z Lecture 3 z Soft tissue injuries sprain


- Slides: 158
z. Lecture 3 z. Soft tissue injuries, sprain DR CHIRAG ASSISTANT PROFESSOR DEPT OF ORTHOPAEDICS SBKS MIRC SUMANDEEP VIDYAPEETH VADODARA 1
DRUJ dislocation TFCC injury 2
Scope z. Introduction z. Anatomy z. Biomechanics z. Examination z. Investigation z. DRUJ dislocation z. TFCC injuries 3
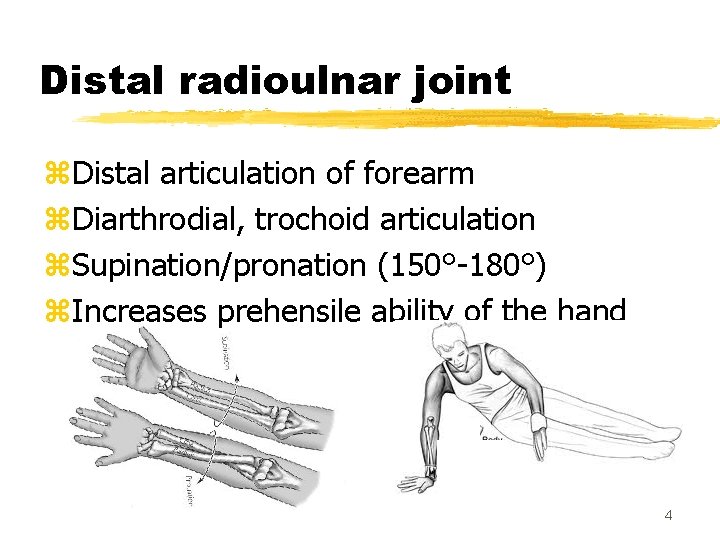
Distal radioulnar joint z. Distal articulation of forearm z. Diarthrodial, trochoid articulation z. Supination/pronation (150°-180°) z. Increases prehensile ability of the hand 4
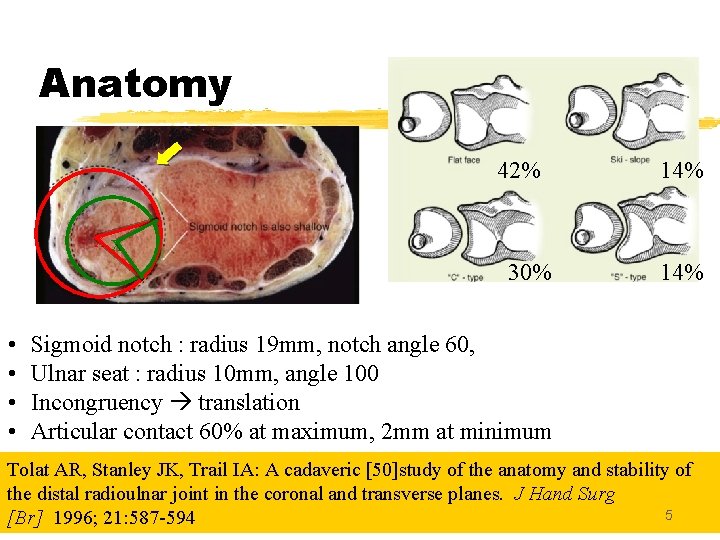
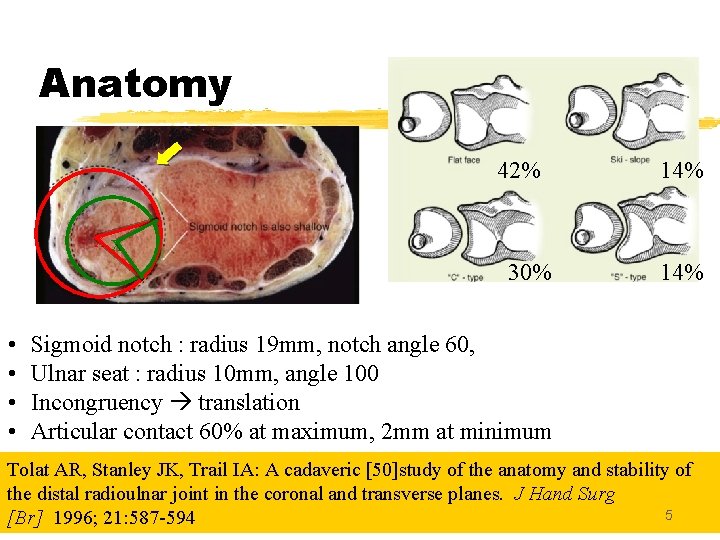
Anatomy 42% 14% xx 30% • • 14% Sigmoid notch : radius 19 mm, notch angle 60, Ulnar seat : radius 10 mm, angle 100 Incongruency translation Articular contact 60% at maximum, 2 mm at minimum Tolat AR, Stanley JK, Trail IA: A cadaveric [50]study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg 5 [Br] 1996; 21: 587 -594
6
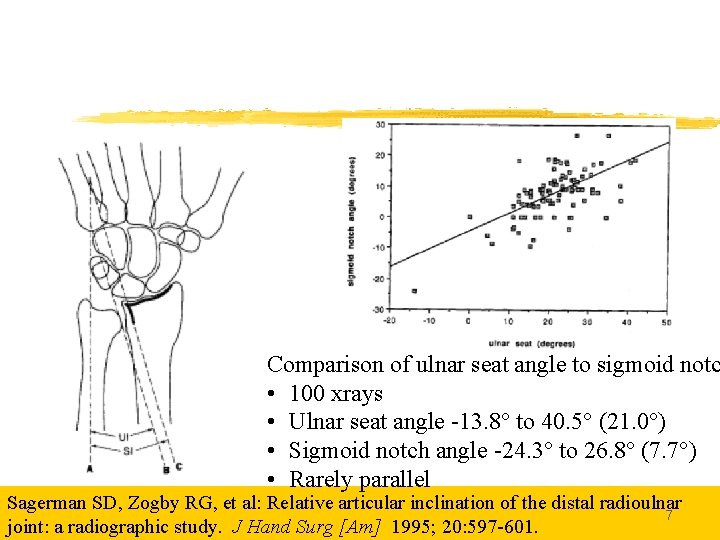
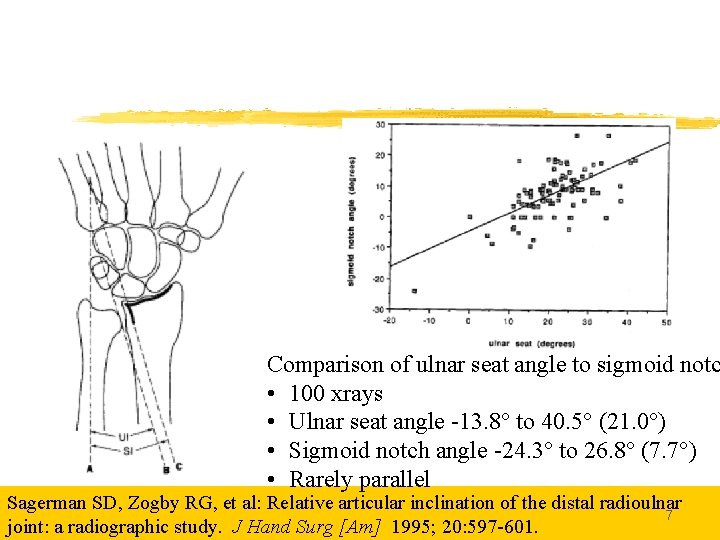
Comparison of ulnar seat angle to sigmoid notc • 100 xrays • Ulnar seat angle -13. 8° to 40. 5° (21. 0°) • Sigmoid notch angle -24. 3° to 26. 8° (7. 7°) • Rarely parallel Sagerman SD, Zogby RG, et al: Relative articular inclination of the distal radioulnar 7 joint: a radiographic study. J Hand Surg [Am] 1995; 20: 597 -601.
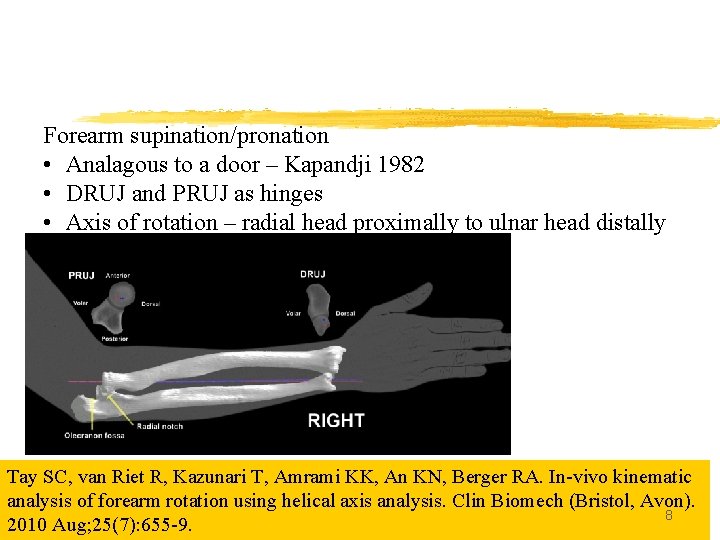
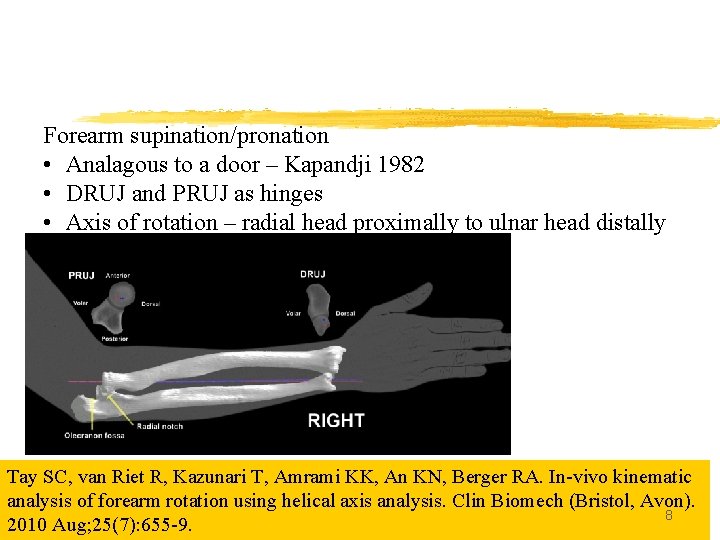
Forearm supination/pronation • Analagous to a door – Kapandji 1982 • DRUJ and PRUJ as hinges • Axis of rotation – radial head proximally to ulnar head distally Tay SC, van Riet R, Kazunari T, Amrami KK, An KN, Berger RA. In-vivo kinematic analysis of forearm rotation using helical axis analysis. Clin Biomech (Bristol, Avon). 8 2010 Aug; 25(7): 655 -9.
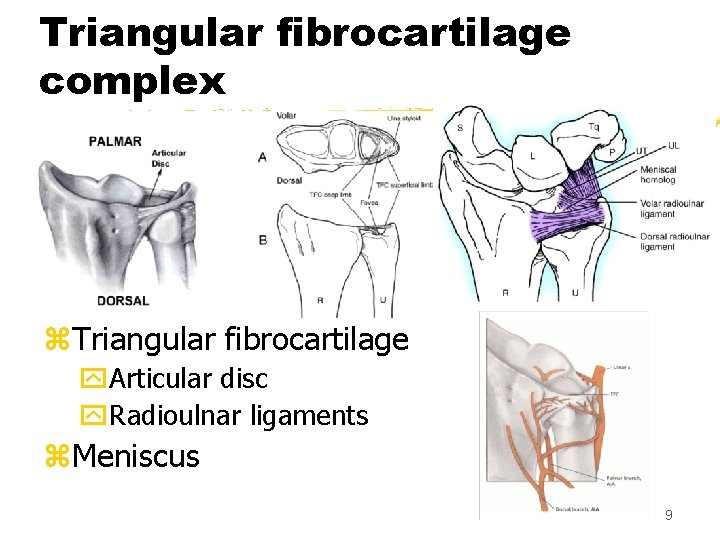
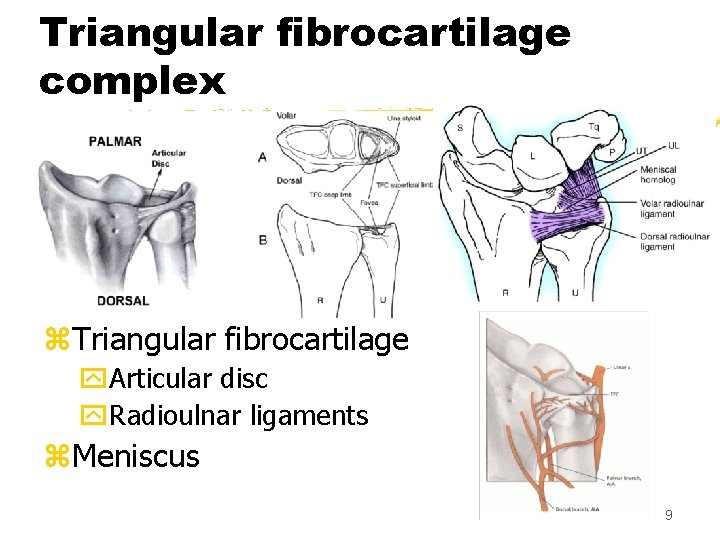
Triangular fibrocartilage complex z. Triangular fibrocartilage y. Articular disc y. Radioulnar ligaments z. Meniscus 9
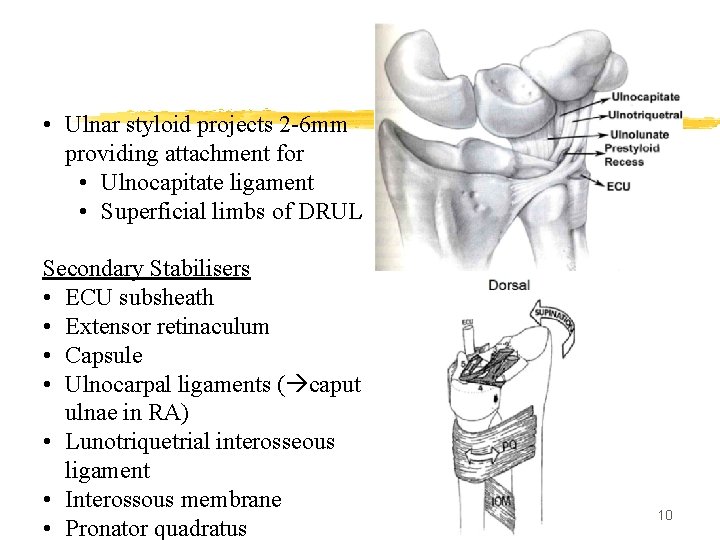
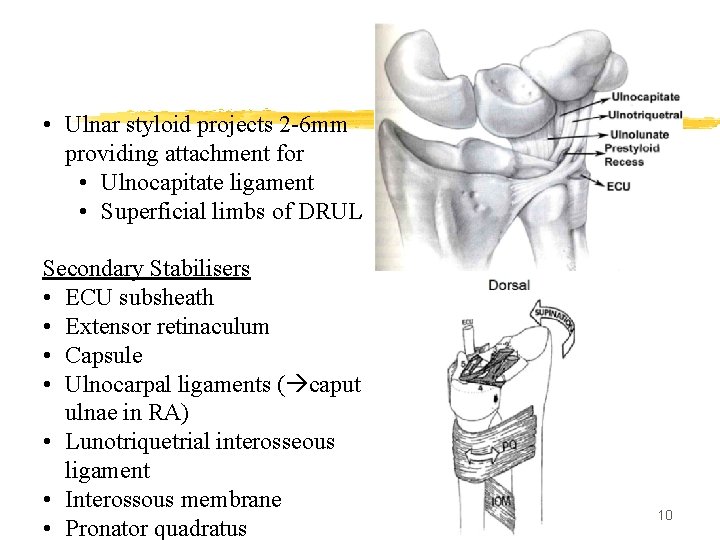
• Ulnar styloid projects 2 -6 mm providing attachment for • Ulnocapitate ligament • Superficial limbs of DRUL Secondary Stabilisers • ECU subsheath • Extensor retinaculum • Capsule • Ulnocarpal ligaments ( caput ulnae in RA) • Lunotriquetrial interosseous ligament • Interossous membrane • Pronator quadratus 10
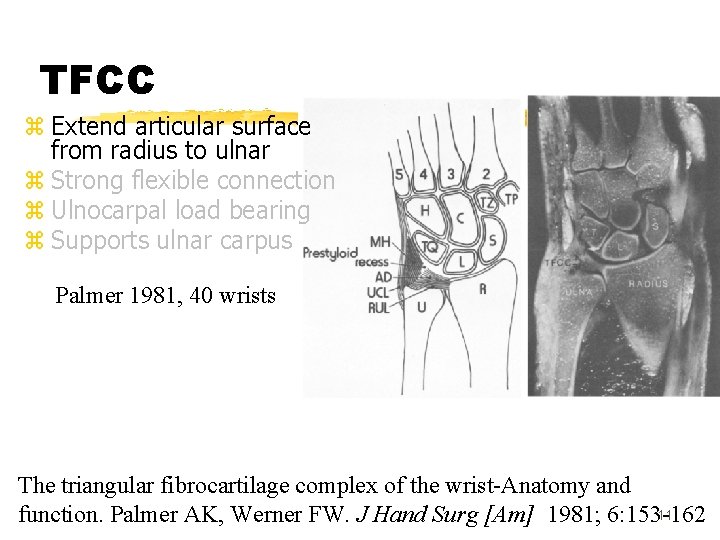
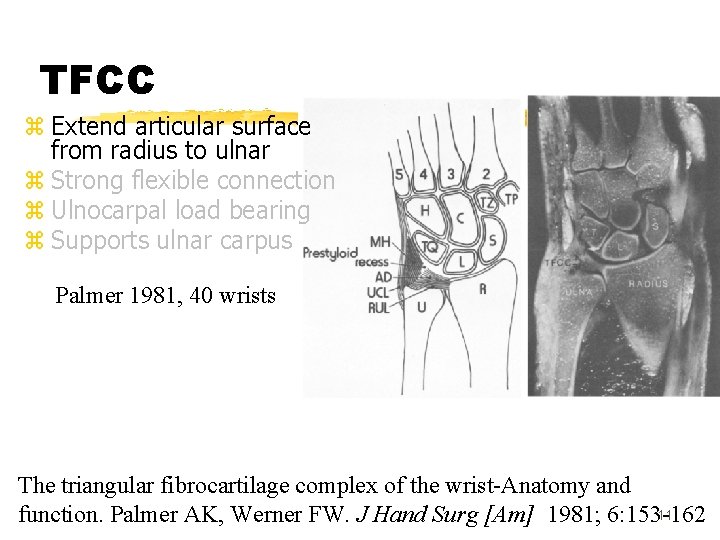
TFCC z Extend articular surface from radius to ulnar z Strong flexible connection z Ulnocarpal load bearing z Supports ulnar carpus Palmer 1981, 40 wrists The triangular fibrocartilage complex of the wrist-Anatomy and 11 function. Palmer AK, Werner FW. J Hand Surg [Am] 1981; 6: 153 -162
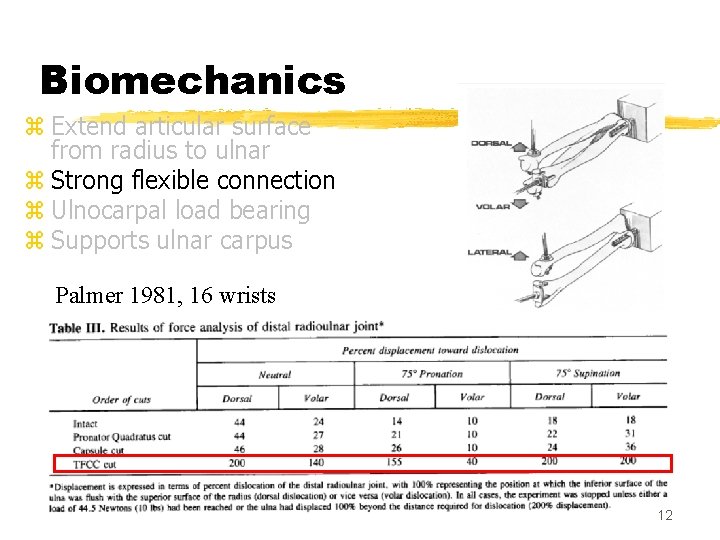
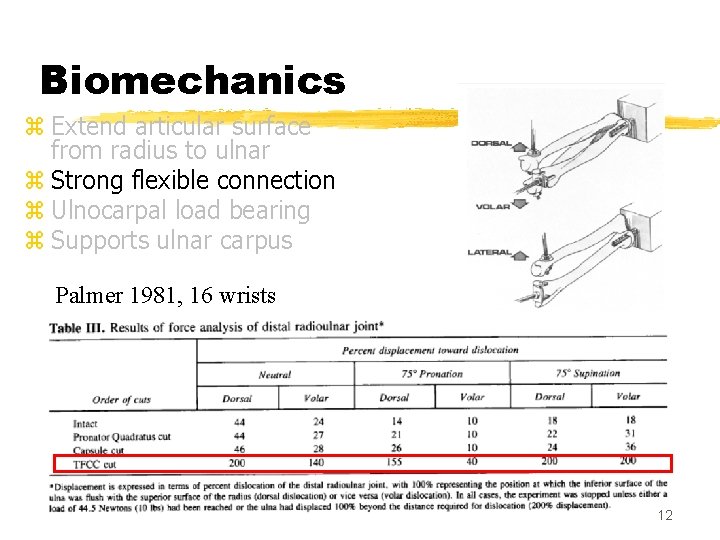
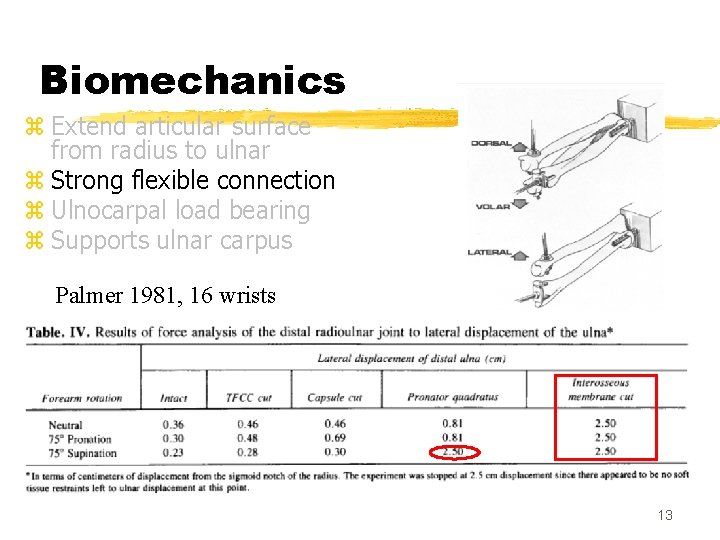
Biomechanics z Extend articular surface from radius to ulnar z Strong flexible connection z Ulnocarpal load bearing z Supports ulnar carpus Palmer 1981, 16 wrists 12
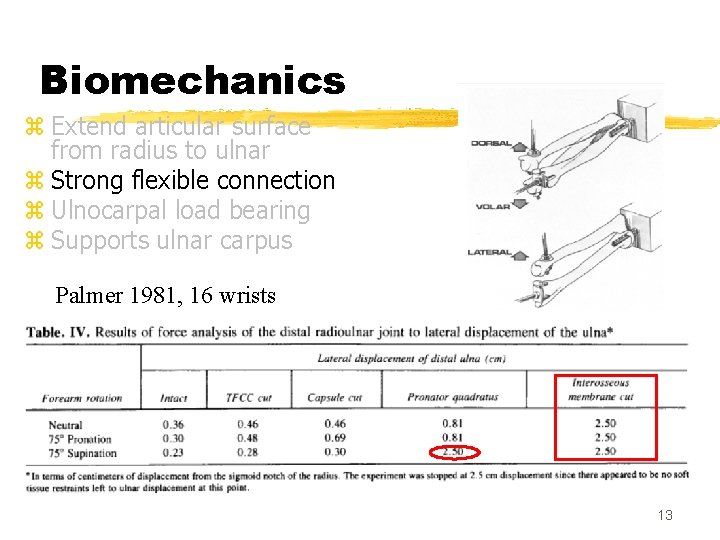
Biomechanics z Extend articular surface from radius to ulnar z Strong flexible connection z Ulnocarpal load bearing z Supports ulnar carpus Palmer 1981, 16 wrists 13
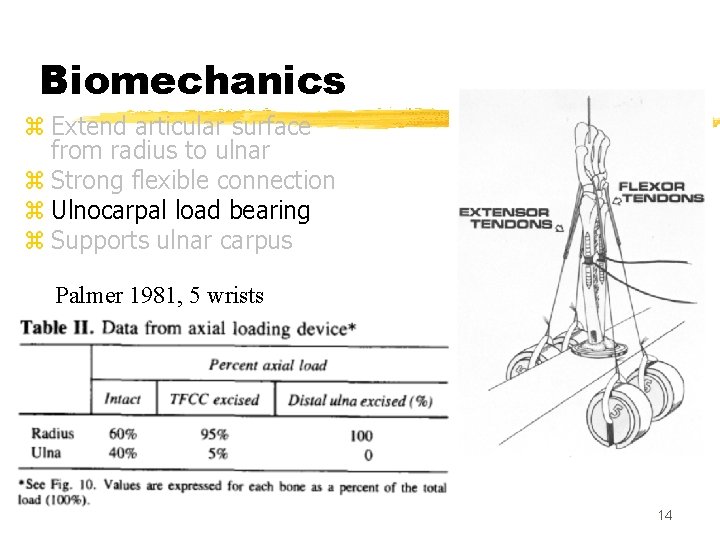
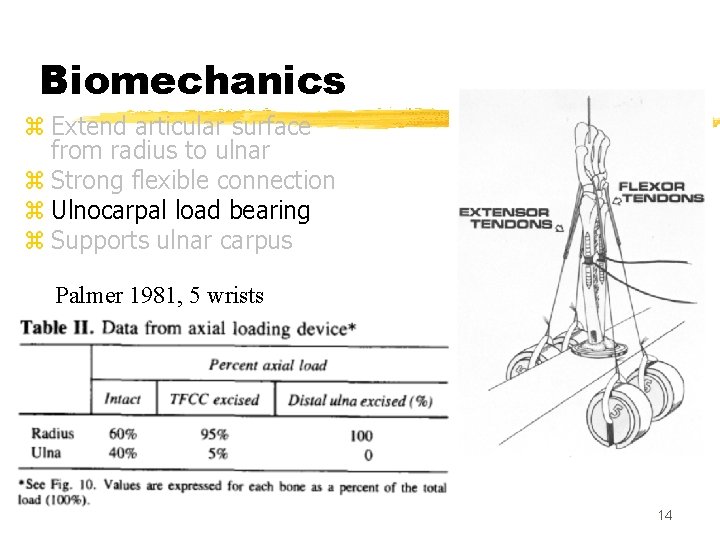
Biomechanics z Extend articular surface from radius to ulnar z Strong flexible connection z Ulnocarpal load bearing z Supports ulnar carpus Palmer 1981, 5 wrists 14
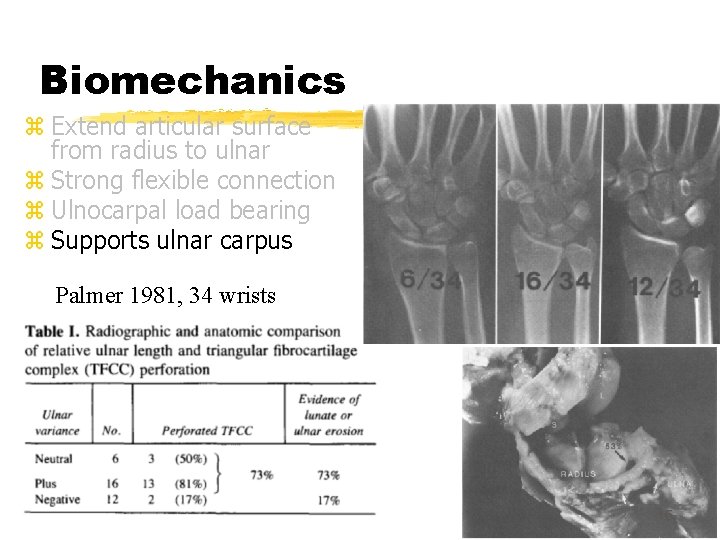
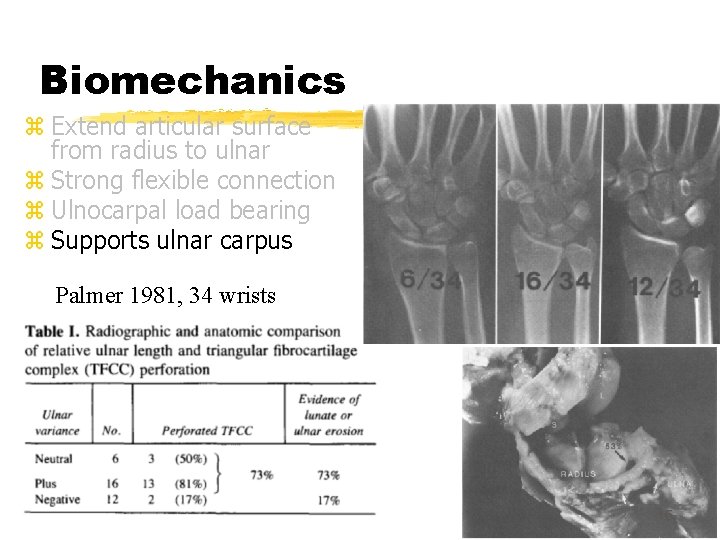
Biomechanics z Extend articular surface from radius to ulnar z Strong flexible connection z Ulnocarpal load bearing z Supports ulnar carpus Palmer 1981, 34 wrists 15
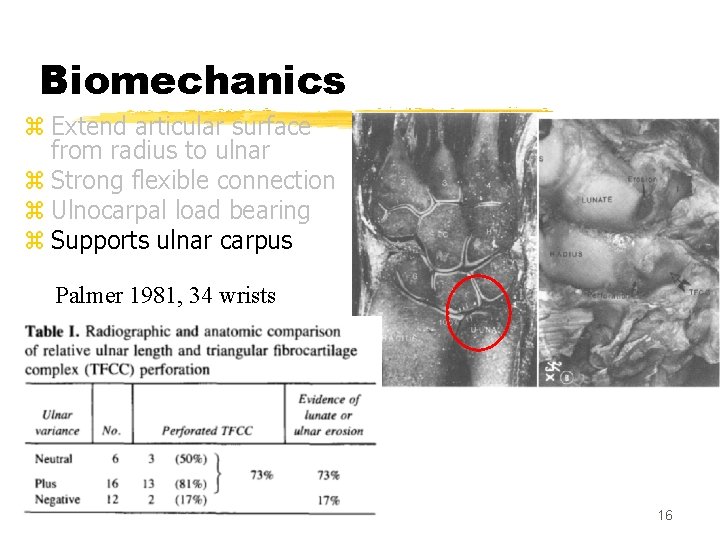
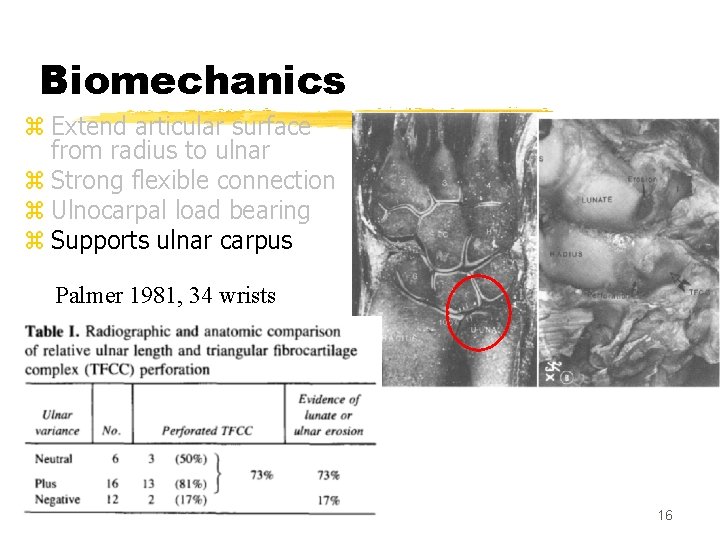
Biomechanics z Extend articular surface from radius to ulnar z Strong flexible connection z Ulnocarpal load bearing z Supports ulnar carpus Palmer 1981, 34 wrists 16
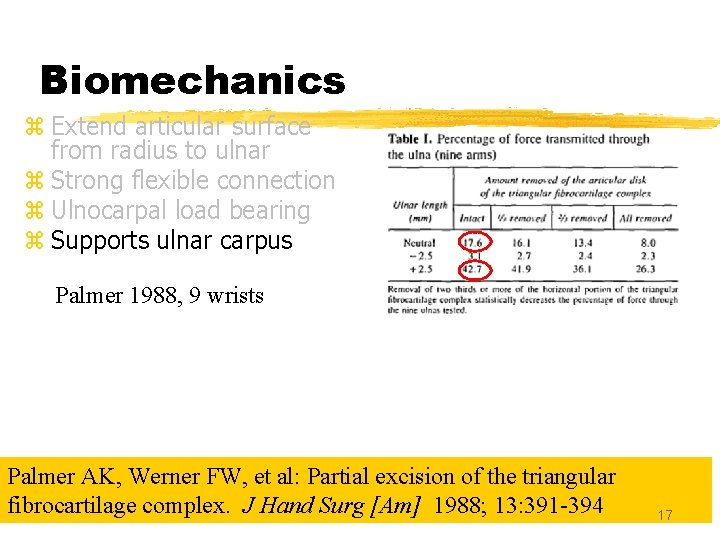
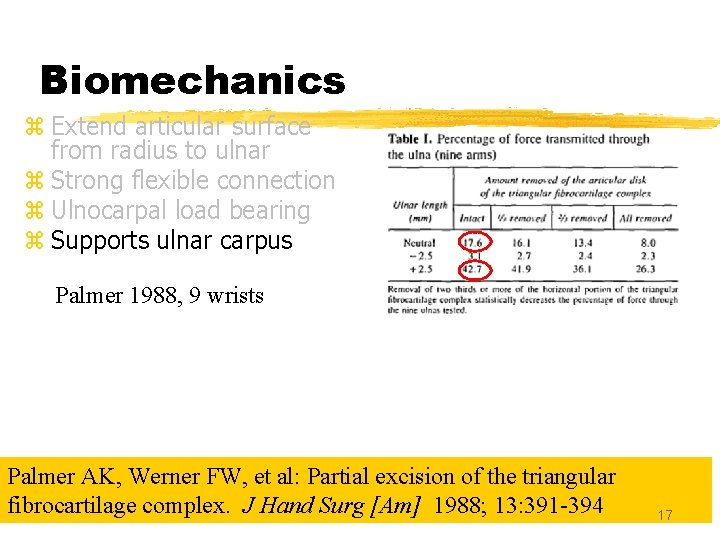
Biomechanics z Extend articular surface from radius to ulnar z Strong flexible connection z Ulnocarpal load bearing z Supports ulnar carpus Palmer 1988, 9 wrists Palmer AK, Werner FW, et al: Partial excision of the triangular fibrocartilage complex. J Hand Surg [Am] 1988; 13: 391 -394 17
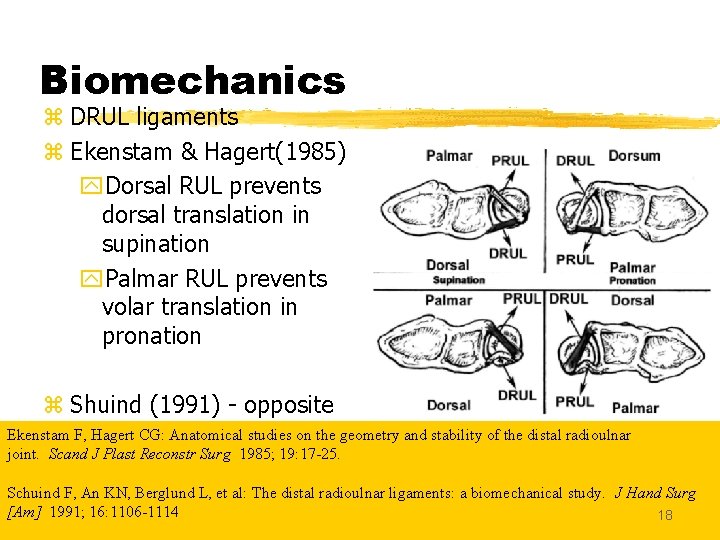
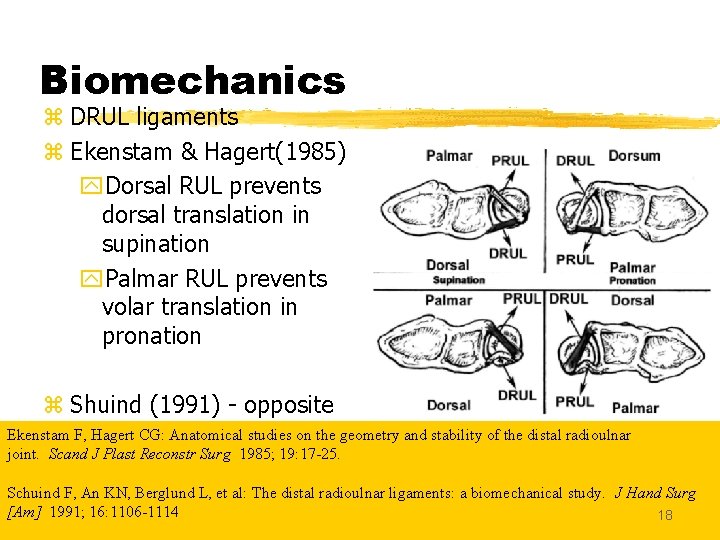
Biomechanics z DRUL ligaments z Ekenstam & Hagert(1985) y. Dorsal RUL prevents dorsal translation in supination y. Palmar RUL prevents volar translation in pronation z Shuind (1991) - opposite Ekenstam F, Hagert CG: Anatomical studies on the geometry and stability of the distal radioulnar joint. Scand J Plast Reconstr Surg 1985; 19: 17 -25. Schuind F, An KN, Berglund L, et al: The distal radioulnar ligaments: a biomechanical study. J Hand Surg [Am] 1991; 16: 1106 -1114 18
