Venous and Lymphatic drainage of Lower limb Dr
Venous and Lymphatic drainage of Lower limb Dr Shivram Bhat P

Learning objectives • To learn the origin, termination, course, tributaries and applied anatomy of veins of lower limb. • To learn about the different groups of lymphnodes and their applied anatomy.
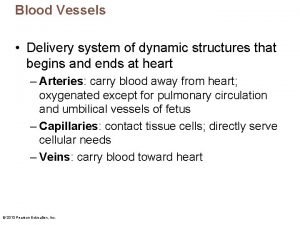
Veins of the lower limb • Divided in to two groups • Superficial veins • Deep veins
Venous drainage of lower limb • Superficial veins – are in the subcutaneous tissue • They have thicker wall compared to other superficial veins • Not accompanied by any arteries • Have many valves • These break the venous column into shorter segments • They are connected to the deep veins by many perforating veins
Venous drainage of lower limb • Deep veins – lie deep to the deep fascia, enclosed in a tight sleeve of deep fascia • Accompany the arteries – venae comitantes • They occur as paired, frequently interconnecting veins that flank the accompanying artery • The pulsation of these arteries compress the vein and help in the movement of venous blood
Veins of the lower limb • Superficial: • Great (long) saphenous vein • Short (small) saphenous vein • Many tributaries of the above veins • Deep veins: accompany arteries • Anterior tibial • Posterior tibial • Popliteal • Femoral • Plantar arch and its tributaries
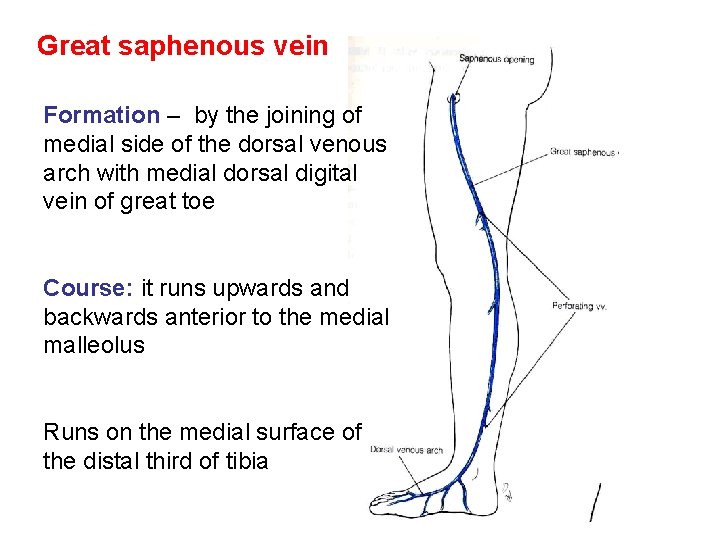
Great saphenous vein Formation – by the joining of medial side of the dorsal venous arch with medial dorsal digital vein of great toe Course: it runs upwards and backwards anterior to the medial malleolus Runs on the medial surface of the distal third of tibia
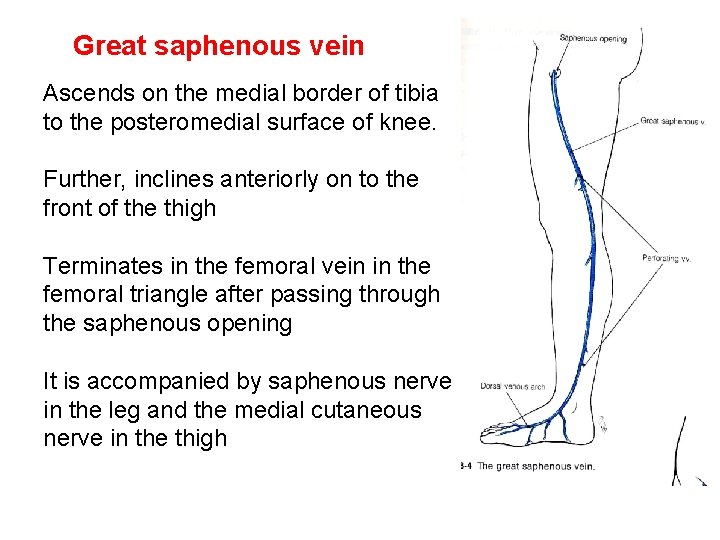
Great saphenous vein Ascends on the medial border of tibia to the posteromedial surface of knee. Further, inclines anteriorly on to the front of the thigh Terminates in the femoral vein in the femoral triangle after passing through the saphenous opening It is accompanied by saphenous nerve in the leg and the medial cutaneous nerve in the thigh
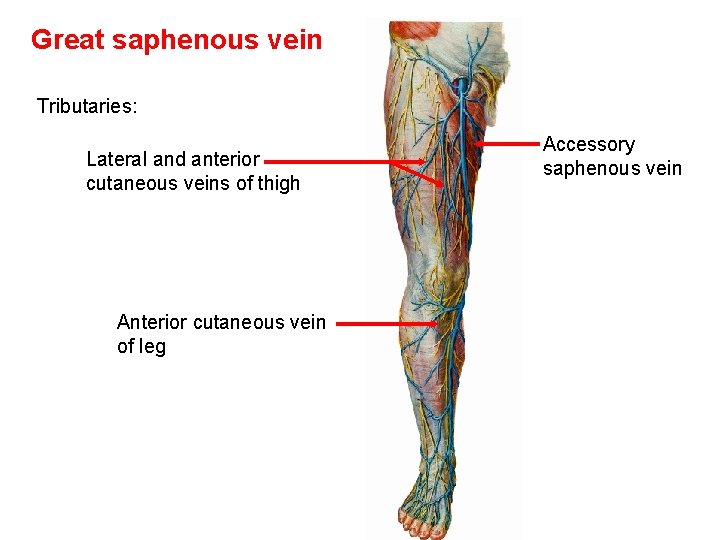
Great saphenous vein Tributaries: Lateral and anterior cutaneous veins of thigh Anterior cutaneous vein of leg Accessory saphenous vein
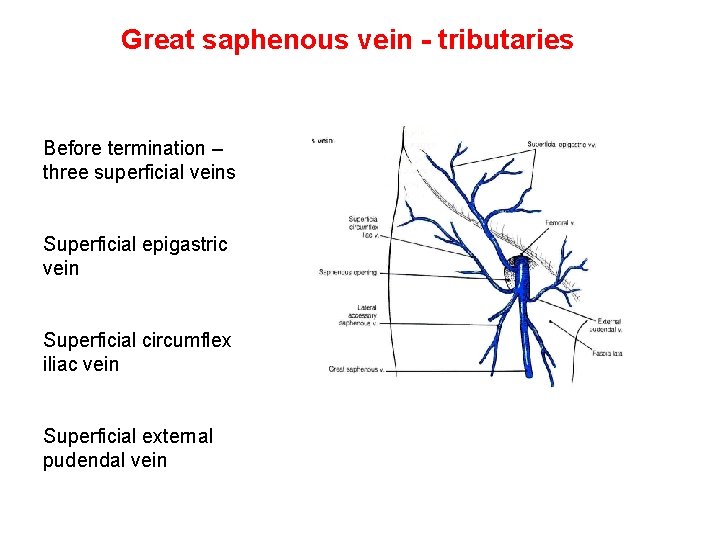
