Saladin Ch 21 Lymphatic Immune Systems Lymphatic System

![Lymph & Lymphatic Vessels – [Trunks: Lumbar, intestinal, subclavian bronchomediastinal, & juglar] – From Lymph & Lymphatic Vessels – [Trunks: Lumbar, intestinal, subclavian bronchomediastinal, & juglar] – From](https://slidetodoc.com/presentation_image_h2/d2e7e1cf236d360b90e602727fa25f25/image-8.jpg)
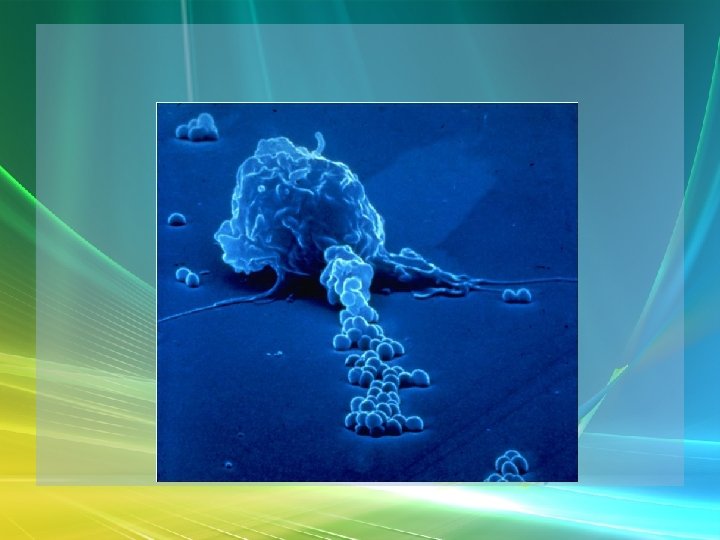
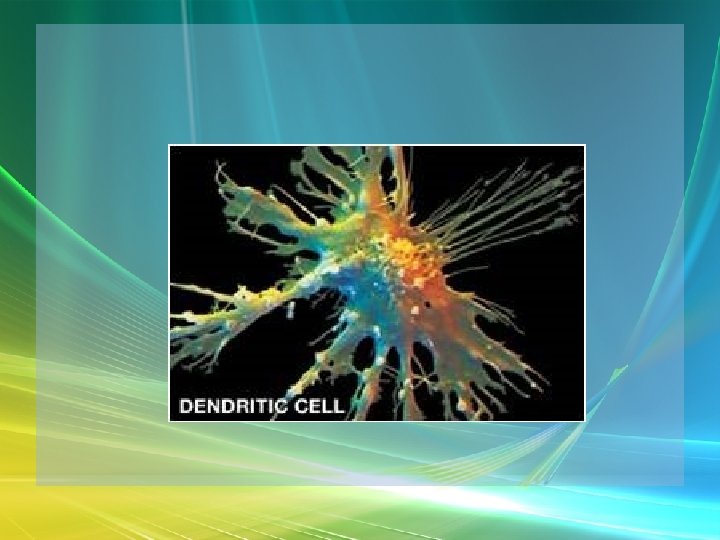
![Lymphatic Cells – Macrophages [Phago. & APC's] – Dendritic Cells [activate T cells - Lymphatic Cells – Macrophages [Phago. & APC's] – Dendritic Cells [activate T cells -](https://slidetodoc.com/presentation_image_h2/d2e7e1cf236d360b90e602727fa25f25/image-13.jpg)

![Non-specific Disease Resistance – Lymphocytes - 3 classes [specific and non] 80% T, 15% Non-specific Disease Resistance – Lymphocytes - 3 classes [specific and non] 80% T, 15%](https://slidetodoc.com/presentation_image_h2/d2e7e1cf236d360b90e602727fa25f25/image-42.jpg)

![Specific Immunity T-Cell Activation • Activation [clonal selection] – 2 steps – Recognition & Specific Immunity T-Cell Activation • Activation [clonal selection] – 2 steps – Recognition &](https://slidetodoc.com/presentation_image_h2/d2e7e1cf236d360b90e602727fa25f25/image-81.jpg)


- Slides: 108
Saladin Ch. 21 Lymphatic & Immune Systems
Lymphatic System General • Lymphatic System - composed of lymph, lymphatic vessels, and lymphatic tissue • Functions of Lymphatic system functions – Draining of interstitial fluid – Transporting dietary lipids/lipid soluble vitamins from GI to blood. – Facilitating the Immune Response - by B and T lymphocytes.

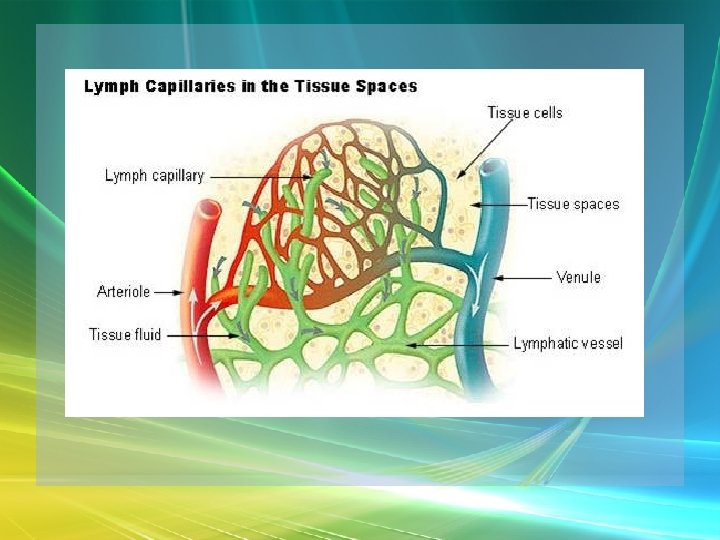
Lymph & Lymphatic Vessels Lymph – Usually clear, colorless, derived from blood plasma but with less protein – Lacteals - specialized capillaries along the small intestine - pick up lipids - gives fluid white, opaque look = chyle – Contains large numbers of lymphocytes, etc.
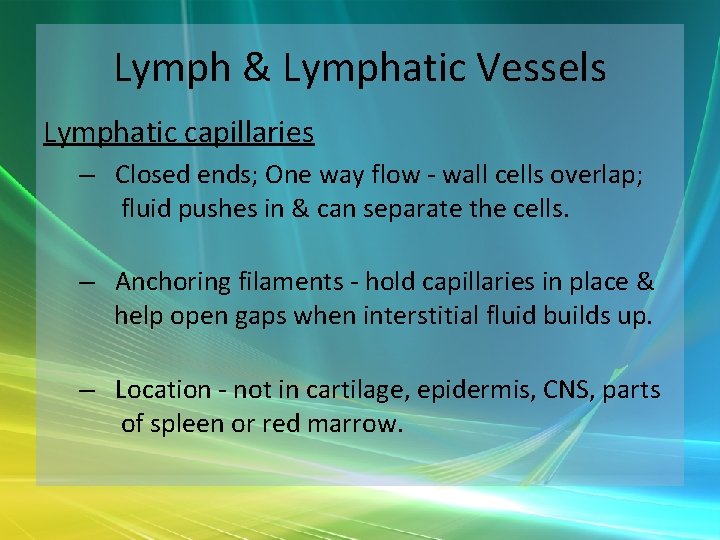
Lymph & Lymphatic Vessels Lymphatic capillaries – Closed ends; One way flow - wall cells overlap; fluid pushes in & can separate the cells. – Anchoring filaments - hold capillaries in place & help open gaps when interstitial fluid builds up. – Location - not in cartilage, epidermis, CNS, parts of spleen or red marrow.
Lymph & Lymphatic Vessels Lymph trunk and ducts • In embryo form from buds from veins - similar structure. • Flow - capillaries into vessels into nodes. After passing through a string of nodes - goes into "trunks“
![Lymph Lymphatic Vessels Trunks Lumbar intestinal subclavian bronchomediastinal juglar From Lymph & Lymphatic Vessels – [Trunks: Lumbar, intestinal, subclavian bronchomediastinal, & juglar] – From](https://slidetodoc.com/presentation_image_h2/d2e7e1cf236d360b90e602727fa25f25/image-8.jpg)
Lymph & Lymphatic Vessels – [Trunks: Lumbar, intestinal, subclavian bronchomediastinal, & juglar] – From trunks, lymph flows into either the thoracic duct or the right lymphatic duct – From the ducts, flow is into venous blood
Lymph & Lymphatic Vessels • Right lymphatic duct – Drains from upper R side – Drains into R. subclavian vein – Trunk feeders - R juglar from R head and neck, R subclavian from R upper limb, R bronchmediastinal from R thorax.
Lymph & Lymphatic Vessels • Thoracic Duct - begins as cisterna chyli anterior to L 2 vertebra – Receives from left of head & neck, chest, left upper limb, & all of the body below the ribs. – Drains into the left subclavian vein – Feeder trunks - lower body -R & L lumbar, intestinal
Lymph & Lymphatic Vessels – Lumbars drain from lower limbs, pelvis, kidneys, adrenals & abdominal wall. – Intestinal drains from intestines, pancreas, spleen & liver – From the neck, the thoracic duct gets lymph from the l. juglar, l. subclavian, l. bronchomediastinal trunks
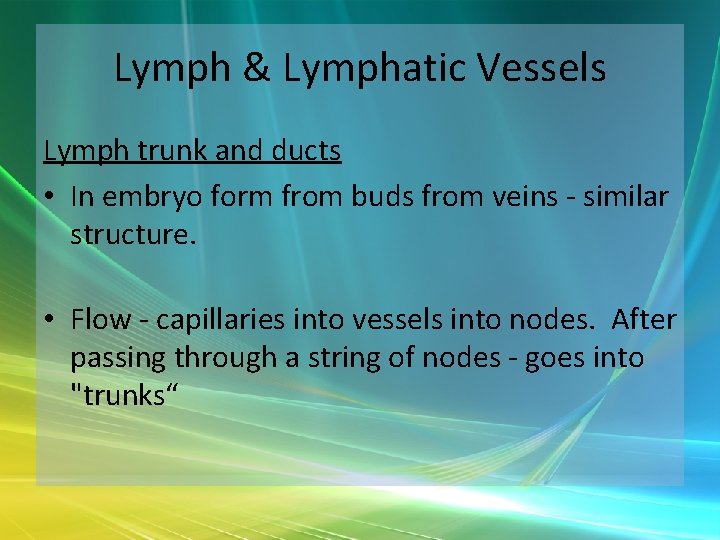
Lymphatic Cells • Lymphocytes - stem cells divide to produce B & T cells – Produced in red marrow – B cells may become plasma cells that produce antibody – Pluripotent cells in red marrow pre-T cells thymus to mature.
![Lymphatic Cells Macrophages Phago APCs Dendritic Cells activate T cells Lymphatic Cells – Macrophages [Phago. & APC's] – Dendritic Cells [activate T cells -](https://slidetodoc.com/presentation_image_h2/d2e7e1cf236d360b90e602727fa25f25/image-13.jpg)
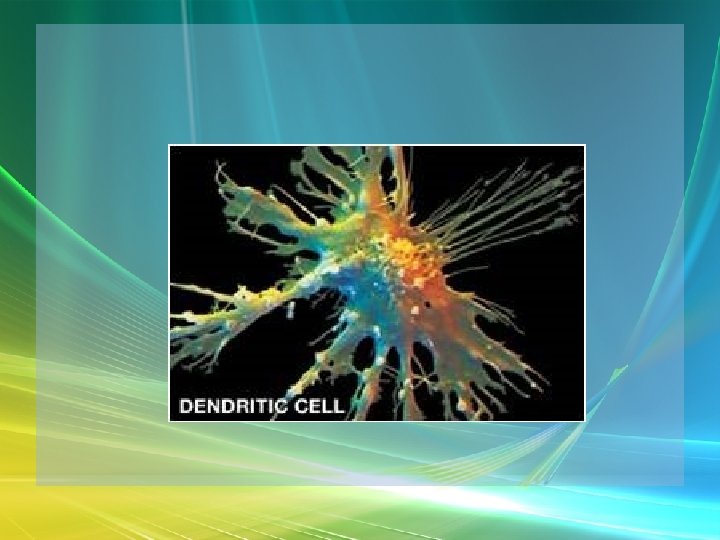
Lymphatic Cells – Macrophages [Phago. & APC's] – Dendritic Cells [activate T cells - APC's] – Reticular cells – fibroblasts that produce reticular fibers for tissue “stroma”
Lymphatic Tissue • Aggregations of lymphocytes in connective tissues of mucus membranes • MALT, Galt, nodules, Peyer's patches

Malt – Peyer’s Patches
Lymphoid Organs • Include marrow, thymus, lymph nodes, spleen, tonsils • Red Bone Marrow --> lymphocytes [review blood chapter]
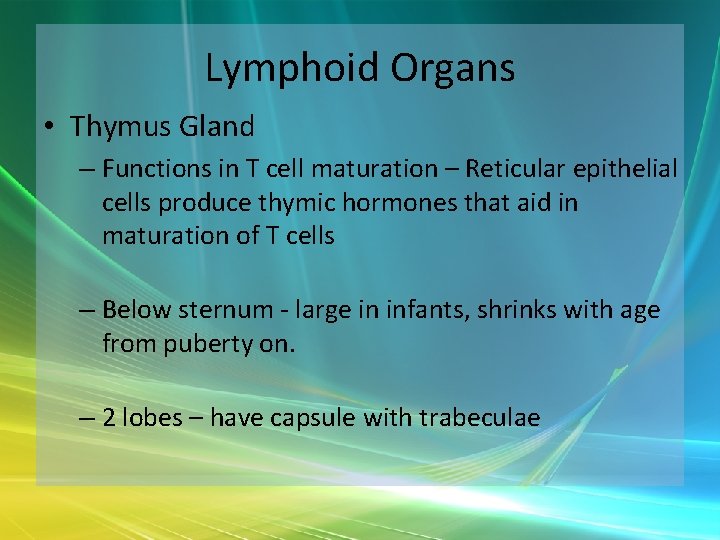
Lymphoid Organs • Thymus Gland – Functions in T cell maturation – Reticular epithelial cells produce thymic hormones that aid in maturation of T cells – Below sternum - large in infants, shrinks with age from puberty on. – 2 lobes – have capsule with trabeculae
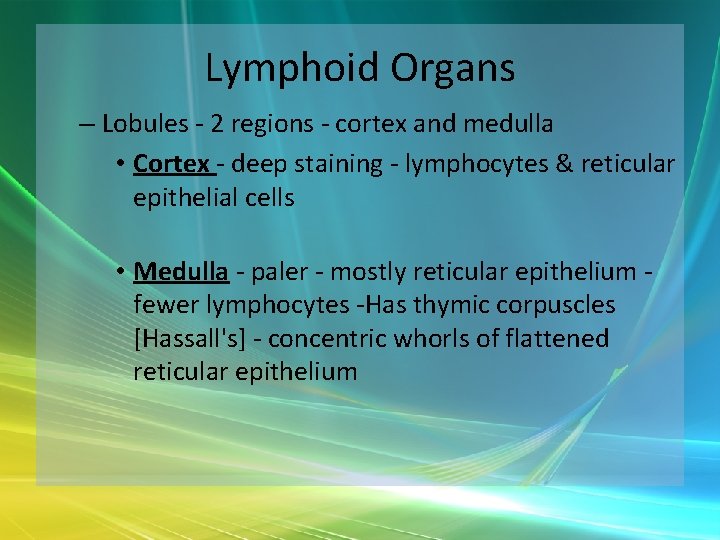
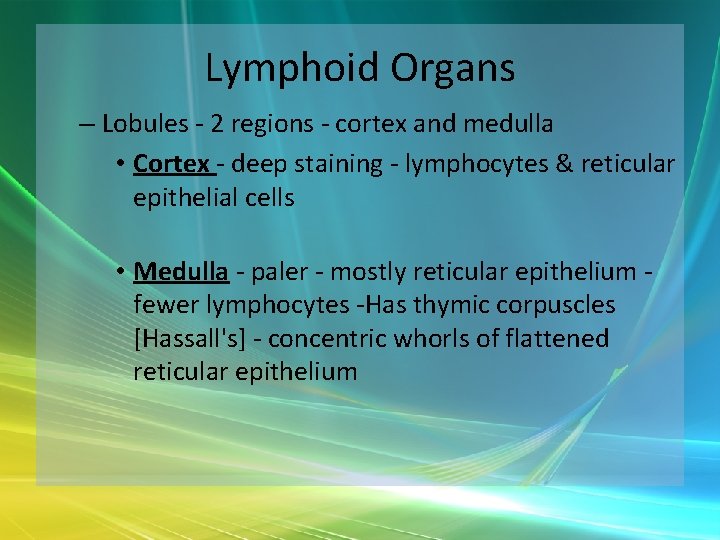
Lymphoid Organs – Lobules - 2 regions - cortex and medulla • Cortex - deep staining - lymphocytes & reticular epithelial cells • Medulla - paler - mostly reticular epithelium fewer lymphocytes -Has thymic corpuscles [Hassall's] - concentric whorls of flattened reticular epithelium
Thymus
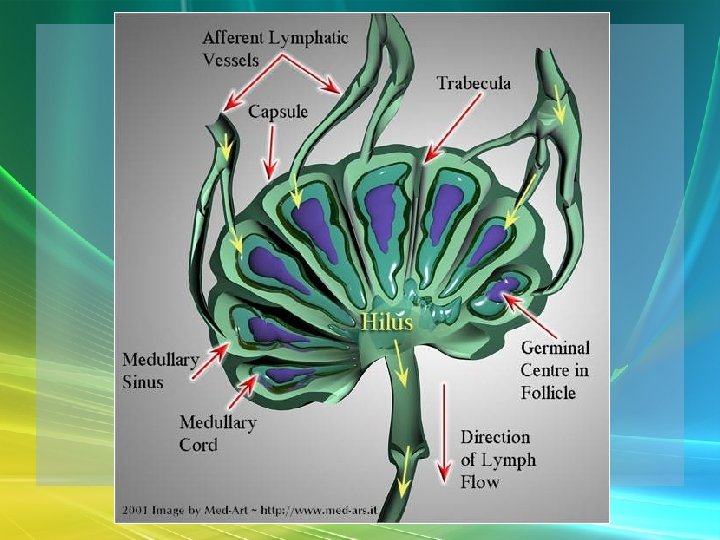
Lymphoid Organs • Lymph Nodes - about 600 bean-shaped organs – Concentrated in axillae, groin & near mammaries. – Function: • Trap material on reticular fibers, • Clear out foreign & damaged materials through phagocytosis, • Immune processes
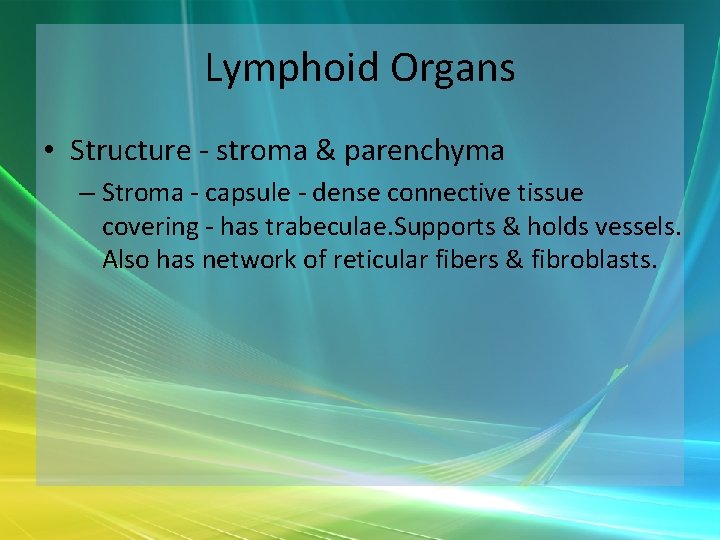
Lymphoid Organs • Structure - stroma & parenchyma – Stroma - capsule - dense connective tissue covering - has trabeculae. Supports & holds vessels. Also has network of reticular fibers & fibroblasts.
