Immunity III Lymphatic System Lecture Outline 1 Introduction


- Slides: 35
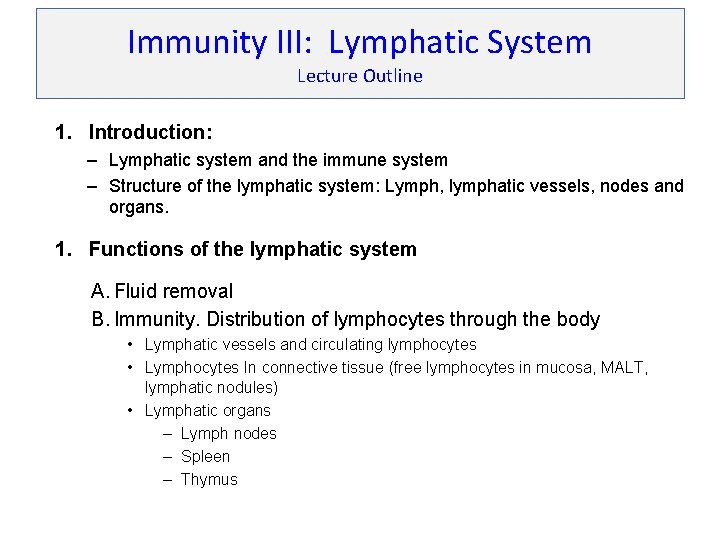
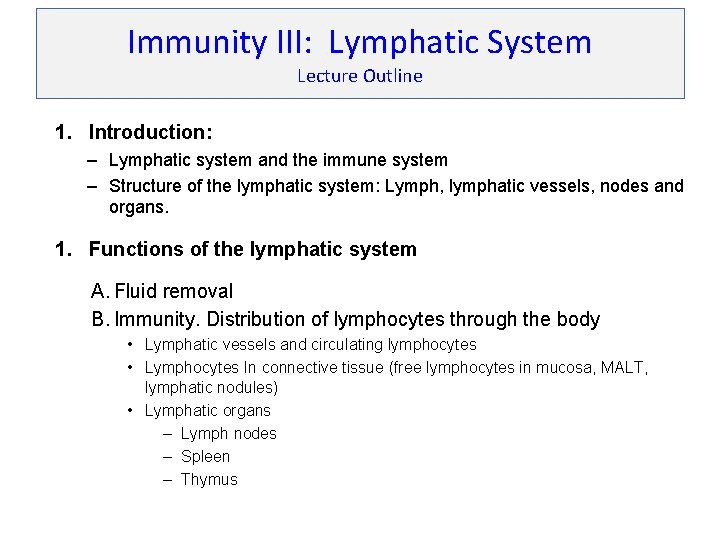
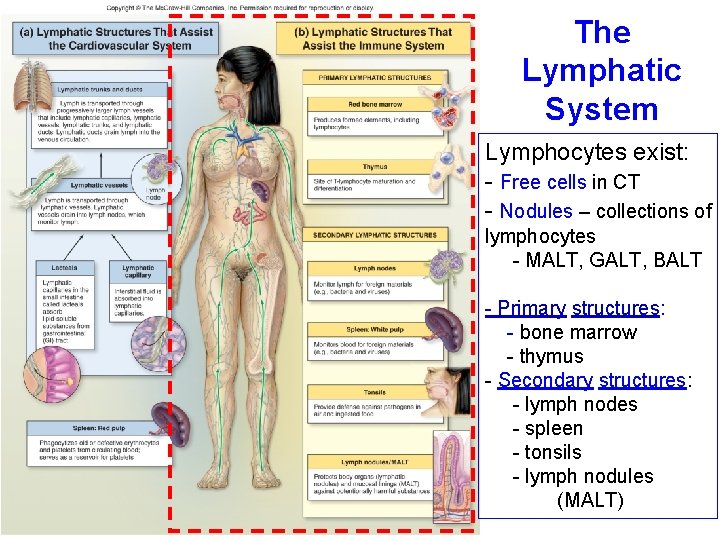
Immunity III: Lymphatic System Lecture Outline 1. Introduction: – Lymphatic system and the immune system – Structure of the lymphatic system: Lymph, lymphatic vessels, nodes and organs. 1. Functions of the lymphatic system A. Fluid removal B. Immunity. Distribution of lymphocytes through the body • Lymphatic vessels and circulating lymphocytes • Lymphocytes In connective tissue (free lymphocytes in mucosa, MALT, lymphatic nodules) • Lymphatic organs – Lymph nodes – Spleen – Thymus
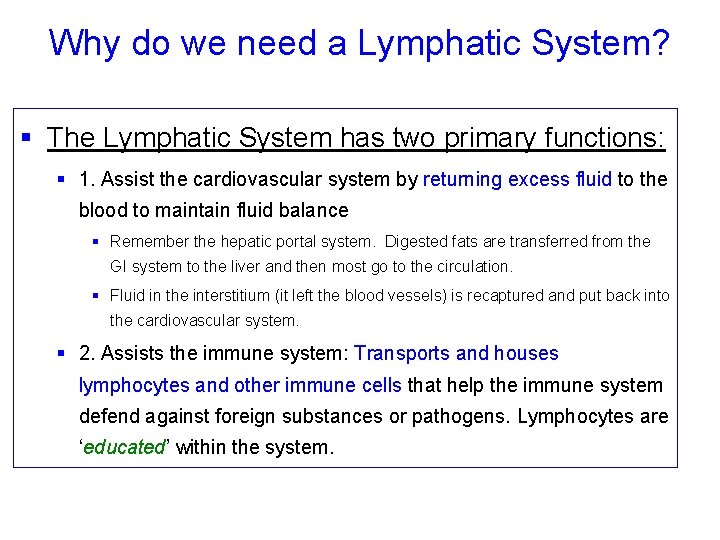
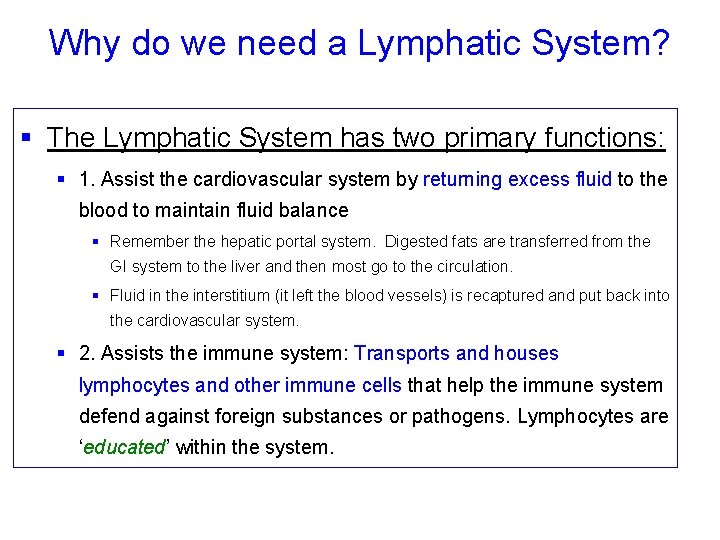
Why do we need a Lymphatic System? § The Lymphatic System has two primary functions: § 1. Assist the cardiovascular system by returning excess fluid to the blood to maintain fluid balance § Remember the hepatic portal system. Digested fats are transferred from the GI system to the liver and then most go to the circulation. § Fluid in the interstitium (it left the blood vessels) is recaptured and put back into the cardiovascular system. § 2. Assists the immune system: Transports and houses lymphocytes and other immune cells that help the immune system defend against foreign substances or pathogens. Lymphocytes are ‘educated’ within the system.
