Lymphatic and Immune System Biology 12 Chapter 13
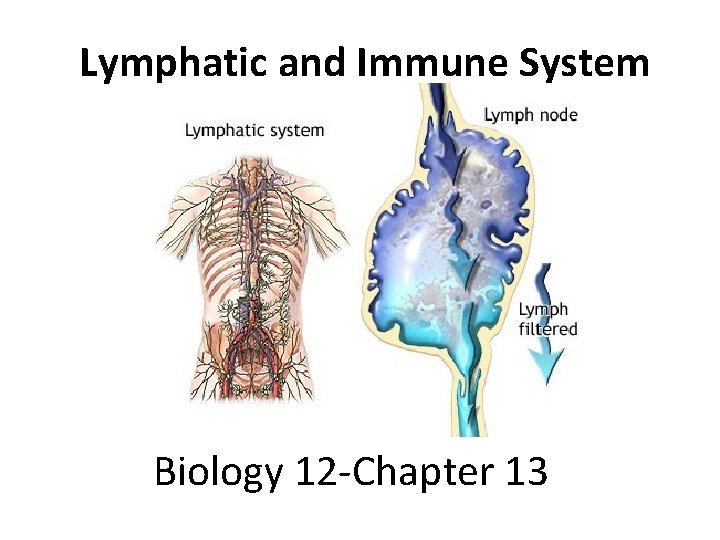
Lymphatic and Immune System Biology 12 -Chapter 13
Overview/Objectives • 13. 1 - The Lymph System o Functions of the lymphatic system o Lymphatic organs • 13. 2 - Non-specific and Specific Defenses o Immunity and the differences between non-specific and specific defenses o Examples of non-specific defenses o Blood cells responsible for specific defences and their functions • 13. 3 - Induced Immunity o Difference between active and passive immunity • 13. 4 - Immunity Side Effects o Complications and disorders with the immune system
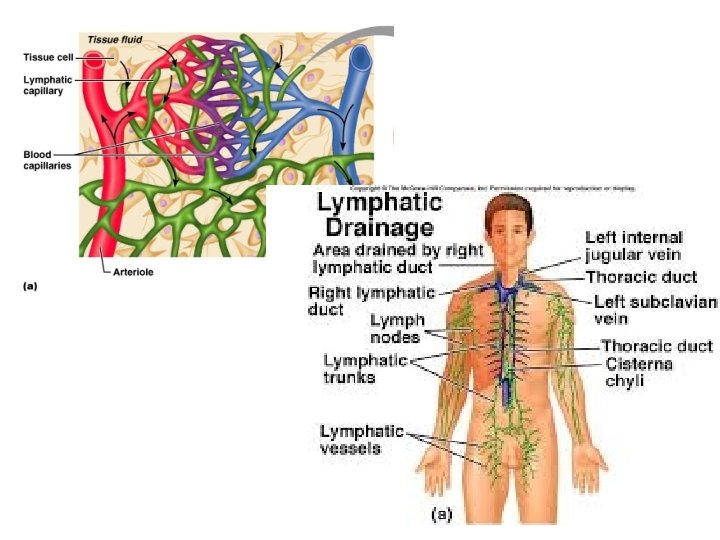
13. 1 - The Lymphatic System • Consists of lymphatic vessels and lymphatic organs • Closely associated with the cardiovascular system • 3 main functions: 1. Lymphatic capillaries take up excess tissue fluid and return it to the blood 2. Lacteals absorb fats from the digestive tract & transport them to the blood stream 3. Help Defend the body against disease
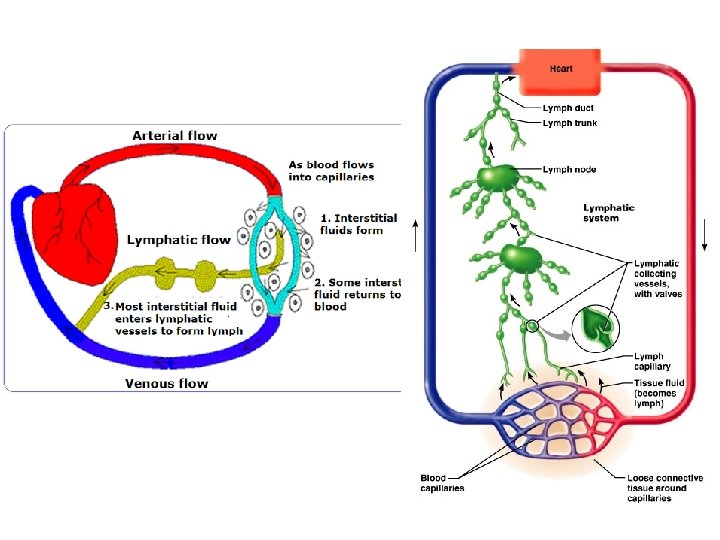
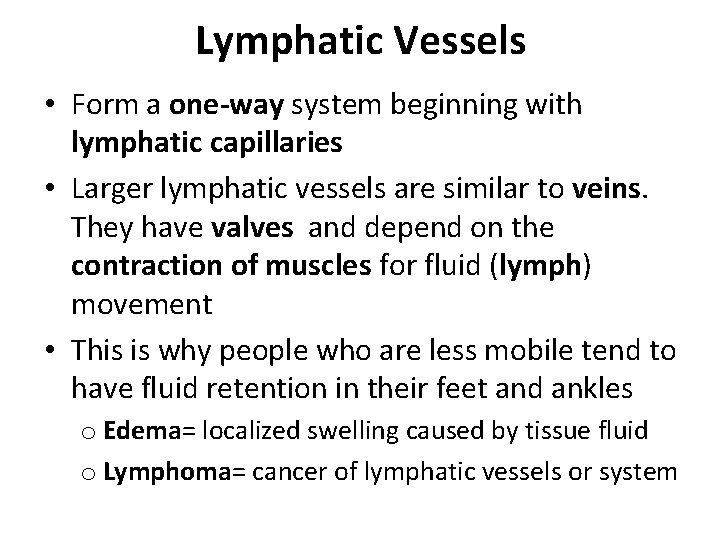
Lymphatic Vessels • Form a one-way system beginning with lymphatic capillaries • Larger lymphatic vessels are similar to veins. They have valves and depend on the contraction of muscles for fluid (lymph) movement • This is why people who are less mobile tend to have fluid retention in their feet and ankles o Edema= localized swelling caused by tissue fluid o Lymphoma= cancer of lymphatic vessels or system