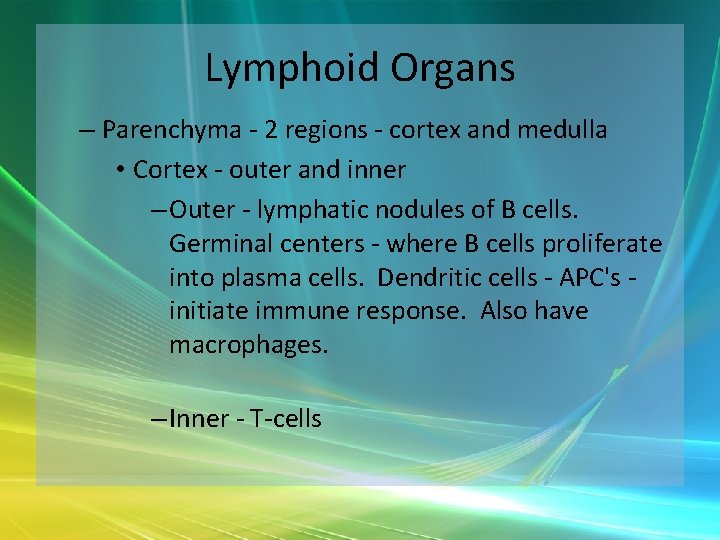
Lymphoid Organs – Parenchyma - 2 regions - cortex and medulla • Cortex - outer and inner – Outer - lymphatic nodules of B cells. Germinal centers - where B cells proliferate into plasma cells. Dendritic cells - APC's initiate immune response. Also have macrophages. – Inner - T-cells
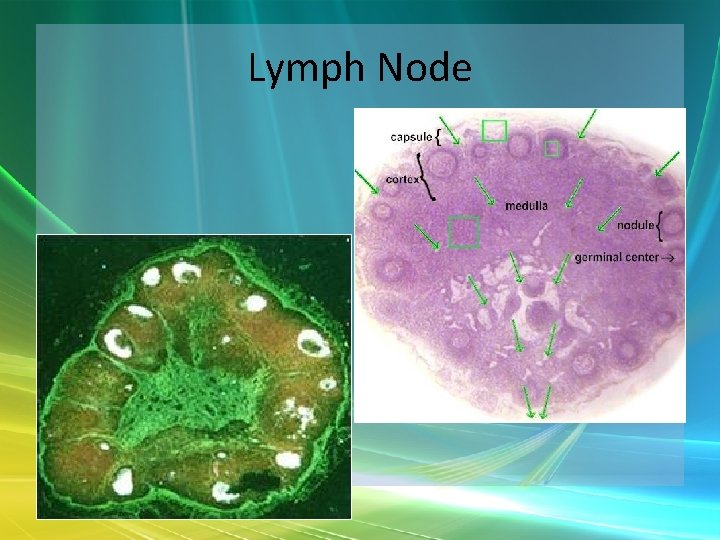
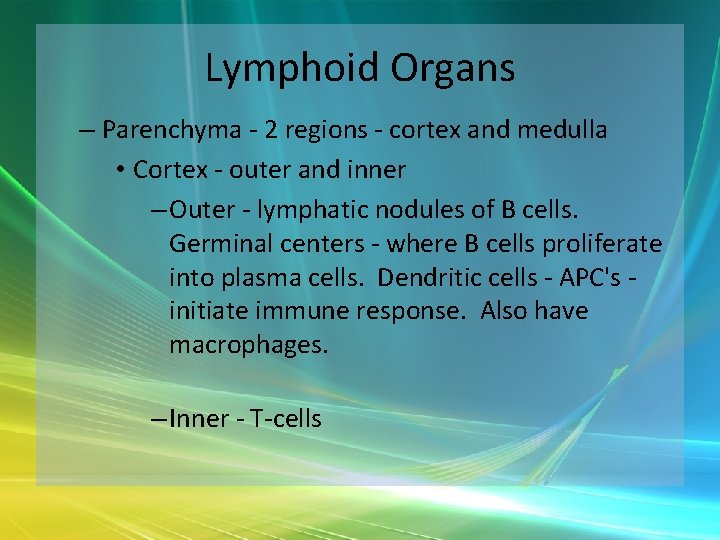
Lymph Node
Lymphoid Organs • Medulla – B & T cells, plasma cells tightly packed in "medullary cords“ – Lymph nodes have unidirectional flow - enters through afferent vessels sinuses efferent lymphatic vessels. [Hilus - place where efferent vessels emerge. ] – Lymph flows through a series of nodes --> quite clean at the end.
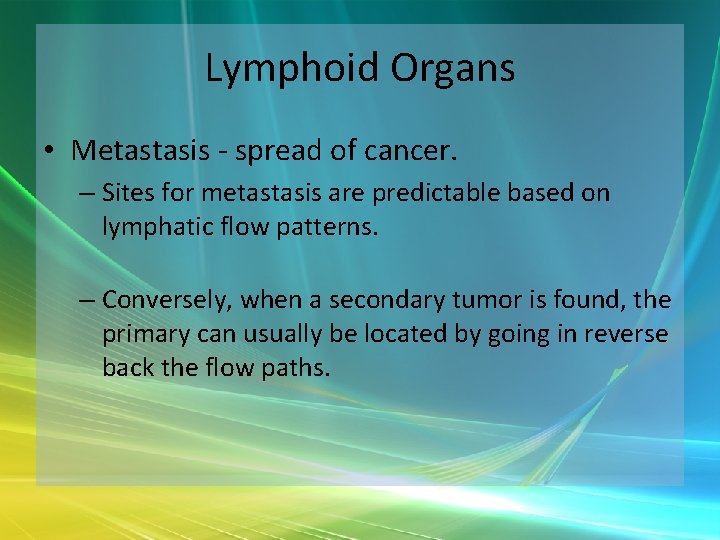
Lymphoid Organs • Metastasis - spread of cancer. – Sites for metastasis are predictable based on lymphatic flow patterns. – Conversely, when a secondary tumor is found, the primary can usually be located by going in reverse back the flow paths.
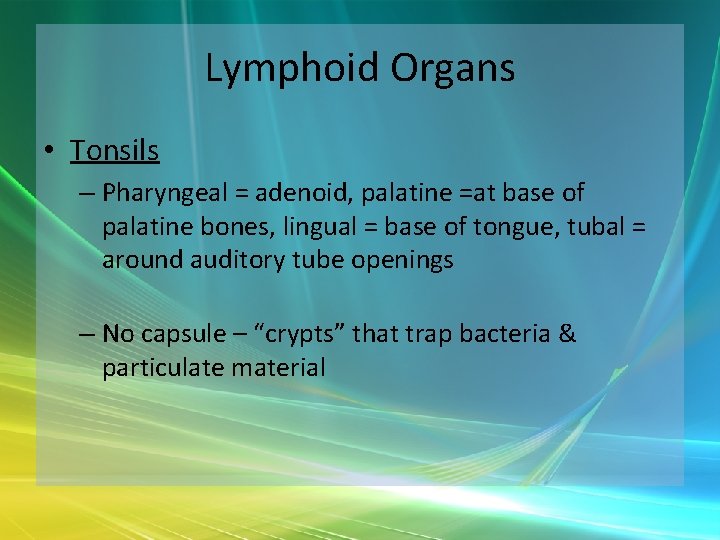
Lymphoid Organs • Tonsils – Pharyngeal = adenoid, palatine =at base of palatine bones, lingual = base of tongue, tubal = around auditory tube openings – No capsule – “crypts” that trap bacteria & particulate material
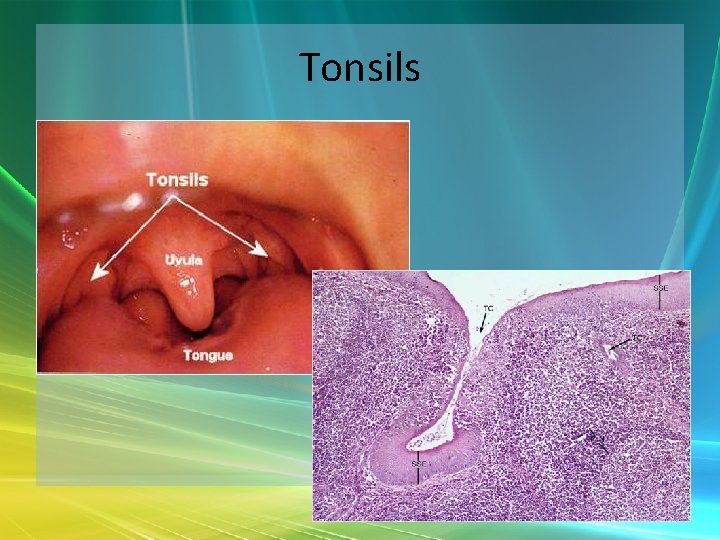
Tonsils
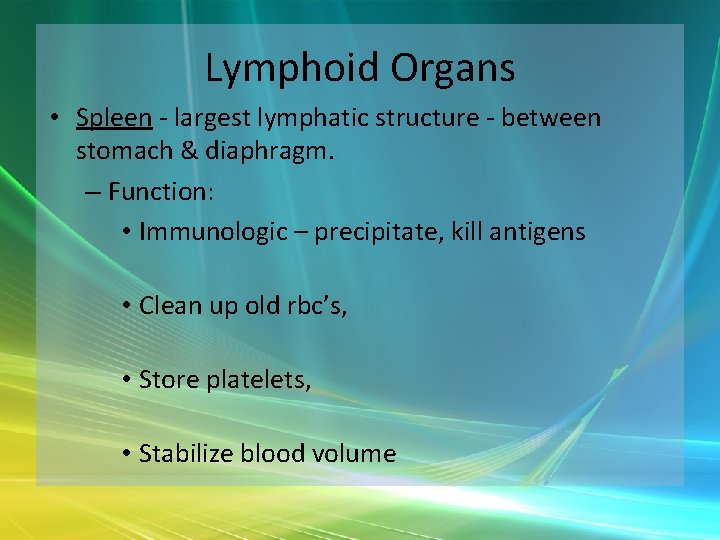
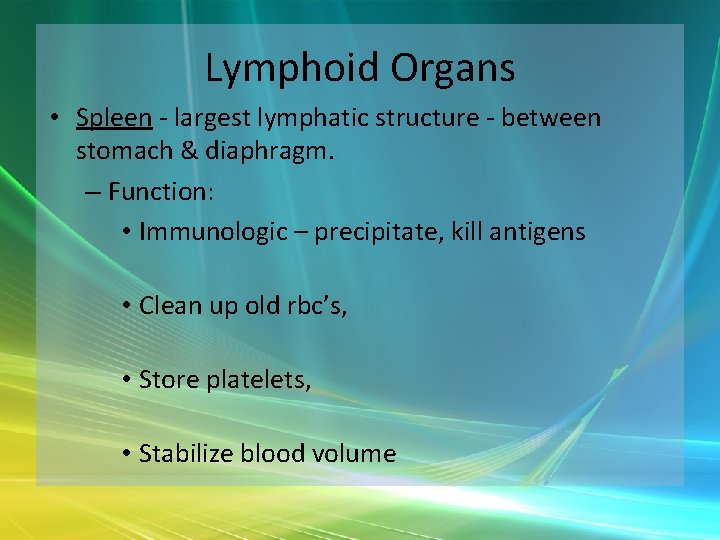
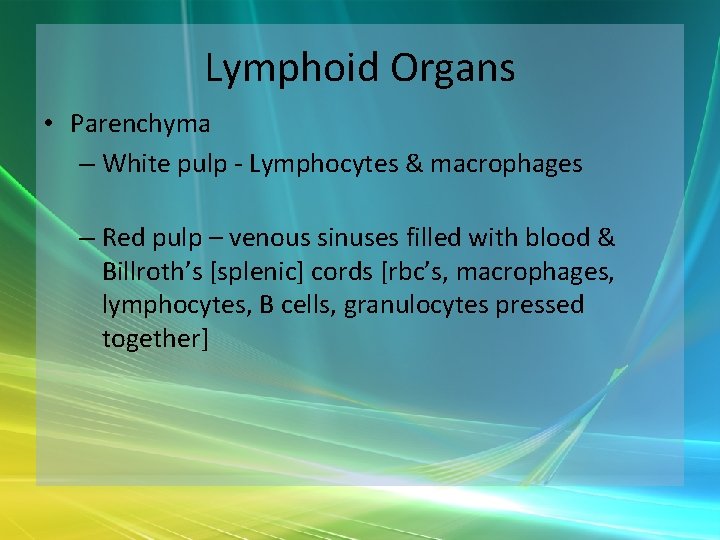
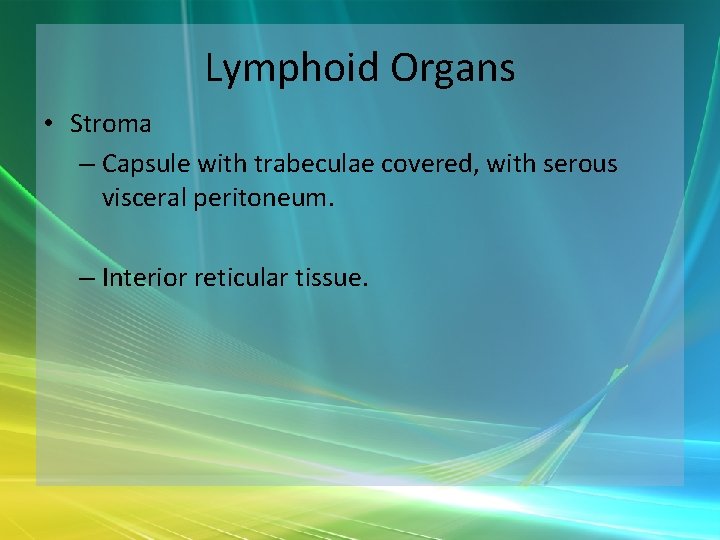
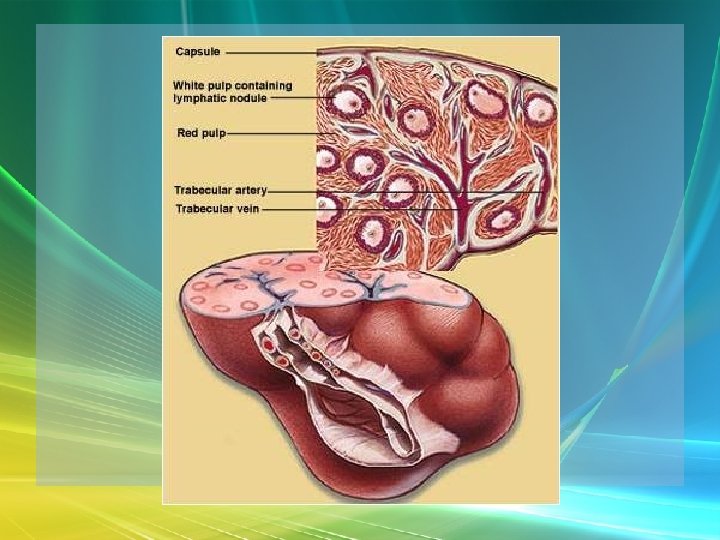
Lymphoid Organs • Spleen - largest lymphatic structure - between stomach & diaphragm. – Function: • Immunologic – precipitate, kill antigens • Clean up old rbc’s, • Store platelets, • Stabilize blood volume
Lymphoid Organs • Parenchyma – White pulp - Lymphocytes & macrophages – Red pulp – venous sinuses filled with blood & Billroth’s [splenic] cords [rbc’s, macrophages, lymphocytes, B cells, granulocytes pressed together]
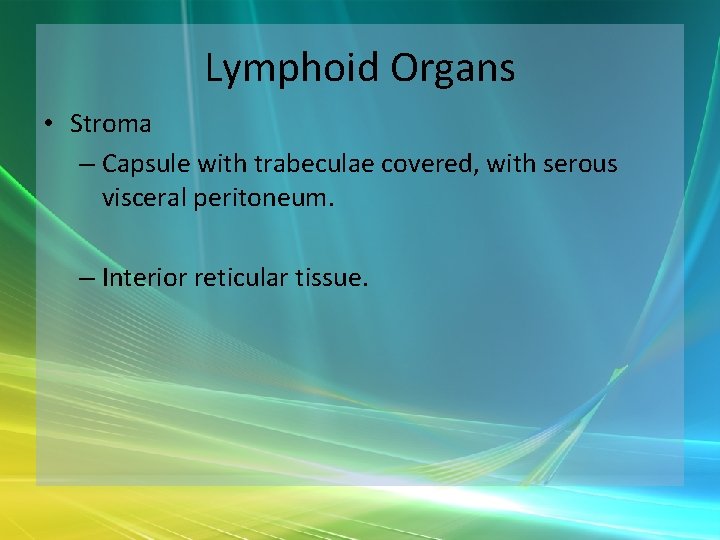
Lymphoid Organs • Stroma – Capsule with trabeculae covered, with serous visceral peritoneum. – Interior reticular tissue.