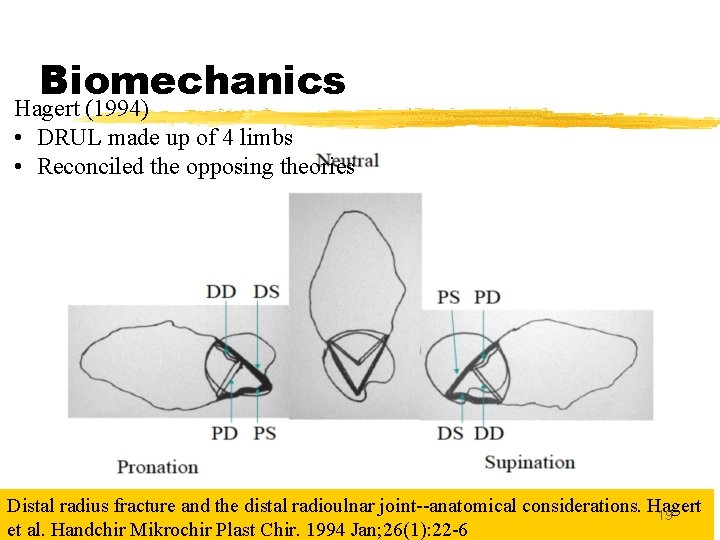
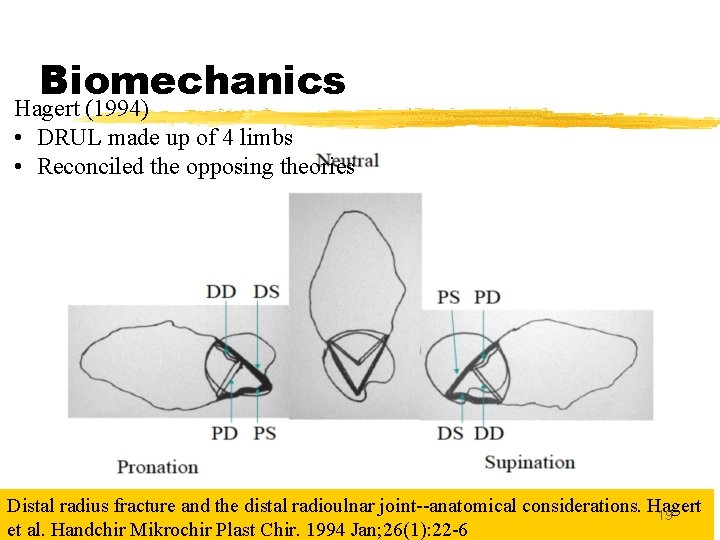
Biomechanics Hagert (1994) • DRUL made up of 4 limbs • Reconciled the opposing theories Distal radius fracture and the distal radioulnar joint--anatomical considerations. Hagert 19 et al. Handchir Mikrochir Plast Chir. 1994 Jan; 26(1): 22 -6
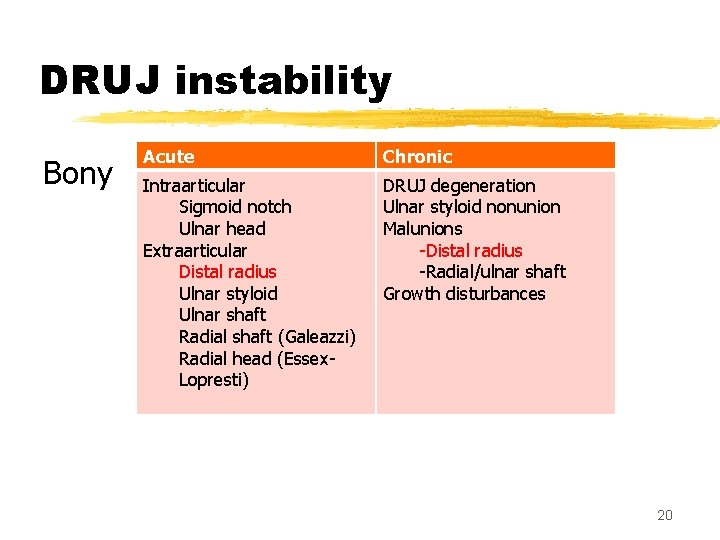
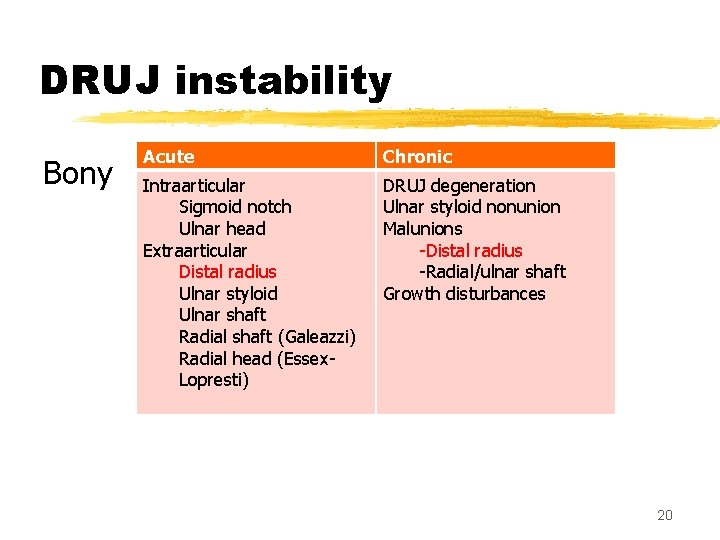
DRUJ instability Bony Acute Chronic Intraarticular Sigmoid notch Ulnar head Extraarticular Distal radius Ulnar styloid Ulnar shaft Radial shaft (Galeazzi) Radial head (Essex. Lopresti) DRUJ degeneration Ulnar styloid nonunion Malunions -Distal radius -Radial/ulnar shaft Growth disturbances 20
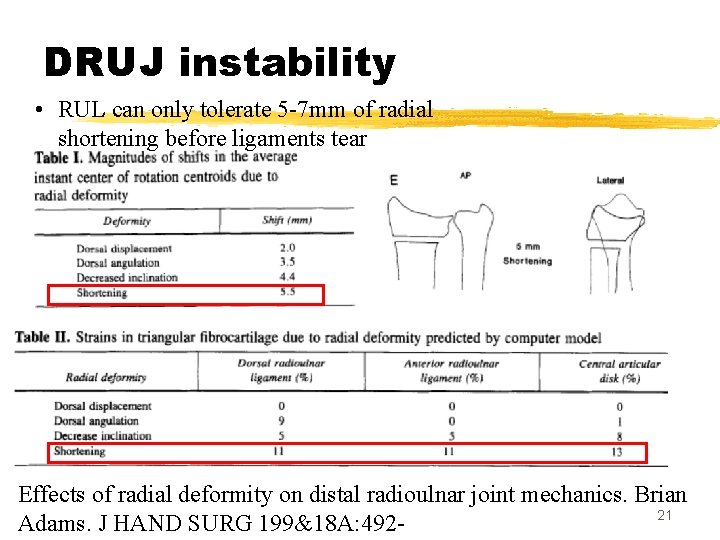
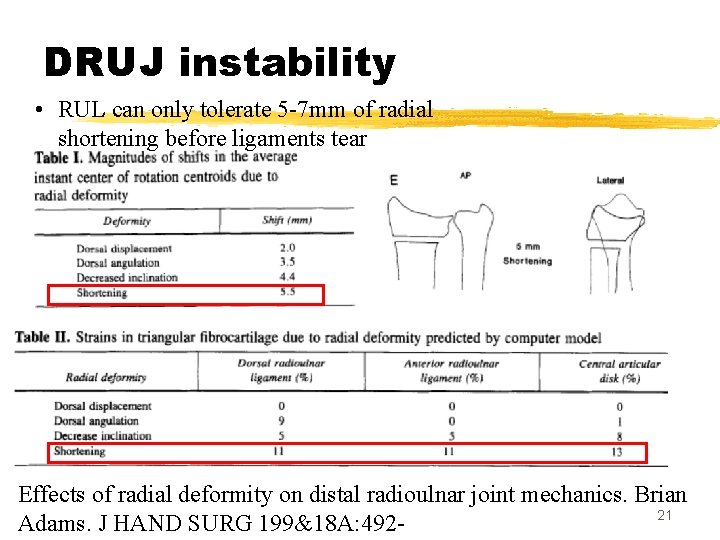
DRUJ instability • RUL can only tolerate 5 -7 mm of radial shortening before ligaments tear Effects of radial deformity on distal radioulnar joint mechanics. Brian 21 Adams. J HAND SURG 199&18 A: 492 -
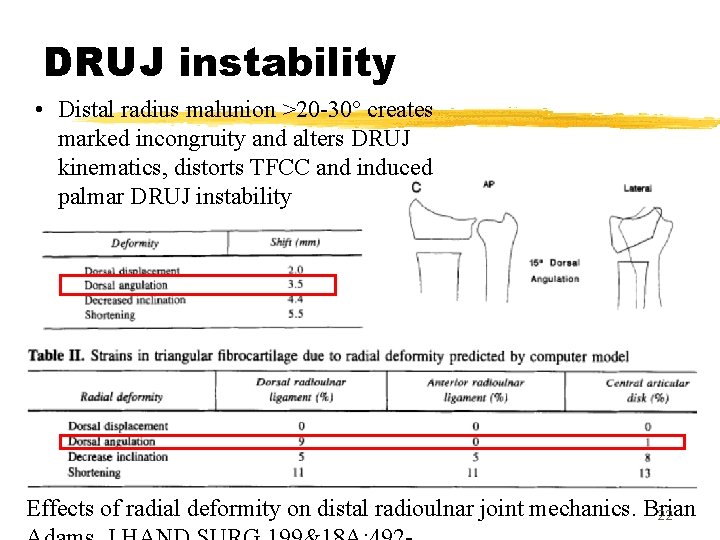
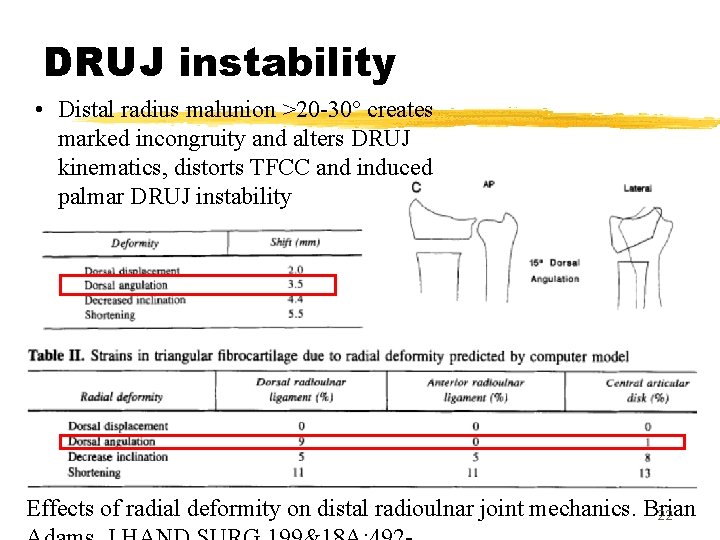
DRUJ instability • Distal radius malunion >20 -30° creates marked incongruity and alters DRUJ kinematics, distorts TFCC and induced palmar DRUJ instability Effects of radial deformity on distal radioulnar joint mechanics. Brian 22
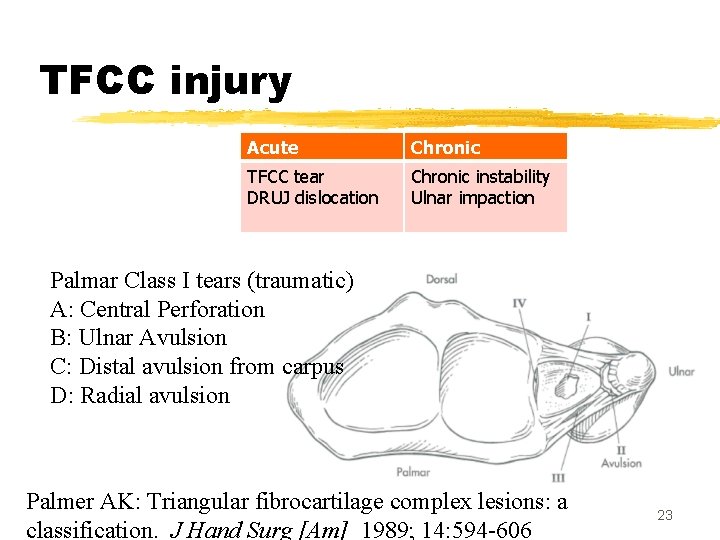
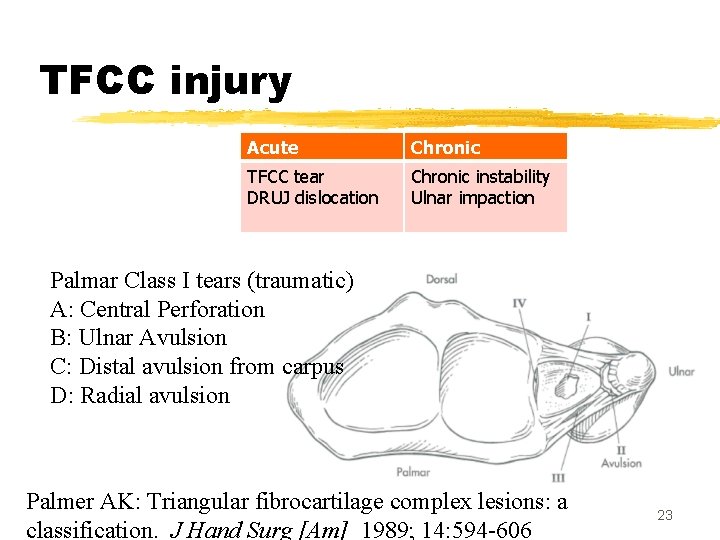
TFCC injury Acute Chronic TFCC tear DRUJ dislocation Chronic instability Ulnar impaction Palmar Class I tears (traumatic) A: Central Perforation B: Ulnar Avulsion C: Distal avulsion from carpus D: Radial avulsion Palmer AK: Triangular fibrocartilage complex lesions: a classification. J Hand Surg [Am] 1989; 14: 594 -606 23
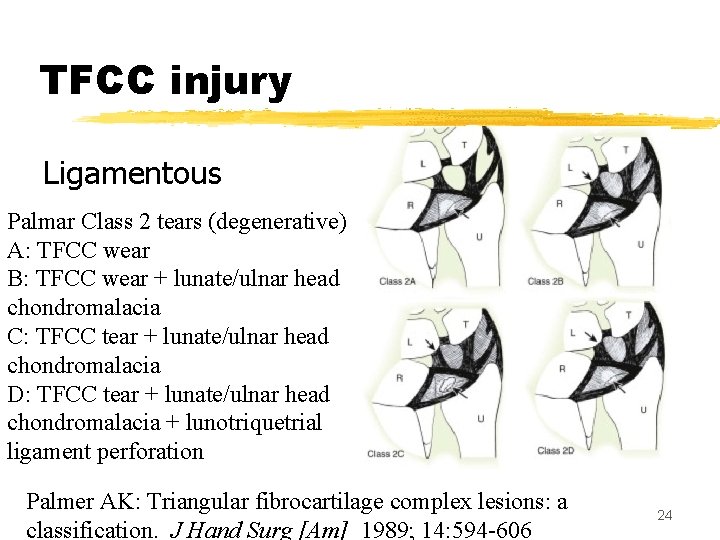
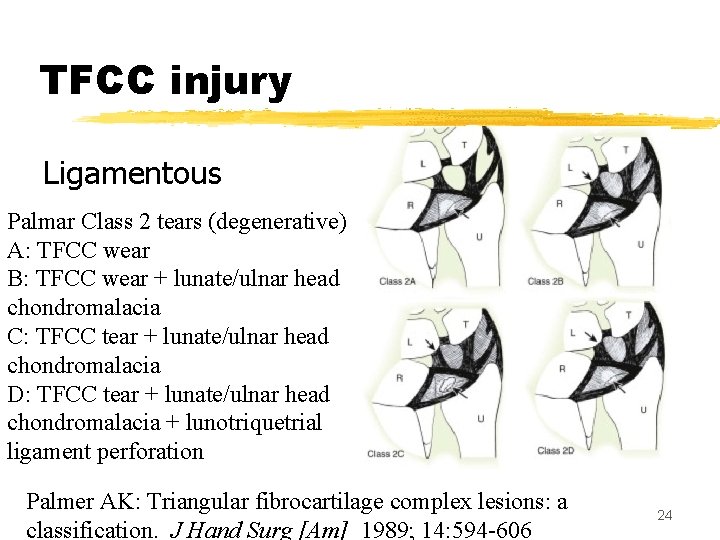
TFCC injury Ligamentous Palmar Class 2 tears (degenerative) A: TFCC wear B: TFCC wear + lunate/ulnar head chondromalacia C: TFCC tear + lunate/ulnar head chondromalacia D: TFCC tear + lunate/ulnar head chondromalacia + lunotriquetrial ligament perforation Palmer AK: Triangular fibrocartilage complex lesions: a classification. J Hand Surg [Am] 1989; 14: 594 -606 24
Examination z. Careful guided history-taking z. Observation z. Palpation z. ROM z. Specific tests z. Eliminate other causes of ulnar wrist pain z. Grip strength z. Compare with normal side 25
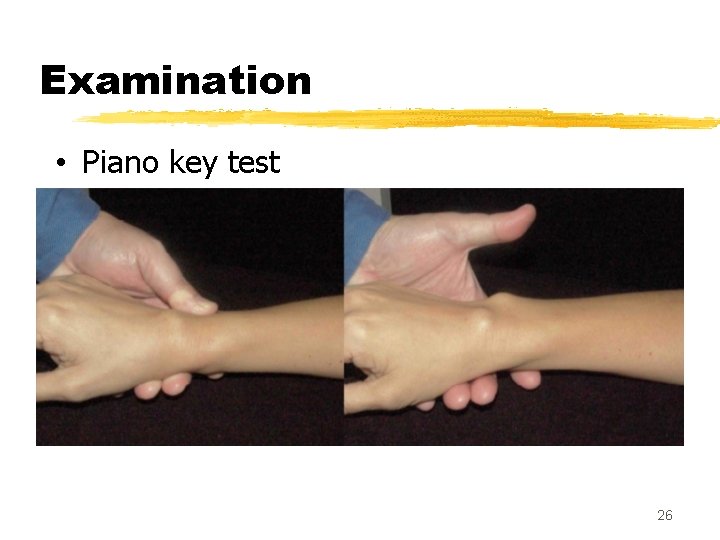
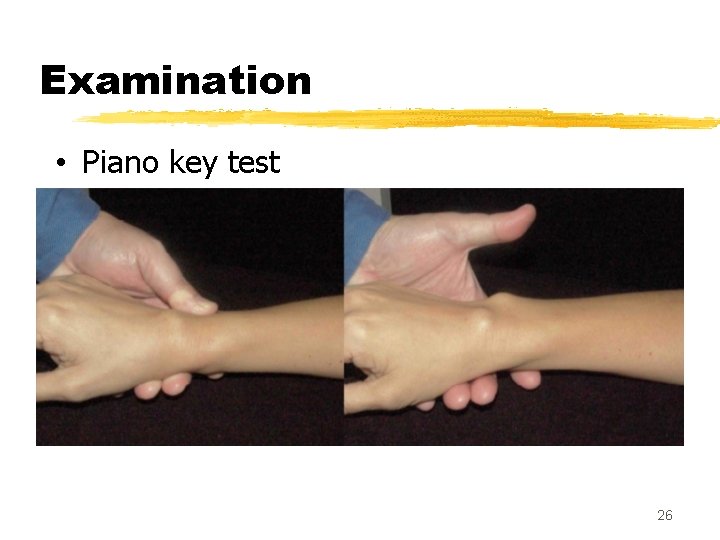
Examination • Piano key test 26
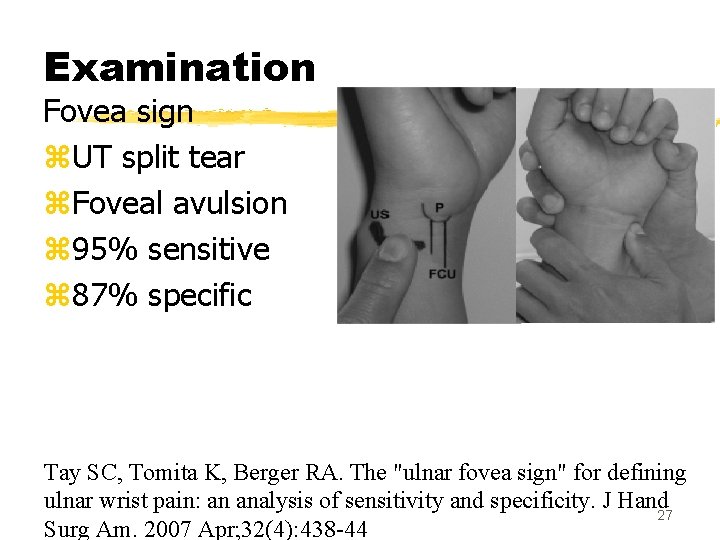
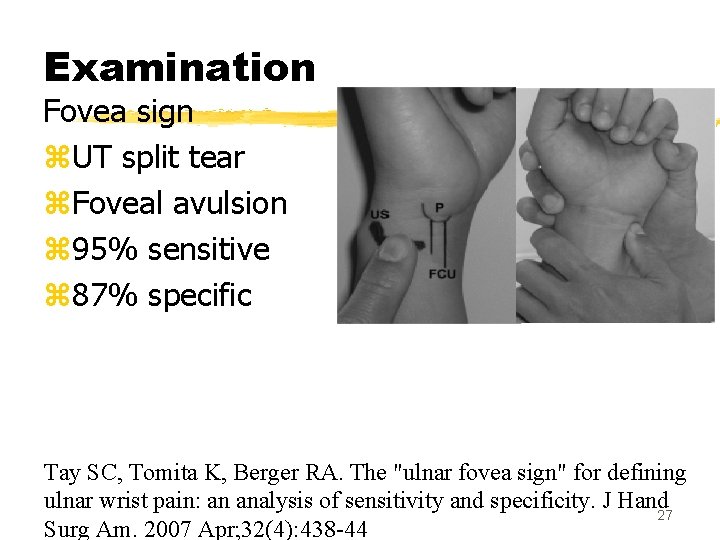
Examination Fovea sign z. UT split tear z. Foveal avulsion z 95% sensitive z 87% specific Tay SC, Tomita K, Berger RA. The "ulnar fovea sign" for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand 27 Surg Am. 2007 Apr; 32(4): 438 -44
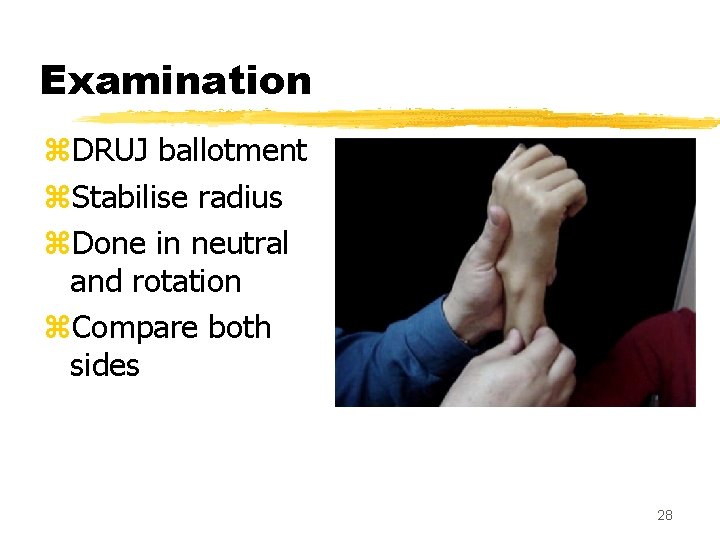
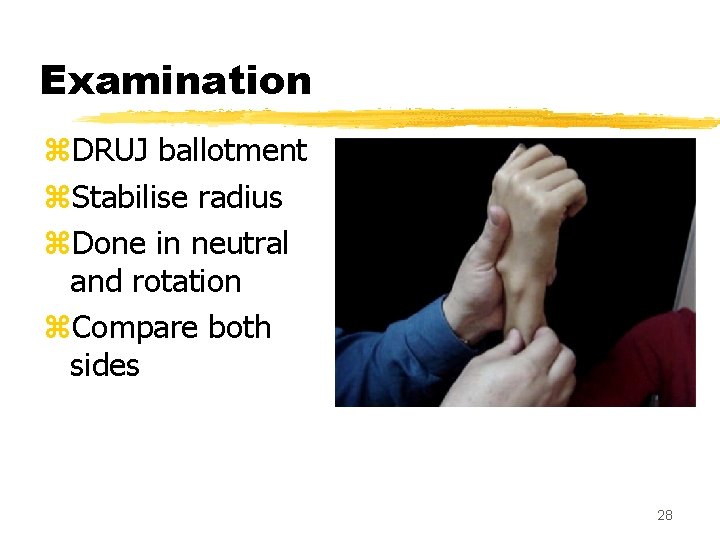
Examination z. DRUJ ballotment z. Stabilise radius z. Done in neutral and rotation z. Compare both sides 28
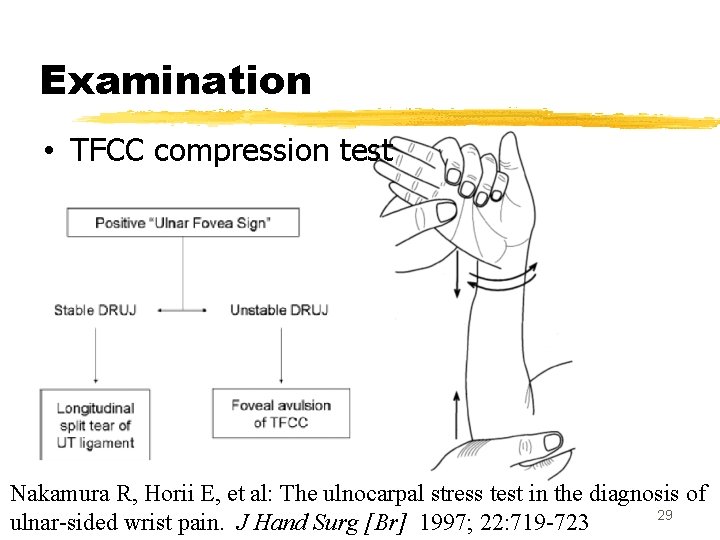
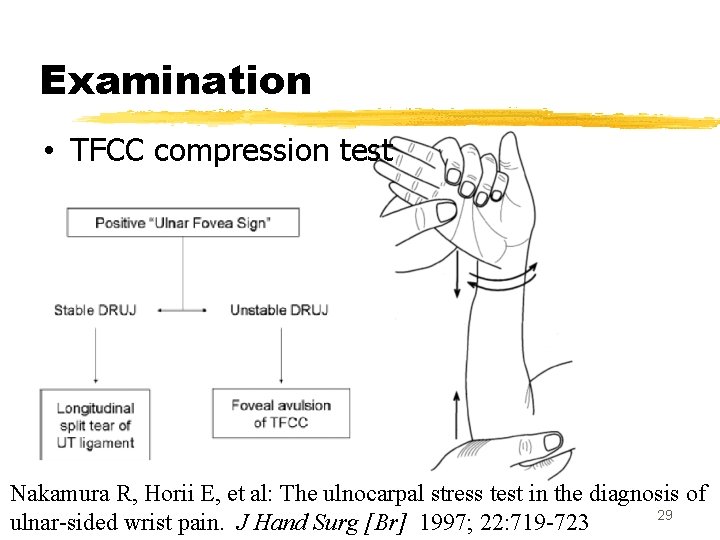
Examination • TFCC compression test Nakamura R, Horii E, et al: The ulnocarpal stress test in the diagnosis of 29 ulnar-sided wrist pain. J Hand Surg [Br] 1997; 22: 719 -723
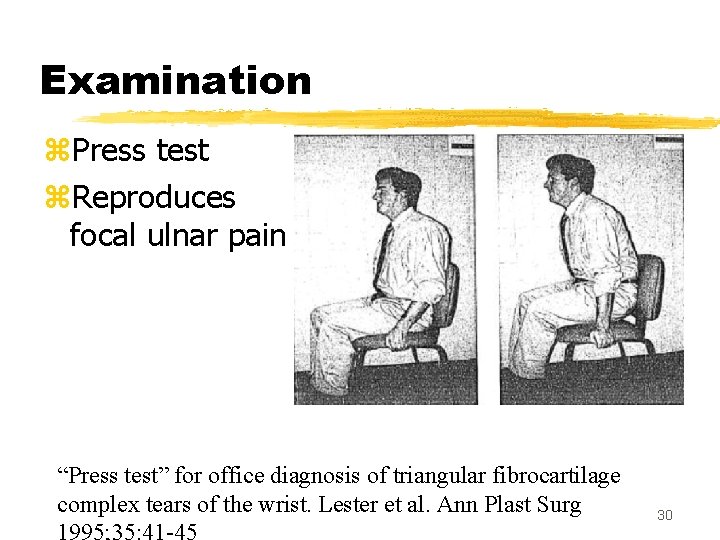
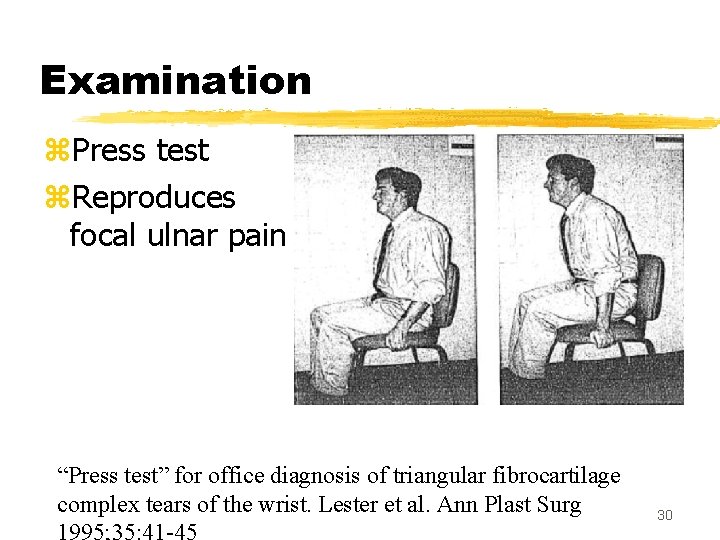
Examination z. Press test z. Reproduces focal ulnar pain “Press test” for office diagnosis of triangular fibrocartilage complex tears of the wrist. Lester et al. Ann Plast Surg 30
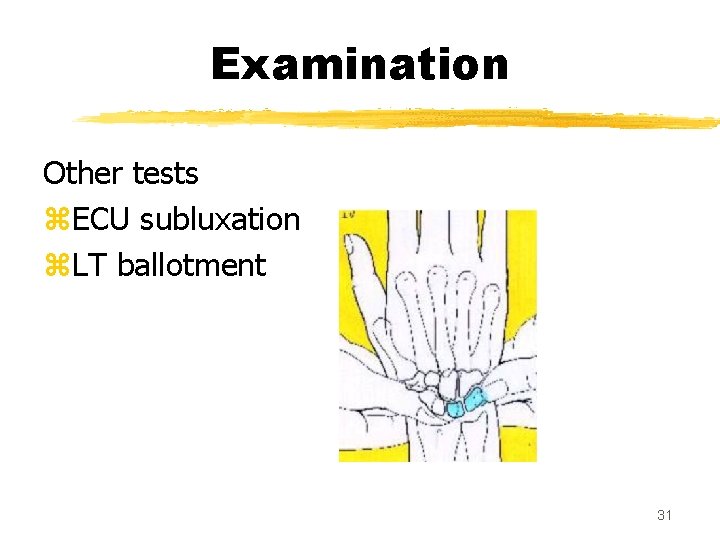
Examination Other tests z. ECU subluxation z. LT ballotment 31
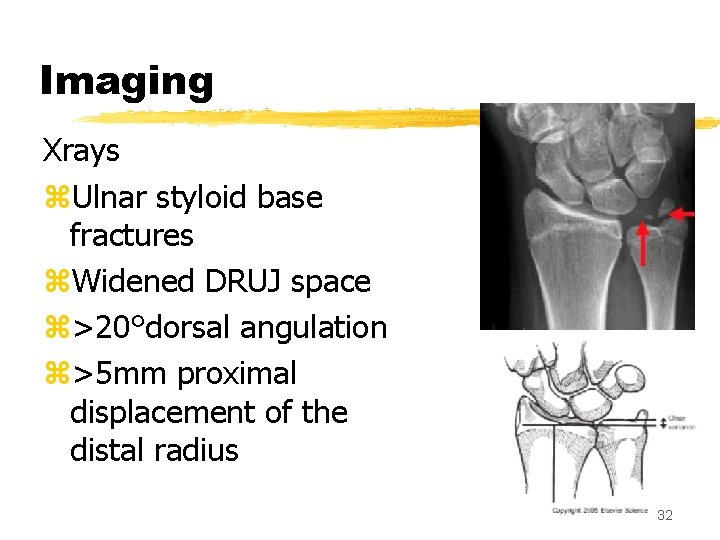
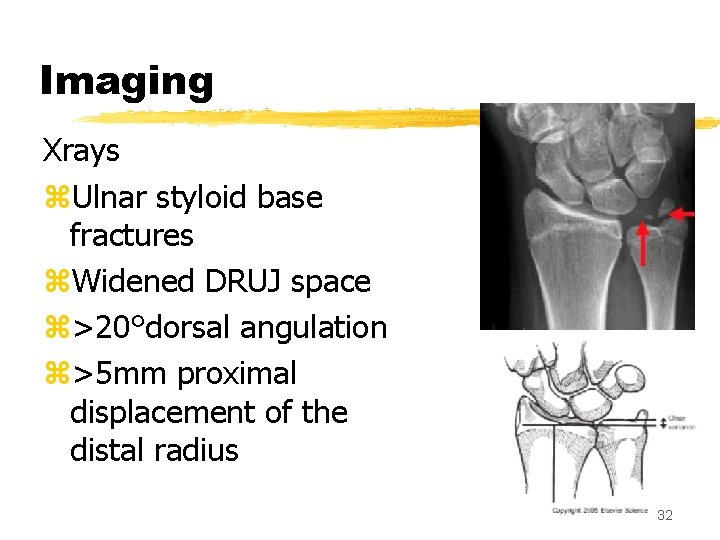
Imaging Xrays z. Ulnar styloid base fractures z. Widened DRUJ space z>20°dorsal angulation z>5 mm proximal displacement of the distal radius 32
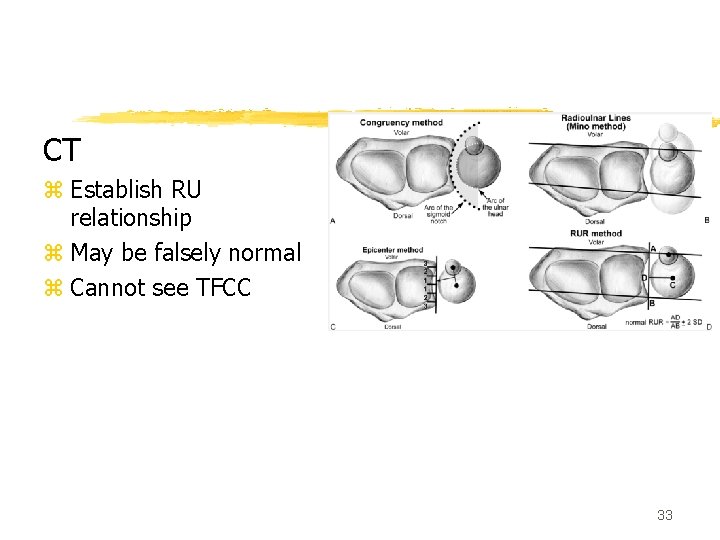
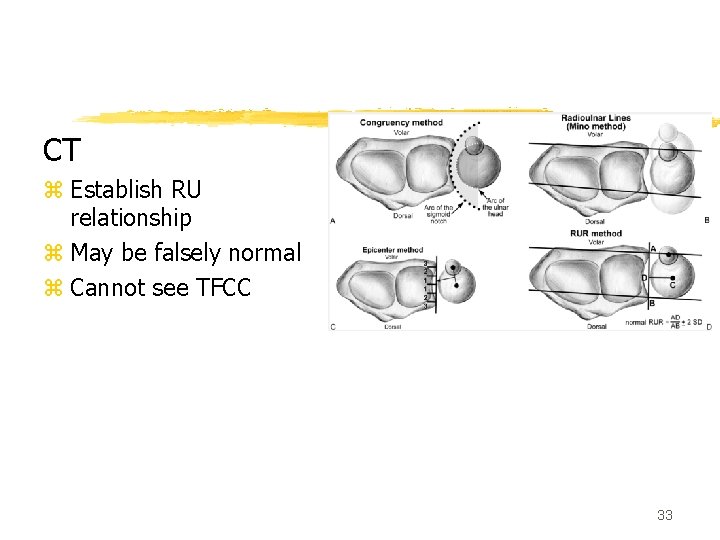
CT z Establish RU relationship z May be falsely normal z Cannot see TFCC 33
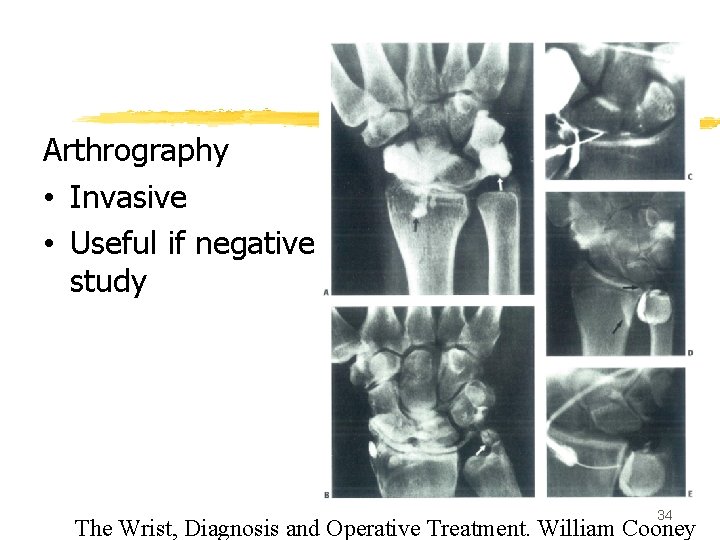
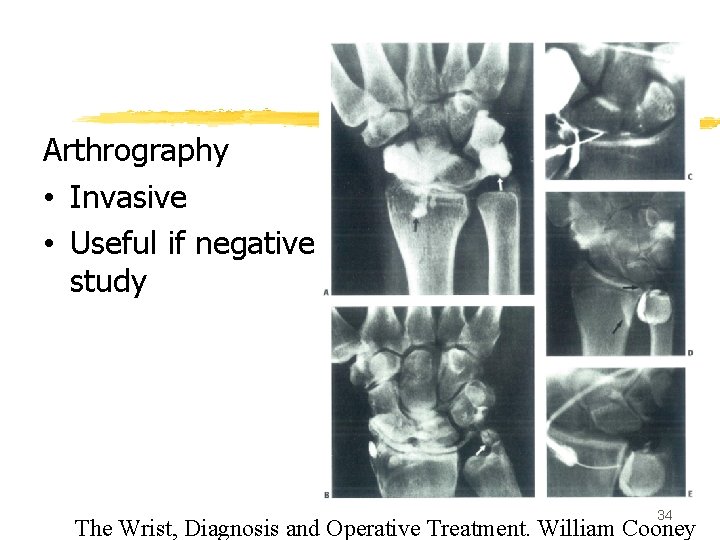
Arthrography • Invasive • Useful if negative study 34 The Wrist, Diagnosis and Operative Treatment. William Cooney
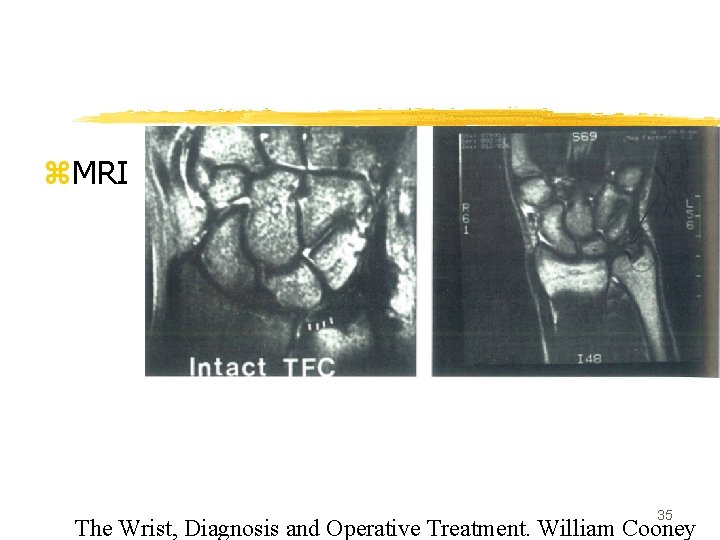
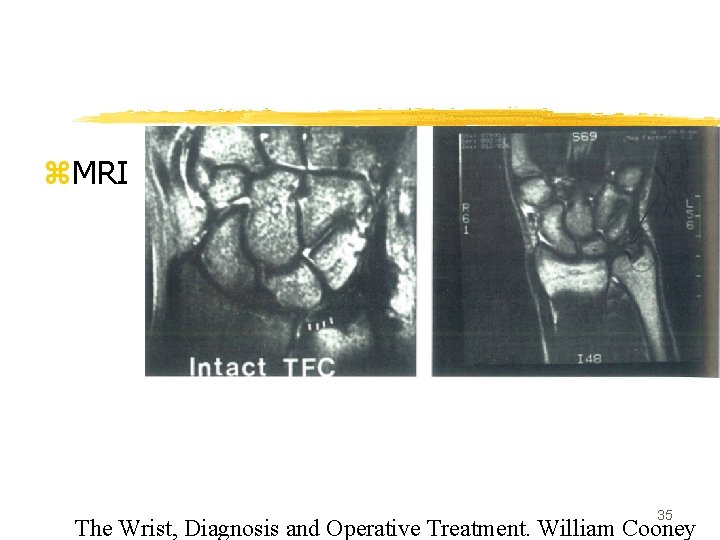
z. MRI 35 The Wrist, Diagnosis and Operative Treatment. William Cooney
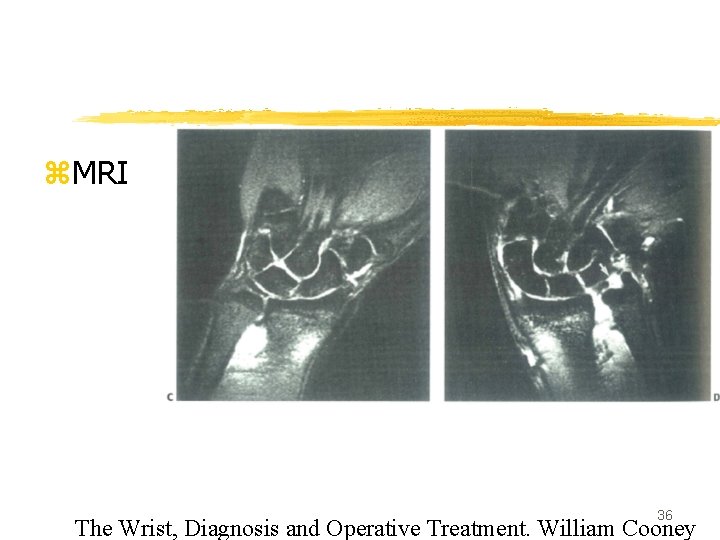
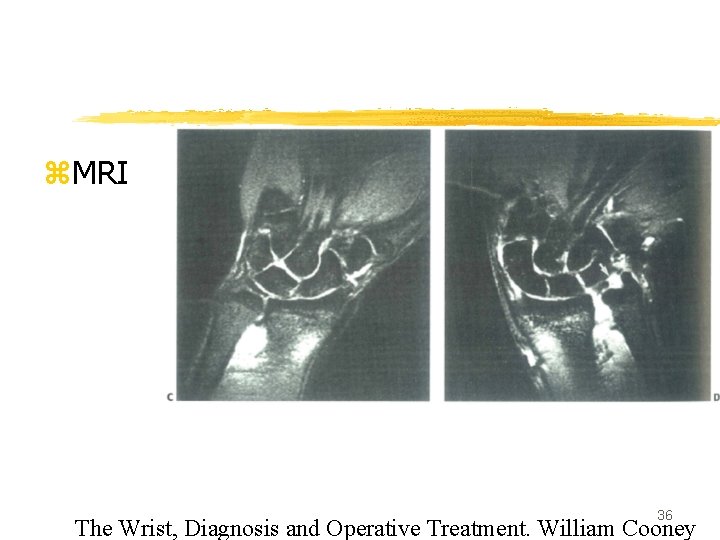
z. MRI 36 The Wrist, Diagnosis and Operative Treatment. William Cooney
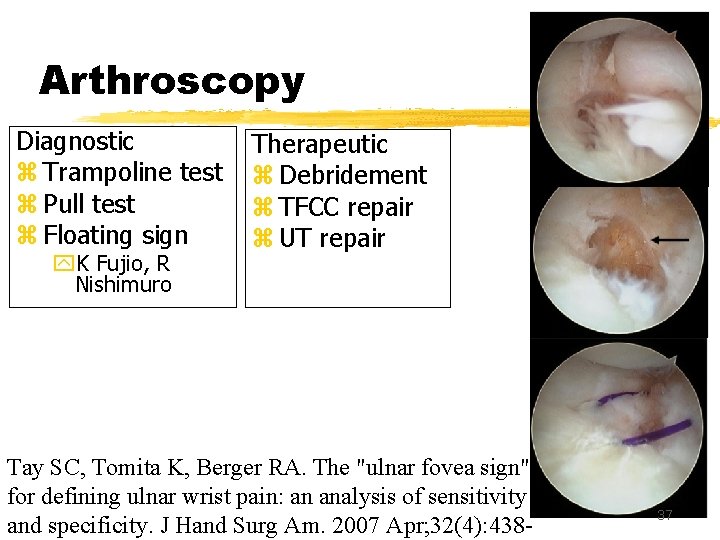
