Immunology The Lymphatic System Lymphatic System p Lymphatic




- Slides: 80

Immunology The Lymphatic System
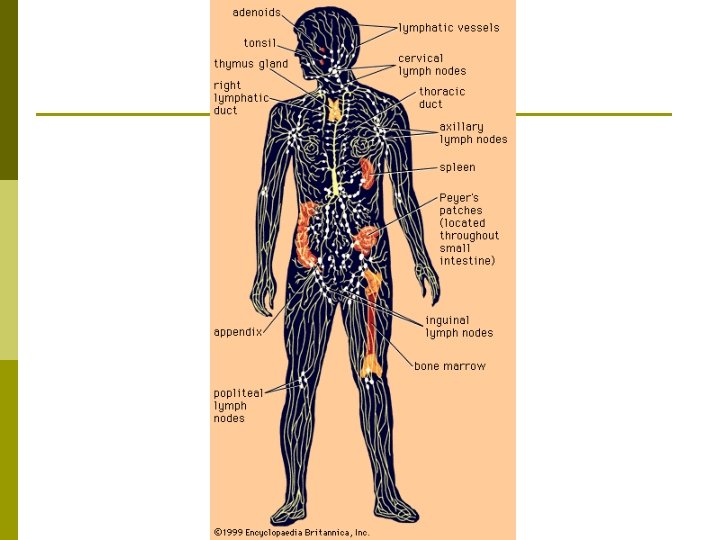
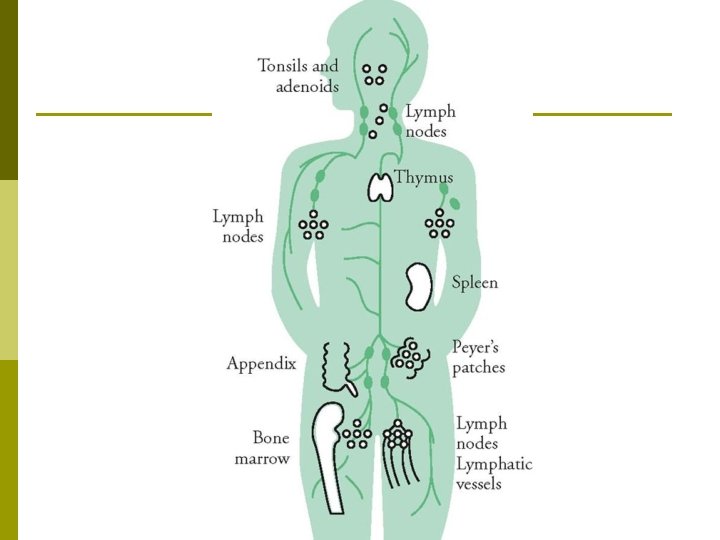
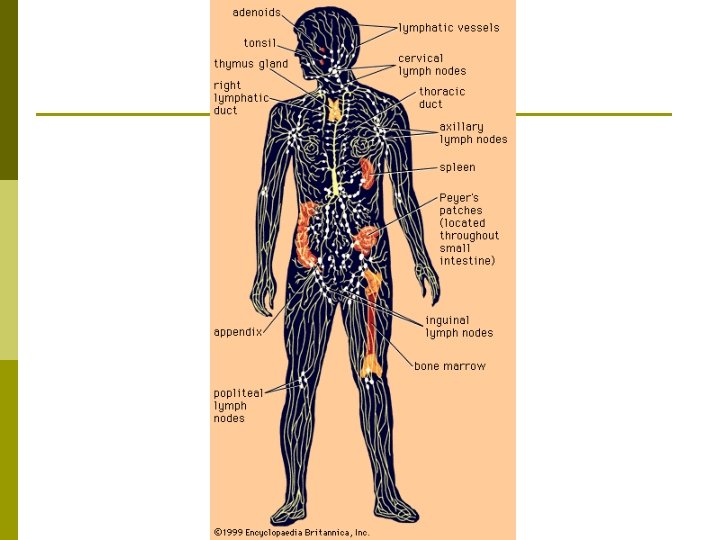
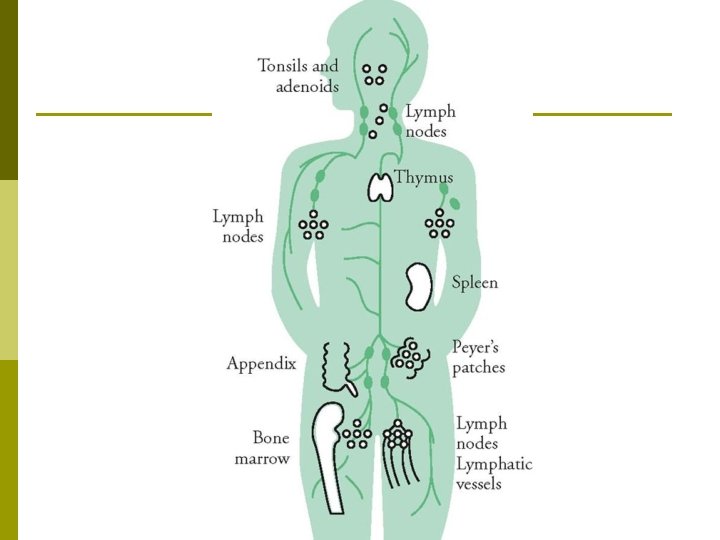
Lymphatic System p Lymphatic System: Provides the body with a defense mechanism against foreign invaders. n n n Most interstitial fluid surrounding the capillary beds is reabsorbed into the capillaries - the lymphatic ducts picks up the remaining interstitial. Pathogens are filtered out through the lymph nodes. Lymph nodes contain concentrations of lymphocytes & macrophages to respond with to the pathogens.
Lymphatic System Lymph: The clear fluid in the lymphatic vessels. p Subclavian Veins return the lymph into the heart. p
The Lymphatic System p Major Functions of the Lymphatic System: n n n Draining excess fluid from tissues to be returned to the bloodstream. Transporting lipids & vitamins reabsorbed in the gastrointestinal tract to the bloodstream. Activating the body’s immune response to pathogens.
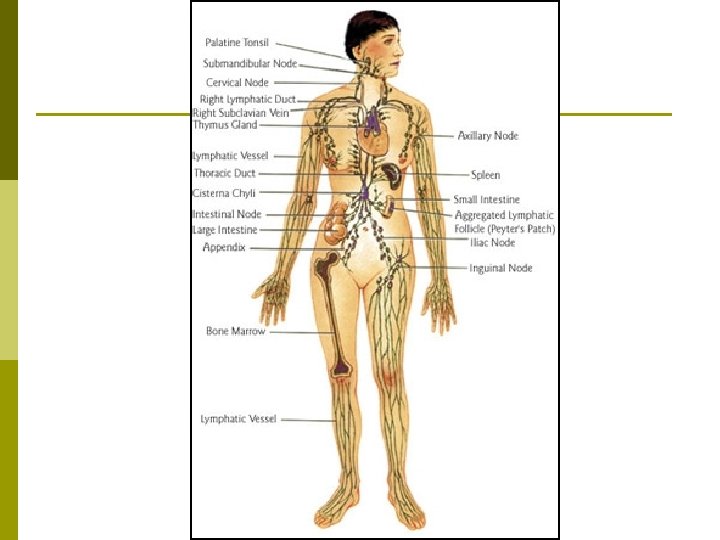
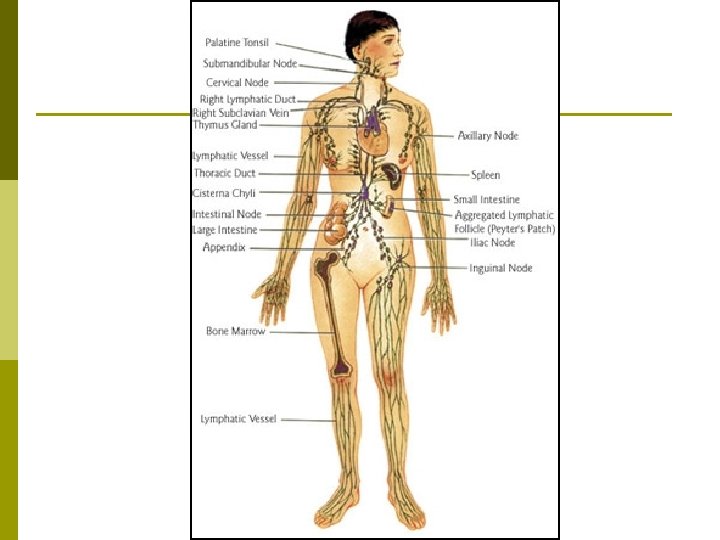
Lymphatic Anatomy p p Lymph: Clear fluid within the lymphatic vessels that has been reabsorbed from the interstitial fluid. Lymphatic Vessels: The vessel system that provides transportation for the lymph. n Lymphatic Capillaries: The start of the lymphatic system – endothelial cells that are closed at one end & have flaps that work as valves. p p n n These allow fluid & large proteins & foreign bodies to enter. Lacteals: Lymphatic capillaries in the small intestine that specialize in transporting lipids. Lymphatic Vessels: Structured in the same 3 layers as the blood vessels, but with thinner walls & more valves. Lymph Nodes: Bean-shaped structures positioned at regular intervals along the lymphatic vessel routes. p Approximately 600 total in the lymphatic system.