Non-specific Disease Resistance • Non-specific Resistance to Disease –> immediate protection against a wide variety of pathogens & foreign substances – NO memory – always the same – Pathogen = a disease-causing agent
Non-specific Disease Resistance – Lines of Defense: 1 - external barriers - non-specific 2 - non-specific internal responses 3 - immune system - specific
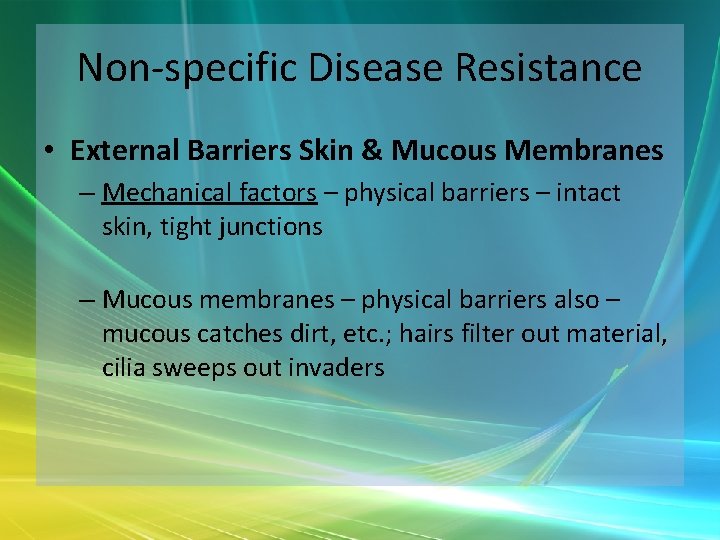
Non-specific Disease Resistance • External Barriers Skin & Mucous Membranes – Mechanical factors – physical barriers – intact skin, tight junctions – Mucous membranes – physical barriers also – mucous catches dirt, etc. ; hairs filter out material, cilia sweeps out invaders
Non-specific Disease Resistance • Chemical Factors: – Defensins – p. H of skin [3 -5] antimicrobial – Sweat – flushes, contains lactic acid = acid mantle
Non-specific Disease Resistance – Tears – dilute agents. Also some lysozyme antibiotic properties – Saliva – same Urine / vaginal secretions – Dermal hyaluronic acid - viscous - hard to traverse Some organisms have hyaluronidase to dissolve it.
Non-specific Disease Resistance • Internal Defenses - Leukocytes & Macrophages Phagocytes – eat foreign matter – Neutrophils – in most body tissues. In addition to phagocytosis, use respiratory burst - series of reactions/agents that create H 2 O 2, HCl. O & superoxide ions that destroy bacteria
Non-specific Disease Resistance – Eosinophils – can attack parasitic worms, promote basophil action, reduce inflammatory response – Basophils - secrete histamine - vasodilator and Heparin - anticoagulant [both also released by mast cells].
![Nonspecific Disease Resistance Lymphocytes 3 classes specific and non 80 T 15 Non-specific Disease Resistance – Lymphocytes - 3 classes [specific and non] 80% T, 15%](https://slidetodoc.com/presentation_image_h2/d2e7e1cf236d360b90e602727fa25f25/image-42.jpg)
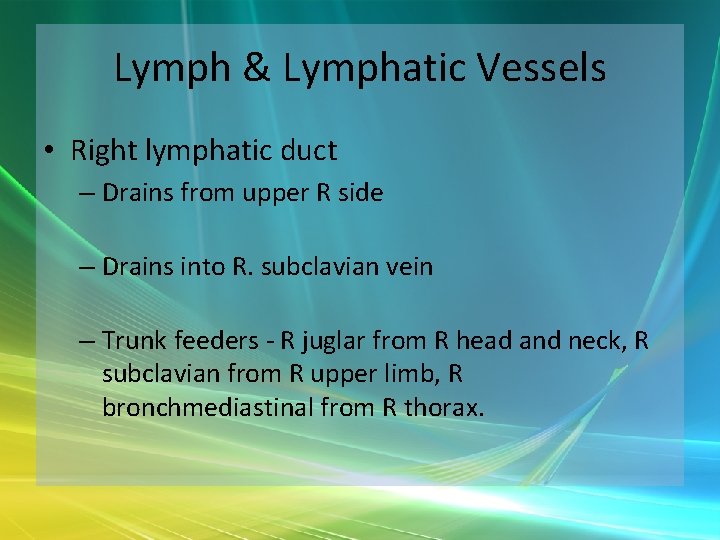
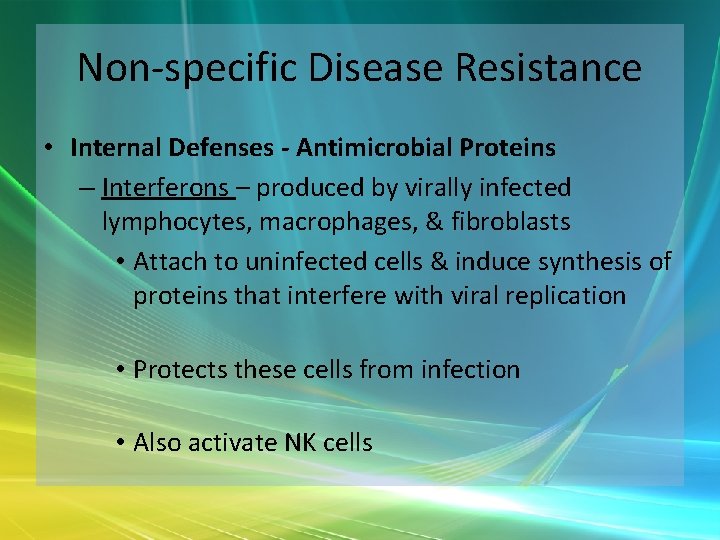
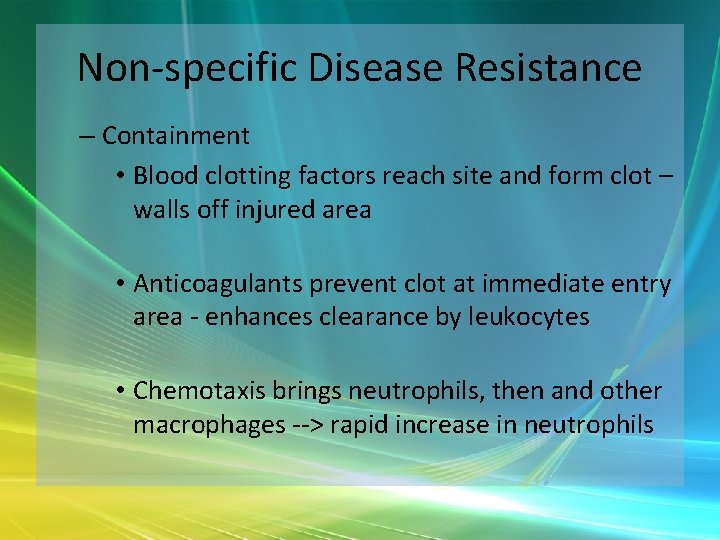
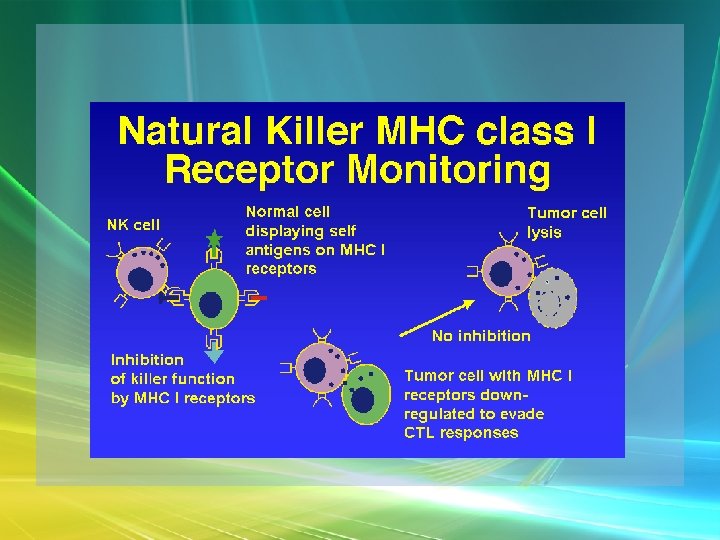
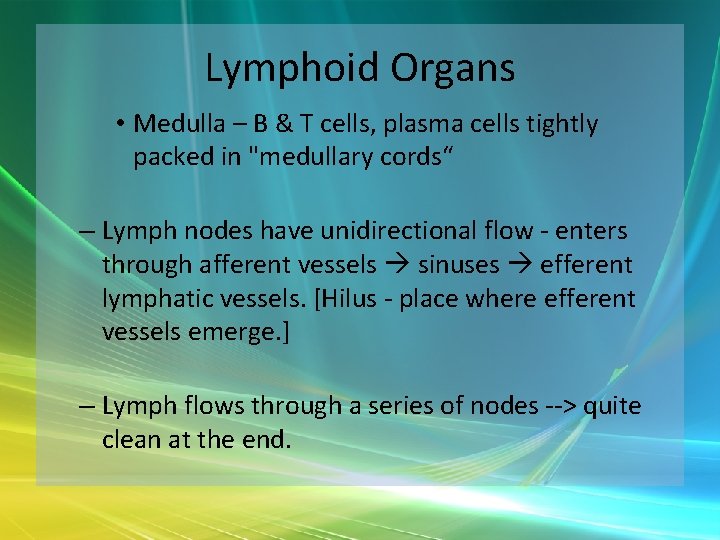
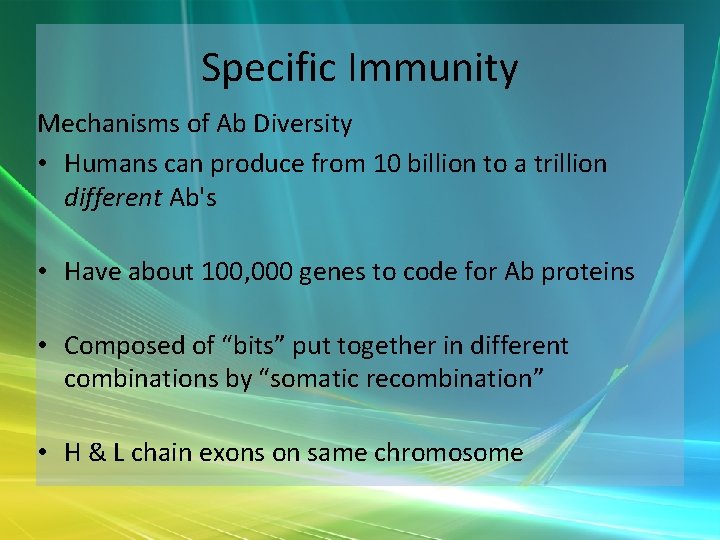
Non-specific Disease Resistance – Lymphocytes - 3 classes [specific and non] 80% T, 15% B, 5% NK – Monocytes – Special "macrophages" - dendritic cells, microglia, alveolar, hepatic
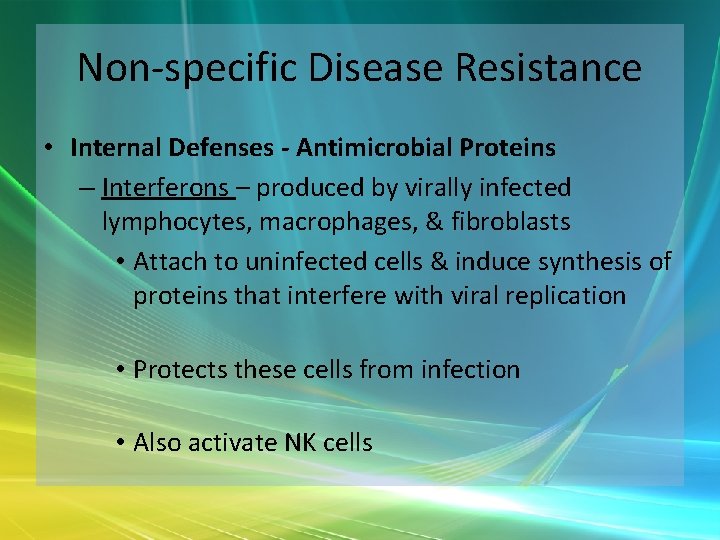
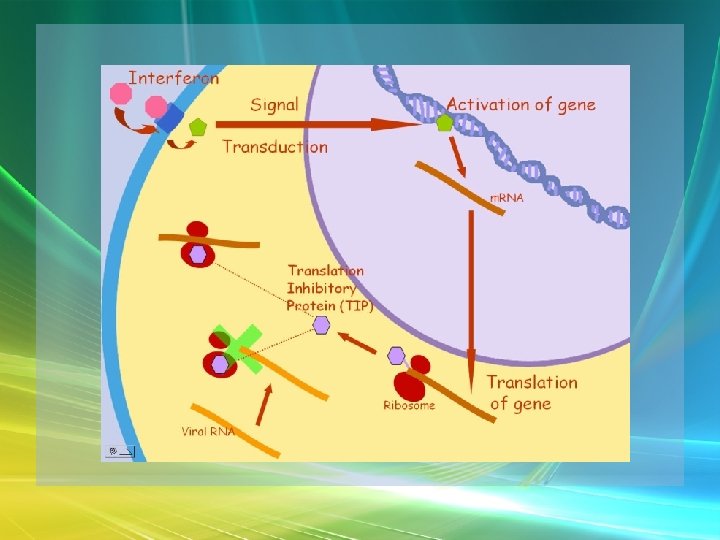
Non-specific Disease Resistance • Internal Defenses - Antimicrobial Proteins – Interferons – produced by virally infected lymphocytes, macrophages, & fibroblasts • Attach to uninfected cells & induce synthesis of proteins that interfere with viral replication • Protects these cells from infection • Also activate NK cells
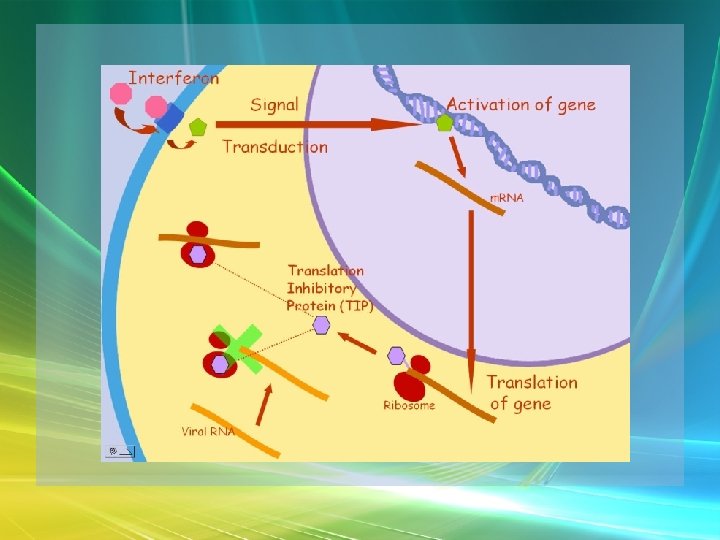
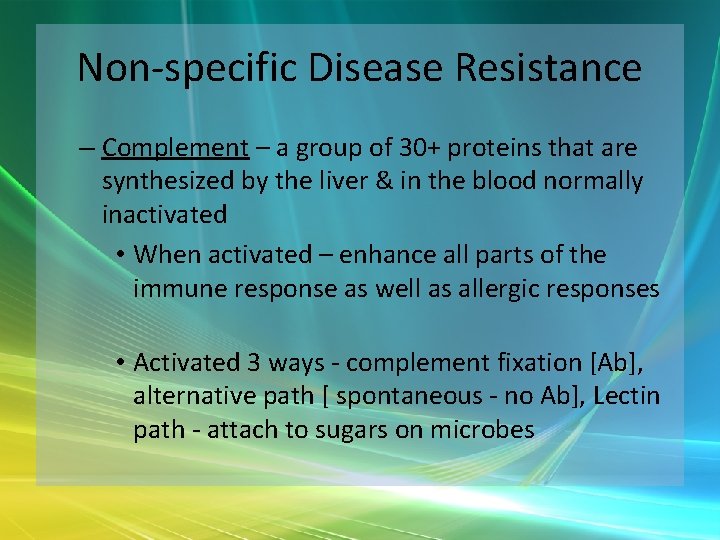
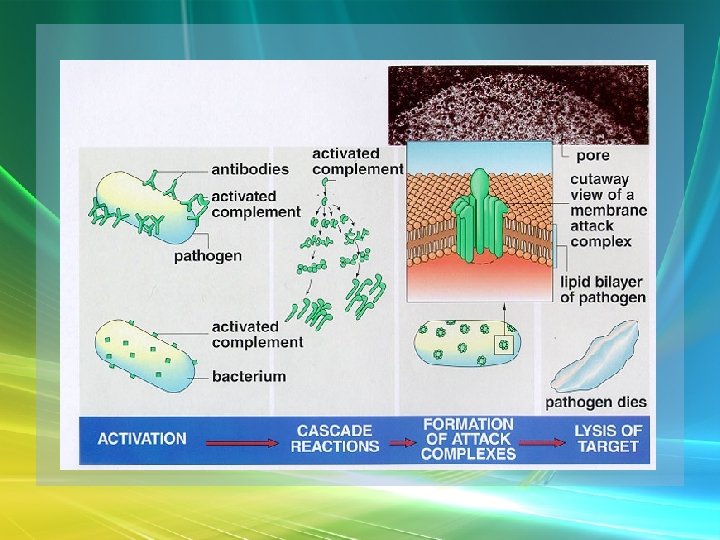
Non-specific Disease Resistance – Complement – a group of 30+ proteins that are synthesized by the liver & in the blood normally inactivated • When activated – enhance all parts of the immune response as well as allergic responses • Activated 3 ways - complement fixation [Ab], alternative path [ spontaneous - no Ab], Lectin path - attach to sugars on microbes