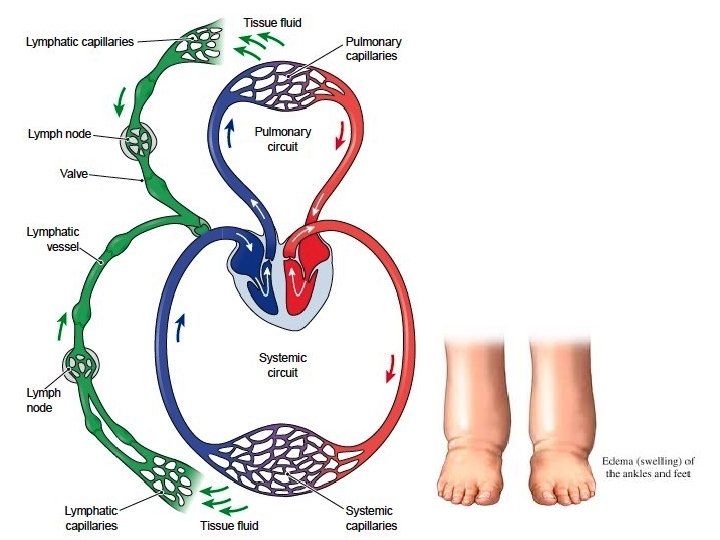
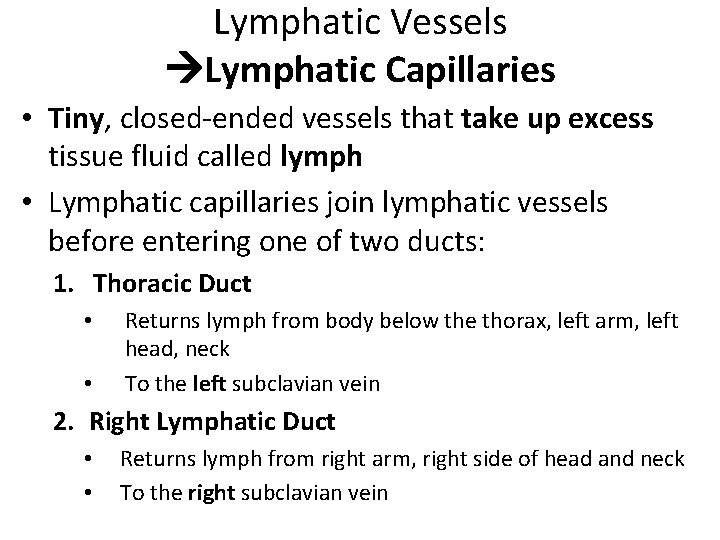
Lymphatic Vessels Lymphatic Capillaries • Tiny, closed-ended vessels that take up excess tissue fluid called lymph • Lymphatic capillaries join lymphatic vessels before entering one of two ducts: 1. Thoracic Duct • • Returns lymph from body below the thorax, left arm, left head, neck To the left subclavian vein 2. Right Lymphatic Duct • • Returns lymph from right arm, right side of head and neck To the right subclavian vein
Lymphatic Organs • Contain large numbers of lymphocytes (white blood cells) = immunity o B lymphocytes (B cells) o T lymphocytes (T cells) = both are produced and mature in the primary lymphatic organs
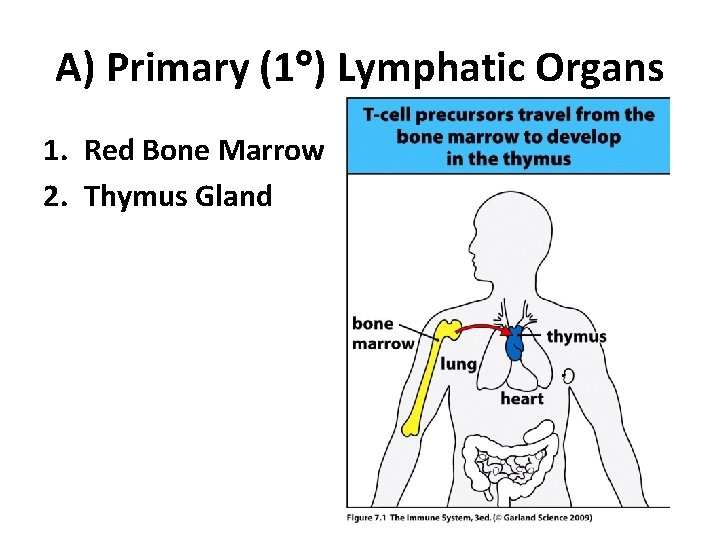
A) Primary (1 ) Lymphatic Organs 1. Red Bone Marrow 2. Thymus Gland
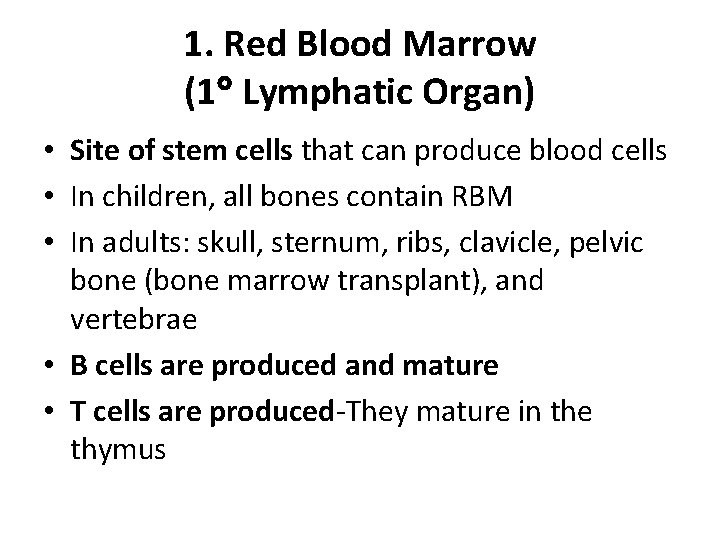
1. Red Blood Marrow (1 Lymphatic Organ) • Site of stem cells that can produce blood cells • In children, all bones contain RBM • In adults: skull, sternum, ribs, clavicle, pelvic bone (bone marrow transplant), and vertebrae • B cells are produced and mature • T cells are produced-They mature in the thymus
Red Bone Marrow
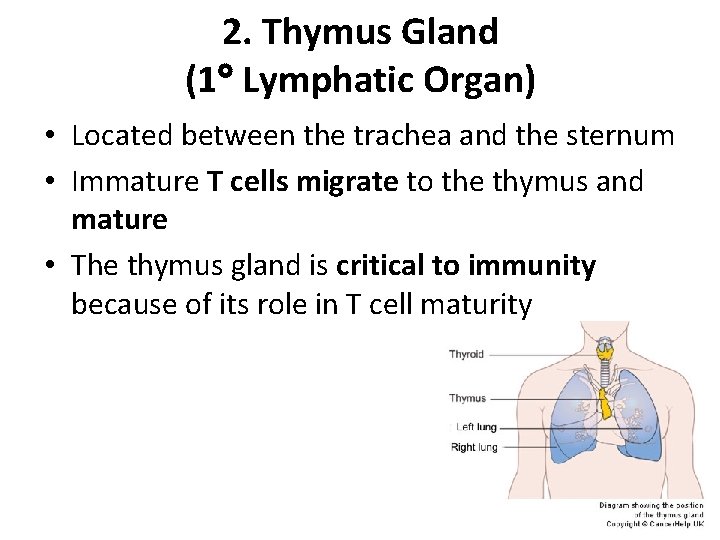
