Lymphatic and immune system Lymphatic System Lymphatic vessels

- Slides: 32
Lymphatic and immune system
Lymphatic System
Lymphatic vessels The lymphatic vessels form a one-way system in which lymph flows only toward the heart Starts in the lymph capillaries(between tissue cells and blood capillaries) in loose connective tissue Lymph capillaries flow into lymphatic connecting vessels and then to the lymphatic ducts Lymphatic trunks drain large areas of the body and empty lymph back to the circulatory system via the thoracic duct or the right lymphatic duct Lymphatic vessels are low-pressure vessels, much like veins Lymph is a colorless fluid containing white blood cells, that bathes the tissues and drains through the lymphatic system into the bloodstream.
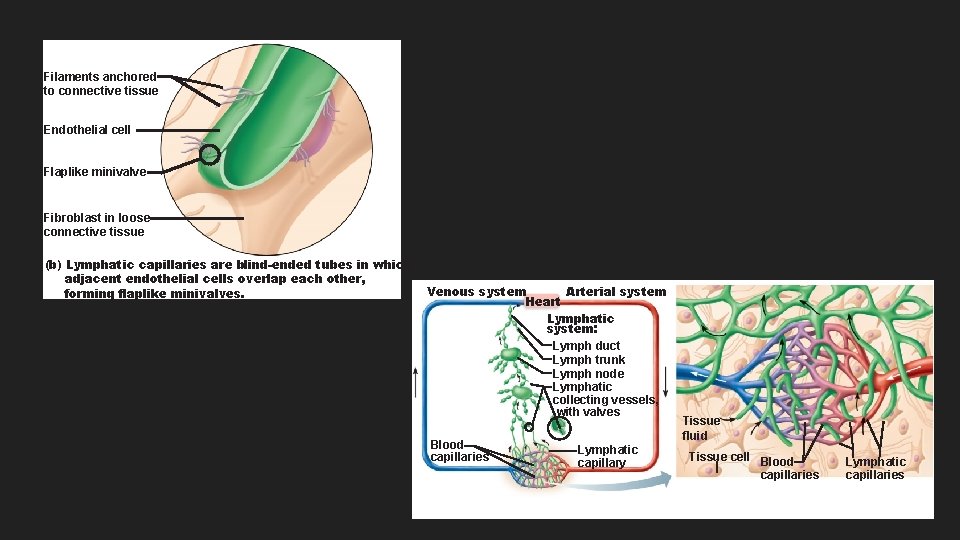
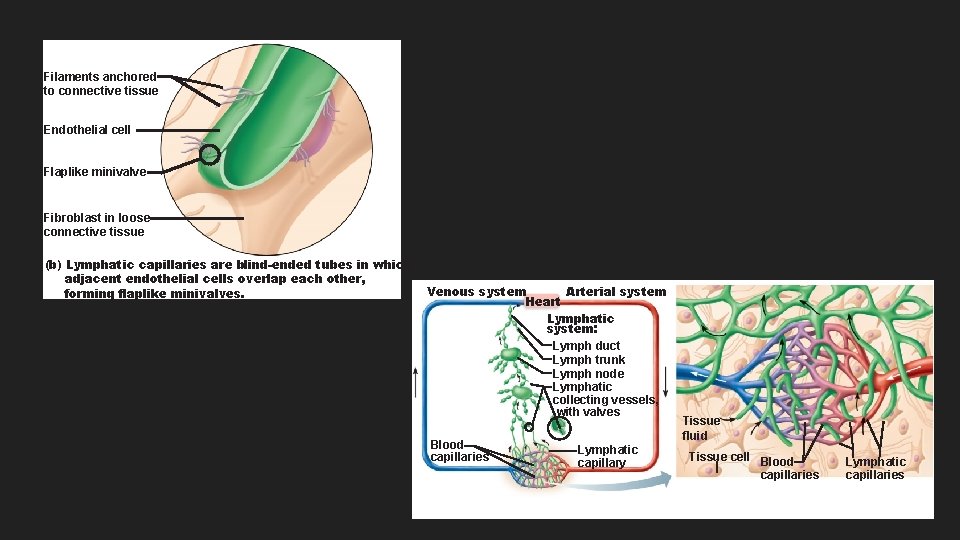
