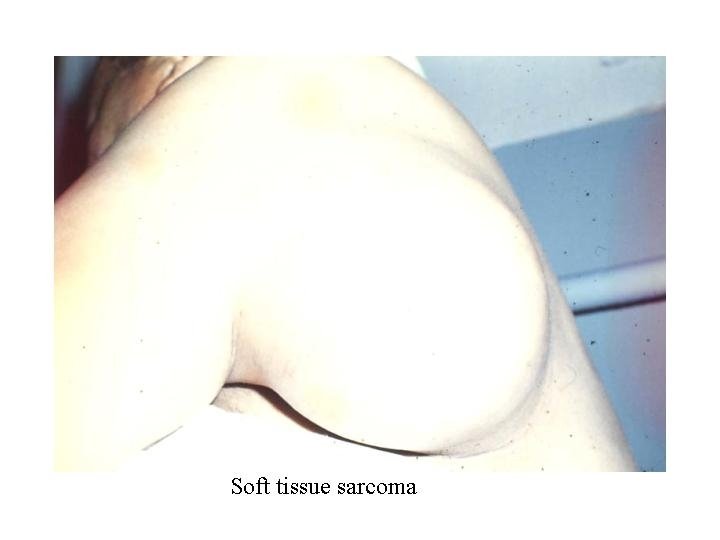
Soft tissue sarcomas of adults Soft Tissue Sarcoma





- Slides: 60
Soft tissue sarcomas of adults
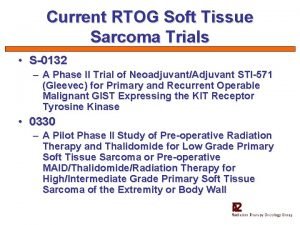
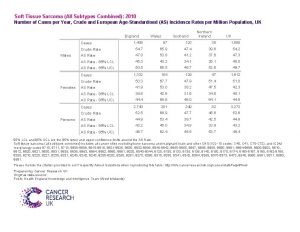
Soft Tissue Sarcoma Epidemiology • Incidence: 2/100. 000 per year • Frequency: 0, 8 -1% of all malignant tumours • Aetiology: widely unknown
Soft Tissue Sarcoma Predisposing Factors • • Ionising radiation Genetic predisposition – Neurofibromatosis – Li-Fraumeni Syndrome – fam. Retinoblastoma – fam. Polyposis coli • Radiation – Increase MFH • Viruses – HIV and kaposi sarcoma • Exposure to chemicals – Phenoxyacetic acid – Chlorophenole – Thorotrast (radioactive) – Vinylchloride – Arsenic • Chron. Lymphatic edema – Stewart-Treves Syndrome
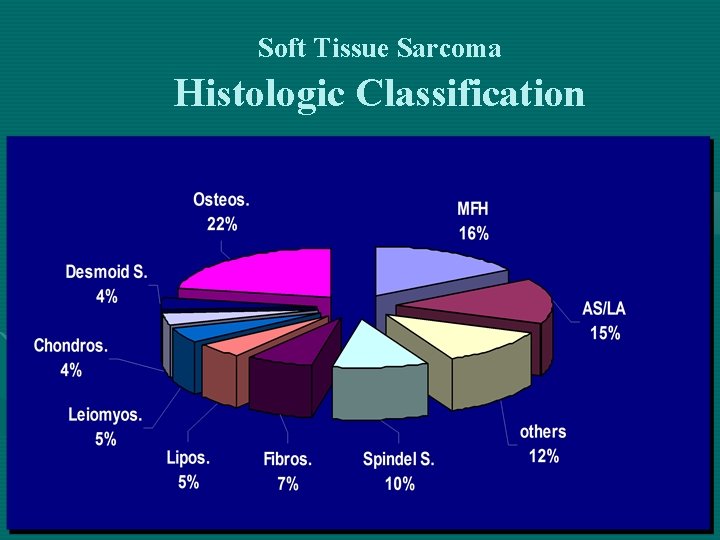
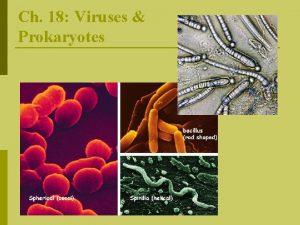
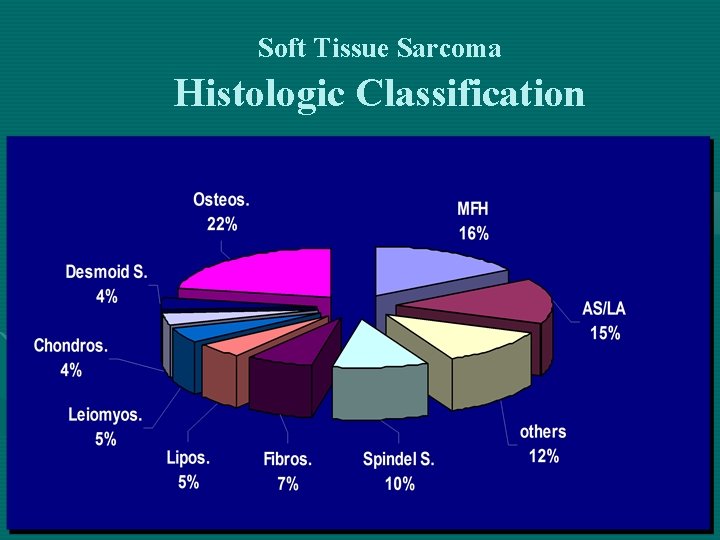
Soft Tissue Sarcoma Histologic Classification
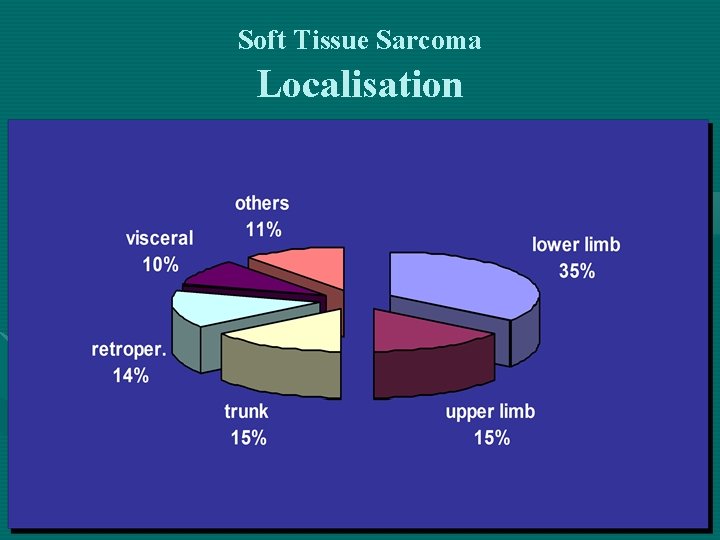
