n size of infarct, position n pumping efficiency? n conduction efficiency, heart rhythm
Pathologies (cont. ) n Treatment n clot-dissolving agents n angioplasty n Reperfusion damage n re-establishing blood flow may damage tissue n oxygen free radicals - electrically charged molecules w/ unpaired electron n radicals attack proteins (enzymes), neurotransmitters, nucleic acids, plasma membranes n further damage to previously undamaged tissue or already damaged tissue
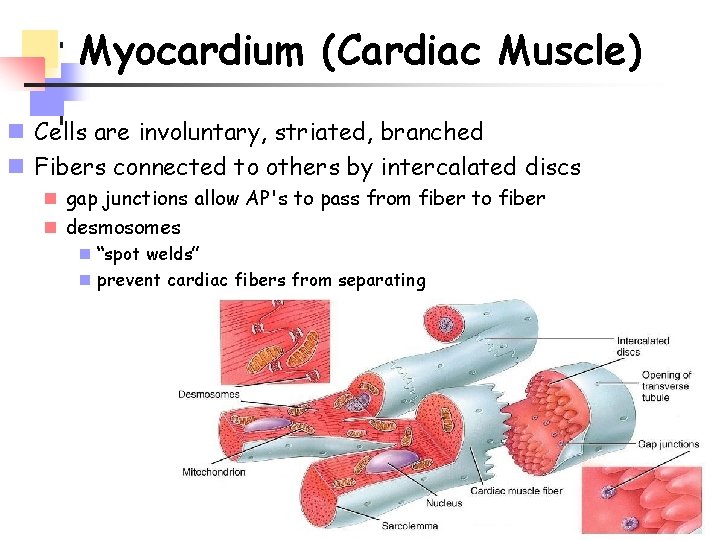
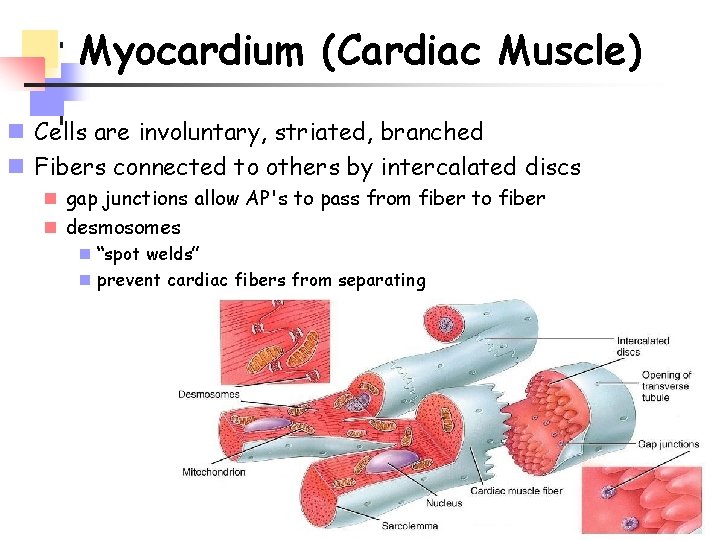
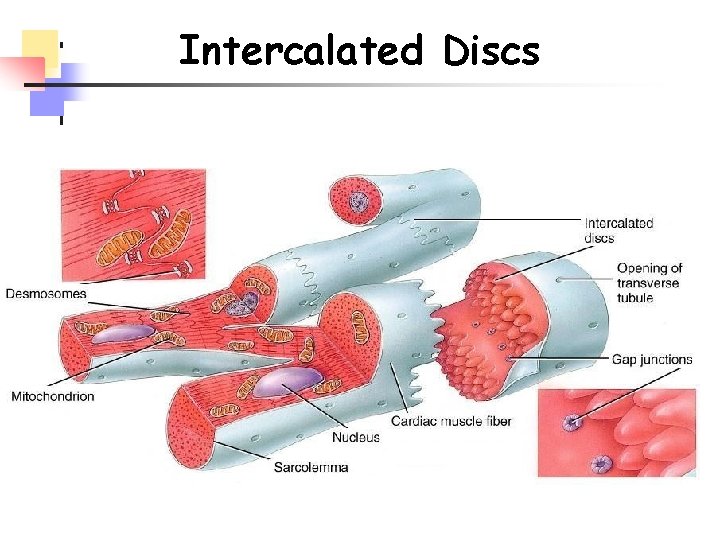
Myocardium (Cardiac Muscle) n Cells are involuntary, striated, branched n Fibers connected to others by intercalated discs n gap junctions allow AP's to pass from fiber to fiber n desmosomes n “spot welds” n prevent cardiac fibers from separating
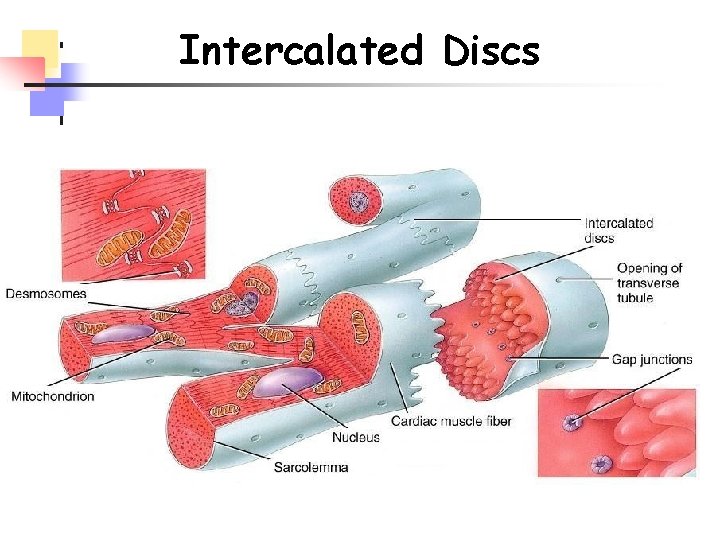