Filaments anchored to connective tissue Endothelial cell Flaplike minivalve Fibroblast in loose connective tissue (b) Lymphatic capillaries are blind-ended tubes in which adjacent endothelial cells overlap each other, forming flaplike minivalves. Venous system Arterial system Heart Lymphatic system: Lymph duct Lymph trunk Lymph node Lymphatic collecting vessels, with valves Blood capillaries Lymphatic capillary Tissue fluid Tissue cell Blood capillaries Lymphatic capillaries
Lymphoid Cells and tissue Lymphatic cells Lymphocytes- made in red marrow and mature into T lymphocytes and B lymphocytes Macrophages- activate T lymphocytes Dendritic cells- active T lymphocytes Reticular cells- produce stroma Lymphatic tissue house and proliferate lymphocytes
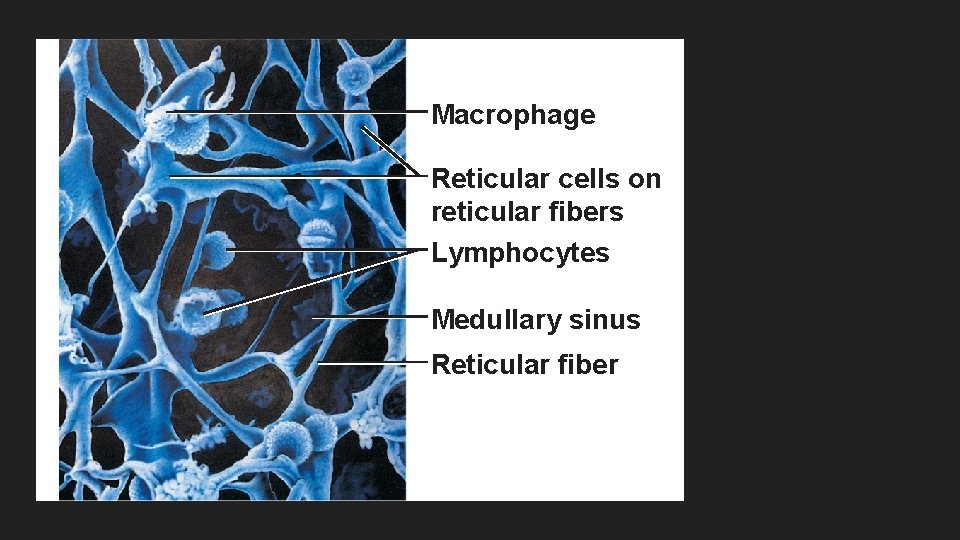
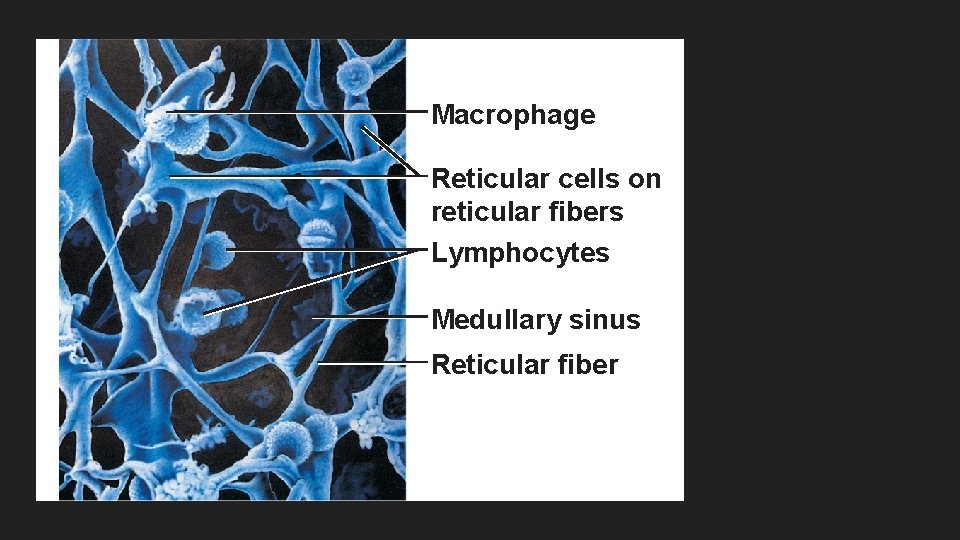
Macrophage Reticular cells on reticular fibers Lymphocytes Medullary sinus Reticular fiber
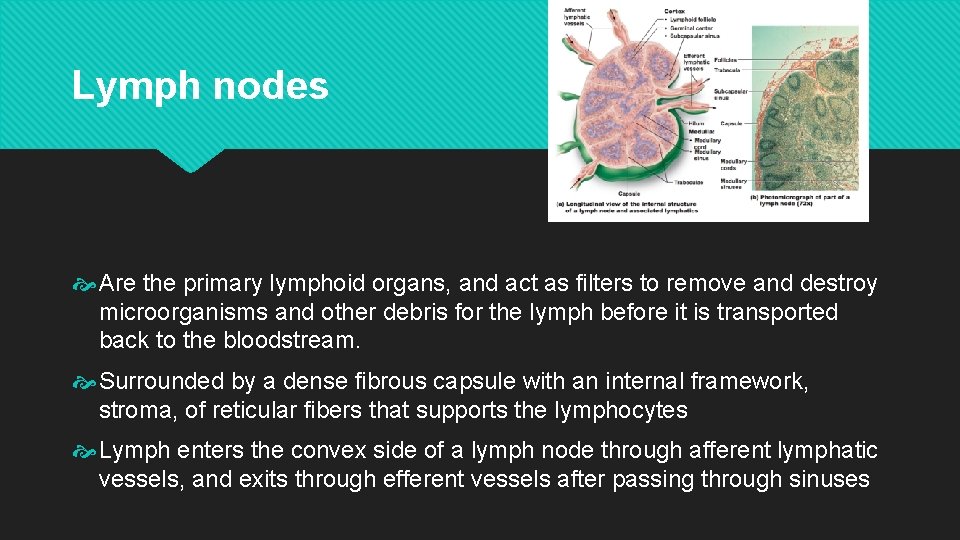