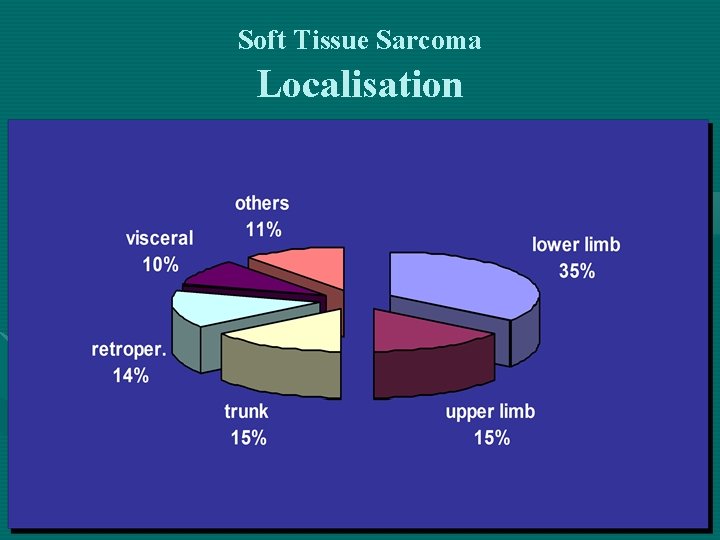
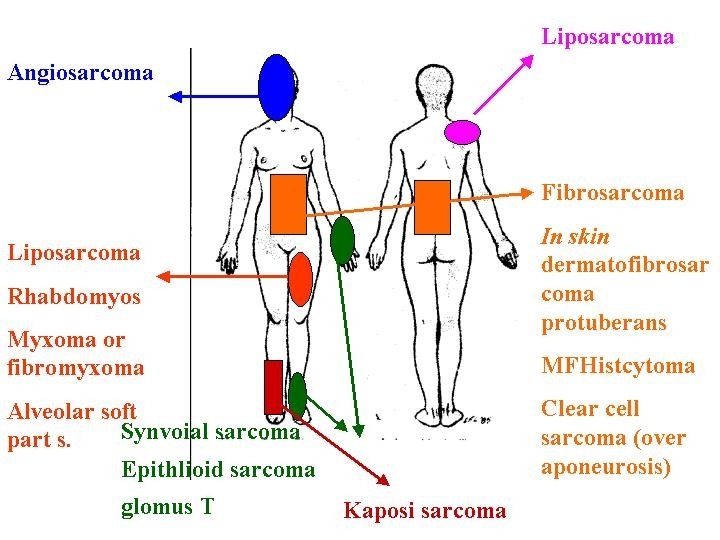
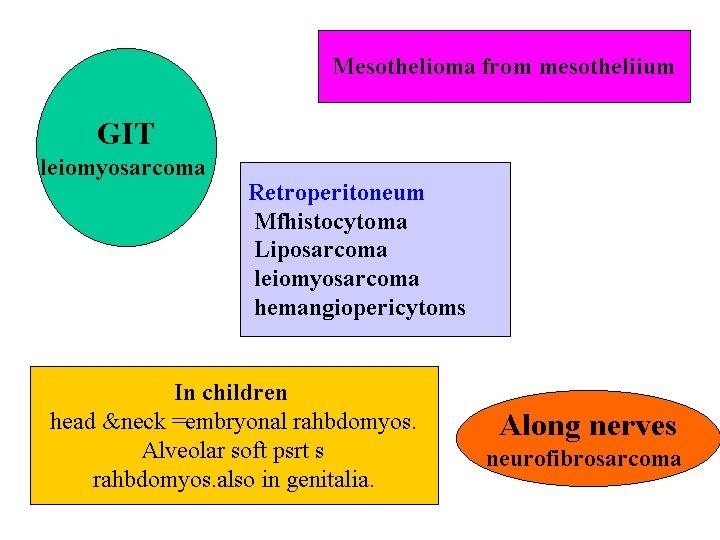
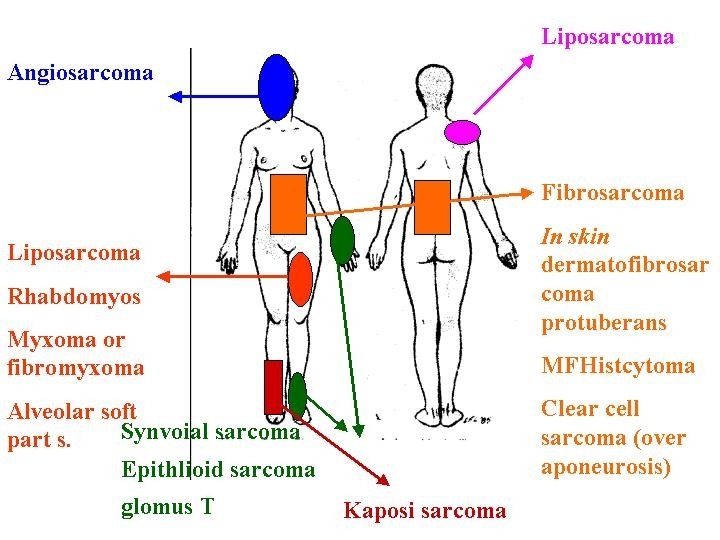
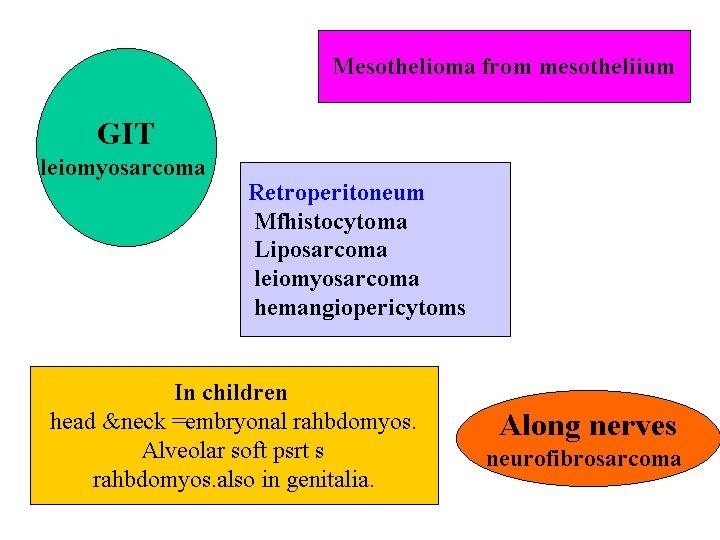
Soft Tissue Sarcoma Localisation
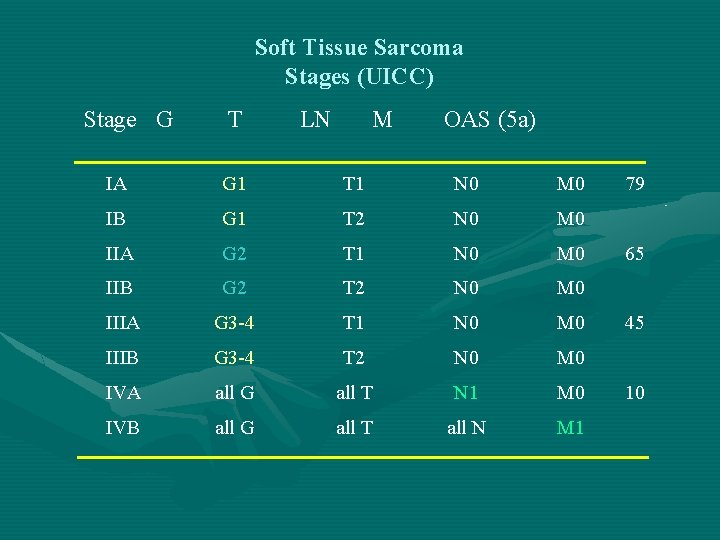
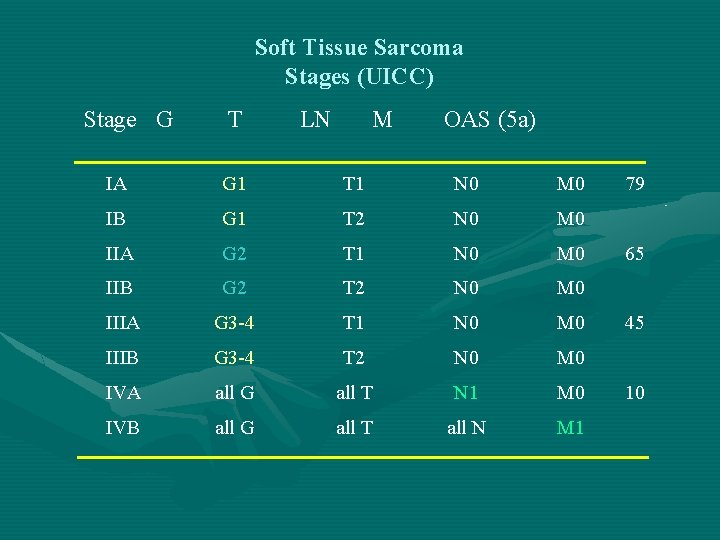
Soft Tissue Sarcoma Stages (UICC) Stage G T LN M OAS (5 a) IA G 1 T 1 N 0 M 0 IB G 1 T 2 N 0 M 0 IIA G 2 T 1 N 0 M 0 IIB G 2 T 2 N 0 M 0 IIIA G 3 -4 T 1 N 0 M 0 IIIB G 3 -4 T 2 N 0 M 0 IVA all G all T N 1 M 0 IVB all G all T all N M 1 79 65 45 10
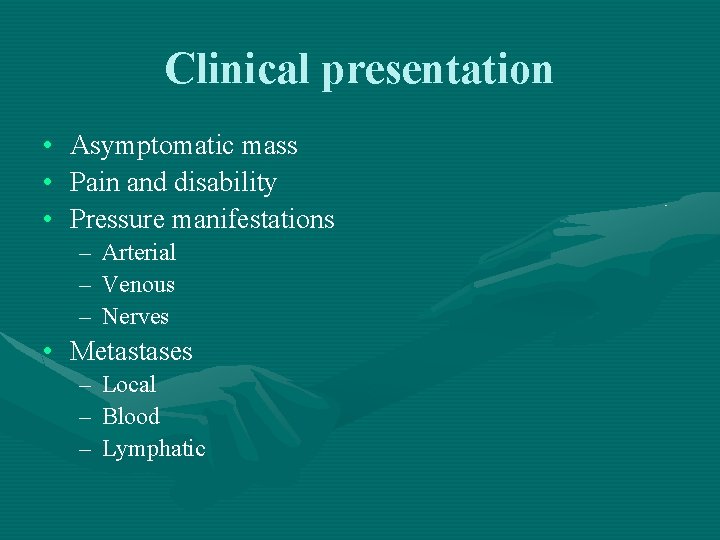
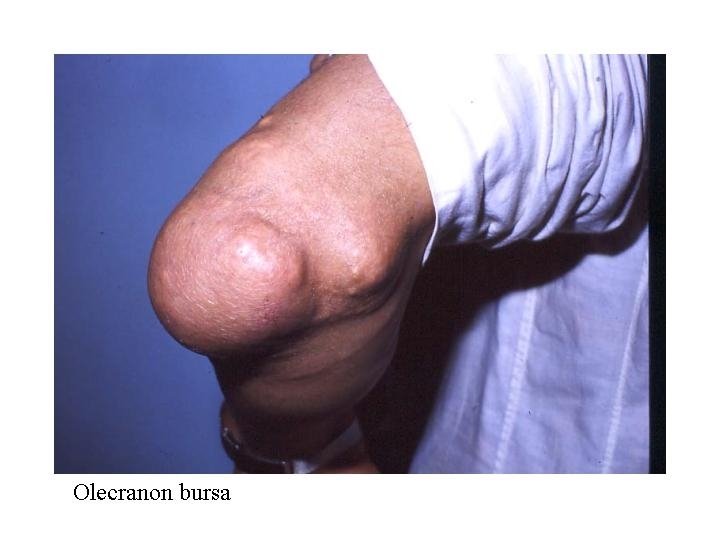
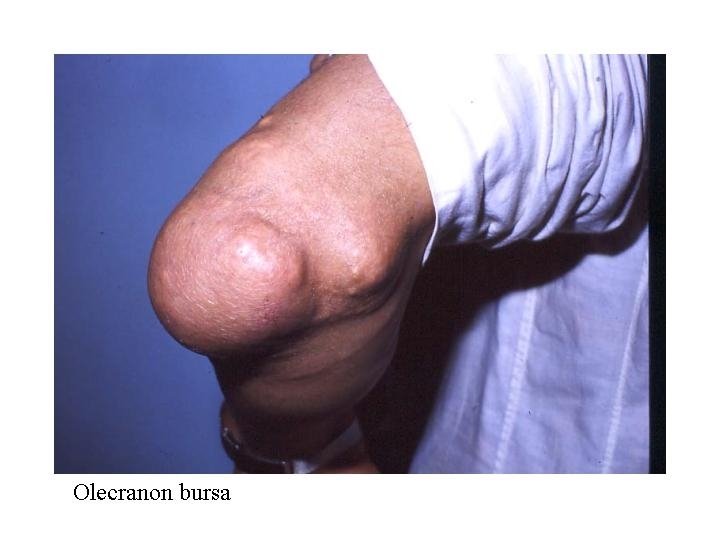
Clinical presentation • • • Asymptomatic mass Pain and disability Pressure manifestations – – – Arterial Venous Nerves • Metastases – – – Local Blood Lymphatic





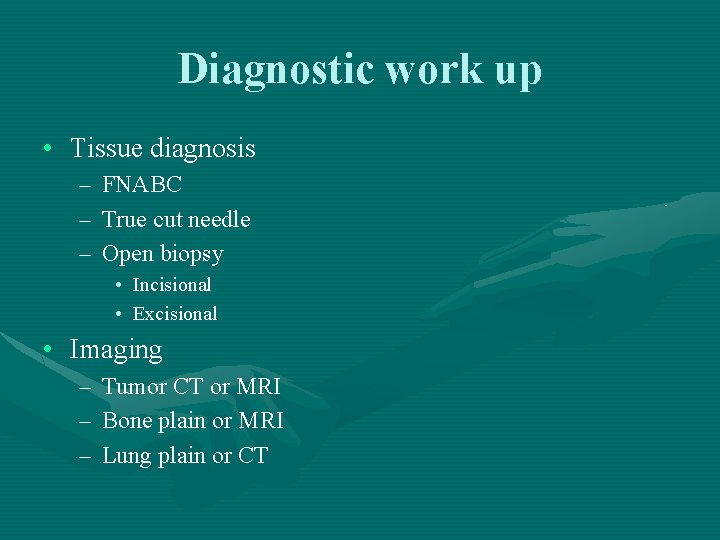
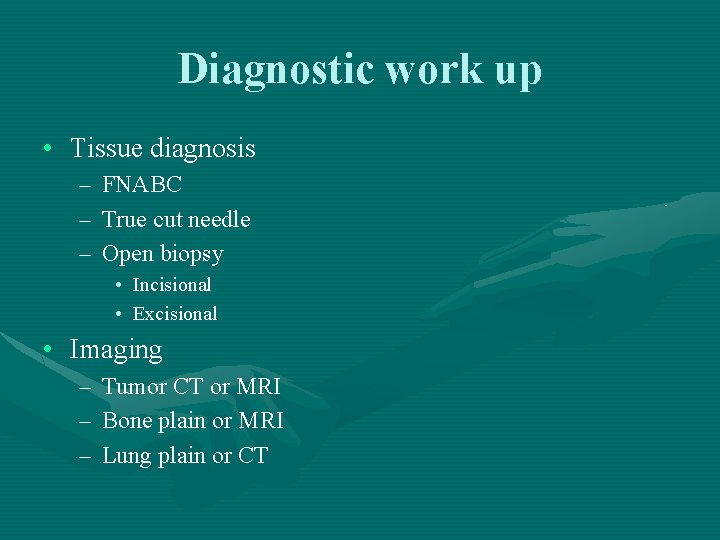