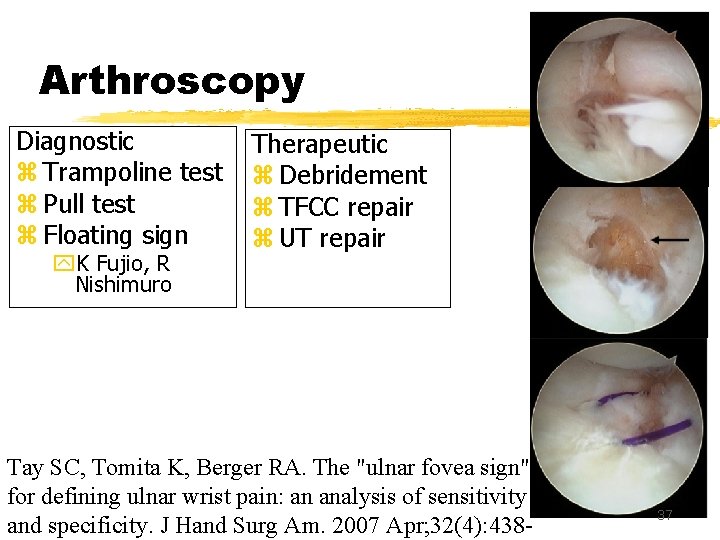
Arthroscopy Diagnostic z Trampoline test z Pull test z Floating sign y. K Fujio, R Nishimuro Therapeutic z Debridement z TFCC repair z UT repair Tay SC, Tomita K, Berger RA. The "ulnar fovea sign" for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg Am. 2007 Apr; 32(4): 438 - 37
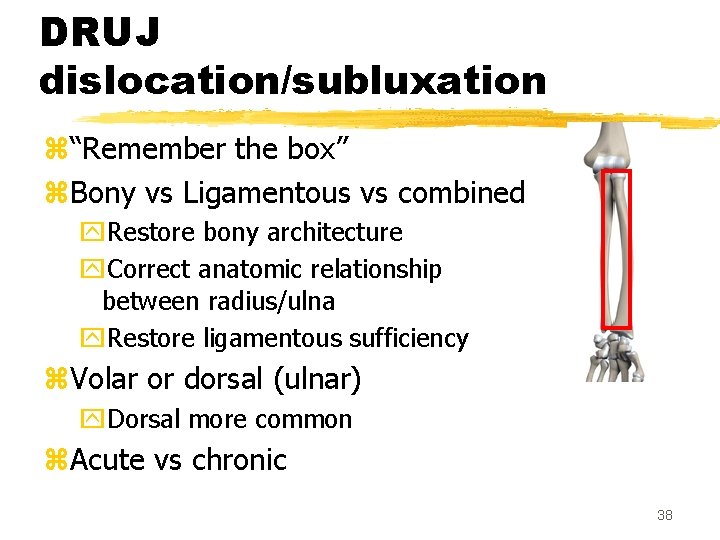
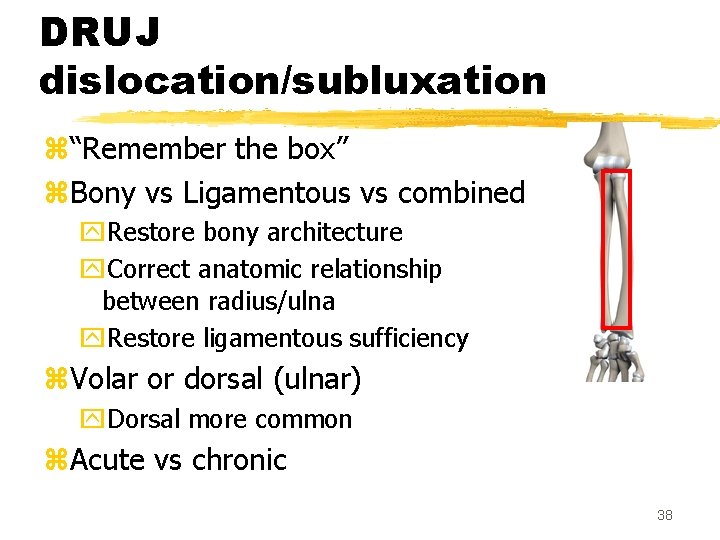
DRUJ dislocation/subluxation z“Remember the box” z. Bony vs Ligamentous vs combined y. Restore bony architecture y. Correct anatomic relationship between radius/ulna y. Restore ligamentous sufficiency z. Volar or dorsal (ulnar) y. Dorsal more common z. Acute vs chronic 38
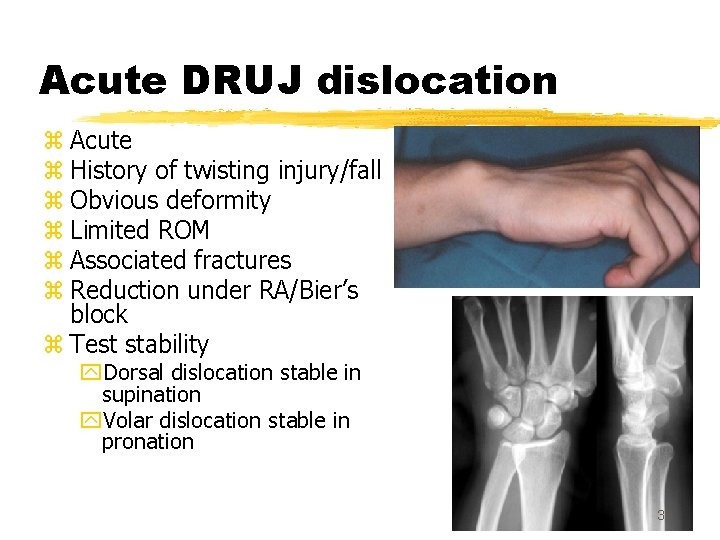
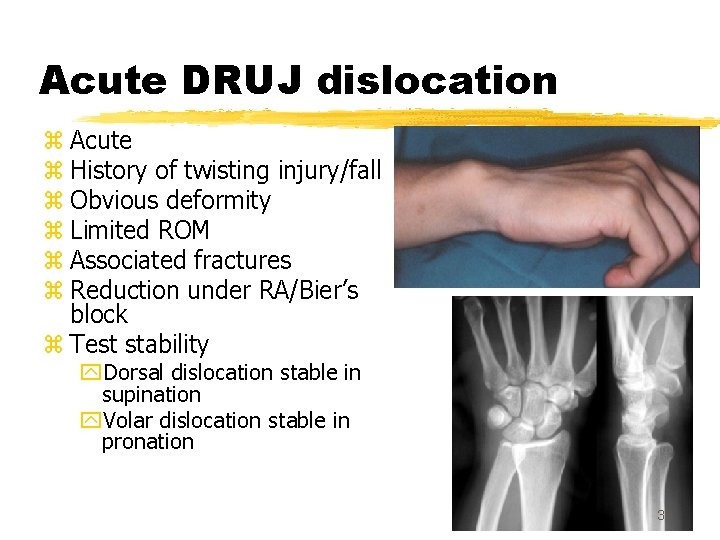
Acute DRUJ dislocation z Acute z History of twisting injury/fall z Obvious deformity z Limited ROM z Associated fractures z Reduction under RA/Bier’s block z Test stability y. Dorsal dislocation stable in supination y. Volar dislocation stable in pronation 39
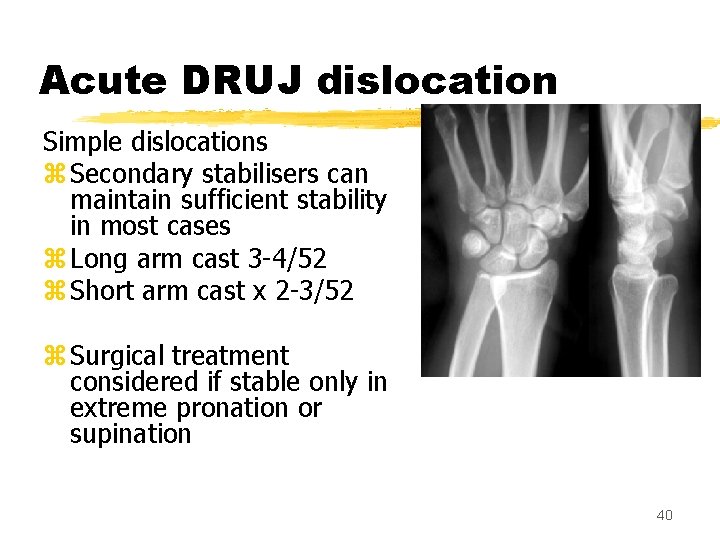
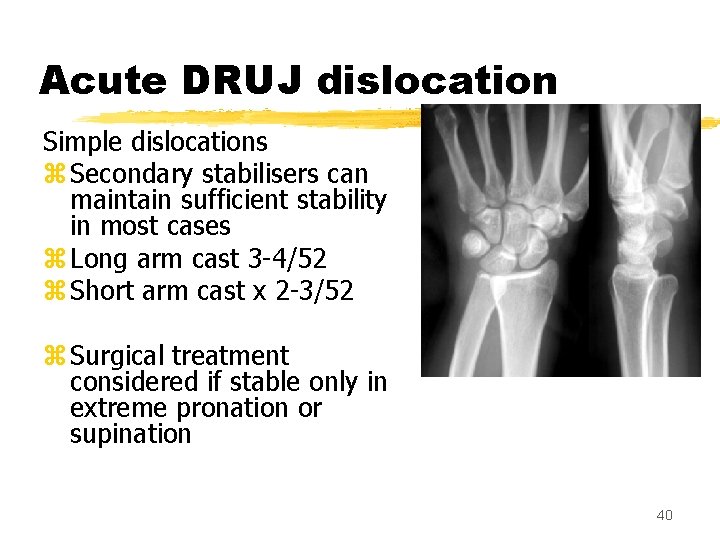
Acute DRUJ dislocation Simple dislocations z Secondary stabilisers can maintain sufficient stability in most cases z Long arm cast 3 -4/52 z Short arm cast x 2 -3/52 z Surgical treatment considered if stable only in extreme pronation or supination 40
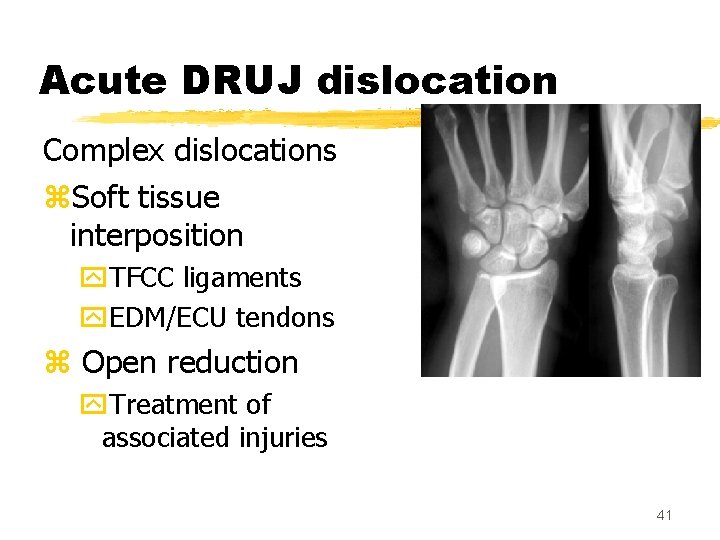
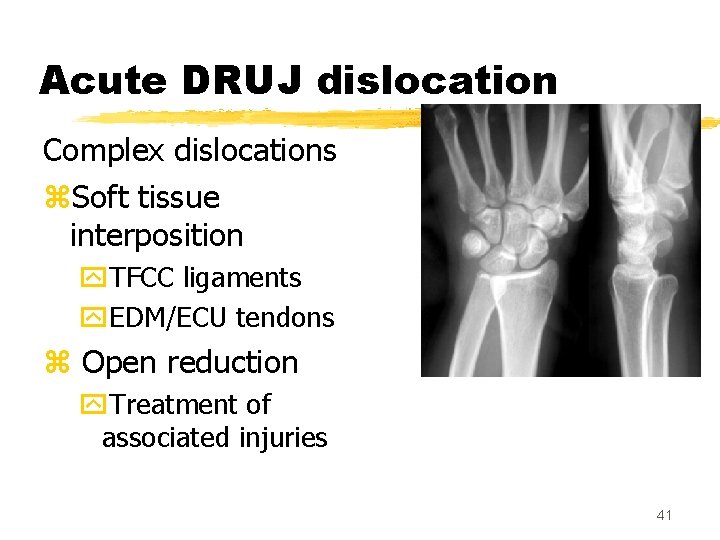
Acute DRUJ dislocation Complex dislocations z. Soft tissue interposition y. TFCC ligaments y. EDM/ECU tendons z Open reduction y. Treatment of associated injuries 41
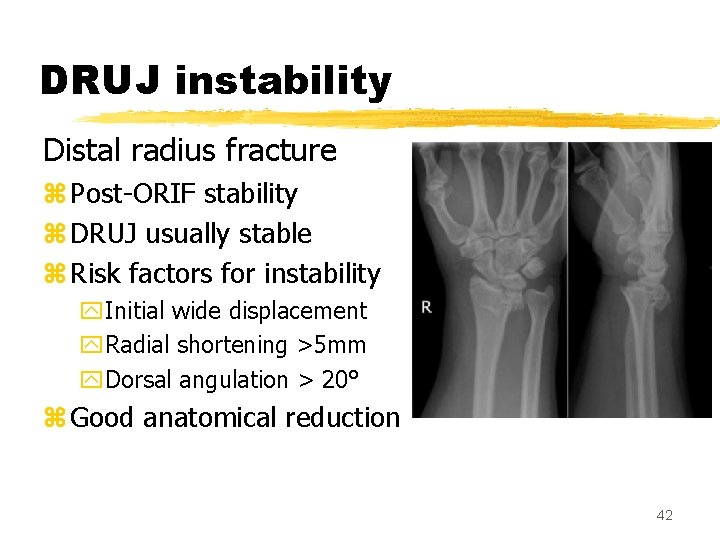
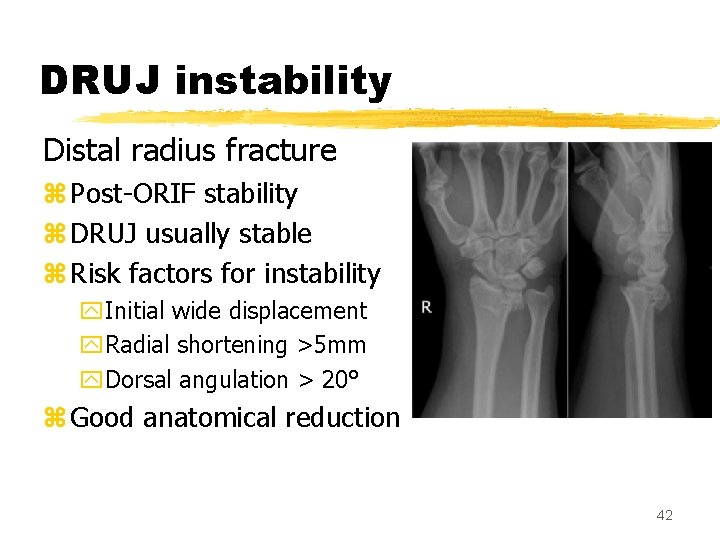
DRUJ instability Distal radius fracture z Post-ORIF stability z DRUJ usually stable z Risk factors for instability y. Initial wide displacement y. Radial shortening >5 mm y. Dorsal angulation > 20° z Good anatomical reduction 42
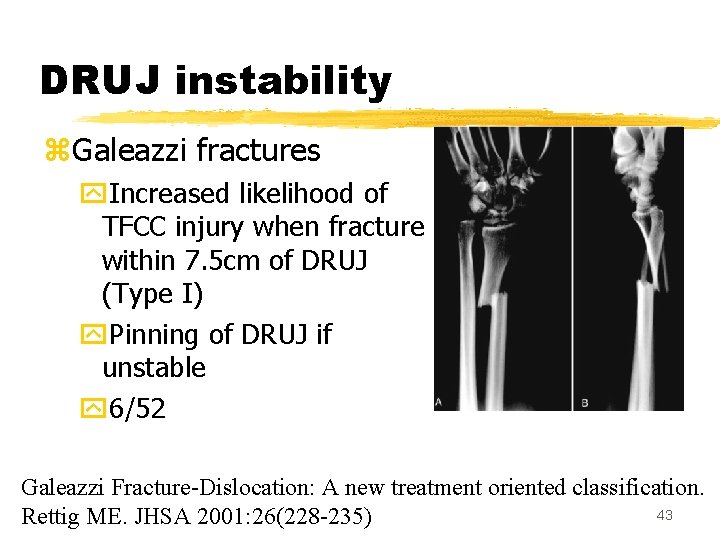
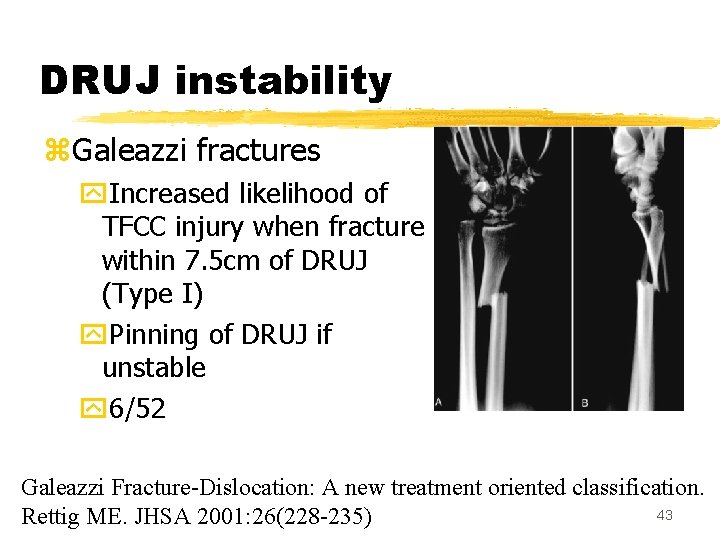
DRUJ instability z. Galeazzi fractures y. Increased likelihood of TFCC injury when fracture within 7. 5 cm of DRUJ (Type I) y. Pinning of DRUJ if unstable y 6/52 Galeazzi Fracture-Dislocation: A new treatment oriented classification. 43 Rettig ME. JHSA 2001: 26(228 -235)
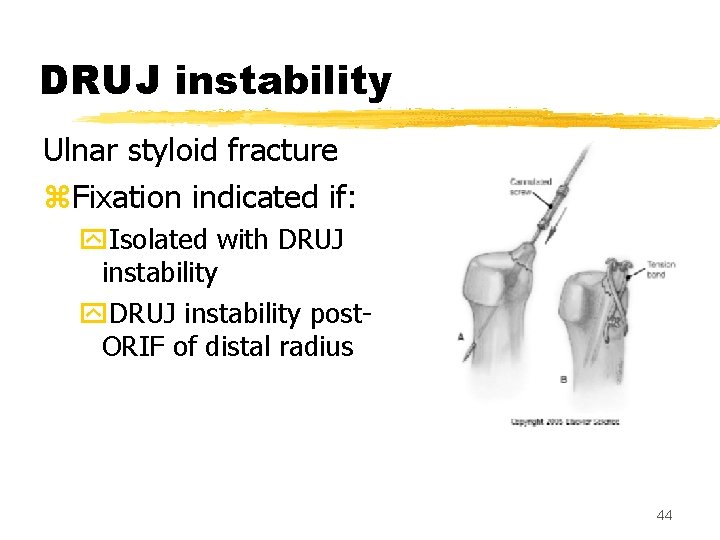
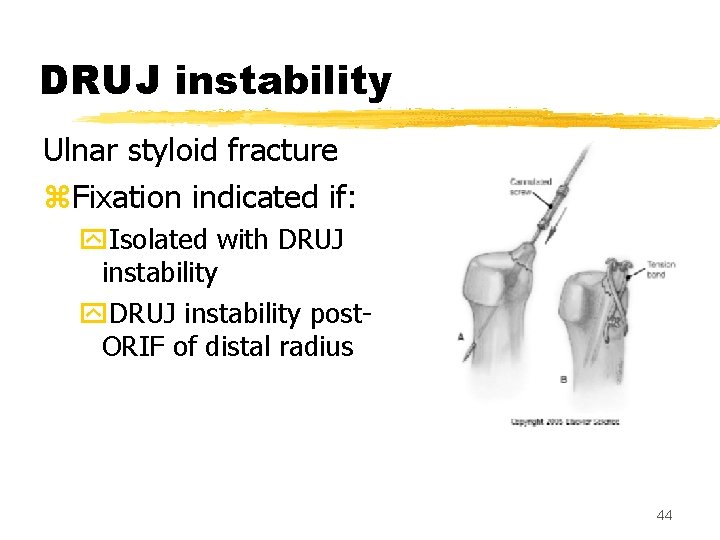
DRUJ instability Ulnar styloid fracture z. Fixation indicated if: y. Isolated with DRUJ instability y. DRUJ instability post. ORIF of distal radius 44
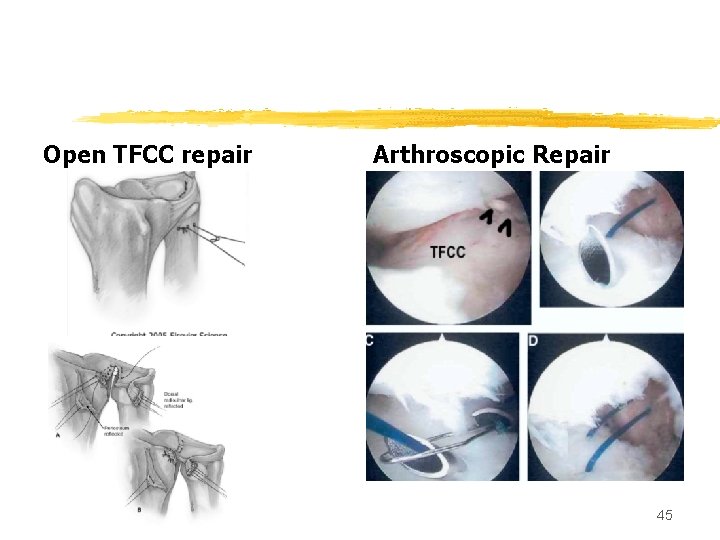
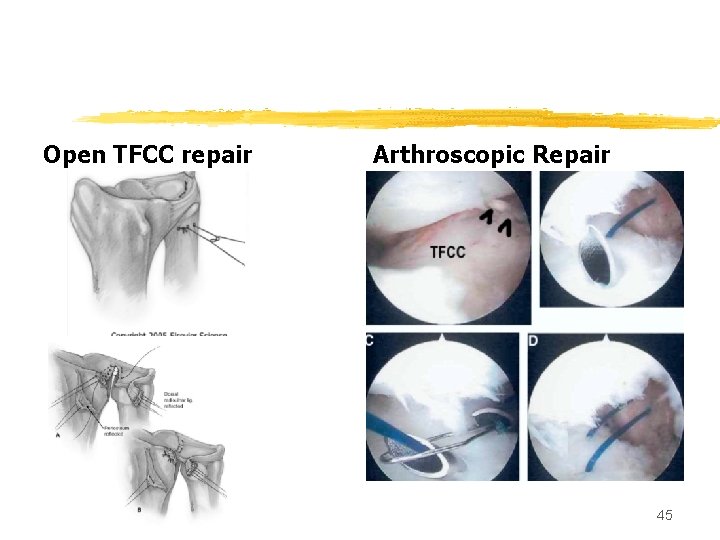
Open TFCC repair Arthroscopic Repair 45
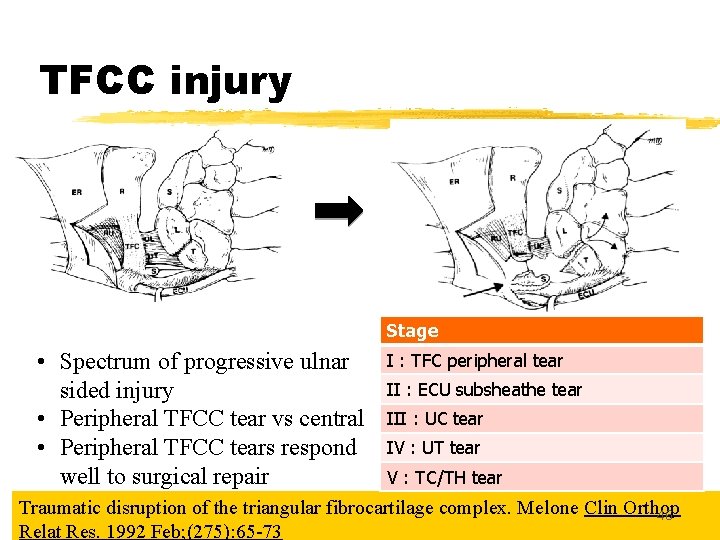
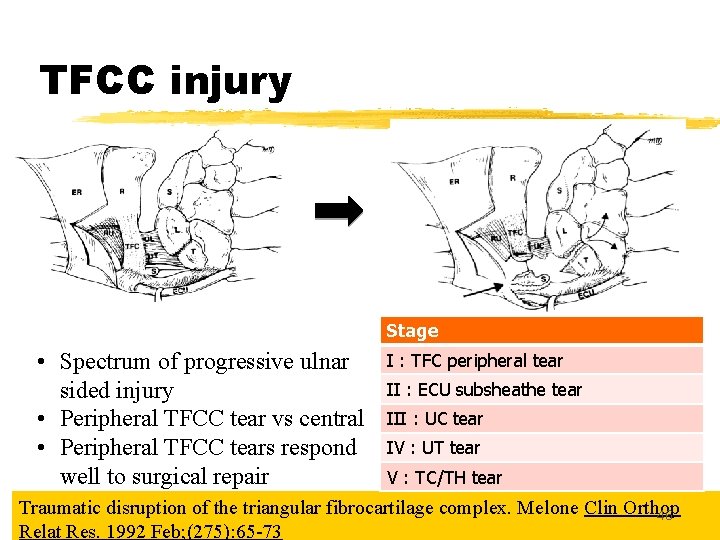
TFCC injury Stage • Spectrum of progressive ulnar sided injury • Peripheral TFCC tear vs central • Peripheral TFCC tears respond well to surgical repair I : TFC peripheral tear II : ECU subsheathe tear III : UC tear IV : UT tear V : TC/TH tear Traumatic disruption of the triangular fibrocartilage complex. Melone Clin Orthop 46 Relat Res. 1992 Feb; (275): 65 -73
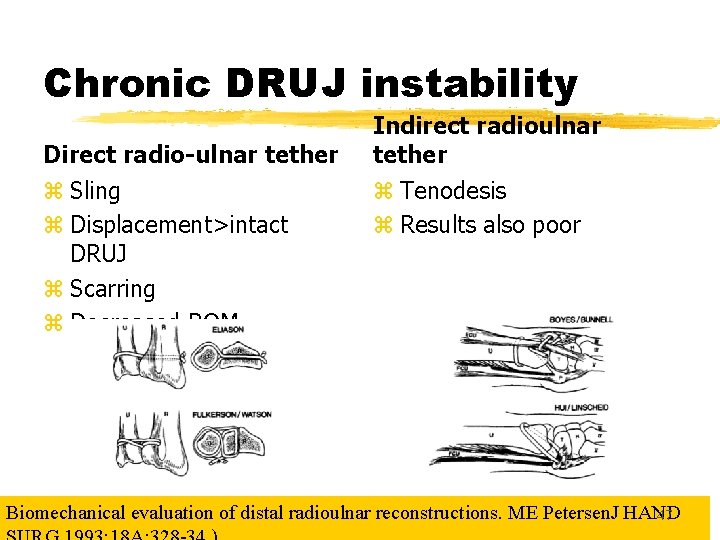
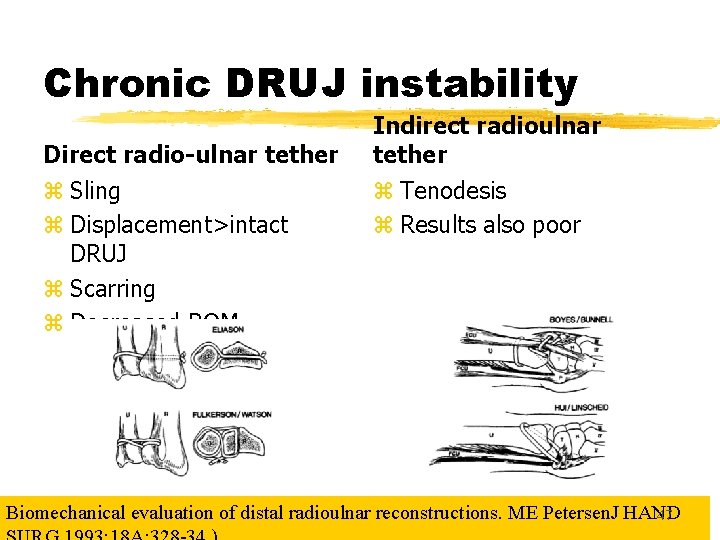
Chronic DRUJ instability Direct radio-ulnar tether z Sling z Displacement>intact DRUJ z Scarring z Decreased ROM Indirect radioulnar tether z Tenodesis z Results also poor Biomechanical evaluation of distal radioulnar reconstructions. ME Petersen. J HAND 47
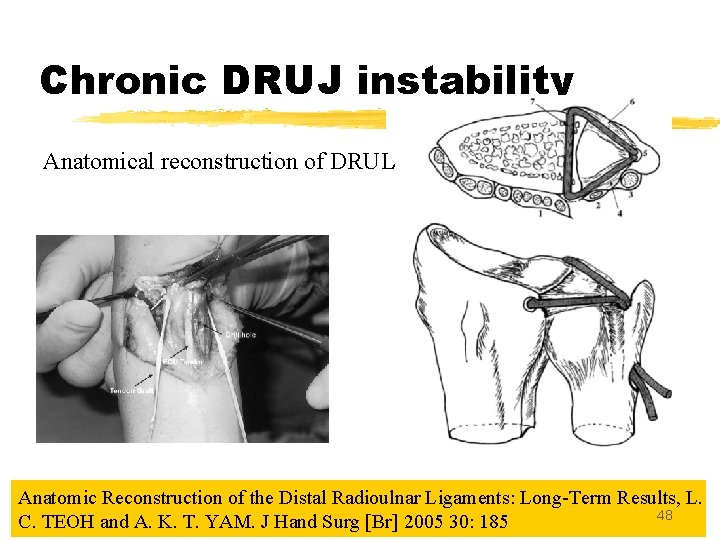
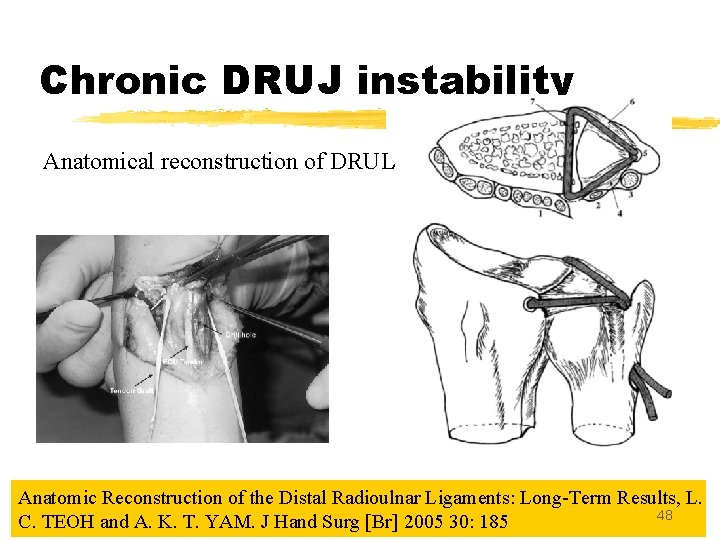
Chronic DRUJ instability Anatomical reconstruction of DRUL Anatomic Reconstruction of the Distal Radioulnar Ligaments: Long-Term Results, L. 48 C. TEOH and A. K. T. YAM. J Hand Surg [Br] 2005 30: 185
Conclusion z. DRUJ one of the 2 major joints involved in forearm supination/pronation z. Bony and ligamentous integrity z. Treatment of DRUJ problems require anatomical and biomechanical knowledge of joint 49
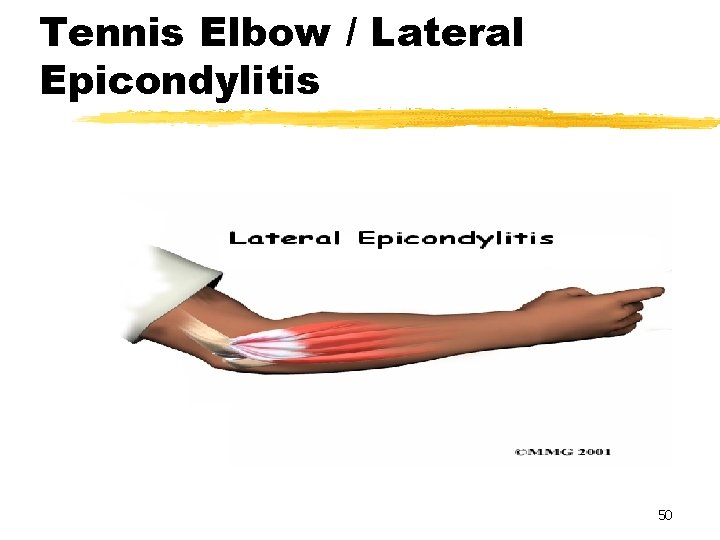
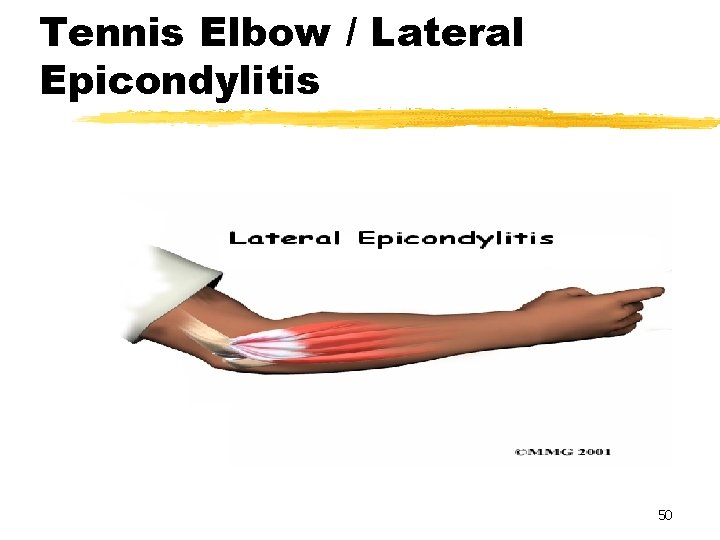
Tennis Elbow / Lateral Epicondylitis 50
Objectives z To understand what tennis elbow is z To understand the anatomy of the elbow z To understand the muscles and tendons effected by tennis elbow z To understand how tennis elbow is recognized z To understand how tennis elbow is treated z To understand how tennis elbow can be prevented 51
Definition Tennis Elbow Defined: Tennis elbow is an overuse injury of the elbow joint. It is commonly found in tennis and golf players, especially the “weekend warrior” type. The medical term for tennis elbow is lateral epicondylitis or radiohumeral bursitis 52
Anatomy The elbow joint is made up of the following bones, muscles and ligaments. z. Humerus, Radius and Ulna. z. Biceps and Triceps. z. Lateral and medial epicondyle. z. Wrist flexor and extensor muscles. z. Ulna collateral ligament. 53