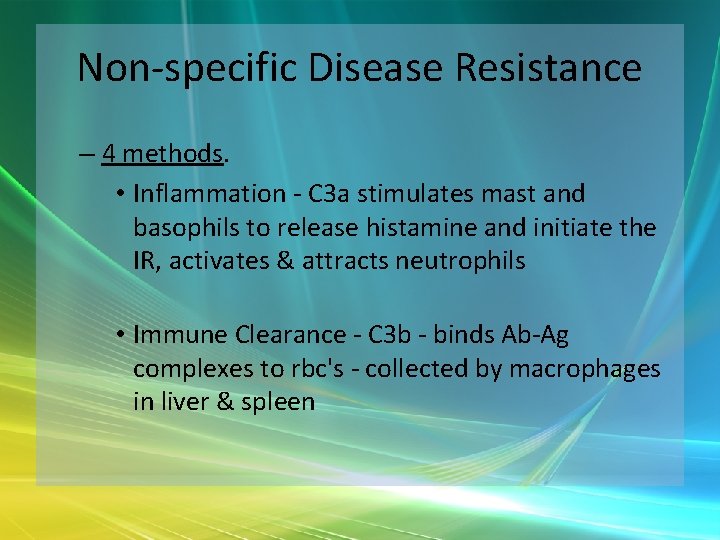
Non-specific Disease Resistance – 4 methods. • Inflammation - C 3 a stimulates mast and basophils to release histamine and initiate the IR, activates & attracts neutrophils • Immune Clearance - C 3 b - binds Ab-Ag complexes to rbc's - collected by macrophages in liver & spleen
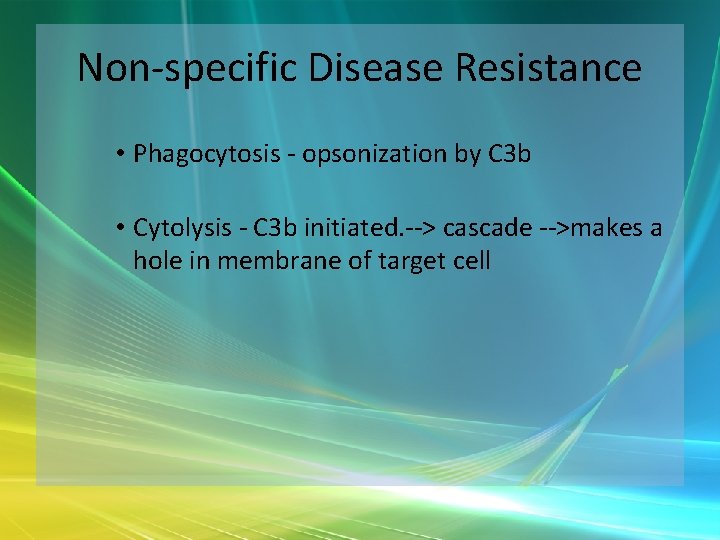
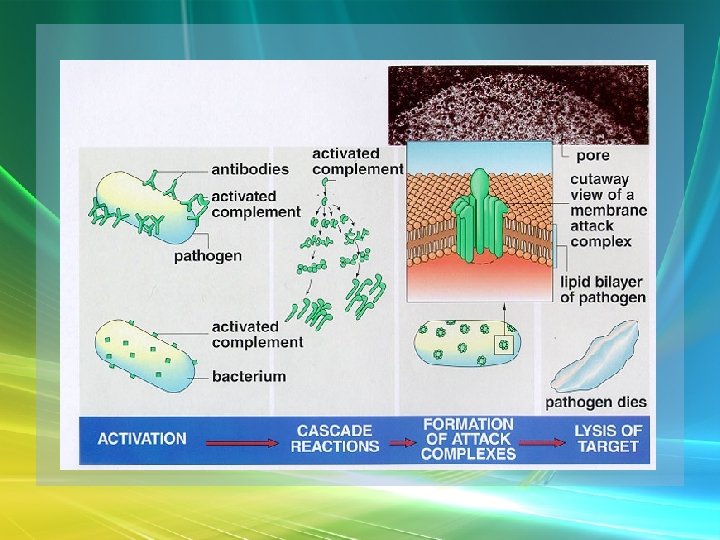
Non-specific Disease Resistance • Phagocytosis - opsonization by C 3 b • Cytolysis - C 3 b initiated. --> cascade -->makes a hole in membrane of target cell
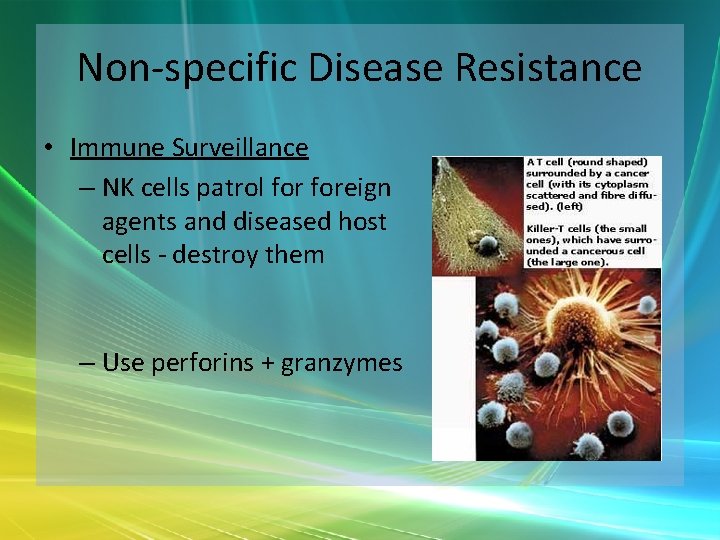
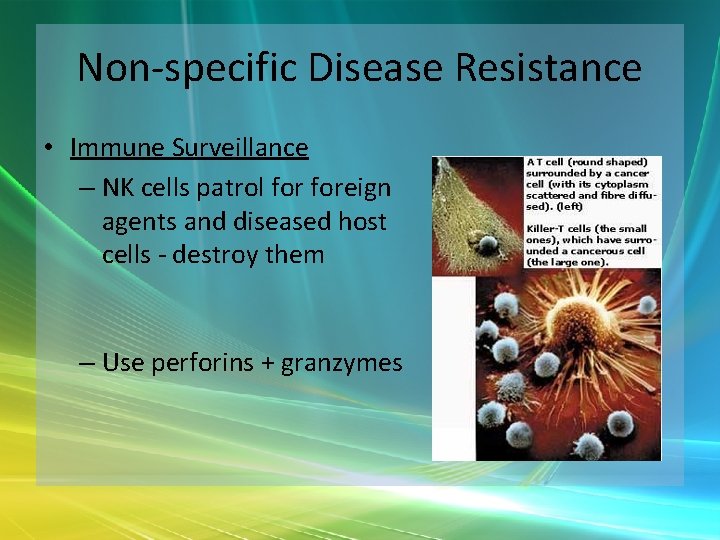
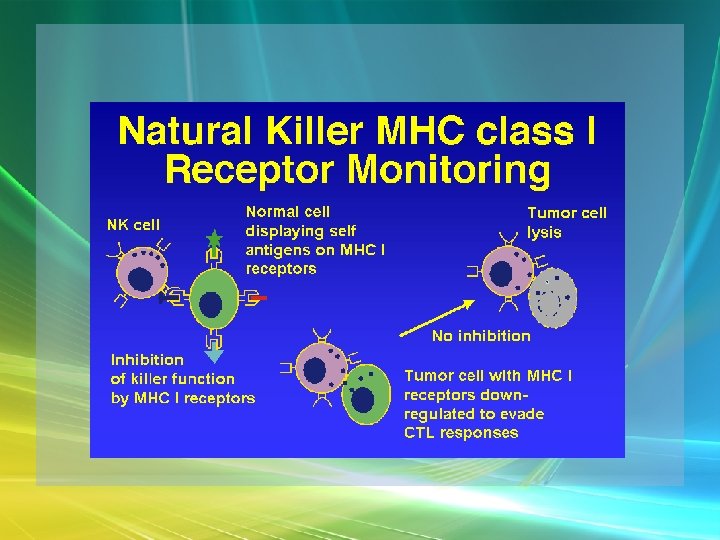
Non-specific Disease Resistance • Immune Surveillance – NK cells patrol foreign agents and diseased host cells - destroy them – Use perforins + granzymes
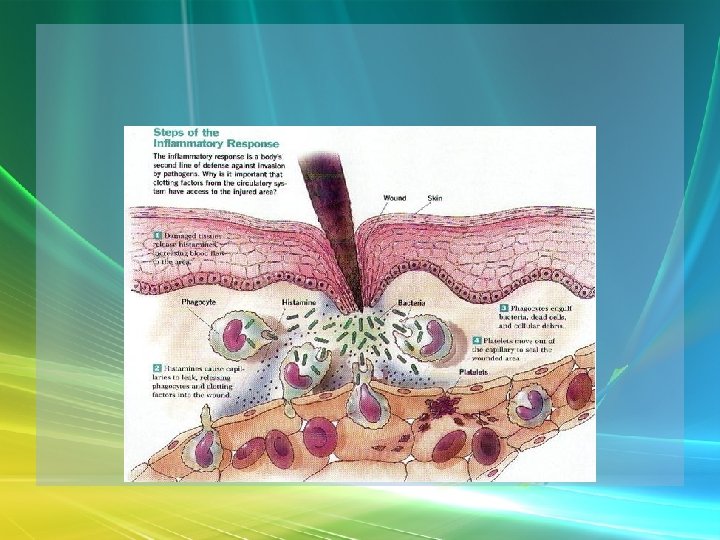
Non-specific Disease Resistance • Inflammation – tumor, rubror, calor and pain – 3 stages – mobilization = vasodilation and increased permeability, emigration, containments & destruction, tissue repair [see table 21. 1 for cells and chemicals]
Non-specific Disease Resistance • Sequence of inflammation events – Vasodilation • Causes – normal or damaged cells release histamine & other vasoactive chemicals --> • Dilation & increased permeability --> redness, heat & swelling

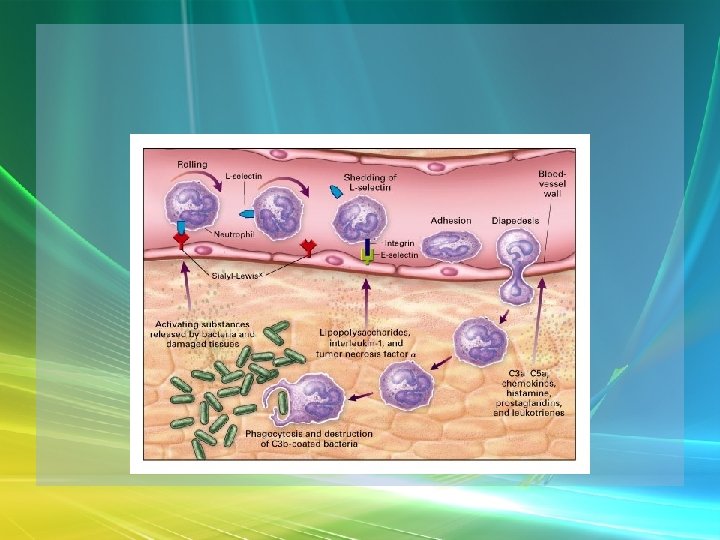
Non-specific Disease Resistance – Emigration - Neutrophils, then macrophages come into clean up - Attracted by cytokines • Margination – neutrophils in vessels adhere to walls of vessel near injury due to selectins • Diapedesis – neutrophils leave vessels
Non-specific Disease Resistance • Chemotaxis – neutrophils outside vessels attracted to site of injury • Pain is produced from damaged sensors or irritation by toxic substances & bradykinin. Prostaglandins also increase pain
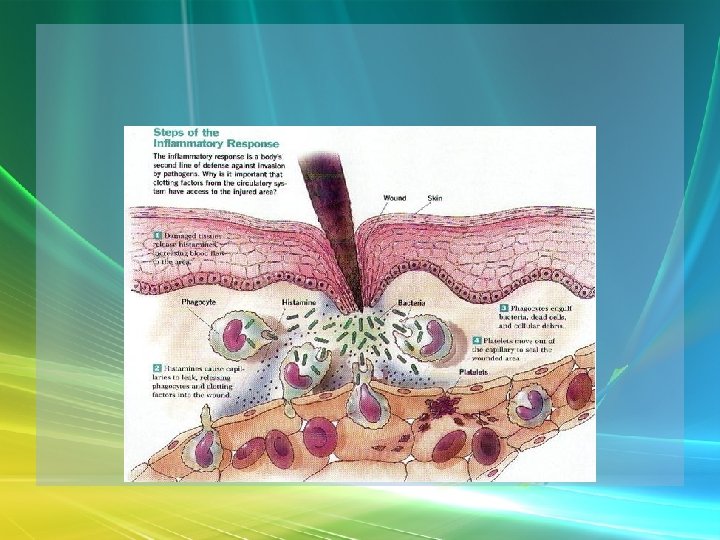
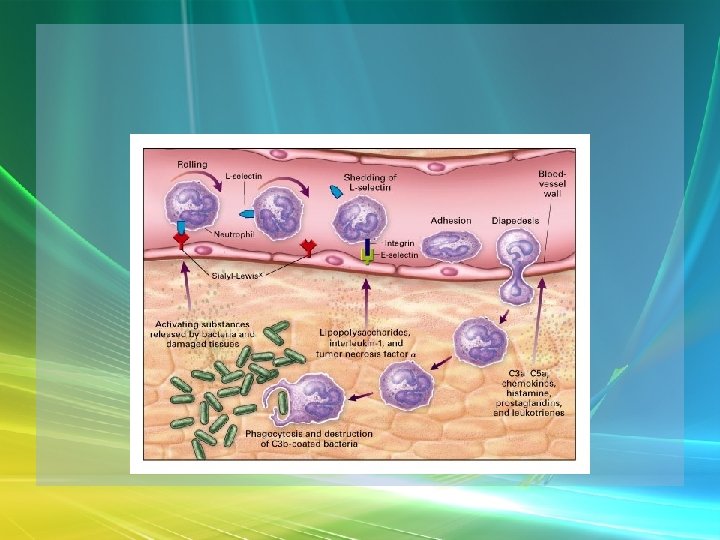
Non-specific Disease Resistance – Containment • Blood clotting factors reach site and form clot – walls off injured area • Anticoagulants prevent clot at immediate entry area - enhances clearance by leukocytes • Chemotaxis brings neutrophils, then and other macrophages --> rapid increase in neutrophils
Non-specific Disease Resistance – Tissue Cleanup & Repair • Monocytes do phagocytosis & are Agpresenting cells • Pus forms [dead material] – Ulcer – open edge, abscess – all enclosed • Platelet-derived growth factor stimulates fibroblasts --> collagen --> scaffold for new cells
Non-specific Disease Resistance • Fever – increase in body temperature produced by the hypothalamus – In response to pyrogens secreted by leukocytes and macrophages – Accompanies infection and inflammation – Promotes interferon production, inhibits bacterial growth, speeds up metabolism --> faster repair
Non-specific Disease Resistance – Reye Syndrome • Children less than 15 yo - with acute viral infection - brain swelling, etc. • Can be triggered by use of aspirin.
