SHINE Serving the Health Information Needs of Elders





- Slides: 105
SHINE Serving the Health Information Needs of Elders
Medicare Part A & B “Original Medicare”
Medicare Overview Medicare is a health insurance program for § People 65 years of age and older (not necessarily full retirement age) § People under age 65 with disabilities (deemed “disabled” by Social Security for at least 24 months) § People under age 65 and have ALS or ESRD Note: Medicare is NOT Medicaid (which is health insurance for very low income population)
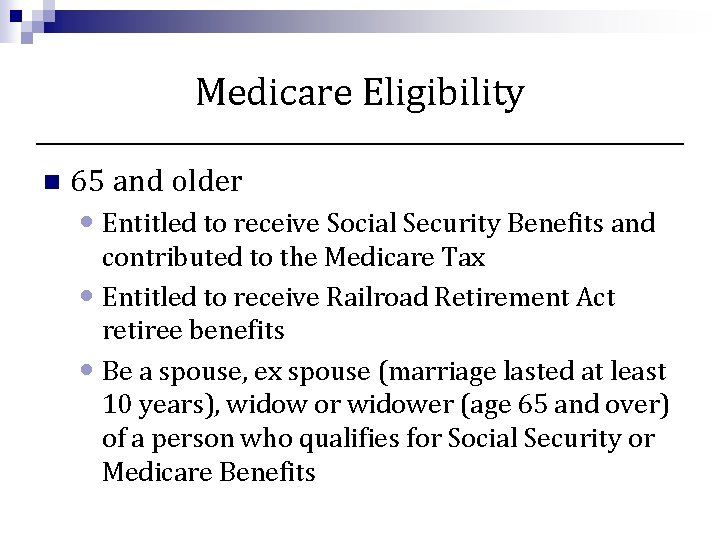
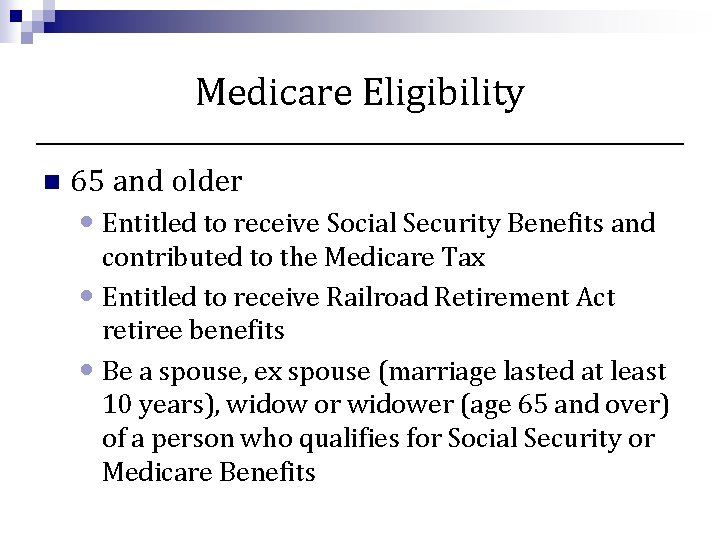
Medicare Eligibility n 65 and older • Entitled to receive Social Security Benefits and contributed to the Medicare Tax • Entitled to receive Railroad Retirement Act retiree benefits • Be a spouse, ex spouse (marriage lasted at least 10 years), widow or widower (age 65 and over) of a person who qualifies for Social Security or Medicare Benefits
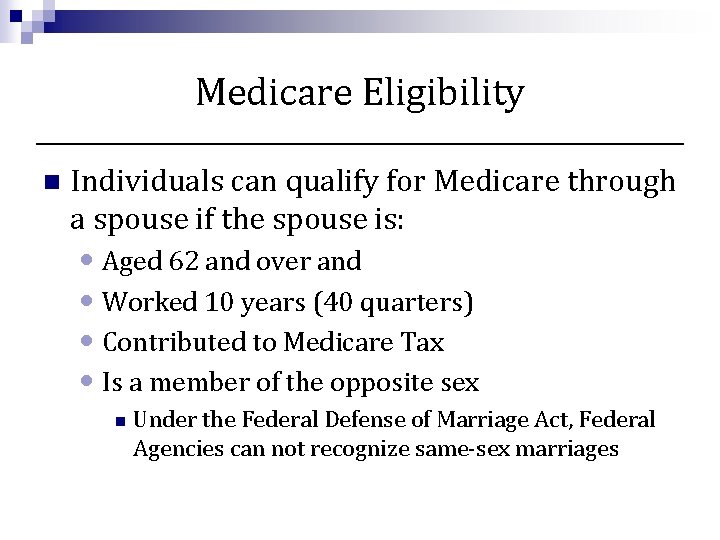
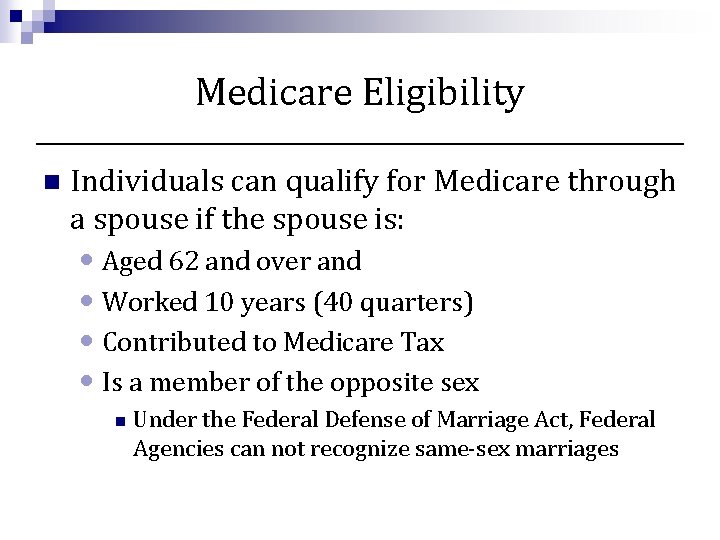
Medicare Eligibility n Individuals can qualify for Medicare through a spouse if the spouse is: • Aged 62 and over and • Worked 10 years (40 quarters) • Contributed to Medicare Tax • Is a member of the opposite sex n Under the Federal Defense of Marriage Act, Federal Agencies can not recognize same-sex marriages
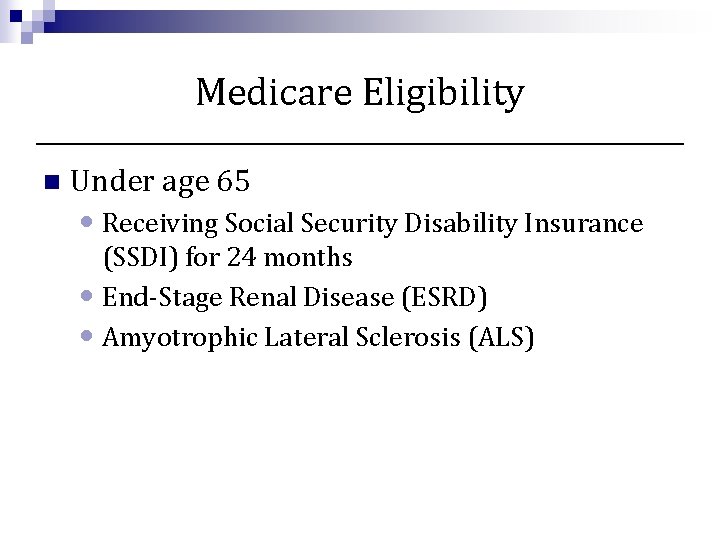
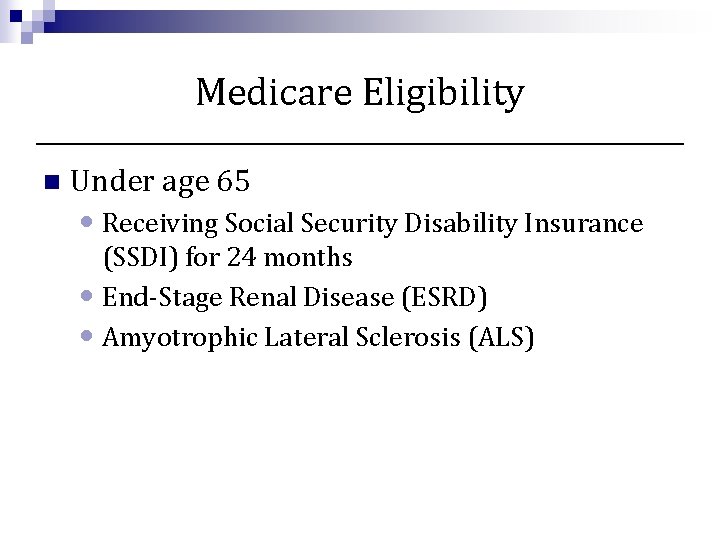
Medicare Eligibility n Under age 65 • Receiving Social Security Disability Insurance (SSDI) for 24 months • End-Stage Renal Disease (ESRD) • Amyotrophic Lateral Sclerosis (ALS)
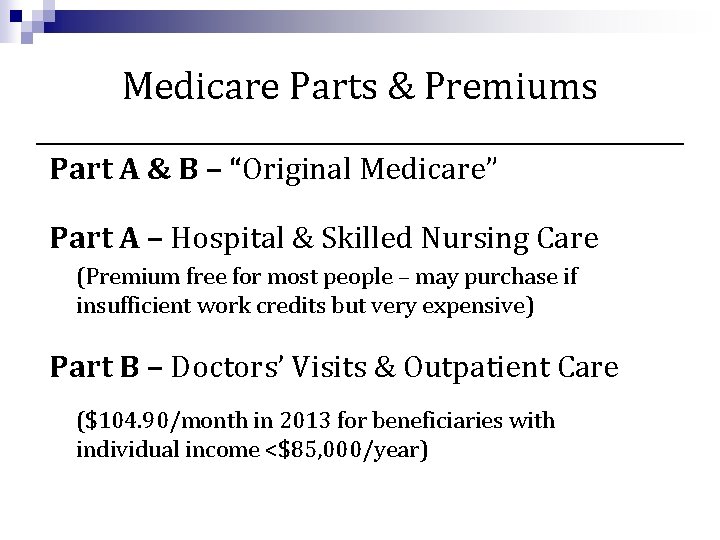
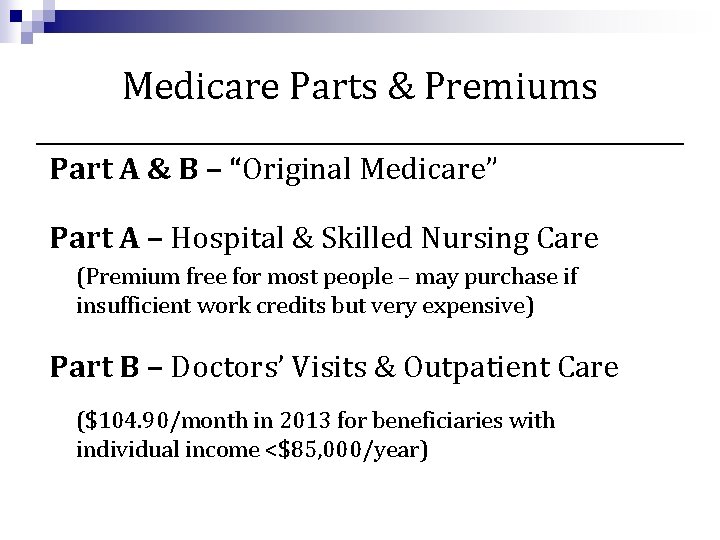
Medicare Parts & Premiums Part A & B – “Original Medicare” Part A – Hospital & Skilled Nursing Care (Premium free for most people – may purchase if insufficient work credits but very expensive) Part B – Doctors’ Visits & Outpatient Care ($104. 90/month in 2013 for beneficiaries with individual income <$85, 000/year)
Medicare Agencies n Beneficiaries must enroll through Social Security Administration (SSA) for Medicare Benefits • If already receiving Social Security before turning 65, enrollment into Part A and Part B is automatic • If not already receiving Social Security benefits an individual must contact Social Security (in-person, online, or phone) to enroll into Medicare n n n Initial Enrollment Period is the 3 months before, the month of, and 3 months after, an individuals 65 th birthday. May delay enrolling into Social Security Benefits Medicare is administered by The Centers for Medicare & Medicaid Services (CMS)
Delayed Enrollment n May enroll into Medicare Part A at anytime once eligible • Most people enroll in Part A when they turn 65 since it is usually premium free n. Special Enrollment Period for Part B • People may delay enrollment without penalty if covered through active employment by themselves or spouse* n. Will have a 8 month Special Enrollment Period when active employment ends otherwise may have to pay a penalty. n. COBRA does not qualify as “active” employment and does NOT protect an individual from the Part B late enrollment penalty *DOMA excludes Medicare from recognizing same-sex spouses
Delayed Enrollment n. General Enrollment Period for Part B • January 1 – March 31 • Coverage effective July 1 n. Part B Penalty for delayed enrollment • increased premium of 10% for each 12 months of delayed enrollment • Lifetime • Increases with increases in premium
Medicare Part A n Part A helps cover: • Inpatient care in hospitals • Inpatient care in a skilled nursing facility • Hospice care services • Home health care services Medicare does NOT cover Long Term Care
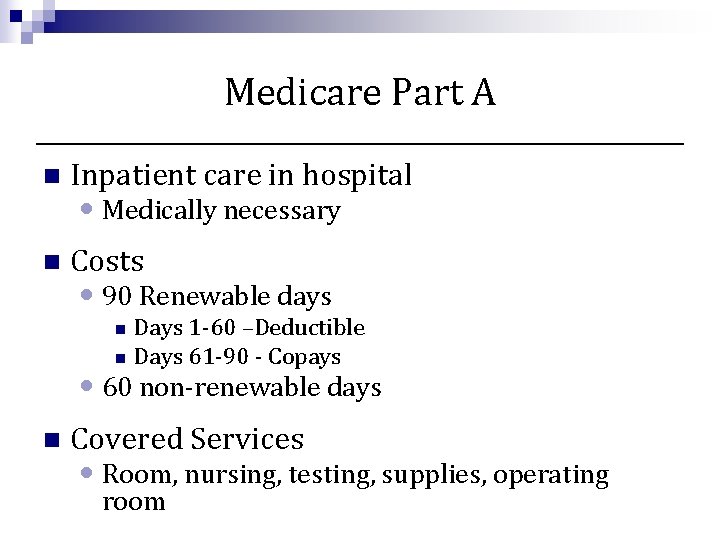
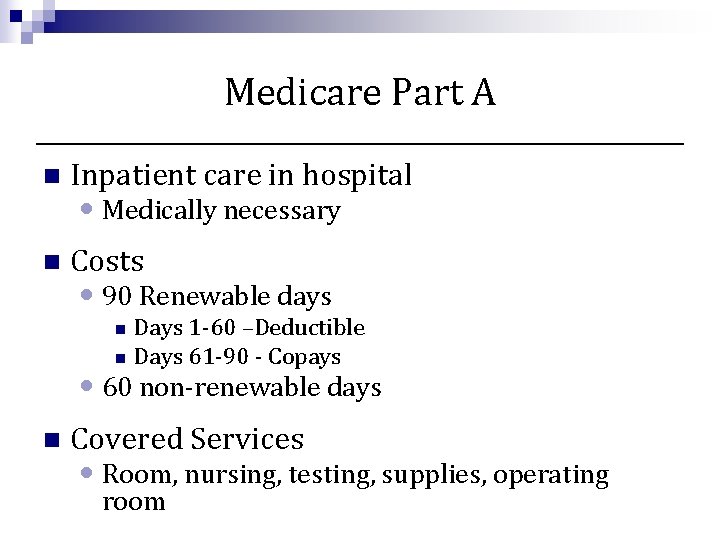
Medicare Part A n Inpatient care in hospital n Costs • Medically necessary • 90 Renewable days Days 1 -60 –Deductible n Days 61 -90 - Copays n • 60 non-renewable days n Covered Services • Room, nursing, testing, supplies, operating room
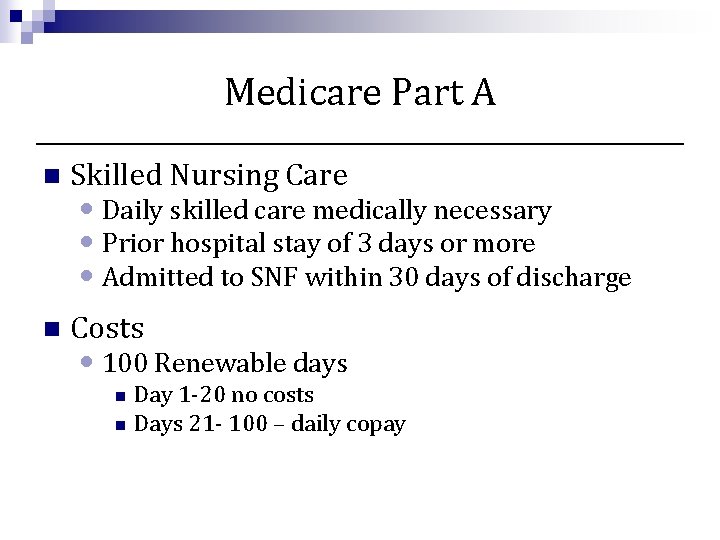
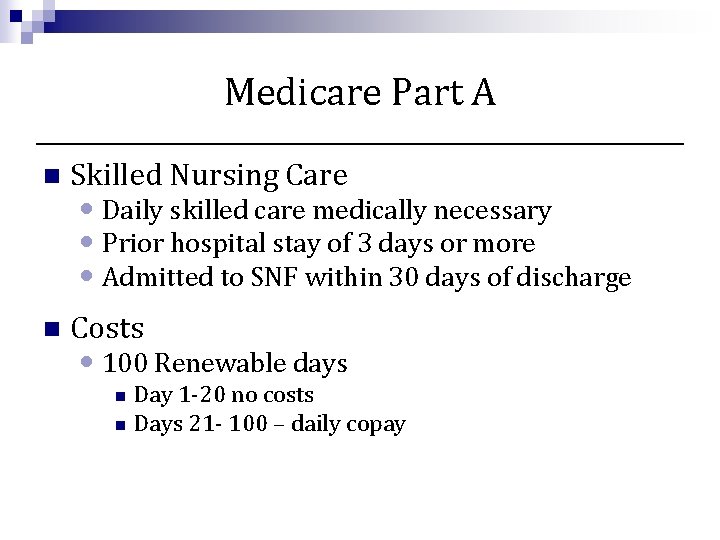
Medicare Part A n Skilled Nursing Care n Costs • Daily skilled care medically necessary • Prior hospital stay of 3 days or more • Admitted to SNF within 30 days of discharge • 100 Renewable days Day 1 -20 no costs n Days 21 - 100 – daily copay n
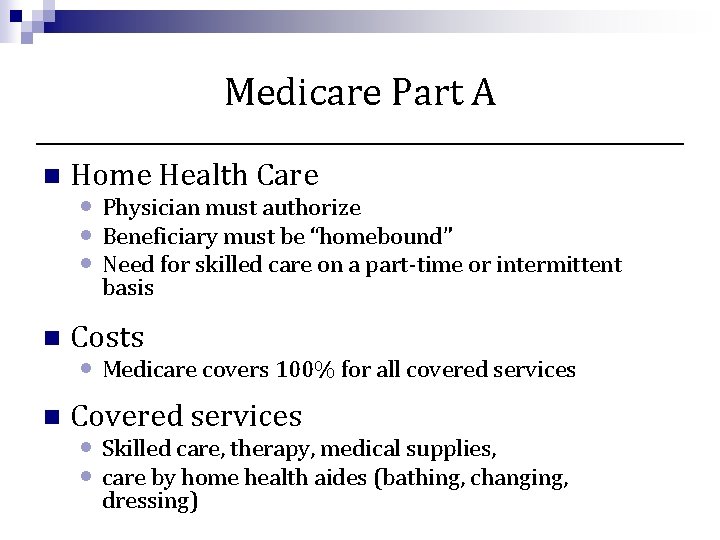
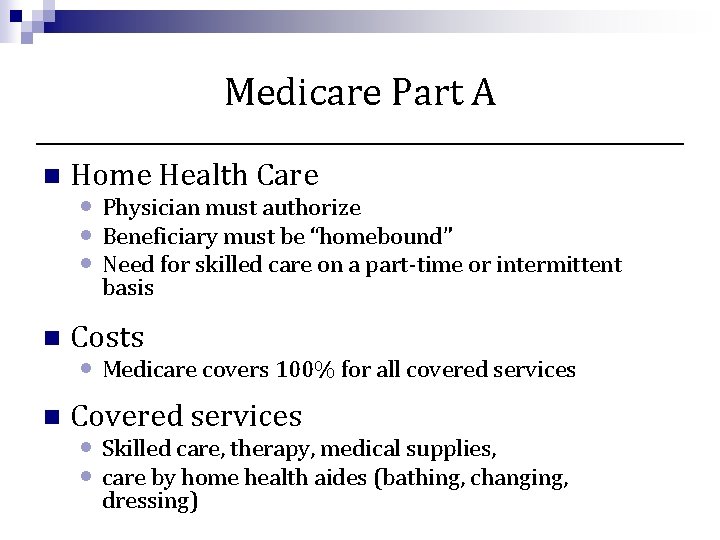
Medicare Part A n Home Health Care • Physician must authorize • Beneficiary must be “homebound” • Need for skilled care on a part-time or intermittent basis n Costs • Medicare covers 100% for all covered services n Covered services • Skilled care, therapy, medical supplies, • care by home health aides (bathing, changing, dressing)
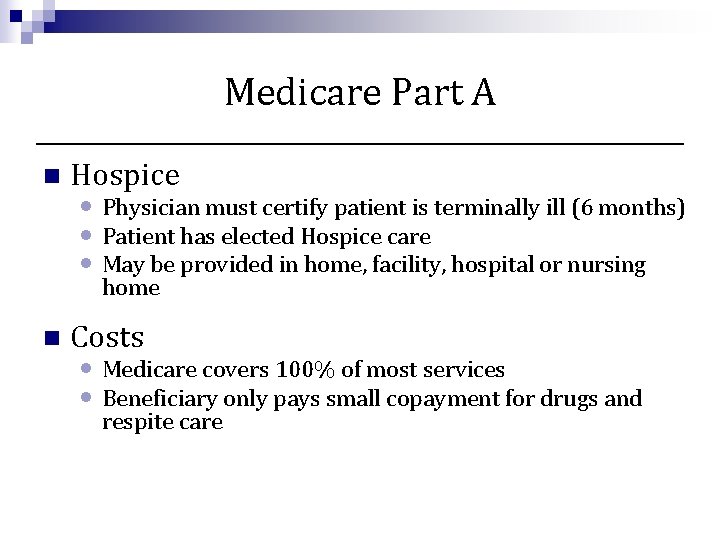
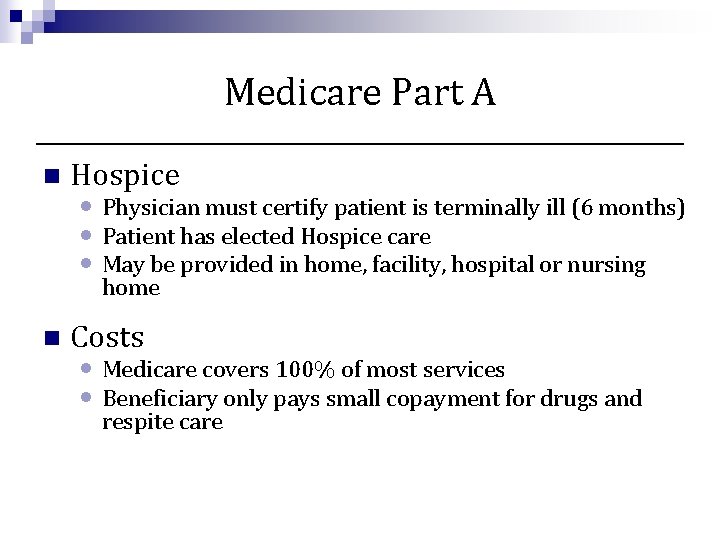
Medicare Part A n Hospice • Physician must certify patient is terminally ill (6 months) • Patient has elected Hospice care • May be provided in home, facility, hospital or nursing home n Costs • Medicare covers 100% of most services • Beneficiary only pays small copayment for drugs and respite care