Intercalated Discs
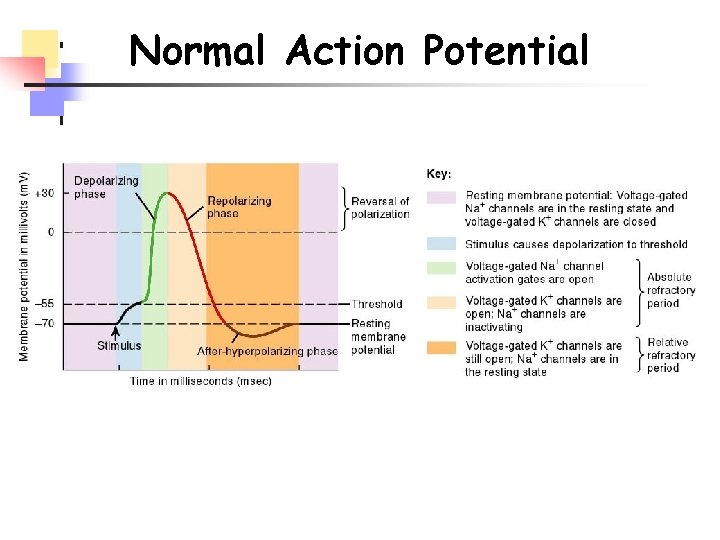
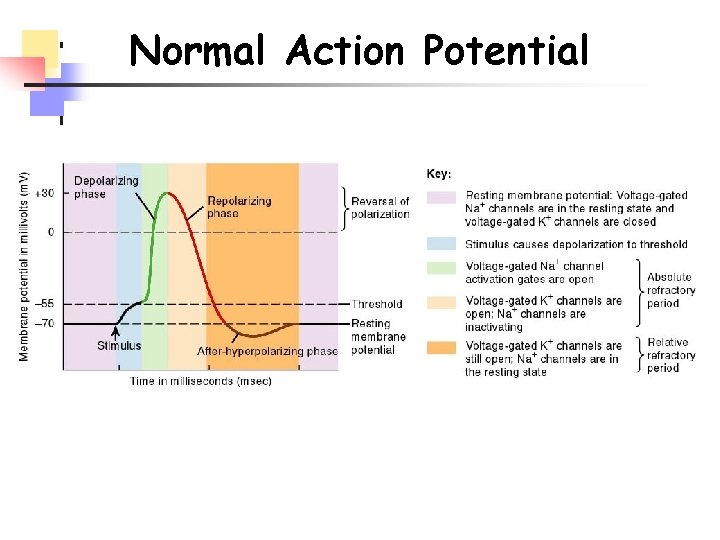
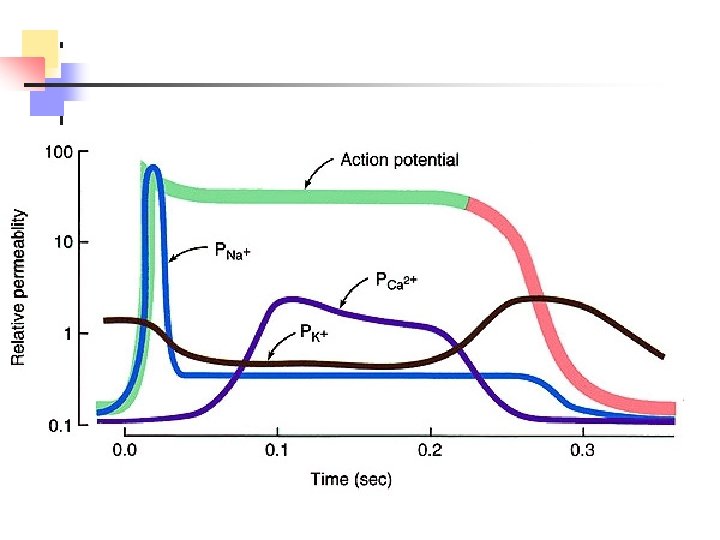
Normal Action Potential
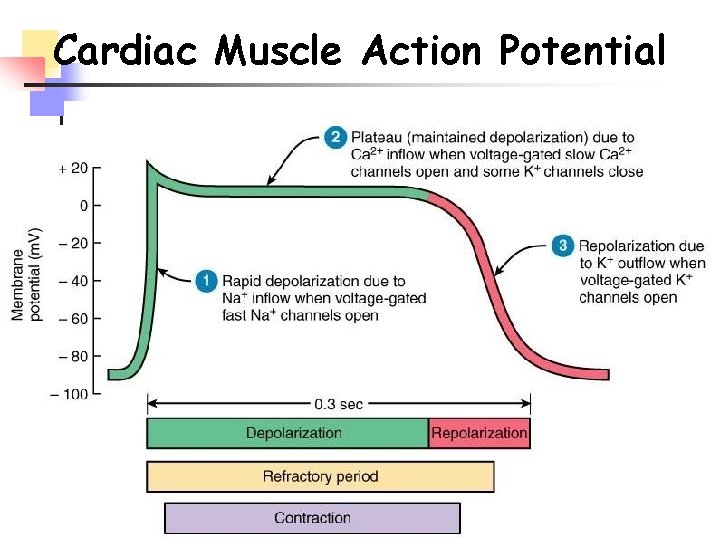
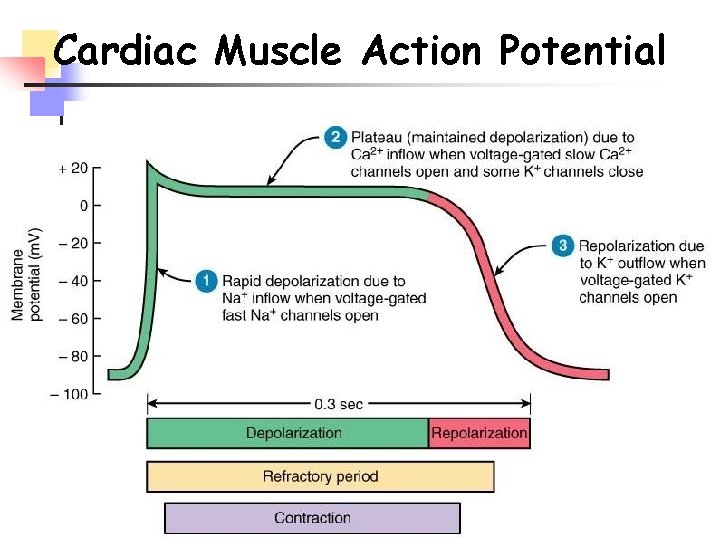
Cardiac Muscle Action Potential
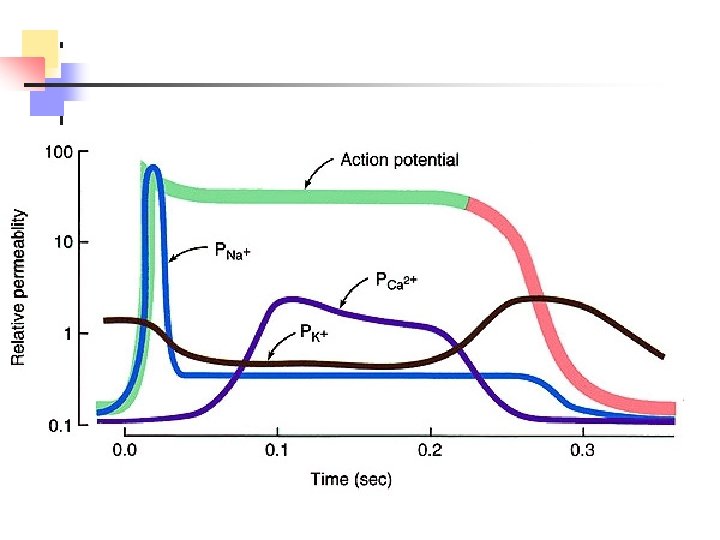
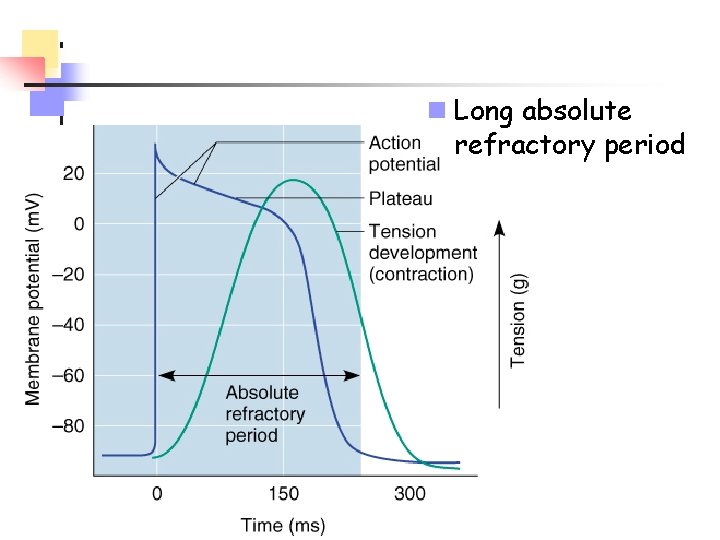
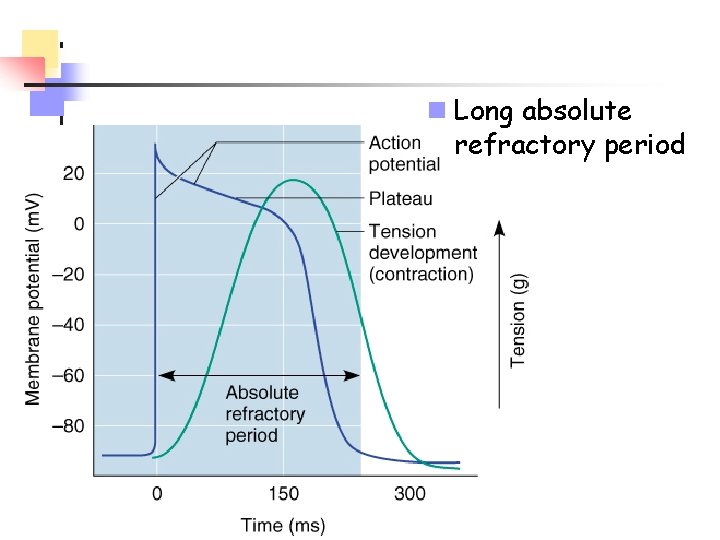
n Long absolute refractory period
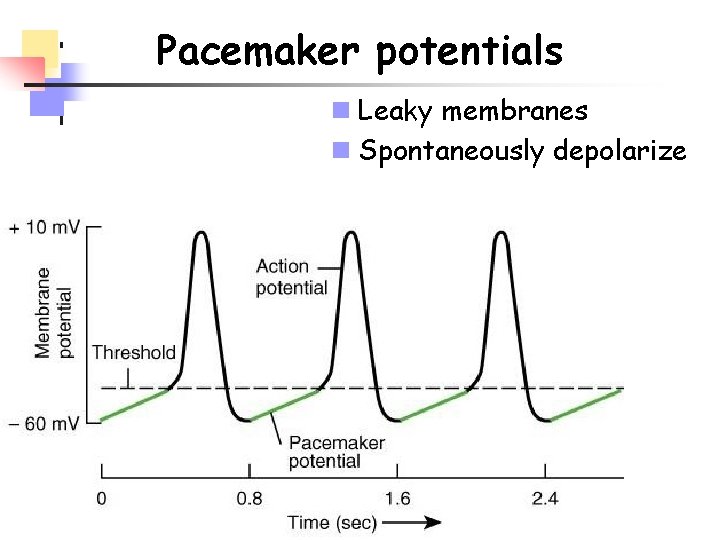
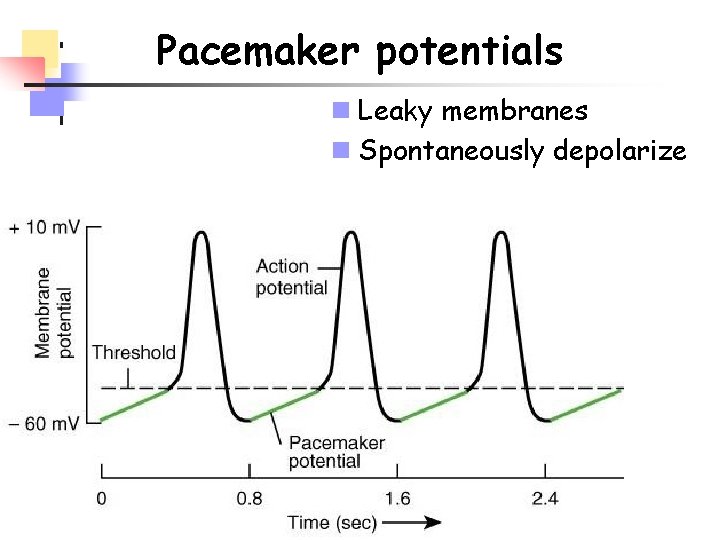
Pacemaker potentials n Leaky membranes n Spontaneously depolarize
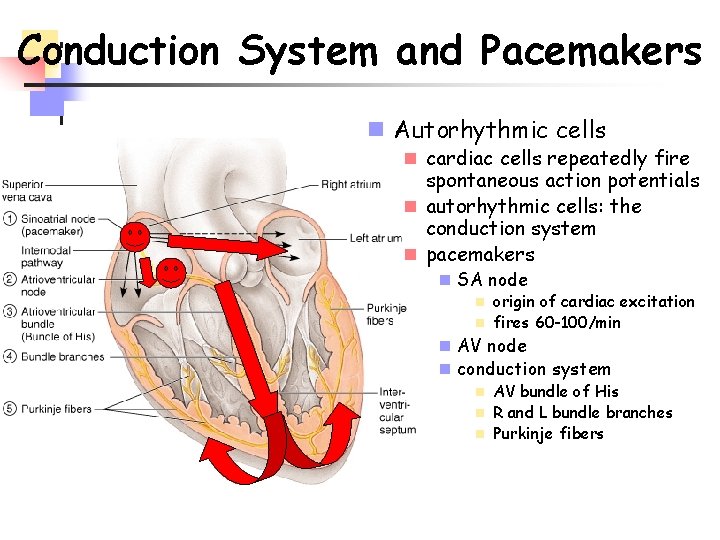
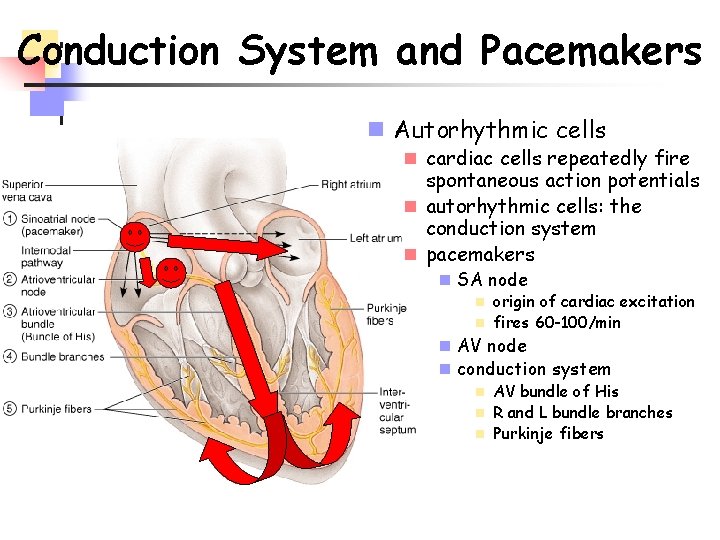
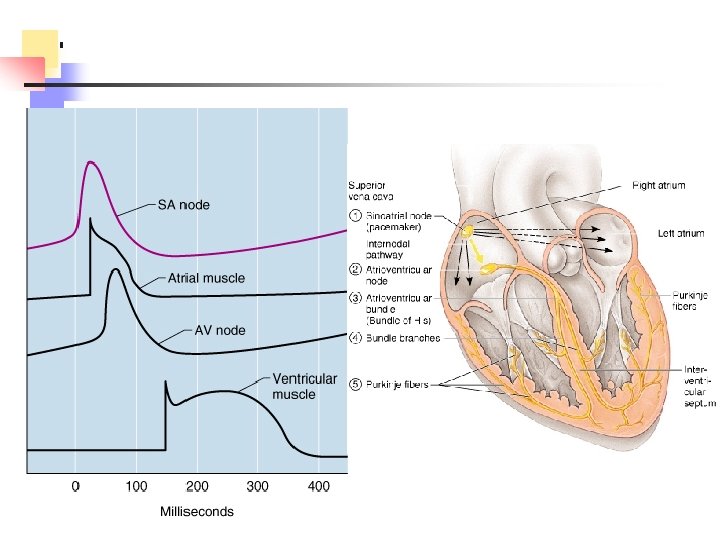
Conduction System and Pacemakers n Autorhythmic cells n cardiac cells repeatedly fire spontaneous action potentials n autorhythmic cells: the conduction system