Great saphenous vein - tributaries Before termination – three superficial veins Superficial epigastric vein Superficial circumflex iliac vein Superficial external pudendal vein
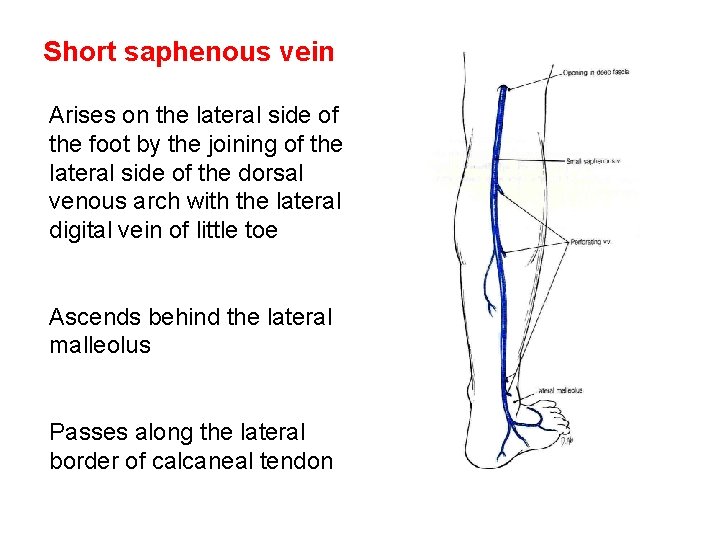
Short saphenous vein Arises on the lateral side of the foot by the joining of the lateral side of the dorsal venous arch with the lateral digital vein of little toe Ascends behind the lateral malleolus Passes along the lateral border of calcaneal tendon
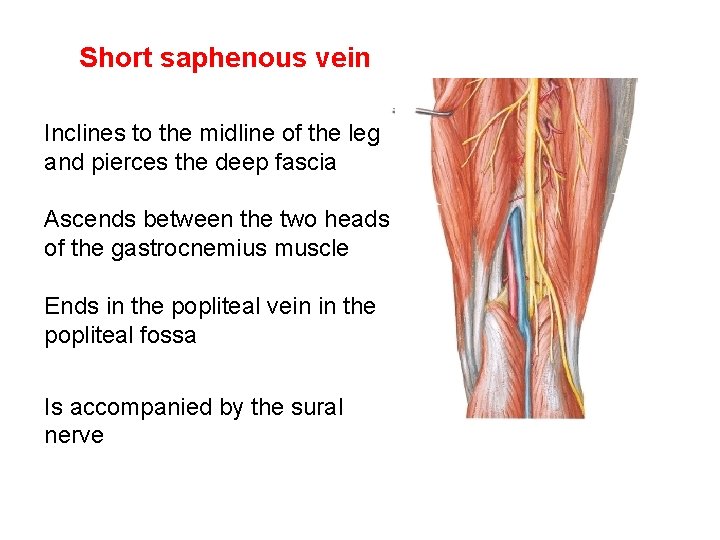
Short saphenous vein Inclines to the midline of the leg and pierces the deep fascia Ascends between the two heads of the gastrocnemius muscle Ends in the popliteal vein in the popliteal fossa Is accompanied by the sural nerve

Perforating veins/perforators Connect superficial veins with deep veins They pierce the deep fascia obliquely Contain valves that allow flow of blood from superficial veins to deep veins
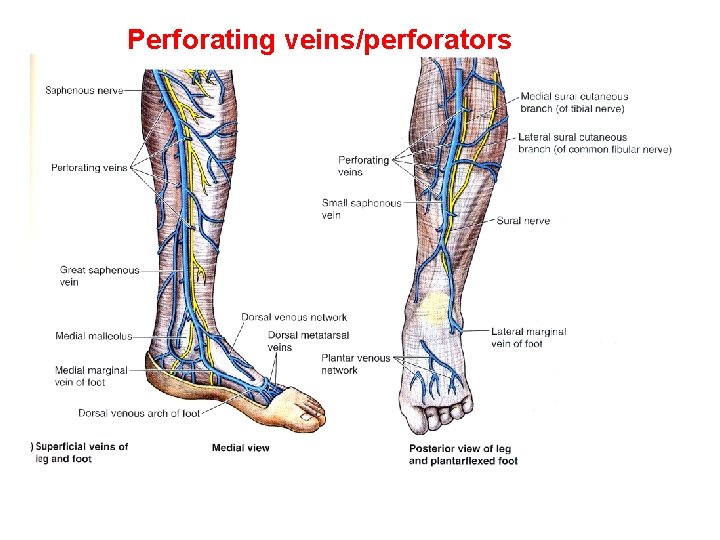
Perforating veins/perforators
Perforating veins/perforators • Flow from superficial to deep veins is important for venous return from lower limbs. • It enables the muscular contractions to propel the venous blood to heart against the pull of gravity • This is referred as musculovenous pump