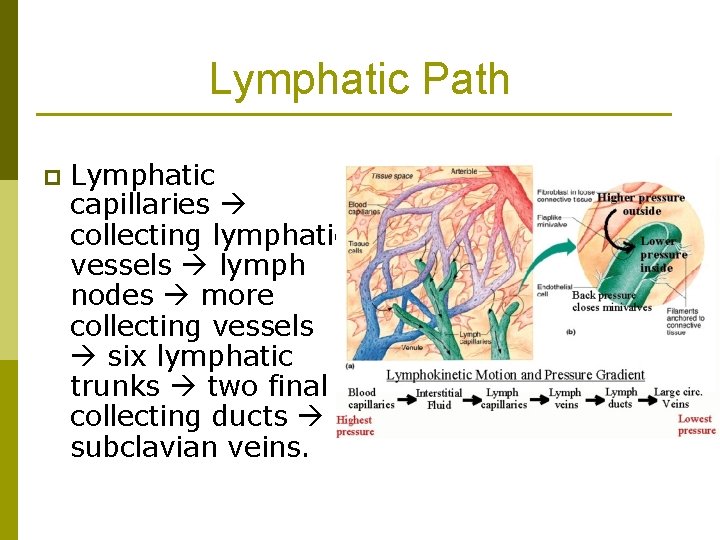
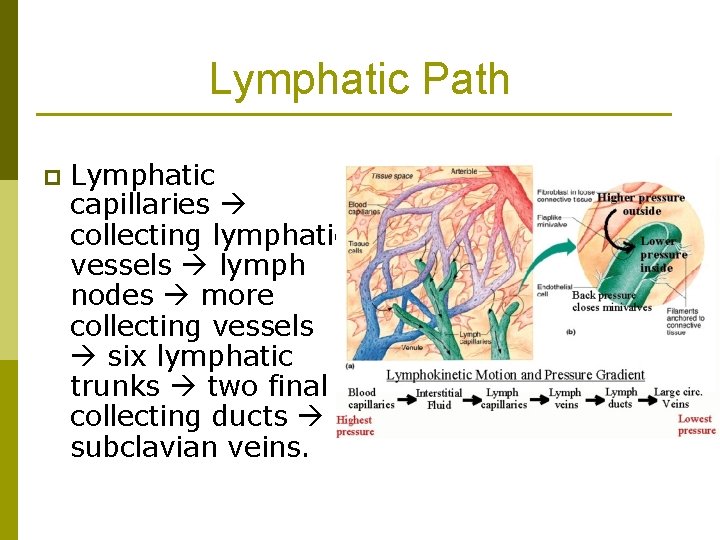
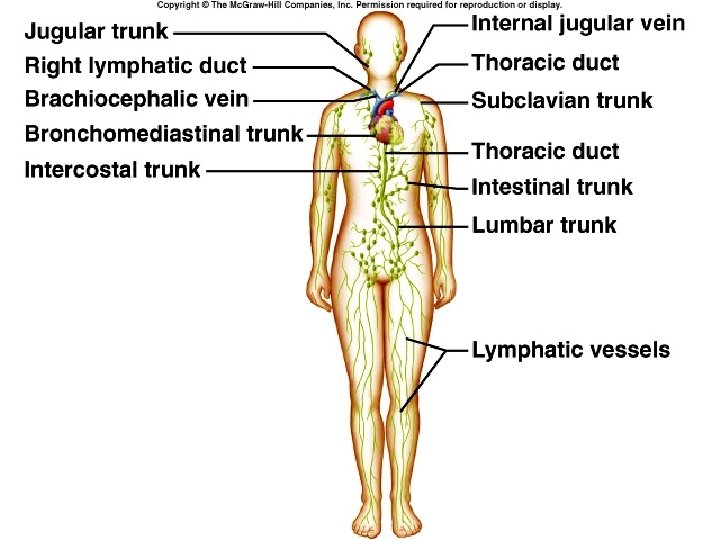
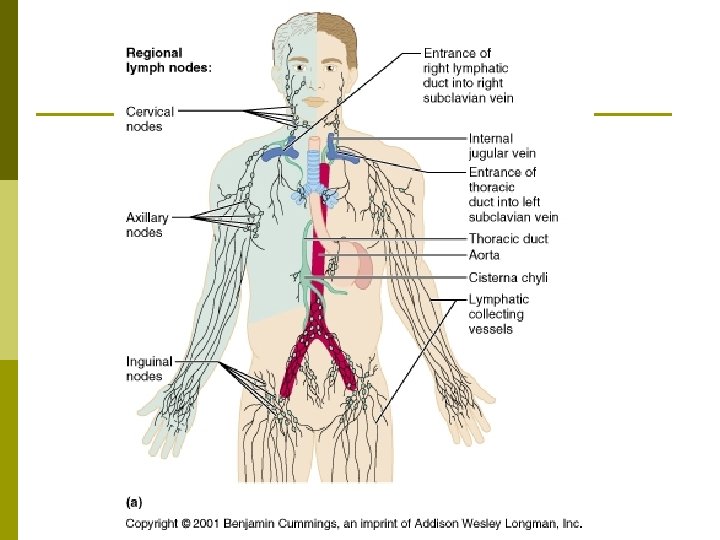
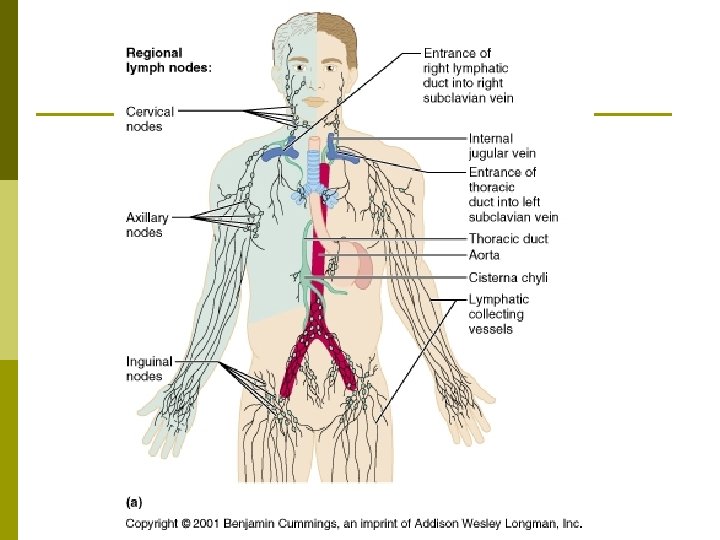
Lymphatic Path p Lymphatic capillaries collecting lymphatic vessels lymph nodes more collecting vessels six lymphatic trunks two final collecting ducts subclavian veins.
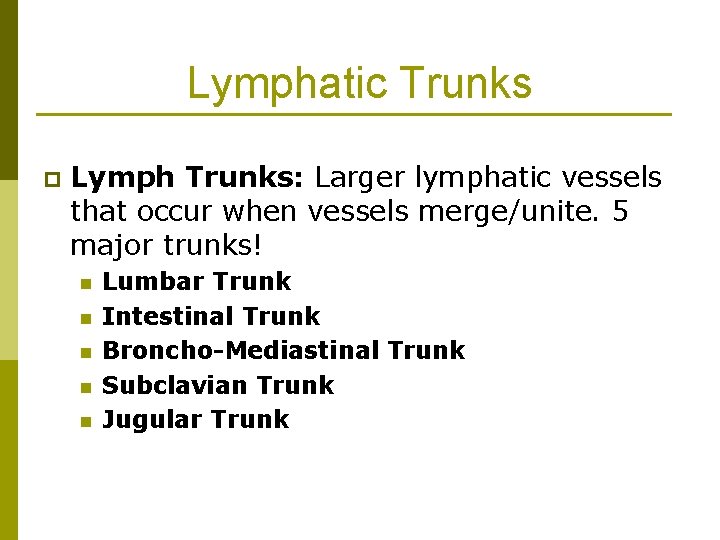
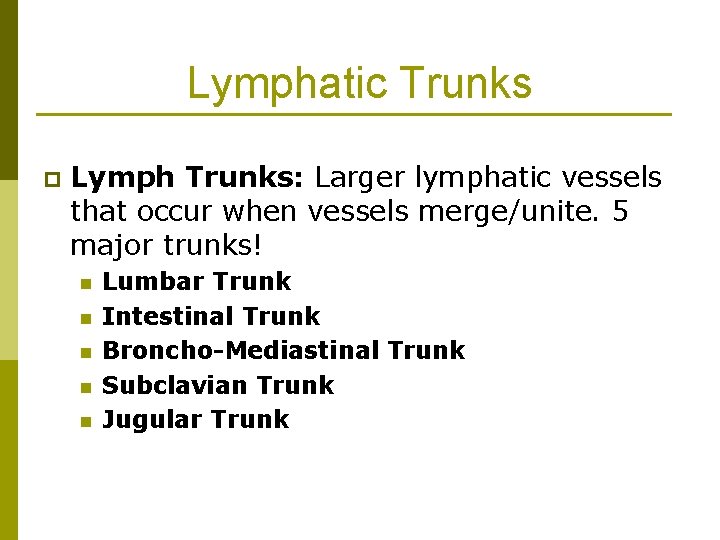
Lymphatic Trunks p Lymph Trunks: Larger lymphatic vessels that occur when vessels merge/unite. 5 major trunks! n n n Lumbar Trunk Intestinal Trunk Broncho-Mediastinal Trunk Subclavian Trunk Jugular Trunk
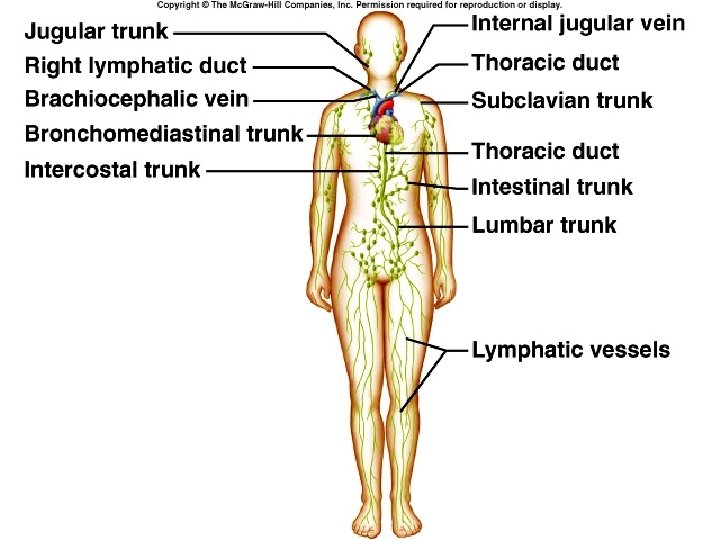
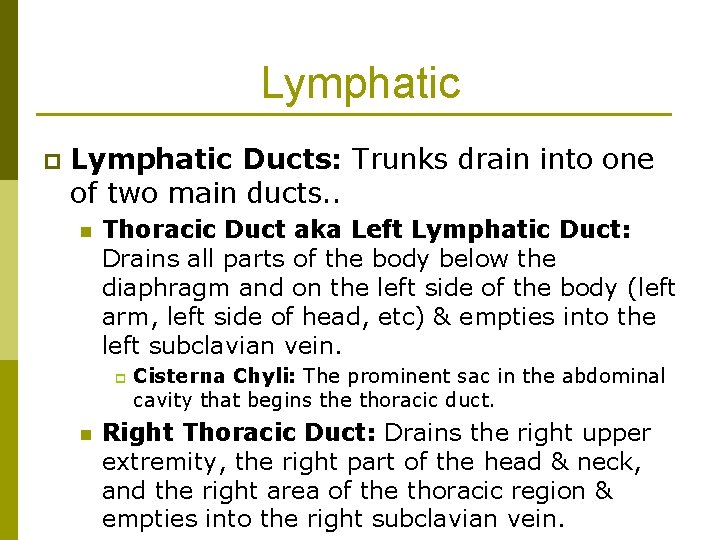
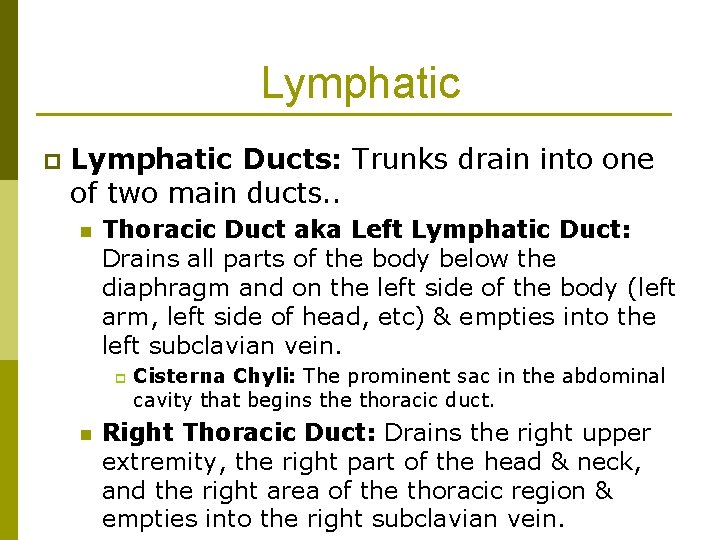
Lymphatic p Lymphatic Ducts: Trunks drain into one of two main ducts. . n Thoracic Duct aka Left Lymphatic Duct: Drains all parts of the body below the diaphragm and on the left side of the body (left arm, left side of head, etc) & empties into the left subclavian vein. p n Cisterna Chyli: The prominent sac in the abdominal cavity that begins the thoracic duct. Right Thoracic Duct: Drains the right upper extremity, the right part of the head & neck, and the right area of the thoracic region & empties into the right subclavian vein.