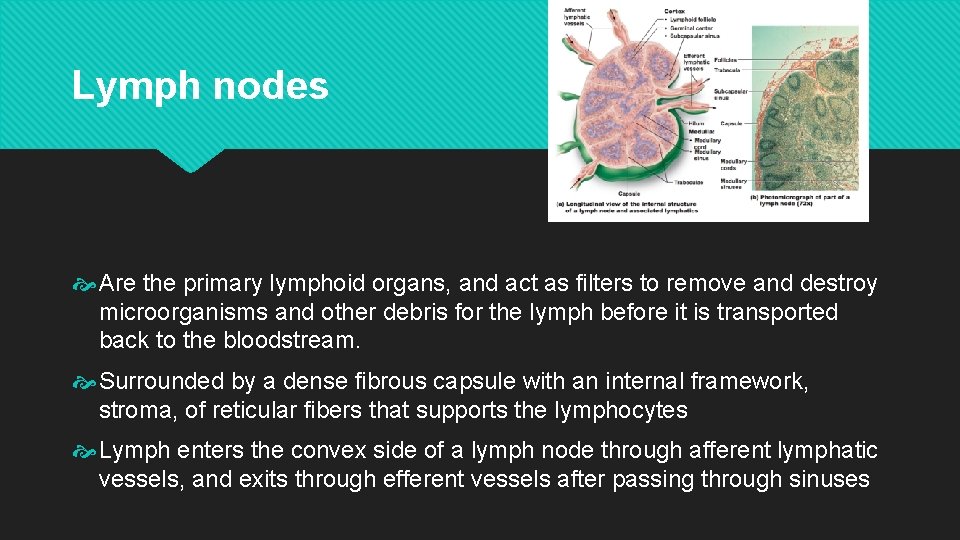
Lymph nodes Are the primary lymphoid organs, and act as filters to remove and destroy microorganisms and other debris for the lymph before it is transported back to the bloodstream. Surrounded by a dense fibrous capsule with an internal framework, stroma, of reticular fibers that supports the lymphocytes Lymph enters the convex side of a lymph node through afferent lymphatic vessels, and exits through efferent vessels after passing through sinuses
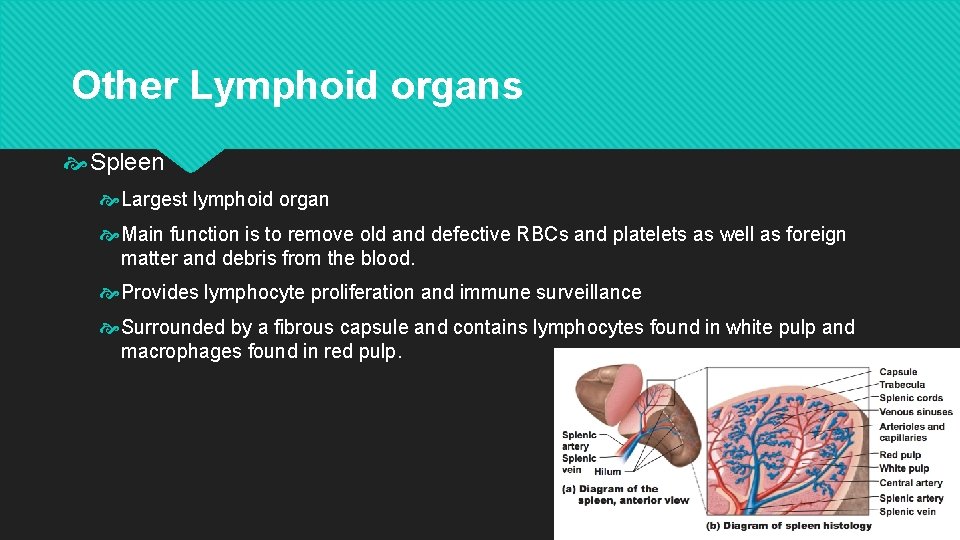
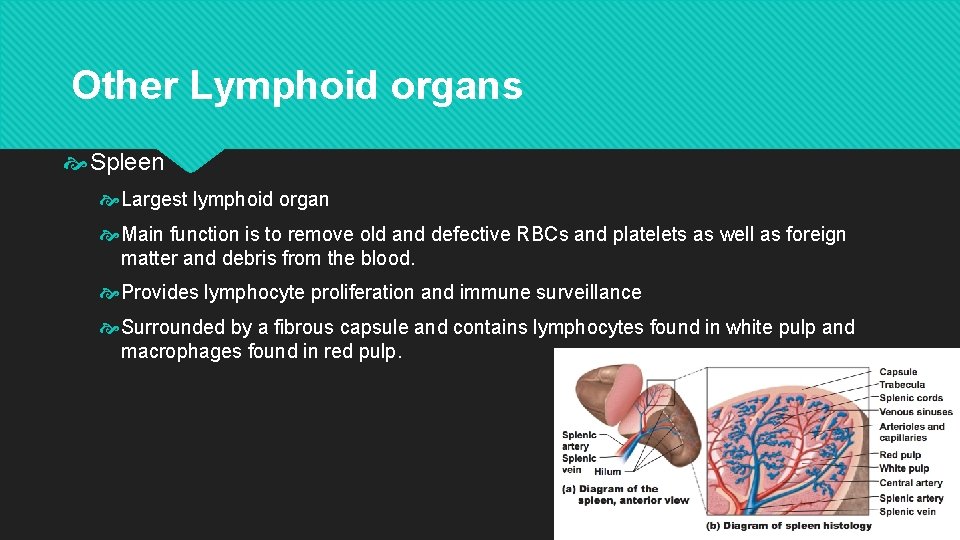
Other Lymphoid organs Spleen Largest lymphoid organ Main function is to remove old and defective RBCs and platelets as well as foreign matter and debris from the blood. Provides lymphocyte proliferation and immune surveillance Surrounded by a fibrous capsule and contains lymphocytes found in white pulp and macrophages found in red pulp.