Specific Immunity • General Aspects of Specific Immunity – Immunity is systemic – body-wide – Immunity is specific - ability of the body to defend itself against specific invading agents such as bacteria, toxins, viruses & alien tissues.
Specific Immunity – Requires initial exposure before can develop "memory" of the agent remains after infection--> continued defense. – Antigens [Ag] are substances that provoke such an immune response [usually “foreign”]
Specific Immunity • Forms of Immunity – 2 classes of response: • Cell-mediated – cells [lymphocytes] attack other cells. – Intracellular agents • Humoral Response – antibody-mediated. Ab usually in body fluids. Extracellular agents & molecular pathogens
Specific Immunity – Active versus Passive Immunity • Active – make our own Ab/T cells – Natural – infection/exposure to fully active Ag B and T cell memory – Artificial – vaccination [mostly B cell responses – not T]
Specific Immunity • Passive – get Ab from elsewhere – Natural – maternal – placenta & milk – Artificial – pooled gamma globulin
Specific Immunity Ag’s - trigger immune responses • Immunogenicity – ability to provoke either a T or B cell response • Reactivity – ability of Ag to react with Ab or cells provoked • If an Ag does both it is “complete Ag”
Specific Immunity • Ag’s include whole or parts of microbes, bacterial toxins, pollen, egg white, blood cells, tissues • Large molecules made of small repeating units usually evoke no response • Hapten – a substance that cannot evoke a response by itself, but can if bound to something else [e. g. , a cell receptor].
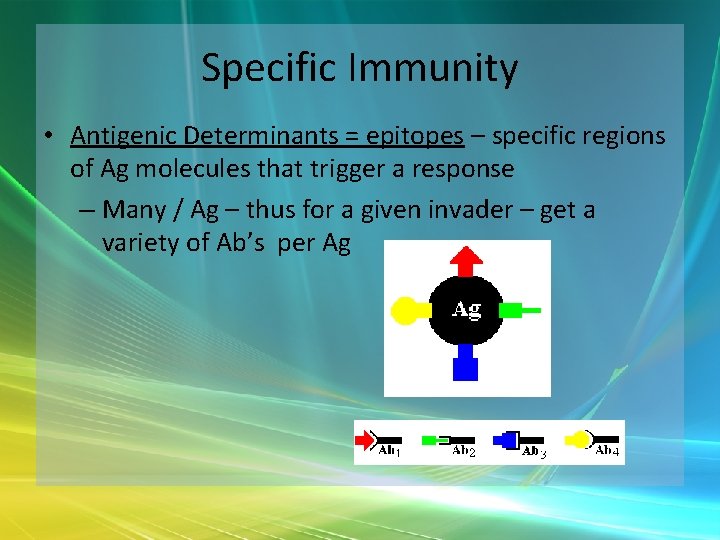
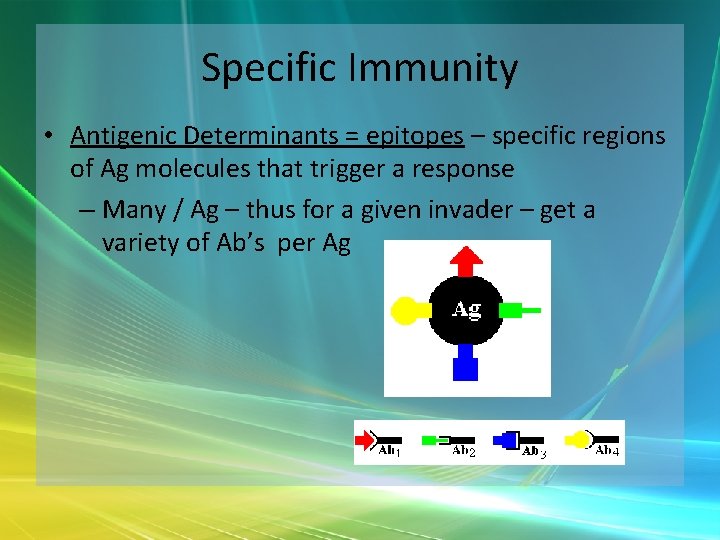
Specific Immunity • Antigenic Determinants = epitopes – specific regions of Ag molecules that trigger a response – Many / Ag – thus for a given invader – get a variety of Ab’s per Ag
Specific Immunity Lymphocytes - Cells of the Immune System • Develop from pluripotent red marrow cells • 3 populations of lymphocytes – NK, B’s and T’s • T’s cells leave marrow and go to the thymus for final processing by thymic hormones
Specific Immunity – Becoming immunocompetent means being able to recognize a foreign antigen & not responding to self-antigens. Tested for self-recognition • 1) must be able to bind MHC molecules bearing Ag presented for recognition, & • 2) must NOT react with “self” Ag. If they do, they are eliminated. Those that pass --> clones
Specific Immunity • B’s mature into “immunocompetent” cells in the marrow throughout life humoral responses [Develop receptors for 1 AG – receptors are AB’s. ] – B cells that recognize self-antigens are either inactivated in the marrow, or killed • Each individual B or T cell is genetically programmed to recognize only one antigenic determinant
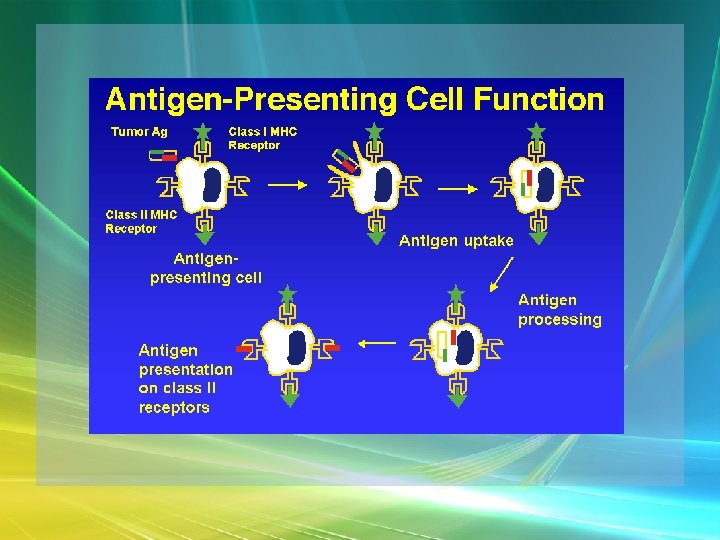
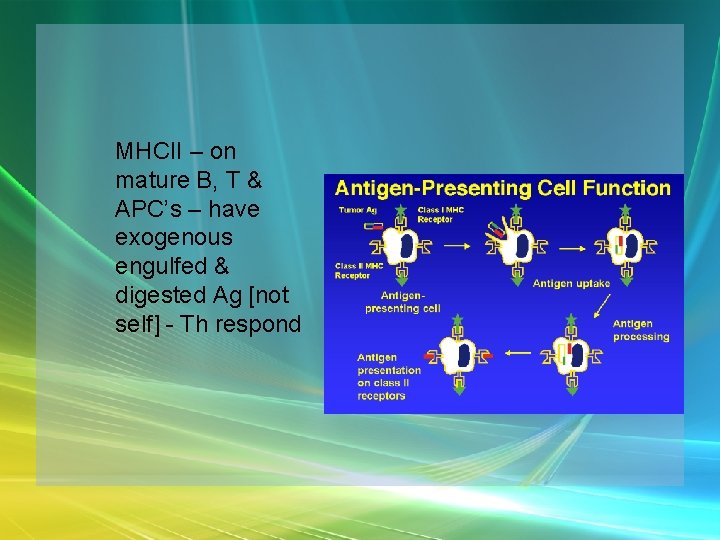
Specific Immunity Antigen-Presenting Cells - Pathway of Ag processing for response • T cells usually need help recognizing Ag, they require APC's - B cells, or macrophages, or reticular cells, or dendritic cells.