n pacemakers n SA node n origin of cardiac excitation n fires 60 -100/min n AV node n conduction system n AV bundle of His n R and L bundle branches n Purkinje fibers
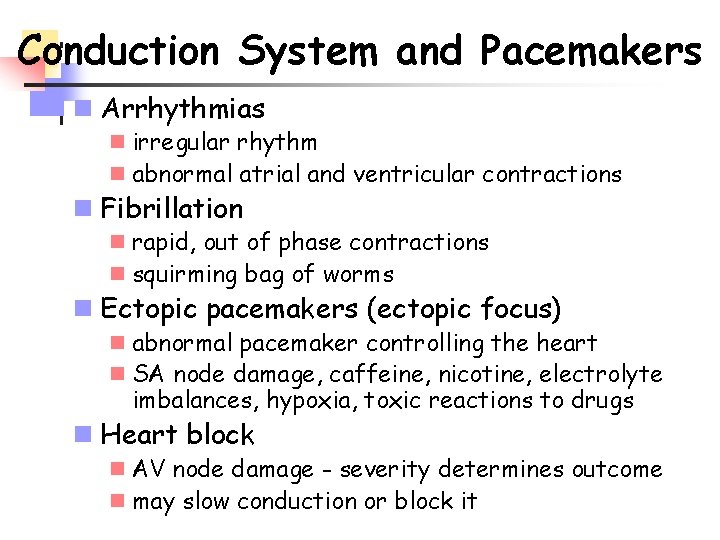
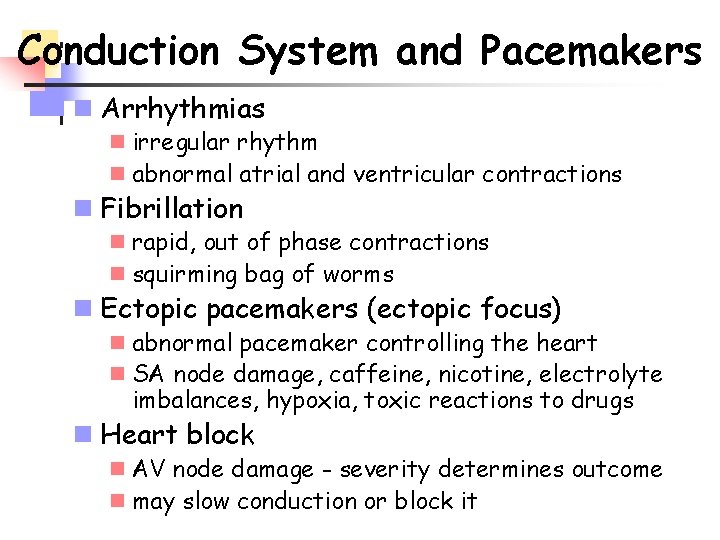
Conduction System and Pacemakers n Arrhythmias n irregular rhythm n abnormal atrial and ventricular contractions n Fibrillation n rapid, out of phase contractions n squirming bag of worms n Ectopic pacemakers (ectopic focus) n abnormal pacemaker controlling the heart n SA node damage, caffeine, nicotine, electrolyte imbalances, hypoxia, toxic reactions to drugs n Heart block n AV node damage - severity determines outcome n may slow conduction or block it
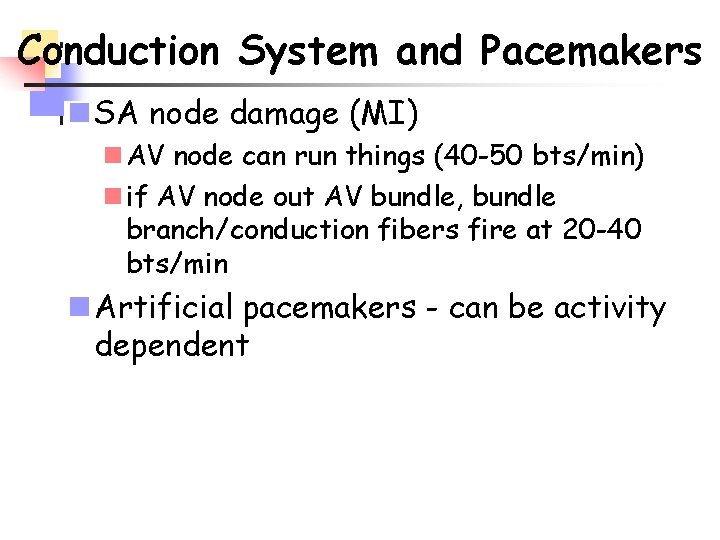
Conduction System and Pacemakers n SA node damage (MI) n AV node can run things (40 -50 bts/min) n if AV node out AV bundle, bundle branch/conduction fibers fire at 20 -40 bts/min n Artificial pacemakers - can be activity dependent
