NICHE Nurses Improving Care of Health System Elders
















- Slides: 44

NICHE Nurses Improving Care of Health System Elders The SPICES Tool February, 2011 Rita La. Reau MSN GNP BC Geriatric Clinical Nurse Specialist Bronson Methodist Hospital lareaur@bronsonhg. org
Learning Objectives Upon completion of this program the learner will be able to: • Describe a basic assessment tool for assessment of the geriatric patient. • State demographics related to falls in older adults. • State interventions to prevent a fall.

Older Adult Patients ¨ Older Adult Patients > age 65 ¨ Challenge to health care providers ¨ Numerous & complex diagnoses ¨ Shorter hospital stays ¨ Navigation through hospital process ¨ Potential for cascade of poor outcomes
Hartford Institute ¨ Nurses Improving Care for Health System ¨ ¨ Elders (NICHE) 1992 Sponsored by John A. Hartford Foundation Institute for Geriatric Nursing @ New York University National nursing led initiative: Nationally Recognized Nursing Leaders Currently over 200 NICHE sites Geriatric Resource Nurse (GRN) Model
NICHE Outcomes ¨ Enhance Nursing Knowledge and Skills ¨ ¨ Regarding the Treatment of Common Geriatric Syndromes Increase Patient Satisfaction Decrease Length of Stay Reduce Readmission Rates Reduce Costs Associated with Elder Care.
Evidenced Based Practice ¨ Research based protocols that focus specifically on common geriatric care syndromes ¨ Reflect current research and standards including those developed by The Agency For Health Care Policy Research (AHCPR) ¨ Accessible and usable by bedside nurses
Evidenced Based Resources ¨ http: //nicheprogram. org ¨ http: //www. consultgerirn. org ¨ Hartford Institute Protocols Book ¨ Evidenced Based NICHE Tools: Handout

Geriatric Syndromes ¨ Physical Restraints ¨ Depression ¨ Pressure Ulcers ¨ Incontinence ¨ Sleep Disturbances ¨ Eating/Feeding ¨ Advance Directives ¨ Acute Confusion/ ¨ Pain Management Delirium ¨ Medication Management ¨ Falls ¨ Discharge Planning ¨ Assessing Cognitive Function ¨ Functional Assessment
Bronson NICHE Program ¨ Geriatric Independent Study Modules ¨ NICHE AGEducation Day (8 hours) ¨ Support for Gerontological Nurse Certification
NICHE Clinical Support Geriatric Resource Nurse (GRN) Program ¨ Geriatric Clinical Nurse Specialist (GCNS) ¨ Certified GRNs ¨ GCNS supports GRNs in their new roles – Instruction – Nurse-to-Nurse Consultation – Resource Development – Geriatric Clinical Excellence ¨ Assesses selected geriatric patients in context of geriatric syndromes
GRN Rounding/Consult ¨ Assist staff in assessing, planning, implementing, and evaluating geriatric care according to SPICES Tool ¨ Evaluate and provide feedback to staff regarding SPICES Tool assessments and interventions ¨ Augment staff knowledge and attitudes as they relate to geriatric care.
GRN Rounding/Consult ¨ Disseminate information about geriatric care management through a variety of ways including – Documentation • Progress Notes • Care. Graph ¨ Collaborate with NICHE Council and other resource people as necessary.

SPICES Tool GRN Core Screening Tool – Raises awareness and triggers further evaluation & documentation üSkin Impairment üPoor Nutrition üIncontinence üConfusion üEvidence of Falls üSleep Disturbances
Geriatric Assessment Rounding GRNs ¨ Use SPICES Tool for assessing patients > age 70 – Problems with • Skin – Skin Integrity Score < 18 (Braden Tool) • Problems with Eating – Less than 80% ideal Body Weight – % food eaten < 25% > 6 days (25% > $ days (80+ Yrs) • Incontinence – Stress/Urge/Functional/Diarrhea/Foley
Geriatric Assessment Rounding • Cognition – Mini-Cog, Geriatric Depression Scale (GDS) – Positive Confusion Assessment Method (CAM), Anxiety – Sensory Impairment – Evidence of Dementia, Depression • Evidence of Falls – Confusion, Depression, Elimination, Dizziness, Gender, Antiepileptics, BZD, Mobility/Get Up and Go • Sleep – Difficulty falling/ staying asleep – Sleep promotion interventions