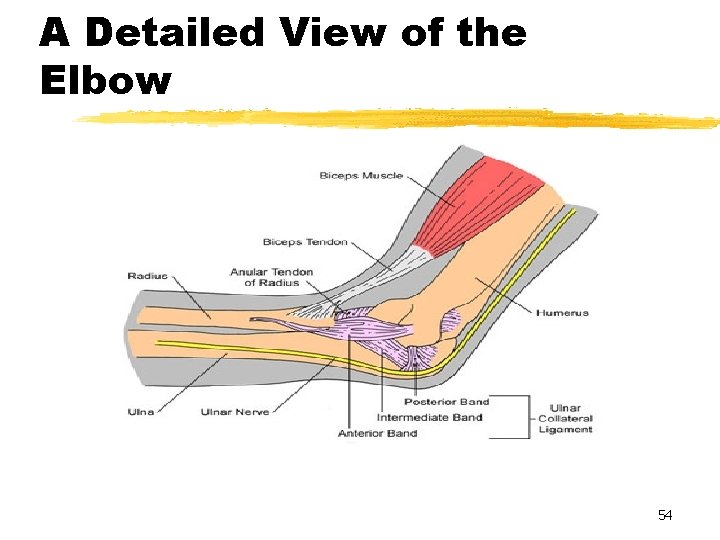
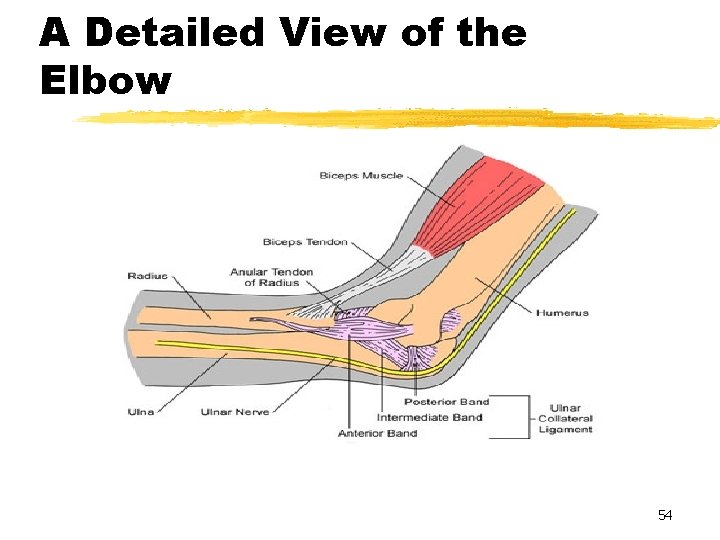
A Detailed View of the Elbow 54
How Tennis Elbow Occurs As stated earlier, tennis elbow is an overuse injury. The most common mechanism of injury to this joint is continuous forceful extension of the forearm with pronation of the forearm. This movement is most typically seen in the backhand stroke of tennis and in the downswing portion of a golf swing. 55
Prevalence z Tennis elbow is found to have an impact on 13% of the general population. z Most commonly affecting men and women from the ages of 40 -50 years of age. z However, tennis elbow can still present itself in people of all ages who are not properly condition to perform the activities which will tend to cause this injury. Examples are the weekend golf and tennis players who are not commonly active. 56
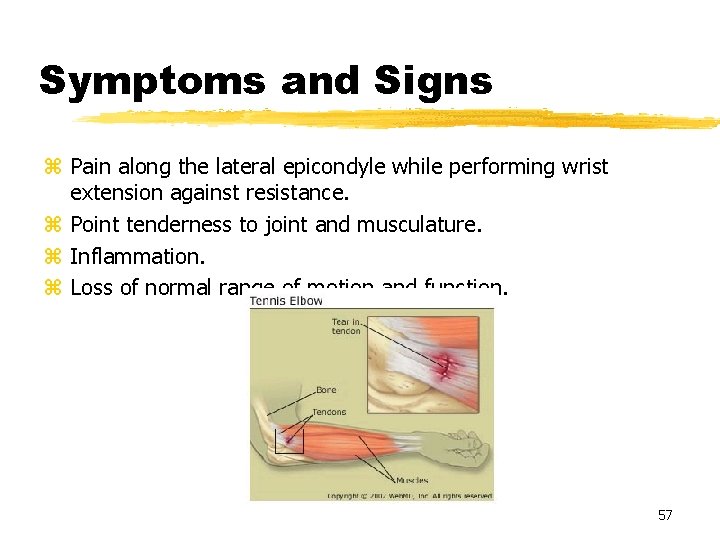
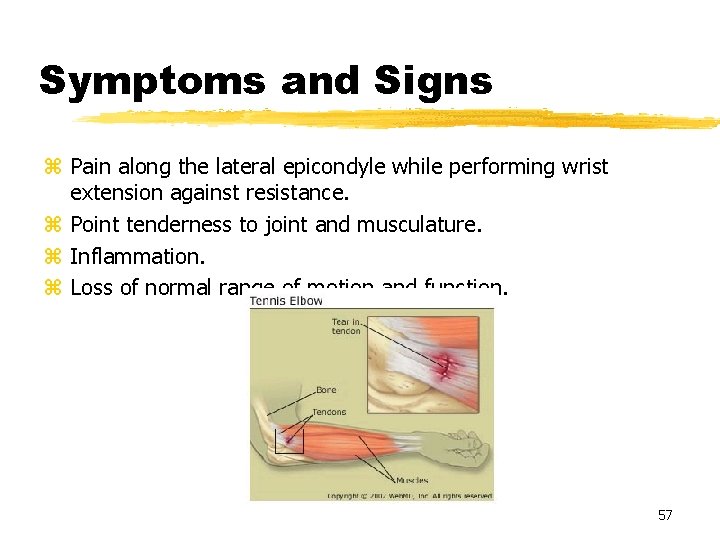
Symptoms and Signs z Pain along the lateral epicondyle while performing wrist extension against resistance. z Point tenderness to joint and musculature. z Inflammation. z Loss of normal range of motion and function. 57
Nirschl Classification of Phases of Lateral Epicondylitis (Tennis Elbow) PHASES OF PAIN Phase 0: No pain or soreness Phase 1: Stiffness or mild soreness after exercise activity. Pain is usually gone in 24 hours. Phase 2: Mild stiffness and soreness before activity which disappears with warm up. No pain during activity, but mild soreness after activity that disappears within 24 hours. Phase 3: Same as above with mild pain during activity which does not alter activity, disappearing in 24 -48 hours. Counterforce bracing may be considered here as well as mild anti-inflammatory medication. Phase 4: Mild to moderate pain before, during, and after exercise which alters the exercise or activity. Phase 4 is indicative of some level of tendon damage. 58
Classification Scale Continued Phase 5: Moderate or greater pain before, during, and after exercise or activity, forcing the patient to discontinue the exercise. Usually reflects permanent tendon damage Phase 6 Phase 5 pain that persists with complete rest. Pain disrupts and many activities have to be eliminated. Phase 7: Phase 6 pain with disruption of sleep on a consistent basis. Pain is aching in nature and intensifies with activity. Pain phases 5, 6, and 7 indicate increasing percentages of permanent tendon damage 59
Treatments Common treatments for tennis elbow: y. Rehabilitation. y. Use of a forearm brace. y. Use of injections of cortisone. y. Strengthening and stretching exercises. y. Rest, ice and compression. 60

Two Examples of Treatment 61
Typical Rehabilitation Program General stretching: active isolated stretching and dynamic movements. Wrist flexion/extension: 3 sets of 10 using tubing. Elbow flexion/extension: same as above. Forearm Pronation/Supination: 3 sets of 10 with 5 pound weight. Radial /Ulnar deviation: 3 sets of 10 with 3 pound weight. Eccentric loading of wrist extensors: 1 set of 10 with 25 pound dumbbell. Simulated tennis swings: forehand, backhand serve. Using either a cable cross machine or a 3 pound weighted racket. 62
Return to Play and Prevention These two concepts really come combined with one another. As long as a person is scoring low enough on the pain scale from the earlier slides, usually from phases 0 -3, they can come back or continue to be active. Also, if a player is just coming off of a rehab program and continues to use the exercises and or the brace for the forearm, they should be able to perform the necessary movements required by their sport of choice. 63
References z Signs and symptoms of athletic injuries. Gallaspy, James; Douglas may, J copyright 1996. z Fundamentals of sports injury management. Anderson, Marcia; Hall, Susan copyright 1997. z Tennis elbow. Buchbinder, Rachelle; Green, sally; Struijs, peter. American family physician. March 2007. z Lateral Epicondylosis: A case study of conservative care utilizing ART and rehabilitation. Howitt, Scott. Journal of Canadian chiropractic association. 2006. z Lateral Epicondylitis: review and current concepts. Faro, Frances; Moriatis wolf, Jennifer. Journal of hand surgery. Oct. 2007. 64
SLAP LESIONS 65
Outline z. Anatomy of the Glenoid Labrum z. Function of the Labrum z. Definition of SLAP lesions z. Classification of SLAP lesions z. Etiology of SLAP Lesions z. Diagnosis z. Management 66
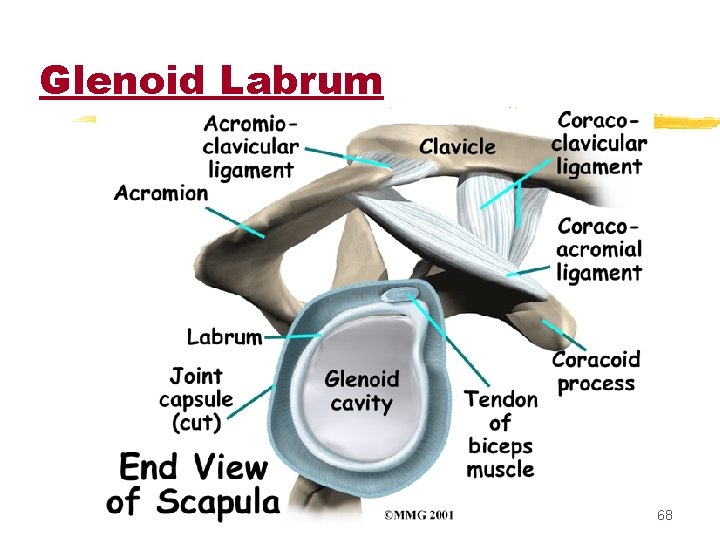
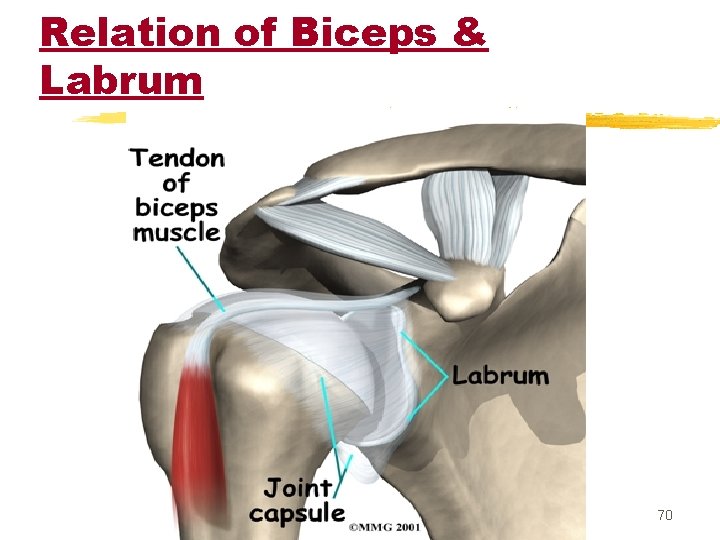