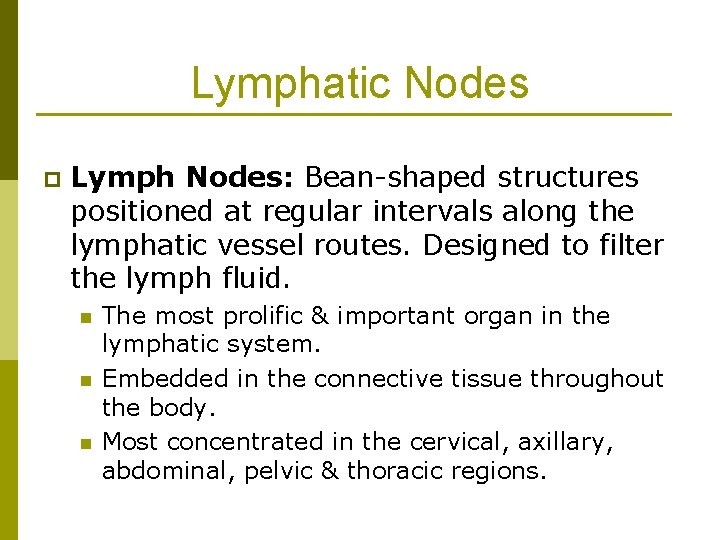
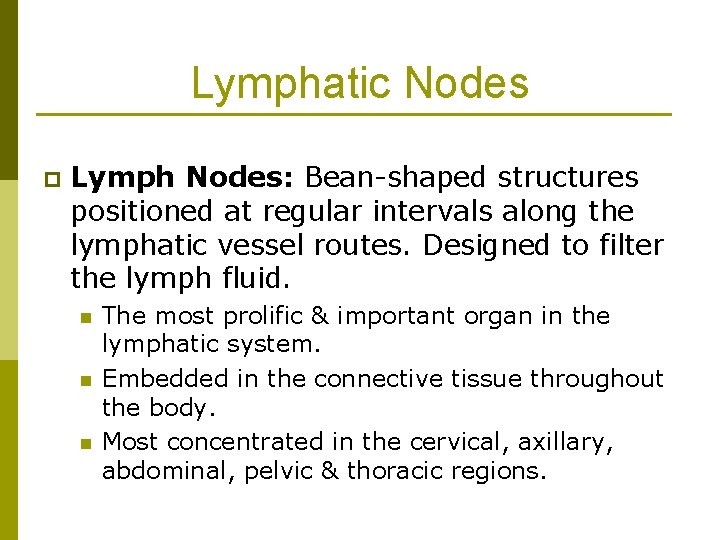
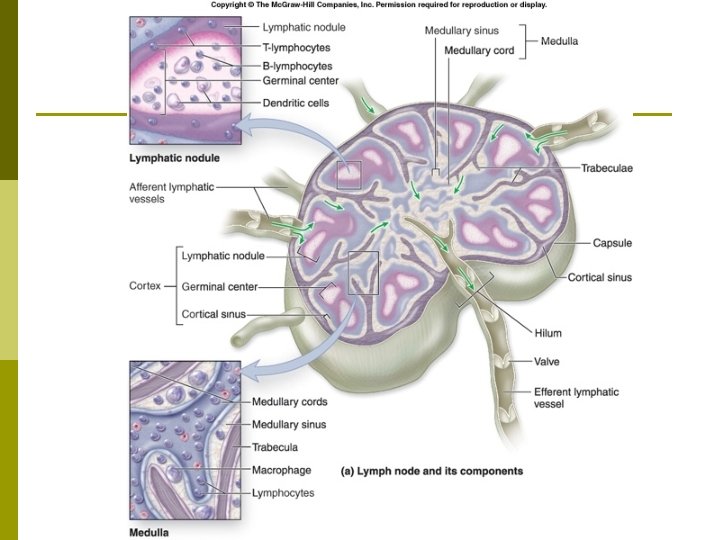
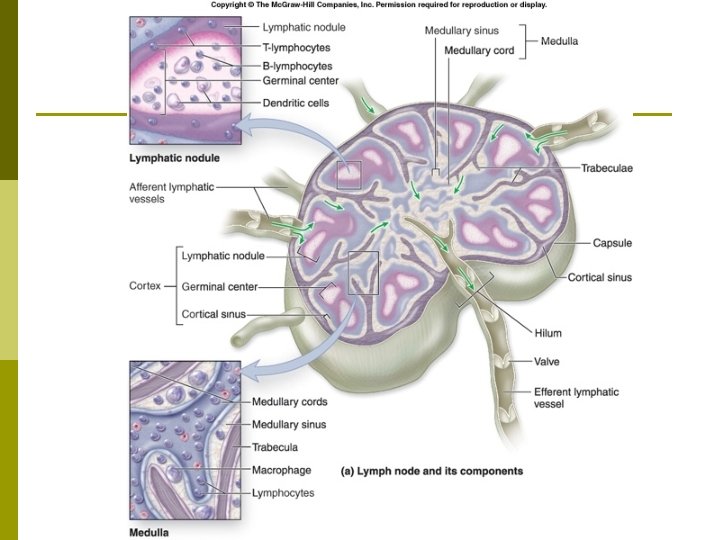
Lymphatic Nodes p Lymph Nodes: Bean-shaped structures positioned at regular intervals along the lymphatic vessel routes. Designed to filter the lymph fluid. n n n The most prolific & important organ in the lymphatic system. Embedded in the connective tissue throughout the body. Most concentrated in the cervical, axillary, abdominal, pelvic & thoracic regions.
Lymphatic Nodes Capsule: Layers of connective tissue that cover the lymph node. p Trabeculae: Extensions that divide the node into compartments & provide support & a network for blood vessels to travel along. p
Lymphatic Nodes p Cortex: Outer layer of the lymph node. n n p The outer area is responsible for collecting the B-lymphocytes or B-cells. The inner area is responsible for collecting Tcells. Medulla: The inner part of the lymph node that holds a concentration of macrophages, in addition to B cells & plasma cells.
Lymphatic Nodes Afferent Lymphatic Vessels: Structure that lymph enters the node through and directs the lymph inward toward the sinuses. p Sinuses: The portion of the lymph node where most of the filtering takes place. p Efferent Lymphatic Vessels: Structures that leave the node at the hilum. p n Hilum: A small depression where the efferent lymphatic vessels leave the lymph node.
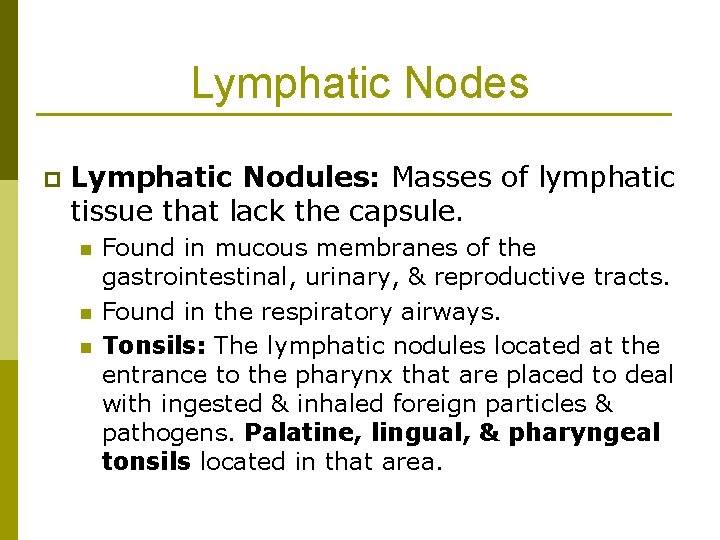
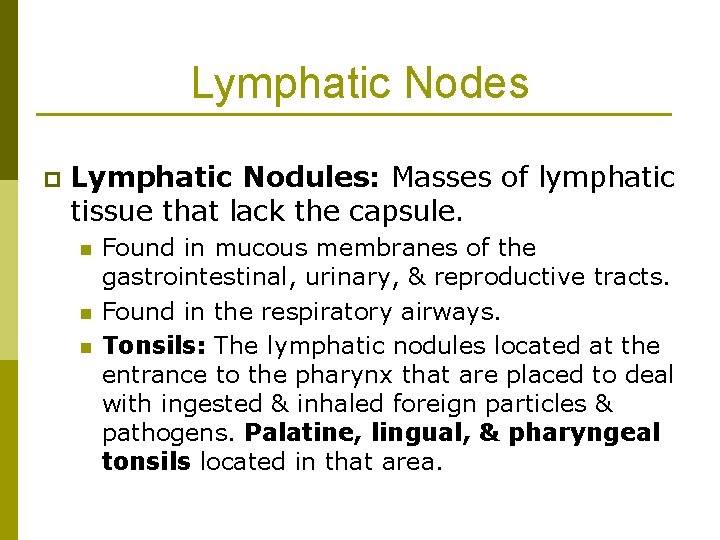
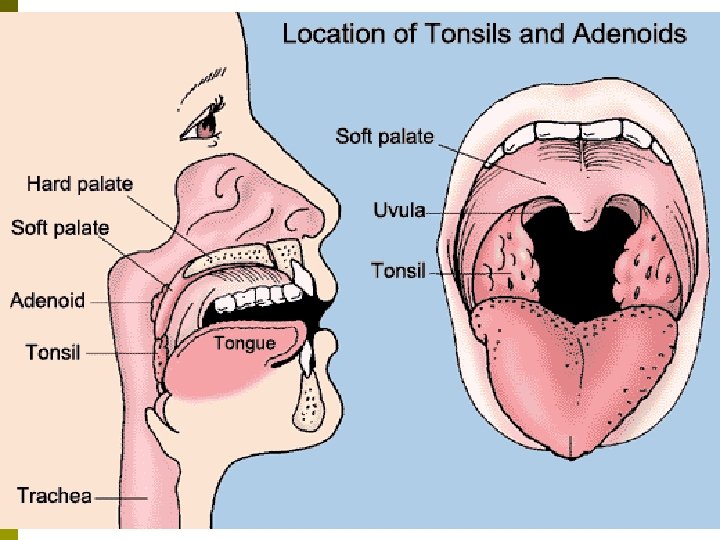
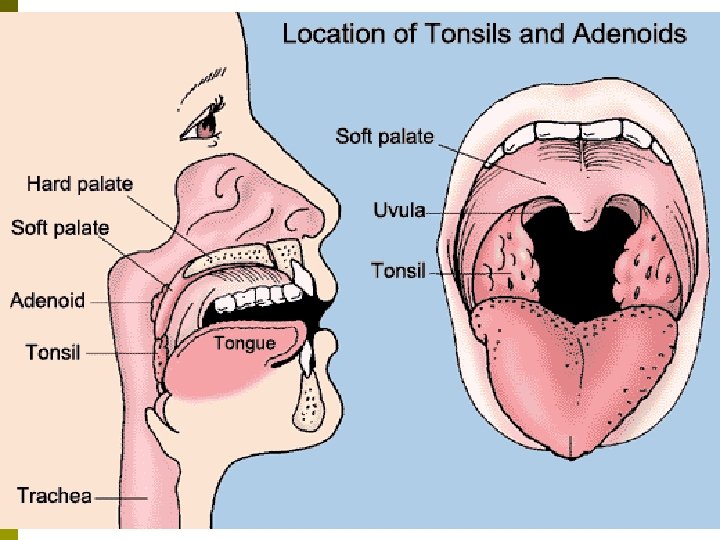
Lymphatic Nodes p Lymphatic Nodules: Masses of lymphatic tissue that lack the capsule. n n n Found in mucous membranes of the gastrointestinal, urinary, & reproductive tracts. Found in the respiratory airways. Tonsils: The lymphatic nodules located at the entrance to the pharynx that are placed to deal with ingested & inhaled foreign particles & pathogens. Palatine, lingual, & pharyngeal tonsils located in that area.