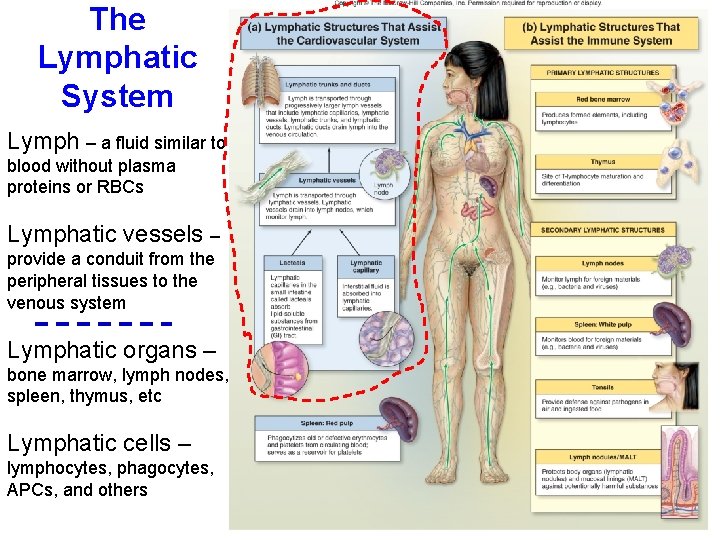
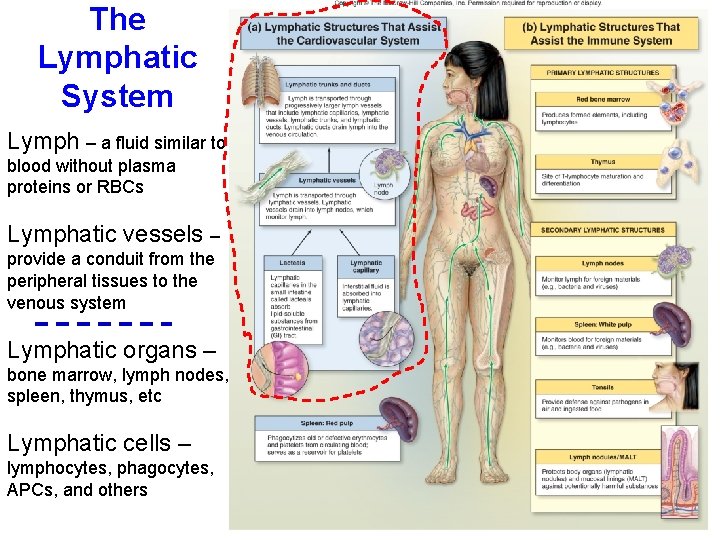
The Lymphatic System Lymph – a fluid similar to blood without plasma proteins or RBCs Lymphatic vessels – provide a conduit from the peripheral tissues to the venous system Lymphatic organs – bone marrow, lymph nodes, spleen, thymus, etc Lymphatic cells – lymphocytes, phagocytes, APCs, and others
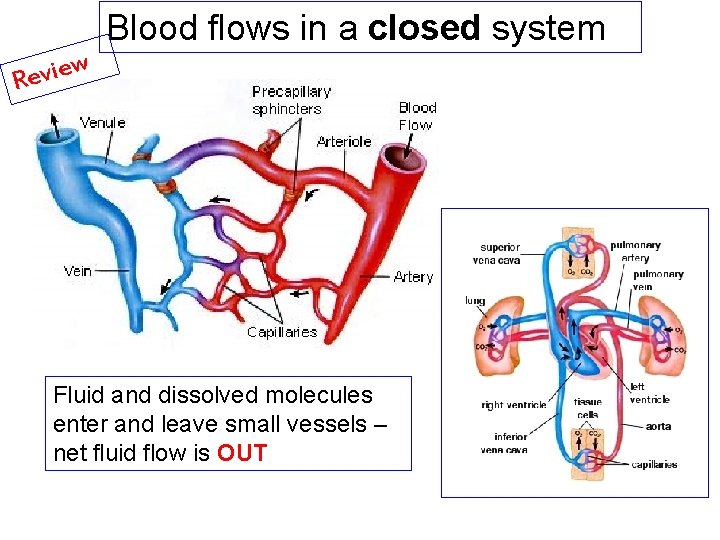
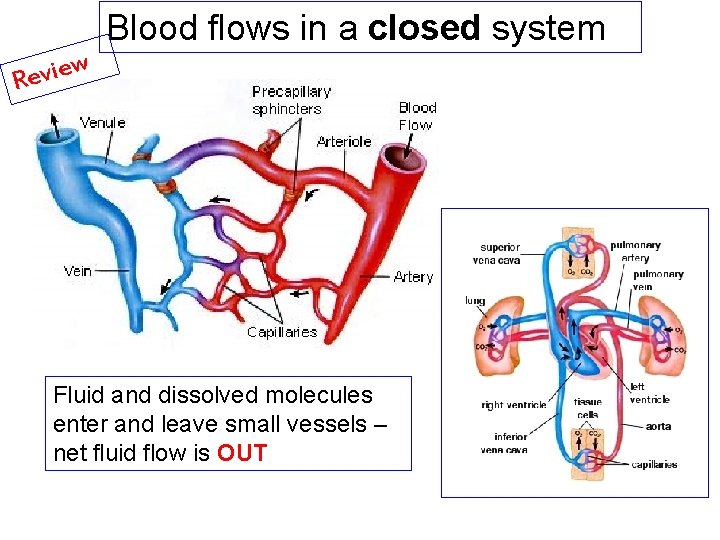
Blood flows in a closed system w e i v e R Fluid and dissolved molecules enter and leave small vessels – net fluid flow is OUT
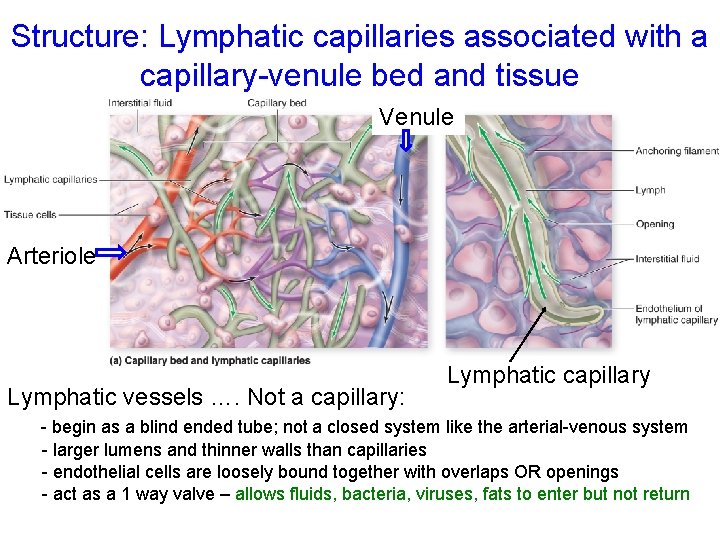
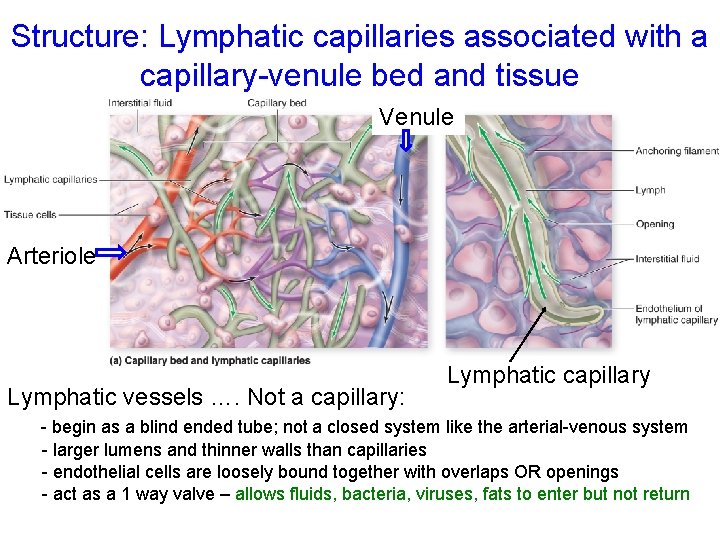
Structure: Lymphatic capillaries associated with a capillary-venule bed and tissue Venule Arteriole Lymphatic vessels …. Not a capillary: Lymphatic capillary - begin as a blind ended tube; not a closed system like the arterial-venous system - larger lumens and thinner walls than capillaries - endothelial cells are loosely bound together with overlaps OR openings - act as a 1 way valve – allows fluids, bacteria, viruses, fats to enter but not return
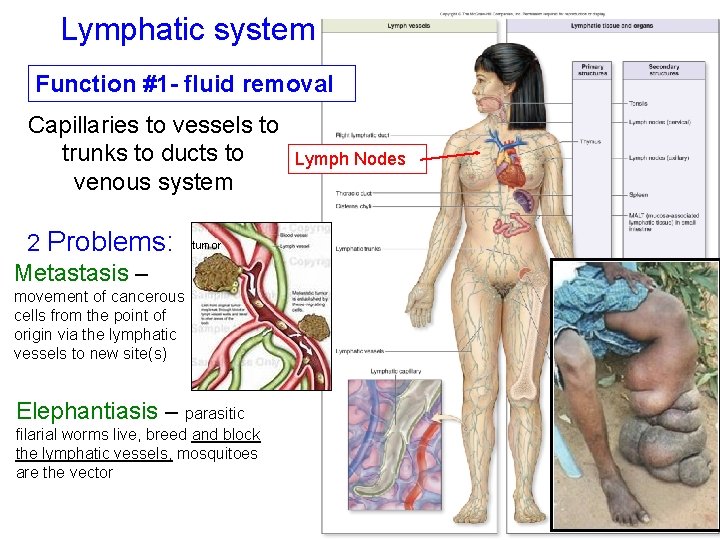
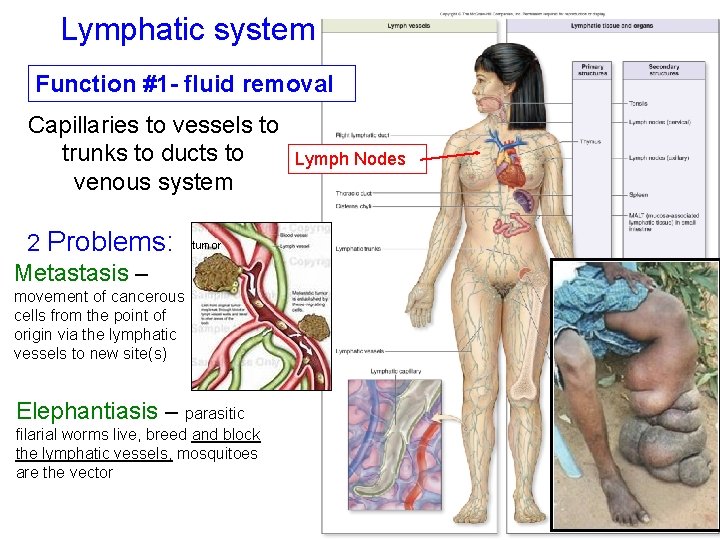
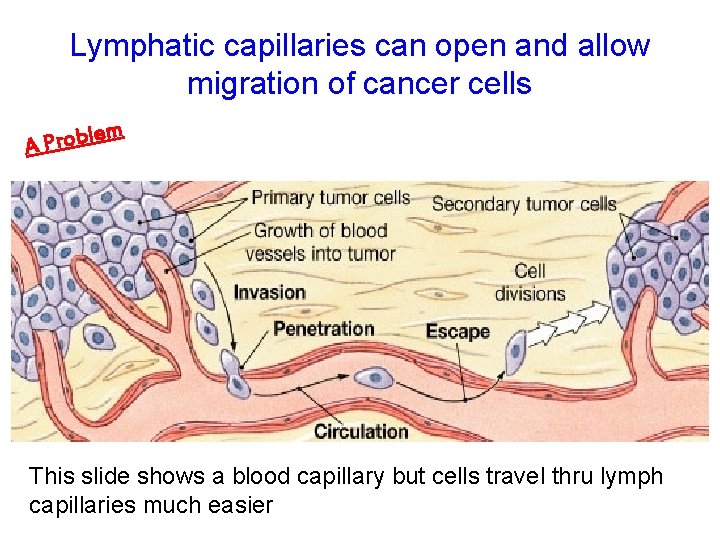
Lymphatic system Function #1 - fluid removal Capillaries to vessels to trunks to ducts to venous system 2 Problems: Metastasis – tumor movement of cancerous cells from the point of origin via the lymphatic vessels to new site(s) Elephantiasis – parasitic filarial worms live, breed and block the lymphatic vessels, mosquitoes are the vector Lymph Nodes
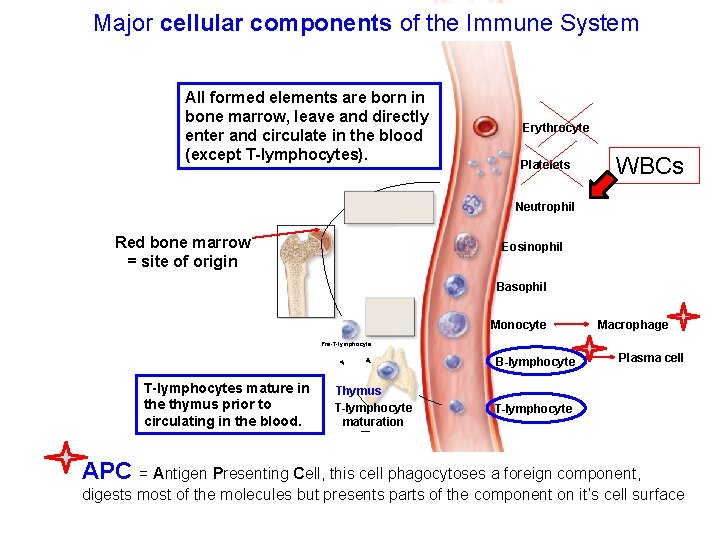
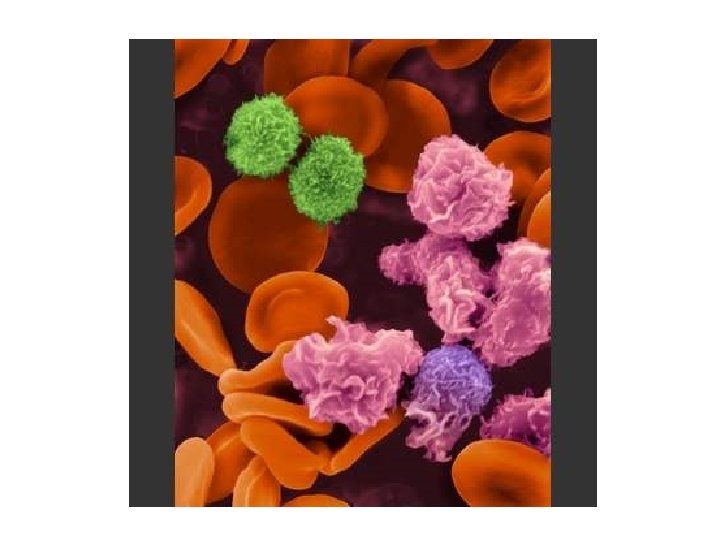
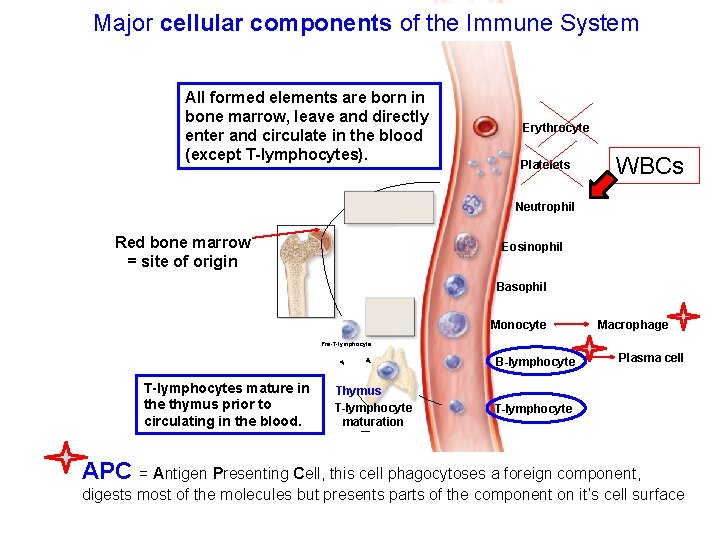
Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Major cellular components of the Immune System All formed elements are born in bone marrow, leave and directly enter and circulate in the blood (except T-lymphocytes). Erythrocyte Platelets WBCs Neutrophil Red bone marrow = site of origin Eosinophil Basophil Monocyte