Anatomy of the Glenoid Labrum z Labrum, Capsule, Biceps tendon and Subscapularis muscle are derived from the same embryological cells. z Labrum is a fibrocartilaginous tissue with sparse elastin fibers. z Acts as a transition between the hyaline cartilage of the glenoid and the fibrous joint capsule. Inferiorly, the labrum blends with the articular cartilage of the glenoid. z Functions as a stabilizing and load-sharing structure and serves as a site for ligamentous attachment. 67
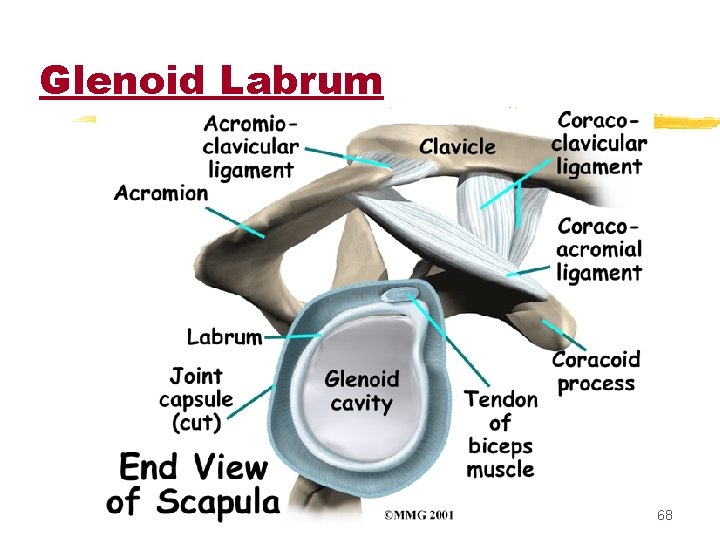
Glenoid Labrum 68
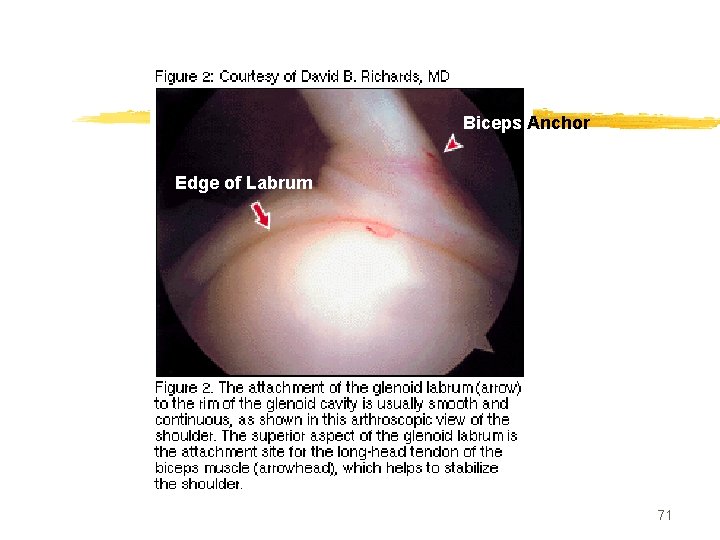
Biceps Anchor z. Broad origin from the supraglenoid tubercle AND the superior labrum at the 12 o-clock position. z. Supraglenoid tubercle is 5 mm medial to the superior edge of the glenoid rim. It has a variable origin, with some reports of 100% origin from the labrum alone. 69
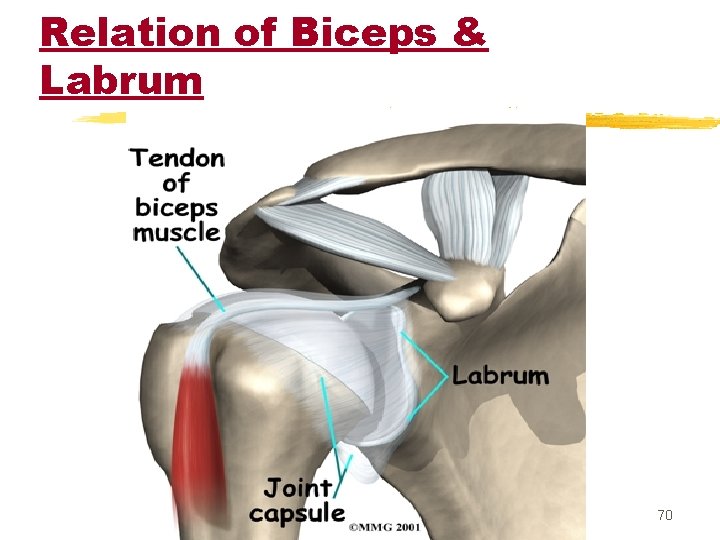
Relation of Biceps & Labrum 70
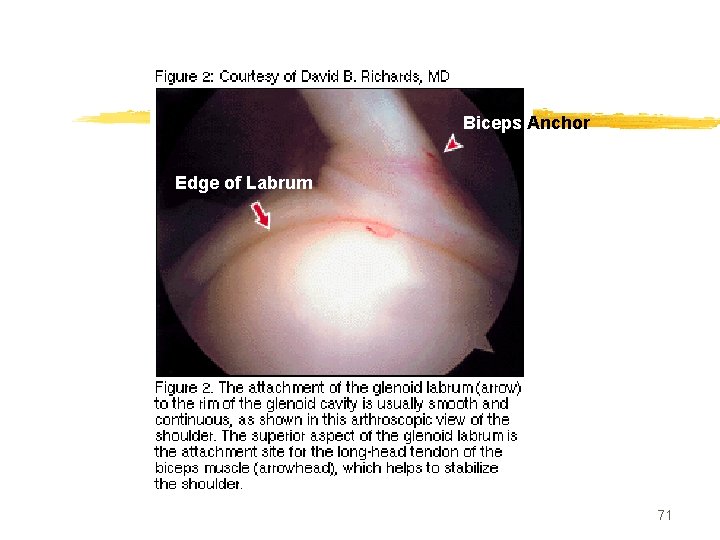
Biceps Anchor Edge of Labrum 71
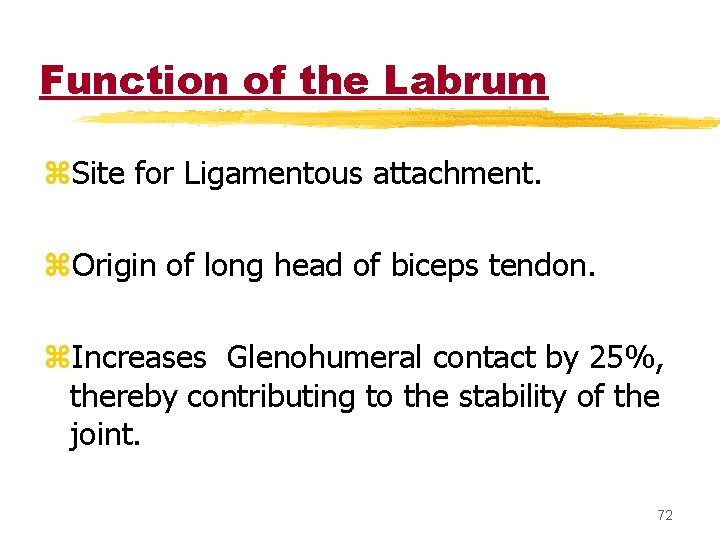
Function of the Labrum z. Site for Ligamentous attachment. z. Origin of long head of biceps tendon. z. Increases Glenohumeral contact by 25%, thereby contributing to the stability of the joint. 72
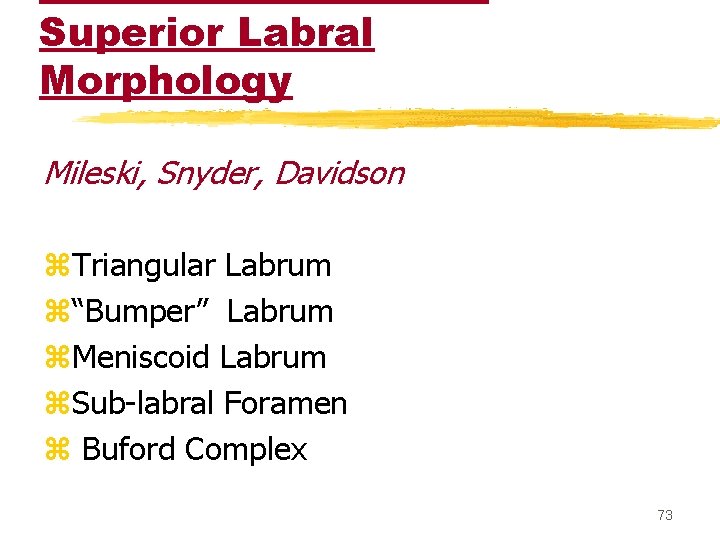
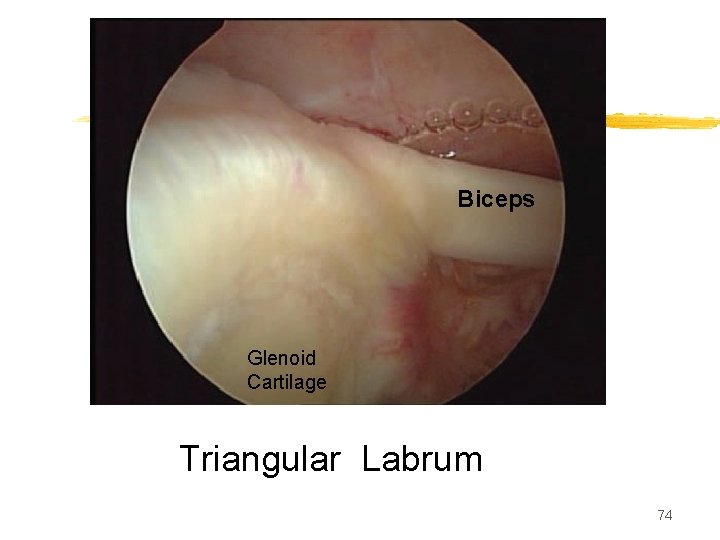
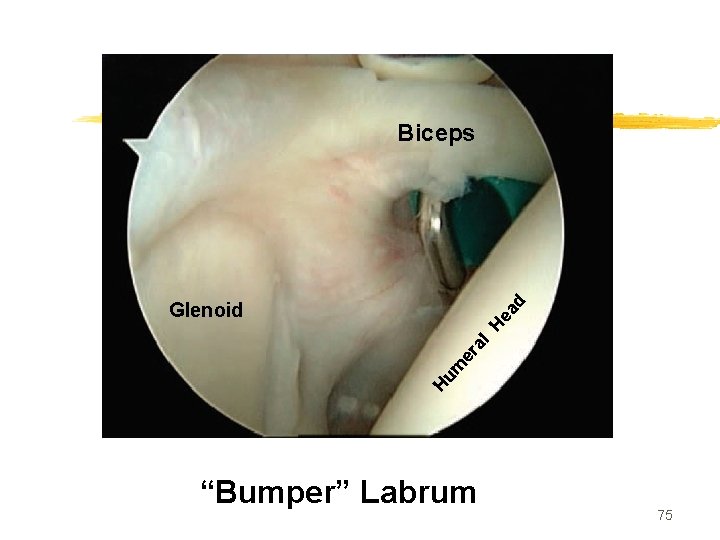
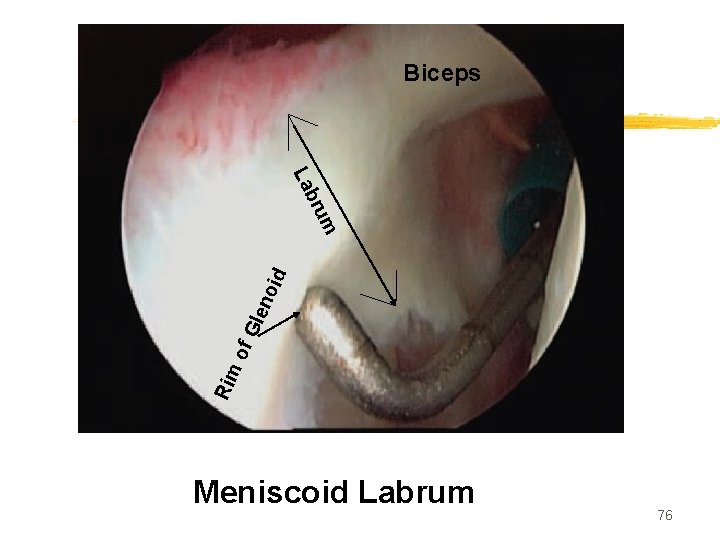
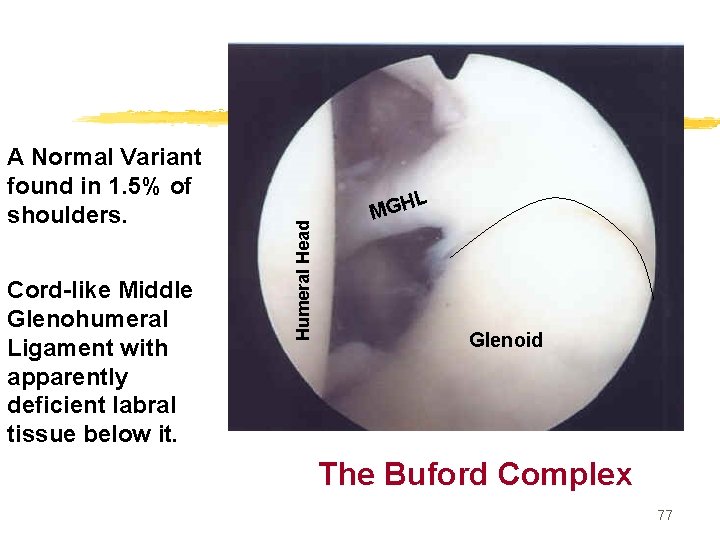
Superior Labral Morphology Mileski, Snyder, Davidson z. Triangular Labrum z“Bumper” Labrum z. Meniscoid Labrum z. Sub-labral Foramen z Buford Complex 73
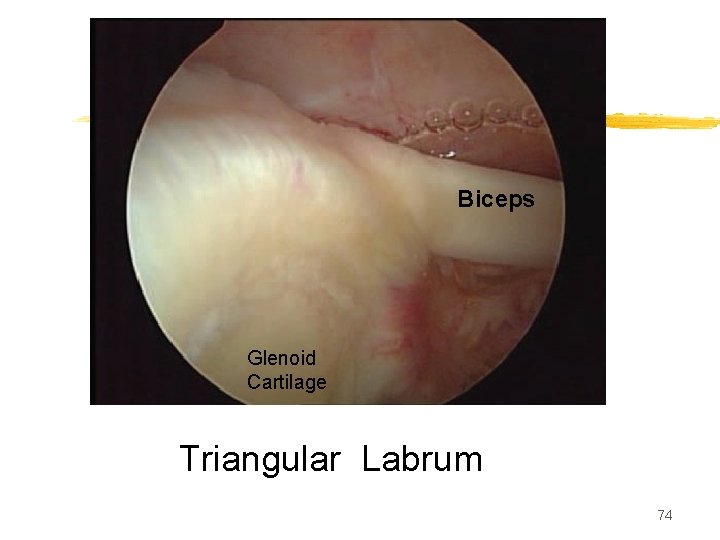
Biceps Glenoid Cartilage Triangular Labrum 74
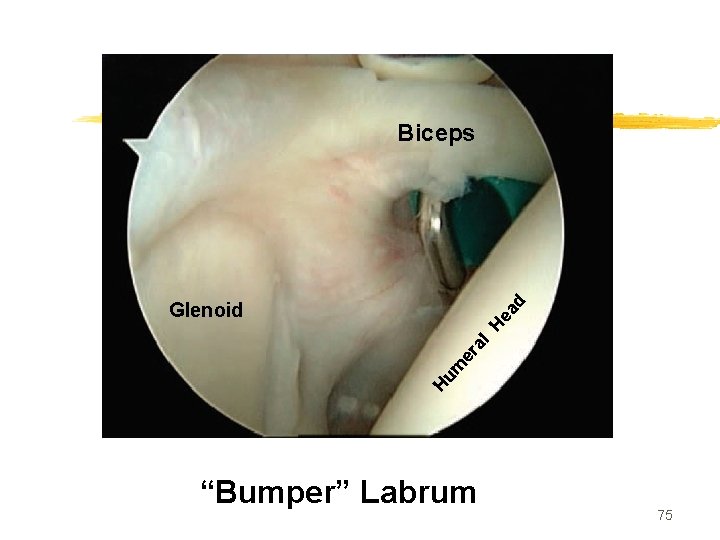
Biceps Hu m er al He ad Glenoid “Bumper” Labrum 75
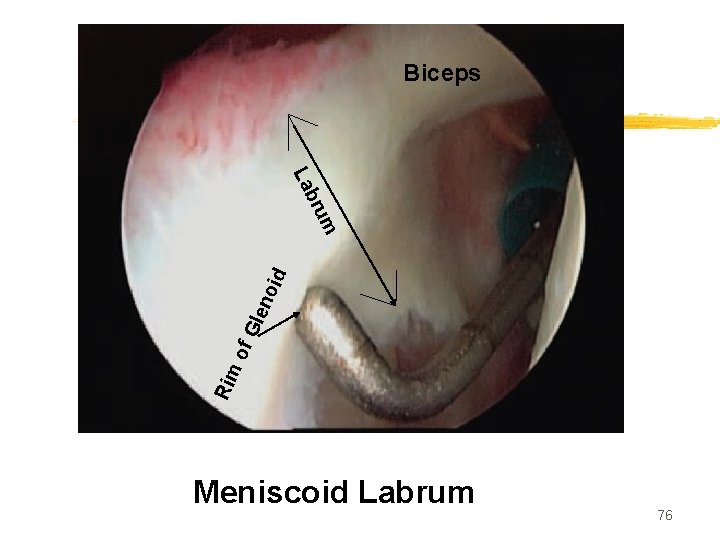
Biceps Rim of Gle no id rum b La Meniscoid Labrum 76
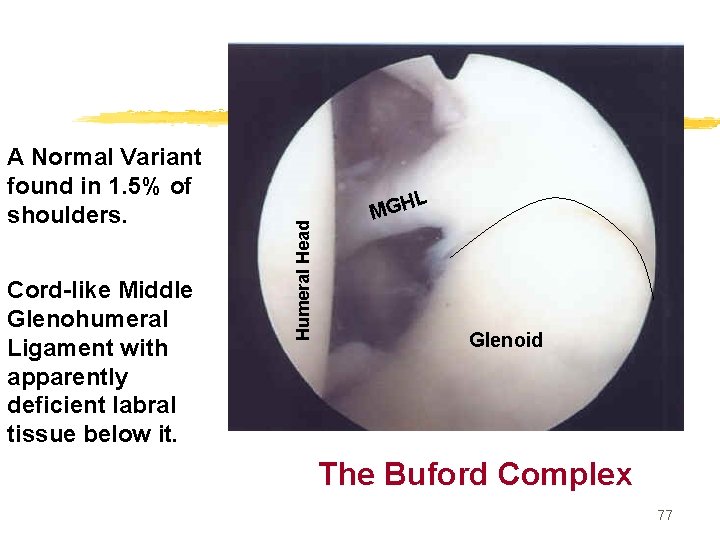
Cord-like Middle Glenohumeral Ligament with apparently deficient labral tissue below it. L Humeral Head A Normal Variant found in 1. 5% of shoulders. MGH Glenoid The Buford Complex 77
Definition of SLAP lesions z. Term SLAP coined by Snyder et al. z. Superior Labrum Anterior and Posterior (to the biceps anchor) z. Refers to lesions of the superior labrum 78
Classification…. . by Snyder 79
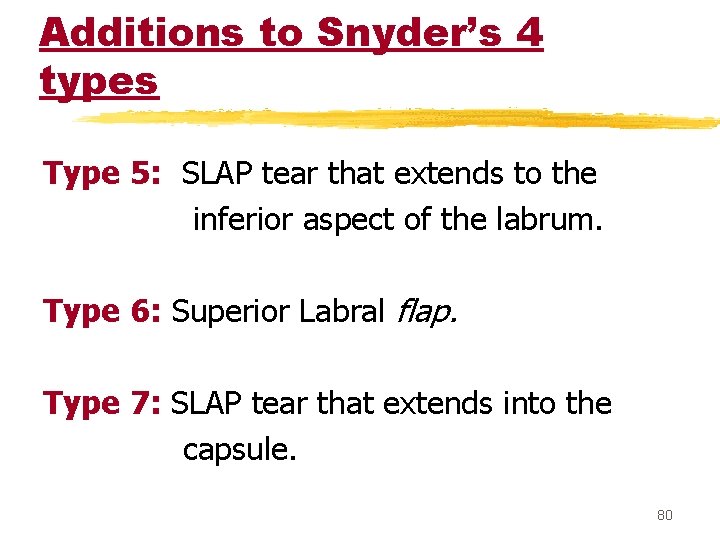
Additions to Snyder’s 4 types Type 5: SLAP tear that extends to the inferior aspect of the labrum. Type 6: Superior Labral flap. Type 7: SLAP tear that extends into the capsule. 80
Etiology of SLAP Lesions z There is controversy regarding the actual mechanism/s resulting in SLAP lesions. Theories include: Primary shoulder instability leading to internal impingement of the labrum. Traction injury from biceps during the deceleration phase of throwing. Traction/twisting injury from biceps during the late cocking phase of throwing (abduction and external rotation) Compression injury from a FOOSH. 81
Etiology of SLAP Lesions z. Likely, each theory has it’s own merit for a given SLAP pattern, as there are biomechanical or clinical studies supporting each one. 82
Internal Impingement Caused by Excessive External rotation and Extension Undersurface of rotator cuff impinges against superior posterior labrum and glenoid, causing damage to all three. G. Walsh, 1992 83
Diagnosis is Difficult z History and symptoms are generally vague and not specific. z SLAP lesions are often associated with other pathology (instability, rotator cuff disease, tight posterior capsule…) that make physical exam non-specific. z The many normal variants make MRI interpretation difficult. z Assessing labral stability on MRI can be difficult. 84
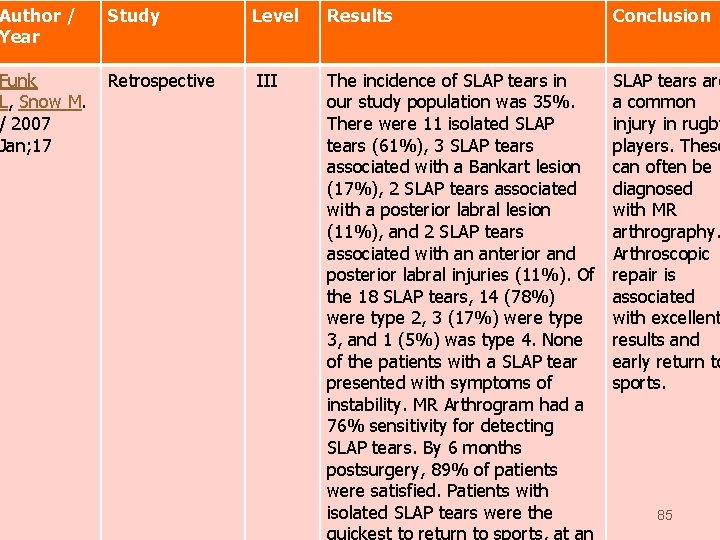
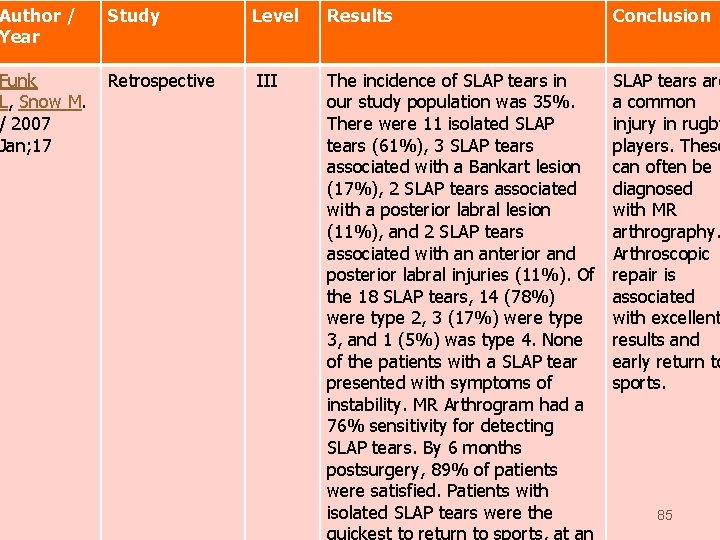
Author / Year Study Funk L, Snow M. / 2007 Jan; 17 Retrospective Level III Results Conclusion The incidence of SLAP tears in our study population was 35%. There were 11 isolated SLAP tears (61%), 3 SLAP tears associated with a Bankart lesion (17%), 2 SLAP tears associated with a posterior labral lesion (11%), and 2 SLAP tears associated with an anterior and posterior labral injuries (11%). Of the 18 SLAP tears, 14 (78%) were type 2, 3 (17%) were type 3, and 1 (5%) was type 4. None of the patients with a SLAP tear presented with symptoms of instability. MR Arthrogram had a 76% sensitivity for detecting SLAP tears. By 6 months postsurgery, 89% of patients were satisfied. Patients with isolated SLAP tears were the SLAP tears are a common injury in rugby players. These can often be diagnosed with MR arthrography. Arthroscopic repair is associated with excellent results and early return to sports. 85
Foot Disorders zdeformities zarthritis zpain 86
Plantar Fasciitis 87
Objectives z. Review the patho-physiology of PF z. Review the underlying causes z. Review the numerous treatment methods z. Describe a rehabilitation program z. Recommend a return-to-play program 88