Diagnostic work up • Tissue diagnosis – FNABC – True cut needle – Open biopsy • Incisional • Excisional • Imaging – Tumor CT or MRI – Bone plain or MRI – Lung plain or CT
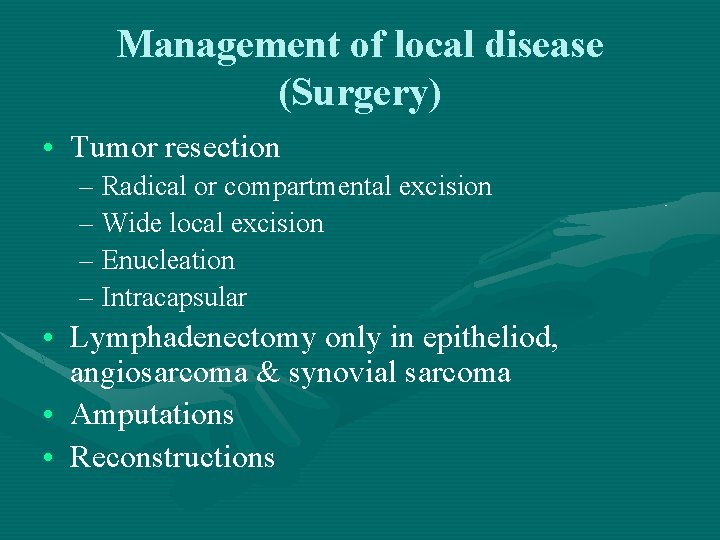
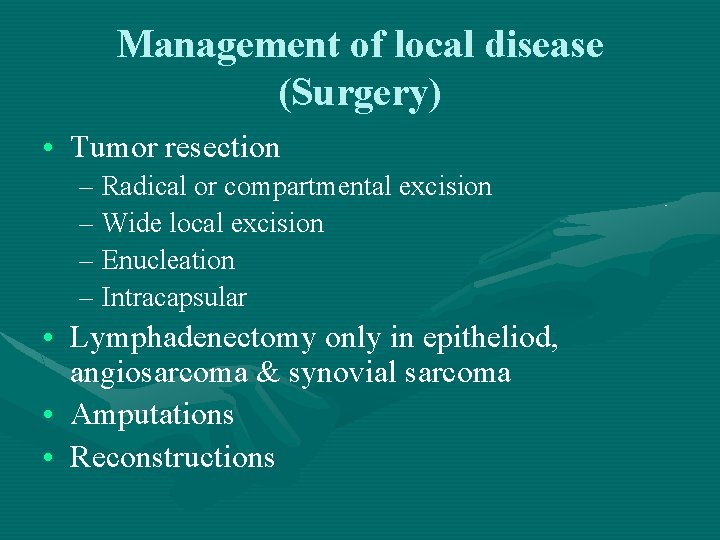
Management of local disease (Surgery) • Tumor resection – Radical or compartmental excision – Wide local excision – Enucleation – Intracapsular • Lymphadenectomy only in epitheliod, angiosarcoma & synovial sarcoma • Amputations • Reconstructions
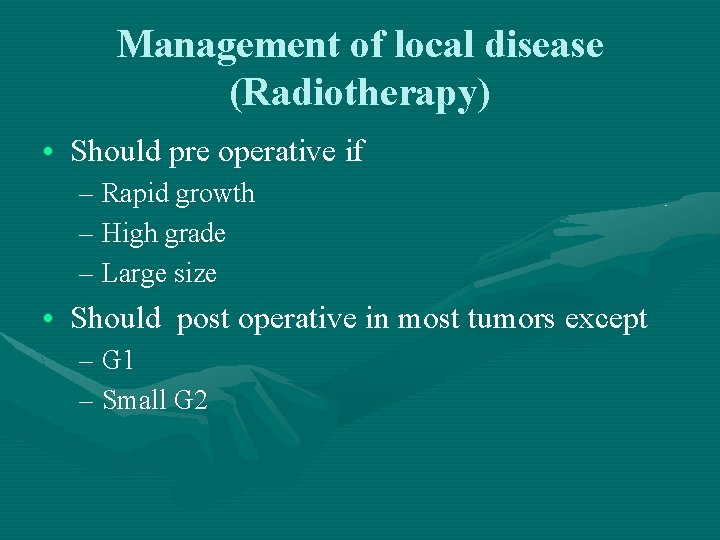
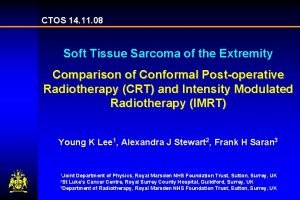
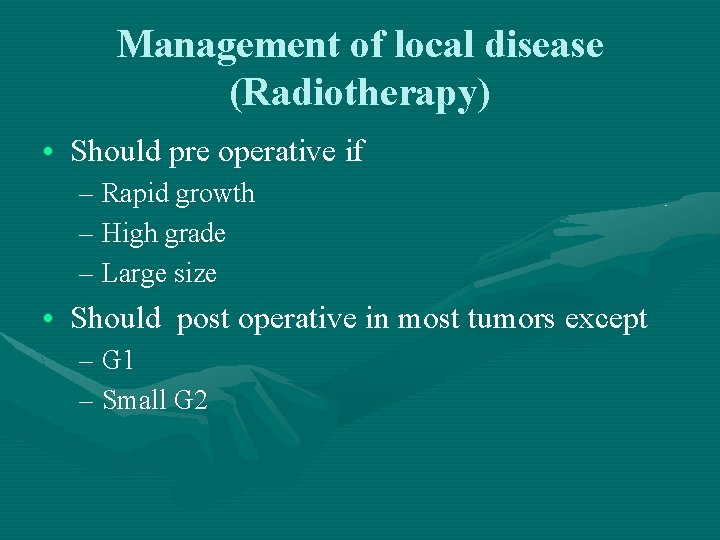
Management of local disease (Radiotherapy) • Should pre operative if – Rapid growth – High grade – Large size • Should post operative in most tumors except – G 1 – Small G 2
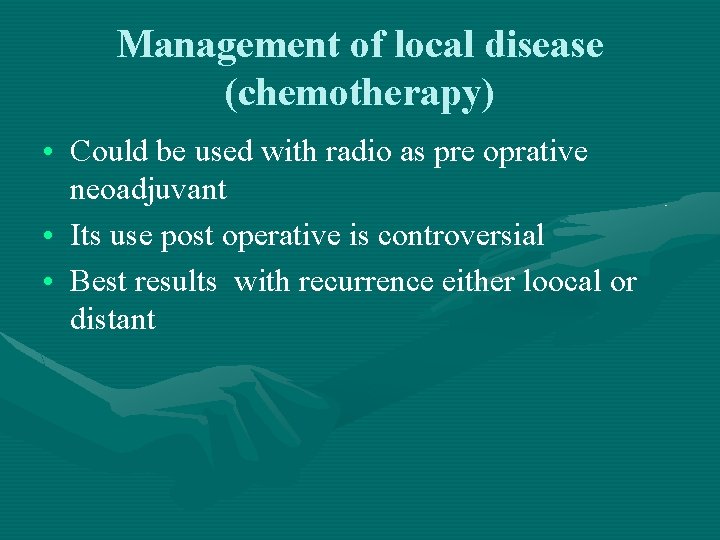
Management of local disease (chemotherapy) • Could be used with radio as pre oprative neoadjuvant • Its use post operative is controversial • Best results with recurrence either loocal or distant