Reasons for Geriatric Resource Nurse Consult Some potential reasons for consult: § Delirium § Dementia § Sitter § Falls § Sleep Problems § Problems with eating § Use of Diversional Activities
Evidence of Falls/Function

What Do These People Have in Common? ¨ Laura Ashley (Fashion Designer) ¨ Robert Atkins (Doctor) ¨ George Washington Carver (Inventor) ¨ Genghis Khan (Royalty) ¨ Robert Peel (Head of State) ¨ Kurt Vonnegut (Author) ¨ William the Conqueror (Royalty) ¨ Malcolm Baldrige (Politician)
Cause of Death: Accidental Fall

Why Do We Need to Be Concerned? ¨ Injuries ¨ Deaths ¨ Associated complications ¨ Costs
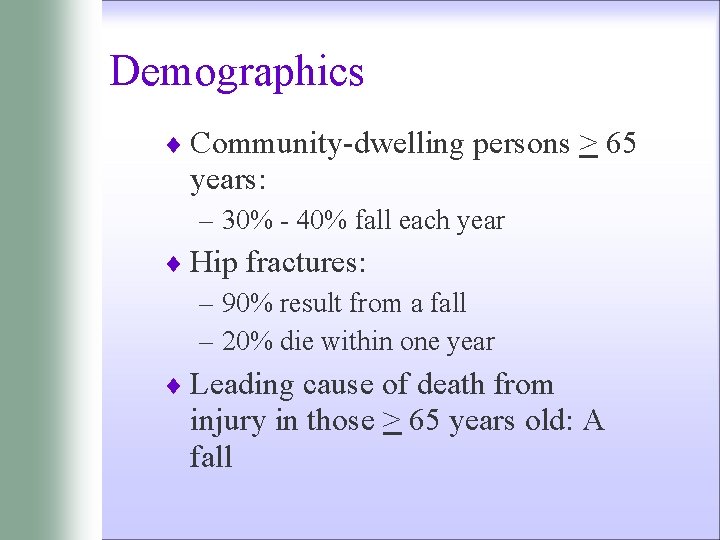
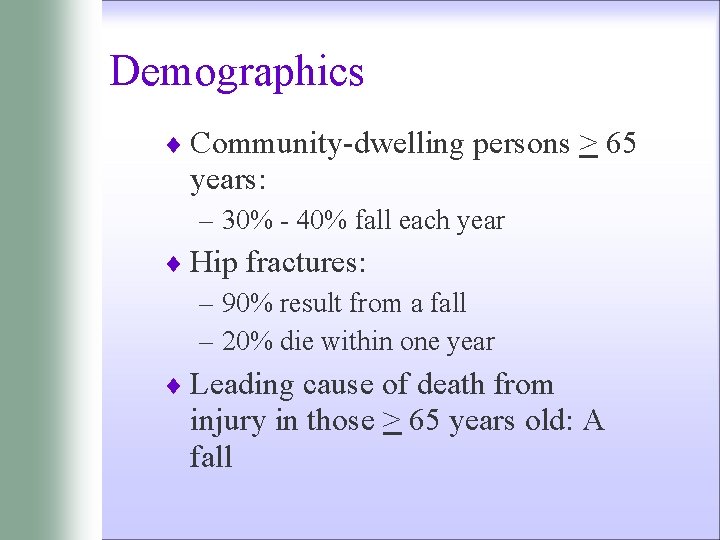
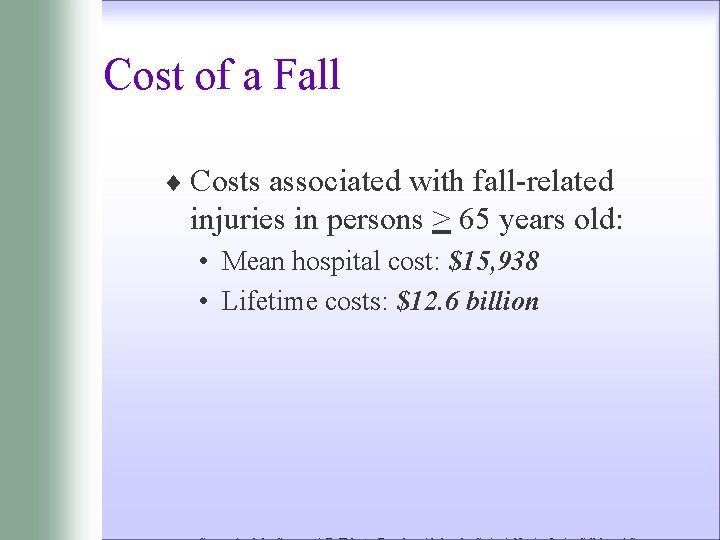
Demographics ¨ Community-dwelling persons > 65 years: – 30% - 40% fall each year ¨ Hip fractures: – 90% result from a fall – 20% die within one year ¨ Leading cause of death from injury in those > 65 years old: A fall