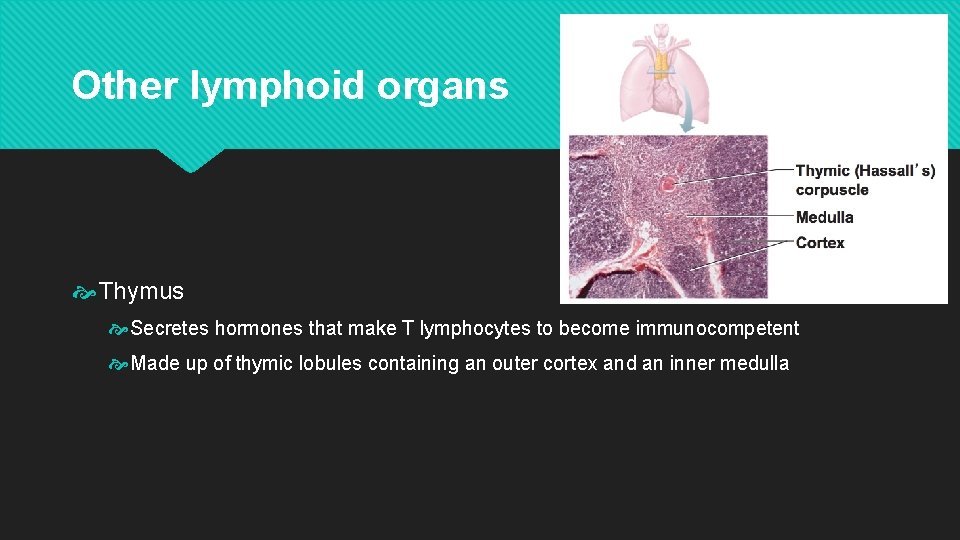
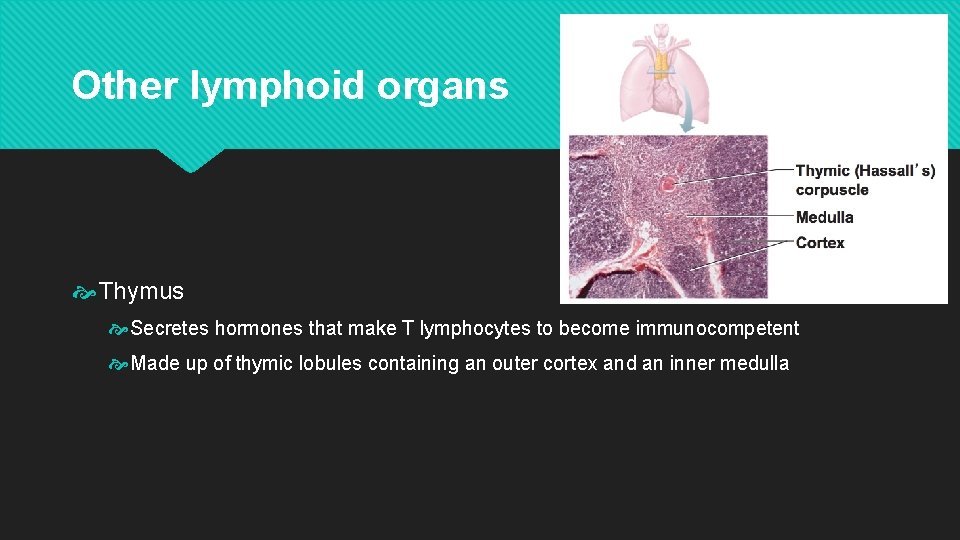
Other lymphoid organs Thymus Secretes hormones that make T lymphocytes to become immunocompetent Made up of thymic lobules containing an outer cortex and an inner medulla
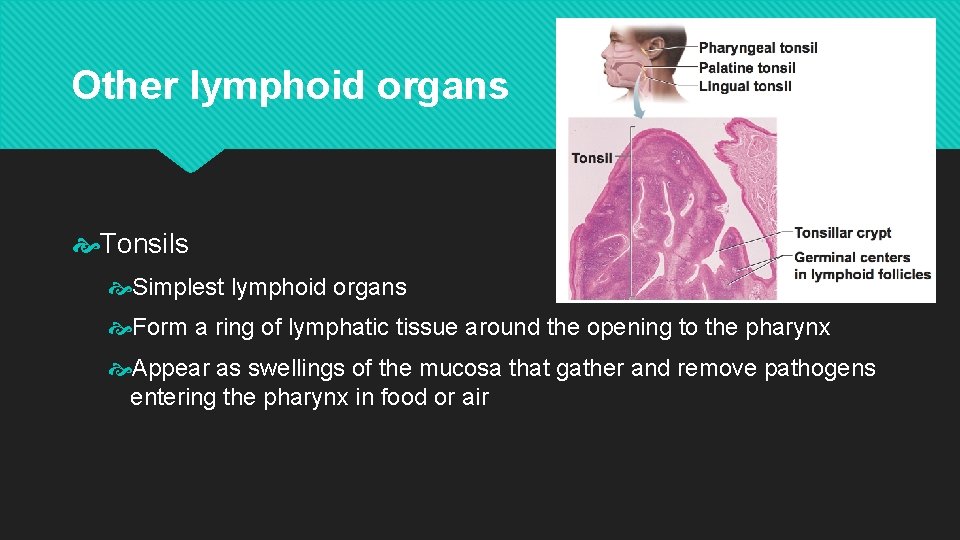
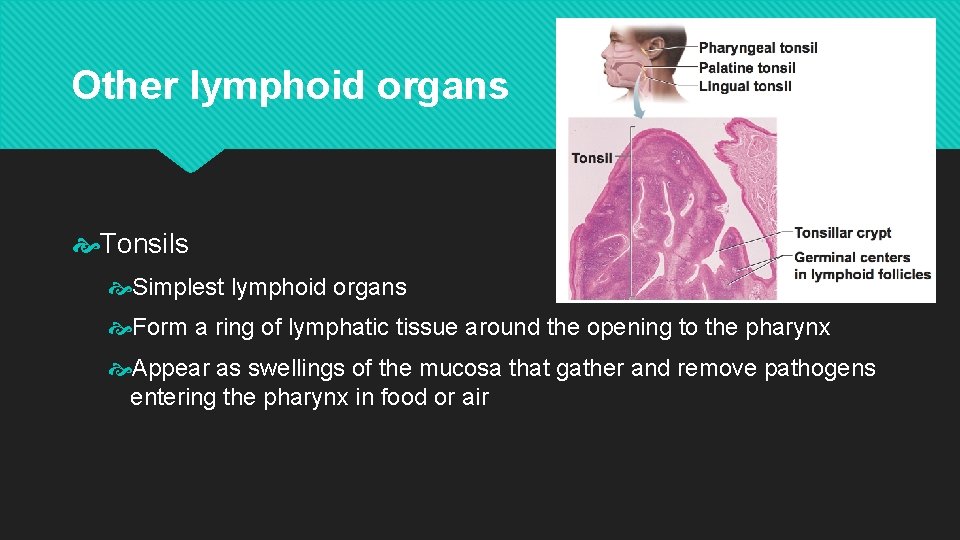
Other lymphoid organs Tonsils Simplest lymphoid organs Form a ring of lymphatic tissue around the opening to the pharynx Appear as swellings of the mucosa that gather and remove pathogens entering the pharynx in food or air
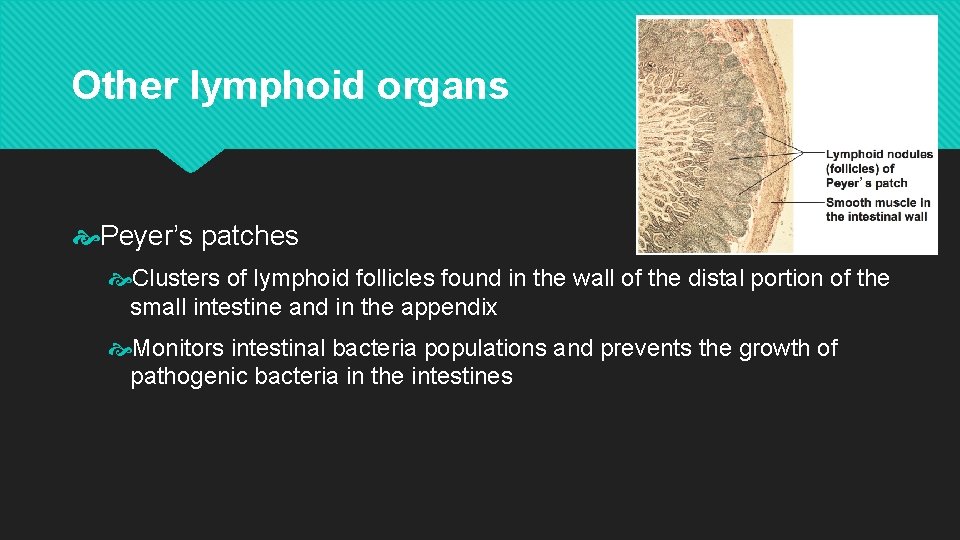