Macrophage Pre-T-lymphocyte B-lymphocyte T-lymphocytes mature in the thymus prior to circulating in the blood. Thymus T-lymphocyte maturation Plasma cell T-lymphocyte APC = Antigen Presenting Cell, this cell phagocytoses a foreign component, digests most of the molecules but presents parts of the component on it’s cell surface
Function #2 of the Lymphatic System: involvement with Immunity o Centered around the Production, Maintenance, and Distribution of lymphocytes o Lymphocytes are produced in o red bone marrow and then ‘educated’ in bone marrow or ‘educated’ in the thymus o ‘Educated’ lymphocytes are then located in o Connective tissues or lymphatic tissues (e. g. , tonsils) o Lymphatic organs (e. g. , spleen, thymus, lymph nodes) o Lymphocyte distribution varies depending on health and injury site or infection
General aspects about lymphocytes § Education of lymphocytes § Occurs in bone marrow and B lymphocytes leave § Occurs in thymus and T lymphocytes leave § Migrate via blood vessels or lymphatic vessels to occupy: § Connective tissue (CT) as free cells or in lymphatic nodules § Lymph nodes § Spleen § ‘Like soldiers in the field – just waiting …”
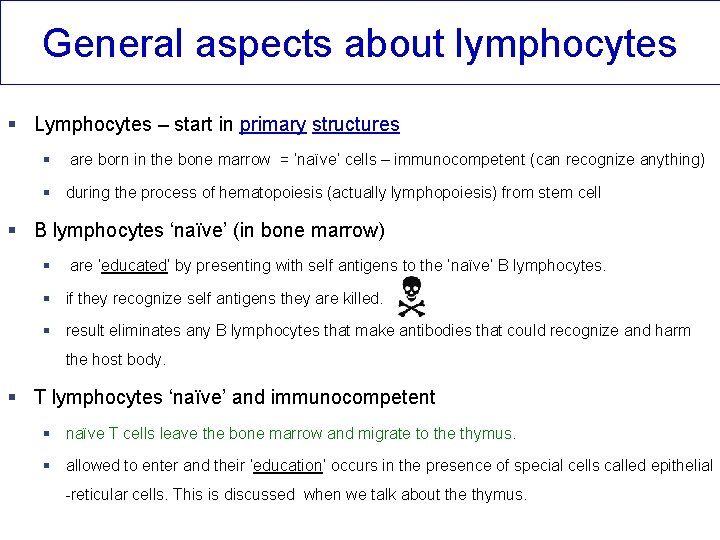
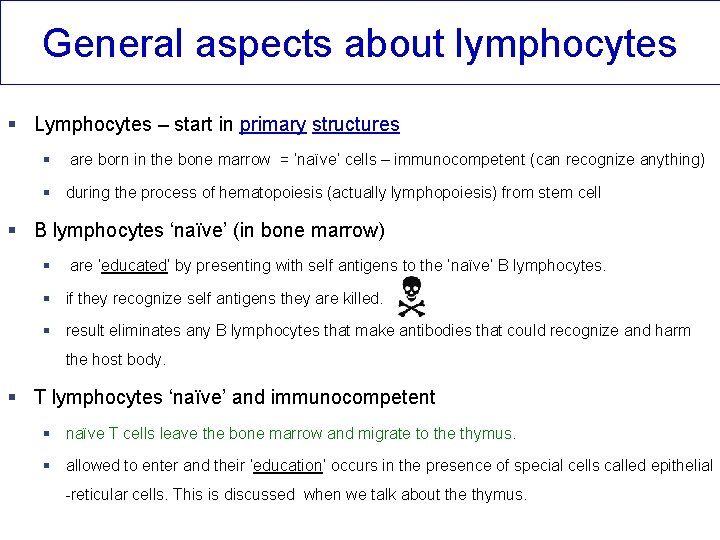
General aspects about lymphocytes § Lymphocytes – start in primary structures § are born in the bone marrow = ‘naïve’ cells – immunocompetent (can recognize anything) § during the process of hematopoiesis (actually lymphopoiesis) from stem cell § B lymphocytes ‘naïve’ (in bone marrow) § are ‘educated’ by presenting with self antigens to the ‘naïve’ B lymphocytes. § if they recognize self antigens they are killed. § result eliminates any B lymphocytes that make antibodies that could recognize and harm the host body. § T lymphocytes ‘naïve’ and immunocompetent § naïve T cells leave the bone marrow and migrate to the thymus. § allowed to enter and their ‘education’ occurs in the presence of special cells called epithelial -reticular cells. This is discussed when we talk about the thymus.