Demographics ¨ Falls are associated with: • Decline in functional status • Development of “fear of falling” • Greater likelihood of nursing home placement
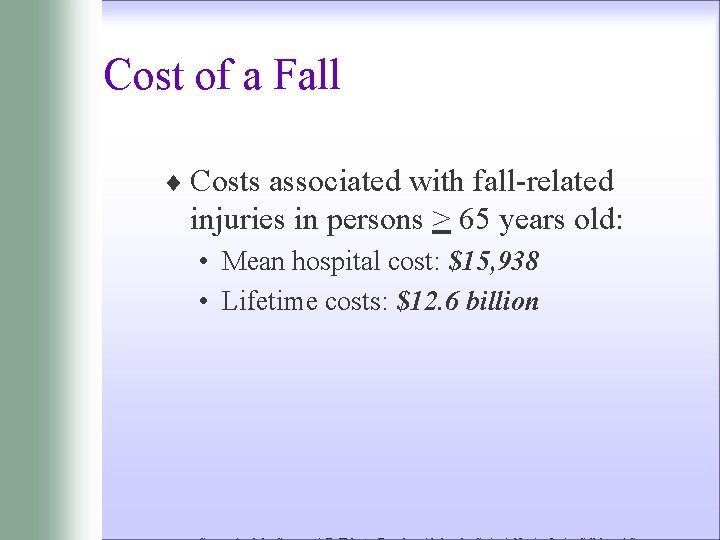
Cost of a Fall ¨ Costs associated with fall-related injuries in persons > 65 years old: • Mean hospital cost: $15, 938 • Lifetime costs: $12. 6 billion
Fall - Defined ¨ Fall: A fall is an unplanned descent to the floor ( or extension of the floor, e. g. , trash can or other equipment) with or without injury to the patient. ¨ All types of falls are to be included whether they result from physiological reasons (fainting) or environmental reasons (slippery floor).
Fall - Defined ¨ Include assisted falls – when a staff member attempts to minimize the impact of the fall. ¨ Included in this definition are patients found lying on the floor unable to account for their situation.
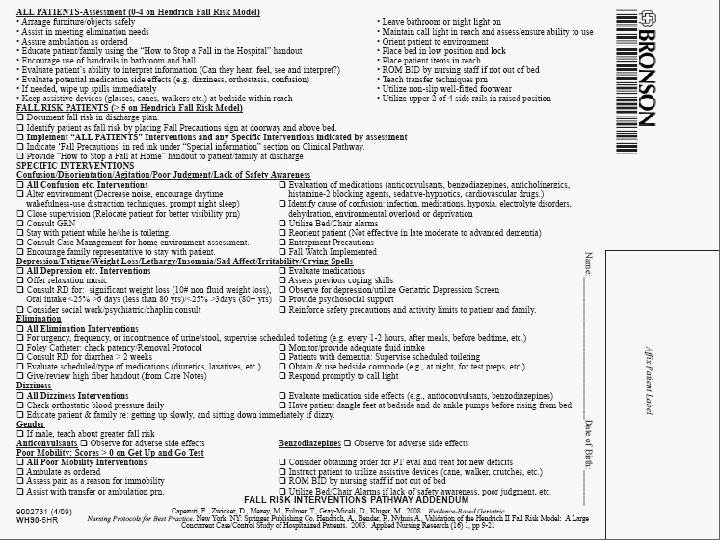
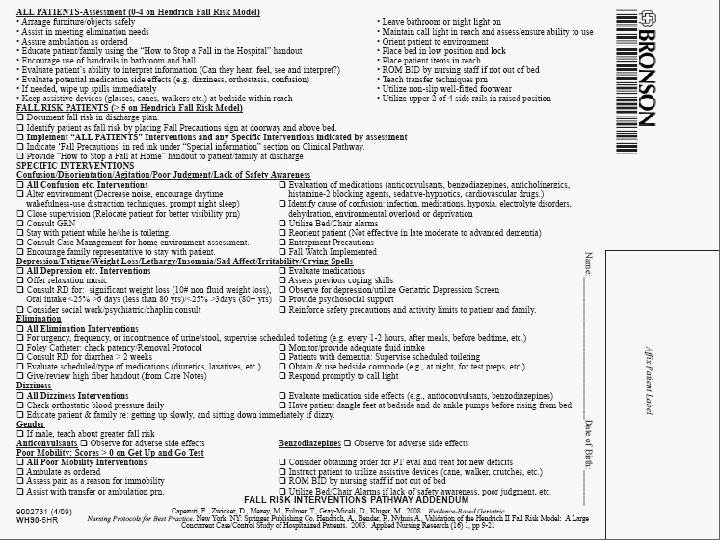
Fall Prevention: All Patients ¨Orient patient to environment ¨Educate patient/family using: – The Fall Prevention Scripting • Use Teach. Back – Prevent Falls in the Hospital handout – Both located on the Nurses and Clinician’s page under Fall Prevention Resource Tools ¨Orient to ‘Call to Stop a Fall’ sign ¨Maintain call light in reach and assess/ensure ability to use.
Fall Prevention: All Patients (1) ¨ Place bed in low position and lock ¨ Utilize non-slip well-fitted footwear ¨ Leave bathroom or night light on ¨ Wipe up spills immediately ¨ Arrange furniture/objects safely ¨ Place patient items in reach