Perforating veins/perforators • The outward expansion of the muscles during contraction is limited in the lower limb due to thick deep fascia • This compresses the veins, ‘milking’ the blood superiorly towards the heart – this is called musculovenous pump
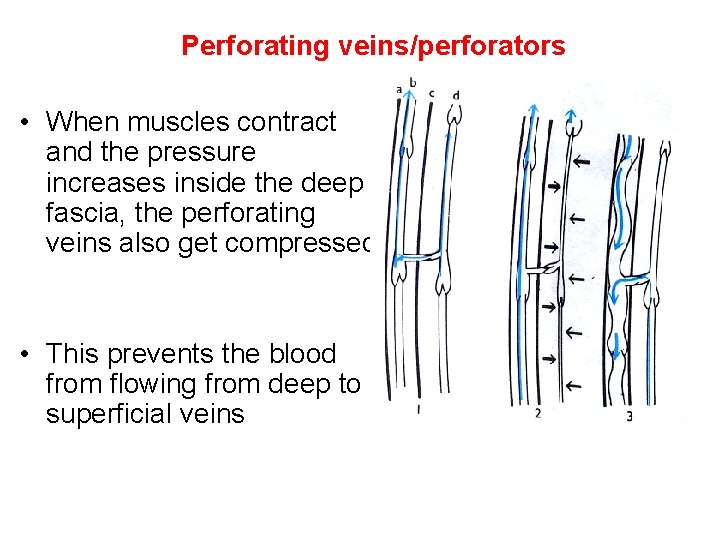
Perforating veins/perforators • When muscles contract and the pressure increases inside the deep fascia, the perforating veins also get compressed. • This prevents the blood from flowing from deep to superficial veins
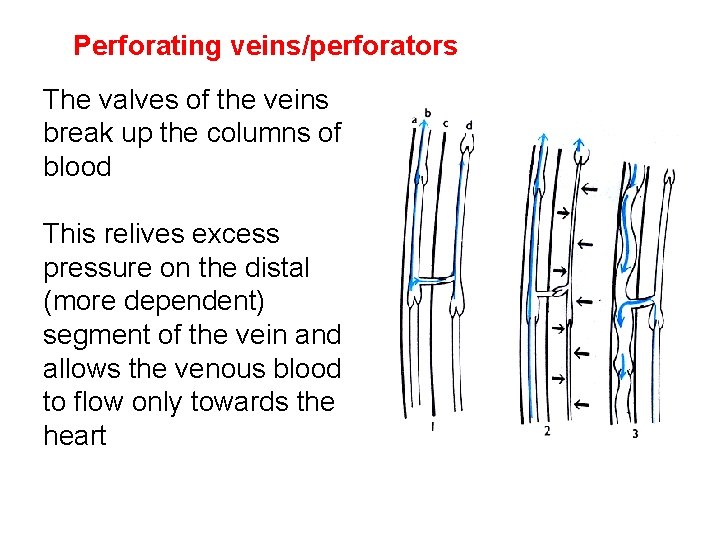
Perforating veins/perforators The valves of the veins break up the columns of blood This relives excess pressure on the distal (more dependent) segment of the vein and allows the venous blood to flow only towards the heart
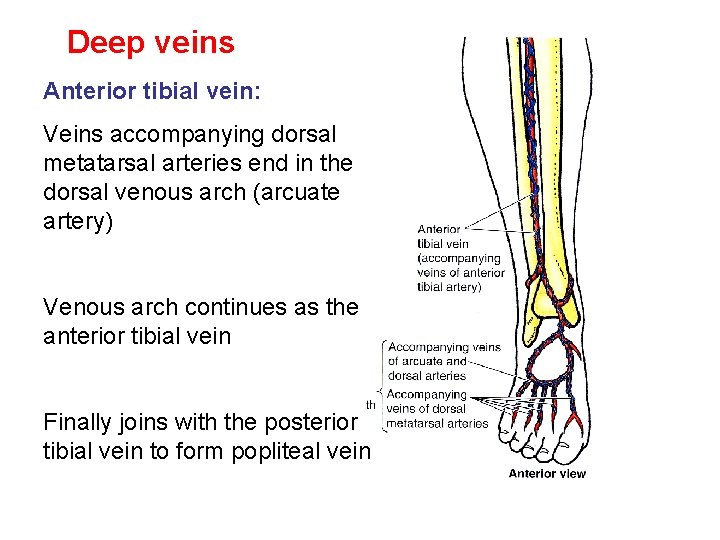
Deep veins Anterior tibial vein: Veins accompanying dorsal metatarsal arteries end in the dorsal venous arch (arcuate artery) Venous arch continues as the anterior tibial vein Finally joins with the posterior tibial vein to form popliteal vein
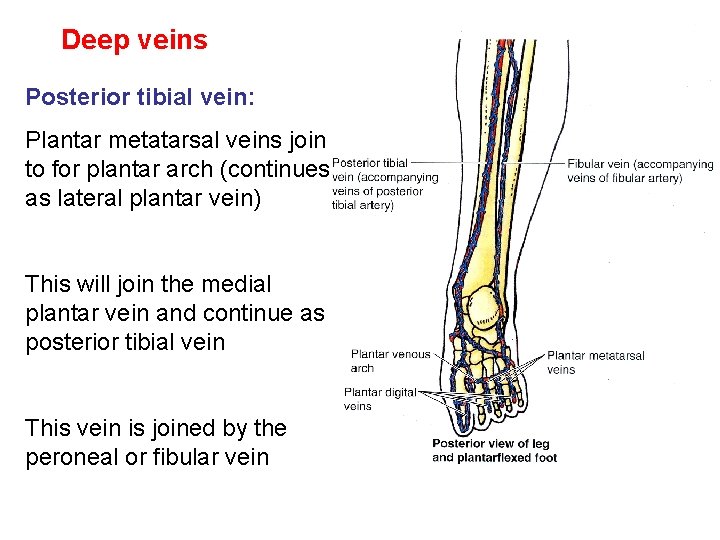