2. Thymus Gland (1 Lymphatic Organ) • Located between the trachea and the sternum • Immature T cells migrate to the thymus and mature • The thymus gland is critical to immunity because of its role in T cell maturity
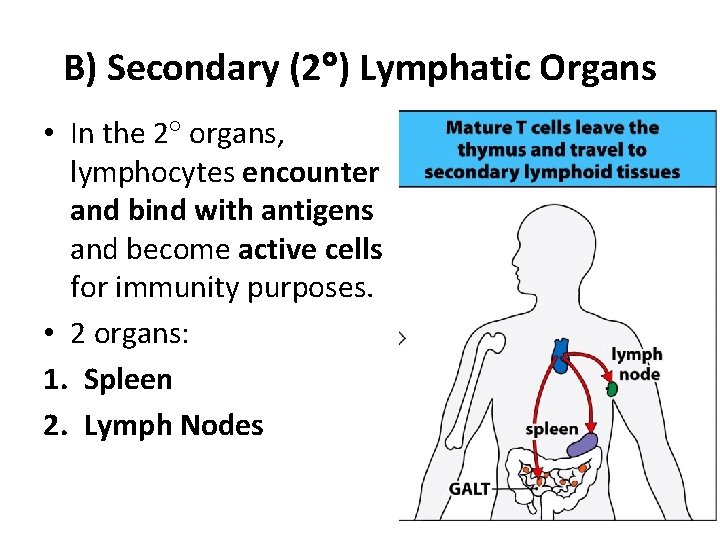
B) Secondary (2 ) Lymphatic Organs • In the 2 organs, lymphocytes encounter and bind with antigens and become active cells for immunity purposes. • 2 organs: 1. Spleen 2. Lymph Nodes
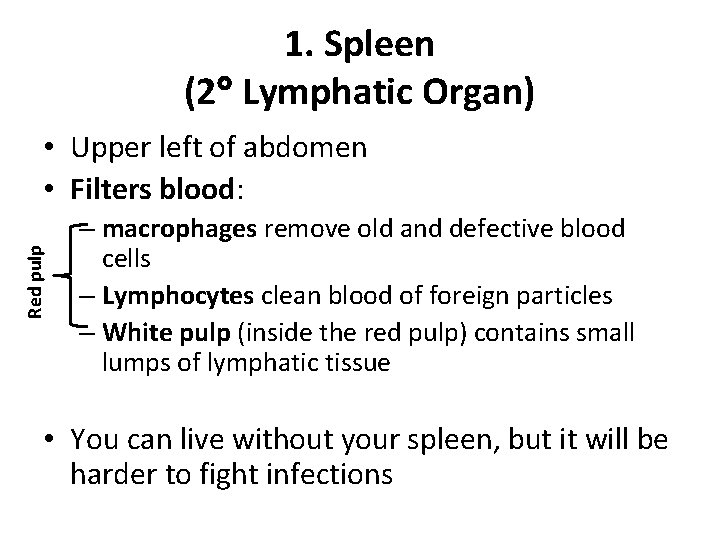
1. Spleen (2 Lymphatic Organ) Red pulp • Upper left of abdomen • Filters blood: – macrophages remove old and defective blood cells – Lymphocytes clean blood of foreign particles – White pulp (inside the red pulp) contains small lumps of lymphatic tissue • You can live without your spleen, but it will be harder to fight infections
Spleen
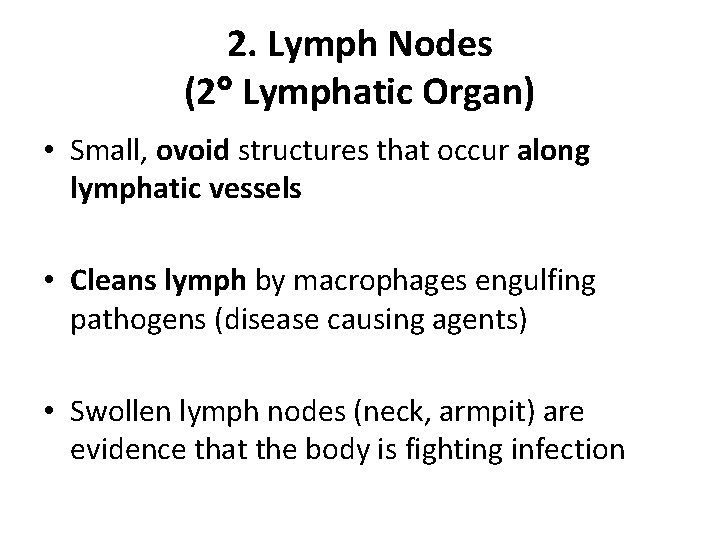
2. Lymph Nodes (2 Lymphatic Organ) • Small, ovoid structures that occur along lymphatic vessels • Cleans lymph by macrophages engulfing pathogens (disease causing agents) • Swollen lymph nodes (neck, armpit) are evidence that the body is fighting infection
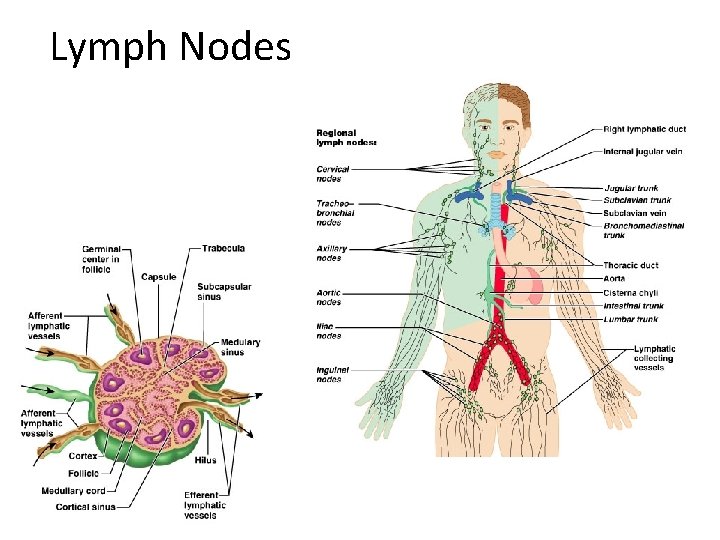
Lymph Nodes
13. 2 Specific and Nonspecific Defenses • Immunity= the body’s capability to repel foreign substances, pathogens and cancer cells o A) Nonspecific Immunity = indiscriminate barrier o B) Specific Immunity= requires a certain antigen to be present o Antigen= any molecule that stimulates an immune system