Medicare Part B n Part B helps cover: • Physician services • Out-patient hospital services • Preventive services • Medical Equipment and Supplies • Ambulance • Medically-necessary services n Services or supplies that are needed to diagnose to treat your medical condition
Medicare Part B - Preventive Benefits n ACA provides access to many free preventive benefits • Mammograms • Some pap smear and pelvic exams • Colorectal Screenings • Diabetes Self-Management Training/Tests • Bone Mass Measurements • Prostate Cancer Screening • Depression screening • Obesity screening and counseling • Alcohol misuse screening and counseling • Annual Wellness Visit n n n Update individual’s medical & family history Record height, weight, body mass index, blood pressure and other routine measurements Provide personal health advice and coordinate appropriate referrals and health education
Medicare Part B - Preventive Benefits n Most preventive services are not subject to • Deductible • 20% copayments n Free Annual Wellness Visit • NOT a physical exam • Services provided beyond scope of AWV may be subject to deductible and/or copayments
Medicare Part B n Physician services • No network or referral needed • After annual deductible, 20% copayment Medicare approved amount n Accepting Assignment – accepting the Medicare approved amount as payment in full n n Ban on balance billing n In other states there an excess charges of 15% is allowable for physicians not accepting assignment
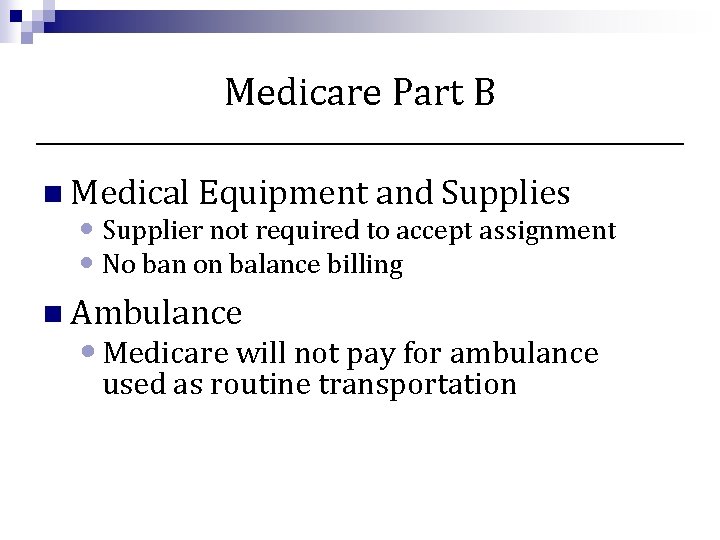
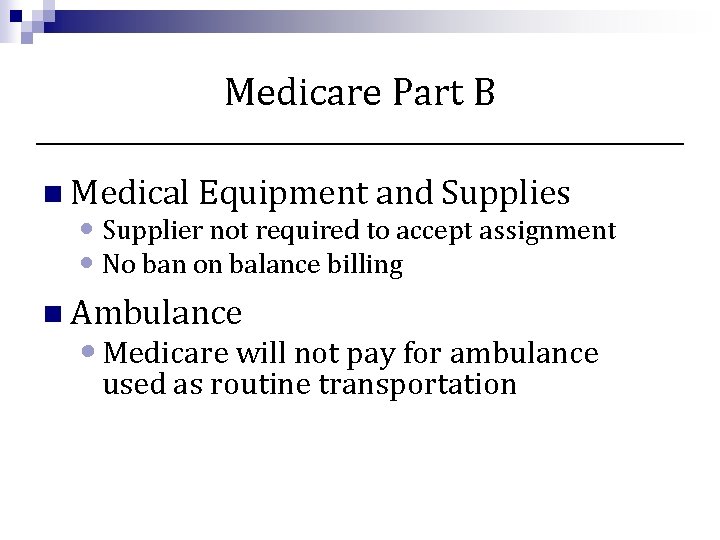
Medicare Part B n Medical Equipment and Supplies • Supplier not required to accept assignment • No ban on balance billing n Ambulance • Medicare will not pay for ambulance used as routine transportation
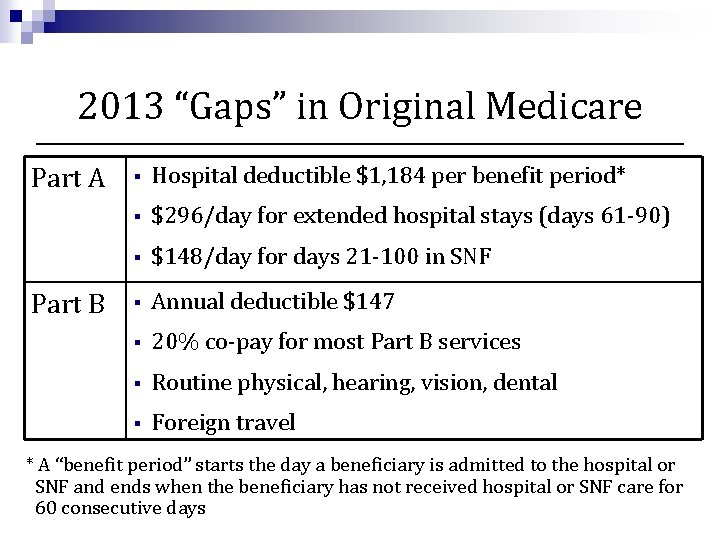
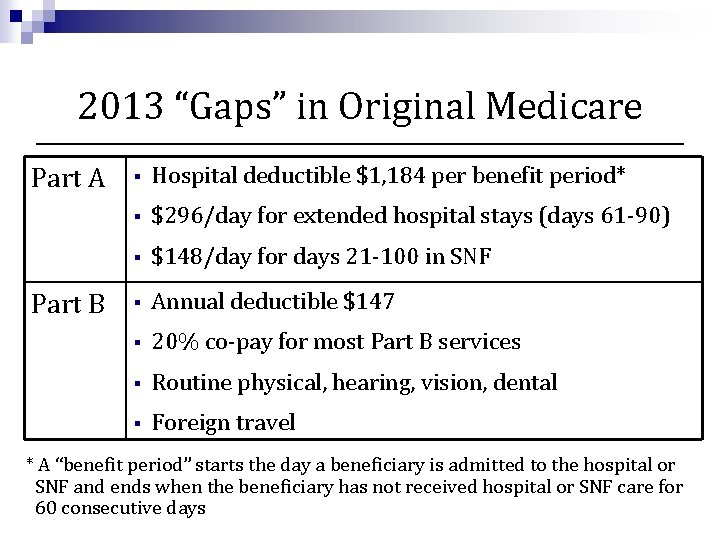
2013 “Gaps” in Original Medicare Part A Part B § Hospital deductible $1, 184 per benefit period* § $296/day for extended hospital stays (days 61 -90) § $148/day for days 21 -100 in SNF § Annual deductible $147 § 20% co-pay for most Part B services § Routine physical, hearing, vision, dental § Foreign travel * A “benefit period” starts the day a beneficiary is admitted to the hospital or SNF and ends when the beneficiary has not received hospital or SNF care for 60 consecutive days

Medicare Part C (Medicare Advantage Plans) & Medigap Plans
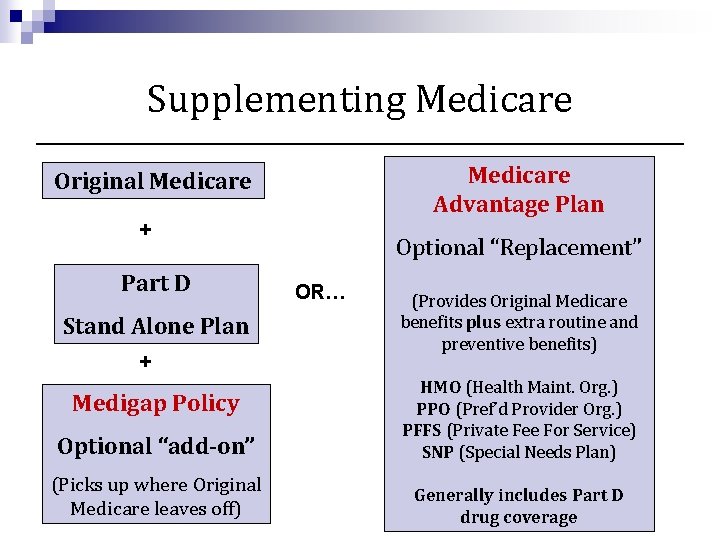
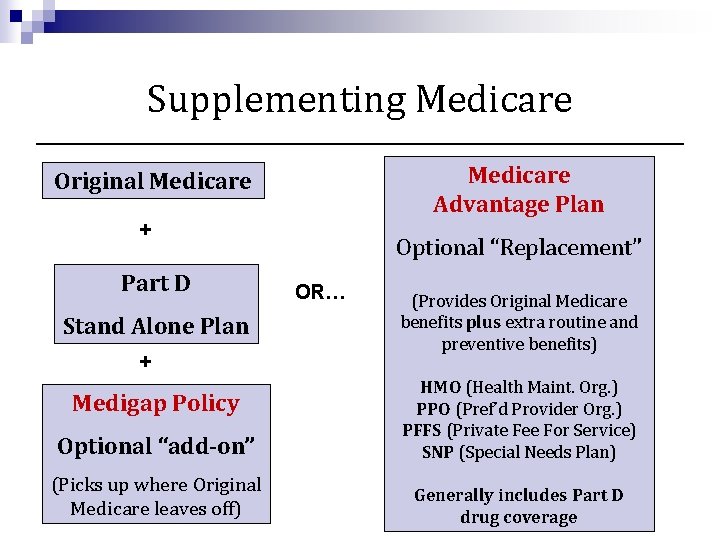
Supplementing Medicare Advantage Plan Original Medicare + Part D Stand Alone Plan + Optional “Replacement” OR… (Provides Original Medicare benefits plus extra routine and preventive benefits) Optional “add-on” HMO (Health Maint. Org. ) PPO (Pref’d Provider Org. ) PFFS (Private Fee For Service) SNP (Special Needs Plan) (Picks up where Original Medicare leaves off) Generally includes Part D drug coverage Medigap Policy
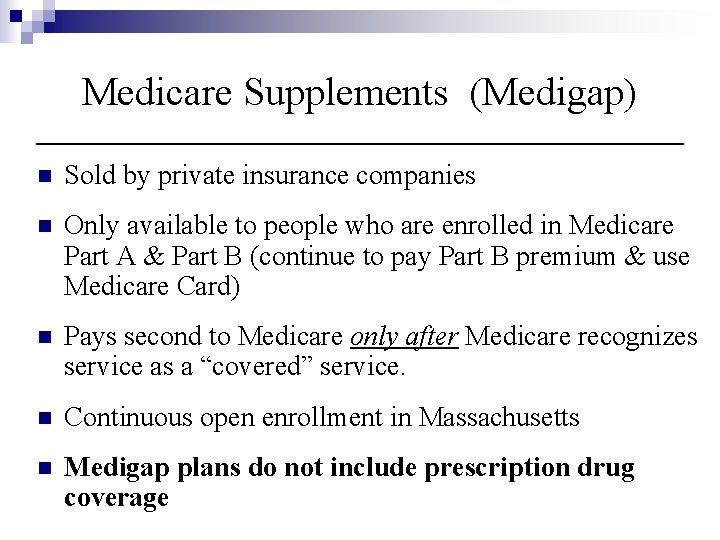
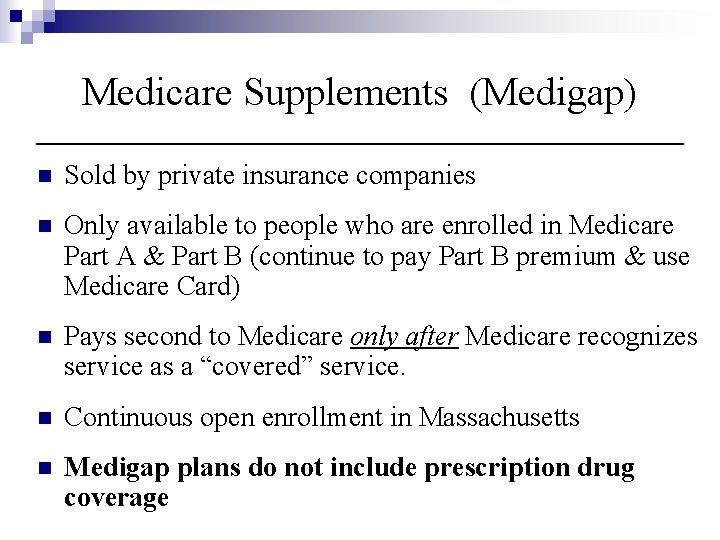
Medicare Supplements (Medigap) n Sold by private insurance companies n Only available to people who are enrolled in Medicare Part A & Part B (continue to pay Part B premium & use Medicare Card) n Pays second to Medicare only after Medicare recognizes service as a “covered” service. n Continuous open enrollment in Massachusetts n Medigap plans do not include prescription drug coverage
Medigap Plans § Two Medigap Plans Sold in Massachusetts § Core - leaves some gaps behind (including hospital deductible & SNF co-pays), but costs less § Supplement 1 - covers all gaps – but costs more § Both plans allow members to choose their own doctors, specialists, and hospitals without referrals NOTE: Some people are covered through older policies no longer available to new members (e. g. “Medex Gold”)

Medigap Plans in 2013 Medigap Carriers Medicare Supplement Core Medicare Supplement 1 Blue. Cross Blue. Shield of Mass $96. 38 $183. 73 Fallon $100. 25 $182. 00 Harvard Pilgrim Health Care $100. 50 $189. 50 Health New England $97. 00 $189. 00 Humana $137. 18 $214. 41 Tufts $102. 71 $199. 70 United Health. Care $122. 75 $211. 50
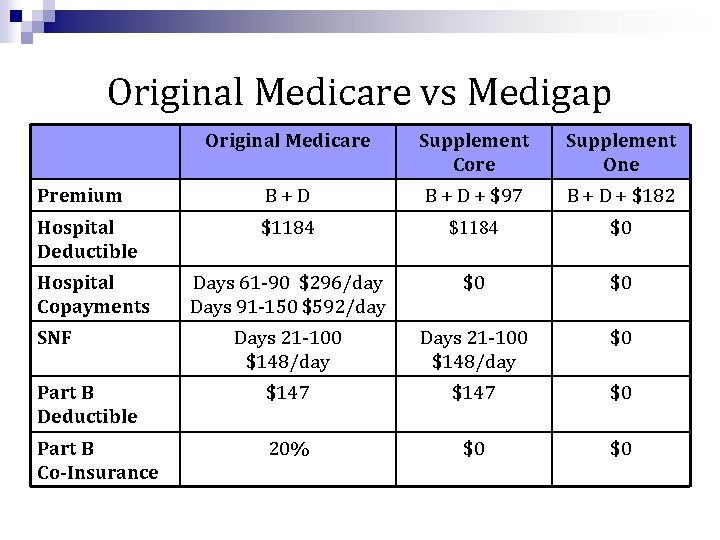
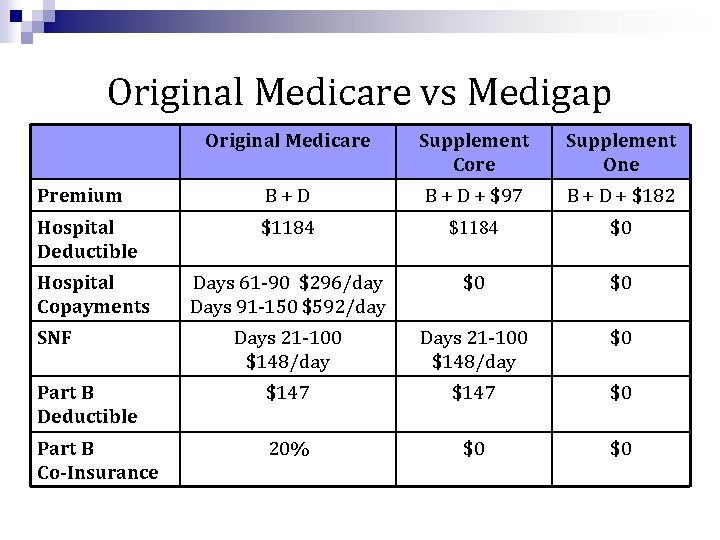
Original Medicare vs Medigap Original Medicare Supplement Core Supplement One Premium B+D B + D + $97 B + D + $182 Hospital Deductible $1184 $0 Days 61 -90 $296/day Days 91 -150 $592/day $0 $0 Days 21 -100 $148/day $0 Part B Deductible $147 $0 Part B Co-Insurance 20% $0 $0 Hospital Copayments SNF
Medigap Plans § No matter which company a beneficiary selects for coverage they will receive the same benefits § Some Medigap plans offer a discount of up to 15% to beneficiaries who enroll within 6 months of their Medicare Enrollment. § If an individual switches Medigap companies he or she must notify the previous company. § If an individual leaves a plan that is no longer sold they will be unable to return to that plan.