Deep veins Posterior tibial vein: Plantar metatarsal veins join to for plantar arch (continues as lateral plantar vein) This will join the medial plantar vein and continue as posterior tibial vein This vein is joined by the peroneal or fibular vein
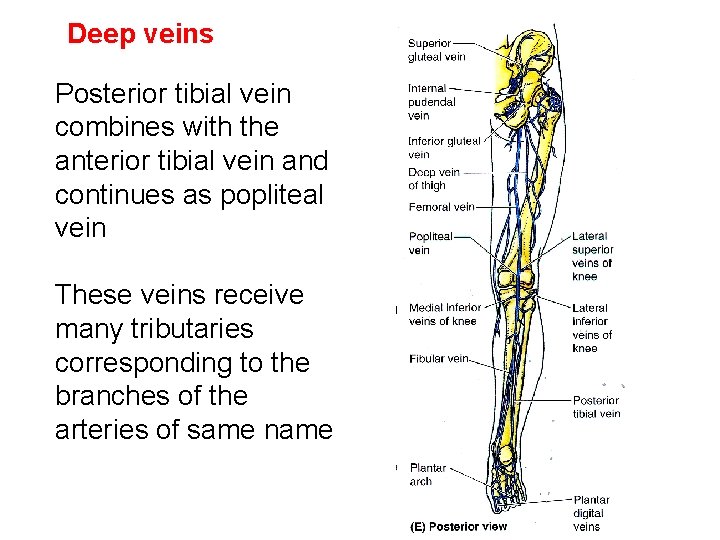
Deep veins Posterior tibial vein combines with the anterior tibial vein and continues as popliteal vein These veins receive many tributaries corresponding to the branches of the arteries of same name
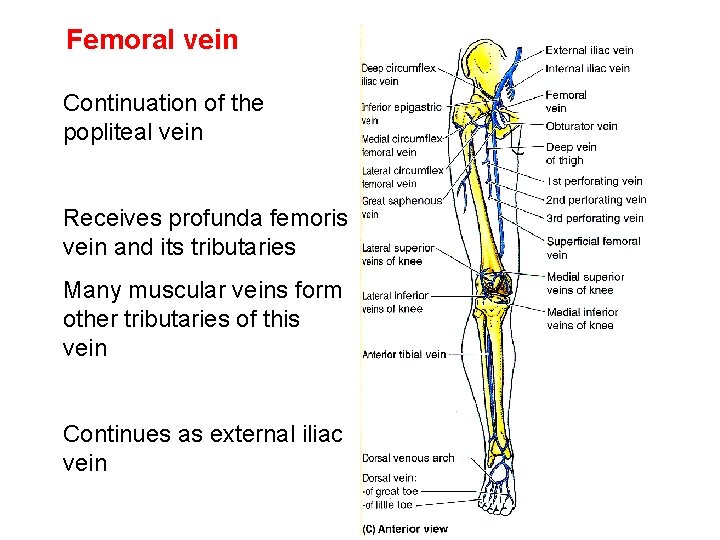
Femoral vein Continuation of the popliteal vein Receives profunda femoris vein and its tributaries Many muscular veins form other tributaries of this vein Continues as external iliac vein
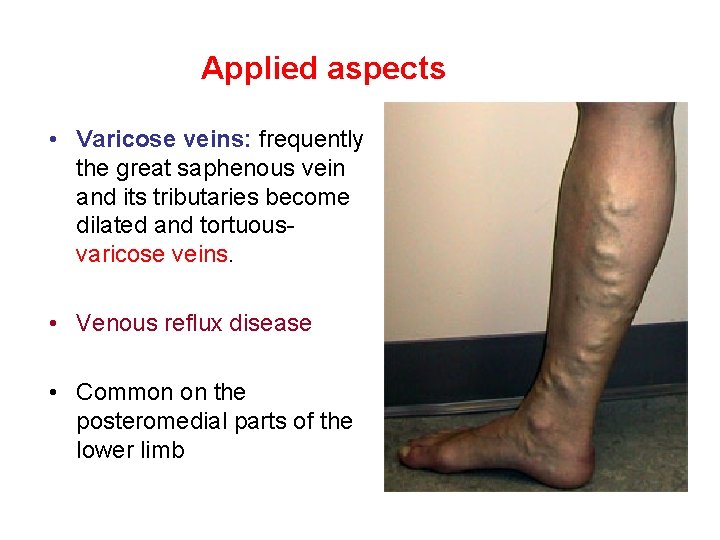
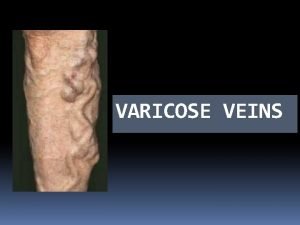
Applied aspects • Varicose veins: frequently the great saphenous vein and its tributaries become dilated and tortuousvaricose veins. • Venous reflux disease • Common on the posteromedial parts of the lower limb
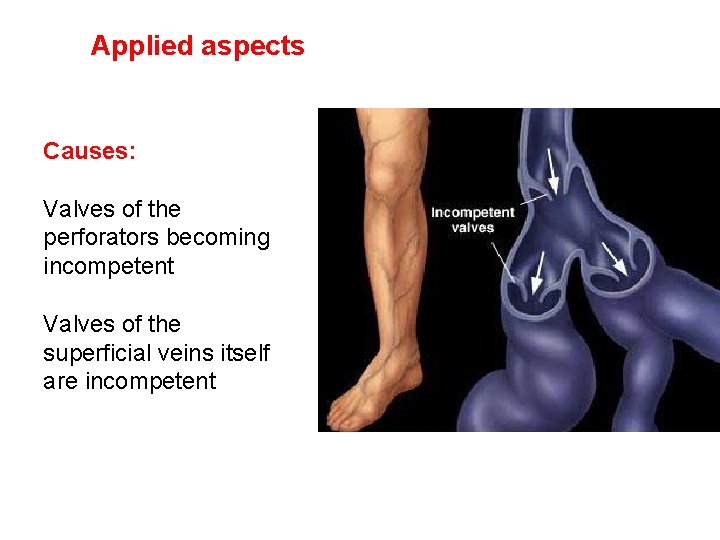
Applied aspects Causes: Valves of the perforators becoming incompetent Valves of the superficial veins itself are incompetent