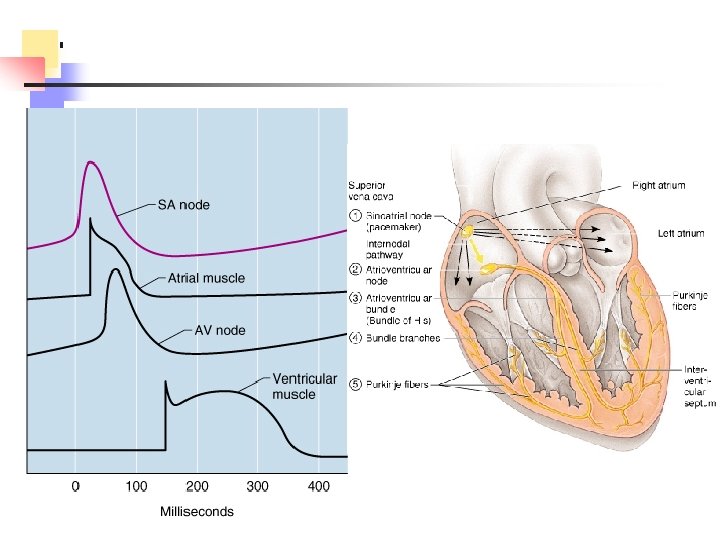
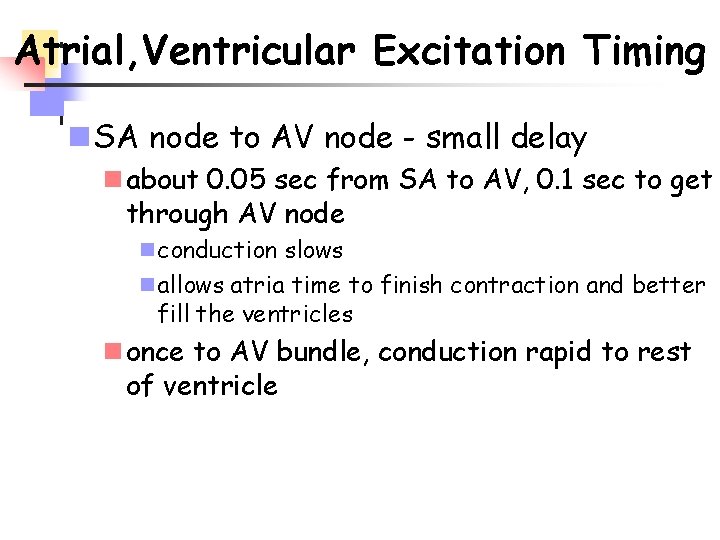
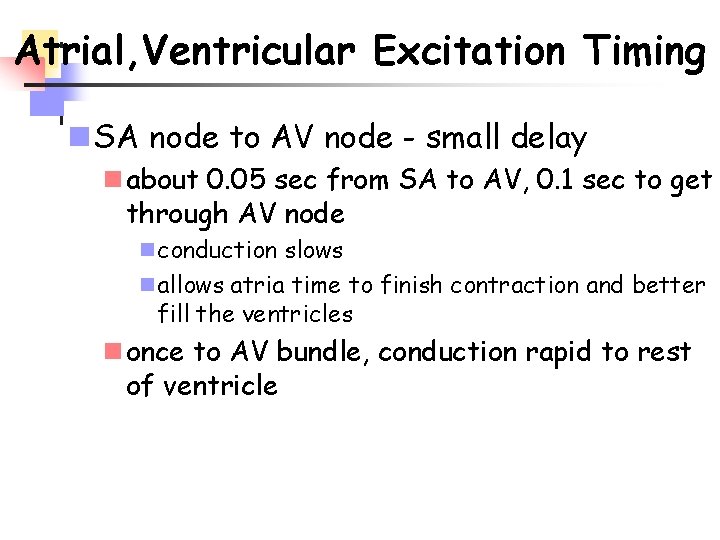
Atrial, Ventricular Excitation Timing n SA node to AV node - small delay n about 0. 05 sec from SA to AV, 0. 1 sec to get through AV node n conduction slows n allows atria time to finish contraction and better fill the ventricles n once to AV bundle, conduction rapid to rest of ventricle
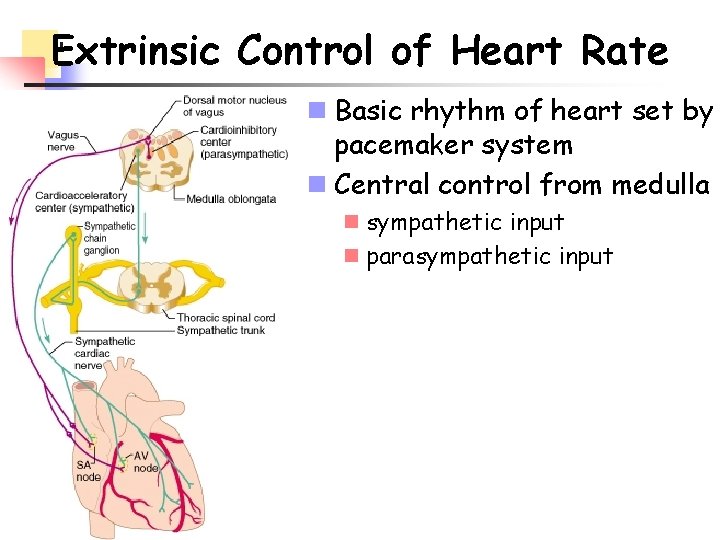
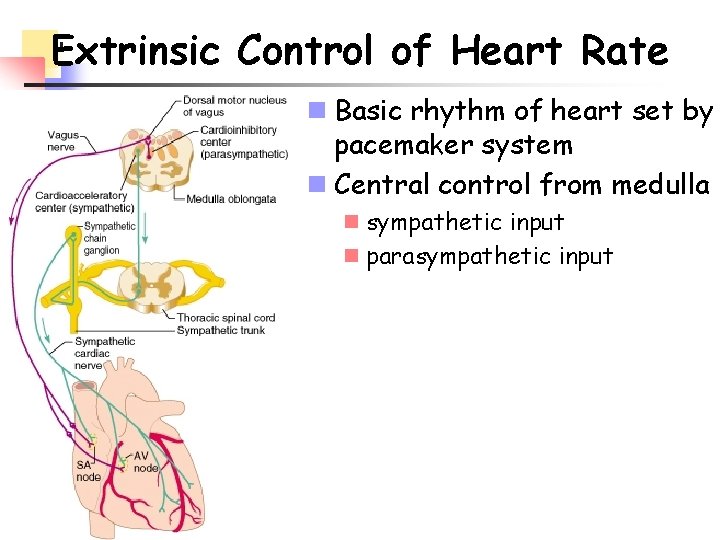
Extrinsic Control of Heart Rate n Basic rhythm of heart set by pacemaker system n Central control from medulla n sympathetic input n parasympathetic input
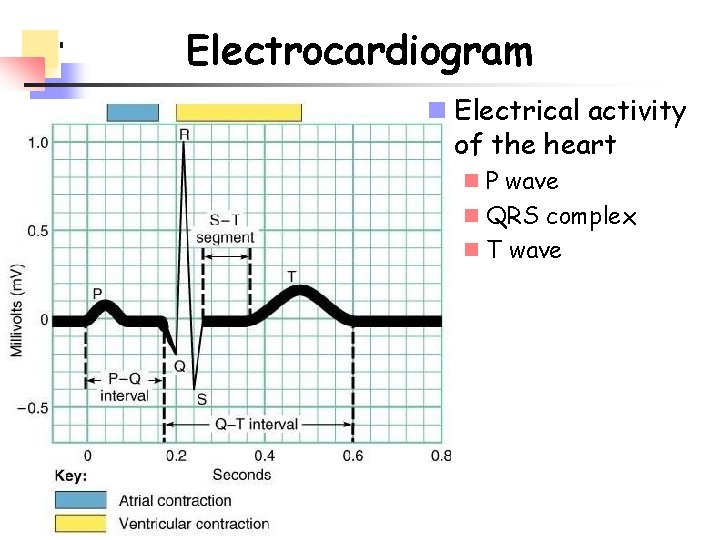
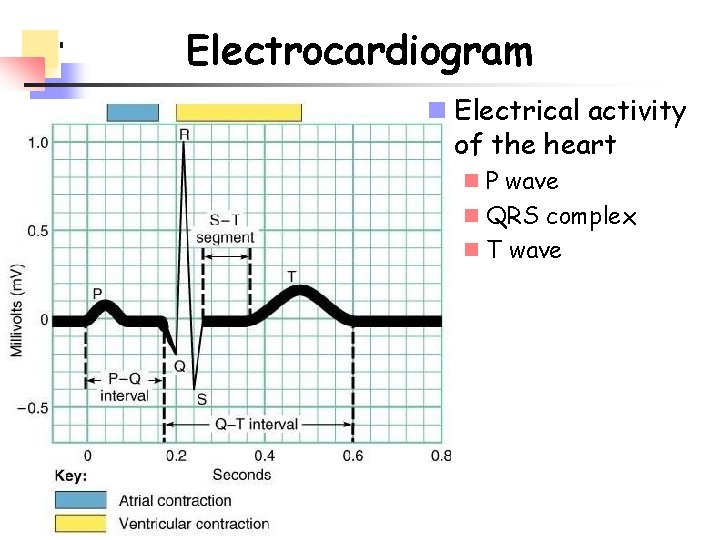
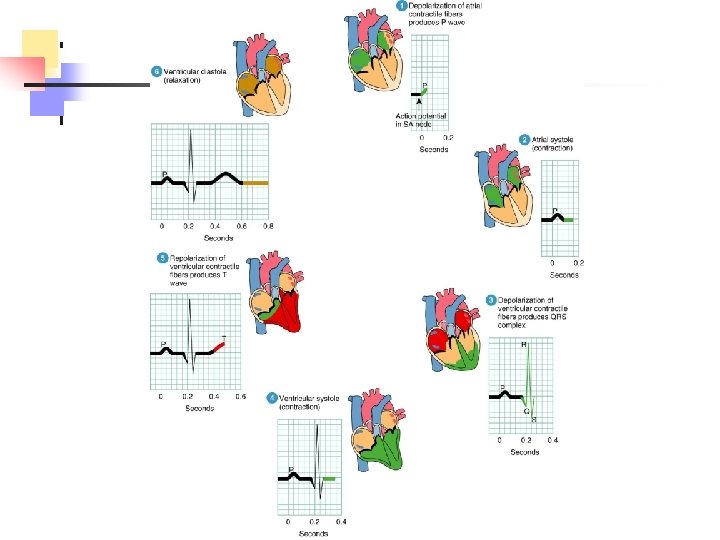