A) Nonspecific Defenses 4 Types: 1. 2. 3. 4. Barriers to entry Inflammatory Reaction Natural Killer Cells Protective Proteins
1. Barriers to Entry (Nonspecific Defence) • Mechanical barriers= skin and mucus membranes • Oil gland secretions= kill bacteria on the skin • Ciliated cells= line the respiratory tract • Stomach acid= low p. H kills bacteria or inhibits growth • Beneficial helper bacteria= in large intestine will kill invading bacteria
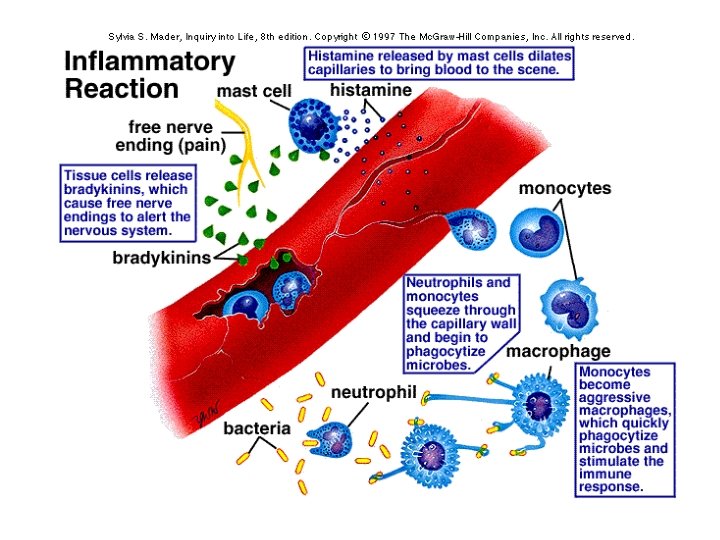
2. Inflammatory Reaction (Nonspecific Defence) • Inflammatory Reaction = series of events that occur when tissue is damaged I. II. IV. V. Damaged tissues release histamine and mast cells (white blood cell) causes capillaries to dilate bringing blood to the scene (redness and heat) Capillaries become more permeable accumulation of tissue fluid swelling stimulates nerve endings = pain Neutrophils and monocytes squeeze through capillary walls begin to phagocytize pathogens Dendritic cells (in skin, lungs, intestine) and macrophages (in most tissue) phagocytize pathogens stimulate immune response Blood clots wall of capillary preventing blood loss
3. Natural Killer Cells (Nonspecific Defence) • Large, granular lymphocytes that kill virus infected cells and tumor cells • They bind to these cells and release a molecule into the cell that causes apoptosis (=cell death) • Cells in your body have “self” proteins (recognition on the surface which bind to receptors on NLK cells) • Without these “self” proteins, the NK cells bind & kill