Specific Immunity • Self-Ag’s - Major Histocompatibility Complex = MHC – On membrane surfaces – glycoproteins – Also called HLA Ag’s – first found on wbc’s – Unique - usually recognize them before birth & don't attack
Specific Immunity • APC’s engulf foreign particles & then present fragments on their own cell surfaces, “signal flags. ” – Strategically located so as to ensure coverage of all body parts & tissues – Secrete proteins interleukins that activate T cells & stimulate killer cells • T-cells circulate [enhances chances of encountering the AG]
Specific Immunity Cell-Mediated Immunity – Targets body cells infected with viruses or bacteria, abnormal or cancerous cells, & foreign transplants • T cells classed by type of “cell differentiation” glycoprotein on their surfaces – CD 4 - helper T cells – CD 8 - cytotoxic T cells
Specific Immunity Recognition: • T cells only “recognize” processed fragments of protein Ag’s displayed on cell surfaces • Antigen Recognition and MHC Restriction – 2 types of MHC’s are important to T cell activation • MHCI are found on all self cells except red blood cells
Specific Immunity – Pick up endogenous materials on way to surface - display them. If Ag is foreign material from inside cells [e. g. , viral protein], it is recognized – T cells [Tc]kill the cell showing it
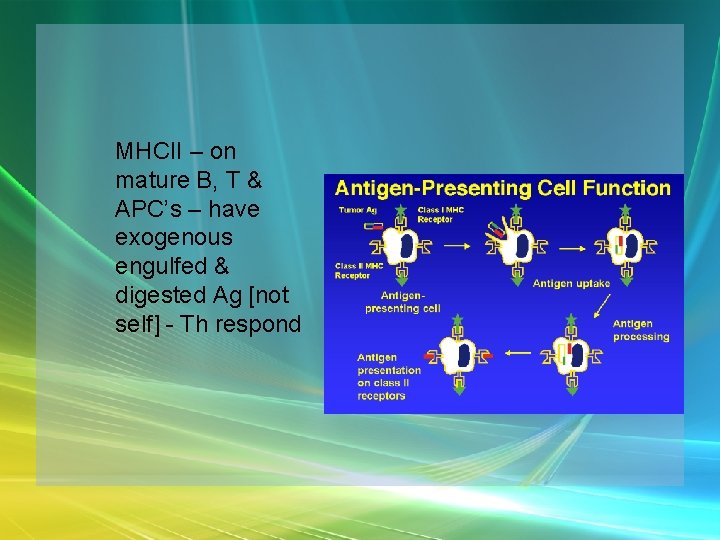
MHCII – on mature B, T & APC’s – have exogenous engulfed & digested Ag [not self] - Th respond
![Specific Immunity TCell Activation Activation clonal selection 2 steps Recognition Specific Immunity T-Cell Activation • Activation [clonal selection] – 2 steps – Recognition &](https://slidetodoc.com/presentation_image_h2/d2e7e1cf236d360b90e602727fa25f25/image-81.jpg)
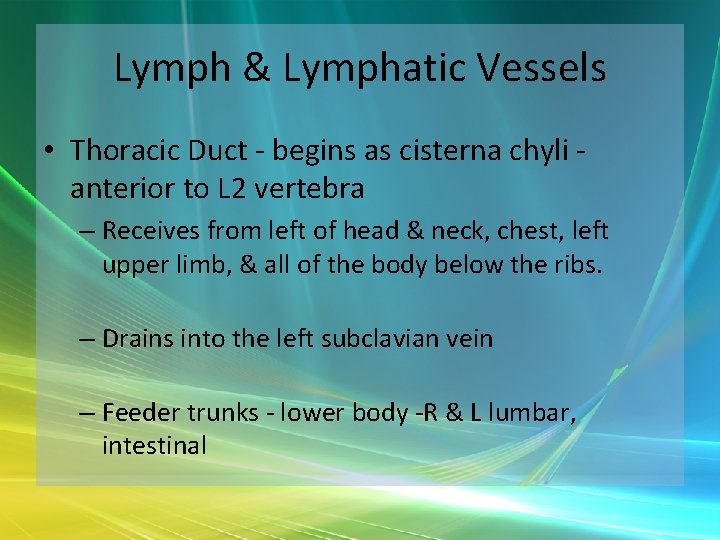
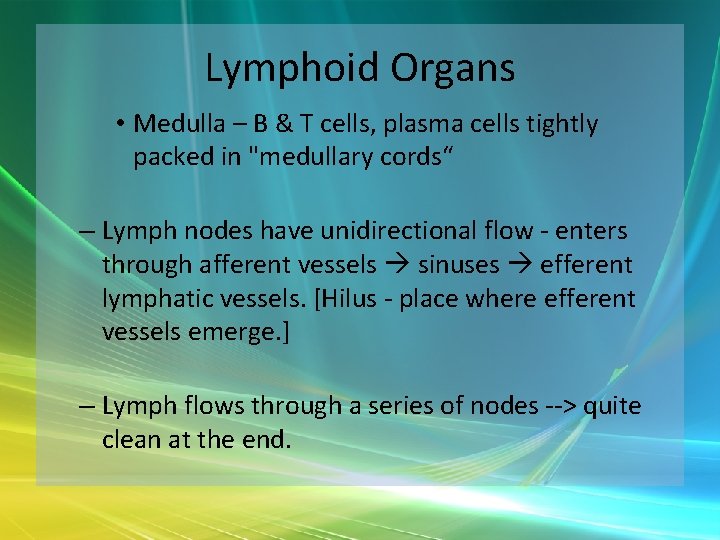
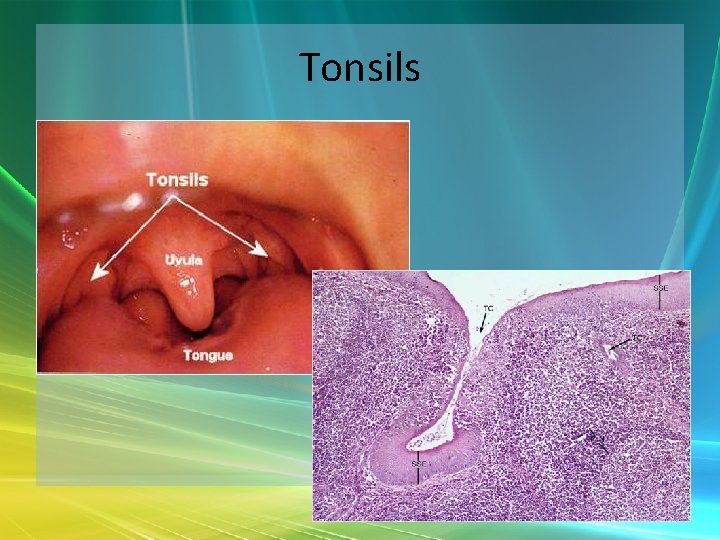
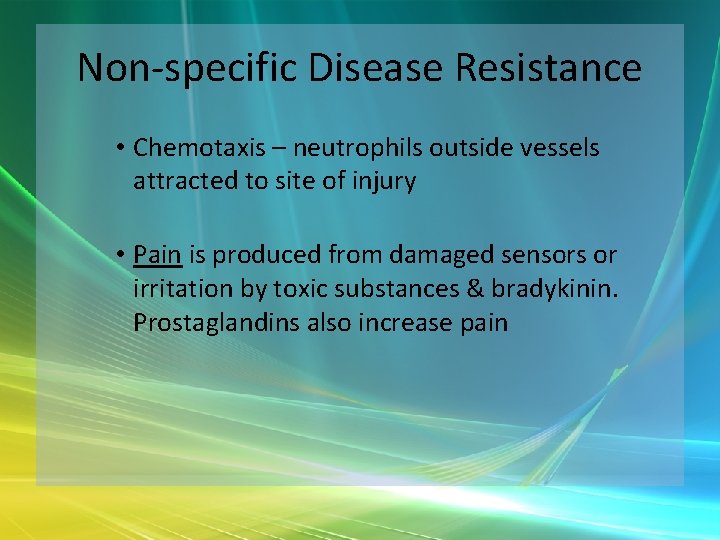
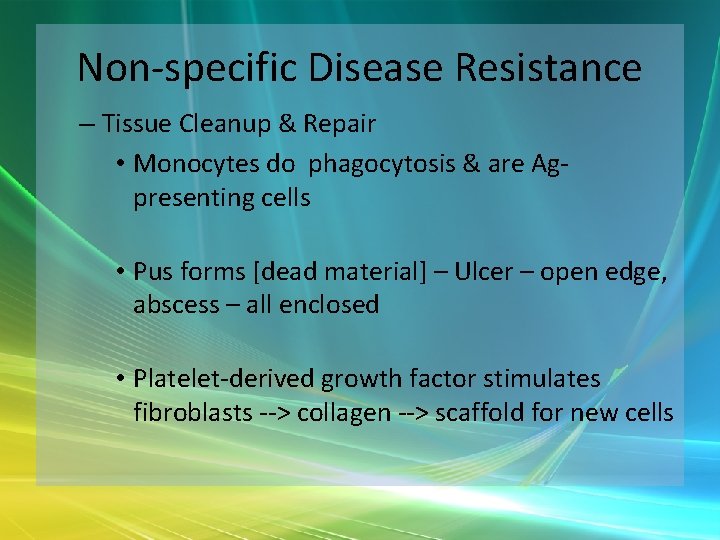
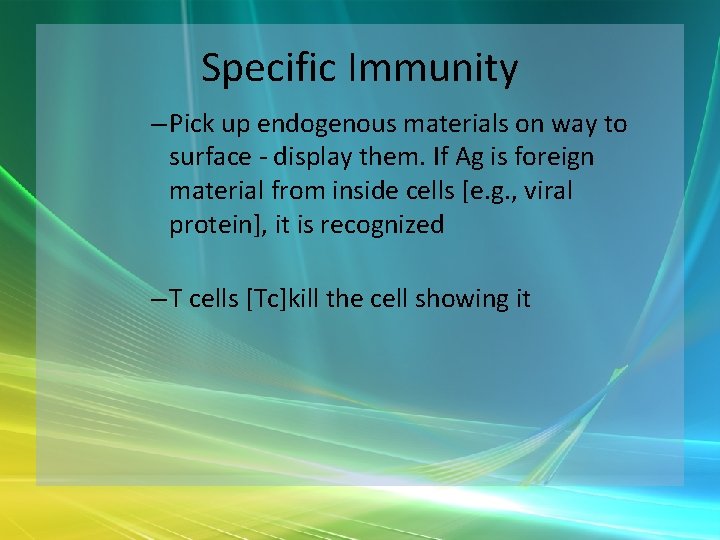
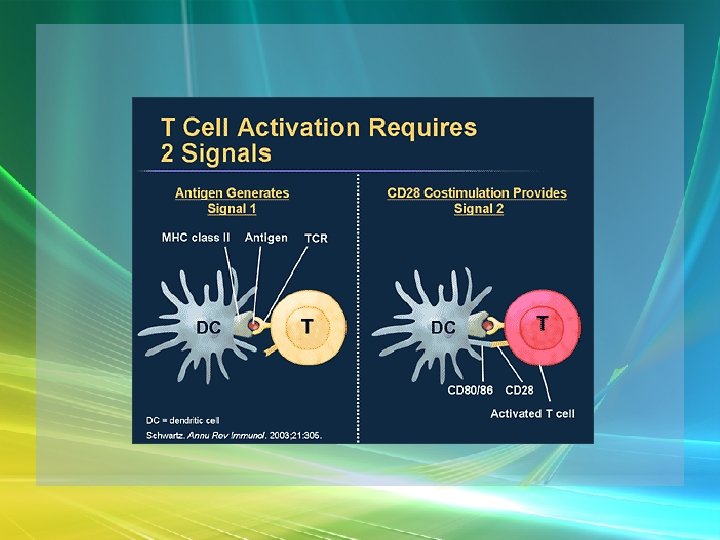
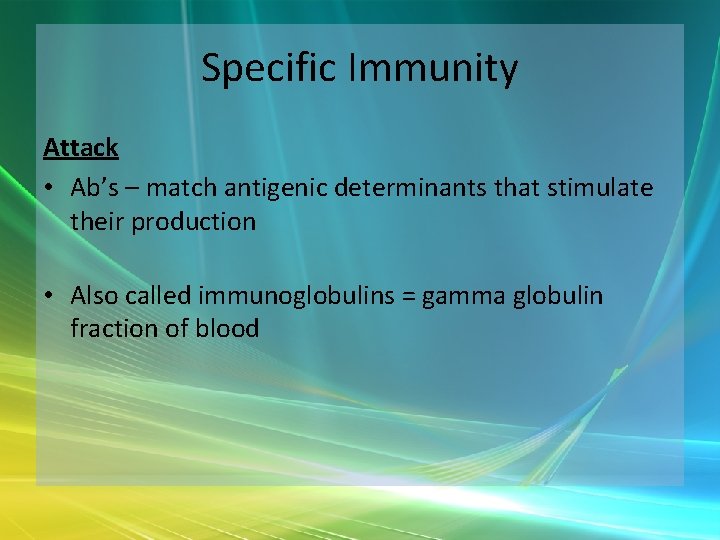
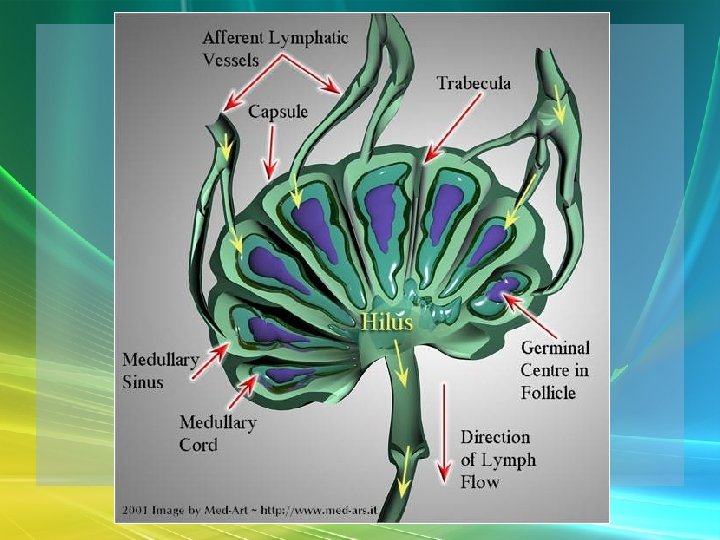
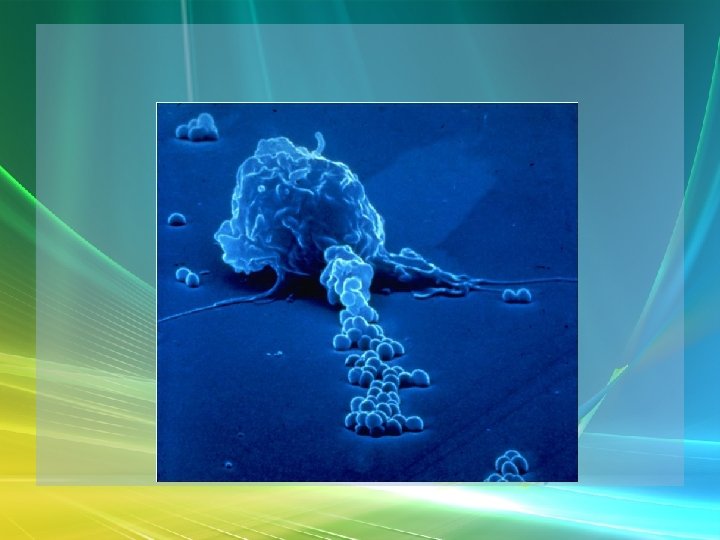
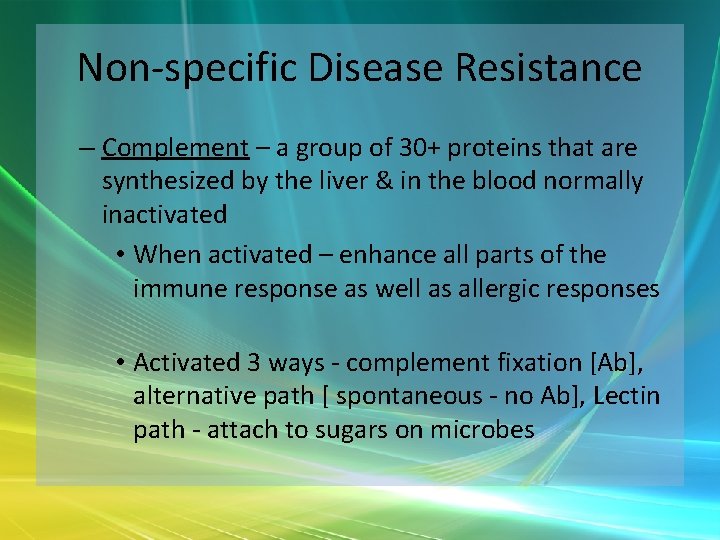
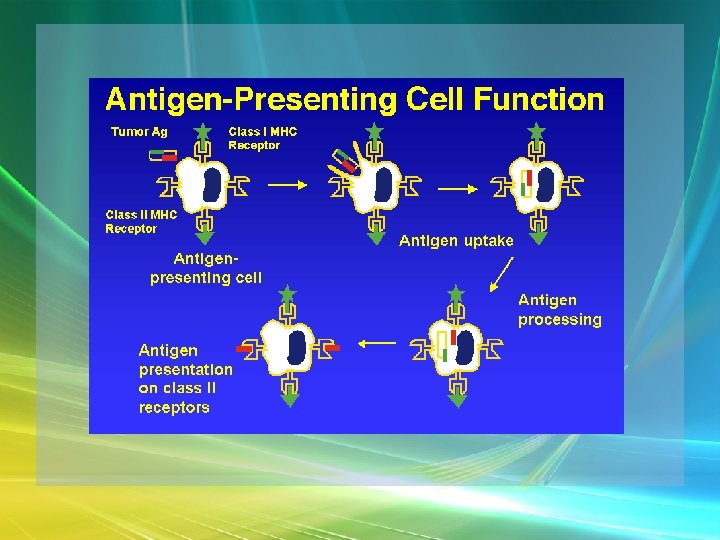
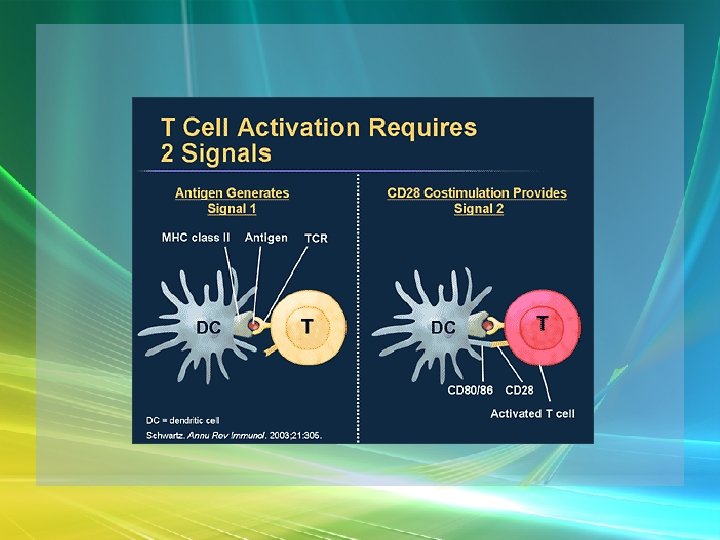
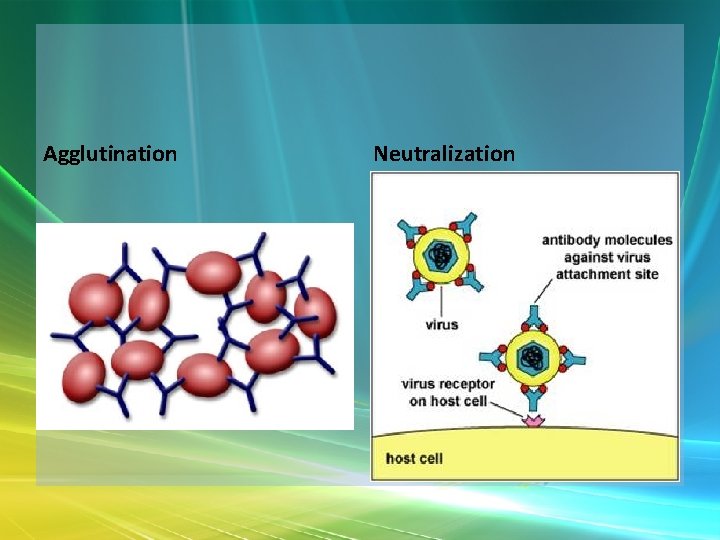
Specific Immunity T-Cell Activation • Activation [clonal selection] – 2 steps – Recognition & binding to presented complex by a specific T-cell receptor – Co-stimulation – required second signal – from cytokines, & plasma membrane molecules on APC’s
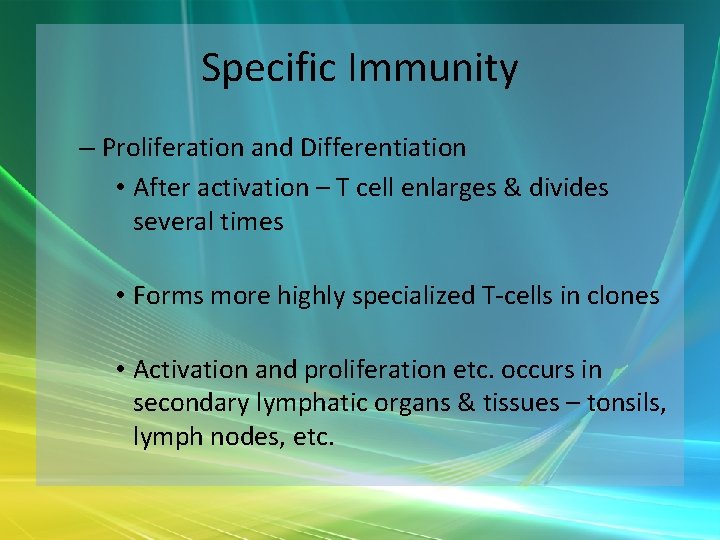
Specific Immunity – Proliferation and Differentiation • After activation – T cell enlarges & divides several times • Forms more highly specialized T-cells in clones • Activation and proliferation etc. occurs in secondary lymphatic organs & tissues – tonsils, lymph nodes, etc.