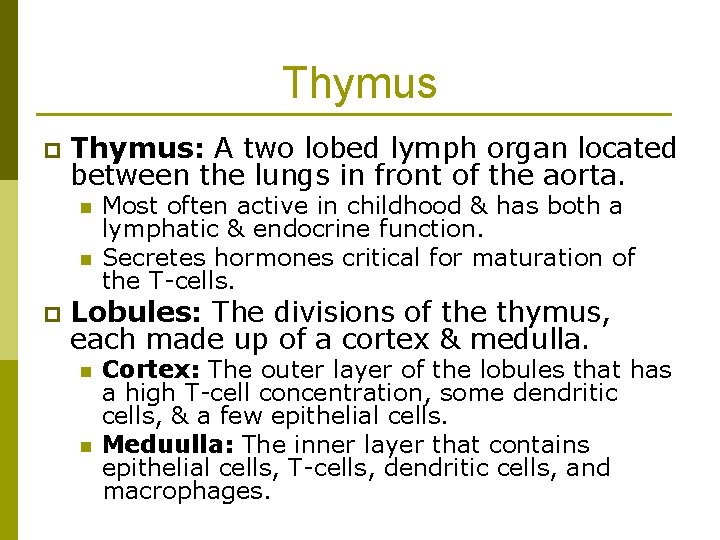
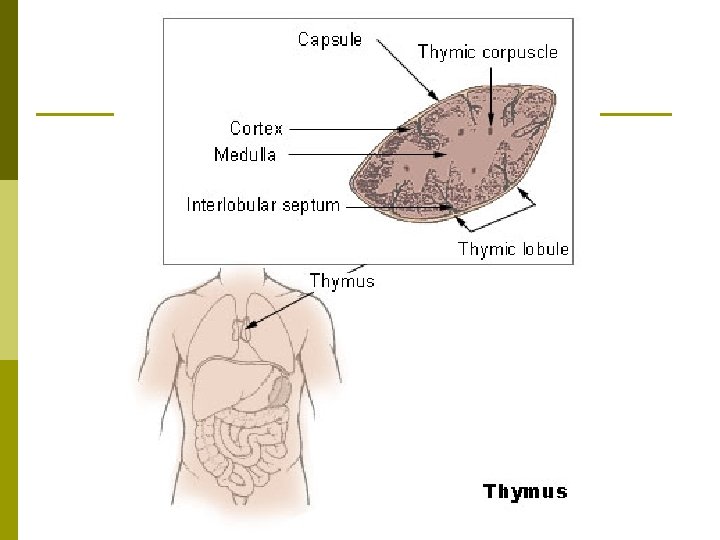
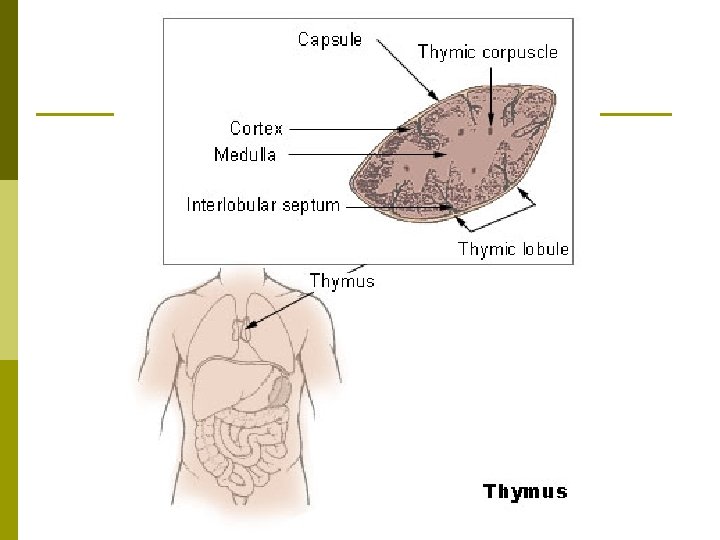
Thymus p Thymus: A two lobed lymph organ located between the lungs in front of the aorta. n n p Most often active in childhood & has both a lymphatic & endocrine function. Secretes hormones critical for maturation of the T-cells. Lobules: The divisions of the thymus, each made up of a cortex & medulla. n n Cortex: The outer layer of the lobules that has a high T-cell concentration, some dendritic cells, & a few epithelial cells. Meduulla: The inner layer that contains epithelial cells, T-cells, dendritic cells, and macrophages.
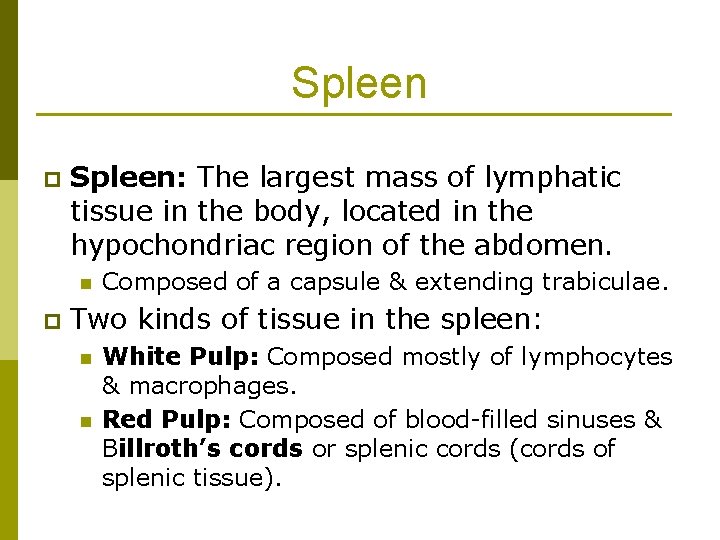
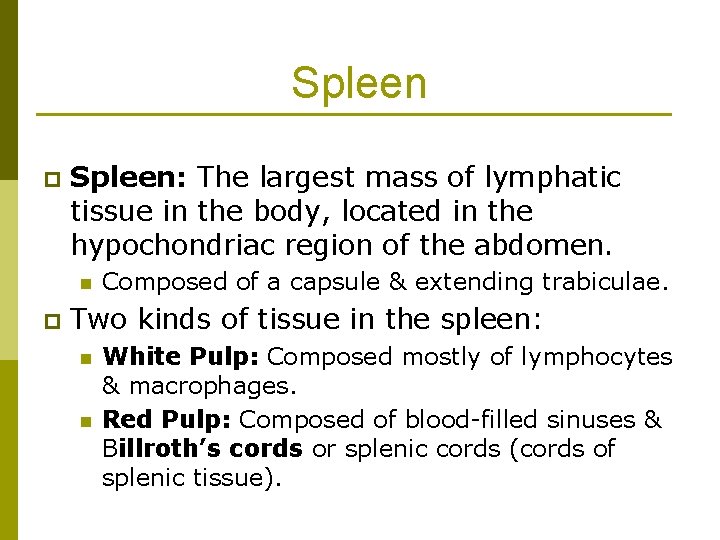
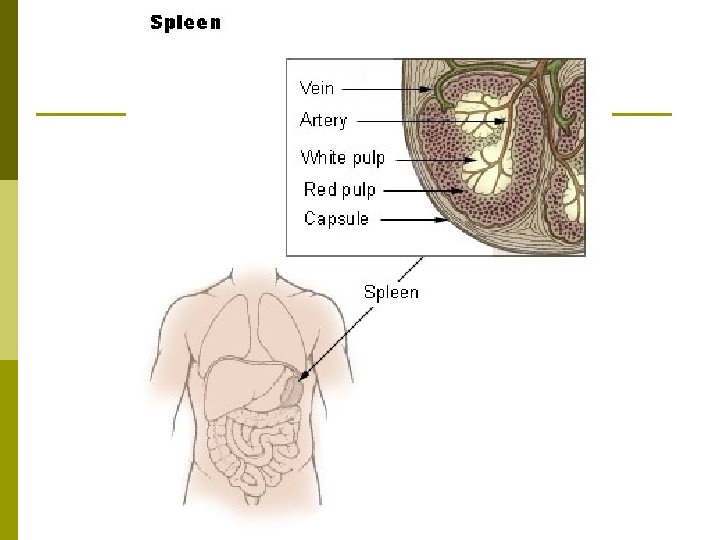
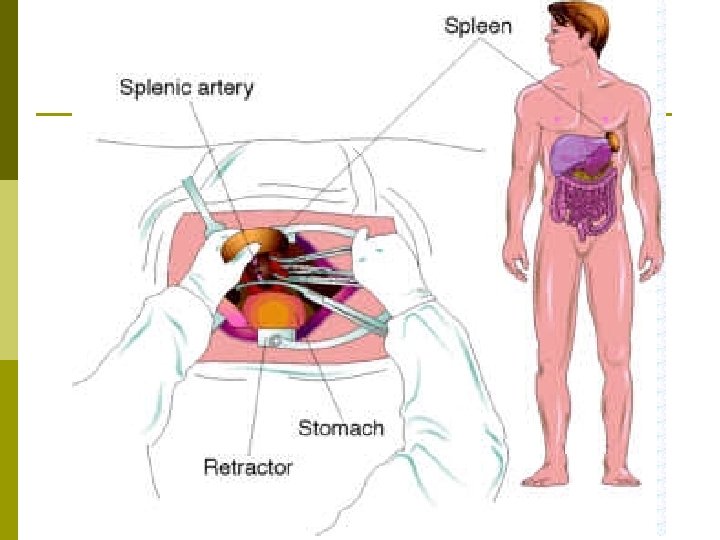
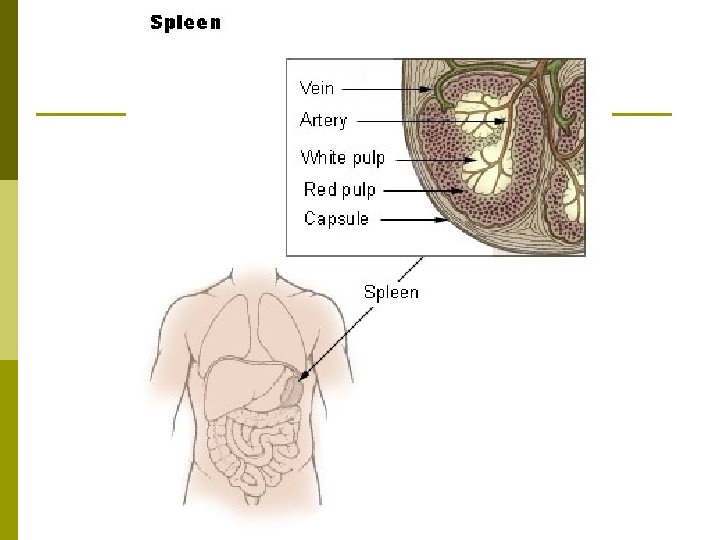
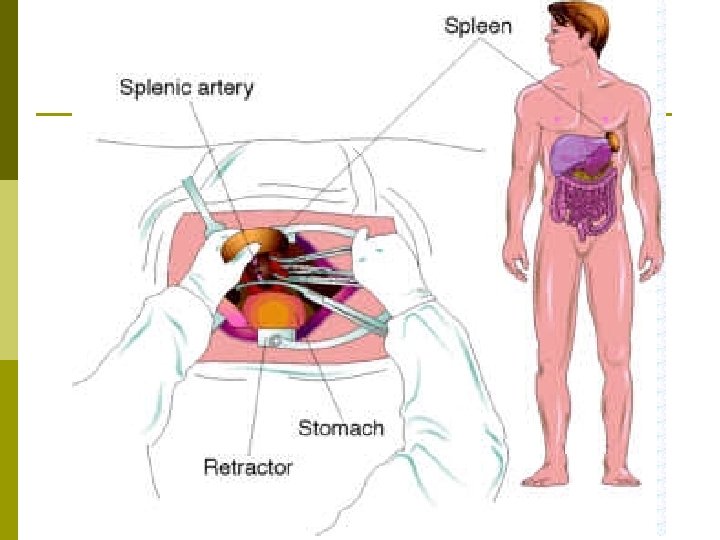
Spleen p Spleen: The largest mass of lymphatic tissue in the body, located in the hypochondriac region of the abdomen. n p Composed of a capsule & extending trabiculae. Two kinds of tissue in the spleen: n n White Pulp: Composed mostly of lymphocytes & macrophages. Red Pulp: Composed of blood-filled sinuses & Billroth’s cords or splenic cords (cords of splenic tissue).
Spleen p Primary functions of the Spleen: n n p Reservoir for blood Place for destroying old red blood cells Filter for the blood Creation of blood cells during fetal development Ruptured Spleen: A common physical injury that typically results in hemorrhage & can put the patient at risk for sepsis (blood infection).
Immune Response p Immune Responses: The defensive actions our body takes to respond to foreign invaders. n n Nonspecific or Innate Defenses: Defenses that are innate & not geared toward specific pathogens. A generic response! Immunity: The defense system where lymphocytes target & destroy specific pathogens. A learned response!
Immune Response p First Line of Defense: The first steps our body takes to defend against foreign invaders. n n Epidermis: Keratinized cells form many layers that very few pathogens can infiltrate. Mucous Membranes: Epithelial layers lining body cavities secrete mucus to trap microbes & contains protective chemicals.