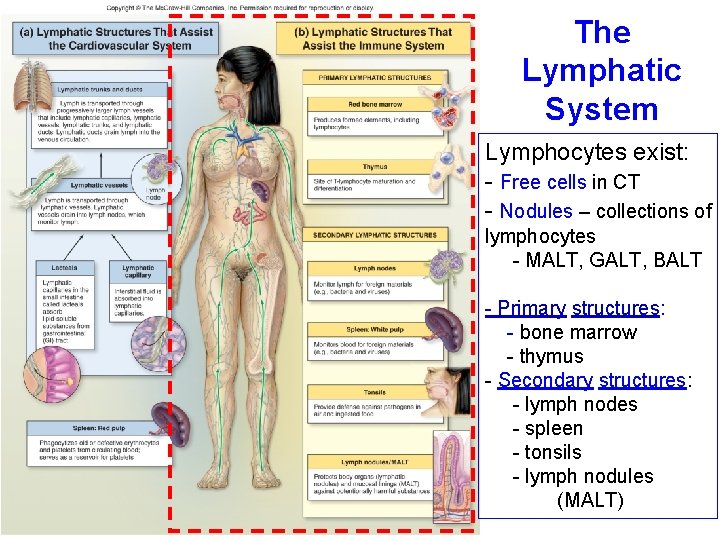
The Lymphatic System Lymphocytes exist: - Free cells in CT - Nodules – collections of lymphocytes - MALT, GALT, BALT - Primary structures: - bone marrow - thymus - Secondary structures: - lymph nodes - spleen - tonsils - lymph nodules (MALT)
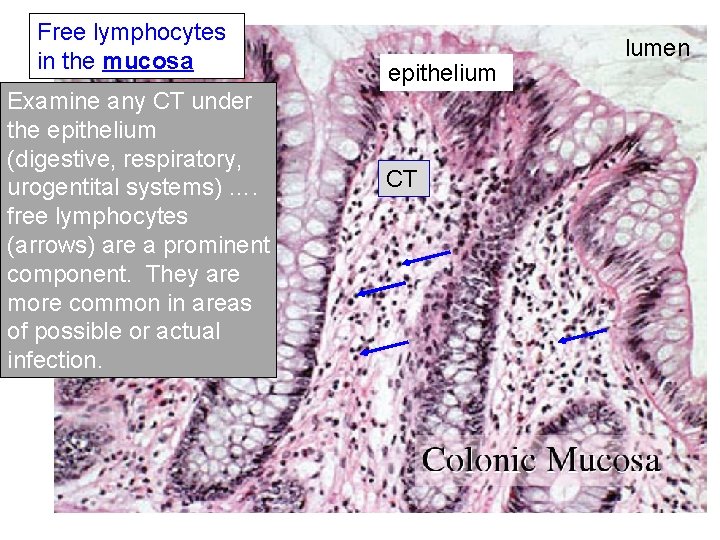
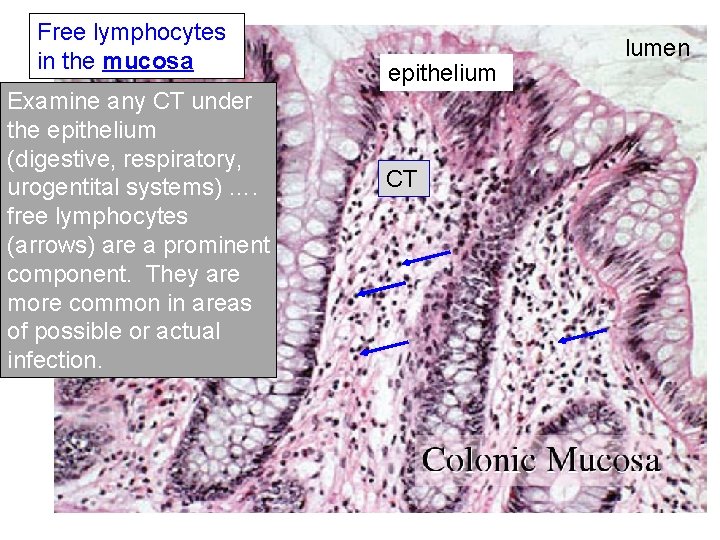
Free lymphocytes in the mucosa Examine any CT under the epithelium (digestive, respiratory, urogentital systems) …. free lymphocytes (arrows) are a prominent component. They are more common in areas of possible or actual infection. epithelium CT Colonic Mucosa lumen
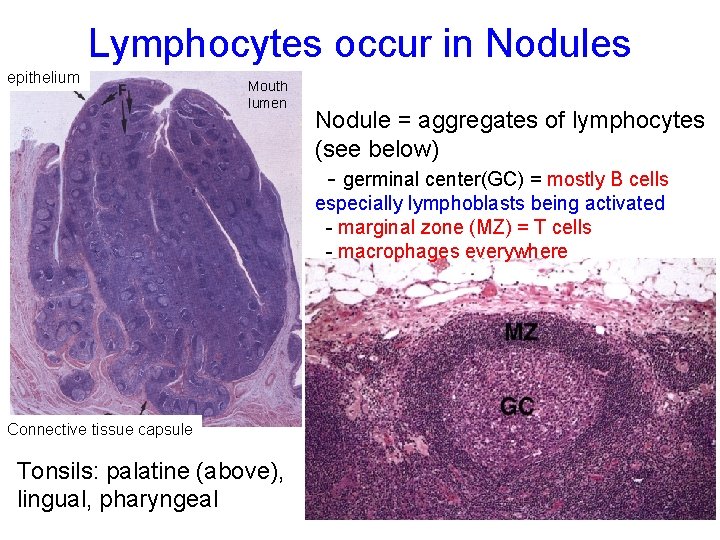
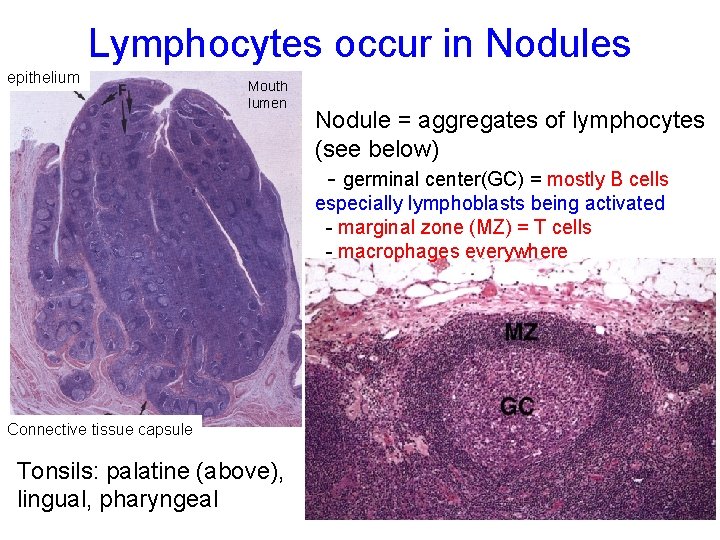
Lymphocytes occur in Nodules epithelium Mouth lumen Nodule = aggregates of lymphocytes (see below) - germinal center(GC) = mostly B cells especially lymphoblasts being activated - marginal zone (MZ) = T cells - macrophages everywhere Connective tissue capsule Tonsils: palatine (above), lingual, pharyngeal
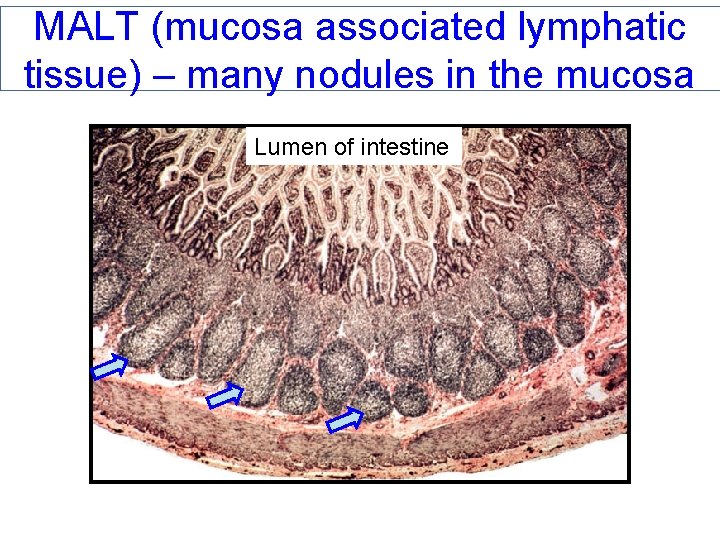
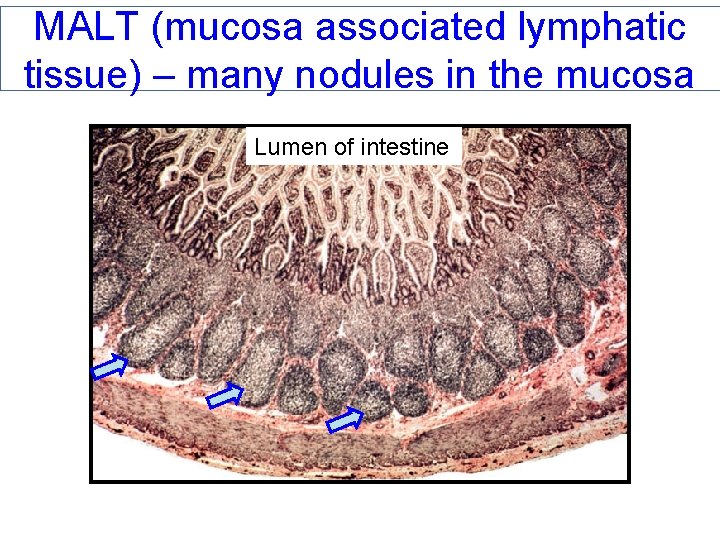
MALT (mucosa associated lymphatic tissue) – many nodules in the mucosa Lumen of intestine
Lymphatic Organs = Secondary Structures • Lymphatic Organs • Lymph nodes • Spleen • Thymus • 20 structures are separated from surrounding tissues by a fibrous connective tissue capsule (lymphatic nodules are not!)