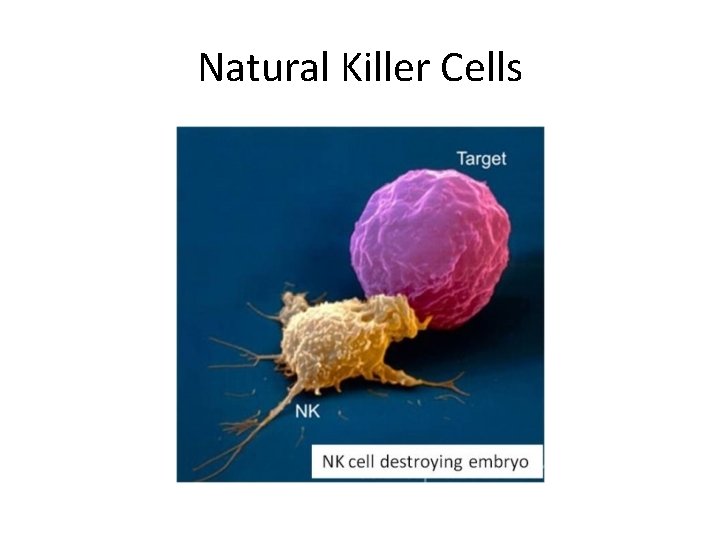
Natural Killer Cells
4. Protective Proteins (Nonspecific Defence) • Blood plasma proteins = amplify the inflammatory response by triggering a histamine release & attracting phagocytes (neutrophils or macrophages) • Membrane attack complex= can be formed by proteins that produce holes in the surface of bacteria or viruses then they burst • Interferons= proteins produced by a virus infected cell, warning other non infected cells in the area. Also produce substance that interfere with viral replication
B) Specific Defences • Takes 5 -7 days to activate, but then last a long time • Depend on the action of B cells & T cells • Through antigen recognition because of specific antigen receptors • Each lymphocyte has 1 receptor type (lock & key) o B cells= give rise to plasma cells, which produce antibodies to combine with and neutralize an antigen o T cells= do NOT produce antibodies they release chemicals to regulate the immune response or develop into cytotoxic T cells= attack and kill virus infected cells and tumor cells • Once threat has passes apoptosis (programmed cell death)