Immune Response p p Mucous membranes in the nose have hairs that filter microbes from the air. Mucous membranes of the upper respiratory tract contain cilia to trap microbes & propel them back up the airway & out of the body. Lacrimal apparatus of the eye contains lysozyme which clears the eyes of pollutants & microbes. Saliva can wash microbes from the teeth & mouth.
Immune Response Sebum created by the sebaceous glands of the skin prevent the growth of some bacteria. p Stomach acid, lysozome enzymes in perspiration, and avid in the vagina deter pathogens. p Hyaluronic acid, found in connective tissue, inhibits the spred of pathogens in that tissue. p
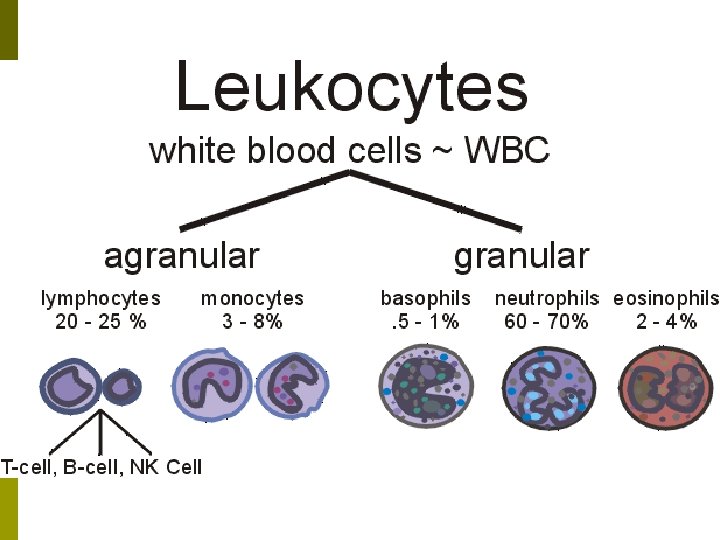
Immune Response p Second Line of Defense: The body’s internal defenses that take over if a pathogen gets through the first line of defense. n n n Leukocytes Macrophages Antimicrobial Proteins
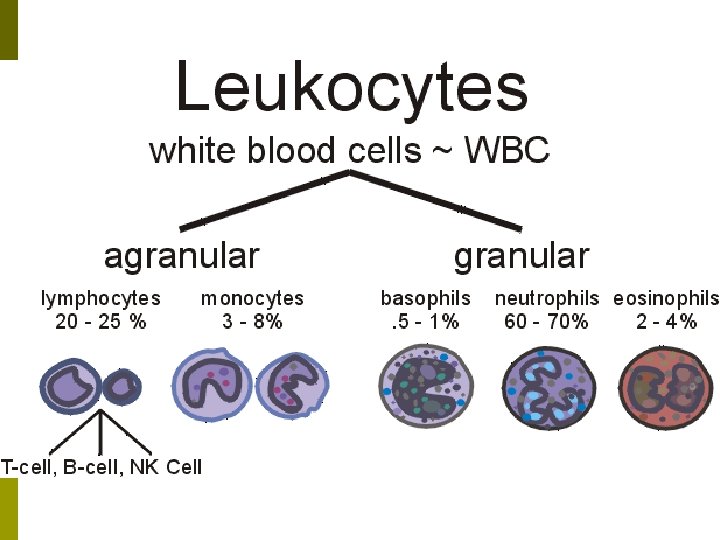
Immune Response p Leukocytes: 5 major categories. n n Neutrophils: Phagocytic cells that wander throughout the connective tissue destroying bacterias. Eosinophils: Phagocytic cells that destroy allergens, antigen & anti-body complexes, & some inflammatory chemicals. Surround larger parasites & attack them with enzymes to weaken or destroy them. p Defend against allergies & parasitic worm infections. p n Basophils: Helper cells that secrete vasodilators & anticoagulants in order to speed other leukocytes to the infected zone.
Immune Response n Lymphocytes: A variety of cells active in the immune response. p n Natural Killer Cells (NK Cells): Attack any cell with an unusual plasma membrane, such as cells that are infected by a virus or have become cancerous. § Cytolysis: Perforin protein is injected into the cell to cause it to “explode”. § Granzymes: Cause the cell to self-destruct. § Found in the spleen, red bone marrow, & lymph nodes. Monocytes: Wandering cells that eventually turn into macrophages.