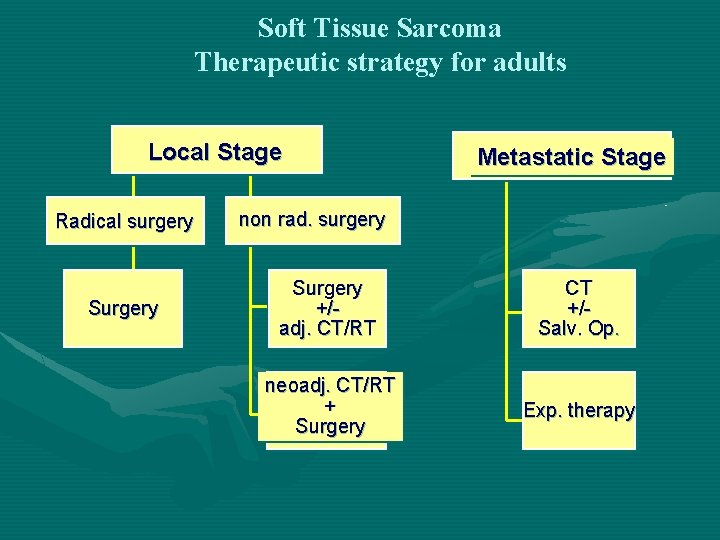
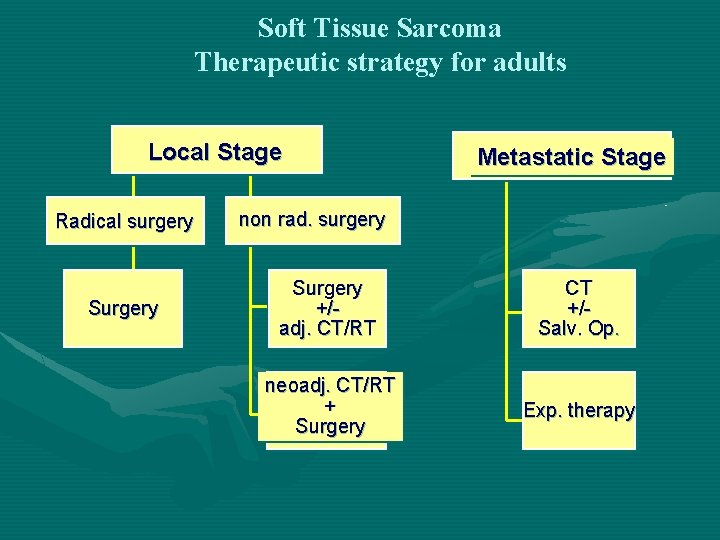
Soft Tissue Sarcoma Therapeutic strategy for adults Local Stage Radical surgery Surgery Metastatic Stage non rad. surgery Surgery +/adj. CT/RT CT +/Salv. Op. neoadj. CT/RT + Surgery Exp. therapy
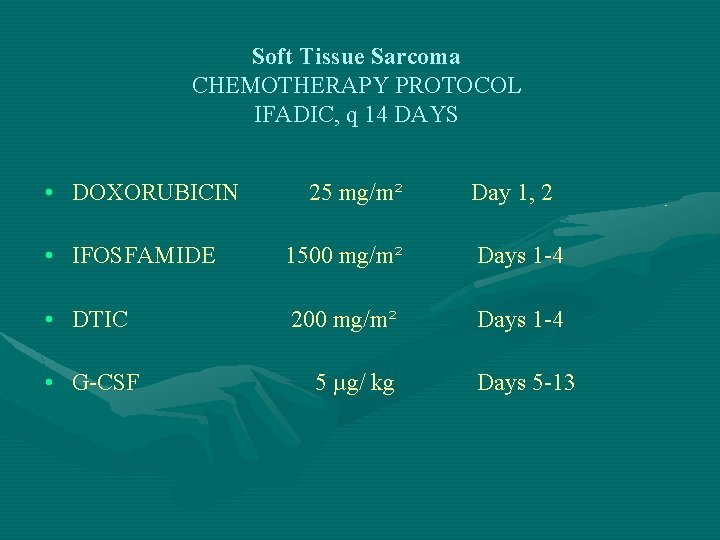
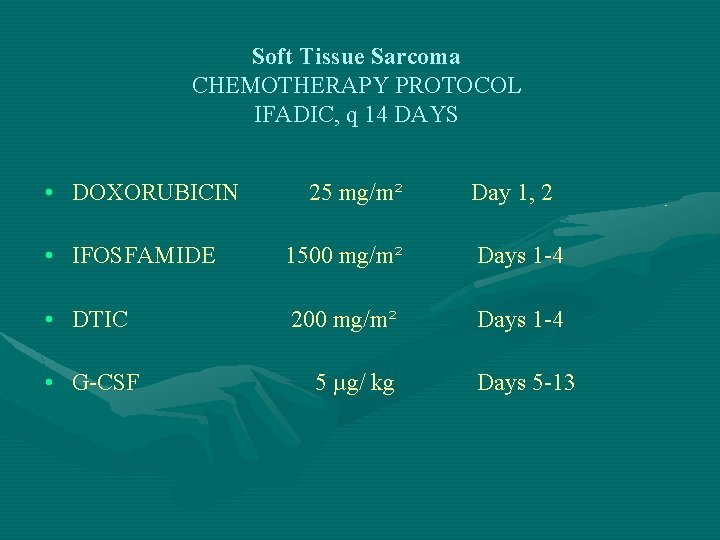
Soft Tissue Sarcoma CHEMOTHERAPY PROTOCOL IFADIC, q 14 DAYS • DOXORUBICIN 25 mg/m² Day 1, 2 • IFOSFAMIDE 1500 mg/m² Days 1 -4 • DTIC 200 mg/m² Days 1 -4 • G-CSF 5 µg/ kg Days 5 -13
Surgery of the wound and infections
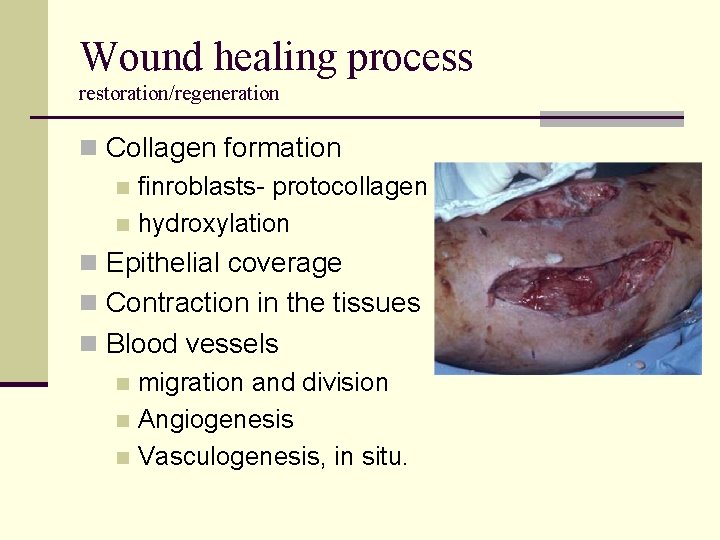
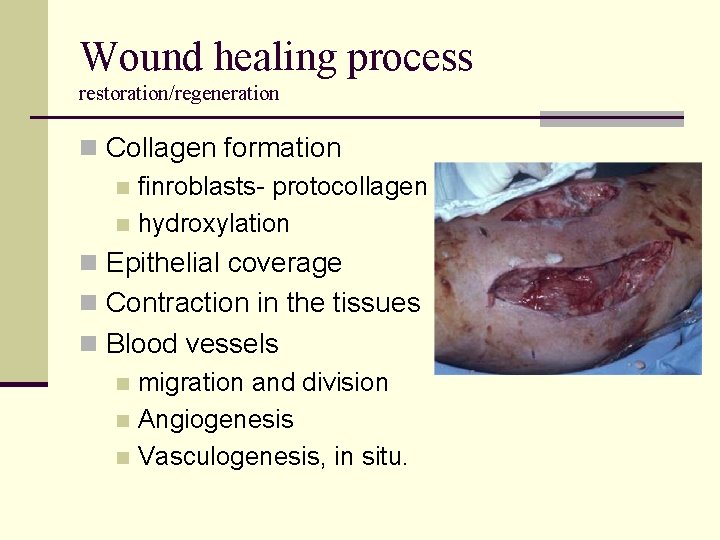
Wound healing process restoration/regeneration n Collagen formation n finroblasts- protocollagen n hydroxylation n Epithelial coverage n Contraction in the tissues n Blood vessels n migration and division n Angiogenesis n Vasculogenesis, in situ.