Magnitude of the problem z. Affects 10% of runners z. Affects numerous other athletes ysoldiers ysoccer, basketball, tennis, gymnastics, others z 2 million Americans treated per year z. Significant interference in athletics 89
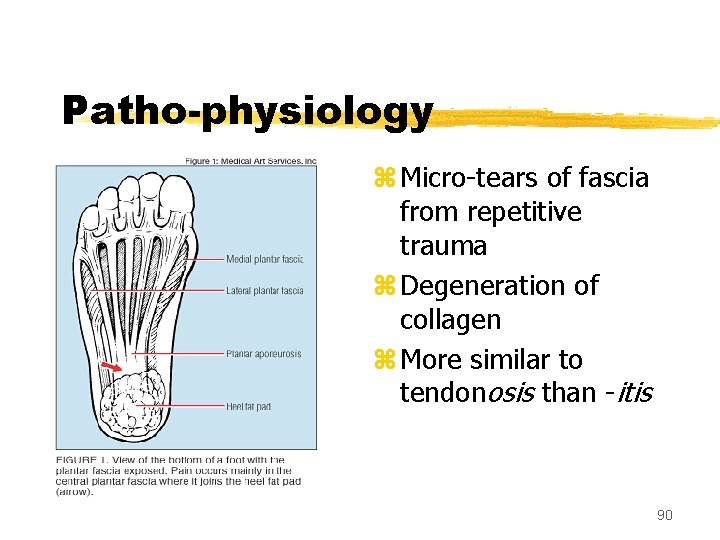
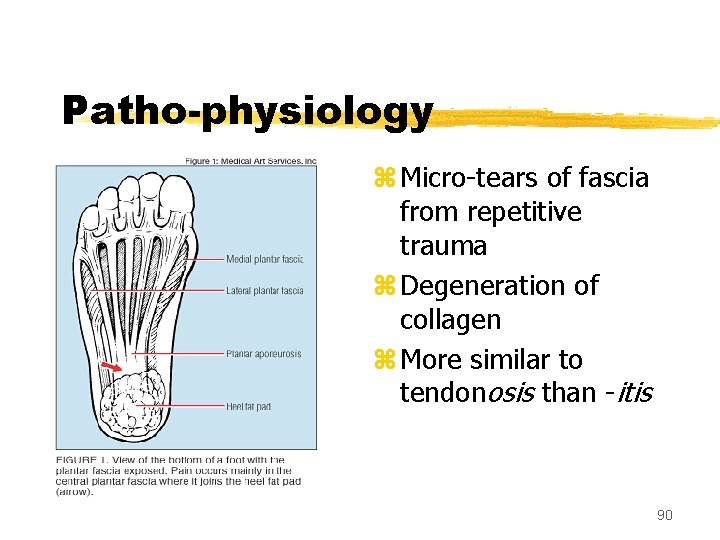
Patho-physiology z Micro-tears of fascia from repetitive trauma z Degeneration of collagen z More similar to tendonosis than -itis 90
Clinical features z. Severe plantar foot pain aggravated by weight bearing with first steps of the AM z. May improve after a few minutes of running, then worsen z. Deep ache over anteromedial calcaneus z. TTP over plantar medial calcaneal tubercle z. Tight heel cord a common finding 91
Predisposing factors z. Extrinsic factors y. Training errors y. Improper footwear (300 mile rule) y. Unyielding running surfaces z. Intrinsic factors y. Pes planus w/ hyperpronation y. Pes cavus w/ supination y. Tight heel cords y. Weak intrinsic foot muscles 92
History z. Training regimen (any changes prior? ) z. Exacerbating activities z. Duration z. Past treatments z. Other medical problems z. Miles on running shoes 93
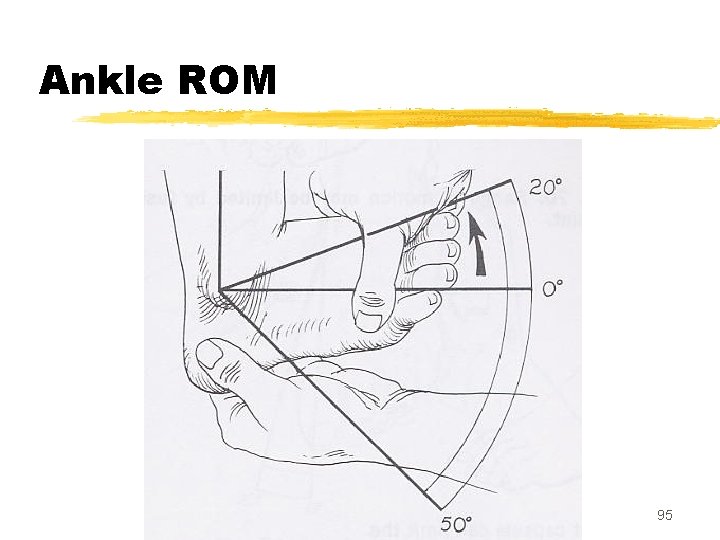
Examination z. Establish point of maximal tenderness z. Evaluate for other tenderness z. Ankle ROM (tight Achilles? ) z. Evaluate longitudinal arches z. Look at running shoes/boots 94
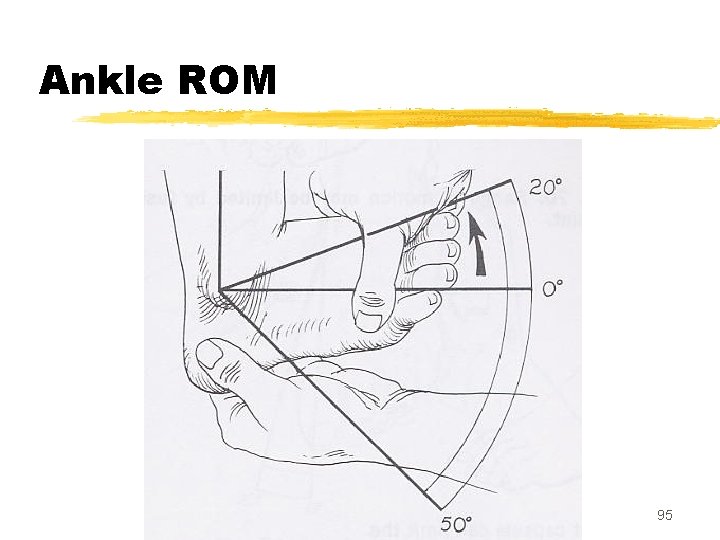
Ankle ROM 95
Radiology? z. Rarely useful; not needed in most cases z. What about heel spurs? y. Probably negligible x 13% prevalence xonly 5% of those c/o heel pain 96
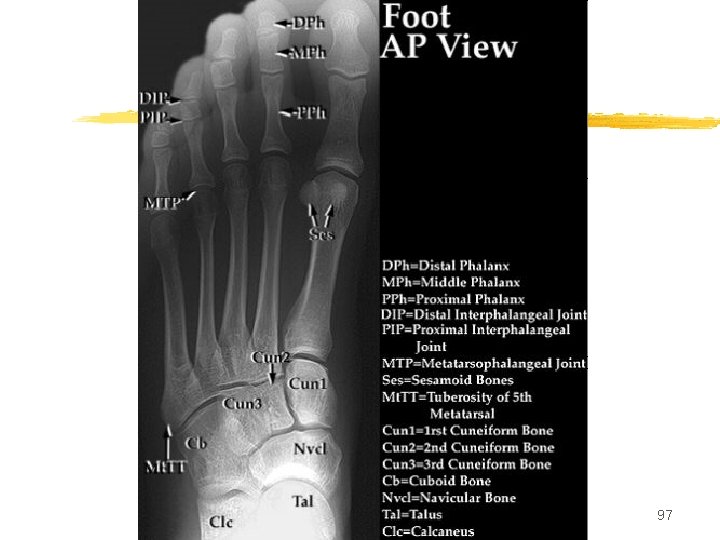
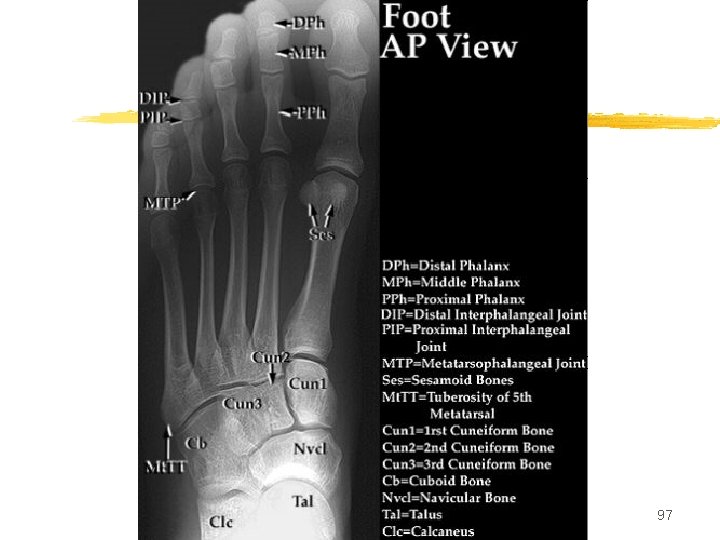
97
98
99
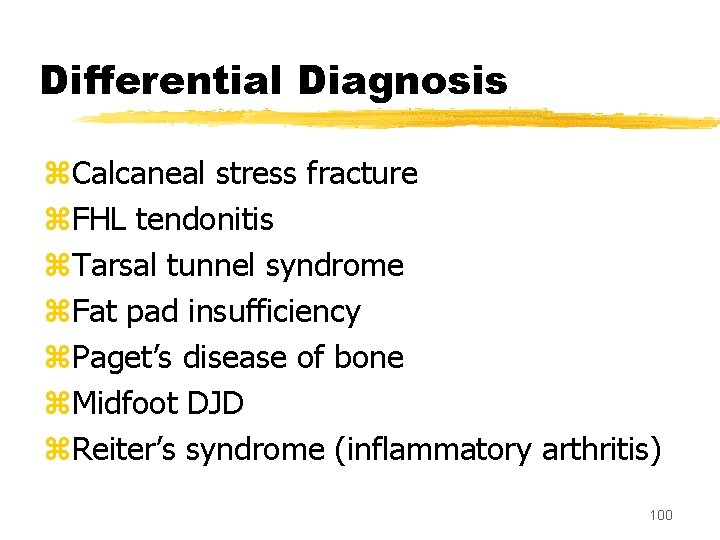
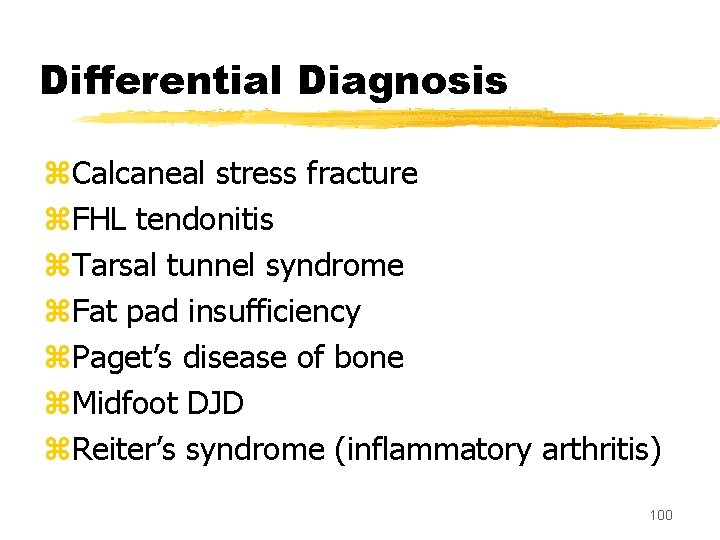
Differential Diagnosis z. Calcaneal stress fracture z. FHL tendonitis z. Tarsal tunnel syndrome z. Fat pad insufficiency z. Paget’s disease of bone z. Midfoot DJD z. Reiter’s syndrome (inflammatory arthritis) 100
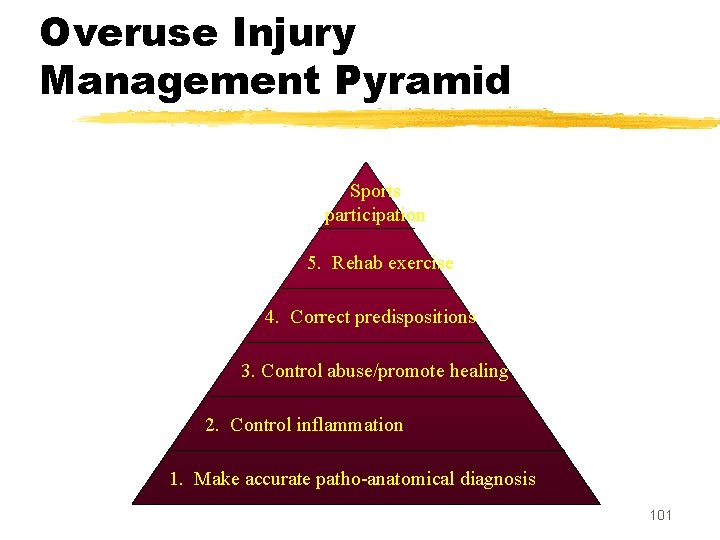
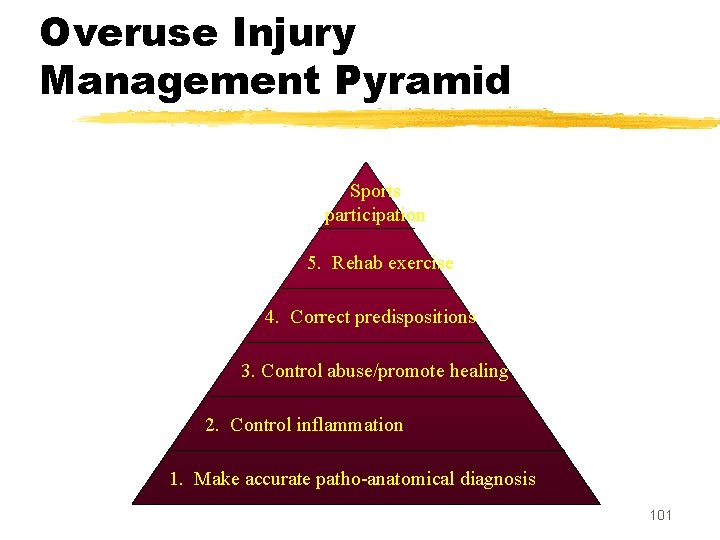
Overuse Injury Management Pyramid Sports participation 5. Rehab exercise 4. Correct predispositions 3. Control abuse/promote healing 2. Control inflammation 1. Make accurate patho-anatomical diagnosis 101
1. Control inflammation z. Ice massage z. NSAID z. Iontopheresis z. Steroid injection 102
Control inflammation (cont): Ice Massage z 15 minutes rolling on frozen juice can z. Ice baths z. After activity, several times a day 103
Control inflammation (cont): NSAID z. Short course, 2 weeks z. Largely analgesic properties z. Useful, but MINOR role in treatment 104
Control inflammation (cont): Iontopheresis z. Ultrasound using corticosteroid cream z. Six treatments over 2 weeks z. One study: Ionto vs sham ymore rapid sx relief and improvement at 2 wks yno better than sham at 1 month x. Gudeman et al, Am J Sports Med 1997 z. Marginal benefit z. Consider cost and compliance 105
Control inflammation (cont): Steroid Injection z. Quicker pain relief at 1 mo but no longterm advantage y. Crawford et al, Rheum 1999. z. Predisposes to PF rupture, which causes chronic pain y. Acevedo JI et al, 1998: 765 pts tx’d for PF x. Those tx’d w/ injection: 44 ruptures (10%) x. Others: 7 ruptures (1%) 106
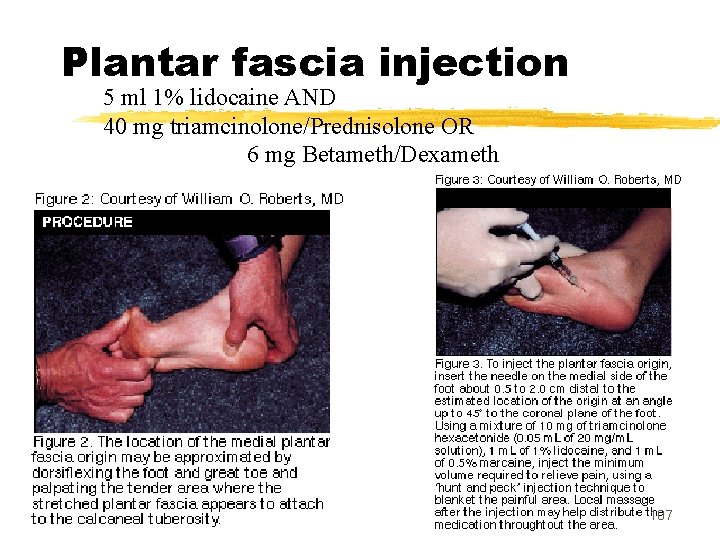
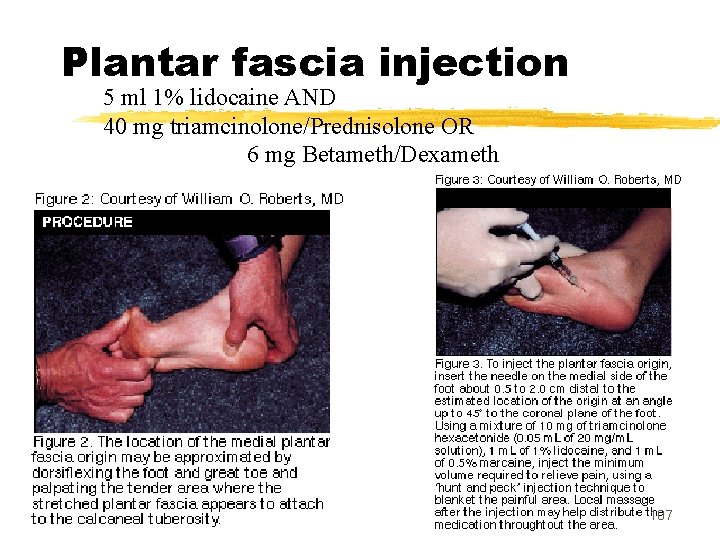
Plantar fascia injection 5 ml 1% lidocaine AND 40 mg triamcinolone/Prednisolone OR 6 mg Betameth/Dexameth 107
2. Protect from ongoing abuse z. Only do activity that is NON-painful ycross training useful, e. g. bike, deep pool running yif running, less distance/hills/speed z. Increase 10% a week, if improving z. Expect 8 -12 weeks to resume full activity for athletes 108
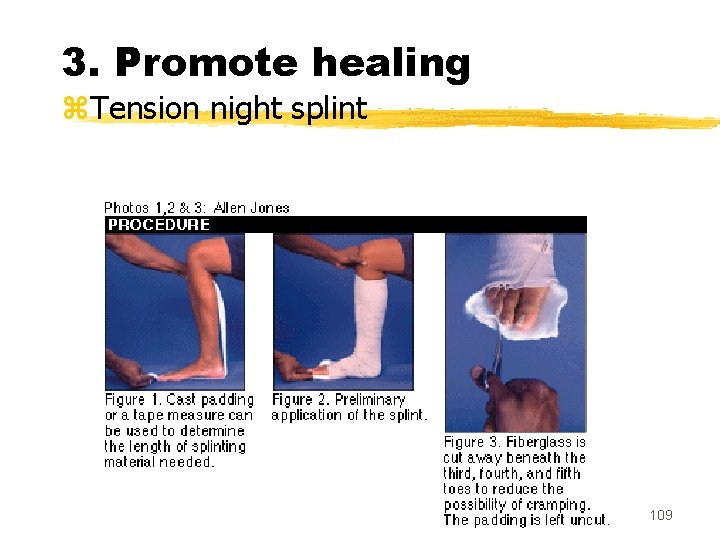
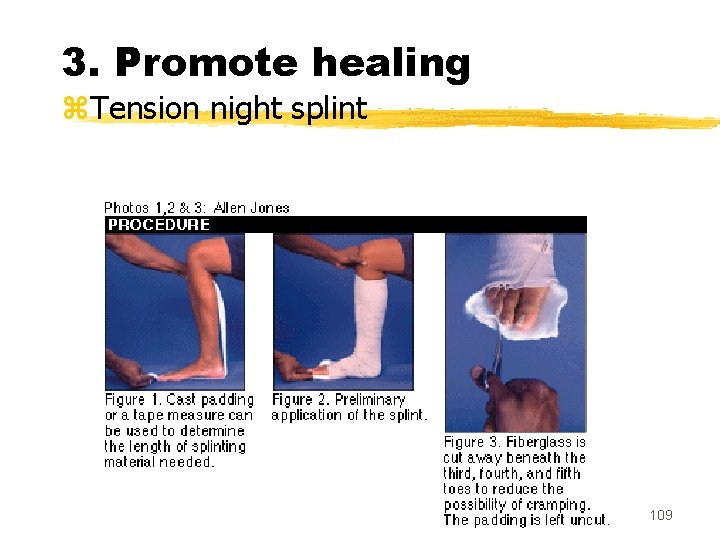
3. Promote healing z. Tension night splint 109
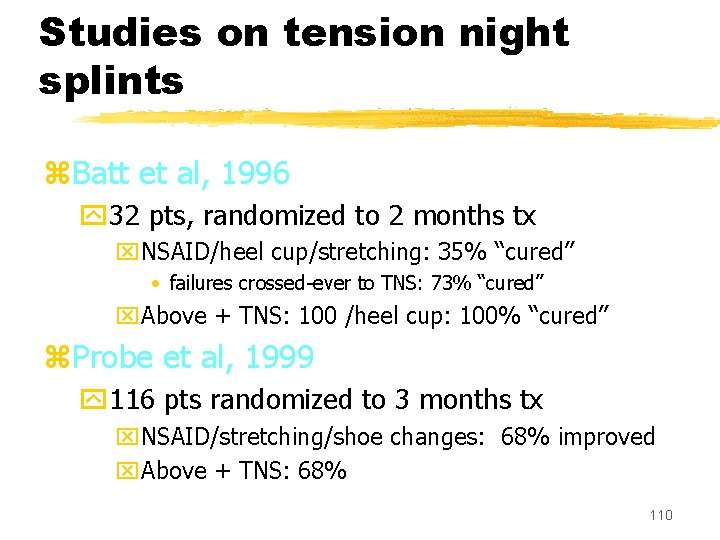
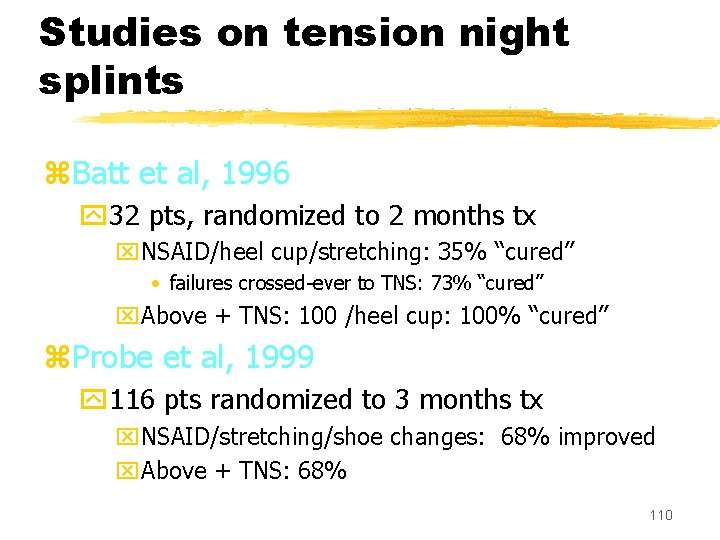
Studies on tension night splints z. Batt et al, 1996 y 32 pts, randomized to 2 months tx x. NSAID/heel cup/stretching: 35% “cured” • failures crossed-ever to TNS: 73% “cured” x. Above + TNS: 100 /heel cup: 100% “cured” z. Probe et al, 1999 y 116 pts randomized to 3 months tx x. NSAID/stretching/shoe changes: 68% improved x. Above + TNS: 68% 110
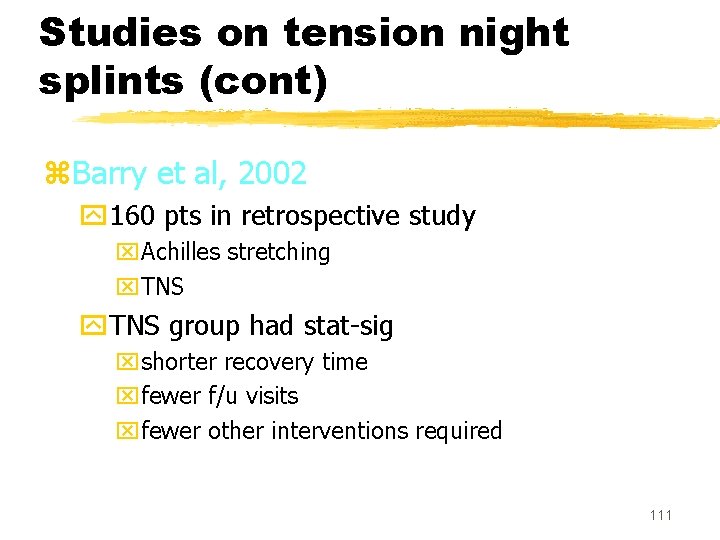
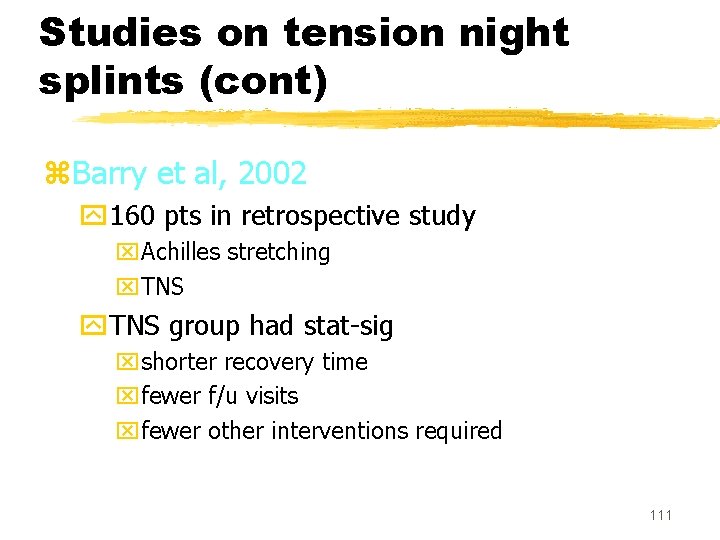
Studies on tension night splints (cont) z. Barry et al, 2002 y 160 pts in retrospective study x. Achilles stretching x. TNS y. TNS group had stat-sig xshorter recovery time xfewer f/u visits xfewer other interventions required 111
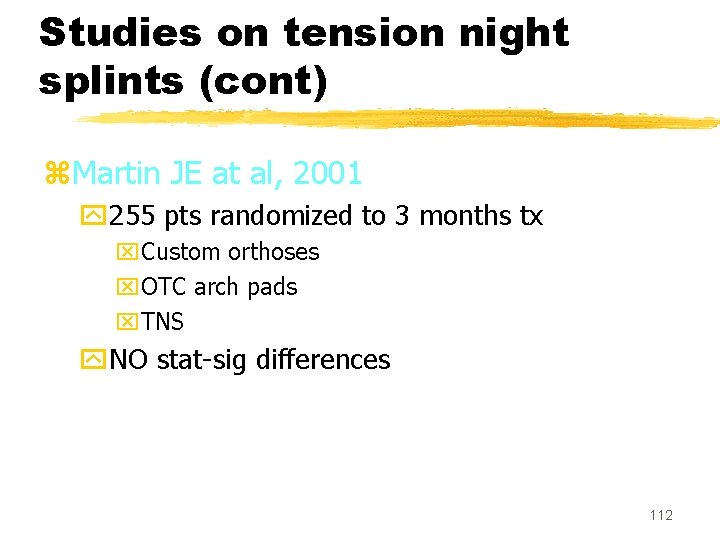
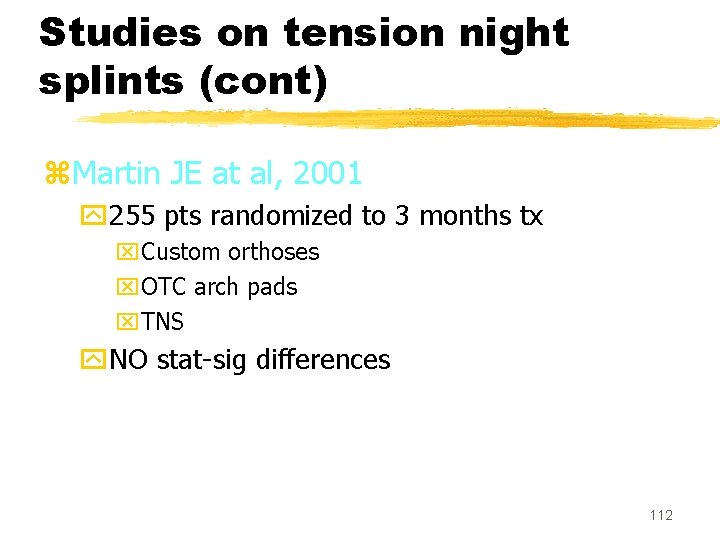