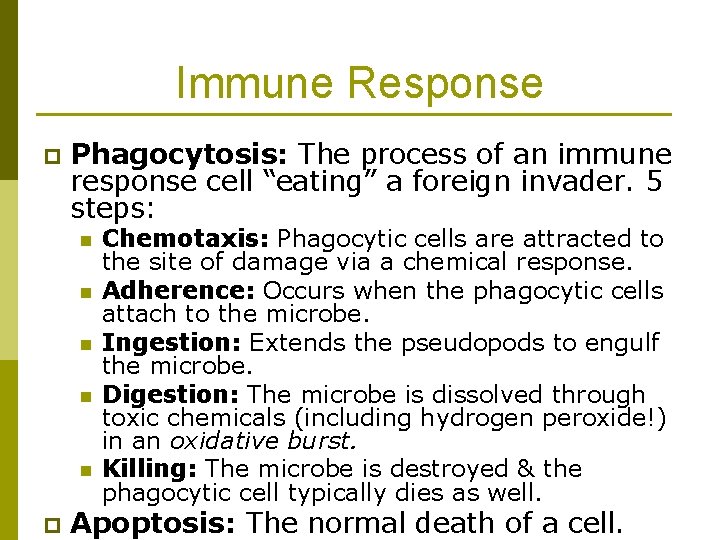
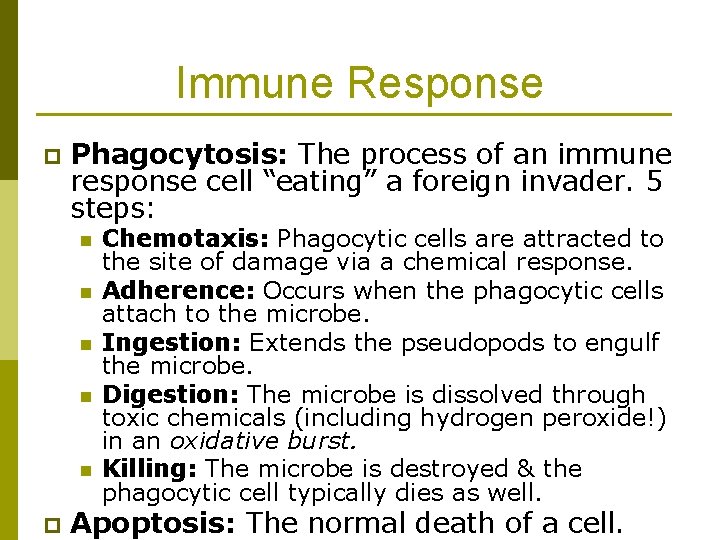
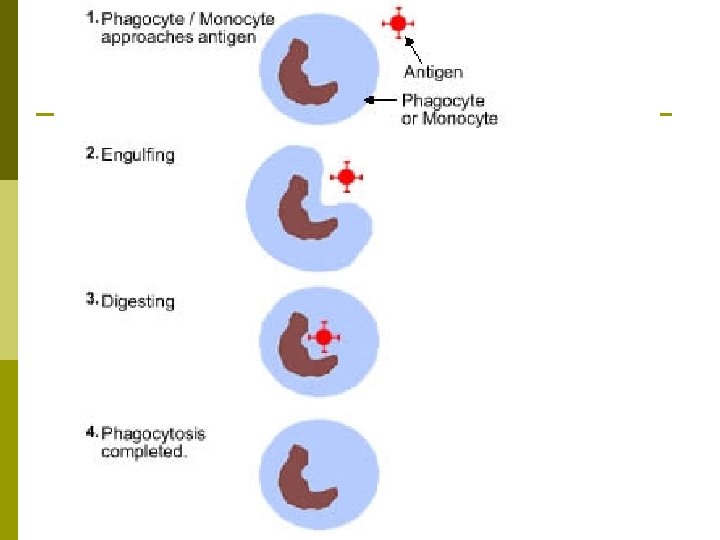
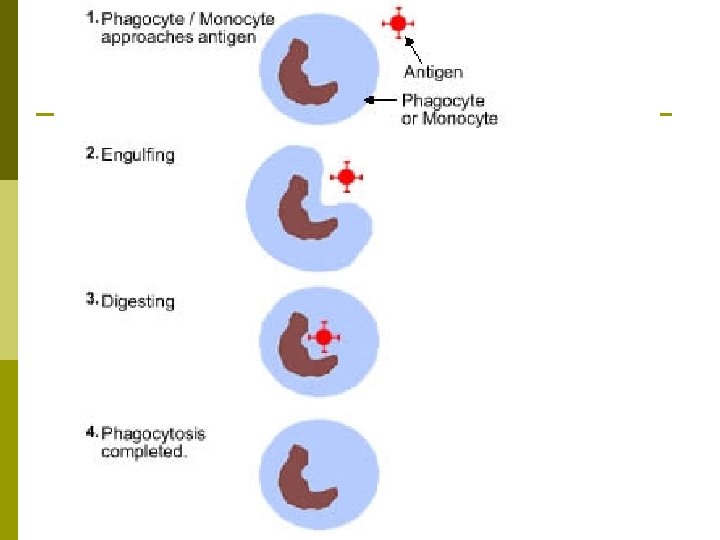
Immune Response p Phagocytosis: The process of an immune response cell “eating” a foreign invader. 5 steps: n n n p Chemotaxis: Phagocytic cells are attracted to the site of damage via a chemical response. Adherence: Occurs when the phagocytic cells attach to the microbe. Ingestion: Extends the pseudopods to engulf the microbe. Digestion: The microbe is dissolved through toxic chemicals (including hydrogen peroxide!) in an oxidative burst. Killing: The microbe is destroyed & the phagocytic cell typically dies as well. Apoptosis: The normal death of a cell.
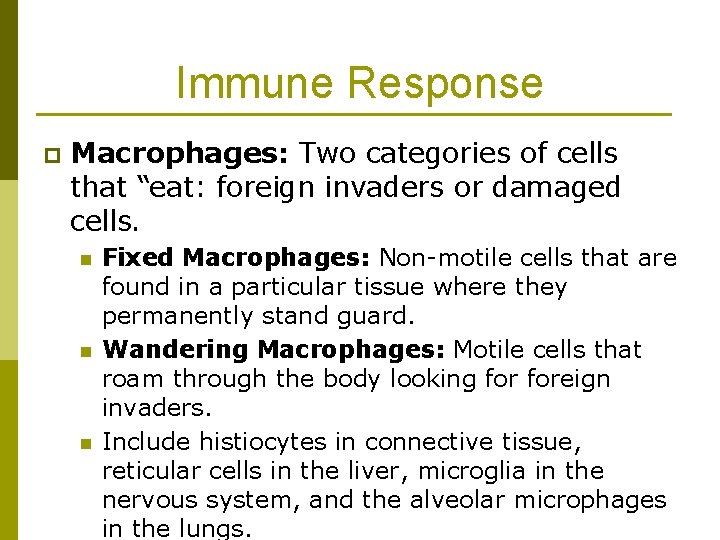
Immune Response p Macrophages: Two categories of cells that “eat: foreign invaders or damaged cells. n n n Fixed Macrophages: Non-motile cells that are found in a particular tissue where they permanently stand guard. Wandering Macrophages: Motile cells that roam through the body looking foreign invaders. Include histiocytes in connective tissue, reticular cells in the liver, microglia in the nervous system, and the alveolar microphages in the lungs.
Immune Response p Antimicrobial Proteins: Found in the blood and intestinal fluid to prevent infection. 3 types n Interferons (IFNs): Polypeptides secreted by cells that have been invaded by a virus. p p n n Travel to adjacent cells & stimulate the production of antiviral proteins. Activate natural killer cells & macrophages & aid in the destruction of cancerous cells. Transferrins: Can bind to & reduce the amount of iron available in bacteria, which can inhibit the spread of certain bacteria. Complement System: Group of twenty plus beta gobulins (proteins in the blood plasma) that enhance the immune, allergic, & inflammatory reactions. p Optimization: Where the complement system chemically coats the surface of bacteria which in tern makes them
Inflammation: One of the body’s most common responses to tissue damage. Occurs in roughly the same way in any tissue. p Four Cardinal signs of Inflammation: p n n Redness Swelling Heat Pain

Inflammation p 3 Stages of Inflammation: n Vasodilation of Blood Vessels: Increases blood flow & increases the permeability of capillaries. Prompted by histamines & kinins. p Capillary dilation is the cause of redness. p n Emigration (Movement) of Phagocytes: Phagocytes move to effected areas to remove dead cells & toxins. Basophils secrete leukotrienes to increase this reaction. p Leukocytosis: The sudden increase of white blood cells migrating to the area. p n Repair of Damaged Tissues: The tissues repaire itself. p Platelet Derived Growth Factor (PDGF): Prompts fibroblasts to multiply faster & speed up tissue repair.

Fever p Fever: An increase in body temperature often due to the interaction of bacteria & macrophages. n Interleukin-1: Released by macrophages, which triggers prostaglandin E to be secreted by the hypothalamus, which increases the body’s internal thermostat. Positive Effects: Promotes interferon activity, speeds up metabolism & other processes that aid in repair, slows down the growth of some bacteria & viruses. p Negative Effects: Cellular dysfunction & brain damage possible if the fever gets too high. p

Immune System: A combination of cells designed to recognize specific foreign substances & neutralize or destroy them. p Specific Immune Defenses: The cells are specifically geared toward fighting certain invaders, and remembers previous foreign invaders so that they can be rapidly eliminated in the future. p
Immune System p Two Divisions of the Immune System: n n Humoral Immunity aka Antibody-Mediated Immunity: Involves antibodies which bind to foreign substances like toxins & bacteria to “tag” or mark them for destruction. Driven by T cells & B cells. Cellular Immunity: Cell-mediated immunity which includes the actions of lymphocytes that attack foreign cells or cells infected with cancer, viruses, or parasites. Driven by T cells.
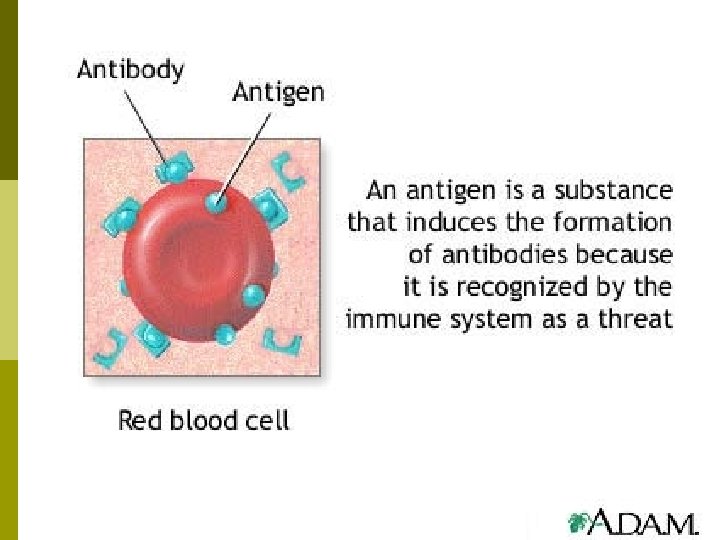
Antigens p Antigen (Ag): Any substance recognized as foreign to the body & triggering an immune response. n p Typically large molecules, often proteins. Two defining characteristics: n n Immunogenicity: Stimulate the immune system to produce specific antibodies. Reactivity: An antigen will react with the appropriate antibody once it is produced.