Specific Defences Continued Characteristics of B cells q. Antibody mediated immunity against pathogens q. Produced and mature in bone marrow q. Reside in lymph nodes and spleen, circulate in blood and lymph q. Directly recognize antigen undergo clonal selection q. Clonal expansion produces antibody secreting plasma cells and memory B cells Figure 13. 5 in textbook
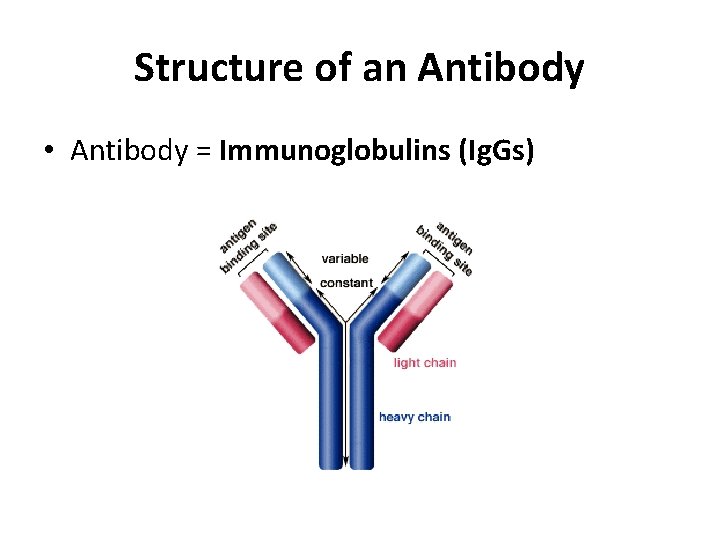
Structure of an Antibody • Antibody = Immunoglobulins (Ig. Gs)
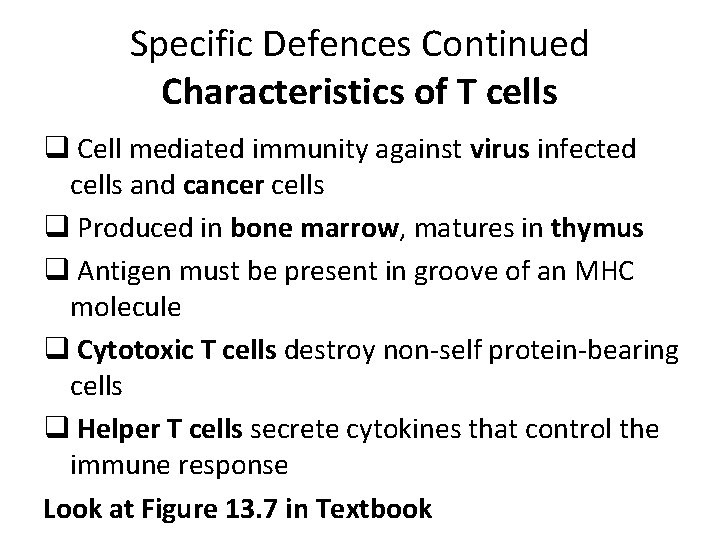
Specific Defences Continued Characteristics of T cells q Cell mediated immunity against virus infected cells and cancer cells q Produced in bone marrow, matures in thymus q Antigen must be present in groove of an MHC molecule q Cytotoxic T cells destroy non-self protein-bearing cells q Helper T cells secrete cytokines that control the immune response Look at Figure 13. 7 in Textbook
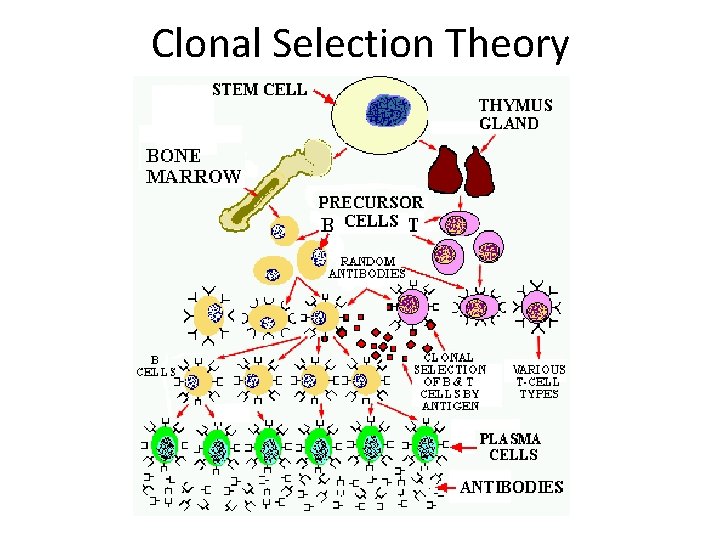
Clonal Selection Theory
13. 3 Induced Immunity • Induced immunity= occurs naturally through infection or is brought about artificially • Two types: 1. Active Immunity 2. Passive Immunity
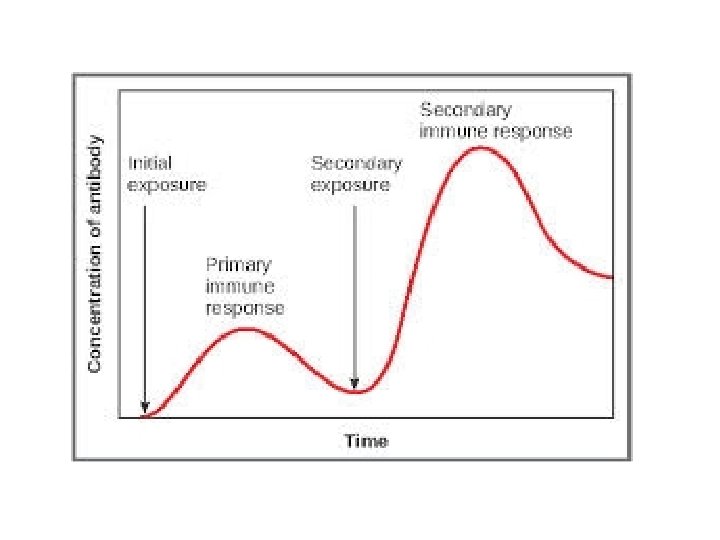
1. Active Immunity • Develops naturally after infection of a pathogen • Induced through immunization the use of a vaccine (substances that contain an antigen to which the immune system responds and prepares antibodies for) – After a vaccine is given, the immune response can be followed by measuring the amount of the developed antibodies in the plasma = antibody titre (the blood/plasma sample & test) – “Boosters” are secondary vaccines given to “boost” the level of the titre, and to ensure proper antibody level