Fall Prevention: All Patients (2) ¨ Teach transfer techniques prn ¨ Assist in meeting elimination needs ¨ Evaluate potential medication side effects ¨ Assure ambulation as ordered ¨ Encourage use of handrails in bathroom and hall
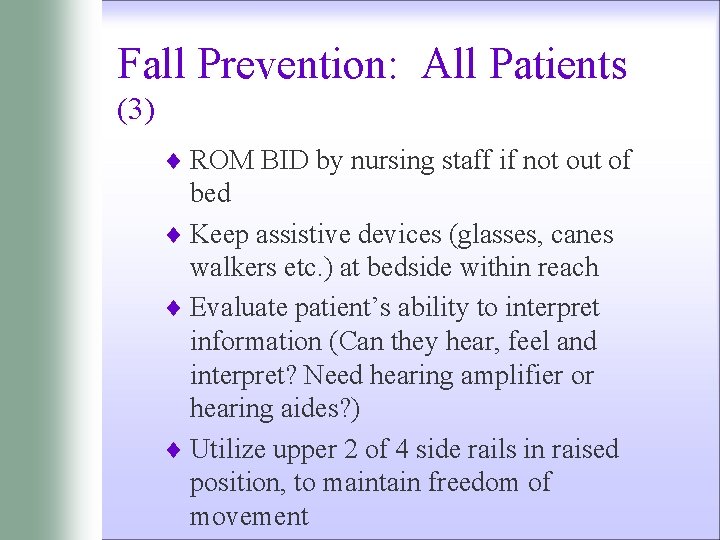
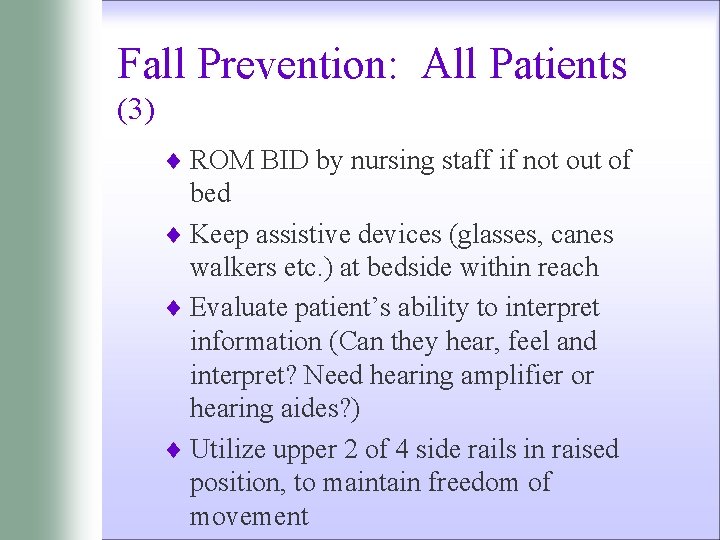
Fall Prevention: All Patients (3) ¨ ROM BID by nursing staff if not out of bed ¨ Keep assistive devices (glasses, canes walkers etc. ) at bedside within reach ¨ Evaluate patient’s ability to interpret information (Can they hear, feel and interpret? Need hearing amplifier or hearing aides? ) ¨ Utilize upper 2 of 4 side rails in raised position, to maintain freedom of movement