Medicare Advantage Plans (Medicare Part C) n Private plans contract with Medicare to provide coverage comparable to “Original” Medicare n Plans may additional benefits (e. g. dental check ups, vision screening, eye glasses, hearing aids) n Plans usually charge additional premium & co-pays n Members must still pay Part B premium n Plans use networks of physicians
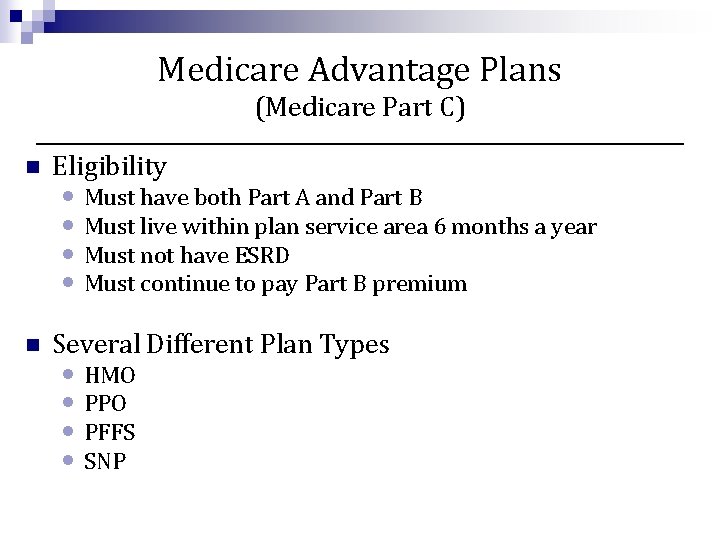
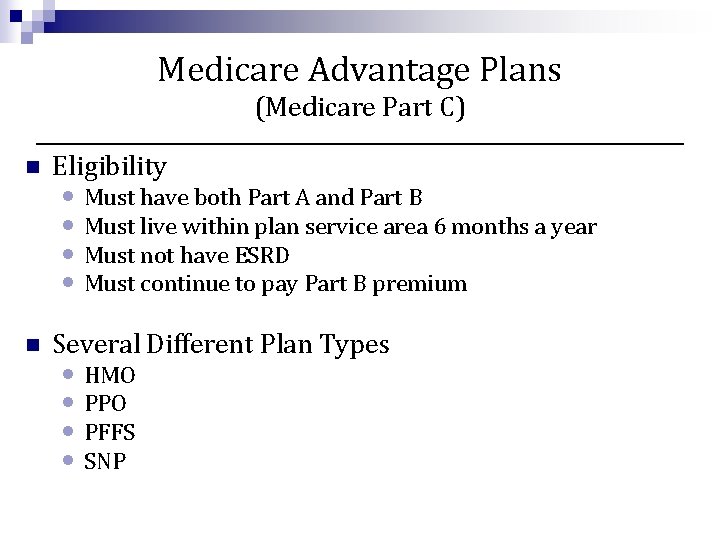
Medicare Advantage Plans (Medicare Part C) n Eligibility n Several Different Plan Types • Must have both Part A and Part B • Must live within plan service area 6 months a year • Must not have ESRD • Must continue to pay Part B premium • HMO • PPO • PFFS • SNP
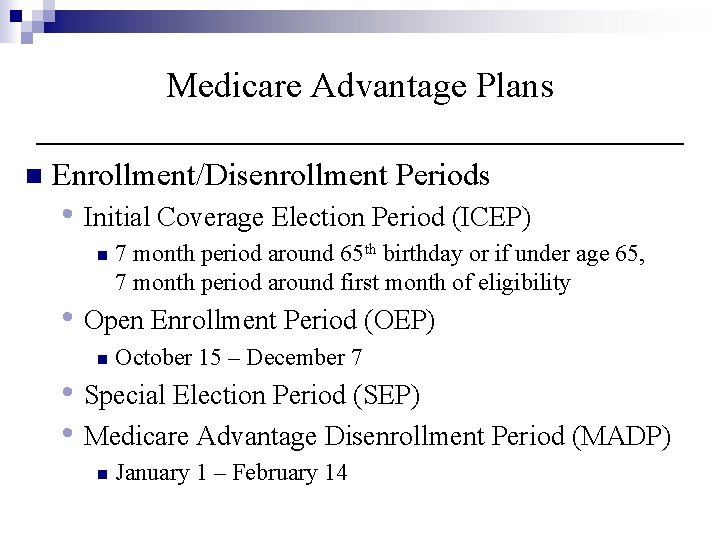
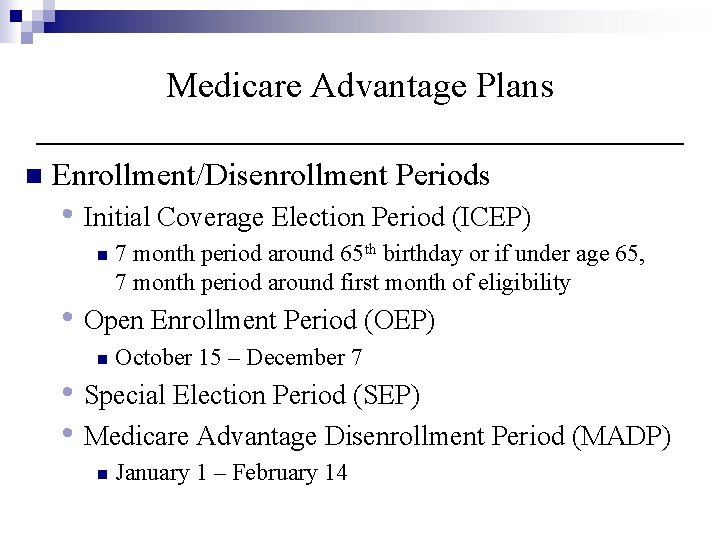
Medicare Advantage Plans n Enrollment/Disenrollment Periods • Initial Coverage Election Period (ICEP) n 7 month period around 65 th birthday or if under age 65, 7 month period around first month of eligibility • Open Enrollment Period (OEP) n October 15 – December 7 • Special Election Period (SEP) • Medicare Advantage Disenrollment Period (MADP) n January 1 – February 14
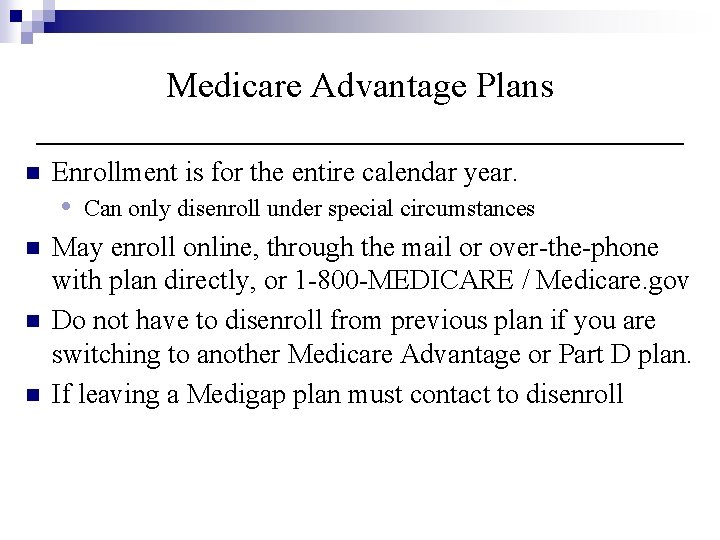
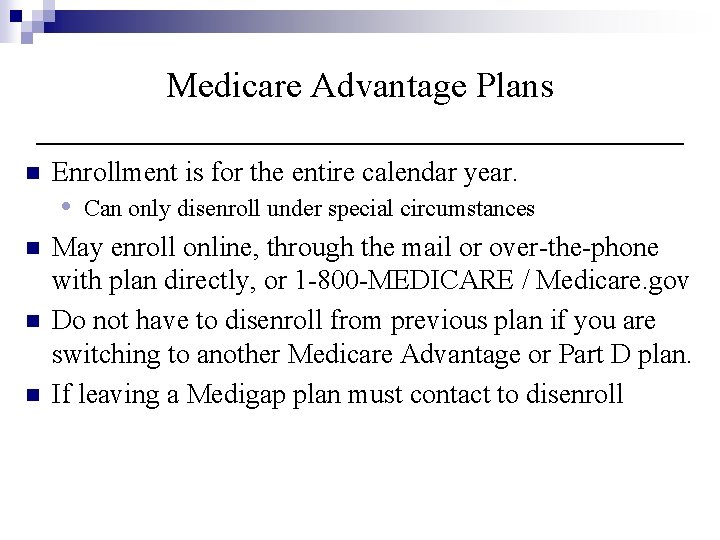
Medicare Advantage Plans n Enrollment is for the entire calendar year. • n n n Can only disenroll under special circumstances May enroll online, through the mail or over-the-phone with plan directly, or 1 -800 -MEDICARE / Medicare. gov Do not have to disenroll from previous plan if you are switching to another Medicare Advantage or Part D plan. If leaving a Medigap plan must contact to disenroll
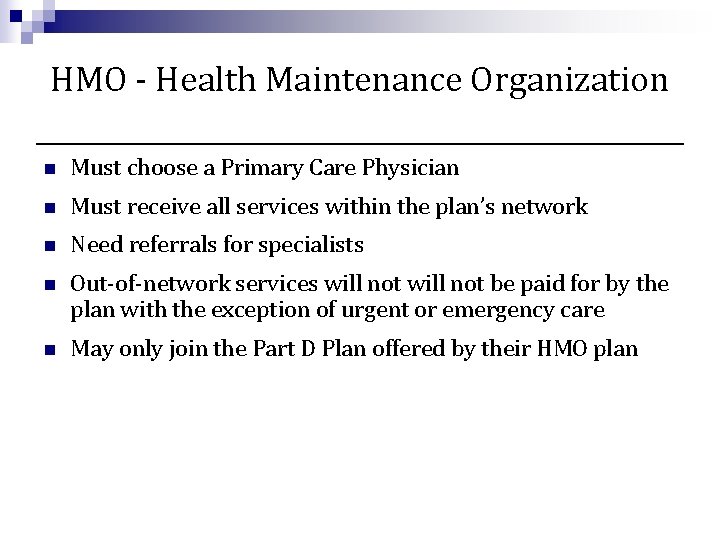
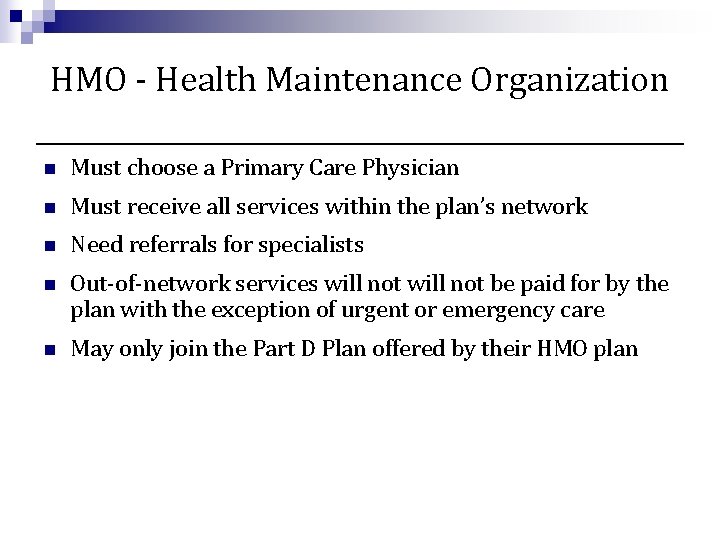
HMO - Health Maintenance Organization n Must choose a Primary Care Physician n Must receive all services within the plan’s network n Need referrals for specialists n Out-of-network services will not be paid for by the plan with the exception of urgent or emergency care n May only join the Part D Plan offered by their HMO plan
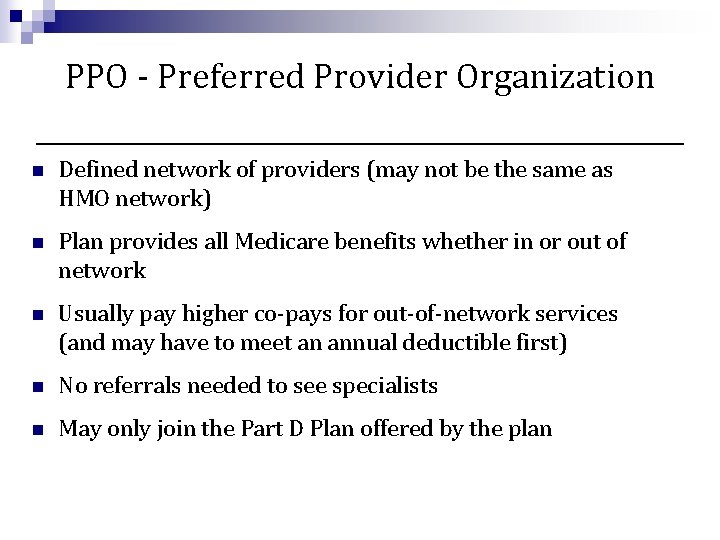
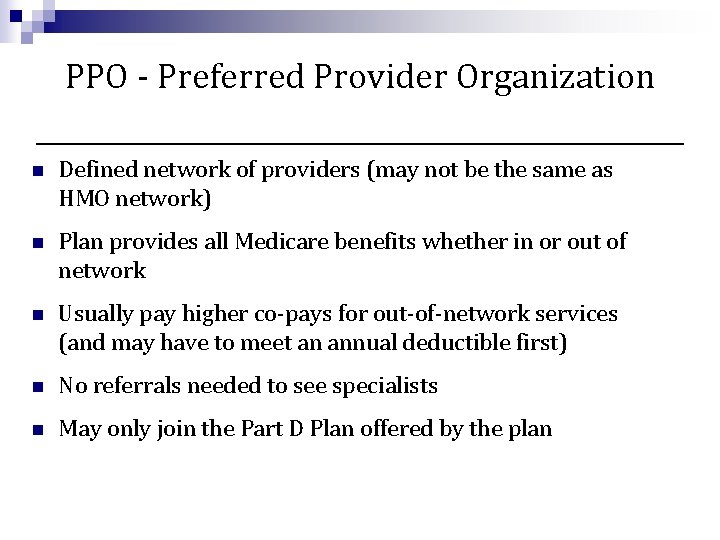
PPO - Preferred Provider Organization n Defined network of providers (may not be the same as HMO network) n Plan provides all Medicare benefits whether in or out of network n Usually pay higher co-pays for out-of-network services (and may have to meet an annual deductible first) n No referrals needed to see specialists n May only join the Part D Plan offered by the plan
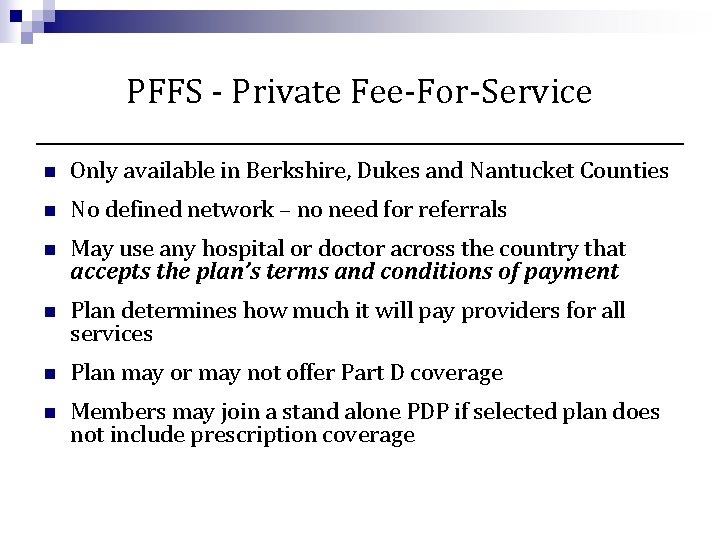
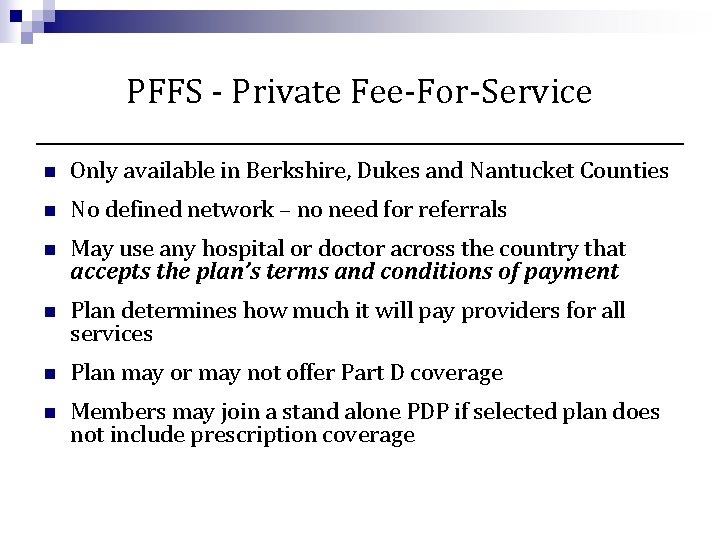
PFFS - Private Fee-For-Service n Only available in Berkshire, Dukes and Nantucket Counties n No defined network – no need for referrals n May use any hospital or doctor across the country that accepts the plan’s terms and conditions of payment n Plan determines how much it will pay providers for all services n Plan may or may not offer Part D coverage n Members may join a stand alone PDP if selected plan does not include prescription coverage
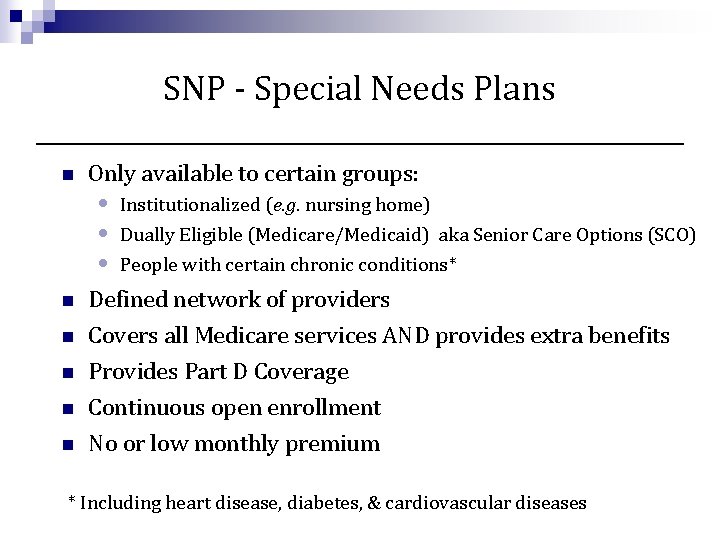
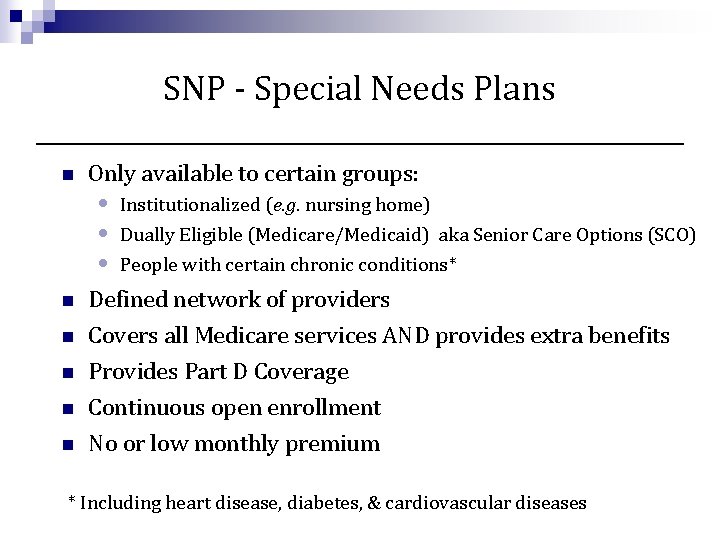
SNP - Special Needs Plans n Only available to certain groups: • • • n n n Institutionalized (e. g. nursing home) Dually Eligible (Medicare/Medicaid) aka Senior Care Options (SCO) People with certain chronic conditions* Defined network of providers Covers all Medicare services AND provides extra benefits Provides Part D Coverage Continuous open enrollment No or low monthly premium * Including heart disease, diabetes, & cardiovascular diseases
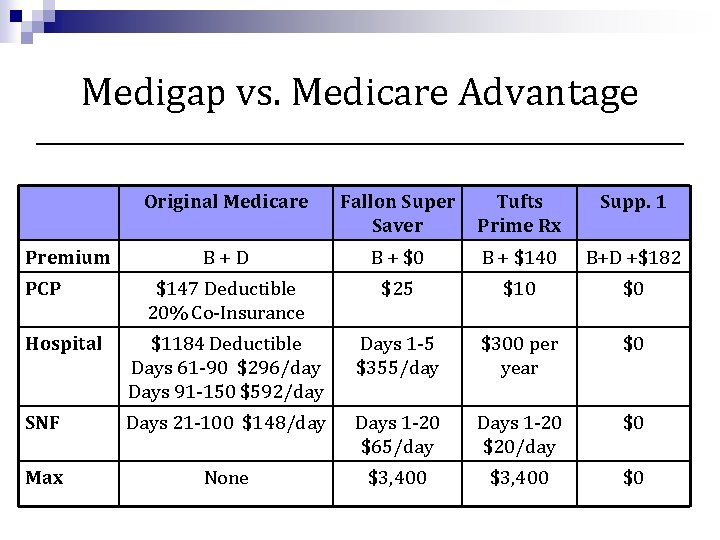
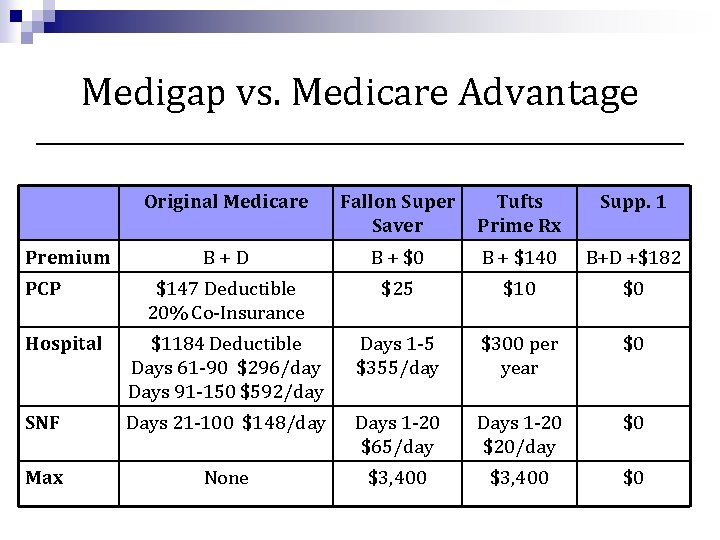
Medigap vs. Medicare Advantage Original Medicare Fallon Super Saver Tufts Prime Rx Supp. 1 B+D B + $0 B + $140 B+D +$182 $147 Deductible 20% Co-Insurance $25 $10 $0 Hospital $1184 Deductible Days 61 -90 $296/day Days 91 -150 $592/day Days 1 -5 $355/day $300 per year $0 SNF Days 21 -100 $148/day Days 1 -20 $65/day Days 1 -20 $20/day $0 Max None $3, 400 $0 Premium PCP
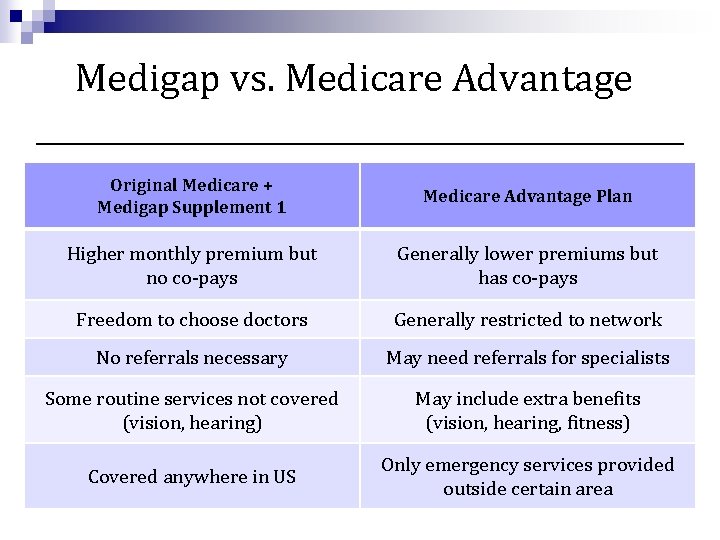
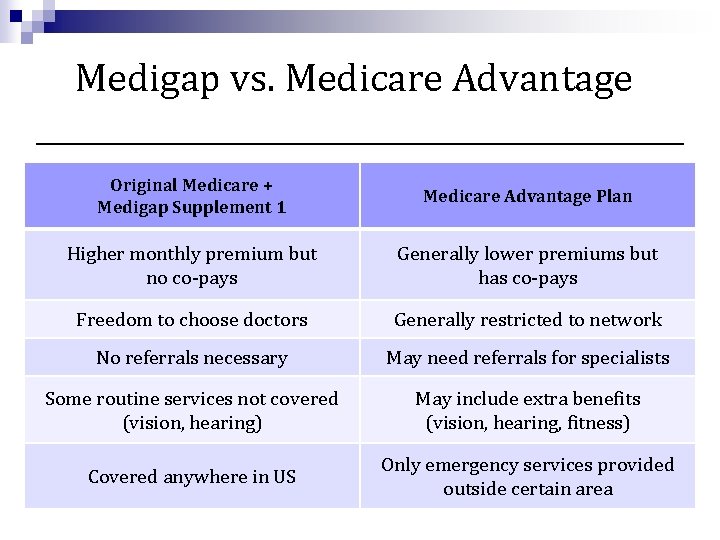
Medigap vs. Medicare Advantage Original Medicare + Medigap Supplement 1 Medicare Advantage Plan Higher monthly premium but no co-pays Generally lower premiums but has co-pays Freedom to choose doctors Generally restricted to network No referrals necessary May need referrals for specialists Some routine services not covered (vision, hearing) May include extra benefits (vision, hearing, fitness) Covered anywhere in US Only emergency services provided outside certain area
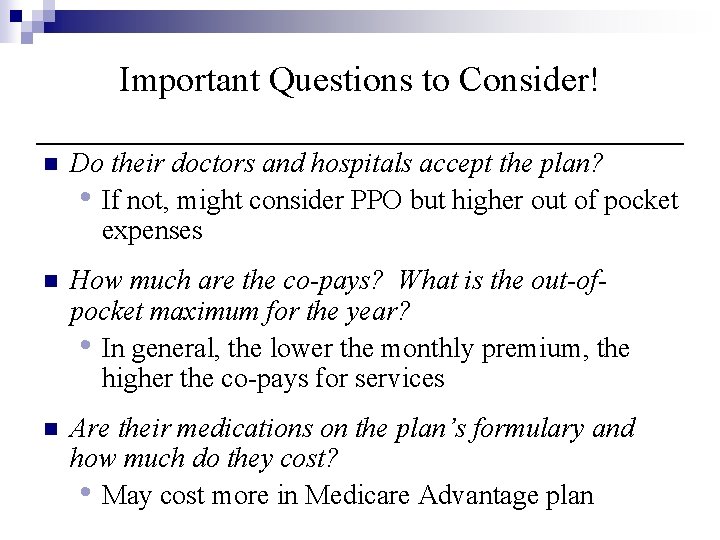