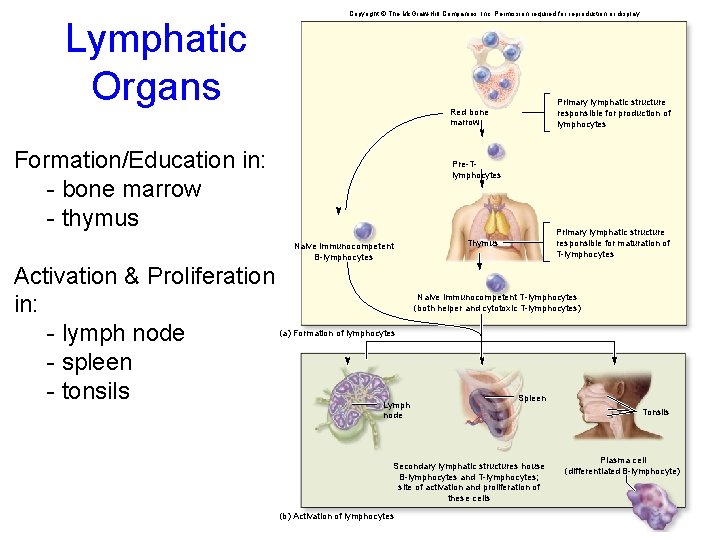
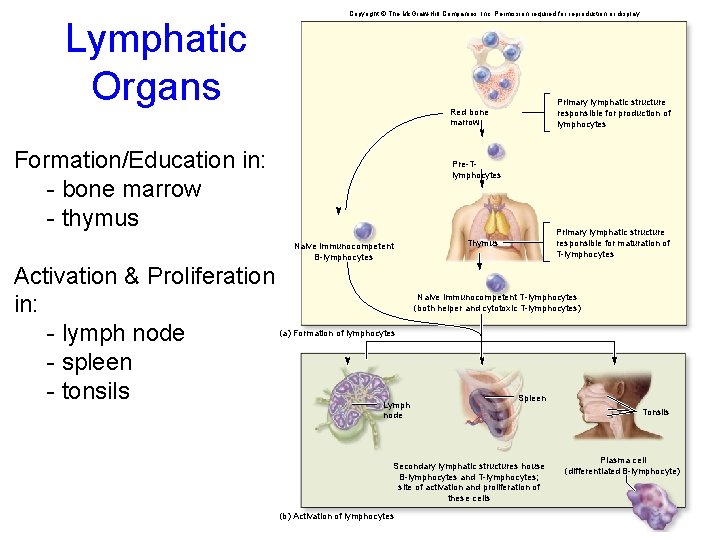
Lymphatic Organs Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Formation/Education in: - bone marrow - thymus Pre-Tlymphocytes Naive immunocompetent B-lymphocytes Activation & Proliferation in: - lymph node - spleen - tonsils Primary lymphatic structure responsible for production of lymphocytes Red bone marrow Primary lymphatic structure responsible for maturation of T-lymphocytes Thymus Naive immunocompetent T-lymphocytes (both helper and cytotoxic T-lymphocytes) (a) Formation of lymphocytes Lymph node Spleen Secondary lymphatic structures house B-lymphocytes and T-lymphocytes; site of activation and proliferation of these cells (b) Activation of lymphocytes Tonsils Plasma cell (differentiated B-lymphocyte)
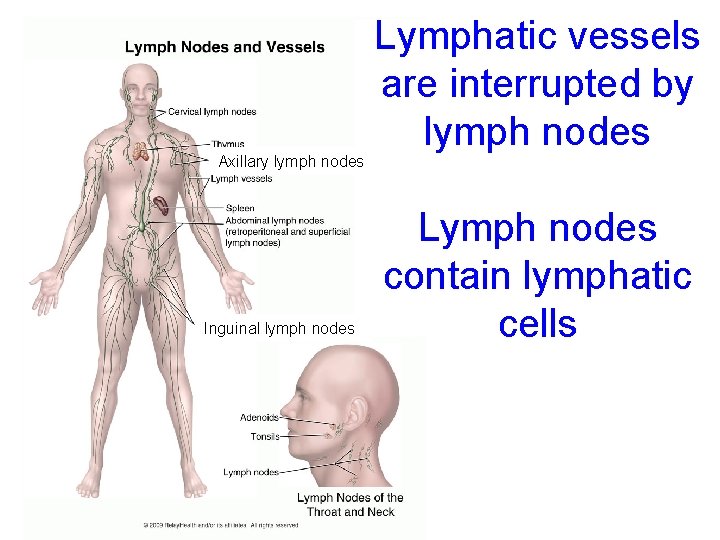
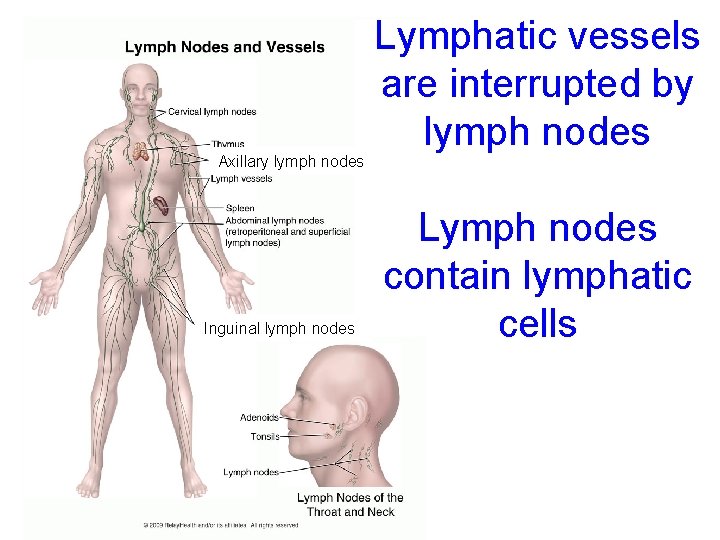
Axillary lymph nodes Inguinal lymph nodes Lymphatic vessels are interrupted by lymph nodes Lymph nodes contain lymphatic cells
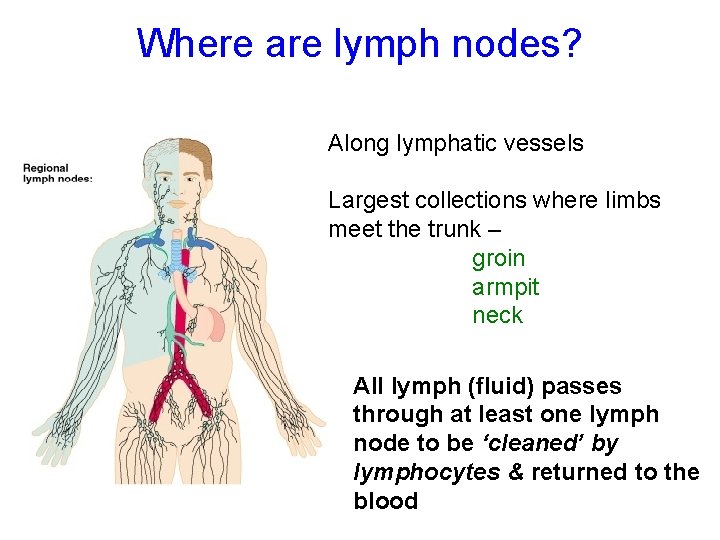
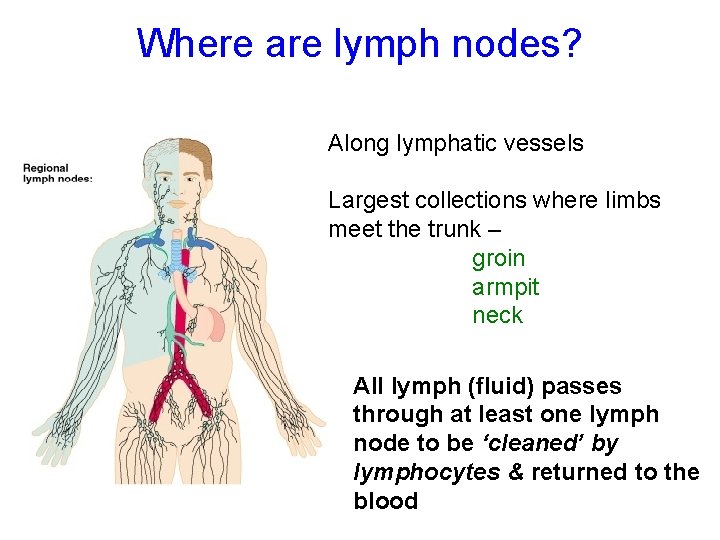
Where are lymph nodes? Along lymphatic vessels Largest collections where limbs meet the trunk – groin armpit neck All lymph (fluid) passes through at least one lymph node to be ‘cleaned’ by lymphocytes & returned to the blood
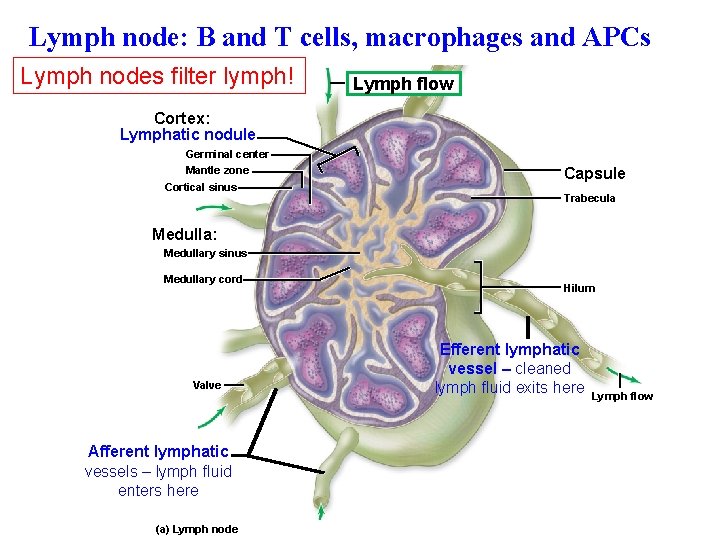
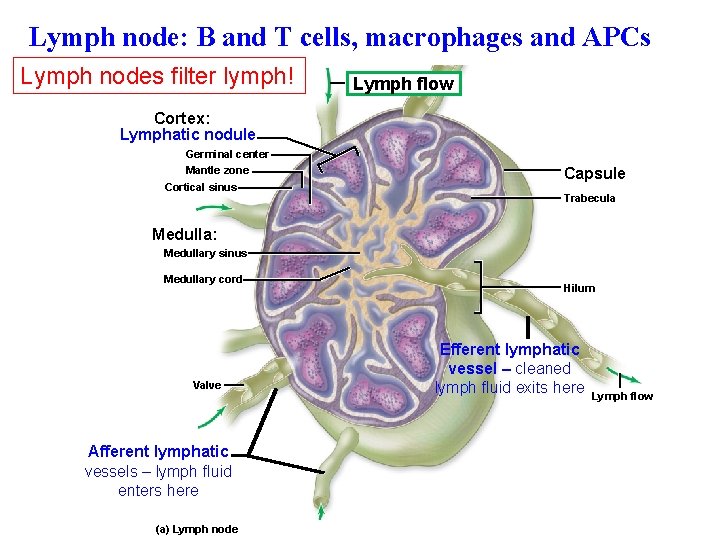
Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Lymph node: B and T cells, macrophages and APCs Lymph nodes filter lymph! Lymph flow Cortex: Lymphatic nodule Germinal center Mantle zone Cortical sinus Capsule Trabecula Medulla: Medullary sinus Medullary cord Valve Afferent lymphatic vessels – lymph fluid enters here (a) Lymph node Hilum Efferent lymphatic vessel – cleaned lymph fluid exits here Lymph flow