Hendrich II Fall Risk Model ¨ Fall Risk Assessment Tool used at Bronson ¨ Identifies patient risk factors that contribute to fall potential. Hendrich, A. , Bender, P. , Nyhuis A. , Validation of the Hendrich II Fall Risk Model: A Large Concurrent Case/Control Study of Hospitalized Patients. 2003. Applied Nursing Research (16) 1, pp 9 -21
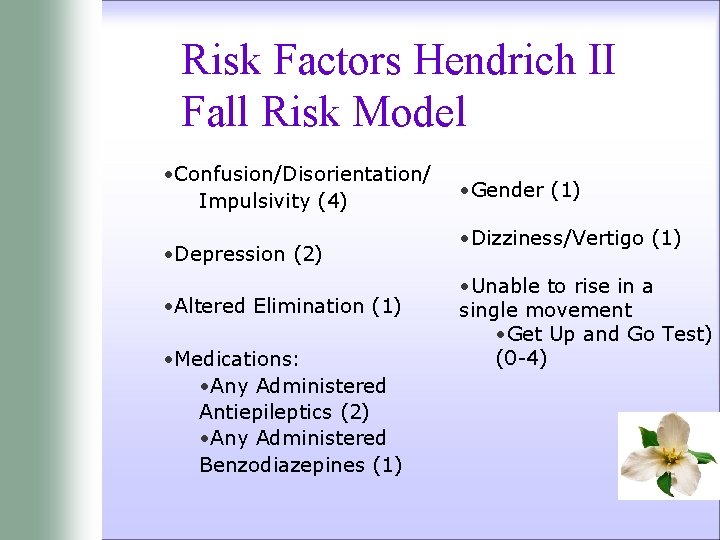
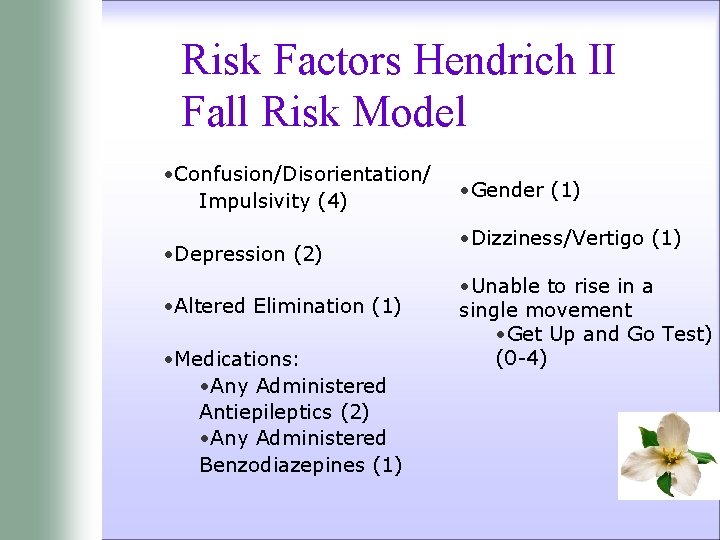
Risk Factors Hendrich II Fall Risk Model • Confusion/Disorientation/ Impulsivity (4) • Depression (2) • Altered Elimination (1) • Medications: • Any Administered Antiepileptics (2) • Any Administered Benzodiazepines (1) • Gender (1) • Dizziness/Vertigo (1) • Unable to rise in a single movement • Get Up and Go Test) (0 -4)