Electrocardiogram n Electrical activity of the heart n P wave n QRS complex n T wave
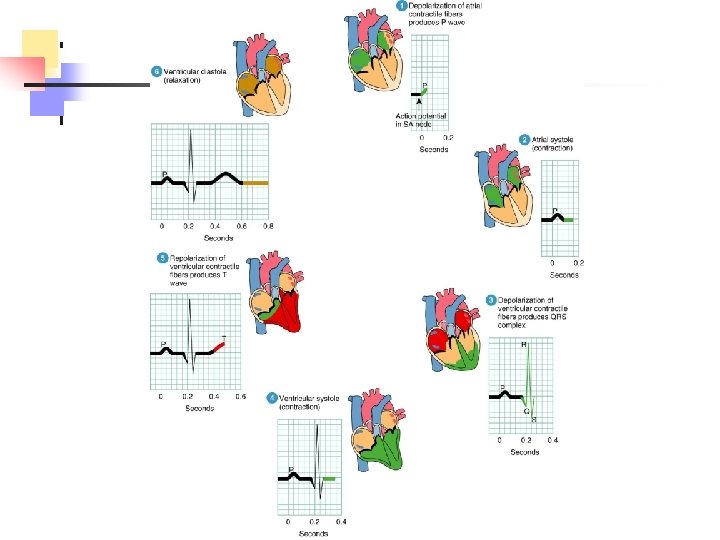
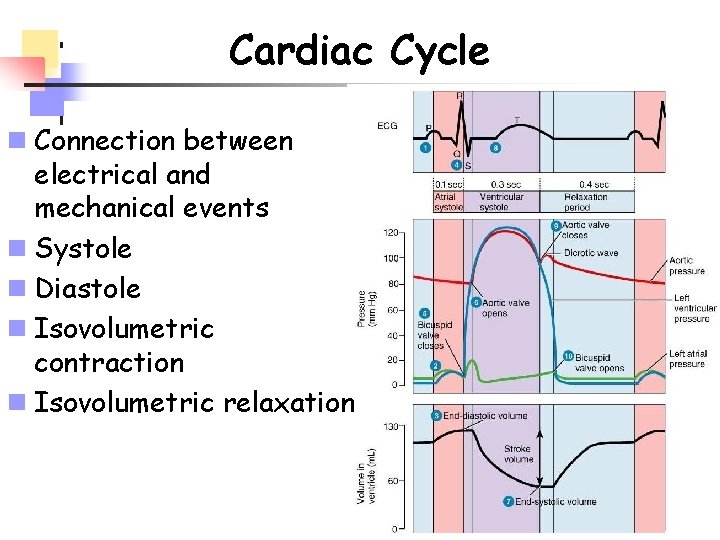
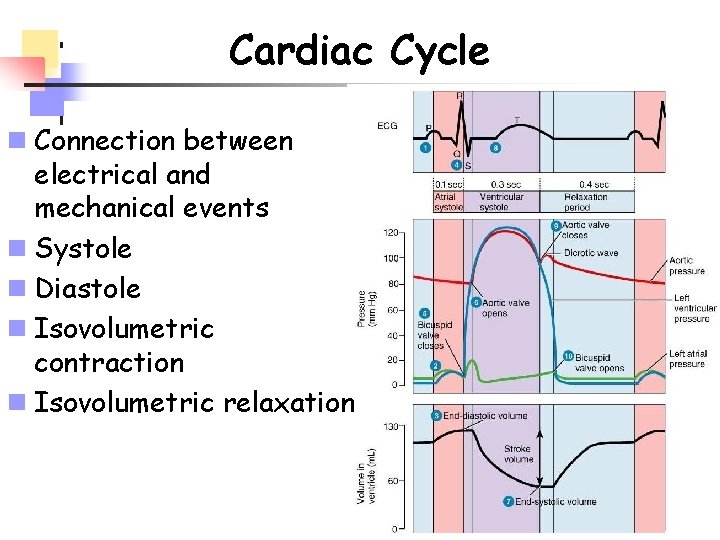
Cardiac Cycle n Connection between electrical and mechanical events n Systole n Diastole n Isovolumetric contraction n Isovolumetric relaxation
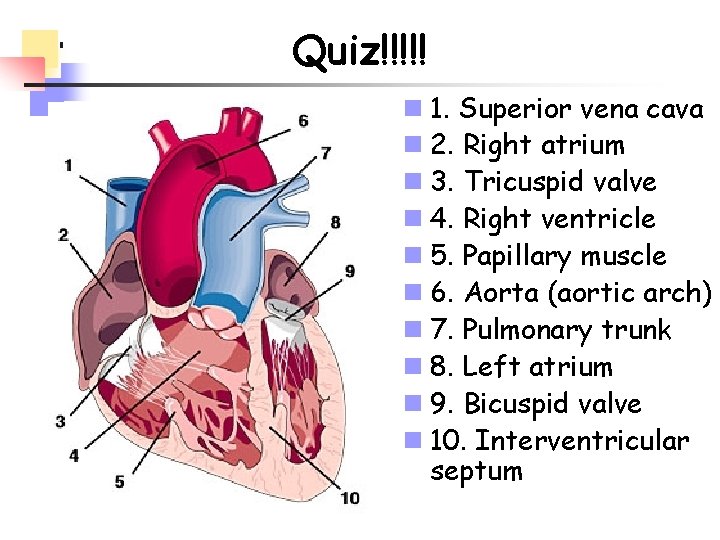
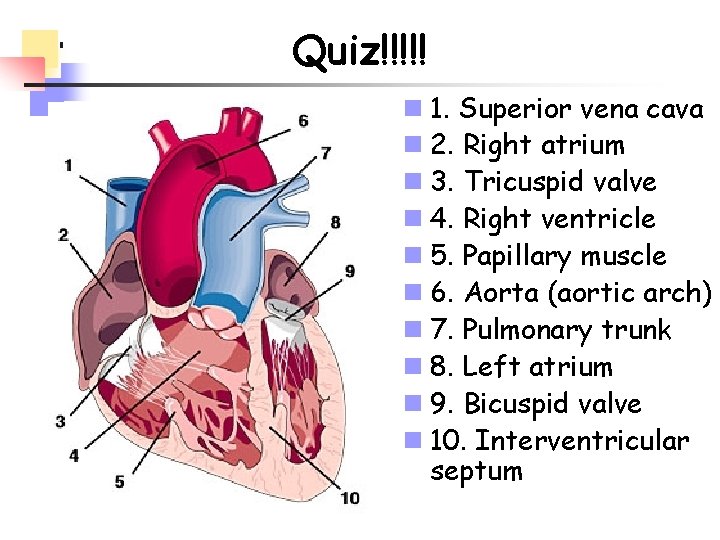
Quiz!!!!! n 1. Superior vena cava n 2. Right atrium n 3. Tricuspid valve n 4. Right ventricle n 5. Papillary muscle n 6. Aorta (aortic arch) n 7. Pulmonary trunk n 8. Left atrium n 9. Bicuspid valve n 10. Interventricular septum
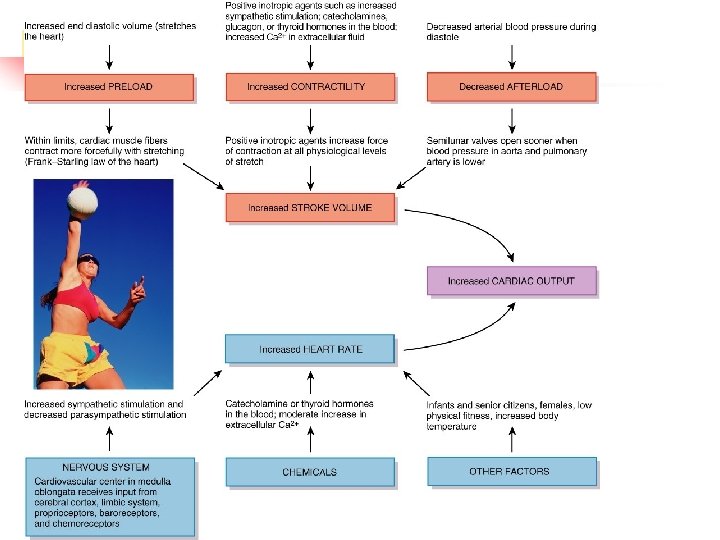
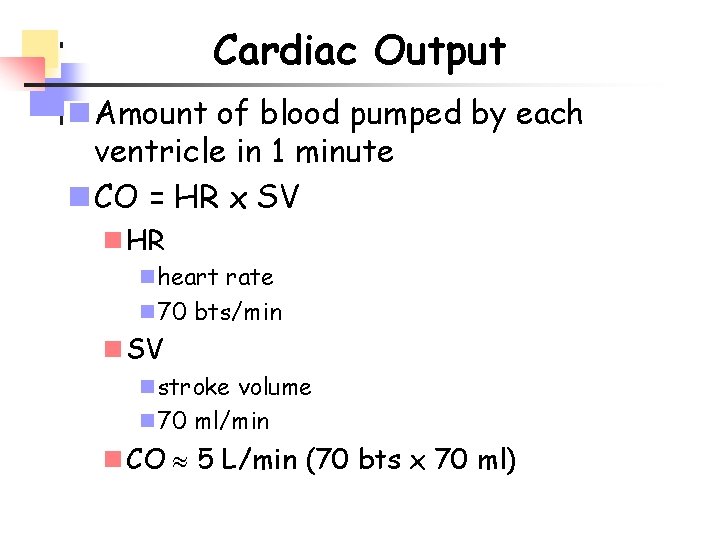
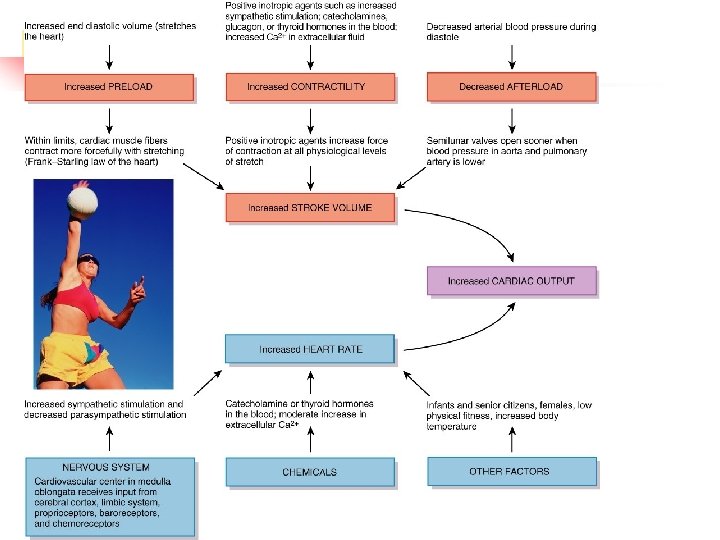