Important Questions to Consider! n Do their doctors and hospitals accept the plan? • If not, might consider PPO but higher out of pocket expenses n How much are the co-pays? What is the out-ofpocket maximum for the year? • In general, the lower the monthly premium, the higher the co-pays for services n Are their medications on the plan’s formulary and how much do they cost? • May cost more in Medicare Advantage plan
Other ways to Supplement Medicare for Certain Populations n Retiree Health Plans (group plans) • Each retiree plan is different • Request an outline of benefits to learn about plan n Medicaid/Mass. Health (for very low-income) • Part A and B deductibles and copayments covered in full if seeing a Mass. Health physician. n Veterans Health Care • Supplements copayments when visiting a VA Physician, Health Clinic or Hospital
Medicare Part D
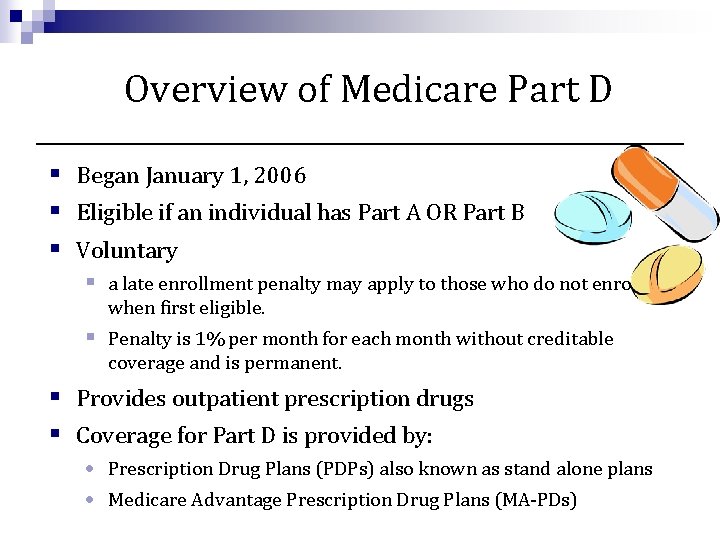
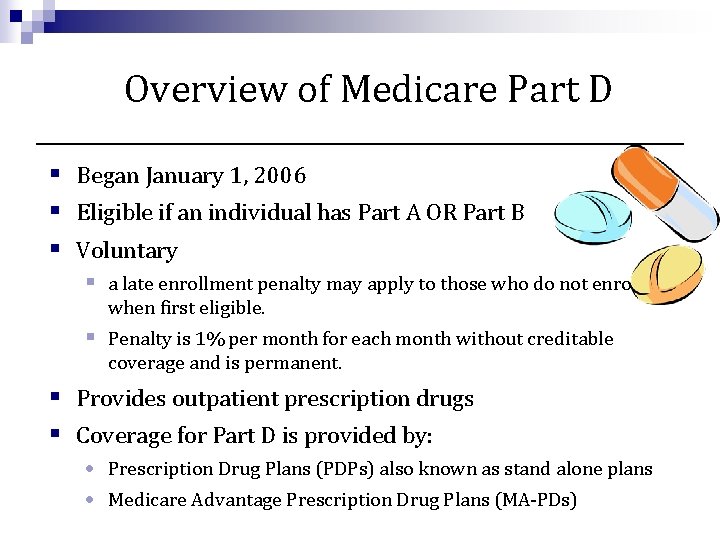
Overview of Medicare Part D § Began January 1, 2006 § Eligible if an individual has Part A OR Part B § Voluntary § a late enrollment penalty may apply to those who do not enroll when first eligible. § Penalty is 1% per month for each month without creditable coverage and is permanent. § Provides outpatient prescription drugs § Coverage for Part D is provided by: • Prescription Drug Plans (PDPs) also known as stand alone plans • Medicare Advantage Prescription Drug Plans (MA-PDs)
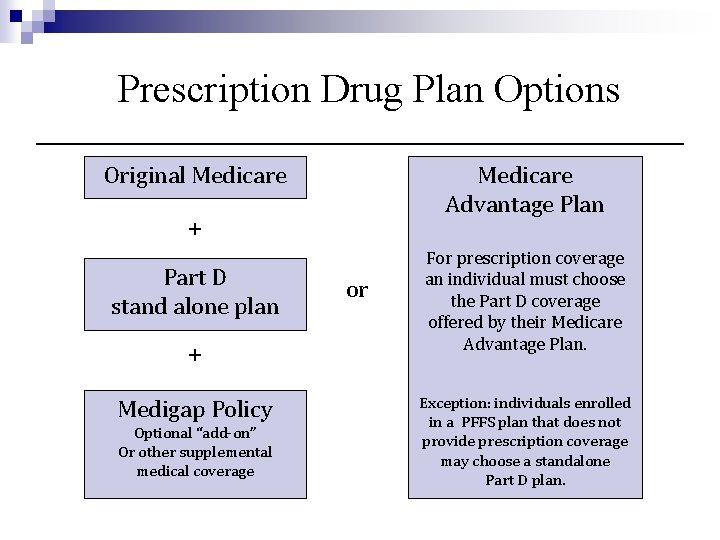
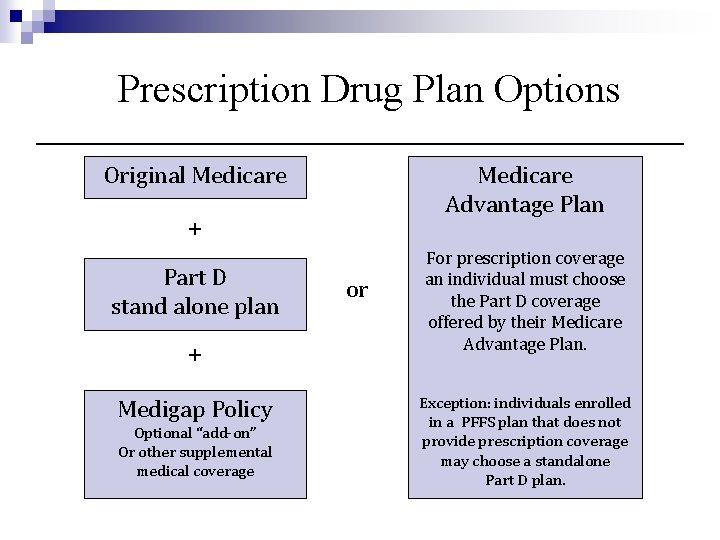
Prescription Drug Plan Options Original Medicare Advantage Plan + Part D stand alone plan + Medigap Policy Optional “add-on” Or other supplemental medical coverage or For prescription coverage an individual must choose the Part D coverage offered by their Medicare Advantage Plan. Exception: individuals enrolled in a PFFS plan that does not provide prescription coverage may choose a standalone Part D plan.
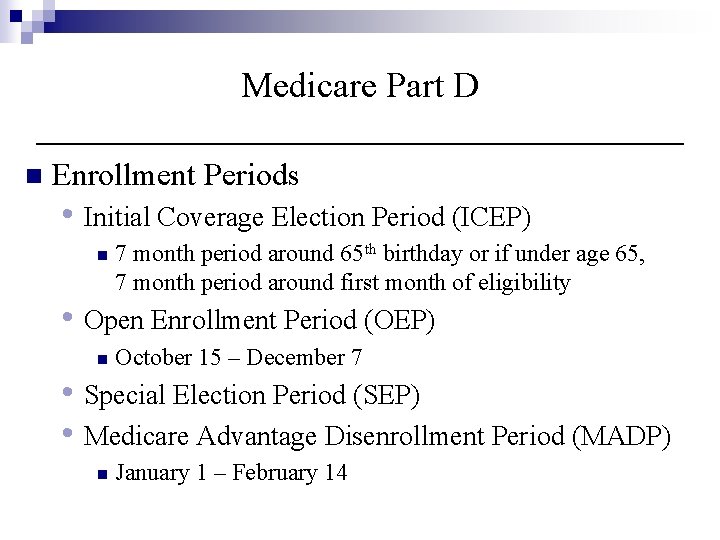
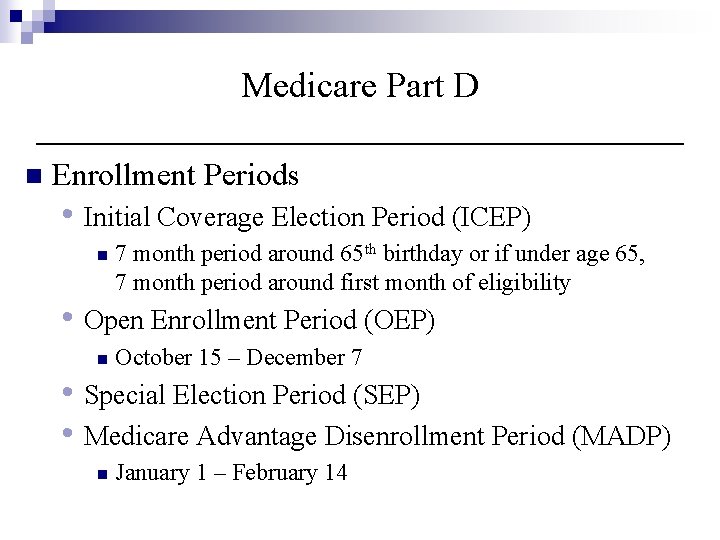
Medicare Part D n Enrollment Periods • Initial Coverage Election Period (ICEP) n 7 month period around 65 th birthday or if under age 65, 7 month period around first month of eligibility • Open Enrollment Period (OEP) n October 15 – December 7 • Special Election Period (SEP) • Medicare Advantage Disenrollment Period (MADP) n January 1 – February 14
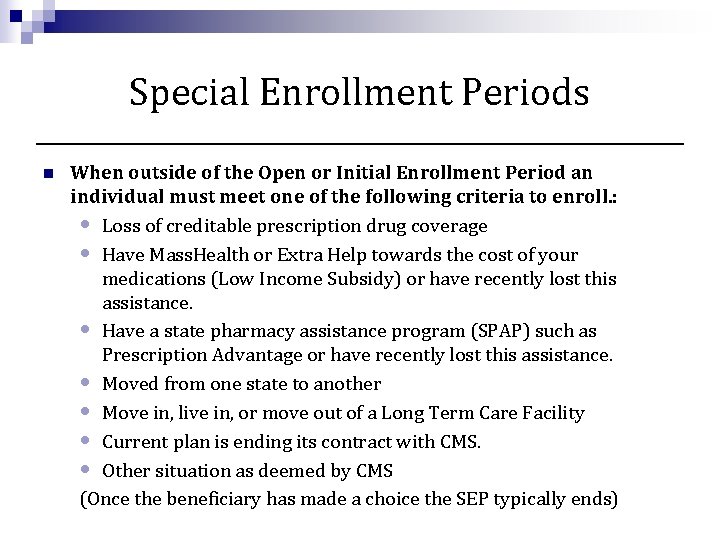
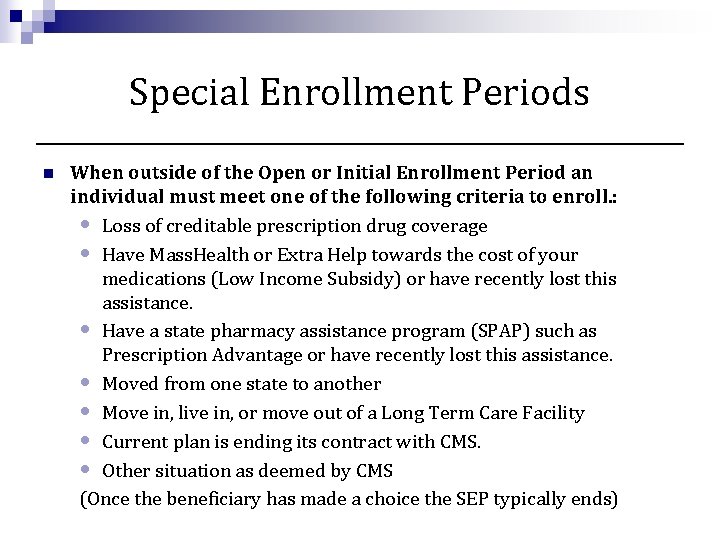
Special Enrollment Periods n When outside of the Open or Initial Enrollment Period an individual must meet one of the following criteria to enroll. : • Loss of creditable prescription drug coverage • Have Mass. Health or Extra Help towards the cost of your medications (Low Income Subsidy) or have recently lost this assistance. • Have a state pharmacy assistance program (SPAP) such as Prescription Advantage or have recently lost this assistance. • Moved from one state to another • Move in, live in, or move out of a Long Term Care Facility • Current plan is ending its contract with CMS. • Other situation as deemed by CMS (Once the beneficiary has made a choice the SEP typically ends)
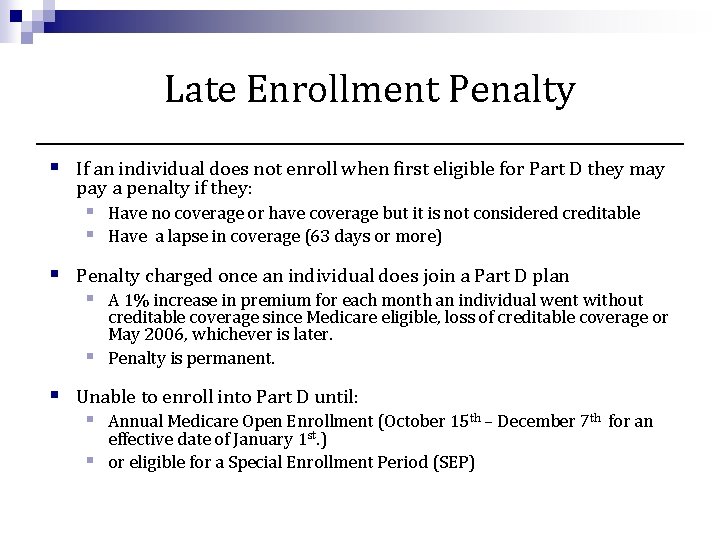
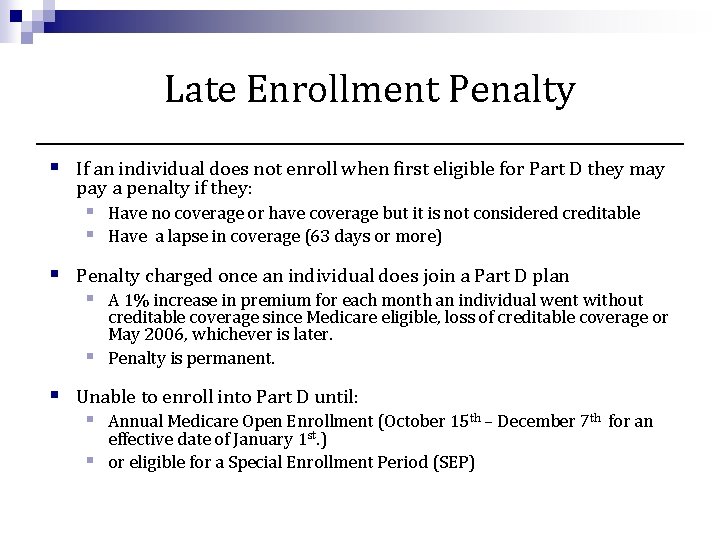
Late Enrollment Penalty § If an individual does not enroll when first eligible for Part D they may pay a penalty if they: § Have no coverage or have coverage but it is not considered creditable § Have a lapse in coverage (63 days or more) § Penalty charged once an individual does join a Part D plan § A 1% increase in premium for each month an individual went without creditable coverage since Medicare eligible, loss of creditable coverage or May 2006, whichever is later. § Penalty is permanent. § Unable to enroll into Part D until: § Annual Medicare Open Enrollment (October 15 th – December 7 th for an effective date of January 1 st. ) § or eligible for a Special Enrollment Period (SEP)
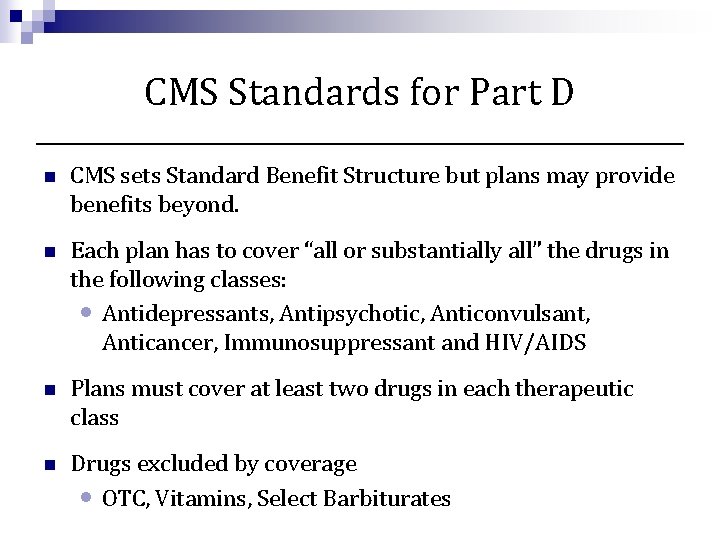
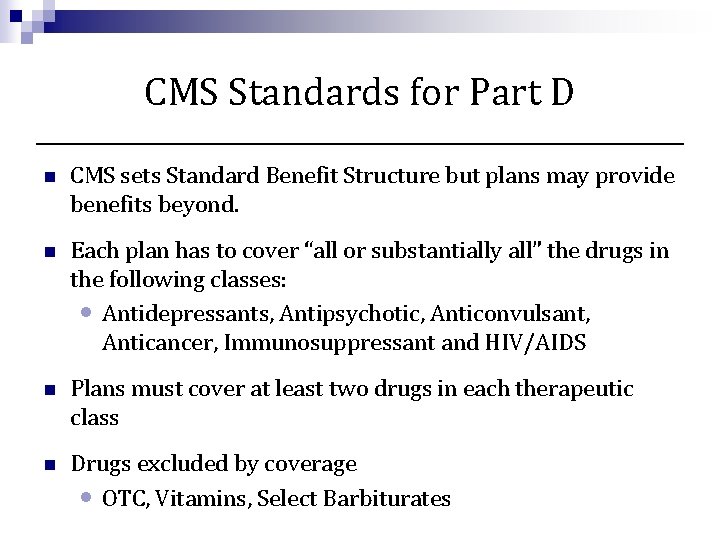
CMS Standards for Part D n CMS sets Standard Benefit Structure but plans may provide benefits beyond. n Each plan has to cover “all or substantially all” the drugs in the following classes: • Antidepressants, Antipsychotic, Anticonvulsant, Anticancer, Immunosuppressant and HIV/AIDS n Plans must cover at least two drugs in each therapeutic class n Drugs excluded by coverage • OTC, Vitamins, Select Barbiturates
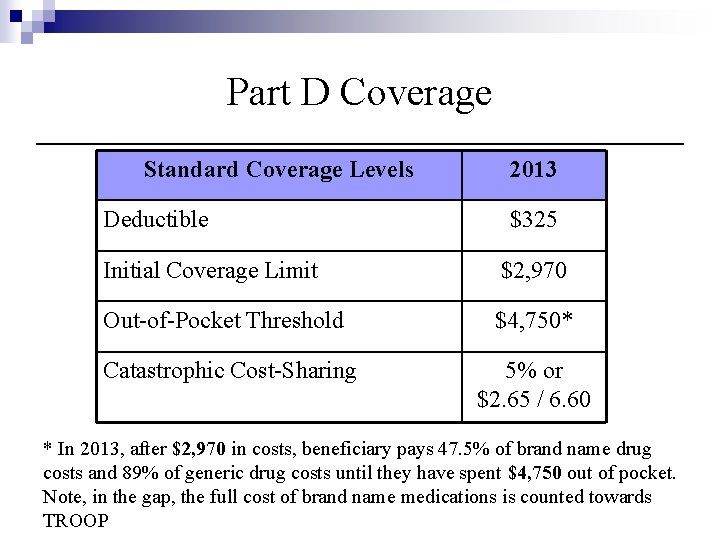
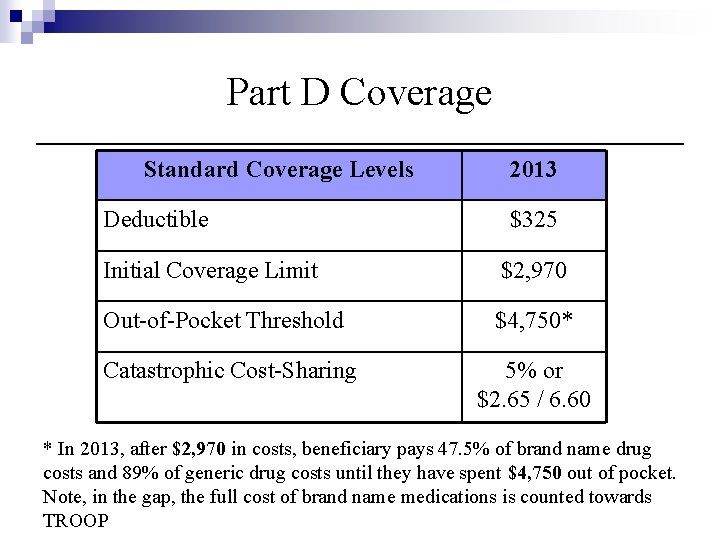
Part D Coverage Standard Coverage Levels Deductible 2013 $325 Initial Coverage Limit $2, 970 Out-of-Pocket Threshold $4, 750* Catastrophic Cost-Sharing 5% or $2. 65 / 6. 60 * In 2013, after $2, 970 in costs, beneficiary pays 47. 5% of brand name drug costs and 89% of generic drug costs until they have spent $4, 750 out of pocket. Note, in the gap, the full cost of brand name medications is counted towards TROOP