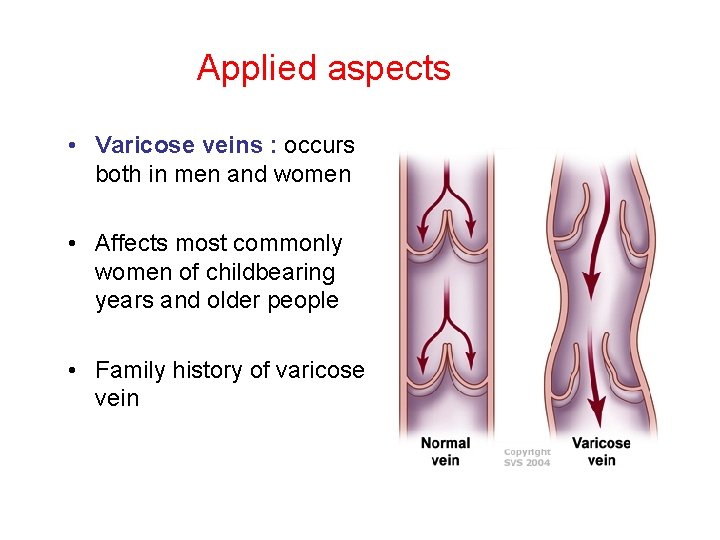
Applied aspects • Varicose veins : occurs both in men and women • Affects most commonly women of childbearing years and older people • Family history of varicose vein
Varicose veins • Common among persons standing for long durations • Pregnant women • Sedentary habit • Weight gain
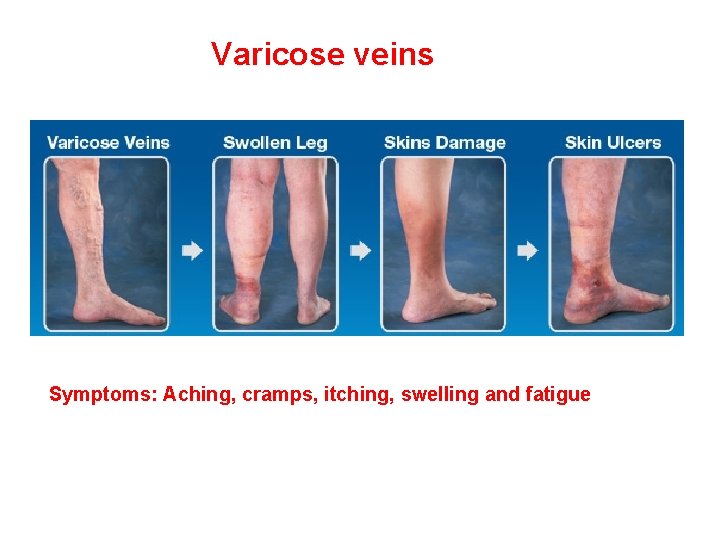
Varicose veins Symptoms: Aching, cramps, itching, swelling and fatigue
Applied aspects • Venous thrombosis: blood clot formation e. g. bone fracture • Venous stasis (stagnation) is another cause of clot formation. • Stasis occurs due to: • Incompetent deep fascia that fails to resist muscle expansion, diminishing the effectiveness of musculovenous pump
Applied aspects • External pressure on the veins from the bedding during prolonged hospitalisation or from tight cast or bandage • Muscular inactivity – during an overseas flight
Applied aspects • Thrombophlebitis: inflammation with clot formation may develop around vein • A thrombus can break free from lower limb vein and reach the lungs, constitutes pulmonary thromboembolism. • A large embolus may obstruct the pulmonary artery and cause death.