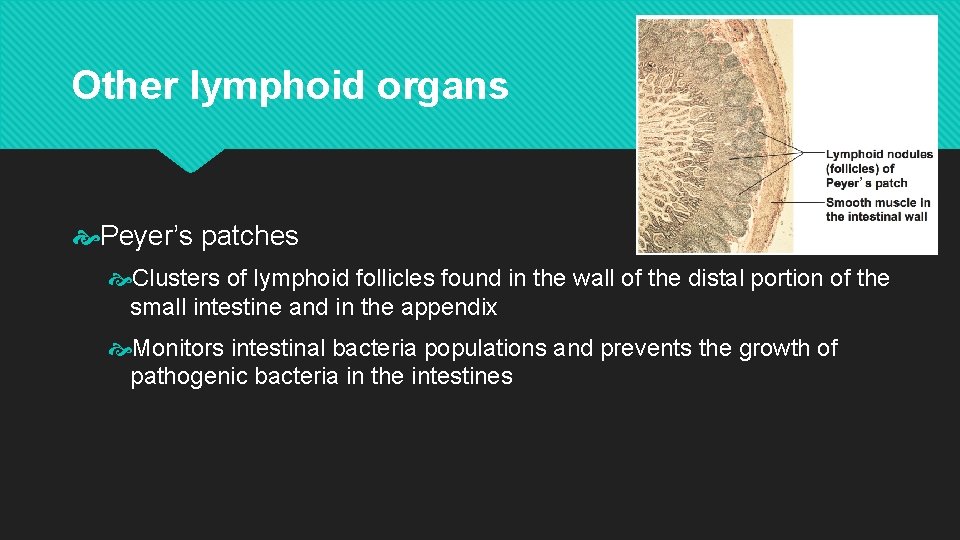
Other lymphoid organs Peyer’s patches Clusters of lymphoid follicles found in the wall of the distal portion of the small intestine and in the appendix Monitors intestinal bacteria populations and prevents the growth of pathogenic bacteria in the intestines

Immune System
Innate Defenses Surface Barriers Skin - physical barrier to most microorganisms and their enzymes and toxins. Mucous membranes - line all body cavities open to the exterior and function as an additional physical barrier. Secretions of the epithelial tissues - acidic secretions, sebum, hydrochloric acid, saliva, and mucus.