Studies on tension night splints (cont) z. Martin JE at al, 2001 y 255 pts randomized to 3 months tx x. Custom orthoses x. OTC arch pads x. TNS y. NO stat-sig differences 112
Night splint conclusions z. Mixed results in studies z. May try if initial response poor 113
4. Correct predisposing factors z. Work on Achilles inflexibility z. Change running surface? z. New shoes? z. OTC arch pads yconsider custom orthotics if no response z. Educate on training principles (10% rule) 114
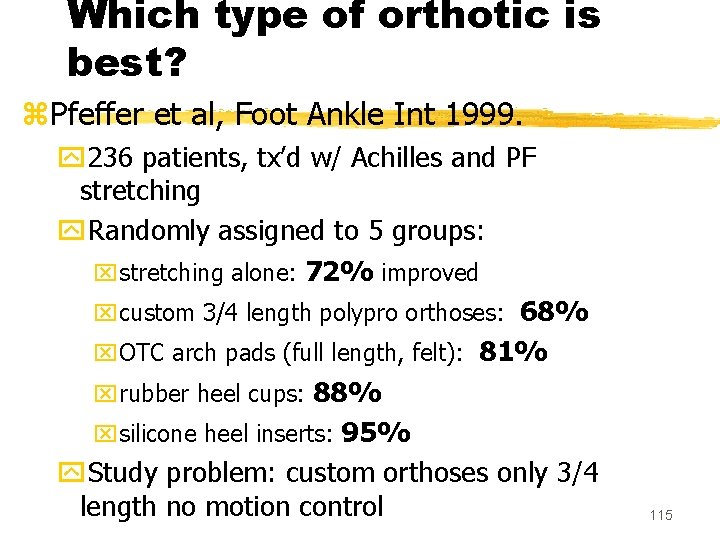
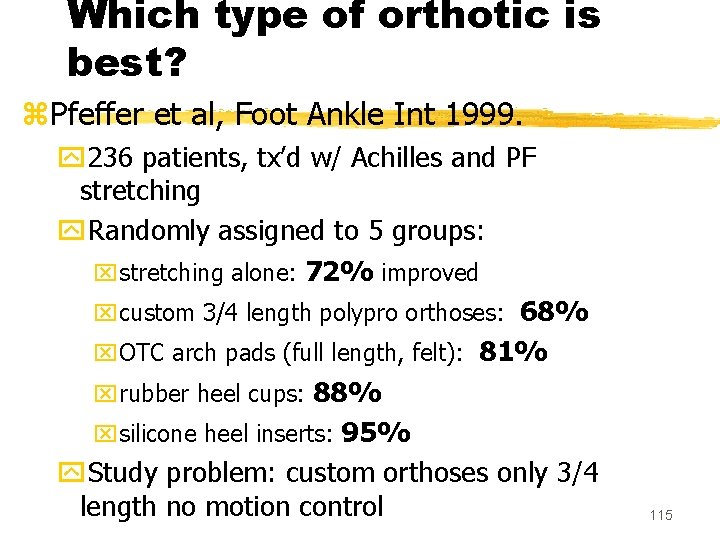
Which type of orthotic is best? z. Pfeffer et al, Foot Ankle Int 1999. y 236 patients, tx’d w/ Achilles and PF stretching y. Randomly assigned to 5 groups: xstretching alone: 72% improved xcustom 3/4 length polypro orthoses: 68% x. OTC arch pads (full length, felt): 81% xrubber heel cups: 88% xsilicone heel inserts: 95% y. Study problem: custom orthoses only 3/4 length no motion control 115
Which type of orthotic is best? (cont) z. Martin JE at al, 2001 y 255 pts randomized to 3 months tx x. Custom orthoses x. OTC arch pads x. TNS y. NO stat-sig differences 116
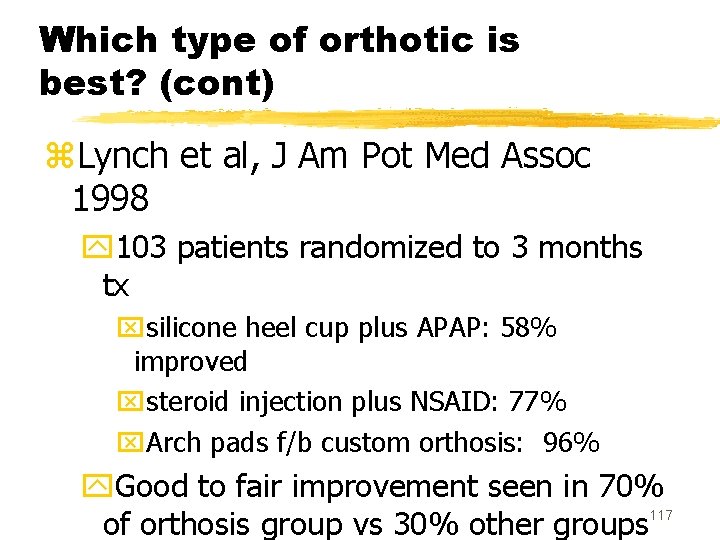
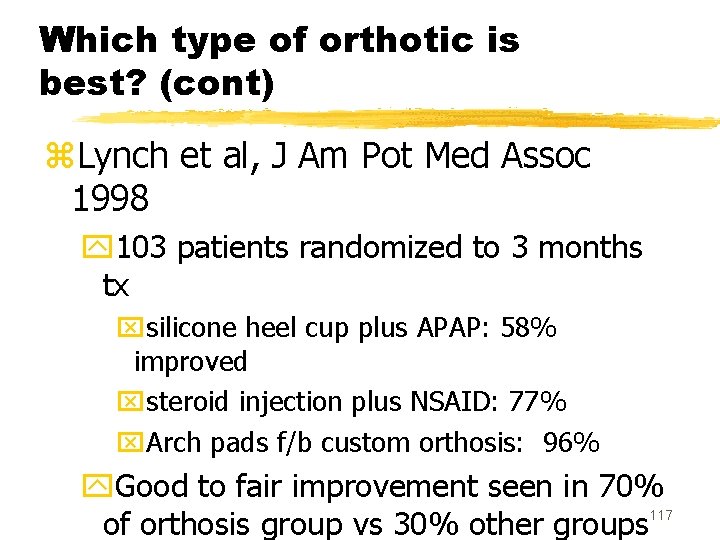
Which type of orthotic is best? (cont) z. Lynch et al, J Am Pot Med Assoc 1998 y 103 patients randomized to 3 months tx xsilicone heel cup plus APAP: 58% improved xsteroid injection plus NSAID: 77% x. Arch pads f/b custom orthosis: 96% y. Good to fair improvement seen in 70% 117 of orthosis group vs 30% other groups
Which type of orthosis is best? Conclusions: z. Use low-cost orthoses first y. OTC arch pads, OR y. Heel cups, OR y. Silicone heel pads z. Consider custom arch pads if good response 118
5. Rehabilitative exercise: Principles z. Overall flexibility puts less strain on PF y. Achilles, longitudinal arch z. Intrinsic foot muscles support the PF z. Ankle stability reduces stress on PF z. Improved running form protects the PF ylower leg strength and flexibility 119
Rehabilitative exercises z 1 -2 x/day Achilles stretching z. Daily eccentric (stair edge) heel ex’s y 2 sets of 15 to fatigue z. Barefoot heel/toe/backward walking while carrying weights z. Towel toe-grabbing (intrinsic foot muscles) z. Ankle tubing strength ex’s (inv/ev/DF) 120
Typical treatment protocol New patient z. Profile to control abuse z 2 wks piroxicam z. Ice massage 4 x/day z. OTC arch pads or gel heel cup z. Handout for exercises, esp heel stretching zf/u 2 wks; reinforce need for rehab ex’s; modify profile 121
Poor response after 1 month z. Add tension night splint (brace shop) z. Refer for custom orthotics z. Refer to Physical Therapy for more instruction on rehab z. Consider steroid injection for those who require rapid pain relief/return to duty 122
Poor response after 2 months z. Make sure patient is doing what you Rx’d z. Discuss option of steroid injection x 1 123
PF Surgery z. Indications y. Failure of 12 months of conservative tx using multiple methods y 9 months of continuous profiles z. Effectiveness 90% z. Recovery several months z. Evans Podiatry practice ywrite P 3 profile and refer for MMRB yrare surgery 124
In the research pipeline z. Lithotripsy y. Europe y. Possible alternative to surgery for chronic PF 125
Summary z. Time is required for recovery (pt ed) z. Rehab exercise is critical in healing z. Look for predisposing factors and correct them z. Use multiple treatments z<10% need surgery 126
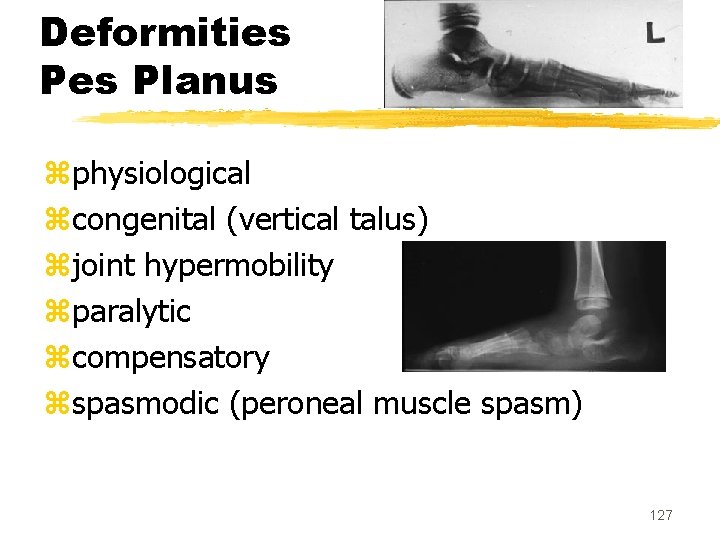
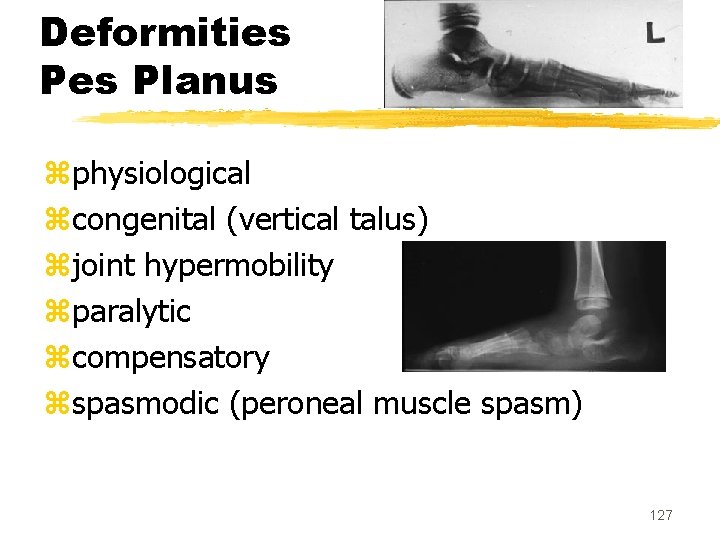
Deformities Planus zphysiological zcongenital (vertical talus) zjoint hypermobility zparalytic zcompensatory zspasmodic (peroneal muscle spasm) 127
Pes Planus Peroneal muscle spasm xtarsal coalition xinfection xinflammatory arthritis xfractures 128
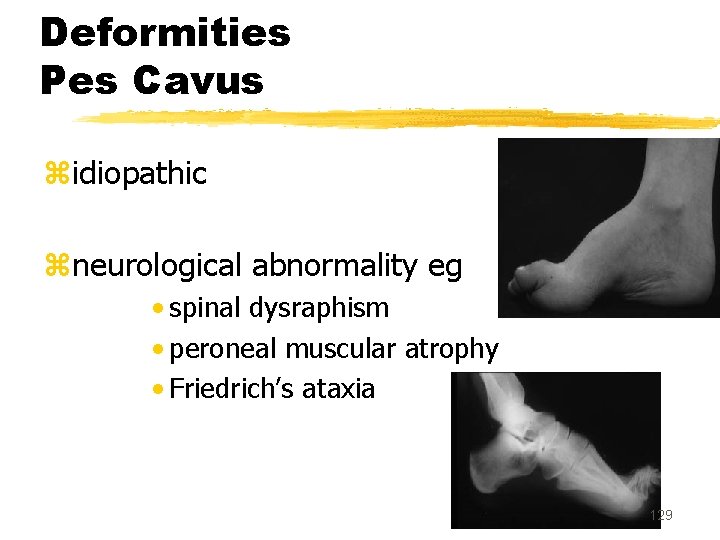
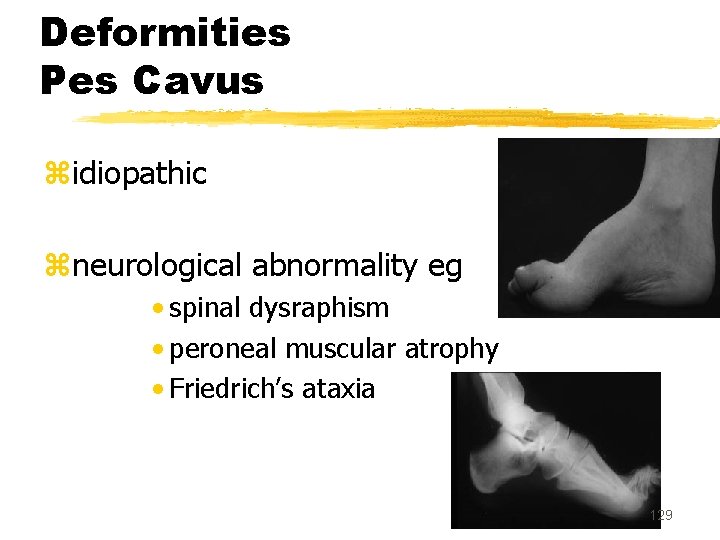
Deformities Pes Cavus zidiopathic zneurological abnormality eg • spinal dysraphism • peroneal muscular atrophy • Friedrich’s ataxia 129
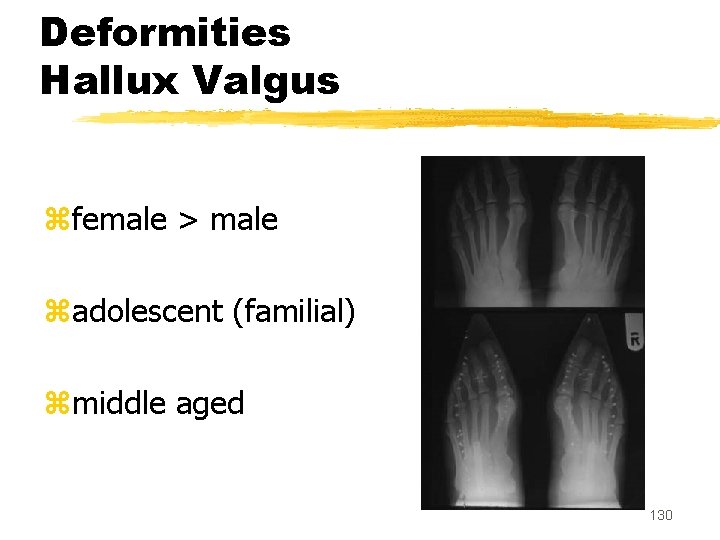
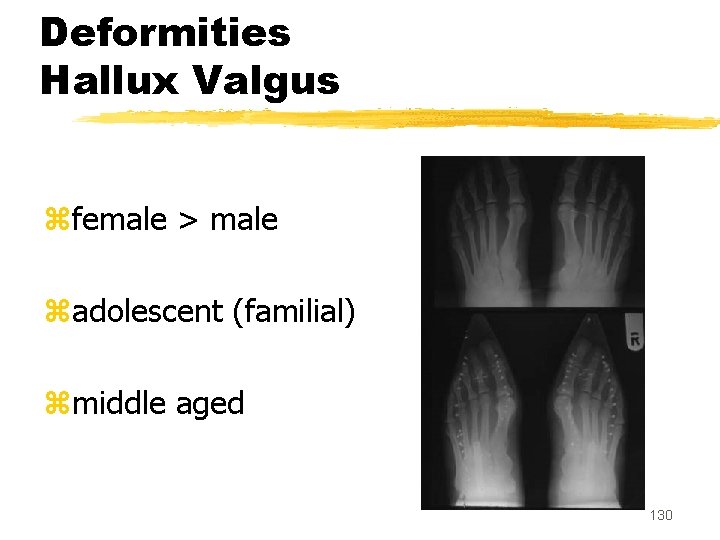
Deformities Hallux Valgus zfemale > male zadolescent (familial) zmiddle aged 130
Hallux Valgus symptoms zdeformity zpain ¨bunion ©metatarsalgia ªMT-P OA «hammer toe 131
Hallux Valgus treatment z. Soft tissue balancing zdistal osteotomy zproximal osteotomy zexcision zfusion 132
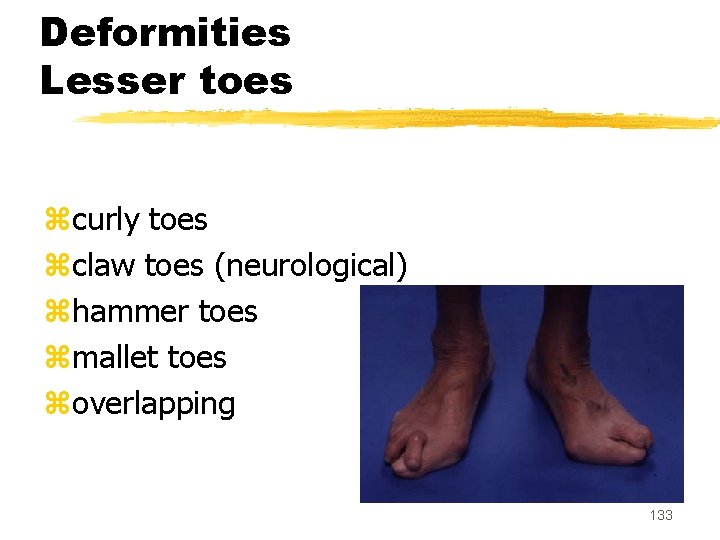
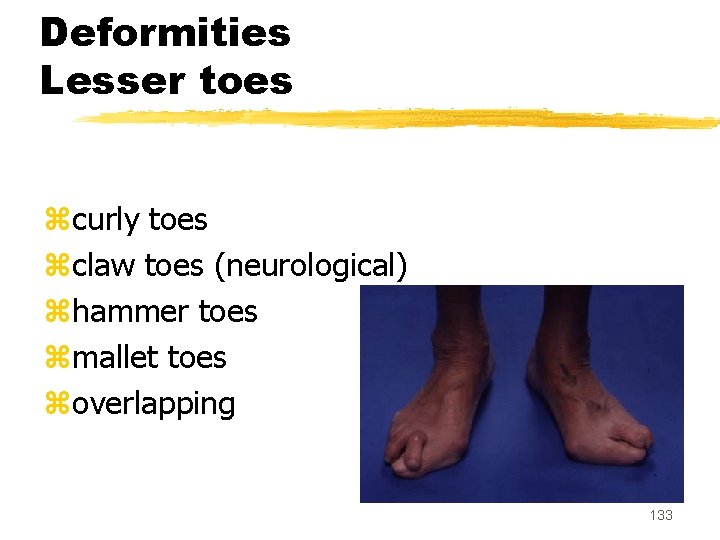
Deformities Lesser toes zcurly toes zclaw toes (neurological) zhammer toes zmallet toes zoverlapping 133
Lesser toe deformities treatment zmodify footwear ztendon release / transfer zexcision zarthrodesis 134
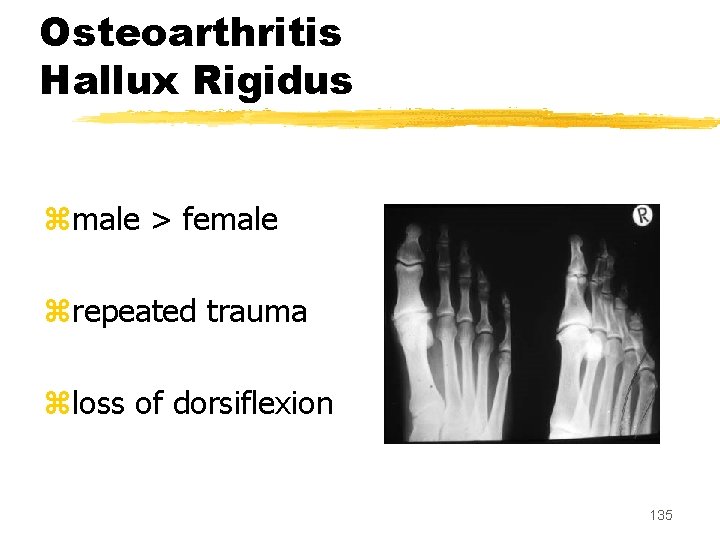
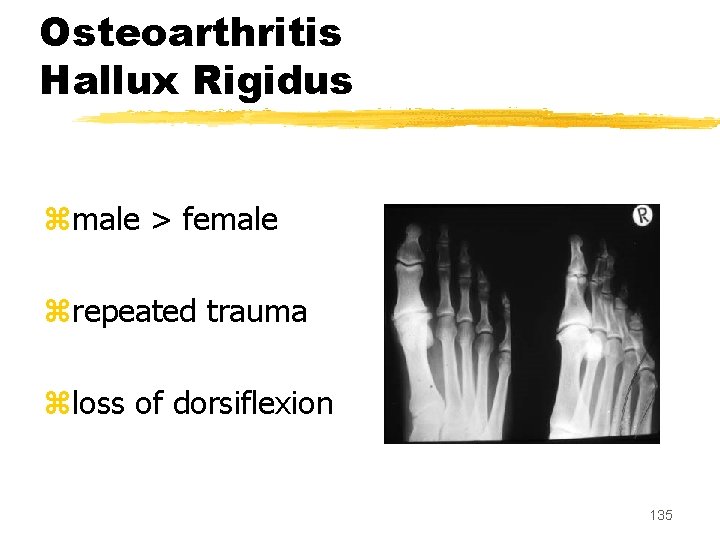