How to Enroll Into Medicare Part D n n n Review plan options • • • Consider cost, coverage, quality, and convenience Plan Finder Tool on Medicare. gov Seek assistance from SHINE or other agencies Contact plan directly or call 1 -800 -Medicare • Enrollment can take place on the phone, online, or through a mailed in paper application. Enrollment form will ask for: • • • General contact information Medicare card information Method for premium payment (direct or through Social Security check)
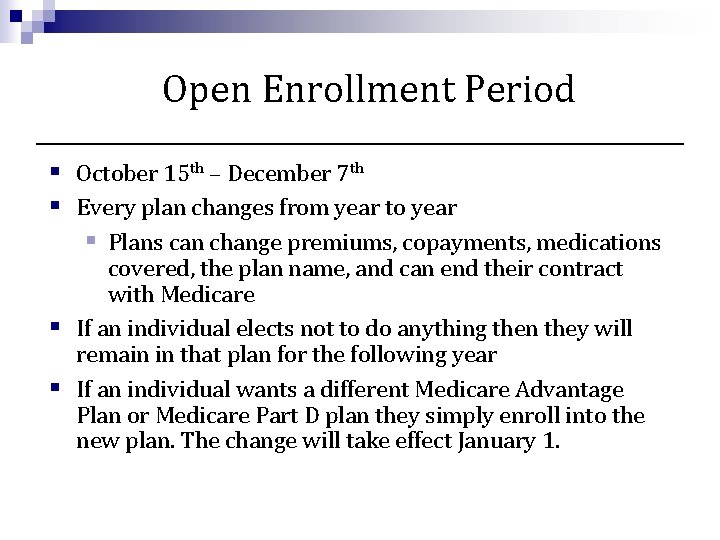
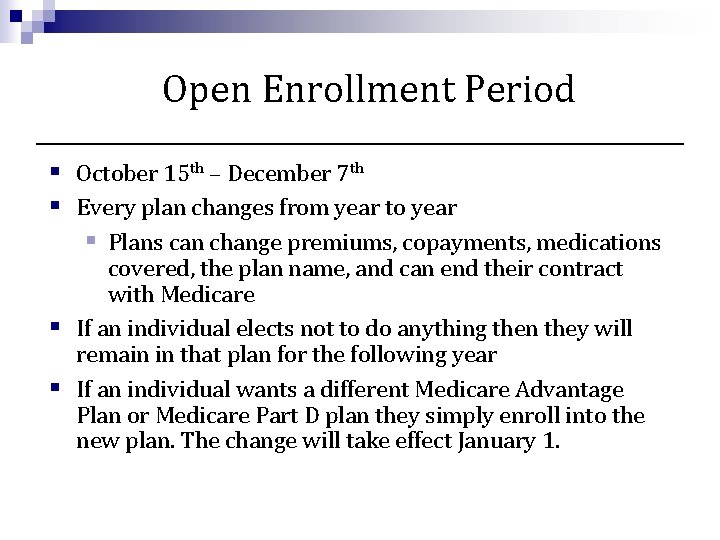
Open Enrollment Period § October 15 th – December 7 th § Every plan changes from year to year § Plans can change premiums, copayments, medications covered, the plan name, and can end their contract with Medicare § If an individual elects not to do anything then they will remain in that plan for the following year § If an individual wants a different Medicare Advantage Plan or Medicare Part D plan they simply enroll into the new plan. The change will take effect January 1.
A note about Supplement 2 n Medigap Supplement 2 is no longer sold (as of 12/31/05) • Most common Supplement 2 plan is Medex Gold. • Very high monthly premium • Provides comprehensive prescription coverage with no gaps n If an individual wants to drop the coverage to join Medicare Part D they must have an SEP or wait until the Annual Coordinated Election Period October 15 th – December 7 th. n If an individual chooses to leave plan they are unable to rejoin at any time.
Assistance with prescription costs: Mass. Health Extra Help / Low Income Subsidy Prescription Advantage
Mass. Health and Medicare Part D n Individuals with Mass. Health and Medicare considered “Dual Eligible” n Since January 1, 2006, Mass. Health no longer provides primary prescription coverage to Medicare beneficiaries. • Mass. Health remains to pay for certain classes of medications directly since Medicare does not cover them. These drug classes are: n n n Select Barbiturates (used to treat cancer, epilepsy or chronic mental health conditions ) Certain Over the Counter Medications (Ibuprofen & acetaminophen) Dual Eligible individuals must receive primary coverage through a Medicare Part D plan

Auto-Enrollment of Duals n Individuals who have Mass. Health and become eligible for Medicare auto-enrolled into the Limited Income Newly Eligible Transition Program (LI-Net) (this process began on 1/1/2010) • The LI-Net program, administered by Humana, provides coverage for individuals for two months. • After two months, if a dual-eligible individual has not selected a plan on their own they will be auto-enrolled into a randomly selected plan below the benchmark. n $0 Monthly Premium n Plan may not cover all medications • Dual Eligible Individuals can change plans monthly (continuous SEP), coverage begins first of the following month.
Extra Help / Low Income Subsidy n Extra Help, also knows as a Low Income Subsidy, is a federal assistance program to help low-income and low-asset Medicare beneficiaries with costs related to Medicare Part D. n Individuals with Mass. Health assistance are Automatically eligible for this program and do not need to apply n Auto-Assignment (Li-Net) and Re-assignment (plan changes in the fall) processes are also used for those who qualify for Extra Help n Extra Help subsidizes: • Premiums, Deductibles, Copayments, Coverage Gap • Late Enrollment Penalty • Does not subsidize non-formulary or excluded medications
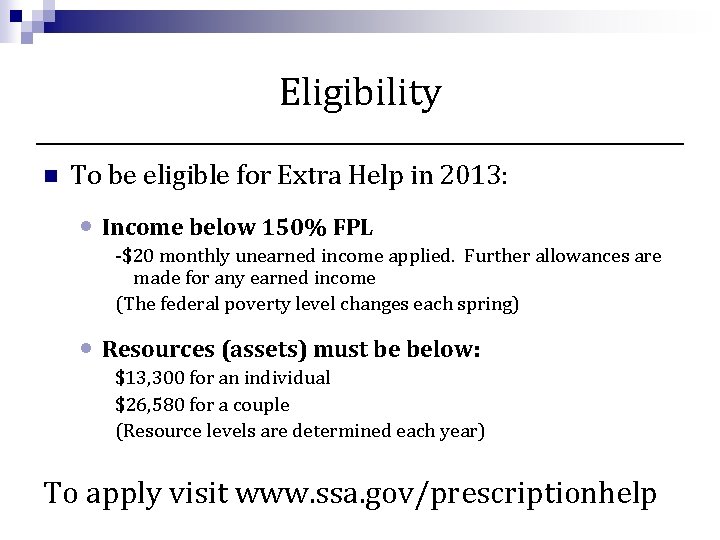
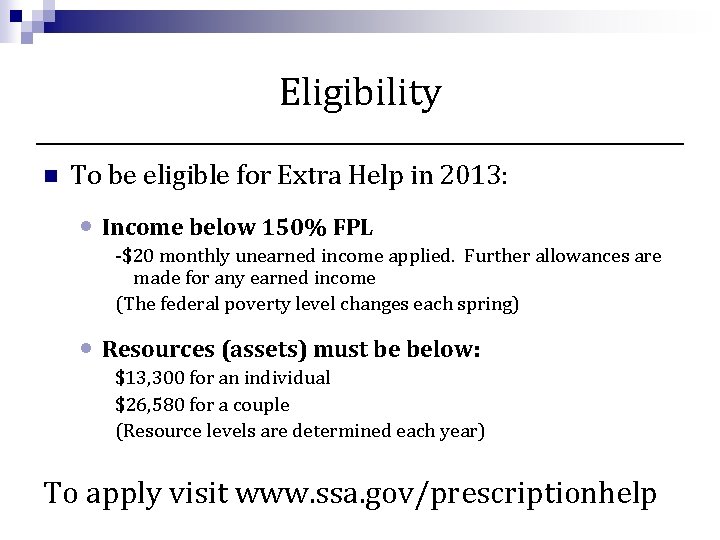
Eligibility n To be eligible for Extra Help in 2013: • Income below 150% FPL -$20 monthly unearned income applied. Further allowances are made for any earned income (The federal poverty level changes each spring) • Resources (assets) must be below: $13, 300 for an individual $26, 580 for a couple (Resource levels are determined each year) To apply visit www. ssa. gov/prescriptionhelp
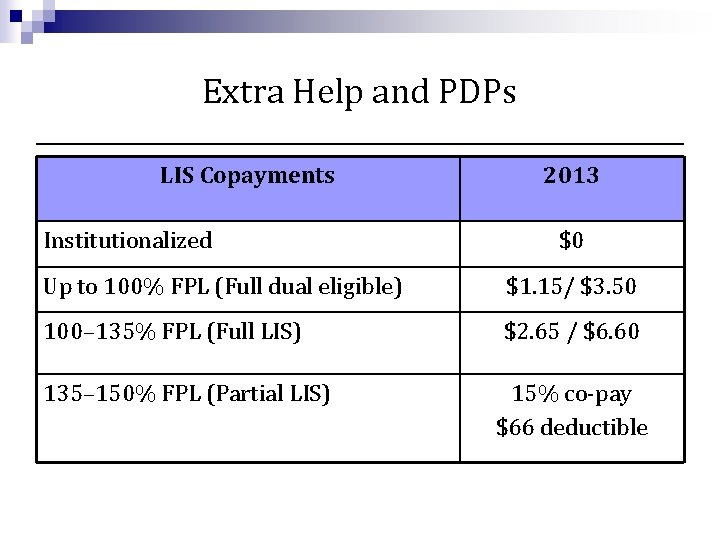
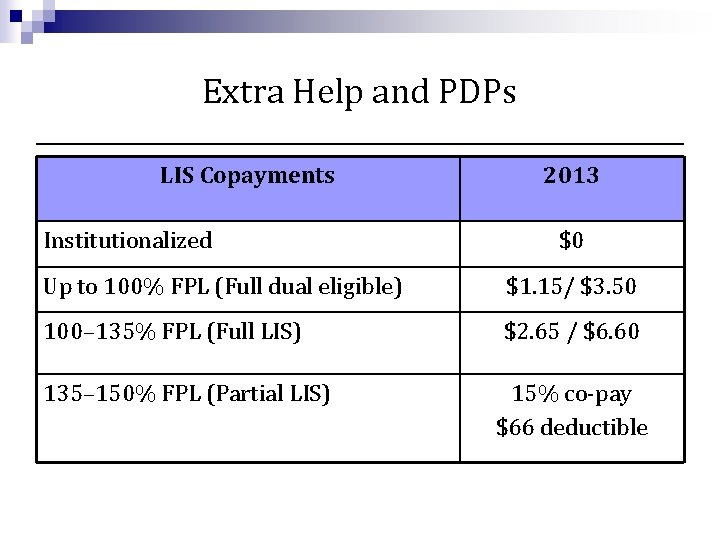
Extra Help and PDPs LIS Copayments Institutionalized 2013 $0 Up to 100% FPL (Full dual eligible) $1. 15/ $3. 50 100– 135% FPL (Full LIS) $2. 65 / $6. 60 135– 150% FPL (Partial LIS) 15% co-pay $66 deductible
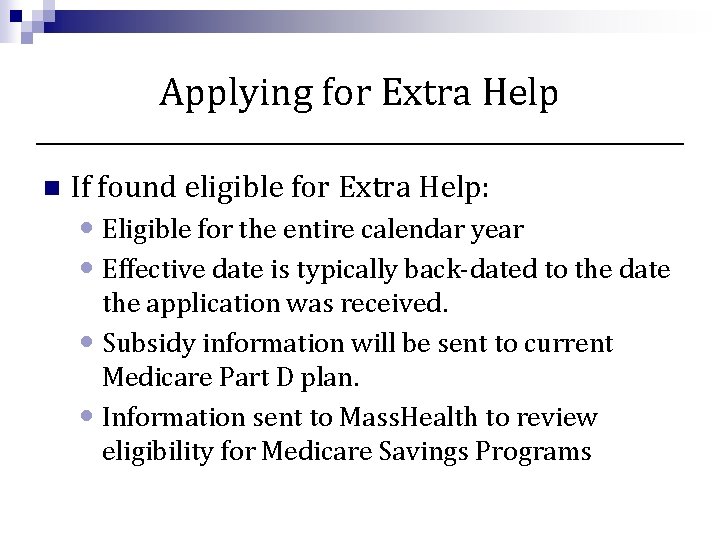
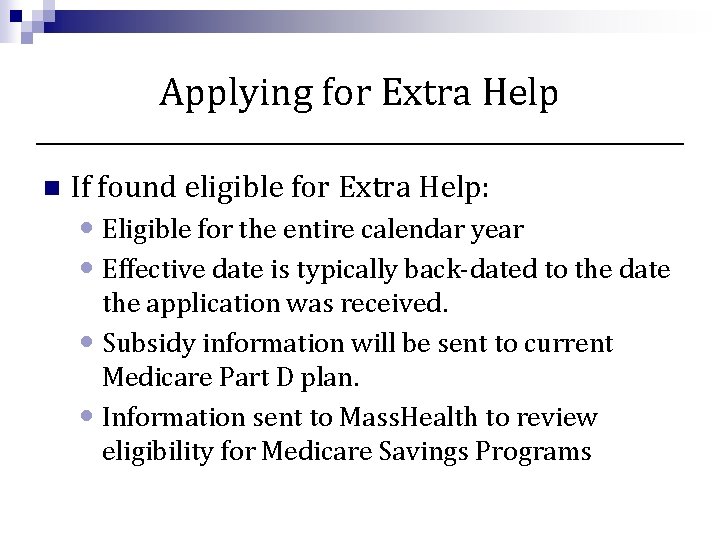
Applying for Extra Help n If found eligible for Extra Help: • Eligible for the entire calendar year • Effective date is typically back-dated to the date the application was received. • Subsidy information will be sent to current Medicare Part D plan. • Information sent to Mass. Health to review eligibility for Medicare Savings Programs
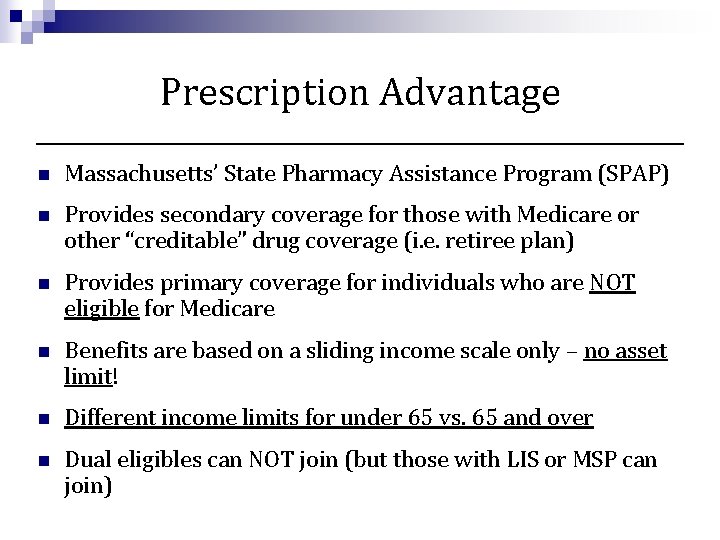
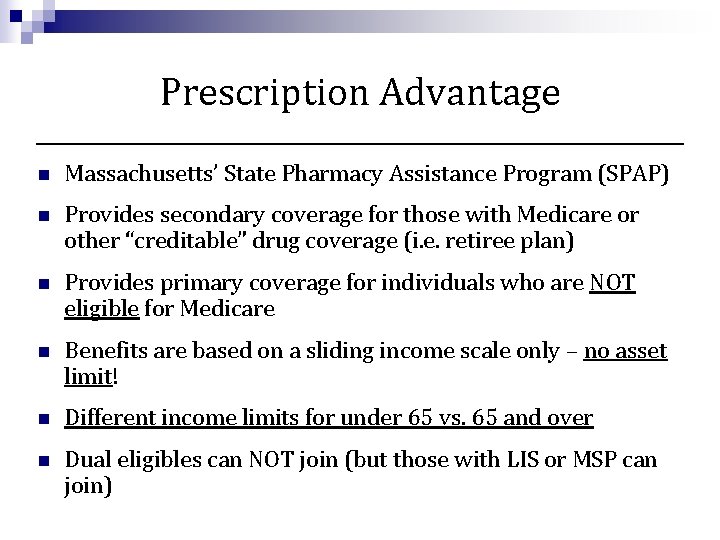