Cardiac Output n Amount of blood pumped by each ventricle in 1 minute n CO = HR x SV n HR n heart rate n 70 bts/min n SV n stroke volume n 70 ml/min n CO 5 L/min (70 bts x 70 ml)
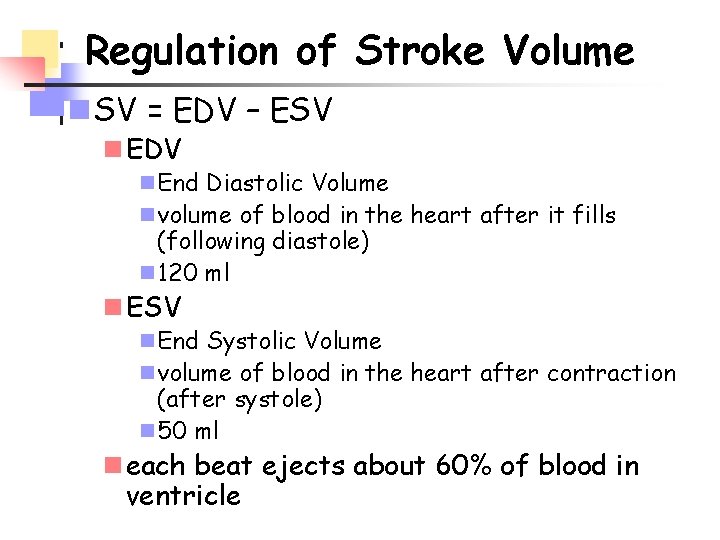
Regulation of Stroke Volume n SV = EDV – ESV n EDV n End Diastolic Volume n volume of blood in the heart after it fills (following diastole) n 120 ml n ESV n End Systolic Volume n volume of blood in the heart after contraction (after systole) n 50 ml n each beat ejects about 60% of blood in ventricle
n Most important factors in regulating SV: preload, contractility and afterload n Preload n degree of stretch of cardiac muscle cells before contraction n determined by EDV n Contractility n increase in contractile strength separate from stretch and EDV n determined by changes in Ca++ availability n Afterload n pressure that must be overcome for ventricles to eject blood from heart n determined by TPR
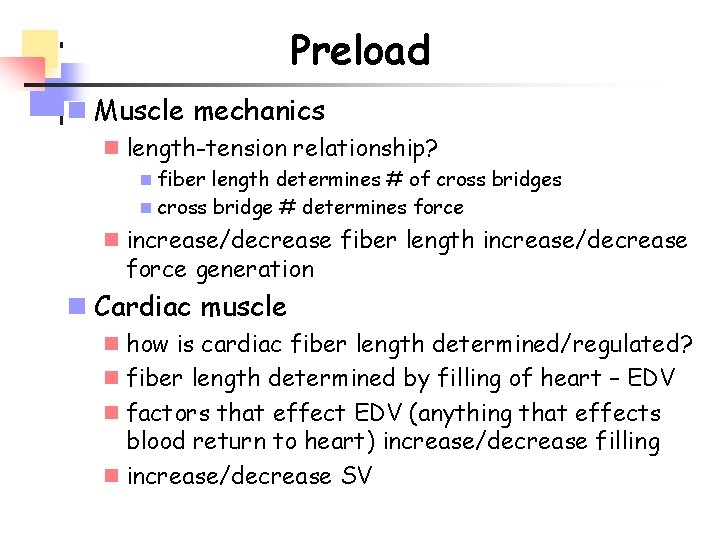