Applied aspects • Saphenous venous graft: commonly used for coronary artery bypass surgery • Reasons: easily accessible • Sufficient length between a tributary and perforating vein so that a usable length can be harvested
Applied aspects • Wall contains higher percentage of muscle and elastic fibers • When part of vein is used for bypass the vein is reversed so that valves do not obstruct the flow of blood in the graft • Long saphenous vein is useful in emergency transfusion
Investigations • Venography – function of the vein and their valves • Doppler ultrasound – useful to study the flow of blood and patency of the vein
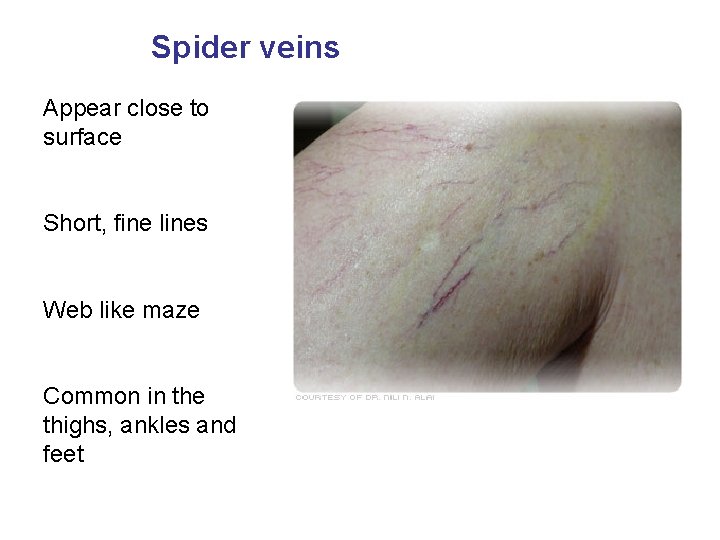