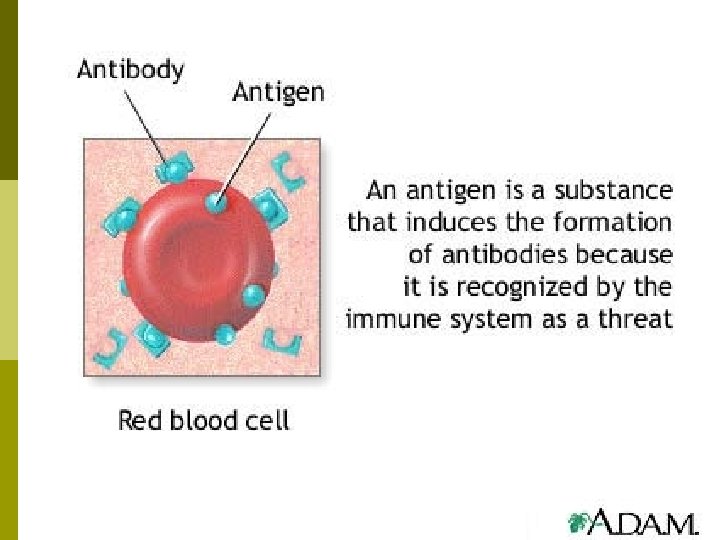
Antigens p Epitope: The part of a molecule that initiates an immune response. n n n The antigen could be an entire microbe. Typically it is just a portion of the microbe or a specific chemical or toxin component. Antigens can include blood cells of a different type, pollen, egg whites, etc.
Antigens p Haptens: Smaller substances that can cause reactivity, but not full immunogenicity. n n Stimulate an immune response only if attached to a larger carrier molecule. Example: Toxin in poison ivy, which only triggers a response when bound to particular proteins in the body.
Antigen Processing p Antigen Processing: The means by which the body recognizes that a foreign antigen is present. n Differs depending on whether the antigen is inside or outside the body cell, which determines if the body engages in cellular or humoral immunity responses.
Antigen Processing p Major Histocompatability Complex (MHC): “Self-antigens” that are unique to all of your body cells except red blood cells. n n Help T-cells recognize which cells are foreign. MHC-1 s: Cells that posses MHC and are labeled “you” by the T-cells.
Antigen Processing p Two types of antigens: n Exogenous Antigens: Those found outside of the body cells that include bacteria, parasitic worms, pollens & viruses that have not yet infected body cells. p n Antigen-Presenting Cells (APCs): Macrophages & B-cells that phagocytize the antigen, then display the resulting peptide fragments on the plasma membrane to trigger T-cells (called MCH-2’s). Endogenous Antigens: Those found inside the body cells and are either viral proteins produced by a virus-infected cell or a cancerous cell. p Most cells with endogenous antigens process them & display them on their cell membranes to signal the immune system for help.
Cellular Immunity p Cellular Immunity: Lymphocytes directly attack & destroy foreign cells & infected host cells. n n n Begins with activation of T-Cells or Tlymphocytes by a specific antigen. Millions of T-cells, each with its own T-cell receptor to recognize a specific antigen. Roughly 75% of the lymphocytes in the body.
Cellular Immunity p Types of T-Cells involved in Cell-mediated Response: n n Cytotoxic T-Cells: Responsible for actual attacking of the foreign body or infected cell. Helper T-Cells: Stimulate other helper T-cells, cytotoxic T-cells, and B cells. Suppressor T-Cells: Help regulate the attack & prevent tissue destruction. Memory T-Cells: Remain as an immune response and stimulate faster responses if the same antigen invades again.
Cellular Immunity p Three stages of the Cell Mediated Response: n n n Recognition Attack Memory
Cellular Immunity – Recognition p Recognition: Helper and cytotoxic T-cells patrol the body, examining the MHC of other cells. T-cell receptors recognize & bind to the antigen – the first signal. p Costimulation: The need for a second signal of cytokines (Interleukin-2) provided by the helper Tcells. p Cloning: Activated T-Cell then proliferates & differentiates to create a population of clones. p
Cellular Immunity – Attack p Attack: Helper t-cells secrete lymphokines to prompt inflammation & attract neutrophils.
Cellular Immunity – Attack n Cytotoxic T-cells actually attach to the foreign or diseased cell to destroy it. p p Apoptosis: Cytotoxic t-cells bind to the target cell & digest it – granzymes digest the protein of the cell & cause it to break apart. Released microbes are then phagocytized. Cytolysis: Cytotoxic T-cells bind to the infected cell, release perforin to create holes in the plasma membrane, which causes the cell to burst. Granulysis released by the t-cells destroy the microbes. Lymphotoxin: Toxic molecules released by the T-cells which cause the DNA of target cells to fragment, destroying the cell. Suppressor T-cells release lymphokines to inhibit T & B cell activity & prevent damage to healthy tissue.
Cellular Immunity – Memory p Memory: After the first exposure & resulting response, some T-cells become memory cells and “memorize” the foreign invader. n T-Cell Recall Response: The second exposure to the same antigen triggers a faster & more effective response thanks to the memory T-cells.
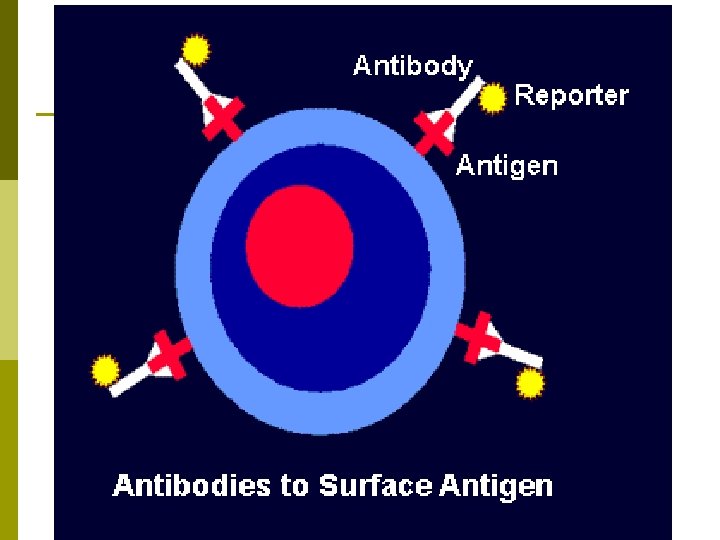
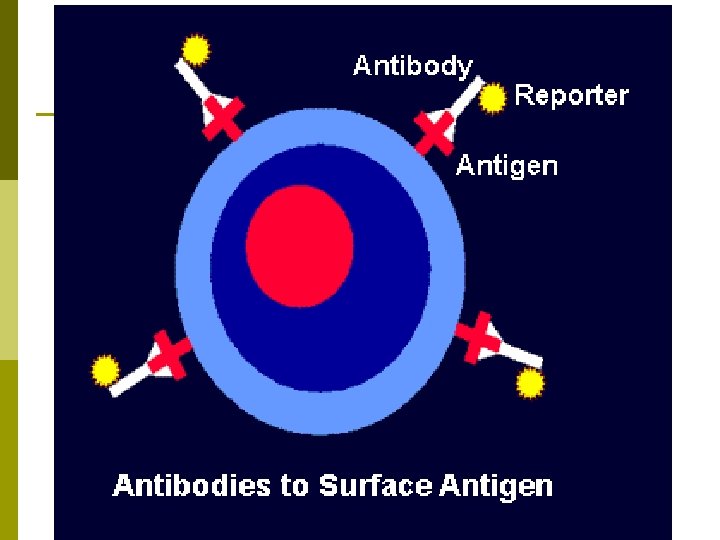
Humoral Immunity aka Antibody. Mediated Immunity: Depends on B cells (B-lymphocytes) to produce antibodies (Ab) to engage in a complex purging process. p Immunoglobulins (Igs): Antibodies made up of glycoproteins called globulins. p n n Two heavy (H) chains & two light (L) chains of polypeptides. Antigen-Binding Site: Tips of each chain are called variable (V) regions & areas where the antibody attaches to the antigen.
Humoral Immunity p 5 classes of antibodies: n n Ig. G: Protect against viruses & bacteria - 80% of antibodies. The only class that can cross the placenta to react the fetus & provide immunity. Ig. A (Secretory antibody): Found in sweat, saliva, mucous, tears, breast milk, & the GI secretions to provide local protection against viruses & bacteria – 15% of antibodies. p n n n Known to decrease in times of stress, which lowers the body’s resistance. Ig. M: Found in the blood & lymph 0 cause agglutination & lysis of microbes, serves as an antigen receptor on the surface of B cells – 5% of antibodies. Ig. D: Acts as an antigen receptor for and activates B cells – 0. 2% of antibodies. Ig. E: Protects against allergies & parasitic worms, located on most cells & basophils – less than 1% of antibodies.
Humoral Immunity p Complement System: Plasma proteins produced by the liver that help destroy microbes through cytolysis – activated by the antigen-antibody complexes. Effects: n n n Activation of Inflammation: Some Complement proteins activate blood flow & histamines, some combat infection & allergies, some chemotactic agents to attract phagocytes. Opsonization: Makes microbes more susceptible to phagocytosis by C 3 b binding to the surface of the microbe & then reacting with receptors on the phagocytes. Cytolysis: Complement proteins combine to form membrane attack complex (MAC) that forms large holes in the microbe’s plasma membrane, resulting in the microbe to uptake fluid too fast and lysing (bursting).
Humoral Immunity p Humoral Immunity Follows 3 General Steps: n n n Recognition Attack Memory
Humoral Immunity – Recognition p Recognition: B-cells bind to antigen & engage in endocytosis of the antigen B-cell receptor complex. Antigen is digested & broken into gragments. p Fragments are displayed on the B-cell membrane, which causes t-cell activation. p Helper factors cause B-cells to begin dividing & differentiating, creating plasma cell clones, which produce & release antibodies. p
Humoral Immunity – Attack p Attack: Antibodies neutralize antigens, immobilize bacteria, activate complement, enhance phagocytosis of other cells, and causes agglutination & precipitation of antigens. p Causes antigens to cluster together and allows them to be phagocytized easier.
Humoral Immunity – Memory p Memory: After the primary immunity response several cloned cells become memory cells that remain for future attacks. n Anamnestic Response: A secondary response within the humoral immunity to a second invasion of the same invader. Typically much faster, more powerful, & more effective.
Humoral Immunity – Memory n Antigen Titer: Measure of memory based on the amount of antigen serum present. p p Primary Response: Antigen titer should be zero for the first several days, but will slowly rise through Ig. M first then Ig. G followed by a gradual decline as the pathogen dies off. Secondary Response: Antigen titer consists of mainly Ig. G antibodies during the primary response, and is more intense.