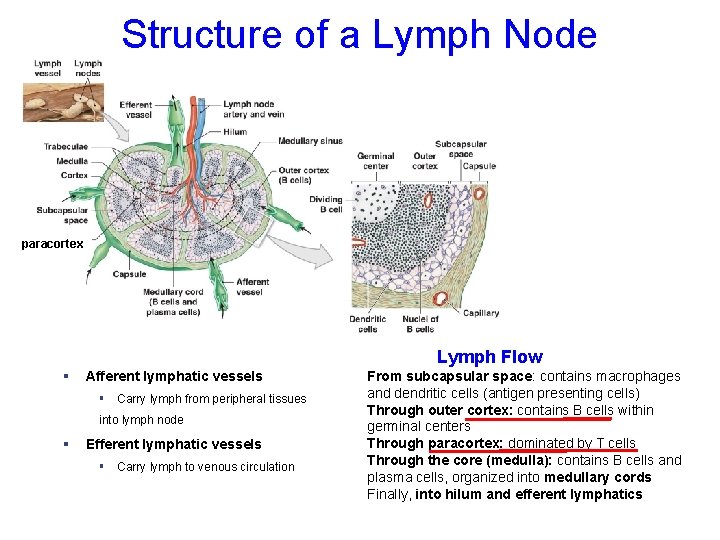
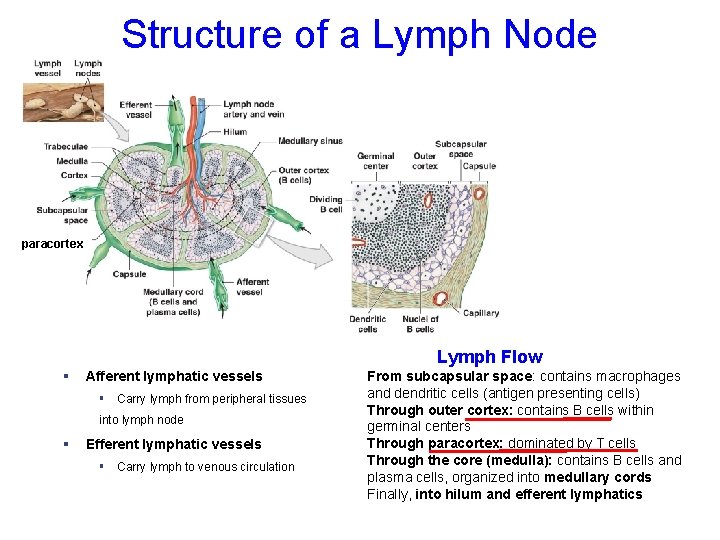
Structure of a Lymph Node paracortex Lymph Flow § Afferent lymphatic vessels § Carry lymph from peripheral tissues into lymph node § Efferent lymphatic vessels § Carry lymph to venous circulation From subcapsular space: contains macrophages and dendritic cells (antigen presenting cells) Through outer cortex: contains B cells within germinal centers Through paracortex: dominated by T cells Through the core (medulla): contains B cells and plasma cells, organized into medullary cords Finally, into hilum and efferent lymphatics
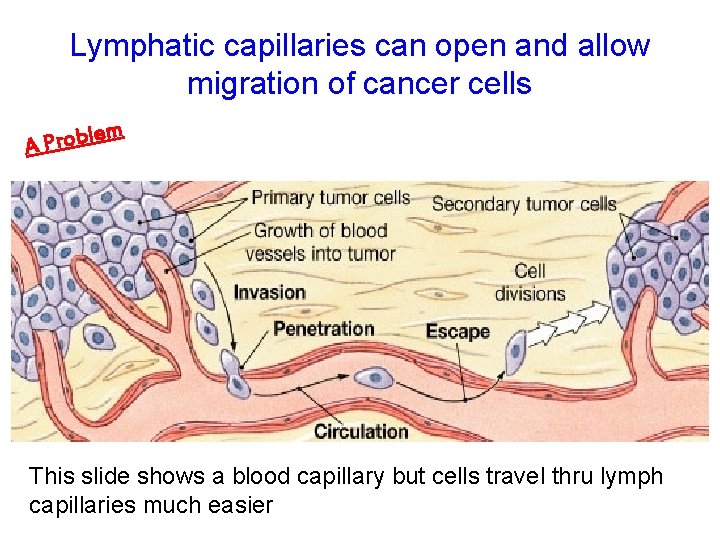
Lymphatic capillaries can open and allow migration of cancer cells lem b o r P A This slide shows a blood capillary but cells travel thru lymph capillaries much easier
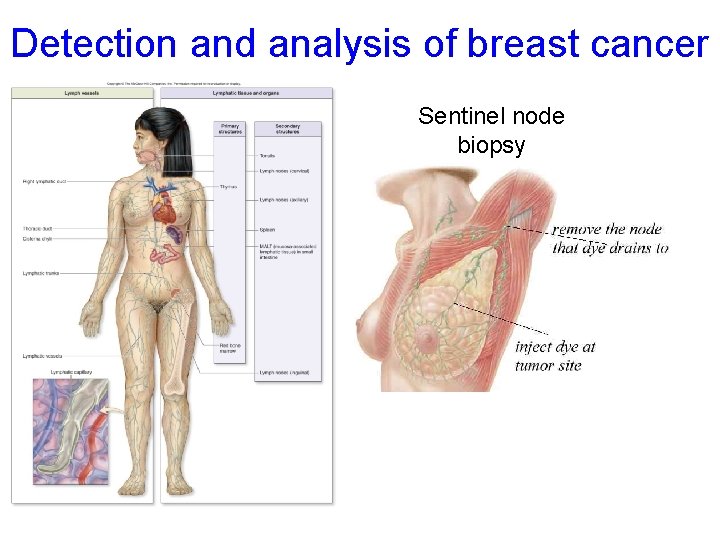
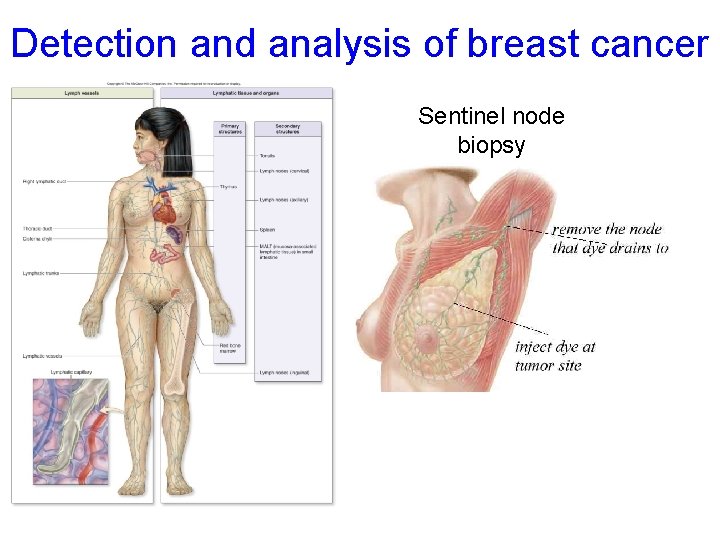
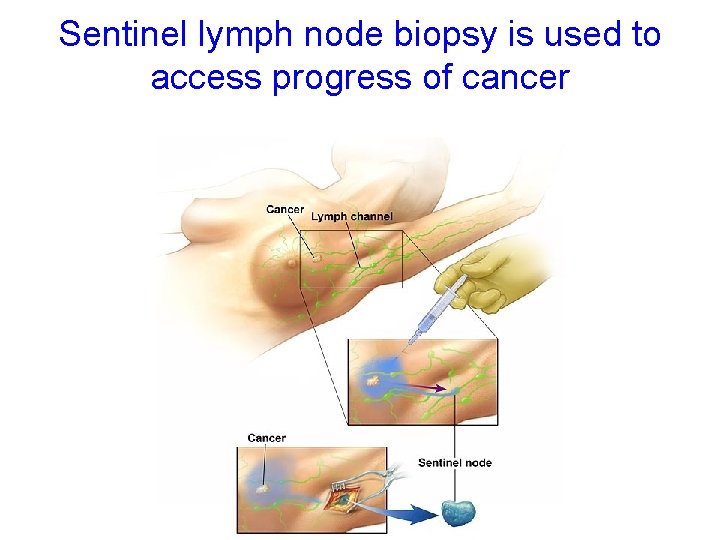
Detection and analysis of breast cancer Sentinel node biopsy
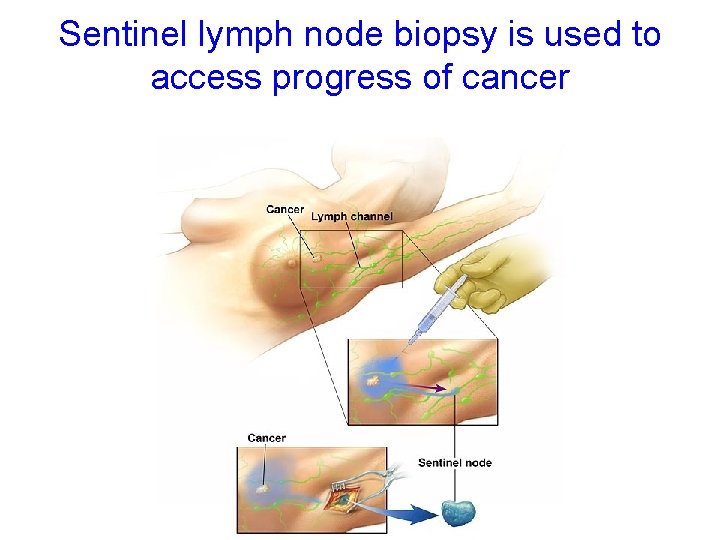
Sentinel lymph node biopsy is used to access progress of cancer
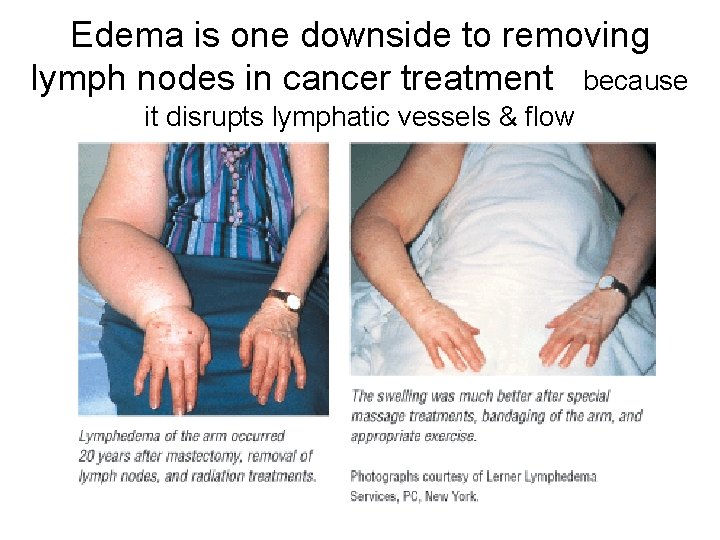
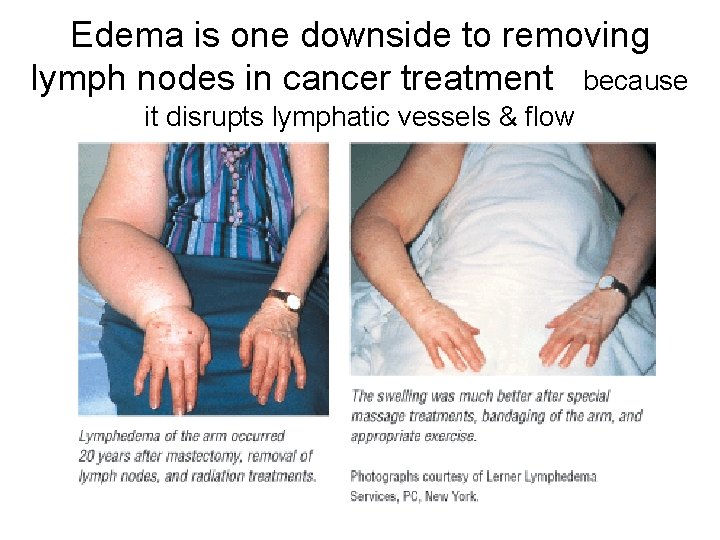
Edema is one downside to removing lymph nodes in cancer treatment because it disrupts lymphatic vessels & flow
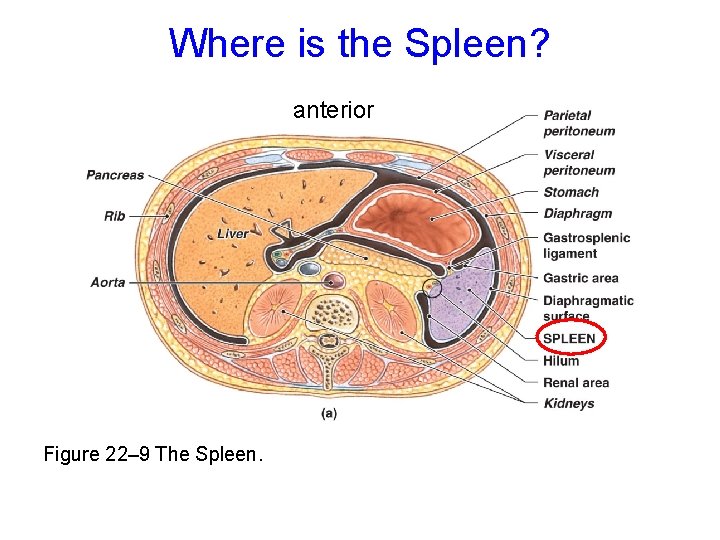
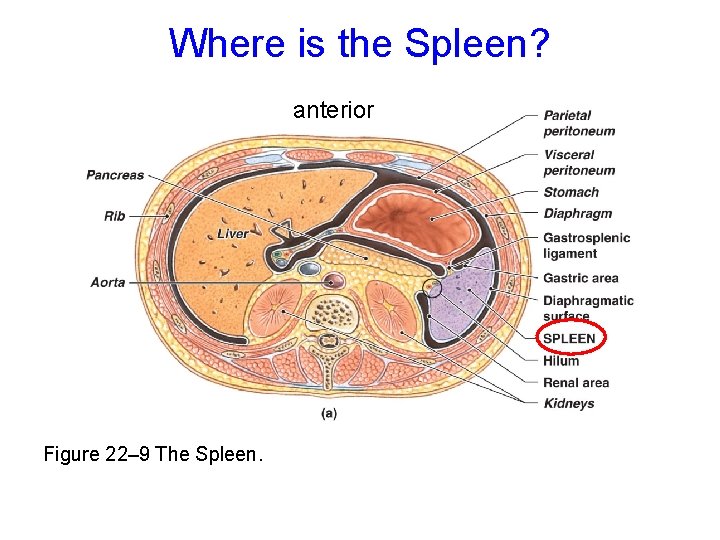
Where is the Spleen? anterior Figure 22– 9 The Spleen.