Wound Healing: Stages n Hemostasis n platelets, endothelial cells, fibrin & fibronectin n Inflammation n neutrophils, macrophages, lymphocytes, growth factors and proteases and cytokines n Proliferation - fibroblasts, epithelial & endothelial n growth factors. n Remodeling - collagenase
Wound healing phases n Lag (24 -48 h) n acute inflammatory response n Prolifaretive (4 -5 weeks) n migration of fibroblasts, capillaries n wound strength: 1 st month 50% 2 nd month 75% 6 th month 95% n Maturation: cross linking, remodelling, contraction
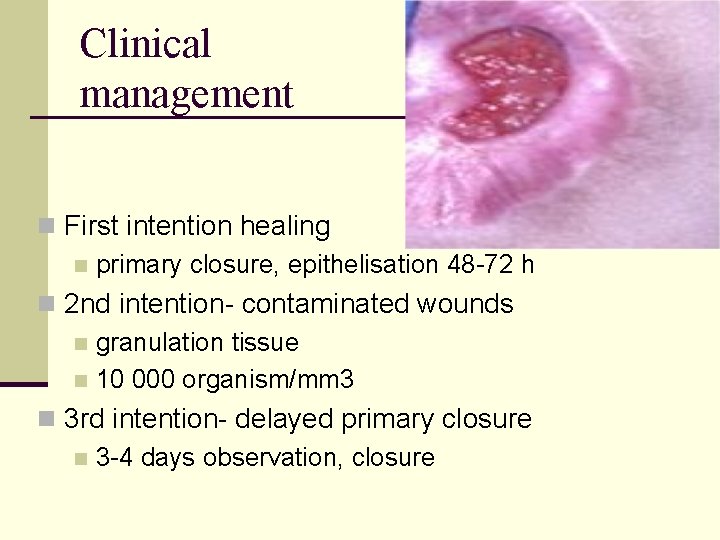
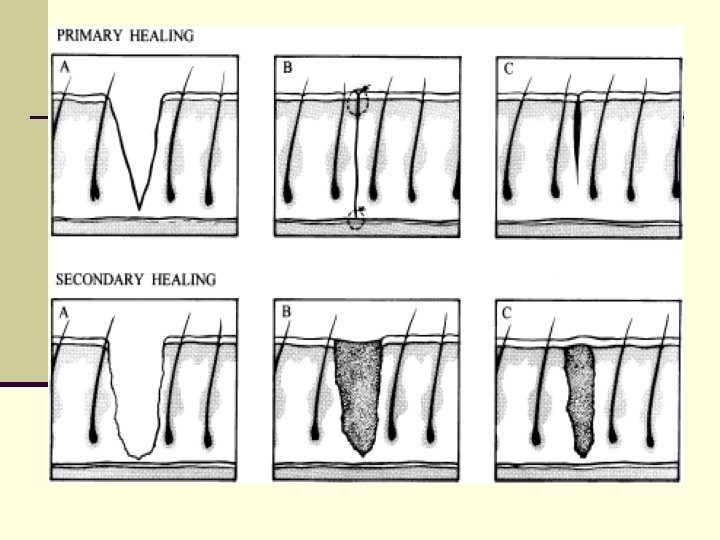
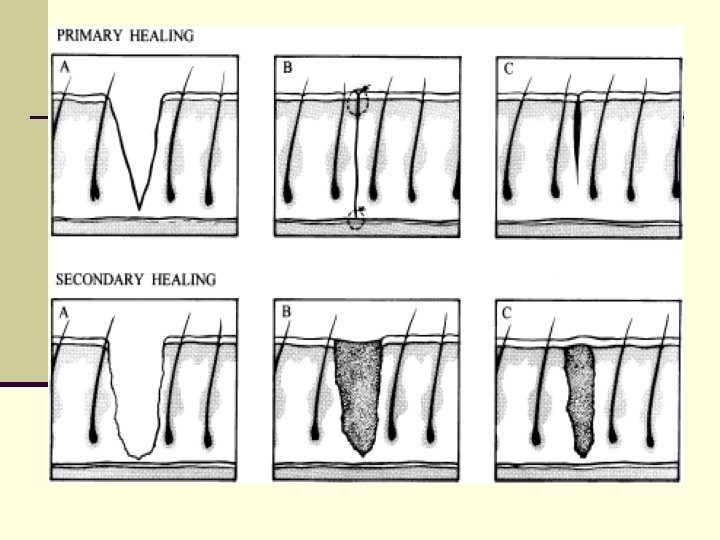
Clinical management n First intention healing n primary closure, epithelisation 48 -72 h n 2 nd intention- contaminated wounds n granulation tissue n 10 000 organism/mm 3 n 3 rd intention- delayed primary closure n 3 -4 days observation, closure
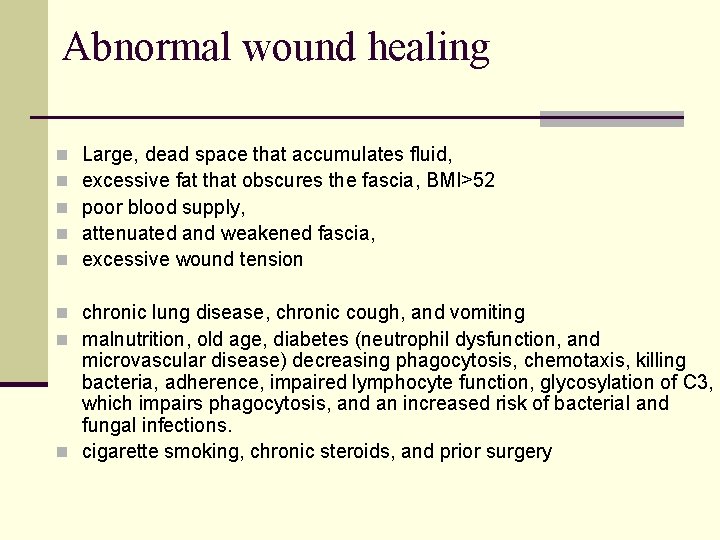
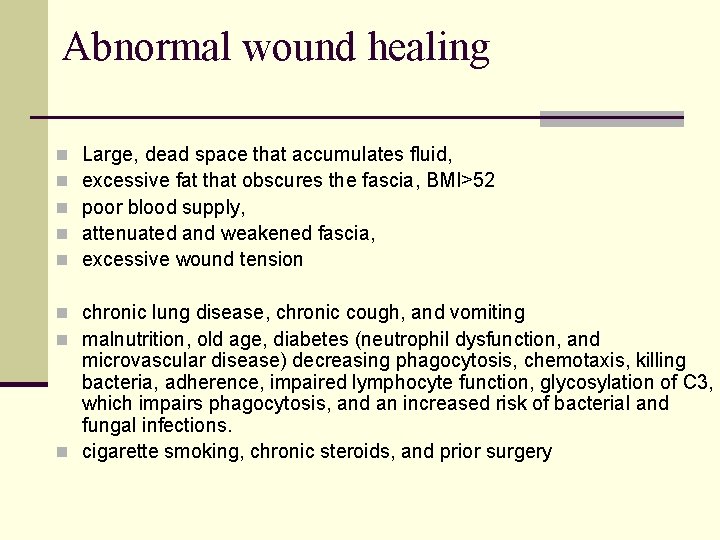
Abnormal wound healing n n n Large, dead space that accumulates fluid, excessive fat that obscures the fascia, BMI>52 poor blood supply, attenuated and weakened fascia, excessive wound tension n chronic lung disease, chronic cough, and vomiting n malnutrition, old age, diabetes (neutrophil dysfunction, and microvascular disease) decreasing phagocytosis, chemotaxis, killing bacteria, adherence, impaired lymphocyte function, glycosylation of C 3, which impairs phagocytosis, and an increased risk of bacterial and fungal infections. n cigarette smoking, chronic steroids, and prior surgery
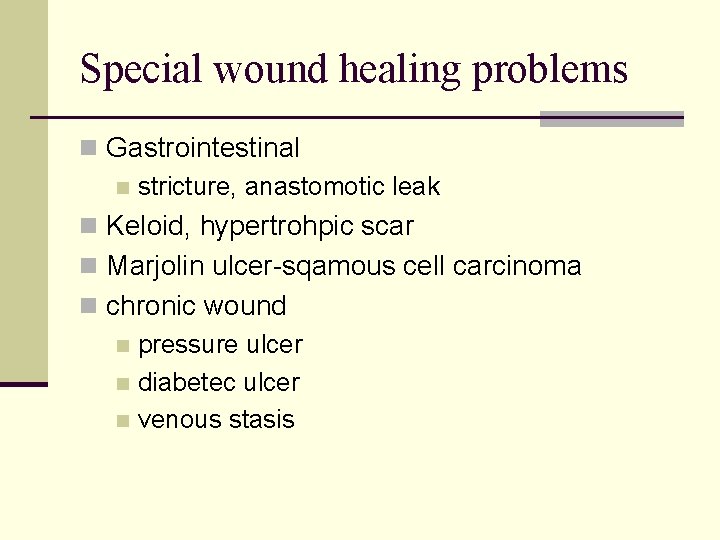
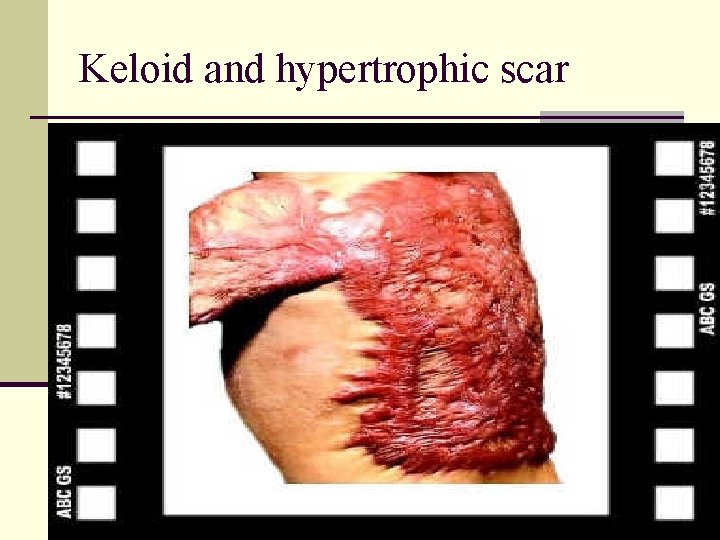
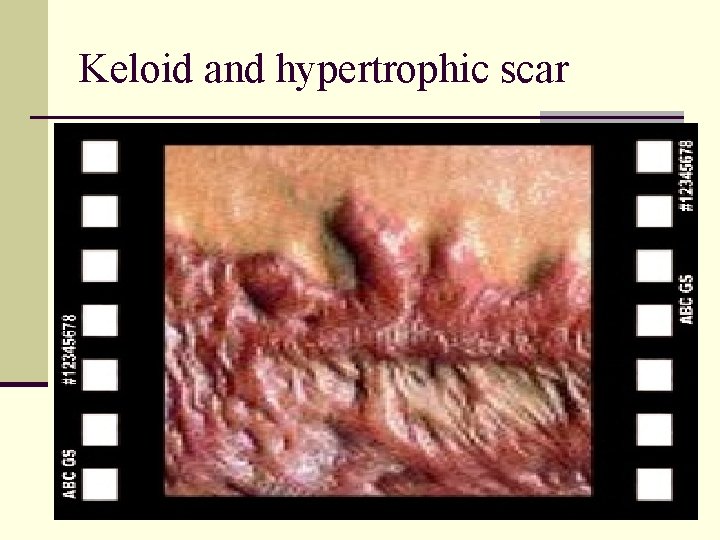
Special wound healing problems n Gastrointestinal n stricture, anastomotic leak n Keloid, hypertrohpic scar n Marjolin ulcer-sqamous cell carcinoma n chronic wound n pressure ulcer n diabetec ulcer n venous stasis
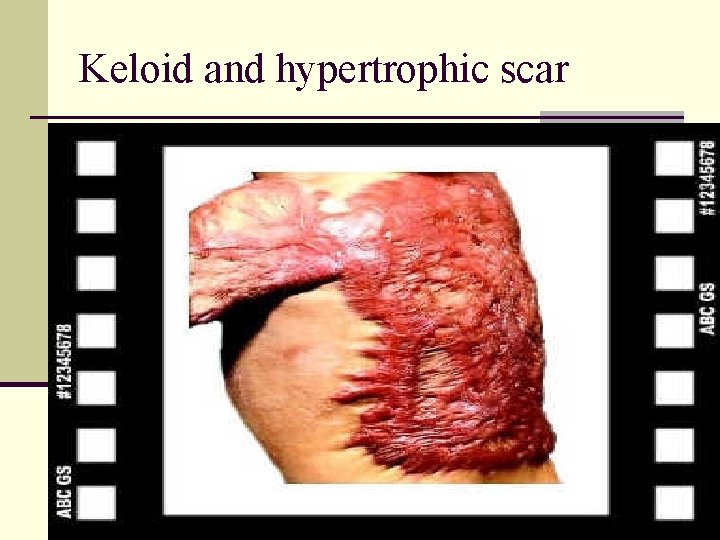
Keloid and hypertrophic scar
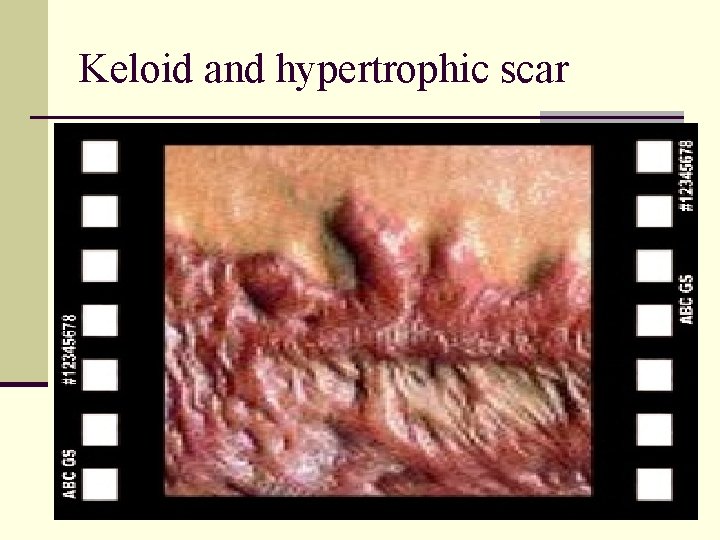
Keloid and hypertrophic scar
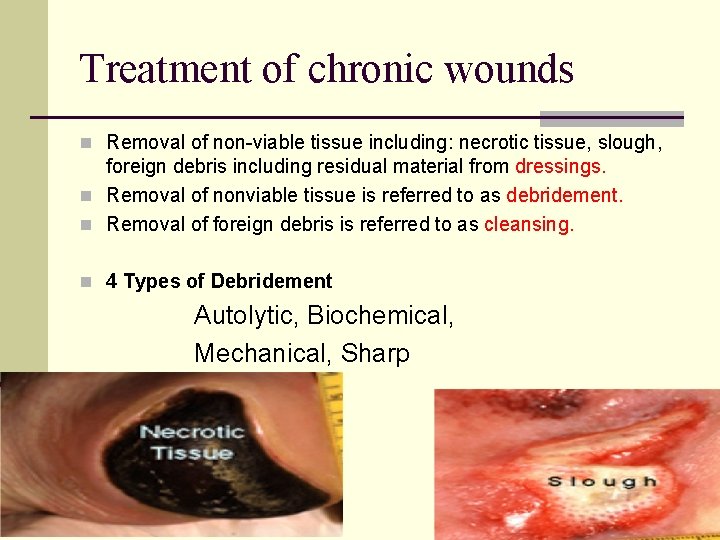
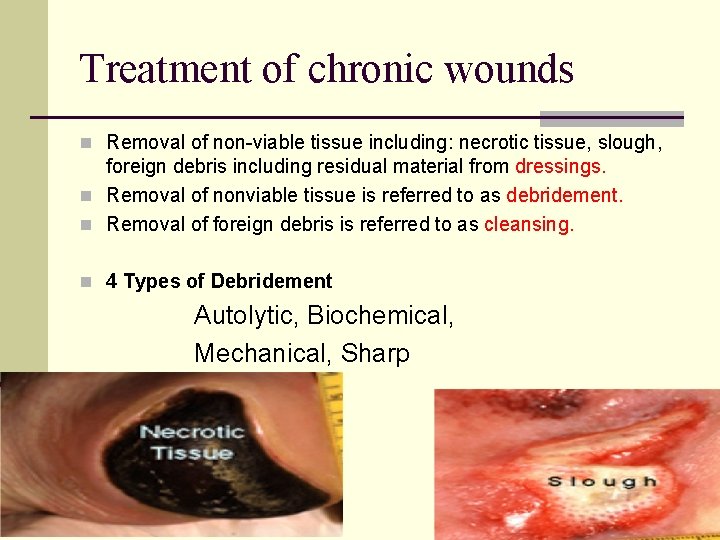
Treatment of chronic wounds n Removal of non-viable tissue including: necrotic tissue, slough, foreign debris including residual material from dressings. n Removal of nonviable tissue is referred to as debridement. n Removal of foreign debris is referred to as cleansing. n 4 Types of Debridement Autolytic, Biochemical, Mechanical, Sharp
Wound etiologies n Arterial n Venous n Diabetic n Trauma n Surgical n Auto-immune n Pressure n Mixed
Chronic wound treatment n Debridement n Cleansing n Maintaining a moist environment n Preventing Further Injury
Debridement n Removal of ALL devitalized tissue n Not the Physical Therapy “Pick and Whittle” n Healthy bleeding tissue introduces beneficial platelets and Growth factors n Allows for thorough investigation of the wound n Remove potentially infected tissue n Obtain appropriate deep cultures