Prescription Advantage n Massachusetts’ State Pharmacy Assistance Program (SPAP) n Provides secondary coverage for those with Medicare or other “creditable” drug coverage (i. e. retiree plan) n Provides primary coverage for individuals who are NOT eligible for Medicare n Benefits are based on a sliding income scale only – no asset limit! n Different income limits for under 65 vs. 65 and over n Dual eligibles can NOT join (but those with LIS or MSP can join)
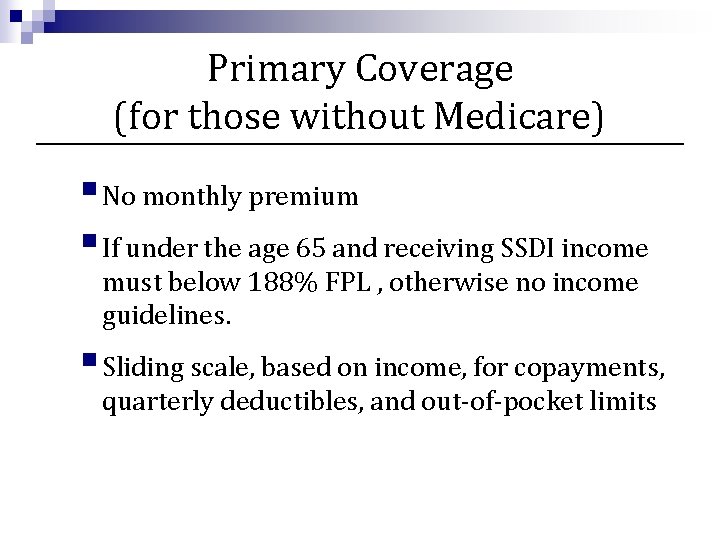
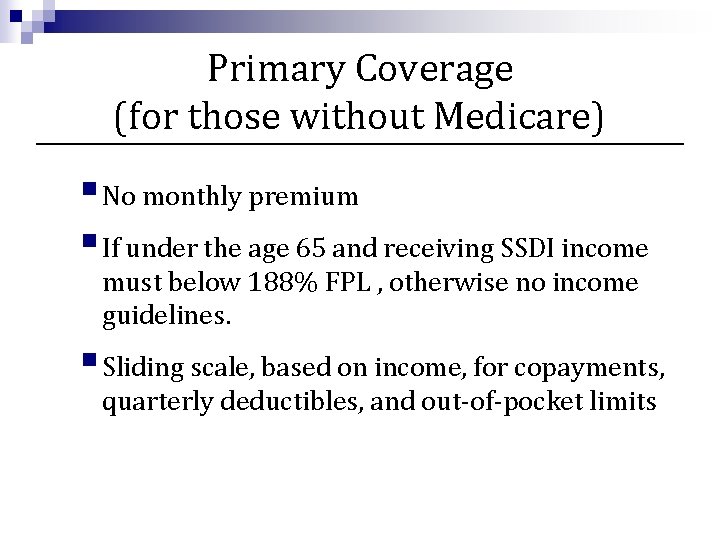
Primary Coverage (for those without Medicare) § No monthly premium § If under the age 65 and receiving SSDI income must below 188% FPL , otherwise no income guidelines. § Sliding scale, based on income, for copayments, quarterly deductibles, and out-of-pocket limits
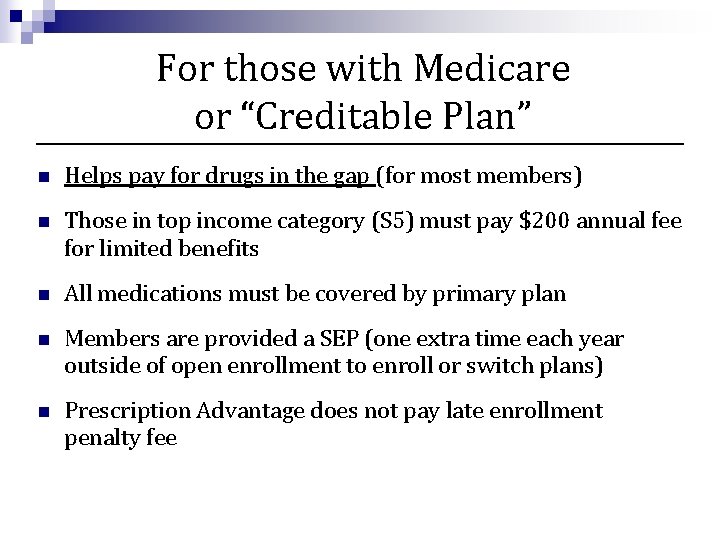
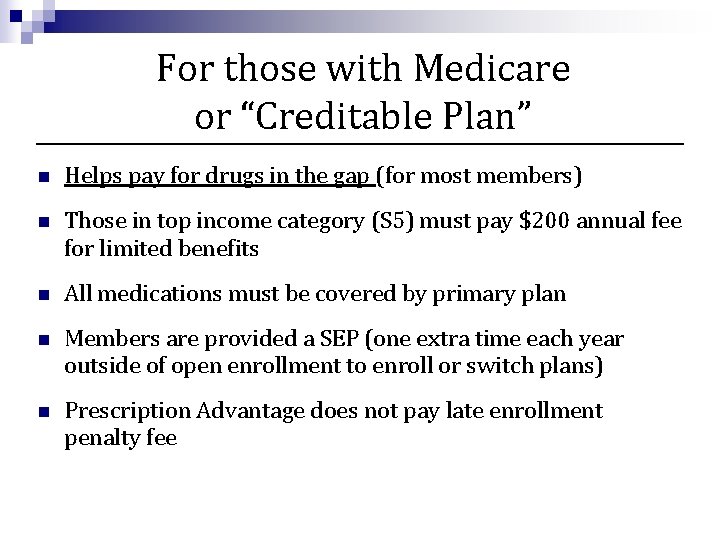
For those with Medicare or “Creditable Plan” n Helps pay for drugs in the gap (for most members) n Those in top income category (S 5) must pay $200 annual fee for limited benefits n All medications must be covered by primary plan n Members are provided a SEP (one extra time each year outside of open enrollment to enroll or switch plans) n Prescription Advantage does not pay late enrollment penalty fee
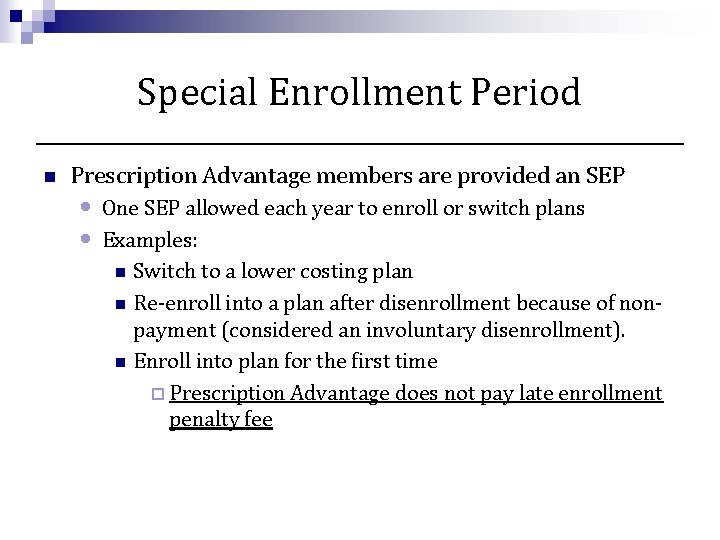
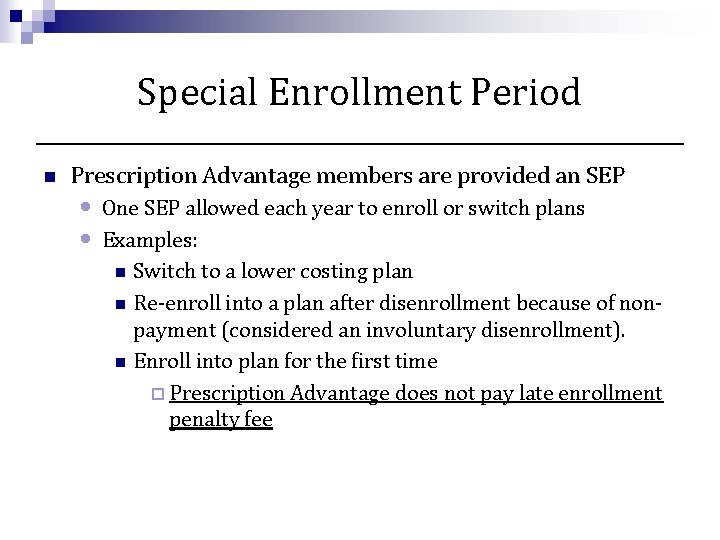
Special Enrollment Period n Prescription Advantage members are provided an SEP • • One SEP allowed each year to enroll or switch plans Examples: n Switch to a lower costing plan n Re-enroll into a plan after disenrollment because of nonpayment (considered an involuntary disenrollment). n Enroll into plan for the first time ¨ Prescription Advantage does not pay late enrollment penalty fee
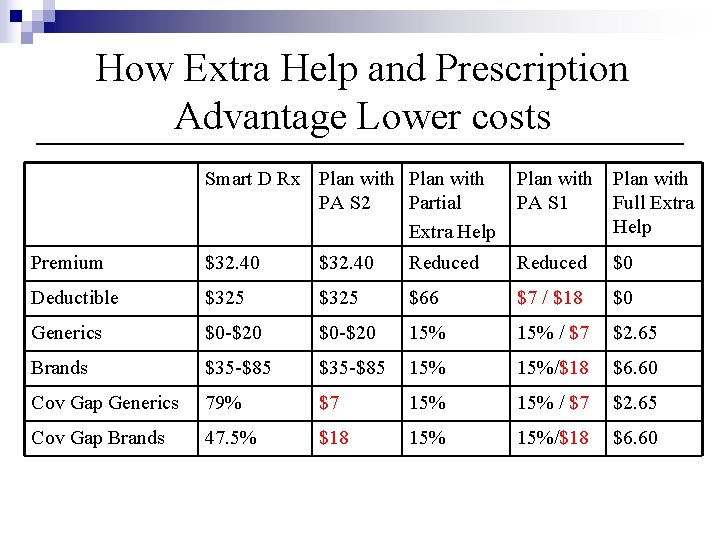
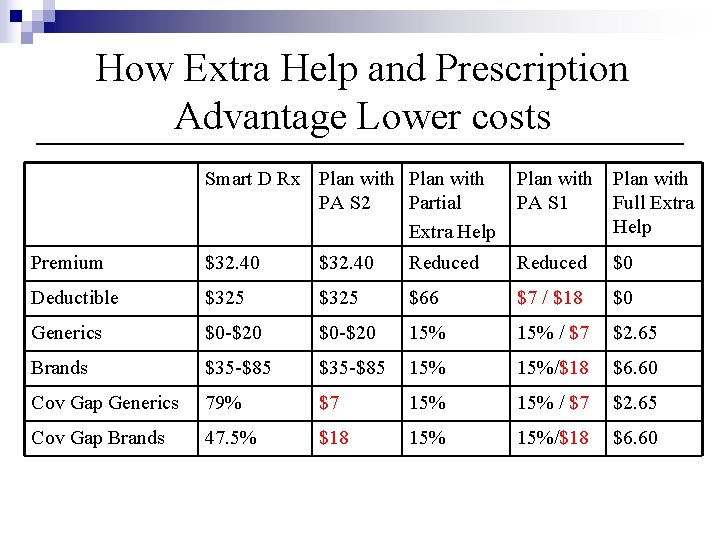
How Extra Help and Prescription Advantage Lower costs Smart D Rx Plan with PA S 2 Partial Extra Help Plan with PA S 1 Full Extra Help Premium $32. 40 Reduced $0 Deductible $325 $66 $7 / $18 $0 Generics $0 -$20 15% / $7 $2. 65 Brands $35 -$85 15%/$18 $6. 60 Cov Gap Generics 79% $7 15% / $7 $2. 65 Cov Gap Brands 47. 5% $18 15%/$18 $6. 60
Other Ways to Lower Prescription Costs n n n Patient Assistance Programs Copay Assistance Foundations Mail Order Generic Pricing Programs Alternative medications
MCPHS Pharmacy Outreach Program (Mass. Med. Line) n Pharmacy Outreach Program of the Massachusetts College of Pharmacy and Health Sciences in Worcester n Partially funded by the Executive Office of Elder Affairs n Toll Free number 1 -866 -633 -1617 n Pharmacist and Case Managers available • Part D Reviews • Screen for financial assistance programs • Provide recommendations for alternative medications • Review for drug interactions
Public Benefits
Supplemental Security Income (SSI) n Raises income to standard of living income level n SSI recipients auto enrolled in Mass. Health & LIS n Must meet income/asset limits n Must also be aged 65+ OR blind or disabled n Beneficiaries enroll through the SSA
Mass. Health Standard n Provides a full range of medical benefits • Including inpatient, outpatient, skilled nursing care, and prescription coverage n Provides secondary coverage for Medicare Beneficiaries • Medicare Part A & B premiums, deductibles & coinsurance • Deemed eligible for Extra Help – can pay for Medicare Part D premium, deductible, and reduce copays for medications
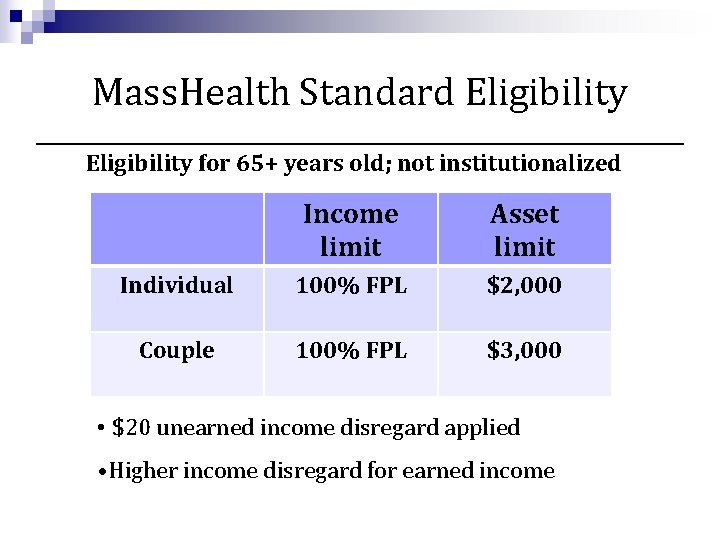
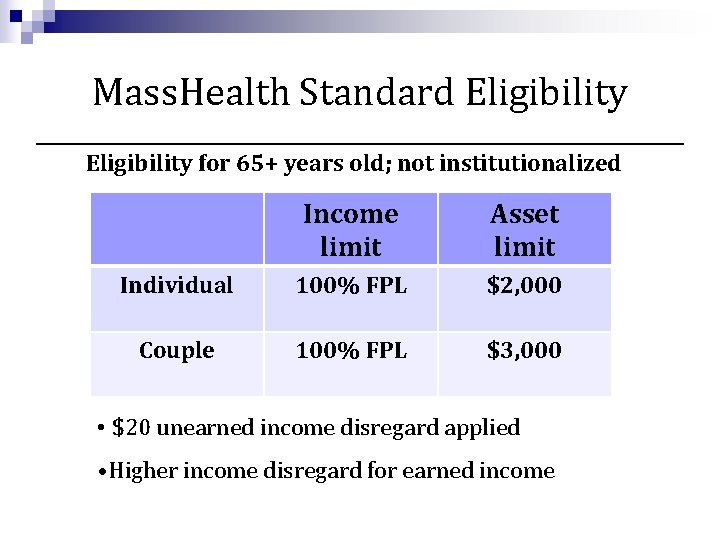
Mass. Health Standard Eligibility for 65+ years old; not institutionalized Income limit Asset limit Individual 100% FPL $2, 000 Couple 100% FPL $3, 000 • $20 unearned income disregard applied • Higher income disregard for earned income
Mass. Health for Caretaker Relatives n. Provides Mass. Health Standard benefits n. Caretaker relative: an adult relative living in the same home with a child under 19 whose parents are not present in the home; who is related to the child by: • Blood • Adoption • Marriage (or is the spouse or former spouse of those relatives)
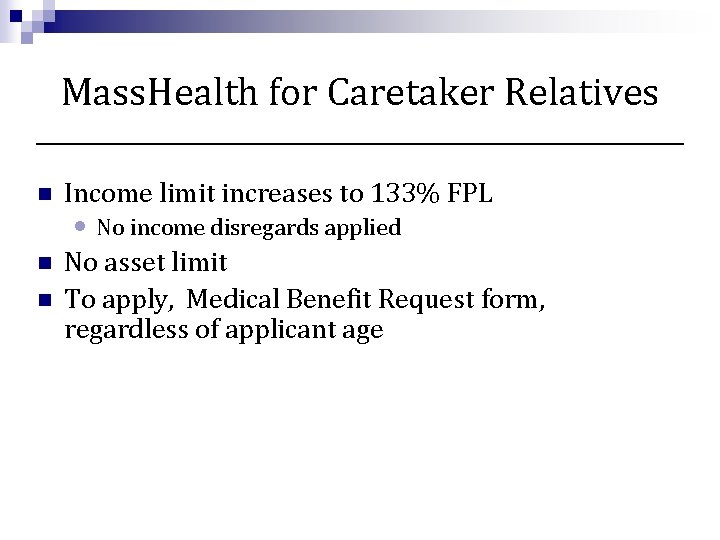
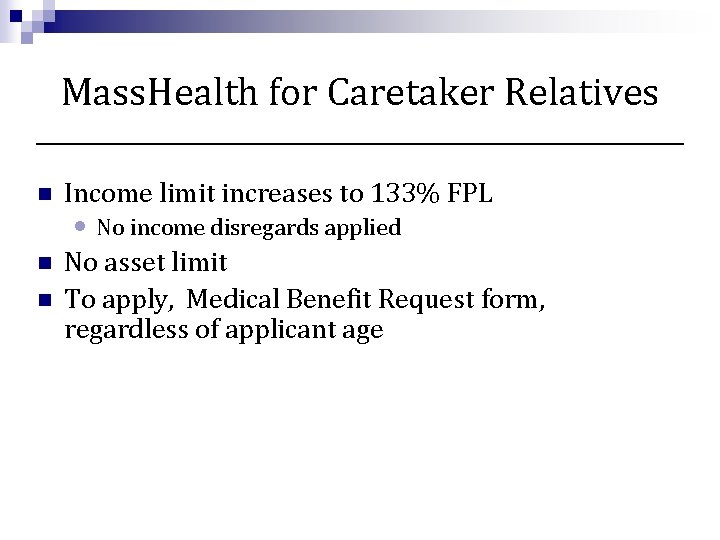
Mass. Health for Caretaker Relatives n Income limit increases to 133% FPL n No asset limit To apply, Medical Benefit Request form, regardless of applicant age n • No income disregards applied
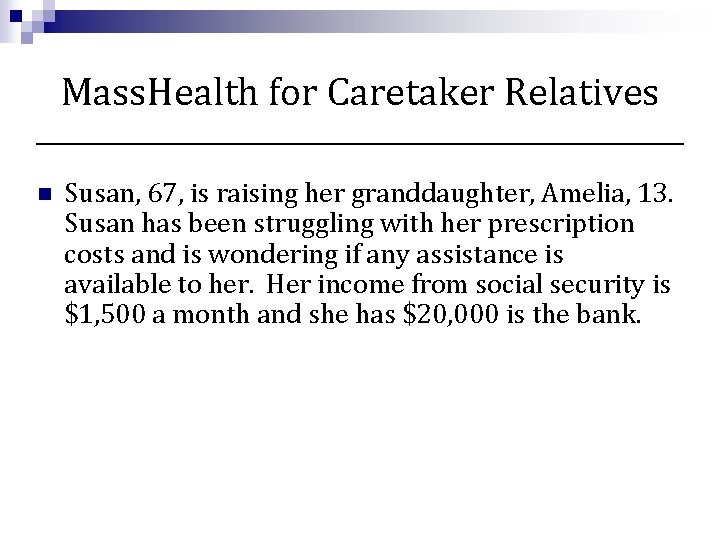
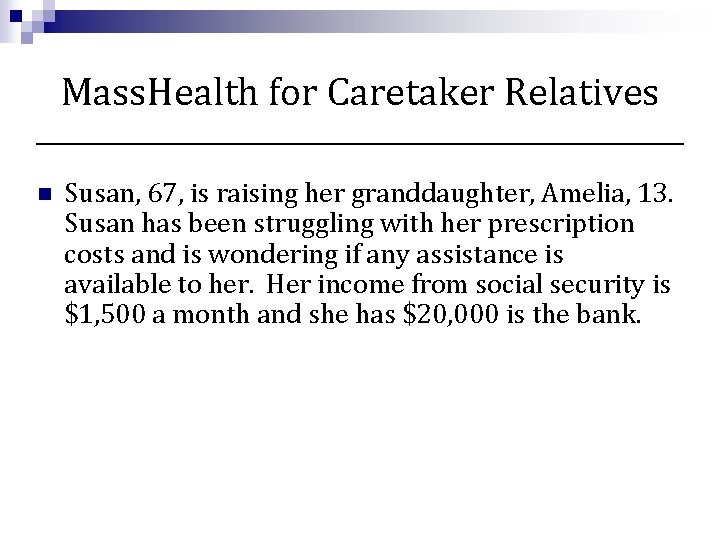
Mass. Health for Caretaker Relatives n Susan, 67, is raising her granddaughter, Amelia, 13. Susan has been struggling with her prescription costs and is wondering if any assistance is available to her. Her income from social security is $1, 500 a month and she has $20, 000 is the bank.