Internal Defenses Phagocytes confront microorganisms that breach the external barriers Macrophages - main phagocytes of the body Neutrophils - first responders and become phagocytic when they encounter infectious material Eosinophils - weakly phagocytic but defend the body against parasitic worms. Mast cells - ability to bind with, ingest, and kill a wide range of bacteria. Natural killer cells - lyse and kill cancer cells and virally infected cells before the adaptive immune system has been activated.
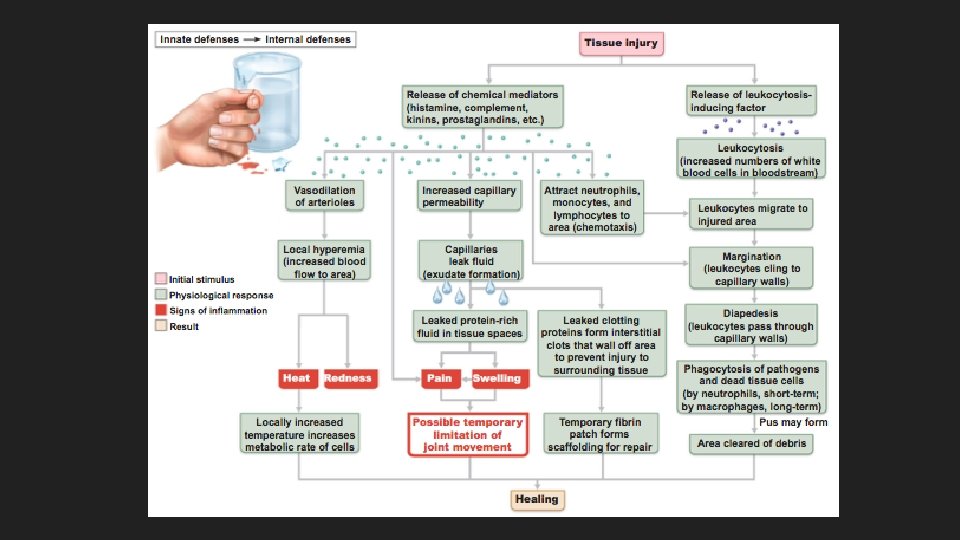
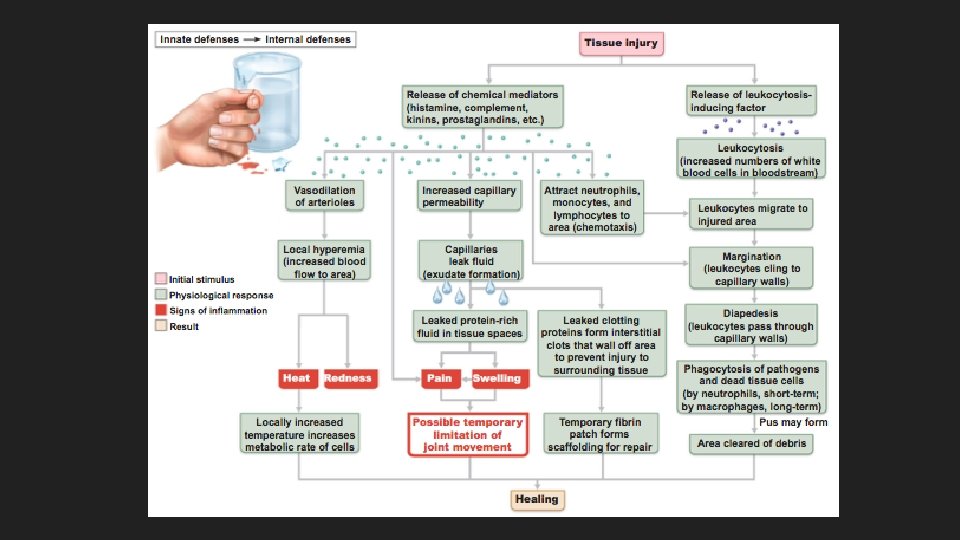
Internal Defenses Inflammation occurs any time the body tissues are injured by physical trauma, intense heat, irritating chemicals, or infection by viruses, fungi, or bacteria. Signs of inflammation - redness, heat, swelling, and pain. Chemicals cause dilation of blood vessels to increase blood flow to the area to increase permeability Soon after inflammation the damaged site is invaded by neutrophils and macrophages.
Internal Defenses Antimicrobial proteins enhance the innate defenses by attacking microorganisms directly or by hindering their ability to reproduce. Interferons - small proteins produced by virally infected cells that help protect surrounding healthy cells. Complement - group of 20 plasma proteins that provide a major mechanism for destroying foreign pathogens in the body. Fever, or an abnormally high body temperature, is a systemic response to microorganisms.
Adaptive Defenses The adaptive defenses recognize and destroy the specific antigen that initiated the response Systemic response not limited to the initial infection site After an initial exposure the immune response is able to recognize the same antigen and mount a faster and stronger defensive attack. Humoral immunity is provided by antibodies produced by B lymphocytes present in bodily fluids. Cellular immunity is associated with T lymphocytes and has living cells as its protective factor.
Antigens are substances that can mobilize the immune system and provoke an immune response Complete antigens are able to stimulate the proliferation of specific lymphocytes and antibodies, and to react with the activated lymphocytes and produced antibodies. Haptens are incomplete antigens that are not capable of stimulating the immune response, but interact with proteins of the body to recognize as potentially harmful. Antigenic determinants are parts of antigens that bind to free antibodies or activated lymphocytes
Adaptive Defensive Cells Lymphocytes originate in the bone marrow and when released become immunocompetent in either the Thymus (T cells) or the Bone marrow (B cells). Antigen-presenting cells engulf antigens and present fragments of these antigens on their surfaces where they can be recognized.