Debridement n Mechanical n Surgical – “Audible Bleeding ? ” n Enzymatic n Autolytic = Hydrogels, hydrocolloids, saline
Is there adequate blood flow to the ulcer? Arterial based wounds n Feel the pulse n Segmental pressures n Doppler examination n Waveforms n Can you examine the microvascular circulation?
Is there adequate blood flow from the ulcer? Venous Stasis Ulcers n Skin discoloration n Hemosiderin deposition n Stasis dermatitis n Lipodermatosclerosis n Loss of hair on the legs n Shiny skin on the tibias
Diabetes multifactorial Increased risk of infection Neuropathy (loss of protective sensation) Vascular effects Macrovascular ( trifurcation disease below the knee ) n Microvascular (affects medial layer to prevent vasodilatation) n Humeral (decreased NO) n n
Infections n Invasion by pathogenic microorganism n Nosocomial n Autoinfection n Virulence n Carriers n Opportunistic bacteria
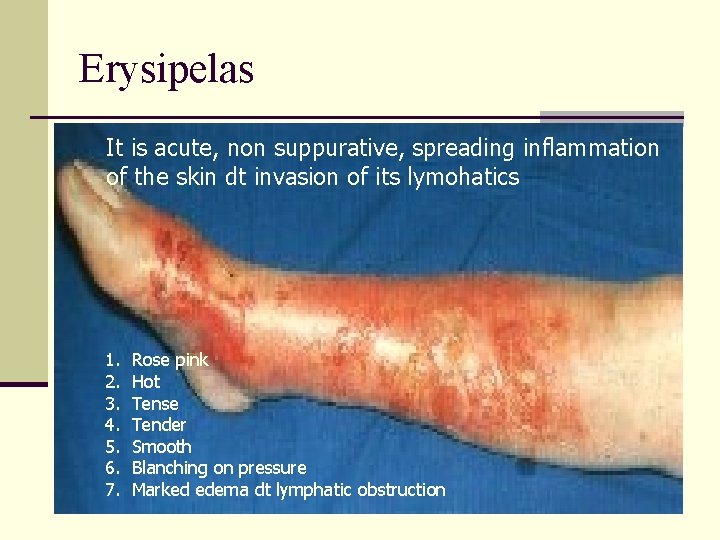
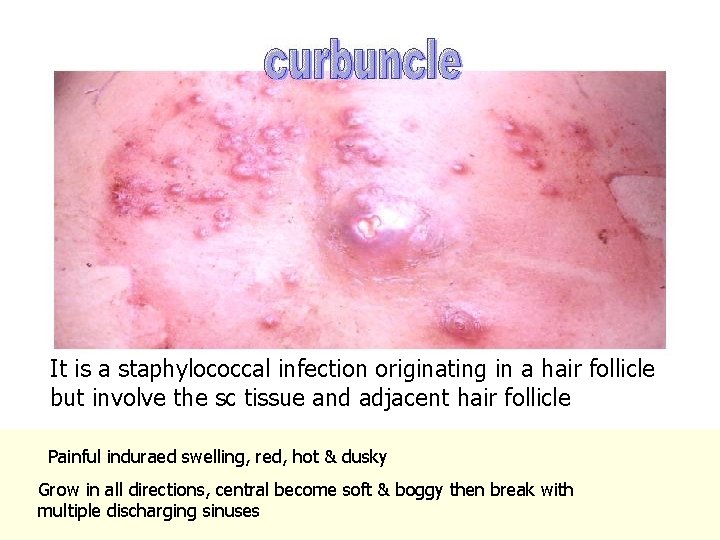
Soft Tissue Infections n n n n cellulitis, intact blood supply Lymphangitis Erysipelas- cellulitis+lymphangitis subcutaneous abscess Impetigo-multiple intraepithelial abscesses Furuncle-sweet glands Carbuncle- subcutaneous tissue n perirectal abscess-fistula at anal crypt n distal phalanx of the finger (felon)
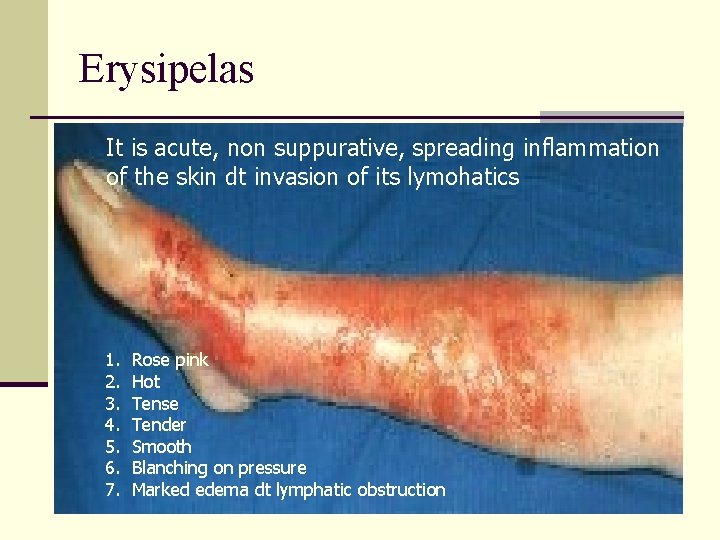
Erysipelas It is acute, non suppurative, spreading inflammation of the skin dt invasion of its lymohatics 1. 2. 3. 4. 5. 6. 7. Rose pink Hot Tense Tender Smooth Blanching on pressure Marked edema dt lymphatic obstruction
Erysipelas n Course n Resolution n Erysipelas migrans n Lymph edema n Gangrene and sloughing n Death n Treatment n Isolation n Rest and elevation n Icthyol or lead subacetate n penicillin
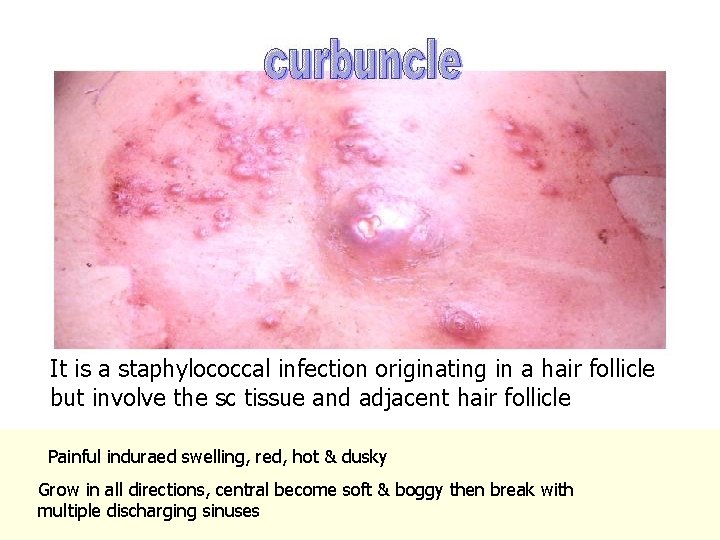
It is a staphylococcal infection originating in a hair follicle but involve the sc tissue and adjacent hair follicle Painful induraed swelling, red, hot & dusky Grow in all directions, central become soft & boggy then break with multiple discharging sinuses
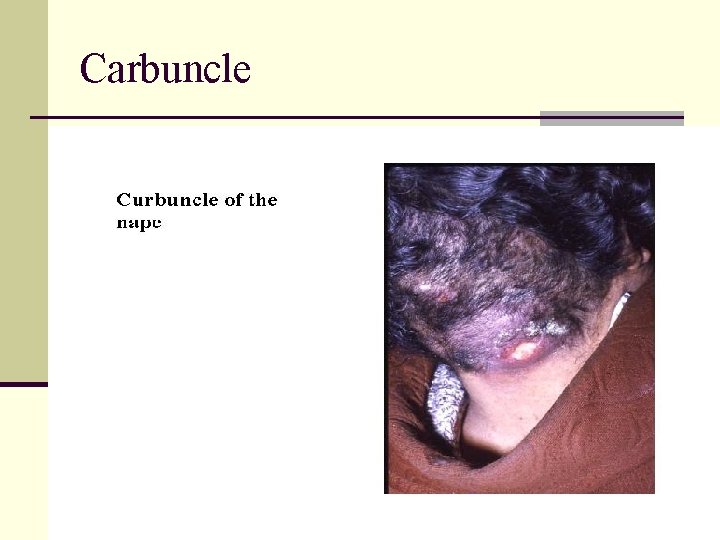
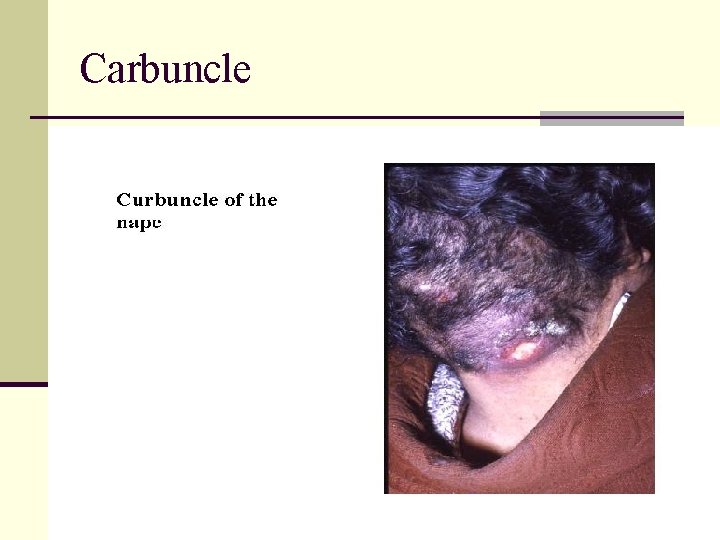
Carbuncle
Gas Gangrene n It is an acute fatal rapidly spreading infection caused by a mixture of gas forming organisms of clostridia group n Predisposing n n n Bad general conditions Local ischemia In-adequte surgical wound care n Clostridial soft tissue include cellulitis and myonecrosis. n n Clostridium perfringens Cl nevyi Cl septicum Cl sordelli
Gas Gangrene Powerful exotoxin n Skin and SC tissue oedematous celluitis with gas that destroy local microcirculation n release RBCs and hemolysis n Early sacchrolytic----- hemolysis--- brick red n Late proteolytic--- H 2 + Fe---- iron sulphide--black color n n Muscles toxins lead to necrosis n Toxins generally