Osteoarthritis Hallux Rigidus zmale > female zrepeated trauma zloss of dorsiflexion 135
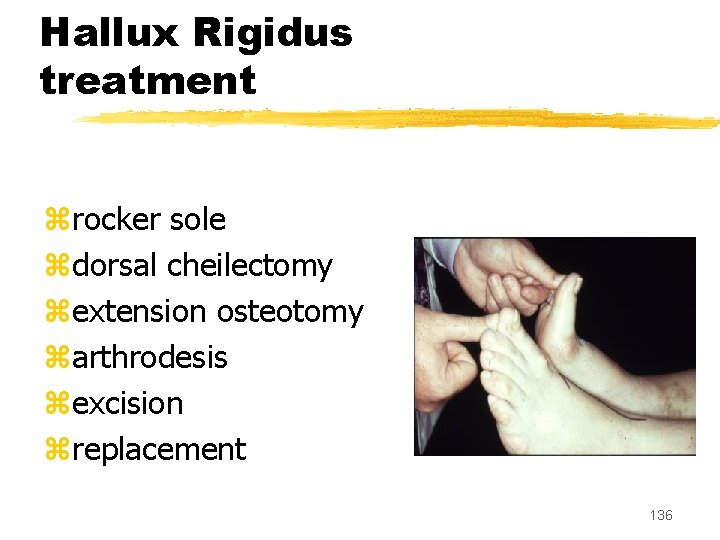
Hallux Rigidus treatment zrocker sole zdorsal cheilectomy zextension osteotomy zarthrodesis zexcision zreplacement 136
Rheumatoid arthritis hindfoot z. Ankle pain and swelling xtenosynovitis xankle or sub-talar joint z. Ankle and tarsal joint erosion and deformity 137
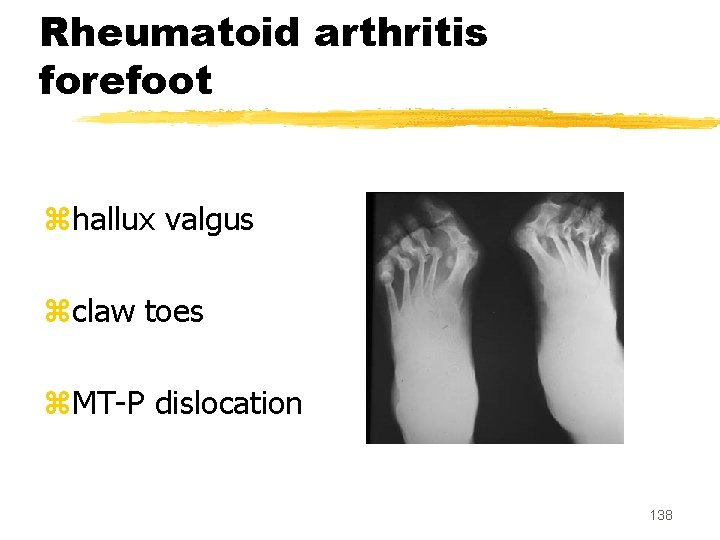
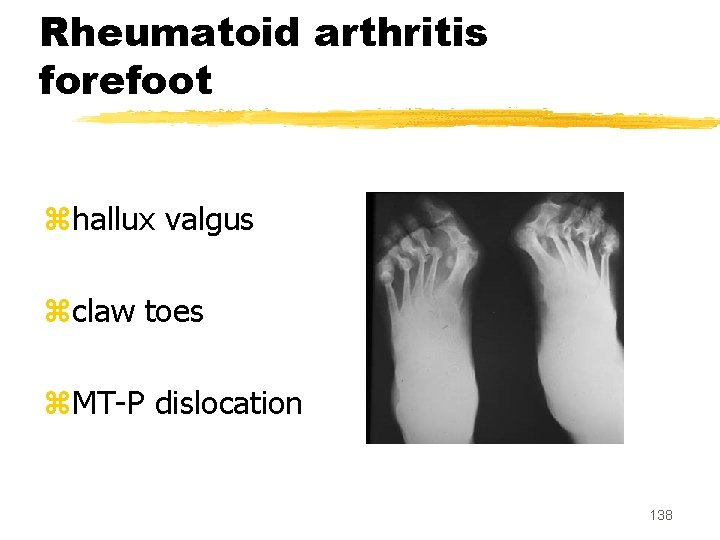
Rheumatoid arthritis forefoot zhallux valgus zclaw toes z. MT-P dislocation 138
Foot pain z. Mechanical pressure • foot-shoe mismatch zjoint inflammation zbone lesion zperipheral vascular disease zmuscle strain 139
Heel pain z. Sever’s disease zheel bumps zperitendonitis zplantar fasciitis • idiopathic • ankylosing spondylitis • Reiter’s disease • gonorrhoea 140
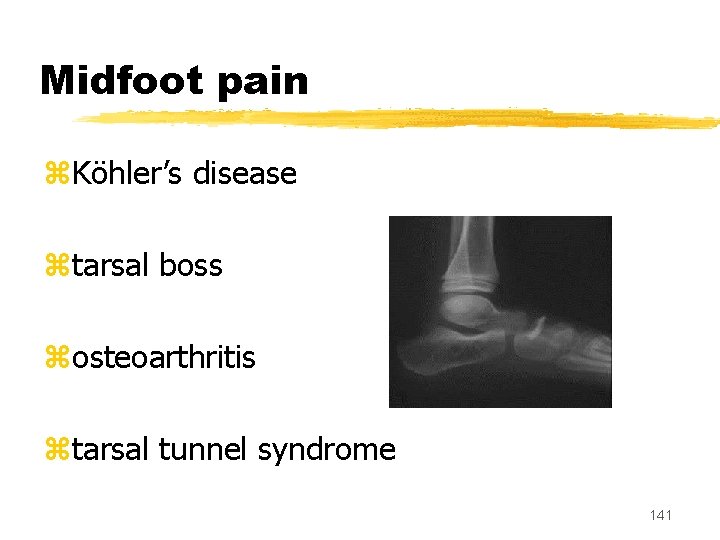
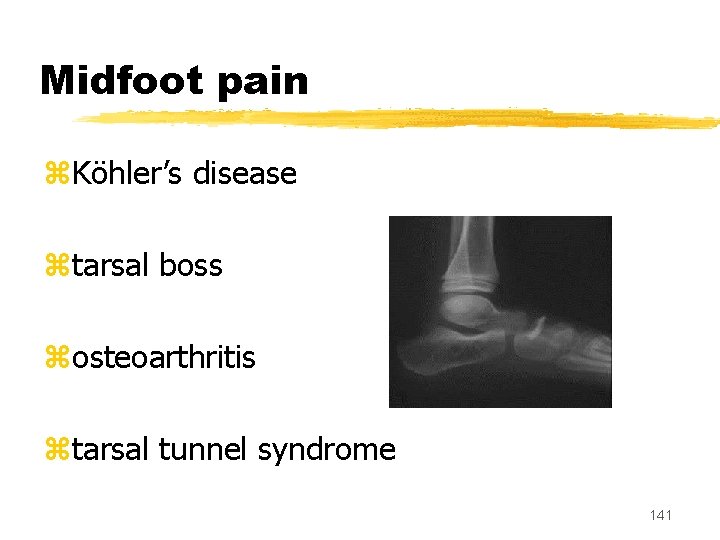
Midfoot pain z. Köhler’s disease ztarsal boss zosteoarthritis ztarsal tunnel syndrome 141
Forefoot pain zhallux valgus zhammer toe z. Freiberg’s disease zstress fracture z. Morton’s neuroma 142
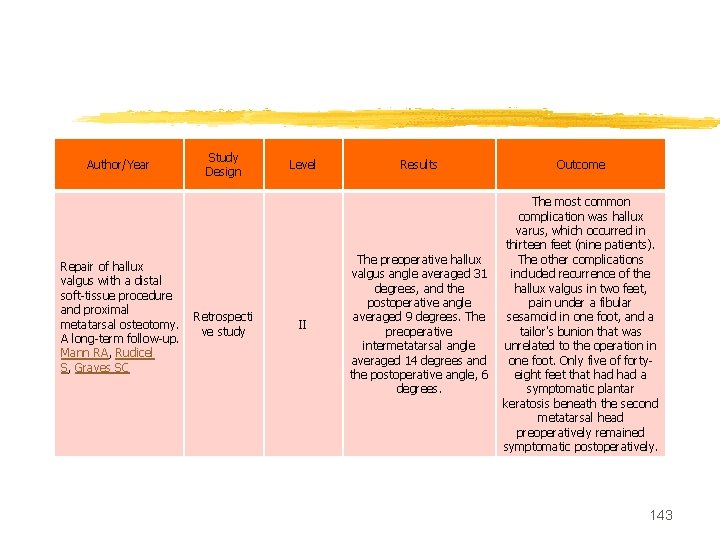
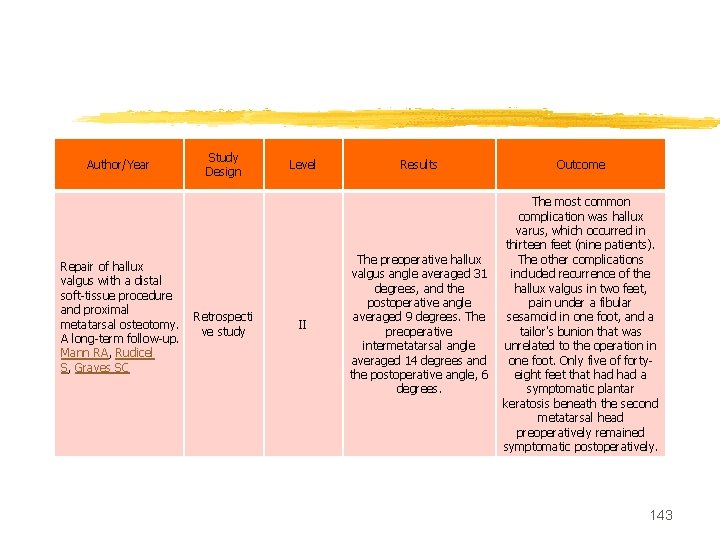
Author/Year Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy. A long-term follow-up. Mann RA, Rudicel S, Graves SC Study Design Retrospecti ve study Level II Results Outcome The preoperative hallux valgus angle averaged 31 degrees, and the postoperative angle averaged 9 degrees. The preoperative intermetatarsal angle averaged 14 degrees and the postoperative angle, 6 degrees. The most common complication was hallux varus, which occurred in thirteen feet (nine patients). The other complications included recurrence of the hallux valgus in two feet, pain under a fibular sesamoid in one foot, and a tailor's bunion that was unrelated to the operation in one foot. Only five of fortyeight feet that had a symptomatic plantar keratosis beneath the second metatarsal head preoperatively remained symptomatic postoperatively. 143
MCQ 1 z. Wrist ganglion most commonly arises from a) Volar b) Dorsal c) Flexor sheath d) None of the above e) All of the above 144
MCQ 2 The causes of forefoot pain include: a) hallux valgus b) hammer toe c) Freiberg’s disease d) stress fracture e) All of the above 145
MCQ 3 z. Dupuytren’s contracture aetiology include a) genetic b) geographical c) smoking d) alcohol e) All of the above 146
MCQ 4 z. The causes of trigger finger include a) idiopathic b) traumatic c) diabetes d) rheumatoid e) All of the above 147
MCQ 5 z. True for dequervain’s tenosynovitis include a) Positive Finkelstein’s test b) Inflammation of first dorsal compartment c) Both of the above d) All of the above e) Tenderness at radial styloid 148
MCQ 6 z. Common treatments for tennis elbow are: a) Rehabilitation. b) Use of a forearm brace. c) Use of injections of cortisone. d) Strengthening and stretching exercises e) All of the above 149
MCQ 7 z. True for tennis elbow are all except a) Lateral epicondylitis b) Common extensor origin c) Elbow brace can be given d) All of the above e) None of the above 150
MCQ 8 z. True for tennis elbow are all except a) Affects 1 -3 per 1000 population b) Affects 40 -50 years male c) Affects tennis players and golfers d) All of the above e) None of the above 151
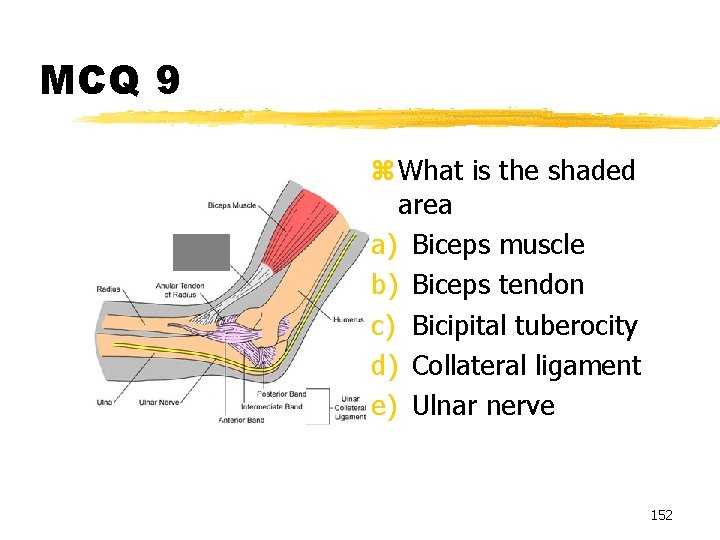
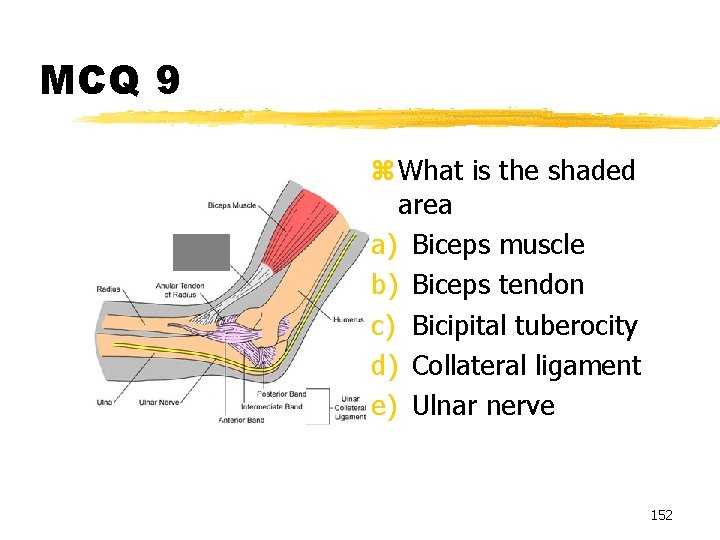
MCQ 9 z What is the shaded area a) Biceps muscle b) Biceps tendon c) Bicipital tuberocity d) Collateral ligament e) Ulnar nerve 152
MCQ 10 The symptoms of tennis elbow are a) Pain along the lateral epicondyle while performing wrist extension against resistance. b) Point tenderness to joint and musculature. c) Inflammation d) Loss of normal range of motion and function e) All of the above 153
MCQ 11 Supraglenoid tubercle is a) 5 mm medial to the superior edge of the glenoid rim b) 5 mm lateral to the superior edge of the glenoid rim c) 5 mm medial to the inferior edge of the glenoid rim d) 5 mm lateral to the inferior edge of the glenoid rim 154 e) None of the above

MCQ 12 z. Long head of biceps tendon is attached to: a) Supraglenoid tubercle b) Infraglenoid tubercle c) Lateral to the glenoid cavity d) Medial to the glenoid cavity e) None of the above 155
MCQ 13 z. Budford complex is: a) Normal Variant found in 1. 5% of the shoulders. b) Abnormal variant c) Both of the above d) None of the above e) Normal variant in 3% of the shoulders 156
MCQ 14 Labrum is a a) fibrocartilaginous tissue with sparse elastin fibers b) Synovial tissue c) Elastic tissue d) All of the above e) None of the above 157
MCQ 15 z. Term SLAP is: a) Superior Labrum Anterior and Posterior b) Supra Labral Tear c) Superior labrum and past tear d) All of the above e) None of the above 158