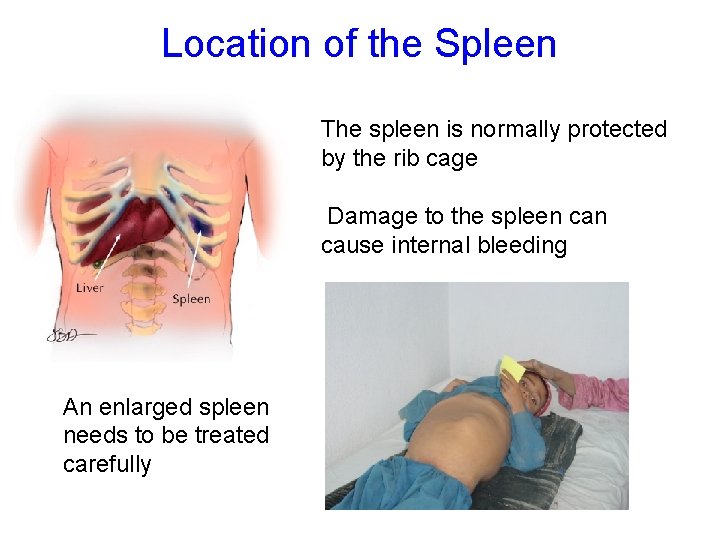
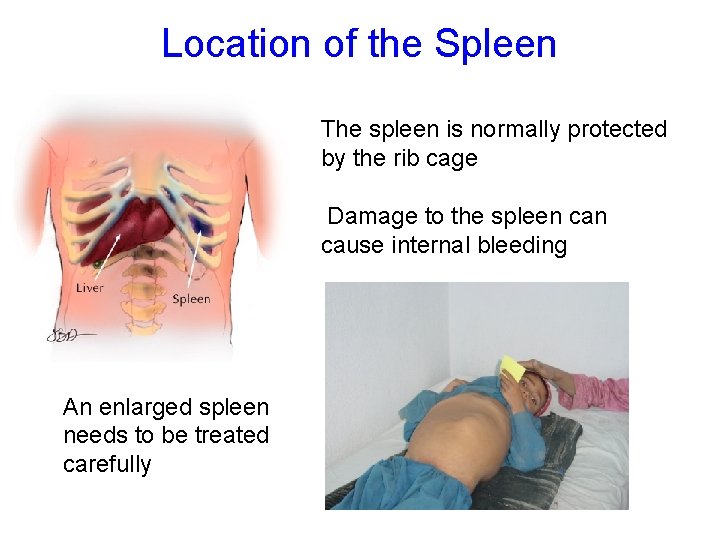
Location of the Spleen The spleen is normally protected by the rib cage Damage to the spleen cause internal bleeding An enlarged spleen needs to be treated carefully
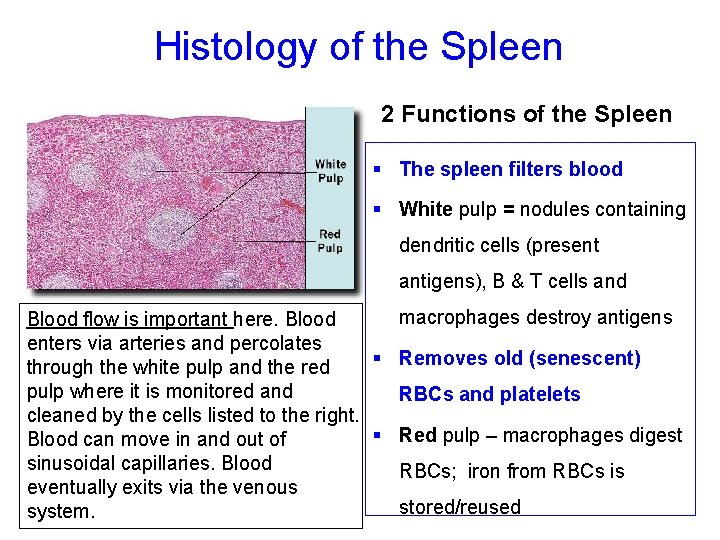
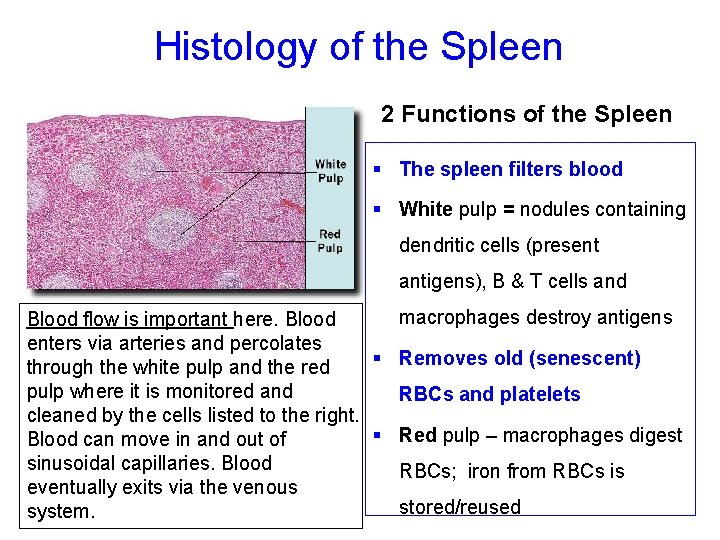
Histology of the Spleen 2 Functions of the Spleen § The spleen filters blood § White pulp = nodules containing dendritic cells (present antigens), B & T cells and macrophages destroy antigens Blood flow is important here. Blood enters via arteries and percolates § Removes old (senescent) through the white pulp and the red pulp where it is monitored and RBCs and platelets cleaned by the cells listed to the right. § Red pulp – macrophages digest Blood can move in and out of sinusoidal capillaries. Blood RBCs; iron from RBCs is eventually exits via the venous stored/reused system.