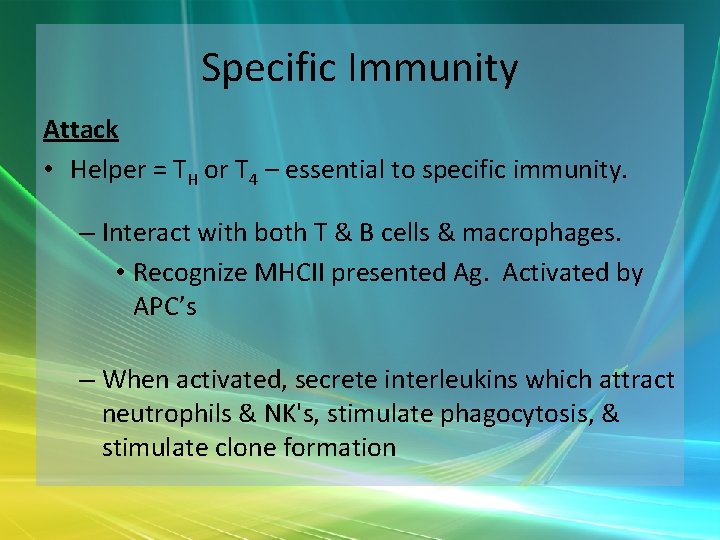
Specific Immunity Attack • Helper = TH or T 4 – essential to specific immunity. – Interact with both T & B cells & macrophages. • Recognize MHCII presented Ag. Activated by APC’s – When activated, secrete interleukins which attract neutrophils & NK's, stimulate phagocytosis, & stimulate clone formation
Specific Immunity • Cytotoxic = TC or T 8 = Killer T cells – Recognize MHCI bound Ag [viral, tumor, transplant] – TC – attach to invader – use Perforin – pokes holes in target cell’s membrane => lysis, interferons, & tumor necrosis factor [kills cancer cells]
Specific Immunity Memory • T Cells– left over after cell-mediated response is done can initiate a new response if the Ag reappears
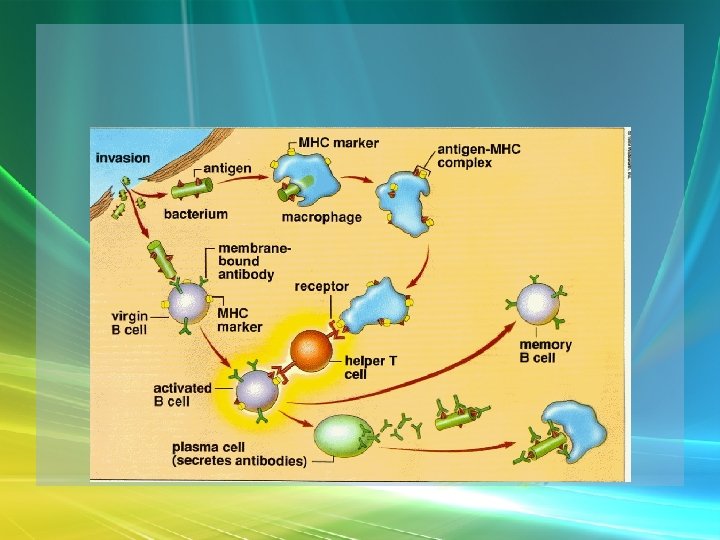
Specific Immunity Humoral Immunity Recognition • B Cells - each has receptors to only one Ag • B cell Ag receptors bind to Ag – several pieces link together & are then endocytosed through receptor mediated process
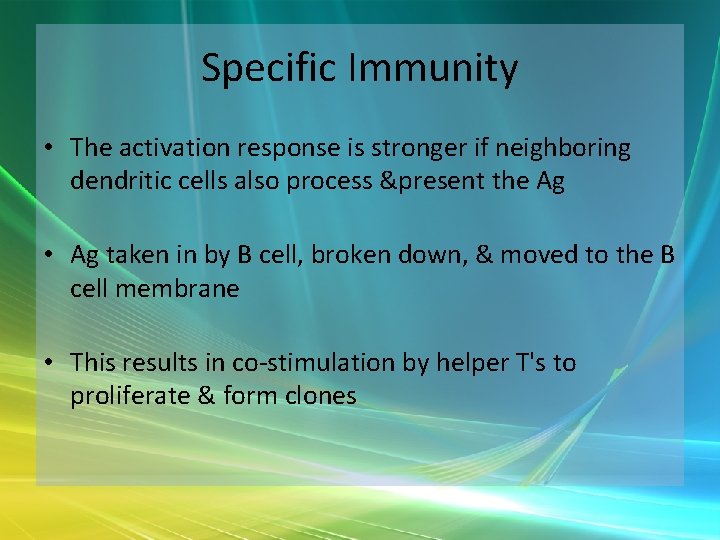
Specific Immunity • The activation response is stronger if neighboring dendritic cells also process &present the Ag • Ag taken in by B cell, broken down, & moved to the B cell membrane • This results in co-stimulation by helper T's to proliferate & form clones
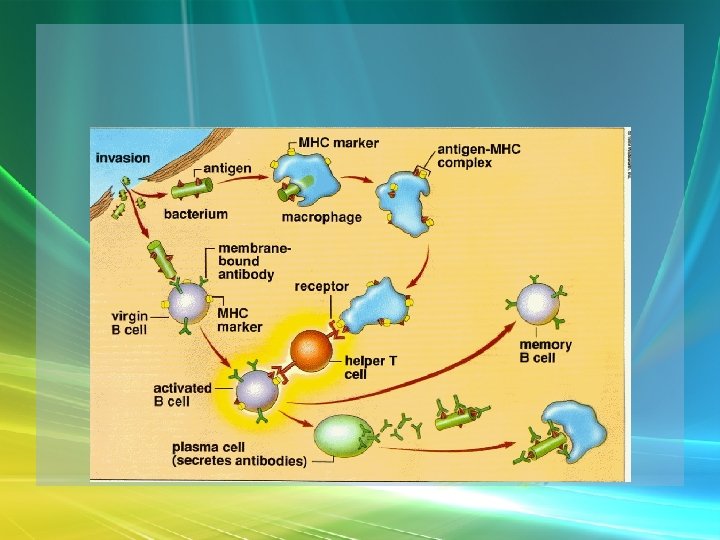
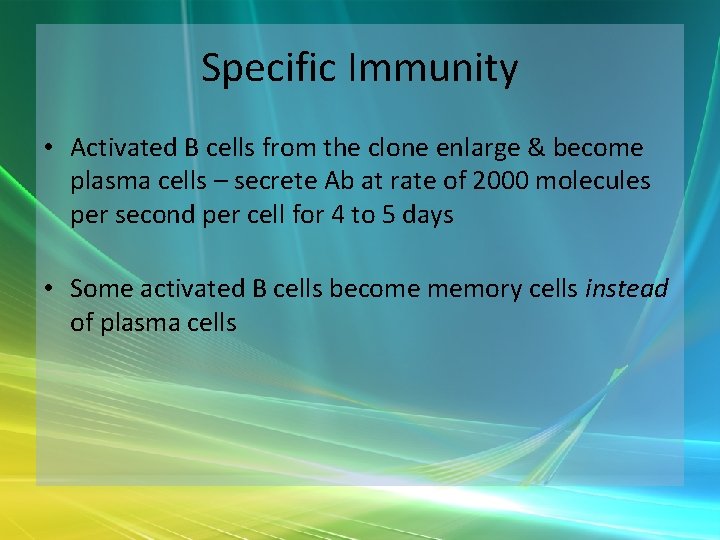
Specific Immunity • Activated B cells from the clone enlarge & become plasma cells – secrete Ab at rate of 2000 molecules per second per cell for 4 to 5 days • Some activated B cells become memory cells instead of plasma cells
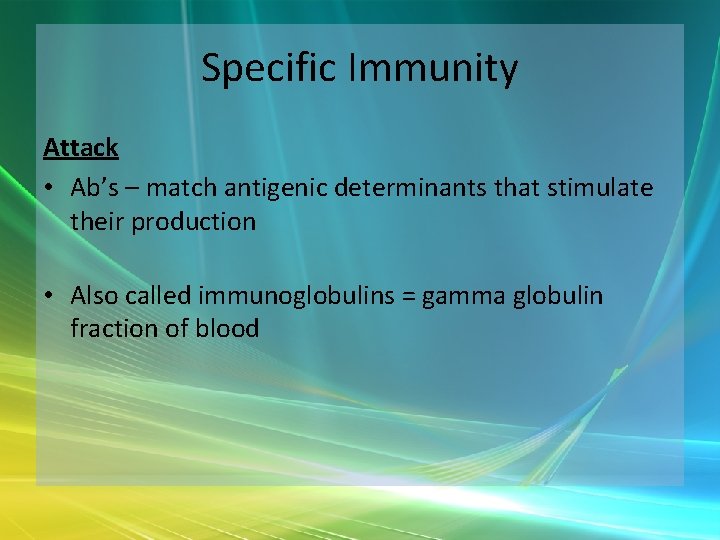
Specific Immunity Attack • Ab’s – match antigenic determinants that stimulate their production • Also called immunoglobulins = gamma globulin fraction of blood
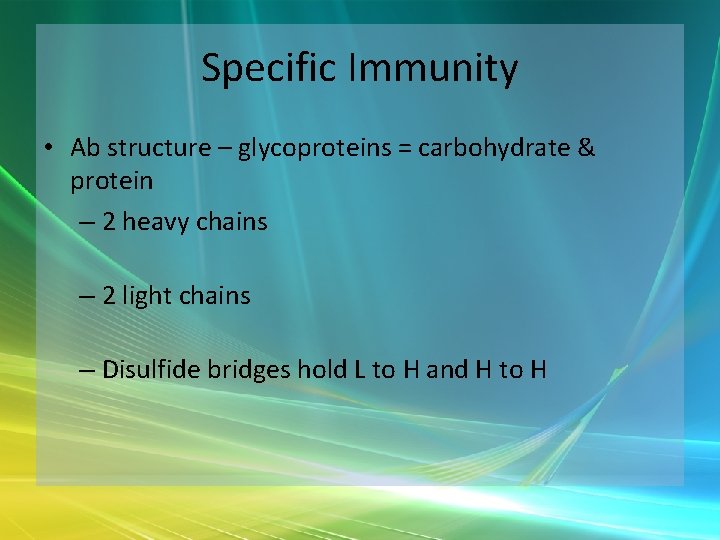
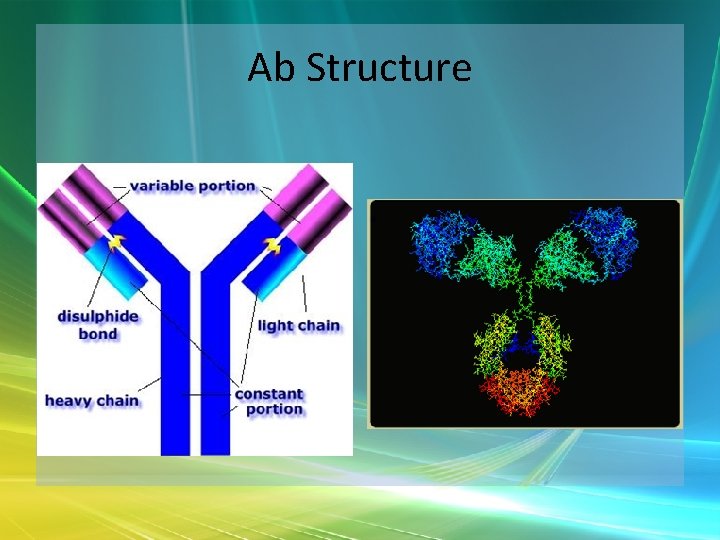
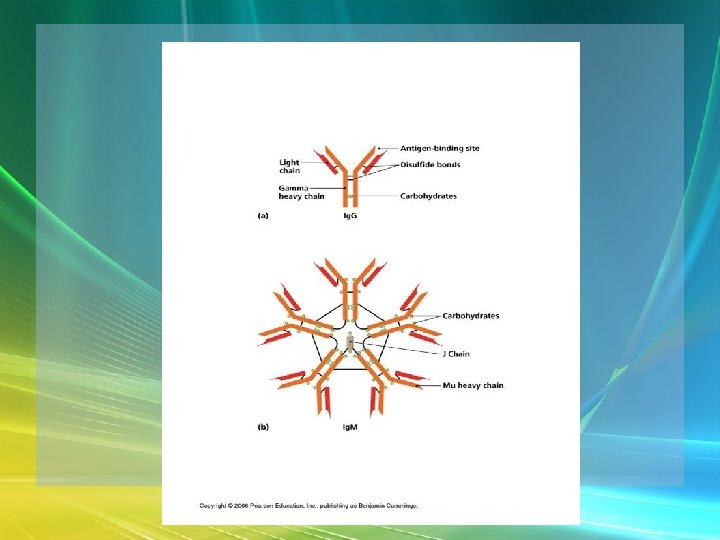
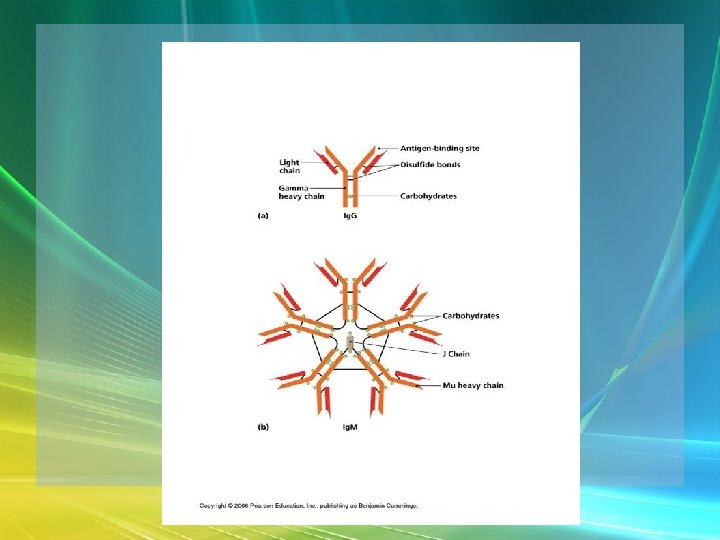
Specific Immunity • Ab structure – glycoproteins = carbohydrate & protein – 2 heavy chains – 2 light chains – Disulfide bridges hold L to H and H to H
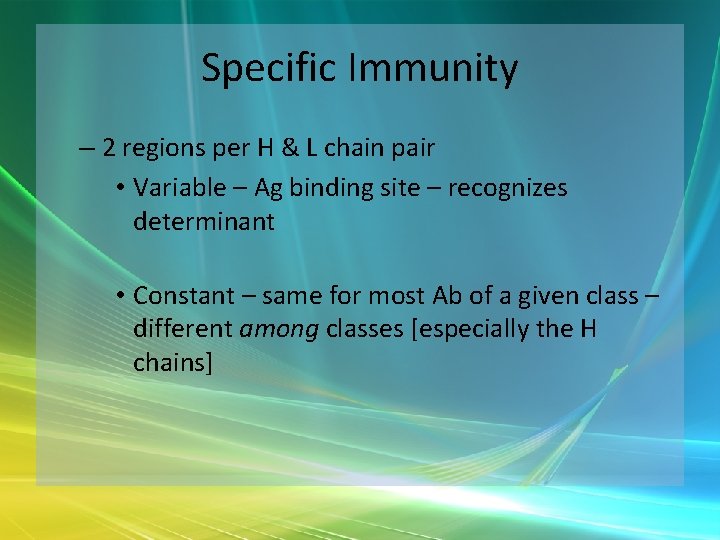
Specific Immunity – 2 regions per H & L chain pair • Variable – Ag binding site – recognizes determinant • Constant – same for most Ab of a given class – different among classes [especially the H chains]
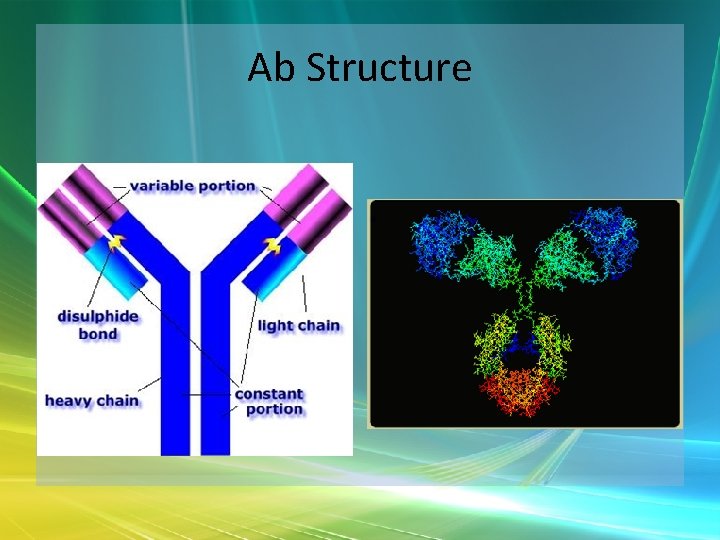
Ab Structure
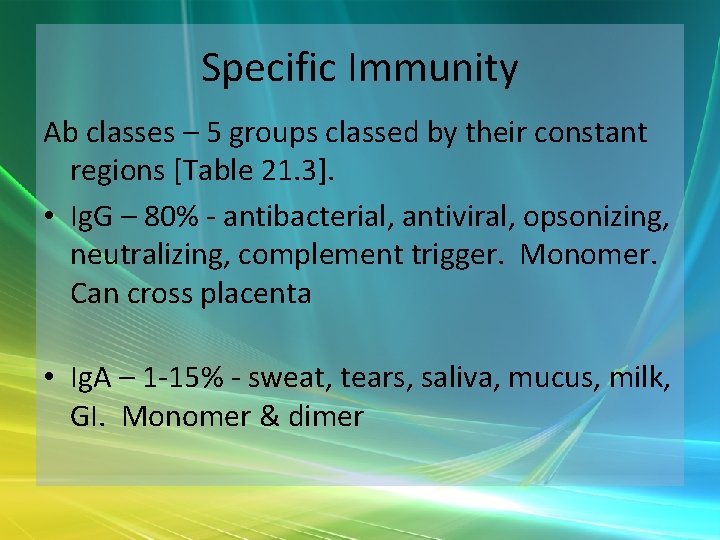
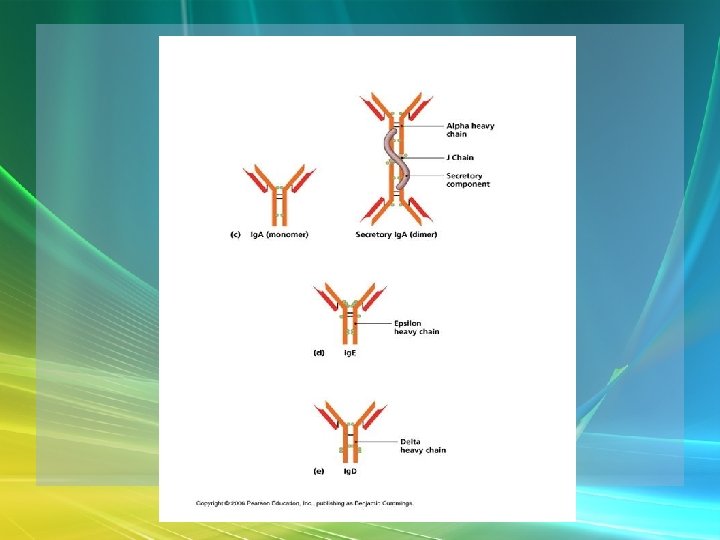
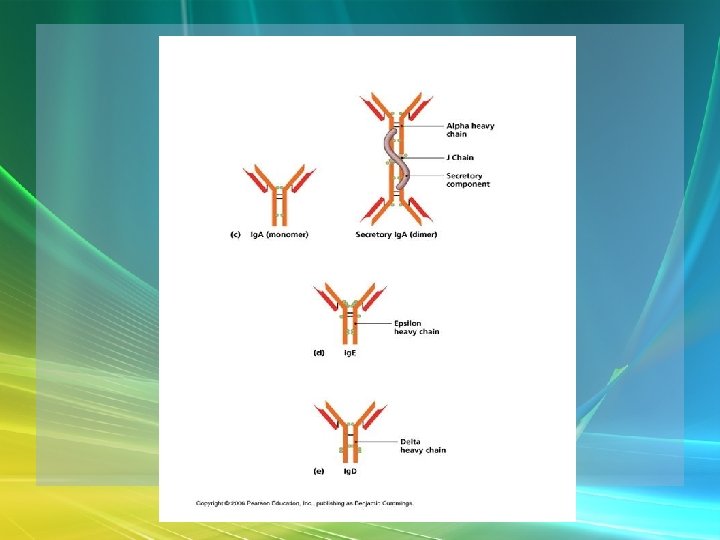