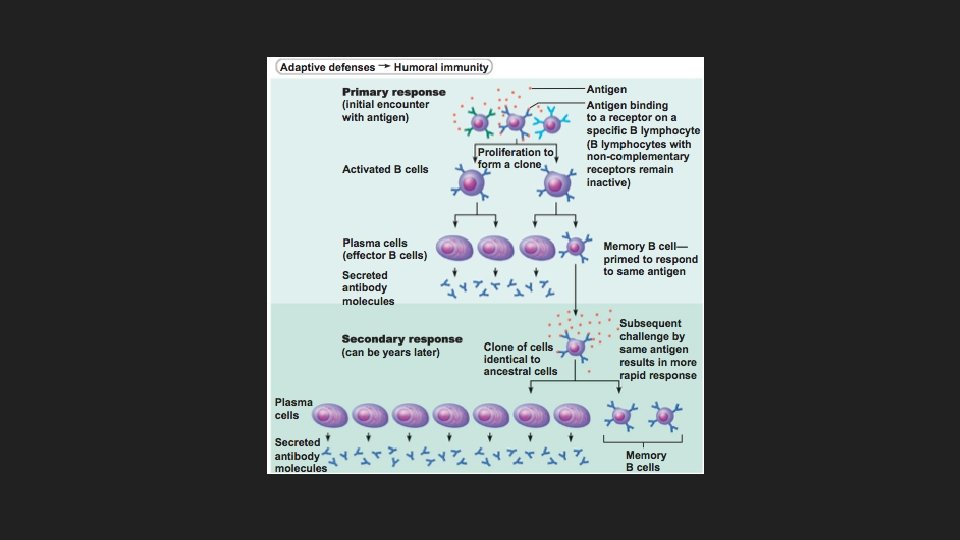
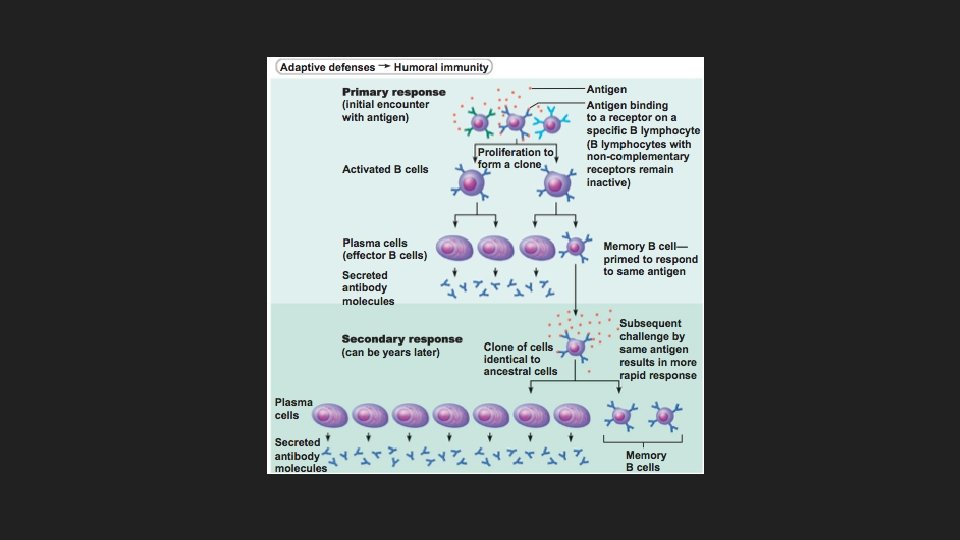
Humoral Immune Response B lymphocytes are activated when antigens bind to its surface receptors. Clonal selection is the process of the B cell growing and multiplying to form an army of cells that are capable of recognizing the same antigens. Plasma cells are the antibody-secreting cells of the humoral response; most clones develop into plasma cells. The clones that do not become plasma cells develop into memory cells.
Humoral Immune Response Immunological memory The primary immune response occurs on first exposure to a particular antigen, with a lag time of about 3 -6 days. The secondary immune response occurs when someone is re-exposed to the same antigen. It is faster, more prolonged, and more effective.