Gas Gangrene ( Clinical picture) n IP = 1 - 3 days n General n Toxemia and prostrtion n Stupor, delirium and death n Local n Brown watery discharge from wound and marked tenderness n Palpable crepitance. n Skin and muscle gangrene early brick red later black n X-rays show GAS
Gas Gangrene ( Clinical Types) 1. Fulminating 2. Massive ( whole limb) 3. Local ( muscle) 4. Gas edema 5. Gas abscess 6. Gas cellulites
Gas Gangrene Prophylaxis n Tetanus immunization n Anti gas gangrene serum 10 cm then 4 cm then 2 cm every 6 hours n Adequate surgical debridement prevents gangrene. n Immediate radical surgical Debridement. n Penicillin in massive doses
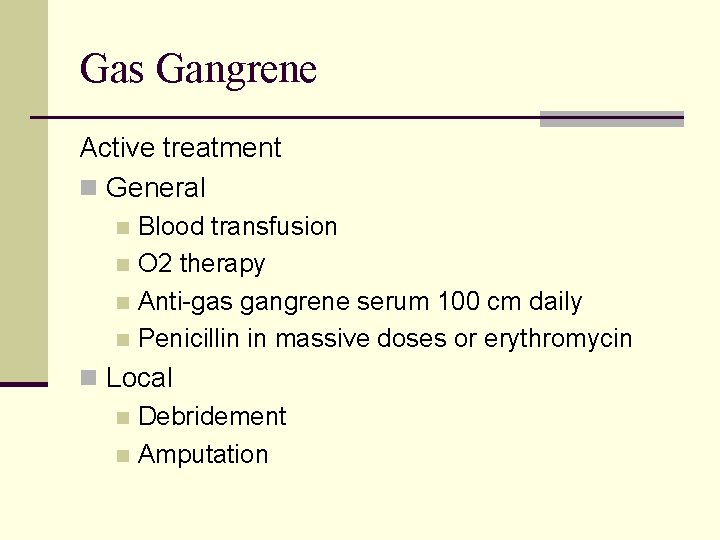
Gas Gangrene Active treatment n General Blood transfusion n O 2 therapy n Anti-gas gangrene serum 100 cm daily n Penicillin in massive doses or erythromycin n n Local n Debridement n Amputation
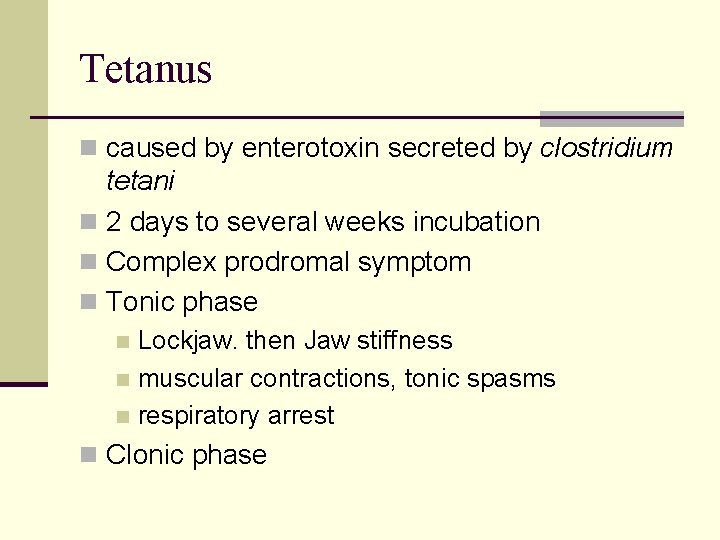
Tetanus n caused by enterotoxin secreted by clostridium tetani n 2 days to several weeks incubation n Complex prodromal symptom n Tonic phase Lockjaw. then Jaw stiffness n muscular contractions, tonic spasms n respiratory arrest n n Clonic phase
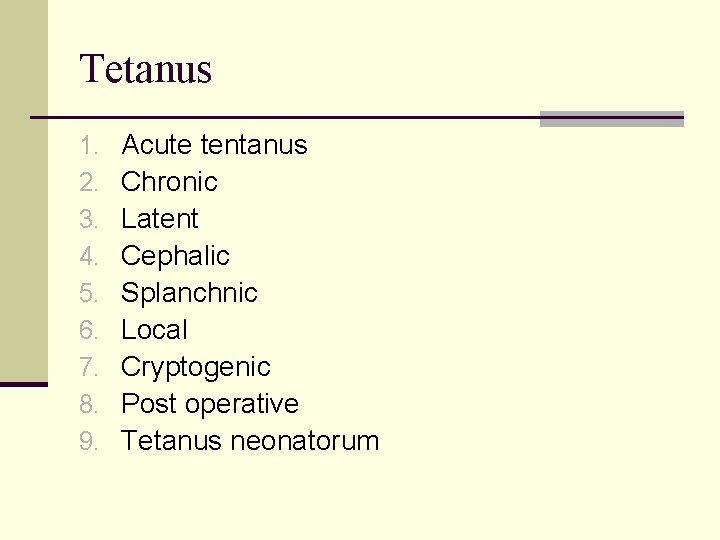
Tetanus 1. 2. 3. 4. 5. 6. 7. 8. 9. Acute tentanus Chronic Latent Cephalic Splanchnic Local Cryptogenic Post operative Tetanus neonatorum
Tetanus (DD) 1. Meningitis 2. Erysipelas 3. Tetany 4. Rabies 5. Strychnine poisoning 6. Local cause of trismus
Tetanus immunotherapy n Adults should receive booster toxoid doses at 10 -year intervals n Who do not have three prior toxoid injectionstetanus diphtheria toxoid (Td) n Tetanus immune globulin (TIG) ATS 1500 unit n ATG 250 IU n
Tetanus (treatment) n Nursing n Anti tetenic serum n ATS n n n 100. 000 u ½ IV and ½ IM 50. 000 U after 7 days ATG one dose only n Penicillin & streptomycin n Wound care n Other measure
Tetanus (treatment) n Stage I n Sedation by luminal or sparine n Stage II n Sedation n NG n Tracheotomy n Stage III n Muscle relaxant as curare 20 – 40 mg IV initial then IM n IPPV n NG tube n Continue till spasm disappear
 For adult
For adult Gottron papula
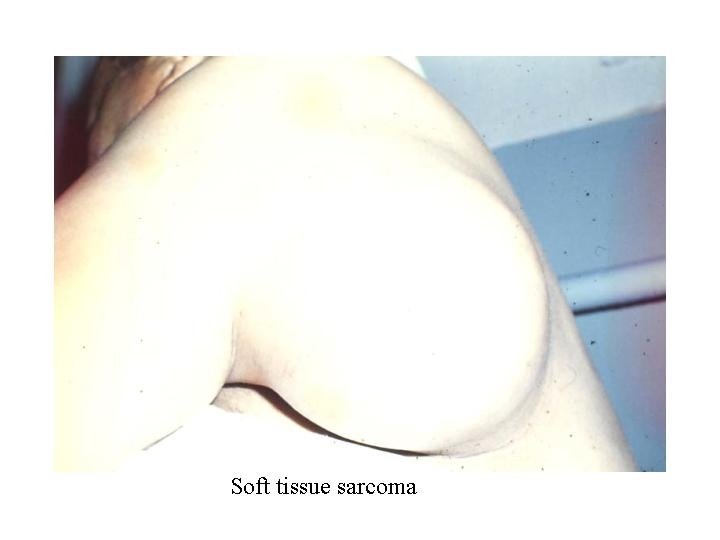
Gottron papula Sarcoma sinovial monofasico
Sarcoma sinovial monofasico Kaposi's sarcoma
Kaposi's sarcoma Leionyosarcoma
Leionyosarcoma Vac ie ewing sarcoma nejm
Vac ie ewing sarcoma nejm Kaposi's sarcoma
Kaposi's sarcoma Kaposi sarcoma herpesvirus
Kaposi sarcoma herpesvirus Sarcoma felino postvacunal
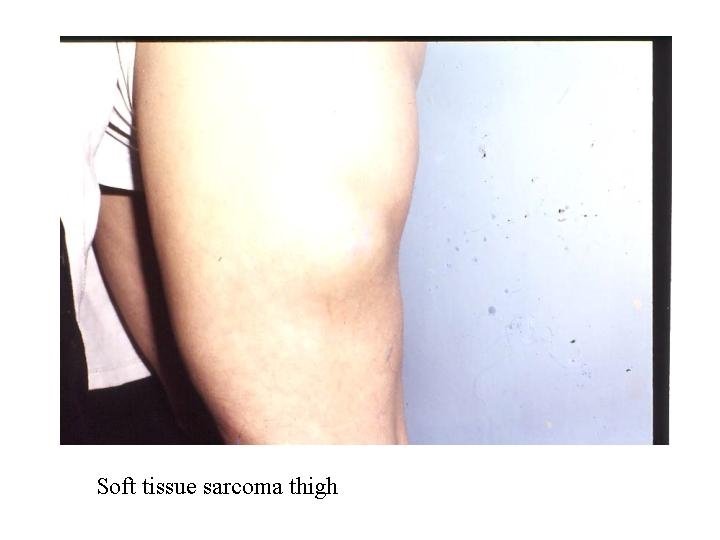
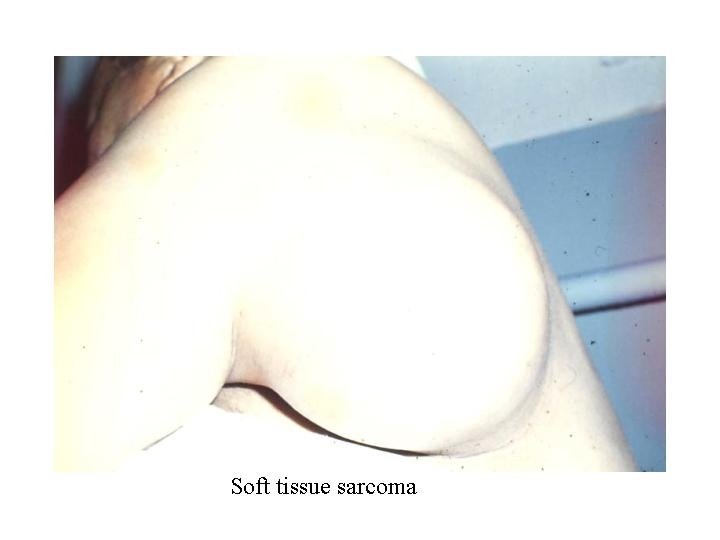
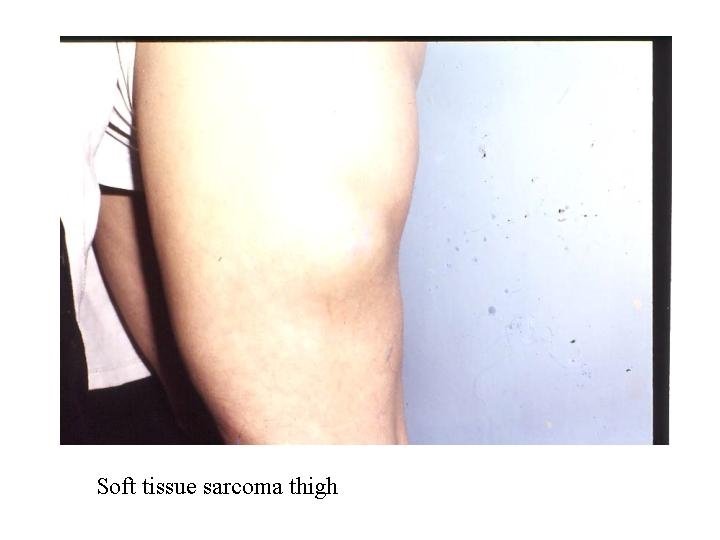
Sarcoma felino postvacunal Thigh sarcoma
Thigh sarcoma Sarcoma epitelioide immagini
Sarcoma epitelioide immagini Open fracture grading
Open fracture grading Safety stand down examples