Spider veins Appear close to surface Short, fine lines Web like maze Common in the thighs, ankles and feet
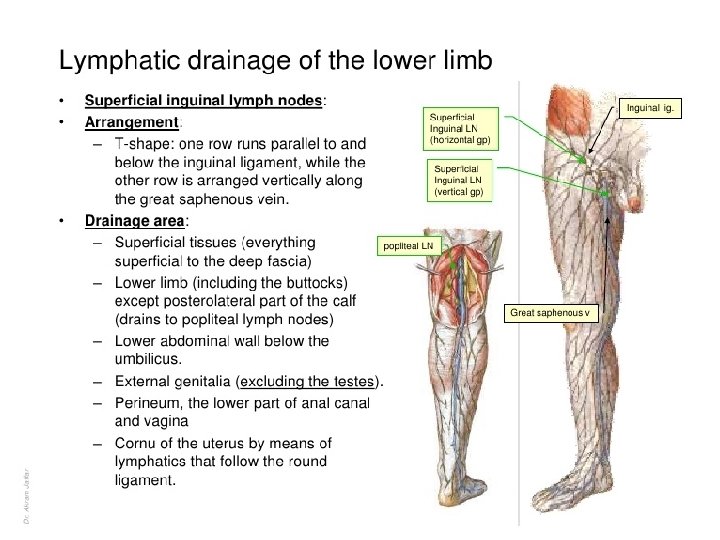
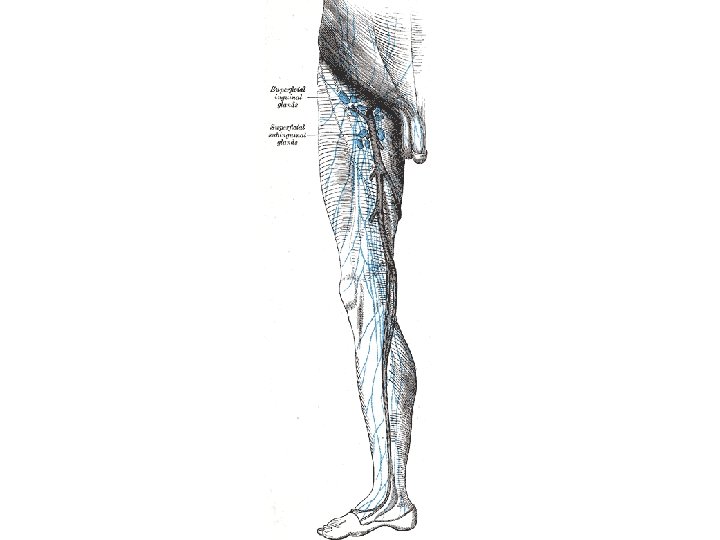
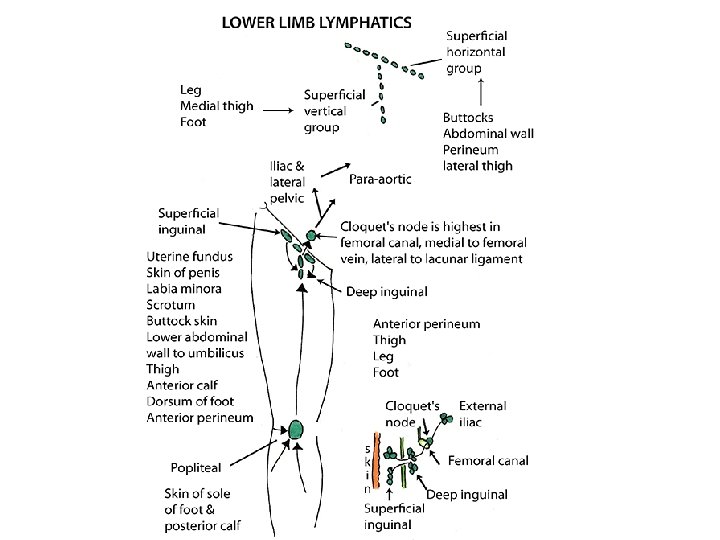
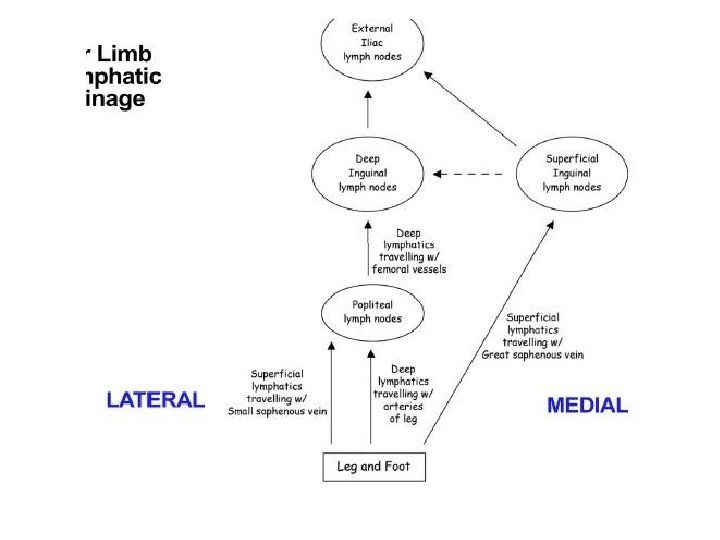
Lymph Nodes of Lower Limb • Nodes – inguinal and popliteal. • Inguinal – superficial and deep group.

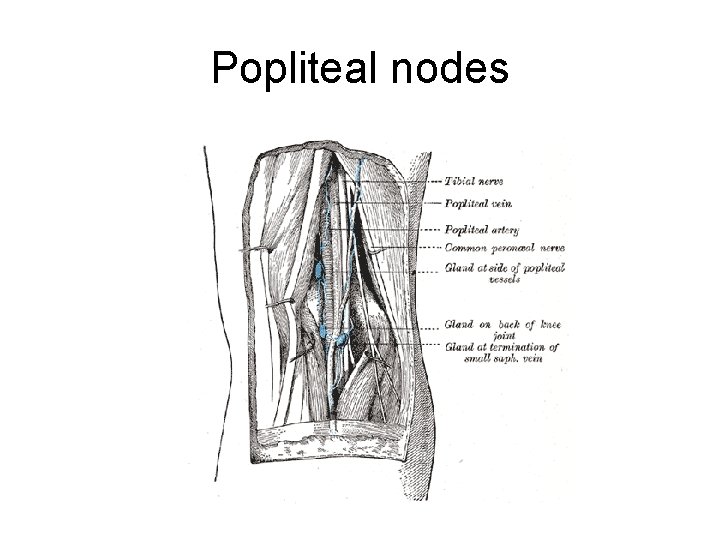
Popliteal nodes
Lymphatic vessels
Applied anatomy • Lymphangitis. • Filariasis. • Lymphoedema.
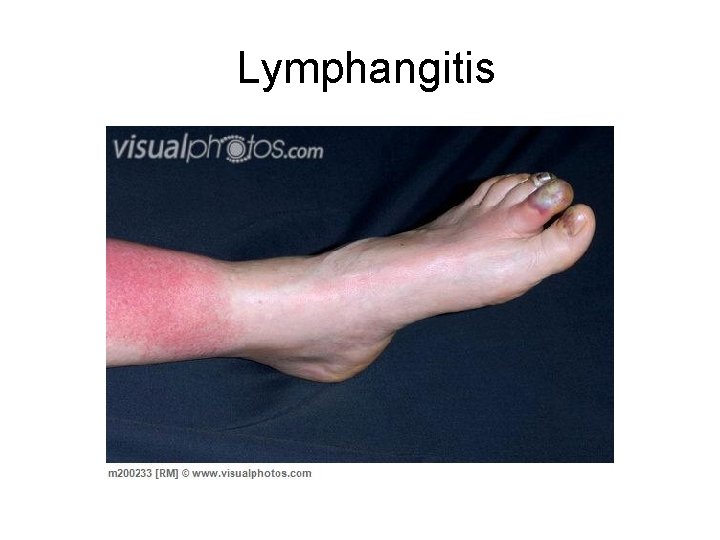
Lymphangitis



Questions • Great saphenous vein. • Inguinal lymph nodes. • Varicose veins.
- Slides: 48