Fall Risk Interventions
Fall Watch Option ¨ ‘Fall Watch’ Option: Reserved for patients who require intensive surveillance. ¨ ‘Fall Watch’ Criteria: • Non-compliance of fall precautions • Impulsive or lack of safety awareness • Discretion of nurse
Fall Watch Option ¨ A magnetic Fall Watch sign is placed on the door frame of any patient identified as high risk. ¨ When passing by that patient room, all hospital employees are to look into the room to observe if the patient is safe.
Fall Watch Option ¨ If safe, employees continue on their way. ¨ If patient is at risk, the employee is to maintain patient safety and put on the call light for assistance. ¨ ‘Fall Watch’ is the responsibility of everyone on the unit to ensure patient safety. ¨ Keep room doors and curtains open.


Community: Interventions to Consider ¨ Cardiac evaluation ¨ Vision improvement ¨ Home safety modifications ¨ Medication reduction ¨ Physical Therapy ¨ Exercise ¨ Tinetti ME, Kumar C. The patient who falls: “It’s always a trade-off. JAMA 2010 Jan 20; 303(3): 258 -66
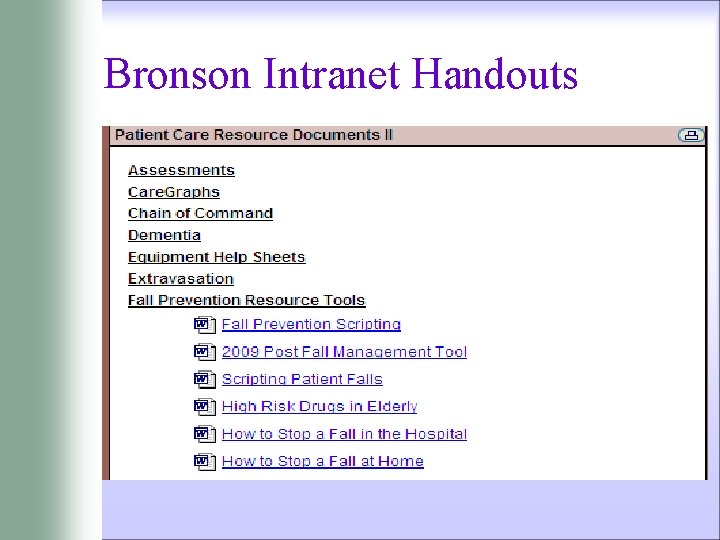
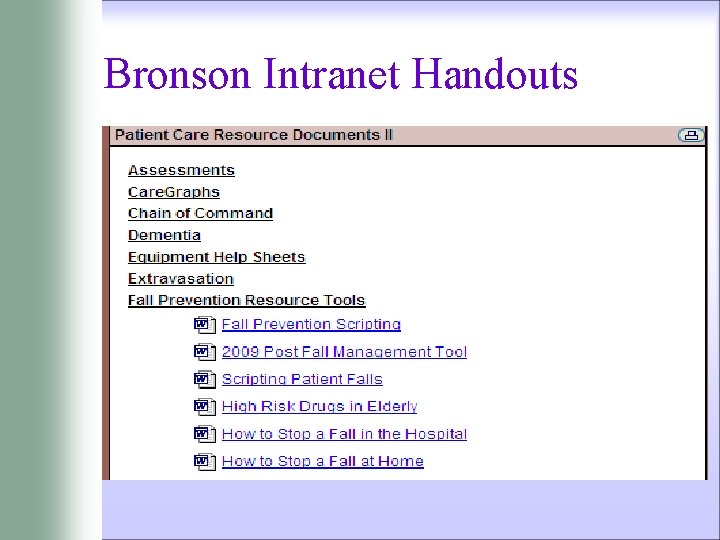
Bronson Intranet Handouts