Preload n Muscle mechanics n length-tension relationship? n fiber length determines # of cross bridges n cross bridge # determines force n increase/decrease fiber length increase/decrease force generation n Cardiac muscle n how is cardiac fiber length determined/regulated? n fiber length determined by filling of heart – EDV n factors that effect EDV (anything that effects blood return to heart) increase/decrease filling n increase/decrease SV
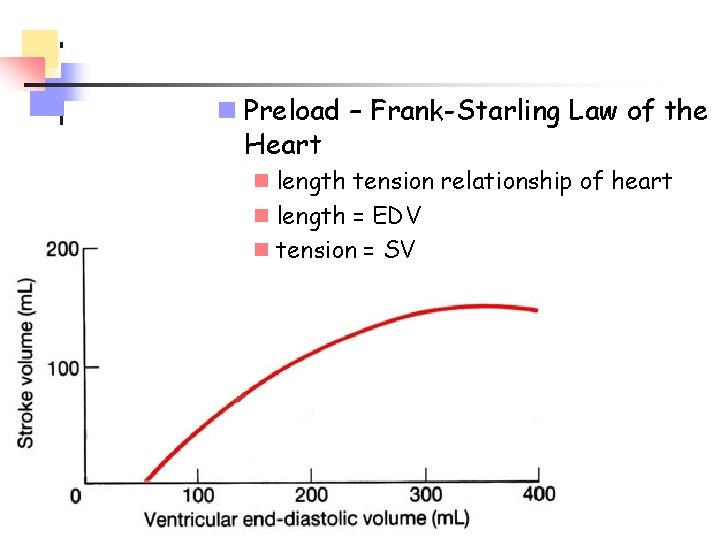
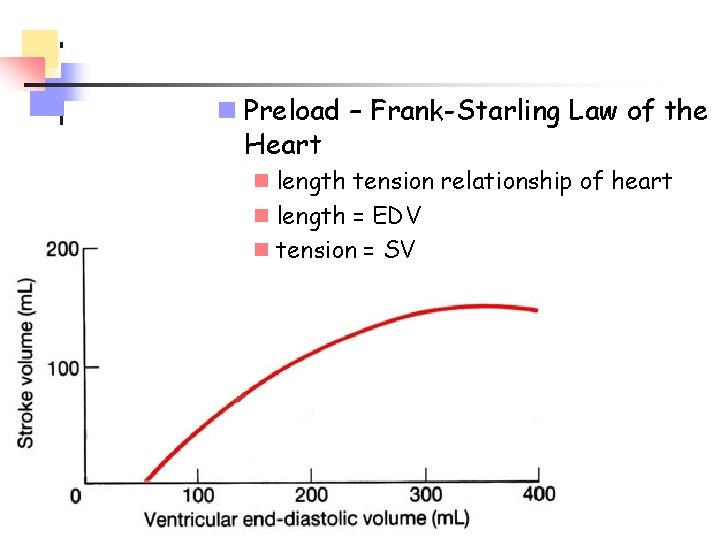
n Preload – Frank-Starling Law of the Heart n length tension relationship of heart n length = EDV n tension = SV
Contractility n Increase in contractile strength separate from stretch and EDV n Do not change fiber length but increase contraction force? n what determines force? n how can we change this if we don’t change length?