Safety stand down examples Periarticular soft tissue swelling
Periarticular soft tissue swelling Soft tissue rheumatism
Soft tissue rheumatism Jones and bartlett learning
Jones and bartlett learning Soft tissue rheumatoid arthritis
Soft tissue rheumatoid arthritis Soft tissue hounsfield units
Soft tissue hounsfield units How is aerolar tissue different than aerenchyma tissue?
How is aerolar tissue different than aerenchyma tissue? Somerset safeguarding adults board
Somerset safeguarding adults board Differences between the male and female skeleton
Differences between the male and female skeleton English alphabet for adults
English alphabet for adults Lanugo hair
Lanugo hair For adults formation
For adults formation Mental health and older adults
Mental health and older adults Adults spend about ______% of their sleep in rem sleep.
Adults spend about ______% of their sleep in rem sleep. Office of aging and adults services
Office of aging and adults services Tana brown
Tana brown For adult
For adult Love languages for adults
Love languages for adults Steve nickolaisen
Steve nickolaisen Worcestershire safeguarding adults board
Worcestershire safeguarding adults board Superlative of superiority
Superlative of superiority Hypersecretion of growth hormone in adults
Hypersecretion of growth hormone in adults Idea definition of emotional disturbance
Idea definition of emotional disturbance Clovis unified special education
Clovis unified special education Portsmouth safeguarding
Portsmouth safeguarding Relationship scenarios
Relationship scenarios Self-determination worksheets pdf
Self-determination worksheets pdf Life cycle of enterobius vermicularis
Life cycle of enterobius vermicularis Nonverbal learning disorder symptoms in adults
Nonverbal learning disorder symptoms in adults Dose calculation formula for adults
Dose calculation formula for adults Chester cheetah chewed a chunk of cheap cheddar cheese
Chester cheetah chewed a chunk of cheap cheddar cheese Vital signs normal range for pediatrics
Vital signs normal range for pediatrics Anticipatory guidance for elderly
Anticipatory guidance for elderly Vitals normal ranges
Vitals normal ranges Antihyperglycemic therapy in adults with type 2 diabetes
Antihyperglycemic therapy in adults with type 2 diabetes Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Beverly thomassian
Beverly thomassian Placement of aed pads on adults
Placement of aed pads on adults Bakersfield adults school
Bakersfield adults school Type 1 diabetes in adults diagnosis and management
Type 1 diabetes in adults diagnosis and management Tta adults
Tta adults David howe ent
David howe ent Schistosoma
Schistosoma Renal
Renal Oaas
Oaas 1 inch
1 inch What are aeds
What are aeds Normal adult vital signs
Normal adult vital signs Chest compression for infant 2 rescuer
Chest compression for infant 2 rescuer