Questions? NICHE Nurses Improving Care of Health System Elders The SPICES Tool
 Nurses improving care for healthsystem elders
Nurses improving care for healthsystem elders Can a realized niche be larger than a fundamental niche
Can a realized niche be larger than a fundamental niche Niche partitioning
Niche partitioning Improving chronic illness care model
Improving chronic illness care model International society of nurses in cancer care
International society of nurses in cancer care Functions of chn
Functions of chn Primary secondary tertiary health care definition
Primary secondary tertiary health care definition Care value base health and social care
Care value base health and social care Health and social component 3
Health and social component 3 Council of elders sparta
Council of elders sparta Peck's theory of ego integrity
Peck's theory of ego integrity 24 thrones in heaven
24 thrones in heaven Church elders training
Church elders training Certificate for church elders
Certificate for church elders Qualifications for elders 1 timothy
Qualifications for elders 1 timothy Qualities of an elder
Qualities of an elder Service delivery objective
Service delivery objective Secondary care definition
Secondary care definition Introduction to healthcare delivery systems
Introduction to healthcare delivery systems Health care system definition
Health care system definition Ten steps to advancing college reading skills answers
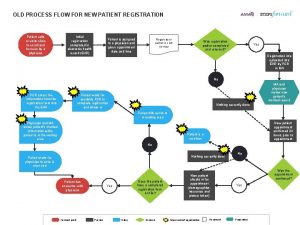
Ten steps to advancing college reading skills answers Improving patient registration process
Improving patient registration process Improving vocabulary skills 4th edition
Improving vocabulary skills 4th edition Condone noun form
Condone noun form Peer inspections a pragmatic view
Peer inspections a pragmatic view Chapter 12 lesson 2 improving your fitness
Chapter 12 lesson 2 improving your fitness Improving software economics set 1
Improving software economics set 1 Service quality and productivity
Service quality and productivity A linear-time heuristic for improving network partitions
A linear-time heuristic for improving network partitions Benefits and difficulties of improving quality
Benefits and difficulties of improving quality Improving own learning and performance examples
Improving own learning and performance examples Gap model of service quality with examples
Gap model of service quality with examples Ten steps to improving college reading skills
Ten steps to improving college reading skills Collins title productivity
Collins title productivity Chapter 13 sentence check 2 answer key
Chapter 13 sentence check 2 answer key A sense of belonging improving student retention
A sense of belonging improving student retention Using assessment data for improving teaching practice
Using assessment data for improving teaching practice Behavioral assessment scale for intercultural competence
Behavioral assessment scale for intercultural competence Refactoring improving the design of existing code
Refactoring improving the design of existing code Writing by
Writing by Improving vocabulary skills chapter 9
Improving vocabulary skills chapter 9 Improving the reliability of commodity operating systems
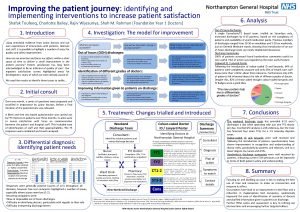
Improving the reliability of commodity operating systems Improving the patient journey
Improving the patient journey Improving student learning one teacher at a time
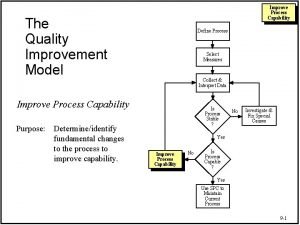
Improving student learning one teacher at a time Improving process capability means;
Improving process capability means;