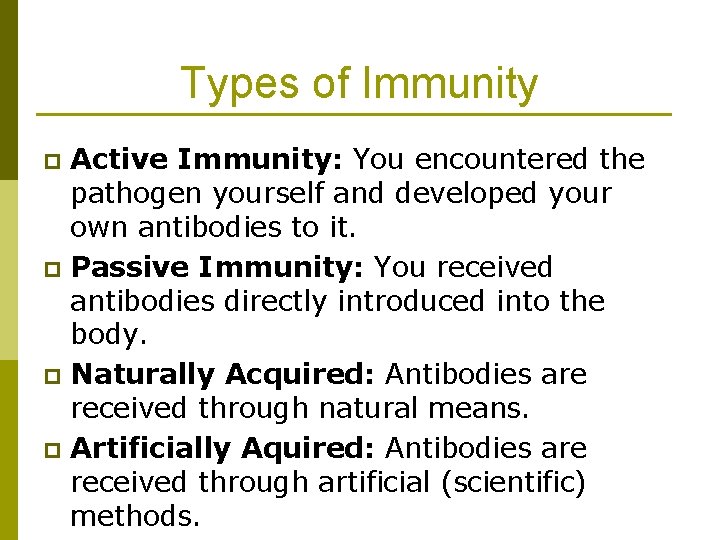
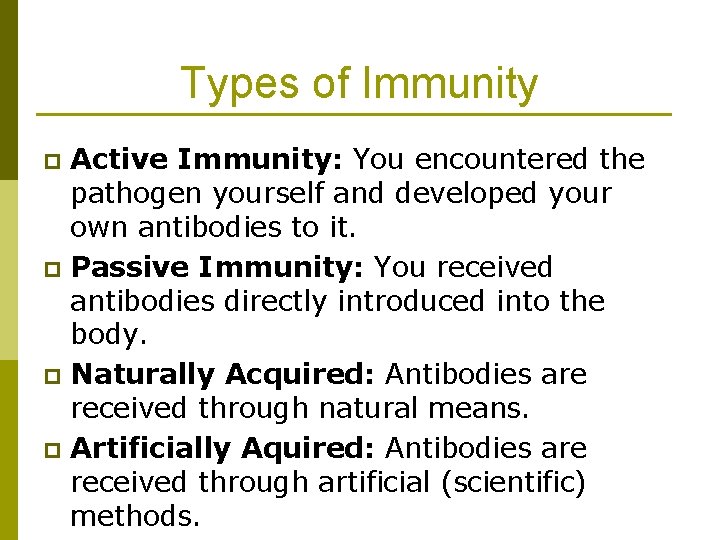
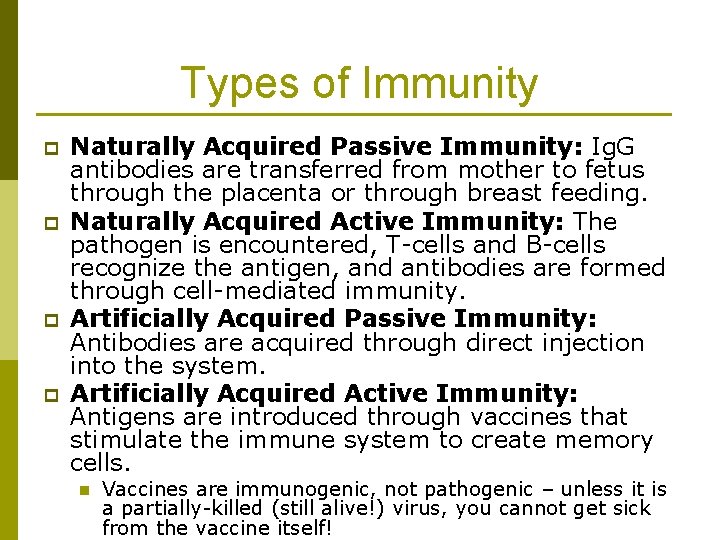
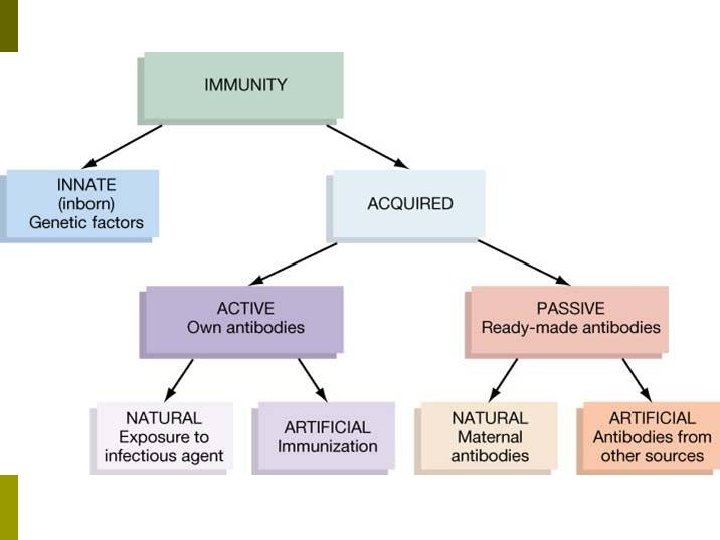
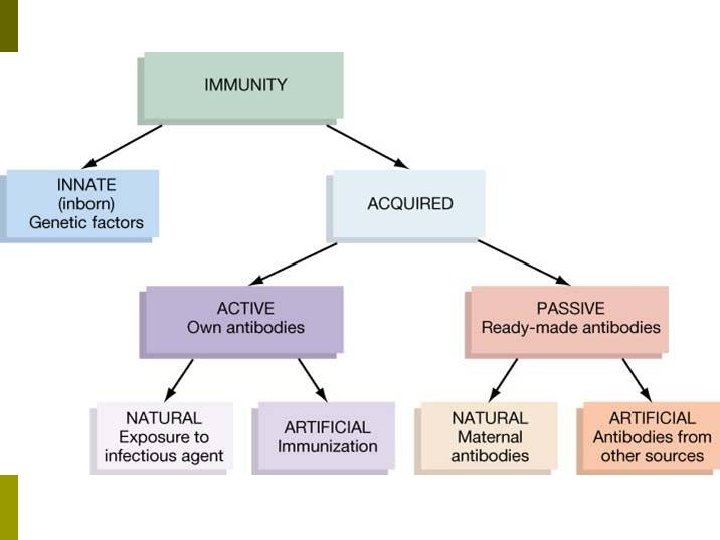
Types of Immunity Active Immunity: You encountered the pathogen yourself and developed your own antibodies to it. p Passive Immunity: You received antibodies directly introduced into the body. p Naturally Acquired: Antibodies are received through natural means. p Artificially Aquired: Antibodies are received through artificial (scientific) methods. p
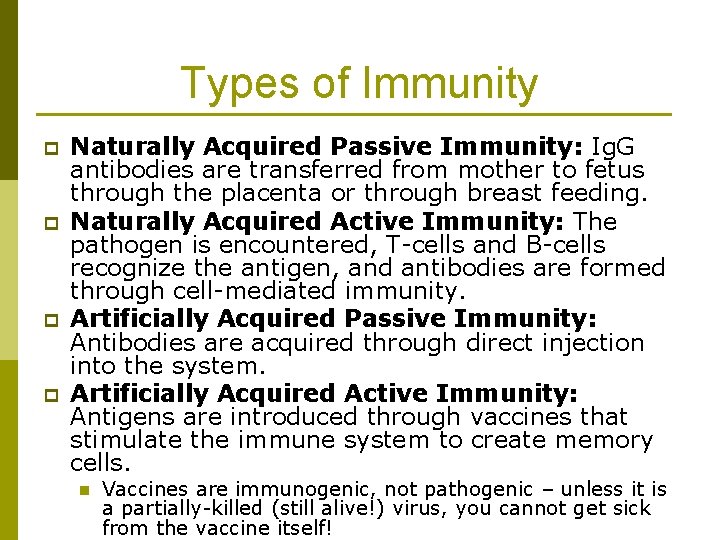
Types of Immunity p p Naturally Acquired Passive Immunity: Ig. G antibodies are transferred from mother to fetus through the placenta or through breast feeding. Naturally Acquired Active Immunity: The pathogen is encountered, T-cells and B-cells recognize the antigen, and antibodies are formed through cell-mediated immunity. Artificially Acquired Passive Immunity: Antibodies are acquired through direct injection into the system. Artificially Acquired Active Immunity: Antigens are introduced through vaccines that stimulate the immune system to create memory cells. n Vaccines are immunogenic, not pathogenic – unless it is a partially-killed (still alive!) virus, you cannot get sick from the vaccine itself!
Immune System Disorders p Hypersensitivity: When the immune system reacts to a substance that is normally not reacted to. n Allergens: The substance being reacted to.
Immune System Disorders p 4 Types of Hypersensitivity: n Type 1: Acute or Anaphylactic Reactions: The most common reaction – caused by mast cells and basophiles reacting to allergens. Common Symptoms: Inflammation, edema, mucus production, congestion, cramps, vometing, diarrhea. p Can cause… airway constrictions, weakened contractions of the heart muscles. p Treatment: Epinephrine injections, Benadryl, respiratory support. p Common Causes: Bee stings, latex, antibiotics, certain chemicals, etc. p
Immune System Disorders n Type 2: Cytotoxic Reactions: caused by antibodies attacking a person’s own blood or tissue cells. Symptoms: Destruction of the cells via cytolysis. p Common cause: Incompatible blood transfusions. p
Immune System Disorders n Type 3: Immunne-Complex Reactions: Caused when immune complexes avoid phagocytosis & become trapped in the endothelium of blood vessels. Symptoms: Inglammation. p Common Example: Rheumatoid Arthritis p
Immune System Disorders n Type 4: Delayed Hypersensitive Reaction: Occur when the antigen presenting cells travel from lymph node to lymph node & display the allergen to helper T cells, which then migrate to the site of allergen entry to cause inflammation. Symptoms: Inflammation & rashes p Common Cause: Poison ivy, poison oak, Tuberculosis titer test. p
Immune System Disorders p Autoimmune Disease: Marked by failure of the immune system to properly distinguish the body’s own cells from foreign antigens. n n Results: Immune system produces antibodies that attack antigens & the body’s own tissues. 5% of adults in the US have autoimmune disease.
Immune System Disorders p T-cells: Must have TWO traits to function properly…. n n Self-Recognition: The ability to recognize the body’s own major histocompatability complex (MHC) proteins – you must recognize your own cells! Self-Tollerance: Lack of reactivity to peptide fragments from your own proteins – don’t attack your own cells!
Immune System Disorders p Severe Combined Immunodeficiency Disease (SCID): Congenital disorder where B & T cells are deficient. n n Leaves children highly susceptible to infections so they must live in protective enclosures. Can be cured via red bone marrow cells with very similar MCH antigens. p n n Can provide normal stem cells to give rise to normal B & T cells. Can also be treated with gene therapy of good copies of the defective cells with treatments every few months for life. Fortunately VERY rare!
Immune System Disorders p Acquired Immune Deficiency Syndrome (AIDS): Immunodificiency disease caused by the Human Immunodeficiency Virus (HIV). n n p p HIV is a retrovirus that carries genetic information on its RNA instead of DN. Infects cells, replicates via RNA, & causes the infected cell to reproduce viral cells through cell division. Primarily targets helper T-cells. Transmitted through exchange of blood & some bodily fluids. HIV & AIDS are typically the cause of immune compromization that leads to death from opportunistic infections. HIV has reached epidemic proportions & has claimed over 20, 000 lives so far.