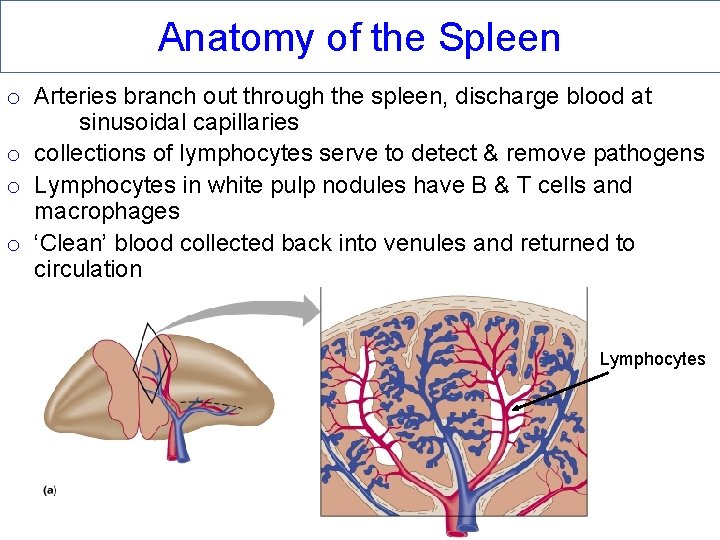
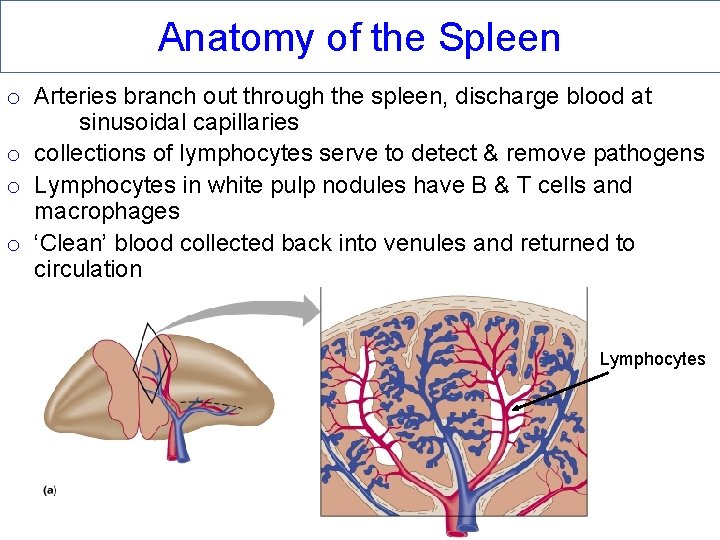
Anatomy of the Spleen o Arteries branch out through the spleen, discharge blood at sinusoidal capillaries o collections of lymphocytes serve to detect & remove pathogens o Lymphocytes in white pulp nodules have B & T cells and macrophages o ‘Clean’ blood collected back into venules and returned to circulation Lymphocytes

Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Thyroid gland Fig. 21. 5 Trachea Thymus Lungs Heart Diaphragm (a) Child (left) and adult (right) thorax, anterior view Thymic tissue Trabecula Cortex Adipose connective tissue Capsule LM 5 x LM 20 x Medulla (b) Micrograph of child’s thymus (c) Micrograph of adult’s thymus b : © The Mc. Graw-Hill Companies, Inc. /Al Telser, photographer; c: © Dr. Thomas Caceci, Virginia- Maryland Regional College of Veterinary Medicine involution
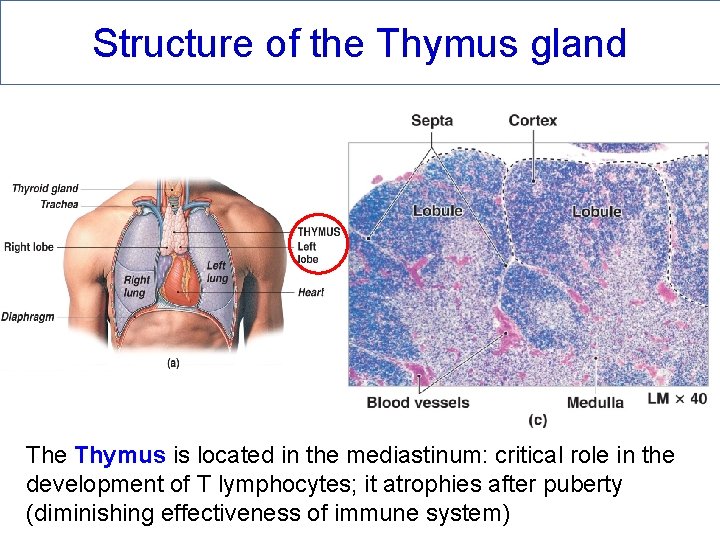
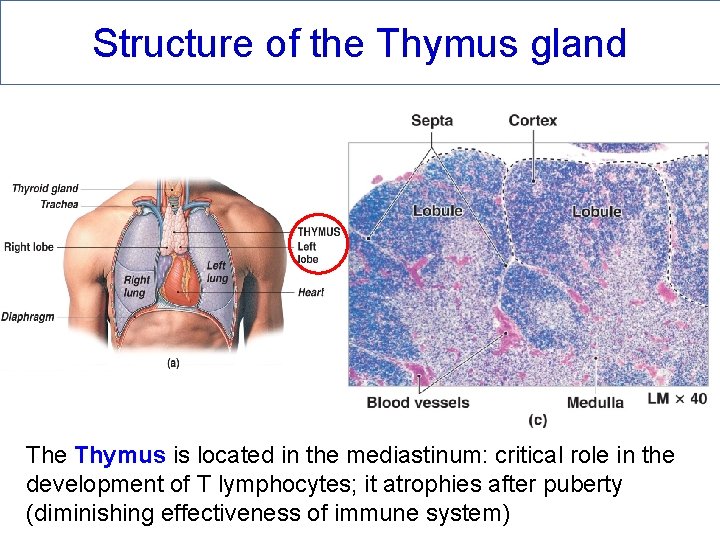
Structure of the Thymus gland The Thymus is located in the mediastinum: critical role in the development of T lymphocytes; it atrophies after puberty (diminishing effectiveness of immune system)
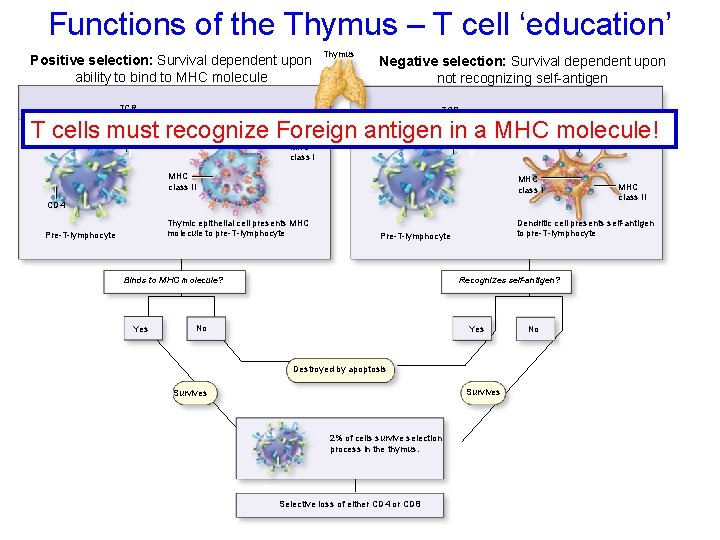
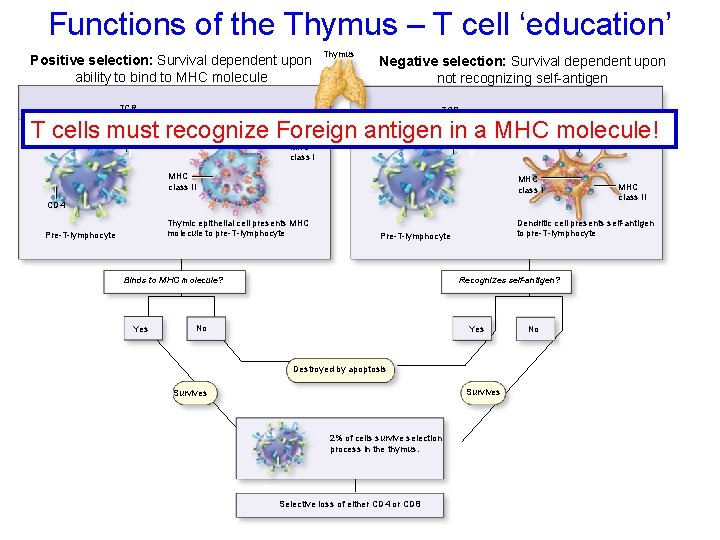
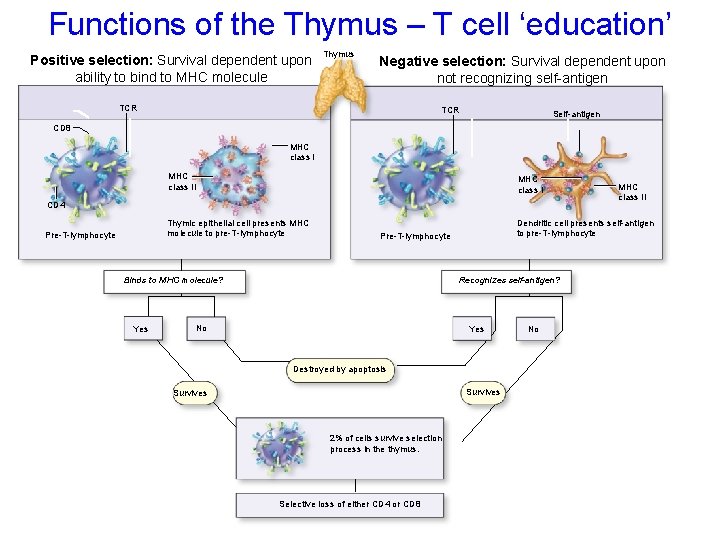
Functions of the Thymus – T cell ‘education’ Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Positive selection: Survival dependent upon ability to bind to MHC molecule Thymus Negative selection: Survival dependent upon not recognizing self-antigen TCR Self-antigen T cells must recognize Foreign antigen in a MHC molecule! CD 8 MHC class II MHC class I CD 4 Thymic epithelial cell presents MHC molecule to pre-T-lymphocyte Pre-T-lymphocyte Yes Dendritic cell presents self-antigen to pre-T-lymphocyte Pre-T-lymphocyte Recognizes self-antigen? Binds to MHC molecule? No Yes Destroyed by apoptosis Survives 2% of cells survive selection process in the thymus. Selective loss of either CD 4 or CD 8 MHC class II No
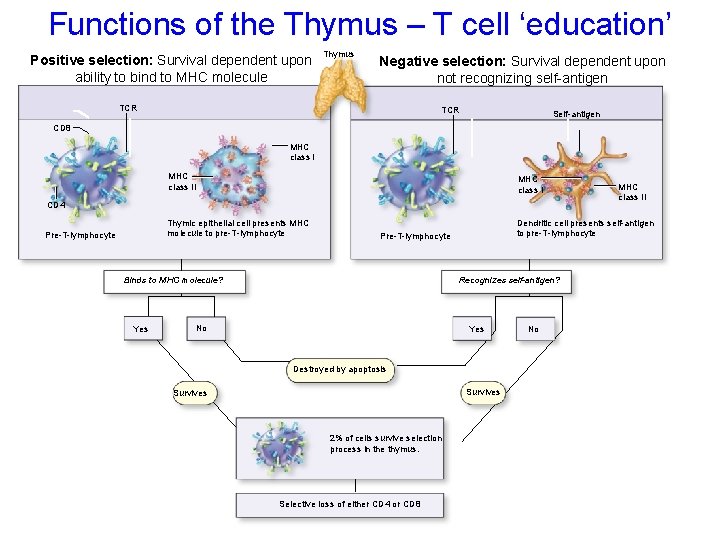
Functions of the Thymus – T cell ‘education’ Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Positive selection: Survival dependent upon ability to bind to MHC molecule Thymus Negative selection: Survival dependent upon not recognizing self-antigen TCR Self-antigen CD 8 MHC class II MHC class I CD 4 Thymic epithelial cell presents MHC molecule to pre-T-lymphocyte Pre-T-lymphocyte Yes Dendritic cell presents self-antigen to pre-T-lymphocyte Pre-T-lymphocyte Recognizes self-antigen? Binds to MHC molecule? No Yes Destroyed by apoptosis Survives 2% of cells survive selection process in the thymus. Selective loss of either CD 4 or CD 8 MHC class II No

To partake or not to partake?