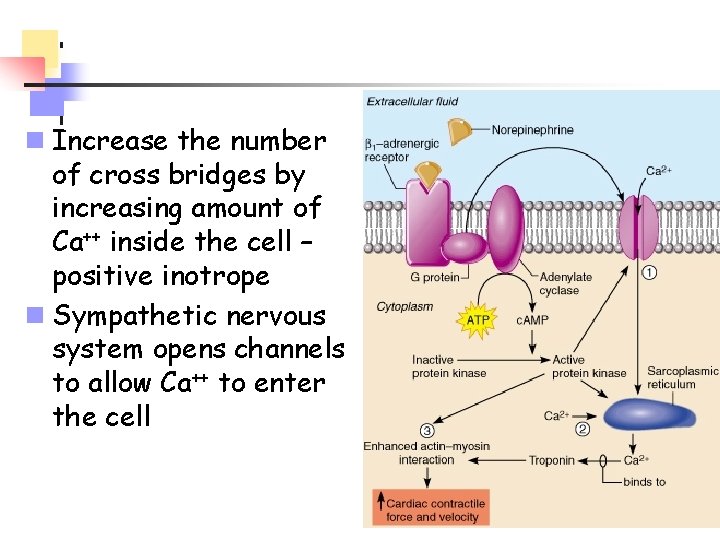
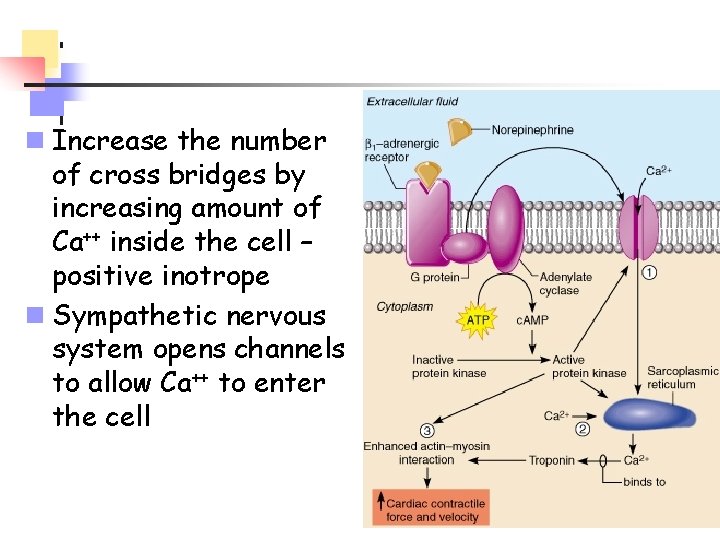
n Increase the number of cross bridges by increasing amount of Ca++ inside the cell – positive inotrope n Sympathetic nervous system opens channels to allow Ca++ to enter the cell
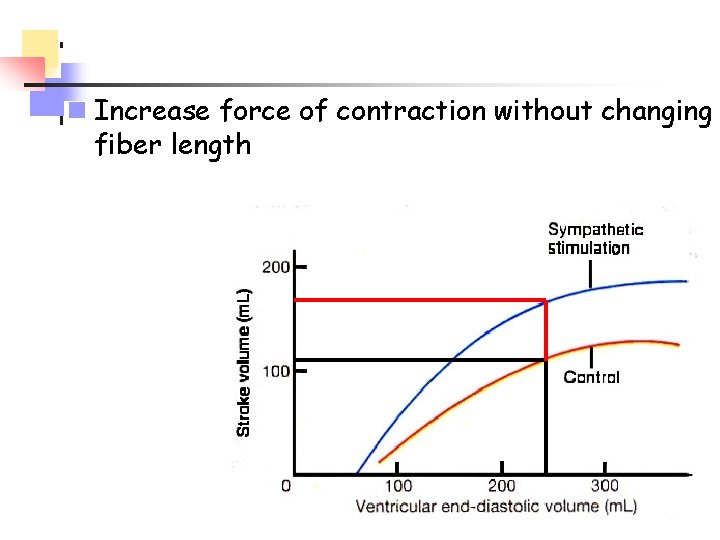
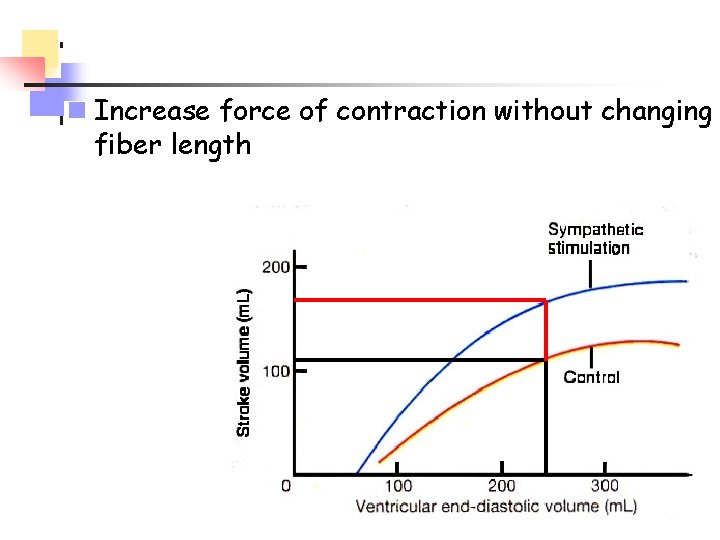
n Increase force of contraction without changing fiber length
Afterload n Flow = P/R n If blood pressure is high (TPR), difficult for heart to eject blood n More blood remains in ventricle with each beat n Heart has to work harder to eject blood, change the length/tension of the heart
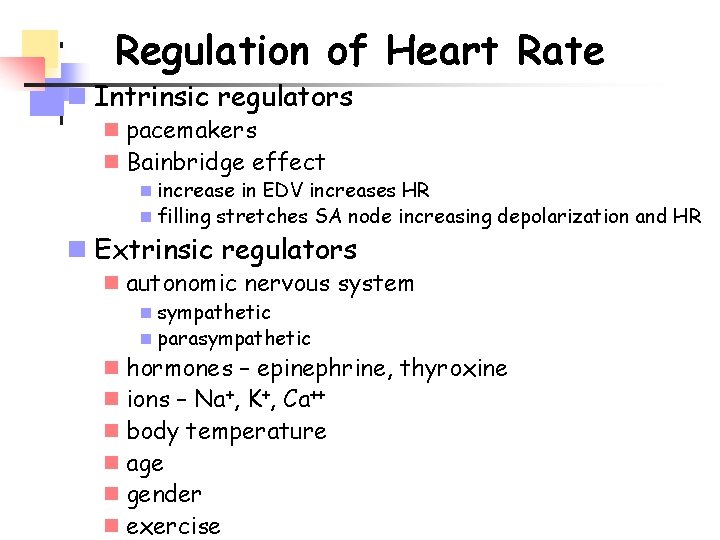
Regulation of Heart Rate n Intrinsic regulators n pacemakers n Bainbridge effect n increase in EDV increases HR n filling stretches SA node increasing depolarization and HR n Extrinsic regulators n autonomic nervous system n sympathetic n parasympathetic n hormones – epinephrine, thyroxine n ions – Na+, K+, Ca++ n body temperature n age n gender n exercise