Specific Immunity Ab classes – 5 groups classed by their constant regions [Table 21. 3]. • Ig. G – 80% - antibacterial, antiviral, opsonizing, neutralizing, complement trigger. Monomer. Can cross placenta • Ig. A – 1 -15% - sweat, tears, saliva, mucus, milk, GI. Monomer & dimer
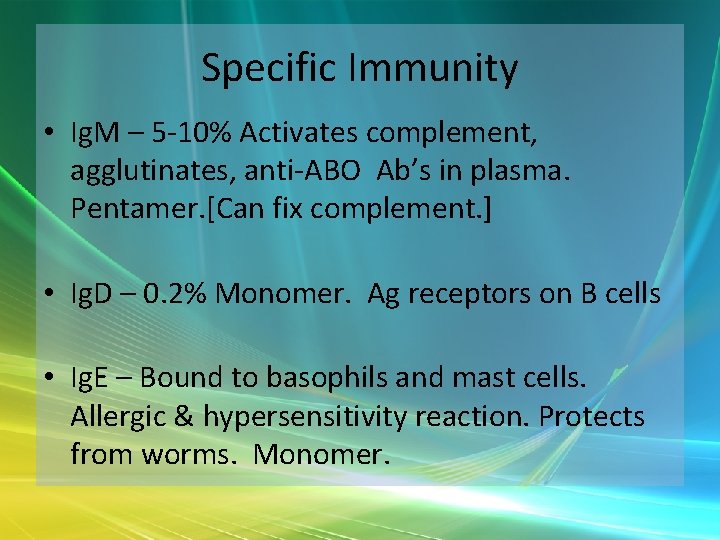
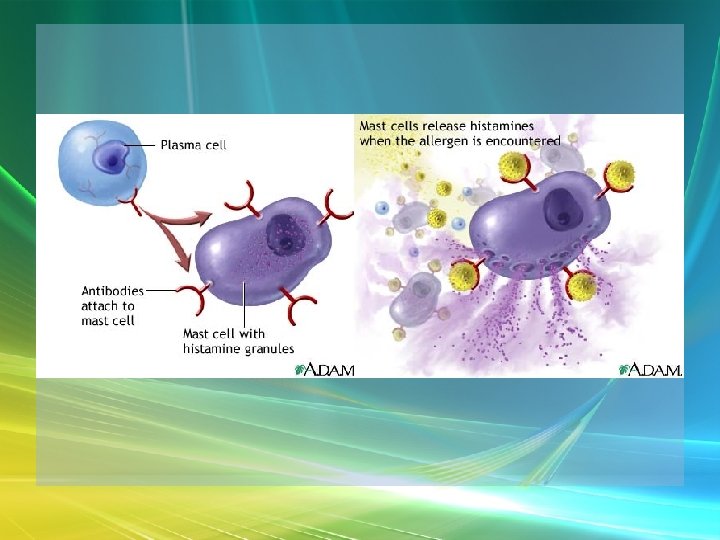
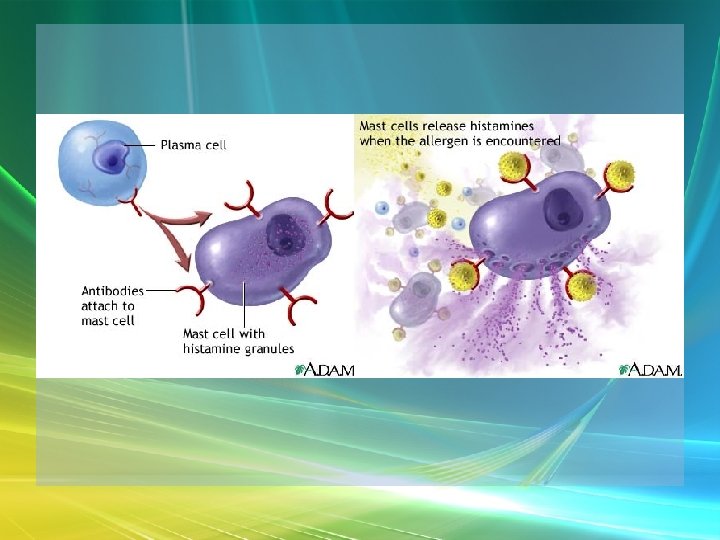
Specific Immunity • Ig. M – 5 -10% Activates complement, agglutinates, anti-ABO Ab’s in plasma. Pentamer. [Can fix complement. ] • Ig. D – 0. 2% Monomer. Ag receptors on B cells • Ig. E – Bound to basophils and mast cells. Allergic & hypersensitivity reaction. Protects from worms. Monomer.
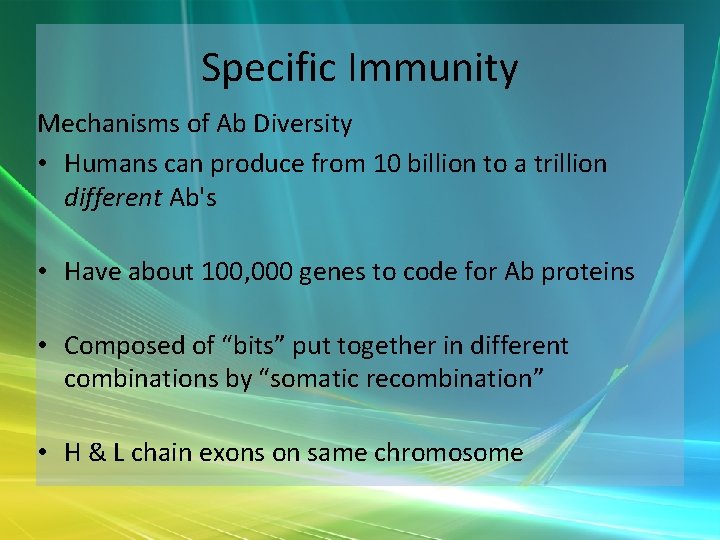
Specific Immunity Mechanisms of Ab Diversity • Humans can produce from 10 billion to a trillion different Ab's • Have about 100, 000 genes to code for Ab proteins • Composed of “bits” put together in different combinations by “somatic recombination” • H & L chain exons on same chromosome

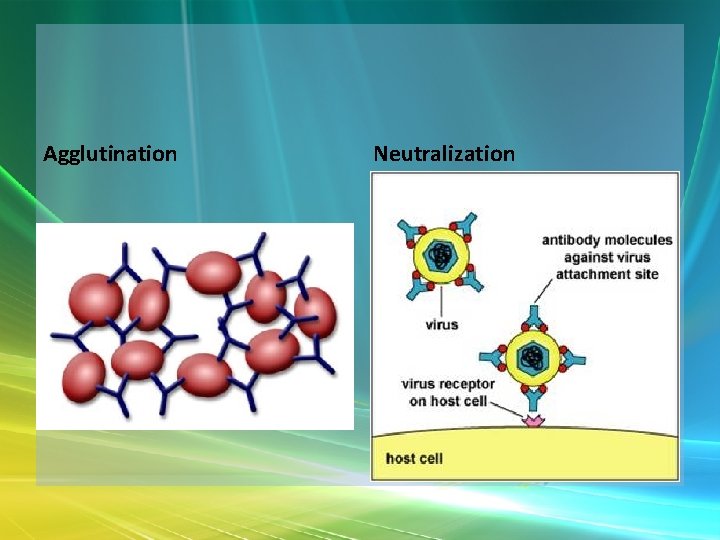
Specific Immunity Ab Actions – inactivate and tag for destruction • Neutralization – bind to & block antigen/toxin • Agglutination/ precipitation –clumping • Complement Fixation • Complement also stimulates inflammatory response in region, Opsonization – coat & make sticky to phagocytes
Agglutination Neutralization
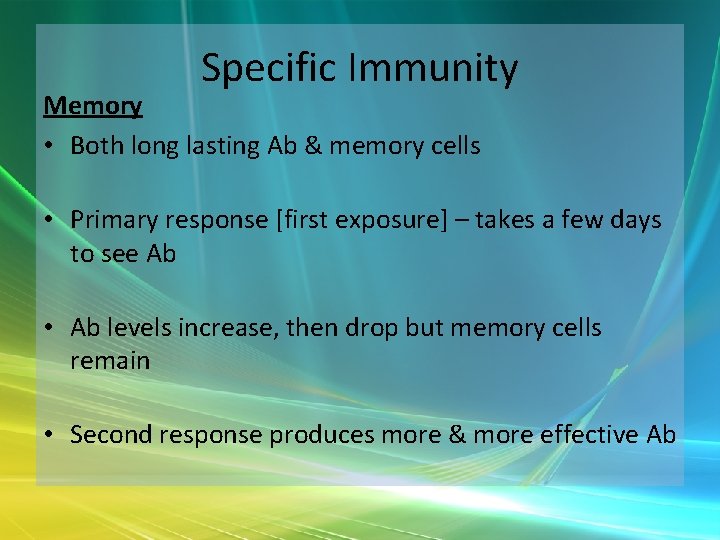
Specific Immunity Memory • Both long lasting Ab & memory cells • Primary response [first exposure] – takes a few days to see Ab • Ab levels increase, then drop but memory cells remain • Second response produces more & more effective Ab

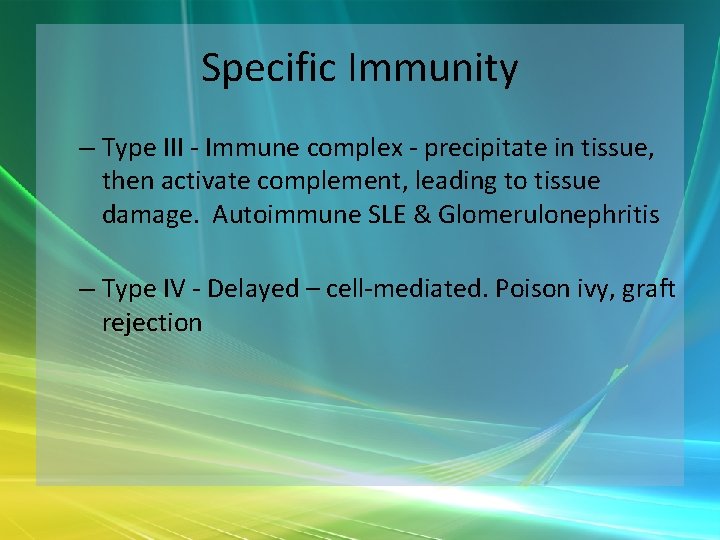
Specific Immunity Immune System Disorders • Allergy – hypersensitivity. One system has 4 types: – Type I = immediate [acute] - hay fever, etc. Anaphylactic shock can occur. – Type II - antibody-dependent cytotoxic [Ab opsonizes or complement fixation] Transfusion reactions, some drug reactions
Specific Immunity – Type III - Immune complex - precipitate in tissue, then activate complement, leading to tissue damage. Autoimmune SLE & Glomerulonephritis – Type IV - Delayed – cell-mediated. Poison ivy, graft rejection
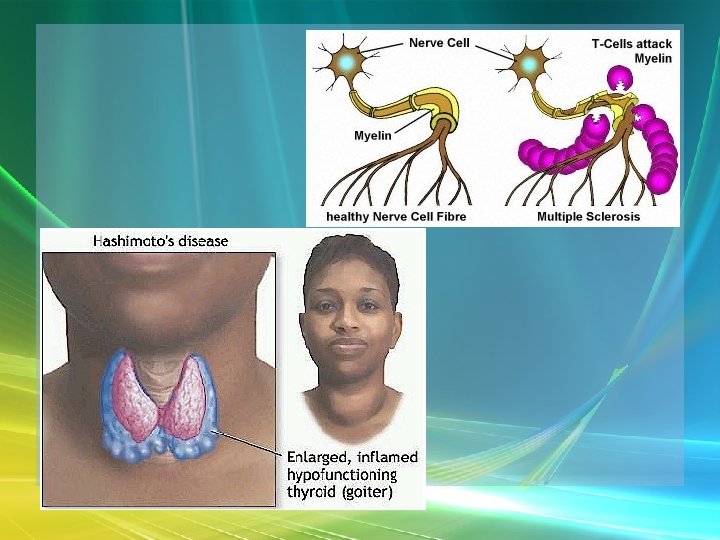
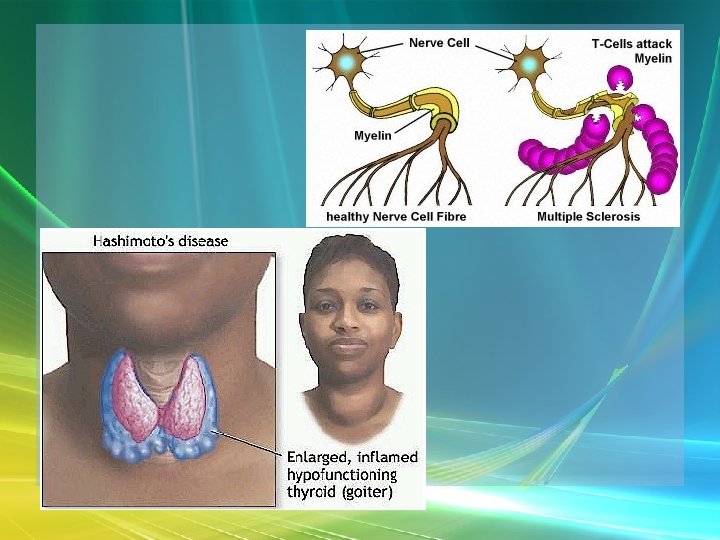
Specific Immunity Autoimmune Diseases • Failures of self-tolerance • 3 causes - cross-reactivity [e. g. , strep], abnormal exposure to occult Ag [usually sequestered]Hashimoto's thyroiditis], Change in self-Ag structure [type I diabetes]
Specific Immunity • Immunodeficiency Diseases – SCID - "boy in bubble“ – AIDS - review on own