2. Passive Immunity • Occurs when an individual is given prepared antibodies • It is temporary as the antibodies are NOT produced by the individual’s plasma cells Infants: 1. Newborns- have passive immunity to some diseases because antibodies have crosses the placenta from the mother’s blood (last a few months) 2. Breast feeding- in the first few days, mother’s milk contains colostrum (fluid high in antibodies) that helps passive immunity • Antibody injections- can help prevent illness in a person unexpectedly exposed to an infectious disease ex. Antivenom injections (snake bite)
13. 4 Immunity Side Effects Allergies: • Hypersensitivities to substances called allergens ex. Food, animal hair, pollen • The allergic reaction can be immediate (common) or delayed (not common): – Allergens (antigens) attach to the antibodies on mast cells in tissues and bloodstream – Histamine is released (air born allergens) causes mucous membranes of nose and eyes to release fluid – Airway can restrict causing breathing difficulties (especially if the person has asthma) – Food allergies cause nausea, vomiting and diarrhea
Allergies continued Anaphylatic Shock: • Immediate and often life threatening response to an allergen, because it has entered the blood stream • Blood pressure drops rapidly because of increased permeability of the capillaries by histamine • Drug to help = Epinephrine (Epi. Pen) = Adrenaline
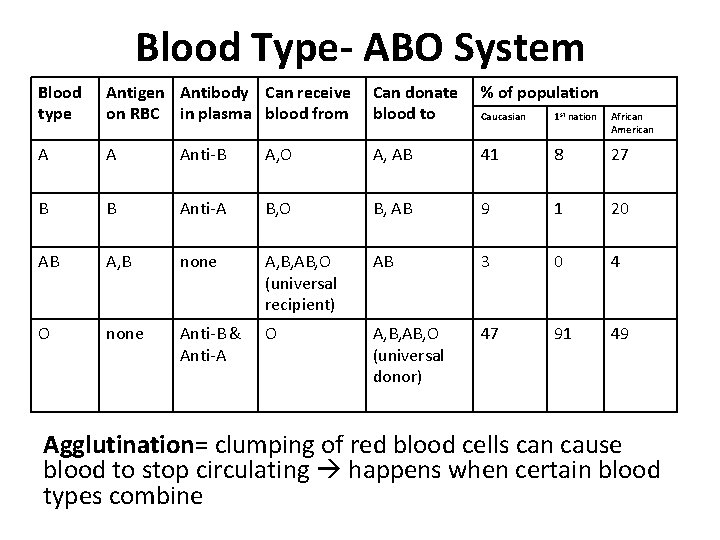
Blood Type- ABO System Blood type Antigen Antibody Can receive on RBC in plasma blood from Can donate blood to % of population Caucasian 1 st nation African American A A Anti-B A, O A, AB 41 8 27 B B Anti-A B, O B, AB 9 1 20 AB A, B none A, B, AB, O (universal recipient) AB 3 0 4 O none Anti-B & Anti-A O A, B, AB, O (universal donor) 47 91 49 Agglutination= clumping of red blood cells can cause blood to stop circulating happens when certain blood types combine
Blood Type – Rh Factor • Important antigen on red blood cells in matching blood types Ø Rh positive (Rh+)= (85% of US population) Ø Rh negative (Rh-)= (15% of US population) • If mother and baby have different Rh factor can affect subsequent pregnancies because of antibody production give Rh immunoglobulin injection
More Immunity Issues • Tissue Rejection= rejection of transplanted tissue because recipient’s immune system doesn’t recognize as “self” immunosuppressive drugs • Autoimmune disease= T cells or antibodies mistakenly attack the body’s own cells if they bear foreign antigens – Myasthenia gravis – Multiple sclerosis (MS) – Systemic lupus erythematosis (SLE) – Rheumatoid arthritis – Severe combined immunodeficiency disease (SCID)
- Slides: 40