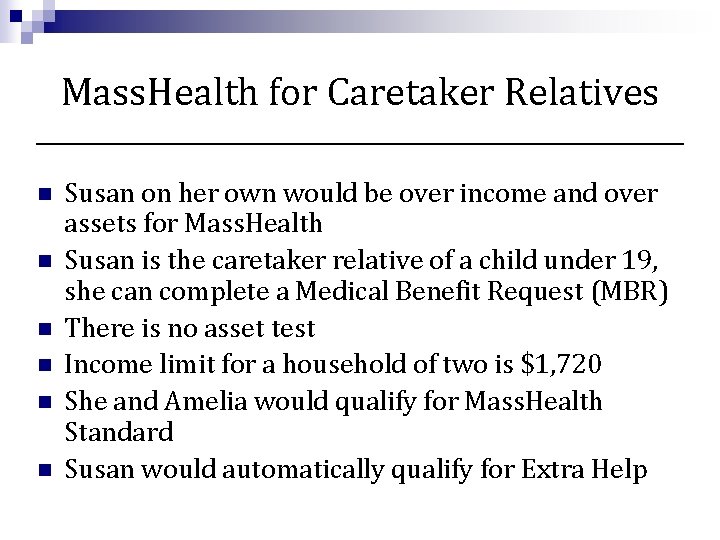
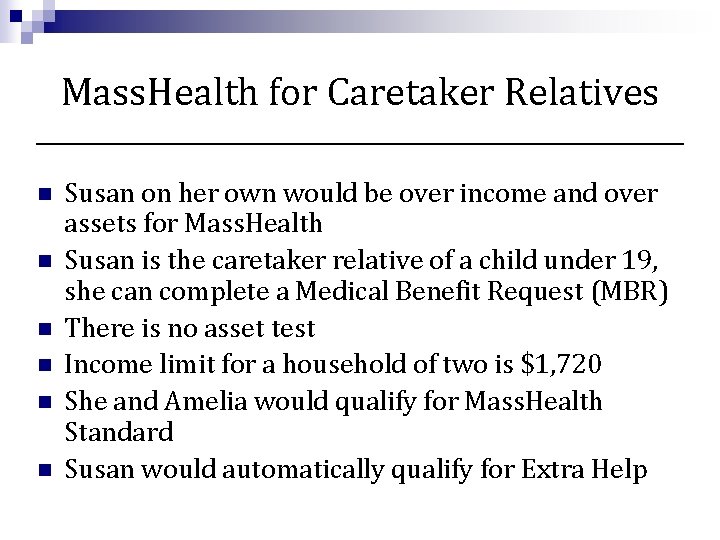
Mass. Health for Caretaker Relatives n n n Susan on her own would be over income and over assets for Mass. Health Susan is the caretaker relative of a child under 19, she can complete a Medical Benefit Request (MBR) There is no asset test Income limit for a household of two is $1, 720 She and Amelia would qualify for Mass. Health Standard Susan would automatically qualify for Extra Help
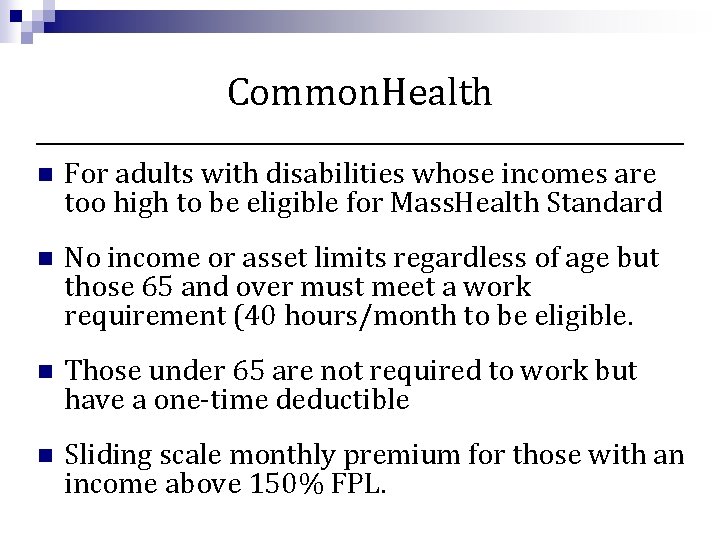
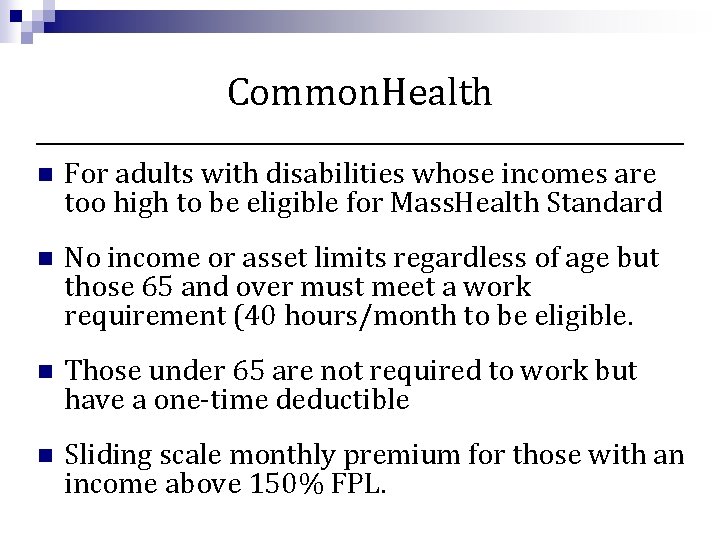
Common. Health n For adults with disabilities whose incomes are too high to be eligible for Mass. Health Standard n No income or asset limits regardless of age but those 65 and over must meet a work requirement (40 hours/month to be eligible. n Those under 65 are not required to work but have a one-time deductible n Sliding scale monthly premium for those with an income above 150% FPL.
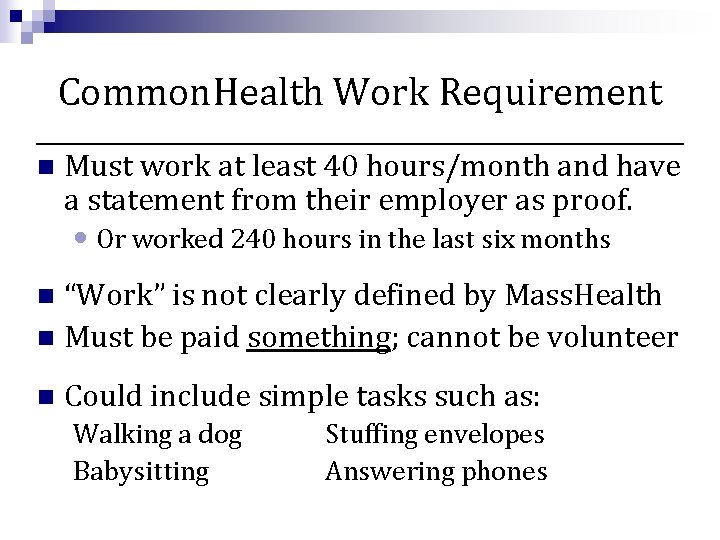
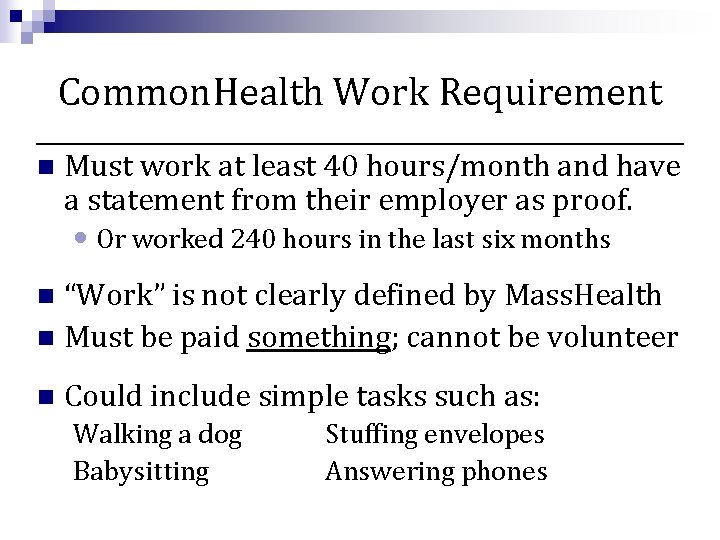
Common. Health Work Requirement n Must work at least 40 hours/month and have a statement from their employer as proof. • Or worked 240 hours in the last six months “Work” is not clearly defined by Mass. Health n Must be paid something; cannot be volunteer n n Could include simple tasks such as: Walking a dog Babysitting Stuffing envelopes Answering phones
Common. Health n Regardless of age complete a Mass. Health MBR. • Recommendation: Write Common. Health on the front of the application if submitting in a paper form. n If approved will receive many of the same benefits Mass. Health Standard members receive • Inpatient and Outpatient Services • Transportation services • Automatically qualify for Extra Help for Part D • May not qualify for Part B premium assistance.
Common. Health n Robert is disabled and not working. He has been on Common. Health for a year. He is about to turn 65. He is concerned about his costs under Medicare. His social security check is $1, 600 a month and he has about $10, 000 in his savings account.
Common. Health n n Once Robert turns 65 he will only be able to maintain Common. Health if he is able to work 40 hours / month. Common. Health will assist him with his Medicare Part A and Part B deductibles and coinsurance He will automatically qualify for Extra Help with his prescription Medications. Since his income is over 150% FPL he will have to pay a monthly premium for Common. Health and will have to pay his Part B premium.
Personal Care Attendant (PCA) Program n For individuals who need assistance with at least two Activities of Daily Living (ADL’s) such as bathing, dressing, eating, taking medicines. n Provides beneficiary Mass. Health Standard and coverage for personal care attendant services n Beneficiary hires their own Personal Care Attendant • Can be a family member or friend, but not: n A spouse n A parent of a child receiving the services n Legally responsible relative
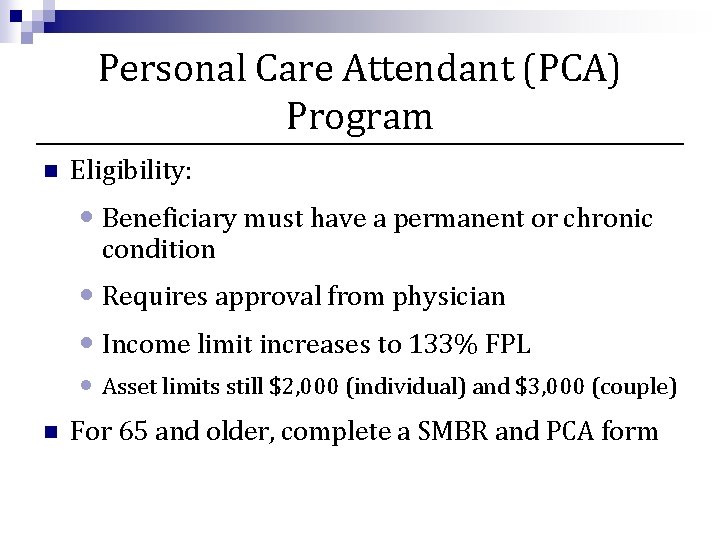
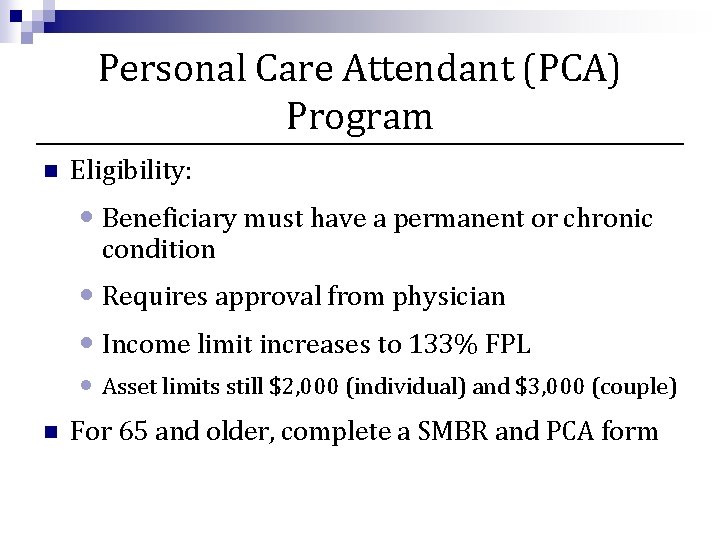
Personal Care Attendant (PCA) Program n Eligibility: • Beneficiary must have a permanent or chronic condition • Requires approval from physician • Income limit increases to 133% FPL • Asset limits still $2, 000 (individual) and $3, 000 (couple) n For 65 and older, complete a SMBR and PCA form
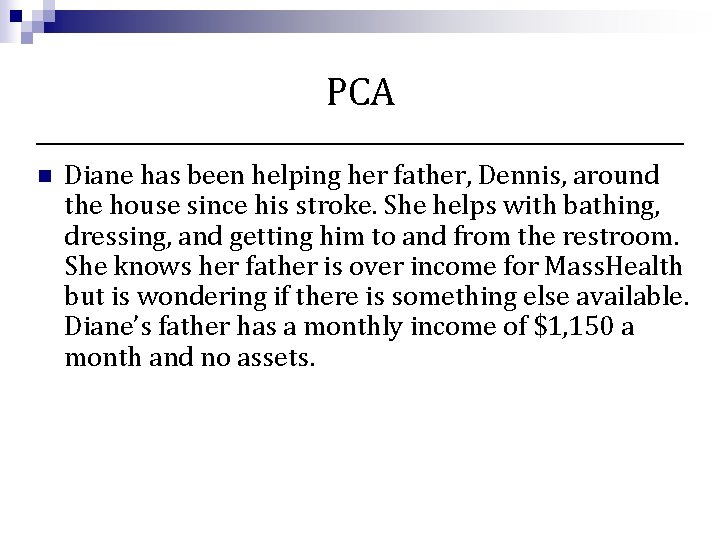
PCA n Diane has been helping her father, Dennis, around the house since his stroke. She helps with bathing, dressing, and getting him to and from the restroom. She knows her father is over income for Mass. Health but is wondering if there is something else available. Diane’s father has a monthly income of $1, 150 a month and no assets.
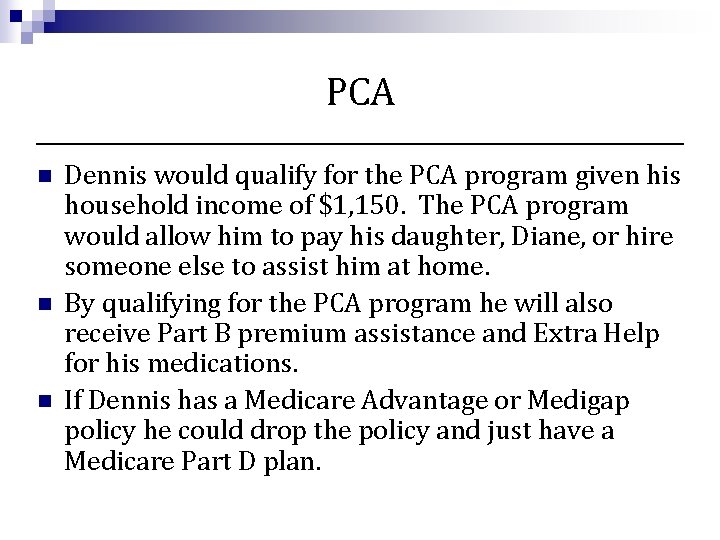
PCA n n n Dennis would qualify for the PCA program given his household income of $1, 150. The PCA program would allow him to pay his daughter, Diane, or hire someone else to assist him at home. By qualifying for the PCA program he will also receive Part B premium assistance and Extra Help for his medications. If Dennis has a Medicare Advantage or Medigap policy he could drop the policy and just have a Medicare Part D plan.