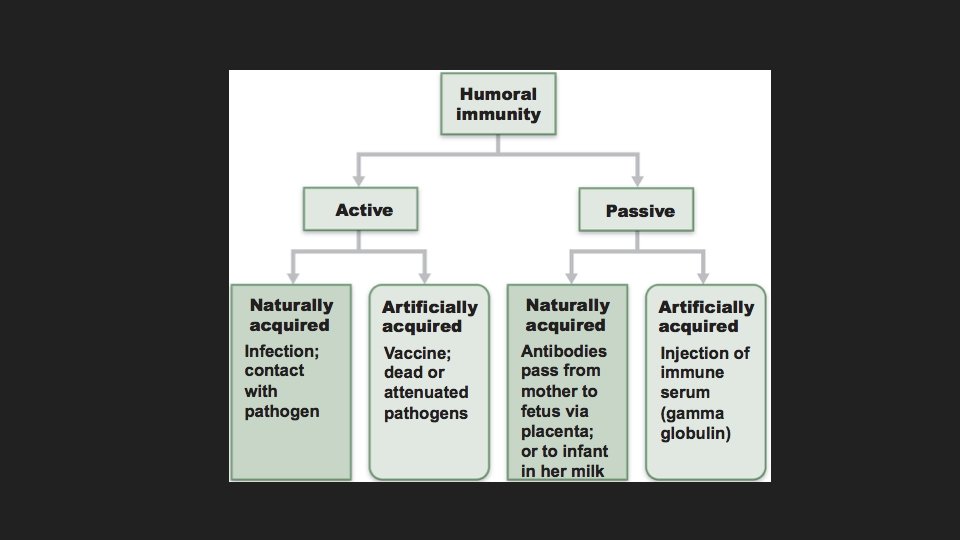
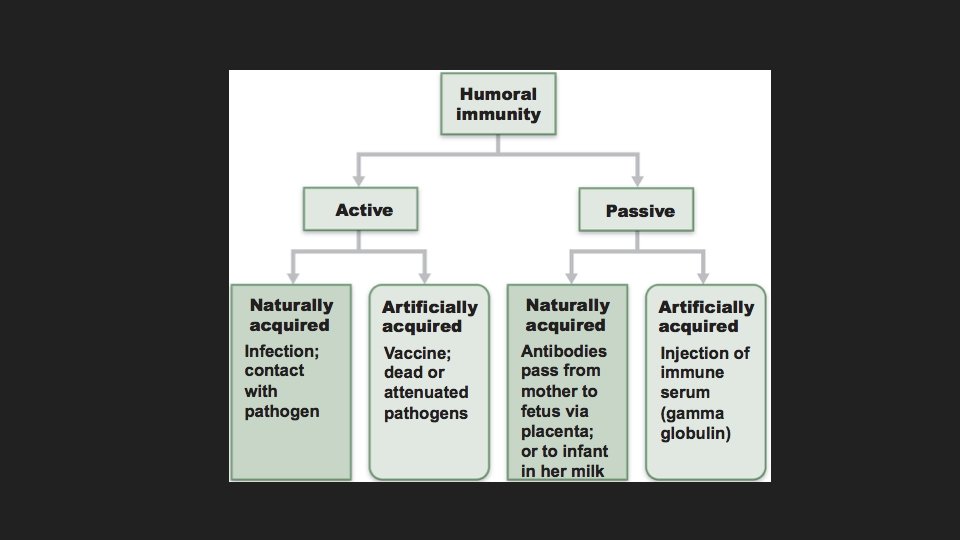
Humoral Immune Response Active immunity occurs when the body mounts an immune response to an antigen. Naturally acquired active immunity occurs when a person suffers through the symptoms of an infection. Artificially acquired active immunity occurs when a person is given a vaccine
Humoral Immune Response Passive immunity occurs when a person is given preformed antibodies. Naturally acquired passive immunity occurs when a mother’s antibodies enter fetal circulation. Artificially acquired passive immunity occurs when a person is given preformed antibodies that have been harvested from another person.
Humoral Immune Response Antibodies, immunoglobulins, are proteins secreted by plasma cells in response to an antigen that are capable of binding to that antigen. Complement fixation and activation - complement binds to antibodies attached to antigens, and leads to lysis of the cell. Neutralization - antibodies block specific sites on viruses ausing them to lose their toxic effects. Agglutination - antibodies cross-link to antigens on cells, causing clumping. Precipitation - soluble molecules are cross-linked into large complexes that settle out of solution.
Cell-Mediated Immune Response T cells must accomplish a double recognition process: they must recognize both self (an MHC protein of a body cell) and nonself (antigen) at the same time. T cell activation Step 1: T cell antigen receptors (TCRs) bind to an antigen-MHC complex on the surface of a body cell. Step 2: A T cell must recognize one or more co-stimulatory signals. Once activated, a T cell enlarges and proliferates to form a clone of cells that differentiate and perform functions according to their T cell class.
Cell-Mediated Immune Response Specific T cell roles Helper T cells - stimulate proliferation of other T cells and B cells that have already become bound to antigen. Without helper T cells there is no adaptive immune response Cytotoxic T cells - only T cells that can directly attack and kill other cells displaying antigen Regulatory T cells - release cytokines that suppress the activity of both B cells and other types of T cells. Gamma delta T cells - found in the intestine and are more similar to NK cells than other T cells.
Cell-Mediated Immune Response Organ transplants and prevention of rejection Grafts Autographs - transplanted from one body site to another in the same person. Isografts – transplanted from a genetically identical individual, identical twin. Allografts - transplanted from individuals that are not genetically identical but belong to the same species Xenografts – transplanted from individuals of different species Transplant success depends on the similarity of the tissues because cytotoxic T cells, NK cells, and antibodies work to destroy foreign tissues.
Homeostatic Imbalances Immunodeficiencies are any congenital or acquired conditions that cause immune cells, phagocytes, or complement to behave abnormally. Severe combined immunodeficiency (SCID) - congenital condition that produces a deficit of B and T cells. Acquired immune deficiency syndrome (AIDS) - cripples the immune system by interfering with helper T cells.
Homeostatic Imbalances Autoimmune diseases occur when the immune system loses its ability to differentiate between self and nonself cells and ultimately destroys itself. Hypersensitivities are the result of the immune system causing tissue damage as it fights off a perceived threat that would otherwise be harmless. Immediate hypersensitivities (allergies) - begin within seconds after contact and last about half an hour. Subacute hypersensitivities (some allergies) - take 1 -3 hours to occur and last 10 -15 hours Delayed hypersensitivity (transplants) - reactions take 1 -3 days to occur and may take weeks to go away.