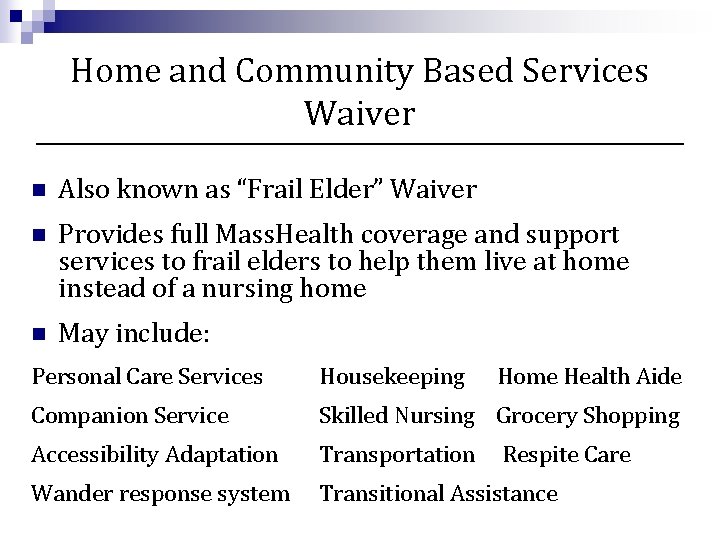
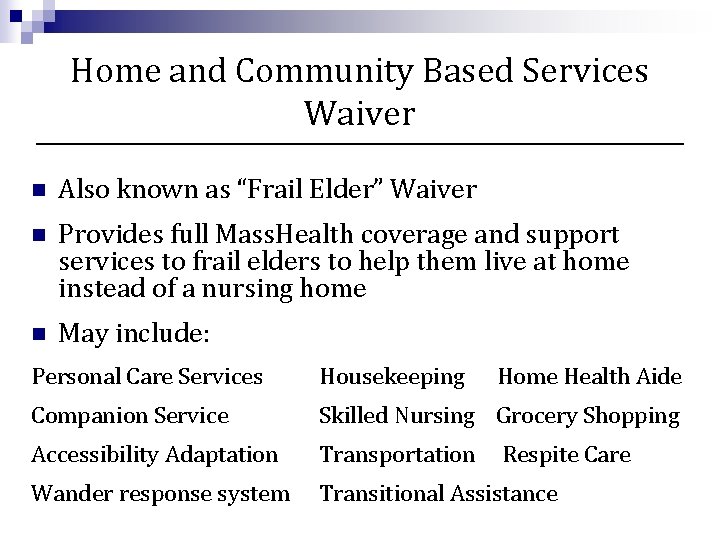
Home and Community Based Services Waiver n Also known as “Frail Elder” Waiver n Provides full Mass. Health coverage and support services to frail elders to help them live at home instead of a nursing home n May include: Personal Care Services Housekeeping Home Health Aide Companion Service Skilled Nursing Grocery Shopping Accessibility Adaptation Transportation Wander response system Transitional Assistance Respite Care
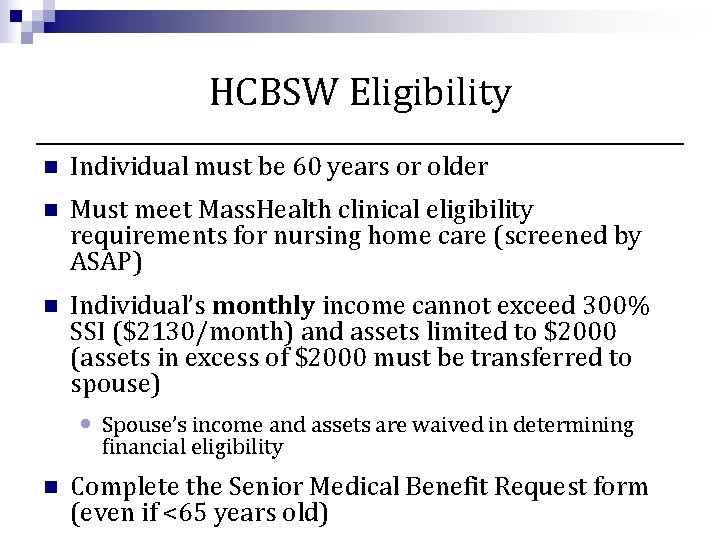
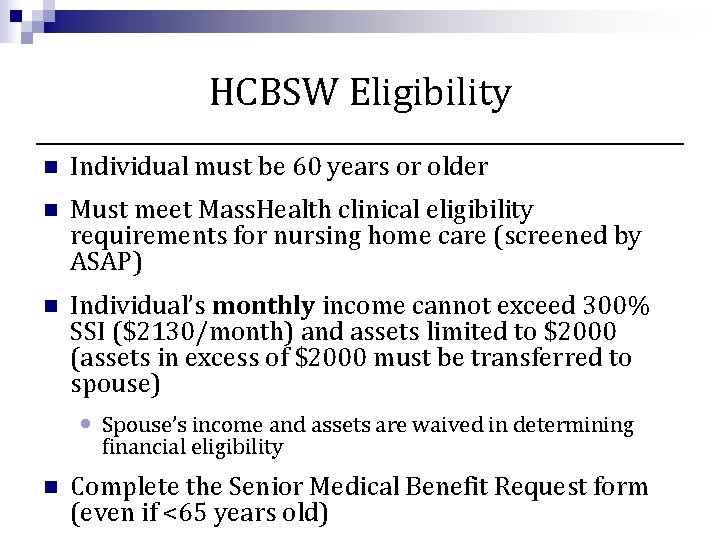
HCBSW Eligibility n Individual must be 60 years or older n Must meet Mass. Health clinical eligibility requirements for nursing home care (screened by ASAP) n Individual’s monthly income cannot exceed 300% SSI ($2130/month) and assets limited to $2000 (assets in excess of $2000 must be transferred to spouse) • Spouse’s income and assets are waived in determining financial eligibility n Complete the Senior Medical Benefit Request form (even if <65 years old)
HCBSW n Sandy, 71 has been taking care of her husband Jim, 75, who has Parkinson's Disease. His level of care is more than Sandy can handle on her own. She is considering moving her husband to a nursing home but she is hoping there is a way to keep her husband at home. She is seeking assistance. Sandy’s income is $1, 300 a month Jim’s income is $1, 800 a month. Combined they have $25, 000 in the bank.
HCBSW n Jim may qualify for HCBSW if he meets the clinical eligibility requirement. n Even though Jim and Sandy have a combined income of $3, 100 a month, only Jim’s income is counted. n Jim’s assets must be below $2, 000 to qualify. Sandy’s assets would not be counted. In order to qualify for the program Sandy must have at least $23, 000 in assets transferred to her name only.
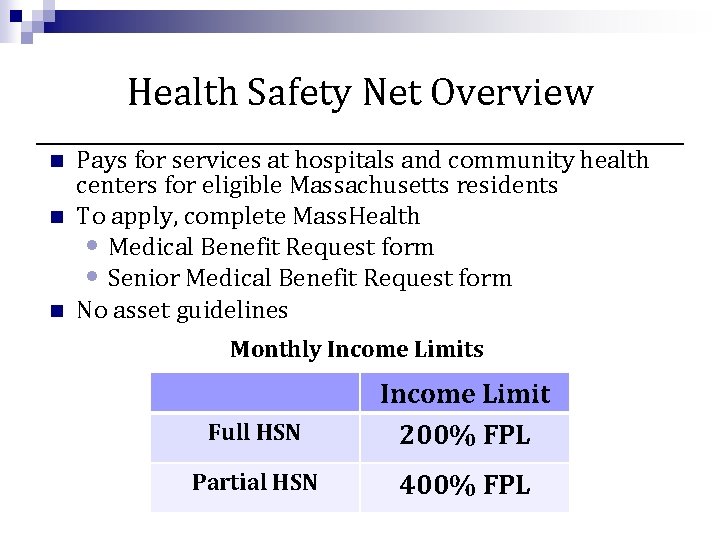
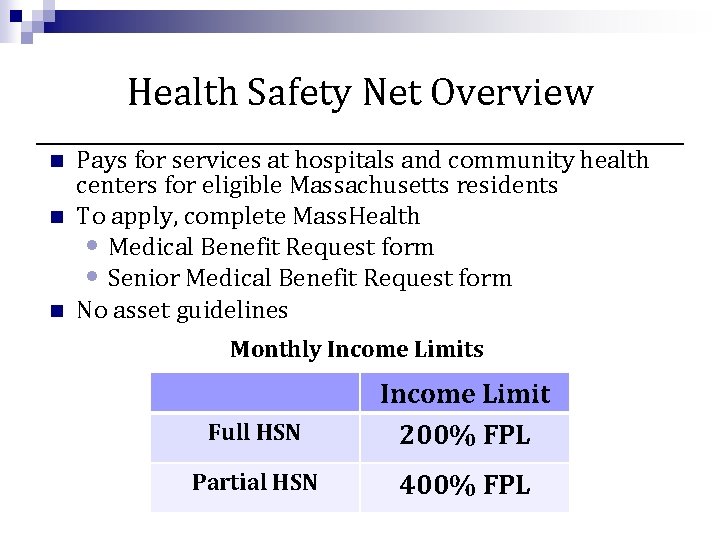
Health Safety Net Overview n n n Pays for services at hospitals and community health centers for eligible Massachusetts residents To apply, complete Mass. Health • Medical Benefit Request form • Senior Medical Benefit Request form No asset guidelines Monthly Income Limits Full HSN Income Limit 200% FPL Partial HSN 400% FPL
Health Safety Net and Medicare has many “gaps” n Part A deductible: • $1, 184 per benefit period n Part A co-payments: • Days 61 -90: $296/day • Days 91 -150: $592/day n
Health Safety Net and Medicare Can cover all of the Part A deductible and Part A co-payments if eligible for full HSN n Must first meet HSN deductible if eligible for partial HSN n Beneficiary could select more affordable Medicare supplemental coverage if HSN is in place n
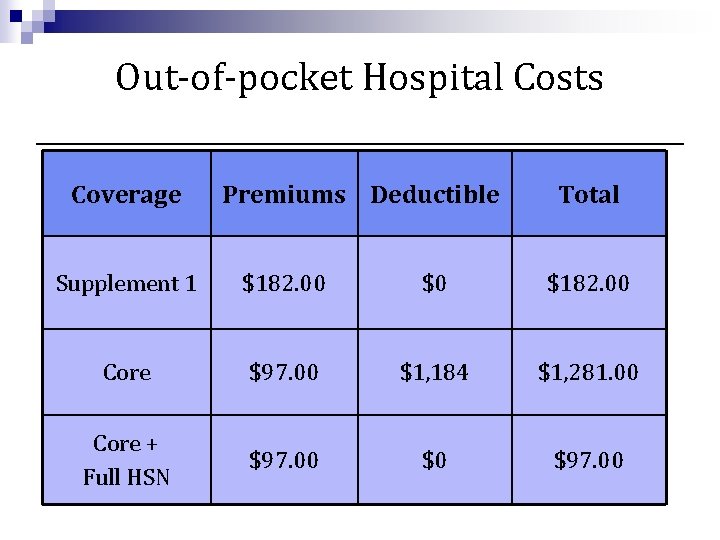
Case Example Judy is hospitalized for 10 days. How much will she pay if she has: • Medicare A & B, Medicare Supplement 1 • Medicare A & B, Medicare Supplement Core, Health Safety Net
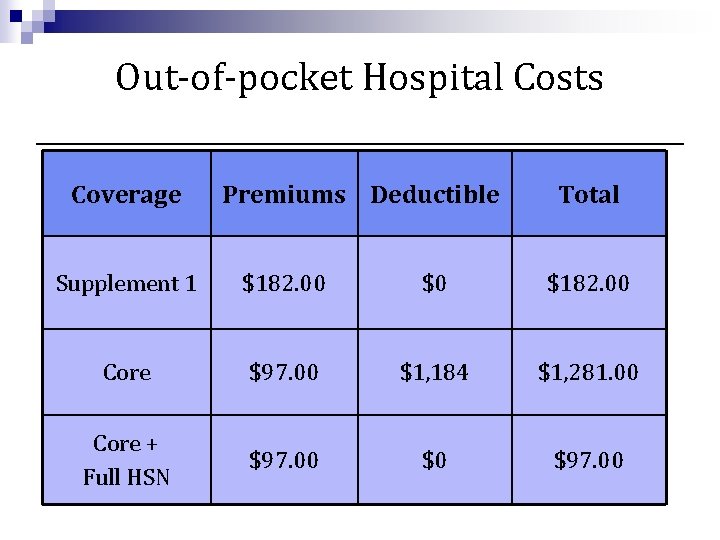
Out-of-pocket Hospital Costs Coverage Premiums Deductible Total Supplement 1 $182. 00 $0 $182. 00 Core $97. 00 $1, 184 $1, 281. 00 Core + Full HSN $97. 00 $0 $97. 00
Word of Caution n If a client is eligible for HSN and is considering downgrading from a Medigap Supplement 1 plan to a Core plan, be sure to advise them on the additional benefits included in Supplement 1 • Foreign travel (only a select number of Core plans cover foreign travel) • SNF coinsurance for days 21 -100 • Part B annual deductible
Health Safety Net and Medications n Health Safety Net can also cover medications • Two general rules for coverage Prescription is being filled at a facility with a pharmacy that can bill HSN (Typically a hospital or community health center) n Prescription is written by a physician at that same facility. n • $3. 65/medication • Deductible is not applicable

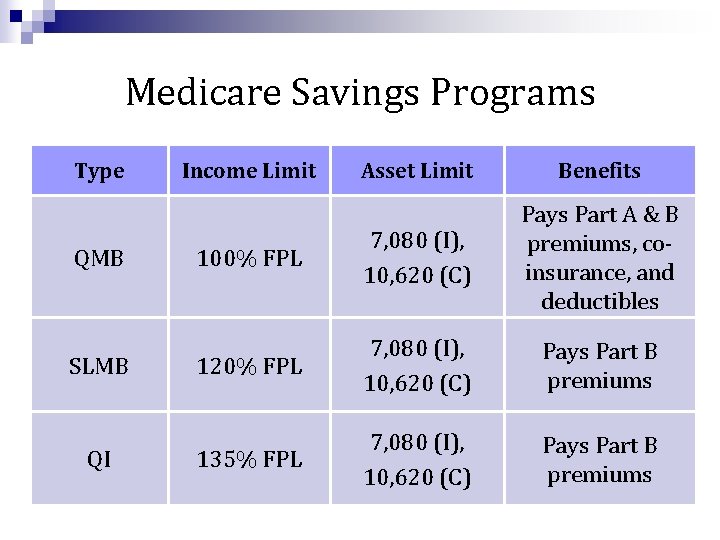
Medicare Savings Programs for Medicare beneficiaries to help pay for some Medicare co-pays and/or premiums: n QMB-Qualified Medicare Beneficiary - Pays Premiums, copayments and deductibles n SLMB-Specified Low-income Medicare Beneficiary - Pays Part B premium only n QI-Qualifying Individual – Pays Part B premium only
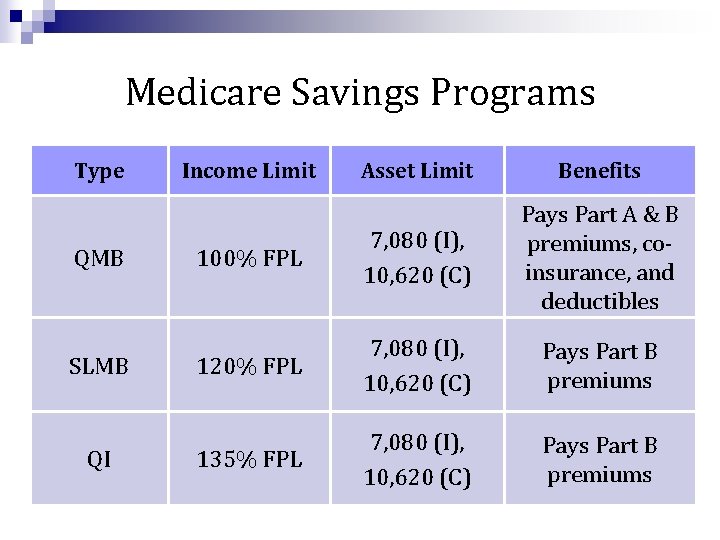
Medicare Savings Programs Type QMB SLMB QI Income Limit Asset Limit Benefits 100% FPL 7, 080 (I), 10, 620 (C) Pays Part A & B premiums, coinsurance, and deductibles 120% FPL 7, 080 (I), 10, 620 (C) Pays Part B premiums 135% FPL 7, 080 (I), 10, 620 (C) Pays Part B premiums
MSP Application Process n To qualify for QMB, must complete a full Mass. Health application n To qualify for SLMB or QI-1, completed either a full Mass. Health application or a Mass. Health Buy-In Application n If an individual qualifies they will also be approved for Full Extra Help with Prescription Costs.
Case Example n n n David has an income of $1, 100 a month and has $5, 000 in the bank. David can complete a Mass. Health Buy-In Application. If approved, • his Part B premium would be subsidized • He would also receive Extra Help, reducing his prescription premium, deductible, and copays.
Commonwealth Care n Health insurance coverage for uninsured adults n Also for those on COBRA or those paying full nongroup premium n Must have income at or below 300% FPL n Premiums and co-pays vary based on income and plan choice Note: Medicare beneficiaries are not eligible
Medicare Appeals, Fraud and Abuse
Medicare Appeals n Beneficiaries have the right to a fair/efficient process for appealing decisions about healthcare payment or services n Expedited appeals available in most situations n Under Part D rules, beneficiaries have a right to a plan “Coverage Determination” concerning coverage or cost of a prescribed drug - this must be issued within 72 hours (24 hours, if expedited) n All steps in the appeal process have specific time frames and other requirements – it is very important to be aware of time limits for appeals
Appealable Events n Medicare denies a request for a health care service, supply, or prescription n Medicare denies payment for health care that the beneficiary has already received n Medicare stops covering services that the beneficiary is already receiving n Medicare pays a different amount than the beneficiary believes it should
The Medicare Advocacy Project n Provides advice/free legal representation to Massachusetts Medicare beneficiaries n Serves elders and persons with disabilities who are enrolled in either Original Medicare or a Medicare Advantage Plan n Offers public education and training on Medicare issues, including updates on changes in the Medicare program
Examples of Problems Referred to MAP § § § § § Durable medical equipment coverage Skilled nursing facility care coverage denials Early hospital discharges Ambulance transportation Physician’s services denials Access to Medicare covered home health care Drug coverage exceptions and appeals Disputed Low Income Subsidy Determinations Premium penalties
Fraud and Abuse in Medicare and Medicaid n Health Care Fraud: Intentional deceptions or misrepresentation a person knowingly makes that could result in improper payment to a provider or unnecessary delivery of services to a beneficiary. n Health Care Abuse: Unintentional incidents or practices of health care providers that are inconsistent with sound business practice, and that result in improper payments by Medicare to a medical provider.
How Medicare Beneficiaries can Protect Themselves n Be aware of bills for services never received n Review medical statements to verify that services being billed for seem appropriate n Never accept unsolicited deliveries or services n Guard Medicare and/or Medicaid card numbers like a credit card number
 Jesus light of the world shine upon us
Jesus light of the world shine upon us Shine jesus shine fill this land with the father's glory
Shine jesus shine fill this land with the father's glory Primary needs and secondary needs
Primary needs and secondary needs Primary needs and secondary needs
Primary needs and secondary needs Henry murray theory
Henry murray theory Strategic gender needs and practical gender needs
Strategic gender needs and practical gender needs Types of needs in esp
Types of needs in esp Similarities between health education and health promotion
Similarities between health education and health promotion Spartan council of elders
Spartan council of elders Peck's theory of ego integrity
Peck's theory of ego integrity 24 thrones in heaven
24 thrones in heaven Bronson intranet
Bronson intranet Church elders training
Church elders training Elders digest
Elders digest Qualifications for elders 1 timothy
Qualifications for elders 1 timothy Qualities of an elder
Qualities of an elder 4 attributes that a health-literate individual needs
4 attributes that a health-literate individual needs Hierarchy of emotions
Hierarchy of emotions Kaiser permanente community health needs assessment
Kaiser permanente community health needs assessment 4 attributes that a health-literate individual needs
4 attributes that a health-literate individual needs Health needs assessment
Health needs assessment A company database needs to store information
A company database needs to store information She lit a candle
She lit a candle Genetický kód
Genetický kód Paper that lets the light shine through
Paper that lets the light shine through Arise and shine communication
Arise and shine communication Shine trial
Shine trial How standard costs are prepared
How standard costs are prepared Naylor shine tables
Naylor shine tables Pribnowův box
Pribnowův box Shine wherever you go
Shine wherever you go Overdriving your headlights means
Overdriving your headlights means Come on everybody stand up stand stamp your feet
Come on everybody stand up stand stamp your feet Overdriving headlights means
Overdriving headlights means Bernadette farrell christ be our light
Bernadette farrell christ be our light Unit 3 rain or shine
Unit 3 rain or shine Alliiteration
Alliiteration Shine certification
Shine certification Rise and shine primary school
Rise and shine primary school Shine bright like a diamond figurative language
Shine bright like a diamond figurative language The crystal stars have just begun to shine
The crystal stars have just begun to shine Shine dalgarnova sekvence
Shine dalgarnova sekvence Virelangue portugais
Virelangue portugais Shine theory ted talk
Shine theory ted talk Let your light shine vbs
Let your light shine vbs Andrew chinn shine among them
Andrew chinn shine among them Rise and shine isaiah
Rise and shine isaiah Wobble hipotezi
Wobble hipotezi Overdriving headlights means
Overdriving headlights means Is the shine of chrome physical or chemical
Is the shine of chrome physical or chemical Is the shine of chrome physical or chemical
Is the shine of chrome physical or chemical Algorithm for if-else statement in c
Algorithm for if-else statement in c Shinewithlight
Shinewithlight Introduction poetry by billy collins
Introduction poetry by billy collins Diseases with vaccines
Diseases with vaccines Shine forth
Shine forth Nanny shine has got fair hair
Nanny shine has got fair hair Happy family
Happy family Shine counselor
Shine counselor Your light will shine when all else fades
Your light will shine when all else fades Inside out
Inside out Polycistronní
Polycistronní Bonide leaf shine and moisture guard
Bonide leaf shine and moisture guard Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Thang điểm glasgow
Thang điểm glasgow Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 101012 bằng
101012 bằng Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số nguyên tố là số gì
Số nguyên tố là số gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Wine label
Wine label